Optimizing Brain Imaging Parameters for Individual Differences: From Acquisition to Personalized Clinical Translation
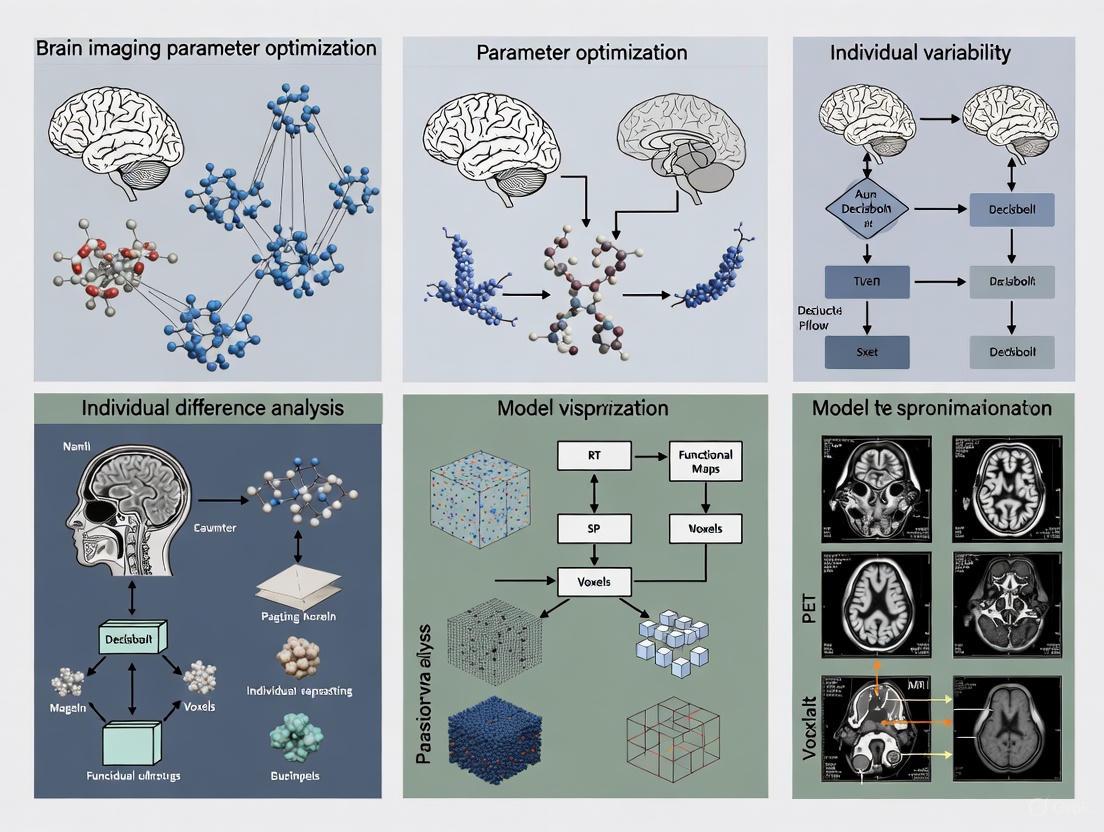
This article provides a comprehensive framework for optimizing brain imaging parameters to better capture and interpret individual differences in neuroscience research and clinical applications.
Optimizing Brain Imaging Parameters for Individual Differences: From Acquisition to Personalized Clinical Translation
Abstract
This article provides a comprehensive framework for optimizing brain imaging parameters to better capture and interpret individual differences in neuroscience research and clinical applications. It explores the foundational need to move beyond group-level analyses, details methodological advances in fMRI and DTI that enhance effect sizes, and presents systematic strategies for optimizing preprocessing pipelines to improve reliability and statistical power. Furthermore, it evaluates validation frameworks and comparative performance of analytical models. Designed for researchers and drug development professionals, this review synthesizes current best practices and emerging trends, including AI integration, to guide the development of more robust, reproducible, and individually sensitive neuroimaging protocols.
Why One-Size-Fits-All Fails: The Imperative for Individualized Neuroimaging
The Challenge of Effect Sizes and Reliability in Individual Differences Research
FAQs on Effect Shes and Reliability
What is the "reliability paradox" in individual differences research? The reliability paradox describes a common situation in cognitive sciences where measurement tools that robustly produce within-group effects (e.g., a task that consistently shows an effect in a group of participants) tend to have low test-retest reliability. This low reliability makes the same tools unsuitable for studying differences between individuals [1] [2]. At its core, this happens because creating a strong within-group effect often involves minimizing the natural variability between subjects, which is the very same variability that individual differences research seeks to measure reliably [2].
Does poor measurement reliability only affect individual differences studies? No, this is a common misconception. Poor measurement reliability attenuates (weakens) observed group differences as well [1] [2]. Some studies have erroneously suggested that reliability is only a concern for correlational studies of individuals, but both group and individual differences are affected because they both rely on the dimension of between-subject variability. When measurement reliability is low, the observed effect sizes in group comparisons (e.g., patient vs. control) are smaller than the true effect sizes in the population [2].
How does reliability affect the observed effect size in my experiments? Measurement reliability directly attenuates the observed effect size in your data. The following table summarizes how the true effect size is reduced to the observed effect size based on reliability [2].
| True Effect Size (d_true) | Reliability (ICC) | Observed Effect Size (d_obs) |
|---|---|---|
| 0.8 | 0.9 | 0.76 |
| 0.8 | 0.7 | 0.67 |
| 0.8 | 0.5 | 0.57 |
| 0.8 | 0.3 | 0.44 |
Formula: ( d_{obs} = d_{true} \times \sqrt{ICC} )
What are the implications for statistical power and sample size? Low reliability drastically increases the sample size required to achieve sufficient statistical power. As reliability decreases, the observed effect size becomes smaller, and you need a much larger sample to detect that smaller effect [2].
| Target Effect Size (d) | Reliability (ICC) | Observed Effect Size (d_obs) | Sample Size Needed for 80% Power |
|---|---|---|---|
| 0.8 | 0.9 | 0.76 | 56 |
| 0.8 | 0.7 | 0.67 | 71 |
| 0.8 | 0.5 | 0.57 | 98 |
| 0.8 | 0.3 | 0.44 | 162 |
Troubleshooting Guide: Addressing Poor Reliability
This workflow provides a systematic approach for diagnosing and resolving reliability issues in your research data [3] [4].
Step 1: Identify the Problem Define the specific nature of the reliability issue. Is it low test-retest reliability (ICC) for a behavioral task, or high variability in neuroimaging parameters? Review your data to confirm the signal is much noisier than expected [3] [4].
Step 2: Repeat the Experiment Before making any changes, simply repeat the experiment if it's not cost or time-prohibitive. This helps determine if the problem was a one-time mistake (e.g., incorrect reagent volume, extra wash steps) or a consistent, systematic issue [3].
Step 3: Verify with Controls Ensure you have the appropriate positive and negative controls in place. For example, if a neural signal is dim, include a control that uses a protein known to be highly expressed in the tissue. If the control also fails, the problem likely lies with the protocol or equipment [3].
Step 4: Check Equipment & Materials Inspect all reagents, software, and hardware. Molecular biology reagents can be sensitive to improper storage (e.g., temperature). In neuroimaging, ensure all system parameters and analysis software versions are correct and compatible [3].
Step 5: Change One Variable at a Time Generate a list of variables that could be causing the low reliability (e.g., fixation time, antibody concentration, analysis parameters). Systematically change only one variable at a time to isolate the root cause [3] [4]. For parameter optimization in neural decoding, consider using an automated framework like NEDECO, which can efficiently search complex parameter spaces [5].
Step 6: Document Everything Keep detailed notes in your lab notebook of every change made and the corresponding outcome. This creates a valuable record for your future self and your colleagues [3] [4].
The Scientist's Toolkit
| Category | Item | Function |
|---|---|---|
| Statistical Analysis | Intraclass Correlation Coefficient (ICC) | Quantifies test-retest reliability of a measure by partitioning between-subject and error variance [2]. |
| Statistical Analysis | Cohen's d* | An effect size metric for group comparisons that does not assume equal variances between groups [2]. |
| Software & Tools | NEDECO (NEural DEcoding COnfiguration) | An automated parameter optimization framework for neural decoding systems that can improve accuracy and time-efficiency [5]. |
| Software & Tools | Data Color Picker / Viz Palette | Tools for selecting accessible color palettes for data visualization, crucial for highlighting results without distorting meaning [6]. |
| Methodological Framework | Brain Tissue Phantom with Engineered Cells | An in vitro assay for modeling in vivo optical conditions to optimize imaging parameters for deep-brain bioluminescence activity imaging before animal experiments [7]. |
| 3-hydroxy-2-(pyridin-4-yl)-1H-inden-1-one | 3-hydroxy-2-(pyridin-4-yl)-1H-inden-1-one|CAS 67592-40-9 | |
| Thallium(III) bromide | Thallium(III) Bromide | High Purity | For Research | High-purity Thallium(III) Bromide for materials science and chemical synthesis research. For Research Use Only. Not for human or veterinary use. |
Technical Support Center: FAQs & Troubleshooting
Frequently Asked Questions
Q1: Why is my fMRI analysis producing unexpectedly high false positive rates?
A high false positive rate is often traced to the statistical method used for cluster-level inference [8]. A 2016 study found that one common method, when based on Gaussian random field theory, could yield false positive rates up to 70% instead of the assumed 5% [8]. This issue affected software packages including AFNI (which contained a bug, since fixed in 2015), FSL, and SPM [8].
- Troubleshooting Steps:
- Verify Software Version: Confirm you are using an AFNI version updated after 2015 [8].
- Use Non-Parametric Methods: Switch to non-parametric inference methods, such as permutation testing, which were validated as a robust alternative in the Eklund et al. study [8].
- Check Your Data: Use the open data from the Eklund et al. paper to validate your analysis pipeline.
Q2: Our research focuses on individual differences, but we are struggling with low effect sizes. What strategies can we employ?
Optimizing effect sizes is crucial for robust individual differences research, potentially reducing the required sample size from thousands to hundreds [9]. The following table summarizes four core strategies.
Table: Strategies for Optimizing Effect Sizes in Individual Differences Neuroimaging Research
| Strategy | Core Principle | Implementation Example |
|---|---|---|
| Theoretical Matching [9] | Maximize the association between the neuroimaging task and the behavioral construct. | Select a response inhibition task that is a strong phenotypic marker for the specific impulsivity trait you are studying. |
| Increase Measurement Reliability [9] | Improve the reliability of both neural and behavioral measures to reduce noise. | Use multiple runs of a task and aggregate data to enhance the signal-to-noise ratio for neural measurements [9]. |
| Individualization [9] | Tailor stimuli or analysis to individual participants' characteristics. | Adjust the difficulty of a cognitive task in real-time based on individual performance to ensure optimal engagement. |
| Multivariate Cross-Validation [9] | Use multivariate models with cross-validation instead of univariate mass-testing. | Employ a predictive model with cross-validation to assess how well a pattern of brain activity predicts a trait, rather than testing each voxel individually. |
Q3: How should we organize our neuroimaging dataset to ensure compatibility with modern analysis pipelines and promote reproducibility?
Adopt the Brain Imaging Data Structure (BIDS) standard [10]. BIDS provides a simple and human-readable way to organize data, which is critical for machine readability, pipeline interoperability, and reproducibility.
- Solution Steps:
- Follow the Structure: Organize your data with a main project directory and subdirectories for each participant (e.g.,
sub-control01). Within these, create modality-specific folders likeanat,func,dwi, andfmap[10]. - Use Standardized Naming: Name files consistently to include key entities like subject ID, session, task, and modality (e.g.,
sub-control01_task-nback_bold.nii.gz) [10]. - Include Sidecar Files: Provide accompanying
.jsonfiles for each data file to store critical metadata about acquisition parameters [10].
- Follow the Structure: Organize your data with a main project directory and subdirectories for each participant (e.g.,
Q4: What are the best practices for sharing data and analysis code to ensure the reproducibility of our findings?
The OHBM Committee on Best Practices (COBIDAS) provides detailed recommendations [11].
- Actionable Checklist:
- Share Multiple Data Forms: Where feasible, share data in multiple states – from raw (DICOM) to preprocessed, to enable different types of reanalysis [11].
- Report Transparently: Document and report all aspects of your study, including researcher degrees of freedom and analytical paths that were attempted but not successful [11].
- Share Analysis Code: Publish the exact code and parameters used for your analysis to enable "computational reproducibility," where others can re-run your analysis on the same data [11].
The Scientist's Toolkit
Table: Essential Software Tools for Neuroimaging Personalization Research
| Tool Name | Primary Function | Relevance to Personalization |
|---|---|---|
| Nibabel [10] | Reading/Writing Neuroimaging Data | Foundational library for data access; essential for all custom analysis pipelines. |
| Nilearn / BrainIAK [10] | Machine Learning for fMRI | Implements multivariate approaches and cross-validation, key for optimizing effect sizes [9]. |
| DIPY [10] | Diffusion MRI Analysis | Enables analysis of white matter microstructure and structural connectivity, a core component of individual differences. |
| Nipype [10] | Pipeline Integration | Allows creation of reproducible workflows that combine tools from different software packages (e.g., FSL, AFNI, FreeSurfer). |
| AFNI, FSL, SPM [12] | fMRI Data Analysis | Standard tools for univariate GLM analysis; require careful configuration to control false positives [8]. |
| BIDS Validator | Data Standardization | Ensures your dataset is compliant with the BIDS standard, facilitating data sharing and pipeline use [10]. |
| 1,5-Dimethyl-3-phenylpyrazole | 1,5-Dimethyl-3-phenylpyrazole, CAS:10250-60-9, MF:C11H12N2, MW:172.23 g/mol | Chemical Reagent |
| 2H-Azepin-2-one, hexahydro-1-(2-propenyl)- | 2H-Azepin-2-one, hexahydro-1-(2-propenyl)-, CAS:17356-28-4, MF:C9H15NO, MW:153.22 g/mol | Chemical Reagent |
Experimental Protocols & Workflows
Protocol 1: Reproducible fMRI Analysis Pipeline with Nipype
This protocol outlines a robust workflow for task-based fMRI analysis, integrating quality control and best practices for statistical inference.
Protocol 2: Optimization of Effect Sizes for Individual Differences
This methodology details the steps for designing a study to maximize the detectability of brain-behavior relationships.
Linking Neural Circuit Variability to Behavior and Clinical Phenotypes
Troubleshooting Guide: Common Experimental Challenges
FAQ: Addressing Key Methodological Hurdles
1. How can I distinguish true neural signal from noise when studying individual variability? Historically, neural variability was dismissed as noise, but it is now recognized as a meaningful biological signal. To distinguish signal from noise:
- Employ Precision Functional Mapping: Collect extensive data from individual participants (e.g., 10 hours per subject) to create reliable individual-specific brain maps, as this can reveal unique networks common across some, but not all, people [13].
- Leverage Task-Based Paradigms: Study variability within disorder-relevant tasks, as moment-to-moment neural fluctuations are a crucial substrate for cognition and can be a biomarker for psychiatric conditions [14].
- Utilize Longitudinal Designs: Track individuals over time to establish stable, trait-like neural patterns versus state-dependent variations [14].
2. What is the best approach for linking a specific neural circuit perturbation to a behavioral change? Establishing a causal relationship requires more than just observing correlation.
- Multi-Paradigm Validation: Avoid relying on a single behavioral test. Use additional paradigms or procedures to support your initial data interpretation. For example, if using an automated lever-press task, also record behavior with a webcam to qualitatively assess factors like motor behavior, arousal, or exploration that the automated system might miss [15].
- Precise Circuit Manipulation: Use interventional tools like optogenetics, chemogenetics, or deep brain stimulation (DBS) to change neural circuit dynamics and observe subsequent behavioral effects [16]. For DBS, develop algorithms to individually "tune" stimulation parameters (site, intensity, timing) for each patient's specific brain circuit response [13].
- Describe Behavior Precisely: Report observed behaviors in precise terms separate from speculation. Overgeneralization of conclusions is a common pitfall [15].
3. My brain imaging data shows inconsistent results across subjects. How can I account for high individual variability? Individual variability is a feature, not a bug, of brain organization.
- Shift from Group-Averages to Individual-Focus: Group-averaged data can mask important individual differences in brain structure and function. Use precision brain imaging to map structure, function, and connectivity in single individuals [13].
- Identify Individual Networks: Recognize that some functional brain networks are common across people, while others are unique to single individuals. These unique networks may underlie behavioral variability [13].
- Control Technical Factors: In MRI, technical factors like field-of-view (FOV) phase and phase oversampling significantly impact scan time and consistency. Optimizing these parameters is crucial for reproducible data [17].
4. How can I optimize brain imaging parameters to balance scan time, resolution, and patient comfort? Technical optimization is key for quality data.
- Adjust Specific MRI Parameters: Research shows that altering the FOV phase and phase oversampling can significantly reduce scan time without necessarily compromising spatial resolution. For example, one study reduced scan time from 3.47 minutes to 2.18 minutes by optimizing these parameters [17].
- Ensure Proper Patient Positioning: Use head holders and secure the patient's head with chin and head straps. Position the canthomeatal line (from the outer eye corner to the ear canal) vertically perpendicular to the imaging table to standardize orientation and reduce motion artifacts [18].
- Follow Radiopharmaceutical Protocols: For molecular brain imaging (SPECT/PET), strictly adhere to the injection and acquisition parameters in the package insert to ensure consistent and interpretable results [18].
Experimental Protocols & Methodologies
Protocol 1: Precision Functional Mapping for Individual Brain Network Identification
Objective: To create high-resolution maps of functional brain organization unique to individual participants [13].
Procedure:
- Data Acquisition: Acquire high-resolution functional MRI (fMRI) data from individual participants. A typical protocol involves collecting approximately 10 hours of scanning data per subject to achieve sufficient signal-to-noise [13].
- Preprocessing: Standard fMRI preprocessing steps (motion correction, normalization, etc.) should be applied.
- Individual Network Analysis: Analyze the fMRI time-series data to identify functional networks within each individual's brain without relying on group-averaged templates. This can reveal:
- Common Networks: Networks that appear across many individuals.
- Unique Networks: Networks that are specific to a single individual, which may explain unique behavioral traits [13].
- Validation: Correlate the identified individual-specific network configurations with behavioral measures.
Protocol 2: Linking Genetic Risk to Neural Circuitry and Behavior in Adolescents
Objective: To investigate how polygenic risk for behavioral traits (BIS/BAS) influences striatal structure and emotional symptoms [19].
Procedure:
- Participant Cohort: Utilize a large-scale dataset like the Adolescent Brain Cognitive Development (ABCD) Study, which includes children around 9-11 years old [19].
- Genotyping & Polygenic Risk Score (PRS) Calculation:
- Perform genome-wide association studies (GWAS) on Behavioral Inhibition System (BIS) and Behavioral Activation System (BAS) traits in a discovery sample.
- Calculate PRS for each participant in the target sample using the GWAS summary statistics, representing their genetic predisposition for these traits [19].
- Diffusion-Weighted Imaging (DWI) Processing:
- Preprocess DWI data to correct for distortions, eddy currents, and head motion.
- Use probabilistic tractography (e.g., with FSL's
probtrackx2) to model the structural connectivity between the striatum and cortical regions [19].
- Striatal Structural Gradient (SSG) Analysis: Compute a low-dimensional representation (gradient) of the striatal connectivity matrix to summarize its macroscale anatomical organization [19].
- Statistical Modeling: Test the association between BIS/BAS PRS, the SSG, and symptoms of anxiety and depression using mediation analysis to see if striatal structure mediates the genetic effect on emotion [19].
Data Presentation
Table 1: Impact of MRI Parameter Adjustments on Scan Time
This table summarizes quantitative findings from a study investigating how technical factors in MRI affect acquisition time, essential for designing efficient and comfortable imaging protocols [17].
| Technical Factor | Original Protocol Value | Optimized Protocol Value | Effect on Scan Time | Statistical Significance (p-value) |
|---|---|---|---|---|
| Field-of-View (FOV) | 230 mm | 217 mm | No direct significant effect | p = 0.716 |
| FOV Phase | 90% | 93.88% | Significant reduction | p < 0.001 |
| Phase Oversampling | 0% | 13.96% | Significant reduction | p < 0.001 |
| Cross-talk | Not specified | 38.79 (avg) | No significant effect | p = 0.215 |
| Total Scan Time | 3.47 minutes | 2.18 minutes | ~37% reduction | N/A |
Table 2: Research Reagent Solutions for Neural Circuit Analysis
This table lists key tools and reagents used in modern circuit mapping and manipulation, illustrating the interdisciplinary nature of the field [16] [20] [15].
| Reagent / Tool | Category | Primary Function | Key Consideration |
|---|---|---|---|
| Viral Tracers (e.g., AAVs, Lentiviruses) | Circuit Tracing | Identify efferent (anterograde) and afferent (retrograde) connections of specific neuronal populations [20]. | High selectivity; can be genetically targeted to cell types. |
| Conventional Tracers (e.g., CTB, Fluorogold) | Circuit Tracing | Map neural pathways via anterograde or retrograde axonal transport. Compatible with light microscopy [20]. | Well-established; less complex than viral tools but offer less genetic specificity. |
| Optogenetics Tools (e.g., Channelrhodopsin) | Circuit Manipulation | Precisely activate or inhibit specific neural populations with light to test causal roles in behavior [16] [15]. | Requires genetic access and light delivery; provides millisecond-scale temporal precision. |
| Chemogenetics Tools (e.g., DREADDs) | Circuit Manipulation | Remotely modulate neural activity in specific cells using administered designer drugs [16] [15]. | Less temporally precise than optogenetics but does not require implanted hardware. |
| Deep Brain Stimulation (DBS) | Circuit Manipulation | Electrical stimulation of brain areas to modulate circuit function, often for therapeutic purposes [13]. | New algorithms can individualize stimulation parameters for better outcomes. |
Methodological Visualizations
Diagram 1: Neural Circuit Investigation Workflow
Diagram 2: Precision Imaging vs. Group-Average Paradigm
FAQs: Understanding Inter-Subject Variability
1. What is inter-subject variability in brain imaging and why should we treat it as data rather than noise? Inter-subject variability refers to the natural differences in brain anatomy and function between individuals. Rather than treating this variance as measurement noise, modern neuroscience recognizes it as scientifically and clinically valuable data. This variability is the natural output of a noisy, plastic system (the brain) where each subject embodies a particular parameterization of that system. Understanding this variability helps reveal different cognitive strategies, predict recovery capacity after brain damage, and explain wide differences in human abilities and disabilities [21].
2. What are the main anatomical sources of inter-subject variability? The main structural and physiological parameters that govern individual-specific brain parameterization include: grey matter density, cortical thickness, morphological anatomy, white matter circuitry (tracts and pathways), myelination, callosal topography, functional connectivity, brain oscillations and rhythms, metabolism, vasculature, and neurotransmitters [21].
3. Does functional variability increase further from primary sensory regions? Contrary to what might be expected, evidence suggests that inter-subject anatomical variability does not necessarily increase with distance from neural periphery. Studies of primary visual, somatosensory, motor cortices, and higher-order language areas have shown consistent anatomical variability across these regions [22].
4. How does cognitive strategy contribute to functional variability? Different subjects may employ different cognitive strategies to perform the same task, engaging distinct neural pathways. For example, in reading tasks, subjects may emphasize semantic versus nonsemantic reading strategies, activating different frontal cortex regions. This "degeneracy" (where the same task can be performed in multiple ways) is a dominant source of intersubject variability [21] [23].
5. What are the key methodological challenges in measuring individual differences? The main challenge involves distinguishing true between-subject differences from within-subject variation. The brain is a dynamic system, and any single measurement captures only a snapshot of brain function at a given moment. Sources of variation exist across multiple time scales - from moment-to-moment fluctuations to day-to-day changes in factors like attention, diurnal rhythms, and environmental influences [24].
Troubleshooting Guides
Issue 1: Poor Prediction Accuracy in Brain-Behavior Association Studies
Problem: Low prediction accuracy when associating brain measures with behavioral traits or clinical outcomes.
Solutions:
- Increase scan duration: For fMRI scans ≤20 minutes, prediction accuracy increases linearly with the logarithm of total scan duration (sample size × scan time). Aim for at least 20-30 minutes per subject, with 30 minutes being most cost-effective on average [25].
- Implement precision mapping: Collect extensive data per participant (e.g., >20-30 minutes of fMRI data) to improve reliability of individual-level estimates [26].
- Use individualized parcellations: Rather than assuming group-level correspondence, model individual-specific patterns of brain organization. Hyper-aligning fine-grained features of functional connectivity can markedly improve prediction of general intelligence compared to region-based approaches [26].
- Address measurement error in behavior: Extend cognitive task duration (e.g., from 5 minutes to 60 minutes) to improve precision of behavioral measures, as measurement error in behavioral variables attenuates prediction performance [26].
Issue 2: High Variability in Group-Level ICA Components
Problem: Group independent component analysis (ICA) fails to adequately capture inter-subject variability in spatial activation patterns.
Solutions:
- Assess spatial variability impact: When spatial activations moderately overlap across subjects, GICA captures spatial variability well. However, with minimal overlap, estimation of subject-specific spatial maps fails [27].
- Use joint amplitude estimation: When estimating component amplitude (level of activation) across subjects, use a joint estimator across both temporal and spatial domains, especially when spatial variability is present [27].
- Optimize model order: Consider ICA model order as a factor affecting ability to compare subject activations appropriately [27].
- Employ dual regression: Use dual regression approaches to estimate subject-specific spatial maps and time courses from group-level components [27].
Issue 3: Accounting for Different Cognitive Strategies in Task-Based fMRI
Problem: Unexplained variability in activation patterns may reflect subjects employing different cognitive strategies for the same task.
Solutions:
- Identify strategies post-hoc: Use data-driven approaches like Gaussian Mixture Models (GMM) to identify subgroups of subjects with similar activation patterns, then determine if these correspond to different cognitive strategies [23].
- Design constrained tasks: For tasks where strategies are known a priori, use experimental manipulations to implicitly or explicitly push participants toward a particular strategy [21].
- Collect strategy reports: Include subjective reports and behavioral measures that might indicate strategy use [21].
- Analyze by subgroup: Rather than averaging across all subjects, analyze data separately for different strategy subgroups to avoid false negatives and false positives in group averages [21].
Experimental Protocols & Methodologies
Protocol 1: Precision Functional Mapping for Individual-Specific Brain Organization
Purpose: To map individual-specific functional organization of the brain, revealing networks that may be unique to individuals or common across participants.
Methodology:
- Data Collection: Acquire 10+ hours of individual fMRI data per participant across multiple sessions [13].
- Preprocessing: Standard preprocessing including slice timing correction, realignment, coregistration, normalization, spatial smoothing, and bandpass filtering.
- Individualized Analysis: Analyze data at the individual level rather than relying solely on group averages.
- Network Identification: Identify both common networks across individuals and unique, person-specific networks [13].
Applications: Revealing physically interwoven but functionally distinct networks (e.g., language and social thinking networks in the frontal lobe); identifying novel brain networks in individuals that may underlie behavioral variability [13].
Purpose: To identify distinct subgroups of subjects that explain the main sources of variability in neuronal activation for a specific task.
Methodology (as implemented for reading activation):
- Data Collection: Collect fMRI data from a large sample (n=76) with varied demographic characteristics performing the task of interest [23].
- Initial Analysis: Perform one-sample t-test on all subjects, treating intersubject variability as error variance.
- Dimension Reduction: Apply Principal Component Analysis to the error variance to capture main sources of variance.
- Subgroup Identification: Use Gaussian Mixture Modeling to probabilistically assign subjects to different subgroups.
- Characterization: Conduct post-hoc analyses to determine defining differences between identified groups (e.g., demographic factors, cognitive strategies) [23].
Key Findings from Reading Study: Age and reading strategy (semantic vs. nonsemantic) were the most prominent sources of variability, more significant than handedness, sex, or lateralization [23].
Table 1: Effect of Scan Duration and Sample Size on Prediction Accuracy in BWAS
| Total Scan Duration (min) | Prediction Accuracy (Pearson's r) | Interchangeability of Scan Time & Sample Size |
|---|---|---|
| Short (≤20 min) | Lower | Highly interchangeable; logarithmic increase with total duration |
| 20-30 min | Moderate | Sample size becomes progressively more important |
| ≥30 min | Higher | Diminishing returns for longer scans; 30 min most cost-effective |
Table 2: Primary Sources of Inter-Subject Variability and Assessment Methods
| Variability Source | Assessment Method | Key Findings |
|---|---|---|
| Cognitive Strategy | Gaussian Mixture Models [23] | Different strategies employ distinct neural pathways |
| Age Effects | Post-hoc grouping analysis [23] | Significant effect on reading activation patterns |
| Structural Parameters | Morphometric analysis [21] | Grey matter density, cortical thickness, white matter connectivity |
| Functional Connectivity | Inter-subject Functional Correlation [28] | Hierarchical organization of extrinsic/intrinsic systems |
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Variability Research
| Tool/Technique | Function | Application Context |
|---|---|---|
| Precision fMRI Mapping | Maps individual-specific functional organization | Identifying unique and common brain networks across individuals |
| Group ICA with Dual Regression | Captures inter-subject variability in spatial patterns | Analyzing multi-subject datasets while accounting for individual differences |
| Inter-Subject Functional Correlation (ISFC) | Measures stimulus-driven functional connectivity across subjects | Dissecting extrinsically- and intrinsically-driven processes during naturalistic stimulation |
| Gaussian Mixture Modeling (GMM) | Identifies subgroups explaining main variability sources | Data-driven approach to detect different cognitive strategies |
| Hyper-Alignment | Aligns fine-grained functional features across individuals | Improves prediction of behavioral traits from brain measures |
| diethyl 1H-indole-2,5-dicarboxylate | Diethyl 1H-indole-2,5-dicarboxylate|CAS 127221-02-7 | |
| 1-[(4-Methylphenyl)methyl]-1,4-diazepane | 1-[(4-Methylphenyl)methyl]-1,4-diazepane |
Research Workflow Diagrams
Precision Research Workflow for Individual Differences
Sources of Inter-Subject Variability
Advanced Acquisition and Analysis: Boosting Sensitivity to Individual Brains
Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Which design should I choose for a pre-surgical mapping of language areas in a patient with a brain tumor? A: For clinical applications like pre-surgical mapping, where the goal is robust localization of function, evidence suggests that a rapid event-related design can provide comparable or even higher detection power than a blocked design, particularly in patients [29]. It can generate more sensitive language maps and is less sensitive to head motion, which is a common concern in patient populations [29].
Q2: I am concerned about participants predicting the order of stimuli in my experiment. How can I mitigate this? A: Stimulus-order predictability is a known confound in block designs. An event-related design, particularly one with a jittered inter-stimulus interval (ISI), randomizes the presentation of stimuli, which helps to minimize a subject's expectation effects and habituation [29] [30]. This is one of the key theoretical advantages of event-related fMRI.
Q3: My primary research goal is to study individual differences in brain function. What design considerations are most important? A: Standard task-fMRI analyses often suffer from limited reliability, which is a major hurdle for individual differences research. To enhance this, consider moving beyond simple activation comparisons. Recent approaches involve deriving neural signatures from large datasets that classify brain states related to task conditions (e.g., high vs. low working memory load). These signatures have been shown to be more reliable and have stronger associations with behavior and cognition than standard activation estimates [31]. Furthermore, ensure your paradigm has high test-retest reliability at the single-subject level, which is not a given for all cognitive tasks [32].
Q4: I've heard that software errors can affect fMRI results. What should I do? A: It is critical to use the latest versions of analysis software and to be aware that errors have been discovered in popular tools in the past [33]. If you have published work using a software version in which an error was later identified, the recommended practice is to re-run your analyses with the corrected version and, in consultation with the journal, consider a corrective communication if the results change substantially [33].
Q5: How can I improve the test-retest reliability of my fMRI activations? A: Reliability can be poor at the single-voxel level due to limited signal-to-noise ratio [32]. However, the reliability of hemispheric lateralization indices tends to be higher [32]. Focusing on network-level or multivariate measures (like neural signatures) rather than isolated voxel activations can also improve reliability for individual differences research [31].
Troubleshooting Common Experimental Design Problems
| Problem | Symptoms | Possible Causes & Solutions |
|---|---|---|
| Low Detection Power | Weak or non-existent activation in expected brain regions; low statistical values. | Cause: Design lacks efficiency for the psychological process of interest. Solution: For simple contrasts, use a blocked design for its high statistical power [29] [30]. For more complex cognitive tasks, a rapid event-related design can be equally effective and avoid predictability [29]. |
| Low Reliability for Individual Differences | Brain-behavior correlations are weak or unreplicable; activation patterns are unstable across sessions. | Cause: Standard activation measures have limited test-retest reliability [31] [32]. Solution: Use paradigms with proven single-subject reliability [32]. Employ machine learning-derived neural signatures trained to distinguish task conditions, which show higher reliability and stronger behavioral associations [31]. |
| Stimulus-Order Confounds | Activation may be influenced by participant anticipation or habituation rather than the cognitive process itself. | Cause: Predictable trial sequence in a blocked design [30]. Solution: Switch to a rapid event-related design with jittered ISI to randomize stimulus order and reduce expectation effects [29]. |
| Suboptimal Design for MVPA/BCI | Poor single-trial classification accuracy for Brain-Computer Interface or Multi-Voxel Pattern Analysis applications. | Cause: Pure block designs may induce participant strategies and adaptation; pure event-related designs lack rest periods for feedback processing. Solution: Consider a hybrid blocked fast-event-related design, which combines rest periods with randomly alternating trials and has shown promising decoding accuracy and stability [34]. |
Quantitative Data Comparison of fMRI Designs
Performance Metrics Across Design Types
Table 1: A comparison of key characteristics for blocked, event-related, and hybrid fMRI designs.
| Design Feature | Blocked Design | Event-Related (Rapid) | Hybrid Design |
|---|---|---|---|
| Statistical Power/Detection Sensitivity | High [29] [30] | Comparable to or can be higher than blocked in some contexts (e.g., patient presurgical mapping) [29] | High, close to block design performance [34] |
| Stimulus Order Predictability | High, a potential confound [30] | Low, due to randomization [29] [30] | Moderate, depends on implementation |
| Resistance to Head Motion | Less sensitive [29] | More sensitive [29] | Information missing from search results |
| Ability to Isolate Single Trials | No | Yes, allows for post-hoc sorting by behavior [30] | Yes |
| Suitability for BCI/MVPA | Considered safe but may induce strategies [34] | Allows random alternation but lacks rest for feedback [34] | High, a viable alternative [34] |
| Ease of Implementation | Simple [30] | More complicated; requires careful timing [30] | More complicated |
Experimental Protocols from Key Studies
Table 2: Detailed methodologies from cited experiments comparing fMRI designs.
| Study | Participants | Task | Design Comparisons Key Parameters |
|---|---|---|---|
| Xuan et al., 2008 [29] | 6 healthy controls & 8 brain tumor patients | Vocalized antonym generation | Blocked: Alternating task/rest blocks. Event-Related: Rapid, jittered ISI (stochastic design). Imaging: 3.0T GE, TR=2000 ms. |
| Chee et al., 2003 [30] | 12 (Exp1), 8 (Exp2), & 12 (Exp3) healthy volunteers | Semantic associative judgment on word triplets (Word Frequency Effect) | Exp1 (Blocked): Alternating blocks of high/low-frequency words vs. size-judgment control. Exp2 (Blocked): Same task vs. fixation control. Exp3 (Event-Related): Rapid mixed design, randomized stimuli with variable fixation (4,6,8,10s). Imaging: 2.0T Bruker, TR=2000 ms. |
| Schuster et al., 2017 [32] | Study 1: 15; Study 2: 20 healthy volunteers | Visuospatial processing (Landmark task) | Paradigm Comparison (Study 1): Compared Landmark, "dots-in-space," and mental rotation tasks. Reliability (Study 2): Test-retest of Landmark task across two sessions (5-8 days apart). Focus on lateralization index (LI) reliability. |
| Gembris et al., (Preprint) [31] | 9,024 early adolescents | Emotional n-back fMRI task (working memory) | Neural Signature Approach: Derived a classifier distinguishing high vs. low working memory load from fMRI activation patterns to capture individual differences. |
Signaling Pathways and Workflows
fMRI Experimental Design Workflow
The Scientist's Toolkit
Essential Research Reagents and Materials
Table 3: Key software tools and resources for fMRI experimental design and analysis.
| Item Name | Type | Primary Function | Key Considerations |
|---|---|---|---|
| GingerALE | Software | A meta-analysis tool for combining results from multiple fMRI studies [33]. | Ensure you are using the latest version to avoid known statistical correction errors found in past releases [33]. |
| Neural Signature Classifier | Analytical Method | A machine-learning model derived from fMRI data to distinguish between task conditions and capture individual differences [31]. | More reliable and sensitive to brain-behavior relationships than standard activation analysis; requires a substantial training dataset [31]. |
| Rapid Event-Related Design | Experimental Paradigm | Presents discrete, short-duration events in a randomized, jittered fashion to reduce predictability [29]. | Ideal for isolating single trials and reducing expectation confounds; requires careful optimization of timing (ISI/ITI) [29] [30]. |
| Hemispheric Lateralization Index (LI) | Analytical Metric | Quantifies the relative dominance of brain activation in one hemisphere over the other for a specific function [32]. | Can be a robust and reliable measure at the single-subject level, even when single-voxel activation maps are not [32]. |
| Hybrid Blocked/Event-Related Design | Experimental Paradigm | Combines the rest periods of a block design with the randomly alternating trials of a rapid event-related design [34]. | A promising alternative for BCI and MVPA studies where pure block designs are sub-optimal due to participant strategy and adaptation [34]. |
| N-(4-fluorophenyl)cyclohexanecarboxamide | N-(4-fluorophenyl)cyclohexanecarboxamide|High Purity | N-(4-fluorophenyl)cyclohexanecarboxamide is a chemical research reagent. It is For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| DL-Theanine | DL-Theanine, CAS:34271-54-0, MF:C7H14N2O3, MW:174.2 g/mol | Chemical Reagent | Bench Chemicals |
Frequently Asked Questions (FAQs)
Q1: What are the most common sources of error in DTI data that affect microstructural analysis?
The primary sources of error in DTI data are random noise and systematic spatial errors. Random noise, which results in a low signal-to-noise ratio (SNR), disrupts the accurate quantification of diffusion metrics and can obscure fine anatomical details, especially in small white matter tracts [35] [36]. Systematic errors are largely caused by spatial inhomogeneities of the magnetic field gradients. These imperfections cause the actual diffusion weighting (the b-matrix) to vary spatially, leading to inaccurate calculations of the diffusion tensor and biased DTI metrics, even if the SNR is high [35] [37]. Correcting for both types of error is crucial for obtaining accurate, reliable data for studying individual brain differences.
Q2: Which specific artifacts are exacerbated at high magnetic field strengths like 7 Tesla, and how can they be mitigated?
At ultra-high fields like 7 Tesla, DTI is particularly prone to N/2 ghosting artifacts and eddy current-induced image shifts and geometric distortions [38]. These artifacts are amplified due to increased B0 inhomogeneities and the stronger diffusion gradients often used. A novel method to mitigate these issues involves a two-pronged approach:
- Optimized Navigator Echo Placement: Using a navigator echo (Nav2) acquired after the diffusion gradients, rather than before them, more accurately captures the phase perturbations induced by the gradients, leading to superior ghosting artifact correction. One study demonstrated a 41% reduction in N/2 ghosting artifacts with this method [38].
- Dummy Diffusion Gradients: Incorporating dummy gradients with opposite polarity to the main diffusion gradients helps to pre-emphasize the gradient system and reduce eddy current-induced B0 shifts, thereby improving image stability and geometric accuracy [38].
Q3: How can we acquire reliable DTI data in the presence of metal implants, such as in post-operative spinal cord studies?
Metal implants cause severe magnetic field inhomogeneities, leading to profound geometric distortions that traditionally render DTI ineffective. An effective solution is the rFOV-PS-EPI (reduced Field-Of-View Phase-Segmented EPI) sequence [39]. This technique combines two strategies:
- Reduced FOV (rFOV): Uses a two-dimensional radiofrequency (2DRF) pulse to excite a smaller area, minimizing the region affected by susceptibility artifacts.
- Phase-Segmented EPI (PS-EPI): Acquires data over multiple shots, allowing for higher resolution and reduced distortion compared to single-shot EPI.
This combined approach has been shown to produce DTI images with significantly reduced geometric distortion and signal void near cervical spine implants, enabling post-surgical evaluation that was previously not feasible [39].
Troubleshooting Guides
Table 1: Troubleshooting Common DTI Artifacts
| Artifact/Symptom | Root Cause | Corrective Action | Key Experimental Parameters |
|---|---|---|---|
| Low SNR & Noisy Metrics | Insufficient signal averaging; high-resolution acquisition | Implement a denoising algorithm that leverages spatial similarity and diffusion redundancy [36]. | Pre-denoising with local kernel PCA; post-filtering with non-local mean [36]. |
| Spatially Inaccurate FA/MD Maps | Gradient field nonlinearities (systematic error) | Apply B-matrix Spatial Distribution (BSD) correction using a calibrated phantom [35] [37]. | Scanner-specific spherical harmonic functions or phantom-based b(r)-matrix mapping [37]. |
| Geometric Distortions & Ghosting | Eddy currents & phase inconsistencies (esp. at 7T) | Use optimized navigator echoes (Nav2) + dummy diffusion gradients [38]. | Navigator placed after diffusion gradients; dummy gradient momentum at 0.5x main gradient [38]. |
| Metal-Induced Severe Distortions | Magnetic field inhomogeneity from implants | Employ a rFOV-PS-EPI acquisition sequence [39]. | 2DRF pulse for FOV reduction; phase-encoding segmentation [39]. |
| Through-Plane Partial Volume Effects | Large voxel size in slice direction | Use 3D reduced-FOV multiplexed sensitivity encoding (3D-rFOV-MUSE) for high-resolution isotropic acquisition [40]. | Isotropic resolution (e.g., 1.0 mm³); cardiac triggering; navigator-based shot-to-shot phase correction [40]. |
Table 2: Research Reagent Solutions for DTI
| Item | Function in DTI Acquisition | Example Specification/Application |
|---|---|---|
| Isotropic Diffusion Phantom | Serves as a ground truth reference for validating DTI metrics and calibrating BSD correction for systematic errors [37]. | Phantom with known, spatially resolved diffusion tensor field (D(r)) for scanner-specific calibration [37]. |
| Anisotropic Diffusion Phantom | Provides a structured reference to evaluate the accuracy of fiber tracking and the correction of gradient nonlinearities [37]. | Phantom with defined anisotropic structures (e.g., synthetic fibers) to test tractography fidelity [37]. |
| Cervical Spine Phantom with Implant | Enables the development and testing of metal artifact reduction sequences in a controlled setting. | Custom-built model with titanium alloy implants and an asparagus stalk as a spinal cord surrogate [39]. |
| Cryogenic Radiofrequency Coils | Significantly boosts the Signal-to-Noise Ratio (SNR), which is critical for high-resolution DTI in small structures or rodent brains [41]. | Two-element transmit/receive ( ^1H ) cryogenic surface coil for rodent imaging at 11.7 T [41]. |
Experimental Protocols
Protocol 1: Combined Denoising and BSD Correction for Enhanced Metric Accuracy
This protocol details the steps to minimize both random noise and systematic spatial errors in a brain DTI study, which is vital for detecting subtle individual differences [35].
Workflow Overview
Methodology:
- Data Acquisition: Acquire multi-directional DWI data using a single-shot EPI sequence on a 3T or higher scanner. Include a sufficient number of diffusion directions and b-values (e.g., b=1000 s/mm²) for tensor fitting.
- Denoising: Process the magnitude DWI images using a denoising algorithm that exploits both spatial similarity (via patch-based non-local mean filtering) and diffusion redundancy (via local kernel principal component analysis) to improve SNR without blurring critical anatomical details [36].
- BSD Correction: Characterize the spatial distribution of the b-matrix, b(r), using a pre-calibrated isotropic or anisotropic phantom scanned with the same protocol. Apply this spatial correction to the in-vivo DWI data to account for gradient field nonlinearities [35] [37].
- Tensor Estimation and Analysis: Recompute the diffusion tensor and derive maps of FA, MD, AD, and RD. Subsequent analysis in structures like the corpus callosum and internal capsule will show significantly improved accuracy and reliability [35].
Protocol 2: High-Fidelity 3D DTI of the Cervical Spinal Cord
This protocol is designed for high-resolution, distortion-reduced imaging of the cervical spinal cord, addressing challenges like small tissue size and CSF pulsation [40].
Workflow Overview
Methodology:
- Sequence: Use a 3D reduced-FOV multiplexed sensitivity encoding (3D-rFOV-MUSE) sequence. This involves a sagittal thin-slab acquisition [40].
- Artifact Suppression:
- rFOV: A 2D RF pulse is applied to restrict the FOV in the phase-encode direction, minimizing distortions from off-resonance effects.
- Cardiac Triggering: Data acquisition is synchronized with the cardiac cycle to minimize pulsation artifacts from cerebrospinal fluid.
- Reconstruction: The MUSE algorithm integrates a self-referenced ghost correction and a 2D navigator-based inter-shot phase correction to simultaneously eliminate Nyquist ghosting and aliasing artifacts from the multi-shot acquisition [40].
- Outcome: This pipeline produces high-resolution (e.g., 1.0 mm isotropic) DTI data of the cervical cord with mitigated through-plane partial volume effects, enabling multi-planar reformation and more accurate quantification of biomarkers [40].
Leveraging Multivariate Pattern Analysis (MVPA) and Neural Signatures
FAQs & Troubleshooting Guides
Data Acquisition & Preprocessing
Q: Our MVPA results are inconsistent across repeated scanning sessions. How can we improve reliability for individual differences research?
A: Inconsistent results often stem from insufficient attention to individual anatomical and functional variability.
- Solution: Move beyond simple volumetric registration to a common template (e.g., MNI152). Employ advanced, functionally-informed alignment techniques to ensure you are comparing functionally homologous regions across subjects [42].
- Multimodal Surface Matching (MSM): A framework that uses a combination of anatomical (cortical folding) and functional data (e.g., from movie-watching or resting-state) to achieve a better vertex-wise match across individuals [42].
- Hyperalignment: This technique projects individual brains into a common high-dimensional "representational space" based on the similarity of their neural response patterns, effectively aligning brains based on function rather than anatomy alone [42].
- Recommendation: For individual differences research, try multiple alignment approaches and report all results to build collective knowledge about best practices [42].
Q: How much data do I need to collect per subject to obtain reliable neural signatures for individual differences studies?
A: Reliability requires substantial data. While traditional group-level fMRI studies often use 15-30 participants, individual differences research demands much larger sample sizes and more data per subject [42].
- Within-Subject: For resting-state fMRI, at least 5 minutes of data are needed, though advanced analyses may require up to 100 minutes for best results [42].
- Between-Subject: Sample size is critical for brain-behavior correlations. One large-scale study (N=1,498) demonstrated that the effect size of brain-behavior correlations only stabilized and became reproducible with sample sizes greater than 500 participants [43]. For smaller studies, using cross-validation and reporting out-of-sample predictive value is essential [42].
MVPA Analysis & Classification
Q: My classifier performance is at chance level. What are the most common causes and fixes?
A: Poor classifier performance can originate from several points in the analysis pipeline.
- Troubleshooting Table:
| Problem Area | Specific Issue | Potential Solution |
|---|---|---|
| Feature Selection | Using too many voxels, including irrelevant ones, leading to the "curse of dimensionality." [44] | Employ feature selection (e.g., ANOVA, recursive feature elimination) or use a searchlight approach to focus on informative voxel clusters [44] [45]. |
| Model Complexity | Using a complex, non-linear classifier with limited data, causing overfitting. | Start with a simple linear classifier like Linear Support Vector Machine (SVM) or Linear Discriminant Analysis (LDA), which are robust and work well with high-dimensional fMRI data [44] [45]. |
| Cross-Validation | Data leakage between training and test sets, giving over-optimistic performance. | Use strict cross-validation (e.g., leave-one-run-out or leave-one-subject-out) and ensure all preprocessing steps are applied independently to training and test sets [44] [45]. |
| Experimental Design | The cognitive states of interest are not robustly distinguished by brain activity patterns. | Pilot your task behaviorally; ensure conditions are perceptually or cognitively distinct. |
Q: Should I use a univariate GLM or MVPA for my study?
A: The choice depends on your research question, as these methods are complementary [44] [45].
- Use Mass-Univariate GLM: When your goal is to localize which specific brain regions are significantly "activated" by a task or condition compared to a baseline. It answers "Where is the effect?" [44] [45].
- Use MVPA: When your goal is to test whether distributed patterns of brain activity, often across multiple voxels or regions, contain information that can discriminate between experimental conditions. It answers "What information is represented?" and is generally more sensitive to distributed representations [44] [45].
- Searchlight Analysis: This MVPA technique offers a middle ground, providing a good balance between sensitivity and spatial localizability by moving a small "searchlight" across the brain to perform multivariate classification at each location [45].
Neural Signatures & Individual Differences
Q: How can I create and validate a neural signature that predicts a behavioral trait?
A: Building a predictive neural signature involves a rigorous, multi-step process to ensure it is valid and generalizable.
- Step 1: Define the Signature. Use a multivariate model (e.g., SVM, LASSO regression) trained on brain activity patterns (features) to predict a behavioral measure (target). For example, a study predicted a target's self-reported emotional intent from an observer's distributed brain activity pattern [46].
- Step 2: Internal Validation. Always use cross-validation (e.g., leave-one-subject-out) to assess performance on held-out data from the same study sample. This controls for overfitting [46].
- Step 3: External Validation. Test the signature's predictive power on a completely new, independent dataset. This is the gold standard for establishing a signature's robustness and utility [42] [46].
- Critical Consideration: Be aware that individual differences can be confounded by anatomical misalignment or non-neural physiological factors (e.g., vascular health). Using functionally-informed alignment and collecting large samples are key to mitigating these issues [42].
Q: We found a brain region that shows a strong group-level effect, but it does not correlate with individual behavior. Why?
A: This is a common and important finding. A region's involvement in a cognitive function at the group level does not automatically mean that its inter-individual variability explains behavioral differences [43].
- Explanation: A large-scale study on episodic memory encoding found that while many regions (e.g., lateral occipital cortex) showed a classic "subsequent memory effect" at the group level, only a subset of these regions (e.g., hippocampus, orbitofrontal cortex, posterior cingulate cortex) had activity levels that accounted for individual variability in memory performance [43].
- Implication: The neural mechanisms supporting a function on average may differ from those that determine how well an individual performs that function. Always directly test brain-behavior correlations for inferences about individual differences [43].
Experimental Protocols & Methodologies
Protocol 1: Standard MVPA Analysis Workflow
This protocol outlines the core steps for a typical MVPA study, from data preparation to statistical inference [44] [45].
- Data Preparation & Preprocessing: Standard fMRI preprocessing (motion correction, slice-timing correction, normalization). Critically, spatial smoothing should be minimized or omitted, as it can blur the fine-grained spatial patterns that MVPA seeks to detect.
- Feature Construction/Selection: For each trial or time point, create a feature vector representing the brain activity pattern. This can be the activity of all voxels within a predefined region of interest (ROI) or across the whole brain. Feature selection can be applied to reduce dimensionality.
- Label Assignment: Assign a class label (e.g., "Face" or "House") to each feature vector based on the experimental condition.
- Classifier Training & Testing with Cross-Validation:
- Split the data into k-folds.
- For each fold, train a classifier (e.g., Linear SVM) on the data from k-1 folds.
- Test the trained classifier on the held-out fold to obtain a prediction.
- Repeat until all folds have been used as the test set.
- Performance Evaluation & Statistical Testing: Calculate the average classification accuracy across all folds. Compare this accuracy to chance level (e.g., 50% for two classes) using a binomial test or permutation testing to establish statistical significance.
MVPA Analysis Workflow
Protocol 2: Establishing a Neural Signature for Individual Differences
This protocol describes the steps for building a neural signature predictive of a continuous behavioral trait, a common goal in individual differences research [43] [46].
- Define Target Behavior: Precisely define and measure the behavioral variable of interest (e.g., empathic accuracy, memory performance).
- Acquire and Preprocess fMRI Data: Use a task that robustly engages the neural systems related to the behavior. Apply preprocessing with advanced inter-subject alignment (e.g., MSM, hyperalignment).
- Extract Neural Features: Create whole-brain maps of parameter estimates (e.g., contrast maps from a GLM) for each subject.
- Train a Predictive Model: Use a regression model with regularization (e.g., LASSO-PCR) to predict the behavioral score from the neural features. Employ leave-one-subject-out cross-validation to avoid overfitting.
- Validate the Signature: Critically, test the signature's predictive power on a completely independent, held-out sample of participants to demonstrate generalizability.
The Scientist's Toolkit
Research Reagent Solutions
Table: Essential Components for MVPA and Neural Signature Research
| Item | Function & Application | Key Considerations |
|---|---|---|
| MVPA Software Toolboxes | Provides high-level functions for classification, regression, cross-validation, and searchlight analysis. | MVPA-Light [45]: A self-contained, fast MATLAB toolbox with native implementations of classifiers. Other options: PyMVPA (Python), The Decoding Toolbox (TDD), LIBSVM/LIBLINEAR interfaces [44] [45]. |
| Advanced Alignment Tools | Improves functional correspondence across subjects for individual differences studies. | Multimodal Surface Matching (MSM) [42]: Aligns cortical surfaces using anatomical and functional data. Hyperalignment [42]: Projects brains into a common model-based representational space. |
| Linear Classifiers | The standard choice for many fMRI-MVPA studies due to their robustness in high-dimensional spaces. | Support Vector Machine (SVM) [44]: Maximizes the margin between classes. Linear Discriminant Analysis (LDA) [45]: Finds a linear combination of features that separates classes. |
| Cross-Validation Scheme | Provides a realistic estimate of model performance and controls for overfitting. | Leave-One-Subject-Out (LOSO): Essential for ensuring that the model generalizes to new individuals, a cornerstone of individual differences research [46]. |
| Standardized Localizer Tasks | Efficiently and reliably identifies subject-specific functional regions of interest. | Why/How Task: Localizes regions for mental state attribution (Theory of Mind) [47]. False-Belief Localizer: The standard for identifying the Theory of Mind network [47]. |
| (3-Chloro-quinoxalin-2-yl)-isopropyl-amine | (3-Chloro-quinoxalin-2-yl)-isopropyl-amine, CAS:1234370-93-4, MF:C11H12ClN3, MW:221.688 | Chemical Reagent |
| Isodiazinon | Isodiazinon|CAS 82463-42-1|For Research | Isodiazinon is a diazinon isomer for environmental fate and toxicity studies. For research use only. Not for human or veterinary use. |
Neural Signature Validation Pipeline
Frequently Asked Questions (FAQs)
Q1: What is the primary limitation of conventional TMS targeting that precision neuromodulation aims to solve? Conventional TMS methods, such as the "5-cm rule" or motor hotspot localization, largely overlook inter-individual variations in brain structure and functional connectivity. This failure to account for individual differences in cortical morphology and brain network organization leads to considerable variability in treatment responses and limits overall clinical efficacy [48].
Q2: How do fMRI and DTI each contribute to personalized TMS targeting? fMRI and DTI provide complementary information for target identification:
- fMRI: Provides high spatial resolution for mapping individual functional brain networks and identifying pathological circuits. For example, in depression, the functional connectivity between the dorsolateral prefrontal cortex (DLPFC) and the subgenual anterior cingulate cortex (sgACC) can predict TMS treatment response [48].
- DTI: Visualizes and quantifies the integrity and trajectories of white matter fibers, elucidating the structural underpinnings of functional connectivity and helping to optimize stimulation pathways [48].
Q3: What is a closed-loop TMS system and what advantage does it offer? A closed-loop TMS system continuously monitors a biomarker representing the brain's state (e.g., via EEG or real-time fMRI) and uses this feedback to dynamically adjust stimulation parameters in real-time. This approach aims to drive the brain from its current state toward a desired state, overcoming the limitations of static, open-loop paradigms and accounting for both inter- and intra-individual variability [49].
Q4: What are common technical challenges when integrating real-time fMRI with TMS? Key challenges include managing the timing between stimulation and data acquisition, selecting the appropriate fMRI context (task-based vs. resting-state), accounting for inherent brain oscillations, defining the dose-response function, and selecting the optimal algorithm for personalizing stimulation parameters based on the feedback signal [49].
Q5: Can you provide an example of a highly successful precision TMS protocol? Stanford Neuromodulation Therapy (SNT) is a pioneering protocol. It uses resting-state fMRI to identify the specific spot in a patient's DLPFC that shows the strongest negative functional correlation with the sgACC. It then applies an accelerated, high-dose intermittent TBS pattern. This individualized approach achieved a remission rate of nearly 80% in patients with treatment-resistant depression in a controlled trial [48].
Troubleshooting Guides
Issue 1: High Inter-Subject Variability in TMS Response
Symptoms: Significant differences in clinical or neurophysiological outcomes between subjects receiving identical TMS stimulation protocols.
Potential Causes & Solutions:
| Step | Problem Area | Diagnostic Check | Solution |
|---|---|---|---|
| 1 | Target Identification | Verify that fMRI-guided targeting (e.g., DLPFC-sgACC anticorrelation) was performed using a validated, standardized processing pipeline. | Implement an individualized targeting workflow using resting-state fMRI to define the stimulation target based on each subject's unique functional connectivity profile [48]. |
| 2 | Skull & Tissue Anatomy | Check if individual anatomical data (e.g., T1-weighted MRI) was used for electric field modeling. | Use finite element method (FEM) modeling based on the subject's own MRI to simulate and optimize the electric field distribution for their specific brain anatomy [48]. |
| 3 | Network State | Assess if the subject's brain state at the time of stimulation was accounted for, as it can dynamically influence response. | Move towards a closed-loop system that uses real-time neuroimaging (EEG/fMRI) to adjust stimulation parameters based on the instantaneous brain state [49]. |
Issue 2: Suboptimal Integration of Multimodal Imaging Data for Targeting
Symptoms: Inconsistent target locations when using different imaging modalities (e.g., fMRI vs. DTI); difficulty fusing data into a single neuronavigation platform.
Potential Causes & Solutions:
| Step | Problem Area | Diagnostic Check | Solution |
|---|---|---|---|
| 1 | Data Co-registration | Confirm the accuracy of co-registration between the subject's fMRI, DTI, and anatomical scans. | Ensure use of high-resolution anatomical scans as the registration baseline and validate alignment precision within the neuronavigation software. |
| 2 | Cross-Modal Fusion | Check if the functional target (fMRI) is structurally connected via the white matter pathways identified by DTI. | Adopt an integrative framework where fMRI identifies the pathological network node, and DTI ensures the stimulation site is optimally connected to that network [48]. |
| 3 | Model Generalizability | Evaluate if the AI/ML model used for target prediction was trained on a dataset with sufficient demographic and clinical diversity. | Utilize machine learning models that are robust to scanner and population differences, or fine-tune models with local data to improve generalizability [48]. |
Experimental Protocols & Data
Key Experimental Protocol: An Integrative Precision TMS Workflow
The following diagram illustrates a step-by-step framework for precision TMS, from diagnosis to closed-loop optimization [48].
Table 1: Clinical Efficacy of Conventional vs. Precision TMS Protocols for Depression
| Protocol | Targeting Method | Key Stimulation Parameters | Approximate Response Rate | Remission Rate | Key References |
|---|---|---|---|---|---|
| Conventional rTMS | Scalp-based "5-cm rule" | 10 Hz, 120% MT, ~3000 pulses/session, 6 weeks | ~50% | ~33% | [50] |
| Precision SNT | fMRI-guided (DLPFC-sgACC) | iTBS, 90% MT, ~1800 pulses/session, 10 sessions/day for 5 days | Not specified | ~80% | [48] |
Table 2: Technical Specifications for Imaging Modalities in Precision TMS
| Modality | Primary Role in TMS | Key Metric for Targeting | Spatial Resolution | Temporal Resolution | Key Contributions |
|---|---|---|---|---|---|
| fMRI | Functional target identification | Functional connectivity (e.g., DLPFC-sgACC anticorrelation) | High (mm) | Low (seconds) | Predicts therapeutic response; identifies pathological circuits [48] |
| DTI | Structural pathway optimization | Fractional Anisotropy (FA), Tractography | High (mm) | N/A | Guides modulation of structural pathways; informs electric field modeling [48] |
| EEG/MEG | Real-time state assessment | Brain oscillations (e.g., Alpha, Theta power) | Low (cm) | High (milliseconds) | Enables closed-loop control by providing real-time feedback on brain state [48] [49] |
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Resources for Precision TMS Research
| Item | Category | Function in Research | Example/Note |
|---|---|---|---|
| 3T MRI Scanner | Imaging Equipment | Acquires high-resolution structural (T1, T2), functional (fMRI), and diffusion (DTI) data. | Essential for obtaining individual-level data for target identification and electric field modeling. |
| Neuronavigation System | Software/Hardware | Co-registers individual MRI data with subject's head to guide precise TMS coil placement. | Ensures accurate targeting of the computationally derived brain location. |
| TMS Stimulator with cTBS/iTBS | Stimulation Equipment | Delivers patterned repetitive magnetic pulses to the targeted cortical area. | Protocols like iTBS allow for efficient, shortened treatment sessions [48]. |
| Computational Modeling Software | Software | Creates finite element models (FEM) from individual MRIs to simulate electric field distributions. | Optimizes stimulation dose by predicting current flow in the individual's brain anatomy [48]. |
| Machine Learning Algorithms | Analytical Tool | Analyzes large-scale neuroimaging and clinical data to predict optimal stimulation targets and treatment response. | Includes support vector machines (SVM), random forests, and deep learning models [48]. |
| Real-time fMRI/EEG Setup | Feedback System | Measures instantaneous brain activity during stimulation for closed-loop control. | Allows for dynamic adjustment of stimulation parameters based on the detected brain state [49]. |
| 2-Amino-1-(3,4-dihydroxyphenyl)ethanone | 2-Amino-1-(3,4-dihydroxyphenyl)ethanone, CAS:499-61-6, MF:C8H9NO3, MW:167.16 g/mol | Chemical Reagent | Bench Chemicals |
| Lithium, (dimethylphenylsilyl)- | Lithium, (dimethylphenylsilyl)-, CAS:3839-31-4, MF:C8H11LiSi, MW:142.2 g/mol | Chemical Reagent | Bench Chemicals |
Pipeline Precision: Systematic Optimization of Preprocessing and Computational Strategies
Troubleshooting Guides
Spatial Smoothing Implementation
Issue: Users expect fMRIPrep to perform spatial smoothing automatically, but outputs lack this step.
Explanation: fMRIPrep is designed as an analysis-agnostic tool that performs minimal preprocessing and intentionally omits spatial smoothing. This step is highly dependent on the specific statistical analysis and hypotheses of your study [51] [52]. Applying an inappropriate kernel size could reduce statistical power or introduce spurious results in downstream analysis.
Solution: Perform spatial smoothing as the first step of your first-level analysis using your preferred statistical package (SPM, FSL, AFNI). Alternatively, apply smoothing directly to the *space-MNI152NLin2009cAsym_desc-preproc_bold.nii.gz files output by fMRIPrep [51].
Exception: If using ICA-AROMA for automated noise removal, the *desc-smoothAROMAnonaggr_bold.nii.gz outputs have already undergone smoothing with the SUSAN filter and should not be smoothed again [51].
Temporal Filtering Configuration
Issue: Preprocessed BOLD time series contain unwanted low-frequency drift or high-frequency noise.
Explanation: fMRIPrep does not apply temporal filters to the main preprocessed BOLD outputs by default. The pipeline calculates noise components but leaves the application of temporal filters to the user's analysis stage [51] [53].
Solution:
- High-pass filtering: Implement during first-level model specification in your analysis software
- Band-pass filtering (for resting-state fMRI): Apply using specialized tools (e.g.,
fslmaths,3dTproject) - Confound regression: Use the comprehensive confounds tables generated by fMRIPrep (
*_desc-confounds_timeseries.tsv) alongside temporal filtering
Motion Correction Diagnostics
Issue: Suspicious motion parameters or poor correction in preprocessed data.
Explanation: fMRIPrep performs head-motion correction (HMC) using FSL's mcflirt and generates extensive motion-related diagnostics [53] [52]. The quality of correction depends on data quality and acquisition parameters.
Troubleshooting Steps:
- Check motion parameters: Review the
*_desc-confounds_timeseries.tsvfile for motion parameters (transx, transy, transz, rotx, roty, rotz) - Assess framewise displacement: Use the
framewise_displacementcolumn in confounds file to identify high-motion volumes - Inspect reports: Carefully examine the visual HTML reports for each subject to identify poor motion correction
- Consider data exclusion: For framewise displacement > 0.5mm, consider excluding volumes or the entire run if excessive motion is present
Frequently Asked Questions (FAQs)
Q1: Why does fMRIPrep not include spatial smoothing and temporal filtering by default?
A1: fMRIPrep follows a "glass box" philosophy and aims to be analysis-agnostic [52]. These steps are highly specific to your research question and analysis method. Leaving them to the user ensures flexibility and prevents inappropriate processing that could compromise different analysis approaches.
Q2: What motion-related outputs does fMRIPrep provide?
A2: fMRIPrep generates comprehensive motion-related data [53]:
- Motion parameters: 6 rigid-body parameters (3 translation, 3 rotation)
- Framewise displacement: A scalar measure of volume-to-volume motion [52]
- DVARS: Rate of change of BOLD signal across volumes
- Motion-corrected BOLD series: In native and standard spaces
- Transform files: For head-motion correction
Q3: How should I handle slice-timing correction in my workflow?
A3: Slice-timing correction is available in current fMRIPrep versions [51]. For older versions, you needed to perform slice-timing correction separately (using SPM, FSL, or AFNI) before running fMRIPrep. Check your fMRIPrep version documentation to confirm implementation.
Q4: What are the computational requirements for running fMRIPrep with these preprocessing steps?
A4: Table: Computational Requirements for fMRIPrep Processing
| Resource Type | Minimum Recommended | Optimal Performance |
|---|---|---|
| CPU Cores | 4 cores | 8-16 cores |
| Memory (RAM) | 8 GB | 16+ GB |
| Processing Time | ~2 hours/subject (with 4 cores) | ~1 hour/subject (with 16 cores) |
| Disk Space | 20-40 GB/subject | 40+ GB/subject (with full outputs) |
These requirements are for fMRIPrep itself; additional resources are needed for subsequent smoothing and filtering steps [54].
Experimental Protocols
Protocol for Validating Motion Correction
Purpose: To verify the quality of motion correction in fMRIPrep outputs.
Steps:
- Run fMRIPrep on your dataset with the
--output-spaces MNI152NLin2009cAsymflag - Extract mean framewise displacement (FD) values from confounds files
- Set exclusion criteria (e.g., mean FD > 0.2mm or >20% volumes with FD > 0.5mm)
- Inspect visual reports for alignment quality between BOLD reference and T1w images
- Correlate motion parameters with task design to identify task-related motion
Protocol for Spatial Smoothing Optimization
Purpose: To determine the optimal smoothing kernel for your analysis.
Steps:
- Extract preprocessed BOLD data from fMRIPrep outputs (
*_desc-preproc_bold.nii.gz) - Apply different smoothing kernels (e.g., 4mm, 6mm, 8mm FWHM) to separate copies
- Run identical first-level analyses on each smoothed dataset
- Compare signal-to-noise ratio and activation patterns
- Select kernel size that balances sensitivity and specificity for your study
Workflow Visualization
fMRIPrep Preprocessing and User-Defined Steps
The Scientist's Toolkit
Table: Essential Software Tools for fMRI Preprocessing and Analysis
| Tool Name | Function in Preprocessing | Application in Analysis |
|---|---|---|
| fMRIPrep | Robust, automated preprocessing pipeline; generates motion-corrected, normalized data | Provides analysis-ready BOLD data and confounds for statistical analysis [55] [52] |
| FSL | Motion correction (mcflirt), ICA-AROMA for noise removal |
Spatial smoothing (susann), temporal filtering, GLM analysis (FEAT) [52] |
| SPM | Slice-timing correction, spatial smoothing | First- and second-level GLM analysis, DCM for effective connectivity |
| AFNI | Slice-timing correction (3dTshift), spatial smoothing (3dBlurInMask) |
Generalized linear modeling (3dDeconvolve), cluster-based thresholding |
| ANTs | Spatial normalization to template space | Advanced registration, region-of-interest analysis |
| FreeSurfer | Cortical surface reconstruction, segmentation | Surface-based analysis, ROI definition from atlases |
| MRIQC | Quality assessment of raw and processed data | Identifying exclusion criteria, dataset quality control [56] [57] |
| 4-[3-(Benzyloxy)phenyl]phenylacetic acid | 4-[3-(Benzyloxy)phenyl]phenylacetic Acid | High-purity 4-[3-(Benzyloxy)phenyl]phenylacetic acid for research. Explore its potential as a synthetic intermediate. For Research Use Only. Not for human or veterinary use. |
| Trihexyl phosphite | Trihexyl phosphite, CAS:6095-42-7, MF:C18H39O3P, MW:334.5 g/mol | Chemical Reagent |
Evaluating the Impact of Preprocessing Choices on Outcome Metrics and Statistical Power
Troubleshooting Guides & FAQs
FAQ: How do preprocessing choices affect my study's statistical power?
Answer: Preprocessing choices are not just technical steps; they directly influence your statistical power by affecting the signal-to-noise ratio in your data. Suboptimal preprocessing can introduce noise or artifacts that obscure true biological effects, increasing the likelihood of Type II errors (false negatives) where you fail to detect real effects [58]. For instance, inadequate motion correction can substantially reduce the quality of brain activation maps, making it difficult to detect true task-related activations even when they exist [58]. Furthermore, failing to account for scanner effects across multi-site studies can introduce non-biological variance that reduces your ability to detect genuine group differences or treatment effects [59].
FAQ: What is the minimum number of participants and trials needed for reliable error-related brain activity measures?
Answer: The required number of participants and trials depends on your imaging modality and the specific neural signals you're investigating. The following table summarizes evidence-based recommendations for error-processing studies:
Table: Stable Sample and Trial Size Estimates for Error-Related Brain Activity
| Modality | Measure | Minimum Participants | Minimum Error Trials | Notes | Source |
|---|---|---|---|---|---|
| ERP | ERN/Ne & Pe | ~30 | 6-8 | Flanker and Go/NoGo tasks | [60] |
| fMRI | BOLD (Error-related) | ~40 | 6-8 | Event-related designs | [60] |
| fMRI | BOLD (General) | 12+ | 20-30 | For 0.5% signal change, α=0.05, block design | [60] |
FAQ: Which harmonization methods effectively remove scanner effects in multi-site brain MRI radiomics?
Answer: Scanner effects from different magnetic field strengths (e.g., 1.5T vs. 3T) and acquisition protocols significantly challenge reproducibility. A combination of methods is most effective:
- ComBat Harmonization: This method, applied to already extracted radiomic features, is considered "essential and vital" for removing scanner effects while preserving biological information [59]. It was originally developed for microarray data and has been successfully adapted for neuroimaging.
- Intensity Normalization: Methods like Z-score, Nyúl, WhiteStripe, and GMM-based normalization work on the MRI images themselves before feature extraction. While they alone cannot fully remove scanner effects at the feature level, they create more comparable images and improve the robustness of subsequent ComBat harmonization [59].
- Recommended Protocol: The most robust pipeline involves first applying intensity normalization to the images, then extracting features, and finally using ComBat on the feature set to harmonize across scanners [59].
FAQ: My fMRI preprocessing pipeline failed. What are the first things I should check?
Answer: Pipeline failures are often due to input data issues. Before investigating complex algorithm parameters, check these fundamentals:
- Data Format: Ensure your files are in a compatible format. Most modern neuroimaging software (like fMRIPrep) requires NIFTI files compressed with
.nii.gzextension. Uncompressed.niifiles can cause crashes [61]. - BIDS Validation: If using a BIDS-organized dataset, run a BIDS validator. Missing required files (like
dataset_description.json) or incorrect directory structure (e.g., session labels in filenames not matching folder paths) are common causes of failure [61]. - Visual Inspection: Always open your raw data in a viewer like FSLEYES. Check for extreme artifacts, obvious registration problems, or unusually blurry images that might indicate a deeper data quality issue [61] [62].
Experimental Protocols
Protocol: Assessing the Impact of Preprocessing on fMRI Power and Reproducibility
This protocol uses the NPAIRS (Nonparametric Prediction, Activation, Influence, and Reproducibility reSampling) framework to evaluate pipeline choices [58].
Objective: To quantify how different preprocessing steps affect the reproducibility and predictive accuracy of fMRI results.
Materials:
- fMRI dataset (e.g., from a Go/NoGo or Trail-Making Test task)
- Computing environment with fMRI analysis software (SPM, FSL, AFNI)
Methodology:
- Data Acquisition: Acquire or obtain a task-based fMRI dataset. The Trail-Making Test adaptation is suitable as it is a clinically relevant task [58].
- Define Pipeline Variations: Create multiple preprocessing pipelines that systematically vary the inclusion of key steps:
- Motion Correction (MC): On/Off
- Motion Parameter Regression (MPR): On/Off
- Physiological Noise Correction (PNC): On/Off
- Temporal Detrending: On/Off
- Spatial Smoothing: Varying kernel sizes (e.g., 4mm, 6mm, 8mm FWHM)
- NPAIRS Analysis: For each pipeline, use cross-validation to generate two key metrics [58]:
- Spatial Reproducibility: Measures the global similarity of statistical parametric maps across splits.
- Predictive Accuracy: Assesses how well a model trained on one data split can predict the experimental condition in another.
- Statistical Comparison: Use non-parametric Friedman rank tests to compare the performance (reproducibility and accuracy) across the different fixed pipelines. For a more advanced analysis, optimize the pipeline on an individual-subject basis and compare to the fixed pipelines.
Expected Outcome: The analysis will reveal which preprocessing steps, or combinations thereof, significantly enhance the sensitivity and reliability of the fMRI data for your specific task and population.
Protocol: Optimizing Scan Parameters for Brain MRI Efficiency
Objective: To reduce MRI scan time without compromising diagnostic image quality by optimizing technical parameters [17].
Materials:
- 1.5T or 3T MRI Scanner
- Phantoms or patient cohorts
Methodology:
- Baseline Scan: Perform a brain MRI scan (e.g., T2-weighted TSE axial) using the institution's standard protocol.
- Parameter Modification: Systematically modify the following parameters in subsequent scans:
- Field of View (FOV): Reduce from a standard value (e.g., 230mm) to a smaller one (e.g., 217mm).
- FOV Phase: Adjust the percentage (e.g., from 90% to 93.88%).
- Phase Oversampling: Increase the percentage (e.g., from 0% to 13.96%).
- Data Collection: Record the scan time and assess image quality for each parameter set. Use quantitative measures (e.g., Signal-to-Noise Ratio) and qualitative radiologist ratings.
- Statistical Analysis: Use ANOVA to test the significance of each parameter's effect on scan time. A study found FOV phase and phase oversampling to have a highly significant impact (p < 0.001), while FOV and slice thickness did not directly affect time [17].
Expected Outcome: Identification of a modified protocol that significantly reduces scan time (e.g., from 3.47 minutes to 2.18 minutes as demonstrated in one study) while maintaining sufficient image quality for diagnosis [17].
Workflow and Signaling Pathways
Brain MRI Preprocessing & Harmonization Workflow
fMRI Preprocessing Pipeline for Power Optimization
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Tools for Brain Imaging Parameter Optimization
| Tool / Method | Function | Application Context | Key Consideration |
|---|---|---|---|
| ComBat Harmonization | Removes batch/scanner effects from extracted features. | Multi-site studies, pooling data from different MRI scanners. | Preserves biological variance while removing non-biological technical variance [59]. |
| Intensity Normalization (e.g., WhiteStripe) | Standardizes image intensity scales across subjects. | Brain MRI radiomics, especially when intensity values lack physical meaning. | Improves image comparability but not sufficient alone for feature-level harmonization [59]. |
| NPAIRS Framework | Provides data-driven metrics (reproducibility & prediction) to evaluate preprocessing pipelines. | Optimizing fMRI preprocessing steps for a specific task or population. | Allows for empirical comparison of pipeline performance without ground truth [58]. |
| fMRIPrep | Automated, robust preprocessing pipeline for fMRI data. | Standardizing initial fMRI preprocessing steps across a lab or study. | Requires BIDS-formatted data; check logs for error details if pipeline fails [61]. |
| G*Power / PASS | Statistical power analysis software to calculate required sample size. | Planning studies to ensure adequate power to detect expected effects. | Requires input of expected effect size, alpha, and desired power [63] [64]. |
| Rigid-Body Motion Correction | Realigns fMRI volumes to correct for head motion. | Virtually all task-based fMRI studies. | Corrects for 6 parameters (3 translation, 3 rotation); largest source of error in fMRI if not addressed [62]. |
Frequently Asked Questions (FAQs)
Q1: My brain imaging algorithm is running slower than expected on the GPU. How can I determine if the bottleneck is computation or memory? A1: The first step is to profile your application using tools like NVIDIA Nsight Systems/Compute. Following this, calculate your kernel's Arithmetic Intensity (AI). AI is the ratio of total FLOPs (Floating-Point Operations) to total bytes accessed from global memory [65]. Compare this value to your GPU's ridge point (e.g., ~13 FLOPs/byte for an A100 GPU). If your AI is below this point, your kernel is memory-bound; if it is above, it is compute-bound [65]. This diagnosis directs you to the appropriate optimization strategies outlined in the guides below.
Q2: I am working with high-resolution 3D brain images that exceed my GPU's VRAM. What strategies can I use? A2: For memory-bound algorithms dealing with large datasets like high-resolution MRI, consider a multi-pass approach [66]. This involves processing the data in smaller, self-contained chunks that fit into the GPU's fast memory resources (shared memory, L1/L2 cache). Additionally, you can reorganize data into self-contained structures to minimize redundant transfers and leverage memory resources whose cache performance is optimized for your specific access patterns (e.g., using texture memory for spatial data with locality) [66] [67].
Q3: My kernel runs out of registers, limiting the number of active threads. How can I reduce register pressure? A3: High register usage per thread can severely limit the number of threads that can run concurrently on a Streaming Multiprocessor (SM), reducing GPU utilization [66]. To optimize a compute-bound kernel, you can:
- Reuse variables via shared memory: Instead of holding many intermediate values in private registers, store them in shared memory for the entire thread block to access [66].
- Increase thread workloads: Assign more data to each thread, which can amortize the cost of register usage over more computations [66].
- Use compiler flags: The CUDA compiler provides flags to control the maximum number of registers used per thread.
Troubleshooting Guides
Optimization Guide for Memory-Bound Kernels
Memory-bound operations are limited by the speed of data transfer from global memory. The goal is to reduce latency and maximize bandwidth [66] [65].
- Symptoms: Low arithmetic intensity, low compute unit utilization, performance is highly sensitive to memory access patterns.
- Diagnosis: Profiling shows long memory transaction times and low FLOPs/sec. AI is below the hardware's ridge point.
- Solutions:
- Leverage Fast Memory Resources: Utilize shared memory as a programmer-managed cache to reuse data within a thread block [66] [65]. For spatial data with locality, consider using texture or constant memory for their optimized caching behavior [66].
- Ensure Coalesced Memory Access: Organize memory accesses so that threads in a warp access contiguous, aligned segments of global memory. This allows the GPU to combine multiple memory transactions into a single, large, efficient operation [68].
- Avoid Shared Memory Bank Conflicts: Structure data in shared memory so that multiple threads accessing it simultaneously do not target the same memory bank, which would cause serialized access [66].
Optimization Guide for Compute-Bound Kernels
Compute-bound operations are limited by the GPU's arithmetic logic units (ALUs). The goal is to maximize computational throughput [66].
- Symptoms: High arithmetic intensity, high compute unit utilization, performance is limited by instruction throughput.
- Diagnosis: Profiling shows high FLOPs/sec. AI is above the hardware's ridge point.
- Solutions:
- Maximize Thread Occupancy for a Single Block: For compute-bound algorithms, maximizing the number of threads in a single block per Multiprocessor (MP) can be more effective than running multiple smaller blocks, as it reduces resource overhead and maximizes data reuse within the SM [66].
- Increase Thread Workloads: Heavier workloads per thread can help hide instruction latency and improve the ratio of computation to memory operations [66].
- Use Mixed-Precision Operations: Leverage Tensor Cores or FP16 operations where numerically stable for your algorithm. This can double the throughput of floating-point operations and reduce memory footprint [69].
- Reduce Register Usage: As outlined in FAQ #3, reducing register pressure via shared memory or compiler directives allows more threads to be active concurrently, increasing parallelism [66].
Experimental Protocols & Data
Protocol: Optimizing a 3D Image Registration Algorithm
This protocol is based on the optimization of a 3D unbiased nonlinear image registration technique, which achieved a 129x speedup over a CPU implementation [66] [67].
1. Problem Decomposition:
- Map the registration problem to a 3D grid of threads, where each thread is responsible for computing the similarity metric and transformation for a single voxel or a small tile of voxels [66].
2. Memory-Bound Phase Optimization:
- The algorithm first loads the reference and floating image patches from global memory.
- Key Technique: Employ a multi-pass approach with data tiling. Sub-regions of the 3D images are loaded into the shared memory of each thread block to enable redundant data reuse across threads calculating neighboring voxels [66].
- Memory Selection: Use texture memory for the image data if the access pattern is spatially coherent, as the texture cache is optimized for 2D/3D locality [66].
3. Compute-Bound Phase Optimization:
- The core computation involves iterative updates to the transformation field based on the similarity metric.
- Key Technique: Reduce registers by storing intermediate transformation values in shared memory. Configure the kernel to use a single, large thread block per Multiprocessor to maximize resource allocation to computation and minimize scheduling overhead [66].
- Heavier thread workloads are achieved by having each thread handle a small 3D tile (e.g., 2x2x2) instead of a single voxel.
4. Validation:
- Compare the output transformation field and the final registered image against a validated CPU implementation to ensure numerical accuracy is maintained.
Quantitative Data for Resource Planning
Table 1: Typical GPU VRAM Requirements for Data Science Workloads (Including Neuroimaging) [69]
| Application Domain | Typical VRAM Requirements | Example Models / Tasks |
|---|---|---|
| Machine Learning | 8 - 12 GB | Scikit-learn models, linear models, clustering |
| Deep Learning | 12 - 24 GB | Convolutional Neural Networks (CNNs), Recurrent Neural Networks (RNNs) |
| Computer Vision | 16 - 32 GB | Object detection (YOLO, R-CNN), semantic segmentation, 3D reconstruction |
| Natural Language Processing | 24 - 48 GB | BERT, GPT-2, large transformer models |
| Advanced AI Research | 48 - 80+ GB | GPT-3 scale models, multi-modal architectures, large-scale reinforcement learning |
Table 2: Performance Improvement with Adequate VRAM and Optimization [66] [69]
| Algorithm / Workload | Unoptimized vs. Optimized GPU Speedup | Peak GPU vs. CPU Speedup |
|---|---|---|
| 3D Unbiased Nonlinear Image Registration | Up to 6x faster than unoptimized GPU | 129x [66] |
| Non-local Means Surface Denoising | Up to 6x faster than unoptimized GPU | 93x [66] |
| General Data Science Workloads | Not Applicable | 300-500% performance improvement with adequate VRAM [69] |
Workflow and Relationship Visualizations
GPU Optimization Decision Pathway
GPU Memory and Compute Hierarchy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for GPU-Accelerated Brain Imaging Research
| Tool / Resource | Function / Role | Relevance to Brain Imaging Parameter Optimization |
|---|---|---|
| NVIDIA Nsight Systems | System-wide performance profiler. | Identifies bottlenecks in the entire processing pipeline, from data loading to kernel execution, crucial for optimizing large-scale population studies [68]. |
| NVIDIA Nsight Compute | Detailed kernel profiler. | Provides granular analysis of GPU kernel performance, including memory access patterns and compute throughput, essential for tuning compute- and memory-bound neuroimaging algorithms [68]. |
| CUDA C++ Programming Guide | Official reference for CUDA programming. | The foundational document for understanding GPU architecture, parallel programming models, and API specifications [68]. |
| BrainSuite | Automated MRI processing toolkit. | Provides a suite of tools for cortical surface extraction, volumetric registration, and diffusion data processing, which can be accelerated and optimized using GPU strategies [70] [71]. |
| LONI Pipeline | Workflow environment for neuroimaging. | Allows researchers to create and execute complex processing workflows that can integrate GPU-accelerated tools, helping to manage the analysis of individual differences across large datasets [70]. |
| Precision fMRI Datasets | High-sampling, individual-specific fMRI data. | Enables the creation of highly reliable functional brain maps for individual participants, which are both the target of optimization and a requirement for studying individual differences in brain function [26]. |
Framework for Automated and Adaptive Pipeline Optimization
Troubleshooting Guides
How do I resolve a pipeline execution timeout?
Issue Description: The pipeline execution is interrupted because it exceeds the maximum allowed runtime. This is common in workflows that process large neuroimaging datasets, such as multimodal MRI analyses [72] [73].
Symptoms:
- Pipeline run fails with a "Pipeline execution timed-out" error message [72].
- Execution logs show the process stopped abruptly after a specific duration (e.g., 15 minutes) [72] [73].
Solutions:
- Increase Timeout Limit: Adjust the pipeline's trigger configuration to allow for a longer execution time, but be mindful of system-wide maximum limits [72].
- Optimize Long-Running Steps: Identify the specific step causing the delay (e.g., an external database query or a large file processing task) and adjust the timeout setting for that individual connector or request [72].
- Restructure the Pipeline: For pipelines processing large volumes of data, split the workflow into smaller, sequential batches using pagination to avoid single, long-running executions [72].
Why is my pipeline failing with an Out of Memory (OOM) error?
Issue Description: The pipeline is terminated because it consumes more memory than allocated. This frequently occurs when handling high-dimensional data from sources like 7T MRI scanners or when processing large files without sufficient memory management [74] [72].
Symptoms:
- Execution is aborted with an "Out of Memory" or "OOM" error [72].
- In cloud environments, the pipeline container may restart unexpectedly [72].
Solutions:
- Identify the Cause: Use monitoring tools to analyze logs and pinpoint the step where memory usage spikes. This is often a data transformation or an operation on a large dataset [72].
- Optimize Data Flow: Implement pagination to reduce the data volume processed in a single batch. For complex flows, split the pipeline into primary and secondary pipelines to distribute the memory load [72].
- Adjust Deployment Settings: After restructuring, test the pipeline. If the error persists, increase the allocated memory (pipeline size) for the deployment [72].
How can I fix a pipeline that fails due to connection issues?
Issue Description: The pipeline cannot communicate with an external service, database, or API. This can disrupt workflows that rely on external data sources or computational resources [72].
Symptoms:
- Error logs show messages like "Connection is not available," "Connection timed out," or authentication failures [72].
- The pipeline fails on a specific step designed to interact with an external system [73].
Solutions:
- Verify Service Status: Confirm that the external server or service is available and running.
- Check Credentials and Endpoints: Ensure all endpoints, URLs, and authentication tokens (e.g., for databases or REST APIs) are correctly configured and up-to-date [72] [73].
- Review Network Configuration: For self-hosted agents, verify that the network firewall and security groups allow outbound connections to the required services [73].
What should I do if my pipeline fails on a command-line task?
Issue Description: A task executing a script or command (e.g., for data preprocessing) fails, halting the pipeline. This is common in neuroimaging pipelines that call external software tools for image analysis [73].
Symptoms:
- The log for a command-line task (e.g.,
cmd-line,script) shows a specific error code or message [73]. - The exact command executed by the task is visible in the logs and can be tested locally [73].
Solutions:
- Reproduce the Error Locally: Copy the failing command from the pipeline logs and run it in your local environment to diagnose the issue [73].
- Check File Paths and Dependencies: The build environment on the pipeline agent may have a different layout than your local machine. Verify that all necessary tools, libraries, and files are present and accessible in the agent's environment [73].
- Review Script Logic: Check for errors in the script itself, such as typos or incorrect logic [73].
Frequently Asked Questions (FAQs)
What are the most common root causes of pipeline failures?
Understanding the root cause is key to resolving pipeline issues, which are often signaled by superficial errors (proximal causes) [75]. The table below summarizes common root causes.
Table: Common Root Causes of Pipeline Failures
| Root Cause | Description | Example in a Research Context |
|---|---|---|
| Infrastructure Error | The underlying system lacks resources or hits a limit [75]. | Maxing out API call limits, running out of memory (OOM) when processing large neuroimaging files [75] [72]. |
| Configuration Error | Incorrect settings in the pipeline or its connections [72]. | An invalid endpoint for a service, incorrect file path for an input dataset, or a missing required parameter [72]. |
| Bug in Code | An error in the pipeline's logic or a custom script [75]. | A new version of a data transformation script contains a syntax error or logical flaw [75]. |
| User Error | Incorrect input or operation by a user [75]. | Entering the wrong schema name or an invalid parameter value when triggering the pipeline [75]. |
| Data Partner Issue | Failure or issue with an external data source [75]. | A vendor or collaborator fails to deliver expected neuroimaging data on schedule, causing the pipeline to fail [75]. |
| Permission Issue | The pipeline lacks authorization to access a resource [75] [73]. | The service account used by the pipeline does not have "read" permissions for a required cloud storage bucket containing subject data [73]. |
My model performs well on training data but generalizes poorly to new data. How can I improve robustness?
Poor generalization is a significant challenge in neuroimaging, especially with small, heterogeneous cohorts, as often encountered in individual differences research and rare disease studies [74] [76] [77].
Solutions:
- Increase Measurement Reliability: Optimize the reliability of both neural and behavioral measures. This can involve using better neuroimaging tasks, improving preprocessing, and ensuring higher-quality data, which directly increases the observable effect size and model robustness [76].
- Apply Data Augmentation: Use techniques like rotation, scaling, and noise injection to artificially expand your training dataset, helping the model learn more invariant features and reducing overfitting [77].
- Utilize Transfer Learning: Leverage models pre-trained on larger, public neuroimaging datasets. Fine-tuning these models on your specific, smaller cohort can significantly improve performance and generalization [77].
- Employ Cross-Validation: Use robust cross-validation strategies (e.g., leave-one-site-out) to evaluate model performance more accurately and ensure it is not biased by site-specific effects or data splits [76].
My dataset is small, which limits my model's performance. What optimization strategies can I use?
Small sample sizes are a major constraint in fields like neuroimaging research on individual differences and rare neurological diseases [74] [76]. While collecting more data is ideal, several optimization strategies can maximize the utility of existing data.
Solutions:
- Theoretical Matching: Carefully align your neuroimaging tasks with the specific behavioral or cognitive constructs you are investigating. A tighter match leads to stronger brain-behavior correlations and larger effect sizes, making better use of limited data [76].
- Feature Selection and Normalization: Implement subject-wise feature normalization to control for inter-individual variability. However, note that in very small cohorts, aggressive feature selection may have limited utility [74].
- Leverage Multimodal Data: Integrate complementary data types (e.g., combining structural, functional, and diffusion MRI) to provide a richer feature set for the model to learn from, potentially capturing synergistic effects that are not apparent in a single modality [74].
- Use Simpler Models: For very small cohorts, complex deep learning models are prone to overfitting. Simpler models or linear classifiers with appropriate regularization may yield more reliable and interpretable results [74] [77].
Diagnostic Protocols and Workflows
Step-by-Step Pipeline Failure Diagnosis
Follow this systematic workflow to identify the root cause of a pipeline failure.
Procedure:
- Gather Initial Information: Collect the execution key, the exact error message, and the timestamp from the pipeline run summary or logs [72] [73].
- Access Pipeline and Execution Logs: Open the pipeline configuration and the detailed execution logs side-by-side to compare what was supposed to happen with what actually occurred [72].
- Analyze Logs for Error Context: Scan the logs of the failing task. Look for error messages, stack traces, and clues about the point of failure. Configure verbose logs if the default logs are insufficient [73].
- Compare with a Successful Run: Identify a similar data input that was processed successfully. Compare the logs of the successful and failed executions to find the point of divergence in the data flow [72].
- Formulate a Hypothesis: Based on the evidence, determine the most likely root cause (e.g., a specific bad data input, a code bug in a transformation, or an infrastructure timeout) [75].
- Test Hypothesis and Implement Fix: This could involve correcting a configuration, fixing a script, adding data validation, or adjusting resource allocations. After implementing the fix, rerun the pipeline to verify the issue is resolved [72].
Workflow for Machine Learning Pipeline Optimization in Small Cohorts
This protocol outlines a methodology for optimizing machine learning pipelines when data is limited, a common scenario in brain imaging research on individual differences [74].
Procedure:
- Data Preprocessing: Apply subject-wise feature normalization to control for inter-individual variability. Implement data augmentation techniques (e.g., adding noise, spatial transformations) to artificially expand the training set [74] [77].
- Model Selection: Prioritize simpler, more interpretable models or linear classifiers with strong regularization to mitigate overfitting. For complex problems, consider using transfer learning by fine-tuning a model pre-trained on a larger, public dataset [74] [77].
- Robust Evaluation: Employ a nested cross-validation strategy to more accurately assess model performance and tune hyperparameters without optimistic bias. The primary focus should be on metrics that reflect generalizability to unseen data [76].
- Error Analysis: Systematically analyze where and how the model fails. This analysis can reveal limitations in the data and provide actionable insights [74].
- Dataset Enrichment: Based on the error analysis, the most effective long-term strategy is often to enrich the dataset. This can be done by acquiring more data, integrating additional modalities (e.g., adding DTI to structural MRI), or maximizing information extraction from existing data [74] [76].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Components for an Automated and Adaptive Optimization Pipeline
| Item | Function | Application in Brain Imaging |
|---|---|---|
| Model-Informed Drug Development (MIDD) Approaches | Quantitative frameworks (e.g., exposure-response, QSP) that use models and simulations to integrate all available data for informed decision-making [78]. | Used in oncology dose optimization to understand the relationship between drug exposure, safety, and efficacy, moving beyond the Maximum Tolerated Dose (MTD) paradigm [78] [79]. |
| Adaptive Clinical Trial Designs | Trial designs (e.g., seamless Phase 2/3) that allow for pre-planned modifications based on interim data, such as dropping ineffective doses [78] [79]. | Enables more efficient dose optimization in oncology drug development by leveraging early data to select the most promising dose for continued evaluation [79]. |
| Multimodal Data Integration | The process of combining different types of neuroimaging data (e.g., T1-weighted, DTI, fMRI) into a single analytical pipeline [74] [77]. | Crucial for capturing the full complexity of brain structure and function. In small cohorts, it maximizes information yield and can reveal synergistic effects between modalities [74]. |
| Symbolic Regression & Automated Feature Engineering | Computational methods that generate candidate objective functions or features from raw data through mathematical transformations [80]. | In drug optimization, frameworks like AMODO-EO use this to discover emergent, chemically meaningful objectives (e.g., HBA/RTB ratio) not predefined by researchers [80]. |
| Hyperparameter Optimization Strategies | Methods for automatically tuning the configuration settings of machine learning models [74]. | While crucial for performance, their gains can be marginal in very small cohorts. The focus should be on robust, efficient methods rather than exhaustive search [74]. |
Benchmarking Success: Validation Frameworks and Model Comparisons for Reliable Findings
FAQ: Core Validation Concepts
Q1: Why should we move beyond the Area Under the ROC Curve (AUC) for validating predictive models in brain research?
While AUC is appropriate for classification tasks, it has limitations for regression analyses common in neuroimaging. Statistical associations established in a sample do not necessarily guarantee predictive accuracy in new individuals or populations. Overreliance on in-sample model fit indices, including correlation coefficients, can produce misleadingly optimistic performance estimates. Best practices recommend using multiple complementary metrics to provide a more comprehensive and accurate assessment of a model's predictive validity [81].
Q2: What specific methodological errors most commonly threaten the reproducibility of predictive brain-behavior models?
Several key methodological errors can compromise reproducibility:
- Inappropriate Cross-Validation: Failing to ensure the cross-validation procedure encompasses all operations applied to the data, leading to overoptimistic performance estimates [81] [82].
- Ignoring Confounding Biases: Overlooking the biasing impact of confounding variables (e.g., age, scanner site, motion) which can create spurious brain-behavior associations [82].
- Small Sample Sizes: Performing prediction analyses with samples smaller than several hundred observations, which severely limits the stability and generalizability of findings [81].
- Biased ROI Analyses: Conducting circular analyses by defining regions of interest (ROIs) based on the same data used for the statistical test, which inflates effect sizes [83].
Q3: How does within-individual variation impact the measurement of individual differences in brain function?
The brain is a dynamic system, and its functional measurements naturally vary from moment to moment. This within-individual variation can be misinterpreted as meaningful between-individual differences if not properly accounted for. Sources of this variation range from moment-to-moment fluctuations in brain state to longer-term influences like diurnal rhythms, sleep quality, and caffeine intake. When within-individual variation is high relative to between-individual variation, it becomes difficult to reliably differentiate one individual from another, undermining the goal of individual differences research [24].
FAQ: Experimental Protocols & Troubleshooting
Q4: What is a detailed protocol for establishing predictive validity in a neuroimaging study?
The following protocol outlines a rigorous approach for a machine learning-based prediction study, emphasizing steps to ensure reproducibility.
Table: Experimental Protocol for Predictive Validity in Neuroimaging
| Step | Action | Purpose & Key Details |
|---|---|---|
| 1. Data Splitting | Split data into independent training, validation, and (if available) hold-out test sets. | Prevents data leakage and provides unbiased performance estimates. The test set should never be used for model training or parameter tuning [82]. |
| 2. Feature Preprocessing | Clean and preprocess features (e.g., confounder regression, harmonization for multi-site data). | Reduces unwanted variability and the influence of confounding biases. Techniques like ComBat can be used for site harmonization [82] [84]. |
| 3. Model Training with Cross-Validation | Train the model on the training set using a k-fold cross-validation (not leave-one-out) scheme. | Provides a robust internal estimate of model performance while preventing overfitting. The entire preprocessing pipeline must be nested within the cross-validation loop [81]. |
| 4. External Validation | Apply the final model, with all its fixed parameters, to the untouched validation or test set. | This is the gold standard for establishing generalizable predictive performance. Performance on this set is the primary indicator of real-world utility [81] [82]. |
| 5. Performance Reporting | Report multiple metrics, such as the coefficient of determination (R²) using sums of squares, median absolute error, and C-Index for survival analysis. | Avoids the pitfalls of correlation and provides a more nuanced view of model accuracy [81] [84]. |
Q5: Our model performs well in cross-validation but fails on new data. What are the primary troubleshooting steps?
This classic sign of overfitting suggests the model has learned patterns specific to your training sample that do not generalize. Follow this troubleshooting guide:
Troubleshooting Workflow for Generalization Failure
Q6: How can we optimize MRI acquisition parameters to improve the reliability of individual difference measurements?
Optimizing parameters is a balance between signal-to-noise ratio (SNR), resolution, and scan time. The table below summarizes key considerations, particularly for perfusion imaging and general structural/functional scans.
Table: MRI Parameter Optimization for Reliable Individual Differences Research
| Parameter | Recommendation for Reliability | Rationale & Troubleshooting Notes |
|---|---|---|
| Field Strength | Use the highest available (e.g., 3T). | Higher field strength significantly improves SNR, which is often a limiting factor in techniques like ASL [85]. |
| Spatial Resolution | Avoid "high-resolution" when SNR-limited; use 64x64 to 128x128 matrices for 2D ASL. | Higher resolution sacrifices SNR. Unreliable results can occur with low contrast-to-noise ratio (CNR), which can falsely overestimate perfusion metrics [85] [86]. |
| Repetition Time (TR) | Use a long TR (>3500 ms for ASL). | Allows substantial relaxation of labeled spins between acquisitions, improving signal fidelity [85]. |
| Inversion Time (TI) | Tailor to population (shorter for children, longer for elderly). | Must account for differences in circulation times. A multi-TI sequence can help estimate optimal TI for each patient [85]. |
| Phase Oversampling | Increase phase oversampling. | Can enhance SNR and allow for a reduced scan time without compromising image quality, improving patient comfort and data quality [17]. |
| Signal Averages | Use multiple averages (30-50 for 2D ASL at 3T). | Necessary to maintain acceptable SNR at reasonable imaging times [85]. |
The Scientist's Toolkit
Table: Essential Research Reagents & Computational Tools
| Tool / Solution | Function / Application | Use Case Example |
|---|---|---|
| Cross-Validation (k-fold) | A resampling method used to evaluate models on limited data samples. Provides a more reliable estimate of out-of-sample performance than leave-one-out CV [81]. | Used during model training to tune hyperparameters without touching the held-out test set. |
| Confounder Regression / Harmonization | Statistical techniques to control for the influence of nuisance variables (e.g., age, sex) or technical factors (e.g., scanner site). | Using ComBat to harmonize data from a multi-site study before building a predictive model of treatment response [82] [84]. |
| Precision Functional Mapping | An individualized approach using long fMRI scans to map brain organization at the level of a single person. | Revealing unique, person-specific brain networks that are missed by group-averaging, which may underlie individual behavioral variability [13]. |
| Arterial Spin Labeling (ASL) | An MRI technique to measure cerebral blood flow without exogenous contrast agents. | Tracking changes in brain perfusion in response to treatment in pediatric ADHD populations [13] [85]. |
| Cancer Imaging Phenomics Toolkit (CaPTk) | An open-source software platform for quantitative radiomic analysis of medical images. | Extracting robust radiomic features from glioblastoma multiforme (GBM) tumors on MRI to predict overall survival [84]. |
Predictive Modeling Workflow for Reproducibility
Comparative Performance of Univariate (GLM) vs. Multivariate (CVA, ML) Models
Frequently Asked Questions
What is the fundamental difference between univariate and multivariate analysis in neuroimaging? A univariate analysis, like the General Linear Model (GLM), tests for statistical effects one voxel at a time. It characterizes region-specific responses based on assumptions about the data. In contrast, a multivariate analysis, such as Canonical Variates Analysis (CVA) or other machine learning models, analyzes the data from all voxels simultaneously. These methods are often exploratory and data-driven, with the potential to identify distributed activation patterns that reveal neural networks and functional connectivity [87] [88].
When should I prefer a multivariate model over a univariate GLM? You should consider a multivariate model when your research question involves:
- Predicting brain states or behavior: Multivariate models like CVA are inherently designed for prediction and often show higher prediction accuracy [87].
- Identifying distributed patterns: If you suspect the neural signature of a cognitive process or disease is spread across multiple brain regions in a coordinated way, multivariate methods can capture these patterns more effectively than univariate methods [88].
- Analyzing individual differences: Multivariate frameworks can better handle the complex, multi-variable relationships that define differences between individuals [89].
I've heard GLM is more reproducible. Is this true? Yes, studies have directly compared the performance metrics of GLM and CVA pipelines and found that while multivariate CVA generally provides higher prediction accuracy, the univariate GLM often yields more reproducible statistical parametric images (SPIs). This highlights a key trade-off between the two approaches [87] [90].
Are there specific preprocessing steps that are more critical for one model over the other? Core preprocessing steps are essential for both. However, research on GLM-based pipelines has found that spatial smoothing and high-pass filtering (temporal detrending) significantly increase pipeline performance and are considered essential for robust analysis. The impact of other steps, like slice timing correction, may be less consistent [87]. The best practice is to optimize these steps for your specific pipeline and data.
How can these models be used in clinical drug development? Both univariate and multivariate neuroimaging analyses can serve as pharmacodynamic biomarkers in drug development. They can help answer critical questions such as:
- Brain Penetration: Does the drug affect brain function?
- Functional Target Engagement: What is the drug's impact on clinically relevant brain systems?
- Dose Selection: What is the dose-response relationship for these brain effects? [91] Using fMRI, for example, a GLM can show if a drug changes activation in a target region, while a multivariate approach could reveal if the drug alters entire functional networks.
Troubleshooting Guides
Low Statistical Power or Inconsistent Results
- Problem: Your analysis fails to find significant effects, or results change dramatically with small changes in data or preprocessing.
- Solutions:
- Check Preprocessing: Ensure that essential steps like spatial smoothing and high-pass temporal filtering are correctly applied, as they are proven to significantly improve the robustness of GLM analysis [87].
- Consider Model Trade-offs: If you are using a univariate GLM and need higher prediction accuracy, consider testing a multivariate model like CVA. Conversely, if you are using a multivariate model and require higher reproducibility, a GLM might be more suitable [87]. A consensus approach that leverages the strengths of both may be necessary for the most accurate activation patterns [87].
- Increase Sample Size: For individual differences research in particular, underpowered studies are a common pitfall. Traditional Phase 1 drug trials with 4-6 patients per dose, for example, are often underpowered for functional neuroimaging outcomes, leading to unreliable results [91].
Handling Individual Differences in Brain-Behavior Relationships
- Problem: Group-level results do not adequately represent the individuals in your study, or you are struggling to model the complex relationship between multiple brain measures and a behavioral trait.
- Solutions:
- Move Beyond Simple Correlation: Avoid relying solely on bivariate correlations between a single voxel's activation and a behavioral score. These designs have psychometric limitations and cannot model complex, multi-faceted relationships [89].
- Adopt Latent Variable Models: Use statistical frameworks from psychometric theory, such as Structural Equation Modeling (SEM). These models allow you to define a latent construct (e.g., "working memory capacity") from multiple observed measures (e.g., several task scores, activation in multiple regions), providing a more robust and valid assessment of individual differences [89].
Interpreting Conflicting Univariate and Multivariate Results
- Problem: In a regression study, all your variables were significant in univariate analysis, but only one remained significant in a multivariate model.
- Solutions:
- This is an expected outcome: It often means that while each variable has a significant individual (marginal) relationship with the outcome, the multivariate model has identified that only one variable provides unique predictive information when all others are accounted for. This is common when predictor variables are correlated with each other.
- Report it clearly: You can report this by stating: "The univariable analyses showed a statistically significant relationship between all variables and the outcome. When adjusting for confounders with multivariable analysis, only variable X remained statistically significant." This indicates that the effect of the other variables may be mediated through or shared with variable X [92].
Performance Data and Experimental Protocols
Table 1: Quantitative Comparison of GLM vs. CVA Performance on Real fMRI Data
This table summarizes findings from a systematic evaluation of GLM- and CVA-based fMRI processing pipelines using a cross-validation framework on real block-design fMRI data [87] [90].
| Performance Metric | General Linear Model (GLM) | Canonical Variates Analysis (CVA) | Interpretation |
|---|---|---|---|
| Prediction Accuracy | Lower | Higher | CVA's multivariate nature is better at predicting brain states in new data. |
| Reproducibility (SPI Correlation) | Higher | Lower | GLM produces more stable and repeatable activation maps across data splits. |
| Essential Preprocessing | Spatial smoothing, high-pass filtering | (Informed by GLM findings; pipeline optimization recommended) | These steps significantly boost GLM performance [87]. |
| Impact of Slice Timing/Global Normalization | Little consistent impact | (Informed by GLM findings; pipeline optimization recommended) | These steps showed minimal effect on GLM pipeline performance [87]. |
Experimental Protocol: Evaluating an fMRI Processing Pipeline with NPAIRS
This protocol outlines the NPAIRS (Nonparametric Prediction, Activation, Influence, and Reproducibility Resampling) framework, which allows for the evaluation of processing pipelines on real fMRI data without requiring a known ground truth [87] [90].
- Data Splitting: Split your fMRI dataset into two independent halves (e.g., by odd/even runs or sessions). One half is designated the training set, the other the test set.
- Model Training: Apply your chosen processing pipeline (e.g., a specific GLM or CVA model with a defined set of preprocessing steps) to the training set to estimate the model parameters.
- Prediction: Apply the estimated model parameters to the independent test set. Prediction accuracy (P) is calculated as the average posterior probability of correctly predicting the experimental condition (e.g., baseline vs. activation) for each volume in the test set.
- Reproducibility Calculation: Generate a statistical parametric image (SPI) from each of the two independent splits. Reproducibility (R) is calculated as the Pearson correlation between the two SPIs across all voxels.
- Cross-Validation and Iteration: Repeat steps 1-4, swapping the training and test sets, and across multiple resamplings (e.g., different split-half pairs) to build a distribution of (P, R) performance measures.
- Pipeline Optimization: Plot the (P, R) results for different pipelines (e.g., with/without a preprocessing step, or GLM vs. CVA) to identify the pipeline that offers the best trade-off between prediction accuracy and reproducibility for your specific data and research question.
NPAIRS Evaluation Workflow: A cross-validation framework for evaluating fMRI pipelines based on prediction accuracy and reproducibility.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Software and Analytical Tools
| Item Name | Function / Application | Key Context |
|---|---|---|
| General Linear Model (GLM) | A univariate framework for fitting a linear model to the time course of each voxel, testing the significance of experimental conditions relative to baseline. | The cornerstone of traditional fMRI analysis; implemented in SPM, FSL, AFNI [93] [94]. |
| Canonical Variates Analysis (CVA) | A multivariate method that maximizes separation between experimental conditions relative to within-condition variation. Identifies distributed patterns (canonical images) that best discriminate conditions. | Often shows higher prediction accuracy than GLM; useful for identifying network-level effects [87] [95]. |
| NPAIRS Package | A software package that implements the NPAIRS framework for pipeline evaluation without simulated data, providing prediction and reproducibility metrics. | Enables empirical optimization and comparison of different analysis pipelines on real fMRI data [87] [90]. |
| FSL (FEAT) | A comprehensive fMRI analysis software suite that includes a GLM-based implementation for first-level (single-subject) and higher-level (group) analysis. | A standard tool used in comparative performance studies [87]. |
| Structural Equation Modeling (SEM) | A latent variable modeling technique from psychometrics that allows for testing complex brain-behavior relationships by modeling constructs from multiple observed variables. | Highly recommended for robust individual differences research to overcome limitations of simple correlations [89]. |
| Machine Learning Classifiers | A broad class of multivariate algorithms (e.g., support vector machines) used for "decoding" mental states from distributed brain activity patterns. | Represents the evolution of multivariate pattern analysis beyond CVA; enables advanced predictive modeling [88]. |
Assessing Test-Retest Reliability and Longitudinal Stability of Imaging Biomarkers
FAQ: Navigating Imaging Biomarker Reliability
Q1: Why do my study's brain-wide associations between imaging measures and behavior lack statistical power, even with a reasonable sample size?
High within-individual variation in functional neuroimaging measurements can drastically reduce statistical power for detecting brain-behavior associations. Even if a "ground truth" relationship exists, the observed correlation can become inconsistent or insignificant across samples because the measurement variability is often misinterpreted as true interindividual difference. Optimizing power requires study designs that account for this within-subject variance, for instance, by using repeated measurements [24].
Q2: Our task-fMRI study in children revealed poor long-term stability of individual differences. Is this a common challenge?
Yes, poor reliability and stability of task-fMRI measures is a recognized challenge, particularly in developmental populations. One large-scale study of children found that the stability of individual differences in task-fMRI measures across time was "poor" in virtually all brain regions examined. Participant motion had a pronounced negative effect on these estimates. This essential issue urgently needs addressing through optimization of task designs, scanning parameters, and data processing methods [96].
Q3: Can functional near-infrared spectroscopy (fNIRS) serve as a reliable biomarker for assessing executive function in individuals?
Currently, the interpretation of fNIRS signals at the single-subject level is limited by low test-retest reliability. While group-level analyses can reveal specific frontal activation patterns during executive tasks, individual-level activation shows strong intra-individual variability across sessions. More research is needed to optimize fNIRS reliability before it can be routinely applied for clinical assessment in individuals [97].
Q4: What is a practical MRI design to track individual brain aging trajectories over a short period, like one year?
The "cluster scanning" design is a promising approach. This method involves densely repeating rapid structural MRI scans (e.g., eight 1-minute scans) at each longitudinal timepoint. By pooling these rapid scans, measurement error is substantially reduced, enabling the detection of individual differences in brain atrophy rates over a one-year interval, which would be obscured by the noise of standard single-scan protocols [98].
Troubleshooting Guides
Problem: Low Test-Retest Reliability in Functional Connectivity Measures
Background: You find that functional connectivity (FC) estimates from resting-state fMRI are unstable within the same individual across sessions, hampering individual differences research.
Solution: Implement a "stacking" approach that combines information across multiple MRI modalities.
- Root Cause: Single-modality FC measures can be influenced by moment-to-moment changes in brain state, attention, and other transient factors, contributing to high within-individual variance [24].
- Action Plan:
- Data Acquisition: Collect multiple imaging modalities from the same individuals, specifically including task-fMRI contrasts (from tasks like working memory or inhibitory control) in addition to resting-state FC and structural MRI [99].
- Model Building:
- First, build separate prediction models for each modality (e.g., a model using only task contrasts, another using only resting-state FC).
- Then, use the predicted values from these individual models as new features in a second-level "stacked" model.
- Outcome: This stacked model integrates stable information from across the brain and different measurement types, significantly improving the test-retest reliability of the resultant brain-based scores [99].
Problem: Inability to Detect Individual-Specific Brain Atrophy Over One Year
Background: Standard longitudinal structural MRI fails to detect significant brain change in individuals over one-year intervals because the annual atrophy rate is smaller than the measurement error of a standard scan.
Solution: Adopt a "cluster scanning" protocol to achieve high-precision measurement [98].
- Root Cause: The measurement error for a standard structural scan of hippocampal volume is approximately 2-5%, while the expected annual atrophy rate is only 1-3% in cognitively unimpaired older adults. The signal of true change is buried in noise [98].
- Action Plan:
- Protocol Design: At each longitudinal visit, acquire multiple rapid, high-resolution structural scans (e.g., eight scans of 1-minute each) instead of a single standard-length scan.
- Data Processing: Pool the estimates from the multiple rapid scans through within-individual averaging or modeling.
- Outcome: This reduces measurement error nearly threefold, making the annual change detectable and allowing for the characterization of individual trajectories of brain aging [98].
Table 1: Test-Retest Measurement Error for Hippocampal Volume Using Different Scanning Protocols [98]
| Scanning Protocol | Left Hippocampus Error (mm³) | Left Hippocampus Error (%) | Right Hippocampus Error (mm³) | Right Hippocampus Error (%) |
|---|---|---|---|---|
| Single Rapid Scan (1'12") | 92.4 | 3.4% | 82.9 | 2.3% |
| Single Standard Scan (5'12") | 99.1 | 3.4% | 80.8 | 2.2% |
| Eight Rapid Scans (Pooled) | 33.2 | 1.0% | 39.0 | 1.1% |
Table 2: Comparative Reliability of Neuroimaging Modalities for Predicting Cognitive Abilities [99]
| Imaging Modality | Predictability (Out-of-sample r) | Test-Retest Reliability (ICC) | Notes | |
|---|---|---|---|---|
| Task-fMRI Contrasts | ~0.5 - 0.6 | Poor (as single areas) | Primary driver of stacked model performance | |
| Structural MRI | Lower than task-fMRI | Excellent (near ceiling) | High stability but lower predictive power | |
| Resting-State FC | Variable | Moderate to High | ||
| Stacked Model (Multiple modalities) | ~0.5 - 0.6 | >0.75 (Excellent) | Integrates strengths of all modalities |
Experimental Protocols
Protocol 1: Cluster Scanning for Longitudinal Structural MRI
Objective: To precisely estimate the one-year rate of brain structural change (e.g., hippocampal atrophy) within individuals by minimizing measurement error [98].
Methodology:
- Participant Schedule: Schedule each participant for three main longitudinal timepoints spaced evenly across one year (e.g., Baseline, Month 6, Month 12).
- Session Design: At each main timepoint, conduct two separate MRI sessions ("test" and "retest") on different days to directly estimate measurement error.
- Scanning Protocol: During each session, acquire a "cluster" of eight rapid T1-weighted structural scans (e.g., 1 minute 12 seconds each, accelerated with compressed sensing). A standard clinical structural scan may also be acquired for comparison.
- Data Analysis:
- Process each rapid scan individually to extract morphometric measures (e.g., hippocampal volume).
- For each session, calculate the average volume across the eight scans to create a high-precision estimate.
- Model the longitudinal trajectory of change using the high-precision estimates from the three main timepoints.
Protocol 2: Stacking Method for Reliable Brain-Behavior Prediction
Objective: To improve the predictability, reliability, and generalizability of brain-wide association studies (BWAS) for cognitive abilities by combining information from multiple MRI modalities [99].
Methodology:
- Data Collection: Acquire multi-modal MRI data from participants, including:
- Task-fMRI: Multiple tasks probing executive functions (e.g., working memory, inhibition).
- Resting-state fMRI: For functional connectivity (FC) analysis.
- Structural MRI: For cortical thickness, area, and volume.
- Feature Extraction:
- For task-fMRI, extract contrast maps for each task.
- For resting-state, compute a whole-brain functional connectivity matrix.
- For structural data, extract regional measures.
- Model Stacking:
- Step 1 (Base Models): Train separate machine learning models (e.g., ridge regression) to predict the behavioral measure (e.g., cognitive ability score) using features from each modality independently.
- Step 2 (Meta-Features): Use each base model to generate predicted scores for all participants. These predictions become the new "meta-features."
- Step 3 (Stacked Model): Train a final model (e.g., linear model) using the meta-features to predict the behavioral outcome.
- Validation: Evaluate the stacked model's performance using out-of-sample prediction, test-retest reliability, and generalizability to independent datasets.
Conceptual and Experimental Workflows
Diagram 1: Protocol optimization workflow for reliable biomarker studies.
Diagram 2: Cluster scanning workflow for precise longitudinal measurement.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Analytical Tools for Reliability Research
| Item / Solution | Function / Application | Key Consideration |
|---|---|---|
| Compressed Sensing MRI Sequences | Enables acquisition of rapid, high-resolution structural scans (e.g., 1-minute T1-weighted) for cluster scanning [98]. | Reduces participant burden, making dense sampling feasible. |
| Multi-Echo fMRI Sequences | Improves signal quality in functional MRI by allowing for better removal of non-neural noise [100]. | Can shorten the requisite scan time for reliable individual-specific functional mapping. |
| Machine Learning Stacking Algorithms | Combines predictions from multiple neuroimaging modalities into a single, more reliable and accurate model [99]. | Crucial for boosting the test-retest reliability of brain-behavior predictions. |
| Contrast-Based BBB Leakage Quantification | Adapts standard clinical MRI perfusion data to quantify blood-brain barrier disruption as a biomarker for vascular cognitive decline [101]. | Leverages widely available scan types, facilitating broader research adoption. |
| High-Precision Morphometry Pipelines | Software (e.g., FreeSurfer, ANTs) for estimating brain structure volumes and cortical thickness from T1-weighted MRI [98]. | Required for processing dense clusters of structural scans to generate precise averages. |
Power Analysis and Sample Size Estimation for Individual Differences Studies
Frequently Asked Questions (FAQs)
FAQ 1: Why are brain-wide association studies (BWAS) for certain cognitive traits, like inhibitory control, often underpowered?
Insufficient data per participant is a major cause of underpowered studies. Individual-level estimates of traits like inhibitory control can be highly variable when based on limited testing (e.g., only 40 trials in some datasets). This high within-subject measurement noise inflates estimates of between-subject variability and, in turn, attenuates correlations between brain and behavioral measures [26]. Precision approaches, which collect extensive data per participant (e.g., over 5,000 trials across multiple sessions), demonstrate that increasing data per person mitigates this noise and improves the reliability of individual estimates, which is fundamental for powerful individual differences research [26].
FAQ 2: What is the trade-off between the number of participants and the amount of data collected per participant?
For a fixed total resource budget, there is a trade-off between sample size (N) and scan time per participant (T). Research shows that prediction accuracy in BWAS increases with the total scan duration (N × T). Initially, for scans up to about 20 minutes, sample size and scan time are somewhat interchangeable; you can compensate for a smaller sample with longer scans and vice-versa [25]. However, diminishing returns set in for longer scan times. Beyond 20-30 minutes, increasing the sample size becomes more effective for boosting prediction accuracy than further increasing scan duration [25]. Cost analyses suggest that 30-minute scans are often the most cost-effective [25].
FAQ 3: How can I improve the reliability of my behavioral task for individual differences research?
The reliability of your measurement instrument is paramount. Key strategies include [102]:
- Increase Task Length: Extending the duration of cognitive tasks (e.g., from 5 minutes to 60 minutes) can significantly improve the predictive power of the measures [26].
- Assess Internal Consistency: Ensure that the items or trials within your task correlate with each other, indicating they are measuring a single construct.
- Evaluate Test-Retest Reliability: A good task should produce stable scores when the same participant is tested on separate occasions. A variable cannot correlate with another more than it correlates with itself [102].
- Use Standardized Protocols: Avoid ad-hoc, self-selected stimuli. Use validated tasks or invest the substantial time required to develop and validate new ones properly [102].
FAQ 4: Beyond sample size, what key parameter should be optimized in an MRI study for power?
For fMRI-based studies, the scan time per participant is a critical parameter. Longer fMRI scans improve the reliability of functional connectivity estimates. More than 20-30 minutes of fMRI data is often required for precise individual-level brain measures [26]. One study found that optimizing for longer scan times (around 30 minutes) can yield up to 22% cost savings compared to using shorter 10-minute scans, while achieving the same prediction accuracy [25].
FAQ 5: What analytical approaches can maximize signal in individual differences studies?
To maximize signal, move beyond group-level analyses to individualized approaches [26]:
- Individual-Specific Parcellations: Deriving functional brain networks from parcellations defined for each individual, rather than using a one-size-fits-all group template, improves behavioral prediction [26].
- Hyper-Alignment: Using fine-grained, individual-specific functional connectivity patterns for analysis rather than relying on region-based group averages [26].
- Targeted Experimental Manipulations: Designing tasks that specifically probe the cognitive function of interest can help maximize the relevant neural signal [26].
Troubleshooting Guides
Issue 1: Low Prediction Accuracy Despite Large Sample Size
Problem: Your BWAS has a large number of participants, but the accuracy for predicting behavioral phenotypes remains unacceptably low.
Solution Steps:
- Diagnose Measurement Reliability: Check the test-retest reliability and internal consistency of your behavioral phenotype. Low reliability is a primary cause of low prediction accuracy [102]. If reliability is poor, the solution is not a larger sample but a better measure.
- Evaluate Brain Measure Precision: Assess the reliability of your brain imaging measures. For functional connectivity, use intra-class correlation (ICC) or split-half reliability. If you have less than 20-30 minutes of fMRI data per person, your brain measures may be too noisy [26].
- Increase Data per Participant: If measurements are unreliable, consider a precision approach. Collect more data per participant, either by lengthening the task or adding multiple testing sessions [26].
- Refine Analytical Models: Implement individualized analysis frameworks, such as creating individual-specific brain parcellations or using hyper-alignment techniques, to better capture each person's unique brain organization [26].
Issue 2: Determining the Optimal Sample Size and Scan Duration
Problem: You are designing a new BWAS and need to determine the most cost-effective balance between the number of participants and the scan time per participant.
Solution Steps:
- Define Your Phenotype: Understand that different phenotypes have different prediction ceilings. Crystallized intelligence (e.g., vocabulary) is typically better predicted than inhibitory control or self-reported clinical symptoms [26].
- Use the Reference Model: Consult existing models based on large datasets. The relationship between total scan duration (N × T) and prediction accuracy (r) for many phenotypes follows a logarithmic pattern: r = a + b × log(N × T) [25].
- Perform a Cost-Benefit Analysis: Account for the overhead cost of recruiting each participant (e.g., recruitment, screening, travel). Because of these costs, longer scans can be cheaper than larger samples for achieving the same accuracy. The following table summarizes key findings from a large-scale analysis [25]:
Table 1: Cost and Performance Trade-offs in BWAS Design
| Scan Time (minutes) | Relative Cost-Efficiency | Key Considerations |
|---|---|---|
| 10 | Low | Often cost-inefficient; not recommended for high prediction performance. |
| 20 | Medium | The point where interchangeability with sample size begins to diminish. |
| 30 | High (Optimal) | On average, the most cost-effective, yielding ~22% savings over 10-min scans. |
| >30 | Medium | Cheaper to overshoot than undershoot; diminishing returns are significant. |
- Make a Final Decision: For most scenarios, aim for a scan time of at least 30 minutes. If studying a rare population with high recruitment overhead, consider even longer scan times per participant [25].
Experimental Protocols
Protocol 1: Implementing a Precision fMRI Approach for Individual Differences
Purpose: To obtain highly reliable individual-level estimates of brain function and behavior by maximizing data collection per participant.
Methodology:
- Participant Scheduling: Schedule each participant for multiple testing sessions (e.g., 3-5 sessions) conducted on separate days [26].
- fMRI Data Acquisition:
- Behavioral Phenotyping:
- Data Analysis:
- Preprocess fMRI data using standard pipelines.
- Generate individual-specific brain parcellations for each participant [26].
- Calculate functional connectivity matrices from the entire dataset for each individual.
- Use machine learning models (e.g., kernel ridge regression) with cross-validation to predict behavior from brain connectivity [25].
Diagram 1: Precision fMRI protocol workflow.
Protocol 2: A Framework for Evaluating Behavioral Task Reliability
Purpose: To systematically assess and ensure that a behavioral task is suitable for measuring individual differences.
Methodology:
- Pilot Testing:
- Administer the task to a small but diverse pilot sample.
- Collect a sufficiently large number of trials or items per participant.
- Calculate Internal Consistency:
- For tasks not based on aggregate scores over a time limit, calculate internal consistency (e.g., using Cronbach's Alpha or Split-Half reliability) [102].
- The expectation is that performance on one set of items/trials correlates with performance on another set.
- Assess Test-Retest Reliability:
- Re-administer the task to the same pilot participants after a suitable time interval (e.g., one week for a stable trait) [102].
- Calculate the correlation (e.g., Pearson's r) between scores from the two testing sessions. A high correlation indicates the task measures a stable trait.
- Iterate and Validate:
- If reliability metrics are low, refine the task (e.g., modify instructions, adjust trial numbers, remove ambiguous stimuli) and repeat the piloting process.
- Once satisfactory reliability is achieved, validate the task by correlating its scores with established measures of the same or related constructs [102].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Resources for Individual Differences Research
| Item | Function & Application | Key Considerations |
|---|---|---|
| High-Sampling Datasets | Provide extensive within-participant data for developing and testing reliability of measures. Examples: densely sampled individual data [26]. | Critical for establishing the upper limit of reliability for behavioral and brain measures. |
| Consortium Datasets (e.g., HCP, ABCD, UK Biobank) | Provide large sample sizes (N) for studying population-level effects and testing multivariate prediction models [26]. | Effects are typically small. Best for final validation, not for developing reliable tasks. |
| Reliability Analysis Software | Tools (e.g., in R, Python, SPSS) to calculate internal consistency and test-retest reliability metrics [102]. | A prerequisite for any individual differences study. Never interpret a correlation without knowledge of measure reliability. |
| Individual-Specific Parcellation Algorithms | Software to define functional brain networks unique to each individual, rather than using a group-average atlas [26]. | Improves the precision of brain measures and enhances behavioral prediction accuracy. |
| Prediction Modeling Tools | Machine learning libraries (e.g., scikit-learn in Python) for implementing kernel ridge regression, linear ridge regression, and cross-validation [25]. | Multivariate models that combine information from across the brain generally lead to better predictions than univariate approaches. |
Conclusion
Optimizing brain imaging for individual differences is a multi-faceted endeavor crucial for advancing both basic neuroscience and clinical applications. The integration of optimized acquisition protocols, robust preprocessing pipelines, and validated multivariate analytical models significantly enhances the reliability and effect sizes of neuroimaging measures. Future directions point toward the deep integration of AI and machine learning with multimodal data (fMRI, DTI, EEG) to create closed-loop systems for real-time parameter adjustment and personalized therapeutic interventions, such as precision TMS. Embracing these strategies, as outlined by initiatives like the BRAIN Initiative 2025, will be paramount in translating group-level findings into meaningful predictions and treatments for the individual, ultimately fulfilling the promise of personalized medicine in neurology and psychiatry.
References
- 1. poor measurement reliability attenuates group differences [https://pubmed.ncbi.nlm.nih.gov/41169915/]
- 2. Clarifying the reliability paradox: poor measurement ... [https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2025.1592658/full]
- 3. Troubleshooting Protocols - Biological Sciences: Summer ... [https://guides.library.cmu.edu/biologicalsciencesSRI/troubleshooting]
- 4. 5 Steps to Follow for Troubleshooting Experiments [https://blog.edvotek.com/2022/06/21/5-steps-to-follow-for-troubleshooting-experiments/]
- 5. A parameter-optimization framework for neural decoding ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2023.938689/full]
- 6. How to choose colors for data visualizations [https://www.atlassian.com/data/charts/how-to-choose-colors-data-visualization]
- 7. Method for optimizing imaging parameters to record ... [https://pubmed.ncbi.nlm.nih.gov/38550774/]
- 8. Has a software bug really called decades of brain imaging ... [https://www.theguardian.com/science/head-quarters/2016/sep/30/has-a-software-bug-really-called-decades-of-brain-imaging-research-into-question]
- 9. Beyond Increasing Sample Sizes: Optimizing Effect ... [https://pure.psu.edu/en/publications/beyond-increasing-sample-sizes-optimizing-effect-sizes-in-neuroim/]
- 10. 11. Data science tools for neuroimaging [https://neuroimaging-data-science.org/content/005-nipy/001-nipy.html]
- 11. Best practices in data analysis and sharing ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5685169/]
- 12. Data Analysis Lab Software [http://www.bmap.ucla.edu/services/data_analysis/data_analysis_lab_software/]
- 13. Precision brain mapping: A new frontier in personalized ... [https://www.eurekalert.org/news-releases/1106509]
- 14. The Promise of Investigating Neural Variability in ... [https://www.sciencedirect.com/science/article/pii/S0006322325001027]
- 15. Behavioral Responses to Neural Circuit Control [https://pmc.ncbi.nlm.nih.gov/articles/PMC8270009/]
- 16. BRAIN 2025: A Scientific Vision - BRAIN Initiative - NIH [http://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 17. Optimizing imaging resolution in brain MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC10478647/]
- 18. How to Acquire the Best Brain Images Possible [https://tech.snmjournals.org/content/47/1/13]
- 19. Genetic and striatal structural connection linking behavioral ... [https://www.nature.com/articles/s41398-025-03687-8]
- 20. A Student's Guide to Neural Circuit Tracing [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2019.00897/full]
- 21. Interpreting and Utilising Intersubject Variability in Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5962820/]
- 22. Does inter-subject variability in cortical functional ... [https://scholars.uthscsa.edu/en/publications/does-inter-subject-variability-in-cortical-functional-organizatio/]
- 23. The Main Sources of Intersubject Variability in Neuronal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2766833/]
- 24. Challenges in measuring individual differences of brain function [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319922/]
- 25. Longer scans boost prediction and cut costs in brain-wide ... [https://www.nature.com/articles/s41586-025-09250-1]
- 26. Using Precision Approaches to Improve Brain-Behavior ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12483401/]
- 27. Capturing inter-subject variability with group independent ... [https://www.sciencedirect.com/science/article/abs/pii/S1053811911011712]
- 28. Inter-subject Functional Correlation Reveal a Hierarchical ... [https://www.nature.com/articles/s41598-017-11324-8]
- 29. Comparison of blocked and event-related fMRI designs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3036974/]
- 30. Comparison of block and eventâ€related fMRI designs in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6871864/]
- 31. Enhancing task fMRI individual difference research ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/39974058/]
- 32. Comparison of fMRI paradigms assessing visuospatial ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0186344]
- 33. What To Do About Software Errors in fMRI? [https://www.discovermagazine.com/what-to-do-about-software-errors-in-fmri-9345]
- 34. Optimizing fMRI experimental design for MVPA-based BCI ... [https://www.sciencedirect.com/science/article/pii/S1053811918320615]
- 35. Reduction of systematic errors in diffusion tensor imaging ... [https://www.sciencedirect.com/science/article/pii/S0010482525008546]
- 36. Noise reduction in magnitude diffusion-weighted images ... [https://pubmed.ncbi.nlm.nih.gov/39892480/]
- 37. Diagnostic performance of a multi-shell DTI protocol and its ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1618582/full]
- 38. Reducing Eddy Current Artifacts With Dummy Gradients ... [https://i-mri.org/DOIx.php?id=10.13104/imri.2025.0013]
- 39. Metal Artifact Reduction Around Cervical Spine Implant Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10841892/]
- 40. High-resolution and high-fidelity diffusion tensor imaging of ... [https://pubmed.ncbi.nlm.nih.gov/40016879]
- 41. DTI Data Acquisition: Scanners and Coils [https://bio-protocol.org/exchange/minidetail?id=8446786&type=30]
- 42. Building a science of individual differences from fMRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4886721/]
- 43. Neurofunctional underpinnings of individual differences in ... [https://www.nature.com/articles/s41467-023-41380-w]
- 44. Multivoxel Pattern Analysis for fMRI Data: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3529504/]
- 45. MVPA-Light: A Classification and Regression Toolbox for ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.00289/full]
- 46. Neural signatures of emotional intent and inference align ... [https://www.nature.com/articles/s41467-025-59931-8]
- 47. Validating the Why/How Contrast for Functional MRI Studies of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4111963/]
- 48. Precision TMS through the integration of neuroimaging and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515893/]
- 49. Closing the loop between brain and electrical stimulation [https://www.nature.com/articles/s41398-023-02565-5]
- 50. Transcranial Magnetic Stimulation -TMS [https://www.neuromodulation.com/TMS]
- 51. Fmriprep smoothing option [https://neurostars.org/t/fmriprep-smoothing-option/259]
- 52. FMRIPrep: a robust preprocessing pipeline for functional MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC6319393/]
- 53. Outputs of fMRIPrep [https://fmriprep.org/en/23.2.3/outputs.html]
- 54. FAQ - Frequently Asked Questions [https://fmriprep.org/en/stable/faq.html]
- 55. fMRIPrep: A Robust Preprocessing Pipeline for fMRI Data ... [https://fmriprep.org/]
- 56. Quality control in functional MRI studies with MRIQC and ... [https://pubmed.ncbi.nlm.nih.gov/37555175/]
- 57. Quality control in functional MRI studies with MRIQC and ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2022.1073734/full]
- 58. Optimizing preprocessing and analysis pipelines for single ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4898950/]
- 59. Impact of Preprocessing and Harmonization Methods on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8232807/]
- 60. Neuroimaging Measures of Error-Processing [https://pmc.ncbi.nlm.nih.gov/articles/PMC4860744/]
- 61. Fmriprep error - Preprocessing did not finish successfully [https://neurostars.org/t/fmriprep-error-preprocessing-did-not-finish-successfully/19910?page=2]
- 62. What are the steps for preprocessing fMRI data? [https://mriquestions.com/data-pre-processing.html]
- 63. Statistical Power and Why It Matters | A Simple Introduction [https://www.scribbr.com/statistics/statistical-power/]
- 64. Introduction to Power Analysis - OARC Stats - UCLA [https://stats.oarc.ucla.edu/other/mult-pkg/seminars/intro-power/]
- 65. Basic facts about GPUs | Damek Davis' Website [https://damek.github.io/random/basic-facts-about-gpus/]
- 66. CUDA Optimization Strategies for Compute- and Memory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3262956/]
- 67. and memory-bound neuroimaging algorithms [https://www.sciencedirect.com/science/article/abs/pii/S0169260710002750]
- 68. CUDA C++ Best Practices Guide [https://docs.nvidia.com/cuda/cuda-c-best-practices-guide/]
- 69. How Much GPU Memory Do You Need in a Data Science ... [https://www.hp.com/us-en/shop/tech-takes/gpu-memory-requirements-data-science-workstation]
- 70. Software - Laboratory of NeuroImaging [https://loni.usc.edu/research/software]
- 71. start · BrainSuite [https://brainsuite.org/]
- 72. How to resolve common pipeline issues | Troubleshooting [https://docs.digibee.com/documentation/troubleshooting/common-issues/common-pipeline-issues]
- 73. Troubleshoot pipeline runs - Azure Pipelines [https://learn.microsoft.com/en-us/azure/devops/pipelines/troubleshooting/troubleshooting?view=azure-devops]
- 74. Evaluating machine learning pipelines for multimodal ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2025.1568116/full]
- 75. A list of the 13 most common pipeline data issues ... [https://www.ibm.com/think/insights/data-issues]
- 76. Optimizing Effect Sizes in Neuroimaging Research on ... [https://pubmed.ncbi.nlm.nih.gov/39792657/]
- 77. Machine Learning in MRI Brain Imaging: A Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609805/]
- 78. FDA-AACR Strategies for Optimizing Dosages for Oncology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12536354/]
- 79. Adaptive phase 2/3 design with dose optimization [https://www.sciencedirect.com/science/article/pii/S1551714425002423]
- 80. AMODO-EO: A Practical Framework for Adaptive Objective ... [https://chemrxiv.org/engage/chemrxiv/article-details/68a1e064a94eede1542c01e6]
- 81. Establishment of Best Practices for Evidence for Prediction [https://pubmed.ncbi.nlm.nih.gov/31774490/]
- 82. Overview of Challenges in Brain-based Predictive Modeling [https://www.sciencedirect.com/science/article/pii/S000632232501460X]
- 83. Frequently Asked Questions - Andy's Brain Book! [https://andysbrainbook.readthedocs.io/en/latest/FrequentlyAskedQuestions/FrequentlyAskedQuestions.html]
- 84. Reproducible and Interpretable Machine Learning-Based ... [https://www.mdpi.com/2072-6694/16/19/3351]
- 85. ASL Parameters [https://mriquestions.com/asl-parameters.html]
- 86. Practical guidance to identify and troubleshoot suboptimal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10913595/]
- 87. Evaluation and Comparison of GLM- and CVA-based fMRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4277234/]
- 88. Machine learning in neuroimaging: from research to clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9732070/]
- 89. Neuroimaging of Individual Differences: A Latent Variable ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6980382/]
- 90. Evaluation and comparison of GLM- and CVA-based fMRI ... [https://www.sciencedirect.com/science/article/abs/pii/S1053811908002565]
- 91. Opportunities for use of neuroimaging in de-risking drug ... [https://www.nature.com/articles/s41386-024-01970-8]
- 92. Univariable and multivariable analyses [https://www.pvalue.io/univariate-and-multivariate-analysis/]
- 93. Chapter 4: The General Linear Model - Andy's Brain Book! [https://andysbrainbook.readthedocs.io/en/latest/fMRI_Short_Course/Statistics/04_Stats_General_Linear_Model.html]
- 94. The General Linear Model (GLM) [https://www.brainvoyager.com/bv/doc/UsersGuide/StatisticalAnalysis/TheGeneralLinearModel.html]
- 95. Canonical Variates Analysis - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/canonical-variates-analysis]
- 96. Reliability and stability challenges in ABCD task fMRI data [https://www.sciencedirect.com/science/article/pii/S1053811922001756]
- 97. Test–retest reliability of functional near infrared ... [https://www.sciencedirect.com/science/article/pii/S0925492725000484]
- 98. Precision Estimates of Longitudinal Brain Aging Capture ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11888524/]
- 99. Improving Predictability, Reliability and Generalisability of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11092590/]
- 100. Psychiatric neuroimaging designs for individualised, cohort ... [https://www.nature.com/articles/s41386-024-01918-y]
- 101. New Imaging Technique Uses Blood-Brain Barrier Leaks to ... [https://www.hopkinsmedicine.org/news/articles/2025/10/new-imaging-technique-uses-blood-brain-barrier-leaks-to-predict-vascular-dementia-risk]
- 102. Designing and evaluating tasks to measure individual ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10899130/]