Portable Low-Field MRI: Democratizing Clinical Neuroscience and Drug Development
Portable low-field magnetic resonance imaging (LF-MRI) is re-emerging as a transformative technology for clinical neuroscience and therapeutic development.
Portable Low-Field MRI: Democratizing Clinical Neuroscience and Drug Development
Abstract
Portable low-field magnetic resonance imaging (LF-MRI) is re-emerging as a transformative technology for clinical neuroscience and therapeutic development. Once limited by lower signal-to-noise ratio, modern LF-MRI systems now integrate advanced hardware design, artificial intelligence-based reconstruction, and refined pulse sequences to deliver clinically viable imaging. This article explores the foundational principles, methodological applications, and optimization strategies for LF-MRI, highlighting its potential to expand neuroimaging access into point-of-care, intensive care, and resource-limited settings. We validate its diagnostic performance against conventional high-field MRI and CT, examining its specific utility for conditions like hydrocephalus, stroke, and neurodegenerative diseases. For researchers and drug development professionals, LF-MRI offers a platform for decentralized clinical trials, longitudinal monitoring, and inclusion of underrepresented populations, ultimately promising to democratize neuroscience research and accelerate therapeutic innovation.
The Resurgence of Low-Field MRI: Principles and Drivers
Portable low-field Magnetic Resonance Imaging (MRI) represents a paradigm shift in medical imaging, moving away from fixed, high-power installations towards accessible, point-of-care diagnostic tools. Within the context of clinical neuroscience research, these systems are redefining the boundaries of where and how brain imaging can be conducted. Portable low-field MRI is broadly defined as MRI technology operating at field strengths below 1.5 Tesla that features physical portability, reduced infrastructure requirements, and significantly lower operational costs compared to conventional high-field systems [1]. The "low-field" designation historically indicated inferior image quality, but modern implementations integrate advanced reconstruction algorithms, refined imaging techniques, and improved hardware design to significantly narrow this performance gap [1].
For neuroscience researchers and drug development professionals, these systems offer unprecedented opportunities to conduct longitudinal studies, monitor therapeutic efficacy in real-time, and expand research into non-traditional settings. The technological evolution of low-field MRI challenges the long-held notion that high field strength is prerequisite for diagnostic utility, instead emphasizing optimized hardware and software integration to deliver clinically relevant image quality [1]. This guide establishes the technical foundations, classifications, and methodological frameworks essential for leveraging portable low-field MRI in neuroscience research applications, with particular focus on field strength parameters that define system capabilities and limitations.
Technical Specifications and Field Strength Classification
The classification of portable low-field MRI systems is primarily governed by their static magnetic field strength (B₀), measured in Tesla (T), which serves as the fundamental determinant of their operational characteristics and potential applications. Field strength directly influences key imaging parameters including signal-to-noise ratio (SNR), contrast mechanisms, and hardware requirements [1]. The historical progression of MRI technology toward higher field strengths was largely driven by the pursuit of greater SNR and spatial resolution; however, contemporary low-field systems demonstrate that field strength is not the sole determinant of image quality, with advanced hardware and computational approaches effectively compensating for lower inherent signal [1].
Table 1: Field Strength Classification of Portable Low-Field MRI Systems
| Classification | Field Strength Range | Representative Systems | Primary Research Applications |
|---|---|---|---|
| Ultra-Low-Field (ULF) | < 0.1 T (e.g., 46-64 mT) | Hyperfine Swoop (0.064 T) | Point-of-care neuroimaging, dementia screening, ARIA-E monitoring, ambulance transport studies [1] [2] [3] |
| Very-Low-Field (VLF) | 0.1 T - 0.5 T | Custom research systems (e.g., 50 mT) | Intraoperative imaging, continuous brain monitoring, technical development studies [4] |
| Mid-Low-Field | 0.5 T - 1.5 T | Siemens MAGNETOM Free.Max (0.55 T) | Musculoskeletal imaging, abdominal imaging, functional MRI feasibility studies [1] [4] |
Table 2: Quantitative Performance Characteristics Across Field Strengths
| Parameter | Ultra-Low-Field (64 mT) | Mid-Low-Field (0.55 T) | Conventional High-Field (1.5 T) |
|---|---|---|---|
| Approximate Cost | Up to 50-60% less than 1.5T [1] | 40-50% of 1.5T system cost [1] | Reference (>$1M per Tesla) [1] |
| Installation Cost Reduction | Up to 70% (no shielding, no reinforced flooring) [1] | Significant savings | Reference |
| Maintenance Cost Reduction | Up to 45% (no cryogenics) [1] | Moderate savings | Reference |
| Typical Spatial Resolution | Limited (e.g., 1.6-5 mm slice thickness) [2] | Moderate to High | High (<1 mm isotropic) |
| Key Advantages | Portability, safety near metals, lower acoustic noise, patient comfort [1] | Balance of performance and accessibility, reduced artifacts [1] | Gold standard for image quality and resolution |
The operational advantages of portable low-field systems extend beyond field strength specifications to encompass practical implementation benefits. These systems typically utilize compact superconducting magnets (e.g., Siemens MAGNETOM Free.Max) or high-performance permanent magnets (e.g., Hyperfine Swoop) that eliminate requirements for cryogenic cooling and substantially reduce electricity consumption [1]. This magnet technology, combined with optimized radiofrequency (RF) coil designs that minimize resistance and thermal noise, enables diagnostic-quality imaging in diverse environments from intensive care units to mobile research vehicles [1]. For neuroscience research, this facilitates study designs previously considered impractical, including home-based imaging, monitoring during therapeutic interventions, and rapid serial assessment of disease progression.
Key Experimental Protocols and Methodologies
Protocol for Brain Morphometry Analysis Using Ultra-Low-Field MRI
The validation of portable low-field MRI for quantitative neuroimaging requires rigorous methodological frameworks to ensure research-grade data quality. Hsu et al. developed an optimized protocol specifically for brain volume analysis using ultra-low-field (ULF) MRI, achieving reliable morphometric measurements with a scan time of approximately 15 minutes [4]. This protocol employs deep learning enhancement methods trained on the optimized acquisition to improve the accuracy and reliability of subsequent volumetric analyses.
Methodology Details:
- Data Acquisition: The protocol utilizes T1-weighted and T2-weighted sequences optimized for ULF systems. Specific parameters are tailored to maximize contrast-to-noise ratio within time constraints.
- Image Enhancement: A dedicated deep learning framework processes acquired ULF images to enhance quality and resolution before morphometric analysis.
- Validation Approach: Processed images are segmented into 33 distinct brain regions using automated parcellation tools. The volumetric measurements from ULF data are statistically compared against reference measurements obtained from high-field (3T) MRI scans to assess concordance.
- Quality Control: The protocol incorporates bootstrapping methods to propagate segmentation uncertainties, providing confidence intervals for volumetric estimates rather than single-point measurements [4].
This methodology demonstrates that with optimized acquisition and computational enhancement, ULF MRI can yield brain morphometric measurements that correlate strongly with high-field references, enabling longitudinal tracking of brain volume changes in clinical research settings where traditional MRI is impractical.
Protocol for Contrast-Enhanced Tumor Imaging
The application of contrast-enhanced imaging in portable low-field MRI systems addresses a critical need in neuro-oncology research, particularly for monitoring treatment response. Altaf et al. established the first documented protocol for post-contrast enhancement in a portable ultra-low-field (pULF) MRI system for brain tumor imaging [2]. This protocol successfully identified tumor presence that was subsequently confirmed histologically, validating the clinical relevance of the methodology.
Methodology Details:
- Patient Preparation: Standard gadolinium-based contrast agent (0.10 mmol/kg) administered intravenously.
- Imaging Sequences: The comprehensive protocol includes T2 Axial, T2 sagittal, T2-weighted FLAIR (TR: 4,000 ms, TE: 166.72 ms), T1 Axial, and DWI + ADC sequences (TR: 1,000 ms, TE: 76.04 ms).
- Spatial Resolution: For T1 and T2 sequences, pixel spacing of 1.6 mm with slice thickness of 5 mm; for DWI and ADC sequences, pixel spacing of 2.4 mm with slice thickness of 5.88 mm.
- Timing: Total scan time of 31 minutes for post-contrast imaging, with a 15-minute interval between high-field and pULF-MRI scanning to account for patient and equipment positioning.
- Validation: Comparative assessment with high-field (1.5T) MRI confirmed lesion detection, though with noted reductions in contrast-to-noise ratio and lesion conspicuity compared to standard MRI [2].
This protocol demonstrates that despite technical challenges, contrast-enhanced neuroimaging is feasible with pULF-MRI systems, potentially enabling brain tumor monitoring in resource-limited research settings where conventional MRI is unavailable.
Protocol for ARIA-E Detection in Alzheimer's Therapy Monitoring
The CARE PMR study established a specialized protocol for detecting Amyloid-Related Imaging Abnormalities with Edema (ARIA-E) in patients receiving amyloid-targeting therapies for Alzheimer's disease [3]. This application highlights the particular value of portable MRI for frequent monitoring requirements in clinical trials.
Methodology Details:
- Study Design: Multi-site prospective trial assessing clinical utility and workflow benefits of portable MRI for ARIA detection.
- Imaging Protocol: Standardized acquisition protocol optimized for edema detection on ultra-low-field system.
- Analysis Method: Images interpreted by trained physicians with comparison to high-field MRI reference standard.
- Performance Metrics: Demonstrated 100% sensitivity for detecting mild to moderate ARIA-E, supporting use as triage tool despite some cases still requiring high-field MRI for comprehensive evaluation [3].
This protocol validates portable low-field MRI as an effective screening tool for treatment-related adverse events, facilitating the practical implementation of appropriate monitoring guidelines for novel Alzheimer's therapies in both clinical and research settings.
The Researcher's Toolkit: Essential Methods and Reagents
Table 3: Essential Research Reagent Solutions for Portable Low-Field MRI Studies
| Reagent/Resource | Function/Application | Implementation Example |
|---|---|---|
| Gadolinium Chelates | Contrast enhancement for lesion characterization | 0.10 mmol/kg for tumor imaging at 64 mT; effective across field strengths from 0.15 T to 1.5 T [2] |
| Deep Learning Models (LoHiResGAN) | Image quality enhancement through low-to-high-field translation | Improves SNR and spatial resolution; enables automated brain morphometry on ULF data [5] |
| Segmentation Algorithms (SynthSeg+) | Automated volumetric brain analysis | Provides robust segmentation across various MRI resolutions and contrasts; enables quantitative studies [5] |
| Superparamagnetic Iron Oxide Particles | Alternative contrast mechanism | "Negative enhancers" with strong susceptibility effects; potential for cellular tracking in neuroscience research [2] |
| Macromolecular Gd-based Agents | Advanced contrast for angiogenesis imaging | Molecular weight range 64-17,500 d; investigational for tumor characterization [2] |
The research toolkit for portable low-field MRI extends beyond traditional contrast agents to encompass computational resources that are equally critical for generating research-grade data. Deep learning models specifically address the inherent signal-to-noise limitations of low-field systems through image-to-image translation techniques that synthesize high-field-like images from low-field acquisitions [5]. The LoHiResGAN architecture, which incorporates ResNet components and structural similarity index measure (SSIM) loss functions, has demonstrated superior performance in generating synthetic high-field images that preserve essential morphological information while significantly improving quantitative measurement consistency across diverse brain regions [5]. These computational tools, combined with robust segmentation algorithms like SynthSeg+ that maintain performance across varying image contrasts and resolutions, form an essential component of the modern low-field MRI research pipeline [5].
Emerging Applications in Clinical Neuroscience Research
Portable low-field MRI systems are enabling novel research paradigms across multiple neuroscience domains by removing traditional barriers to MRI access. In neurodegenerative disease research, these systems are being deployed for dementia screening in outpatient clinics and for monitoring treatment safety in Alzheimer's clinical trials [6] [3]. The ACE-AD study at the University of Kansas Alzheimer's Disease Research Center exemplifies this approach, combining portable MRI with cognitive testing and blood biomarkers in a single nurse-led clinic visit to expedite diagnosis and improve accessibility for rural and underserved populations [6].
In neuro-oncology research, portable systems demonstrate feasibility for both diagnostic applications and treatment monitoring. The documented case of contrast-enhanced tumor imaging at 0.064 T establishes a foundation for future studies investigating tumor progression and treatment response in settings where conventional MRI is unavailable [2]. Additionally, technical innovations presented at the 2025 ISMRM conference highlight emerging capabilities including functional MRI at 0.55 T, which demonstrates feasibility despite traditionally being considered a high-field application [4]. This expansion of functional imaging to low-field systems could potentially enable task-based fMRI studies in naturalistic environments beyond the scanner room, opening new avenues for cognitive neuroscience investigation.
The methodological frameworks and technical specifications detailed in this guide provide neuroscience researchers with the foundational knowledge required to strategically implement portable low-field MRI across diverse research scenarios. As the technology continues to evolve through hardware refinements and computational advances, these systems are positioned to fundamentally transform the scope and accessibility of neuroimaging research, particularly for longitudinal studies, point-of-care applications, and research involving special populations where conventional MRI presents logistical challenges.
Magnetic resonance imaging (MRI) at low magnetic field strengths (conventionally defined as <0.5 T, and more recently encompassing systems down to 0.01 T) is experiencing a remarkable renaissance in clinical neuroscience research [1] [7]. This renewed interest challenges the long-held notion that high magnetic field strength is inherently superior, driven instead by the distinct advantages of portable, low-cost systems that can expand access to neuroimaging [8] [9]. For researchers and drug development professionals, understanding the core physical principles of signal-to-noise ratio (SNR), contrast-to-noise ratio (CNR), and relaxometry at low fields is paramount to leveraging this technology effectively. The fundamental trade-off in low-field MRI is the reduced signal strength, which must be balanced against benefits including reduced susceptibility artifacts near metallic hardware or air-tissue interfaces, lower specific absorption rate (SAR) enhancing patient safety, and significantly lower operational costs and infrastructure demands [1] [10]. These characteristics make low-field systems particularly valuable for point-of-care imaging, monitoring neurological conditions in intensive care settings, and conducting large-scale population studies in resource-limited environments, thereby addressing critical gaps in global healthcare accessibility [8] [11].
Fundamental Physics of Signal and Contrast at Low Field
Signal-to-Noise Ratio (SNR) Fundamentals
The signal-to-noise ratio represents the most critical determinant of image quality in MRI, quantifying the strength of the desired signal relative to background noise. The fundamental challenge of low-field MRI lies in the physics of signal generation: the net magnetization vector (M0), which forms the basis of the MR signal, is directly proportional to the static magnetic field strength (B0) [1]. This relationship establishes a fundamental field strength dependency for the MR signal. However, the complete theoretical framework for SNR is more nuanced, incorporating both signal and noise contributions from the sample and radiofrequency (RF) coil.
The voltage induced in an RF receiver coil by the precessing magnetization is governed by Faraday's Law of Induction, which states that the induced electromotive force is proportional to the rate of change of magnetic flux. Since the precession frequency (Larmor frequency) increases linearly with B0, the overall MR signal exhibits a quadratic dependence on the static magnetic field (Signal ∝ B₀²) [10]. The noise in MRI systems originates primarily from Johnson-Nyquist noise in the conductive components of the receiver coil and the subject being imaged. In the low-field regime (typically below 0.1 T), where the noise from the sample is comparable to or less than the coil noise, the overall SNR demonstrates a dependence of approximately SNR ∝ B₀^(3/2) [10] [7]. At ultra-low fields (<0.01 T), where coil noise dominates, the relationship may approach SNR ∝ B₀ [7].
Table 1: SNR Dependence on Magnetic Field Strength Across Different Regimes
| Field Strength Regime | Theoretical SNR Dependence | Dominant Noise Source | Practical Implications |
|---|---|---|---|
| Ultra-Low-Field (<0.01 T) | ∝ B₀ | Coil resistance | Maximum benefit from coil optimization; longest acquisition times |
| Very-Low-Field (0.01-0.1 T) | ∝ B₀^(3/2) | Mixed (Coil & Sample) | Balanced hardware/software optimization needed |
| Mid-Field (0.1-1 T) | ∝ B₀^(7/4) to ∝ B₀² | Sample dielectric losses | Closest performance to high-field; most clinical low-field systems |
Contrast-to-Noise Ratio (CNR) and Relaxometry
While SNR measures overall signal quality, contrast-to-noise ratio (CNR) defines the ability to distinguish between different tissue types. CNR is calculated as the difference in signal intensity between two tissues divided by the background noise [12]. At low field strengths, the longitudinal (T1) and transverse (T2) relaxation times of tissues exhibit distinct behavior that directly impacts image contrast.
T1 relaxation times demonstrate a strong field dependence, with values decreasing as field strength decreases [10]. This phenomenon occurs because the dominant relaxation mechanisms at lower fields are more efficient. For example, the T1 of gray matter decreases from approximately 1500 ms at 3 T to around 600 ms at 0.1 T [10]. This reduction has significant implications for sequence parameters: shorter repetition times (TR) can be used in T1-weighted sequences without saturating the signal, potentially reducing scan times.
In contrast, T2 and T2* relaxation times increase at lower field strengths due to reduced susceptibility effects and diminished influence of diffusion through intrinsic field inhomogeneities [10]. This T2 prolongation enhances signal in T2-weighted sequences and reduces artifacts near tissue-air interfaces or metallic implants, representing a key advantage for postoperative imaging and musculoskeletal applications [1].
Table 2: Field Dependence of Relaxation Parameters for Brain Tissues
| Tissue Type | Relaxation Parameter | Field Dependence Model | Approximate Value at 0.055 T |
|---|---|---|---|
| Gray Matter | T1 | T1(ms) = 1160 × (γB₀)^(0.376) [10] | ~650 ms |
| T2* | T2*(ms) = 90 × e^(-0.142×B₀) [10] | ~85 ms | |
| White Matter | T1 | T1(ms) = 710 × (γB₀)^(0.382) [10] | ~450 ms |
| T2* | T2*(ms) = 64 × e^(-0.132×B₀) [10] | ~62 ms | |
| Blood | T1 | T1(ms) = 3350 × (γB₀)^(0.340) [10] | ~1200 ms |
The field dependence of relaxation times means that the CNR efficiency (CNR per unit time) follows different optimization rules than at high field. T1-weighted CNR between gray and white matter is generally reduced at low field, while T2-weighted CNR may be preserved or even enhanced in certain scenarios [10]. Proton-density weighted imaging often provides excellent CNR at low fields due to the reduced T1 weighting and lower power requirements for RF pulses.
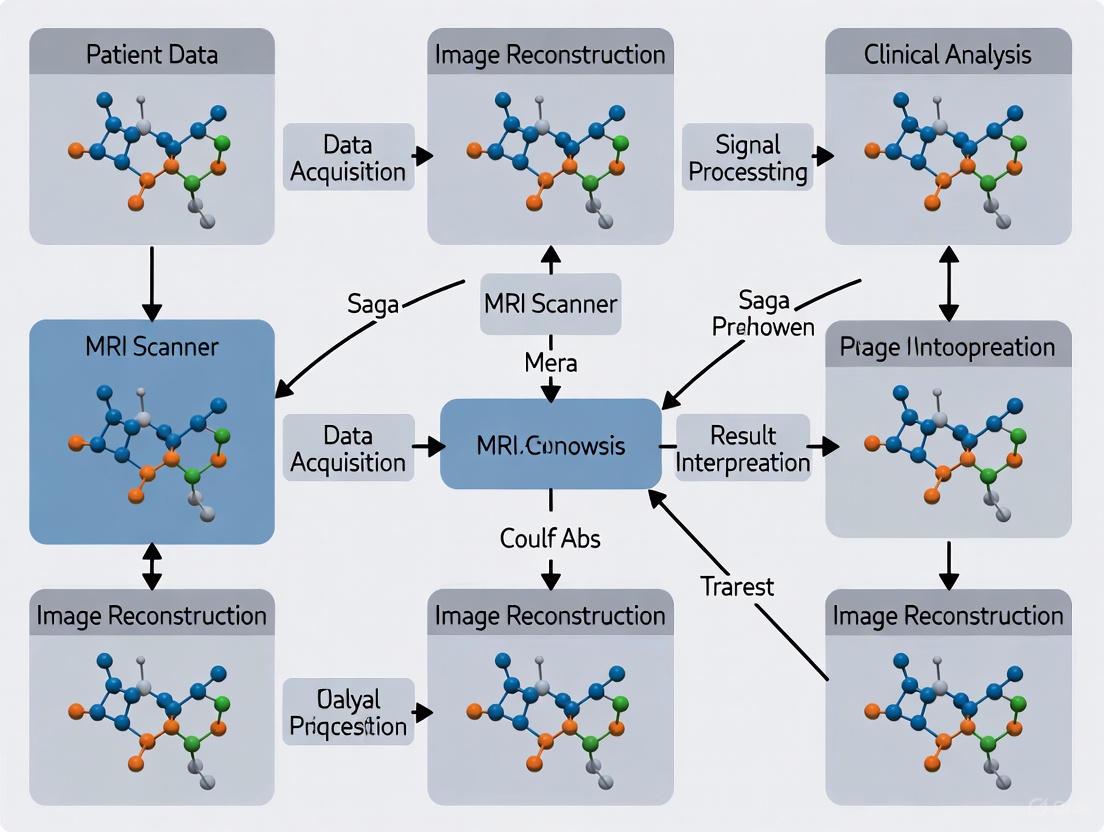
Figure 1: Fundamental Relationships Governing SNR and CNR at Low Magnetic Fields. The diagram illustrates how static magnetic field strength (B₀) influences signal generation, noise contributions, and relaxation parameters that collectively determine the resulting SNR and CNR in low-field MRI.
Technical Strategies for SNR Enhancement at Low Field
Hardware Optimization Approaches
Modern low-field MRI systems incorporate sophisticated hardware designs to mitigate the inherent SNR limitations. Permanent magnet technology has advanced significantly, with contemporary systems utilizing samarium-cobalt (SmCo) or neodymium-iron-boron (NdFeB) magnets offering improved temperature stability and field homogeneity [9] [11]. These magnets enable compact designs with weights ranging from 350-750 kg for brain-dedicated systems, making them truly portable [9] [11].
RF coil design is particularly critical at low field, where the reduced resonance frequency places the system in the quasi-static regime, altering the traditional noise contributions. Several innovative approaches have been implemented:
- Superconducting RF coils: Operating at high or low temperatures to minimize resistance and thermal noise, thereby improving SNR [1].
- Multimodal surface coils: Leveraging multiple resonant modes to increase RF field efficiency and enhance image quality [1].
- Optimized coil arrays: Multi-channel arrays designed specifically for the lower Larmor frequencies encountered at low field [13].
Gradient system performance has also seen substantial improvements, with modern low-field systems incorporating optimized gradient coils that provide sufficient strength and switching rates for clinical imaging while maintaining low acoustic noise and power consumption [11].
Software and Reconstruction Techniques
Advanced software solutions play a pivotal role in compensating for the reduced SNR at low field strengths, often leveraging developments originally made for high-field systems:
- Advanced k-space sampling: Non-Cartesian trajectories such as spiral and radial sampling provide more efficient k-space coverage and inherent motion robustness [13]. These approaches increase the sampling duty cycle (T_sampling in Equation 2), directly improving SNR efficiency.
- Parallel imaging and compressed sensing: These techniques enable accelerated acquisitions by undersampling k-space, allowing for either shorter scan times or increased averages within the same timeframe to boost SNR [13].
- Deep learning reconstruction: Convolutional neural networks (CNNs) and other deep learning architectures can effectively denoise images, suppress artifacts, and even enhance resolution beyond the intrinsic acquisition limits [13] [11]. These methods can learn complex mappings from noisy low-field images to their cleaner high-field counterparts when trained on paired datasets.
- Electromagnetic interference (EMI) cancellation: Operating without RF shielding requires sophisticated EMI cancellation algorithms. Deep learning approaches have demonstrated remarkable success in predicting and removing dynamically changing EMI signals captured by strategically placed reference coils [9] [13].
Table 3: Software Solutions for SNR Enhancement in Low-Field MRI
| Technique Category | Specific Methods | Key Principle | Impact on SNR Efficiency |
|---|---|---|---|
| Acquisition Strategies | Radial/Spiral Trajectories | Efficient k-space coverage; oversampling center | Increases sampling duty cycle |
| Balanced Steady-State Free Precession (bSSFP) | Optimal signal for given TR | Maximizes signal per unit time | |
| Reconstruction Methods | Parallel Imaging (SENSE, GRAPPA) | k-space undersampling with multiple coils | Enables more averages in fixed time |
| Compressed Sensing | Leveraging image sparsity | Reduces required sampling | |
| Post-Processing | Deep Learning Denoising | Learned noise patterns from training data | Direct noise suppression |
| Super-Resolution Networks | Synthesizing high-frequency information | Enhanced apparent resolution | |
| EMI Cancellation | Adaptive Filtering | Reference-based interference modeling | Reduces structured noise |
Experimental Protocols for Low-Field MRI Research
SNR Quantification Methodology
Accurate quantification of SNR is essential for validating system performance and optimizing sequences. The recommended methodology involves:
- Dual-Acquisition Technique: Acquire two identical datasets with identical parameters and reconstruct them separately [12]. This approach provides the most reliable SNR measurement in clinical imaging scenarios.
- Region of Interest (ROI) Analysis: Place uniform ROIs in background air and in homogeneous tissue regions (e.g., central white matter).
- SNR Calculation: Calculate SNR as SNR = Stissue / σbackground, where Stissue is the mean signal intensity in tissue and σbackground is the standard deviation in background noise [12].
- Correlation Analysis: For enhanced precision, use the correlation function of two independent acquisitions to quantify SNR, which provides robustness against structured noise [12].
For systems with array coils, combine ROIs from multiple elements to ensure comprehensive noise characterization. When employing parallel imaging, account for the spatially varying noise amplification (g-factor) in SNR calculations.
Protocol Optimization for Neuroscience Applications
Implementing clinical neuroimaging protocols at low field requires careful parameter adjustment to account for the altered relaxation times and contrast mechanisms:
- T1-Weighted Imaging: Utilize the shorter T1 values to reduce TR and increase slice coverage within a given time. While T1-weighted CNR is generally reduced at low field, optimized protocols can still provide diagnostically useful images [14] [11].
- T2-Weighted Imaging: Leverage the prolonged T2 times to employ longer echo times (TE) while maintaining signal. T2-weighted images often provide superior CNR compared to T1-weighted images at low field [14].
- Fluid-Attenuated Inversion Recovery (FLAIR): Adjust inversion times (TI) based on the field-dependent T1 values of cerebrospinal fluid (CSF) and brain tissue. FLAIR-like imaging has been successfully implemented at 0.055 T for detecting pathologies like white matter lesions [9].
- Diffusion-Weighted Imaging (DWI): The reduced T2 weighting at low field can be advantageous for DWI, allowing for stronger diffusion weighting. Isotropic DWI has been demonstrated at 0.055 T for stroke detection [9].
For volumetric analysis in neuroscience research, the "TomoBrain" approach has shown promise, combining orthogonal imaging directions (axial, coronal, and sagittal) for T2-weighted images to form higher resolution image volumes suitable for automated segmentation of gray matter, white matter, and hippocampal volumes [14].
Figure 2: Comprehensive Experimental Workflow for Low-Field MRI in Neuroscience Research. The diagram outlines the key stages in designing and executing low-field MRI experiments, from hardware preparation through data acquisition to advanced reconstruction and quantitative analysis.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Tools for Low-Field MRI Development and Validation
| Tool Category | Specific Examples | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Phantom Materials | NiCl₂-doped agarose gels | Mimicking tissue T1/T2 values | Concentration optimization for field strength |
| Structured resolution phantoms | Spatial resolution assessment | Must account for lower resolution limits | |
| EMI Cancellation Systems | Deep learning models (U-Net, CNN) | Predicting and removing EMI | Requires training on paired shielded/unshielded data |
| Reference sensor arrays | Capturing environmental EMI | Strategic placement around scanner | |
| Image Reconstruction Software | Compressed sensing libraries | Accelerated acquisition reconstruction | Parameter optimization for low SNR regime |
| Parallel imaging toolboxes (SENSE, GRAPPA) | Accelerated parallel imaging | Coil sensitivity mapping at low field | |
| Quantitative Analysis Tools | Automated segmentation (SynthSeg, FreeSurfer) | Brain volume quantification | Validation against high-field references |
| SNR/CNR calculation scripts | Objective image quality assessment | Implementation of dual-acquisition method | |
| Magnet Design Components | Samarium-Cobalt (SmCo) permanent magnets | B₀ field generation with thermal stability | Preferred over NdFeB for temperature stability |
| Passive shimming components | B₀ homogeneity optimization | Ferromagnetic pieces for field correction |
The physics of SNR, CNR, and relaxometry at low magnetic fields presents both challenges and unique opportunities for clinical neuroscience research. While the reduced polarization at low field strengths inherently limits SNR, this can be effectively mitigated through sophisticated hardware design, optimized pulse sequences, and advanced reconstruction algorithms. The distinct relaxation properties at low field create contrast mechanisms that differ from conventional high-field MRI, requiring specialized protocol development but offering advantages for specific applications. For drug development professionals and neuroscientists, low-field portable MRI systems represent a transformative technology that can democratize access to neuroimaging, enable longitudinal monitoring at point-of-care, and facilitate large-scale population studies. As hardware miniaturization and artificial intelligence-driven reconstruction continue to advance, the performance gap between low-field and high-field systems will further narrow, solidifying the role of portable MRI as an indispensable tool in clinical neuroscience research.
Magnetic resonance imaging (MRI) has undergone a significant pendulum swing in technological emphasis over its development history. The narrative of MRI field strength is characterized by an early dominance of low-field systems, a subsequent industry-wide shift toward high-field machines driven by signal-to-noise ratio (SNR) advantages, and a contemporary renaissance of low-field technology fueled by engineering innovations and specific clinical needs. This evolution is particularly relevant within clinical neuroscience research, where the portability, cost-effectiveness, and unique imaging characteristics of modern low-field systems are opening new possibilities for study design and patient access. Understanding this historical trajectory provides essential context for evaluating the current and future role of portable low-field MRI in neuroscientific investigation and therapeutic development.
The Early Dominance of Low-Field MRI Systems
Technological Foundations of Early MRI
The initial development and commercialization of MRI technology in the 1980s were dominated by low-field systems, broadly defined as those operating at field strengths below 1.5 Tesla (T) [1]. These early scanners predominantly utilized resistive magnets or permanent magnets [1] [15]. Resistive magnets, while inexpensive and relatively straightforward to manufacture, were constrained to maximum field strengths of approximately 0.28 T and consumed substantial electrical power during operation [1]. Permanent magnets emerged as an alternative technology, offering the advantage of passive operation without continuous electrical current and enabling open scanner designs that improved patient comfort [1]. However, these systems were limited to approximately 0.4 T and exhibited sensitivity to temperature fluctuations, lacked dynamic shimming capabilities, and provided limited gradient performance [1].
Table 1: Characteristics of Early Low-Field MRI Magnet Technologies
| Magnet Type | Maximum Field Strength | Key Advantages | Primary Limitations |
|---|---|---|---|
| Resistive | ~0.28 T | Low manufacturing cost, relative ease of production | High power consumption, limited field strength |
| Permanent | ~0.4 T | Passive operation (no electrical current), open design possibilities | Temperature sensitivity, limited shimming and gradient performance |
Despite these technological constraints, low-field systems established MRI as a vital clinical tool during this formative period, providing unparalleled soft-tissue contrast without ionizing radiation.
The Shift Toward High-Field Systems
The 1980s and 1990s witnessed a decisive transition in the MRI market toward high-field systems. The introduction of the first 1.5T scanners in 1985 marked a turning point [15]. The subsequent decades saw a widening "citation gap" as scientific and clinical literature increasingly focused on high-field applications [15]. This shift was driven by a fundamental physical principle: SNR is directly proportional to the strength and homogeneity of the static magnetic field [1]. Higher field strengths yielded superior SNR, which translated to improved spatial resolution, reduced scan times, and enhanced contrast sensitivity [15] [16]. The development of superconducting magnets was instrumental in this transition, enabling stable high field strengths and superior image quality, albeit with substantial infrastructure demands including cryogenic cooling using liquid helium [1] [16]. Consequently, low-field MRI was largely relegated to niche applications or cost-sensitive environments, while 1.5T and later 3.0T systems became the clinical standard in high-income countries [1] [15].
The Present-Day Technological Renaissance
Drivers of the Low-Field Revival
The renewed academic, industry, and philanthropic interest in low-field MRI since the late 2010s stems from converging factors that address the limitations of both historical low-field and contemporary high-field systems.
Economic Accessibility: The high cost of high-field MRI represents a significant barrier to global healthcare access. The capital cost of a high-field system has been estimated to approach $1 million USD per tesla of field strength [1] [15]. In contrast, a modern 0.55T system may cost only 40-50% as much as a standard 1.5T scanner [1]. Additional savings are realized through reduced installation costs (up to 70% less), diminished infrastructure requirements (no reinforced flooring or copper shielding), and lower ongoing maintenance expenses (up to 45% less) [1]. This economic proposition is crucial for expanding access in low- and middle-income countries (LMICs) and underserved rural areas [15].
Technological Innovations: Advances in hardware and software have effectively mitigated the traditional image quality limitations of low-field MRI. Improved magnet designs, sophisticated gradient systems, and optimized radiofrequency (RF) coils have enhanced baseline performance [1] [15]. Furthermore, artificial intelligence (AI) and deep learning reconstruction techniques now compensate for lower intrinsic SNR by denoising images and reducing acquisition times, significantly narrowing the performance gap with high-field systems for specific diagnostic tasks [1] [15].
Clinical and Operational Advantages: Modern low-field systems offer unique benefits aligned with evolving clinical needs. Their portability enables point-of-care imaging in intensive care units, emergency departments, and even ambulances [1]. They demonstrate reduced susceptibility artifacts, proving particularly valuable for imaging patients with metallic implants [1]. Enhanced patient comfort through quieter operation and more open designs improves tolerance and reduces scan termination rates [1].
Key Modern Low-Field Systems and Specifications
The current market landscape reflects this renaissance, with several low-field systems receiving FDA clearance and demonstrating clinical utility.
Table 2: Representative Modern Low-Field MRI Systems
| System Name | Field Strength | Primary Application | Key Technological Features |
|---|---|---|---|
| Hyperfine Swoop | 0.064 T | Portable head imaging | First FDA-cleared portable MRI; utilizes permanent magnets; can be integrated into mobile platforms [1] [15] |
| Siemens MAGNETOM Free.Max | 0.55 T | General purpose | Compact superconducting magnet; demonstrates advanced engineering for high-performance low-field imaging [1] [15] |
| Synaptive Evry | 0.5 T | Intraoperative | Designed for surgical guidance; integrates with operative workflow [15] |
| Aspect Embrace | 1.0 T | Neonatal | Tailored for infant imaging; addresses specific pediatric clinical needs [15] |
These systems exemplify the trend toward application-specific design, moving beyond the one-size-fits-all approach of earlier MRI generations.
Experimental Protocols and Validation in Clinical Neuroscience
Methodology for Diagnostic Accuracy Studies
Rigorous validation against clinical reference standards is essential for establishing low-field MRI in neuroscience research. The following protocol, derived from a hydrocephalus diagnostic study, provides a template for such validation [17].
- Patient Cohort: Recruit a sufficient sample size (e.g., N=130) with suspected pathology (e.g., hydrocephalus) to ensure statistical power [17].
- Multimodal Imaging: Each participant undergoes imaging with three modalities: the experimental mobile low-field (ML) MRI, conventional CT, and high-field 3.0T MRI as a reference standard [17].
- Image Analysis: Acquire key quantitative ventricular measurements from all three imaging modalities. Examples include ventricular volume, Evan's index (ratio of the maximum width of the frontal horns of the lateral ventricles to the maximal internal diameter of the skull), and callosal angle [17].
- Statistical Validation: Calculate Intraclass Correlation Coefficients (ICC) to assess agreement between ML MRI and reference standards. ICC values >0.95 indicate excellent reliability [17]. Perform Bland-Altman analysis to evaluate measurement bias and limits of agreement. Construct Receiver Operating Characteristic (ROC) curves to determine diagnostic accuracy, reporting Area Under the Curve (AUC), sensitivity, specificity, and overall accuracy [17].
Quantitative Imaging Biomarker Acquisition
In neuroscience, quantitative MRI (qMRI) provides objective biomarkers for disease tracking. Low-field systems must demonstrate capability in acquiring these metrics.
- T1/T2 Relaxometry: Measures longitudinal (T1) and transverse (T2) relaxation times in milliseconds (ms), sensitive to tissue composition like myelin content [18]. Acquisition involves inversion-recovery (IR) or variable flip angle (VFA) sequences for T1, and multi-echo spin echo (MESE) for T2, typically requiring 4-8 minutes [18].
- Diffusion Metrics: Apparent Diffusion Coefficient (ADC, mm²/s) and Fractional Anisotropy (FA) derived from diffusion-weighted imaging (DWI) sequences, sensitive to microstructural integrity and white matter organization [18].
- Quantitative Susceptibility Mapping (QSM): Maps magnetic susceptibility (χ, ppm) to quantify brain iron deposition in neurodegenerative diseases, utilizing multi-echo gradient echo sequences [19].
- Volumetry: Regional brain volumes (cm³) and cortical thickness (mm) obtained from 3D T1-weighted sequences, crucial for tracking atrophy in dementia [18].
Table 3: Essential Research Reagents and Materials for Low-Field MRI Neuroscience Studies
| Item | Function/Application | Technical Specification |
|---|---|---|
| Phantom Kits | Validation of quantitative metrics (T1, T2, ADC); system calibration | Multimodal phantoms with known relaxation times and diffusion properties [18] |
| AI Reconstruction Software | Image denoising; resolution enhancement; acceleration of acquisition | Deep learning models (e.g., convolutional neural networks) trained on low/high-field image pairs [1] [15] |
| Perfusion Analysis Plugin | Calculation of hemodynamic parametric maps (e.g., CBF, CBV) from DCE-MRI data | Certified software (e.g., UMMperfusion 1.5.2) [20] |
| Tri-Variate Color Mapping Algorithm | Fusion of multiparametric MRI data (e.g., T2, ADC, PBF) into a single intuitive visualization | Custom MATLAB scripts implementing CIELAB color space for perceptual uniformity [20] |
Technical Workflows and Visualization
Workflow for Advanced Color Visualization of Multiparametric Data
The integration of multiple quantitative parameters is a challenge in neuroscience. The following workflow, adapted from a proven methodology, details the process for creating informative tri-variate color maps [20].
Diagram Title: Tri-Variate MRI Color Mapping
This visualization technique translates complex multiparametric data (e.g., T2-weighted images, Apparent Diffusion Coefficient maps, and perfusion maps) into a single, intuitively interpretable image by leveraging the three-dimensional CIELAB color space, which is perceptually uniform to the human visual system [20]. The process ensures that Euclidean distances in the data correspond linearly to perceived color differences, maximizing information transfer to the researcher [20]. This method has demonstrated diagnostic performance comparable to conventional side-by-side radiological evaluation in prostate cancer, and is equally applicable to neuroscience datasets [20].
Technical Implementation of a Portable MRI System
The deployment of a truly portable MRI system for point-of-care neuroscience research involves a specialized technical pipeline, from data acquisition to image interpretation.
Diagram Title: Portable MRI Data Pipeline
This workflow highlights the integrated role of portable hardware (e.g., the Hyperfine Swoop) and advanced software. The hardware employs permanent magnets, minimal RF shielding, and operates on standard power sources [1] [15]. The acquisition utilizes SNR-efficient strategies like balanced steady-state free precession (bSSFP) or long readout spiral imaging to maximize information per unit time [15]. The computational processing heavily relies on AI-driven reconstruction to overcome inherent SNR limitations, and finally generates the quantitative maps essential for neuroscience research [1] [15]. Visualization should employ perceptually uniform color scales (e.g., "jet" or "hot" scales) that have been shown to improve performance in intensity discrimination tasks compared to grayscale [21].
The field of clinical neuroscience research is undergoing a transformative shift with the advent of portable low-field Magnetic Resonance Imaging (MRI) systems. For decades, MRI has been a cornerstone of neurological investigation, yet its utility has been constrained by the high costs, limited accessibility, and substantial infrastructure demands of conventional high-field scanners. The re-emergence of low-field MRI, powered by significant advancements in hardware miniaturization, artificial intelligence (AI)-based image reconstruction, and sustainable design principles, is poised to democratize this critical technology [22] [23]. These innovations are creating a new paradigm where high-quality neuroimaging can be performed at the point-of-care, in resource-limited settings, and within novel research environments, thereby accelerating the pace of discovery in neuroscience and drug development. This whitepaper details the core technological drivers behind this revolution, providing a technical guide for researchers and scientists leveraging these tools for advanced clinical neuroscience applications.
Hardware Miniaturization: Enabling Portability and Accessibility
The development of portable MRI systems has been fundamentally enabled by breakthroughs in magnet design and hardware miniaturization. Traditional high-field MRI systems rely on large, heavy superconducting magnets that require costly infrastructure, including cryogenic cooling with liquid helium and specialized shielding [22]. In contrast, modern portable low-field systems utilize innovative magnet technologies that dramatically reduce their size, weight, and operational complexity.
Core Magnet Technologies
Contemporary portable low-field MRI systems primarily employ two types of magnet technologies, each with distinct advantages for neuroscience research:
- Permanent Magnets: Constructed from materials that generate a persistent magnetic field without requiring external power, permanent magnets enable truly portable and passive operation. Systems like the Hyperfine Swoop, the first FDA-cleared portable MRI, utilize this technology, operating at ultra-low field strengths (e.g., 0.064 Tesla) [22]. Their key advantages include zero helium consumption and minimal power requirements, making them ideal for bedside or mobile deployment.
- Compact Superconducting Magnets: Newer systems, such as the Siemens MAGNETOM Free.Max, are leveraging compact superconducting magnets that do not require active cooling or substantial electricity [22]. These designs maintain the stability and field homogeneity benefits of superconductivity while significantly reducing the size and infrastructure burden compared to their high-field counterparts.
The miniaturization of these core components has a direct and profound impact on the logistical and economic feasibility of MRI. As summarized in the table below, low-field portable systems offer substantial reductions in cost and infrastructure compared to traditional 1.5T systems.
Table 1: Economic and Infrastructure Comparison of MRI Systems
| Characteristic | Traditional 1.5T MRI | Modern Low-Field MRI |
|---|---|---|
| Estimated Capital Cost | ~$1 million USD per tesla [22] | 40-50% of a 1.5T system [22] |
| Installation & Transport Costs | Baseline (High) | Up to 70% reduction [22] |
| Maintenance Costs | Baseline (High) | Up to 45% lower [22] |
| Infrastructure Needs | Reinforced flooring, copper shielding, dedicated HVAC [22] | Significantly reduced or eliminated [22] |
| Power Consumption | High | Lower operational power demands [24] |
Neuroscience Research Applications
The portability enabled by hardware miniaturization unlocks novel research applications:
- Point-of-Care Neuroimaging: Researchers can perform brain imaging in intensive care units (ICUs), emergency departments, and stroke units, facilitating rapid diagnosis and monitoring of neurological conditions like traumatic brain injury and stroke without moving critically ill patients [22] [23].
- In-Situ and Longitudinal Studies: Proof-of-concept studies have demonstrated the integration of portable MRI into a standard van for home-based neuroimaging, enabling longitudinal studies of brain development or neurodegenerative diseases in community settings [22].
- Imaging Patients with Implants: Low-field systems produce reduced susceptibility artifacts near metallic hardware, making them particularly suitable for postoperative neurosurgical imaging and research involving patients with implants [22] [23].
AI and Deep Learning Reconstruction: Compensating for SNR Limitations
A fundamental challenge in low-field MRI is the inherently lower signal-to-noise ratio (SNR) compared to high-field systems. While hardware improvements contribute, the most significant gains in image quality are now being achieved through software, specifically artificial intelligence and deep learning-based reconstruction algorithms.
Technical Approaches and Experimental Protocols
AI-based reconstruction methods are designed to mitigate the SNR penalty and accelerate acquisition. The following table outlines key methodologies and their implementation in recent experimental protocols.
Table 2: AI-Based Reconstruction Methods for Low-Field MRI
| AI Method | Technical Function | Experimental Protocol & Application | Impact on Low-Field Neuroimaging |
|---|---|---|---|
| Deep Learning Denoising | Neural networks are trained to remove noise from MRI images, often using self-supervised learning techniques that do not require fully clean reference data [25]. | Protocol: A self-supervised learning method using Average-to-Average (Avg2Avg) loss was implemented for 0.55T MRI [25]. This technique adapts to the specific noise profile of the scanner. | Encourages the use of 0.55T and other low-SNR MRI scanners, making imaging more affordable and accessible for large-scale research studies [25]. |
| Accelerated Acquisition Reconstruction | Neural networks learn to reconstruct high-quality images from highly undersampled k-space data, dramatically reducing scan time [26]. | Protocol: A joint-attention deep learning network was used to reconstruct pre- and post-contrast T1-weighted 3D brain tumor images from accelerated acquisitions, exploiting correlations across sequences [25]. | Enables significant reductions in MRI protocol time, improving patient comfort and throughput, which is critical for clinical trials [25]. |
| Physics-Coupled Synthetic Data Generation | Generates synthetic MRI data from natural images by incorporating MRI physics models, enabling effective denoising without the need for large, difficult-to-acquire in-vivo datasets [25]. | Protocol: A method was developed to train a complex MRI denoising model using physics-coupled synthetic data derived from natural images, achieving performance on par with models trained on in-vivo data [25]. | Reduces dependence on large in-vivo datasets, addressing a major practical bottleneck in developing AI tools for low-field MRI [25]. |
These protocols demonstrate that AI is not merely an incremental improvement but a transformative technology that redefines the performance boundaries of low-field MRI. For neuroscience research, this translates to diagnostic-quality brain images acquired in shorter times or at lower field strengths, facilitating more efficient research workflows.
Visualization of AI-Driven Image Reconstruction Workflow
The diagram below illustrates a generalized workflow for AI-accelerated image reconstruction in low-field MRI, integrating the key methods described above.
Diagram 1: AI-Driven Low-Field MRI Reconstruction. This workflow shows how undersampled or noisy data from a low-field scanner is processed through an AI reconstruction engine, often incorporating a dedicated denoising step, to produce a high-quality image suitable for neuroscience research.
Sustainable Design: Environmental and Economic Imperatives
The push for sustainability in healthcare is redefining medical imaging. Portable low-field MRI systems align perfectly with this trend, offering significant advantages in energy efficiency and environmental impact over their high-field counterparts.
Energy Consumption and Regulatory Drivers
MRI systems are among the most energy-intensive devices in a hospital [24]. The energy demands of high-field scanners are driven by the need to maintain strong magnetic fields (particularly for superconducting magnets) and operate powerful gradient and cooling systems. In response, the U.S. Environmental Protection Agency (EPA) has introduced the first-ever ENERGY STAR guidelines for medical imaging equipment, with an effective date of November 3, 2025 [24]. These specifications focus on automatic and manual power management features, emphasizing transitions to low-power modes during periods of inactivity. Low-field portable systems, with their inherently lower power demands for magnet operation and reduced cooling needs, are well-positioned to meet these new sustainability benchmarks.
Broader Sustainability Benefits
Sustainable design in portable MRI extends beyond energy consumption:
- Reduced Helium Dependency: Many portable systems using permanent magnets or novel compact superconductors eliminate or drastically reduce the consumption of liquid helium, a finite natural resource [22] [23].
- Lifecycle and Waste Reduction: Innovations like syringeless contrast injectors (e.g., Bracco's Max 3) help reduce plastic waste associated with MRI procedures [27].
- Economic Sustainability: The lower total cost of ownership—encompassing acquisition, installation, maintenance, and energy—makes low-field MRI economically sustainable for a wider range of research institutions and healthcare systems, thereby expanding the global research footprint [22].
The Scientist's Toolkit: Key Research Reagent Solutions
For neuroscientists designing experiments with portable low-field MRI, a suite of specialized "research reagents"—both chemical and computational—is essential. The following table details key components of this toolkit.
Table 3: Essential Research Toolkit for Portable Low-Field MRI in Neuroscience
| Tool / Reagent | Function / Application in Research |
|---|---|
| Macrocyclic GBCAs (e.g., VUEWAY) | Gadolinium-based contrast agents designed for effective enhancement at lower doses (e.g., 0.05 mmol/kg), minimizing gadolinium exposure in longitudinal studies and reducing environmental excretion [27]. |
| AI-Powered Contrast Enhancement Software (e.g., AiMIFY) | Software that uses AI to amplify image contrast in post-processing, potentially allowing for diagnostic-quality images with standard or reduced contrast doses, enhancing safety for research participants [27]. |
| AI Reconstruction Algorithms (e.g., Denoising, Super-Resolution) | Computational tools essential for enhancing SNR and resolution in low-field images. These are critical for extracting high-fidelity quantitative data on brain microstructure and pathology from inherently noisier datasets [26] [25]. |
| Multiparametric Quantitative Mapping Sequences | Advanced pulse sequences (e.g., MR Fingerprinting) for simultaneous T1, T2, and T2* mapping. When combined with AI reconstruction, these enable rapid, quantitative assessment of tissue properties in a single breath-hold or acquisition, crucial for studying disease biomarkers [25]. |
| Cloud-Based Imaging Platforms | Platforms that facilitate the transfer, storage, and remote analysis of imaging data, enabling multi-center neuroscience trials and collaboration by aggregating data from geographically dispersed portable scanners [28]. |
The convergence of hardware miniaturization, AI-driven reconstruction, and sustainable design is not merely improving portable low-field MRI—it is creating a new, versatile tool for clinical neuroscience. These innovation drivers are deeply interconnected: compact hardware enables portability, which creates a need for robust AI to ensure diagnostic quality, and the entire system is bound together by a design philosophy that prioritizes economic and environmental sustainability. For researchers and drug development professionals, this means unprecedented access to neuroimaging capabilities directly at the point of care, in the community, and within diverse populations previously excluded from advanced imaging research. As these technologies continue to mature, evidenced by a robust pipeline of AI research and evolving sustainability standards, portable low-field MRI is set to become an indispensable component of the modern neuroscience toolkit, powering more inclusive, efficient, and impactful brain research.
The pursuit of understanding the human brain is one of science's most ambitious endeavors, yet the benefits of neuroscience research remain starkly inaccessible to large portions of the global population. Low- and middle-income countries (LMICs) carry over 70% of the world's neurological disease burden but generate only a small fraction of global neuroimaging research [8]. This disparity stems not from a lack of scientific interest but from systemic barriers in healthcare and research infrastructure that have created what can be termed the "global neuroscience equity gap."
The core of this challenge lies in the traditional tools of neuroscience itself. Conventional high-field magnetic resonance imaging (MRI) systems, operating at 1.5 Tesla or higher, have remained the gold standard for clinical neuroscience research despite their profound limitations in global accessibility. These systems require specialized infrastructure, substantial financial investment (often approaching $1 million USD per tesla of field strength), cryogenic cooling, significant power demands, and highly trained personnel [22]. The result is a dramatic imbalance in global research capacity—whereas Japan has approximately 276 MRI scanners per 5 million people, West African nations average just 1.1 scanners per 5 million people, representing a 178-fold discrepancy in accessibility [8].
This paper argues that addressing this equity gap requires a fundamental reimagining of neuroscience research infrastructure, with portable low-field MRI (LF-MRI) technology serving as a catalytic platform for democratizing global brain research. Operating at field strengths below 0.1 Tesla, these systems represent not merely a scaled-down version of conventional MRI but a paradigm shift in how neuroscience research can be conducted in resource-limited settings worldwide [8].
Low-Field MRI Technology: Technical Foundations and Innovations
Physical Principles and Historical Context
Low-field MRI technology represents a return to the foundational principles of magnetic resonance imaging, leveraging modern engineering innovations to overcome historical limitations. The earliest MRI scanners deployed in the 1980s were predominantly low-field systems utilizing resistive or permanent magnets, but they fell out of favor as the field prioritized increasing magnetic field strength to improve signal-to-noise ratio (SNR) and spatial resolution [22]. This historical trajectory created a persistent assumption that "low field means low quality means low utility"—a misconception that has hindered technological development for global applications [8].
The physics of signal generation in MRI begins with the static magnetic field (B₀), measured in Tesla, which aligns hydrogen proton spins in biological tissues. When radiofrequency (RF) energy pulses are applied at the resonance frequency, protons are excited and subsequently relax, emitting signals that are spatially encoded using gradients and reconstructed into anatomical images. While SNR is directly proportional to field strength, this relationship is no longer the sole determinant of diagnostic utility, thanks to revolutionary advances in hardware design, acquisition physics, and computational reconstruction methods [22].
Modern Technical Advancements
Contemporary LF-MRI systems incorporate multiple technological innovations that collectively overcome the traditional limitations of low-field imaging:
Advanced Magnet Designs: Modern systems utilize compact superconducting magnets or high-performance permanent magnets that eliminate the need for liquid helium cryogenics and reduce power requirements. Innovations like Halbach array configurations optimize magnetic field homogeneity while minimizing weight and size [22] [4].
Enhanced RF Coils: Sophisticated receiver coil designs, including superconducting RF coils and multimodal surface coils, significantly improve SNR by minimizing resistance and thermal noise. These innovations enhance signal detection capabilities despite lower field strengths [22].
Artificial Intelligence Reconstruction: Deep learning algorithms and advanced reconstruction techniques substantially enhance image quality from LF-MRI systems. These computational methods can compensate for lower intrinsic SNR, enabling diagnostic-quality images previously achievable only with high-field systems [8] [22].
Portable System Architecture: Unlike conventional MRI systems weighing tons and requiring dedicated facilities, modern LF-MRI devices are designed for mobility. The Hyperfine Swoop, the first FDA-cleared portable MRI system, exemplifies this approach, enabling brain imaging at the point-of-care without infrastructure modifications [22].
Open-Source Platforms: A growing movement toward open-source hardware and software for LF-MRI promises to accelerate innovation and adaptation for specific research needs in diverse global settings [8].
Table 1: Key Technical Innovations in Modern Low-Field MRI
| Innovation Category | Specific Technologies | Performance Impact |
|---|---|---|
| Magnet Design | Halbach arrays, compact superconducting magnets, permanent magnets | Reduced size/weight, eliminated cryogenics, improved field homogeneity |
| RF Coils | Superconducting coils, multimodal surface coils, optimized geometries | Enhanced signal-to-noise ratio, improved signal detection |
| Image Reconstruction | AI-enhanced reconstruction, deep learning algorithms, noise reduction | Improved image quality, diagnostic utility comparable to high-field |
| System Architecture | Portable designs, single-sided configurations, battery operation | Enabled point-of-care imaging, reduced infrastructure requirements |
| Data Acquisition | Optimized pulse sequences, parallel imaging, accelerated protocols | Reduced scan times, motion artifact minimization |
Quantitative Evidence: Validating LF-MRI for Neuroscience Research
Diagnostic Performance and Clinical Utility
Empirical studies across diverse clinical settings have demonstrated that LF-MRI systems provide sufficient image quality for meaningful neuroscience research and clinical diagnosis. In a feasibility study conducted in remote Canada, implementation of a 0.064T portable MRI system produced diagnostic-quality images in 100% of 25 patients scanned, despite the challenging environment [29]. Notably, the technology demonstrated particular value in triaging patients, with an estimated 44% of patients avoiding transfer to a tertiary center for neuroimaging [29].
The diagnostic performance of LF-MRI extends across multiple neurological conditions. In a notable study of 221 patients with multiple sclerosis, researchers found no significant difference in diagnostic accuracy between 0.5T and 1.5T scanners, with both achieving an area under the curve of 0.96 [22]. This demonstrates that field strength alone does not determine diagnostic utility when modern acquisition and reconstruction techniques are employed.
Economic Advantages and Implementation Cost Analysis
The economic case for LF-MRI in global neuroscience research is compelling, with substantial cost advantages across the technology lifecycle:
Table 2: Comparative Cost Analysis: Low-Field vs. High-Field MRI Implementation
| Cost Component | High-Field MRI (1.5T-3T) | Low-Field MRI (<0.1T) | Cost Reduction |
|---|---|---|---|
| Capital Equipment | $1-3 million | $50,000-$500,000 | 50-90% |
| Installation/Infrastructure | Reinforced flooring, magnetic shielding, dedicated HVAC | Minimal infrastructure modifications | Up to 70% |
| Maintenance/Service | Expensive service contracts, cryogen replenishment | Lower maintenance costs, no cryogenics | Up to 45% |
| Transportation | Specialized transport, significant expenses | Highly portable, standard transport | >80% |
| Space Requirements | Dedicated suite (400-500 sq ft) | Standard room or mobile deployment | ~60% |
A detailed cost analysis of portable MRI implementation in remote Canada demonstrated significant healthcare system savings of approximately $854,841 based on 50 patients scanned over one year. A five-year budget impact analysis projected nearly $8 million in cumulative savings compared to patient transfers for conventional MRI [29]. Similar economic advantages were documented in prostate cancer imaging, where LF-MRI guided biopsy procedures demonstrated substantial cost efficiency compared to high-field approaches [30].
Research-Grade Data Capabilities
Beyond clinical triage, LF-MRI systems are increasingly capable of supporting sophisticated neuroscience research. A 2025 feasibility study demonstrated that task-based functional MRI (fMRI) is achievable at 0.55T, opening possibilities for functional neuroimaging in diverse global populations previously excluded from such research [4]. Additionally, methodological innovations in ultra-low-field protocol optimization enable reliable brain volume analysis with scan times of approximately 15 minutes, making population-scale neuroimaging studies feasible in resource-limited settings [4].
The Society for Equity Neuroscience (SEQUINS), established in 2024, exemplifies the growing institutional recognition that addressing brain health inequities requires dedicated research infrastructure capable of reaching underrepresented populations [31]. LF-MRI technology aligns precisely with this mission by enabling neuroimaging research across diverse geographic, socioeconomic, and cultural contexts.
Implementation Framework: Protocols for Global Neuroscience Research
Technical Protocol for LF-MRI Neuroscience Studies
Implementing successful neuroscience research with LF-MRI requires standardized protocols optimized for lower field strengths. The following methodology has been validated across multiple research contexts:
Equipment and Reagents:
- Portable LF-MRI system (0.064T-0.1T operating field)
- Integrated or compatible RF head coils
- Battery pack or standard power source (110V/220V)
- DICOM-compatible workstation for image reconstruction
- Secure data transmission capability (PACS network)
- AI-enhanced image reconstruction software
Imaging Protocol:
- System Calibration: Quality assurance checks including signal-to-noise ratio measurement and geometric distortion assessment
- Patient Positioning: Supine position with head immobilization using system-specific cushions
- Protocol Selection: Anatomical T1-weighted and T2-weighted sequences optimized for low-field
- Parameter Optimization: Repetition Time (TR): 500-2000ms; Echo Time (TE): 20-100ms; Matrix Size: 160×160 to 256×256; Slice Thickness: 3-5mm
- Data Acquisition: Scan duration 15-30 minutes depending on protocol complexity
- Image Reconstruction: Application of AI-based enhancement algorithms
- Quality Assessment: Real-time evaluation of diagnostic quality
- Data Management: Secure transfer to PACS with automated backup
This protocol has demonstrated feasibility in remote settings with scan success rates exceeding 95% and diagnostic quality adequate for quantitative volumetric analysis and lesion detection [29] [4].
Research Reagent Solutions for LF-MRI Neuroscience
Table 3: Essential Research Materials for Low-Field MRI Neuroscience Studies
| Research Reagent/Material | Function/Application | Technical Specifications |
|---|---|---|
| Portable LF-MRI System | Primary imaging hardware for data acquisition | 0.064T-0.1T field strength, portable design, battery capability |
| AI Reconstruction Software | Image quality enhancement, noise reduction | Deep learning algorithms trained on matched low-field/high-field datasets |
| Quality Assurance Phantom | System calibration, performance validation | Geometric distortion assessment, SNR measurement, contrast resolution |
| Mobile Data Transmission Unit | Secure image transfer from remote locations | DICOM-compatible, encrypted transmission to central PACS |
| Open-Source Analysis Platform | Standardized image processing, volumetric analysis | Compatible with low-field image characteristics, automated processing |
Diagram 1: LF-MRI Research Implementation Workflow
Implementation Strategy for Global Neuroscience Equity
Building Research Capacity in Resource-Limited Settings
Successful implementation of LF-MRI neuroscience research requires a comprehensive approach that addresses both technical and social dimensions of global research partnerships. The "Second Track" program pioneered by Global Access Partners provides a valuable model, fostering innovative, cross-disciplinary approaches to complex problems through collaboration between community, government, and business stakeholders [32]. This approach emphasizes moving beyond policy discussion to focus on the "how" and "who" of policy delivery—exactly the implementation gap that often hinders global research equity.
Critical components of successful capacity building include:
Localized Training Pathways: Developing sustainable expertise through hands-on training programs for local researchers and technicians, creating a self-sustaining research ecosystem rather than creating dependency on external expertise [8].
Research Infrastructure Co-Development: Engaging local researchers in system customization and protocol development to ensure technologies are appropriately adapted to local healthcare contexts and research priorities [8].
Ethical Data Governance Frameworks: Establishing clear protocols for data ownership, sharing, and utilization that prioritize equitable benefits for participating communities and respect local norms and regulations [8].
Cross-Sector Partnerships: Creating sustainable collaborations between academic institutions, healthcare providers, technology developers, and community organizations to ensure research addresses locally relevant questions while maintaining scientific rigor [32].
Addressing Underrepresentation in Neuroscience Research
The equity imperative in neuroscience extends beyond geographic access to include representation of diverse populations in research. Current neurological studies disproportionately represent Western, educated, industrialized populations, creating critical gaps in understanding brain health across different genetic backgrounds, environmental exposures, and cultural contexts [31]. The Society for Equity Neuroscience (SEQUINS) has identified this representation gap as a fundamental challenge for the field, noting that certain racial and ethnic communities, lower socioeconomic groups, and marginalized populations experience both poorer neurological outcomes and systematic underrepresentation in research [31].
LF-MRI technology directly addresses this challenge through its unique ability to deploy research infrastructure directly to underserved communities. Mobile research units, such as those highlighted by the Global Alzheimer's Platform Foundation, demonstrate how portable neuroimaging can increase participation of historically underrepresented populations in clinical research [33]. Similarly, the ENACT Act legislation recognizes that increasing diversity in clinical trials requires fundamentally rethinking research infrastructure to reduce participation burdens and expand outreach to underrepresented communities [34].
Diagram 2: Multidimensional Strategy for Neuroscience Equity
Future Directions and Implementation Challenges
While LF-MRI technology presents transformative potential for global neuroscience equity, several challenges require ongoing attention. Technical limitations in spatial resolution and scan times continue to improve but remain considerations for certain research applications. The development of comprehensive training curricula specifically designed for LF-MRI operators in resource-limited settings is essential for sustainable implementation. Perhaps most critically, establishing sustainable funding models and business cases for LF-MRI deployment in LMICs requires coordinated effort across technology developers, funding agencies, and healthcare systems.
The research community is actively addressing these challenges through initiatives such as the International Society for Magnetic Resonance in Medicine (ISMRM) Low-Field Study Group, which coordinates technical innovation and knowledge sharing [4]. Recent advances presented at the 2025 ISMRM conference include improved B₀ homogeneity through active cooling of permanent magnets, novel RF coil designs for enhanced transmit efficiency, and optimized protocols for specific research applications including neurodevelopment and aging [4].
The global access gap in neuroscience research represents both an ethical imperative and a scientific limitation. Portable low-field MRI technology offers a transformative pathway toward more equitable, representative, and globally relevant brain research. By fundamentally reimagining research infrastructure to prioritize accessibility, adaptability, and local capacity building, the neuroscience community can address both the ethical challenges of research equity and the scientific limitations of unrepresentative sampling.
The technical evidence is compelling: modern LF-MRI systems provide diagnostically relevant image quality, research-grade data capabilities, and substantial economic advantages over conventional high-field systems. When implemented within a framework of equitable partnership, community engagement, and local capacity building, this technology can democratize neuroscience research and ensure that brain health discoveries benefit all global populations, not merely the most privileged.
Realizing this vision requires coordinated action across researchers, technology developers, funding agencies, and policy makers. Through collective commitment to research equity, the neuroscience community can harness LF-MRI technology to create a more inclusive, representative, and effective global research ecosystem—transforming the equity imperative from moral aspiration to scientific reality.
Deploying Portable MRI: From Bedside to Global Health Neuroscience
Point-of-care (POC) neuroimaging represents a paradigm shift in diagnostic medicine, bringing advanced imaging capabilities directly to the patient bedside. The development of portable, low-field magnetic resonance imaging (MRI) systems has enabled this transformation, particularly for critically ill patients in intensive care units (ICUs), emergency departments (EDs), and intraoperative settings. These innovative technologies operate at magnetic field strengths substantially lower than conventional high-field MRI systems (typically 1.5-3 T), utilizing strengths ranging from 0.064 T to 0.55 T to provide diagnostic-quality imaging at the point of care [1] [35].
The fundamental advantage of portable low-field MRI lies in its ability to perform neuroimaging without the risks and logistical challenges associated with intrahospital transport of critically ill patients. Studies have demonstrated that intrahospital transport carries significant risks, with adverse event rates as high as 60% and serious adverse events occurring in nearly 10% of transports [36]. These include severe hypoxia, hypotension, accidental extubation, and equipment failure [36]. Portable MRI technology eliminates these risks while providing timely diagnostic information that can guide clinical decision-making in time-sensitive neurological emergencies.
This technical guide examines the clinical applications, technological foundations, and implementation methodologies for portable low-field MRI systems in critical care and emergency settings, framed within the broader context of clinical neuroscience research.
Technical Specifications of Portable Low-Field MRI Systems
Fundamental Physical Principles
Low-field MRI systems operate on the same fundamental physical principles as high-field systems but with important technical distinctions. The signal generation process in MRI involves three key steps: (1) alignment of hydrogen proton spins with the static magnetic field (B0), creating a net magnetization vector; (2) excitation of these protons using radiofrequency (RF) energy pulses at the resonance frequency; and (3) detection of the signal generated as protons relax back to equilibrium, characterized by T1 (longitudinal) and T2 (transverse) relaxation processes [1].
The signal-to-noise ratio (SNR) in MRI is directly proportional to the strength and homogeneity of the static magnetic field. While higher field strengths generally produce higher SNR, recent innovations in magnet design, RF coil technology, and advanced reconstruction algorithms have significantly narrowed the performance gap between low-field and high-field systems [1]. Modern low-field systems incorporate engineering advances including compact superconducting magnets (e.g., Siemens MAGNETOM Free.Max) or high-performance permanent magnets (e.g., Hyperfine Swoop) that do not require active cooling or substantial electricity [1].
System Specifications and Capabilities
The Hyperfine Swoop system, as a representative portable MRI device, operates at 0.064 T magnetic field strength and has received FDA 510(k) clearance for clinical use [37] [35]. Key technical specifications include:
- Physical dimensions: Height of 140 cm, width of 86 cm, and weight of approximately 630 kg [35]
- Power requirements: Standard 15 A, 110 V wall outlet without need for cryogens [35]
- Imaging sequences: T1-weighted fast spin-echo, T2-weighted fast spin-echo, fluid-attenuated inversion recovery (FLAIR), and diffusion-weighted imaging (DWI) with apparent diffusion coefficient (ADC) sequences [37]
- Gradient system: Biplanar, unshielded with peak gradient amplitudes of 25-26 mT/m and slew rates of 23-67 T/m/s [35]
- Acoustic noise: 60-80 dB within the head coil [35]
The system features a 5 Gauss (0.5 mT) collapsible ring guard that extends to a diameter of 158 cm during operation, defining the safety boundary [35]. The vertical space between the two magnets is 32 cm, accommodating a head coil measuring 26 cm long, 26 cm high, and 20 cm wide [35].
Table 1: Technical Specifications of Representative Portable MRI Systems
| Parameter | Hyperfine Swoop | Conventional 1.5T MRI |
|---|---|---|
| Magnetic Field Strength | 0.064 T | 1.5 T |
| Power Requirements | Standard 110 V outlet | Dedicated high-voltage supply |
| Infrastructure Needs | None | RF shielding, quench pipes, reinforced flooring |
| Weight | ~630 kg | 3,000-10,000 kg |
| Acoustic Noise | 60-80 dB | 85-110 dB |
| Typical Exam Time | 17-51 minutes | 30-60 minutes |
| Safety Zone | 1.58 m diameter | Entire room restricted |
Clinical Applications in ICU and Emergency Department Settings
Diagnostic Capabilities and Performance
Portable low-field MRI systems have demonstrated significant diagnostic capabilities across multiple neurological conditions in critical care settings. A systematic review of nine studies comprising 410 adults and 14 neonates from ICU and ED settings identified five primary types of brain abnormalities diagnosable using portable MRI: (1) hemorrhage, (2) stroke, (3) infections, (4) injury, and (5) neoplasms [38].
For intracerebral hemorrhage (ICH) detection, a study evaluating 144 portable MRI examinations (56 ICH, 48 acute ischemic stroke, 40 healthy controls) reported sensitivity of 80.4% (95% CI: 0.68-0.90) and specificity of 96.6% (95% CI: 0.90-0.99) [39]. The technology demonstrated particularly high sensitivity for detecting intraventricular hemorrhage (92.8%) and supratentorial ICH (88%) [39]. Manually segmented hematoma volumes from portable MRI correlated strongly with conventional imaging volumes (ICC = 0.955), and these volumes correlated with NIH Stroke Scale scores and clinical outcomes at discharge [39].
In acute ischemic stroke, portable MRI has proven valuable for identifying acute infarctions not apparent on CT. Of 23 diagnostic portable MRI examinations with comparison CT available, three (13%) demonstrated acute infarctions not visible on CT scans [37]. This capability is particularly significant for patients with contraindications to transport or those requiring frequent monitoring of evolving pathology.
Operational Impact and Workflow Integration
The integration of portable MRI into critical care workflows has demonstrated substantial operational benefits through reduced transport requirements and decreased imaging turnaround times. A retrospective analysis of ICU neuroimaging requisitions found that portable MRI could potentially replace fixed CT in 21% and fixed MRI in 26.5% of cases, which would translate to capacity increases allowing 1,676 additional patients to undergo fixed CT and 324 additional patients to undergo fixed MRI annually at the studied institutions [36].
Table 2: Operational Metrics for Portable MRI in Critical Care Settings
| Metric | Emergency Department | Intensive Care Unit |
|---|---|---|
| Median Turnaround Time (POC MRI) | 3.4 hours | 5.3 hours |
| Median Turnaround Time (Fixed MRI) | 3.7 hours | 11.7 hours |
| Statistical Significance (vs. Fixed MRI) | P = 0.90 | P = 0.01 |
| Percentage of Total MRI Examinations | 3% (13/486) | 15% (23/152) |
| Diagnostic Quality Rate | 72% (26/36 exams) | 72% (26/36 exams) |
| Non-diagnostic Reasons | Motion artifact (5/10), technologist error (2/10), patient habitus (2/10), external artifact (1/10) |
Turnaround time studies revealed significant efficiency gains, particularly in ICU settings where portable MRI demonstrated a median turnaround time of 5.3 hours compared to 11.7 hours for fixed MRI (P = 0.01) [37]. In the emergency department, portable MRI turnaround time was 3.4 hours versus 3.7 hours for fixed MRI (P = 0.90) [37]. The slightly improved but not statistically significant difference in ED settings may reflect the higher priority typically given to ED patients for fixed MRI access.
Safety Profile and Patient Tolerance
Portable MRI exhibits an excellent safety profile for critically ill patients. In multiple studies, no adverse events were reported during portable MRI imaging, and patients remained connected to all intravenous lines and ICU monitoring equipment during sequence acquisition [35] [39]. The low magnetic field strength (0.064 T) significantly reduces risks associated with ferromagnetic projectiles and eliminates the need for specialized screening of most medical equipment [35].
Patient tolerance is enhanced due to several factors: reduced acoustic noise (60-80 dB), larger bore size, and shorter examination times [1] [35]. The system's open configuration reduces claustrophobia and enables continued access to patients for clinical monitoring and intervention during imaging [1].
Research Applications and Quantitative Methodologies
Automated Brain Morphometry in Neurodegenerative Disease
Recent advances have demonstrated the application of portable low-field MRI combined with machine learning algorithms for quantitative assessment of brain structures in neurodegenerative diseases such as Alzheimer's disease (AD). Researchers have developed specialized pipelines (LF-SynthSR) that enhance the resolution of low-field images for subsequent segmentation (SynthSeg) to enable volumetric analysis [40].
In evaluation of hippocampal volumes, the correlation between 1 mm MP-RAGE high-field MRI (3T) and low-field MRI using the LF-SynthSR v2 pipeline was r = 0.89 (95% CI: 0.80-0.99) when using T1-weighted images as input [40]. The absolute symmetrized percent difference (ASPD) for hippocampal volume was 3.3% (IQR: 1.8-7.2%) when using T1-weighted images and 2.3% (IQR: 0.5-4.4%) when using T2-weighted images, demonstrating high agreement with high-field MRI [40].
Voxel size and geometry significantly influence measurement accuracy in low-field MRI. For hippocampal volumes, ASPD differences relative to high-field ground truth were <5% for all resolutions when voxel dimensions were isotropic and ≤3 mm [40]. These findings indicate that with appropriate acquisition parameters and processing pipelines, portable MRI can provide reliable volumetric assessments for tracking disease progression in neurodegenerative disorders.
White Matter Hyperintensity Quantification
Beyond brain morphometry, specialized algorithms (WMH-SynthSeg) have been developed to enable automated quantification of white matter hyperintensity (WMH) burden from FLAIR images acquired at low field strengths [40]. WMH volume represents an important biomarker for cerebral small vessel disease, which frequently coexists with Alzheimer's pathology and contributes to cognitive impairment.
The implementation of this automated segmentation pipeline on portable MRI systems expands their capability for comprehensive dementia assessment, particularly in resource-limited settings or for point-of-care applications where serial monitoring is required [40].
Implementation Protocols and Methodological Framework
Patient Screening and Safety Protocols
Successful implementation of portable MRI in critical care settings requires standardized screening and safety protocols. The methodology includes:
- Patient eligibility assessment: Review of demographic data, clinical course characteristics, and available conventional neuroimaging from electronic medical records [35]
- Contraindication screening: Exclusion of patients with pacemakers, defibrillators, implanted medication pumps, vagus nerve stimulators, deep-brain stimulators, or programmable shunts; MRI-incompatible surgical hardware; suspected intraocular metal; or spinal fractures [35]
- Pregnancy and age considerations: Exclusion of patients who are pregnant or <18 years old [35]
- Clinical tolerance evaluation: Consultation with bedside nurses to assess patient ability to lie flat for scan duration, with flat trials performed when necessary [35]
The portable MRI device is safe for use with biomedical devices that have been cleared for magnets of field strength 1.5T and below [35]. Standard ICU ferromagnetic equipment (including vital signs monitors, IV infusion pumps, ventilators, and dialysis machines) can remain in the room but must be positioned outside the 5 Gauss line [35].
Scanning Procedures and Sequence Protocols
Standardized scanning procedures ensure consistent image quality and diagnostic utility:
- Device positioning: The portable MRI system is positioned at the patient's bedside with the extendable bridge adjoining the head of the bed [35]
- Head positioning: The patient's head is positioned within the head coil, which has dimensions of 26 cm long, 26 cm high, and 20 cm wide [35]
- Sequence acquisition: Standard protocols include T1-weighted, T2-weighted, FLAIR, and diffusion-weighted imaging sequences with acquisition times ranging from approximately 2 to 13 minutes per sequence [35]
- Protocol customization: Imaging protocols can be tailored to specific clinical questions or pathologies of interest [35]
The mean examination time for a portable MRI protocol including pre-scan calibration, localizer, T2-weighted, and FLAIR imaging is approximately 18 minutes [39].
Quality Control and Multi-Center Standardization
As portable MRI systems are deployed across diverse clinical and research settings, quality control frameworks become essential for ensuring consistent performance. The UNITY Project, an international neuroimaging network utilizing portable MRI systems, has implemented a comprehensive quality control framework involving 17 sites across 12 countries [41].
This framework utilizes a commercially available phantom and automated, open-source analysis tools to quantify:
- Signal-to-noise ratio (SNR)
- Image contrast
- Geometric distortions
Studies have demonstrated that portable MRI image quality remains robust across varying operational environments, though Larmor frequency shows significant correlation with room temperature, as do image noise and contrast metrics [41]. Image distortions are typically less than 2.5 mm with high robustness over time [41].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Analytical Tools for Portable MRI Studies
| Item | Specification/Function | Application Context |
|---|---|---|
| Portable MRI System | 0.064 T (Hyperfine Swoop) or comparable system; includes integrated head coil | Primary imaging hardware for point-of-care neuroimaging |
| Quality Control Phantom | Commercially available MRI phantom (e.g., CaliberMRI) | Standardized quantification of SNR, contrast, geometric distortion in multi-center studies |
| LF-SynthSR Pipeline | Machine learning algorithm for super-resolution enhancement of low-field images | Resolution improvement for subsequent automated segmentation |
| SynthSeg Tool | Deep learning-based segmentation tool for brain morphometry | Automated volumetric analysis of brain structures |
| WMH-SynthSeg Algorithm | Specialized segmentation tool for white matter hyperintensities | Quantification of white matter lesion burden from FLAIR images |
| DICOM Viewing Workstation | Clinical-grade imaging software with measurement capabilities | Image interpretation and manual segmentation when required |
| Electronic Medical Record Access | Integration capability for clinical correlation | Association of imaging findings with clinical data |
Visual Workflows and Technical Diagrams
Figure 1: Portable MRI Clinical Implementation Workflow. This diagram illustrates the standardized protocol for point-of-care MRI implementation in critical care settings, from patient screening through data integration.
Figure 2: Technical and Operational Comparison Between Low-Field and High-Field MRI Systems. This diagram contrasts the fundamental characteristics of portable low-field MRI with conventional high-field systems, highlighting complementary strengths and applications.
Future Directions and Research Applications
The evolution of portable low-field MRI technology continues with several promising research directions:
Technological Advancements
Current research focuses on enhancing the capabilities of low-field systems through:
- Advanced magnet designs: Polygonal Halbach arrays and sparse permanent magnet arrays that achieve stronger, more homogeneous fields with reduced weight [4]
- Improved RF coils: Toroid-inspired RF volume coils and superconducting RF coils that enhance transmit efficiency and signal-to-noise ratio [4]
- Optimized gradient systems: eGaN-transistor-based gradient amplifier designs that reduce size, cost, and acoustic noise while maintaining performance [4]
- Thermal stability systems: Active water cooling of permanent magnets to address temperature-dependent B0-drift, particularly challenging with balanced steady-state free precession sequences [4]
Novel Clinical and Research Applications
Emerging applications extend beyond critical care diagnostics to include:
- Functional MRI: Recent studies demonstrate reliable task-based fMRI is feasible on 0.55 T scanners, potentially broadening functional neuroimaging access [4]
- Continuous brain monitoring: Development of single-sided "helmet" magnets enabling potentially continuous brain imaging in acute-care settings [4]
- Elastometry: Compact MR instruments for quantitative characterization of tissue elasticity, valuable for routine monitoring applications [4]
- Ambulance-based imaging: Proof-of-concept demonstrations of diagnostic-quality imaging during active ambulance transport using telemedicine-equipped mobile stroke units [1]
Global Health Implementation
The reduced infrastructure requirements and cost profile of portable MRI systems present opportunities to address global health disparities in neuroimaging access. The UNITY Project exemplifies this direction, deploying portable MRI systems globally to characterize neurodevelopment in low and middle-income settings [41]. Similar approaches could expand access to neuroimaging for dementia care, acute stroke management, and neurotrauma in resource-limited environments.
Portable low-field MRI systems represent a transformative technology for point-of-care neuroimaging in critical care settings. The documented capabilities in detecting intracerebral hemorrhage, acute infarction, and other neurological pathologies, combined with operational benefits through reduced transport risks and improved imaging turnaround times, establish this technology as a valuable addition to the clinical neuroscience arsenal.
Ongoing technological refinements in magnet design, RF coil technology, and reconstruction algorithms continue to enhance the diagnostic capabilities of these systems. Furthermore, the development of standardized implementation protocols and quality control frameworks supports the reproducible deployment of portable MRI across diverse healthcare environments.
For clinical neuroscience researchers and drug development professionals, portable low-field MRI offers novel opportunities for serial monitoring of neurological conditions, recruitment of patient populations traditionally excluded from MRI studies, and expansion of neuroimaging research into community and global health settings. As the technology continues to evolve, its integration with artificial intelligence and development of specialized quantitative pipelines will further enhance its research utility, potentially enabling new biomarkers for therapeutic development and clinical trial endpoints.
Low-field portable MRI (LF pMRI) represents a transformative advancement in neuroimaging, offering a safe, cost-effective, and point-of-care imaging solution for clinical neuroscience research and drug development [42]. The Hyperfine Swoop MRI system, which operates at a magnetic field strength of 0.064 Tesla (T) and is currently the only FDA and Health Canada approved LF pMRI system, exemplifies this technology [42]. Unlike conventional high-field MRI systems confined to radiology departments, LF pMRI enables bedside imaging, making it particularly valuable for longitudinal studies in therapeutic trials, research in resource-limited settings, and monitoring patients who cannot be easily transported [42] [43]. However, the transition to low-field strength introduces unique interpretive challenges and operational limitations that require specialized protocol optimization to ensure diagnostic utility for neurological conditions [42]. This guide provides a comprehensive framework for developing and optimizing imaging protocols specifically for neurological applications at low field strengths, with a focus on maximizing data quality within the constraints of portable systems.
Key Challenges in Low-Field Neuroimaging
The primary challenge in low-field neuroimaging stems from the fundamentally lower signal-to-noise ratio (SNR) compared to high-field systems [42]. This reduction in signal can compromise image resolution and the ability to detect subtle pathological changes critical for early diagnosis of neurological disorders. Furthermore, LF pMRI is more susceptible to specific artifacts and presents unique operational considerations regarding patient positioning and protocol selection [42]. These factors must be carefully managed during protocol development.
For researchers and pharmaceutical professionals, these limitations directly impact the ability to generate high-quality, quantifiable imaging biomarkers for clinical trials. The following table summarizes the core challenges and their implications for neuroscience research.
Table 1: Key Challenges in Low-Field Neuroimaging and Research Implications
| Challenge | Technical Basis | Impact on Neuroscience Research |
|---|---|---|
| Reduced Signal-to-Noise Ratio (SNR) | Inherently lower signal at lower magnetic field strengths [42]. | Limits resolution for visualizing subtle atrophy, small lesions, or early microstructural changes in conditions like Alzheimer's disease. |
| Unique Artifact Profiles | Increased sensitivity to environmental interference and different magnetic susceptibilities [42]. | Can mimic pathology or obscure true findings, potentially compromising data integrity in multi-center trials. |
| Operational Constraints | Bedside use in non-shielded environments; patient positioning variability [42]. | Introduces potential variability in data acquisition, requiring strict standardization for longitudinal studies. |
Optimized Protocol Sequences for Neurological Conditions
Protocol optimization for LF pMRI involves balancing acquisition time with diagnostic yield. Evidence suggests that streamlined protocols with a limited number of core sequences can maintain high diagnostic accuracy for a broad range of neurological complaints [44]. A foundational study conducted at a major academic center found that an abbreviated MRI protocol could effectively evaluate patients with new neurological complaints [44]. The research demonstrated that a limited sequence set was sufficient for accurate interpretation, highlighting the potential for optimized, efficient protocols in both clinical and research settings.
The core sequences must be tailored to the specific neurological condition under investigation. The following section details optimized protocol recommendations for key neurological domains relevant to clinical trials and neuroscience research.
Core Protocol for General Neurological Screening
For a general screening protocol, such as in a population study or a trial enrolling patients with diverse neurological symptoms, a minimal set of sequences is recommended. This protocol provides a balance between scan time and comprehensive brain coverage.
Table 2: Core Protocol for General Neurological Screening
| Sequence | Key Parameters & Optimizations | Primary Diagnostic Utility | Scan Time (Approx.) |
|---|---|---|---|
| Sagittal T1-weighted | Use balanced settings to optimize gray-white matter contrast. | Assesses global brain anatomy, midline structures, and cortical thickness. | 2-4 minutes |
| Axial T2-weighted FLAIR | Critical for pathological yield; may require increased averages to boost SNR. | Detects white matter hyperintensities, plaques (MS), edema, and gliosis. | 4-6 minutes |
| Axial Diffusion-Weighted Imaging (DWI) | Single-shot EPI with derived ADC maps is essential. | Identifies acute ischemia, abscesses, and highly cellular tumors. | 3-5 minutes |
This three-sequence protocol (T1, FLAIR, DWI) was validated in a clinical study, where it formed the basis for accurate neuroradiologist interpretation in a majority of cases [44].
Advanced Protocol for Specific Neurological Disorders
For research focused on specific disease pathways, additional sequences are necessary to capture relevant pathological features. The protocols below build upon the core screening set.
Table 3: Advanced Protocols for Specific Neurological Disorders
| Research Focus | Recommended Protocol | Rationale and Optimization Tips |
|---|---|---|
| Neurodegenerative Diseases (e.g., Alzheimer's, Parkinson's) | Core Protocol + T2* GRE or SWI | T2* GRE/SWI is sensitive to iron deposition and microbleeds. At low field, these sequences help characterize neurodegenerative pathology and vascular contributions [42] [44]. |
| Neuro-oncology (Brain Tumors) | Core Protocol + Contrast-Enhanced T1-weighted | The utility of contrast is highly dependent on achieving sufficient SNR at low field. Requires careful optimization of timing and dosage to visualize blood-brain barrier breakdown [42]. |
| Cerebrovascular Disease | Core Protocol + T2* GRE/SWI + MR Angiography (MRA) | T2* GRE/SWI detects microbleeds and hemorrhages. Time-of-flight MRA can be challenging at low field but may be optimized for larger vessels to assess for stenosis or occlusion. |
The addition of a susceptibility-weighted sequence (T2* GRE or SWI) to the core three-sequence protocol was shown to improve diagnostic confidence and yield, particularly for detecting vascular pathologies [44].
Experimental Protocol for Protocol Validation
To validate any LF pMRI protocol for a research study, a structured experimental methodology is required. The following workflow, derived from established research methods, ensures systematic evaluation.
Diagram 1: Workflow for Validating an Abbreviated MRI Protocol
Detailed Methodology
Patient Selection and Study Design:
- A retrospective or prospective cohort of patients with the neurological condition of interest should be selected.
- Inclusion criteria should mirror the intended use-case (e.g., patients with new cognitive complaints for a dementia trial) [44].
- Studies are typically partitioned into groups to test different abbreviated protocol configurations.
Image Acquisition and Dataset Creation:
- All patients undergo the full, extended MRI protocol on the LF pMRI system, which serves as the reference standard.
- For each patient, a separate dataset is created containing only the sequences from the proposed abbreviated protocol [44].
Blinded Interpretation:
- Staff researchers or neuroradiologists, blinded to the full protocol results and the original report, interpret the abbreviated datasets.
- Readers are provided only with the limited clinical history and must formulate a diagnostic impression based solely on the sequences in the test protocol [44].
- To eliminate recall bias, cases originally interpreted by a reader should be reassigned.
Reference Standard and Discrepancy Analysis:
- The original clinical report generated from the full, unblinded protocol serves as the reference standard.
- The impressions from the blinded read are systematically compared to the reference standard.
- All discrepancies are categorized by clinical significance:
- Major Discrepancy: A finding likely to have a significant impact on patient management or trial enrollment (e.g., missing a tumor or acute infarct) [44].
- Minor Discrepancy: A finding with unlikely significant clinical impact (e.g., missing a focus of old microhemorrhage).
- For any discrepancy, reviewers should re-inspect the abbreviated dataset to determine if the finding was perceptible but initially missed (perceptual error) or truly undetectable due to protocol limitations [44].
Data Analysis:
- The primary outcome is the diagnostic accuracy of the abbreviated protocol, calculated as its agreement with the reference standard.
- Statistical measures include sensitivity, specificity, and overall accuracy.
- The rate of major discrepancies should be minimal (e.g., <1-2%) for the protocol to be deemed acceptable for research use.
Integration of Computational Analysis
The limitations of LF pMRI can be partially mitigated by advanced computational models, which are increasingly vital for the early and accurate diagnosis of neurological disorders. Deep learning (DL) models can enhance image quality and extract subtle biomarkers from lower-resolution scans.
Spatio-temporal modeling is particularly powerful for longitudinal trials. Hybrid DL models, such as the STGCN-ViT, combine Convolutional Neural Networks (CNN) for spatial feature extraction, Spatial-Temporal Graph Convolutional Networks (STGCN) for tracking anatomical changes over time, and Vision Transformers (ViT) with Attention Mechanisms (AM) to focus on critical brain regions [45]. When applied to datasets like OASIS, such models have achieved accuracies exceeding 93% in classifying neurological disorders, demonstrating that computational analysis can significantly augment the value of LF pMRI data in research [45].
Diagram 2: Computational Analysis Pipeline for LF pMRI Data
The Scientist's Toolkit: Research Reagent Solutions
Implementing and validating LF pMRI protocols requires a combination of hardware, software, and data resources. The following table details essential components of the research toolkit.
Table 4: Essential Research Toolkit for Low-Field MRI Protocol Development
| Tool Category | Specific Item / Solution | Function in Protocol Development |
|---|---|---|
| Imaging Hardware | Hyperfine Swoop MRI System (0.064 T) [42] | The primary imaging platform for data acquisition; requires optimization of patient positioning and scanning parameters. |
| Phantom Reagents | Geometric Phantoms; Anthropomorphic Head Phantoms | Used for daily quality assurance, calibration, and standardized measurement of SNR, geometric accuracy, and contrast. |
| Contrast Agents | Gadolinium-Based Contrast Agents (GBCA) | Used in perfusion studies and for enhancing tumor visualization; dosing and timing require optimization for low-field [42]. |
| Computational Tools | CNN-STGCN-ViT Hybrid Models [45] | AI models for spatial-feature extraction, tracking disease progression over time, and improving diagnostic accuracy from LF pMRI data. |
| Reference Datasets | Open Access Series of Imaging Studies (OASIS) [45] | Publicly available benchmark datasets used for training, validating, and testing computational models on neuroimaging data. |
| Analysis Software | Medical Image Processing Toolkits (e.g., FSL, SPM) | Software for quantitative image analysis, including volumetric segmentation, lesion mapping, and voxel-based morphometry. |
Magnetic resonance imaging (MRI) is a cornerstone of modern clinical medicine and neuroscience, yet it remains largely inaccessible for large-scale population studies due to high costs, complex infrastructure requirements, and geographical limitations [8]. Portable low-field MRI (LF-MRI) systems, operating at magnetic field strengths below 0.1 Tesla, are emerging as transformative tools that overcome these barriers, enabling researchers to expand neuroimaging cohorts beyond traditional laboratory settings [1] [8]. These systems leverage advances in hardware engineering, acquisition physics, and artificial intelligence (AI) to deliver clinically meaningful images with radically improved accessibility [46] [8]. This technical guide examines the implementation of portable LF-MRI for community-based and longitudinal studies, providing researchers with methodologies, technical specifications, and experimental frameworks to deploy this technology effectively within clinical neuroscience research.
The historical development of MRI has followed a trajectory toward higher field strengths, driven by the pursuit of increased signal-to-noise ratio (SNR) and spatial resolution [1]. However, this paradigm has created significant accessibility challenges, with approximately 66% of the global population lacking access to MRI as of 2019 [1]. Portable LF-MRI represents a fundamental shift in this approach, prioritizing accessibility, cost-effectiveness, and point-of-care deployment without sacrificing diagnostic capability [1] [8]. These systems are catalyzing a new era in neuroimaging research by enabling studies in community settings, remote populations, and longitudinal frameworks that were previously impractical with conventional high-field systems.
Technical Foundations of Portable Low-Field MRI
System Architecture and Hardware Innovations
Portable LF-MRI systems employ distinct magnet technologies that enable their compact form factor and reduced infrastructure requirements. Unlike conventional superconducting magnets that require cryogenic cooling, modern portable systems primarily utilize permanent magnets or compact superconducting designs that operate without liquid helium [1]. The Hyperfine Swoop system, for instance, employs a permanent magnet design operating at 0.064 Tesla, requiring only a standard electrical outlet for operation [47] [6]. Similarly, research prototypes have demonstrated effective imaging at 0.055 Tesla using samarium-cobalt permanent magnets, which offer superior temperature stability compared to neodymium-based alternatives [9].
A critical engineering challenge for portable MRI operating in unshielded environments is mitigating electromagnetic interference (EMI). Innovative solutions have emerged to address this limitation. Some systems employ deep learning-driven EMI cancellation that uses strategically placed sensing coils to model and subtract interference dynamically during acquisition [9]. The Hyperfine system implements a proprietary EMI removal method that enables operation without traditional radiofrequency shielding cages [9]. These advancements allow diagnostic-quality imaging in diverse environments including community health centers, ambulances, and even patient homes [1] [9].
Image Quality Enhancement Through Advanced Reconstruction
While lower magnetic field strength inherently reduces SNR compared to high-field systems, portable LF-MRI leverages sophisticated computational methods to overcome this limitation. AI-based reconstruction techniques have proven particularly valuable, with deep learning algorithms trained on matched low-field and high-field datasets to enhance image quality and extract quantitative measurements [48]. These approaches have demonstrated performance comparable to conventional MRI in measuring structurally relevant features in Alzheimer's disease, including hippocampal volume and white matter hyperintensities [48].
The integration of AI throughout the imaging pipeline represents a fundamental shift in low-field MRI methodology. Rather than relying solely on physical improvements to hardware, these systems leverage computational advances to extract maximum information from acquired signals [8] [48]. This synergy between hardware and software enables portable systems to achieve diagnostic-quality images despite technical constraints of low field strength [1].
Table 1: Technical Specifications of Representative Portable Low-Field MRI Systems
| Parameter | Hyperfine Swoop | Research Prototype [9] | Conventional 1.5T MRI |
|---|---|---|---|
| Magnetic Field Strength | 0.064 T | 0.055 T | 1.5 T |
| Magnet Type | Permanent magnet | Samarium-cobalt permanent magnet | Superconducting magnet |
| Power Requirements | Standard wall outlet | Two-phase 220V 15A | Dedicated high-voltage supply |
| Shielding Requirements | None (EMI cancellation) | None (deep learning EMI cancellation) | Magnetic and RF shielding rooms |
| System Weight | Portable (exact weight not specified) | ~750 kg | 3,000-4,500 kg |
| 5 Gauss Fringe Field | Minimal (enables point-of-care use) | Within 0.45-0.9 m from magnet center | Extensive (requires dedicated room) |
| Installation Cost | Significant reduction (>50% vs. 1.5T) [1] | Low-cost prototype | ~$1 million per Tesla [1] |
Implementation Framework for Research Studies
Experimental Design Considerations
Implementing portable LF-MRI in community-based and longitudinal studies requires careful methodological planning across several domains. Study design must account for the technical capabilities of low-field systems while leveraging their unique advantages for specific research questions. Key considerations include:
Population Access: Portable systems enable imaging of participants who cannot travel to imaging facilities, including elderly populations, individuals with mobility limitations, and residents in remote communities [8] [6]. The UNITY project exemplifies this approach, utilizing low-field systems to characterize neurodevelopment in sub-Saharan Africa and South Asia where conventional MRI is unavailable [49].
Longitudinal Frequency: Reduced cost and increased accessibility facilitate repeated measurements at shorter intervals, capturing dynamic processes in neurodevelopment, disease progression, and treatment response [49] [6]. The portability of these systems ensures consistent imaging parameters across timepoints, even when studies span multiple locations.
Environmental Control: Unlike controlled laboratory environments, community-based imaging occurs in diverse settings with variable ambient conditions. Protocols must account for potential electromagnetic interference, temperature fluctuations, and space constraints while ensuring consistent data quality [9].
Protocol Implementation and Optimization
Standard neuroimaging protocols can be successfully implemented on portable LF-MRI systems, though acquisition parameters require optimization for lower field strength. Essential sequences for brain imaging include:
T1-Weighted Imaging: Provides anatomical reference with gray matter-white matter contrast valuable for volumetric analyses [9]. At low field strengths, T1 relaxation times decrease, requiring adjustment of repetition time (TR) and echo time (TE) parameters.
T2-Weighted and FLAIR Imaging: Detects pathological changes including white matter lesions, edema, and other tissue abnormalities [9]. The reduced susceptibility artifacts at low fields can improve visualization near tissue-air interfaces.
Diffusion-Weighted Imaging (DWI): Identifies acute ischemia and characterizes tissue microstructure through water diffusion measurement [9]. Successful DWI implementation has been demonstrated at 0.055T with appropriate gradient optimization.
Quantitative Mapping: Emerging techniques enable T1 and T2 relaxometry measurements, providing objective biomarkers for tissue characterization [48]. These quantitative approaches are particularly valuable for longitudinal studies tracking disease progression or treatment effects.
Table 2: Research Reagent Solutions for Portable MRI Studies
| Component | Function | Implementation Examples |
|---|---|---|
| Portable MRI System | Image acquisition in community settings | Hyperfine Swoop (0.064T), Research prototype (0.055T) [6] [9] |
| AI Reconstruction Software | Image quality enhancement and quantitative analysis | Optive AI on Hyperfine systems, Deep learning algorithms for EMI cancellation [47] [9] |
| Sequence Programming Platform | Protocol development and customization | Hyperfine PULSE platform for sequence development and sharing [47] |
| Mobile Integration Platform | Transporting MRI to research participants | Vehicle-integrated systems for in-home neuroimaging [1] |
| Quality Assurance Phantoms | System performance validation across locations | Geometric accuracy, SNR, and contrast resolution phantoms |
Data Processing and Analysis Workflow
The data pipeline for portable MRI studies extends from acquisition through quantitative analysis, with specialized approaches addressing the unique characteristics of low-field data:
Preprocessing: Includes artifact correction, noise reduction, and intensity normalization. AI-based methods effectively address system-specific limitations including bias field correction and noise suppression [48] [9].
Cross-Modal Enhancement: Some implementations leverage paired high-field and low-field datasets to train algorithms that enhance low-field images, either through direct super-resolution or feature extraction optimized for low-field characteristics [48].
Quantitative Analysis: Automated segmentation and measurement of structural volumes (e.g., hippocampal volume, white matter hyperintensity burden) provide objective biomarkers for research endpoints [48] [6]. These measurements have demonstrated strong correlation with high-field MRI values when appropriate correction algorithms are applied.
Applications in Clinical Neuroscience Research
Neurodevelopmental and Pediatric Studies
Portable LF-MRI enables previously impossible longitudinal studies of brain development in community settings. The UNITY project exemplifies this application, characterizing neurodevelopment across diverse global populations where conventional MRI is unavailable [49]. By deploying low-field systems in sub-Saharan Africa and South Asia, researchers can establish normative trajectories of brain growth and identify environmental factors influencing development [49]. The reduced acoustic noise and more open design of portable systems improve tolerance in pediatric populations, potentially reducing sedation requirements [1].
Neurodegenerative Disease and Aging Research
Large-scale studies of aging populations benefit substantially from portable neuroimaging. Research at Massachusetts General Hospital has demonstrated that low-field MRI with AI augmentation accurately measures Alzheimer's disease biomarkers including hippocampal volume and white matter hyperintensity burden [48]. The University of Kansas Alzheimer's Disease Research Center is implementing the Swoop system in the ACE-AD study, combining portable MRI with cognitive testing and blood biomarkers in a single clinical visit to streamline dementia diagnosis [6]. This approach is particularly valuable for monitoring treatment response in novel Alzheimer's therapies, where regular MRI surveillance is required [6].
Global Health and Health Disparities Research
Portable LF-MRI addresses critical disparities in neuroimaging access between high-income and low-middle-income countries (LMICs). In West Africa, where approximately 84 MRI scanners serve a population of 372.6 million people (1.1 scanners per 5 million people), portable systems offer a viable solution for expanding diagnostic and research capabilities [8]. This increased access enables population-scale studies of neurodevelopment, aging, and neurogenetics in genetically diverse populations historically underrepresented in neuroimaging research [8].
Methodological Validation Framework
Technical Validation and Quality Assurance
Implementing portable MRI in research requires rigorous validation against established imaging biomarkers. The following framework ensures scientific rigor:
Phantom Validation: Geometric accuracy, resolution, SNR, and contrast-to-noise ratio should be quantified using standardized phantoms across imaging locations [1] [9]. These measurements establish baseline performance and monitor system stability over time.
Clinical Correlation Studies: Method validation should include direct comparison with high-field MRI in relevant patient populations [48] [9]. Studies should assess both quantitative measurements (e.g., volumetric analyses) and qualitative diagnostic interpretations.
Longitudinal Stability Assessment: For studies with repeated measurements, system performance must be monitored throughout the study period using standardized protocols to ensure data consistency [49].
Statistical Considerations for Study Design
The unique characteristics of portable MRI data necessitate specific statistical approaches:
Sample Size Calculations: Power analysis should account for potentially increased measurement variability in low-field data compared to conventional systems. Pilot studies can inform variance estimates for key outcome measures.
Multi-Center Harmonization: Studies deploying multiple portable systems require harmonization protocols to minimize inter-scanner variability, including standardized acquisition protocols and cross-calibration procedures [49].
Missing Data Strategies: Community-based studies may experience higher rates of missing data due to variable imaging environments. Statistical analysis plans should specify appropriate methods for handling missing data.
Table 3: Methodological Comparison of Portable vs. Conventional MRI in Research Applications
| Research Dimension | Portable Low-Field MRI | Conventional High-Field MRI |
|---|---|---|
| Participant Access | Community-based, home-based, remote populations [1] [49] | Limited to imaging facilities |
| Longitudinal Frequency | High-frequency sampling feasible due to reduced cost and accessibility [49] | Limited by cost and participant burden |
| Population Diversity | Enhanced diversity including rural, elderly, mobility-limited [8] [6] | Often limited to urban populations near imaging centers |
| Quantitative Biomarkers | AI-enhanced measurements of volume, lesion burden [48] | Direct quantitative measurements |
| Environmental Control | Variable conditions requiring adaptive protocols [9] | Highly controlled imaging environments |
| Implementation Scalability | High scalability across multiple sites [8] | Limited by infrastructure costs |
Implementation Challenges and Solutions
Technical Limitations and Mitigation Strategies
Despite significant advances, portable LF-MRI systems face inherent technical limitations that researchers must consider:
Spatial Resolution and SNR: The fundamental trade-off between field strength and SNR remains, though advanced reconstruction algorithms substantially mitigate this limitation [1] [48]. Protocol optimization should prioritize contrast-to-noise ratio over absolute spatial resolution for most applications.
Sequence Limitations: Not all advanced sequences available on high-field systems can be directly implemented on portable platforms. Researchers should validate essential sequences for their specific research questions and adapt acquisition parameters appropriately [9].
Artifact Management: Unique artifact profiles differ from conventional MRI and require specialized processing approaches [9]. Regular quality assurance and artifact detection protocols ensure data integrity throughout the study lifecycle.
Operational and Logistical Considerations
Deploying portable MRI in research contexts presents unique operational challenges:
Regulatory Compliance: Portable systems require appropriate regulatory clearance for research use, with specific considerations for community-based deployment outside traditional clinical environments [6].
Training Requirements: Operating portable systems in diverse settings requires training both technical staff and community-based research personnel in system operation, safety protocols, and basic troubleshooting [8].
Data Management: Community-based imaging generates large datasets requiring secure transmission from field locations to central analysis facilities. Robust data governance frameworks must address privacy, security, and ethical considerations [49] [8].
Future Directions and Emerging Capabilities
The rapid evolution of portable MRI technology suggests several promising research applications:
Multi-Modal Biomarker Integration: Combining portable MRI with other portable technologies (e.g., EEG, functional near-infrared spectroscopy) enables comprehensive characterization of brain structure and function in naturalistic environments [8].
Real-Time Adaptive Imaging: Machine learning approaches may enable real-time protocol optimization based on initial imaging findings, personalizing acquisition protocols to individual participants or specific research questions [47].
Open-Source Platforms: Initiatives like the Hyperfine PULSE platform create ecosystems for sequence development and sharing, accelerating methodological innovation across the research community [47].
Global Neuroimaging Networks: Standardized portable systems enable truly global research collaborations studying brain development, aging, and disease across diverse populations and environments [49] [8].
Portable low-field MRI systems represent a paradigm shift in clinical neuroscience research, transforming neuroimaging from a centralized, facility-limited tool to a distributed, accessible technology. By enabling community-based and longitudinal studies across diverse populations, these systems address critical limitations in research cohort diversity and ecological validity. While technical constraints require careful methodological adaptation, the integration of advanced reconstruction algorithms and optimized acquisition protocols enables robust research applications across neurodevelopment, aging, and global health domains. As technology continues to evolve, portable MRI promises to fundamentally expand the scope and scale of neuroimaging research, creating new opportunities to understand brain structure and function across populations, environments, and the lifespan.
The integration of portable low-field MRI (LF-MRI) systems into drug development pipelines represents a transformative approach for monitoring treatment response and disease progression. Operating at field strengths below 0.1 Tesla, these scanners address critical bottlenecks in clinical trials by providing objective, quantifiable biomarkers directly at the point-of-care, thus enabling more frequent and accessible assessment of therapeutic efficacy. This technical guide details the application of LF-MRI for pharmacodynamic measurements, longitudinal tracking of neurological conditions, and patient stratification in clinical studies. Supported by case studies and structured protocols, we demonstrate how the unique advantages of LF-MRI—including its portability, reduced infrastructure needs, and lower operational costs—can de-risk drug development and accelerate the translation of novel neurotherapeutics, particularly within the framework of precision medicine.
Portable low-field MRI (LF-MRI) is redefining the possibilities for structural and functional brain imaging in clinical trial settings. Defined as systems operating at magnetic field strengths of 100 mT (0.1T) or less [8], modern LF-MRI technology has overcome historical limitations of image quality through advances in hardware engineering, acquisition physics, and AI-powered image reconstruction [8] [22]. Unlike conventional high-field systems requiring massive infrastructure, LF-MRI devices are characterized by their portability, significantly lower cost (40-50% less than 1.5T systems), and reduced operational demands [22], making them suitable for deployment in diverse environments from clinical centers to remote field locations.
The fundamental physical principles of MRI remain consistent across field strengths; however, LF-MRI offers distinct advantages for drug development. Reduced susceptibility artifacts near metallic implants or air-tissue interfaces improve imaging capabilities in postoperative patients or those with medical devices [22]. Furthermore, the quieter operation and more open designs of many LF-MRI systems enhance patient comfort and compliance—critical factors for longitudinal studies requiring repeated measurements [22]. For clinical trial sponsors, the dramatically lower capital and maintenance costs (up to 45% less) present an opportunity to deploy multiple imaging systems across trial sites, standardizing data collection while containing costs [22].
Most importantly for therapeutic development, LF-MRI provides a platform for obtaining quantitative imaging biomarkers that can objectively track disease progression and treatment response. As the field moves toward precision medicine approaches, these biomarkers serve as essential tools for establishing target engagement, optimizing dosing, and identifying patient subgroups most likely to respond to therapy [50].
LF-MRI as a Pharmacodynamic Biomarker
In early-phase clinical trials, a primary challenge is determining whether an investigational compound engages its intended biological target in the human brain. Low-field MRI can provide critical functional pharmacodynamic biomarkers that demonstrate both brain penetration and biological activity, thereby de-risking subsequent development phases.
Functional Target Engagement
Different neuroimaging modalities provide complementary perspectives on drug effects in the brain. While PET imaging directly measures molecular target occupancy, functional MRI (fMRI) and electroencephalography (EEG) assess downstream functional consequences of target engagement [50]. LF-MRI systems capable of functional imaging can detect drug-induced changes in brain activation patterns, connectivity, and network dynamics, providing evidence that a compound modulates clinically relevant neural systems.
A key application involves establishing dose-response relationships for functional brain effects. Traditional Phase 1 studies with 4-6 participants per dose are typically underpowered for detecting clinically meaningful pharmacodynamic effects [50]. LF-MRI enables larger, more frequent scanning sessions at lower cost, facilitating better-powered dose-finding studies that identify optimal therapeutic ranges before advancing to larger trials.
Table: Neuroimaging Modalities for Pharmacodynamic Assessment in Drug Development
| Modality | Measured Parameter | Primary Use in Pharmacodynamics | Advantages for LF-MRI |
|---|---|---|---|
| fMRI | Task-based or resting-state brain activation | Functional target engagement | Portable systems enable testing in naturalistic environments; reduced movement artifacts |
| EEG | Event-related potentials (ERP) | Neural processing speed and attention | Direct neuronal measurement; compatible with LF-MRI environment |
| ASL | Cerebral blood flow | Perfusion changes | Quantifies cerebral blood flow without contrast; absolute quantification |
| DWI/DTI | White matter microstructure | Structural connectivity changes | Sensitive to axonal injury and recovery; no contrast needed |
Experimental Protocol: Establishing Functional Target Engagement
Objective: To determine whether an investigational compound engages functional neural targets using portable LF-MRI.
Population: Healthy volunteers or patient population (n=20-40 per dose group for adequate power).
Imaging Protocol:
- Baseline Scan: Acquire structural images (T1-weighted, T2-weighted), resting-state fMRI (10 minutes), and task-based fMRI during cognitive/emotional paradigm.
- Drug Administration: Randomized, placebo-controlled, dose-ranging design.
- Post-Dose Scans: Repeat fMRI at predetermined intervals (e.g., 1, 3, 6, 24 hours) based on pharmacokinetic profile.
- Data Analysis:
- Preprocess structural and functional data (motion correction, normalization).
- Calculate amplitude of low-frequency fluctuations (ALFF) from resting-state data.
- Analyze task-based activation in pre-specified regions of interest (ROIs).
- Perform seed-based or independent component analysis for functional connectivity.
- Model dose-response relationships for significant functional changes.
Key Outputs: Dose-dependent changes in functional activation/connectivity; optimal biological dose determination; correlation between functional changes and drug plasma levels.
Monitoring Treatment Response and Disease Progression
Longitudinal monitoring of disease progression and treatment response represents a core application for LF-MRI in clinical trials. By providing objective, quantifiable markers of neurological status, these systems enable more sensitive detection of therapeutic effects than clinical rating scales alone.
Tracking Structural and Functional Connectivity
Advanced diffusion MRI techniques performed on LF-MRI systems can quantify microstructural changes in white matter tracts that correlate with disease progression and treatment response. Differential tractography, an emerging analysis technique, measures how connections between brain regions appear or disappear over time, as well as how existing connections grow or shrink [51].
In a study of GM1 gangliosidosis, a rare neurodegenerative disease, researchers utilized differential tractography to track neuronal degeneration. They found that the number and size of neuronal connections decreased over time in patients while increasing in healthy children [51]. Importantly, patients with greater clinical deterioration showed larger decreases in connectivity measures, demonstrating the biomarker's clinical validity [51]. This approach is now being used in a clinical trial of gene therapy for GM1 gangliosidosis, where it may provide an early signal of efficacy before clinical improvements become apparent [51].
Experimental Protocol: Longitudinal Monitoring of Progressive Neurological Disorders
Objective: To quantify disease progression and treatment response using serial LF-MRI scans in a neurodegenerative disease trial.
Population: Patients with confirmed diagnosis (e.g., Alzheimer's disease, Parkinson's disease, rare neurological disorders); sample size based on expected effect size and trial duration.
Imaging Protocol (Repeat at baseline, 3, 6, and 12 months):
- Structural Imaging: High-resolution T1-weighted and T2-weighted sequences for volumetric analysis.
- Diffusion MRI: Multi-shell diffusion-weighted imaging for tensor and kurtosis metrics.
- Resting-State fMRI: 10-15 minutes of eyes-open rest for functional connectivity.
- ASL Perfusion: Cerebral blood flow measurement.
Data Analysis:
- Perform voxel-based morphometry or surface-based cortical thickness analysis.
- Calculate diffusion metrics (fractional anisotropy, mean diffusivity) in specific white matter tracts.
- Apply differential tractography to quantify connectivity changes over time [51].
- Compute functional connectivity matrices and network properties (e.g., modularity, efficiency).
- Quantify regional cerebral blood flow using ASL.
Key Outputs: Rate of brain atrophy; changes in white matter integrity; alterations in functional networks; correlation between imaging biomarkers and clinical scores.
Quantitative Biomarkers for Clinical Trials
LF-MRI provides multiple quantitative biomarkers suitable for tracking therapeutic outcomes across neurological and psychiatric conditions. The table below summarizes key imaging biomarkers applicable to drug development.
Table: Quantitative LF-MRI Biomarkers for Treatment Response Monitoring
| Biomarker Category | Specific Metrics | Clinical Trial Applications | Technical Considerations for LF-MRI |
|---|---|---|---|
| Structural Measures | Cortical thickness, Brain volume, Lesion load | Neurodegenerative diseases, Multiple sclerosis, Neurodevelopmental disorders | Lower spatial resolution compensated by longitudinal within-subject designs |
| White Matter Integrity | Fractional anisotropy, Mean diffusivity, Fiber density | Demyelinating diseases, Stroke recovery, Traumatic brain injury | Enhanced diffusion contrast at lower fields; adequate for tractography |
| Functional Connectivity | Network modularity, Hub connectivity, Default mode network integrity | Psychiatric disorders, Neurodegenerative diseases, Cognitive impairment | Reduced BOLD sensitivity but sufficient for network-level analyses |
| Cerebral Perfusion | Cerebral blood flow, Arterial transit time | Cerebrovascular disease, Vascular dementia, Stroke | ASL techniques benefit from longer T1 at low field; quantitative without contrast |
| Metabolic Imaging | Magnetic resonance spectroscopy metabolites | Inborn errors of metabolism, Neuro-oncology, Neurodegeneration | Lower spectral resolution but sufficient for major metabolite quantification |
Patient Stratification and Enrichment Strategies
Beyond tracking treatment response, LF-MRI biomarkers can optimize clinical trial design by identifying patient populations most likely to respond to investigational therapies.
Precision Psychiatry and Neuroimaging
The high failure rate of psychiatric drug development (over 94% of compounds failing after Phase I) [52] underscores the need for better stratification approaches. LF-MRI can identify neurophysiological subtypes within diagnostic categories that may respond differentially to treatment. For example, patients with major depressive disorder showing specific patterns of functional connectivity might be more responsive to certain mechanistically distinct antidepressants.
This precision medicine approach—using neuroimaging to guide patient selection—is increasingly feasible with portable LF-MRI systems that can be deployed across multiple trial sites. This enables consistent biomarker assessment during screening, ensuring enrolled participants share the neurobiological characteristics targeted by the investigational therapy [50].
Experimental Protocol: Patient Stratification Using LF-MRI Biomarkers
Objective: To enrich clinical trial populations using LF-MRI biomarkers predictive of treatment response.
Population: Patients meeting clinical criteria for a disorder; sample size sufficient to identify biomarker-positive subgroup.
Imaging Protocol (During screening phase):
- Structural MRI: T1-weighted, T2-weighted, FLAIR sequences.
- Resting-State fMRI: 15 minutes for functional connectivity analysis.
- Task-Based fMRI: Paradigm targeting neural systems relevant to drug mechanism.
- Diffusion MRI: For white matter assessment if relevant to disease.
Data Analysis:
- Extract features from each modality (e.g., connectivity strength, activation magnitude, volumetric measures).
- Use machine learning approaches to identify biomarker signatures predictive of treatment response.
- Establish cutoff values for biomarker positivity based on previous data or healthy controls.
- Randomize biomarker-positive patients to treatment versus control.
Key Outputs: Proportion of biomarker-positive patients; differential treatment effect in biomarker-positive versus biomarker-negative subgroups; positive and negative predictive values of biomarker.
Successful implementation of LF-MRI in therapeutic development requires both technical infrastructure and analytical capabilities. The following table details essential components of the LF-MRI research toolkit.
Table: Research Reagent Solutions for LF-MRI Studies in Drug Development
| Resource Category | Specific Tools | Function in Drug Development | Implementation Notes |
|---|---|---|---|
| Portable LF-MRI Systems | Hyperfine Swoop, Siemens MAGNETOM Free.Max | Deployable imaging at clinical sites, point-of-care assessment | Select systems based on field strength (0.055T-0.1T), sequence capabilities, and portability needs |
| Multi-modal Phantoms | Geometric phantoms, Diffusion phantoms, Functional MRI phantoms | Quality assurance, Cross-site standardization, Longitudinal calibration | Essential for multi-center trials; validate measurement stability across time |
| AI Reconstruction Platforms | Deep learning reconstruction algorithms, Denoising networks | Image quality enhancement, SNR improvement at low field strengths | Can be integrated with scanner software; require validation for quantitative measurements |
| Automated Analysis Pipelines | FSL, FreeSurfer, SPM, DPABI, Tractography tools | Standardized processing of structural, functional, diffusion data | Enable high-throughput analysis; reduce analyst-induced variability |
| Clinical Rating Integration | Electronic clinical outcome assessments, Cognitive batteries | Correlation of imaging biomarkers with clinical endpoints | Synchronize assessment timing with imaging; use digital biomarkers when possible |
Portable low-field MRI systems represent a paradigm shift in how biomarkers can be integrated throughout the drug development pipeline. From demonstrating functional target engagement in early-phase trials to monoring disease progression and enriching patient populations in late-stage studies, LF-MRI provides a versatile platform for obtaining quantitative, objective measures of therapeutic effects on the brain. The accessibility, portability, and cost-effectiveness of these systems address critical limitations of conventional MRI, enabling more frequent assessment, broader patient participation, and deployment across diverse clinical settings.
As LF-MRI technology continues to advance—with improvements in AI-based reconstruction, sequence optimization, and multi-parametric imaging—its utility in drug development will expand further. Widespread adoption will require standardized acquisition protocols, validated analytical pipelines, and regulatory qualification of specific biomarkers. However, the foundation is firmly established for LF-MRI to become an indispensable tool in the development of novel therapeutics for neurological and psychiatric disorders, ultimately accelerating the delivery of effective treatments to patients worldwide.
Magnetic resonance imaging is a cornerstone of modern medical diagnostics, yet its global distribution remains markedly inequitable. Approximately 90% of the world's population lacks access to MRI, with the most severe shortages affecting low- and middle-income countries (LMICs) [15] [53]. This disparity is particularly pronounced in Sub-Saharan Africa, where the average availability falls to one MRI scanner per million people, compared to nearly 40 scanners per million in the United States [54] [55]. In West Africa, the situation is even more critical, with only 84 MRI facilities serving a population of over 370 million people [53].
The fundamental barriers to conventional high-field MRI implementation in resource-constrained environments are multifaceted. Traditional 1.5T and 3.0T systems require substantial financial investment, with acquisition costs approaching $1 million USD per tesla of field strength [1] [15]. Beyond initial purchase, these systems demand extensive infrastructure including reinforced flooring, electromagnetic shielding, stable power supplies, and cryogenic cooling systems—requirements that are often impractical in many healthcare settings [1] [15]. Additionally, the shortage of trained personnel, including radiologists, technologists, and maintenance engineers, further compounds the accessibility challenge [53] [55].
Within this context, portable low-field MRI systems represent a paradigm shift in medical imaging accessibility. Defined broadly as systems operating at field strengths below 1.5T, these technologies leverage hardware and software innovations to overcome traditional barriers while maintaining diagnostic capability for specific clinical applications [1] [15]. This technical guide examines the transformative potential of low-field MRI systems within global health, with particular emphasis on their application in clinical neuroscience research in resource-limited settings.
Technological Basis of Low-Field MRI Systems
Hardware Innovations and Physical Principles
The core technological advances enabling modern low-field MRI systems span magnet design, radiofrequency (RF) coils, and gradient systems. Unlike their high-field counterparts that predominantly use superconducting magnets requiring liquid helium cooling, contemporary low-field systems often employ compact superconducting magnets or high-performance permanent magnets that operate passively without electrical current or cryogenic support [1]. For instance, the Hyperfine Swoop system utilizes a 0.064T permanent magnet, while the Siemens Magnetom Free.Max incorporates a 0.55T compact superconducting magnet [1] [15].
These design innovations yield substantial practical advantages. Low-field systems demonstrate significantly reduced power requirements, with some portable units drawing as little as 900W—enabling operation from standard wall outlets or portable generators [56]. Their substantially lower weight (approximately 140kg for the Hyperfine Swoop versus thousands of kilograms for conventional systems) and smaller physical footprint enable novel deployment paradigms, including true portability [1] [56].
From a physics perspective, the primary trade-off for these advantages is reduced signal-to-noise ratio (SNR) at lower field strengths. While SNR is directly proportional to static magnetic field strength, recent innovations have substantially mitigated this limitation through optimized hardware design and advanced signal processing techniques [1]. Additionally, low-field systems exhibit distinct relaxivity characteristics, including shorter T1 relaxation times and reduced susceptibility artifacts, which can be advantageous for specific clinical applications, particularly near metallic implants or air-tissue interfaces [1] [15].
Software and Reconstruction Advances
Modern low-field MRI systems leverage sophisticated computational approaches to overcome inherent SNR limitations. Deep learning reconstruction algorithms have proven particularly valuable, enabling image quality that approaches diagnostic standards of higher-field systems [15] [5]. These artificial intelligence (AI)-driven techniques employ generative adversarial networks (GANs), U-Net architectures, and specialized models like LoHiResGAN to enhance image resolution, reduce noise, and generate synthetic high-field images from low-field inputs [5].
The LoHiResGAN model exemplifies this approach, incorporating ResNet components within a conditional GAN framework and utilizing a composite loss function that includes structural similarity index measure (SSIM) to preserve perceptual image quality [5]. When applied to 64mT MRI data, this method demonstrated significant improvement in normalized root-mean-squared error and peak signal-to-noise ratio compared to other state-of-the-art models, enabling more consistent brain morphometry measurements across various brain regions [5].
Additional software innovations include SNR-efficient acquisition strategies such as balanced steady-state free precession (bSSFP), MR fingerprinting, and long readout spiral imaging, which maximize information capture per unit time [15]. These approaches are particularly valuable in low-field environments where extended scan times may be impractical due to patient factors or clinical workflow constraints.
Table 1: Comparison of Representative Low-Field MRI Systems
| Manufacturer | Model | Field Strength | Key Features | Portability | Primary Applications |
|---|---|---|---|---|---|
| Hyperfine | Swoop | 0.064T | Wheel-based, battery-powered, ~140kg | Full portability | Brain imaging |
| Siemens | Magnetom Free.Max | 0.55T | Compact superconducting magnet | Limited portability | General purpose |
| Promaxo | - | 0.058-0.074T | Single-sided open configuration | Portable | Prostate interventions |
| Synaptive | Evry | 0.5T | - | Limited portability | Intraoperative |
Clinical Applications and Validation
Neuroimaging in Resource-Limited Settings
Neuroimaging represents the most extensively validated application for portable low-field MRI in resource-constrained environments. At Queen Elizabeth Central Hospital in Malawi—a tertiary care facility serving approximately one million people—implementation of a Hyperfine Swoop system demonstrated substantial clinical impact across diverse neurological conditions [56]. In a case series of 31 pediatric patients, low-field MRI provided diagnostically adequate images for conditions including cerebral abscess, intracranial tumors, sequelae of stroke, and post-traumatic abnormalities [56].
Two illustrative cases from this experience highlight the clinical utility: A 12-year-old male with head trauma underwent low-field MRI that revealed a frontal bone fracture with subdural hematoma, enabling appropriate conservative management and avoiding unnecessary surgical intervention. In a second case, a 4-year-old male presenting with coma and seizures was found to have unilateral cerebral atrophy and middle cerebral artery narrowing, redirecting the diagnostic evaluation toward chronic vasculopathy rather than acute infectious etiology [56].
These findings demonstrate that low-field MRI can provide sufficient diagnostic information to guide clinical decision-making in settings where no alternative cross-sectional imaging modalities are available. Importantly, the portability of these systems enables use in critically ill patients who cannot be transported to dedicated radiology departments [1] [56].
Beyond Neuroimaging: Expanding Applications
While neuroimaging applications are most advanced, low-field MRI technology shows promise for other clinical domains relevant to global health. In musculoskeletal imaging, the reduced susceptibility artifacts near metallic hardware make low-field systems particularly suitable for postoperative evaluation of orthopedic implants [1] [15]. For cardiac applications, though technically challenging at lower field strengths, research suggests potential for congenital heart disease assessment when combined with AI-based image enhancement techniques [55].
Interventional procedures represent another promising application. The open configuration of systems like the Promaxo prostate scanner facilitates MRI-guided biopsies and procedures without the spatial constraints of traditional closed-bore systems [15] [30]. A cost-efficiency analysis of portable low-field MRI for prostate cancer diagnosis demonstrated substantial cost savings compared to high-field systems, with comparable procedural times and potentially improved accessibility [30].
Implementation and Operational Protocols
Deployment Models and Workflow Integration
The implementation of low-field MRI systems in resource-constrained settings follows several distinct models, each with specific operational considerations:
Tertiary care center with low-field MRI only: In this scenario, exemplified by the Malawi experience, the low-field system serves as the sole cross-sectional imaging modality for neurological conditions [56]. Implementation requires minimal infrastructure modifications—primarily ensuring adequate space and standard power outlets—with operational protocols focused on appropriate patient selection and recognition of the system's diagnostic limitations.
Tertiary care center with mixed high-field and low-field systems: In this model, low-field systems complement existing high-field capabilities, serving as supplemental scanners for specific applications such as ICU monitoring, intraoperative imaging, or patients with contraindications to high-field imaging [15] [56]. Operational protocols emphasize appropriate triage between systems based on clinical question and patient factors.
Mobile deployment in peripheral healthcare facilities: The inherent portability of certain low-field systems enables truly mobile implementation, bringing MRI capabilities to remote or underserved areas [54]. The "Scan-a-van" concept—integrating a Hyperfine Swoop system into a modified cargo van—demonstrates the feasibility of this approach, with successful acquisition of diagnostic-quality images in community settings [54].
Table 2: Infrastructure Requirements: Low-Field vs. High-Field MRI
| Infrastructure Component | Conventional High-Field MRI | Portable Low-Field MRI |
|---|---|---|
| Power requirements | 480V 3-phase, dedicated electrical supply | Standard wall outlet (110V/220V), ~900W peak |
| Shielding | Dedicated radiofrequency shielding room | No fixed shielding required |
| Flooring | Reinforced flooring often required | Standard flooring adequate |
| Cooling system | Liquid helium cryogenic system | Passive cooling or standard air conditioning |
| Space requirements | Dedicated large room (>50m²) | Standard room or mobile deployment |
| Installation time | Weeks to months | Hours to days |
| Regulatory perimeter | Extensive controlled access area | Minimal safety zone |
Experimental Protocols for Technical Validation
For researchers implementing low-field MRI systems in resource-limited settings, rigorous technical validation is essential. The following protocols provide frameworks for system assessment:
Image Quality Assessment Protocol:
- Phantom imaging: Utilize standardized MRI phantoms to quantify geometric accuracy, spatial resolution, and signal-to-noise ratio across sequences [54].
- In vivo validation: Perform comparative imaging in healthy volunteers using identical sequences on both low-field and available high-field systems [5].
- Quantitative analysis: Calculate SNR, contrast-to-noise ratio (CNR), and geometric distortion metrics using established computational methods [54] [5].
- Clinical validation: Assess diagnostic concordance for relevant pathological conditions through blinded reader studies [56].
AI-Enhanced Image Reconstruction Protocol:
- Data acquisition: Acquire paired low-field and high-field datasets from the same participants using standardized imaging protocols [5].
- Preprocessing: Implement bias field correction, intensity normalization, and spatial registration using tools such as FSL or SPM [5].
- Model training: Employ appropriate deep learning architectures (e.g., LoHiResGAN, CycleGAN) for image translation, utilizing SSIM and MAE composite loss functions [5].
- Validation: Quantitatively compare synthetic high-field images to actual high-field data using normalized root-mean-squared error, SSIM, and peak signal-to-noise ratio metrics [5].
Operational Cost Considerations
The economic aspects of low-field MRI implementation differ substantially from conventional systems. Acquisition costs for low-field systems are significantly lower, estimated at 40-50% of a standard 1.5T scanner [1]. More substantial savings emerge in operational expenses: installation costs can be reduced by up to 70% due to elimination of shielding requirements and structural modifications, while annual maintenance costs may be 45% lower than high-field systems [1].
Beyond direct financial metrics, operational protocols must account for context-appropriate reimbursement models, local workforce training requirements, and sustainable service maintenance arrangements—all critical factors for long-term viability in resource-constrained environments [53] [56].
The Research Toolkit: Technical Specifications
Table 3: Essential Research Components for Low-Field MRI Implementation
| Component | Technical Specification | Research Function |
|---|---|---|
| Low-field MRI unit | 0.064T-0.55T field strength; portable or fixed installation | Primary image acquisition hardware |
| AI reconstruction platform | GPU-accelerated computing; deep learning frameworks (TensorFlow, PyTorch) | Image quality enhancement and analysis |
| Phantom validation tools | Geometric distortion phantoms; SNR measurement tools | System performance quantification |
| Data preprocessing pipeline | FSL, SPM, or custom MATLAB/Python scripts | Image registration, normalization, and cleanup |
| Mobile deployment platform | Modified vehicle with power supply; environmental monitoring | Field research in remote locations |
| Quality assurance protocol | Automated tracking of SNR, artifacts, geometric accuracy | Longitudinal system performance monitoring |
Implementation Workflow
The deployment of low-field MRI technology follows a systematic workflow from site assessment through clinical integration. The diagram below illustrates this process:
Future Directions and Research Agenda
The ongoing evolution of low-field MRI technology presents several promising research directions with particular relevance to global health applications. Continued refinement of AI-based reconstruction algorithms represents an immediate priority, with potential to further narrow the image quality gap between low-field and high-field systems [5]. Additionally, the development of application-specific pulse sequences optimized for the unique relaxivity properties of low-field systems could enhance diagnostic performance for targeted clinical indications [15].
From an implementation perspective, research should focus on sustainable service delivery models appropriate for resource-constrained environments, including context-appropriate maintenance protocols, training pathways for local technicians, and innovative financing mechanisms [53] [56]. The integration of low-field MRI with emerging telehealth platforms could further expand access through remote interpretation and decision support [55].
For clinical neuroscience research specifically, methodological work is needed to establish validated quantitative biomarkers derived from low-field systems, enabling their use in longitudinal studies and interventional trials in diverse global populations [5]. Finally, cross-disciplinary collaboration between engineers, clinical researchers, and global health implementation specialists will be essential to fully realize the potential of these technologies to address healthcare disparities in neurological care.
Portable low-field MRI systems represent a transformative approach to addressing profound global disparities in medical imaging access. Through innovative engineering and advanced computational methods, these technologies overcome traditional barriers of cost, infrastructure, and operational complexity that have previously limited MRI availability in resource-constrained settings. While technical compromises exist, particularly regarding spatial resolution and signal-to-noise ratio, clinical validation across diverse contexts demonstrates substantial diagnostic utility—especially for neurological applications.
For clinical neuroscience researchers working in global health contexts, low-field MRI offers unprecedented opportunities to study brain health and disease in previously inaccessible populations. The ongoing development of this technology, particularly through AI-enhanced image reconstruction and optimized acquisition protocols, promises continued improvement in diagnostic capabilities. When implemented through thoughtful, context-appropriate models that address local needs and constraints, low-field MRI systems have significant potential to advance both clinical care and research equity in neurology worldwide.
Overcoming Technical Hurdles: Strategies for Enhancing Low-Field MRI Performance
The resurgence of portable low-field MRI (LF-MRI) systems represents a paradigm shift in making magnetic resonance imaging accessible for global clinical neuroscience research [8]. A primary obstacle to the widespread adoption of this technology is the inherent low signal-to-noise ratio (SNR) at reduced magnetic field strengths [1] [23]. Whereas high-field systems benefit from greater net magnetization, the signal in ultra-low-field (ULF-MRI) systems, typically operating below 0.2 Tesla, is significantly diminished, traditionally resulting in images with lower spatial resolution and reduced clarity [23]. However, the convergence of advanced hardware engineering, sophisticated acquisition physics, and artificial intelligence (AI)-driven software solutions is systematically closing this performance gap [1]. This technical guide examines the current state of denoising and AI-based image reconstruction techniques that are essential for enhancing the diagnostic and research utility of portable low-field MRI systems in neuroscience.
Core Technical Approaches to SNR Enhancement
Native Noise Modeling and Denoising
A significant innovation in low-field MRI denoising involves moving beyond simple Gaussian noise models to capture the true Rician distribution of noise found in actual LF-MRI data [57]. The Native Noise Denoising (NND) approach leverages the inherent noise characteristics from acquired low-field images themselves. The methodology involves obtaining noise profiles from corner patches of low-field images and iteratively adding statistically similar noise to high-field images to create a paired noisy-clean dataset for training [57]. This process results in a robust training set that enables deep learning models to learn more effective filtering for real-world low-field conditions.
Quantitative Performance: When applied to very low-field data (0.05T), the NND approach has demonstrated substantial improvements, achieving SNR enhancements of 32.76% on the M4Raw dataset (0.3T), 19.02% on in vivo brain MRI (0.05T), and 8.16% on phantom images (0.05T) [57]. Qualitative assessments through difference maps and line intensity plots further confirm that NND preserves structural details and edges more effectively than methods trained on random Gaussian noise [57].
Deep Learning Reconstruction Frameworks
Deep learning has revolutionized MRI reconstruction by enabling accelerated acquisition and improved image quality without sacrificing diagnostic fidelity [26]. Neural networks can be trained to reconstruct high-quality images from substantially undersampled k-space data, dramatically reducing scan times while maintaining diagnostic quality [25] [26].
Innovative Architectures: Recent research presented at the ISMRM 2025 conference highlights several advanced frameworks:
- Noise-Adaptive MRI Denoising Using Self-Supervised Learning: This approach utilizes an Average-to-Average (Avg2Avg) loss function that could greatly encourage the use of 0.55T MRI and other low-SNR scanners [25].
- Physics-Coupled Synthetic Data Generation: This method generates physics-informed synthetic data from natural images, enabling effective complex MRI denoising without in-vivo data, thus addressing practical challenges in data collection [25].
- Dual-Branch Joint Training Framework: An unsupervised approach for reconstructing highly undersampled 3D cones cardiac image navigators, showing promise for scenarios where fully sampled data is unavailable [25].
Table 1: Quantitative Performance of Advanced Denoising Techniques
| Technique | Field Strength | SNR Improvement | Key Innovation | Application Context |
|---|---|---|---|---|
| Native Noise Denoising (NND) [57] | 0.05T | 19.02% (in vivo) | Leverages native Rician noise characteristics from LF-MRI | Brain imaging, phantom studies |
| Noise-Adaptive Self-Supervised Learning [25] | 0.55T | Not specified | Avg2Avg loss function without clean reference | General low-SNR MRI environments |
| Physics-Coupled Synthetic Data [25] | Multi-field | Performance par with in-vivo-trained models | Generates data from natural images without in-vivo scans | Data-scarce environments |
| Deep-ERx2 [25] | 3T & 7T | Enables high-resolution (3.4 mm isotropic) | Deep learning reconstruction for spectroscopic imaging | Metabolic imaging with clinical feasibility |
Integrated Hardware and Software Solutions
The performance gap between low-field and high-field systems is being addressed through co-optimization of hardware and software. Modern low-field systems incorporate compact superconducting magnets or high-performance permanent magnets that do not require active cooling or substantial electricity [1]. Simultaneously, optimized RF coil design through superconducting coils or multimodal surface coils minimizes resistance and thermal noise, improving the fundamental signal capture [1].
The integration of AI-based post-processing with enhanced hardware has enabled applications such as the "TomoBrain" approach for brain volumetry, where combining orthogonal imaging directions for T2-weighted images forms a higher resolution image volume suitable for quantitative neuroimaging biomarkers [14]. This integration has demonstrated "strong" within-subject correlation across magnetic field strengths and "good to excellent" within-subject repeatability at ultra-low field, making it viable for population-level brain research [14].
Experimental Protocols and Methodologies
Native Noise Denoising Protocol
The NND methodology follows a structured pipeline with three distinct stages [57]:
Noise Modeling Phase: Determine noise characteristics of target LF-MRI images by analyzing pixel intensity distributions from corner patches of actual low-field images, which typically follow a Rician distribution rather than Gaussian.
Training Data Generation: Iteratively add the characterized native noise to high-field complex images, monitoring SNR at each step until the simulated low-field images match the target SNR characteristics of real low-field data.
Model Training and Inference: Train a U-Net based denoising autoencoder on the paired dataset using a patch-wise approach where N×N patches are randomly extracted, then apply the trained model to full low-field images for denoising.
This protocol emphasizes the importance of iterative noise matching rather than single-step addition to account for variations in signal levels across different images, even from the same scanner [57].
AI-Based Reconstruction for Quantitative Mapping
A protocol presented for cardiac imaging at 0.55T demonstrates how AI enables comprehensive quantitative mapping within clinically feasible breath-hold periods [25]:
Acquisition: Implement a single breath-hold, 16-heartbeat sequence using a dual rosette trajectory Magnetic Resonance Fingerprinting (MRF) acquisition.
Reconstruction: Apply a deep image prior reconstruction algorithm to simultaneously generate T1, T2, T2*, and proton density fat fraction maps from the highly accelerated acquisition.
This approach reduces both the time and number of breathholds required for a comprehensive cardiac scan, addressing a major limitation in quantitative MRI assessment [25].
Multi-Plane Acquisition for Volumetric Analysis
The "TomoBrain" protocol for accurate brain volumetry at ultra-low fields involves [14]:
Multi-Plane Acquisition: Obtain T1- and T2-weighted brain images in axial, coronal, and sagittal planes using a portable 0.064T scanner (Hyperfine Swoop).
Image Integration: Combine orthogonal imaging directions, particularly for T2-weighted images, to form a higher resolution image volume.
Deep Learning Segmentation: Apply specialized tools (SynthSR and SynthSeg) to boost resolution and provide automatic segmentation without extensive training data.
This protocol specifically notes that T2-weighted images consistently show higher correlation, agreement, and repeatability than T1-weighted counterparts at ultra-low field strengths [14].
Visualization of Methodologies
Native Noise Denoising Workflow
Diagram 1: Native noise denoising workflow for LF-MRI.
Deep Learning Reconstruction Pipeline
Diagram 2: AI-based reconstruction pipeline for accelerated LF-MRI.
Table 2: Essential Research Reagents and Computational Tools for LF-MRI Enhancement
| Tool/Resource | Type | Function/Purpose | Example Implementation |
|---|---|---|---|
| Native Noise Modeling | Algorithm | Models true Rician noise distribution from LF-MRI data | Extract noise from corner patches of 0.05T images [57] |
| U-Net Architecture | Deep Learning Model | Denoising autoencoder for image enhancement | Patch-wise training on simulated noisy-clean pairs [57] |
| SynthSR & SynthSeg | Software Tools | MRI resolution boosting and automatic segmentation | Brain volumetry from ultra-low-field images [14] |
| Dual Rosette Trajectory MRF | Acquisition Protocol | Enables rapid multi-parametric mapping | Cardiac T1, T2, T2*, fat fraction in single breathhold [25] |
| Hyperfine Swoop | Portable MRI Hardware | 0.064T portable scanner for point-of-care imaging | TomoBrain protocol for multi-plane acquisition [14] |
| Physics-Coupled Synthetic Data Generator | Data Simulation | Creates training data without in-vivo scans | Using natural images with MR physics constraints [25] |
| Self-Supervised Learning with Avg2Avg Loss | Training Framework | Denoising without clean reference data | Noise-adaptive reconstruction for 0.55T MRI [25] |
The integration of advanced denoising techniques and AI-based reconstruction represents a transformative development for portable low-field MRI systems in clinical neuroscience research. Methods such as native noise modeling, which accounts for the true Rician distribution of noise in LF-MRI, and sophisticated deep learning architectures that enable rapid, high-quality reconstruction from undersampled data are systematically addressing the fundamental challenge of low SNR. When combined with hardware innovations and optimized acquisition protocols like the TomoBrain approach for multi-plane imaging, these computational advances are establishing ultra-low-field MRI as a viable platform for quantitative neuroimaging research. As these technologies continue to mature, they hold the potential to democratize access to MRI worldwide, enabling large-scale population studies and clinical neuroscience research in diverse and resource-limited settings previously excluded from the neuroimaging revolution.
Portable low-field Magnetic Resonance Imaging (MRI) systems are catalyzing a paradigm shift in clinical neuroscience research, enabling point-of-care and remote neuroimaging. This transformation is largely driven by significant hardware innovations that counter the traditional limitations of low-field systems, particularly low signal-to-noise ratio (SNR) and field inhomogeneity. These innovations focus on the three core subsystems that define an MRI scanner's performance: the permanent magnet arrays generating the static magnetic field (B₀), the radiofrequency (RF) coils responsible for signal transmission and reception, and the gradient systems enabling spatial encoding. For researchers and drug development professionals, understanding these technological advances is critical for deploying these systems in clinical trials, biomarker discovery, and therapeutic monitoring. This whitepaper provides an in-depth technical analysis of the latest hardware advancements, complete with quantitative performance data and experimental methodologies, framing them within the context of modern neuroscience applications.
Permanent Magnet Designs
The permanent magnet is the cornerstone of a portable, low-field MRI system, defining its fundamental field strength and homogeneity. Recent designs have moved beyond traditional Halbach cylinders to optimize field strength, homogeneity, and manufacturability for brain-specific imaging.
Asymmetric and Polygonal Arrays
A key innovation is the development of asymmetric permanent magnet arrays. One design for a portable MR head imager combines elliptical and circular magnet elements in an asymmetric arrangement. This configuration achieves a field strength of 55 mT with an initial inhomogeneity of 16984 ppm within a 20 cm diameter spherical volume (DSV). After the application of shim magnets, the inhomogeneity is dramatically reduced to 3665 ppm, making it viable for diagnostic brain imaging [58]. The primary goal of this approach is to significantly improve field homogeneity while simplifying the manufacturing process, a critical consideration for commercial production.
Another frontier involves exploring novel geometries. Research into polygonal Halbach arrays and other hybrid shapes lays the groundwork for layered arrays that can produce stronger and more homogeneous fields. These designs are supported by mathematical formulas that enable the optimization of magnet cross-sections, opening new avenues for compact and efficient magnet design [4].
Practical Design Considerations and Performance Characterization
Transitioning from an ideal numerical model to a real-world magnet array introduces practical challenges. A critical analysis of very-low-field MRI scanners highlights that the spatial homogeneity of the B₀ field is highly sensitive to factors such as manufacturing tolerances, material imperfections, and the numerical approximations used in design simulations. Discrepancies between theoretical expectations and measured performance on fabricated magnets are a key focus, underscoring the importance of using high-fidelity models that account for real-world physical constraints [59].
Furthermore, the performance of permanent magnets is not static; it is susceptible to environmental factors. Thermal dependence poses a significant challenge, as B₀ drift can occur with temperature fluctuations, particularly affecting balanced steady-state free precession (bSSFP) sequences. An experimental study demonstrated that active water cooling of the magnets themselves provides an effective solution to stabilize the B₀ field, ensuring consistent image quality [4].
Table 1: Performance Metrics of Advanced Permanent Magnet Designs
| Magnet Design Type | Reported Field Strength (B₀) | Initial Inhomogeneity (ppm) | Post-Shimming Inhomogeneity (ppm) | Key Innovation |
|---|---|---|---|---|
| Asymmetric Array [58] | 55 mT | 16,984 (within 20cm DSV) | 3,665 (within 20cm DSV) | Combination of elliptical and circular elements |
| Polygonal Halbach Array [4] | Information Not Specified | Information Not Specified | Information Not Specified | Layered arrays with versatile polygonal cross-sections |
| Single-Sided "Helmet" Magnet [4] | 50 mT | Information Not Specified | Information Not Specified | 7 kg weight, built-in 50 mT/m gradient for readout |
Radiofrequency (RF) Coils
In low-field MRI, the RF coil is paramount for achieving adequate SNR. Innovations here focus on enhancing transmit/receive efficiency and mitigating the heightened sensitivity to electromagnetic interference (EMI) encountered in unshielded environments.
Toroidal Coils for EMI Rejection
A groundbreaking design is the toroidal RF volume coil, inspired by anapole structures. This coil consists of six rings, each containing four continuous wires wound around an elliptical 3D-printed former, creating an uninterrupted wire structure. It is designed for systems with an axial B₀ field direction [60].
The primary advantage of this design is its intrinsic immunity to EMI. When evaluated on a 47 mT Halbach array system for neuroimaging, the toroidal coil—used in combination with a grounding belt wrapped around the subject—achieved a noise level comparable to a widely used spiral head coil that required additional passive aluminum shielding. Crucially, it maintained comparable transmit and receive efficiency [60]. This demonstrates that the toroidal coil can potentially eliminate or reduce the need for bulky passive shielding or complex post-processing algorithms to suppress EMI, a significant step toward true portability.
Local Transmit Resonators
For specific applications, such as abdominal imaging with single-sided low-field systems, localized RF resonators offer a solution to limitations in B₁⁺-field strength and penetration depth. One innovation is a local transmit RF-resonator that enhances transmit efficiency within a targeted region. This design improves image quality and enables deeper, more effective imaging in challenging anatomical areas, expanding the clinical utility of open, low-field systems [4].
Gradient Systems
Gradient performance is a major determinant of image resolution, acquisition speed, and the feasibility of advanced sequences like diffusion MRI. Innovations in gradient systems for portable MRI are occurring alongside revolutionary advances in high-field systems for neuroscience.
Ultra-High Performance Head-Only Gradients
The Connectome 2.0 scanner exemplifies the extreme of gradient performance, targeting mesoscopic connectomics. Its gradient system is a asymmetric, head-only coil with a three-layer geometry. It achieves a remarkable gradient strength of 500 mT/m and a slew rate of 600 T/m/s, representing a fivefold performance increase over state-of-the-art clinical scanners [61].
Key engineering innovations include:
- PNS Balancing: The use of an intermediate coil winding layer allowed for reshaping magnetic fields to raise peripheral nerve stimulation (PNS) thresholds. This design increased the worst-case PNS threshold by 41%, maximizing the usable gradient performance without causing patient discomfort [61].
- Compact Design: A smaller inner diameter of 44 cm, compared to the 61 cm of the earlier Connectome 1.0 scanner, resulted in a 30% higher gradient sensitivity (0.42 mT/m/A). This higher efficiency reduces the demands on gradient amplifiers [61].
Gradient Amplifiers and Portable System Integration
For truly portable low-field systems, the supporting electronics must also be miniaturized. Innovations in eGaN (enhanced Gallium Nitride) transistor-based gradient amplifiers are addressing this need. These designs shrink the size and cost of amplifiers while suppressing noise by switching at an optimized frequency that avoids interference with the Larmor frequency. Such improvements are critical for enhancing the overall mobility and accessibility of low-field MRI [4].
Table 2: Key Specifications of Advanced Gradient Systems
| Gradient System | Maximum Strength (mT/m) | Maximum Slew Rate (T/m/s) | Inner Diameter | Key Feature |
|---|---|---|---|---|
| Connectome 2.0 Scanner [61] | 500 | 600 | 44 cm | 3-layer asymmetric head-only coil; PNS balancing |
| Typical Clinical Scanner [61] | 40 - 80 | ~200 | ~60 cm (whole-body) | Standard whole-body gradient performance |
| Portable System eGaN Amplifier [4] | Information Not Specified | Information Not Specified | Information Not Specified | Reduced size/cost; optimized switch-mode operation |
Experimental Protocols for System Validation
Rigorous experimental validation is essential to quantify the performance of these hardware innovations. The following protocols are derived from the cited research.
Protocol 1: Validating B₀ Homogeneity and Shimming
This protocol is based on the methodology for characterizing an asymmetric permanent magnet array [58].
- Magnet Characterization: Place the fabricated permanent magnet array on a non-magnetic bench. Using a 3-axis Gauss meter and a precision robotic arm, map the B₀ field inside the imaging volume, focusing on a 20 cm DSV.
- Field Inhomogeneity Calculation: Compute the initial field inhomogeneity in parts per million (ppm) from the field map data.
- Passive Shimming: Introduce small, strategically placed shim magnets into the array structure. Re-map the B₀ field to measure the new field profile.
- Performance Metric: Calculate the post-shimming inhomogeneity (ppm). The reported result was a reduction from 16,984 ppm to 3,665 ppm [58].
Protocol 2: Evaluating RF Coil EMI Performance
This protocol details the evaluation of a toroidal RF coil's noise rejection capability [60].
- Experimental Setup: Install the prototype toroidal RF coil on a Halbach array MRI system operating at 47 mT. For comparison, install a standard spiral head coil on the same system.
- Noise Measurement: Acquire MRI data without a subject present. For the toroidal coil, use a grounding belt. For the spiral coil, use both a grounding belt and passive aluminum shielding.
- In Vivo Validation: Image a human subject with both coil setups, ensuring the use of the respective grounding/shielding methods for each.
- Performance Metric: Compare the noise levels in the background of the images and the SNR within the brain tissue. The toroidal coil with a grounding belt should achieve noise levels comparable to the spiral coil with grounding and shielding [60].
Visualization of Hardware Integration and Validation
The following diagram illustrates the relationship between the core hardware components and the experimental workflow for validating a portable low-field MRI system.
The Scientist's Toolkit: Research Reagent Solutions
For researchers aiming to implement or validate these hardware innovations, the following table details essential "research reagents" and their functions in this context.
Table 3: Essential Research Materials for Low-Field MRI Hardware Development
| Item / Material | Function / Role in R&D | Example Context |
|---|---|---|
| High-Performance Permanent Magnets (e.g., Ndfeb) | To construct arrays that generate a strong and stable static B₀ field. | The core building block of Halbach, asymmetric, and polygonal magnet arrays [58] [4]. |
| 3D-Printed Coil Formers | To provide a custom, lightweight, and precise mechanical structure for winding RF coils. | Used for creating the elliptical former for the toroidal RF coil [60]. |
| Passive Shim Magnets | Small magnets used to fine-tune the magnetic field and improve its homogeneity. | Critical for reducing B₀ inhomogeneity from over 16,000 ppm to under 4,000 ppm [58]. |
| eGaN Transistors | Semiconductor components for building compact, efficient, and low-noise gradient power amplifiers. | Enable the design of smaller gradient amplifiers for portable systems [4]. |
| Active Cooling Systems | To regulate the temperature of permanent magnets, stabilizing the B₀ field against thermal drift. | A water-cooling system was used to mitigate B₀ drift in Halbach arrays [4]. |
| Grounding Belts / EMI Shields | Materials and devices used to manage electromagnetic interference from the environment. | A grounding belt was used with the toroidal coil; aluminum shielding was a baseline for the spiral coil [60]. |
The concerted advancement of permanent magnet designs, RF coils, and gradient systems is transforming portable low-field MRI from a concept of limited utility into a powerful tool for clinical neuroscience. Asymmetric and polygonal magnet arrays provide the foundational field with improved homogeneity; toroidal and local RF coils deliver enhanced signal integrity and EMI resilience; and novel gradient technologies enable faster and higher-resolution encoding. For researchers and drug developers, these hardware innovations open new possibilities for conducting neuroimaging studies directly at the point-of-care, in resource-limited settings, and for monitoring patients over time with reduced cost and complexity. This technological progress promises to democratize access to high-quality MRI, thereby accelerating research into neurological disorders and expanding the horizons of brain health assessment.
In magnetic resonance imaging (MRI), soft tissue contrast is primarily governed by the manipulation of spin-lattice (T1), spin-spin (T2), and effective spin-spin (T2) relaxation times. Pulse sequence optimization is the process of tailoring radiofrequency (RF) pulses, gradient waveforms, and signal readout parameters to accentuate these relaxation differences for specific diagnostic purposes. In the context of portable low-field MRI systems, which operate at magnetic field strengths below 0.2 T to 0.55 T, this optimization becomes critically important [1] [23]. These systems face inherent challenges, including a lower signal-to-noise ratio (SNR) and reduced contrast-to-noise ratio (CNR) compared to their high-field counterparts [23]. However, they also offer distinct advantages for clinical neuroscience research, such as reduced susceptibility artifacts, greater accessibility for point-of-care studies, and enhanced patient safety, particularly for individuals with metallic implants [1] [40]. This technical guide details the core principles and advanced methodologies for optimizing T1, T2, and T2 weighting to maximize diagnostic utility in portable low-field MRI systems, providing a framework for researchers and drug development professionals working to validate these technologies for neurodegenerative disease tracking.
Foundational Physics of Tissue Contrast and Low-Field Considerations
Relaxation Mechanisms and Contrast Weighting
- T1-Weighting: T1 relaxation is the process by which spins recover their longitudinal magnetization after an RF excitation. T1-weighted (T1w) sequences are optimized to maximize signal differences based on tissue-specific T1 recovery rates. At lower field strengths, T1 relaxation times are generally shorter, which must be accounted for during sequence timing selection [23].
- T2-Weighting: T2 relaxation describes the loss of phase coherence among spins in the transverse plane. T2-weighted (T2w) sequences are designed to highlight differences in this decay. T2 values are less dependent on field strength, making T2w contrasts relatively more stable across different platforms [62].
- T2-Weighting: T2 relaxation incorporates the irreversible T2 decay with reversible dephasing caused by local magnetic field inhomogeneities. T2-weighted sequences, such as those used in susceptibility-weighted imaging (SWI), are highly sensitive to blood products and calcification. A significant advantage of low-field MRI is the reduction of susceptibility artifacts, which mitigates the signal loss and distortion that can plague T2-weighted imaging at high fields [1] [23].
The Low-Field Challenge: SNR and Acquisition Time
The fundamental relationship between field strength (B₀) and signal imposes practical constraints on low-field imaging. The signal is proportional to B₀², while the acquisition time required to maintain a constant SNR increases supra-linearly as the field strength decreases [23]. The acquisition time (T_ACQ) scales as follows:
TACQ,L = ( (B0,H) / (B0,L) )^(2 • powereff) • TACQ,H
Here, powereff is a contrast-dependent coefficient (e.g., ~1.04 for T2*-weighted and ~0.90 for T1-weighted images) [23]. Consequently, pulse sequence optimization at low field must not only manipulate contrast but also strategically balance scan time, resolution, and SNR.
Optimization Strategies for Core Contrast Weightings
T1-Weighting Optimization
For low-field systems, T1w optimization often employs spoiled gradient echo (SGRE) sequences due to their speed and volumetric (3D) acquisition capability.
- Parameter Adjustment: The flip angle (α) and repetition time (TR) are the primary levers for T1 weighting. The flip angle can be optimized using the Ernst angle formula, which provides the angle that maximizes signal for a given T1 and TR: α_Ernst = arccos(e^(-TR/T1)) [63]. At low field, with shorter T1 values, the optimal Ernst angles are typically larger than those used at high field for the same TR.
- Advanced Methodologies: A novel approach for low-field systems involves RF phase-modulated GRE imaging. Using small, specific RF phase increments (e.g., 1-3°), this method can encode T1-weighted contrast into the imaginary component of the complex signal. This technique is particularly powerful as it allows for the simultaneous acquisition of T1w and T2w contrasts from a single scan, a significant efficiency gain for low-field protocols [62].
Table 1: Key Parameters for T1-Weighting Optimization in Low-Field SGRE
| Parameter | Impact on Contrast | Low-Field Consideration | Typical Range (Low-Field) |
|---|---|---|---|
| Flip Angle (α) | Lower angles reduce T1-weighting; use Ernst angle for max signal. | Shorter tissue T1 values push the Ernst angle higher. | 20° - 80° |
| Repetition Time (TR) | Shorter TR increases T1-weighting. | Can use shorter TR than high-field due to shorter T1, speeding up scans. | 10 - 50 ms |
| RF Phase Increment (θ) | Large increments (>10°) yield standard T1w; small increments (1-3°) enable simultaneous T1w/T2w. | Critical parameter for advanced multi-contrast sequences. | 1° - 30° |
| Echo Time (TE) | Should be as short as possible to minimize T2* contamination. | Minimizing TE is crucial to combat lower inherent SNR. | 2 - 5 ms |
T2-Weighting Optimization
Traditional T2w imaging relies on spin-echo (SE) or fast spin-echo (FSE) sequences, but these can be time-consuming, especially for 3D acquisitions at low field.
- Parameter Adjustment: The echo time (TE) is the dominant parameter for T2 weighting. To achieve heavy T2 weighting, the TE should be on the order of the T2 values of the tissues of interest. However, at low field, long TEs exacerbate SNR penalties.
- Advanced Methodologies: The aforementioned RF phase-modulated GRE with small phase increments encodes T2-weighted contrast into the real component of the signal [62]. Dual-echo steady-state (DESS) is another efficient 3D sequence that can be optimized for T2w fluid attenuation at ultra-high fields, and its principles are being adapted for low-field use to provide robust fluid signal [64]. Furthermore, AI-driven pulse sequence discovery frameworks are now being used to generate novel sequences that maximize T2 contrast within the physical constraints of low-field scanners [65].
T2*-Weighting and Fluid-Attenuated Imaging
- T2-Weighting: Achieved using relatively long TE in a GRE sequence. At low field, the longer T2 values and reduced susceptibility artifacts make this weighting more robust near tissue-air interfaces or metallic implants, albeit with a lower dynamic range for detecting subtle susceptibility effects [1].
- FLAIR at Low-Field: T2-weighted Fluid-Attenuated Inversion Recovery (FLAIR) is essential in neuroimaging for nulling the CSF signal and highlighting periventricular lesions. Implementing FLAIR at low field requires careful optimization of the inversion time (TI) to account for the field-strength dependence of T1. Machine learning pipelines, such as those developed for Alzheimer's disease evaluation, have successfully synthesized FLAIR-like contrasts and automated the quantification of white matter hyperintensities from low-field images [40].
Experimental Protocols for Low-Field Contrast Validation
Protocol 1: Simultaneous T1w and T2w 3D Imaging
This protocol is based on the RF phase-modulated GRE method, which is highly efficient for low-field systems [62].
- Pulse Sequence: 3D RF phase-modulated Gradient Echo.
- Core Parameters: TR = 6-10 ms, TE = Min full, Flip Angle = 15°-25°, RF Phase Increment (θ) = 2°.
- Background Phase Removal: Acquire two passes of the sequence with opposite RF phase increments (e.g., +θ and -θ). Perform a phase subtraction to eliminate time-independent background phase shifts from system imperfections.
- Contrast Extraction: Following acquisition and reconstruction:
- The T2-weighted image is derived from the Real component of the complex signal.
- The T1-weighted image is derived from the Imaginary component of the complex signal.
- Validation: Compare the relative signal intensity of brain tissues (GM, WM, CSF) against simulations and conventional T1w and T2w fast spin-echo images acquired in the same session [62].
Protocol 2: Automated Sequence Optimization Framework
This protocol uses a closed-loop, derivative-free optimization algorithm to tailor sequences for specific low-field applications, such as maximizing tumor-to-tissue contrast [66].
- Phantom: Use a phantom with multiple tissue-mimicking inserts covering a range of T1 and T2 values relevant to the brain.
- Algorithm Setup: Employ a Covariance Matrix Adaptation Evolution Strategy (CMA-ES) or a Genetic Algorithm (GA). CMA-ES is preferred due to faster convergence [66].
- Parametrization: Define a set of mutable pulse sequence parameters (e.g., TR, TE, α, inversion times) within the optimization algorithm.
- Cost Function: The algorithm's goal is to minimize a cost function. Two common goals are:
- Contrast Matching: Minimize the mean-square error between the acquired image and a target image with desired contrast.
- Contrast Maximization: Maximize the signal difference (contrast) between two specified tissue types in the phantom.
- Iteration: The algorithm repeatedly updates the sequence parameters, executes the sequence on the scanner, acquires new data, and computes the cost function until convergence is reached [66].
The workflow for this automated optimization is outlined below.
Protocol 3: Machine Learning-Enhanced Morphometry for Neurodegeneration
This protocol validates T1w sequences for quantifying brain volume loss in conditions like Alzheimer's disease [40].
- Acquisition: Acquire 3D T1w images on the portable low-field scanner. For optimal results, use an isotropic voxel size of ≤ 3 mm. Acquisition times can range from 2 to 10 minutes depending on the sequence and resolution [40].
- Super-Resolution and Contrast Synthesis: Process the native low-resolution, low-SNR T1w images through a machine learning pipeline (e.g., LF-SynthSR v2). This tool synthetically generates a high-resolution (1 mm isotropic), T1w MP-RAGE-like image from the low-field input [40].
- Automated Segmentation: Feed the synthesized high-resolution image into a robust segmentation tool (e.g., SynthSeg) to obtain volumetric measures of key structures like the hippocampus, lateral ventricles, and whole brain [40].
- Validation: Compare the volumes obtained from the low-field pipeline against "ground truth" segmentations from conventional 3T MRI using metrics like correlation, absolute symmetrized percent difference (ASPD), and Dice similarity coefficient for spatial overlap [40].
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful pulse sequence optimization and validation for low-field MRI requires a combination of physical tools and computational resources.
Table 2: Essential Research Toolkit for Low-Field MRI Sequence Development
| Tool / Material | Function / Description | Relevance to Low-Field Optimization |
|---|---|---|
| Multi-Contrast Phantom | An object with inserts of known, stable T1 and T2 values used for calibration and validation. | Essential for initial sequence testing, optimizing contrast, and monitoring scanner performance without subject variability. |
| Open-Sequence Platform | Software (e.g., Pulseq, gammaSTAR) that allows full control over sequence timing, shapes, and gradients. | Critical for implementing novel sequences like RF phase-modulated GRE or vendor-agnostic optimized protocols [65] [64]. |
| AI-Based Reconstruction Tools | Machine learning algorithms for denoising, super-resolution, and synthetic contrast generation. | Mitigates low SNR and resolution; enables volumetric analysis from low-field images (e.g., LF-SynthSR) [40]. |
| Derivative-Free Optimization Library | Software implementing algorithms like CMA-ES or Genetic Algorithms. | Automates the search for optimal sequence parameters for a specific diagnostic task on a given scanner [66]. |
| Normative Relaxometry Database | A database of published, peer-reviewed T1 and T2 values for normal human tissues. | Informs realistic parameter bounds for simulations and optimization (e.g., mriToolbox Parameter Database) [63]. |
The optimization of T1, T2, and T2* weighting is not merely a technical exercise but a fundamental requirement for unlocking the full potential of portable low-field MRI in clinical neuroscience research. By leveraging advanced techniques such as RF phase modulation for simultaneous multi-contrast acquisition, AI-driven super-resolution for morphometry, and automated frameworks for task-specific optimization, researchers can overcome the inherent SNR limitations of low-field systems. The experimental protocols and tools detailed in this guide provide a roadmap for developing and validating robust, diagnostically powerful imaging sequences. As these technologies mature, they promise to democratize high-quality MRI, enabling large-scale longitudinal studies and therapeutic monitoring in diverse, real-world settings from clinics to homes, thereby transforming the landscape of neurological drug development and patient care.
In clinical neuroscience research, magnetic resonance imaging (MRI) is indispensable for visualizing brain structure and function. However, a fundamental trade-off exists between imaging time, signal-to-noise ratio (SNR), and spatial resolution [67]. For portable low-field MRI systems, which are gaining prominence for their accessibility and point-of-care capabilities, managing this balance is paramount. These systems, often defined as operating at field strengths below 0.1 T to 0.55 T, inherently face challenges with lower SNR and potential limitations in spatial resolution compared to high-field counterparts [1] [15] [68]. The drive towards portable and low-field MRI is fueled by the need to expand global access to neuroimaging, enable in-home or bedside monitoring, and reduce the costs and infrastructure demands associated with high-field systems [1] [9]. This technical guide details the strategies and methodologies for optimizing acquisition protocols on low-field systems to achieve a diagnostically viable balance between scan duration and image quality, thereby facilitating their effective use in clinical neuroscience and drug development research.
Fundamental Trade-offs in Low-Field MRI Acquisition
The performance of any MRI system is governed by a core set of physical principles. In low-field MRI, these principles present distinct challenges and opportunities that must be understood to optimize acquisition protocols.
- Signal-to-Noise Ratio (SNR) and Field Strength: SNR is directly proportional to the strength of the static magnetic field (B₀) [1]. Low-field systems (e.g., 0.055 T, 0.064 T) inherently produce a lower signal than high-field systems (1.5 T, 3 T). This lower SNR must be managed to produce clinically useful images [5] [9].
- The Time-Resolution-SNR Triangle: A fundamental triangle of trade-offs exists between scan time, spatial resolution, and SNR [67]. For a constant SNR, increasing spatial resolution necessitates a longer scan time. Conversely, to decrease scan time while maintaining resolution, SNR must be sacrificed, leading to noisier images. Low-field MRI accentuates these trade-offs, making strategic protocol adjustments critical.
- Inherent Advantages of Low-Field: Despite SNR challenges, low-field MRI offers unique benefits valuable for clinical research. These include reduced susceptibility artifacts, which is advantageous for imaging near metallic implants or air-tissue interfaces; lower acoustic noise; improved patient comfort and reduced claustrophobia due to more open designs; and significantly lower costs for acquisition, installation, and maintenance [1] [15] [68].
Table 1: Key Advantages and Mitigation Strategies for Low-Field MRI
| Advantage | Technical Detail | Research Implication |
|---|---|---|
| Portability & Accessibility | Compact footprint, lower weight, no cryogenics, can operate from standard power outlets [1] [9]. | Enables point-of-care and in-home neuroimaging, facilitates research in remote or resource-limited settings [1] [5]. |
| Reduced Susceptibility Artifacts | Lower B₀ field strength minimizes magnetic susceptibility differences between tissues and implants [1] [15]. | Improved imaging for patients with orthopedic hardware or other implants; reduced artifacts near sinuses. |
| Patient Comfort & Safety | Quieter operation, open bore designs, reduced specific absorption rate (SAR) [1] [15]. | Higher participant tolerance, fewer scan terminations, safer for certain implanted devices, ideal for pediatric and claustrophobic populations. |
| Lower Operational Cost | Cheaper to manufacture, purchase, install, and maintain. Reduced infrastructure and siting requirements [1] [15]. | Makes longitudinal studies and large-scale population screening more economically feasible. |
Protocol Optimization for Time Management
Optimizing pulse sequence parameters is the most direct method for balancing scan time and image quality. A 2023 study on a 1.5 T system provides a quantitative framework for this optimization, the principles of which are directly applicable to low-field systems [69].
Key Modifiable Parameters and Experimental Findings
The study systematically altered specific parameters in a T2-weighted Turbo Spin Echo (TSE) brain protocol to assess their impact on scan time. The original protocol (FOV 230 mm, FOV phase 90%, phase oversampling 0%) had a scan time of 3.47 minutes. A modified protocol (FOV 217 mm, FOV phase 93.98%, phase oversampling 13.96%) achieved a diagnostically viable scan in 2.18 minutes, a 37% reduction in acquisition time [69].
Statistical analysis of the results revealed that not all parameters equally impacted scan duration [69]:
- FOV Phase and Phase Oversampling: These parameters had a highly significant impact on scan time (p < 0.001). Increasing the FOV phase percentage and phase oversampling directly increased the number of phase encoding steps, thereby lengthening the scan.
- Field of View (FOV) and Cross-talk: Changes in these parameters showed no statistically significant direct effect on scan time (p=0.716 and p=0.215, respectively). However, reducing the FOV can increase spatial resolution but also raises the likelihood of aliasing artifacts.
Table 2: Impact of Technical Parameters on Scan Time and Image Quality [69]
| Parameter | Impact on Scan Time | Impact on Image Quality | Recommendation for Low-Field Optimization |
|---|---|---|---|
| FOV Phase | Highly Significant (p<0.001) | Directly influences spatial resolution in the phase encoding direction. | Carefully optimize to the minimum required value to avoid unnecessary time increases. |
| Phase Oversampling | Highly Significant (p<0.001) | Prevents wrap-around (aliasing) artifacts. | Use judiciously; only increase from 0% if aliasing is observed. |
| Field of View (FOV) | Not Significant (p=0.716) | Smaller FOV increases spatial resolution but may cause aliasing. | Reduce to increase resolution, but monitor for aliasing artifacts. |
| Slice Thickness | Not Directly Measured | Thicker slices increase SNR but cause partial volume averaging, blurring fine details. | Balance is key. Use thinner slices for high-contrast structures and thicker slices for SNR-starved sequences. |
| Number of Slices | Not Directly Measured | More slices provide greater anatomical coverage but require more time. | Set to cover the required anatomy without excessive overlap or gaps. |
Experimental Protocol for Parameter Optimization
Objective: To determine the optimal set of sequence parameters that minimizes scan time while preserving diagnostic image quality for T2-weighted brain imaging on a low-field MRI system.
Methodology:
- Baseline Acquisition: Acquire a dataset using the manufacturer's default T2-weighted TSE protocol.
- Iterative Modification: Systematically adjust one parameter at a time:
- Reduce the FOV in 5% increments.
- Adjust the FOV phase to find the minimum value without aliasing.
- Incrementally increase phase oversampling from 0% only if aliasing is present.
- Modify slice thickness and the number of slices to ensure complete brain coverage.
- Data Analysis: For each modified protocol, record the precise scan time. The image quality must be evaluated both quantitatively (e.g., measuring SNR in a region of interest) and qualitatively by an experienced neuroradiologist using a 5-point Likert scale to assess diagnostic confidence, noise, and artifact levels.
- Statistical Analysis: Employ regression analysis to model the relationship between parameter changes and scan time, and use ANOVA to test for significant differences in image quality scores between protocols.
This methodology allows researchers to build a customized, optimized protocol library for their specific low-field scanner and research needs.
Advanced Computational and Hardware Solutions
Beyond simple parameter adjustment, advanced hardware designs and computational methods are dramatically reshaping the time-resolution balance in low-field MRI.
Deep Learning for Image Enhancement
A primary strategy to overcome the SNR and resolution limitations of low-field MRI is to use deep learning models to enhance the acquired images. These models are trained on paired datasets of low-field and high-field images, learning a mapping function to generate synthetic high-quality images from low-quality inputs.
One study developed LoHiResGAN, an image-to-image translation model that enhances 0.064 T MRI scans to synthetic 3T-like quality [5]. The model employs a generative adversarial network (GAN) architecture with ResNet components for stable training and incorporates a loss function that includes the Structural Similarity Index Measure (SSIM) to preserve perceptual image quality. The results demonstrated that synthetic images significantly improved quantitative image quality metrics (SSIM, PSNR) and provided more consistent brain morphometry measurements across 33 brain regions compared to the original low-field images [5].
Another vendor-provided solution, the Precise IQ Engine (PIQE), is an image-domain deep learning reconstruction method that enables super-resolution without additional scans [67]. A study evaluating PIQE found that when the acquisition matrix was set to at least 0.87 mm/pixel, the reconstructed images achieved spatial resolution and quality equivalent to full-resolution acquisitions while reducing scan time by up to 70% [67]. Aggressive downsampling beyond this point led to image degradation, highlighting the need for a balanced initial acquisition.
The following diagram illustrates a typical deep learning workflow for enhancing low-field MRI images.
Hardware Innovations for Portability and Efficiency
Modern low-field scanners incorporate novel hardware designs that contribute to efficiency.
- Magnet Technology: The use of permanent magnets (e.g., Samarium-Cobalt) eliminates the need for costly cryogenic cooling, reduces power consumption, and enables open, patient-friendly designs [15] [9]. Compact superconducting magnets are also emerging in new low-field systems [1].
- Shielding-Free Operation: Traditional RF shielding cages are a major cost and installation barrier. New systems use deep learning-driven electromagnetic interference (EMI) cancellation techniques. By strategically placing EMI sensing coils and using AI to model and subtract noise from the MRI signal, these systems can operate in unshielded environments without compromising image quality [9].
- Optimized RF Coils: Advanced receiver coil designs, such as superconducting coils or multi-modal surface coils, are being developed to maximize signal pickup and improve the intrinsic SNR at low field strengths [1].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Materials and Technologies for Low-Field MRI Research
| Item / Technology | Function in Research | Example & Notes |
|---|---|---|
| Portable Low-Field MRI Scanner | Core hardware for image acquisition in non-traditional settings. | Hyperfine Swoop (0.064 T); MAGNETOM Free.Max (0.55 T). Characterized by portability and lower infrastructure needs [1] [5]. |
| Deep Learning Reconstruction Software | Software to enhance SNR and/or resolution, thereby reducing required scan time. | Canon PIQE (image-domain); GE AIR Recon DL; Siemens Deep Resolve (k-space domain). Can be vendor-provided or developed in-house [67]. |
| Paired Low-/High-Field Dataset | A curated set of co-registered images essential for training and validating super-resolution and image enhancement models. | Must include scans of the same subject on both a low-field (e.g., 0.055 T) and a high-field (e.g., 3 T) scanner [5]. |
| EMI Cancellation System | Hardware/software suite that enables operation without a RF-shielded room, crucial for true portability. | Uses external sensing coils and algorithms (e.g., deep learning) to subtract environmental noise from the MRI signal [9]. |
| Phantom for Quality Control | An object with known geometry and properties used to quantitatively monitor scanner performance and sequence optimization. | Used for tasks like verifying resolution claims and measuring SNR [67]. |
Integrated Workflow for Clinical Neuroscience Research
Translating these technical optimizations into a practical research workflow is essential for generating reliable, high-quality data. The following diagram outlines an integrated protocol from subject recruitment to data analysis.
Workflow Steps:
- Subject Preparation: Screen for contraindications and obtain informed consent, noting the increased compatibility of low-field MRI with certain implants [1] [15].
- Protocol Selection: Choose pulse sequences (e.g., T1-weighted, T2-weighted, FLAIR-like, DWI) tailored to the specific research objective, such as monitoring tumor progression or quantifying white matter hyperintensities [9].
- Scan Acquisition: Execute the scan using the pre-optimized protocol parameters (e.g., reduced FOV, minimized phase oversampling) to achieve the target resolution within the shortest feasible time [69].
- Image Enhancement: Process the raw image data through a validated deep learning model (e.g., LoHiResGAN, PIQE) to generate a synthetic high-field-quality image for analysis [67] [5].
- Quality Control: A critical step where a researcher or radiologist reviews the enhanced images for artifacts and ensures they meet the quality standards for the subsequent quantitative analysis. This may involve checking against a phantom scan [67].
- Quantitative Analysis: Perform the final research analysis, such as automated volumetry, lesion segmentation, or tractography, on the enhanced images [5].
The effective management of acquisition time in portable low-field MRI is not a single action but a comprehensive strategy. It requires the deliberate optimization of pulse sequence parameters, the integration of sophisticated deep learning reconstruction techniques, and the leveraging of novel hardware designs that prioritize efficiency and accessibility. For researchers in clinical neuroscience and drug development, mastering this balance is the key to unlocking the full potential of low-field MRI. This technology promises to democratize neuroimaging by enabling large-scale longitudinal studies, inclusion of underserved populations, and true point-of-care research, ultimately accelerating the pace of discovery in brain health and disease.
The integration of portable low-field magnetic resonance imaging (MRI) systems into clinical neuroscience research represents a paradigm shift, offering unprecedented access to neuroimaging in diverse, resource-constrained, and point-of-care settings. While the technological advancements of low-field systems, particularly those operating at ∼0.55 Tesla, are well-documented, their successful deployment hinges on solving critical operational challenges [70] [71]. These systems, celebrated for their reduced siting requirements and helium-free operation, introduce unique complexities in training, maintenance, and data infrastructure that differ substantially from those of conventional high-field MRI suites [70] [72]. This technical guide provides a comprehensive framework for establishing robust operational protocols for low-field MRI systems in clinical neuroscience research. It addresses the entire lifecycle—from operator training and sustainable maintenance schedules to the creation of data harmonization pipelines—ensuring that the scientific potential of these transformative devices is fully realized through operational excellence, data integrity, and reproducible research outputs.
Training Frameworks for Diverse Research Environments
Effective training is the cornerstone of reliable data acquisition in low-field MRI operations, particularly in non-traditional research environments that may lack onsite MRI physicists or experienced technologists. The training model must be efficient, scalable, and tailored to operators with potentially varied backgrounds.
Core Competencies and Efficient Training Protocols
A field study deploying a 0.55T MRI system in a resource-constrained setting demonstrated that MRI-naive technologists could achieve self-sufficient scanning proficiency after training on just 37 patients [71]. This rapid proficiency curve suggests that low-field systems, often designed with simplified workflows, can be effectively operationalized by a broader range of research staff. The core competencies for operators should extend beyond simple button-pushing to encompass:
- Protocol Selection and Optimization: Understanding which sequences and protocols are appropriate for specific clinical neuroscience research questions, from structural volumetry to functional connectivity studies.
- Basic Problem-Solving: Ability to identify and troubleshoot common artifacts, particularly those unique to low-field environments, and perform basic quality assurance procedures [73].
- Patient Safety and Screening: Rigorous training on safety protocols in environments that may lack the rigid physical controls of traditional MRI suites, with emphasis on ferromagnetic detection and patient monitoring [74].
Leveraging AI for Training and Operational Support
Artificial intelligence (AI) integrated into modern MRI systems can significantly reduce the cognitive load on operators and mitigate the impact of staffing shortages. AI-driven automation assists in several key areas:
- Automated Planning: AI-powered tools can automate scan planning, a task that typically requires significant expertise, thereby reducing variability and dependency on highly specialized operators [75].
- Workflow Simplification: Integrated AI solutions streamline complex examination workflows, minimizing manual steps and allowing technologists to focus more on patient interaction and less on complex sequence parameter adjustments [70] [75].
Table: Key Performance Improvements from Optimized Training and Operational Protocols
| Operational Area | Traditional Workflow | Optimized Low-Field Workflow | Improvement/Outcome |
|---|---|---|---|
| Technologist Training | Extended training period | Training on 37 patients [71] | Rapid self-sufficiency for MRI-naive staff |
| Scan Planning | Manual, expert-dependent | AI-powered automation [75] | Reduced variability and operator dependency |
| Workflow Complexity | High number of manual steps | AI-integrated streamlined workflows [70] | Lower cognitive load, reduced staffing strain |
| Examination Throughput | Standard turnover times | Dedicated prep bays and dual-table systems [76] | Turnaround reduced by 2-6 minutes per exam [76] |
Sustainable Maintenance Protocols for Field Reliability
Maintenance is a critical determinant of long-term data integrity and system availability. Low-field MRI systems, often deployed in remote or low-resource settings, require maintenance strategies that are both robust and feasible to implement outside of major urban centers.
Preventive Maintenance Schedules and Checklists
A rigorous preventive maintenance (PM) program can prevent up to 80% of equipment failures and extend asset lifecycles by 20-30% [77]. The financial impact is significant, with reactive maintenance costing 3-5 times more than preventive approaches. A comprehensive PM schedule for a low-field MRI system should include:
- Daily Tasks: Visual inspections for physical damage, checks of emergency equipment (e.g., fire extinguishers, quench pipes), verification of environmental controls (temperature, humidity), and basic system power checks [74].
- Weekly Tasks: Calibration verification, consumable level checks, and basic diagnostic tests on gradient and radiofrequency (RF) systems [77].
- Monthly Tasks: Comprehensive performance testing, detailed inspections of RF coils and transmission lines, and verification of patient handling systems [74] [77].
- Quarterly/Annual Tasks: Major calibrations, software updates, magnetic field homogeneity testing, and comprehensive safety protocol audits [78] [77].
The shift to helium-free magnet systems, a key feature of many new low-field platforms, eliminates the need for cryogen replenishment and associated monitoring, substantially simplifying the maintenance regimen and improving feasibility in remote locations [70] [72] [75].
Maintenance Execution and Documentation
Who performs the maintenance is as important as the schedule itself. Options include manufacturer service contracts, third-party service providers, and in-house biomedical technicians. The choice depends on local expertise, budget, and service availability. Key considerations include:
- Certification and Training: Ensure technicians are certified and have specific training on the low-field model in use [78].
- Documentation: Meticulous record-keeping is essential for regulatory compliance, warranty protection, and performance trending. A digital maintenance management system can improve compliance by up to 90% [77]. Essential documentation includes maintenance logs, performance data, parts usage, and incident reports [74].
Table: Economic Impact of Preventive vs. Reactive Maintenance for MRI Systems
| Maintenance Factor | Preventive Maintenance | Reactive Maintenance | Notes |
|---|---|---|---|
| Annual Cost | 2-4% of initial purchase price [77] | 3-5x higher than preventive [77] | For a $1M system, PM costs $20k-$40k annually |
| Equipment Lifespan | Extended by 20-30% [77] | Often shortened | Delays capital replacement costs |
| Unplanned Downtime | Reduced by 60-75% [77] | Frequent and unpredictable | Cost of downtime can exceed $50k/hour [77] |
| Helium-Cost & Logistics | Eliminated in helium-free systems [70] | N/A | Major operational advantage for low-field MRI in remote areas |
Data Infrastructure and Harmonization for Multi-Site Research
For clinical neuroscience research, especially multi-center trials, data integrity and cross-site comparability are paramount. The "Cycle of Quality" framework emphasizes that quality spans from acquisition and analysis to dissemination, forming a dynamic, interconnected process [73].
The Challenge of Scanner Variability and Harmonization Solutions
Even with standardized vendor sequences, heterogeneity in gradient strengths, slew rates, and reconstruction filters leads to inconsistent outputs across scanners, confounding longitudinal and multi-site study findings [73]. Solutions involve both prospective and retrospective harmonization:
- Prospective Harmonization: Utilizing vendor-independent, open-source platforms like Pulseq and Gadgetron to define and implement standardized, reproducible acquisition protocols across all research sites [73].
- Retrospective Harmonization: Applying statistical corrections in image or feature space to mitigate site-specific effects. This requires rigorous validation through "traveling-heads" studies or phantom-based assessments to benchmark success [73].
Quality Control and the Role of AI
Maintaining quality in a decentralized network of low-field scanners requires robust, automated quality control (QC) pipelines. This goes beyond traditional signal-to-noise ratio (SNR) measurements to include:
- Advanced Metrics: Task-based evaluations, artifact quantification, and visual integrity scores that better capture diagnostic utility [73].
- AI-Powered QC: AI models can assist in automated image analysis, segmenting anatomical structures, and evaluating images for artifacts or other quality issues, thus providing scalable QC for large, multi-site datasets [70] [73].
- Remote Monitoring Dashboards: For remote scanning setups, centralized protocol management and automated QA dashboards with real-time performance monitoring are critical for maintaining consistency and identifying drift in scanner performance [73].
Low-Field MRI Multi-Site Data Harmonization Workflow: This diagram outlines the integrated process for ensuring data quality and comparability in multi-site clinical neuroscience research using low-field MRI, combining prospective and retrospective harmonization strategies.
Integrated Operational Framework for Deployments
Success in diverse environments requires an integrated approach where training, maintenance, and data management are not siloed but are part of a cohesive operational strategy.
The "Smart Suite" and Workflow Optimization
Physical and workflow design dramatically impacts operational efficiency. Facilities designed for high-volume throughput, dubbed "Smart Suites," employ strategies such as:
- Dockable Tables: Two scanner tables per room allow one patient to be scanned while the next is prepared, cutting room turnaround time from ~12 minutes to about 2 minutes [76].
- Dedicated Preparation Bays: Located directly across from the scanner, these bays enable seamless patient turnover and have been shown to reduce exam times for brain and spine protocols by 2-6 minutes [76].
The Researcher's Toolkit for Low-Field MRI Operations
Table: Essential Research Reagent Solutions for Low-Field MRI Operations
| Tool/Reagent Category | Specific Example | Function in Operational Context |
|---|---|---|
| Digital Infrastructure | Pulseq [73] | Open-source platform for defining and sharing standardized MRI pulse sequences, enabling prospective harmonization. |
| Quality Control Phantoms | Geometric and multi-parameter phantoms [73] | Provides ground truth for scanner performance monitoring, calibration, and cross-site comparability validation. |
| AI Software Suites | Deep Resolve [70], AI-Rad Companion [70] | AI-based reconstruction and analysis tools that boost image quality, accelerate scans, and automate segmentation. |
| Data Harmonization Tools | Statistical harmonization models (e.g., Combat) [73] | Algorithmic tools for retrospective correction of site-effects in multi-site imaging data. |
| Maintenance Management | Computerized Maintenance Management System (CMMS) [77] | Digital platform for scheduling maintenance, tracking inventory, and documenting all service activities. |
Integrated Operational Framework for Low-Field MRI: This diagram visualizes the interdependence of the three core operational pillars (Training, Maintenance, and Data), supported by cross-cutting elements like AI integration and documentation systems.
The operational integration of portable low-field MRI into clinical neuroscience research demands a deliberate and integrated approach to training, maintenance, and data infrastructure. By adopting streamlined, evidence-based training models; implementing rigorous, sustainable maintenance schedules; and building data harmonization into the core of the research workflow, researchers can ensure that these powerful tools deliver on their promise of accessible, high-quality neuroimaging. The frameworks and protocols outlined in this guide provide a pathway to achieving operational excellence, thereby enabling robust, reproducible neuroscience discoveries across the globe, from urban clinics to the most remote field settings.
Benchmarking Diagnostic Performance: Low-Field vs. Conventional Neuroimaging
Portable low-field magnetic resonance imaging (LF-MRI) is an emerging technology poised to transform clinical neuroscience research and neurotherapeutic development. For decades, the neuroimaging field has been dominated by high-field systems (1.5T and 3T) that offer high spatial resolution but require substantial infrastructure, costly maintenance, and fixed installations. Recent advances in magnet design, hardware miniaturization, and artificial intelligence (AI)-based reconstruction algorithms have renewed interest in low-field systems, defined as those operating at field strengths below 1.5T [1]. These portable technologies offer distinct advantages for longitudinal studies, point-of-care assessment, and global health applications where conventional MRI cannot be deployed.
This technical review provides a comprehensive evaluation of the diagnostic accuracy of portable LF-MRI across three neurologically significant conditions: hydrocephalus, stroke, and intracranial hemorrhage. Within the context of a broader thesis on portable systems for clinical neuroscience research, we synthesize quantitative evidence from recent comparative studies, detail experimental methodologies, and analyze the technological innovations that enable these platforms to overcome traditional signal-to-noise limitations. For researchers and drug development professionals, this assessment provides critical insights into the validation status and appropriate application domains of these transformative technologies.
Technological Foundations of Portable Low-Field MRI
The physical principles of MRI remain consistent across field strengths, but portable LF-MRI systems employ specific engineering innovations to achieve diagnostic capability despite lower signal-to-noise ratios (SNR). Modern portable systems typically utilize compact superconducting magnets (e.g., Siemens MAGNETOM Free.Max) or high-performance permanent magnets (e.g., Hyperfine Swoop), which do not require active cryogenic cooling or substantial electrical infrastructure [1]. These design improvements result in systems with smaller physical footprints, reduced power demands, and sufficient B0 homogeneity for clinical imaging.
Key hardware advancements include optimized radiofrequency (RF) coils that minimize resistance and thermal noise to improve SNR, and multimodal surface coils that leverage multiple resonant modes to increase RF field efficiency [1]. From a software perspective, deep learning reconstruction algorithms have proven particularly valuable for enhancing image quality. Techniques like joint super-resolution and contrast synthesis (LF-SynthSR) can transform native low-resolution LF-MRI images into 1 mm isotropic T1-weighted magnetization-prepared rapid gradient-echo (MP-RAGE)-like images suitable for automated morphometric analysis [40].
Beyond technical specifications, portable LF-MRI systems offer practical advantages for research settings: reduced specific absorption rate (SAR) decreasing risks for patients with implants, quieter operation improving patient tolerance, and open configurations minimizing claustrophobia [1]. Perhaps most significantly, their portability enables novel research paradigms, including bedside imaging in intensive care units, intraoperative monitoring, and even home-based imaging deployments [1].
Comparative Diagnostic Accuracy Across Neurological Conditions
Hydrocephalus Detection and Monitoring
Hydrocephalus, characterized by abnormal cerebrospinal fluid accumulation, requires precise ventricular measurement for diagnosis and monitoring. A recent retrospective cohort study directly compared the diagnostic accuracy of mobile low-field MRI (ML MRI) against CT and 3.0T MRI in 130 patients with suspected hydrocephalus [79] [17]. The study demonstrated exceptional agreement between modalities, with intraclass correlation coefficients (ICC) > 0.95 for key ventricular measurements when comparing ML MRI to CT [79]. Receiver operating characteristic (ROC) analysis revealed an area under the curve (AUC) of 0.943 for ML MRI, closely matching CT (AUC 0.954) and 3.0T MRI (AUC 0.975) [79]. The sensitivity, specificity, and overall accuracy of ML MRI for hydrocephalus diagnosis were 96.00%, 96.67%, and 96.15%, respectively [79] [17].
Table 1: Diagnostic Performance of Mobile Low-Field MRI for Hydrocephalus
| Metric | ML MRI | CT | 3.0T MRI |
|---|---|---|---|
| Area Under Curve (AUC) | 0.943 | 0.954 | 0.975 |
| Sensitivity | 96.00% | - | - |
| Specificity | 96.67% | - | - |
| Accuracy | 96.15% | - | - |
| ICC vs. CT | >0.95 | - | - |
Beyond quantitative metrics, clinical case reports demonstrate that portable ultra-low-field (ULF) MRI can identify the underlying etiology of congenital hydrocephalus when ultrasound fails to detect pathology. In two neonatal cases, ULF MRI at 0.064T revealed posterior fossa tumors causing hydrocephalus that were not detected on repeated cranial ultrasounds performed by experienced operators [80]. The ULF imaging characterized specific tumor signaling patterns and even detected intracerebral metastases in one case, significantly altering treatment planning and prognosis [80].
Acute Stroke Evaluation
In acute stroke care, rapid neuroimaging is prerequisite for treatment decisions, yet remains inaccessible in many global regions. A pilot study evaluating portable ultra-low-field (pULF) MRI at 0.064T in a European tertiary stroke center demonstrated its potential to support treatment decisions when high-field MRI is unavailable [81]. The study included 17 consecutive patients with suspected ischemic stroke, 12 of whom had confirmed ischemic lesions on high-field MRI.
Table 2: Diagnostic Performance of Portable MRI in Acute Stroke
| Metric | Performance |
|---|---|
| Lesion Detection Rate | 8/12 cases (66.7%) |
| Missed Lesions | 4 infarcts <6mm diameter |
| Treatment Decision Concordance | 100% |
| Key Limitations | Long acquisition times, lack of vessel imaging, limited hemorrhage-sensitive sequences |
The investigation revealed that pULF-MRI detected ischemic lesions in 8 of the 12 confirmed cases (66.7%), with all undetected infarcts measuring less than 6mm in diameter [81]. Most significantly, in all cases, virtual treatment decisions based solely on pULF-MRI findings by a blinded clinical team matched the actual clinical decisions made with high-field MRI, demonstrating its potential utility in guiding acute intervention [81]. The authors noted important limitations including longer acquisition times and the absence of vessel imaging sequences, which restrict comprehensive stroke characterization [81].
Intracranial Hemorrhage Detection
Intracranial hemorrhage (ICH) detection represents a critical application where AI augmentation significantly enhances both conventional CT and emerging MRI technologies. A comprehensive meta-analysis of 73 studies evaluating deep learning (DL) models for ICH detection on non-contrast CT reported a pooled sensitivity of 0.92 (95% CI 0.90-0.94) and specificity of 0.94 (95% CI 0.92-0.95) [82]. The area under the curve (AUC) for DL models was 0.96 (95% CI 0.95-0.97), demonstrating high overall discriminative ability [82].
For portable MRI systems, which face inherent challenges in hemorrhage detection due to lower resolution and contrast-to-noise ratios, sophisticated AI monitoring frameworks have been developed to ensure reliability. The Ensembled Monitoring Model (EMM) framework addresses the "black-box" nature of commercial AI products by providing real-time confidence assessments without requiring access to internal model components [83]. In a validation study of 2,919 CT scans for ICH detection, EMM successfully categorized AI prediction confidence into increased, similar, or decreased confidence tiers, enabling appropriate radiologist review pathways [83].
The integration of AI assistance into clinical workflows has demonstrated tangible benefits beyond mere diagnostic accuracy. A retrospective study of 956 non-contrast brain CT scans found that implementing AI software for ICH detection significantly optimized radiologists' workflow without compromising diagnostic performance [84]. Following AI integration, the early diagnosis rate for ICH cases increased significantly from 49% to 76%, and the median reading order of ICH cases decreased from 7.25 to 1.5, indicating more rapid prioritization of critical findings [84].
Experimental Protocols and Methodologies
Hydrocephalus Study Protocol
The comparative study of mobile low-field MRI for hydrocephalus diagnosis employed a retrospective cohort design with 130 participants undergoing three imaging modalities: ML MRI, CT, and 3.0T MRI [79] [17]. Key ventricular measurements including Evans' index, frontal and occipital horn ratios, and callosal angle were systematically compared across modalities. Statistical analysis included intraclass correlation coefficients (ICC) for measurement reliability, Bland-Altman analysis for inter-modality agreement, and ROC curve analysis for diagnostic performance [79]. The ML MRI system utilized was the Hyperfine Swoop portable scanner operating at 0.064T, with acquisition sequences optimized for ventricular visualization including T1-weighted, T2-weighted, and FLAIR sequences [17].
Stroke Imaging Protocol
The pilot study of portable ULF-MRI in acute stroke care employed a prospective design with consecutive patients presenting with suspected ischemic stroke at a tertiary care center [81]. Participants underwent both pULF-MRI using the 0.064T Swoop system and standard high-field MRI. The pULF-MRI protocol included T1-weighted, T2-weighted, FLAIR, and diffusion-weighted imaging (DWI) sequences with b-values of 0 and 900 s/mm² [81]. High-field MRI (1.5T or 3T) served as the reference standard, with images independently evaluated by blinded neuroradiologists. The primary outcomes included lesion detection rate and concordance of treatment decisions between modalities [81].
AI-Assisted ICH Detection Protocol
The development and validation of AI systems for ICH detection typically follows a structured methodology. The meta-analysis by [82] documented that most studies utilized convolutional neural networks (CNN) trained on large datasets of non-contrast head CT scans, with ground truth established by expert neuroradiologist interpretations. The Ensembled Monitoring Model (EMM) employed a distinctive approach with five sub-models of diverse architectures trained for identical ICH detection tasks [83]. Agreement between the primary model and EMM sub-models was measured in discrete 20% increments, with confidence tiers established based on stratification thresholds that corresponded to increased, similar, or decreased confidence relative to the primary AI's baseline performance [83].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Portable MRI Studies
| Item | Specifications | Research Function |
|---|---|---|
| Portable MRI System | Hyperfine Swoop, 0.064T, portable | Primary imaging hardware for low-field data acquisition |
| AI Reconstruction Software | LF-SynthSR v2 with SynthSeg | Super-resolution and automated brain morphometry |
| Validation Phantom Set | Geometric and anthropomorphic phantoms | System calibration and image quality quantification |
| Multi-sequence Protocol | T1, T2, FLAIR, DWI sequences | Comprehensive tissue characterization |
| Clinical Reference Standards | 3T MRI, CT imaging systems | Ground truth for diagnostic accuracy studies |
| Automated Segmentation Tools | WMH-SynthSeg for white matter hyperintensities | Quantitative lesion volume measurement |
| Statistical Analysis Package | R, Python with specialized medical imaging libraries | Quantitative analysis of performance metrics |
Discussion and Research Implications
The accumulating evidence demonstrates that portable low-field MRI systems have reached a technological maturity that warrants their serious consideration as tools for clinical neuroscience research and therapeutic development. The high diagnostic accuracy for hydrocephalus (96.15% overall accuracy) [79], concordant treatment decisions in stroke [81], and successful AI integration for ICH detection [83] [84] collectively validate their research utility.
For drug development professionals, portable LF-MRI offers particular advantages for longitudinal therapeutic monitoring. The absence of ionizing radiation enables repeated imaging sessions without cumulative exposure risk, while the portability facilitates serial assessment in non-traditional settings [1] [40]. This is especially valuable for pediatric populations [80], critically ill patients who cannot be transported, and multi-center trials where scanner variability typically introduces significant noise.
The integration of AI technologies across the imaging pipeline—from acquisition to interpretation—represents the most promising direction for enhancing LF-MRI research applications. AI-based reconstruction algorithms like LF-SynthSR effectively mitigate the inherent SNR limitations of low-field systems [40], while confidence monitoring frameworks like EMM address the validation challenges inherent in "black-box" AI systems [83]. For researchers, these tools provide both quantitative morphometric outputs (e.g., hippocampal volumes, WMH burden) and quality assurance metrics essential for rigorous study design.
Persistent limitations include reduced sensitivity for small ischemic lesions (<6mm) [81], longer acquisition times compared to conventional MRI, and limited sequences for specialized applications like vessel imaging or spectroscopy. These constraints necessitate careful consideration of appropriate use cases and may require complementary imaging for comprehensive assessment.
Future research directions should focus on protocol optimization for specific neurologic conditions, validation of automated segmentation tools across diverse populations, and development of standardized phantoms for cross-site calibration. As portable LF-MRI technology continues to evolve, its role in democratizing access to neuroimaging and enabling novel research paradigms appears increasingly assured.
Portable low-field MRI systems represent a transformative technology for clinical neuroscience research, with demonstrated diagnostic accuracy across multiple neurological conditions that support their research applications. For hydrocephalus evaluation, ML MRI achieves accuracy exceeding 96% compared to reference standards [79] [17]. In acute stroke, portable ULF-MRI provides sufficient information to guide treatment decisions when higher-field systems are unavailable [81]. For intracranial hemorrhage detection, AI-assisted platforms both improve detection accuracy and optimize workflow efficiency [83] [82] [84].
These technological advances, coupled with the practical advantages of portability, reduced cost, and enhanced patient accessibility, position portable LF-MRI as a valuable tool for researchers and drug development professionals. Future developments in AI-based image reconstruction and analysis promise to further narrow the performance gap with high-field systems while enabling novel research applications in diverse settings. As validation evidence continues to accumulate, portable LF-MRI systems are poised to expand neuroimaging research beyond traditional radiology departments into point-of-care, community-based, and global health contexts.
The emergence of portable low-field magnetic resonance imaging (MRI) systems represents a paradigm shift in clinical neuroscience research, offering unprecedented access to neuroimaging in point-of-care, resource-limited, and longitudinal study settings. Unlike conventional high-field MRI systems that operate at 1.5 Tesla or 3.0 Tesla, portable low-field systems typically function at field strengths below 0.2 Tesla, with some devices operating as low as 0.064 Tesla [39]. These systems challenge the long-held notion that higher field strength invariably equates to superior clinical utility, instead emphasizing specific application-focused validation [1]. For research scientists and drug development professionals, the adoption of these technologies hinges on rigorous, quantitative demonstrations of their reliability and validity against established reference standards.
Quantitative statistical measures including Intraclass Correlation Coefficients (ICC), Bland-Altman analysis, and Receiver Operating Characteristic (ROC) curves provide the essential framework for this validation. ICC quantifies the reliability of measurements across different imaging platforms; Bland-Altman analysis assesses agreement between methods by evaluating measurement bias and limits of agreement; and ROC analysis determines diagnostic accuracy by plotting sensitivity against specificity across various decision thresholds [85]. Together, these methods offer a comprehensive statistical foundation for establishing whether low-field MRI can generate research-grade data comparable to conventional CT and high-field MRI, thereby enabling their integration into clinical neuroscience research protocols and therapeutic development pipelines.
Core Quantitative Metrics and Their Interpretation in Imaging Research
Intraclass Correlation Coefficient (ICC)
The Intraclass Correlation Coefficient (ICC) is a reliability metric that evaluates the consistency or agreement of quantitative measurements made by different devices or raters. In the context of validating low-field MRI, ICC assesses how closely continuous measurements (e.g., ventricular volumes, cartilage T2 relaxation times) align with those obtained from reference standard imaging [86].
ICC values range from 0 to 1, with higher values indicating stronger agreement. Conventional interpretation guidelines suggest: ICC < 0.50 indicates poor reliability, 0.50-0.75 indicates moderate reliability, 0.75-0.90 indicates good reliability, and > 0.90 indicates excellent reliability [87]. For low-field MRI to be considered a viable replacement for conventional imaging in quantitative research applications, ICC values should typically exceed 0.90, demonstrating excellent measurement agreement.
Bland-Altman Analysis
Bland-Altman analysis, also known as the "limits of agreement" method, provides a comprehensive assessment of measurement agreement between two quantitative techniques by evaluating both systematic bias and random measurement error [86]. This method involves plotting the differences between paired measurements from two devices against their means, visually revealing patterns of disagreement that might not be apparent through correlation coefficients alone.
The key outputs of Bland-Altman analysis include:
- Mean difference (bias): The average discrepancy between measurements from the two methods, indicating systematic over- or under-estimation.
- Limits of Agreement (LoA): Defined as the mean difference ± 1.96 standard deviations of the differences, representing the range within which 95% of measurement discrepancies fall.
- Clinical acceptability: Determined by whether the observed bias and LoA fall within pre-specified tolerances based on biological or clinical relevance [86].
Receiver Operating Characteristic (ROC) Analysis
Receiver Operating Characteristic (ROC) analysis evaluates the diagnostic performance of a classification test across all possible decision thresholds [85]. In low-field MRI validation, ROC curves quantify how effectively the technology distinguishes between pathological and normal states compared to a reference standard.
The primary metric derived from ROC analysis is the Area Under the Curve (AUC), which represents the probability that the test will correctly rank a randomly chosen positive case higher than a randomly chosen negative case. AUC values range from 0.5 (no discriminative power) to 1.0 (perfect discrimination), with values above 0.9 typically considered excellent [79] [17]. Additional diagnostic performance metrics include sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV), which are particularly valuable for establishing clinical utility in specific diagnostic scenarios such as hydrocephalus or intracerebral hemorrhage detection [79] [39].
Performance of Low-Field MRI Across Clinical Neuroscience Applications
Table 1: Diagnostic Performance of Low-Field MRI in Neurological Applications
| Clinical Application | Reference Standard | ICC Value | ROC AUC | Sensitivity/Specificity | Study Details |
|---|---|---|---|---|---|
| Hydrocephalus Diagnosis [79] | CT & 3.0T MRI | > 0.95 | 0.943 | 96.0%/96.7% | 130 patients; ventricular measurements |
| Intracerebral Hemorrhage Detection [39] | CT & 1.5T/3T MRI | - | - | 80.4%/96.6% | 144 exams; bedside imaging |
| Pediatric Ventricular Volume [86] | 1.5T/3T MRI | ~0.99 (correlation) | - | - | 17 patients; mean bias 2.06% |
| Knee Chondropathy [87] | Arthroscopy | 0.753 (inter-reader) | 0.714 | - | 52 patients; T2 mapping |
Hydrocephalus and Ventricular Volume Assessment
Hydrocephalus, characterized by abnormal cerebrospinal fluid accumulation and ventricular enlargement, represents a key application where low-field MRI has demonstrated particularly strong performance. A comprehensive retrospective cohort study of 130 patients with suspected hydrocephalus compared mobile low-field strength MRI (ML MRI) against both CT and 3.0T MRI [79] [17]. The study reported exceptional agreement, with ICC values exceeding 0.95 for key ventricular measurements compared to CT, indicating near-perfect reliability for quantitative assessment of ventricular size [79].
The diagnostic performance for hydrocephalus detection was equally impressive, with ML MRI achieving an AUC of 0.943, closely matching CT (AUC 0.954) and 3.0T MRI (AUC 0.975) [79] [17]. The technology demonstrated 96.00% sensitivity, 96.67% specificity, and 96.15% overall accuracy in distinguishing hydrocephalus cases from controls [79]. Bland-Altman analysis further confirmed high consistency across imaging modalities, with minimal systematic bias in ventricular measurements [17]. This robust performance profile, combined with the portability and absence of ionizing radiation, positions low-field MRI as a promising tool for both initial diagnosis and long-term monitoring of hydrocephalus patients, particularly in resource-limited settings or for bedside imaging in critical care units [79] [17].
Intracerebral Hemorrhage Detection
The evaluation of intracerebral hemorrhage (ICH) represents another critical application where low-field MRI has undergone rigorous validation. A landmark study conducted at Yale New Haven Hospital evaluated 144 portable MRI (pMRI) examinations using a 0.064T Hyperfine Swoop system at the bedside [39]. The study demonstrated that board-certified neuroradiologists correctly detected ICH with 80.4% sensitivity (45 of 56 cases) and 96.6% specificity (85 of 88 blood-negative cases) compared to conventional neuroimaging (CT or 1.5T/3T MRI) [39].
Performance varied by hemorrhage location, with supratentorial ICH (the most common presentation) detected at 88.0% sensitivity and intraventricular hemorrhage (IVH) identified at 92.8% sensitivity [39]. Manually segmented hematoma volumes and ABC/2 estimated volumes on pMRI strongly correlated with conventional imaging volumes (ICC = 0.955 and ICC = 0.875, respectively), and these measurements correlated significantly with NIH Stroke Scale scores and clinical outcomes at discharge [39]. This demonstrates that pMRI not only detects hemorrhage but also provides quantitatively meaningful volumetric data for prognostication, all while operating at the bedside with patients connected to critical monitoring equipment and intravenous lines [39].
Pediatric Ventricular Volume Measurement
In pediatric applications, a study focusing on ventricular volume quantification demonstrated remarkable agreement between low-field portable MRI and standard MRI systems [86]. The research involved 17 pediatric patients who underwent both portable (Hyperfine Swoop) and conventional (1.5T or 3T Siemens) imaging, with ventricular volumes manually segmented and compared [86].
Bland-Altman analysis revealed a minimal mean bias of 2.06%, indicating a slight tendency for portable MRI to overestimate ventricular volumes, though this discrepancy fell well within pre-specified clinical acceptability limits of 15% [86]. The correlation between modalities was nearly perfect (r² = 0.9993), while the limits of agreement ranged from -8.64% to 12.78% [86]. This exceptional agreement underscores the potential of low-field MRI for serial ventricular volume monitoring in pediatric populations, reducing the need for anesthesia or sedation typically required for conventional MRI in young patients, and minimizing radiation exposure compared to CT [86].
Experimental Protocols for Low-Field MRI Validation
Protocol for Hydrocephalus Evaluation
Table 2: Key Experimental Protocols from Cited Studies
| Protocol Component | Hydrocephalus Study [79] | Intracerebral Hemorrhage [39] | Pediatric Ventricles [86] | Knee Chondropathy [87] |
|---|---|---|---|---|
| Sample Size | 130 patients | 144 exams (56 ICH, 48 AIS, 40 controls) | 17 patients | 52 patients |
| Low-Field Device | Mobile low-field MRI | Hyperfine Swoop (0.064 T) | Hyperfine Swoop (0.064 T) | Esaote O-scan (0.31 T) |
| Reference Standard | CT & 3.0 T MRI | CT or 1.5T/3T MRI | 1.5T/3T MRI | Arthroscopy |
| Key Sequences | T2-weighted for ventricular measurements | T2-weighted, FLAIR | T2-weighted spin-echo | 3D SHARC for T2 mapping |
| Primary Metrics | Ventricular dimensions | ICH presence/absence, volume | Ventricular volume | T2 relaxation time |
| Statistical Analysis | ICC, Bland-Altman, ROC | Sensitivity, specificity, ICC for volumes | Bland-Altman, correlation | ROC, ICC, Cohen's κ |
The hydrocephalus validation study employed a retrospective cohort design enrolling 130 patients with suspected hydrocephalus who underwent imaging via mobile low-field MRI (ML MRI), CT, and 3.0T MRI [79] [17]. Key ventricular measurements including Evans' index, frontal and occipital horn widths, and third ventricular dimensions were obtained across all modalities by blinded reviewers [79]. Statistical analysis incorporated ICC for measurement reliability, Bland-Altman plots for agreement assessment, and ROC analysis for diagnostic accuracy determination using clinical diagnosis as the reference standard [17]. This comprehensive approach allowed researchers to simultaneously evaluate the technology's reliability for quantitative measurements and its accuracy for clinical diagnosis.
Protocol for Intracerebral Hemorrhage Detection
The ICH detection study implemented a prospective design with patients imaged using both conventional neuroimaging (non-contrast CT or 1.5T/3T MRI) and portable MRI (pMRI) at Yale New Haven Hospital from July 2018 to November 2020 [39]. The pMRI examinations were performed at the bedside with a scan time of approximately 18 minutes per patient, utilizing T2-weighted and FLAIR sequences [39]. Two board-certified neuroradiologists, blinded to clinical information and reference standard results, independently evaluated all pMRI examinations for the presence or absence of ICH, with a third researcher adjudicating cases of disagreement [39]. Additionally, hematoma volumes were manually segmented on both pMRI and conventional images, and ABC/2 estimation was performed to evaluate volumetric agreement [39]. This protocol design enabled assessment of both diagnostic accuracy (sensitivity/specificity) and quantitative measurement reliability (volume correlations) in a real-world clinical setting.
Visualization of Experimental Workflows
Figure 1: Experimental workflow for validating low-field MRI against reference standard imaging modalities, incorporating key statistical analyses including ICC, Bland-Altman, and ROC methods.
The Researcher's Toolkit: Essential Materials and Methods
Table 3: Essential Research Resources for Low-Field MRI Validation Studies
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Imaging Hardware | Hyperfine Swoop (64 mT) [86] [39], Esaote O-scan (0.31 T) [87], Custom Halbach systems (72 mT) [88] | Portable, low-field image acquisition at bedside or in resource-limited settings |
| Reference Standards | 1.5T/3T MRI systems [79] [86], CT scanners [79] [39], Arthroscopy [87] | Ground truth comparison for validation studies |
| Analysis Software | ITK-SNAP [86], MedCalc [87], SPSS [86], Custom Matlab scripts [87] | Image segmentation, statistical analysis, and quantitative measurement |
| Statistical Methods | ICC (two-way random effects) [87], Bland-Altman analysis [86], ROC curves [79] [87] | Reliability assessment, agreement evaluation, and diagnostic performance |
| Quantitative Biomarkers | Ventricular volumes [86], T2 relaxation times [87], Hematoma volumes [39] | Objective measurement of pathological features |
Implications for Clinical Neuroscience Research and Drug Development
The robust quantitative performance of low-field MRI across multiple neurological applications has significant implications for clinical neuroscience research and therapeutic development. The technology's portability enables novel study designs including longitudinal monitoring of neurological conditions at the bedside, imaging in non-traditional settings such as intensive care units [39], and even home-based imaging as demonstrated by Deoni et al., who integrated a 0.064T Hyperfine Swoop system into a standard consumer van [1]. This accessibility addresses a critical barrier in neuroimaging research, particularly for patient populations who cannot tolerate transport to conventional MRI suites or who require frequent monitoring.
For drug development professionals, low-field MRI offers a cost-effective approach to serial imaging biomarkers in clinical trials. The technology's ability to provide quantitative measures such as ventricular volumes in hydrocephalus [79] [86], hematoma volumes in stroke [39], and T2 relaxation times in cartilage degeneration [87] establishes its utility as an endpoint measurement system. Furthermore, the reduced infrastructure requirements and lower operational costs (estimated at 40-50% of conventional 1.5T systems) [1] make multicenter trials more feasible, potentially accelerating recruitment and reducing overall trial costs while maintaining research-grade data quality through rigorous statistical validation.
The comprehensive quantitative validation of portable low-field MRI systems using ICC, Bland-Altman, and ROC analyses demonstrates that these technologies provide research-grade data suitable for clinical neuroscience applications. While field strength limitations persist, particularly for applications requiring high spatial resolution, the performance metrics across neurological conditions consistently show excellent reliability and diagnostic accuracy compared to reference standards. As technological advancements continue to improve image quality through advanced reconstruction algorithms [1] and specialized sequences [87], low-field MRI is poised to expand access to neuroimaging research while providing the rigorous quantitative data necessary for both basic neuroscience and therapeutic development.
In the field of clinical neuroscience research, the renaissance of portable low-field MRI technology is creating new pathways for investigation, particularly in scenarios where conventional high-field systems face limitations. For neuroscientists and drug development professionals, the core advantages of these systems—reduced susceptibility artifacts and enhanced safety for implanted devices—are not merely conveniences but critical capabilities that can expand the boundaries of research [1]. These characteristics enable patient scanning in point-of-care environments and facilitate the inclusion in clinical trials of patient populations previously deemed unsuitable for MRI, such as those with deep brain stimulation systems or other metallic implants [89]. This technical guide delves into the physical principles underlying these advantages, presents quantitative experimental data, and outlines protocols for leveraging these benefits in neuroscience research settings.
The Physics of Reduced Susceptibility Artifacts
Fundamental Principles
Susceptibility artifacts in MRI arise from local magnetic field inhomogeneities created at the interfaces between materials with different magnetic susceptibilities, such as tissue-air or tissue-metal boundaries [1]. These inhomogeneities cause dephasing of proton spins and lead to signal loss, geometric distortion, and bright spots in the image. The degree of artifact is directly proportional to the strength of the static magnetic field (B₀); at lower field strengths, these effects are significantly diminished.
For neuroscience researchers, this translates to notably cleaner imaging near skull base regions (where air-tissue interfaces are common) and in patients with metallic dental work or surgical implants [1]. The reduction in susceptibility artifacts provides more accurate structural information, which is particularly valuable for volumetric studies and surgical planning.
Quantitative Comparison
Table 1: Quantitative Comparison of Susceptibility Artifacts at Different Field Strengths
| Field Strength | Relative Artifact Size | Impact on Anatomical Detail | Signal Void Volume |
|---|---|---|---|
| 3.0 Tesla | High | Severe distortion near interfaces | Large |
| 1.5 Tesla | Moderate | Moderate distortion | Moderate |
| 0.55 Tesla | Low | Mild distortion | Small |
| 0.064 Tesla | Very Low | Minimal distortion | Minimal |
Implant Safety: Mechanisms and Nuances
Theoretical Safety Advantages
Low-field MRI systems offer several theoretical safety advantages for patients with implants:
- Reduced Radiofrequency (RF) Energy Deposition: The specific absorption rate (SAR) decreases with lower field strengths, minimizing the risk of tissue heating near conductive implants [1].
- Diminished Magnetic Forces: The weaker static magnetic field results in substantially lower translational and rotational forces on ferromagnetic components [1].
- Lower Gradient-Induced Stimulation: Reduced slew rates and gradient amplitudes decrease the risk of peripheral nerve stimulation [1].
These characteristics make low-field systems particularly attractive for imaging patients with deep brain stimulation (DBS) systems, vagus nerve stimulators, and other neuromodulation devices that are increasingly relevant in neuroscience research and therapeutic development [89].
Complex Reality of RF Heating
Contrary to blanket assumptions of enhanced safety, recent investigations reveal a more complex picture of RF heating interactions at low fields. A systematic simulation study examining 368 wire models demonstrated that localized heating can sometimes be higher at 0.55T than at 1.5T, particularly for insulated wires of specific lengths [89].
The "antenna effect"—where implanted leads couple with the electric field—can intensify local SAR in tissue. The resonance length for this effect is longer at lower frequencies, meaning that certain lead geometries may unexpectedly demonstrate increased heating risks at low fields [89].
Table 2: Maximum SAR (W/kg) Comparison for Different Implant Configurations
| Implant Type | Configuration | 1.5T (64 MHz) | 0.55T (23 MHz) | Notes |
|---|---|---|---|---|
| DBS Lead | Lead only (40 cm) | 57.1 | 3.6 | Significant reduction at low field |
| DBS System | Full system (100 cm + IPG) | 37.1 | 52.2 | 40.8% increase at low field |
| Straight Insulated Wire | 45 cm apparent length | 120 (peak) | 25 (peak) | Resonance at different lengths |
| Straight Insulated Wire | 115 cm apparent length | 30 (peak) | 150 (peak) | Resonance at different lengths |
Experimental Protocol: Implant Safety Assessment
Objective: To quantify RF-induced heating for specific implant configurations at low-field strengths.
Methodology:
- Simulation Setup: Create finite element models of RF coils tuned to target frequencies (e.g., 23 MHz for 0.55T, 64 MHz for 1.5T) [89].
- Wire Modeling: Develop models of both insulated and uninsulated wires with varying:
- Apparent lengths (10-120 cm in 5 cm intervals)
- Geometries (straight and helical with different pitches)
- Tip exposure (typically 2 mm)
- Phantom Properties: Use cylindrical average tissue-mimicking phantom (σ = 0.5 S/m, εr = 64) [89].
- SAR Calculation: Compute 0.1 g-average SAR (MaxSAR) in a high-resolution mesh (rms length = 1.5 mm) around the tip [89].
- Validation: Compare simulation results with phantom measurements using fiber optic temperature probes.
Analysis:
- Identify resonance lengths for different wire geometries at each field strength.
- Compare peak SAR values for clinically relevant implant configurations.
- Develop safety guidelines for specific implant categories.
Technical Enhancements for Research Applications
Advanced Image Reconstruction
Modern low-field systems employ sophisticated artificial intelligence and deep learning algorithms to overcome intrinsic signal-to-noise limitations. The LoHiResGAN model, for instance, demonstrates how image-to-image translation can enhance 64mT portable MRI scans to approximate 3T quality [5]. This approach uses a generative adversarial network (GAN) architecture with ResNet components and incorporates structural similarity index measure (SSIM) loss to preserve perceptual image quality [5].
For quantitative neuroscience applications, the OPTIMUM (OPTImized MUltiparametric MRI) framework enables rapid acquisition of multiple parameter maps (T1, T2, T2*, M0, ΔB0, B1+) in a single 8.5-minute scan at 0.1T [90]. This is particularly valuable for drug development studies requiring longitudinal monitoring of tissue property changes.
Multi-Parametric Imaging and Visualization
Low-field MRI benefits from higher dispersion of nuclear spin relaxation rates, providing enhanced contrast between tissue types despite lower overall signal [90]. Advanced visualization techniques using tri-variate color maps in CIELAB color space allow researchers to simultaneously represent three parametric measurements in a single image, facilitating pattern recognition in complex datasets [20].
Table 3: Research Reagent Solutions for Low-Field MRI Neuroscience Studies
| Reagent/Resource | Function | Application Examples |
|---|---|---|
| OPTIMUM Framework | Rapid multi-parametric quantification | Simultaneous T1, T2, T2*, M0, ΔB0, B1+ mapping in 8.5 minutes [90] |
| LoHiResGAN | Image quality enhancement | Translation of 64mT images to synthetic 3T quality [5] |
| Tri-variate CIELAB Color Maps | Multi-parameter visualization | Simultaneous display of three parametric maps in perceptual uniform color space [20] |
| SynthSeg+ | Automated brain morphometry | Whole-brain segmentation regardless of MRI contrast or resolution [5] |
| ANTs Registration | Atlas-based segmentation | Multi-stage mapping for volumetric analysis of developmental brain data [91] |
Experimental Protocol: Neuroscience Applications
Developmental Brain Imaging
Objective: To track early brain development using low-field MRI in neonatal populations.
Methodology:
- Subject Population: Infant cohorts (e.g., 1-70 days postnatal) [91].
- Imaging Parameters: 0.35T system, T2-weighted FSE sequences, in-plane resolution ~0.85mm, slice thickness 6-7mm [91].
- Processing Pipeline:
- N4 bias field correction
- Manual brain mask segmentation
- Multi-stage atlas registration (rigid, affine, SyN)
- Expectation-maximization algorithm for whole-brain segmentation
- Volumetric Analysis: Measure growth trajectories for specific structures (white matter, gray matter, lateral ventricles, deep gray nuclei) [91].
Advantages: Reduced acoustic noise, lower SAR, minimal susceptibility artifacts from immature skull structures, and bedside capability for NICU applications [91].
Safety Workflow for Implanted Devices
Objective: To establish a safe imaging protocol for neuroscience study participants with implanted devices.
Methodology:
- Pre-Scan Assessment (Code 76014-76016):
- Identify and verify all implant components
- Review manufacturer's MR conditional requirements
- Document contraindications and specific instructions [92]
- Risk-Benefit Analysis:
- Evaluate diagnostic utility versus potential risks
- Consult with medical physicist for complex cases [92]
- Day-of-Scan Procedures (Code 76017-76019):
- Device programming to MR-safe mode (if required)
- Customize sequence parameters to minimize SAR
- Implement appropriate positioning and immobilization [92]
- Post-scan Verification:
- Confirm device functional status
- Document any adverse events
Low-field portable MRI systems present distinct advantages for clinical neuroscience research through their inherent reduction of susceptibility artifacts and enhanced compatibility with metallic implants. However, researchers must recognize that implant safety is not absolute and requires careful consideration of lead geometry and configuration. The integration of advanced reconstruction algorithms and multi-parametric quantification techniques continues to narrow the performance gap with high-field systems, making low-field MRI an increasingly powerful tool for studying brain development, neurodegenerative conditions, and therapeutic interventions in diverse patient populations and research settings.
Portable low-field magnetic resonance imaging (LF-MRI) systems, typically operating at field strengths below 0.1 T, are emerging as transformative tools for clinical neuroscience research [8]. By offering unparalleled accessibility through portability, lower cost, and reduced infrastructure requirements, these systems promise to democratize neuroimaging in point-of-care, resource-limited, and bedside settings [1] [8]. However, their integration into rigorous research paradigms requires a clear-eyed assessment of their technical limitations, particularly regarding spatial resolution and lesion detection thresholds. The fundamental trade-off between field strength and signal-to-noise ratio (SNR) establishes an inherent physical constraint that directly impacts the fidelity of quantitative biomarker measurements [1] [23]. This whitepaper details these critical limitations, provides quantitative evidence from validation studies, and outlines experimental protocols and computational strategies to mitigate these challenges for drug development and neuroscience research.
Physical Principles and Technical Constraints
The Signal-to-Noise Ratio Challenge
The performance of any MRI system is fundamentally governed by its static magnetic field strength (B₀). The net magnetization vector, which is the source of the MRI signal, is directly proportional to B₀ [1] [23]. Consequently, portable ultra-low-field (ULF) MRI systems, operating at field strengths like 0.064 T, experience a significantly reduced signal compared to conventional high-field (HF) systems (1.5 T or 3 T). A primary technical challenge is the subsequent reduction in signal-to-noise ratio (SNR). Empirical models indicate that SNR scales approximately with a power of B₀, often cited as B₀^², though the exact exponent depends on the specific contrast mechanism and hardware [23]. This results in a substantially lower baseline SNR for portable LF-MRI, which directly constrains its spatial resolution and lesion detection capabilities [1] [23].
The Interplay Between Resolution and Acquisition Time
To maintain a diagnostically usable SNR at lower field strengths, a trade-off must be made between spatial resolution and acquisition time. The acquisition time (TACQ) required to maintain consistent SNR between a high-field (B₀,H) and a low-field (B₀,L) system increases supra-linearly, following the relationship: TACQ,L = (B₀,H / B₀,L)^(2•powereff) • TACQ,H where "powereff" is a sequence-dependent coefficient [23]. Alternatively, spatial resolution must be sacrificed, scaling as: resL = (B₀,H / B₀,L)^(powereff/3) • res_H [23]. This physical reality means that portable LF-MRI protocols must either employ longer scan times to achieve resolutions comparable to HF-MRI or accept larger voxel sizes, which limits the visibility of small anatomical structures and lesions.
Table 1: Key Physical Constraints of Portable Low-Field MRI (sub-0.1 T)
| Technical Parameter | Relationship to Field Strength (B₀) | Practical Implication for Portable LF-MRI |
|---|---|---|
| Signal-to-Noise Ratio (SNR) | ~ B₀^² | Inherently lower signal, leading to noisier images and limiting resolution. |
| Spatial Resolution | ~ B₀^(powereff/3) | Larger voxel sizes are required to maintain a reasonable SNR without prohibitively long scans. |
| Acquisition Time | ~ (1/B₀)^(2•powereff) | Longer scan times are needed to compensate for low SNR to approach HF-MRI quality. |
| Larmor Frequency | ω₀ = γB₀ | Lower RF frequency reduces specific absorption rate (SAR), enhancing patient safety [1] [23]. |
Quantitative Limitations in Lesion Detection
Validation studies directly comparing portable LF-MRI with established HF-MRI have quantified its performance in detecting pathological lesions, a core task in clinical neuroscience.
Detection of White Matter Lesions in Multiple Sclerosis
A pivotal study investigating multiple sclerosis (MS) provided clear metrics for lesion detection sensitivity. In this prospective, cross-sectional study, 33 adults with confirmed MS underwent same-day brain MRI on both 3T and 64mT (0.064 T) portable (Hyperfine Swoop) scanners [93].
- Sensitivity for Patients: The portable 64mT scanner identified lesions in 94% (31/33) of the patients with confirmed MS on 3T MRI [93].
- Size Detection Threshold: The critical limitation was revealed in the size of the smallest detectable lesions. The study found the average smallest lesion manually detected was 5.7 ± 1.3 mm in maximum diameter at 64mT, compared to 2.1 ± 0.6 mm at 3T [93]. This threshold closely approaches the spatial resolution (5 mm slice thickness) of the low-field sequences used.
- Lesion Volume Correlation: Automated lesion volume estimates between the two scanners were highly correlated (r = 0.89, p < 0.001), though a bias was observed where 64mT segmentations over-estimated low lesion volumes and under-estimated high volumes [93].
Detection of Acute Ischemic Stroke Lesions
A 2025 pilot study on acute stroke care further defined detection limits. The study involved consecutive patients with suspected ischemic stroke who underwent both portable ultra-low-field (pULF) MRI and HF-MRI [94].
- Sensitivity for Infarcts: pULF-MRI detected ischemic lesions in 8 out of 12 cases (67%) where a lesion was present on HF-MRI [94].
- Size Detection Threshold: The four infarcts missed by the pULF-MRI were all smaller than 6 mm in diameter, confirming a similar detection threshold as seen in MS research [94].
Table 2: Quantitative Performance of Portable LF-MRI in Lesion Detection
| Clinical Context | Reference Standard | Portable LF-MRI Sensitivity | Minimum Detectable Lesion Size | Key Study Findings |
|---|---|---|---|---|
| Multiple Sclerosis [93] | 3T MRI | 94% (31/33 patients) | 5.7 mm mean minimum diameter | High correlation in total lesion volume (r=0.89) but smaller lesions (<5mm) are missed. |
| Acute Ischemic Stroke [94] | HF-MRI (1.5T/3T) | 67% (8/12 lesions) | <6 mm diameter | All undetected lesions were smaller than 6mm. Treatment decisions based on pULF-MRI matched clinical decisions. |
Experimental Protocols for Validation
To assess the capabilities and limitations of a portable LF-MRI system in a research setting, the following experimental protocols, derived from the cited literature, are recommended.
Protocol for Cross-Field Lesion Validation
Objective: To quantitatively compare the lesion detection rate and volume measurements between a portable LF-MRI and a high-field MRI system. Methods:
- Participant Recruitment: Recruit a cohort of patients with a condition known to cause visible lesions (e.g., Multiple Sclerosis, stroke sequelae). A sample size of at least 30 participants is recommended for initial validation [93].
- Image Acquisition: Perform same-day MRI scans on each participant using both the portable LF-MRI system (e.g., Hyperfine Swoop) and a reference high-field scanner (1.5T or 3T). For the LF-MRI, acquire T2-weighted FLAIR and Diffusion-Weighted Imaging (DWI) sequences. For HF-MRI, acquire a protocol including FLAIR, DWI, and T2* sequences [94] [93].
- Blinded Image Assessment: Have experienced neuroradiologists and neurologists, who are blinded to the clinical information and HF-MRI results, review the portable LF-MRI scans. Readers should document the number, location, and size of all identified lesions [94].
- Ground Truth Comparison: Compare the findings from the blinded read against the gold standard HF-MRI readings. Calculate sensitivity and specificity for lesion detection on a per-patient and per-lesion basis. Manually measure the diameter of the smallest detected lesion on both systems [93].
- Volumetric Analysis: Use automated lesion segmentation algorithms (e.g., SynthSeg) on both the LF-MRI and HF-MRI datasets. Calculate total lesion volumes and perform correlation analysis (e.g., Pearson correlation) and agreement analysis (e.g., Bland-Altman plots) [93] [14].
Protocol for Enhancing Resolution with Multi-Acquisition
Objective: To improve spatial resolution and SNR for portable LF-MRI through multi-acquisition image averaging. Methods:
- Image Acquisition: Acquire multiple volumetric scans (e.g., T2-weighted images) in orthogonal planes (axial, coronal, and sagittal) from the same subject using the portable LF-MRI system [14].
- Image Co-registration: Use a linear image registration tool (e.g., FMRIB's Linear Image Registration Tool - FLIRT) to precisely align all acquired image volumes into a common space [5].
- Image Averaging / Super-Resolution: Employ a multi-acquisition volume averaging technique to generate a higher-resolution image volume. This "TomoBrain" approach combines data from orthogonal imaging directions to create a single image with effectively increased resolution and SNR [14].
- Validation: Compare the quantitative morphometry results (e.g., volumes of gray matter, white matter, hippocampus) derived from the enhanced LF-MRI image against those obtained from a reference HF-MRI scan [14].
Advancing Research with Computational Solutions
AI-Based Image Enhancement
Deep learning models are being developed to bridge the quality gap between LF- and HF-MRI. These models perform image-to-image translation, enhancing the resolution and SNR of LF-MRI scans to synthetically generate images that resemble those from HF-MRI.
- Model Architecture: The LoHiResGAN model is an example of a conditional Generative Adversarial Network (cGAN) that uses ResNet-based components in a U-Net-like architecture. It is trained on paired datasets of low-field (64mT) and high-field (3T) MRI sequences from the same subjects [5].
- Loss Function: To improve perceptual quality, such models can incorporate the Structural Similarity Index Measure (SSIM) as an additional loss component alongside traditional losses like Mean Absolute Error (MAE). This helps the generated images better preserve structural details [5].
- Performance: Studies show that synthetic 3T images generated from 64mT inputs using LoHiResGAN significantly improve image quality metrics (e.g., Normalized Root-Mean-Squared Error, Peak Signal-to-Noise Ratio) and provide more consistent brain morphometry measurements across various brain regions when referenced to true 3T images [5].
Innovative Acquisition Sequences
Technical innovations in acquisition physics also contribute to mitigating limitations. For instance, Spatiotemporal Encoding (SPEN) MRI has been implemented on portable low-field systems as an alternative to traditional Echo-Planar Imaging (EPI) [95].
- Advantage: SPEN-based imaging is less sensitive to magnetic field inhomogeneities, which are more challenging to correct at low fields. This results in reduced geometric distortions compared to EPI, providing more robust and accurate images for diffusion-weighted imaging (DWI) and functional MRI [95].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Resources for Portable Low-Field MRI Research
| Resource Category | Specific Example | Function in Research |
|---|---|---|
| Imaging Hardware | Hyperfine Swoop (0.064 T) | Portable MRI scanner for point-of-care data acquisition. |
| Reference Scanner | Siemens 3T MAGNETOM | High-field system for establishing ground truth image quality and lesion labels. |
| Image Registration Tool | FMRIB's Linear Image Registration Tool (FLIRT) | Co-registers paired LF and HF images for voxel-wise comparison and training [5]. |
| Automated Segmentation | SynthSeg / SynthSR | AI-based tool for segmenting brain structures and estimating volumes from low-field and low-resolution MRI [5] [14]. |
| Deep Learning Model | LoHiResGAN | Image-to-image translation network for enhancing LF-MRI quality and generating synthetic HF-like images [5]. |
| Multi-Acquisition Method | TomoBrain Protocol | A specific acquisition and processing workflow that combines orthogonal image planes to boost effective resolution [14]. |
Portable low-field MRI represents a paradigm shift for neuroscience research, offering the potential for decentralized, large-scale studies. However, this promise is tempered by well-defined physical constraints. The core limitations of spatial resolution and lesion detection thresholds, with a current practical sensitivity for lesions larger than approximately 5-6 mm, must be explicitly acknowledged in research design [94] [93]. These constraints currently preclude the study of fine-grained neuroanatomy or small lesions. Despite this, validated applications exist in monitoring larger pathologies in MS and stroke. The path forward lies in the strategic integration of sophisticated experimental protocols, multi-acquisition techniques, and advanced computational tools like AI-based enhancement. By understanding and actively mitigating these limitations, researchers can robustly leverage portable LF-MRI to advance clinical neuroscience and therapeutic development in both traditional and novel settings.
The advent of portable low-field MRI (pMRI) systems represents a paradigm shift in neuroimaging, offering a practical solution to expand the scope and settings of clinical neuroscience research. This technical guide provides a comprehensive analysis of the total cost of ownership (TCO) and implementation logistics for these systems. By synthesizing current financial data, operational frameworks, and emerging research applications, this document serves as a strategic resource for researchers and drug development professionals seeking to deploy pMRI technology. The analysis demonstrates that while pMRI involves trade-offs in spatial resolution, its dramatically lower acquisition and operational costs, combined with unique portability advantages, can justify integration into diversified neuroimaging research programs, particularly for longitudinal studies, point-of-care assessments, and research involving underserved populations.
For decades, high-field MRI has been the undisputed cornerstone of in vivo neuroscience research, providing unparalleled soft tissue contrast. However, its utility is constrained by significant barriers: immense capital investment, stringent siting requirements, and operational costs that limit patient access and study design flexibility. It is estimated that as of 2019, 66% of the global population lacked access to MRI [1].
The development of portable, low-field MRI systems (<0.1 T) challenges this paradigm. Technological advances in magnet design, RF coils, and artificial intelligence (AI)-based image reconstruction have significantly narrowed the performance gap for many clinical applications [1]. For the neuroscience researcher, these systems are not merely weaker versions of their high-field counterparts; they are a new class of tool that enables fundamentally different research approaches—from scanning participants in their homes to conducting neuroimaging studies in remote, resource-limited communities [96] [97]. This guide provides a detailed cost-benefit and operational framework to inform the successful deployment of pMRI in research contexts.
Total Cost of Ownership (TCO) Analysis
The Total Cost of Ownership provides a holistic financial perspective, moving beyond the initial purchase price to encompass all costs incurred over the system's operational life. Understanding TCO is critical for accurate budgeting and strategic justification.
Core TCO Components
A comprehensive TCO model for an MRI scanner extends from initial fund allocation through decommissioning. The largest expense category is consistently human resources, which can account for approximately 35% of the total cost, while the initial scanner purchase accounts for only about 17% of the TCO over a 10-year ownership life [98]. The major cost components are detailed below.
Table 1: Total Cost of Ownership (TCO) Components for MRI Systems
| Cost Category | Description | Considerations for Portable Low-Field MRI |
|---|---|---|
| Capital Acquisition | Purchase price of the scanner and essential hardware. | Significantly lower than high-field systems; a 0.55-T system may cost 40-50% of a 1.5-T scanner [1]. |
| Installation & Siting | Costs for facility modification, shielding, electrical work, and logistics. | Can be reduced by up to 70%; often requires no reinforced flooring, copper shielding, or dedicated HVAC [1]. |
| Human Resources | Salaries and benefits for all operational staff (technologists, nurses, schedulers, etc.). | May be lower due to simplified operation; potential for remote scanning models [98]. |
| Service & Maintenance | Annual service contracts, parts, and cryogens. | Estimated to be up to 45% lower, particularly for systems without cryogenic cooling [1]. |
| Supplies & Contrast | Consumables, contrast agents, and small equipment. | Assumed comparable, though lower SAR may impact contrast usage [98]. |
| IT Infrastructure | PACS, image storage, networking, and cloud-based AI analysis platforms. | Critical for pMRI; enables remote interpretation and data processing [96]. |
| Utilities & Overhead | Power, cooling, and administrative overhead. | Reduced energy consumption and facility demands [1]. |
Comparative Cost Analysis: Portable vs. Fixed High-Field MRI
Acquisition and Installation Costs
The market for MRI systems can be segmented into tiers. Conventional high-field (1.5T or 3T) systems typically fall into the premium tier, with costs often exceeding $1 million for new wide-bore models [99]. In stark contrast, portable low-field systems operate in a different financial realm.
- Portable MRI Cost Tiers: Entry-level and portable MRI systems can be acquired in the $100,000 to $450,000 range, with ultra-low-field systems like the Hyperfine Swoop representing the lower end of this spectrum [99].
- Infrastructure Savings: The siting advantages are profound. A portable 0.064 T system can be installed in a standard clinical room without major structural modifications, whereas a high-field system requires substantial investment in quench pipe installation, magnetic shielding, and specialized cooling systems [1] [100]. One feasibility study reported installation and transport cost savings of up to 70% for a low-field system [1].
Operational and Maintenance Costs
Ongoing costs are a pivotal factor in TCO. Annual service contracts for fixed high-field MRI from major manufacturers (Siemens, GE, Philips) range from approximately $42,000 to $134,000 [99]. Maintenance costs for low-field systems can be up to 45% lower due to the absence of cryogenic systems and simpler overall design [1].
Table 2: Comparative Cost Analysis: Remote Implementation Scenario
| Cost Factor | Patient Transfer for Fixed MRI | Portable MRI Deployment | Notes/Savings |
|---|---|---|---|
| Model Basis | Transporting 50 patients via charter flight over 1 year [29]. | Installing one portable MRI system for 1 year of operation [29]. | Analysis from a remote Canadian setting. |
| Total Annual Cost | Higher cost of patient logistics and fixed MRI use. | Lower cost of local operation. | Net annual savings: $854,841 [29]. |
| 5-Year Budget Impact | Cumulative high costs for patient transport. | Lower cumulative costs despite initial hardware outlay. | Projected 5-year savings: Nearly $8 million [29] [100]. |
| Clinical Utility | Provides full diagnostic workup. | Serves as a powerful triage tool; 44% of patients still required transfer for higher-resolution imaging [100]. | Portable MRI improves triage, avoiding unnecessary transfers for 56% of patients. |
Operational Implementation Logistics
Successful integration of pMRI into a research workflow requires careful planning of physical, human, and technical resources.
Site Planning and Technical Requirements
The operational workflow for deploying a pMRI system involves a series of coordinated steps from site assessment through to data interpretation.
Diagram 1: Portable MRI Research Workflow
Key logistical considerations include:
- Space and Power: Unlike high-field systems, pMRI units like the Hyperfine Swoop can operate on standard wall power and fit in a standard room, eliminating the need for dedicated electrical lines or chilled-water cooling [1] [100].
- Safety and Screening: While the static magnetic field is lower and associated projectile risk is reduced, safety protocols for ferromagnetic objects and implants remain mandatory. The specific absorption rate (SAR) is lower, reducing risks of tissue heating [1].
- Data Handling: The research workflow relies on secure PACS networks or cloud platforms for transmitting image data to neuroradiologists or central research teams for interpretation [100]. This is integral to the model of operation in remote settings.
Human Resource and Training Models
The operational model for pMRI can diverge from traditional MRI by leveraging simplified operation.
- Diversified Operator Pool: With simplified interfaces and autonomous operation features, pMRI systems can be operated not only by certified MRI technologists but also by nurses, physicians, or trained research staff after appropriate training [96] [100]. This can alleviate shortages of highly skilled technologists.
- Centralized Remote Scanning Model: A TCO analysis suggests a strategy where a smaller number of expert technologists conduct scanning remotely for multiple sites, reducing the need for highly skilled (and highly paid) technologists at each scanner location, despite increasing IT costs [98].
Experimental Protocols and Research Applications in Neuroscience
The portability and low cost of pMRI open new avenues for experimental design in neuroscience research and drug development.
Detailed Methodology: Field-Based Neuroimaging Research
A proven protocol for deploying pMRI in a remote or community setting involves the following stages [29] [100]:
- Site Preparation and Community Engagement: A foundational step is consulting with local community leaders and ethics boards. This aligns with ethical guidance emphasizing community partnership and co-creation of knowledge [96] [101]. The physical installation requires only a standard room.
- Operator Training: Research personnel (e.g., nurses, x-ray technologists) undergo training on system operation, safety protocols, and patient handling. Training is typically condensed compared to that for high-field MRI systems.
- Participant Enrollment and Scanning: Participants are enrolled based on research indications. Scanning protocols are executed, often including axial T1-weighted fast spin echo, T2-weighted fast spin echo, and T2-weighted fluid-attenuated inversion recovery (FLAIR) sequences.
- Image Transfer and Interpretation: Images are transmitted via a secure PACS network to neuroradiologists available for 24/7 interpretation. Report turnaround times are recorded to ensure timely clinical feedback, if applicable.
- Data Analysis and Triage: Images are analyzed for research outcomes. In hybrid clinical-research settings, the data is used for triage; for example, in one study, pMRI successfully identified the 56% of patients who did not require transfer to a fixed MRI, while correctly flagging 44% for further workup [100].
Key Research Applications
Portable MRI is demonstrating utility in several neuroscience research domains:
- Neurodevelopmental Studies in Low-Resource Settings: pMRI enables longitudinal studies of brain volume and the impact of environmental factors on child development in geographically diverse populations [96].
- Neurodegenerative and Cerebrovascular Disease: Research is ongoing to use pMRI for tracking white matter lesions in multiple sclerosis and for the diagnosis and monitoring of stroke in emergency departments and ambulances [1] [96].
- Point-of-Care Imaging for Critical Care Neuroscience: pMRI allows for serial imaging of patients who are too critically ill to be moved, such as those in ICU on life support or in isolation, facilitating research on brain injury and recovery [1] [96].
The Scientist's Toolkit: Research Reagent Solutions
Deploying a pMRI research program requires both hardware and specialized software "reagents."
Table 3: Essential Research Materials and Tools for Portable MRI
| Item / Solution | Function / Role in Research | Example / Specification |
|---|---|---|
| Portable MRI Scanner | Core hardware for data acquisition in non-traditional settings. | Hyperfine Swoop (0.064 T); Promaxo system (0.058-0.074 T) [100] [30]. |
| AI-Based Reconstruction Software | Enhances signal-to-noise ratio and image clarity from inherently low-SNR data. | Integrated software suites using deep learning to reduce scan times and improve diagnostic utility [1]. |
| Cloud PACS & Data Platform | Enables secure data transfer from remote sites, remote expert interpretation, and centralized data storage. | Essential for studies in remote areas lacking on-site neuroradiology expertise [96] [100]. |
| Specialized RF Coils | Optimize signal reception for specific anatomical regions, improving data quality. | Superconducting or multimodal surface coils designed for low-field systems [1]. |
| Open-Source Analysis Platforms | Provide tools for processing and analyzing low-field MRI data, often integrating with existing neuroimaging software (e.g., FSL, SPM). | Critical for standardizing data analysis pipelines across diverse research sites. |
Discussion: Strategic Integration and Ethical Considerations
Cost-Benefit and Strategic Value
The financial analysis compellingly supports pMRI as a cost-effective tool for specific research niches. The value proposition is not that pMRI will replace high-field systems, but that it democratizes access to neuroimaging and enables study designs previously considered impractical or too costly. The multi-million dollar savings demonstrated in remote implementations highlight its power to reallocate scarce healthcare research resources more efficiently [29] [100]. For drug development, pMRI offers a modality for more frequent monitoring and inclusion of participants from a wider geographic and socioeconomic spectrum, potentially increasing the generalizability of trial results.
Navigating Ethical, Legal, and Social Implications (ELSI)
The deployment of pMRI in community and remote settings introduces a suite of ELSI challenges that require proactive management [96] [101]. An interdisciplinary Working Group has provided consensus recommendations addressing:
- Community Engagement and Partnership: Research must be designed to provide local value and avoid "helicopter research." This involves ongoing partnership with local communities in the co-creation of research questions, conduct, and dissemination of findings [101].
- Safety and Oversight: As pMRI becomes accessible to researchers outside traditional neuroimaging fields, robust safety protocols and IRB oversight are essential to protect participants and bystanders in less-controlled environments [96].
- Data Privacy and Incidental Findings: Protocols must be established for secure data handling, especially when using cloud platforms, and for the management and return of clinically relevant incidental findings discovered during research scans [96] [102].
Portable low-field MRI systems present a financially viable and operationally feasible tool for advancing clinical neuroscience research. The Total Cost of Ownership is substantially lower than that of high-field systems, not only in acquisition but also in installation, siting, and maintenance. This cost advantage, coupled with the unique capability for field-based research, allows investigators to conduct neuroimaging studies in community settings, remote populations, and point-of-care environments, thereby addressing long-standing challenges of accessibility and representativeness in brain research. Successful implementation requires careful attention to operational logistics, appropriate application selection, and, crucially, a firm commitment to navigating the associated ethical landscape. When strategically integrated into a research portfolio, pMRI serves not as a replacement for high-field imaging, but as a transformative tool for broadening the horizons of neuroscience.
Conclusion
Portable low-field MRI is poised to fundamentally reshape clinical neuroscience and drug development by breaking down traditional barriers of cost, infrastructure, and accessibility. The synthesis of evidence confirms that while resolution gaps persist, technological advancements in AI and hardware have established LF-MRI as a diagnostically valid tool for a growing range of neurological conditions. Its portability enables novel research paradigms, from decentralized clinical trials that improve patient recruitment and retention to large-scale population studies in genetically diverse, underrepresented communities. For the pharmaceutical industry, this technology offers a practical means for frequent, longitudinal monitoring of therapeutic efficacy in real-world settings. Future progress hinges on the development of open-source, scalable systems; robust training pathways for global operators; and continued innovation in quantitative imaging. The ultimate impact of LF-MRI extends beyond technical specifications—it represents a pivotal step toward equitable, patient-centric neuroscience research and a more inclusive future for global brain health.
References
- 1. Low-field and portable MRI technology - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549457/]
- 2. Initial insights into post-contrast enhancement in ultra-low- ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1507522/full]
- 3. Hyperfine Swoop® AI-Powered Portable MRI System ... [https://investors.hyperfine.io/news-releases/news-release-details/hyperfine-swoopr-ai-powered-portable-mri-system-demonstrates-100]
- 4. ISMRM25 - Low-Field MRI [https://www.ismrm.org/25/program-files/PP-20.htm]
- 5. Improving portable low-field MRI image quality through ... [https://www.nature.com/articles/s41598-023-48438-1]
- 6. Hyperfine Swoop® AI-Powered Portable MRI System ... [https://investors.hyperfine.io/news-releases/news-release-details/hyperfine-swoopr-ai-powered-portable-mri-system-showcased]
- 7. Low-Field MRI: How Low Can We Go? A Fresh View on an ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2020.00172/full]
- 8. Low field, high impact: democratizing MRI for clinical and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12529269/]
- 9. A low-cost and shielding-free ultra-low-field brain MRI ... [https://www.nature.com/articles/s41467-021-27317-1]
- 10. Low‐field MRI: An MR physics perspective - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6590434/]
- 11. Brain imaging with portable low-field MRI - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10497072/]
- 12. Quantification and improvement of the signal-to-noise ratio ... [https://www.sciencedirect.com/science/article/pii/S0730725X96002196]
- 13. MRI at low field: A review of software solutions for improving ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11605168/]
- 14. Ultra-Low-Field MRI and AI Tools Yield Accurate Brain ... [https://cai2r.net/ultra-low-field-mri-and-ai-tools-yield-accurate-brain-volumes-if-you-tomobrain/]
- 15. Low‐field MRI: Clinical promise and challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9771987/]
- 16. Low-Field vs High-Field MRI: what's the difference? [https://hallmarq.net/2023/07/18/low-field-vs-high-field-mri-whats-the-difference/]
- 17. Accuracy and Clinical Application Prospects of Mobile Low ... [https://www.sciencedirect.com/science/article/pii/S0361923025003971]
- 18. Quantitative MRI in Neuroimaging: A Review of Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562573/]
- 19. Advances in neuroimaging applications of quantitative ... [https://www.sciencedirect.com/science/article/pii/S2950162825000165]
- 20. Color-coded visualization of magnetic resonance imaging ... [https://www.nature.com/articles/srep41107]
- 21. Effect of color visualization and display hardware on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5148121/]
- 22. Low-field and portable MRI technology: advancements and ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-025-00638-2]
- 23. Ultra-low-field MRI: a David versus Goliath challenge in ... [https://link.springer.com/article/10.1007/s11547-025-02091-y]
- 24. Emerging Sustainability Standards Are Redefining Medical ... [https://www.intertek.com/blog/2025/02-04-medical-imaging-systems-sustainability/]
- 25. ISMRM25 - Image Reconstruction Using AI [https://www.ismrm.org/25/program-files/D-15.htm]
- 26. Rapid, Deep-Learning-Based Magnetic Resonance ... [https://engineering.nyu.edu/events/2025/11/11/rapid-deep-learning-based-magnetic-resonance-imaging-mri-reconstructions-overview]
- 27. Bracco Shapes the Future of Radiology at RSNA 2025 [https://www.bracco.com/en-us/article/bracco-shapes-future-radiology-rsna-2025]
- 28. Portable MRI Market Size, Trends & Forecast 2025 to 2035 [https://www.futuremarketinsights.com/reports/portable-mri-market]
- 29. Feasibility and Cost Analysis of Portable MRI ... [https://pubmed.ncbi.nlm.nih.gov/37434471/]
- 30. Cost-efficient analysis of a portable low field magnetic ... [https://www.frontiersin.org/journals/urology/articles/10.3389/fruro.2022.966862/full]
- 31. The society for equity neuroscience (SEQUINS) - PubMed - NIH [https://pubmed.ncbi.nlm.nih.gov/40395217/]
- 32. Global Access Partners (GAP): Home [https://globalaccesspartners.org/]
- 33. A Letter From the President: GAP's 2025 IRI Virtual ... [https://globalalzplatform.org/2025/11/19/a-letter-from-the-president-gaps-2025-iri-virtual-conference/]
- 34. The Equity in Neuroscience and Alzheimer's Clinical Trials ... [https://www.alz.org/news/2021/the-equity-in-neuroscience-and-alzheimer-s-clinical-trials-enact-act-introduced-in-congress]
- 35. Methodology for Low-Field, Portable Magnetic Resonance ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2021.760321/full]
- 36. Potential application of ultra-low field portable MRI in the ICU ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10551136/]
- 37. Point-of-Care Brain MRI: Preliminary Results from a Single- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9713449/]
- 38. Applications of portable magnetic resonance imaging in ... [https://ejrnm.springeropen.com/articles/10.1186/s43055-025-01457-6]
- 39. Portable, bedside, low-field magnetic resonance imaging ... [https://www.nature.com/articles/s41467-021-25441-6]
- 40. Portable, low-field magnetic resonance imaging for ... [https://www.nature.com/articles/s41467-024-54972-x]
- 41. Characterization of Portable Ultra-Low Field MRI Scanners ... [https://pubmed.ncbi.nlm.nih.gov/40405769/]
- 42. Tips and challenges for clinical use and interpretation of low ... field [https://pubmed.ncbi.nlm.nih.gov/39976637/]
- 43. Emerging Trends in MRI to Watch in Systems 2025 [https://www.linkedin.com/pulse/emerging-trends-mri-systems-watch-2025-market-intelligence-hub-wopgf]
- 44. Optimal Brain MRI Protocol for New Neurological Complaint [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0110803]
- 45. Optimizing the early diagnosis of neurological disorders ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12217182/]
- 46. Low field, high impact: democratizing MRI for clinical and ... [https://pubmed.ncbi.nlm.nih.gov/41112323/]
- 47. Hyperfine PULSE Platform to Drive Portable MRI Innovation [https://hyperfinemri.com/about/news/press-release-hyperfine-launches-pulse-platform-to-accelerate-adoption-and-innovation-of-ai-powered-portable-mri]
- 48. Portable MRI Shows Promise for Expanding Brain Imaging ... [https://www.massgeneralbrigham.org/en/about/newsroom/press-releases/portable-mri-shows-promise-expanding-brain-imaging-alzheimers-disease]
- 49. UNITY: A low-field magnetic resonance neuroimaging ... [https://www.sciencedirect.com/science/article/pii/S1878929324000586]
- 50. Opportunities for use of neuroimaging in de-risking drug ... [https://www.nature.com/articles/s41386-024-01970-8]
- 51. Accelerating Therapeutic Development for Brain Illnesses [https://irp.nih.gov/blog/post/2025/09/accelerating-therapeutic-development-for-brain-illnesses]
- 52. Can Neuroimaging Save Psychedelic Drug Development? [https://www.perceptive.com/news/can-neuroimaging-save-psychedelic-drug-development/]
- 53. Impact of Magnetic Resonance Imaging on Healthcare in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10112545/]
- 54. Development of a mobile low-field MRI scanner [https://www.nature.com/articles/s41598-022-09760-2]
- 55. Applying artificial intelligence to cardiac MRI to diagnose ... [https://www.nature.com/articles/s43856-025-01179-w]
- 56. Case-based review of low-field MRI in resource-constrained ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12579540/]
- 57. Denoising very low-field magnetic resonance images using ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1501801/full]
- 58. Design of Asymmetric Permanent Magnet Arrays for the ... [https://archive.ismrm.org/2025/0904.html]
- 59. [2509.11762] Very-low-field MRI scanners: from the ideal to ... [https://arxiv.org/abs/2509.11762]
- 60. Design and performance of a toroidal radiofrequency ... [https://pubmed.ncbi.nlm.nih.gov/40991825/]
- 61. Ultra-high gradient connectomics and microstructure MRI ... [https://www.nature.com/articles/s41551-025-01457-x]
- 62. Simultaneous T1- and T2-Weighted 3D MRI Using RF ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9006307/]
- 63. mriToolbox - Home [https://www.mritoolbox.com/]
- 64. Pulse Sequence Design & Acceleration Methods for ... [https://www.ismrm.org/25/program-files/D-08.htm]
- 65. MRI Pulse Sequences and AI Techniques at ISMRM 2025 [https://www.mevis.fraunhofer.de/en/press-and-scicom/institute-news/2025/mri-pulse-sequences-and-ai-techniques-at-ismrm-2025.html]
- 66. Multi-parametric optimization of magnetic resonance ... [https://www.sciencedirect.com/science/article/pii/S240563162300088X]
- 67. Verification of resolution and imaging time for high ... [https://www.sciencedirect.com/science/article/abs/pii/S0730725X2500147X]
- 68. Applications, limitations and advancements of ultra-low ... [https://surgicalneurologyint.com/surgicalint-articles/applications-limitations-and-advancements-of-ultra-low-field-magnetic-resonance-imaging-a-scoping-review/]
- 69. Optimizing imaging resolution in brain MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC10478647/]
- 70. What's New in MRI Technology — 2025 Edition [https://www.cassling.com/blog/whats-new-in-mri-technology-2025-edition]
- 71. Experience from planning and operationalising a 0.55 T ... [https://archive.ismrm.org/2025/1650.html]
- 72. MRI Equipment Breakthroughs 2025 [https://openmedscience.com/mri-equipment-breakthroughs-how-2025-innovations-transform-patient-care/]
- 73. ESMRMB 2025 focus topic: cycle of quality—from concept to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255560/]
- 74. MRI Machine Maintenance Checklist - 2025 [https://www.fieldex.com/en/checklist/mri-machine-maintenance-checklist]
- 75. Advancing Cardiac MRI with AI at RSNA 2025 [https://www.philips.com/a-w/about/news/archive/standard/news/articles/2025/philips-advances-cardiac-mr-with-a-new-suite-of-innovations-powered-by-ai-to-expand-patient-access-and-improve-diagnostic-precision.html]
- 76. Optimized MRI Suites Enable High-Volume Turnaround, ... [https://www.rsna.org/news/2025/may/optimized-mri-suites]
- 77. Medical Imaging Equipment: Preventive Maintenance for ... [https://oxmaint.com/blog/post/medical-imaging-equipment-preventive-maintenance-for-diagnostic-accuracy]
- 78. MRI Preventive Maintenance - A Guide for Medical Facilities [https://directmedimaging.com/mri-preventive-maintenance-a-guide-for-medical-facilities/]
- 79. Accuracy and clinical application prospects of mobile low ... [https://pubmed.ncbi.nlm.nih.gov/41138929/]
- 80. Case Report: Ultralow-field portable MRI improves the ... [https://www.frontiersin.org/journals/pediatrics/articles/10.3389/fped.2025.1463314/full]
- 81. Portable ultra-low-field MRI in acute stroke care: A pilot study [https://pubmed.ncbi.nlm.nih.gov/40515383/]
- 82. Diagnostic Accuracy of Deep Learning for Intracranial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11989428/]
- 83. Automated real-time assessment of intracranial ... [https://www.nature.com/articles/s41746-025-02007-0]
- 84. Impact of a computed tomography-based artificial ... [https://www.dirjournal.org/articles/impact-of-a-computed-tomography-based-artificial-intelligence-software-on-radiologists-workflow-for-detecting-acute-intracranial-hemorrhage/doi/dir.2025.253301]
- 85. Receiver Operating Characteristics (ROCs) [https://yonelinas.faculty.ucdavis.edu/roc-analysis/]
- 86. Low-Field Portable MR Imaging to Evaluate Ventricular ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11383396/]
- 87. Knee Cartilage Quantification: Performance of Low-Field ... [https://www.mdpi.com/2313-433X/11/11/401]
- 88. Portable magnetic resonance imaging of patients indoors ... [https://www.nature.com/articles/s41598-022-17472-w]
- 89. Low-field MRI's Spark on Implant Safety - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10842192/]
- 90. Fast Quantitative Low-Field Magnetic Resonance Imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8903217/]
- 91. A Low-Field MRI Dataset For Spatiotemporal Analysis of ... [https://www.nature.com/articles/s41597-025-04450-w]
- 92. New MR Safety CPT Codes in 2025 [https://www.acr.org/Clinical-Resources/Publications-and-Research/ACR-Bulletin/New-MR-Safety-CPT-Codes-in-2025]
- 93. Sensitivity of portable low - field for... magnetic resonance imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC9421456/]
- 94. Portable ultra-low-field MRI in acute stroke care: A pilot study [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170540/]
- 95. Spatiotemporal Encoding MRI in a Portable Low-Field ... [https://archive.ismrm.org/2025/0008.html]
- 96. Ethical, legal, and policy challenges in field-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11157461/]
- 97. Low-Cost and Portable MRI - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC10644353/]
- 98. A total cost of ownership (TCO) model ... [https://cds.ismrm.org/protected/20MProceedings/PDFfiles/4158.html]
- 99. How Much Does an MRI Machine Cost in 2025? [https://www.blockimaging.com/bid/92623/mri-machine-cost-and-price-guide]
- 100. Feasibility and Cost Analysis of Portable MRI ... [https://www.cambridge.org/core/journals/canadian-journal-of-neurological-sciences/article/feasibility-and-cost-analysis-of-portable-mri-implementation-in-a-remote-setting-in-canada/B1039FF8205E6090A9CEC701B33D49FE]
- 101. Emerging ethical issues raised by highly portable MRI ... [https://www.sciencedirect.com/science/article/pii/S1053811921004870]
- 102. The Dawn of Highly Portable AI-Enabled MRI Research in ... [https://neuroethicssociety.org/posts/the-dawn-of-highly-portable-ai-enabled-mri-research-in-the-community-proactively-addressing-elsi-challenges/]