Optimizing EEG Montages: Strategies to Reduce Setup Time and Enhance Data Quality for Clinical Research
This article provides a comprehensive guide for researchers and drug development professionals on implementing optimal EEG electrode montages to significantly reduce setup time without compromising data quality.
Optimizing EEG Montages: Strategies to Reduce Setup Time and Enhance Data Quality for Clinical Research
Abstract
This article provides a comprehensive guide for researchers and drug development professionals on implementing optimal EEG electrode montages to significantly reduce setup time without compromising data quality. It explores the foundational principles of electrode reduction, systematic methodologies for identifying key electrode subsets, and practical troubleshooting for real-world application. By synthesizing recent evidence from meta-analyses and validation studies, the content offers actionable strategies for deploying efficient EEG protocols in clinical trials and research settings, facilitating faster participant throughput and improved practicality while maintaining scientific rigor.
The Science and Necessity of EEG Montage Optimization
The Critical Burden of Traditional EEG Setup in Research
Traditional electroencephalography (EEG) setups present a significant bottleneck in neuroscience research, creating a critical burden through lengthy application times, technical complexity, and limited practicality for real-world applications. These challenges are particularly pronounced in studies requiring rapid prototyping, longitudinal monitoring, or diverse participant populations. The operational costs of maintaining traditional EEG infrastructure are substantial, with labor accounting for up to 98% of expenditures in dedicated 24-hour services [1]. Furthermore, patient discomfort and restricted mobility during monitoring compromise data quality and ecological validity [1].
Fortunately, emerging research on optimal electrode montages is paving the way for radical efficiency improvements. Systematic electrode reduction studies demonstrate that researchers can reduce channel counts by 50% or more without significant performance degradation in various applications [2]. This technical support center provides actionable methodologies and troubleshooting guides to help researchers implement these advances, reduce setup time, and maintain data quality through optimized experimental protocols.
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: How many electrodes can I safely eliminate from my EEG setup without compromising data integrity? The optimal number varies by application, but systematic reductions of 50-75% are often achievable. For neonatal sleep state classification, research shows that a single properly selected channel (C3) can achieve 80.75% accuracy compared to multi-channel setups [3] [4]. In speech imagery brain-computer interfaces (BCIs), 64 channels can be reduced by 50% without significant performance loss [2]. The key is methodical validation rather than arbitrary reduction.
Q2: Are there standardized "optimal" electrode positions for specific research applications? While certain regions show consistent importance (e.g., left hemisphere electrodes for neonatal sleep classification), optimal configurations are often subject-specific [2]. Research indicates that relevant areas are distributed across the cortex rather than limited to classically defined functional regions [2]. Population-based optimization approaches can approximate individualized optimization, but perfect consistency across datasets remains elusive [5].
Q3: What is the most effective method for selecting which electrodes to keep in a reduced montage? Wrapper methods systematically evaluate channel subsets based on classification accuracy and are recommended over filter or embedded methods due to superior performance [2]. These methods work by iteratively excluding electrodes while monitoring performance metrics, providing a data-driven approach to montage optimization [2].
Q4: How can I troubleshoot persistent reference/ground electrode issues during setup? Reference electrode problems often manifest as uniformly poor signal quality across channels. Troubleshooting should include: reapplying the ground electrode with proper skin preparation; testing alternative ground placements (hand, sternum); removing all metal accessories; and swapping reference and ground electrode placements [6]. If issues persist, systematically check each component in the signal chain from software to participant [6].
Common Technical Issues & Solutions
| Symptom | Potential Reasons | Troubleshooting Actions |
|---|---|---|
| Missing Channels [7] | Dry electrodes, loose connections, incorrect amplifier settings | Check electrode-skin impedance; verify all physical connections; ensure amplifiers aren't set to same channel [8] [7] |
| Noisy/Poor Recordings [7] | Poor ground, artifact contamination, equipment malfunction | Verify ground connection; use targeted artifact cleaning [9]; check for nearby electronic devices; restart amplifier/software [6] |
| Spotty/Intermittent Signal [7] | Drying electrolyte, unstable electrode contact, equipment issues | Reapply electrodes with fresh conductive paste; check electrode integrity; swap headbox if issue persists [6] [7] |
| Global Signal Quality Issues | Ground loop interference, reference oversaturation [6] | Use AC-coupled ground adapter [8]; test with ground placed further from reference; ensure single ground point [8] [6] |
Experimental Protocols for Electrode Optimization
Systematic Electrode Reduction Methodology
The following workflow provides a standardized approach for determining the minimal electrode set required for your specific research application:
Protocol Details:
- Initial Setup: Begin with your standard high-density montage (e.g., 64-channel) collecting data for your specific task [2].
- Preprocessing: Apply standardized preprocessing including artifact removal techniques such as targeted artifact reduction in components to minimize false positive effects [9].
- Feature Extraction: Extract comprehensive linear and nonlinear features in time and frequency domains. Consider incorporating features like Detrended Fluctuation Analysis (DFA), Lyapunov exponent, and multiscale fluctuation entropy, which have shown utility in reduced-montage applications [3] [4].
- Classification & Evaluation: Establish baseline performance metrics using your standard analysis pipeline.
- Systematic Reduction: Implement wrapper methods to iteratively remove electrodes based on their contribution to classification accuracy [2].
- Validation: Cross-validate optimal montage on separate datasets and participants to ensure generalizability.
Population-Based Montage Optimization
For studies without resources for subject-specific optimization, population-based approaches provide a practical alternative:
Key Findings from Population Optimization Research:
- Population-based electric field optimization demonstrates comparable focality and targeting accuracy to individualized analysis, with differences up to 17% [5].
- Age mismatch between population proxy and target individual reduces focality by up to 8.3% compared to age-matched optimization [5].
- Populations larger than 40 individuals provide consistent optimization results with negligible inconsistencies [5].
Quantitative Performance Data of Reduced Montages
Electrode Reduction Performance Across Applications
| Research Application | Original Channels | Reduced Channels | Performance Metric | Result |
|---|---|---|---|---|
| Neonatal Sleep Staging [3] [4] | Multiple | Single (C3) | Classification Accuracy | 80.75% ± 0.82% |
| Neonatal Sleep Staging [3] [4] | Multiple | 4 Left-Side Electrodes | Classification Accuracy | 82.71% ± 0.88% |
| Speech Imagery BCI [2] | 64 | 32 (50% reduction) | Classification Accuracy | No Significant Loss |
| Imagined Speech Detection [2] | 14 | 6-8 | Classification Accuracy | Up to 90% |
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function/Application | Key Characteristics |
|---|---|---|
| Dry Electrode EEG Systems [1] | Enables rapid application without skin preparation; ideal for reduced montage setups | Ultra-high impedance amplifiers (>47 GOhms); handles contact impedances up to 1-2 MOhms |
| Targeted Artifact Cleaning [9] | Addresses artifact contamination in reduced montages where fewer channels are available | RELAX pipeline (EEGLAB plugin); targets artifact periods/frequencies rather than subtracting entire components |
| Wrapper Method Algorithms [2] | Systematically identifies optimal electrode subsets based on performance metrics | Iteratively excludes electrodes while monitoring classification accuracy |
| SMOTE Technique [3] [4] | Addresses class imbalance in datasets when working with reduced signal information | Synthetic minority over-sampling technique; improves classifier performance with limited channels |
| PCA for Feature Selection [3] [4] | Reduces feature dimensionality to complement electrode reduction | Prioritizes most significant features from time/frequency domain analysis |
Advanced Methodologies for Specific Research Domains
Domain-Specific Electrode Optimization Protocols
Neonatal Sleep State Classification Protocol:
- Collect EEG data from multiple channels including bilateral coverage.
- Extract 94 linear and nonlinear features in time and frequency domains.
- Apply SMOTE technique to address class imbalance.
- Use Principal Component Analysis (PCA) for feature prioritization.
- Test single-channel performance systematically across all electrodes.
- Validate findings showing left-side electrodes (particularly C3) provide superior accuracy (82.71%) compared to right-side electrodes (81.14%) [3] [4].
Speech Imagery BCI Optimization Protocol:
- Record EEG data from 64 electrodes during speech imagery tasks.
- Implement wrapper function with objectives of minimizing error rate and channel count.
- Use random forest classifier for channel subset evaluation.
- Identify subject-specific optimal configurations rather than assuming universal positions.
- Validate that relevant areas are distributed across cortex, not limited to left hemisphere [2].
Remote Troubleshooting Framework
For research teams managing multiple testing sites or remote data collection, systematic troubleshooting is essential:
Remote Troubleshooting Protocol:
- Electrode/Cap Connections: Verify proper connections; re-clean/re-apply electrodes; add conductive gel; swap questionable electrodes [6] [10].
- Software/Computer/Amplifier: Restart recording software; reboot computer and amplifier; verify cable connections [6].
- Headbox & Cables: Swap headbox if available; test different electrode connections; verify physical integrity of all cables [6].
- Participant-Specific Factors: Remove metal accessories; check for hairstyle/products interfering; test alternative ground placements; evaluate for potential oversaturation [6].
- Documentation: Record the issue and solution for team knowledge sharing and future troubleshooting efficiency [10].
By implementing these methodologies and troubleshooting approaches, researchers can significantly reduce the critical burden of traditional EEG setups while maintaining data quality and expanding research capabilities through optimized electrode montages.
Core Concepts: Standardized Systems and Montages
What is the International 10-20 System and why is it fundamental to EEG research?
The International 10-20 System is a standardized method for placing scalp electrodes to ensure consistent and replicable EEG recordings across different subjects and sessions. Developed by Herbert Jasper in 1957, it is based on the relationship between electrode location and the underlying cerebral cortex [11] [12]. The system's name comes from the fact that distances between adjacent electrodes are either 10% or 20% of the total front-to-back or right-to-left distance of the skull. Key anatomical landmarks used for measurement are the nasion (the depressed area between the eyes, just above the bridge of the nose), the inion (the crest point at the back of the skull), and the preauricular points (in front of each ear) [11].
Electrode Nomenclature:
- Letters indicate the brain region or lobe the electrode covers: Fp (pre-frontal or frontal pole), F (frontal), C (central), T (temporal), P (parietal), and O (occipital) [11] [12].
- Numbers indicate the distance from the midline. Even numbers are on the right hemisphere, odd numbers are on the left, and the 'z' (for zero) denotes electrodes placed on the midline sagittal plane (e.g., Fz, Cz, Pz) [11] [12].
What is an EEG montage and how does a differential amplifier work?
An EEG montage is a combination of derivations, which are specific pairs of electrodes assigned to an amplifier's inputs [13]. The core technology behind interpreting these derivations is the differential amplifier.
A differential amplifier takes two input signals (Input 1 and Input 2, often labeled active and reference) and amplifies the difference in voltage between them, while suppressing any voltage that is common to both. This process is called Common Mode Rejection (CMR) [13]. It is crucial for eliminating pervasive environmental artifacts, such as 50/60 Hz electrical mains interference, which are present equally in both inputs and are therefore subtracted out. This allows the "real" EEG activity, which typically has different voltages at the two electrode sites, to be visible [13].
What are the common types of EEG montages?
- Referential Montage: Each active electrode on the scalp is compared to a single, theoretically "neutral" reference electrode (e.g., on the ear or mastoid) [13].
- Bipolar Montage: A "daisy-chain" configuration where electrodes are linked in sequence (e.g., Fp1-F3, F3-C3, C3-P3). This is effective for localizing transient events like epileptiform activity [14].
What are the extended systems beyond the 10-20 system?
To achieve higher spatial resolution, extended systems like the 10-10 system (10% division) and the 10-5 system (5% division) were developed. These fill in intermediate sites between the original 10-20 electrodes, allowing for high-density EEG recordings with 64, 128, or more channels [11] [12]. The Modified Combinatorial Nomenclature (MCN) was introduced to name these new electrode sites using letter combinations like AF (between Fp and F), FC (between F and C), and CP (between C and P) [11].
Troubleshooting Guides & FAQs
This section addresses common practical challenges in EEG research.
Frequently Asked Questions
Q1: My EEG signal is noisy with 50/60 Hz "fuzzy" waves. What should I check? This is typically 50/60 Hz mains artifact. The differential amplifier's Common Mode Rejection is designed to eliminate this. If it persists, check:
- Electrode Impedance: Ensure all electrodes, including ground and reference, have low and stable impedance (typically < 5-10 kΩ). High impedance unbalances the amplifier and reduces CMR effectiveness [6] [14].
- Ground Connection: Verify the ground electrode is properly applied. A faulty ground can cause this artifact across all channels [6] [13].
- Cable Integrity: Check for damaged or loose cables that could break the signal balance [6].
Q2: One of my electrode impedance readings is persistently high (greyed out). How can I resolve this?
- Re-prep the site: Clean the scalp area again and re-apply conductive paste or gel to ensure good skin contact [6].
- Swap the electrode: Replace the problematic electrode with a new one to rule out a "dead" or faulty sensor [6].
- Check for bridging: Inspect if excess gel has created an electrical bridge between two adjacent electrodes, which can cause abnormal readings [6].
- Inspect the hardware: If the issue persists, check the cap connection and, as a last resort, try a different headbox or amplifier input to isolate a hardware fault [6].
Q3: How critical is precise electrode placement? What is the impact of a small misplacement? For most standard EEG analyses (e.g., spectral power, event-related potentials), minor placement errors have a relatively small impact. A simulation study using a realistic head model found that electrode displacements with a mean of 5 mm introduced a source localization error of only about 2 mm for normal, noisy EEG signals [15] [16]. This error is generally negligible compared to those caused by biological and environmental noise. However, for advanced applications like precise dipole source localization or TMS-EEG co-registration, highly accurate placement (aided by digitization) is recommended [15] [17].
Q4: For my study on neonatal sleep, which electrode montage would provide optimal results with minimal setup time? Research on neonatal sleep state classification suggests that a limited, optimized montage can be highly effective. A 2025 study found that a single C3 channel (left central) achieved an accuracy of 80.75% using an LSTM classifier. Furthermore, a configuration using four left-side electrodes (C3, F3, etc.) achieved a higher accuracy of 82.71% compared to four right-side electrodes (81.14%) [18]. This indicates that a minimal montage focused on the left hemisphere can reduce technical complexity and setup time while maintaining high performance for this specific application.
Systematic Troubleshooting Flowchart
Follow this logical pathway to diagnose common EEG hardware issues.
Experimental Protocols & Data
This section provides a summary of key experimental methodologies and quantitative findings from recent literature.
Experimental Protocol: Neonatal Sleep State Classification with Optimized Montage
Objective: To classify neonatal sleep states using an LSTM classifier and identify an optimal electrode setup to reduce complexity [18].
Methodology:
- Data Acquisition: EEG data was collected from 64 infants (36-43 weeks age) at Fudan University Children's Hospital. A total of 16,803 30-second EEG segments were used [18].
- Feature Extraction: A comprehensive set of 94 linear and nonlinear features in time and frequency domains were extracted, including novel features like Detrended Fluctuation Analysis (DFA), Lyapunov exponent, and multiscale fluctuation entropy [18].
- Data Balancing: The SMOTE technique was used to address class imbalance [18].
- Feature Reduction: Principal Component Analysis (PCA) was applied to identify and prioritize the most significant features [18].
- Classification & Electrode Optimization: An LSTM classifier was trained and tested using different electrode configurations (single channel, four left-side, four right-side) to compare performance [18].
Key Performance Data (Classification Accuracy):
| Electrode Configuration | Accuracy (%) | Kappa Value |
|---|---|---|
| Single C3 Channel | 80.75% ± 0.82 | 0.76 |
| Four Left-Side Electrodes | 82.71% ± 0.88 | 0.78 |
| Four Right-Side Electrodes | 81.14% ± 0.77 | 0.76 |
Source: Siddiqa et al., 2025, Frontiers in Computational Neuroscience [18].
Experimental Protocol: RBF Neural Network for EEG Dynamics Reconstruction
Objective: To reconstruct EEG dynamics and extract age-related neural characteristics using a Radial Basis Function (RBF) neural network optimized by Particle Swarm Optimization (PSO) [14].
Methodology:
- Data Acquisition: Resting-state EEG was recorded from 142 participants across multiple age groups using a 32-channel system following the 10-20 system [14].
- Preprocessing: Signals were bandpass filtered (1–35 Hz) and artifacts were removed using Independent Component Analysis (ICA). A longitudinal bipolar montage (e.g., Fp1-F3, F3-C3, C3-P3, P3-O1) was used for analysis [14].
- Dimensionality Reduction: Principal Component Analysis (PCA) was applied to reduce the 18-dimensional EEG signals to three-dimensional sequences [14].
- Model Training & Optimization: An RBF neural network was trained on the EEG time-series data, with Particle Swarm Optimization (PSO) used to optimize model parameters and identify fixed points in the reconstructed neural system [14].
Key Performance Data (Model Accuracy):
| Metric | Value |
|---|---|
| Normalized Root Mean Square Error (NRMSE) | 0.0671 ± 0.0074 |
| Pearson Correlation Coefficient | 0.892 ± 0.0678 |
Source: Front. Neurosci., 2025 [14].
The Scientist's Toolkit: Essential Research Materials
A selection of key reagents, materials, and software used in modern EEG experiments.
| Item | Function & Application |
|---|---|
| SMOTE Technique | A data preprocessing technique used to solve class imbalance in datasets, crucial for building unbiased classifiers in tasks like sleep stage classification [18]. |
| Principal Component Analysis (PCA) | A statistical procedure for feature reduction; used to identify and prioritize the most significant features from a large set of extracted EEG features [18] [14]. |
| Independent Component Analysis (ICA) | A computational method for separating multivariate signals into additive subcomponents, widely used for artifact removal (e.g., eye blinks, muscle activity) from EEG data [14]. |
| LSTM Network | A type of recurrent neural network (RNN) well-suited for classifying and predicting time-series data, such as EEG sequences for sleep staging or seizure detection [18]. |
| RBF Neural Network | A type of artificial neural network that uses radial basis functions as activation functions. Useful for reconstructing EEG dynamics and modeling non-linear systems [14]. |
| Particle Swarm Optimization (PSO) | A computational method for optimizing a problem by iteratively trying to improve a candidate solution. Used to optimize parameters of neural network models for EEG analysis [14]. |
| Sintered Ag/AgCl Electrodes | Electrodes made from sintered silver/silver-chloride, providing a low noise floor, stable half-cell potential, and resistance to polarization, ideal for high-fidelity recordings [17]. |
| Ultra-Flat (3 mm) Electrodes | Specially designed, low-profile electrodes that minimize the distance between the TMS coil and scalp, reducing artifacts and improving stimulation precision in combined TMS-EEG studies [17]. |
Electroencephalography (EEG) is a foundational tool in neuroscience and clinical research. However, a significant practical challenge persists: the trade-off between data richness and the time-consuming, complex setup of multi-electrode systems. This is especially critical in applications involving vulnerable populations, such as neonates, or in the development of wearable brain-computer interfaces (BCIs). This article examines the evidence for optimizing electrode count, providing technical support for researchers aiming to reduce setup time while preserving data integrity.
Frequently Asked Questions (FAQs)
Q1: What is the core trade-off between the number of electrodes and setup time? The primary trade-off lies between data comprehensiveness and practical feasibility. Multi-channel EEG systems (e.g., 32+ electrodes) provide high spatial resolution and detailed brain mapping but require lengthy setup times of 30 minutes or more. This can cause participant discomfort and reluctance, particularly in clinical or repeated-measurement settings [19]. Minimal-channel systems significantly reduce setup time and improve user comfort but require careful electrode placement to ensure the collected data is sufficient for the specific research or clinical question.
Q2: Can a single EEG channel provide reliable data for classification tasks? Yes, for specific, well-defined tasks. Research on neonatal sleep state classification demonstrated that a single channel (C3) could achieve an accuracy of 80.75% ± 0.82% in classifying five sleep stages [3]. This indicates that for certain applications, a single, optimally placed electrode can capture sufficient information, dramatically reducing technical complexity and the risk of skin irritation.
Q3: Where should minimal electrodes be placed for motor imagery tasks? For motor imagery (MI) tasks, such as imagining hand movements, the sensorimotor cortex is key. One study identified that a configuration of nine electrodes over the central scalp regions (F3, Fz, F4, C3, Cz, C4, P3, Pz, and P4) provided high classification accuracy with a moderate setup time, representing a minimal setup for a successful BCI application [19].
Q4: What is the "end of chain" phenomenon in bipolar montages? In bipolar montages, where electrodes are linked in a chain, the first and last electrodes in each chain lack a second point of comparison. This "end of chain" phenomenon means you only see half of any potential phase reversals at these electrodes (like Fp1, Fp2, O1, O2), which can hinder the localization of electrical activity. This can be mitigated by using alternative montages, such as a circumferential montage [20].
Troubleshooting Guide: Common EEG Setup Issues
Problem: Persistent high impedance or abnormal signal in one or multiple channels.
| Troubleshooting Step | Actions & Checks |
|---|---|
| 1. Check Electrode Connections | Ensure all electrodes are plugged in correctly. Re-clean and re-apply the problematic electrode(s) with appropriate conductive paste or gel. Swap the suspect electrode with a known good one to rule out a "dead" electrode [6]. |
| 2. Inspect Ground/Reference | The ground (GND) electrode can affect all channels. Reapply the GND, ensuring proper skin preparation. Try alternative GND placements (e.g., hand, sternum) to isolate the issue [6]. |
| 3. Verify Hardware Function | Restart the acquisition software, computer, and amplifier. If possible, test the setup with a different headbox or on a different acquisition system in another room to rule out hardware failure [6]. |
| 4. Check for Participant Factors | Ask the participant to remove all metal accessories. Consider if hairstyle, skin products, or unique skin properties (e.g., static electricity, moisture levels) might be causing bridging or signal oversaturation [6]. |
The logical workflow for systematic troubleshooting is outlined below:
Recent studies provide quantitative evidence for optimizing electrode count across different applications. The following table summarizes key findings from the literature.
Table 1: Evidence for Electrode Number Optimization in Different Applications
| Application | Optimal Electrode Configuration | Performance Metrics | Key Findings |
|---|---|---|---|
| Neonatal Sleep Staging [3] | Single channel: C3 | Accuracy: 80.75% ± 0.82%Kappa: 0.76 | A single, optimally placed electrode can provide high classification accuracy for sleep states, reducing setup complexity. |
| Neonatal Sleep Staging [3] | Multi-channel: Four left-side electrodes (F3, C3, T3, P3) | Accuracy: 82.71% ± 0.88%Kappa: 0.78 | A small, asymmetric cluster can outperform both single-channel and other multi-channel configurations (e.g., four right-side electrodes: 81.14% accuracy). |
| Hand Motor Imagery (BCI) [19] | 9 electrodes (F3, Fz, F4, C3, Cz, C4, P3, Pz, P4) | High classification accuracy | This configuration was selected as the minimal channel setup that provided high accuracy with a moderate, user-friendly setup time. |
The process of determining the minimal number of electrodes for a wearable BCI, as investigated in one study, involves a structured experimental and analytical workflow.
The Scientist's Toolkit: Research Reagents & Materials
Table 2: Essential Components for EEG-Based BCI Research
| Item / Technique | Function / Description |
|---|---|
| International 10-20 System | Standardized method for electrode placement on the scalp, ensuring consistency and reproducibility across studies [20] [21]. |
| Differential Amplifier | Amplifies the voltage difference between two electrodes, effectively cancelling out common noise (common mode rejection) to improve the signal-to-noise ratio [21]. |
| Filter Bank Feature Extraction | A signal processing technique that decomposes the EEG signal into multiple frequency bands, which is particularly useful for detecting event-related desynchronization/synchronization (ERD/ERS) in motor imagery tasks [19]. |
| Common Spatial Pattern (CSP) | A spatial filtering algorithm used to optimize the discrimination between two classes of EEG signals (e.g., left vs. right hand motor imagery) [19]. |
| SMOTE Technique | Synthetic Minority Over-sampling Technique. Used to address class imbalance in datasets by generating synthetic samples of the underrepresented classes, improving classifier performance [3]. |
| Spherical Spline Interpolation (SSI) | A mathematical method to estimate the signal of a faulty or missing electrode based on the signals from surrounding electrodes. Note: One study found it may not improve classification accuracy for minimal channels [19]. |
Troubleshooting Guides and FAQs
FAQ 1: How many electrodes can I realistically remove from a standard 64-channel system without significantly hurting my classification accuracy?
A systematic evaluation of electrode reduction for Speech Imagery Brain-Computer Interfaces (SI-BCIs) found that the original 64 channels could be reduced by 50% without a significant loss in classification accuracy [2]. This indicates that for many applications, a 32-channel setup may be sufficient, striking a balance between performance and practicality.
However, the optimal configuration is highly subject-specific. The same study could not identify a single, consistent set of optimal electrode positions across different datasets and individuals [2]. Therefore, while a 50% reduction is a good rule of thumb, the best approach is to individually tailor the electrode configuration for each user or research population.
FAQ 2: Are there specific brain regions where electrode placement is more critical for accurate classification?
The importance of electrode placement is task-dependent, and contrary to common assumptions, critical areas may not be limited to the classic brain regions associated with a task.
- For Neonatal Sleep Staging: Research suggests a hemispheric bias. One study found that classification accuracy for four left-side electrodes was higher (82.71% ± 0.88%) than for four right-side electrodes (81.14% ± 0.77%) [3]. Furthermore, a single C3 channel (over the left central cortex) achieved an accuracy of 80.75% ± 0.82%, which was superior to other single channels tested [3].
- For Speech Imagery (SI-BCIs): Relevant areas were not limited to the left hemisphere (traditionally responsible for speech) but were distributed across the cortex [2]. This suggests that a broad coverage, rather than a focused placement on classic language areas, might be necessary for optimal decoding of imagined speech.
FAQ 3: My classification performance drops when the EEG cap is repositioned or used on a new subject. How can I mitigate this electrode shift problem?
Electrode placement variability is a recognized challenge that reduces classification robustness. A recent solution is the Adaptive Channel Mixing Layer (ACML), a plug-and-play preprocessing module for deep learning models [22].
- How it works: The ACML applies a learnable transformation matrix to the input EEG signals, dynamically re-weighting channels based on their inter-correlations. This helps compensate for spatial misalignments caused by cap repositioning or anatomical differences between subjects [22].
- Performance: Experimental validation showed that integrating ACML improved classification accuracy (up to 1.4%) and kappa scores (up to 0.018) across subjects, enhancing resilience to electrode shifts [22].
FAQ 4: Does rigorous preprocessing for artifact removal always lead to better decoding performance?
Not necessarily. A systematic multiverse analysis of preprocessing choices revealed a counterintuitive finding: artifact correction steps often decrease decoding performance [23].
- Reason: Artifacts (like eye movements or muscle activity) can be systematically associated with the task or condition being decoded. For example, in a visual attention task (N2pc), eye movements are predictive of the target location. Removing these "artifacts" also removes the predictive signal, hurting performance [23].
- Recommendation: While removing artifacts is crucial for the interpretability of neural signals and model validity, researchers focused purely on maximizing decoding accuracy should carefully evaluate the impact of each artifact correction step. The study also found that using a higher high-pass filter cutoff consistently increased decoding performance [23].
FAQ 5: Can I use a population-optimized electrode montage instead of creating individualized setups for every subject?
Yes, population-optimized approaches are a viable and practical strategy. Research in transcranial temporal interference stimulation (tTIS) has demonstrated that montages optimized using group-level electric field analysis can achieve targeting effects comparable to individualized optimization, with a difference of up to 17% in focality [5].
- Key Factor - Population Size: The accuracy of this approach depends on the size of the representative population. Insufficient population size leads to inconsistencies, but these are negligible for populations larger than 40 individuals [5].
- Key Factor - Age Matching: Age mismatch between the population proxy and the target individual can reduce focality by up to 8.3%, so using an age-matched population proxy is recommended [5].
This approach eliminates the need for individual MRI scans, significantly enhancing the accessibility and practicality of optimized montages [5].
Performance Metrics for Electrode Montages
Table 1: Quantitative Performance of Different Electrode Setups
| Application | Optimal Setup | Performance Metrics | Key Findings |
|---|---|---|---|
| Neonatal Sleep Staging [3] | Single C3 channel | Accuracy: 80.75% ± 0.82%Kappa: 0.76 | Single-channel performance can be high, reducing system complexity. |
| Four left-side electrodes | Accuracy: 82.71% ± 0.88%Kappa: 0.78 | Left-side electrodes showed a slight performance advantage over right-side. | |
| Speech Imagery BCI [2] | 50% reduced montage (32 channels) | No significant performance loss vs. 64-channel setup. | A 32-channel setup balances accuracy and practicality for SI-BCIs. |
| Motor Imagery BCI [22] | Standard setup + ACML | Accuracy: +1.4% improvementKappa: +0.018 improvement | The ACML module robustly improves performance against electrode shift. |
Experimental Protocols for Key Studies
Protocol 1: Systematic Electrode Reduction for SI-BCIs [2]
- Data Acquisition: Collect EEG data from multiple subjects (e.g., 15+) using a 64-electrode system (10-20 placement).
- Preprocessing: Filter data to remove artifacts and limit the frequency spectrum to the relevant band.
- Feature Extraction & Classification: Apply standard feature extraction (e.g., band power) and classification (e.g., Random Forest) methods.
- Iterative Electrode Reduction: Use a wrapper method algorithm to systematically exclude electrodes one-by-one based on their impact on classification accuracy. The cycle of feature extraction and classification is repeated with the remaining electrodes until only one channel remains.
- Analysis: Identify the point at which classification performance begins to drop significantly and analyze the spatial distribution of the most relevant electrodes.
Protocol 2: Evaluating Population vs. Individual Montage Optimization [5]
- Head Model Creation: Develop personalized computational head models from structural MRIs of a large cohort (>40 individuals).
- Lead-Field Calculation: For each model, calculate the electric field (E-field) distribution for a range of possible electrode montages.
- Optimization:
- Individualized: Optimize the montage for each subject to maximize E-field intensity/focality in a target brain region.
- Population-based: Use a group-level algorithm to find a single montage that optimizes the E-field across the entire population cohort.
- Validation: Use leave-one-out cross-validation to compare the targeting accuracy (focality and intensity) of the population-optimized montage against the individualized montages.
Research Reagent Solutions
Table 2: Essential Tools for EEG Montage Optimization Research
| Item | Function in Research | Example / Note |
|---|---|---|
| High-Density EEG System | Provides the initial, high-resolution brain activity data required for systematic electrode reduction studies. | 64-channel systems with Brain Products LiveAmp hardware are commonly used [2]. |
| Dry Electrode Headsets | Enable practical, long-term monitoring with faster setup times, facilitating real-world data collection. | QUASAR sensors with ultra-high impedance amplifiers allow recording through hair without gel [1]. |
| Computational Head Models | Allow for in-silico testing and optimization of electrode montages without requiring physical experiments on subjects. | Created from structural MRIs using software like SimNibs [5] [24]. |
| Adaptive Preprocessing Algorithms | Mitigate performance degradation caused by real-world variability like electrode shift between sessions. | The Adaptive Channel Mixing Layer (ACML) is a plug-and-play deep learning module [22]. |
| Artifact Removal Tools | Clean non-neural noise from EEG data, though their use requires careful evaluation regarding decoding goals. | RELAX EEGLAB plugin; Independent Component Analysis (ICA) [9] [23]. |
Workflow for Electrode Montage Optimization
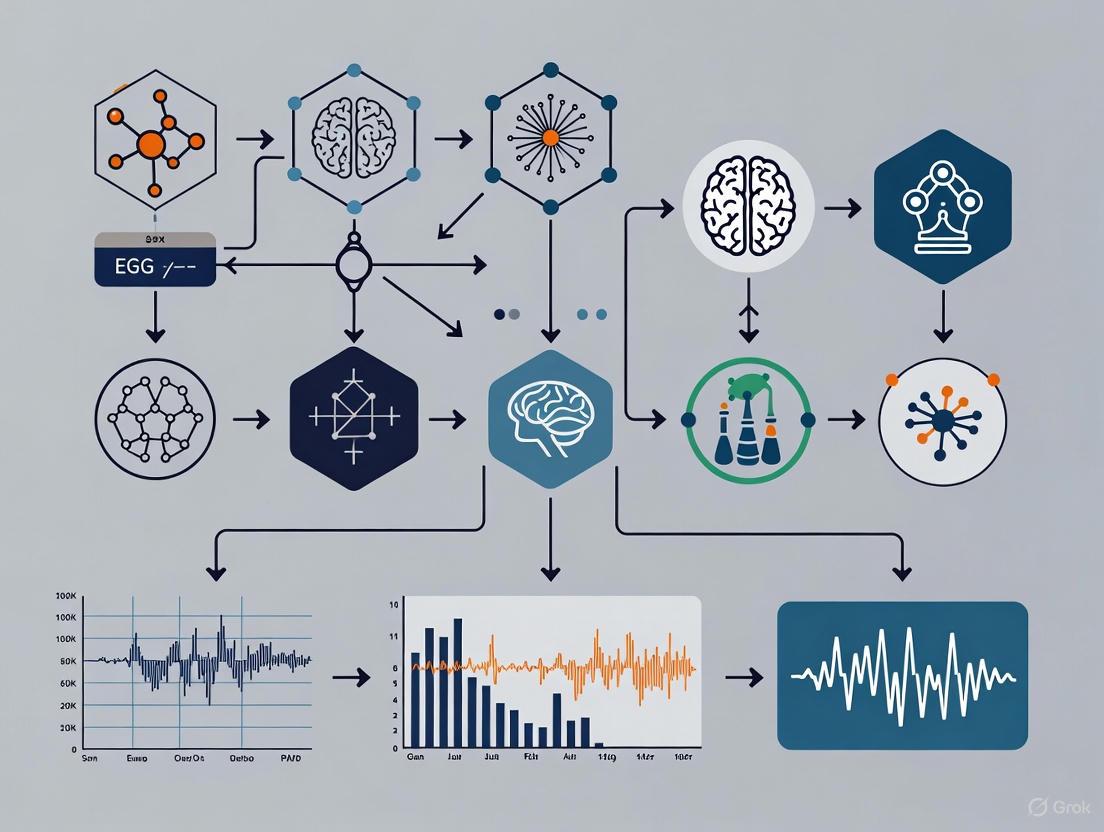
The diagram below outlines a systematic workflow for optimizing an electrode montage, integrating insights from the cited research.
Systematic Approaches for Identifying Optimal Electrode Subsets
Frequently Asked Questions (FAQs)
FAQ 1: Why should I use a Genetic Algorithm for EEG electrode selection instead of a simple filter method?
Genetic Algorithms (GAs) are a powerful choice for this optimization problem because they perform a global search and are less prone to getting stuck in local minima compared to simpler methods [25]. For EEG electrode selection, you are searching for the best combination of electrodes from a very large set of possibilities; GAs efficiently evolve a population of potential solutions (electrode subsets) over generations to find a high-performing, near-optimal configuration [26]. Unlike filter methods that rank electrodes individually, GAs can capture the complex interactions between different electrode sites, leading to a subset that works well collectively for your specific task, such as source localization or signal classification [27] [28].
FAQ 2: My wrapper method is taking too long to run. What can I do to reduce computation time?
The computational expense of wrapper methods is a common challenge [27] [28]. You can address this with several strategies:
- Pre-filtering: Use a fast filter method (e.g., based on mutual information or variance) to remove clearly irrelevant electrodes before applying the more computationally intensive wrapper method [27].
- Set a Feature Limit: Define a maximum number of features (electrodes) to select, which significantly shortens the search process in forward selection or recursive elimination [28].
- Use Cross-Validation Wisely: While cross-validation is essential to prevent overfitting, using a lower number of folds (e.g., 5-fold instead of 10-fold) can speed up the evaluation process [27].
- Leverage Hybrid Algorithms: For GAs, use techniques like "dominant block" mining or association rules to reduce problem complexity and increase solving speed [29].
FAQ 3: I've found an optimal electrode set in my offline analysis. How do I validate it for real-world use?
An optimal electrode set identified through offline analysis must be validated prospectively in an online experiment to confirm its viability [30]. This involves:
- Prospective Testing: Recruit a new cohort of subjects and conduct online sessions using only the reduced electrode configuration [30].
- Performance Comparison: Compare key performance metrics (e.g., classification accuracy, information transfer rate, source localization error) between the reduced set and the full, high-density electrode set [30] [2].
- Statistical Analysis: Perform statistical tests to confirm that there is no significant difference in performance between the full and reduced configurations. A successful validation shows that the reduced set does not degrade system performance while offering practical benefits [30].
Troubleshooting Guides
Problem: Genetic Algorithm Converges Too Quickly to a Sub-Optimal Electrode Set
- Symptoms: The algorithm's performance plateaus early, and the resulting electrode subsets are inconsistent or perform poorly on new data.
- Causes: This is often caused by a loss of population diversity, leading to premature convergence [29].
- Solutions:
- Increase Mutation Rate: Slightly increase the probability of mutation to introduce new genetic material and explore new areas of the solution space [25].
- Implement Chaotic Search: Use an improved Tent map or other chaotic algorithms to enhance the quality and diversity of the initial population, preventing early convergence to local optima [29].
- Review Selection Pressure: Ensure your selection mechanism (e.g., tournament size) is not too strong, which can cause the population to be overrun by a few fit but sub-optimal individuals too early in the process.
Problem: Wrapper Method Leads to Overfitting
- Symptoms: The selected electrode subset performs exceptionally well on your training data but generalizes poorly to unseen test data or new subjects.
- Causes: The method has over-optimized for the specific nuances and noise in your training dataset [27] [28].
- Solutions:
- Strict Cross-Validation: Always use nested cross-validation for a more robust evaluation of the selected feature set. This means having an outer loop for estimating generalization performance and an inner loop for the feature selection process itself [27].
- Simplify the Model: Use a simpler classifier within the wrapper during the selection phase, or increase regularization parameters to make the model less prone to fitting noise.
- Combine with Filter Methods: As a pre-processing step, use a filter method to select a broader, relevant set of electrodes before applying the wrapper method, which reduces the chance of the wrapper finding spurious correlations in a vast search space [27].
Problem: Inconsistent Optimal Electrode Positions Across Subjects
- Symptoms: The algorithm identifies different "optimal" electrode subsets for each subject in your study, making it difficult to define a standard montage.
- Causes: This is a common and expected finding, as brain anatomy and functional topography vary between individuals [2].
- Solutions:
- Subject-Specific Configuration: Accept that optimal configurations are often subject-dependent. The methodology can be applied to find a personalized optimal set for each user, which is then used in all subsequent sessions [2].
- Population-Level Analysis: If a universal set is required, run the optimization algorithm on data from multiple subjects concurrently. Techniques like Gibbs sampling can be used to find a set of electrodes that provides good performance across the entire subject population, even if it is not the absolute best for any single individual [30].
Experimental Data and Protocols
Table 1: Performance of Optimized Low-Density EEG Electrode Sets
This table summarizes quantitative results from key studies that successfully employed algorithm-driven optimization to reduce electrode count.
| Study / Application | Full Montage (Number of Electrodes) | Optimized Montage (Number of Electrodes) | Key Performance Metric | Performance: Full vs. Optimized |
|---|---|---|---|---|
| EEG Source Localization [26] | 231 (HD-EEG) | 6 - 8 | Single-source localization error | Equal or better accuracy in >88% of cases (synthetic) and >63% of cases (real data) |
| P300 Speller [30] | 32 | 4 | Online classification accuracy | No significant difference in subject performance |
| Speech Imagery BCI [2] | 64 | 32 (50% reduction) | Classification accuracy | No significant performance loss |
Table 2: Key Research Reagent Solutions for Algorithm-Driven EEG Optimization
This table details essential computational tools and algorithms used in this field.
| Reagent / Solution | Type | Primary Function in Experiment | Example Use Case |
|---|---|---|---|
| Non-dominated Sorting GA II (NSGA-II) [26] | Multi-objective Genetic Algorithm | Finds optimal trade-off between minimizing electrode count and minimizing localization/classification error. | Automated selection of minimal electrode subsets for accurate EEG source estimation [26]. |
| Gibbs Sampling [30] | Markov Chain Monte Carlo (MCMC) Method | Finds the optimal electrode configuration based on the joint probability of EEG data and known labels. | Optimizing EEG electrode number and placement for P300 speller systems across a subject population [30]. |
| Recursive Feature Elimination (RFE) [27] [2] | Wrapper Feature Selection Method | Recursively removes the least important electrodes (features) based on a model's weights or importance scores. | Systematic reduction of electrodes for Speech Imagery BCI; often used with linear models or SVMs [27] [2]. |
| Stepwise Linear Discriminant Analysis (SWLDA) [30] | Statistical Method / Wrapper | Automatically adds or removes features based on their statistical significance in classifying target vs. non-target stimuli. | A core component for feature selection and classification in P300 BCI systems [30]. |
Detailed Experimental Protocol: GA for Minimal Electrode Selection
The following workflow, based on the NSGA-II methodology, is used to find the minimal electrode subset for accurate EEG source localization [26]:
- Input Preparation: Gather the required inputs: the EEG/ERP signals, a validated head model for source reconstruction, and the ground-truth location of the source activity (if available).
- Population Initialization: Randomly generate an initial population of "chromosomes," where each chromosome is a binary vector representing a possible electrode subset (e.g., a value of '1' means the electrode is included).
- Fitness Calculation: For each chromosome (electrode subset) in the population:
- Reconstruct Sources: Solve the EEG inverse problem (e.g., using wMNE, sLORETA, or MSP) using only the selected electrodes.
- Calculate Localization Error: Compute the error between the estimated source location and the ground-truth location.
- Assign Fitness Scores: The two fitness scores for the multi-objective algorithm are: (1) the localization error (to be minimized), and (2) the number of selected electrodes (to be minimized).
- Evolutionary Loop: Create a new generation by applying:
- Selection: Preferentially select parent chromosomes with better (lower) fitness scores.
- Crossover: Combine pairs of parents to create "offspring" chromosomes, mixing their electrode subsets.
- Mutation: Randomly flip bits in the offspring chromosomes (add or remove electrodes) to maintain diversity.
- Termination and Output: Repeat the evolutionary loop until a stopping criterion is met (e.g., a fixed number of generations). The output is a set of non-dominated "Pareto-optimal" solutions, representing the best possible trade-offs between accuracy and electrode count.
Workflow and Signaling Pathway Diagrams
GA for Electrode Selection
Wrapper Method Logic
Population-Based vs. Subject-Specific Electrode Configurations
Frequently Asked Questions
What is the core difference between population-based and subject-specific electrode configurations? A population-based configuration is a single, fixed set of electrode locations determined to be optimal for a group of users or a specific task. In contrast, a subject-specific configuration is a unique set of electrodes tailored to an individual user, often identified through an initial calibration procedure using a full EEG cap [30] [2].
When should I use a population-based configuration? Population-based setups are ideal for:
- Rapid Deployment: Applications where speed and ease of setup are critical, and a slight reduction in performance is acceptable [30].
- Standardized Tasks: Well-established paradigms where neural signatures are consistently localized across individuals, such as the P300 speller, where a set of four posterior electrodes (PO7, PO8, POz, CPz) may suffice [30].
- Large-Scale Screening: Clinical trials or studies where minimizing setup time and technician burden is a primary concern [31].
When is a subject-specific configuration necessary? Subject-specific configurations are recommended for:
- Complex Cognitive Tasks: Paradigms like speech imagery, where relevant brain activity is distributed across the cortex and varies significantly between individuals [2].
- Maximizing Performance: Applications where achieving the highest possible classification accuracy or source localization precision is the main goal [26].
- Patient Populations: Scenarios involving users with specific neurological conditions or brain anatomy variations that may alter typical brain activation patterns [30].
Can I reduce the number of electrodes without losing significant data quality? Yes, multiple studies demonstrate that electrode counts can often be substantially reduced. Research on speech imagery BCIs showed that 64 channels could be reduced by 50% (to 32 channels) without a significant loss in classification accuracy [2]. Similarly, for certain EEG source localization tasks, optimal subsets as small as 6 to 8 electrodes can achieve accuracy equal to or better than high-density setups with over 200 channels [26].
Are there automated methods to find the optimal electrode set? Yes, several computational methods exist:
- Wrapper Methods: These algorithms (e.g., sequential backward elimination) systematically evaluate the performance of different electrode subsets by iteratively removing the least important channel and re-evaluating the classifier [2].
- Genetic Algorithms: Multi-objective optimization algorithms, like NSGA-II, can simultaneously minimize the number of electrodes and the localization error or maximize classification accuracy to find optimal configurations [26].
- Gibbs Sampling: A Markov chain Monte Carlo method that can be used to find the set of electrodes that optimizes the joint probability of the EEG data and known labels for a given population [30].
Troubleshooting Guides
Issue 1: Poor Classification Accuracy with a Population-Based Configuration
Problem: Your BCI system or neural biomarker analysis is performing poorly with a standard, fixed electrode montage.
Solution:
- Verify Signal Quality: First, confirm that the poor performance is not due to simple signal quality issues like high impedance or excessive noise from movement [32].
- Switch to a Subject-Specific Approach: For complex tasks like imagined speech, a universal configuration is often suboptimal. Implement a subject-specific channel selection protocol [2].
- Implement a Calibration Session:
- Record an initial session using a high-density EEG system (e.g., 64 electrodes).
- Use a wrapper method or genetic algorithm to identify the subset of electrodes that provides the best task classification accuracy for that specific individual.
- Use this personalized subset for all subsequent sessions [2] [26].
Issue 2: High Setup Time with a Full High-Density EEG System
Problem: The process of applying a full 64+ electrode cap is too time-consuming for your study protocol or clinical application.
Solution:
- Adopt a Pre-Defined Reduced Set: For standard tasks (e.g., P300), use a validated, population-based reduced set. For example, a 4-electrode setup (PO7, PO8, POz, CPz) has been shown to be effective for P300 spellers, drastically cutting setup time [30].
- Use Dry Electrode Systems: Consider using dry-electrode EEG headsets. Studies show they can reduce setup time by nearly 50% compared to standard wet EEG systems while maintaining adequate data quality for many applications like resting-state EEG and P300 measurements [31].
- Optimize for Your Population: If your study focuses on a specific population and task, use historical data to derive your own optimized, fixed montage, balancing channel count and performance for your specific needs [30] [26].
Issue 3: inconsistent or Noisy Signals from Specific Electrodes
Problem: Certain channels consistently show poor signal quality, complicating data analysis.
Solution:
- Systematic Troubleshooting: Follow a step-by-step approach to isolate the cause [6]:
- Check Electrodes/Cap: Ensure all connections are secure. Re-clean and re-apply problematic electrodes. Try swapping electrodes to rule out a "dead" sensor [6] [32].
- Check Software/Amplifier: Restart the acquisition software and amplifier. If possible, test the setup in a different room or with a different amplifier system to rule out hardware failure [6].
- Check the Headbox: Swap out the headbox to see if the issue persists [6].
- Check Participant-Specific Factors: Remove all metal accessories. Check for hair products or static that might cause "bridging" between electrodes. Try alternative ground electrode placements (e.g., hand, sternum) [6].
- Exclude and Compensate: If a hardware issue is ruled out and the signal cannot be cleaned, note that some electrode reduction algorithms are robust to the exclusion of a small number of noisy channels. Proceed with your analysis using the remaining good channels [2] [26].
Experimental Protocols & Data
Protocol 1: Gibbs Sampling for Population-Based P300 Speller Configuration
This method finds an optimal electrode set for a group of users [30].
- Data Collection: Collect P300 speller data from a cohort of subjects (e.g., 15+) using a high-density system (e.g., 32 electrodes).
- Feature Extraction: For each stimulus, extract a feature vector from the 600ms of post-stimulus EEG data.
- Model Setup: Represent channel inclusion with a binary vector
c, wherec_j = 1if channeljis used. - Gibbs Sampling: Run a Gibbs sampling algorithm to explore the state space of possible electrode combinations. The algorithm iteratively selects and updates the state of each channel (
c_j) based on its probability given the states of all other channels (c_{-j}) and the known labels. - Validation: The resulting optimal set (e.g., 4 electrodes: PO7, PO8, POz, CPz) should be validated prospectively in a new group of subjects against the full electrode set to confirm non-inferior performance.
Protocol 2: Wrapper Method for Subject-Specific Configuration in Speech Imagery BCI
This protocol is ideal for tailoring a BCI to an individual user for a complex task [2].
- Full Cap Recording: Record EEG data (e.g., with a 64-electrode cap) while the participant performs the imagined speech task.
- Preprocessing: Apply standard preprocessing: bandpass filtering and artifact removal (e.g., using ICA).
- Initial Classification: Extract features (e.g., band power, Riemannian geometry features) and establish a baseline classification accuracy using a classifier (e.g., SVM, LDA) with all electrodes.
- Iterative Electrode Reduction:
- Use a wrapper method to rank the importance of each electrode.
- Remove the least important electrode.
- Retrain the classifier and re-evaluate the accuracy with the reduced set.
- Repeat this process until only one electrode remains.
- Select Optimal Subset: Plot classification accuracy against the number of electrodes. The optimal subject-specific set is the smallest number of electrodes before a significant drop in performance occurs. Research shows this can often be around 50% of the original channels for speech imagery [2].
Quantitative Data on Electrode Reduction
Table 1: Performance of Reduced Electrode Configurations Across Studies
| EEG Paradigm | Full Channel Count | Reduced Channel Count | Performance Outcome | Source |
|---|---|---|---|---|
| P300 Speller | 32 | 4 | No significant difference in online performance compared to full set. | [30] |
| Speech Imagery BCI | 64 | 32 (50% reduction) | No significant performance loss in classification accuracy. | [2] |
| EEG Source Localization (Single Source) | 231 (HD-EEG) | 6-8 | Equal or better localization accuracy in >88% (synthetic) and >63% (real) of cases. | [26] |
| EEG Source Localization (Three Sources) | 231 (HD-EEG) | 8, 12, 16 | Equal or better accuracy in 58%, 76%, and 82% of cases, respectively. | [26] |
Table 2: Practical Trade-offs: Setup Time & Comfort
| EEG System Type | Average Setup Time | Technician Ease of Setup (0-10) | Participant Comfort | Source |
|---|---|---|---|---|
| Standard Wet EEG | Benchmark | 7 (Median) | Highest overall comfort | [31] |
| Dry-Electrode EEG | ~50% faster than standard | 9 (Median for fastest device) | Matched standard EEG at best, but varied | [31] |
Methodologies and Workflows
Electrode Reduction Workflow Using a Wrapper Method
The Scientist's Toolkit
Table 3: Essential Research Reagents and Solutions
| Item / Method | Function / Description | Example Use Case |
|---|---|---|
| Genetic Algorithm (NSGA-II) | A multi-objective optimization algorithm used to find electrode subsets that minimize channel count while minimizing source localization error. | Automated selection of minimal electrode sets for accurate EEG source estimation [26]. |
| Gibbs Sampling | A Markov chain Monte Carlo (MCMC) method for estimating high-dimensional distributions to find optimal electrode configurations across a population. | Identifying a population-based set of 4 posterior electrodes for a P300 speller [30]. |
| Wrapper Methods | Feature selection methods that "wrap" around a specific classification model, evaluating electrode subsets based on their actual predictive performance. | Iteratively reducing electrodes for subject-specific Speech Imagery BCIs without significant accuracy loss [2]. |
| Dry-Electrode EEG Systems | EEG headsets using dry contacts that do not require conductive gel, significantly reducing setup and clean-up time. | Reducing patient and site burden in clinical trials for resting-state and P300 measurements [31]. |
| High-Impedance Amplifiers | Amplifiers capable of handling very high electrode-skin contact impedances (>1 GOhm), crucial for obtaining good signals with dry electrodes. | Enabling stable recordings from dry-electrode systems like ear-EEG and headbands [1] [31]. |
The following table summarizes key quantitative findings from studies evaluating reduced EEG montages for seizure detection.
| Study Population | Number of Electrodes in Reduced Montage | Sensitivity for Seizure Detection | Specificity for Seizure Detection | Key Limitations |
|---|---|---|---|---|
| Pediatric (Epilepsy Monitoring Unit) [33] | 8 | 65.3% | 96.8% | Lower sensitivity for generalized (44%), central (43%), and parietal (71%) seizures. |
| Hospitalized Adults [34] | 7 | 70% | 96% | Poor sensitivity for generalized seizures (55%) and nonconvulsive status epilepticus (55%). |
| Critically Ill Adults [33] | 10 | 67% | Not Specified | Sensitivity is generally reduced compared to full montages. |
Experimental Protocols for Validation
Protocol 1: Retrospective Digital Lead Reduction
This methodology is commonly used to simulate a reduced montage from existing full-montage EEG data [33] [34].
- Data Collection: Obtain full-montage EEG recordings (typically 21 electrodes) from a relevant patient population (e.g., an Epilepsy Monitoring Unit). Include both ictal (seizure) and non-ictal control sequences [33].
- Selection and Anonymization: Randomly select a set of EEG sequences containing a variety of seizure types (focal, generalized, status epilepticus) and control sequences. Anonymize all data [33].
- Digital Montage Reduction: Use EEG software to digitally resample the full montage down to the target reduced montage (e.g., 7 or 8 electrodes). Common electrodes for an 8-lead montage include FP1, FP2, C3, C4, T7, T8, O1, and O2 [33].
- Blinded Review: Have board-certified epileptologists or experienced reviewers evaluate the reduced-montage recordings. Reviewers must be blinded to the original clinical report, patient details, and video data [33] [34].
- Data Analysis: Compare the reviewers' findings from the reduced montage against the original, full-montage EEG report (the "gold standard"). Calculate sensitivity, specificity, and detection rates by seizure type and localization [33] [34].
Protocol 2: Evaluating the Impact of Seizure Localization
This analysis is integral to understanding the performance gaps of reduced montages.
- Categorization by Lobe: Using the gold-standard full-montage reports, categorize each seizure by its onset zone (e.g., frontal, temporal, central, parietal, occipital, generalized) [33].
- Calculate Detection Rates: For each localization category, calculate the proportion of seizures that were successfully identified by the reviewers using the reduced montage [33].
- Statistical Comparison: Use statistical tests, such as Fisher's exact test, to determine if the rate of missed seizures is significantly different across brain regions [33].
FAQs and Troubleshooting Guides
Q1: What is the primary trade-off when using a reduced EEG montage for seizure detection?
The primary trade-off is between setup efficiency and diagnostic sensitivity. While reduced montages (7-10 electrodes) significantly decrease application time and complexity, this comes at the cost of lowered sensitivity for detecting seizures, particularly those that are generalized or originate in brain regions not covered by the sparse electrode array [33] [34]. Specificity, however, remains high, meaning that if a seizure is identified on a reduced montage, it is very likely to be a true positive [33] [34].
Q2: For which type of seizures are reduced montages most likely to fail?
Reduced montages show the highest rates of missed detections for parietal lobe seizures (up to 71% missed) and generalized seizures (up to 44% missed) [33]. They also demonstrate poor sensitivity for nonconvulsive status epilepticus (NCSE) and generalized ictal patterns [34]. This is because the limited spatial coverage may not capture seizure activity originating in "silent" brain areas or diffuse activity that requires broader sampling for confident identification.
Q3: We are getting a poor signal from our reference (REF) electrode during setup. What are the systematic troubleshooting steps?
A faulty reference electrode can affect all EEG channels. Follow this systematic workflow to isolate the issue [6]:
Q4: When is it acceptable to proceed with data collection if signal quality issues cannot be fully resolved?
The decision depends on the primary outcome variable of your study [6]:
- If EEG is a secondary variable: In time-sensitive protocols where EEG is not the primary measure, it may be acceptable to proceed with data collection once all troubleshooting steps are exhausted. The signal may improve as electrodes settle [6].
- If EEG is the primary outcome: For studies where EEG data is the critical outcome (e.g., seizure detection studies), every effort must be made to get a clean signal. If unresolved, the session should be canceled and rescheduled to ensure data integrity [6].
The Scientist's Toolkit: Essential Materials
The table below details key materials and their functions for setting up and validating reduced EEG montages.
| Item / Reagent | Function / Application |
|---|---|
| Ten20 Paste | Conductive paste used to secure cup electrodes and ensure a stable, low-impedance connection between the electrode and the scalp [35]. |
| Gold Cup Electrodes | Reusable electrodes for high-fidelity signal acquisition. Often color-coded for consistent setup (e.g., white for reference, black for bias/ground) [35]. |
| Medical Tape | Provides extra stability to electrodes, particularly those on curved surfaces or areas prone to movement (e.g., earlobes), preventing them from falling off during long recordings [35]. |
| Electrode Starter Kit | A kit typically containing electrodes of specific colors, wires, and paste, ensuring consistency with software color-coding protocols and standardizing the setup process [35]. |
| Digital EEG Software (e.g., EDFbrowser) | Free and open-source software used to review, annotate, and convert EEG files. Essential for the digital montage reduction process in retrospective studies [33]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Is a 4-electrode setup truly sufficient for accurate P300 spelling, and what performance level can I expect?
Yes, research demonstrates that a properly optimized set of four electrodes can perform statistically identically to a full 32-electrode setup in online prospective testing. One study found a specific four-electrode set (PO8, PO7, POz, CPZ) performed effectively, with no significant difference in performance compared to the full montage [36]. The average bit rates plateaued after four channels, with no significant gains from additional electrodes [36].
Q2: Which specific electrode locations form an optimal 4-electrode montage?
Evidence points to posterior electrode placements being critical. A Gibbs sampling method identified the combination PO8, PO7, POz, and CPZ as optimal across a subject population [36]. These locations cover the parietal-occipital regions where the P300 signal is strongest.
Q3: What is the primary methodological approach for selecting an optimal minimal electrode set?
A Gibbs sampling method can identify optimal electrode configurations across a subject population by evaluating the joint distribution of EEG signals and known labels [36]. This approach finds a single, effective configuration for an entire population, eliminating the need for individual calibration.
Q4: My system's performance dropped significantly after moving to a reduced montage. What should I check?
- Verify Electrode Positions: Confirm that the electrodes are placed precisely on PO8, PO7, POz, and CPZ according to the 10-10 international system.
- Check Signal Quality: Ensure impedance values are below 10 kΩ for all electrodes to guarantee good signal quality [37].
- Retrain the Classifier: Always retrain your classification algorithm (e.g., SWLDA, Naïve Bayes) on data collected from the new, reduced montage. Classifier performance is highly dependent on the specific channels used [38].
Q5: How does electrode reduction impact the practical setup and use of a P300 speller?
Reducing electrodes directly addresses major barriers to clinical adoption:
- Reduces system setup time and complexity [36].
- Lowers hardware costs due to fewer electrodes and simpler amplifiers [37] [36].
- Decreases computational requirements and signal bandwidth needs [36].
- Improves user comfort, enhancing prospects for long-term use [38].
Common Issues and Solutions
| Problem Area | Specific Issue | Recommended Solution |
|---|---|---|
| Signal Quality | Low signal-to-noise ratio (SNR) | Verify electrode impedance (<10 kΩ); ensure proper scalp preparation [37]. |
| System Performance | Low classification accuracy with reduced montage | Retrain classifier with new montage data; confirm optimal electrode placement (PO8, PO7, POz, CPZ) [36] [38]. |
| Experimental Design | Inconsistent P300 elicitation | Standardize stimulus parameters (e.g., inter-stimulus interval ~200ms); ensure user focus on target [39]. |
| Data Processing | Inefficient channel selection | Implement Gibbs sampling or Jumpwise Regression for robust, computationally efficient selection [37] [36]. |
Performance Data for Electrode Configurations
Table 1: Comparative Performance of Different P300 Speller Electrode Montages
| Number of Electrodes | Specific Electrodes | Key Performance Metrics | Reference |
|---|---|---|---|
| 32 (Full Montage) | Standard 10-10 system locations | Baseline performance | [36] |
| 8 (Common Reduced) | C3, Cz, C4, P3, Pz, P4, O1, O2 | Statistically significant P300 detection (p<0.01) with medium/large effect sizes [39] | [39] |
| 6 (Empirically Chosen) | Fz, Cz, Pz, Oz, P3, P4 | Common research configuration | [36] |
| 4 (Optimized) | PO8, PO7, POz, CPZ | No significant performance difference vs. full montage; performance plateau | [36] |
Table 2: Quantitative Performance Metrics from P300 Studies with Electrode Reduction
| Study Focus | Optimal Channel Count | Accuracy | Information Transfer Rate (ITR) | Key Finding |
|---|---|---|---|---|
| Wireless P300 System [39] | 8+ electrodes | 85% (40 trials) to 100% (100 trials) | Not Reported | System functionality confirmed with wireless stimulus presentation |
| Population Optimization [36] | 4 electrodes | Not significantly different from 32-channel | Plateau after 4 electrodes (26.4 bits/min with 3 electrodes) | Gibbs sampling identified population-optimal montage |
| Genetic Algorithm Optimization [26] | 6-8 electrodes (Source Localization) | Comparable to HD-EEG (>88% cases) | Not Applicable | Method identifies minimal electrode subsets for specific source activities |
Experimental Protocols
Detailed Methodology: Validating a 4-Electrode P300 Speller
Objective: To determine if an optimized 4-electrode montage (PO8, PO7, POz, CPZ) can achieve performance statistically equivalent to a full 32-electrode montage in online P300 speller operation [36].
Equipment and Setup:
- EEG amplifier system (e.g., g.tec amplifiers)
- Electrode cap with 32 channels in established configuration
- Active EEG electrodes
- Stimulus presentation computer running BCI2000 or similar software
- Display monitor for P300 speller grid
Participant Preparation:
- 15+ healthy subjects with normal or corrected-to-normal vision
- Apply electrode cap according to 10-10 international system
- Reduce impedance for all electrodes to <10 kΩ [37]
- Ground electrode on forehead, reference on right earlobe [40]
Data Collection Protocol:
- Calibration Phase: Present "PACK MY BOX WITH FIVE DOZEN LIQUOR JUGS" for subject to spell with full 32-electrode montage [40] [36].
- Stimulus Parameters: Use Row/Column paradigm (Farwell & Donchin, 1988) with 5-15 repetitions [40].
- Signal Processing: Bandpass filter EEG data to [0.5 Hz, 30 Hz] and digitize at 256 Hz [37].
- Classifier Training: Employ Naïve Bayes classifier or Stepwise Linear Discriminant Analysis (SWLDA) on calibration data [36] [41].
Experimental Conditions:
- Full Montage: Online testing with all 32 electrodes
- Reduced Montage: Online testing with only PO8, PO7, POz, CPZ electrodes
- Control Condition: Test with empirically chosen 6-electrode set (Fz, Cz, Pz, Oz, P3, P4) for comparison
Data Analysis:
- Perform repeated-measures ANOVA to compare bit rates between conditions
- Use paired t-tests for pairwise comparisons with Bonferroni correction
- Calculate information transfer rate (ITR) as primary performance metric [36]
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for P300 Speller Studies
| Item | Specification/Example | Primary Function |
|---|---|---|
| EEG Amplifier | g.tec g.USBamp, OpenBCI board [37] [40] | Signal acquisition and digitization |
| Electrode Cap | 32-channel cap with 10-10 international system [36] | Standardized electrode placement |
| Active EEG Electrodes | Guger Technologies active electrodes [36] | Improved signal quality with pre-amplification |
| Electrode Gel | Electrolyte gel | Maintain conductivity and reduce impedance |
| BCI Software Suite | BCI2000, OpenViBE [37] [40] | Experiment control, data acquisition, and signal processing |
| Stimulus Presentation Monitor | Standard computer monitor | Visual presentation of P300 speller grid |
| Classifier Algorithms | Naïve Bayes, SWLDA [36] [41] | Translation of EEG features into character selection |
Methodology Visualization
Diagram 1: Electrode Optimization and Validation Workflow
Diagram 2: Optimal 4-Electrode Montage for P300 Speller
Implementing Dry Electrode and Wearable Systems for Rapid Deployment
Troubleshooting Guide
This guide addresses common technical challenges when using dry-electrode EEG systems for rapid deployment, helping researchers maintain data quality and experimental efficiency.
Table 1: Common Technical Issues and Solutions
| Problem Category | Specific Issue | Possible Causes | Recommended Solutions & Verification Steps |
|---|---|---|---|
| Signal Quality | Poor signal-to-noise ratio, high-frequency noise [31] | High electrode-skin impedance; Motion artifacts; Environmental electrical interference. | Ensure proper sensor-scalp contact via headset adjustment; Use systems with built-in common-mode follower circuitry and Faraday cages [42] [43]. |
| Signal Quality | Attenuated low-frequency (<6 Hz) or induced gamma (40-80 Hz) activity [31] | Hardware limitations of specific dry-electrode systems. | Benchmark device performance for target frequency band; Avoid these bands for analysis or select a system validated for them [31]. |
| Subject Comfort & Compliance | Discomfort during prolonged use, declining comfort over time [31] | Excessive pressure from rigid electrode structures; Improper headset fit. | Select systems with ergonomic designs and adjustable straps; Limit recording session length; Use soft foam padding [42]. |
| Operational Efficiency | Prolonged setup or cleaning | Complex montages; Lack of technician training. | Use pre-configured headbands; Implement standardized training protocols [44]. Opt for devices with easy cleaning (e.g., with 70% alcohol) [42]. |
| Data Integrity | Inconsistent performance in reduced-electrode montages [45] | Use of a generic, non-optimized electrode subset. | Employ systematic electrode reduction algorithms (e.g., wrapper methods) to identify subject-specific optimal channels [45]. |
Frequently Asked Questions (FAQs)
Q1: How does the signal quality of dry-electrode EEG compare to conventional wet EEG? High-quality dry-electrode systems can perform on par with wet EEG for many applications. Studies show over 90% correlation with wet system signals and adequate capture of resting-state EEG and P300 evoked potentials [42] [31]. However, some dry systems may face challenges with very low-frequency (<6 Hz) or induced gamma activity, so device selection should be matched to the research context [31].
Q2: To what extent can we reduce the number of electrodes without significant performance loss? Substantial reduction is often possible. Research on Speech Imagery BCIs found that 64 channels could be reduced by 50% without a significant loss in classification accuracy [45]. For P300 speller systems, a minimal set of just four optimized electrodes has been shown to perform statistically identically to a full 32-electrode montage [36]. The optimal configuration is often subject-specific [45].
Q3: What are the key factors in choosing a dry-electrode system for a clinical trial setting? Key factors include [31]:
- Data Quality for the Application: Ensure the system captures the neural signals of interest (e.g., P300, resting-state).
- Setup and Clean-up Speed: Dry systems can be up to twice as fast as wet EEG, reducing site burden.
- Participant Comfort: While a key advantage, comfort varies by device and can decline over time.
- Ease of Use: Technicians rate some dry systems as significantly easier to set up and clean.
Q4: How can I identify the optimal subset of electrodes for my specific BCI experiment? A systematic, data-driven approach is recommended. A wrapper method, which evaluates channel subsets based on classification accuracy, is an effective technique [45]. This involves iteratively reducing electrodes and re-evaluating performance to find the minimal set that maintains high accuracy for your task and subject pool.
Experimental Protocols for Electrode Optimization
This section provides a detailed methodology for conducting electrode reduction studies, a core research area for minimizing setup time.
Protocol 1: Systematic Electrode Reduction for a Specific BCI Paradigm
This protocol is based on research that successfully reduced channels for Speech Imagery and P300 speller BCIs [45] [36].
1. Objective: To determine the minimal number of EEG electrodes and their optimal positions for a specific BCI task (e.g., motor imagery, P300) without significantly compromising classification accuracy.
2. Materials and Equipment:
- EEG system with a high channel count (e.g., 64 electrodes).
- Standardized stimulus presentation software.
- Computing environment with machine learning libraries (e.g., Python scikit-learn, MATLAB).
3. Procedure:
- Step 1: Data Collection. Record EEG data from multiple subjects using a full high-density montage (e.g., 64-channels based on the 10-20 system) while they perform the target BCI task.
- Step 2: Preprocessing. Apply standard preprocessing: band-pass filtering (e.g., 0.5-40 Hz), artifact removal (e.g., using ICA), and epoching.
- Step 3: Feature Extraction. Extract relevant features from the epoched data. Common features include time-domain (e.g., mean amplitude, variance), frequency-domain (e.g., band power), and nonlinear features (e.g., entropy) [18].
- Step 4: Electrode Reduction Algorithm.
- Implement a wrapper method for electrode selection [45].
- Start with the full set of electrodes.
- In each iteration, train and evaluate a classifier (e.g., LDA, SVM, Naïve Bayes) using a subset of electrodes.
- Rank or select electrodes based on their contribution to classification accuracy (e.g., using a method like Gibbs sampling) [36].
- Iteratively remove the least important electrode and re-evaluate performance until only one channel remains.
- Step 5: Performance Validation. Validate the optimal reduced set identified in Step 4 through prospective online testing with new subjects, comparing its performance against the full montage.
The workflow for this protocol is outlined below.
Protocol 2: Benchmarking Dry-Electrode System Performance
This protocol outlines a method for quantitatively comparing dry-electrode systems against a gold-standard wet EEG, as used in clinical trial research [31].
1. Objective: To benchmark the performance of one or more dry-electrode EEG devices against a standard wet EEG system across multiple neurophysiological tasks.
2. Materials and Equipment:
- Dry-electrode EEG device(s) under evaluation.
- Standard wet-EEG system (control).
- A suite of tasks for biomarker assessment (e.g., resting-state, auditory oddball P300, steady-state visual evoked potentials).
3. Procedure:
- Step 1: Study Population. Recruit a cohort of healthy participants or target patient population.
- Step 2: Experimental Design. Employ a within-subjects or cross-over design where each participant is tested with all EEG systems, ideally on separate days to avoid fatigue.
- Step 3: Data Acquisition. For each system, record EEG while participants complete the task battery. Meticulously log setup and clean-up times.
- Step 4: Subjective Burden Assessment. Administer standardized questionnaires to participants (e.g., comfort ratings) and technicians (e.g., ease of use ratings) after each session.
- Step 5: Quantitative Signal Analysis. Preprocess all data uniformly. Compare key signal metrics between devices, such as:
- Signal-to-noise ratio for evoked potentials (e.g., P300 amplitude).
- Power in relevant frequency bands during resting-state.
- Classification accuracy in a BCI paradigm.
Research Reagent Solutions
Table 2: Essential Materials for Dry-Electrode EEG Research
| Item | Function & Rationale |
|---|---|
| Dry-Electrode EEG Headsets (e.g., DSI-7, DSI-24, CGX Quick-20R, Zeto zEEG) | Mobile, gel-free acquisition systems designed for rapid setup. Key for reducing deployment time and participant burden [31] [42]. |
| Conductive Gel Pods (for semi-dry systems) | Used in some point-of-care systems (e.g., BrainWatch) for rapid, integrated gel dispensing. A compromise maintaining signal quality with faster setup than traditional wet EEG [44]. |
| Auxiliary Sensors (ECG, EMG, EOG, GSR) | Synchronized with EEG to measure physiology and identify artifacts (e.g., eye blinks, muscle activity), improving data interpretation [43]. |
| Wireless Trigger Hub | Simplifies synchronization of the EEG system with external devices like eye-trackers and stimulus presentation software, which is crucial for timed experiments in mobile settings [43]. |
| Data Acquisition & Analysis Software (e.g., DSI-Streamer, NeuroWorks, BCILAB, EEGLAB) | Software for recording, visualizing, and processing raw EEG data. Compatibility with analysis platforms is vital for research [42] [44]. |
| Cognitive State Classification Tools (e.g., QStates) | Machine learning software for classifying cognitive states (e.g., workload, engagement) from EEG data, enabling higher-level analysis [42] [43]. |
The decision-making process for implementing a rapid-deployment system, based on the cited research, is summarized in the following diagram.
Solving Practical Challenges in Reduced Montage Implementation
Addressing Anatomical Variability in Electrode Placement
This technical support center provides troubleshooting guides and FAQs to help researchers address the critical challenge of anatomical variability in electrode placement. Proper placement is essential for data quality, source localization accuracy, and the reliability of conclusions in EEG research and drug development.
Troubleshooting Guides
Guide 1: Poor Source Localization Accuracy
Problem: Inaccurate reconstruction of neural activity sources, often due to improper head modeling or electrode coregistration [46] [47].
Solution: Implement an individualized forward modeling approach.
- Acquire Individual Anatomy: Obtain a structural T1-weighted MRI for each subject [46].
- Digitize Electrode Positions: Use a 3D digitizer to record the precise location of each electrode relative to anatomical fiducials (nasion, left/right preauricular points) [46].
- Generate Head Model: Create a Boundary Element Method (BEM) or Finite Element Method (FEM) head model using specialized software (e.g., SimNIBS, MNE-Python, FieldTrip). Using SimNIBS for highly accurate anatomical modeling has been shown to substantially improve the EEG forward solution compared to established pipelines in other software [47].
- Coregister Electrodes: Align the digitized electrode positions with the individual's head model for source estimation [46].
Guide 2: Low Signal Quality in Specific Demographics
Problem: Poor signal quality in participants with dense hair, textured hairstyles, or unique head anatomy [1].
Solution: Adapt electrode application and technology.
- Skin Preparation: Clean placement sites thoroughly with alcohol pads or soap and water. For very hairy sites, careful shaving might be necessary [48].
- Electrode Choice: Consider dry electrode technology, which is suitable for recording through hair without skin preparation or gel. These systems often feature high-impedance amplifiers to handle higher contact impedances [1].
- Mechanical Stability: Use caps or stabilization systems with patented mechanical isolation designs to minimize movement artifacts [1].
Guide 3: Inconsistent Cross-Subject & Cross-Session Data
Problem: High variability in EEG patterns across different subjects or recording sessions due to electrode placement shifts [22].
Solution: Use spatial normalization and adaptive signal processing.
- Anatomical Projection: For on-scalp sensors (like OPM-MEG or bespoke EEG arrays), apply an anatomical projection method. This method digitally extends the 10-20 system to map 3D sensor positions to a consistent 2D topography based on digitized head shape and fiducials, creating anatomically veridical representations that are comparable across individuals [49].
- Signal-Level Adjustment: Integrate an Adaptive Channel Mixing Layer (ACML) into deep learning models. This plug-and-play module uses a learnable weight matrix to dynamically re-weigh input signals based on inter-channel correlations, compensating for spatial misalignments [22].
Table 1: Impact of Individualization Steps on Auditory Cortex Source Localization (dSPM Inverse Solution)
| Configuration | Anatomy | Electrodes | P1 Amplitude (Left Hemisphere) | N1 Amplitude (Left Hemisphere) | Spatial Leakage (P1, Left) |
|---|---|---|---|---|---|
| 1 | Template | Template | Lowest | Lowest | Highest |
| 2 | Template | Individual | Higher | Higher | Lower |
| 3 | Individual | Template | High | High | Medium |
| 4 | Individual | Individual | Highest | Highest | Lowest |
Source: Adapted from [46]. Data demonstrates that full individualization yields the most focal and robust source estimates.
Frequently Asked Questions (FAQs)
Q1: What is the single biggest source of error in EEG electrode placement? The most significant source of error is the inaccurate coregistration of electrode positions with the subject's individual anatomy. Using template electrode positions (e.g., a manufacturer's layout) on a template head model can introduce substantial errors in the forward solution, which are especially pronounced in occipital and posterior brain areas [47]. One study found that if digitized positions are unavailable, using a set of measured positions from a standard head template is preferable to the manufacturer's layout [47].
Q2: How does anatomical variability specifically affect drug development research? In drug development, researchers often look for subtle, robust neural biomarkers of a drug's effect. Anatomical variability and electrode misplacement add noise and systematic bias to the signal. This can obscure true drug-induced changes in brain activity or create false positives, ultimately reducing the sensitivity and reliability of the EEG as a biomarker, which can impact clinical trial outcomes [46].
Q3: Are there computational methods to correct for placement errors after data collection? Yes, emerging computational methods show promise. The Adaptive Channel Mixing Layer (ACML) is a deep learning technique that applies a learnable linear transformation to input signals, effectively remixing channels to compensate for spatial displacement, improving cross-session classification performance [22]. Furthermore, anatomical projection methods can retroactively map 3D sensor positions from a digitized head shape to a standardized 2D space, improving group-level analysis and visualization [49].
Q4: Our lab cannot acquire MRIs for every subject. What is the best alternative? Using a highly accurate, standardized template head model (e.g., ICBM 2009c) with your subjects' digitized electrode positions is a viable alternative. Research has proven that established source localization pipelines using a shared template forward model can still produce neurophysiologically plausible activation patterns for many cognitive tasks [50]. The key is to use real, digitized electrode positions rather than a generic manufacturer layout [47] [50].
Experimental Protocols
Protocol 1: Quantifying the Impact of Anatomical Accuracy
Objective: To evaluate how individual versus template anatomy affects source localization accuracy of auditory evoked potentials [46].
Methodology:
- Participants: Recruit a cohort of healthy adults.
- Data Acquisition:
- Acquire individual T1-weighted MRIs.
- Record individual electrode positions with a 3D digitizer.
- Perform EEG recording during an auditory task (e.g., presentation of harmonic tones).
- Head Modeling:
- Condition 1 (Fully Individualized): Create a head model (BEM/FEM) from the individual's MRI and coregister with their digitized electrodes.
- Condition 2 (Hybrid): Use the individual's digitized electrodes with a template head model (e.g., ICBM 2009c).
- Condition 3 (Template): Use a template electrode layout on the template head model.
- Source Analysis:
- Calculate the forward solution for each condition.
- Perform source inversion (using dSPM or sLORETA) to estimate activity in the Primary Auditory Cortex (PAC).
- Extract metrics for the P1 and N1 components: peak amplitude, latency, and a spatial leakage metric (power ratio between PAC and surrounding area).
Expected Outcome: Condition 1 (fully individualized) is expected to yield the largest component amplitudes and the least spatial leakage, indicating more focal and accurate source localization [46].
Protocol 2: Validating a Standardized Electrode Montage
Objective: To determine if a reduced, optimal electrode set performs as well as a full high-density array for specific cognitive tasks, such as neonatal sleep stage classification [51].
Methodology:
- Data: Use a pre-existing high-density (e.g., 64-channel) EEG dataset.
- Feature Extraction: From the full dataset, extract a comprehensive set of linear and nonlinear features in time and frequency domains (e.g., including Detrended Fluctuation Analysis, Lyapunov exponent).
- Model Training: Train a classifier (e.g., LSTM) for the task (e.g., sleep stage classification) using the full channel set.
- Channel Optimization:
- Use feature importance ranking (e.g., via Principal Component Analysis) to identify channels that contribute most to classification accuracy.
- Define candidate montages (e.g., single best channel, left-hemisphere clusters, right-hemisphere clusters).
- Performance Comparison: Retrain and test the classifier on the data from the candidate montages only. Compare accuracy and kappa values against the full montage baseline.
Expected Outcome: Research on neonatal sleep found that a single central channel (C3) could achieve ~81% accuracy, and a focused set of four left-side electrodes could slightly outperform a similar right-side set [51]. This protocol can identify a minimal, optimal montage for a given task and population.
Workflow for Protocol 1: Comparing Head Models
The Scientist's Toolkit
Table 2: Essential Research Reagents and Solutions for Individualized EEG
| Item | Function in Research | Example / Specification |
|---|---|---|
| 3D Digitizer | Records the precise 3D spatial coordinates of EEG electrodes relative to anatomical fiducial points (nasion, preauricular). | Electromagnetic or optical tracking systems [46]. |
| Individual T1-weighted MRI | Provides the subject-specific anatomical data required to build an accurate volume conductor model (head model) for forward calculations [46] [47]. | |
| SimNIBS Software | Open-source software for generating highly accurate individual head models, including realistic skull and CSF geometry, using the Finite Element Method (FEM). Shown to reduce forward solution errors [47]. | https://simnibs.github.io/simnibs/ |
| MNE-Python / FieldTrip | Open-source software toolboxes for EEG/MEG data processing. They include pipelines for source analysis, head model creation, and coregistration [47] [50]. | https://mne.tools/https://www.fieldtriptoolbox.org/ |
| Dry Electrode EEG System | Wearable systems using dry electrodes that do not require skin preparation or conductive gel. Enable faster setup and are suitable for recordings through hair, facilitating at-home or naturalistic data collection [1]. | Systems with ultra-high impedance amplifiers (>47 GOhms) to handle contact impedances [1]. |
| ICBM 2009c Template Brain | A standardized, high-resolution nonlinear symmetric template brain. Serves as a common coordinate system and anatomy for forward modeling when individual MRIs are unavailable [50]. |
Mitigating Signal Quality Issues in Non-Ideal Environments
This technical support center provides troubleshooting guides and FAQs to help researchers address common electroencephalography (EEG) signal quality challenges. The guidance is framed within the research goal of reducing EEG setup time through optimal electrode montages, enabling more efficient and robust experiments for drug development and clinical studies.
Troubleshooting Guides
Environmental Electrical Interference
Problem: Significant 50/60 Hz power line noise obscuring the EEG signal of interest.
Solution: Implement a multi-layered approach to eliminate noise sources.
- Check Instrument Grounding: Ensure the EEG system is properly grounded via the third pin of the power plug. A biomedical engineer can verify the wall outlet connection, which is crucial for both safety and reducing line interference [52].
- Modify Laboratory Environment:
- Replace fluorescent or LED lights with incandescent bulbs, as the former can introduce spikes at the power line frequency [52].
- Avoid using dimmer switches for room lights [52].
- Use short, shielded power cords instead of long extension cords, which act as antennas for electromagnetic radiation [52].
- Turn off and unplug all non-essential electronic devices in the vicinity [52].
- Apply Appropriate Filtering: Use the EEG system's built-in 50/60 Hz "notch filter" to selectively reduce this specific interference. Note that this filter should be applied judiciously as it can reduce signal amplitude and create a "ringing" artifact in some types of responses [52].
Physiological Artifacts
Problem: Contamination of the EEG signal from the patient's own biological sources, such as muscle activity.
Solution: Proactive management and post-processing.
- Patient Preparation and Positioning: Instruct the subject to relax their jaw, neck, and facial muscles. A study showed that even the resting activity of the temporalis muscle can generate prominent reflections across the scalp, contaminating signals even at contralateral sites [53]. Ensure the subject's head is comfortably supported to minimize neck muscle engagement.
- Signal Processing Techniques: Employ advanced algorithms to separate neural activity from artifacts.
- Independent Component Analysis (ICA): This technique is highly effective for isolating and removing myogenic (muscle), ocular (eye blink), and cardiac artifacts from the EEG data [53].
- Spatial Filtering: Methods like Common Average Reference (CAR) can help reduce the impact of localized artifacts [53].
Stimulation Artifact in Evoked Potential Studies
Problem: In sensory nerve conduction or auditory/visual evoked potential studies, the large stimulus current can spread and overwhelm the small neurophysiological response.
Solution: Optimize stimulus delivery and use algorithmic correction.
- Prepare the Skin: Clean and dry the skin at the stimulation site thoroughly. This reduces impedance, allowing for lower stimulus intensities and smaller artifacts. Also, dry the skin surface between the stimulation and recording sites to reduce current spread [52].
- Optimize Stimulator Placement: For sensory studies, "rotate" the anode while keeping the cathode over the nerve to find the position that generates the least artifact. Bipolar stimulation can also be effective [52].
- Use Digital Signal Processing: Leverage built-in or custom algorithms, such as an "Enhance" function, which can estimate and subtract the slow, U-shaped stimulus artifact from the recorded signal, providing a cleaner baseline for analysis [52].
Frequently Asked Questions (FAQs)
Q1: How many electrodes are truly necessary for a reliable EEG experiment, such as one involving speech imagery?
A: Research indicates that high-density setups (e.g., 64 electrodes) can often be significantly reduced without major performance loss. One study on speech imagery Brain-Computer Interfaces (BCIs) found that the original 64 channels could be reduced by 50% without a significant drop in classification accuracy [2]. However, the optimal subset was highly subject-specific and distributed across the cortex, not limited to classically defined speech areas [2]. Similarly, a study on neonatal sleep stage classification achieved high accuracy (over 80%) using a single central electrode (C3) [3]. This supports the feasibility of optimized, minimal montages for specific applications.
Q2: What is the impact of slightly misplacing EEG electrodes?
A: Electrode placement variability is a critical challenge that can reduce classification robustness in paradigms like motor imagery. Even a 1 cm displacement can lead to a statistically significant decline in performance [54]. This occurs because the brain regions monitored by a given electrode shift, changing the underlying signal. Modern computational approaches, such as the Adaptive Channel Mixing Layer (ACML), can dynamically adjust input signal weights to compensate for these misalignments, improving resilience to such spatial errors [54].
Q3: Can I use a cost-effective, portable EEG system for advanced research like auditory attention decoding?
A: Yes, validation studies have demonstrated the feasibility of using cost-efficient systems (e.g., based on OpenBCI boards) for complex tasks. One study successfully measured "neural tracking" of speech envelopes and performed auditory attention decoding (AAD) in a non-soundproofed environment [55]. Offline decoder models achieved an average performance of 90% in identifying the attended speaker, proving that robust neural tracking is possible with accessible hardware outside a fully controlled lab [55].
Q4: How does recording time affect the detection of abnormalities in a clinical EEG?
A: Shorter recording times risk missing intermittent abnormalities. A study on pediatric epilepsy found that reducing a standard 20-minute EEG to 15 minutes could miss abnormalities supportive of an epilepsy diagnosis in approximately 6.4% of patients who had such abnormalities [56]. This trade-off between resource efficiency and diagnostic yield must be carefully considered in clinical protocol design.
Experimental Protocols for Key Cited Studies
Protocol 1: Electrode Reduction for a Speech Imagery BCI
This protocol outlines the systematic evaluation of electrode reduction methods as described in [2].
- Data Collection: Record EEG data from participants performing a speech imagery task (e.g., imagining saying specific words) using a high-density cap (e.g., 64 electrodes).
- Preprocessing: Apply band-pass filtering (e.g., 0.5-40 Hz) and remove artifacts using techniques like ICA.
- Feature Extraction: Extract relevant features from the EEG signals (e.g., power spectral density, common spatial patterns).
- Classification: Train a classifier (e.g., Support Vector Machine, Random Forest) to distinguish between the different imagined words using the features from all electrodes.
- Electrode Reduction Loop:
- An electrode reduction algorithm (a "wrapper" method) selects the least contributing electrode and removes it from the dataset.
- The feature extraction and classification steps are repeated with the reduced set.
- This loop continues until only one electrode remains. Classification accuracy is stored at each step.
- Analysis: Plot the classification accuracy against the number of electrodes to identify the optimal balance between setup simplicity and performance.
Protocol 2: Validating a Cost-Efficient EEG Setup for Auditory Attention Decoding (AAD)
This protocol is based on the methodology from [55] for setting up and testing a portable system.
- System Setup:
- EEG Acquisition: Use a cost-efficient amplifier (e.g., OpenBCI Cyton with Daisy Board) with 16 channels.
- Stimulus Presentation & Triggering: Use an Arduino board to synchronize the playback of audio stimuli (from a module like the WAV Trigger) with the EEG recording. The Arduino sends a precise trigger pulse to the EEG amplifier at the exact moment sound begins.
- Experimental Paradigm:
- Participants listen to two competing speech streams (one male, one female) presented dichotically (a different stream to each ear).
- Instruct the participant to focus their attention on one of the two streams.
- Record EEG data for multiple trials (e.g., 5-10 minutes per attended stream).
- Data Analysis - Auditory Attention Decoding:
- Stimulus Envelope: Extract the temporal envelope of each speech stream.
- Decoder Training: Train a linear decoder (e.g., ridge regression) to reconstruct the attended speech envelope from the EEG signals, using time lags of 0-250 ms.
- Performance Evaluation: Calculate the correlation between the reconstructed envelope and the actual attended and unattended speech envelopes. Decoder accuracy is the percentage of trials where the correlation is higher for the attended speech.
Table 1: Impact of Environmental Modifications on Signal Quality
| Modification | Effect on Noise | Key Consideration |
|---|---|---|
| Use Incandescent Lights | Eliminates spikes from fluorescent/LED lights [52] | Less energy-efficient |
| Proper System Grounding | Reduces 50/60 Hz power line interference [52] | Requires verification by a biomedical engineer |
| Remove Dimmer Switches | Eliminates a source of power line spikes [52] | May require changing room infrastructure |
| Use Short, Shielded Cords | Reduces antenna effect and electromagnetic pickup [52] | Less flexibility in lab setup |
| Unplug Unused Devices | Reduces ambient electromagnetic interference [52] | Inconvenient for frequently used equipment |
Table 2: Performance of Reduced Electrode Montages in Various Paradigms
| Research Paradigm | Original Montage | Reduced Montage | Reported Performance |
|---|---|---|---|
| Speech Imagery BCI [2] | 64 electrodes | 32 electrodes (50% reduction) | No significant performance loss |
| Neonatal Sleep Staging [3] | Multi-channel | Single channel (C3) | 80.75% accuracy |
| Auditory Attention Decoding [55] | 16 channels (OpenBCI) | 16 channels (cost-effective system) | 90% offline decoding accuracy |
Experimental Workflow and System Diagrams
Cost-Efficient EEG System Workflow
Systematic Electrode Reduction Protocol
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Key Materials for EEG Experiments in Non-Ideal Environments
| Item | Function / Application | Example / Note |
|---|---|---|
| Disposable Electrodes | Ensures hygiene and standardized recording surface; eliminates cleaning and sharpening of reusable needles [52]. | Pre-gelled surface electrodes for NCS; concentric needle electrodes for EMG. |
| Conductive Electrode Gel | Reduces impedance at the electrode-skin interface, improving signal quality and reducing noise [53]. | Electro-Gel; various brands of NaCl-based or high-viscosity gels. |
| Electrode Caps / Headbands | Provides a standardized and reproducible means of placing electrodes according to systems like the 10-20 system [21]. | EEG Headcap (e.g., MEDCAP); elastic caps with pre-configured electrode holders. |
| Shielded Cables | Prevents cables from acting as antennas, reducing pickup of ambient electromagnetic noise [52]. | Cables with braided shields; prefer short cables over long extension cords. |
| Cost-Efficient EEG Amplifier | Enables research outside traditional lab settings, increasing accessibility and portability [55]. | OpenBCI Cyton Board; systems validated for neural tracking and AAD. |
| Independent Component Analysis (ICA) | A computational "reagent" for separating and removing biological artifacts (muscle, eye blink) from EEG data [53]. | Implemented in software like EEGLAB; requires no physical components. |
| Adaptive Channel Mixing Layer (ACML) | A plug-and-play computational module that mitigates performance degradation from electrode misplacement [54]. | A learnable layer in a neural network that re-weights channels dynamically. |
Adapting Protocols for Special Populations (Pediatric, NDD Patients)
Troubleshooting Guides & FAQs
Frequently Asked Questions
Q1: How can I reduce the number of EEG electrodes for studies involving children with neurodevelopmental disorders (NDD) without compromising data quality?
A: Research demonstrates that the number of electrodes can be significantly reduced by targeting specific brain regions relevant to the condition and task. A study on Speech Imagery Brain-Computer Interfaces (SI-BCIs) found that the original 64 channels could be reduced by 50% without a significant loss in classification accuracy [2]. However, the optimal set of electrodes was highly subject-specific and distributed across the cortex, suggesting that predefined configurations may be suboptimal [2]. For Mild Cognitive Impairment (MCI), a study identified that only four electrodes in the occipital lobe (PO3, PO4, PO7, PO8) were sufficient for effective detection during a working memory task, achieving a sensitivity of 96.2% [57]. When adapting protocols for pediatric or NDD populations, it is crucial to first identify the neural correlates and brain rhythms associated with the specific condition to guide electrode reduction.
Q2: What are the most effective preprocessing methods for cleaning EEG data from pediatric ASD patients?
A: The optimal preprocessing technique depends on whether your priority is maximum signal clarity or preserving the original signal characteristics. A 2025 comparative study on ASD EEG data yielded the following results [58]:
| Preprocessing Method | Key Strength | Best For |
|---|---|---|
| ICA | Superior denoising; Highest Signal-to-Noise Ratio (SNR) [58]. | Applications where signal clarity is the top priority [58]. |
| DWT | Robust feature preservation; Lowest error metrics (MAE, MSE) [58]. | Analyses where preserving the original characteristics of the neural signal is critical [58]. |
| Butterworth Filter | Moderate denoising and feature preservation [58]. | A balanced approach for general-purpose filtering [58]. |
Q3: Are there specific EEG patterns or abnormalities I should look for in children with Autism Spectrum Disorder (ASD)?
A: Yes, quantitative EEG (QEEG) studies have identified distinct patterns in children with ASD. A 2025 exploratory study found that children with mild ASD (Level 1) showed significantly higher amplitude values across all standard frequency bands (Delta, Theta, Alpha, SMR, Beta1, Beta2) compared to their neurotypical peers [59]. Furthermore, an overrepresentation of high-frequency Beta2 waves was discerned in the ASD group [59]. Clinically, another 2025 study reported that epileptiform EEG abnormalities in children with ASD were mainly focal, with a predominance in the left fronto-central temporal region [60]. The presence of widespread epileptiform abnormalities during sleep was correlated with more severe clinical presentations, including a non-verbal profile and greater impairment in social interaction [60].
Q4: What is a major pitfall of common artifact removal methods like ICA, and how can it be avoided?
A: A common pitfall of ICA is that subtracting entire components identified as artifactual can also remove neural signals and, counterintuitively, artificially inflate effect sizes (e.g., for Event-Related Potentials) and bias source localization estimates [9]. This occurs due to imperfect component separation. To avoid this, a targeted cleaning method is recommended. This approach involves cleaning only the artifact-dominated periods (for eye movements) or frequencies (for muscle activity) within a component, rather than subtracting the whole component [9]. This targeted method better preserves neural signals and enhances the reliability of your analysis [9].
Troubleshooting Common Experimental Issues
Issue: Excessive noise and artifacts in EEG recordings from children with NDD due to movement and lack of compliance.
Solution:
- Optimize Preprocessing: Implement a targeted artifact removal pipeline, such as the RELAX method, which selectively cleans artifact periods/frequencies within ICA components instead of removing entire components, thereby preserving more neural data [9].
- Keep Setups Short: Plan shorter recording sessions and use engaging, age-appropriate task paradigms to maintain cooperation.
- Use a Robust Reference: For basic setups, ensure a stable reference electrode is securely attached, such as on an earlobe, using medical tape for extra stability [35].
Issue: Need to validate whether a reduced electrode montage is suitable for my specific research on NDD populations.
Solution:
- Conduct a Pilot Study: Start with a high-density EEG system (e.g., 32 or 64 channels) to record data from your specific population (e.g., children with ASD or patients with Parkinson's disease).
- Apply a Systematic Reduction Workflow: Use a data-driven approach to evaluate the performance of different electrode subsets. The following diagram illustrates a general workflow for optimizing electrode configuration, which can be adapted for NDD research [2] [57].
Protocol 1: Detecting Parkinson's Disease Using Oddball Paradigms and ICA
This protocol, adapted from a 2025 study, uses Independent Component Analysis (ICA) to classify EEG recordings from PD patients and healthy controls [61].
- Population: 25 PD patients (on medication withdrawal) and 25 healthy controls, matched for age and sex [61].
- Task: Auditory oddball paradigm with three sound types:
- Standard: 440 Hz tone (70% of trials).
- Target: 660 Hz tone (15%); participants actively count these.
- Novelty: Natural sounds (15%) [61].
- Data Acquisition: 60-channel EEG, sampled at 500 Hz [61].
- Preprocessing:
- Apply ICA and visually inspect components to identify artifacts (e.g., eye blinks).
- Remove artifactual components and reconstruct clean signals.
- Apply a low-pass FIR filter with a 30 Hz cutoff [61].
- Feature Extraction & Classification:
- Characterize the topological distribution of ICA components, focusing on frontal and central electrodes.
- Use the logarithm of the variance of the ICA components as features.
- Classify using a classifier like Support Vector Machine (SVM) with 5-fold cross-validation [61].
- Expected Outcome: The study achieved a classification accuracy of 88.56%, with 89.36% sensitivity and 87.76% specificity [61].
Protocol 2: Differentiating Mild Cognitive Impairment (MCI) with a Reduced Electrode Set
This protocol details the methodology for identifying an optimal, minimal electrode configuration for detecting MCI during a working memory task [57].
- Population: 21 MCI patients and 20 cognitively normal elderly (NC) controls [57].
- Task: Delayed sample-matching working memory (WM) paradigm. Participants view and remember a sequence of four images during the "coding stage" [57].
- Data Acquisition: 32-channel EEG system [57].
- Analysis for Electrode Reduction:
- Calculate the Power Spectral Density (PSD) for each electrode in the theta (θ) and alpha (α) bands during the WM coding stage.
- Identify electrodes that show the largest significant PSD differences between the MCI and NC groups.
- Group these discriminative electrodes into regional configurations (e.g., occipital OCL4, prefrontal PRL3).
- Build a binary logistic regression model for each configuration and evaluate diagnostic power using ROC curves [57].
The performance of different electrode configurations from this study is summarized below [57]:
| Electrode Configuration | Electrodes Included (Example) | AUC | Sensitivity | Specificity |
|---|---|---|---|---|
| OCL4 | PO3, PO4, PO7, PO8 | 0.765 | 0.962 | - |
| PRL3 | Prefrontal electrodes | 0.683 | 0.794 | - |
| PLL4 | Parietal electrodes | 0.729 | 0.873 | - |
| OPL8 | Occipital + Parietal | 0.830 | 0.943 | - |
Protocol 3: Identifying EEG Biomarkers in Children with Autism Spectrum Disorder (ASD)
This protocol uses QEEG to explore brainwave patterns in children with mild ASD [59].
- Population: 24 children with mild ASD (Level 1) and 24 typically developing children (ages 7-10) [59].
- Data Acquisition: EEG recorded from 13 electrodes (Fz, F3, F4, Cz, C3, C4, P3, Pz, P4, T3, T4, O1, O2) under eyes-open and eyes-closed conditions [59].
- QEEG Analysis:
- Compute the absolute amplitude (in µV) for standard frequency bands: Delta (0.5–4 Hz), Theta (4–8 Hz), Alpha (8–12 Hz), Sensorimotor Rhythm (SMR, 12–15 Hz), Beta1 (15–20 Hz), and Beta2 (20–34 Hz) [59].
- Statistically compare the amplitude values of each band between the ASD and control groups.
- Expected Outcome: The study found significantly higher amplitude values across all bands in the ASD group, with a notable overrepresentation of Beta2 waves [59].
The Scientist's Toolkit
Table: Key Research Reagents and Materials for EEG Studies on Special Populations
| Item | Function / Application | Example / Specification |
|---|---|---|
| High-Density EEG System | Acquiring initial full-head data for subsequent electrode reduction analysis [2] [57]. | 64-channel systems (e.g., Brain Products Live-Amp) are common in research [2]. |
| OpenBCI Hardware | A cost-effective, portable platform for EEG data acquisition, suitable for prototyping wearable setups [35] [58]. | Cyton or Ganglion boards with gold cup electrodes [35]. |
| Ten20 Paste | Conductive electrolyte paste for establishing a stable connection between electrodes and the scalp [35]. | Standard for research-grade wet EEG setups [35]. |
| RELAX Pipeline | A freely available EEGLAB plugin for targeted artifact cleaning, mitigating false positives from standard ICA [9]. | https://github.com/NeilwBailey/RELAX [9]. |
| ADOS-2 | A gold-standard observational assessment tool for diagnosing and characterizing Autism Spectrum Disorder [59] [60]. | Used for participant phenotyping and group confirmation [59]. |
| Butterworth Filter | A standard digital filter for bandpass filtering EEG data, providing a flat response in the passband [58]. | e.g., 0.5 - 40 Hz bandpass for neural signals [58]. |
| Discrete Wavelet Transform (DWT) | A signal processing technique effective for denoising while preserving key signal characteristics in ASD EEG [58]. | Useful for decomposing signals into frequency sub-bands [58]. |
Balancing Computational Load with Feature Extraction Requirements
Frequently Asked Questions (FAQs)
FAQ 1: How much can I realistically reduce the number of EEG electrodes without sacrificing critical data? Research demonstrates that significant electrode reduction is achievable. In speech imagery Brain-Computer Interface (BCI) systems, the original 64 channels can be reduced by 50% without a significant performance loss in classification accuracy [2]. For neonatal sleep state classification, studies show that a single channel (C3) can achieve an accuracy of 80.75% ± 0.82%, which is comparable to more complex setups [3]. The optimal configuration is often highly subject-specific and should be individually tailored [2].
FAQ 2: What are the most efficient feature types for reducing computational load? The choice of features involves a trade-off between computational complexity and informational richness. For a lower computational load, time-domain features (like statistical moments) and frequency-domain features (like power spectral density) are generally less intensive to compute [62]. However, for complex tasks like emotion or sleep stage classification, incorporating non-linear features (such as Sample Entropy, Detrended Fluctuation Analysis, or Lyapunov exponent) can significantly improve accuracy without a prohibitive computational cost [3] [63]. Multi-dimensional features (time-frequency, spatial-temporal) offer the highest information content but require more processing power [62] [64].
FAQ 3: How does electrode placement influence the number of features I need? Optimal electrode placement can reduce the need for extensive spatial features. Research indicates that relevant brain activity is not always limited to classically defined brain areas but can be distributed across the cortex [2]. For instance, in neonatal sleep studies, four left-side electrodes achieved higher classification accuracy (82.71% ± 0.88%) than four right-side electrodes (81.14% ± 0.77%) [3]. Targeting these high-yield regions allows you to extract fewer, more relevant features, thereby lowering the computational load for spatial analysis.
FAQ 4: What is the impact of pre-processing on the overall computational budget? Effective pre-processing is a critical investment. While it adds an initial computational step, it dramatically improves the signal-to-noise ratio. This allows subsequent feature extraction and classification algorithms to work more efficiently, often enabling the use of simpler models or fewer features to achieve the same—or better—accuracy [63] [9]. Advanced artifact removal methods, such as those combining Ensemble Empirical Mode Decomposition (EEMD) and FastICA, can extract purer EEG signals, making feature extraction more effective [63].
Troubleshooting Guides
Problem 1: High Computational Load During Feature Extraction
Symptoms: Model training takes excessively long; system requires high RAM/GPU resources; real-time processing latency is too high.
Possible Causes and Solutions:
| Cause | Diagnostic Steps | Solution |
|---|---|---|
| Excessively High-Dimensional Feature Vector | Review the number of features being extracted per channel. | Employ Feature Selection algorithms (e.g., PCA) to prioritize the most significant features and reduce dimensionality [3] [62]. |
| Inefficient Feature Type for the Task | Evaluate if the feature domain (time, frequency, non-linear) is well-suited for the target application. | For initial trials, start with less computationally complex features (e.g., time-domain statistics) and gradually introduce non-linear or time-frequency features if needed [62]. |
| Redundant EEG Channels | Analyze the contribution of each channel to the classification outcome. | Implement systematic electrode reduction methods to identify and retain only the most informative channels, which directly reduces the total number of features [2] [62]. |
Problem 2: Poor Model Performance After Electrode Reduction
Symptoms: Significant drop in classification accuracy orkappa score after reducing the number of electrodes.
Possible Causes and Solutions:
| Cause | Diagnostic Steps | Solution |
|---|---|---|
| Loss of Spatially Critical Information | Check if the reduced montage excludes brain regions critical for the task. | Do not rely solely on pre-defined anatomical assumptions. Use wrapper methods to find optimal, subject-specific electrode subsets based on classification performance [2]. |
| Inadequate Feature Set | Determine if the current features are too simplistic to capture the neural patterns from fewer channels. | When reducing channels, compensate by extracting more informative features from the remaining ones. Fuse multiple feature types (e.g., time-frequency with non-linear) to enrich the input vector [63] [64]. |
| Suboptimal Channel Combination | Test different combinations of a reduced number of channels. | A combination of a few channels can outperform a single channel. For example, a combination of four left-side electrodes was found to be optimal in one study [3]. Systematically evaluate different subsets. |
Experimental Protocols & Data
Table 1: Performance of Different EEG Channel Setups in Neonatal Sleep Classification
Data derived from [3]
| EEG Setup | Number of Channels | Classification Accuracy | Kappa Value | Key Findings |
|---|---|---|---|---|
| Single Channel (C3) | 1 | 80.75% ± 0.82% | 0.76 | Offers a strong balance between simplicity and performance. |
| Left Hemisphere Set | 4 | 82.71% ± 0.88% | 0.78 | Outperformed the right-side setup in this specific context. |
| Right Hemisphere Set | 4 | 81.14% ± 0.77% | 0.76 | Effective, but slightly less accurate than the left-side setup. |
Table 2: Comparison of EEG Feature Extraction Methods
Data synthesized from [3] [63] [62]
| Feature Domain | Examples | Computational Load | Key Strengths | Ideal Applications |
|---|---|---|---|---|
| Time Domain | Mean, Variance, Hjorth Parameters | Low | Simple, fast to compute, intuitive. | Basic event detection, initial signal characterization. |
| Frequency Domain | Band Power (Delta, Theta, Alpha, Beta, Gamma), Spectral Entropy | Low to Medium | Relates to well-understood brain rhythms. | Sleep staging, arousal/relaxation states, fatigue detection [63]. |
| Non-Linear | Sample Entropy (SampEn), Lyapunov Exponent, DFA, Multiscale Fluctuation Entropy | Medium to High | Captures complex, dynamic properties of brain signals. | Sleep state classification, emotion detection, seizure prediction [3] [64]. |
| Time-Frequency & Spatial-Temporal | Wavelet Transforms, Marginal Hilbert Spectrum (MHS), Phase Locking Value (PLV) | High | Provides a rich, multi-dimensional view of signal dynamics and brain connectivity. | Complex pattern recognition (emotion, motor imagery), network analysis [64] [65]. |
Protocol: Systematic Electrode Reduction for Optimal Montage
This protocol is adapted from methodologies used in speech imagery BCI research [2].
- Data Acquisition & Preprocessing: Record high-density EEG data (e.g., 64 channels) according to the international 10-20 system. Preprocess the data to remove artifacts and filter to the relevant frequency band.
- Baseline Model Training: Extract a comprehensive set of features from all channels and train a classifier to establish a baseline performance accuracy.
- Iterative Electrode Reduction:
- Use a wrapper method that combines a feature extraction technique, a classifier, and a reduction algorithm.
- The algorithm systematically excludes one electrode at a time, based on which removal results in the smallest decrease (or largest increase) in classification accuracy.
- The remaining data is forwarded again through the feature extraction and classification steps.
- This cycle continues until only one channel remains.
- Performance Analysis: Plot the classification accuracy against the number of electrodes to identify the "elbow point"—the point where adding more electrodes no longer provides a significant performance gain.
- Optimal Subset Identification: The subset of electrodes that maintains performance near the baseline with the fewest channels is identified as the optimal montage for that subject or task.
Systematic Electrode Reduction Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in Research |
|---|---|
| Wrapper Method Algorithms | Used for systematic electrode reduction by evaluating channel subsets based on their actual classification accuracy, helping to find the optimal balance between channel count and performance [2]. |
| Noise-Assisted Multivariate Empirical Mode Decomposition (NA-MEMD) | A advanced signal decomposition technique used to process multi-channel EEG data for extracting narrow-band components, which are crucial for subsequent feature analysis like the Marginal Hilbert Spectrum [64]. |
| Fast Independent Component Analysis (FastICA) | An efficient algorithm for blind source separation, crucial for removing artifacts like eye blinks (EOG) and muscle noise from EEG data, resulting in cleaner signals for feature extraction [63]. |
| Phase Locking Value (PLV) | A non-linear metric used to assess functional connectivity between different brain regions by measuring the synchronization of instantaneous phases of EEG signals from different channels [64]. |
| Marginal Hilbert Spectrum (MHS) | Derived from the Hilbert-Huang Transform, it provides a time-frequency distribution of signal energy, capturing local spectral features from non-linear and non-stationary EEG signals [64]. |
| Hybrid CNN-Attention Models | Deep learning architectures that combine Convolutional Neural Networks (CNN) for spatial feature extraction with attention mechanisms to weight the importance of different feature sequences, improving classification accuracy for tasks like motor imagery [65]. |
Troubleshooting Guides
Guide 1: Resolving Synchronization Issues in Multimodal Recordings
Problem: Inconsistent timing between EEG and external devices (like TMS or eye trackers) causes misaligned data, making event-related potential (ERP) analysis unreliable.
Explanation: Precise synchronization is critical for segmenting brain activity and establishing correct correlations. Inaccurate timing can distort ERP waveforms and lead to misguided results [66]. The issue often stems from variable processing delays in stimulus presentation computers or inadequate synchronization protocols between devices [66].
Solution: Implement a robust hardware-based synchronization method.
- Step 1: Diagnose the Source of Jitter
- Check if timing inaccuracies originate from software-based stimulus presentation or from the inter-device communication itself [66].
- Step 2: Choose a Synchronization Method
- For highest precision: Use a photodiode placed on the stimulus screen connected directly to the EEG amplifier. This records the exact moment a visual stimulus is displayed [66].
- For device synchronization: Use Transistor-Transistor Logic (TTL) pulses via direct BNC cable connections. A "heartbeat" signal (e.g., a pulse every 8 seconds) from one device to another allows for post-hoc alignment [67] [66].
- For complex, multi-device setups: Consider software-based solutions like the Lab Streaming Layer (LSL), which provides microsecond-precision timestamping across a network [67].
- Step 3: Validate Synchronization Accuracy
- Record the sync pulses (photodiode or TTL) on a channel of your EEG amplifier. During analysis, verify the consistency of the pulse timings. The temporal accuracy will never exceed the sample period of your slowest device (e.g., ±3.91 ms for a 256 Hz sample rate) [66].
Guide 2: Addressing Artefact-Rich EEG Data in Developmental Populations
Problem: EEG data from children is often contaminated by pronounced movement and muscle artefacts, which are difficult to remove with standard pre-processing pipelines designed for adult data.
Explanation: Children typically exhibit more frequent and pronounced biological artefacts (blinks, movement, EMG). Manual cleaning is time-consuming, subjective, and not scalable for large datasets [68].
Solution: Utilize an automated pre-processing pipeline adapted for developmental data.
- Step 1: Select a Specialized Pipeline
- Implement the RELAX-Jr pipeline, which is fully automated and specifically designed for cleaning EEG data from children [68].
- Step 2: Leverage Adapted Algorithms
- RELAX-Jr uses the 'adjusted-ADJUST' algorithm, which is more sensitive to the increased noise in child data and accounts for their lower alpha peak frequencies [68].
- It employs Multi-channel Wiener Filtering (MWF) and wavelet-enhanced Independent Component Analysis (wICA) to effectively reduce artefacts while preserving neural signals [68].
- Step 3: Assess Cleaning Performance
- Use quantitative metrics to validate the pipeline's effectiveness, such as the Signal-to-Error Ratio and the Artefact-to-Residue Ratio, to ensure artefacts are reduced without removing neural data of interest [68].
Guide 3: Optimizing Electrode Montage for Practical BCI Applications
Problem: A high-density EEG montage provides good performance but is impractical for long-term or real-world use due to long setup times, user discomfort, and hardware costs.
Explanation: While increasing electrode count can enhance spatial information and classification accuracy in paradigms like code-modulated Visual Evoked Potential (cVEP) BCIs, it reduces usability [69].
Solution: Systematically reduce electrode count while monitoring performance impact.
- Step 1: Establish a Baseline
- Begin by running your experiment or analysis with a standard, high-density montage (e.g., 16 electrodes) to establish a baseline performance [69].
- Step 2: Transition to a Minimal Montage
- Switch to a reduced, targeted montage (e.g., 6 electrodes over the occipital-parietal region: Pz, O1, Oz, O2, PO7, PO8) without retraining the classification model initially [69].
- Step 3: Retrain and Re-evaluate
- Expect a performance decline after electrode reduction. Retrain your classification algorithm (e.g., Canonical Correlation Analysis - CCA) on the new data from the reduced montage. This can restore performance to near-baseline levels for many users [69].
- Step 4: Acknowledge Individual Variability
- Be aware that minimal montages may not work reliably for all users due to individual differences in neural response characteristics. A one-size-fits-all approach may not be feasible [69].
Frequently Asked Questions (FAQs)
FAQ 1: What is the most critical step in my EEG pre-processing pipeline that I should focus on?
Research indicates that data segmentation and the choice of re-referencing method have the most significant impact on your final signal quality. While many researchers focus on artefact removal algorithms like ICA, the effect of different ICA algorithms (SOBI vs. Extended Infomax) may be relatively small compared to segmentation and re-referencing [70].
FAQ 2: For TMS-EEG studies, which synchronization paradigm offers the best performance?
A hardware-based approach (Paradigm 3), where TTL pulses generated by the TMS device are directly routed to the EEG amplifier's auxiliary input, provides superior performance. It shows narrower latency distributions, lower time interval error, and higher precision compared to software-based methods [67]. However, this method requires a high-sample-rate EEG amplifier and limits the integration of additional devices [67].
FAQ 3: Can I use a standard, population-optimized electrode montage instead of an individualized one for non-invasive brain stimulation?
Yes, for techniques like transcranial Temporal Interference Stimulation (tTIS), population-optimized montages can approximate individualized optimization. Studies show that montages optimized using group-level electric field analysis achieve comparable focality and intensity to patient-specific MRI-based optimization, with a difference of up to ~17%. This removes the dependency on costly MRI, enhancing accessibility. The accuracy of this proxy depends on population size (ideally >40 individuals) and age match [5].
FAQ 4: My research involves cerebellar tDCS for pain modulation. How can I ensure I am stimulating the target accurately?
Optimizing your electrode montage using current flow modelling software is essential. Systematic comparisons of different montages using simulation tools (e.g., Soterix Medical) can identify the configuration that maximizes electric field strength in the target cerebellar lobe while minimizing unwanted stimulation of other brain regions. For conventional tDCS, a left deltoid anode with a right cerebellar sponge cathode (3cm lateral to inion) is promising. For focal stimulation, a 4x1 high-definition tDCS montage is recommended [71].
Comparative Data Tables
| Paradigm | Description | Key Advantage | Key Limitation | Best For |
|---|---|---|---|---|
| Paradigm 1 (Software) | Simultaneous software pulses to EEG & TMS via LSL. | Allows for additional device integration and inter-pulse control. | Higher latency and timing variability. | Flexible, multi-device setups where top precision is not critical. |
| Paradigm 2 (Software) | Sequential pulse to TMS, then EEG via LSL. | Allows for additional device integration. | Greater variability and lower precision than hardware. | Scenarios requiring some software-mediated control. |
| Paradigm 3 (Hardware) | Direct routing of TMS pulse to EEG amplifier. | Superior performance: Lowest latency, highest precision/accuracy. | Requires high EEG sample rate; limits additional device integration. | Experiments demanding the highest possible timing accuracy. |
| Electrode Configuration | Key Finding | Recommended Action | Practical Implication |
|---|---|---|---|
| 16-Electrode (Baseline) | Establishes baseline performance with high spatial information. | Use as a reference for evaluating reduced setups. | High setup time and cost, lower user comfort. |
| 6-Electrode (No Retraining) | Performance declines on average. | Use for initial, quick assessment of signal viability. | Highlights the loss of discriminative spatial information. |
| 6-Electrode (With Retraining) | Retraining classifier restores near-baseline mean ITR and accuracy. | Essential step for deploying a minimal setup. | Enables a more practical, user-friendly BCI system without major performance loss. |
Experimental Workflow Visualizations
EEG Pre-processing Pipeline
TMS-EEG Synchronization Methods
The Scientist's Toolkit: Essential Research Reagents & Materials
| Item | Function | Application Note |
|---|---|---|
| Lab Streaming Layer (LSL) | A software framework for unified collection of measurement time series in research experiments. | Enables network-based synchronization of multiple devices (EEG, TMS, eye tracker) with microsecond precision [67]. |
| Photodiode | A sensor that detects changes in light intensity. | Placed on a stimulus screen and connected to the EEG amplifier to record the exact onset of visual stimuli, bypassing computer processing delays [66]. |
| TTL Pulse Generator | A device that produces Transistor-Transistor Logic pulses, a standard digital signal. | Used for hardware synchronization between devices (e.g., TMS and EEG) via direct BNC cable connections, minimizing latency [67] [66]. |
| RELAX-Jr Pipeline | A fully automated, open-source EEG pre-processing pipeline. | Specifically adapted for cleaning EEG data from children, who typically have more pronounced movement and muscle artefacts [68]. |
| Current Flow Modelling Software | Software that simulates electric field distributions in the brain. | Critical for optimizing electrode montages in non-invasive brain stimulation (e.g., tDCS, tTIS) to ensure target engagement and avoid off-target effects [5] [71]. |
Measuring Success: Performance Validation and Comparative Analysis
FAQs: Core Metric Definitions and Interpretation
FAQ 1: What do sensitivity and specificity tell us in the context of EEG montage optimization?
Sensitivity and specificity are fundamental metrics for evaluating the performance of a diagnostic test, such as using an optimized EEG montage to classify sleep states or neurological conditions [72].
- Sensitivity is the probability that the test will correctly classify a positive case. In an EEG study, this is the ability to correctly identify the presence of a specific sleep state (e.g., Active Sleep) when it is truly present. It is calculated as the number of true positives divided by the sum of true positives and false negatives [72].
- Specificity is the probability that the test will correctly classify a negative case. For EEG, this is the ability to correctly rule out a specific sleep state when it is truly absent. It is calculated as the number of true negatives divided by the sum of true negatives and false positives [72].
These two metrics are independent of disease prevalence and provide a clear picture of a test's inherent accuracy [72].
FAQ 2: How is the Area Under the Curve (AUC) interpreted for an EEG-based classifier?
The Area Under the Receiver Operating Characteristic (ROC) Curve (AUC) is a single, summary measure of a test's ability to discriminate between two states (e.g., diseased/normal, or between sleep stages) [72] [73].
- AUC Value Interpretation: The AUC value ranges from 0.5 to 1.0 [73]. The following table provides a standard interpretation guide:
| AUC Value | Interpretation Suggestion | Clinical Usability |
|---|---|---|
| 0.9 ≤ AUC | Excellent | High |
| 0.8 ≤ AUC < 0.9 | Considerable | Clinically useful |
| 0.7 ≤ AUC < 0.8 | Fair | Limited clinical utility |
| 0.6 ≤ AUC < 0.7 | Poor | Limited clinical utility |
| 0.5 ≤ AUC < 0.6 | Fail | No better than chance |
- Clinical Context: For a novel EEG montage and classifier, an AUC value above 0.80 is generally considered the threshold for clinical utility [73]. For instance, a study on neonatal sleep state classification using a single EEG channel (C3) reported an accuracy of 80.75%, which, while a different metric, suggests a performance level that would likely correspond to a clinically useful AUC value [3] [4].
FAQ 3: How do I find the optimal cutoff value for a continuous diagnostic test result?
When your EEG feature (e.g., power in a specific frequency band) yields a continuous numerical result, you must select a cutoff value to classify outcomes as positive or negative. The ROC curve is the primary tool for this [73].
Youden Index: A common method to identify the optimal cutoff is the Youden Index (J), which maximizes the overall effectiveness of a test. It is calculated as: J = Sensitivity + Specificity - 1 [73]. The point on the ROC curve that maximizes this value represents the optimal threshold, balancing sensitivity and specificity.
Clinical Considerations: The optimal cutoff may also be chosen based on clinical context. If missing a positive case (e.g., a seizure) is far more costly than a false alarm, you might choose a cutoff that favors higher sensitivity, even if it lowers specificity [72].
Troubleshooting Guide: Addressing Common Experimental Issues
Issue: My classifier has high accuracy but low AUC. What is wrong?
Diagnosis: This discrepancy often indicates that the chosen performance metric is misleading, likely due to a significant class imbalance in your dataset. Accuracy can be artificially inflated if one class dominates the dataset. The AUC provides a more robust picture of the model's true discriminative ability across all thresholds [73].
Solution:
- Verify Class Balance: Check the distribution of your labeled sleep states or conditions. A highly imbalanced dataset is common in real-world physiological data.
- Apply Re-sampling Techniques: Use methods like the Synthetic Minority Over-sampling Technique (SMOTE) to artificially balance the classes in your training data. This technique was successfully employed in neonatal sleep staging research to address class imbalance before model training [3] [4].
- Report Comprehensive Metrics: Always report sensitivity, specificity, AUC, and precision alongside accuracy to give a complete performance profile [73].
Diagnosis: Inconsistent signals can stem from hardware problems, software configuration errors, or participant-specific factors [6].
Solution: Follow a systematic troubleshooting protocol to isolate the cause.
This workflow, adapted from established EEG troubleshooting guidelines [6], helps rule out potential issues step-by-step. For participant-specific issues, the course of action may depend on your study's priorities—proceeding may be acceptable for secondary outcome measures, but canceling and rescheduling is advisable if clean EEG is a primary outcome [6].
Protocol: Methodology for Validating an Optimized EEG Montage
The following protocol is synthesized from recent research on EEG electrode setup optimization [3] [4].
- Data Acquisition: Collect EEG data from a sufficiently large participant cohort (e.g., 64 neonates) using a high-density montage (e.g., 10-20 system) to serve as the ground truth.
- Feature Extraction: From each channel or channel subset, extract a comprehensive set of linear and non-linear features in time and frequency domains. Recent studies have utilized up to 94 features, including novel non-linear measures like Detrended Fluctuation Analysis (DFA), Lyapunov exponent, and Multiscale Fluctuation Entropy [3] [4].
- Address Class Imbalance: Apply the SMOTE technique to the training dataset to create a balanced set of sleep state classes [3] [4].
- Feature Selection: Use Principal Component Analysis (PCA) to reduce dimensionality and prioritize the most significant features [3] [4].
- Model Training & Validation: Train a classifier (e.g., Long Short-Term Memory - LSTM network) and validate its performance using stratified cross-validation.
- Performance Quantification: Evaluate the classifier for various electrode montages (single-channel, hemispheric, etc.) using sensitivity, specificity, accuracy, kappa, and AUC.
Quantitative Performance of Different EEG Montages in Neonatal Sleep Staging
The table below summarizes quantitative results from a study that optimized EEG montages for classifying five neonatal sleep states, demonstrating the trade-offs between montage complexity and performance [3] [4].
| Electrode Montage | Accuracy (%) | Kappa Value | Key Implication for Setup Efficiency |
|---|---|---|---|
| Single Channel (C3) | 80.75 ± 0.82 | 0.76 | Optimal single-channel location; significantly reduces setup time and complexity. |
| Four Left-Side Electrodes | 82.71 ± 0.88 | 0.78 | Slightly superior to right-side; allows for asymmetric, focused montages. |
| Four Right-Side Electrodes | 81.14 ± 0.77 | 0.76 | Good performance, but slightly lower than left-side counterpart. |
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in EEG Montage Research |
|---|---|
| Long Short-Term Memory (LSTM) Network | A type of recurrent neural network ideal for classifying sequential time-series data like EEG sleep stages [3] [4]. |
| SMOTE | A synthetic oversampling technique used to address class imbalance in the dataset, improving model performance on minority classes [3] [4]. |
| Principal Component Analysis (PCA) | A dimensionality reduction technique that identifies the most significant features from a large set, simplifying the model and reducing computation load [3] [4]. |
| Detrended Fluctuation Analysis (DFA) | A novel non-linear feature that quantifies long-range power-law correlations in non-stationary signals like EEG, capturing complexity in brain dynamics [3] [4]. |
| ROC Curve Analysis | The standard method for visualizing the trade-off between sensitivity and specificity and for calculating the AUC, a key metric for diagnostic performance [72] [73]. |
Diagram: Relationship Between Metrics and Montage Optimization
Frequently Asked Questions
Q1: What is the core trade-off between using a reduced montage versus a high-density montage? The primary trade-off is between practical efficiency and diagnostic accuracy. Reduced montages (fewer electrodes) significantly decrease setup time, making EEG more feasible in time-sensitive or resource-limited settings like intensive care units [74] [33]. However, this often comes at the cost of reduced sensitivity, meaning some seizure activity or precise localization details may be missed compared to high-density EEG (HD-EEG) [75] [74].
Q2: For which applications is a reduced electrode montage sufficient? Reduced montages can be sufficient for applications where the primary goal is detecting generalized brain activity or for use as a screening tool [74] [33]. One study on pediatric point-of-care testing found that two-channel EEGs with either frontotemporal or centroparietal placement showed similar sensitivities (around 70-73%) for seizure detection, making them viable for emergency bedside testing [76]. They are also used for monitoring the level of encephalopathy [74].
Q3: When is a high-density montage unequivocally necessary? HD-EEG is crucial when the clinical or research question demands precise localization of brain activity. This is particularly true for:
- Presurgical evaluation for epilepsy: HD-EEG provides superior localization of the epileptogenic zone, which is critical for planning surgery [75] [77] [78].
- Electrical Source Imaging (ESI): Accurate source reconstruction of interictal epileptiform discharges (IEDs) or seizure onsets requires the high spatial sampling of HD-EEG [75] [77] [78].
- Analyzing activity from brain regions with poor coverage in standard montages: HD-EEG's "whole-head" coverage is better at capturing activity from inferior and medial brain surfaces, such as the basal frontal or inferior occipital regions [75].
Q4: Is there a middle-ground solution that balances setup time and accuracy? Yes, recent research explores a "targeted density" montage. This approach uses a standard low-density setup (e.g., 25 electrodes) but adds a cluster of 8-11 extra electrodes around the area of interest (e.g., the region showing the highest amplitude abnormalities on a prior EEG) [77]. Studies have shown that ESI solutions from this targeted montage show high concordance with those from full HD-EEG, offering a promising compromise [77].
Q5: How does electrode reduction impact functional connectivity analysis? Reconstructing functional connectivity from low-density EEG is challenging. Reducing the number of electrodes leads to less reliable reconstructions of coherent sources and their coupling strength [79]. While advanced source reconstruction methods like beamformers can improve results from low-density data, high-density montages remain the gold standard for reliable functional connectivity analysis [79].
Troubleshooting Guides
Problem: Missed Seizures or Poor Localization with Reduced Montage
Potential Causes and Solutions:
- Cause 1: Inherent Low Spatial Sampling. The seizure focus or brain activity might be located in a region not adequately covered by the sparse electrode array.
- Cause 2: Focal Activity Masquerading as Generalized. Activity originating from deep or midline structures can appear generalized on a low-density montage.
- Solution: As demonstrated in Case 1 from the research, HD-EEG can lateralize and localize these falsely generalized discharges, which is critical for guiding appropriate treatment [75].
Problem: High-Density EEG is Too Time-Consuming for Clinical Workflow
Potential Causes and Solutions:
- Cause: The setup of a full HD-EEG (64+ electrodes) is resource-intensive.
- Solution 1: Implement a targeted density montage. If a prior standard EEG suggests a potential focus, use the targeted approach by adding a dense cluster of electrodes over that region. This can provide HD-EEG level accuracy for ESI with only 33-36 total electrodes, drastically reducing setup time [77].
- Solution 2: Use a validated, smaller HD-EEG array. Some studies suggest that a well-designed montage with around 64 electrodes can offer a good balance, as benefits may plateau after a certain number of channels [75].
Data Comparison Tables
Table 1: Quantitative Comparison of Seizure Detection Performance
| Metric | Full Montage (21 Electrodes) | Reduced Montage (8 Electrodes) | Notes / Source |
|---|---|---|---|
| Overall Sensitivity | 0.76 | 0.65 | In a pediatric EMU study; p=0.031 [74] [33] |
| Overall Specificity | 0.96 | 0.97 | Difference was not statistically significant [74] [33] |
| Frontal Lobe Seizures | 73% detected (32/44) | 55% detected (24/44) | 27% were missed with the reduced montage [33] |
| Temporal Lobe Seizures | 70% detected (14/20) | 50% detected (10/20) | 30% were missed with the reduced montage [33] |
| Parietal Lobe Seizures | 29% detected (2/7) | 29% detected (2/7) | 71% were missed with the reduced montage [33] |
Table 2: Comparison of EEG Montage Types for Source Localization
| Montage Type | Typical Electrode Count | Key Advantages | Key Limitations | Best Suited For |
|---|---|---|---|---|
| Reduced Montage | 8 - 25 | Fast setup, high availability, good for generalized patterns [74] [76] | Low sensitivity for focal seizures, poor localization accuracy [74] [33] | ICU screening, emergent bedside testing, brain death confirmation [74] [76] |
| High-Density (HD) Montage | 64 - 256+ | Excellent localization accuracy, superior for ESI, whole-head coverage [75] [77] | Time-consuming setup, resource-intensive, requires specialized expertise [75] [77] | Presurgical epilepsy evaluation, advanced research (e.g., functional connectivity) [75] [79] |
| Targeted Density Montage | ~33 - 36 | High concordance with HD-EEG for ESI, faster setup than full HD-EEG [77] | Requires prior knowledge of potential focus (e.g., from a previous EEG) [77] | Focal epilepsy when a suspected region is known, optimizing clinical workflow [77] |
Experimental Protocols
Protocol 1: Validating a Targeted Density Montage for ESI
This protocol is based on the study by Jegou et al. (2023) [77].
- Objective: To compare the accuracy of Electrical Source Imaging (ESI) from a targeted density montage against the gold standard of full high-density EEG.
- Patient Population: Patients with drug-resistant focal epilepsy undergoing presurgical evaluation.
- Methodology:
- HD-EEG Recording: Acquire EEG data using a full high-density montage (e.g., 83 electrodes).
- IED Identification: Identify and mark interictal epileptiform discharges (IEDs) on the HD-EEG recording.
- Create Targeted Montage:
- From the full 83-electrode set, select the 25 electrodes of a standard international 10-10 montage.
- Identify the electrode showing the highest amplitude spike on the referential montage.
- Add a cluster of 8-11 electrodes around this "hotspot" electrode. The total electrode count for the targeted montage is 33-36.
- Source Imaging: Perform ESI separately for the full HD-EEG data and the data from the targeted montage subset.
- Comparison: Compare the ESI solutions using the distance between peak vertices, sublobar concordance, and qualitative similarity scores by expert review.
- Key Finding: The median distance between the peak vertices of the two montages was 13.2 mm, with sublobar concordance in 93% of foci, demonstrating that the targeted montage can yield highly similar results to full HD-EEG [77].
Protocol 2: Assessing Seizure Detection Sensitivity with Reduced Montages
This protocol is based on the study by Różycki et al. (2022) [74] [33].
- Objective: To quantify the impact of reducing the EEG montage from 21 to 8 electrodes on the sensitivity of seizure pattern detection.
- Study Design: Retrospective analysis of EEGs from a pediatric Epilepsy Monitoring Unit (EMU).
- Methodology:
- Data Selection: Select 95 seizure sequences and 95 seizure-free control sequences from archived EMU recordings.
- Montage Creation: Convert each original sequence into two versions: one with the full 21-electrode montage and one with a reduced 8-electrode montage (FP1, FP2, C3, C4, T7, T8, O1, O2).
- Blinded Review: Two board-certified epileptologists, blinded to the original EMU findings and patient details, review the EEG sequences. Each reviewer assesses both full and reduced montage files from a given seizure in a crossed-over design to avoid bias.
- Statistical Analysis: Calculate the sensitivity and specificity for both montages using the original EMU reports as the gold standard. Compare results using the McNemar test. Analyze missed seizures by brain lobe.
- Key Finding: Sensitivity dropped significantly from 76% with the full montage to 65% with the reduced montage, with the highest rates of missed seizures in the parietal (71%) and central (43%) lobes [74] [33].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for EEG Montage Research
| Item | Function in Research | Example from Literature |
|---|---|---|
| High-Density EEG System | Provides the raw data for comparison and validation of reduced montages. Systems with 64 to 256 channels are typical. | 128-channel ANT-neuro waveguard cap with a Natus amplifier [75]; 122-channel Electrical Geodesics, Inc. system [75]. |
| 3D Electrode Digitizer | Precisely records the 3D spatial location of each EEG electrode on the scalp. Critical for accurate co-registration with MRI and reliable Electrical Source Imaging. | Fastrak digitizer (Polhemus Inc.) [75]. |
| Individual MRI Data | Provides an anatomically accurate head model for constructing the forward model needed for source imaging (ESI). Improves localization accuracy. | T1-weighted multi-echo MPRAGE sequences processed with Freesurfer [75]. |
| Source Imaging Software | Computes the underlying brain sources of the scalp EEG signals. | MNE-C software package [75]; Geosource 2.0 [75]; LAURA algorithm [78]. |
| Realistic Head Model | A computational model (e.g., a 3-layer Boundary Element Model) that simulates how electrical currents propagate through the brain, skull, and scalp. Essential for precise ESI. | BEM model constructed from Freesurfer [75]. |
Workflow and Decision Diagrams
Diagram: Decision Workflow for Montage Selection
Frequently Asked Questions (FAQs)
Q1: What is the core difference between offline analysis and prospective online testing in the context of EEG montage validation? Offline analysis involves processing pre-recorded EEG data to simulate and compare the performance of different electrode montages. In contrast, prospective online testing validates a selected montage in real-time during a live experiment, where the system uses the reduced montage to provide immediate feedback or control an interface [69]. Offline analysis is crucial for initial screening and hypothesis generation, while online testing confirms the setup's practical viability and robustness.
Q2: When reducing my EEG electrode count, why does performance sometimes drop significantly in online tests, even when offline results were promising? A significant drop in online performance often stems from the loss of spatial information and increased sensitivity to noise or artifacts that were not fully accounted for in the offline model [69]. Individual differences in neural response characteristics and head anatomy mean that a generic reduced montage may not work equally well for all users. Retraining the classification model on data from the new, reduced montage can often restore performance to near-baseline levels [69].
Q3: How can I determine the minimum number of electrodes needed for my specific EEG experiment? The minimum number is task-dependent and involves a trade-off between performance and practicality. A systematic approach is recommended:
- Begin with a high-density recording as a gold standard reference [77].
- Perform offline analysis to simulate the performance of various reduced montages.
- For clinical applications like epilepsy focus localization, a targeted approach using 33-36 electrodes over the region of interest can provide high concordance with high-density setups [77].
- For some BCI paradigms, occipital-focused setups with as few as 6 electrodes may be feasible, but this requires careful validation [69].
Q4: What are the key advantages of moving to a simpler, optimal electrode montage? Optimizing your electrode montage directly supports the goal of reducing EEG setup time and enhances practicality. Key advantages include:
- Reduced Setup Time: Fewer electrodes to apply and prepare [69] [77].
- Improved User Comfort: Less obtrusive setups are better for long-term monitoring [69] [80].
- Lower Hardware Costs: Fewer channels may enable the use of more cost-effective amplifier systems [69] [55].
- Increased Portability: Streamlined setups are more suitable for real-world, mobile applications [55] [81].
Troubleshooting Guides
Issue 1: Poor Performance After Switching from a High-Density to a Reduced Electrode Montage
Symptoms:
- Classification accuracy or information transfer rate (ITR) is significantly lower with the new montage compared to offline predictions.
- The real-time decoder fails to function reliably.
| Possible Cause | Diagnostic Steps | Recommended Solution |
|---|---|---|
| Loss of Critical Spatial Information | Review offline analysis to see if performance was already borderline. Check if the removed electrodes were in high-amplitude or functionally critical regions. | Consider a slightly larger montage or a targeted density approach that adds a few electrodes around the region of interest [77]. |
| Suboptimal Electrode Locations | Compare the performance of different reduced configurations (e.g., occipital-only vs. parietal-occipital) from your offline analysis. | Select a montage that is specifically optimized for your paradigm (e.g., occipital sites Oz, O1, O2 for visual evoked potentials) [69]. |
| Model Mismatch | Confirm whether the classification model was trained on data from the high-density montage or the new reduced montage. | Retrain your decoding model using data collected from the new, reduced electrode setup. This adapts the model to the specific spatial characteristics of the new montage [69]. |
| Increased Noise Sensitivity | Inspect the raw signals from the reduced montage for increased noise or artifacts. | Implement adaptive preprocessing techniques, such as an Adaptive Channel Mixing Layer (ACML), which can dynamically adjust for electrode misalignments and noise [82]. |
Issue 2: Handling Variable Electrode Placements Across Sessions or Subjects
Symptoms:
- High performance variance between experimental sessions or across different participants.
- Inconsistent signal quality when the electrode cap is positioned slightly differently.
Solution: Implement adaptive preprocessing algorithms designed to compensate for placement variability. For example, the Adaptive Channel Mixing Layer (ACML) is a plug-and-play module that can be added to your processing pipeline. It uses a learnable transformation matrix to dynamically adjust the weights of input signals based on inter-channel correlations, effectively making your system more robust to electrode shifts [82].
Issue 3: Validating a Novel, Minimal Montage for Clinical Use
Symptoms:
- You have developed a minimal montage for a clinical application (e.g., epilepsy monitoring) and need to prove its efficacy against the gold standard.
Solution: Follow a rigorous validation framework:
- Acquire Gold-Standard Data: Record simultaneous HD-EEG (e.g., 80+ electrodes) from patients [77].
- Create a Targeted Montage: Select a subset of electrodes (e.g., 33-36) that includes standard locations and adds a higher density over the suspected focus area, identified by the highest amplitude interictal epileptiform discharges [77].
- Perform Offline Comparison: Calculate the clinical metric (e.g., Electrical Source Imaging solution) for both the full HD-EEG and the targeted montage.
- Quantify Concordance: Evaluate the distance between the peak source vertices and the sublobar concordance rate. A high concordance (e.g., median distance of ~13mm and >90% sublobar agreement) validates the minimal montage for clinical use [77].
Experimental Protocols for Validation
Protocol 1: A Direct Comparison of Montage Performance
This protocol is ideal for BCI applications, directly testing how electrode reduction affects performance metrics like accuracy and ITR.
1. Objective: To compare the performance of a high-density electrode montage with a reduced montage in an online BCI task.
2. Materials:
- EEG Acquisition System: An amplifier capable of recording from all desired channels (e.g., OpenBCI Cyton/Daisy for cost-effective research [55]).
- Electrode Caps: Standard caps for both high-density (e.g., 16 electrodes) and reduced (e.g., 6 electrodes) configurations.
- Stimulus Presentation Software: To run the BCI paradigm (e.g., cVEP or SSVEP speller).
- Classification Pipeline: Real-time decoding software (e.g., based on Canonical Correlation Analysis for cVEP).
3. Methodology:
- Participants: Recruit a cohort of participants (e.g., n=38) [69].
- Experimental Conditions:
- Condition A (Baseline): Perform the BCI task using the full high-density montage (e.g., 16 electrodes).
- Condition B (Reduced, No Retraining): Switch to the reduced montage (e.g., 6 electrodes) but use the classification model trained on the high-density data.
- Condition C (Reduced, With Retraining): Use the reduced montage with a model retrained on data from that specific montage.
- Data Analysis: For each condition, calculate key performance metrics: Classification Accuracy and Information Transfer Rate (ITR). Compare the averages and variances across conditions.
4. Expected Outcomes:
- You will likely observe a performance decline in Condition B due to lost spatial information.
- Performance in Condition C should recover significantly, potentially reaching near-baseline levels, demonstrating the importance of model retraining [69].
The workflow for this direct comparison is outlined below.
Protocol 2: Validating a Targeted Montage for Clinical Source Imaging
This protocol is designed for clinical applications where the goal is precise localization of neural sources, such as in epilepsy.
1. Objective: To validate that a targeted, low-density EEG montage provides equivalent Electrical Source Imaging (ESI) results to a traditional high-density montage.
2. Materials:
- HD-EEG System: A clinical-grade system with 80+ electrodes [77].
- MRI: Patient's individual structural MRI for creating an accurate head model.
- ESI Software: Software for computing source localization from scalp potentials.
3. Methodology:
- Data Collection: Record HD-EEG (e.g., 83 electrodes) from patients undergoing presurgical evaluation. Identify and mark interictal epileptiform discharges (IEDs) [77].
- Create Targeted Montage:
- Select the standard 25 electrodes from an international 10-20/10-10 system.
- Identify the electrode showing the highest amplitude IED.
- Add 8-11 additional electrodes around this "hot spot" to create a targeted montage of 33-36 electrodes [77].
- Offline Analysis:
- Compute the ESI solution for a representative set of IEDs using both the full HD-EEG data and the subset of data from the targeted montage.
- Validation Metrics:
- Distance between Peak Vertices: Calculate the Euclidean distance (in mm) between the source localization peaks from the two montages.
- Sublobar Concordance: Determine if the solutions localize to the same sublobar region.
- Qualitative Similarity: An expert rater can score the similarity of the source maps on a scale (e.g., 1-5) [77].
4. Expected Outcomes: A successful validation is achieved with a median distance between peaks of less than 15mm, a sublobar concordance rate of over 90%, and a high qualitative similarity score, demonstrating that the targeted montage is clinically viable [77].
The Scientist's Toolkit: Key Research Reagents & Materials
| Item / Solution | Function in Research | Application Context |
|---|---|---|
| High-Density EEG System (e.g., 128-256 channels) | Serves as the gold standard for recording. Provides the ground-truth data against which all reduced montages are validated. | Essential for initial data collection in both Protocol 1 and 2 to ensure no spatial information is lost at the recording stage [77]. |
| Targeted Montage (33-36 electrodes) | A clinically-oriented reduced setup that maintains high density over the region of interest while reducing global electrode count. | Used in presurgical epilepsy evaluation to achieve ESI results concordant with HD-EEG, significantly reducing setup time and resource demand [77]. |
| Adaptive Channel Mixing Layer (ACML) | A software-based preprocessing module that dynamically adjusts input signal weights to compensate for electrode shift and noise. | Improves the robustness of motor imagery BCIs against variability in electrode placement across sessions or subjects [82]. |
| OpenBCI / Cost-Effective Setup | Provides a accessible, portable, and validated hardware platform for EEG data acquisition and real-time processing. | Ideal for prototyping BCI paradigms and conducting research on electrode reduction without the need for prohibitively expensive clinical systems [55] [35]. |
| Dry & In-Ear EEG Electrodes | Electrode technologies that forego conductive gel, prioritizing setup speed, user comfort, and long-term wearability. | Represents the next frontier in portable EEG, enabling research into continuous monitoring in real-world environments outside the lab [80] [81]. |
This technical support center provides troubleshooting guides and FAQs to assist researchers in addressing common experimental challenges, framed within the broader objective of reducing EEG setup complexity through optimal electrode montage research.
Frequently Asked Questions (FAQs)
Q1: How many electrodes can I safely remove from a standard 64-channel speech imagery setup without significantly hurting performance? Recent systematic evaluation indicates that the original 64 channels can typically be reduced by 50% without a significant loss in classification accuracy for imagined speech tasks [2]. The optimal subset is often highly subject-specific, and relevant areas are distributed across the cortex, not limited just to the left-hemisphere language areas [2].
Q2: For neonatal sleep staging, which single EEG channel provides the best classification performance? Research on neonatal sleep state classification has found that the C3 channel achieves an accuracy of 80.75% ± 0.82% (kappa = 0.76) when used with an LSTM classifier and a comprehensive set of linear and non-linear features, making it a strong candidate for single-channel setups [3] [4].
Q3: My imagined speech classification accuracy is low. What is one data-related strategy I can use to improve it? Consider incorporating data from overt speech (where participants actually pronounce words) during model training. One study found that combining overt and imagined speech data in an intra-subject scenario led to accuracy improvements of 3% to 5.17% in several binary word-pair classifications, making it a feasible strategy to boost performance, especially with limited data [83].
Q4: Is there a consistent, pre-defined set of optimal electrodes for all subjects in a speech imagery study? No. Research has shown that a consistent set of optimal electrode positions across different datasets and subjects does not exist [2]. The relevant electrode configurations are highly subject-specific, indicating that electrode montages should be individually tailored for best results [2].
Troubleshooting Guides
Issue: Poor Classification Accuracy in Speech Imagery BCI
Problem: Your model for classifying imagined words (e.g., "stop," "hello") is achieving low accuracy, making the BCI system unreliable.
Investigation and Solution:
- Verify Electrode Count and Placement: Systematically evaluate the number of electrodes you are using. Begin with a full 64-channel setup to establish a baseline performance, then use a wrapper-based electrode reduction algorithm to identify non-essential channels. Remember that you may be able to reduce channels by up to 50%, but the optimal set is likely subject-specific [2].
- Check Your Training Data Strategy:
- If you have a small dataset from the target user, consider augmenting the training set with overt speech data from the same user. The shared characteristics between overt and imagined speech can enhance the model's ability to classify imagined speech alone [83].
- Ensure you are using an analysis window that captures the most relevant brain activity. Research suggests examining temporal windows where Event-Related Potentials (ERPs) for overt and imagined speech show the greatest similarity [83].
- Evaluate Your Feature Set and Model: For complex spatiotemporal patterns in EEG, consider advanced deep learning architectures. A hybrid model combining a 3D-CNN and an RNN has been shown to effectively capture both spatial and long-term temporal features from sequences of topographic maps, achieving an average accuracy of 77.8% for imagined word classification [84].
Recommended Experimental Protocol for Electrode Reduction:
- Preprocessing: Apply bandpass filtering (e.g., 0.5-40 Hz) and artifact removal (e.g., using ICA) to clean the raw EEG data [85] [2].
- Feature Extraction: Extract features from the preprocessed data. Common methods include power spectral densities, common spatial patterns, or deep learning features [2].
- Classification & Reduction Loop:
- Train your chosen classifier (e.g., EEGNet, SVM, Random Forest) and evaluate its accuracy.
- Use a wrapper-based electrode reduction algorithm (e.g., backward elimination) to rank electrodes by importance.
- Iteratively remove the least important electrode and re-evaluate performance until only one channel remains.
- Analysis: Plot accuracy against the number of electrodes to identify the "elbow point" where performance begins to drop significantly, determining the optimal number for your specific application and subject [2].
Issue: Designing a Minimal-Electrode Setup for Neonatal Sleep Staging
Problem: You need to classify neonatal sleep states (Active Sleep, Quiet Sleep) with minimal electrodes to reduce setup time, complexity, and risk of skin irritation for the infant.
Investigation and Solution:
- Start with a Single Channel: Evidence suggests that a single channel, particularly C3, can achieve high accuracy (~80%) for five-state sleep classification in neonates [3] [4]. This should be your baseline for a minimal setup.
- Consider a Small Hemispheric Montage: If performance from a single channel is insufficient, try a small cluster of electrodes. Studies show that a combination of four left-side electrodes can achieve higher accuracy (82.71% ± 0.88%) than four right-side electrodes (81.14% ± 0.77%) [3] [4].
- Implement a Robust Feature Extraction Pipeline: Do not rely on a few simple features. Extract a large set of linear and non-linear features in both time and frequency domains (e.g., including Detrended Fluctuation Analysis, Lyapunov exponent, and Multiscale Fluctuation Entropy) [3] [4].
- Address Class Imbalance: Use techniques like the Synthetic Minority Over-sampling Technique (SMOTE) to balance the distribution of sleep states in your dataset, which improves model generalization [3] [4].
Workflow Diagram: Optimizing EEG Montage for Domain Applications
The following diagram illustrates the general decision workflow for selecting and validating an optimal electrode montage for different BCI applications.
Table 1: Electrode Reduction Findings Across BCI Domains
| Application Domain | Optimal Number of Electrodes | Key Electrode Locations | Reported Performance | Citation |
|---|---|---|---|---|
| Speech Imagery | ~32 (50% reduction from 64) | Distributed across cortex, highly subject-specific | No significant performance loss after 50% reduction | [2] |
| Neonatal Sleep Staging | 1 (Single-channel) | C3 | 80.75% ± 0.82% Accuracy | [3] [4] |
| Neonatal Sleep Staging | 4 (Multi-channel) | Left-hemisphere cluster | 82.71% ± 0.88% Accuracy | [3] [4] |
Table 2: Performance of Data Augmentation Strategies in Speech Imagery
| Strategy | Classification Scenario | Performance Impact | Notes | Citation |
|---|---|---|---|---|
| Adding Overt Speech Data | Intra-subject, Binary word-pairs | +3% to +5.17% accuracy in 4/10 pairs | Increased number of participants surpassing 70% accuracy threshold | [83] |
| Using Overt Speech Alone | Intra-subject, Binary word-pairs | Up to 95% accuracy (highest single result) | May not generalize to all subjects or word pairs | [83] |
The Scientist's Toolkit: Essential Research Reagents
The table below lists key computational tools and methodologies essential for experiments in electrode montage optimization.
| Tool / Technique | Category | Function in Research | Example Use Case |
|---|---|---|---|
| Wrapper Method (e.g., Backward Elimination) | Electrode Reduction Algorithm | Systematically evaluates channel subsets based on classifier performance to find an optimal set. | Identifying the minimal electrode set for a subject-specific Speech Imagery BCI [2]. |
| EEGNet | Deep Learning Model | A compact convolutional neural network designed specifically for EEG-based BCIs. | Classifying imagined speech from EEG signals; can be used within electrode reduction pipelines [83]. |
| Long Short-Term Memory (LSTM) | Deep Learning Model | A type of RNN effective at modeling temporal sequences and long-range dependencies. | Classifying sequential EEG data, such as for neonatal sleep stage classification [3] [4]. |
| Hybrid 3D-CNN + RNN | Deep Learning Model | Captures rich spatiotemporal features from EEG data represented as a sequence of images. | Classifying imagined words from a sequence of EEG topographic maps [84]. |
| Detrended Fluctuation Analysis (DFA) | Feature Extraction | A non-linear method quantifying long-range temporal correlations in a signal. | Extracting informative features from neonatal EEG for sleep stage classification [3] [4]. |
| SMOTE | Data Preprocessing | A technique to address class imbalance by generating synthetic samples of the minority class. | Balancing the number of Active Sleep and Quiet Sleep segments in a neonatal sleep dataset [3] [4]. |
Long-Term Reliability and Multi-Site Reproducibility Assessment
Troubleshooting Guides
Issue 1: High Variability in Longitudinal EEG Measurements
Problem: EEG feature values (e.g., band power) show unexpected fluctuations across repeated monthly measurements in a year-long study, making it difficult to distinguish true neural changes from normal variability. Solution:
- Action 1 → Integrate nonlinear EEG measures: Replace or supplement traditional spectral band power analysis with measures like Higuchi’s fractal dimension (HFD) or Lempel–Ziv complexity (LZC). These have demonstrated greater temporal stability at the individual level over 12 months [86].
- Action 2 → Establish individual baselines: Before the study, calculate intraclass correlation coefficients (ICCs) for your key EEG metrics from a few pilot sessions. This helps quantify the expected normal variability for each participant and provides a reference for evaluating future measurements [86].
- Action 3 → Optimize channel selection: For your specific application (e.g., mild cognitive impairment detection), use a pre-validated, minimal electrode configuration. This reduces setup time and data complexity while focusing on the most relevant brain regions [57].
Issue 2: Inconsistent Findings Across Different Research Sites
Problem: An EEG biomarker (e.g., theta power in the occipital lobe) that robustly identifies a condition at one site fails to replicate at another, despite using the same protocol. Solution:
- Action 1 → Standardize pre-processing: Implement a targeted artifact reduction method, such as the RELAX pipeline. Standardizing this step mitigates false positive effects and source localization biases that can vary between sites due to different artifact profiles [9].
- Action 2 → Use subject-specific montages: When possible, avoid a one-size-fits-all electrode montage. Research shows that optimal electrode configurations for tasks like speech imagery classification are highly subject-specific. If a fixed montage is necessary, validate it across multiple independent datasets to ensure generalizability [2].
- Action 3 → Validate across datasets: Test your analysis pipeline and electrode montage on at least three distinct datasets acquired by different research groups. This confirms the generalizability of your methodology and findings [2].
Issue 3: Suboptimal Electrode Montage Leading to Long Setup Times
Problem: The need for high-density EEG (e.g., 64 electrodes) to capture relevant neural activity makes the system cumbersome, increases setup time, and is impractical for long-term or multi-site studies. Solution:
- Action 1 → Systematically reduce channels: Employ a wrapper-function-based electrode reduction algorithm. This method systematically evaluates the performance of different electrode subsets to find the minimal set that maintains classification accuracy or effect size [2].
- Action 2 → Focus on key regions: For specific clinical questions, leverage existing research on optimized configurations. For instance, in mild cognitive impairment (MCI) detection, a configuration of just four occipital electrodes (PO3, PO4, PO7, PO8) has shown high sensitivity, drastically reducing setup complexity [57].
- Action 3 → Adopt standard positioning: Ensure all electrodes are placed using the international 10-20 system. This standardized method is crucial for ensuring consistency and comparability of data across different subjects and research sites [87].
Frequently Asked Questions (FAQs)
Q1: Which EEG metrics are the most stable for tracking individual changes over a year? Nonlinear measures, particularly Higuchi’s fractal dimension (HFD) and Lempel–Ziv complexity (LZC), have shown greater individual-level temporal stability over 12 months compared to traditional spectral band powers. While band power measures like alpha and theta show excellent reliability at the group level, they can exhibit more substantial within-subject fluctuations in some individuals [86].
Q2: Can I reliably use a reduced set of electrodes for my cognitive monitoring study? Yes, and it is often recommended for practicality and reduced setup time. Evidence indicates that the original 64 channels can often be reduced by 50% or more without significant performance loss. The optimal configuration, however, can be task- and subject-specific. For MCI detection during a working memory task, a 4-electrode occipital configuration has proven effective [57], while for speech imagery, the optimal sites are distributed across the cortex and may need to be individually tailored [2].
Q3: How can I improve the reproducibility of my EEG findings across multiple labs? Key strategies include:
- Standardized Protocols: Use a common, detailed pre-processing pipeline, such as the RELAX method for artifact removal, to minimize site-specific processing biases [9].
- Electrode Positioning: Strictly adhere to the international 10-20 system for electrode placement to ensure spatial consistency [87].
- Cross-Dataset Validation: Test your hypotheses and analysis methods on independent datasets collected by different teams to confirm generalizability [2].
Q4: What is the risk of losing critical neural signals when using a minimal electrode montage? The risk can be mitigated by a data-driven approach to electrode selection. Studies systematically reducing electrodes have found that performance does not drop significantly until a certain threshold is passed (e.g., reducing 64 channels to 32). The key is to identify the montage that retains the most discriminative information for your specific research question, which often does not require full scalp coverage [2] [57].
Q5: How does artifact handling impact the long-term reliability of EEG measures? Proper artifact handling is critical. Conventional methods like subtracting entire independent components (ICs) can remove neural signals along with artifacts, artificially inflating effect sizes and biasing results. Using targeted cleaning methods that remove only the artifact-dominated periods or frequencies from ICs protects neural data integrity, leading to more reliable and valid longitudinal comparisons [9].
Table 1: One-Year Stability of Single-Channel EEG Measures
This table summarizes the intraclass correlation coefficients (ICCs) for various EEG measures over 12 monthly recordings, indicating their reliability for longitudinal studies [86].
| EEG Measure | Frequency Band / Type | Average ICC | Stability Notes |
|---|---|---|---|
| Absolute Band Power | Theta | 0.84 - 0.93 | High reliability, slightly lower in temporal regions. |
| Absolute Band Power | Alpha | 0.86 - 0.94 | Excellent reliability across most sites. |
| Absolute Band Power | Beta | 0.79 - 0.90 | Good reliability, but slightly reduced ICCs in temporal regions. |
| Absolute Band Power | Gamma | 0.75 - 0.88 | Lower reliability in peripheral electrode sites. |
| Higuchi’s Fractal Dimension (HFD) | Nonlinear | 0.87 - 0.95 | Excellent reliability and greater temporal stability than band power. |
| Lempel–Ziv Complexity (LZC) | Nonlinear | 0.85 - 0.94 | High reliability and stability over time. |
Table 2: Performance of Optimized Electrode Configurations for MCI Detection
This table compares the diagnostic power of different electrode montages for distinguishing patients with Mild Cognitive Impairment (MCI) from healthy controls using a binary logistic regression model [57].
| Electrode Configuration | Brain Lobes Covered | Area Under Curve (AUC) | Sensitivity |
|---|---|---|---|
| OCL4 | Occipital | 0.765 | 0.962 |
| PRL3 | Prefrontal | 0.683 | 0.794 |
| PLL4 | Parietal | 0.729 | 0.873 |
| OPL8 | Occipital + Parietal | 0.830 | 0.943 |
| OPL7 | Occipital + Prefrontal | 0.788 | 0.859 |
| PPL7 | Parietal + Prefrontal | 0.769 | 0.938 |
Experimental Protocols
Protocol 1: Assessing Long-Term Stability of EEG Features
Objective: To evaluate the one-year stability of linear and nonlinear EEG measures in healthy individuals for longitudinal study design [86].
- Participants: Recruit a cohort of healthy subjects (e.g., n=9).
- EEG Recording: Schedule and conduct 12 monthly EEG recording sessions for each participant. Use a standardized resting-state protocol (e.g., 5 minutes eyes-closed).
- Data Pre-processing: Apply a standardized pre-processing pipeline (e.g., using the RELAX method [9]) to remove artifacts and ensure data quality across all sessions.
- Feature Extraction: For each session, calculate both linear (Absolute Power in Theta, Alpha, Beta, Gamma bands) and nonlinear (HFD, LZC) measures for predefined channels.
- Statistical Analysis: Compute Intraclass Correlation Coefficients (ICCs) for each feature across the 12 sessions to assess reliability. Also, analyze within-subject variability versus between-subject variability.
Protocol 2: Systematic Optimization of Electrode Montage
Objective: To identify the minimal and optimal set of electrodes for a specific BCI or diagnostic application [2] [57].
- Data Acquisition: Collect high-density EEG data (e.g., 64 channels) from a participant cohort during a specific task (e.g., working memory, speech imagery).
- Baseline Model: Extract features and train a classification/regression model using all available electrodes. Record its performance (e.g., accuracy, AUC) as a baseline.
- Electrode Reduction: Implement a wrapper-function-based reduction algorithm. This algorithm iteratively removes the least important electrode and re-evaluates model performance until only one electrode remains.
- Performance Analysis: Plot the model performance against the number of electrodes. Identify the "elbow point" where performance begins to degrade significantly.
- Validation: Validate the optimal electrode subset identified in Step 4 on a separate, held-out test dataset or, ideally, on independent datasets from other labs [2].
Methodologies and Workflows
Diagram 1: Workflow for optimizing electrode montage to reduce setup time.
Diagram 2: Targeted artifact cleaning pipeline for reproducible data.
The Scientist's Toolkit
Key Research Reagent Solutions
Table: Essential materials and tools for EEG reliability and reproducibility research.
| Item Name | Function / Application | Key Characteristic |
|---|---|---|
| RELAX EEGLAB Plugin | A standardized pre-processing pipeline for targeted artifact reduction. | Mitigates effect size inflation and source localization biases, enhancing validity [9]. |
| Dry Electrode EEG Systems | EEG recording without conductive gel or skin preparation. | Reduces setup time, improves comfort for long-term studies, and maintains signal quality [1]. |
| International 10-20 System | Standardized framework for placing EEG electrodes on the scalp. | Ensures consistency and comparability of data across subjects and research sites [87]. |
| Wrapper-Function Algorithms | Computational methods for systematically reducing the number of EEG electrodes. | Identifies the minimal electrode subset without significant performance loss, enabling compact montages [2]. |
| Nonlinear Feature Sets (HFD, LZC) | A set of metrics for quantifying signal complexity and irregularity. | Provides greater temporal stability for individual-level longitudinal tracking compared to traditional band power [86]. |
Conclusion
The strategic reduction of EEG electrode montages represents a paradigm shift in neurophysiological research, offering a viable path to dramatically reduce setup time while maintaining diagnostic and research validity. Evidence consistently demonstrates that optimized subsets of 4-10 electrodes can achieve performance comparable to high-density systems for specific applications like seizure detection, P300 spellers, and sleep staging. Future directions should focus on developing standardized, application-specific montages, advancing automated optimization algorithms, and validating these approaches across diverse clinical populations. For drug development, these efficient protocols enable more scalable biomarker acquisition in clinical trials, particularly for rare neurodevelopmental disorders where participant burden is a critical concern. The integration of wearable EEG technologies with optimized montages will further accelerate this transition, making high-quality electrophysiological assessment more accessible, practical, and integrated into real-world clinical research workflows.
References
- 1. Why Brain Wearables Are Making Traditional EEG Labs ... [https://globalrph.com/2025/10/why-brain-wearables-are-making-traditional-eeg-labs-obsolete-in-2025/]
- 2. How low can you go: evaluating electrode reduction ... [https://www.frontiersin.org/journals/neuroergonomics/articles/10.3389/fnrgo.2025.1578586/full]
- 3. EEG electrode setup optimization using feature extraction ... [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2025.1506869/full]
- 4. EEG electrode setup optimization using feature extraction ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11825521/]
- 5. Population-optimized electrode montage approximates ... [https://www.sciencedirect.com/science/article/pii/S0010482525005748]
- 6. EEG Trouble Shooting | Center for ... [https://www.centerforsleepandcognition.com/eeg-trouble-shooting]
- 7. EEG Machine Troubleshooting: Symptom Reasons ... [https://www.scribd.com/document/540019750/EEG-Troubleshooting-Pr]
- 8. What are common mistakes and general troubleshooting ... [https://www.biopac.com/knowledge-base/common-mistakesgeneral-troubleshooting/]
- 9. EEG is better when cleaning effectively targets artifacts [https://www.sciencedirect.com/science/article/abs/pii/S1388245725012301]
- 10. Troubleshooting from a Distance [https://www.integrisneuro.com/post/troubleshooting-from-a-distance]
- 11. 10–20 system (EEG) [https://en.wikipedia.org/wiki/10%E2%80%9320_system_(EEG)]
- 12. What Is the 10-20 System for EEG? - TMSi [https://www.tmsi.artinis.com/blog/the-10-20-system-for-eeg]
- 13. : Part 1 - Differential Amplifiers EEG Montages [https://www.biosourcesoftware.com/post/eeg-montages-part-1-differential-amplifiers]
- 14. Dynamic reconstruction of electroencephalogram data using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11985760/]
- 15. The Influence of Electrode Location Errors on EEG Dipole ... [https://pubmed.ncbi.nlm.nih.gov/11514261/]
- 16. The influence of electrode location errors on EEG dipole ... [https://www.sciencedirect.com/science/article/abs/pii/S1388245701005946]
- 17. TMS- Optimized Recordings with 3 mm Ultra-Flat EEG for... Electrodes [https://www.gtec.at/2025/11/14/tms-eeg-recordings-with-3-mm-electrodes/]
- 18. setup EEG using feature extraction... electrode optimization [https://research.birmingham.ac.uk/en/publications/eeg-electrode-setup-optimization-using-feature-extraction-techniq]
- 19. Analysis of Minimal Channel Electroencephalography for ... [https://www.mdpi.com/2079-9292/13/3/565]
- 20. EEG Montages and Technical Components [https://www.learningeeg.com/montages-and-technical-components]
- 21. Appendix 2. Principles of Digital EEG - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK390353/]
- 22. Adaptive EEG preprocessing to mitigate electrode shift ... [https://www.nature.com/articles/s41598-025-24466-x]
- 23. How EEG preprocessing shapes decoding performance [https://www.nature.com/articles/s42003-025-08464-3]
- 24. Group optimization methods for dose planning in tES - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12351633/]
- 25. Mastering Genetic Algorithms in ML (2025 Update): Concepts, Code & Use Cases | by Vaishnavi Yada (Amira) | Medium [https://medium.com/@vaishnaviyada/mastering-genetic-algorithms-in-ml-2025-update-concepts-code-use-cases-59a9dbef08a8]
- 26. Automated methodology for optimal selection of minimum ... [https://www.nature.com/articles/s41598-022-15252-0]
- 27. Wrapper Methods - Feature Selection [https://www.geeksforgeeks.org/machine-learning/wrapper-methods-feature-selection/]
- 28. Understanding Wrapper Methods in Machine Learning - Aris [https://arismuhandisin.medium.com/understanding-wrapper-methods-in-machine-learning-a-guide-to-feature-selection-23f71059abf8]
- 29. New improved hybrid genetic algorithm for optimizing facility layout design of reconfigurable manufacturing system | Scientific Reports [https://www.nature.com/articles/s41598-025-97526-x]
- 30. A Method for Optimizing EEG Electrode Number and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4377128/]
- 31. Benchmarking the utility of dry-electrode ... [https://www.nature.com/articles/s41598-025-18184-7]
- 32. Check Electrodes Message [https://www.eeginfo.com/knowledgebases/212/check-electrodes-message]
- 33. Effects of a reduction of the number of electrodes ... - Nature [https://www.nature.com/articles/s41598-022-08628-9]
- 34. Efficacy of a Reduced Electroencephalography Electrode ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3869310/]
- 35. Setting up for EEG [https://docs.openbci.com/GettingStarted/Biosensing-Setups/EEGSetup/]
- 36. A method for optimizing EEG electrode number and ... [https://www.sciencedirect.com/science/article/abs/pii/S1388245714005069]
- 37. Channel Selection Methods for the P300 Speller - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4106671/]
- 38. Streamlining cVEP Paradigms: Effects of a Minimized ... [https://www.mdpi.com/2076-3425/15/6/549]
- 39. P300 ERP System Utilizing Wireless Visual Stimulus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12196673/]
- 40. Using OpenBCI with OpenViBE CoAdapt P300 Speller [https://openbci.com/community/using-openbci-with-openvibe-coadapt-p300-speller/]
- 41. P300 GUI Guide [https://www.bci2000.org/mediawiki/index.php/P300_GUI_Guide]
- 42. DSI-7 (Wearable Sensing) [https://www.neurospec.com/products/dsi-7]
- 43. DSI-EEG+fNIRS [https://wearablesensing.com/dsi-eegfnirs/]
- 44. BrainWatch Point-of-Care EEG [https://natus.com/neuro/brainwatch/]
- 45. evaluating electrode reduction methods for EEG-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12263900/]
- 46. Effects of individualized brain anatomies and EEG ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9606706/]
- 47. Evaluating the influence of anatomical accuracy and ... [https://www.sciencedirect.com/science/article/pii/S105381192300410X]
- 48. ECG Lead Misplacement: Looking at Common Issues [https://www.gehealthcare.com/insights/article/ecg-lead-misplacement-looking-at-common-issues?srsltid=AfmBOoovdV4yeEQlNSzW3u1iBZn3lqvtN7XeV8_H4eM4RG4TgCG4pFSf]
- 49. Anatomically Veridical On‐Scalp Sensor Topographies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11906917/]
- 50. Evaluation of EEG pre-processing and source localization ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1479569/full]
- 51. EEG electrode setup optimization using feature extraction ... [https://pubmed.ncbi.nlm.nih.gov/39959920/]
- 52. How to reduce noise interference in nerve conduction ... [https://natus.com/insights/how-to-reduce-noise-interference-in-nerve-conduction-studies-and-emg-signals/]
- 53. Interference of tonic muscle activity on the EEG: a single motor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4092367/]
- 54. Adaptive EEG preprocessing to mitigate electrode shift ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12630851/]
- 55. Validation of cost-efficient EEG experimental setup for ... [https://www.nature.com/articles/s41598-023-49990-6]
- 56. Effect of reducing the recording time of standard EEGs on ... [https://www.sciencedirect.com/science/article/pii/S1059131112000933]
- 57. Optimizing electrode configurations for EEG mild cognitive ... [https://www.nature.com/articles/s41598-024-84277-4]
- 58. A comprehensive EEG dataset and performance ... [https://www.nature.com/articles/s41598-025-18934-7]
- 59. Exploratory quantitative EEG characteristics in children ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1689000/full]
- 60. Correlations between EEG abnormalities and clinical ... [https://www.sciencedirect.com/science/article/pii/S3050656525000082]
- 61. Independent component analysis of oddball EEG ... [https://www.nature.com/articles/s41598-025-07645-8]
- 62. Trends in EEG signal feature extraction applications [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2022.1072801/full]
- 63. An improved feature extraction algorithm for EEG-based ... [https://www.nature.com/articles/s41598-025-18554-1]
- 64. An automated extraction of spectral-temporal and spatial ... [https://braininformatics.springeropen.com/articles/10.1186/s40708-025-00265-y]
- 65. A hybrid convolutional neural network with attention-based ... [https://www.sciencedirect.com/science/article/pii/S0006899325000423]
- 66. EEG Sync With Other Biosensors and Software [https://www.bitbrain.com/blog/eeg-synchronization]
- 67. A comparative study to assess synchronisation methods for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11997080/]
- 68. RELAX‐Jr: An Automated Pre‐Processing Pipeline for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11456615/]
- 69. Streamlining cVEP Paradigms: Effects of a Minimized ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12190882/]
- 70. Selecting methods for a modular EEG pre-processing ... [https://www.sciencedirect.com/science/article/pii/S1746809423012636]
- 71. Optimising Electrode Montages in Conventional Transcranial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12025885/]
- 72. ROC curve analysis (AUC, Sensitivity, Specificity, etc.) [https://www.medcalc.org/en/manual/roc-curves.php]
- 73. A guide to interpreting the area under the curve value - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10664195/]
- 74. Effects of a reduction of the number of electrodes in the EEG ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8930978/]
- 75. High density EEG in current clinical practice and opportunities ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8083969/]
- 76. comparison of electrode placement in two-channel EEG [https://www.sciencedirect.com/science/article/abs/pii/S0887899425002073]
- 77. Targeted density electrode placement achieves high ... [https://www.sciencedirect.com/science/article/abs/pii/S138824572300706X]
- 78. Visual analysis of high density EEG: As good as electrical ... [https://www.sciencedirect.com/science/article/pii/S2467981X1930040X]
- 79. Feasibility of Reconstructing Source Functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8556201/]
- 80. Recent Advances in Portable Dry Electrode EEG [https://www.mdpi.com/1424-8220/25/16/5215]
- 81. A Comprehensive Look at In-Ear EEG Electrodes and Their ... [https://www.mdpi.com/1424-8220/25/11/3321]
- 82. Adaptive EEG preprocessing to mitigate electrode shift ... [https://pubmed.ncbi.nlm.nih.gov/41257892/]
- 83. From pronounced to imagined: improving speech decoding ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2025.1583428/full]
- 84. Decoding Imagined Speech from EEG Data: A Hybrid ... [https://www.mdpi.com/2075-1729/14/11/1501]
- 85. A State-of-the-Art Review of EEG-Based Imagined Speech ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9086783/]
- 86. Individual stability of single-channel EEG measures over ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12322233/]
- 87. Understanding the 10-20 System of EEG Electrode Placement – EMOTIV [https://www.emotiv.com/blogs/how-to/understanding-the-10-20-system-of-eeg-electrode-placement]