Non-Invasive Brain-Computer Interfaces: A Comprehensive 2025 Review of Technologies, Clinical Applications, and Future Directions
This article provides a systematic review of the rapidly evolving field of non-invasive Brain-Computer Interfaces (BCIs), tailored for researchers, scientists, and drug development professionals.
Non-Invasive Brain-Computer Interfaces: A Comprehensive 2025 Review of Technologies, Clinical Applications, and Future Directions
Abstract
This article provides a systematic review of the rapidly evolving field of non-invasive Brain-Computer Interfaces (BCIs), tailored for researchers, scientists, and drug development professionals. It covers the fundamental principles of major non-invasive technologies including EEG, fNIRS, and emerging methods like wearable MEG and digital holographic imaging. The review analyzes current methodological approaches and their applications in neurological disorders, spinal cord injury rehabilitation, and cognitive enhancement. It addresses critical technical challenges such as signal quality optimization and presents evidence-based performance comparisons. By synthesizing the latest research trends, clinical validation studies, and technological innovations, this article serves as a comprehensive reference for professionals navigating the transition of non-invasive BCIs from laboratory research to clinical practice and commercial applications.
Principles and Evolution of Non-Invasive Neural Signal Acquisition
Historical Context and Fundamental Principles of Non-Invasive BCI
A Brain-Computer Interface (BCI) establishes a direct communication pathway between the brain and an external device, bypassing the body's normal neuromuscular output channels [1]. This technology has evolved from a scientific curiosity to a robust field with significant applications in medical rehabilitation, assistive technology, and human-computer interaction. Non-invasive BCIs, which record brain activity from the scalp without surgical implantation, represent a particularly accessible and safe category of these interfaces [2] [3]. This whitepaper provides an in-depth technical examination of non-invasive BCI, detailing its historical development, fundamental principles, and the core methodologies that underpin its operation, framed within the context of a broader review and comparison of non-invasive BCI technologies.
Historical Context
The foundations of non-invasive BCI are inextricably linked to the discovery and development of methods to record the brain's electrical activity.
- 19th Century Foundations: The earliest roots of BCI trace back to 1875 when English physicist Richard Caton first recorded electrical signals from the brains of animals [4].
- Birth of Human EEG (1924): The pivotal moment for non-invasive interfacing came in 1924 when German psychiatrist Hans Berger made the first recording of electrical brain activity from a human scalp, a technique he named the electroencephalogram (EEG). His 1930 publication, "Über das Elektrenkephalogramm des Menschen," detailed the identification of alpha and beta waves, laying the groundwork for all subsequent EEG-based BCI research [4].
- First Human BCI (1973): The first successful demonstration of a BCI in a human occurred at the University of California, Los Angeles. Participants in this study, supported by DARPA and the National Science Foundation, learned to control a cursor on a computer screen using their mental activity derived from EEG signals, specifically visual evoked potentials [5] [6].
- Modern Evolution: Over recent decades, the field has rapidly advanced from simple cursor control to the complex operation of robotic devices, exoskeletons, and communication systems, driven by improvements in signal processing, machine learning, and sensor technology [3] [2].
Fundamental Principles and Components
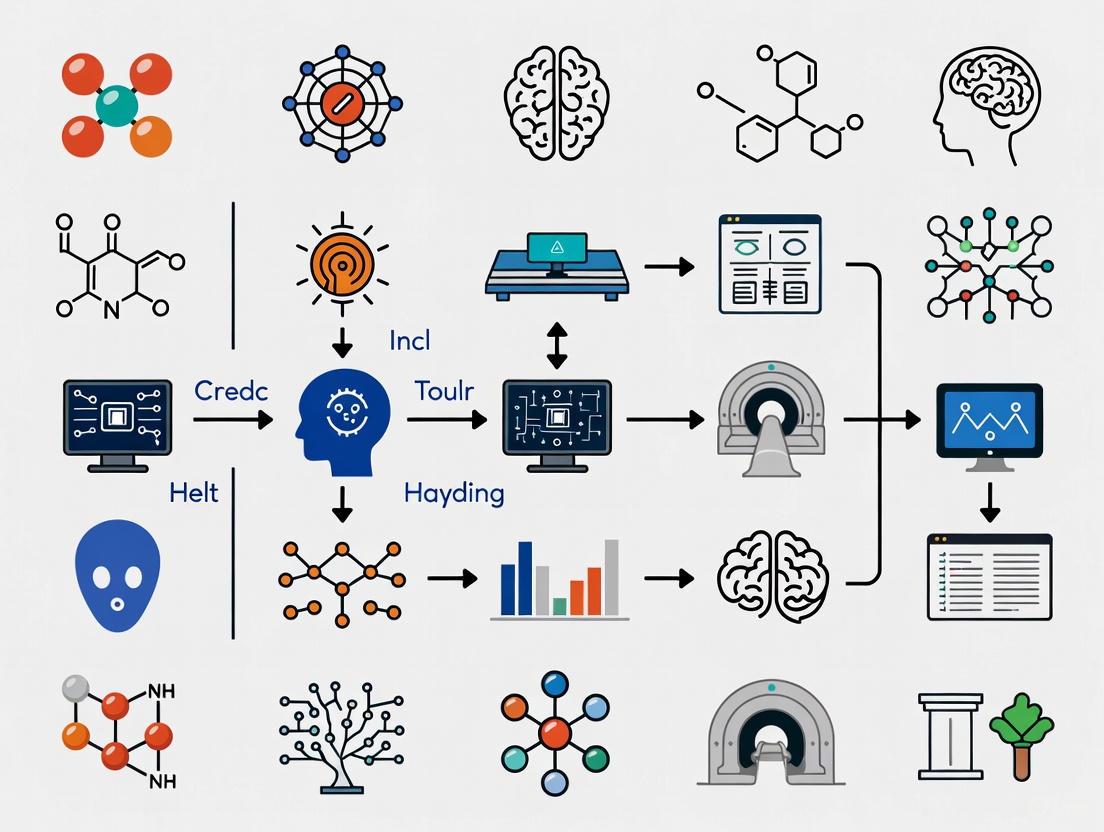
At its core, a BCI is a closed-loop system that translates specific patterns of brain activity into commands for an external device. The system operates through a sequence of four standardized stages, as illustrated in the workflow below.
Figure 1: The standardized workflow of a non-invasive Brain-Computer Interface system, illustrating the sequential stages from signal acquisition to device control and user feedback.
Core BCI Components
- Signal Acquisition: This initial stage involves measuring brain activity. Non-invasive BCIs primarily use Electroencephalography (EEG), which records voltage fluctuations resulting from ionic current flows within the brain's neurons through electrodes placed on the scalp [2] [7]. Other modalities include Magnetoencephalography (MEG), which detects the magnetic fields induced by neuronal electrical currents, and functional Near-Infrared Spectroscopy (fNIRS), which measures hemodynamic activity correlated with neural firing via light absorption [3] [8].
- Preprocessing: The acquired neural signals are characteristically weak and contaminated with noise from both physiological (e.g., eye blinks, muscle movement, heart rate) and external sources (e.g., line interference) [5]. Preprocessing applies techniques such as filtering (to remove irrelevant frequency bands), artifact removal, and signal averaging to enhance the signal-to-noise ratio (SNR) [1] [5].
- Feature Extraction: In this stage, the preprocessed signal is analyzed to identify discriminative patterns or features that correspond to the user's intent. These features can be extracted in the time-domain (e.g., event-related potentials like the P300), frequency-domain (e.g., power in specific frequency bands like Mu or Beta rhythms), or spatial-domain (e.g., patterns across different electrode locations) [5] [1].
- Feature Classification and Translation: The extracted features are fed into a translation algorithm or classifier—often employing machine learning techniques such as Support Vector Machines (SVM) or Neural Networks—which maps the feature vector to a specific output command [1] [5]. This command is then executed by an external device, such as a robotic arm, wheelchair, or speller application [3].
A critical element for effective BCI operation is neuroplasticity, the brain's inherent ability to reorganize itself by forming new neural connections. This allows users to learn, through feedback and training, how to modulate their brain activity to improve BCI control over time [1].
Technical Comparison of Non-Invasive Modalities
The performance of a non-invasive BCI is governed by the inherent properties of its signal acquisition modality. The table below summarizes the key technical benchmarks for the primary non-invasive methods.
Table 1: Technical comparison of major non-invasive brain activity recording modalities used in BCI research.
| Modality | Primary Signal | Spatial Resolution | Temporal Resolution | Portability & Cost | Key Advantages | Key Limitations |
|---|---|---|---|---|---|---|
| EEG | Electrical potentials | ~1 cm | Excellent (ms) | High portability, Low cost [2] | High temporal resolution, low cost, safe, easy to use [2] [4] | Signal degraded by skull/scalp [2] |
| MEG | Magnetic fields | ~2-3 mm | Excellent (ms) | Low portability, Very High cost | Excellent spatiotemporal resolution | Requires shielded room [8] |
| fNIRS | Hemodynamic (blood flow) | ~1 cm | Poor (seconds) | Moderate portability, Moderate cost | Less sensitive to movement artifacts | Low temporal resolution [8] |
| DHI* | Tissue deformation (nanometer) | High (µm-mm) | Good (ms) | Under development | Novel, high-resolution optical signal | Early research stage [9] |
DHI: Digital Holographic Imaging, an emerging technique included for completeness [9].
Detailed Experimental Protocols
To illustrate the practical application of these principles, below are detailed methodologies for two key BCI paradigms: one for motor rehabilitation and another for cognitive intervention.
Protocol 1: Motor Function Rehabilitation for Spinal Cord Injury
A 2025 meta-analysis established a protocol for applying non-invasive BCI to improve motor and sensory function in patients with Spinal Cord Injury (SCI) [10].
- Objective: To quantitatively assess the effects of non-invasive BCI intervention on motor function, sensory function, and the ability to perform activities of daily living (ADL) in SCI patients.
- Study Design: Randomized controlled trial (RCT) or self-controlled trial.
- Participants: Patients with spinal cord injury (AIS grades A-D). The meta-analysis included 109 patients across 9 studies [10].
- Intervention:
- BCI Setup: A non-invasive BCI system, typically using an EEG cap, is configured.
- Paradigm: Patients engage in motor imagery (MI), mentally rehearsing movements (e.g., grasping, walking) without physical execution. The BCI decodes the associated sensorimotor rhythms (EEG power changes in Mu/Beta bands) [10] [5].
- Feedback & Actuation: The decoded motor intention is used to trigger a functional electrical stimulation (FES) device attached to the patient's paralyzed limb or to control a robotic exoskeleton. This creates a closed-loop system where the brain's intention is directly linked to the resulting movement, reinforcing neural pathways [10].
- Outcome Measures:
- Motor Function: ASIA motor score, Lower Extremity Motor Score (LEMS).
- Sensory Function: ASIA sensory scores.
- Activities of Daily Living (ADL): Spinal Cord Independence Measure (SCIM), Barthel Index (BI) [10].
- Key Findings: The meta-analysis concluded that BCI intervention had a statistically significant, medium-effect-size impact on motor function (SMD=0.72) and a large-effect-size impact on sensory function (SMD=0.95) and ADL (SMD=0.85) [10].
Protocol 2: Cognitive-Social Intervention for Autism Spectrum Disorder (ASD)
Non-invasive BCI systems integrated with Virtual Reality (VR) have been developed as intervention tools for school-aged individuals with ASD [7].
- Objective: To improve social and cognitive skills, such as joint attention and emotional recognition, in individuals with ASD.
- Study Design: Controlled intervention study.
- Participants: School-aged children and adolescents diagnosed with ASD.
- Intervention:
- BCI-VR Setup: The user wears a non-invasive EEG headset and a VR headset, creating an immersive and controlled environment.
- Paradigm: The user is presented with social scenarios or cognitive tasks within the VR environment (e.g., recognizing emotions on a virtual character's face, or following a gaze cue).
- Neurofeedback: The BCI system monitors the user's brain states in real-time, such as levels of attention or engagement. Positive performance in the task, or successful self-regulation of the target brain state, is rewarded with success in the VR narrative (e.g., the virtual character smiles), creating a direct feedback loop [7].
- Outcome Measures: Pre- and post-intervention assessments using standardized scales for social responsiveness, cognitive tasks, and analysis of EEG patterns.
- Key Findings: A systematic review of nine such protocols concluded that BCI-VR interventions are safe, with no reported side effects, and show promise for improving core social and cognitive deficits in ASD by leveraging neuroplasticity within a structured and engaging environment [7].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key materials and software tools essential for non-invasive BCI research and experimentation.
| Item Category | Specific Examples | Function & Application in BCI Research |
|---|---|---|
| Signal Acquisition Hardware | EEG systems (e.g., with wet or dry electrodes), fNIRS systems, MEG systems [8] | Measures and digitizes the raw physiological signal from the brain. Dry electrodes are an innovation improving ease of use [8]. |
| Electrodes & Sensors | Ag/AgCl wet electrodes, Gold-plated dry EEG electrodes, fNIRS optodes (light sources & detectors) [8] | The physical interface with the subject; transduces biophysical signals (electrical, optical) into electrical signals. |
| Electrode Gel | Electrolytic gel (for wet EEG systems) | Ensures stable electrical conductivity and reduces impedance between the scalp and electrode. |
| Software Development Kits (SDKs) & Toolboxes | OpenBCI, BCI2000, EEGLAB, FieldTrip [3] | Provides open-source platforms for data acquisition, signal processing, stimulus presentation, and system control, accelerating development. |
| Machine Learning Libraries | Scikit-learn, TensorFlow, PyTorch | Used to build and train custom feature classification and translation algorithms for decoding user intent. |
| Stimulation & Feedback Devices | Functional Electrical Stimulation (FES) systems, robotic exoskeletons, VR headsets [10] [7] | Acts as the effector, converting BCI output commands into functional outcomes for rehabilitation or interaction. |
Non-invasive BCIs represent a dynamic and rapidly advancing frontier in neurotechnology. From their origins in the first EEG recordings to the current development of sophisticated, AI-powered systems for rehabilitation and human-computer interaction, the field has consistently grown in capability and impact. The fundamental principles of signal acquisition, processing, and translation provide a stable framework upon which innovation is built. While challenges remain—particularly in improving signal quality and robustness outside laboratory settings—ongoing research in novel sensors like Digital Holographic Imaging, advanced machine learning algorithms, and user-centered training protocols continues to push the boundaries of what is possible [2] [3] [9]. As these technologies mature, they hold immense potential not only to restore lost function but also to augment human capabilities in the years to come.
Core Neurophysiological Signals and Their Biophysical Origins
Understanding the biophysical origins of neurophysiological signals is foundational to the development and refinement of non-invasive Brain-Computer Interface (BCI) technologies. These signals, which reflect the brain's electrical and hemodynamic activity, provide the primary data source for decoding human intention and cognitive state [2]. The relationship between underlying neural activity and the signals measured by non-invasive techniques is complex, governed by the principles of electromagnetic biophysics and neurovascular coupling [11] [12]. This guide details the core signals leveraged in non-invasive BCIs, specifically examining the physiological processes that generate them and the methodologies required for their experimental investigation. Framed within a broader review of non-invasive BCIs, this resource is intended for researchers and scientists engaged in developing novel diagnostics, neurotherapeutics, and human-machine interaction paradigms.
Core Neurophysiological Signals and Their Measurement
Non-invasive BCIs primarily interface with the brain through two classes of signals: electrophysiological signals, which measure the brain's electrical activity directly, and hemodynamic signals, which measure metabolic changes coupled to neural activity. The following sections and accompanying tables provide a detailed comparison of these signal modalities.
Table 1: Comparison of Core Electrophysiological Signals in Non-Invasive BCI
| Signal Type | Biophysical Origin | Spatial Resolution | Temporal Resolution | Primary Measurement Modality | Key BCI Applications |
|---|---|---|---|---|---|
| Local Field Potentials (LFPs) | Synaptic and dendritic currents from populations of neurons; believed to correlate with BOLD fMRI signals [11]. | ~0.5 - 1 mm (invasively) | Milliseconds | Invasive recordings (ECoG, Utah Array); inferred non-invasively via modeling [12]. | Fundamental research on neural circuit dynamics; reference for HNN modeling of EEG/MEG [12]. |
| Electroencephalography (EEG) | Superficial cortical synaptic activity; summation of synchronized postsynaptic potentials in pyramidal neurons [2] [12]. | Centimeters | ~1-100 milliseconds [13] | Scalp electrodes (10-20 system); wearable wireless sensors [14] [15]. | Motor imagery, P300 speller, cognitive monitoring, neurorehabilitation [13] [16]. |
| Magnetoencephalography (MEG) | Intracellular currents in pyramidal neurons, which generate magnetic fields perpendicular to the electric field measured by EEG [12]. | ~5-10 mm | ~1-100 milliseconds | Superconducting Quantum Interference Devices (SQUIDs) in magnetically shielded rooms [8]. | Mapping sensory and cognitive processing, clinical epilepsy focus localization. |
Table 2: Comparison of Core Hemodynamic Signals in Non-Invasive BCI
| Signal Type | Biophysical Origin | Spatial Resolution | Temporal Resolution | Primary Measurement Modality | Key BCI Applications |
|---|---|---|---|---|---|
| Blood-Oxygen-Level-Dependent (BOLD) fMRI | Changes in local deoxyhemoglobin concentration driven by neurovascular coupling; a mismatch between cerebral blood flow (CBF) and cerebral metabolic rate of oxygen (CMRO2) [11]. | ~1-3 mm | ~1-6 seconds [13] | Functional Magnetic Resonance Imaging (fMRI) scanners. | Brain mapping, connectivity studies, and as a benchmark for other hemodynamic modalities. |
| Functional Near-Infrared Spectroscopy (fNIRS) | Hemodynamic response; changes in concentration of oxygenated (HbO) and deoxygenated hemoglobin (HbR) in cortical blood vessels [13]. | ~1-3 cm | ~1-5 seconds [13] | Wearable headgear with near-infrared light sources and detectors. | Stroke rehabilitation monitoring, motor imagery, passive BCI for cognitive state assessment [13] [17]. |
Quantitative Signal Characteristics
For researchers designing BCI experiments, understanding the quantifiable features of these signals is critical. The table below summarizes key analytical parameters, with a focus on EEG which offers high temporal resolution for dynamic brain monitoring.
Table 3: Quantitative EEG (qEEG) Parameters for BCI Application
| qEEG Parameter | Frequency Range / Calculation | Physiological Correlation & BCI Utility |
|---|---|---|
| Delta Waves | 0.5 - 4.0 Hz | Associated with deep sleep; increased focal power can indicate cortical dysfunction or lesion; useful for monitoring states of impaired consciousness [13]. |
| Theta Waves | 4 - 7 Hz | Linked to memory and emotional processing; can indicate cognitive load or pathology when prominent in awake adults [13]. |
| Alpha Waves | 8 - 12 Hz | Dominant rhythm in relaxed wakefulness with eyes closed; suppression (desynchronization) indicates cortical activation; power <10% may predict poor functional outcome post-stroke [13]. |
| Beta Waves | 13 - 30 Hz | Associated with active concentration and sensorimotor processing; ERD during motor planning/execution is a common BCI input [13]. |
| Gamma Waves | 30 - 150 Hz | Arises from coordinated neuronal firing during demanding cognitive and motor tasks [13]. |
| Power Ratio Index (PRI) | (Delta + Theta Power) / (Alpha + Beta Power) | An increased PRI is associated with recent stroke and poor functional outcomes, serving as a prognostic biomarker in neurorehabilitation [13]. |
| Brain Symmetry Index (BSI) | Mean absolute difference in hemispheric power spectra (1-25 Hz) [13]. | Quantifies interhemispheric asymmetry; values closer to 0 indicate symmetry (healthy), while higher values indicate stroke-related asymmetry; correlates with NIHSS and motor function scores [13]. |
Experimental Methodologies for Signal Acquisition and Analysis
This section provides detailed protocols for acquiring and analyzing the core neurophysiological signals discussed, ensuring methodological rigor and reproducibility.
Protocol for Multimodal EEG-fNIRS Experimentation
This protocol is adapted from studies investigating motor imagery for post-stroke recovery, allowing for the simultaneous capture of electrophysiological and hemodynamic responses [13] [17].
Participant Preparation and Setup:
- EEG Setup: Position an electrode cap according the international 10-20 system. For extended monitoring, use wireless, wearable EEG sensors to improve comfort and compliance [14]. Ensure electrode impedances are maintained below 5 kΩ for optimal signal quality [15].
- fNIRS Setup: Position fNIRS optodes over the motor cortical areas (e.g., C3 and C4 positions of the 10-20 system). Ensure good scalp contact to maximize signal-to-noise ratio.
- Synchronization: Use a hardware or software trigger to synchronize the clocks of the EEG and fNIRS acquisition systems at the start of the experiment [17] [15].
Experimental Paradigm:
- Resting-State Baseline: Record 5 minutes of data while the participant remains at rest with eyes open, followed by 5 minutes with eyes closed. This provides a baseline for both EEG power spectra and hemoglobin concentrations.
- Task Paradigm: Implement a block or event-related design. For motor imagery, instruct the participant to imagine moving their right hand (e.g., for 10 seconds) without performing any actual movement, followed by a rest period (e.g., 20 seconds). Repeat this for multiple trials (e.g., 30-40 trials) and for other limbs (e.g., left hand, feet) as required.
Signal Pre-processing:
- EEG Pre-processing: Apply a band-pass filter (e.g., 0.5-45 Hz). Remove artifacts using automated algorithms (e.g., for ocular, cardiac, and muscle artifacts) or manual inspection. For qEEG analysis, segment data into epochs and transform into the frequency domain using a Fast Fourier Transform (FFT) to calculate Power Spectral Density (PSD) [13] [15].
- fNIRS Pre-processing: Convert raw light intensity signals to optical density, then to concentrations of oxygenated (HbO) and deoxygenated hemoglobin (HbR) using the modified Beer-Lambert law. Apply a band-pass filter to remove physiological noise (e.g., cardiac pulsation ~1 Hz and respiratory cycles ~0.3 Hz) and slow drifts.
Feature Extraction and Multimodal Analysis:
- Unimodal Features: From EEG, extract features such as band power (Alpha, Beta), PRI, and BSI. From fNIRS, extract features like the mean, slope, and peak of the HbO and HbR responses during tasks [13].
- Multilayer Network Analysis: Construct functional brain networks from both EEG and fNIRS data separately. Then, integrate these networks into a multilayer network model to investigate the complementary information between fast electrophysiological and slow hemodynamic connectivity [17].
Protocol for Computational Modeling of EEG/MEG Generators
The Human Neocortical Neurosolver (HNN) provides a method to infer the cellular and network origins of macroscale EEG/MEG signals [12].
Tool Installation and Data Preparation:
- Install HNN software from the public website (https://hnn.brown.edu).
- Prepare the empirical EEG/MEG data. This should be source-localized data representing the current dipole moment over time in ampere-meters (Am) for a specific cortical area.
Forward Model Simulation:
- Input the empirical data into HNN's graphical interface.
- The software's forward model, based on a canonical neocortical circuit, will simulate the primary currents (Jp) generated by intracellular current flow in the dendrites of pyramidal neurons. These currents are the elementary generators of the EEG/MEG signal [12].
Hypothesis Testing and Parameter Manipulation:
- Manipulate model parameters to test hypotheses about the neural circuit dynamics underlying the observed signal. Parameters can include the timing and strength of layer-specific inputs (e.g., thalamocortical inputs), synaptic conductances, and cellular properties.
- Compare the simulated net current dipole output from the model directly with the source-localized empirical data.
Microscale Interpretation:
- Use the model's visualization of microscale features—such as layer-specific local field potentials, individual cell spiking, and somatic voltages—to interpret the circuit-level activity (e.g., the balance of excitation and inhibition) that likely generated the macroscopic signal [12].
Diagram 1: Multimodal EEG-fNIRS experimental workflow for motor imagery tasks, showing parallel processing of electrophysiological and hemodynamic signals.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table catalogues critical hardware, software, and analytical tools required for experimental research in non-invasive BCI.
Table 4: Essential Research Tools for Non-Invasive BCI Development
| Tool / Reagent | Function / Application | Example Specifications / Notes |
|---|---|---|
| EEG Recording System | Acquisition of electrophysiological signals from the scalp. | Includes amplifier (e.g., 32-256 channel), electrode cap (10-20 system), and conductive gel. Systems from companies like TMSI or Brain Products [15]. |
| Wireless/Wearable EEG Sensors | Enables extended-duration, ambulatory EEG monitoring in real-world environments. | Miniaturized, dry-electrode sensors (e.g., REMI sensor), offering high patient acceptance and comfort for long-term use [14]. |
| fNIRS System | Acquisition of hemodynamic signals by measuring cortical oxygenation. | Wearable headgear containing near-infrared light sources and detectors. Offers portability and resistance to motion artifacts compared to fMRI [13]. |
| Multimodal Data Acquisition Software | Synchronized recording from multiple physiological modalities (EEG, fNIRS, ECG, GSR). | Software suites like Neurolab (Bitbrain) enable hardware synchronization for temporal alignment of different data streams [15]. |
| Human Neocortical Neurosolver (HNN) | Open-source software for interpreting the cellular and network origin of human EEG/MEG data. | Uses a biophysical model of a canonical neocortical circuit to simulate current dipoles; allows hypothesis testing without coding [12]. |
| Quantitative EEG (qEEG) Parameters | Analytical metrics for assessing brain state and pathology. | Power Spectral Density (PSD), Power Ratio Index (PRI), Brain Symmetry Index (BSI). Critical for prognostication in stroke and neurorehabilitation [13]. |
Diagram 2: Signaling pathway of the hemodynamic response measured by BOLD-fMRI and fNIRS, showing the relationship between neural activity, neurovascular coupling, and the resulting metabolic changes.
Electroencephalography (EEG), marking its centenary in 2024, remains a fundamental tool for studying human neurophysiology and cognition due to its direct measurement of neuronal activity at millisecond resolution, comparably low cost, and ease of access for multi-site studies [18]. In the specific context of clinical trials for drug development, minimizing patient and clinical site burden is paramount, as lengthy, strenuous site visits can lead to inferior data quality and patient drop-out [18]. Traditional wet-electrode EEG, while considered the gold standard, adds to this burden: electrodes require careful placement with conductive paste, followed by time-consuming cleanup for both patients and staff [18] [19]. These limitations have catalyzed the development and adoption of dry-electrode EEG systems, which operate without conductive gel or complex skin preparation [19]. This transition is a critical component within the broader review of non-invasive Brain-Computer Interface (BCI) technologies, balancing the imperative for high-quality data with the practical needs of modern clinical and research environments. The goal is to provide a comprehensive, technical guide to these innovations, focusing on their performance, applications, and implementation protocols for research scientists and drug development professionals.
Technical Comparison of Electrode Technologies
The core of EEG innovation lies in electrode technology, which acts as the transducer converting the body's ionic currents into electronically processable signals. The choice between wet, dry, and emerging soft electrodes involves a careful trade-off between signal quality, patient comfort, and operational efficiency.
Table 1: Qualitative Comparison of EEG Electrode Types
| Feature | Wet Electrodes | Dry Electrodes | Soft Electrodes |
|---|---|---|---|
| Signal Quality | Strong signal, reliable benchmark [20] | Good, but lower signal correlation possible; susceptible to motion artifacts [20] | Varies with material and manufacturing; stable contact can improve quality [20] |
| Setup Time | Lengthy (requires gel application) [20] | Rapid [18] [20] | Moderate to Rapid [20] |
| Patient Comfort | Discomfort from gel, scalp irritation, messy cleanup [20] | No gel discomfort; can be uncomfortable for long periods [18] [20] | High comfort for extended use, biocompatible [20] |
| Long-Term Recording | Poor (gel dries, altering impedance) [20] | Good (no gel to dry) [21] | Excellent (flexible, conforms to skin) [20] |
| Key Advantage | Established, reliable technology [20] | Speed and ease of use [18] | Biocompatibility and comfort for wearables [20] |
| Primary Limitation | Gel drying affects signal stability; messy [20] | Higher impedance; performance affected by hair and motion [20] | High cost; experimental, limited validation [20] |
Table 2: Quantitative Performance Benchmark from a Clinical Trial Context (2025) [18]
| Device Type | Median Set-up Time (mins) | Median Clean-up Time (mins) | Technician Ease of Set-up (0-10, 10=best) | Technician Ease of Clean-up (0-10, 10=best) |
|---|---|---|---|---|
| Standard Wet EEG | ~20 | ~10 | 7 | 5 |
| Dry-EEG (DSI-24) | ~10 | ~2 | 9 | 9 |
| Dry-EEG (Quick-20r) | ~15 | ~2 | 7 | 9 |
| Dry-EEG (zEEG) | ~15 | ~2 | 7 | 9 |
Dry Electrode Structural Classifications
Dry electrodes can be further categorized based on their structural design and operating principle, which directly impact their performance and suitability for different applications [19]:
- MEMS Dry Electrodes: Utilize micro-needle arrays to gently penetrate the outermost skin layer (stratum corneum) to reduce contact impedance. Materials include silicon (brittle, being phased out), metals, and polymers like PDMS or SU-8 coated with conductive metals (e.g., Gold, Silver) for flexibility and biocompatibility [19].
- Dry Contact Electrodes: Maintain direct contact with the scalp without penetration. They rely on structural designs (e.g., spring-loaded, finger-like) to maintain stable contact, often through hair. Their performance is highly dependent on achieving and maintaining low impedance [19].
- Dry Non-Contact Electrodes: Operate without direct galvanic contact with the skin, measuring capacitive coupling. This eliminates friction and pressure, enhancing comfort, but the signal is more susceptible to environmental noise and motion artifacts [19].
Experimental Protocols and Methodologies for Validation
Rigorous, clinical trial-oriented benchmarking is essential for validating dry-electrode EEG systems. The following methodology, drawn from a recent 2025 study, provides a template for robust comparison [18].
Study Design and Participant Profile
- Objective: To comprehensively compare state-of-the-art dry-electrode EEG devices against a standard wet EEG in a setting that emulates clinical trials as closely as possible.
- Participants: A cohort of n=32 healthy participants is typical for such studies, completing multiple recording days to account for intra- and inter-subject variability.
- Setting: Experiments are performed at a clinical testing site routinely used for early drug development (e.g., Phase 1 & 2 trials) by trained personnel experienced with EEG and clinical trials.
Devices and Montage
- Benchmark Device: A standard wet-EEG system (e.g., QuikCap Neo Net with a Grael amplifier) serving as the gold standard. The montage may include the international 10-20 system plus additional electrodes for comprehensive analysis.
- Dry-Electrode Devices: Three commercially available dry-EEG devices (e.g., DSI-24 from Wearable Sensing, Quick-20R from CGX, zEEG from Zeto) are evaluated. These typically cover the standard 10-20 montage. To ensure a fair comparison, the wet-EEG data can be synthetically subsampled to the 10-20 locations matching the dry devices before preprocessing.
Experimental Tasks and Data Acquisition
The EEG recordings should focus on tasks with biomarker relevance for early clinical trials, including:
- Resting-State Recordings: Eyes-open and eyes-closed conditions to capture baseline brain activity.
- Event-Related Potentials (ERPs): Such as the P300 evoked potential, often used in cognitive assessment.
- Other Task-Related Activity: Auditory and visually driven paradigms to assess various cognitive domains.
Quantitative and Qualitative Metrics
Data collection should encompass both operational and subjective metrics:
- Operational Burden:
- Set-up Time: Measured from start of preparation to start of EEG recording.
- Clean-up Time: Measured from end of recording to a fully cleaned set-up.
- Technician Feedback: Structured questionnaires rating ease of set-up and clean-up on a scale (e.g., 0-10).
- Participant Feedback: Repeated ratings of perceived comfort during the recording to track temporal evolution.
- Signal Quality: Quantitative analysis of the EEG data, including:
- Resting-state quantitative EEG (qEEG)
- ERP amplitude and latency (e.g., P300)
- Power spectral density across frequency bands (e.g., low frequency <6 Hz, induced gamma 40-80 Hz)
Performance Analysis and Application-Specific Utility
The validation of dry-electrode EEG reveals a nuanced performance profile, where utility is highly dependent on the specific application and signal type.
Key Findings from Clinical Benchmarking
The 2025 benchmarking study yielded several critical insights [18]:
- Operational Efficiency: Dry-electrode EEG significantly speeds up experiments. All tested dry devices were faster to set up and clean up than the standard wet EEG, with the fastest device (DSI-24) cutting set-up time by half. Technicians also found dry electrodes easier to work with [18].
- Participant Comfort: Standard wet EEG emerged as the overall most comfortable option, a level that dry-electrode EEG could only match at best. Comfort scores for all devices showed a declining trend over time [18].
- Variable Signal Performance: The quantitative performance of dry-electrode EEG varied strongly across applications. Key findings included:
- Adequate Performance: Quantitative resting-state EEG and P300 evoked activity were adequately captured by dry-electrode EEG, making them suitable for trials where these are primary biomarkers.
- Notable Challenges: Certain signal aspects, such as low-frequency activity (<6 Hz) and induced gamma activity (40–80 Hz), presented significant challenges for the tested dry-electrode systems.
Application in BCI and Neurotechnology
Beyond clinical trials, dry-electrode EEG is a cornerstone of non-invasive BCIs. Its utility spans several domains, bolstered by advances in artificial intelligence for signal processing [19]:
- Emotion Recognition: Using algorithms to classify brainwave patterns associated with different affective states.
- Fatigue and Drowsiness Detection: Monitoring shifts in brain activity indicative of reduced alertness.
- Motor Imagery: Decoding the intention to move a limb, which can be used for prosthetic control or rehabilitation.
- Steady-State Visual Evoked Potentials (SSVEPs): Detecting responses to visual stimuli at specific frequencies, often used for high-speed spelling applications.
Table 3: Dry-Electrode EEG Performance in Key BCI Applications [19]
| BCI Application | Typical Paradigm | Key Signal Features | Dry-EEG Suitability & Notes |
|---|---|---|---|
| Emotion Recognition | Presentation of affective stimuli | Changes in frontal alpha/beta asymmetry; spectral power | Suitable; relies heavily on AI/ML for pattern classification from often noisy signals. |
| Fatigue Detection | Prolonged, monotonous tasks | Increase in theta power, decrease in alpha power | Suitable for longitudinal monitoring; a key advantage of dry systems is long-term wearability. |
| Motor Imagery (MI) | Imagination of limb movement | Event-Related Desynchronization (ERD) in mu/beta rhythms | Moderately suitable; ERD can be obscured by noise, requiring robust preprocessing. |
| P300 ERP | Oddball paradigm | Positive deflection ~300ms post-stimulus | Highly Suitable; consistently shown to be adequately captured by dry EEG systems [18]. |
| SSVEP | Flickering visual stimuli | Oscillatory EEG response at stimulus frequency | Suitable; strong, frequency-specific signals can be reliably detected with dry systems. |
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers designing experiments involving dry-electrode EEG, a set of key materials and technologies is essential.
Table 4: Essential Research Reagents and Materials for Dry-EEG Research
| Item Category | Specific Examples / Models | Function & Rationale |
|---|---|---|
| Dry-EEG Systems | DSI-24 (Wearable Sensing), Quick-20r (CGX), zEEG (Zeto [18] | Primary Data Acquisition: Commercially available systems validated for research and clinical trials. Offer a balance of channel count, portability, and software support. |
| Benchmark Wet-EEG | QuikCap Neo Net with Grael amplifier (Compumedics) [18] | Gold Standard Control: Essential for validating the signal quality and performance of any dry-electrode system in a comparative study. |
| Electrode Materials | Gold (Au), Silver (Ag), Silver/Silver Chloride (Ag/AgCl), Conductive Polymers [20] [19] | Signal Transduction: Material choice impacts impedance, biocompatibility, and long-term stability. Ag/AgCl is a common wet reference; Au and polymers are common for dry. |
| Flexible Substrates | Polydimethylsiloxane (PDMS), Polyimide, Graphene [20] [19] | Conformability & Comfort: Used in "soft" and MEMS electrodes to create flexible, comfortable interfaces that maintain good contact with the scalp. |
| Data Processing Tools | Machine Learning (ML) & Deep Learning (DL) Algorithms (e.g., for classification, regression) [19] | Signal Enhancement & Decoding: Critical for improving the signal-to-noise ratio of dry-EEG and translating brain signals into actionable commands for BCI. |
| Validation Tasks | P300 Oddball, Resting State, Motor Imagery, SSVEP Paradigms [18] [19] | Functional Benchmarking: Standardized experimental protocols to objectively test and compare the performance of different EEG systems. |
The transition from wet to dry electrodes in EEG represents a significant advancement in neurotechnology, particularly for applications demanding low burden and high usability, such as clinical trials and non-invasive BCIs. Evidence from rigorous, clinically-oriented studies demonstrates that dry-electrode EEG can substantially reduce operational time and technician effort while maintaining adequate data quality for a range of applications, including resting-state qEEG and P300 evoked potentials [18]. However, the technology is not a panacea; challenges remain with specific signal types like low-frequency and gamma activity, and patient comfort can be variable [18]. The future of dry-EEG development lies in the coordinated optimization of hardware—through novel materials like graphene and advanced polymer-based MEMS—and sophisticated AI-driven algorithms that can mitigate signal quality issues [19]. For researchers and drug development professionals, the key takeaway is that dry-electrode EEG is a viable and powerful tool, but its successful deployment requires careful matching of the device's capabilities to the specific context of use.
Functional Near-Infrared Spectroscopy (fNIRS) and Hemodynamic Monitoring
Functional Near-Infrared Spectroscopy (fNIRS) is a non-invasive optical neuroimaging technique that enables continuous monitoring of brain function by measuring hemodynamic changes associated with neuronal activity [22]. As a brain-computer interface (BCI) technology, fNIRS offers a unique combination of portability, safety, and moderate spatiotemporal resolution, making it particularly valuable for both clinical and research applications [23] [24]. The core principle of fNIRS relies on tracking neurovascular coupling—the rapid delivery of blood to active neuronal tissue—through quantifying relative concentration changes in oxygenated and deoxygenated hemoglobin [25]. This technical guide examines the fundamental mechanisms, methodological approaches, and implementation protocols of fNIRS-based hemodynamic monitoring within the broader context of non-invasive BCI technologies.
Fundamental Principles of fNIRS
Physiological Basis: Neurovascular Coupling
The foundation of fNIRS rests on neurovascular coupling, the physiological process linking neuronal activation to cerebral hemodynamic changes [24]. When a specific brain region becomes active, the increased neuronal firing rate elevates metabolic demands for oxygen and glucose [24]. This triggers a complex cerebrovascular response:
- Initial oxygen consumption: The sudden increase in neuronal activity causes a brief rise in oxygen utilization, leading to a slight initial increase in deoxygenated hemoglobin (HbR) [26].
- Hemodynamic response: Within 2-5 seconds, cerebral autoregulatory mechanisms trigger localized vasodilation, significantly increasing cerebral blood flow (CBF) to the active region [24].
- Blood oxygenation changes: This increased blood flow delivers oxygen in excess of metabolic demand, resulting in a characteristic increase in oxygenated hemoglobin (HbO) and a concurrent decrease in deoxygenated hemoglobin (HbR) in the venous capillaries [22] [24].
- Return to baseline: After stimulus cessation, hemodynamic parameters gradually return to baseline over 10-15 seconds [26].
This hemodynamic response forms the basis for fNIRS signal detection, with HbO typically demonstrating more pronounced concentration changes than HbR during neuronal activation [23].
Optical Principles and the Modified Beer-Lambert Law
fNIRS utilizes near-infrared light (650-1000 nm wavelength) because biological tissues (skin, skull, dura) demonstrate relatively high transparency in this spectral window, while hemoglobin compounds show distinct absorption characteristics [22] [27]. Within this range, light absorption by water is minimal, while HbO and HbR serve as the primary chromophores (light-absorbing molecules) [24].
The relationship between light attenuation and chromophore concentration is governed by the Modified Beer-Lambert Law [22] [27]:
[ OD = \log\left(\frac{I_0}{I}\right) = \varepsilon \cdot c \cdot d \cdot DPF + G ]
Where:
- (OD) = Optical density
- (I_0) = Incident light intensity
- (I) = Detected light intensity
- (\varepsilon) = Extinction coefficient of chromophore
- (c) = Chromophore concentration
- (d) = Distance between source and detector
- (DPF) = Differential pathlength factor
- (G) = Geometry-dependent factor
By emitting light at multiple wavelengths and measuring attenuation, fNIRS calculates relative concentration changes of HbO and HbR based on their distinct absorption spectra [27]. Below 800 nm, HbR has a higher absorption coefficient, while above 800 nm, HbO is more strongly absorbed [24].
Figure 1: Neurovascular Coupling Pathway. This diagram illustrates the physiological sequence from neuronal activation to detectable fNIRS signals.
fNIRS Instrumentation and Technology
System Components and Configuration
A typical fNIRS system consists of several integrated components that work in concert to generate, transmit, detect, and process near-infrared light [27]:
Light Sources generate near-infrared light at specific wavelengths, typically between 650-1000 nm [22]. Two primary technologies are employed:
- Light-Emitting Diodes (LEDs): Offer advantages in portability, power efficiency, and cost-effectiveness, suitable for most applications with penetration depths up to 2 cm [27].
- Laser Diodes: Provide higher intensity, monochromaticity, and directionality, enabling deeper penetration (up to 3 cm) but often requiring optical fibers and more complex instrumentation [27].
Detectors capture photons that have traversed brain tissue. Common detector types include:
- Pin Photodetectors (PDs): Simple, portable, and low-power but lack internal gain mechanisms [27].
- Avalanche Photodiodes (APDs): Feature internal gain (10 to few 100×), higher sensitivity, and faster response than PDs [27].
- Photomultiplier Tubes (PMTs): Offer extremely high gain (up to 10⁷) and sensitivity but require high voltage supplies and cooling systems, limiting portability [27].
Optical Probes arrange sources and detectors in specific geometries on the scalp. The distance between sources and detectors (typically 3-5 cm) determines penetration depth and spatial resolution [22] [24]. Flexible caps, headbands, or rigid grids maintain proper optode positioning and skin contact.
Data Acquisition System controls light source modulation, synchronizes detection, amplifies signals, and converts analog measurements to digital format for analysis [27].
fNIRS System Types
Three primary fNIRS system architectures have been developed, each with distinct operational principles and applications [24]:
Table 1: fNIRS System Types and Characteristics
| System Type | Operating Principle | Advantages | Limitations | Common Applications |
|---|---|---|---|---|
| Continuous Wave (CW) | Measures light intensity attenuation | Simple, portable, cost-effective, most common | Cannot measure absolute pathlength or concentration | Most BCI and clinical applications [24] |
| Frequency Domain (FD) | Modulates light intensity at radio frequencies; measures amplitude decay and phase shift | Can resolve absorption and scattering coefficients; provides pathlength measurement | More complex and expensive than CW systems | Tissue oxygenation monitoring, quantitative studies [24] |
| Time Domain (TD) | Uses short light pulses; measures temporal point spread function | Highest information content; separates absorption and scattering | Most complex, expensive, and bulky | Research requiring depth resolution [24] |
fNIRS Signal Processing and Analysis
Standard Processing Pipeline
fNIRS data processing follows a structured pipeline to extract meaningful hemodynamic information from raw light intensity measurements [22] [23]:
Figure 2: fNIRS-BCI Signal Processing Workflow. This diagram outlines the standard sequence from raw signal acquisition to interpretable output.
Preprocessing Methods
Preprocessing aims to remove artifacts and enhance signal quality through several approaches:
- Band-pass filtering: Removes physiological noise (cardiac ~1 Hz, respiratory ~0.3 Hz) and very low-frequency drift [23].
- Adaptive filtering: Effectively separates cerebral signals from systemic physiological interference [23].
- Independent Component Analysis (ICA): Identifies and removes artifacts based on statistical independence [23].
- Motion artifact correction: Algorithms specifically designed to identify and compensate for movement-induced signal distortions [25].
Feature Extraction and Classification
For BCI applications, processed hemodynamic signals are converted into discriminative features for classification:
Common Feature Types [23]:
- Mean, peak value, variance of HbO/HbR responses
- Signal slope during initial rise/fall phases
- Higher-order statistics (skewness, kurtosis)
- Waveform morphology parameters
Classification Algorithms [23]:
- Linear Discriminant Analysis (LDA): Simple, computationally efficient, provides good performance for many fNIRS-BCI tasks
- Support Vector Machines (SVM): Effective for non-linear classification problems
- Hidden Markov Models (HMM): Captures temporal dynamics of hemodynamic responses
- Artificial Neural Networks: Powerful for complex pattern recognition with sufficient training data
Experimental Protocols and Methodologies
Protocol Design Considerations
Well-designed experimental protocols are essential for obtaining reliable fNIRS data. Key considerations include:
Paradigm Selection:
- Block design: Alternating periods of task and rest (typically 20-30s each); provides robust signals suitable for initial studies [26].
- Event-related design: Brief, randomized stimuli; allows examination of hemodynamic response shape and timing [26].
- Mixed designs: Combine elements of both block and event-related approaches.
Task Selection Based on Target Brain Regions:
- Prefrontal cortex: Mental arithmetic, working memory tasks, emotional induction, music imagery [23].
- Motor cortex: Motor execution or imagery of limb movements, finger tapping sequences [23].
- Visual cortex: Pattern recognition, visual stimulation tasks.
Standardized Experimental Procedure
A typical fNIRS experiment follows this sequence:
Participant Preparation (10-15 minutes):
- Explain procedure and obtain informed consent
- Measure head circumference and mark fiducial points (nasion, inion, pre-auricular points)
- Position fNIRS cap or probe set according to international 10-20 system or specific cortical landmarks
- Verify signal quality at all channels
Baseline Recording (5-10 minutes):
- Record resting-state activity with eyes open or closed
- Establish individual hemodynamic baseline values
Task Execution (variable, typically 30-60 minutes total):
- Present task instructions and practice trials
- Conduct experimental runs with appropriate rest periods between blocks
- Monitor signal quality throughout session
- Record behavioral performance data synchronized with fNIRS acquisition
Post-experiment Procedures (5 minutes):
- Document probe locations with digital photography or 3D digitization
- Remove equipment and debrief participant
Quality Control Measures
- Signal Quality Assessment: Verify adequate signal-to-noise ratio (>10 dB typically acceptable) [27]
- Motion Artifact Identification: Visual inspection and algorithmic detection of movement-related signal distortions [25]
- Physiological Monitoring: Simultaneous recording of heart rate and respiration can aid artifact rejection [23]
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Materials and Equipment for fNIRS Research
| Item Category | Specific Examples | Function/Purpose | Technical Considerations |
|---|---|---|---|
| fNIRS Instrumentation | Continuous Wave systems (e.g., Hitachi ETG series, NIRx NIRScout) | Generate and detect NIR light; core measurement platform | Channel count, sampling rate, portability, compatibility with auxiliary systems [22] |
| Optical Components | LED/laser sources (690nm, 830nm typical), silicon photodiodes/APDs, fiber optic bundles | Light generation, transmission, and detection | Wavelength options, source intensity, detector sensitivity, fiber flexibility [27] |
| Probe Design Materials | Flexible silicone optode holders, spring-loaded probes, 3D-printed mounts | Maintain optode-scalp contact and positioning geometry | Probe density, customization capability, stability during movement [22] |
| Auxiliary Monitoring | ECG electrodes, respiratory belt, motion capture systems | Record physiological signals for noise regression and artifact correction | Synchronization capability, sampling rate, compatibility with fNIRS system [23] |
| Data Analysis Software | Homer2, NIRS-KIT, MNE-NIRS, custom MATLAB/Python scripts | Signal processing, statistical analysis, visualization | Processing pipeline flexibility, supported algorithms, visualization capabilities [23] |
| Head Localization | 3D digitizers (Polhemus), photogrammetry systems | Precisely document optode positions relative to head landmarks | Accuracy, measurement time, integration with analysis software [23] |
Comparative Analysis with Other Non-Invasive BCIs
Technical Benchmarking
fNIRS occupies a distinct position in the landscape of non-invasive neural monitoring technologies, offering complementary advantages and limitations compared to other modalities:
Table 3: Comparison of Non-Invasive Brain Monitoring Technologies for BCI Applications
| Parameter | fNIRS | EEG | fMRI | MEG |
|---|---|---|---|---|
| Spatial Resolution | 1-3 cm (moderate) [24] | 1-10 cm (poor) [2] | 1-5 mm (high) [24] | 3-10 mm (high) [8] |
| Temporal Resolution | 0.1-1 second (moderate) [24] | <100 ms (excellent) [2] | 1-3 seconds (poor) [24] | <10 ms (excellent) [8] |
| Penetration Depth | Cortical surface (2-3 cm) [27] | Cortical surface | Whole brain | Cortical surface |
| Portability | High [24] [25] | Moderate to high [2] | None (fixed system) | Limited (shielded room) [8] |
| Tolerance to Movement | Moderate [25] | Low (highly motion-sensitive) | Very low | Very low |
| Signal Origin | Hemodynamic (metabolic) | Electrical (neuronal) | Hemodynamic (metabolic) | Magnetic (neuronal) |
| Primary Artifacts | Physiological noise, motion | Ocular/muscular, line noise, motion | Motion, physiological noise | Environmental magnetic fields |
| Cost | Moderate [25] | Low to moderate | Very high | Very high |
Hybrid Approaches: fNIRS-EEG Integration
Combining fNIRS with EEG creates a powerful multimodal platform that captures both hemodynamic and electrophysiological aspects of brain activity simultaneously [23] [27]. This integration offers several advantages:
- Complementary Information: fNIRS provides better spatial localization of cortical activation, while EEG offers superior temporal resolution of neural dynamics [23].
- Artifact Reduction: fNIRS signals can help identify and remove physiological artifacts in EEG data [23].
- Enhanced Classification Accuracy: Combined features often improve BCI performance over either modality alone [23].
- Comprehensive Neurovascular Assessment: Enables investigation of relationships between electrical brain activity and hemodynamic responses [26].
Technical implementation requires careful synchronization of acquisition systems, compatible probe designs that accommodate both modalities, and integrated data analysis approaches [23].
Applications in Clinical and Research Settings
Neurological Rehabilitation
fNIRS has demonstrated significant utility in monitoring and guiding neurorehabilitation:
- Stroke Recovery: Tracking cortical reorganization during motor and cognitive rehabilitation; identifying compensatory activation patterns in ipsilateral hemispheres [24].
- Spinal Cord Injury: Providing alternative control pathways through BCI-based neurofeedback training; showing potential to improve motor function, sensory function, and activities of daily living [10].
- Cognitive Training: Real-time monitoring of prefrontal cortex activity during working memory and executive function tasks [25].
BCI Communication and Control
fNIRS-BCIs offer communication pathways for severely paralyzed patients:
- Binary Communication: Using mental arithmetic, motor imagery, or other cognitive tasks to encode "yes/no" responses [23].
- Advanced Control: Operating assistive devices, wheelchairs, or neuroprostheses through pattern classification of hemodynamic responses [22] [10].
- Commercial Integration: Recent developments enable direct BCI control of consumer devices (e.g., Apple's BCI Human Interface Device profile) [28].
Current Limitations and Future Directions
Despite significant advances, fNIRS technology faces several challenges that guide ongoing research and development:
Technical Limitations
- Depth Sensitivity: Limited to cortical surfaces (typically <3 cm), unable to access subcortical structures [22].
- Spatial Resolution: Inferior to fMRI due to photon scattering in biological tissues [24].
- Physiological Contamination: Systemic physiological changes (blood pressure, heart rate, respiration) can confound cerebral signals [23].
- Individual Anatomical Variability: Skull thickness, cerebrospinal fluid distribution, and other anatomical factors affect light propagation [22].
Emerging Innovations
- High-Density Arrays: Denser optode arrangements enabling tomographic reconstruction and improved spatial resolution [22].
- Wearable Platforms: Fully portable, wireless systems for naturalistic monitoring outside laboratory environments [25].
- Advanced Analysis Methods: Machine learning and deep learning approaches for improved pattern recognition and classification [27].
- Miniaturized Hardware: Integration with wearable electronics and consumer-grade head-mounted devices [28] [8].
- Hybrid Neuroimaging: Continued development of integrated fNIRS-EEG and fNIRS-fMRI platforms for comprehensive brain monitoring [23] [27].
The future trajectory of fNIRS points toward more accessible, robust, and clinically integrated systems that leverage technological advancements in photonics, materials science, and artificial intelligence to expand our understanding of brain function and enhance BCI applications across diverse settings.
Brain-Computer Interface (BCI) technology is undergoing a significant transformation, driven by the demand for high-performance non-invasive systems. While established methods like electroencephalography (EEG) are widely used, their applications are often limited by spatial resolution and signal-to-noise ratio [29]. Emerging modalities are challenging these limitations, offering new pathways to decode neural activity without surgical implants. Two technologies at the forefront of this innovation are wearable Magnetoencephalography (MEG) and Digital Holographic Imaging (DHI). Wearable MEG, leveraging quantum-derived optical pumping, enables unshielded neural recording, while DHI detects nanoscale neural tissue deformations, representing a novel signal class for BCI [9] [30]. This whitepaper provides an in-depth technical analysis of these two modalities, detailing their operating principles, experimental protocols, and comparative standing within the non-invasive BCI landscape, serving as a resource for researchers and drug development professionals.
Wearable Magnetoencephalography (MEG)
Traditional MEG systems are cryogenically cooled and require bulky magnetic shielding, confining their use to controlled laboratory settings [30]. Wearable MEG systems overcome these limitations through Optically Pumped Magnetometers (OPMs). OPMs are compact, highly sensitive magnetic field sensors that operate at room temperature. Their principle is grounded in atomic physics: a vapor cell containing alkali atoms (e.g., Rubidium) is optically pumped with a laser to polarize the atomic spins. When the weak magnetic fields produced by neuronal currents in the brain interact with this polarized ensemble, they cause a measurable change in the atoms' quantum spin state, which is probed by a second laser [30]. This allows for direct detection of neuromagnetic signals with a sensitivity comparable to traditional MEG but with a form factor that enables sensor placement directly on the scalp in a wearable helmet or headset.
Digital Holographic Imaging (DHI)
In contrast to measuring magnetic fields or electrical potentials, DHI detects a fundamentally different physiological correlate of neural activity: nanoscale mechanical deformations of neural tissue that occur during neuronal firing. Researchers at Johns Hopkins APL have developed a DHI system that functions as a remote sensing tool for the brain [9] [31]. The system actively illuminates neural tissue with a laser and records the scattered light on a specialized camera to form a complex image. By analyzing the phase information of this light with nanometer-scale sensitivity, the system can spatially resolve minute changes in brain tissue velocity correlated with action potentials [9]. This approach treats the brain as a complex, cluttered environment where the target signal—neural tissue deformation—must be isolated from physiological noise such as blood flow and respiration.
Quantitative Data and Performance Comparison
The table below summarizes key performance metrics for emerging non-invasive BCI modalities alongside established technologies.
Table 1: Performance Comparison of Non-Invasive BCI Modalities
| Technology | Spatial Resolution | Temporal Resolution | Penetration Depth | Key Measured Signal | Form Factor & Key Advantage |
|---|---|---|---|---|---|
| Wearable MEG (OPM-based) | High (Sub-centimeter) [30] | High (Milliseconds) [30] | Whole Cortex [30] | Magnetic fields from neuronal currents [30] | Wearable helmet; Unshielded operation [30] |
| Digital Holographic Imaging (DHI) | High (Potential for micron-scale) [9] | High (Milliseconds) [9] | Superficial cortical layers (initially) [9] | Nanoscale tissue deformation from neural activity [9] | Bench-top system; Novel signal source & measures intracranial pressure [9] [31] |
| EEG | Low (Several centimeters) [29] | High (Milliseconds) [29] | Whole Cortex [29] | Scalp electrical potentials [29] | Wearable cap; Established & portable [29] |
| fNIRS | Low (1-2 cm) [30] | Low (Seconds) [30] | Superficial cortical layers [30] | Hemodynamic response (blood oxygenation) [30] | Wearable headband; Tracks hemodynamics [30] |
Table 2: Key Research Reagent Solutions for Emerging BCI Modalities
| Item | Function in Research | Specific Example / Technology |
|---|---|---|
| Alkali Vapor Cell | Core sensing element of an OPM; its quantum spin state is altered by neuromagnetic fields. | Rubidium-87 vapor cell in wearable MEG systems [30]. |
| Narrow-Linewidth Laser Diode | Used for optical pumping and probing of the atomic spins in OPMs. | Tuneable laser source for OPM-MEG [30]. |
| Digital Holographic Camera | Records complex wavefront (amplitude and phase) of laser light scattered from neural tissue. | Specialized camera used in Johns Hopkins APL DHI system [9]. |
| Low-Coherence Laser Illuminator | Provides the coherent light source required for holographic interferometry in DHI. | Laser illuminator in the DHI system [9]. |
| Real-Time Signal Processing Unit | Hardware/Software for filtering physiological clutter and extracting neural signals. | Custom software for separating neural tissue velocity from heart rate and blood flow [9] [31]. |
Detailed Experimental Protocols
Protocol for Wearable MEG with OPMs
This protocol outlines the procedure for conducting a motor imagery task using a wearable MEG system.
A. Materials and Setup
- OPM Sensor Array: A helmet or headset integrated with multiple OPM sensors (e.g., based on Rubidium vapor cells).
- Biomagnetic Shielding: While OPMs enable operation in less shielded environments, a compact, active magnetic shielding system is often used for improved signal quality.
- Data Acquisition (DAQ) System: A multi-channel system synchronized to the OPM controls.
- Stimulus Presentation Interface: A monitor or set of headphones to deliver cues to the participant.
- Participant Preparation: The participant dons the wearable MEG helmet. No skin preparation or conductive gel is required. Sensor positions are co-registered with the participant's head anatomy using a digitizer or built-in cameras.
B. Procedure
- System Calibration: The OPM sensors are activated and calibrated. This involves tuning the laser frequencies and magnetic fields to the operating point of the vapor cells for maximum sensitivity.
- Baseline Recording (5 minutes): The participant is instructed to relax with their eyes open, followed by eyes closed, to record a baseline of brain activity and environmental noise.
- Task Execution:
- The participant is seated comfortably and presented with a visual cue (e.g., an arrow pointing left or right) on the stimulus interface.
- Upon seeing the cue, the participant is instructed to imagine moving the corresponding hand (e.g., clenching their left or right fist) without performing any actual movement. Each imagery trial lasts for 4 seconds, followed by a rest period.
- A block of 60-100 trials (30-50 per hand) is performed.
- Data Acquisition: Throughout the task, the DAQ system continuously records the magnetic field data from all OPM channels, time-locked to the task cues.
C. Data Analysis
- Pre-processing: Data is filtered (e.g., 1-40 Hz bandpass) to remove low-frequency drift and high-frequency noise. Artifact rejection algorithms are applied to remove contamination from eye blinks and muscle movement.
- Source Modeling: The cleaned sensor-level data is projected onto a cortical source model derived from an MRI of the participant's brain. This reconstructs the originating neural currents.
- Feature Extraction & Classification: Event-Related Desynchronization (ERD) in the mu (8-12 Hz) and beta (13-30 Hz) frequency bands over the motor cortex is extracted for each trial. A machine learning classifier (e.g., Support Vector Machine) is trained to distinguish between left- and right-hand motor imagery based on these features.
Wearable MEG Experimental Workflow
Protocol for Validating DHI Neural Signals
This protocol describes the core experimental methodology, initially validated in animal models, to confirm that DHI signals are correlated with neural activity.
A. Materials and Setup
- Digital Holographic Imaging System: Comprising a low-coherence laser illuminator, a high-speed camera capable of recording phase information, and a computer for hologram reconstruction.
- In Vivo Cranial Window Preparation: A surgically implanted transparent window into the skull of an anesthetized animal model (e.g., mouse) to provide optical access to the cortex.
- Electrophysiology Setup: A multi-electrode array (MEA) or patch-clamp electrode for simultaneous electrical recording of neural activity (the "gold standard").
- Stimulus Delivery System: Equipment for controlled sensory or electrical stimulation (e.g., a current stimulator for the whisker pad or a foot shock).
B. Procedure
- Surgical Preparation: An animal model is anesthetized, and a cranial window is surgically prepared over the target brain region (e.g., somatosensory cortex).
- System Alignment: The DHI system is aligned to illuminate the cortical tissue through the cranial window. The electrophysiology electrode is positioned to record from the same region.
- Co-registered Recording:
- A controlled stimulus (e.g., a mild electrical pulse to the whisker pad) is administered.
- Simultaneously, the DHI system records a high-speed video sequence of the laser light scattered from the brain tissue.
- The MEA records the resulting electrical neural activity (action potentials and local field potentials).
- Data Collection: This co-registered recording is repeated over hundreds of trials to build a robust dataset for correlation analysis.
C. Data Analysis
- Hologram Processing: The recorded holographic video is processed to reconstruct complex wavefronts, from which nanometer-scale displacements of the tissue over time are calculated, producing a "tissue velocity" map.
- Signal Correlation:
- The timing of the DHI-derived tissue deformation signal is precisely aligned with the electrophysiology recording.
- Cross-correlation analysis is performed between the tissue velocity and the multi-unit activity or local field potential from the MEA.
- A strong, consistent temporal correlation between the electrical spiking and the tissue deformation validates the DHI signal as a proxy for neural activity [9].
DHI Signal Validation Workflow
Current Research Status and Future Trajectory
Wearable MEG
Wearable MEG is transitioning from proof-of-concept demonstrations to application in basic neuroscience and clinical research. The current focus is on improving sensor miniaturization, robustness against environmental interference, and developing algorithms for motion correction and source localization in a dynamic, wearable setting [30]. The modality's ability to provide high-fidelity neural data in unshielded environments positions it as a strong candidate for studying brain network dynamics in naturalistic postures and for long-term monitoring of neurological conditions.
Digital Holographic Imaging
DHI is at an earlier stage of development, with the foundational research successfully demonstrating the detection of a novel neural signal in animal models [9]. The immediate research priority, as stated by the Johns Hopkins APL team, is to demonstrate the potential for basic and clinical neuroscience applications in humans [9] [31]. Key challenges include scaling the technology for human use, improving the penetration depth to access deeper brain structures, and further refining signal processing techniques to isolate neural signals from the complex physiological background in a clinical setting. The serendipitous discovery of its ability to non-invasively measure intracranial pressure suggests a near-term clinical application that could run in parallel to BCI development [31].
Wearable MEG and Digital Holographic Imaging represent two pioneering frontiers in non-invasive BCI. Wearable MEG enhances an established neuroimaging technique with unprecedented flexibility, while DHI introduces a completely new biophysical signal for decoding brain activity. Both modalities offer high spatial and temporal resolution, addressing critical limitations of current non-invasive technologies. For researchers and pharmaceutical developers, these tools promise not only future BCI applications but also new avenues for understanding neural circuitry, evaluating neuro-therapeutics, and monitoring brain health in real-time. The ongoing maturation of these technologies will be critical in shaping a future where high-fidelity, non-invasive brain-computer interfacing is a practical reality.
In non-invasive brain-computer interface (BCI) research, the interplay between spatial and temporal resolution represents a fundamental determinant of system capability and application suitability. Neural signals captured through the skull and scalp present researchers with an inherent technological trade-off: no single non-invasive modality currently provides both high spatial fidelity and high temporal precision. This whitepaper provides a technical analysis of this resolution trade-off across major non-invasive BCI technologies, examining how these characteristics influence experimental design, data interpretation, and practical application in clinical and research settings. The convergence of improved sensor hardware with advanced machine learning algorithms is gradually mitigating these limitations, yet the underlying physical and physiological constraints continue to define the boundaries of what is achievable in non-invasive neural interfacing [32] [2].
Fundamental Concepts in BCI Signal Acquisition
Defining Resolution Metrics
In BCI research, temporal resolution refers to the precision with which a system can measure changes in neural activity over time, typically quantified in milliseconds. This metric determines a system's ability to track rapid neural dynamics such as action potentials and oscillatory activity. Spatial resolution, conversely, describes the smallest distinguishable spatial detail in neural activation patterns, typically measured in millimeters, determining how precisely a system can localize brain activity to specific cortical regions [2].
The inverse problem in neuroimaging stems from the mathematical challenge of inferring precise locations of neural activity within the brain from measurements taken at the scalp surface. This problem is inherently ill-posed, as infinite configurations of neural sources can produce identical surface potential patterns, creating fundamental limitations for spatial localization in non-invasive systems [32].
Physiological Basis of Neural Signals
Non-invasive BCIs primarily measure two types of neural correlates: electromagnetic fields generated by postsynaptic potentials and hemodynamic responses related to metabolic demands. Electromagnetic fields propagate nearly instantaneously but diffuse through resistive tissues, while hemodynamic responses reflect metabolic changes with inherent latency of 1-5 seconds, creating the fundamental dichotomy between fast but blurry signals and slow but localized measurements [2] [33].
Comparative Analysis of Non-Invasive BCI Modalities
Quantitative Resolution Characteristics
Table 1: Technical Specifications of Major Non-Invasive BCI Modalities
| Modality | Spatial Resolution | Temporal Resolution | Penetration Depth | Primary Signal Origin | Key Limitations |
|---|---|---|---|---|---|
| EEG | ~1-3 cm (Low) | <1 ms (Very High) | Superficial cortical layers | Post-synaptic potentials | Skull blurring, poor deep source localization, low signal-to-noise ratio [32] [2] |
| fNIRS | ~1-2 cm (Medium) | 1-5 seconds (Low) | Superficial cortical layers | Hemodynamic response (blood oxygenation) | Slow hemodynamic response, sensitivity to scalp blood flow [32] [34] |
| MEG | ~3-5 mm (High) | <1 ms (Very High) | Entire cortex | Magnetic fields from postsynaptic currents | Bulky equipment, magnetic shielding requirements, high cost [32] [8] |
| fMRI | 1-3 mm (Very High) | 1-5 seconds (Low) | Whole brain | Hemodynamic response (BOLD effect) | Poor temporal resolution, expensive, immobile [33] |
| fUS | ~0.3-0.5 mm (Ultra-High) | ~1-2 seconds (Medium) | Several centimeters | Cerebral blood volume | Requires acoustic window, emerging technology [32] |
Technical Trade-offs and Performance Envelopes
Table 2: Performance Characteristics and Application Suitability
| Modality | Signal-to-Noise Ratio | Portability | Setup Complexity | Best-Suited Applications |
|---|---|---|---|---|
| EEG | Low to Medium | High | Low | Real-time communication, seizure detection, sleep monitoring, cognitive state assessment [2] [8] |
| fNIRS | Medium | Medium | Medium | Neurofeedback, clinical monitoring, brain activation mapping [32] [34] |
| MEG | High | Low | Very High | Basic cognitive neuroscience, epilepsy focus localization, network connectivity [32] [8] |
| fMRI | High | Low | Very High | Precise functional localization, surgical planning, connectomics [33] |
| fUS | Very High (preclinical) | Medium (potential) | High | High-resolution functional imaging, small animal research [32] |
The relationship between spatial and temporal resolution across modalities reveals a fundamental technology frontier where improvements in one dimension typically come at the expense of the other. This trade-off landscape creates distinct application niches for each modality and drives research into multimodal approaches that combine complementary strengths [32].
Experimental Methodologies for Resolution Assessment
Standard Protocols for Characterizing BCI Performance
Temporal Resolution Validation employs repetitive sensory stimulation (visual, auditory, or somatosensory) with inter-stimulus intervals progressively decreased until the system can no longer resolve individual responses. For EEG, this involves presenting stimuli at frequencies from 0.5 Hz to 30+ Hz while measuring the accuracy of response detection and latency measurements. The steady-state visual evoked potential (SSVEP) paradigm represents a standardized approach where subjects view stimuli flickering at specific frequencies while researchers quantify the signal-to-noise ratio of the elicited responses at each frequency [35].
Spatial Resolution Assessment utilizes focal activation paradigms with known neuroanatomical correlates. The finger-tapping motor task reliably activates the hand knob region of the contralateral motor cortex, allowing researchers to quantify the spatial spread of detected activation. For high-density EEG systems, this involves measuring the topographic distribution of sensorimotor rhythm desynchronization during motor imagery and comparing it to the expected focal pattern [33].
Signal-to-Noise Ratio (SNR) Quantification follows standardized metrics such as the wide-band SNR for SSVEP-based BCIs, which calculates the ratio of signal power at stimulation frequencies to the average power in adjacent non-stimulation frequency bins. This approach enables objective comparison across systems and subjects, with higher SNR values indicating better signal quality and potentially higher information transfer rates [35].
Multimodal Integration Protocols
Simultaneous EEG-fMRI recording requires careful artifact mitigation, particularly the removal of ballistocardiographic artifacts in EEG data caused by cardiac-induced head movement in the magnetic field. This approach leverages fMRI's high spatial resolution to constrain the source localization of EEG signals, effectively creating a hybrid modality with both high temporal and spatial resolution [33].
EEG-fNIRS co-registration provides complementary measures of electrical and hemodynamic activity with relatively straightforward technical implementation. Experimental protocols typically synchronize data acquisition systems and use common triggers, with fNIRS optodes placed within the EEG electrode array based on the international 10-20 system. The combined system can track both immediate neural responses (via EEG) and subsequent metabolic changes (via fNIRS) to the same stimuli [32] [2].
Advanced Technical Approaches
Resolution Enhancement Strategies
Sensor Hardware Innovations include high-density electrode arrays (256+ channels) for EEG systems that improve spatial sampling, and dry electrodes that facilitate quicker setup for practical applications. For fNIRS, high-density arrangements of sources and detectors enable tomographic reconstruction approaches that significantly improve spatial resolution beyond conventional topographical mapping [32] [8].
Source Localization Algorithms employ distributed inverse solution methods such as weighted minimum norm estimates (wMNE) and low-resolution electrical tomography (LORETA) to estimate cortical source distributions from scalp EEG recordings. These algorithms incorporate anatomical constraints from structural MRI to improve localization accuracy, partially overcoming the intrinsic limitations of the inverse problem [32].
Machine Learning Enhancement utilizes deep learning architectures trained on large-scale multimodal datasets to learn mapping functions between low-resolution surface measurements and high-resolution neural activity patterns. Self-supervised pretraining across hundreds of subjects has demonstrated significant improvements in decoding accuracy from non-invasive signals, effectively enhancing functional resolution through statistical inference [32].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Experimental Materials for BCI Resolution Studies
| Category | Specific Materials/Reagents | Primary Function | Technical Considerations |
|---|---|---|---|
| Electrode Technologies | Wet electrodes (Ag/AgCl), Dry contact electrodes, Multi-electrode arrays (256+ channels) | Signal acquisition with optimal skin-electrode interface | Electrode impedance determines signal quality; high-density arrays improve spatial sampling [8] |
| Optical Components | LED/laser sources (690-850 nm), Silicon photodiodes, Time-domain/frequency-domain systems | fNIRS light emission and detection | Wavelength selection determines penetration depth and oxygenation measurement specificity [32] [34] |
| Conductive Media | Electrolyte gels, Saline solutions, Conductive pastes | Bridge impedance between skin and electrode | Composition affects impedance stability and recording duration; hypoallergenic formulations reduce skin irritation [8] |
| Phantom Materials | Head phantoms with realistic layers, Synthetic tissues with matched impedance | System validation and calibration | Materials must replicate electrical/optical properties of real tissues for accurate performance assessment [35] |
| Computational Tools | Open-source processing pipelines (EEGLAB, FieldTrip, NIRS-KIT), Deep learning frameworks | Signal processing and analysis | Standardized pipelines enable reproducible analysis; machine learning enhances decoding accuracy [32] [35] |
Future Directions and Emerging Solutions
Technological Convergence Pathways
Functional Ultrasound (fUS) imaging represents a promising emerging modality that potentially bridges the resolution trade-off gap, offering both high spatial resolution (~0.3-0.5 mm) and reasonable temporal resolution (~1-2 seconds) without the size and cost constraints of fMRI. Though currently requiring an acoustic window for optimal performance, transcranial approaches are under active development [32].
Hybrid MEG Systems incorporating optically pumped magnetometers (OPMs) offer the potential for wearable MEG systems that overcome the stationary limitations of traditional SQUID-based systems. These emerging technologies maintain the high temporal and spatial resolution of conventional MEG while enabling movement-tolerant recording environments [32] [8].
AI-Enhanced Resolution approaches leverage large-scale self-supervised learning across massive multimodal datasets to effectively enhance functional resolution. Recent demonstrations show that models pretrained on hundreds of hours of EEG data can decode speech perception and limited inner speech with accuracy previously only achievable with invasive methods [32].
Application-Specific Resolution Requirements
Different BCI applications demand distinct resolution profiles. Communication BCIs for locked-in patients prioritize temporal resolution to maximize information transfer rate, often employing SSVEP paradigms that can achieve rates exceeding 5.42 bits per second [35]. Neurorehabilitation applications require moderate spatial resolution to target specific cortical regions while maintaining sufficient temporal resolution to provide real-time feedback [2]. Brain state monitoring for cognitive assessment typically balances both resolution dimensions to identify distributed network patterns evolving over seconds to minutes [32] [2].
The ongoing resolution optimization across non-invasive BCI modalities continues to expand the application frontier while highlighting the persistent physical and biological constraints that define fundamental limits. Strategic selection of modalities and emerging hybrid approaches will drive the next generation of non-invasive neural interfaces, with resolution characteristics remaining a primary consideration in system design and application targeting [32] [8].
Brain-Computer Interface (BCI) technology represents a revolutionary frontier in direct communication between the human brain and external devices. Non-invasive BCIs, which require no surgical implantation, are gaining significant traction due to their safety profile, accessibility, and potential for widespread application across healthcare, research, and consumer domains. These systems typically use sensors placed on the scalp to monitor brain activity, translating neural signals into executable commands for external devices [36]. The global non-invasive BCI market, valued at $3.89 billion in 2025, is projected to grow at a compound annual growth rate (CAGR) of 16.57%, reaching $8.45 billion by 2034 [36]. This growth is largely driven by technological advancements in machine learning, sensor technology, and increasing demand for brain-controlled assistive technologies [36]. This whitepaper provides an in-depth analysis of the current non-invasive BCI ecosystem, examining key research institutions, global market trends, experimental methodologies, and the future trajectory of this rapidly evolving field.
The non-invasive BCI market is characterized by dynamic growth, regional variation, and diverse application sectors. The following tables summarize key quantitative data for the global landscape.
Table 1: Global Non-Invasive BCI Market Size and Projections
| Metric | Value |
|---|---|
| 2025 Market Size | USD 3.89 Billion [36] |
| 2034 Projected Market Size | USD 8.45 Billion [36] |
| Compound Annual Growth Rate (CAGR) | 16.57% (2025-2034) [36] |
Table 2: Non-Invasive BCI Market Segmentation (2024)
| Segment | Leading Category | Fastest-Growing Category |
|---|---|---|
| By Type | EEG-based BCIs [36] | fNIRS-based BCIs [36] |
| By Application | Healthcare [37] [36] | Communication [36] |
| By Component | Hardware [37] | Hardware [37] |
| By Region | North America [37] [36] | Asia-Pacific [38] [37] |
Analysis of Application Sectors
- Healthcare Dominance: The healthcare sector is the largest application segment, driven by the rising incidence of neurological disorders such as epilepsy, stroke, and Parkinson's disease [37] [36]. Non-invasive BCIs are being developed for neurorehabilitation, mental health monitoring, and providing assistive technologies for individuals with severe physical disabilities [36] [39] [3].
- Emerging Applications: The communication sector is projected to be the fastest-growing application. Non-invasive BCI technology offers novel communication pathways for individuals with severe motor limitations, such as those with advanced ALS or locked-in syndrome, enabling them to interact with their environment [36]. Applications in entertainment, gaming, and smart home control are also expanding, though from a smaller base [37] [36].
Key Research Institutions and Corporate Players
The non-invasive BCI landscape comprises established corporations, specialized neurotechnology companies, and academic research institutions driving innovation.
Leading Corporate Entities
Table 3: Key Companies in the Non-Invasive BCI Space
| Company | Core Technology / Focus | Notable Products/Initiatives |
|---|---|---|
| Kernel | Non-invasive brain activity measurement using light-based neuroimaging [38] | Kernel Flow [38] |
| Emotiv | EEG-based BCIs combined with AI algorithms [40] | EPOC EEG headset series, Insight EEG device [40] |
| BrainCo | EEG signal processing and AI for education and rehabilitation [40] | Focus headbands, AI-controlled prosthetic limbs [40] |
| NeuroSky | Low-cost, consumer-grade EEG biosensors | N/A |
| OpenBCI | Open-source brain-computer interface platform | N/A |
| g.tec medical engineering GmbH | Medical-grade EEG equipment and BCI solutions [36] | N/A |
| Compumedics Neuroscan | Clinical neurodiagnostic and BCI technology [36] | N/A |
Pioneering Research Institutions and Breakthroughs
Academic and government research institutions are the bedrock of fundamental BCI research. Their work often leads to paradigm-shifting advancements.
- Johns Hopkins Applied Physics Laboratory (APL) and School of Medicine: A team from Johns Hopkins has demonstrated a breakthrough in non-invasive, high-resolution recording of neural activity using Digital Holographic Imaging (DHI). This system detects minute neural tissue deformations (on the scale of tens of nanometers) that occur during neuronal firing. This approach, developed under DARPA's Next-Generation Nonsurgical Neurotechnology program, aims to identify a novel signal that can be recorded through the scalp and skull, potentially overcoming the spatial resolution limitations of traditional EEG [9].
- Korea Advanced Institute of Science and Technology (KAIST): Researchers at KAIST have developed brain-machine interfaces that enable users to control robotic hands through thought alone, demonstrating the application of non-invasive BCI in complex motor control tasks [38].
- Indian Institute of Technology Palakkad: Partnered with Neuroleap through a Memorandum of Understanding (MoU) to advance research in BCI technology for neuroenhancement and neurorehabilitation, highlighting the collaborative nature of BCI development in the Asia-Pacific region [38].
Technical Framework and Experimental Protocols
A robust understanding of the technical framework and validation methodologies is essential for research and development in non-invasive BCI.
The Core BCI Workflow
The following diagram illustrates the standard closed-loop workflow for a non-invasive BCI system, which is consistent across most research and application domains.
Detailed Experimental Methodology
For researchers aiming to replicate or design BCI experiments, the following protocol outlines a common methodology for a motor imagery-based BCI, a prevalent paradigm in the field.
Protocol: Motor Imagery BCI for Control
Participant Setup and Calibration:
- EEG Cap Application: Fit the participant with a multi-channel EEG cap according to the international 10-20 system. Apply electrolyte gel to ensure electrode impedance is maintained below 5-10 kΩ to optimize signal quality [2] [3].
- Paradigm Explanation: Instruct the participant on the motor imagery tasks (e.g., imagining left-hand vs. right-hand movement without any physical motion). A visual cue-based paradigm is typically used.
- Baseline Recording: Record a 2-5 minute resting-state EEG with eyes open and closed to establish baseline brain activity.
Data Acquisition and Preprocessing:
- Signal Acquisition: Record EEG data at a sampling rate ≥ 256 Hz. For motor imagery, focus on electrodes over the sensorimotor cortex (e.g., C3, Cz, C4).
- Preprocessing:
- Filtering: Apply a band-pass filter (e.g., 0.5-40 Hz) to remove DC drift and high-frequency noise.
- Artifact Removal: Use algorithms like Independent Component Analysis (ICA) to identify and remove artifacts from eye blinks, eye movements, and muscle activity [39] [3].
- Epoching: Segment the continuous data into epochs time-locked to the presentation of the visual cues (e.g., -1 to 4 seconds relative to cue onset).
Feature Extraction:
- Spectral Analysis: For each epoch, compute the power spectral density in frequency bands relevant to motor imagery: Mu rhythm (8-13 Hz) and Beta rhythm (13-30 Hz). Event-Related Desynchronization (ERD) in these bands over the contralateral motor cortex is a key feature for movement imagination [39] [3].
- Spatio-Temporal Features: Extract features from specific time windows following the cue, often using methods like Common Spatial Patterns (CSP) to enhance the discriminability between two classes of motor imagery [39].
Feature Classification and Output:
- Model Training: Train a classifier (e.g., Support Vector Machine (SVM), Linear Discriminant Analysis (LDA), or a Convolutional Neural Network (CNN)) on a labeled set of the extracted features from a calibration session [39].
- Real-Time Decoding: In an online experiment, the trained model decodes the user's intent in real-time from the processed EEG signal.
- Device Control: The classifier's output (e.g., "left hand" or "right hand") is translated into a control command for an external device, such as moving a cursor on a screen or initiating movement in a prosthetic limb [39] [3].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Research Reagent Solutions for Non-Invasive BCI Experiments
| Item | Function in BCI Research |
|---|---|
| Multi-channel EEG System (e.g., from g.tec, Brain Products) | High-fidelity acquisition of electrical brain activity from the scalp. The core hardware for signal acquisition [36] [3]. |
| Electrode Cap & Electrolyte Gel | Provides stable physical interface and electrical conductivity between the scalp and EEG amplifier. Critical for maintaining low impedance and high-quality signal [3]. |
| Stimulus Presentation Software (e.g., Psychtoolbox, Presentation) | Presents visual, auditory, or tactile cues to the user to elicit specific, time-locked brain responses for the BCI paradigm [39]. |
| Signal Processing Toolboxes (e.g., EEGLAB, BCILAB, MNE-Python) | Open-source software environments for preprocessing, analyzing, and visualizing EEG data. Essential for feature extraction and algorithm development [39] [3]. |
| Machine Learning Libraries (e.g., Scikit-learn, TensorFlow, PyTorch) | Provide algorithms for building and training classifiers to decode brain signals. Deep learning models (CNNs, LSTMs) are increasingly used for improved accuracy [39] [3]. |
Future Research Directions and Challenges
Despite rapid progress, the widespread adoption of non-invasive BCIs faces several technical and practical hurdles that define the agenda for future research.
- Overcoming Signal Limitations: The primary challenge for non-invasive BCIs is the poor signal-to-noise ratio and spatial resolution caused by the signal being filtered by the skull and other tissues [2] [3]. Future research is focused on multimodal integration (e.g., combining EEG with fMRI or fNIRS) and advanced signal processing techniques, including deep learning, to better isolate and decode neural signals from noise [37] [2] [3].
- Improving Classification Accuracy: While deep learning models like Long Short-Term Memory (LSTM) networks have achieved accuracies above 97% in offline analyses of motor imagery, real-time online performance often remains lower and highly variable between users [39]. A significant challenge is the "BCI illiteracy" phenomenon, where a portion of users cannot reliably produce classifiable brain patterns. Developing user-independent, adaptive algorithms that require minimal calibration is a critical research direction [39] [3].
- Pushing the Frontiers of Signal Acquisition: Research into novel acquisition technologies, such as the Digital Holographic Imaging (DHI) pursued by Johns Hopkins APL, aims to discover and leverage entirely new types of neural signals that can be measured non-invasively with higher fidelity [9]. Success in this area could fundamentally shift the capabilities of non-invasive BCIs.
- Addressing Data Scarcity: Deep learning models are data-hungry, but generating large, high-quality EEG datasets from target patient populations (e.g., those with ALS or stroke) is difficult [39]. Research into data augmentation and transfer learning techniques, where models pre-trained on healthy subjects are adapted for patients, is essential for advancing clinical applications [39] [3].
Implementation Strategies and Translational Applications in Biomedicine
Signal Processing Pipelines for Noisy Neural Data
The efficacy of non-invasive Brain-Computer Interfaces (BCIs) is fundamentally constrained by the low signal-to-noise ratio (SNR) inherent in neural signals such as electroencephalography (EEG). Advanced signal processing pipelines are therefore critical for translating raw, noisy data into reliable control commands. This technical guide details the architecture of modern processing pipelines, from acquisition to classification, and evaluates the performance of contemporary methodologies, including deep learning models. Framed within a broader review of non-invasive BCI technologies, this whitepaper provides researchers and drug development professionals with a reference for the computational foundations enabling applications in neurorehabilitation, assistive technology, and clinical diagnostics.
Non-invasive neural signals, while safe and accessible, present significant interpretative challenges due to their inherently low amplitude and susceptibility to contamination from various sources. EEG signals, for instance, typically have amplitudes around 100 µV and must be amplified by approximately 10,000 times to be processed effectively [41]. The resulting low SNR complicates the detection of neural patterns related to cognition, motor intention, or disease biomarkers. Noise sources are diverse, including power line interference, electromyographic (EMG) artifacts from muscle activity, electrooculographic (EOG) artifacts from eye movements, and cardiorespiratory dynamics [42] [41]. Furthermore, the high dimensionality and temporal variability of these signals necessitate robust computational pipelines that can adapt to both the non-stationary nature of brain activity and inter-subject differences [42] [43]. Overcoming these challenges is a prerequisite for developing BCIs capable of precise real-world applications, such as individual finger control of a robotic hand [44] or the longitudinal monitoring of neurodegenerative conditions like Alzheimer's disease [43].
The Standard Signal Processing Pipeline
The transformation of raw neural data into actionable commands follows a sequential pipeline comprising four core stages: signal acquisition, pre-processing, feature extraction, and classification/translation.
Stage 1: Signal Acquisition
This initial stage involves capturing neural signals from the scalp using various modalities.
- Electroencephalography (EEG): The most prevalent modality, EEG uses metal electrodes to capture electrical activity with high temporal resolution, though it suffers from low spatial resolution [41]. Modern systems range from consumer-grade headsets (e.g., 14 electrodes) to research-grade systems with 64 or more channels [41].
- Functional Near-Infrared Spectroscopy (fNIRS): This modality measures hemodynamic responses associated with neural activity using near-infrared light, offering moderate spatial and temporal resolution and greater robustness to movement [41].
- Magnetoencephalography (MEG): MEG measures the magnetic fields produced by neuronal currents, providing high temporal and spatial resolution. However, its requirement for shielded environments and complex equipment often limits it to research settings [8] [41].
- Emerging Sensors: Triboelectric nanogenerators (TENGs) have emerged as self-powered, flexible multi-sensing devices capable of capturing EEG, EMG, and cardiorespiratory dynamics, showing promise for long-term wearable monitoring [42] [45].
Stage 2: Pre-Processing
The goal of pre-processing is to enhance the SNR by isolating neural signals of interest from noise. Common techniques include:
- Filtering: Band-pass filters isolate relevant neural frequency bands (e.g., delta, theta, alpha, beta, gamma), while notch filters remove power line interference (e.g., 50/60 Hz) [41].
- Advanced Denoising: Techniques such as Independent Component Analysis (ICA) are used to separate and remove artifactual components like blinks or heartbeats [41]. Adaptive filtering (e.g., Recursive Least Squares) and wavelet transforms are also employed for robust, non-stationary noise removal [41].
Stage 3: Feature Extraction
This stage reduces the dimensionality of the data by identifying discriminative patterns. Extracted features can be temporal, spectral, or spatial.
- Time-Frequency Decomposition: Wavelet transforms are used to analyze the spectral properties of signals over time [41].
- Spatial Filtering: Algorithms like Common Spatial Patterns (CSP) are optimized to maximize the variance between two classes of motor imagery signals, enhancing the separability of brain states [41].
- Component-Based Summaries: Features may include logarithmic variances derived from CSP or coefficients from other decomposition methods [41].
Stage 4: Classification and Translation
In this final stage, machine learning models map the extracted features to output commands or cognitive states.
- Traditional Models: Support Vector Machines (SVMs) and Linear Discriminant Analysis (LDA) have been widely used for their simplicity and efficacy on handcrafted features [43] [46].
- Deep Learning Models: Convolutional Neural Networks (CNNs) like EEGNet are specifically designed for EEG, learning spatial and temporal features directly from raw or minimally processed signals [46] [44]. Recurrent Neural Networks (RNNs), including Long Short-Term Memory (LSTM) networks, model temporal dependencies, while Transformers are increasingly explored for capturing long-range dependencies [42] [46].
The following diagram illustrates the complete workflow and the flow of data through these stages.
Signal Processing Pipeline Workflow
Quantitative Performance of Processing Methodologies
The performance of signal processing pipelines is quantitatively evaluated using metrics such as decoding accuracy and information transfer rate (ITR). The table below summarizes the performance of different algorithms and paradigms as reported in recent studies.
Table 1: Performance Benchmarks for Neural Signal Processing Pipelines
| Paradigm / Task | Processing Model / Technique | Reported Performance | Context / Application |
|---|---|---|---|
| Individual Finger MI/ME [44] | EEGNet-8.2 with Fine-Tuning | 80.56% accuracy (2-finger), 60.61% accuracy (3-finger) | Real-time robotic hand control |
| Assistive Device Control [41] | LSTM-CNN-RF Ensemble | 96% decoding accuracy | Robust prosthetic control (BRAVE system) |
| P300 Spelling [41] | POMDP-based Recursive Classifier | >85% symbol recognition accuracy | High-speed communication |
| Tactile Sensation Decoding [41] | Deep Learning (CNN) | >65% classification accuracy | Neurohaptics and VR |
| Non-Invasive BCI Market [47] | N/A | Projected CAGR of ~18% (2025-2033) | Market growth indicator for healthcare, communication, and entertainment |
The integration of transfer learning and fine-tuning has proven particularly effective in addressing the challenge of inter-session and inter-subject variability. For example, a study on robotic hand control demonstrated that fine-tuning a base EEGNet model with session-specific data significantly improved real-time decoding performance for motor imagery tasks [44]. Furthermore, adaptive methods that leverage error-related potentials as feedback, as well as domain adaptation networks, are being developed to reduce lengthy user-specific calibration times [41].
Detailed Experimental Protocol: Real-Time Robotic Finger Control
To illustrate a state-of-the-art application of a signal processing pipeline, we detail the methodology from a recent study demonstrating real-time, non-invasive robotic hand control at the individual finger level [44].
Objective
To enable real-time control of a robotic hand at the individual finger level using movement execution (ME) and motor imagery (MI) tasks decoded from scalp EEG signals.
Participant Profile
- Cohort: 21 able-bodied human participants.
- Criteria: All participants had prior experience with limb-level BCI paradigms.
Experimental Design and Workflow
The experiment was conducted over multiple sessions, combining offline training with online testing and model refinement. The workflow is summarized in the diagram below.
Finger Control Experiment Workflow
- Offline Session: Participants were familiarized with the finger ME and MI tasks. Data from this session were used to train a subject-specific base decoding model using the EEGNet-8.2 architecture.
- Online Sessions: Participants completed two online sessions for both ME and MI.
- The base model was used to decode the first half of the runs in each session.
- A fine-tuned model was then created by updating the base model with data collected during the first half of the online session.
- This fine-tuned model was applied to the second half of the runs, with performance compared against the base model.
- Feedback: Participants received real-time visual feedback (on a screen) and physical feedback (from the movement of a robotic hand) during online sessions.
Data Acquisition Parameters
- Paradigms: Movement Execution (ME) and Motor Imagery (MI) of individual fingers (thumb, index, pinky).
- Tasks: Binary (thumb vs. pinky) and ternary (thumb vs. index vs. pinky) classification.
- Model: EEGNet-8.2, a compact convolutional neural network designed for EEG-based BCIs.
- Performance Metrics: Majority voting accuracy, precision, and recall.
Key Findings
- The fine-tuning process led to a significant improvement in MI performance across sessions for both binary and ternary classification tasks.
- The study demonstrated the feasibility of naturalistic, non-invasive robotic finger control using a deep-learning-driven pipeline, achieving high accuracy for complex tasks.
The Scientist's Toolkit: Essential Research Reagents and Materials
The development and implementation of effective signal processing pipelines rely on a suite of hardware, software, and algorithmic tools.
Table 2: Essential Research Tools for Neural Signal Processing
| Category | Item / Technology | Function / Application |
|---|---|---|
| Hardware & Reagents | Dry/Wet EEG Electrodes | Signal acquisition; dry electrodes improve usability for long-term wear [8]. |
| Triboelectric Nanogenerators (TENGs) | Self-powered, flexible multi-sensing for EEG, EMG, and physiological dynamics [42] [45]. | |
| fNIRS Photodetectors | Measures hemodynamic responses via near-infrared light for hybrid BCIs [8] [41]. | |
| Software & Algorithms | EEGNet (CNN) | Provides a versatile and effective architecture for decoding EEG signals from raw data [44] [41]. |
| Common Spatial Patterns (CSP) | Spatial filtering algorithm optimized for maximizing the variance between two classes of motor imagery signals [41]. | |
| Independent Component Analysis (ICA) | Blind source separation technique for artifact removal (e.g., eye blinks, muscle activity) [41]. | |
| Transfer Learning / Fine-Tuning | Adapts pre-trained models to new subjects or sessions, reducing calibration time and improving performance [43] [44]. | |
| Domain Adaptation Networks (e.g., SSVEP-DAN) | Aligns data from source and target domains to minimize calibration needs for new users [41]. |
Emerging Trends
The field of neural signal processing is rapidly evolving, driven by several key trends:
- Brain Foundation Models (BFMs): Inspired by large-language models, BFMs are pre-trained on massive, diverse neural signal datasets (EEG, fMRI) to learn universal representations of brain activity. These models promise robust zero- or few-shot generalization across tasks, subjects, and recording conditions [46].
- Neuromorphic Computing: The integration with spiking neural networks (SNNs) and neuromorphic hardware offers an event-driven, energy-efficient computational paradigm. This is particularly synergistic with the pulse-like outputs of TENG sensors and biological neural signals, enabling ultra-low-power on-device processing [42] [45].
- Hybrid and Adaptive Paradigms: Combining multiple modalities (e.g., EEG + fNIRS) compensates for the weaknesses of individual techniques [41]. Furthermore, the use of reinforcement learning agents that adapt to non-stationary neural signals in real-time is a critical step toward practical, long-term BCI use [41].
Processing noisy neural data remains a central challenge in non-invasive BCI development. The standard pipeline—acquisition, pre-processing, feature extraction, and classification—has been profoundly enhanced by deep learning and adaptive AI, enabling unprecedented applications like dexterous robotic control and continuous health monitoring. Future progress hinges on the development of more generalized models like BFMs, tighter integration with neuromorphic hardware, and a steadfast commitment to addressing ethical concerns around data privacy and user accessibility. For researchers and clinicians, mastering these signal processing pipelines is not merely a technical exercise but a prerequisite for unlocking the transformative potential of non-invasive brain-computer interfaces.
Machine Learning and Deep Learning Approaches for Neural Decoding
Neural decoding, the process of interpreting brain activity to identify cognitive states or intended actions, represents a cornerstone of modern brain-computer interface (BCI) technology. Recent advances in machine learning (ML) and deep learning (DL) have dramatically accelerated the development of non-invasive BCIs, which record neural signals without surgical implantation [48]. These technologies hold particular promise for restoring communication and motor functions in patients with neurological disorders such as ALS, spinal cord injuries, and stroke [38] [49].
The fundamental challenge in non-invasive neural decoding lies in extracting meaningful information from signals that are often noisy, non-stationary, and characterized by low spatial and/or temporal resolution. ML and DL approaches have demonstrated remarkable capabilities in addressing these challenges, enabling decoders that can translate brain signals into commands for external devices or reconstruct perceptual experiences with increasing accuracy [50]. This technical guide provides an in-depth examination of current ML/DL methodologies for neural decoding, with a specific focus on non-invasive approaches that show particular promise for clinical translation.
Neural Signal Modalities and Processing Fundamentals
Non-invasive BCIs employ various recording techniques, each with distinct characteristics and applications. Electroencephalography (EEG) measures electrical activity via electrodes placed on the scalp and offers high temporal resolution but limited spatial resolution [8]. Magnetoencephalography (MEG) detects the magnetic fields generated by neural activity and provides better spatial resolution than EEG but requires bulky, expensive equipment [51]. Functional near-infrared spectroscopy (fNIRS) measures hemodynamic changes associated with neural activity using light, representing a compromise between portability and signal quality [8].
Each modality presents unique preprocessing requirements. EEG typically requires extensive artifact removal (e.g., ocular, muscular), filtering, and spatial enhancement techniques. MEG signals necessitate magnetic shielding and sophisticated source localization methods. The choice of modality involves trade-offs between portability, cost, signal quality, and temporal/spatial resolution, making different modalities suitable for different applications [8].
Table 1: Comparison of Non-Invasive Neural Recording Modalities
| Modality | Temporal Resolution | Spatial Resolution | Portability | Primary Applications |
|---|---|---|---|---|
| EEG | High (milliseconds) | Low (cm) | High | Communication, motor control, sleep studies |
| MEG | High (milliseconds) | Medium (mm-cm) | Low | Language decoding, cognitive research |
| fNIRS | Low (seconds) | Medium (cm) | Medium | Cognitive monitoring, neurofeedback |
| fMRI | Low (seconds) | High (mm) | Low | Visual reconstruction, cognitive studies |
Machine Learning Approaches for Neural Decoding
Traditional machine learning approaches have established strong foundations in neural decoding, particularly for classification tasks and continuous variable prediction.
Linear Models and Support Vector Machines
Linear models such as ridge regression have demonstrated effectiveness for decoding continuous variables from neural signals. In language decoding research, ridge regression has been used to predict word embeddings from M/EEG recordings, with performance peaking within the first 500ms after word onset [51]. These models work by establishing a linear mapping between neural features and target variables, providing interpretable solutions with relatively low computational requirements.
For classification tasks, support vector machines (SVM) have been widely applied to decode cognitive states, movement intentions, and emotional states from fMRI and EEG data [50]. The effectiveness of SVMs stems from their ability to handle high-dimensional data and find optimal decision boundaries even with limited training samples.
Unscented Kalman Filters
The Unscented Kalman Filter (UKF) has emerged as a state-of-the-art algorithm for continuous decoding tasks, particularly in motor control applications. Research has shown that UKF outperforms other methods when using smaller data windows, enabling real-time implementation with rapid convergence [52]. This approach is especially valuable for BCI systems that require low latency, such as those controlling robotic arms or avatars. However, UKF implementations can be vulnerable to noise, necessitating careful preprocessing and parameter tuning [52].
Deep Learning Architectures for Advanced Neural Decoding
Deep learning approaches have demonstrated superior performance in handling the complex, non-linear relationships inherent in neural data, particularly for challenging decoding tasks such as language reconstruction and visual imagery decoding.
Convolutional Neural Networks
Convolutional Neural Networks (CNNs) have been successfully applied to decode perceptual content from brain activity. For visual stimulus reconstruction, researchers have mapped multi-level features of the human visual cortex to the hierarchical features of pre-trained CNNs [50]. This approach leverages the structural similarity between CNNs and the human visual system, enabling the reconstruction of faces and natural images from fMRI data [50].
In EEG-based decoding, EEGNet represents a specialized CNN architecture designed to extract spatially-localized features while minimizing overfitting through depthwise and separable convolutions [51]. While EEGNet provides a solid baseline, studies have shown that more sophisticated architectures significantly outperform it for complex decoding tasks [51].
Recurrent Neural Networks and Transformers
For temporal sequence processing, Gated Recurrent Units (GRUs) and Long Short-Term Memory (LSTM) networks have demonstrated exceptional performance in decoding continuous movement parameters and linguistic content from neural signals [52]. These architectures effectively model the temporal dependencies in neural data, enabling more accurate tracking of dynamically evolving cognitive states.
Transformer architectures, particularly when applied at the sentence level, have shown remarkable improvements in language decoding, yielding approximately 50% performance improvements over previous approaches [51]. The self-attention mechanism in transformers enables the model to capture long-range dependencies in neural recordings, which is essential for decoding coherent linguistic content.
Generative Models for Stimulus Reconstruction
Generative models including Variational Autoencoders (VAEs) and Generative Adversarial Networks (GANs) have pushed the boundaries of visual stimulus reconstruction from brain activity. VAEs provide a theoretically grounded framework that represents the latent space regularization, compressing input data into a distribution over latent space rather than single points [50]. This approach facilitates the generation of diverse outputs from neural patterns but may lack fine details in reconstructed images.
GANs have demonstrated capability in synthesizing high-quality images from brain activity data, with the discriminator network learning to distinguish between real and generated images, thereby training the generator to produce more realistic reconstructions [50]. However, GAN training can be unstable, and the diversity of samples may be limited when working with constrained neural datasets.
Hybrid and Specialized Architectures
Recent research has explored hybrid architectures that combine the strengths of multiple approaches. Quasi Recurrent Neural Networks (QRNNs) have shown particular promise, outperforming other methods in terms of both decoding accuracy and stability for motor decoding tasks [52]. These architectures combine the parallel processing capabilities of CNNs with the temporal modeling strengths of RNNs, making them well-suited for real-time BCI applications.
Reservoir Computing Networks (RCNs) represent another innovative approach that has demonstrated superior performance in predicting functional connectivity in neuronal networks compared to traditional methods like Cross-Correlation and Transfer-Entropy [53]. This makes them particularly valuable for studying network-level dynamics in brain activity.
Table 2: Performance Comparison of Neural Decoding Architectures
| Architecture | Best For | Key Advantages | Reported Performance |
|---|---|---|---|
| EEGNet [51] | Basic EEG decoding | Minimal overfitting, efficient | Baseline performance |
| Transformer + Subject Layer [51] | Language decoding | Cross-subject generalization, contextual understanding | 37% top-10 accuracy (250 words) |
| GRU/QRNN [52] | Continuous motor decoding | Stability, noise robustness | Outperforms UKF with sufficient data |
| GAN/VAE [50] | Visual reconstruction | High-quality image generation | Subjective quality metrics |
| UKF [52] | Real-time motor decoding (small windows) | Fast convergence, low latency | Superior with small tap sizes |
| Reservoir Computing [53] | Connectivity mapping | Effective with limited data | Outperforms correlation-based methods |
Experimental Protocols and Methodologies
Language Decoding Protocol
Recent breakthroughs in language decoding have employed sophisticated protocols across large datasets. A comprehensive study involving 723 participants across nine datasets collected EEG and MEG signals while subjects read or listened to sentences totaling five million words across three languages [51]. The experimental setup presented words via rapid serial visual presentation (RSVP) for reading tasks or auditory playback for listening tasks, with precise word-onset markers synchronized to neural recordings.
The decoding pipeline involved several stages: (1) preprocessing (filtering, artifact removal), (2) feature extraction using subject-specific layers, (3) temporal context modeling with transformers, and (4) contrastive learning to align neural signals with word embeddings. Performance was evaluated using top-k accuracy metrics, with the model achieving up to 37% top-10 accuracy using a retrieval set of 250 words [51].
Language Decoding Workflow: From neural signals to word identification
Motor Decoding Protocol
Motor decoding experiments typically involve participants performing movements while neural signals are recorded. In one comprehensive study, eight healthy subjects walked on a treadmill at 1 mile per hour while EEG data and lower-limb kinematics were simultaneously collected [52]. The protocol included three conditions: resting, goniometer control (movement tracking), and closed-loop BCI control.
The data was split to simulate real-time decoding constraints: the first 80% of goniometer control data formed the training set, the remaining 20% served for validation, and the BCI control section was used for testing. Various decoder architectures were evaluated using different feature sets (delta band, multiple frequency bands) and tap sizes (temporal windows) to determine optimal configurations for real-time implementation [52].
Performance Optimization and Scaling Laws
Data Scaling Effects
Decoding performance demonstrates predictable scaling relationships with dataset size. Language decoding accuracy increases roughly log-linearly with the amount of training data, showing no clear signs of diminishing returns across current dataset sizes [51]. This suggests that continued data collection would yield further improvements in non-invasive decoding systems.
For individual subjects, performance shows a weak but statistically significant relationship with the log volume of data per subject (p < 0.05), indicating that with fixed recording resources, "deep" datasets (few participants with extensive recording sessions) may be more valuable than "broad" datasets (many participants with limited sessions) [51].
Signal Averaging Techniques
Averaging multiple neural responses to the same stimulus dramatically improves decoding accuracy. Studies show that top-10 accuracy for word decoding can double after averaging just 8 predictions in response to the same word, with one dataset reaching nearly 80% accuracy using this technique [51]. This demonstrates that the low signal-to-noise ratio of non-invasive recordings represents a major constraint, which can be partially mitigated through averaging during the testing phase.
Impact of Experimental Factors
Several experimental factors significantly impact decoding performance. Reading tasks consistently yield better decoding results than listening tasks (p < 10^-16), potentially because visual features like word length provide additional discriminative information [51]. MEG recordings outperform EEG (p < 10^-25), reflecting MEG's superior signal-to-noise ratio [51]. These findings highlight the importance of protocol design in maximizing decoding performance.
Key Factors Influencing Neural Decoding Performance
Research Reagent Solutions Toolkit
Table 3: Essential Resources for Neural Decoding Research
| Resource Category | Specific Examples | Function/Purpose |
|---|---|---|
| Public Datasets | 9-dataset language corpus (723 participants) [51] | Training and benchmarking language decoders |
| EEG Systems | BrainVision 64-channel active electrode system [52] | High-quality neural data acquisition |
| Decoding Algorithms | EEGNet, Transformers, GRU, QRNN, UKF [51] [52] | Various approaches for different decoding tasks |
| Preprocessing Tools | Adaptive filtering for ocular artifacts [52] | Signal cleaning and enhancement |
| Feature Sets | Delta band, multiple frequency bands [52] | Input features for decoding models |
| Evaluation Metrics | Top-k accuracy, Pearson correlation, r-value [51] [52] | Performance quantification and comparison |
Machine learning and deep learning approaches have dramatically advanced the capabilities of non-invasive neural decoding systems. Current state-of-the-art models can decode linguistic content, reconstruct perceptual experiences, and predict movement intentions with increasing accuracy. The performance of these systems follows predictable scaling laws with data volume and benefits significantly from appropriate architectural choices and signal processing techniques.
Despite these advances, important challenges remain. Non-invasive systems still struggle with the relatively low signal-to-noise ratio of recorded neural signals, particularly for single-trial decoding. Future research directions likely include developing more sophisticated model architectures specifically designed for neural data characteristics, collecting larger and more diverse datasets, and creating better methods for cross-subject and cross-session generalization. As these technical challenges are addressed, non-invasive neural decoding systems promise to revolutionize both clinical applications and human-computer interaction.
Motor Imagery Paradigms for Rehabilitation and Assistive Technology
Motor Imagery (MI), the mental rehearsal of a motor action without any physical movement, has emerged as a cornerstone of modern non-invasive Brain-Computer Interface (BCI) systems for rehabilitation and assistive technology [2]. By capturing the neural correlates of movement intention, MI-based BCIs create a closed-loop system that can promote neuroplasticity and functional recovery, particularly for patients with neurological injuries such as stroke [54] [55]. The core principle is that during motor imagery, event-related desynchronization (ERD) and event-related synchronization (ERS) occur in the sensorimotor cortex's alpha (8-12 Hz) and beta (18-26 Hz) rhythms, which can be detected and used as control signals [54] [56]. This technical guide provides an in-depth analysis of current MI paradigms, detailing their experimental protocols, underlying neural mechanisms, signal processing methodologies, and their application within the broader context of non-invasive BCI technologies.
Core Motor Imagery Paradigms and Experimental Protocols
The design of the experimental paradigm is critical for eliciting clear and classifiable MI EEG signals. Below are detailed protocols for the most common paradigms.
Standard Motor Imagery Paradigm
The classic MI paradigm involves the visual cue-guided imagination of limb movements.
- Subject Preparation: Subjects sit comfortably 60 cm from a screen. An EEG cap is fitted according to the 10-20 system. Subjects are instructed to remain still, avoid blinking, and focus on the screen.
- Trial Structure: Each trial follows a precise timeline:
- Fixation Cross (0 - 1 s): A red "+" is displayed at the center of the screen. This period serves as a baseline and prepares the subject for the upcoming task.
- Cue Presentation (1 - 5 s): A visual symbol or instruction appears, indicating the specific MI task to be performed (e.g., an arrow for left hand, a different symbol for right hand). The subject continuously performs the cued motor imagery for this 4-second duration. This period is defined as the MI epoch.
- Rest Period (5 - 7 s): The screen displays "Rest," allowing the subject to relax before the next trial.
- Task Types: Common tasks include imagining unilateral hand grasping (left/right), bilateral hand grasping, foot movements, or tongue movements [58] [57]. The tasks are presented in a randomized order across trials to prevent habituation and predictability.
- Block Design: An experiment typically consists of multiple blocks (e.g., 14 blocks), with each block containing a set number of trials per MI task (e.g., 6 trials per type). Breaks of about 5 minutes are provided between consecutive blocks to prevent fatigue [57].
Multi-Paradigm Framework for Upper Limb Rehabilitation
Recent research focuses on collecting data from multiple paradigms for the same subject to compare their efficacy and neural signatures systematically [56]. The following table summarizes a comprehensive multi-paradigm approach for upper limb rehabilitation.
Table 1: Summary of Multi-Paradigm Rehabilitation Protocols
| Paradigm Name | Core Task Description | Key Modality | Primary Application |
|---|---|---|---|
| Motor Execution (ME) | Actual performance of grasp-and-release movements with the left, right, or both hands in response to a visual cue [56]. | Physical Movement | Serves as a baseline for understanding the neural signature of actual movement. |
| Motor Imagery (MI) | Imagination of grasp-and-release movements without any actual motor output, cued by on-screen symbols [56]. | Mental Simulation | Foundational BCI training for inducing neural plasticity. |
| VR-Motor Imagery | Observation and imitation of virtual hand movements in a VR environment, followed by kinesthetic motor imagery [56]. | Virtual Reality | Enhances engagement and provides immersive visual feedback. |
| Mirror Therapy | The "healthy" hand performs movements while observing its mirror reflection as if it were the "affected" hand, aiding motor imagery of the affected limb [56]. | Mirror Visual Illusion | Commonly used for stroke rehabilitation to retrain the affected hemisphere. |
| Glove-Assisted Therapy | Use of a soft robotic glove that provides physical assistance or feedback during movement or imagery tasks [56]. | Haptic Feedback | Closes the sensorimotor loop by providing proprioceptive input. |
The workflow for a typical multi-paradigm study, from subject preparation to data analysis, can be visualized as follows:
Figure 1: Experimental Workflow for a Multi-Paradigm MI-BCI Study. This diagram outlines the sequential process of conducting a study that compares different rehabilitation paradigms on the same subjects, from preparation to final analysis [56].
Neural Correlates and Signal Processing Pathways
Understanding the neural basis of MI and the computational pathway from raw signal to device command is essential for developing effective BCIs.
Neurophysiological Fundamentals
During motor imagery, the brain's sensorimotor areas undergo characteristic changes in oscillatory activity, which are detectable with EEG [54] [56]:
- Event-Related Desynchronization (ERD): A decrease in power in the mu (8-12 Hz) and beta (18-26 Hz) frequency bands over the sensorimotor cortex contralateral to the imagined movement. This reflects an activated cortical state.
- Event-Related Synchronization (ERS): A power increase in the same bands, often occurring in the ipsilateral cortex or post-movement, reflecting an idling or deactivated state.
Functional MRI (fMRI) studies have provided further validation, showing that MI-BCI therapy in stroke patients leads to significant activation in brain regions such as the middle cingulate gyrus, precuneus, inferior parietal gyrus, and precentral gyrus. Furthermore, improvements in motor function have been positively correlated with increased neural activity in the contralateral precentral gyrus, indicating use-dependent plasticity [54].
The MI-BCI Signal Processing Pipeline
The transformation of raw EEG signals into a control command for an assistive device involves a multi-stage processing pipeline. The following diagram illustrates this pathway and the key algorithms used at each stage.
Figure 2: MI-BCI Signal Processing and Classification Pipeline. This pathway details the computational stages from raw signal acquisition to the generation of a device control command, highlighting advanced feature fusion and classification techniques [58] [59] [60].
Advanced Feature Extraction and Classification Algorithms
The low signal-to-noise ratio and non-stationary nature of EEG signals demand sophisticated processing methods. Recent research has focused on hybrid and data-driven approaches to improve classification accuracy and robustness.
Table 2: Performance of Advanced MI-EEG Classification Algorithms
| Algorithm/Model | Core Methodology | Reported Accuracy | Key Advantage |
|---|---|---|---|
| HA-FuseNet [58] | End-to-end network with multi-scale dense connectivity & hybrid attention mechanism. | 77.89% (within-subject) 68.53% (cross-subject) | Robustness to spatial resolution variations and individual differences. |
| SVM-WOA-AdaBoost [59] | Multi-feature fusion (Energy, CSP, AR, PSD) with ensemble learning optimized by Whale Optimization Algorithm. | 95.37% | High accuracy on dataset by combining complementary features and classifiers. |
| EEMD with NN [60] | Data-driven decomposition (Ensemble Empirical Mode Decomposition) for feature extraction. | >15% improvement over EMD | Adaptive filtering for improved signal-to-noise ratio without manual band filtering. |
The Researcher's Toolkit: Essential Materials and Reagents
Conducting MI-BCI research requires a suite of specialized hardware, software, and datasets. The following table catalogs key resources for building and validating MI-BCI systems.
Table 3: Essential Research Toolkit for MI-BCI Development
| Item / Reagent Solution | Specification / Function | Application in MI-BCI Research |
|---|---|---|
| EEG Acquisition System | Multi-channel amplifier with Ag/AgCl or dry electrodes arranged in the 10-20 system. | Captures raw electrical brain activity from the scalp [56] [2]. |
| Conductive Gel / Paste | Electrolyte gel to ensure stable impedance (< 5 kΩ) between electrode and scalp. | Improves signal quality and reduces noise for wet electrode systems [56]. |
| Visual Stimulation Software | Software like Psychtoolbox for MATLAB or Unity 3D for precise cue presentation. | Presents the MI paradigm (cues, timing) and ensures experimental rigor [57] [56]. |
| Data Preprocessing Tools | Tools for FIR filtering, artifact removal (e.g., ICA), and segmentation in MATLAB or Python. | Removes line noise, EOG, and EMG artifacts to clean the raw EEG data [59] [56]. |
| Feature Extraction Libraries | Code for calculating CSP, Wavelet features, PSD, etc. (e.g., MNE-Python, EEGLAB). | Transforms preprocessed signals into discriminative features for classification [58] [59]. |
| Machine Learning Classifiers | Implementations of SVM, Neural Networks, LDA, etc. (e.g., scikit-learn, TensorFlow). | Decodes the MI task from the extracted features [58] [59] [60]. |
| Benchmark Datasets | Public datasets like BCI Competition IV 2a, BNCI Horizon 2022. | Provides standardized data for developing and benchmarking new algorithms [58] [60]. |
| fMRI Scanner | 3T functional MRI scanner. | Validates MI-BCI therapy effects by measuring changes in brain activation and connectivity (e.g., zALFF, zReHo) [54]. |
Clinical Efficacy and Market Outlook
The translation of MI-BCI from a laboratory tool to a clinical and commercial product is underway.
- Clinical Efficacy: A 2024 randomized controlled trial demonstrated that MI-BCI therapy combined with conventional rehabilitation significantly improved upper extremity motor function in chronic stroke patients, as measured by the Fugl-Meyer Assessment (FMA-UE) score. fMRI evidence confirmed that these improvements were correlated with beneficial neuroplastic changes in motor and visuospatial brain regions [54].
- Market Forecast: The broader BCI market is forecast to grow to over US $1.6 billion by 2045, representing a CAGR of 8.4% since 2025. This growth is driven by advancements in both non-invasive and invasive technologies, with applications expanding across medical, assistive, and consumer markets [8].
Motor Imagery paradigms represent a powerful and non-invasive approach for harnessing the brain's plasticity for rehabilitation and assistive technology. The field is maturing from proof-of-concept studies to rigorous clinical validation and early commercialisation. Future development will be guided by the refinement of multi-paradigm approaches, the adoption of robust data-driven and deep learning algorithms for improved classification, and the integration of these systems into sustainable, user-friendly healthcare solutions. The ongoing research into the neural mechanisms underlying BCI therapy will continue to refine treatment strategies, ultimately leading to more personalized and effective interventions for patients.
Brain-Computer Interface (BCI) technology represents a revolutionary approach in neurorehabilitation, establishing a direct communication pathway between the brain and external devices [61]. For patients with neurological damage from Spinal Cord Injury (SCI) or stroke, BCIs offer a promising tool to bypass damaged neural pathways and facilitate recovery of motor and sensory functions [10]. The core mechanism of BCI technology involves measuring brain activity and converting it in real-time into functionally useful outputs, thereby changing the ongoing interactions between the brain and its external or internal environments [62]. This technical guide provides an in-depth analysis of the current applications, experimental protocols, and mechanistic underpinnings of BCI technology within neurorehabilitation, focusing specifically on SCI and stroke recovery.
Technical Foundations of BCI Systems
Core Components and Operational Principles
All BCI systems share a fundamental closed-loop architecture consisting of four sequential components: (1) Signal Acquisition: Electrodes or sensors pick up neural activity, which may be captured non-invasively (e.g., EEG, fNIRS) or via implanted arrays; (2) Preprocessing and Feature Extraction: Algorithms filter noise and extract relevant features from brainwave patterns; (3) Feature Translation: Processed signals are interpreted to decode user intent; and (4) Device Output: The decoded commands control external devices or provide feedback to the user [62] [63]. This closed-loop design – acquire, decode, execute, feedback – forms the backbone of current BCI research and applications in neurorehabilitation [62].
The convergence of deep learning with neural data has significantly advanced BCI capabilities, yielding decoders that can interpret complex brain activity with high accuracy and minimal latency [62]. For instance, speech BCIs can now infer words from brain activity at 99% accuracy with less than 0.25-second latency, feats that were unthinkable just a decade ago [62].
BCI Modalities: Invasive versus Non-Invasive Approaches
BCI systems are broadly categorized based on their level of invasiveness, each with distinct advantages and limitations for neurorehabilitation applications:
Non-Invasive BCIs place recording electrodes or sensors on the scalp or body surface without surgical implantation. Common technologies include Electroencephalography (EEG), functional Near-Infrared Spectroscopy (fNIRS), and Magnetoencephalography (MEG) [2] [8]. These systems are safer, more convenient, and appropriate for wider clinical implementation, though they face challenges with signal resolution and external noise [10] [2].
Invasive BCIs involve surgical implantation of microelectrode arrays directly onto the brain surface or into brain tissue. These systems provide superior signal quality and spatial resolution but carry higher risks and ethical concerns [62] [2]. Prominent examples include Neuralink's ultra-high-bandwidth implantable chip, Synchron's Stentrode delivered via blood vessels, and Precision Neuroscience's "brain film" electrode array [62].
Table 1: Comparison of BCI Modalities for Neurorehabilitation
| Parameter | Non-Invasive BCIs | Invasive BCIs |
|---|---|---|
| Signal Quality | Lower spatial resolution, subject to noise and attenuation | High spatial and temporal resolution |
| Risk Profile | Minimal risk, high safety | Surgical risks, potential tissue response |
| Clinical Accessibility | High, suitable for widespread use | Limited to specialized centers |
| Primary Applications | Rehabilitation training, neurofeedback, assistive control | Communication restoration, advanced motor control |
| Representative Technologies | EEG, fNIRS, MEG | Utah Array, Stentrode, Neuralink |
BCI Applications in Spinal Cord Injury Rehabilitation
Mechanisms of Action in SCI
Spinal Cord Injury disrupts signaling pathways between the brain and somatic effectors, severely impairing motor and sensory functions and activities of daily living (ADL) [10]. Non-invasive BCI techniques provide alternative control pathways by enabling direct use of brain signals to control assistive devices (e.g., exoskeletons, wheelchairs, computers) or functional electrical stimulation (FES) systems [10]. Additionally, closed-loop neurofeedback training potentially facilitates cortical reorganization and reinforcement of residual pathways through real-time feedback, promoting neuroplasticity [10].
A 2025 systematic review and meta-analysis evaluated the effects of non-invasive BCI technology on motor and sensory functions and daily living abilities of SCI patients [10]. The analysis included 9 papers (4 randomized controlled trials and 5 self-controlled trials) with 109 total participants. The results demonstrated that non-invasive BCI intervention had a significant impact on patients' motor function (SMD = 0.72, 95% CI: [0.35,1.09], P < 0.01), sensory function (SMD = 0.95, 95% CI: [0.43,1.48], P < 0.01), and activities of daily living (SMD = 0.85, 95% CI: [0.46,1.24], P < 0.01) [10].
Experimental Protocols and Methodologies for SCI
Subgroup analyses from the meta-analysis revealed that non-invasive BCI interventions in patients with subacute stage SCI showed statistically stronger effects on motor function, sensory function, and ability to perform activities of daily living than in patients with chronic stage SCI [10]. This suggests that the timing of BCI intervention relative to injury onset represents a critical factor in rehabilitation outcomes.
Standardized assessment tools employed in BCI studies for SCI include:
- Motor Function: Berg Balance Scale (BBS), ASIA motor score, Manual Muscle Test (MMT), Lower Extremity Motor Score (LEMS)
- Sensory Function: ASIA sensory scores, sensory ratings
- Activities of Daily Living: Spinal Cord Independence Measure (SCIM), the Barthel Index (BI) [10]
The following diagram illustrates the closed-loop BCI system for SCI rehabilitation:
BCI Closed-Loop in SCI Rehabilitation
BCI Applications in Stroke Rehabilitation
Mechanisms of Action in Stroke
Stroke often results in upper limb dysfunction, which is highly prevalent among patients in the chronic stage of recovery [64]. BCI technology creates a direct link between the brain's electrical signals and external devices, enabling stroke patients with motor disabilities to perform tasks for clinical rehabilitation [64]. The fundamental mechanism involves engaging patients in active movement imagination, which enhances the reconstruction of brain motor-related neural networks. When integrated with BCI technology, this process converts brain signals into executable commands and, combined with multimodal feedback, forms a closed-loop system that effectively improves motor function [64].
Research using functional Near-Infrared Spectroscopy (fNIRS) has demonstrated that BCI-robot training causes substantial changes in cortical activation patterns in stroke patients. When performing upper limb movement tasks, the activation intensity and range of movement-related brain areas significantly enhance, and functional connectivity between cerebral hemispheres strengthens [64]. This provides evidence that BCI training effectively stimulates neuroplasticity, contributing to the reorganization of the motor control network.
Experimental Protocols and Methodologies for Stroke
A 2025 study published in Nature Scientific Reports examined upper-limb functional recovery mechanisms using BCI technology combined with fNIRS neuroimaging [64]. The study employed a rigorous methodological approach:
Participant Selection: Thirty-four ischemic stroke patients with upper limb dysfunction were randomly assigned to either a treatment group or a control group. Participants met specific inclusion criteria: first onset, within one month of onset, Brunnstrom stage II-IV for upper limb and hand hemiplegia, and ability to sustain a sitting position for ≥20 minutes [64].
Intervention Protocol: Both groups received routine upper limb rehabilitation training. The treatment group additionally underwent daily BCI training for 30 minutes, 5 days a week, for 4 consecutive weeks using the Rehabilitation-III-Plus upper-limb BCI therapy instrument [64].
Assessment Methods: Upper limb function was evaluated using the Fugl-Meyer assessment for upper extremity (FMA), and daily living activities were assessed with the modified Barthel index (MBI). fNIRS measured oxygenated hemoglobin values (HbO) in six regions of interest (ROIs) in the cortex: ipsilesional and contralesional primary motor cortex (PMC), supplementary motor area (SMA), and somatosensory motor cortex (SMC) [64].
Key Findings: After treatment, both groups exhibited improvements in FMA and MBI scores, but the BCI group demonstrated significantly greater functional gains at both 2 and 4 weeks. fNIRS data revealed that after 4 weeks, the BCI group showed significantly increased oxygenated hemoglobin levels in PMC and SMA compared to baseline, along with more pronounced PMC activation and higher brain network efficiency relative to the control group [64]. Improvements in brain network efficiency positively correlated with gains in both FMA and MBI scores across the cohort [64].
The following workflow diagram illustrates the experimental protocol from this study:
Stroke BCI Study Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Technologies for BCI Research
| Item | Function | Example Applications |
|---|---|---|
| EEG Cap with Electrodes | Records electrical activity from the scalp | Signal acquisition in non-invasive BCI systems [64] |
| fNIRS System | Measures cortical oxygenation through near-infrared light | Monitoring brain activation patterns in stroke rehabilitation [64] |
| BCI Signal Processing Software | Filters, processes, and classifies neural signals | Feature extraction and translation algorithms [63] |
| Exoskeleton Robotic Hand | Provides physical assistance and feedback | Upper limb rehabilitation in stroke and SCI [64] |
| fNIRS Measurement ROIs | Targets specific brain regions for monitoring | PMC, SMA, SMC in stroke recovery studies [64] |
| AI/ML Algorithms (TL, SVM, CNN) | Enhances signal classification and adaptation | Improving BCI closed-loop performance [63] |
Current Challenges and Future Trajectories
Despite promising results, BCI technology faces several challenges in neurorehabilitation. For non-invasive systems, limitations include signal noise, long calibration requirements, and variability in neural signals [63]. Invasive approaches face issues related to surgical risk, long-term stability, and tissue scarring [62]. Emerging solutions include improved sensor technology, efficient calibration protocols, and advanced AI-driven decoding models [63].
The integration of artificial intelligence and machine learning, particularly transfer learning, support vector machines, and convolutional neural networks, shows significant promise for enhancing BCI closed-loop performance [63]. These methods improve signal classification, feature extraction, and real-time adaptability, enabling more accurate monitoring of cognitive and motor states.
BCI technology represents a transformative approach in neurorehabilitation for both spinal cord injury and stroke recovery. Current evidence demonstrates that both invasive and non-invasive systems can significantly improve motor function, sensory recovery, and activities of daily living in these patient populations. The field stands roughly where gene therapies did in the 2010s or heart stents in the 1980s: on the cusp of graduating from experimental status to regulated clinical use, driven by a mix of startup innovation, academic research, and patient demand [62].
As technologies continue to advance and larger clinical trials are completed, BCI systems are poised to become integral components of neurorehabilitation protocols, offering new hope for functional recovery to individuals with neurological impairments from SCI and stroke. Future research should focus on refining AI models, improving real-time data processing, enhancing user accessibility, and establishing standardized protocols for clinical implementation.
Cognitive Monitoring and Enhancement Applications
Cognitive monitoring and enhancement represent a frontier in applied neuroscience, aiming to quantify, maintain, and improve human cognitive functions such as memory, attention, and executive control. For researchers, scientists, and drug development professionals, non-invasive Brain-Computer Interface (BCI) technologies offer powerful tools for both assessing cognitive status and potentially intervening to enhance performance. These technologies are particularly valuable for conducting longitudinal studies in clinical populations, monitoring cognitive decline, and evaluating the efficacy of pharmacological and non-pharmacological interventions. Unlike invasive BCIs, which require surgical implantation and carry associated medical risks, non-invasive approaches like electroencephalography (EEG) provide a safer, more accessible means of measuring brain activity, though they often face challenges with signal resolution and external noise [2] [3]. This whitepaper, framed within a broader review of non-invasive BCI technologies, details the core technical principles, presents quantitative data on performance, outlines experimental protocols, and visualizes the workflows central to this field.
Technical Framework of Non-Invasive BCIs for Cognitive Applications
At its core, a BCI is a system that measures central nervous system activity and converts it into an artificial output that can replace, restore, enhance, supplement, or improve natural brain outputs [62] [3]. This process creates a new channel for communicating with and controlling the external environment. The general pipeline for non-invasive BCIs, particularly those based on EEG, follows a structured sequence: Signal Acquisition → Preprocessing → Feature Extraction → Classification/Decoding → Output/Feedback [3].
For cognitive monitoring, the "output" is often a quantitative assessment of cognitive status or performance on a specific task. For cognitive enhancement, the system may enter a closed-loop , where the decoded brain state triggers a specific intervention, such as neurostimulation, to modulate brain function in real-time [65]. The non-invasive nature of EEG makes it a cornerstone for these applications; it is relatively low-cost, portable, and offers high temporal resolution, allowing researchers to track neural dynamics on the order of milliseconds [2]. However, its utility is constrained by a lower spatial resolution compared to invasive methods and a susceptibility to artifacts from muscle movement or environmental noise [66] [67].
Quantitative Data in Cognitive Monitoring
Digital cognitive assessments are increasingly used for detecting early cognitive impairment and monitoring change over time. A key consideration when using these tools repeatedly is the phenomenon of practice effects—improvements in test performance due to familiarity with the task rather than genuine cognitive change. These effects can mask early cognitive decline, leading to false-negative results in at-risk populations [68].
A 2025 study systematically evaluated practice effects using the Defense Automated Neurobehavioral Assessment (DANA) battery, a digital tool comprising six tasks designed to measure cognitive domains like processing speed, attention, and working memory [68]. The study analyzed data from 116 participants who completed two DANA sessions approximately 90 days apart.
Table 1: Practice Effects and Cognitive Impairment on DANA Tasks (90-Day Interval)
| DANA Task | Cognitive Domain Assessed | Median Practice Effect (Response Time Improvement) | Association with Cognitive Impairment |
|---|---|---|---|
| Simple Response Time (SRT) | Processing Speed | 4.2% | Significantly slower response times (p < 0.001) |
| Procedural Reaction Time (PRT) | Executive Function, Decision-Making | Data Not Specified | Significantly slower response times (p < 0.001) |
| Go/No-Go (GNG) | Sustained Attention, Impulsivity | Data Not Specified | Significantly slower response times (p < 0.001) |
| Spatial Processing (SP) | Visuospatial Analytic Ability | 0% (No significant improvement) | Not Specified |
| Code Substitution (CS) | Attention, Learning, Visual Scanning | Data Not Specified | Not Specified |
| Match-to-Sample (MTS) | Short-term Memory, Visuospatial Discrimination | Data Not Specified | Not Specified |
Source: Adapted from [68]
The data from this study indicates that practice effects on the DANA battery were generally modest, with response time improvements ranging from 0% to 4.2% across specific tasks over a 90-day interval [68]. Furthermore, cognitive impairment was significantly associated with slower response times on key tasks, demonstrating the tool's sensitivity to cognitive status. Machine learning models (logistic regression and random forest) built on this data achieved accuracies of up to 71% in classifying cognitive status [68]. This framework provides a methodology for researchers to account for practice effects when designing longitudinal cognitive monitoring studies.
Beyond monitoring, non-invasive BCIs have shown promise in direct cognitive enhancement, particularly through closed-loop systems. A 2025 study demonstrated a wearable system combining EEG monitoring with transcranial alternating current stimulation (tACS). This system identified moments of optimal neural excitability for learning and delivered precisely timed stimulation, resulting in a 40% improvement in new vocabulary learning compared to sham stimulation [65].
Experimental Protocols and Methodologies
Protocol 1: Evaluating Practice Effects in Digital Cognitive Assessments
This protocol is based on the 2025 study that used the DANA battery to establish a framework for evaluating practice effects [68].
- Objective: To systematically quantify practice effects and evaluate the sensitivity of a digital cognitive assessment tool for detecting cognitive impairment over time.
- Participants: 116 participants aged 40 and older, sourced from a longitudinal research cohort (e.g., an Alzheimer's Disease Research Center). Participants should be stratified based on cognitive status (intact vs. impaired) using standardized clinical criteria like the Clinical Dementia Rating (CDR) scale.
- Materials and Software:
- Digital Cognitive Battery: The DANA software, administered via a smartphone or tablet. DANA includes tasks like Simple Response Time (SRT), Go/No-Go (GNG), and Spatial Processing (SP).
- Clinical Assessment Data: Demographics, clinical interviews, and neurological examination data collected according to a standardized protocol (e.g., the National Alzheimer's Coordinating Center Uniform Data Set).
- Procedure:
- Baseline Session (Session 1): Participants complete the full DANA battery in an unsupervised, remote setting. The software records response times (milliseconds) and accuracy for each task.
- Follow-up Session (Session 2): After a target interval of 90 days (with an allowable range, e.g., 48-132 days), participants complete the DANA battery again under identical conditions.
- Data Analysis:
- Calculate percent change in mean response time for correct answers between Session 1 and Session 2 for each task to quantify practice effects.
- Use linear regression models with random intercepts to assess the association between cognitive status (independent variable) and response time (dependent variable), while controlling for age, education, and sex.
- Train machine learning classifiers (e.g., logistic regression, random forest) on the response time and demographic data to predict cognitive status, evaluating performance via accuracy and other relevant metrics.
Protocol 2: P300-Based BCI for Environmental Control
This protocol outlines a method for using a P300-based BCI for cognitive tasks like environmental control, which can be adapted to assess attention and working memory.
- Objective: To implement and test a P300 BCI paradigm for controlling external devices, measuring performance through accuracy and information transfer rate.
- Participants: 10 healthy adults with normal or corrected-to-normal vision and no history of neurological disease.
- Materials and Hardware:
- EEG System: A 32-channel EEG cap with active or passive electrodes.
- Stimulus Presentation Screen: A computer monitor to display the BCI paradigm.
- Software: EEG data acquisition software (e.g., BCI2000, OpenVibe) and a stimulus presentation program.
- Stimulus Paradigm:
- A 4x3 matrix of 12 symbols, each representing a different action (e.g., "turn on light," "call phone") is displayed on the screen.
- The symbols are intensified (flashed) in a random sequence. The user is instructed to focus their attention on the symbol they wish to select and mentally count how many times it flashes.
- Procedure:
- EEG Setup: Apply the EEG cap according to the 10-20 international system. Ensure electrode impedances are kept below a threshold (e.g., 10 kΩ).
- Calibration/Training Phase: Record EEG data while the participant focuses on a known, cued symbol. This data is used to train the classifier.
- Online Testing Phase: The participant freely selects symbols without cueing. The system records EEG data, processes it in real-time, and selects the symbol that elicits the strongest P300 response.
- Data Processing & Analysis:
- Preprocessing: Band-pass filter the raw EEG (e.g., 0.1-30 Hz) and artifact removal (e.g., for eye blinks).
- Epoch Extraction: Extract EEG epochs time-locked to each symbol flash (e.g., 0-800 ms post-stimulus).
- Feature Classification: Use a machine learning classifier, such as Random Forest, to distinguish between target (P300 present) and non-target (P300 absent) flashes. The classified outputs are used to determine the participant's selected symbol.
- Performance Calculation: The system's accuracy is calculated as the percentage of correctly identified symbols. The study employing this protocol achieved an average online accuracy of 92.25% [69].
Workflow and System Diagrams
Non-Invasive BCI Cognitive Assessment Workflow
The following diagram illustrates the end-to-end workflow for a typical non-invasive BCI system used for cognitive assessment, from participant setup to data interpretation.
Closed-Loop Cognitive Enhancement System
This diagram details the architecture of a closed-loop system for cognitive enhancement, which dynamically adjusts its operation based on real-time brain activity.
The Scientist's Toolkit: Research Reagent Solutions
The following table catalogues essential hardware, software, and methodological components for building and deploying non-invasive BCIs for cognitive research.
Table 2: Essential Research Tools for Non-Invasive BCI Cognitive Studies
| Item Name | Type | Primary Function | Example Use Case |
|---|---|---|---|
| 32-channel EEG Cap | Hardware | Records electrical brain activity from the scalp. | Acquiring neural signals during a P300 spelling task or resting-state measurement [69]. |
| Dry EEG Electrodes | Hardware | Records EEG without conductive gel; improves user comfort and setup speed. | Enabling quicker setup for longitudinal consumer-grade or frequent cognitive monitoring studies [8]. |
| DANA Battery | Software | A digital battery of cognitive tasks measuring response time across multiple domains. | Longitudinal monitoring of cognitive status and quantifying practice effects in clinical populations [68]. |
| Random Forest Classifier | Algorithm | A machine learning method for classifying brain states from neural features. | Detecting the P300 event-related potential in single-trial EEG data for BCI control [69]. |
| Transcranial Alternating Current Stimulation (tACS) | Hardware/Intervention | Delieves weak oscillating electrical currents to modulate brain rhythms. | Enhancing memory consolidation by applying stimulation during slow-wave sleep [65]. |
| fNIRS System | Hardware | Measures hemodynamic changes in the cortex using near-infrared light. | Monitoring prefrontal cortex activity during complex cognitive tasks where EEG may be too noisy. |
| BCI2000 / OpenVibe | Software Platform | Provides a general-purpose software framework for BCI data acquisition, processing, and validation. | Prototyping and running a motor imagery or P300-based BCI paradigm [3]. |
Flexible Brain Electronic Sensors (FBES) and Wearable System Integration
Flexible Brain Electronic Sensors (FBES) represent a paradigm shift in neural interface technology, forming the core of next-generation non-invasive Brain-Computer Interfaces (BCIs). These sensors, characterized by their superior flexibility, biocompatibility, and ability to form conformal contact with biological tissues, are revolutionizing the landscape of health monitoring, neurological disorder treatment, and human-machine interaction [70]. The evolution from traditional rigid sensors to flexible alternatives addresses critical challenges of mechanical mismatch, tissue damage, and long-term signal stability, thereby accelerating the transition of BCI technologies from laboratory settings to practical healthcare implementations [70] [71]. This technical guide provides a comprehensive analysis of FBES, encompassing their fundamental principles, material foundations, sensor architectures, system integration strategies, and experimental methodologies, framed within the context of non-invasive BCI technology review and comparisons.
The performance of FBES is contingent upon the synergistic integration of materials science, electrical engineering, and biomedical engineering. Unlike traditional rigid sensors that exhibit poor tensile, bending, and fatigue resistance, FBES leverage advanced flexible materials to enable continuous monitoring of brain vital signs with minimal discomfort and risk [70]. With brain signals being exceptionally weak – electroencephalography (EEG) signals measure merely 10–50 μV, and magnetoencephalogram (MEG) signals originating from synchronized activity of 10⁵ neurons show about 100 fT in intensity – the acquisition and anti-noise capabilities of FBES present unique engineering challenges that require multidirectional, multidimensional, and multilevel approaches to physiological signal monitoring [70].
Materials and Manufacturing Technologies
Substrate and Functional Materials
The development of high-performance FBES relies fundamentally on advanced materials that provide mechanical flexibility, stretchability, biocompatibility, and stable electrical properties. Table 1 summarizes the key material classes used in FBES fabrication, their properties, and representative applications.
Table 1: Material Classes for Flexible Brain Electronic Sensors
| Material Class | Key Properties | Representative Materials | Primary Applications |
|---|---|---|---|
| Polymer Substrates | Flexibility, stretchability, biocompatibility | Polyimide (PI), Polydimethylsiloxane (PDMS), Ecoflex, Parylene | Structural support, encapsulation, flexible carriers |
| Conductive Hydrogels | High ionic conductivity, tissue-like mechanics, adhesion | PVA/P(AM/AA/C18)-LiCl double-network hydrogels, PEG-based hydrogels | Electrode-skin interface, signal transduction |
| 2D Materials | Excellent conductivity, high sensitivity, thinness | Graphene, MXene, transition metal sulfides | Active sensing elements, conductive traces |
| Conductive Polymers | Flexibility, mixed ionic-electronic conduction | PEDOT:PSS, polyaniline | Electrode coating, signal acquisition |
| Metallic Materials | High electrical conductivity, stability | Gold nanoparticles, silver nanowires, thin metal films | Electrodes, interconnects |
Polymer substrates serve as the mechanical backbone of FBES, providing physical support while enabling intimate contact with curved and dynamic biological surfaces. Polyimide offers excellent thermal stability and moderate flexibility, making it suitable for microscale patterning [72]. Elastomers like PDMS and Ecoflex provide superior stretchability and skin conformity, with Ecoflex encapsulation demonstrating 50% higher conductance under 250% strain and maintaining stability over 1000 stretching cycles [72].
Conductive hydrogels have emerged as particularly promising materials for FBES due to their tissue-like mechanical properties, high ionic conductivity, and inherent biocompatibility. Recent innovations include double-network (DN) hydrogel designs that significantly enhance mechanical robustness. For instance, PVA/P(AM/AA/C18)-LiCl DN hydrogels incorporate octadecyl groups (C18) to enhance hydrophobicity, skin adhesion, and mechanical flexibility while maintaining stable conductivity in low-temperature environments [73]. These hydrogels demonstrate stable performance for real-time EEG signal acquisition even in challenging conditions.
Two-dimensional materials like graphene and MXene offer exceptional electrical, mechanical, and chemical properties ideal for thin, conformal FBES. Their high surface-to-volume ratio, transparency, and tunable electronic properties enable the development of sensors with high sensitivity and fast response times [74]. These materials can be integrated into heterojunction structures to further enhance conductivity, sensitivity, and stability of flexible devices [74].
Manufacturing Processes and Sensor Architectures
Advanced manufacturing techniques enable the transformation of these innovative materials into functional FBES devices. Micro-nano fabrication techniques based on flexible substrates, including laser processing, nanoimprinting, and high-precision printing, drive flexible devices toward ultra-thin, highly integrated, and multifunctional designs [74]. Printed electronics, roll-to-roll processing, and flexible packaging technology facilitate the large-scale production and application of flexible electronics [74].
Sensor architectures have evolved significantly to optimize performance for neural signal acquisition. The classification of FBES based on invasiveness includes:
Non-invasive Electrodes: Placed on the scalp, forehead, or ear canal without breaching the skin. These include dry, semi-dry, and wet electrodes with various material compositions and interface mechanisms [71]. Recent innovations include microneedle array electrodes (MAEs) that penetrate the stratum corneum to reduce impedance and motion artifacts [71].
Semi-invasive Electrodes: Typically electrocorticography (ECoG) electrodes placed on the brain's surface without penetration. These offer higher spatial resolution than non-invasive approaches while causing fewer infections and immune responses than fully invasive electrodes [71]. Ultrathin (30 μm) micro-ECoG arrays with thousands of channels (1024–2048) improve signal quality and reduce interference [71].
Invasive Electrodes: Penetrate brain tissue to record single neuron potentials, providing the highest signal quality. Flexible versions utilize materials like silicon microneedle arrays (SiMNA) with flexible substrates, hydrogel-based interfaces, and hybrid probes integrating micro-wires, optical fibers, and microfluidic channels in polyacrylamide-alginate hydrogel matrices [71].
Diagram 1: Classification of Flexible Brain Electronic Sensors by Invasiveness
Sensing Mechanisms and Signal Characteristics
FBES operate based on various transduction mechanisms that convert physiological signals into measurable electrical outputs. The choice of sensing mechanism depends on the target application, required sensitivity, spatial and temporal resolution, and power constraints.
Table 2: Sensing Mechanisms in Flexible Brain Electronic Sensors
| Sensing Mechanism | Physical Principle | Key Advantages | Limitations | Applications in BCI |
|---|---|---|---|---|
| Electrochemical | Measures electrical potentials from neural activity | High sensitivity, real-time monitoring, selective detection | Limited lifespan, susceptible to environmental conditions | EEG, ECoG, neural potential recording |
| Piezoelectric | Converts mechanical stress from brain motions into electrical signals | High precision, no external power needed | Limited flexibility, material degradation over time | Seizure detection, intracranial pressure monitoring |
| Capacitive | Measures changes in capacitance due to deformation or proximity | High flexibility, lightweight, low energy consumption | Sensitivity to environmental factors (humidity, temperature) | EEG, motion artifact detection |
| Triboelectric | Generates charge from friction between materials | Self-powered capability, high sensitivity | Signal stability challenges for continuous monitoring | In-ear BCIs, facial expression monitoring |
| Optical | Uses light to detect neural activity-related changes | Immunity to electromagnetic interference, high spatial resolution | Limited penetration depth, requires external components | fNIRS, functional brain imaging |
Electrochemical sensing represents the most common mechanism for electrical neural signal acquisition (EEG, ECoG). FBES based on this mechanism typically use conductive hydrogels or polymer-based electrodes to establish a stable electrochemical interface with the skin or neural tissue [73] [71]. The ionic conductivity of hydrogels enables efficient transmission of bioelectrical signals from the skin to the acquisition system, with recent advances in DN hydrogels significantly improving signal stability and fidelity [73].
Triboelectric sensors have gained attention for their self-powering capabilities, converting mechanical energy from physiological motions into electrical signals. For instance, ear-worn triboelectric sensors have been developed that enable continuous monitoring of facial expressions by harnessing movements from the ear canal [70]. These sensors can operate effectively as part of dual-modal wearable BCI systems when combined with visual stimulation approaches.
The performance characteristics of different BCI technologies vary significantly based on their sensing mechanisms and implementation approaches. Non-invasive technologies like EEG provide broad coverage and safety but suffer from limited spatial resolution and signal attenuation through the skull, which can cause electrical signal attenuation of up to 80–90% [70]. Invasive approaches offer superior signal quality but require surgical implantation and carry associated risks. Semi-invasive strategies attempt to balance these trade-offs, with technologies like the Stentrode demonstrating promising results by being implanted via blood vessels to record signals through vessel walls [62].
System Integration and Engineering Strategies
Self-Powered Systems and Energy Management
The integration of self-powered technologies represents a critical advancement in wearable BCI systems, addressing the fundamental challenge of sustainable energy supply for continuous operation. All-in-one self-powered wearable biosensor systems combine energy harvesting, management, storage, and sensing functionalities into compact, wearable form factors [75]. These systems typically incorporate energy harvesters that capture ambient energy from human motion, temperature gradients, or biochemical sources, converting it into electrical power for system operation.
Recent innovations in self-powered systems for FBES include the development of wireless EEG monitoring systems integrating wearable self-powered flexible sensors [73]. These systems combine advanced hydrogel sensors with self-powered energy harvesting technology, enabling stable and efficient EEG signal acquisition without external power sources. The energy harvester collects mechanical energy from human motion, converts it into electricity, and stores it in integrated lithium batteries to provide real-time, independent power for wearable EEG devices [73].
Power management strategies must carefully match the output of energy harvesting modules with the power consumption requirements of signal processing and transmission modules. This balance is essential for achieving sustainable all-in-one designs that can operate continuously in real-world settings [75]. Recent systems have demonstrated the feasibility of this approach, with some achieving ultra-high output performance that enables functionality even in low-temperature environments, significantly improving reliability during monitoring [73].
Signal Processing and Machine Learning Integration
The integration of advanced signal processing and machine learning algorithms has dramatically enhanced the functionality and performance of FBES-based systems. These computational approaches address challenges such as noise reduction, feature extraction, and classification of neural states.
A representative implementation is the wireless EEG monitoring system that employs the Variational Mode Decomposition (VMD) algorithm to extract multi-scale time-frequency features from EEG signals, combined with Long Short-Term Memory (LSTM) networks for time-series data analysis [73]. This combination has demonstrated significant efficiency and feasibility in real-time sleep staging applications, providing a promising solution for wearable EEG monitoring and sleep health management.
Machine learning further enhances FBES through optimized sensor design and performance refinement. For instance, flexible tactile sensors based on triboelectric nanogenerators have leveraged machine learning for optimized device design, including output signal selection and manufacturing parameter refinement [74]. Through co-design of tactile performance using machine learning and manufacturing parameters, such sensors have achieved classification accuracy of approximately 99.58% for applications like handwriting recognition [74].
The synergy between flexible electronics and AI enables more sophisticated and comprehensive analysis of raw data collected from flexible sensors. Trained models can classify, identify, and predict values based on single or multimodal sensor inputs, significantly expanding the interpretability and utility of FBES systems [74]. This integration is particularly valuable for applications requiring real-time responsiveness and advanced analytics, such as closed-loop robotic control or adaptive BCIs.
Diagram 2: Machine Learning-Enhanced Signal Processing Workflow for FBES
Wireless Communication and System-Level Integration
Wireless transmission represents a critical enabling technology for wearable BCI systems, eliminating cumbersome cables that restrict mobility and real-world application. The evolution of wearable BCI systems for data acquisition and control is increasingly pivoting toward wireless transmission methods, facilitating broader adoption in daily life [70].
Modern wireless EEG systems incorporate flexible printed circuits (FPCs), lithium-polymer batteries, adhesives, and skin-conformable form factors that enable extended monitoring with minimal discomfort [73]. These integrated systems address limitations of traditional EEG monitoring devices in terms of convenience, continuity, and self-powering capability, providing feasible solutions for broader health management applications.
System-level integration also involves the development of novel form factors that enhance wearability and user acceptance. In-ear EEG systems have gained attention due to their proximity to the central nervous system and discreteness [70]. For example, visual and auditory BCI systems based on in-ear bioelectronics that expand spirally along the auditory canal by electrothermal drive have achieved 95% offline accuracy in BCI classification for steady-state visual evoked potentials (SSVEP) [70]. Similarly, integrated arrays of electrochemical and electrophysiological sensors positioned on flexible substrates around headsets enable monitoring of lactate concentration and brain state [70].
Experimental Protocols and Methodologies
Fabrication of Self-Powered Wireless EEG Monitoring System
The development of an integrated self-powered wireless EEG monitoring system involves multiple meticulous steps to ensure optimal performance and reliability:
Hydrogel Sensor Preparation:
- Synthesize PVA/P(AM/AA/C18)-LiCl double-network hydrogel by first creating a P(AM/AA/C18) primary network through free-radical polymerization of acrylamide (AM), acrylic acid (AA), and octadecyl methacrylate (C18) monomers.
- Incorporate the secondary network by introducing polyvinyl alcohol (PVA) solution with lithium chloride (LiCl) as conductive agent.
- Crosslink the structure using ammonium persulfate (APS) as initiator and N,N'-methylene acrylamide (MBAA) as crosslinker.
- Form the DN structure through physical crosslinking and hydrogen bonding, creating a reinforced architecture with greater toughness and tensile strength compared to single-network hydrogels [73].
System Integration:
- Fabricate flexible printed circuits (FPCs) using photolithography and etching processes on polyimide substrates.
- Integrate lithium-polymer batteries with appropriate adhesives for secure attachment to the flexible substrate.
- Assemble the self-powered energy harvester module capable of capturing mechanical energy from human motion.
- Connect the hydrogel sensors to the FPCs, ensuring low-impedance interfaces for optimal signal transmission [73].
System Validation:
- Characterize electrochemical impedance of hydrogel sensors using electrochemical impedance spectroscopy (EIS).
- Evaluate mechanical properties through tensile testing and cyclic strain measurements.
- Validate freeze-resistant properties by testing conductivity and sensor performance at low temperatures.
- Assess signal quality through comparison with commercial EEG systems using standard protocols [73].
Performance Evaluation and Benchmarking
Rigorous performance evaluation is essential for validating FBES systems. Key experimental protocols include:
Signal Quality Assessment:
- Calculate signal-to-noise ratio (SNR) by comparing acquired neural signals to baseline noise levels during rest states.
- Measure electrode-skin contact impedance using impedance spectroscopy at relevant frequencies (typically 1-100 Hz for EEG).
- Evaluate common-mode rejection ratio (CMRR) to assess system capability to reject environmental interference.
- Quantify signal stability through long-term recordings under various conditions (stationary, motion, different environments) [73] [71].
Comparative Studies:
- Conduct parallel recordings with FBES and clinical-grade monitoring systems to establish correlation coefficients.
- Perform user studies to evaluate comfort, ease of use, and long-term wearability across diverse populations.
- Assess robustness to motion artifacts through controlled movement protocols.
- Validate algorithm performance for specific applications (e.g., sleep staging, seizure detection) against expert annotations [73].
Environmental Testing:
- Evaluate performance across temperature and humidity ranges to determine operational limits.
- Test freeze resistance by monitoring signal quality during temperature cycling.
- Assess durability through mechanical stress tests (bending, twisting, stretching) relevant to intended use cases [73].
Research Reagent Solutions and Essential Materials
Successful development and implementation of FBES require specific research reagents and materials optimized for flexible bioelectronics. The following table details essential components and their functions in FBES research and development.
Table 3: Essential Research Reagents and Materials for FBES Development
| Category | Specific Materials | Function/Purpose | Application Examples |
|---|---|---|---|
| Polymer Substrates | Polyimide (PI), PDMS, Ecoflex, Parylene | Flexible structural support, encapsulation | Flexible printed circuits, device packaging |
| Conductive Materials | Gold nanoparticles, silver nanowires, PEDOT:PSS | Electrode fabrication, signal conduction | Neural electrodes, interconnects |
| Hydrogel Components | PVA, acrylamide (AM), acrylic acid (AA), LiCl | Ionic conduction, skin interface | EEG electrodes, biosensing interfaces |
| Crosslinkers & Initiators | MBAA, ammonium persulfate (APS) | Polymer network formation | Hydrogel synthesis, polymer curing |
| 2D Materials | Graphene, MXene, transition metal sulfides | High-sensitivity sensing elements | Active sensor layers, conductive composites |
| Encapsulation Materials | Ecoflex, silicone elastomers | Environmental protection, mechanical stability | Device encapsulation, water resistance |
Current Challenges and Future Directions
Despite significant advances, FBES technology faces several persistent challenges that require continued research and development efforts:
Signal Quality and Stability: The skull's shielding effect and signal attenuation remain fundamental challenges, with electrical conductivity differences between skull (0.01–0.02 S/m) and scalp (0.1–0.3 S/m) resulting in electrical signal attenuation of up to 80–90% [70]. Low-frequency signals like Delta and Theta waves experience the most prominent attenuation. Future research directions focus on developing signal enhancement algorithms and novel sensor placements that bypass skull interference, such as in-ear or endovascular approaches.
Biocompatibility and Long-Term Stability: While flexible materials generally offer improved biocompatibility compared to rigid alternatives, challenges remain in ensuring long-term stability and minimal immune response [70] [71]. For invasive and semi-invasive applications, tissue response to chronic implantation requires further optimization of surface chemistry and mechanical properties to match neural tissue more closely.
Power Management and System Integration: Achieving optimal balance between power consumption and functionality remains challenging for self-powered systems [75]. Future directions include the development of more efficient energy harvesters, low-power electronics, and intelligent power management systems that dynamically adjust operational modes based on available energy and monitoring requirements.
Manufacturing and Scalability: Transitioning from laboratory prototypes to mass-produced devices requires advances in manufacturing techniques that ensure consistency, reliability, and cost-effectiveness [74]. Printed electronics, roll-to-roll processing, and other scalable fabrication methods show promise for addressing these challenges.
Multimodal Integration and Data Fusion: Future FBES systems will increasingly incorporate multiple sensing modalities (electrical, optical, chemical) to provide more comprehensive neural activity monitoring [70]. This approach requires sophisticated data fusion algorithms and careful sensor design to minimize interference between modalities while maximizing synergistic benefits.
The next research hotspots in FBES development will focus on reducing power consumption, optimizing microprocessor performance, implementing advanced machine learning techniques, and exploring multimodal information parallel sampling [70]. These advances will accelerate the utilization of wearable BCI technology based on FBES in brain disease diagnosis, treatment, and rehabilitation, ultimately bridging the gap between laboratory research and practical healthcare implementations.
The field of non-invasive Brain-Computer Interfaces (BCIs) is increasingly embracing multimodal integration to overcome the inherent limitations of single-modality systems. Among the most promising combinations is the integration of electroencephalography (EEG) with functional near-infrared spectroscopy (fNIRS), an approach that captures complementary aspects of brain activity by merging electrophysiological signals with hemodynamic responses [76] [77]. This synergy offers a more comprehensive window into brain function, providing both the millisecond-scale temporal resolution of EEG and the superior spatial localization of fNIRS within a single, portable system [78]. Such hybrid systems are particularly transformative for clinical applications, including neurorehabilitation for stroke and intracerebral hemorrhage (ICH) patients, where understanding the complex relationship between neural electrical activity and vascular responses is critical for developing effective interventions [79] [80].
The technical rationale for this integration is robust. EEG alone suffers from limited spatial resolution and susceptibility to motion artifacts, while fNIRS offers better spatial specificity but slower response times due to the inherent latency of hemodynamic processes [76]. By combining these modalities, researchers can simultaneously monitor rapid neuronal firing and the subsequent metabolic changes in specific cortical regions, enabling a more complete decoding of motor intention, cognitive load, and other brain states [81] [82]. This whitepaper provides an in-depth technical examination of hybrid EEG-fNIRS methodologies, detailing experimental protocols, data analysis frameworks, and implementation tools essential for advancing research in non-invasive BCI technologies.
Technical Foundations of EEG and fNIRS
Core Principles and Complementary Nature
Electroencephalography (EEG) records electrical potentials generated by the synchronous firing of neuronal populations via electrodes placed on the scalp. Its key advantage is exceptional temporal resolution (milliseconds), allowing for real-time tracking of brain dynamics such as event-related potentials (ERPs) and neural oscillations in frequency bands like alpha (8-12 Hz) and beta (12-30 Hz) [76] [78]. However, EEG signals are subject to volume conduction through the skull and cerebrospinal fluid, which blurs their spatial origin and results in relatively poor spatial resolution [76].
Functional Near-Infrared Spectroscopy (fNIRS) is an optical neuroimaging technique that measures hemodynamic changes associated with neural activity. It employs near-infrared light (700-900 nm) to penetrate the scalp and skull, quantifying concentration changes in oxygenated hemoglobin (HbO) and deoxygenated hemoglobin (HbR) based on their distinct absorption spectra [76] [77]. fNIRS provides superior spatial localization (5-10 mm resolution) and is less susceptible to motion artifacts than EEG, making it suitable for more ecologically valid environments [79]. Its primary limitation is a slower temporal response, constrained by the hemodynamic response function which unfolds over seconds [76].
Table 1: Comparative Technical Specifications of EEG and fNIRS
| Feature | EEG | fNIRS |
|---|---|---|
| Measured Signal | Electrical potential from neuronal firing | Hemodynamic changes (HbO & HbR concentration) |
| Temporal Resolution | Millisecond-level (≈1000 Hz) | Slower (≈10 Hz), hemodynamic delay |
| Spatial Resolution | Low (several cm) due to volume conduction | Moderate (5-10 mm), better localization |
| Portability | High | High |
| Artifact Sensitivity | Sensitive to electrical noise & muscle movement | Less susceptible to electrical artifacts |
| Primary Applications | Real-time brain state decoding, event-related potentials | Localized cortical activation mapping, sustained cognitive state monitoring |
Neurophysiological Basis for Integration
The combination of EEG and fNIRS is physiologically grounded in the principle of neurovascular coupling – the tight relationship between neuronal electrical activity and subsequent changes in cerebral blood flow and oxygenation [77]. During localized neural activation, EEG captures the immediate electrophysiological events (e.g., event-related desynchronization in sensorimotor rhythms), while fNIRS tracks the delayed hemodynamic response that supplies oxygen and nutrients to active tissue [79] [80]. This complementary relationship enables researchers to construct a more complete picture of brain function, from initial neural firing to the resulting metabolic demands.
Experimental Design and Methodologies
Motor Imagery Paradigms for Clinical Populations
Standardized experimental paradigms are crucial for eliciting robust, interpretable signals in hybrid BCIs. The motor imagery (MI) paradigm – where participants mentally simulate a movement without executing it – has proven particularly effective for both healthy subjects and clinical populations such as intracerebral hemorrhage (ICH) and stroke patients [79] [80].
A representative protocol from the HEFMI-ICH dataset illustrates a rigorous approach [79]:
- Participant Preparation: The study included 17 normal subjects (mean age 23.6±1.8 years) and 20 ICH patients (mean age 50.8±10.3 years), with clinical assessments using Fugl-Meyer Assessment for Upper Extremities (FMA-UE), Modified Barthel Index (MBI), and modified Rankin Scale (mRS).
- Grip Strength Calibration: To enhance MI vividness, participants underwent a preparatory phase using a dynamometer and stress ball, involving maximal force exertions and grip training at one contraction per second. This reinforced tactile and force-related aspects of movement.
- Task Structure: Each trial began with a 2-second visual cue (directional arrow), followed by a 10-second execution phase where participants performed kinesthetic MI of hand grasping at 1 Hz, concluding with a 15-second rest interval.
- Session Design: Each session contained 30 trials (15 left/right hand MI), with at least two sessions per participant and adjustable inter-session breaks to mitigate fatigue.
This protocol successfully addressed a common challenge in MI studies: some patients initially struggled with the abstract concept of "motor imagery," confirming the need for concrete preparatory exercises to improve signal quality [79].
Signal Acquisition and Hardware Integration
Precise signal acquisition and temporal synchronization are critical technical challenges in multimodal BCI systems. The HEFMI-ICH study employed a synchronized setup with [79]:
- EEG Acquisition: 32 electrodes configured according to an expanded international 10-20 system, recorded at 256 Hz using a g.HIamp amplifier.
- fNIRS Acquisition: 32 optical sources and 30 photodetectors generating 90 measurement channels through source-detector pairing (3 cm separation), recorded at 11 Hz using a continuous-wave NirScan system.
- Temporal Synchronization: Event markers from E-Prime 3.0 simultaneously triggered both recording systems during experimental paradigms.
- Customized Cap Design: A hybrid EEG-fNIRS cap with optimized topography ensured comprehensive coverage of prefrontal, motor, and association cortices while maintaining consistent probe placement.
The integration of EEG electrodes and fNIRS optodes presents substantial technical challenges. Current approaches include using flexible EEG caps as a foundation with punctures for fNIRS probes, though this can lead to inconsistent scalp coupling pressure [77]. Emerging solutions involve 3D-printed customized helmets and cryogenic thermoplastic sheets that can be molded to individual head shapes, improving comfort and signal stability [77].
Diagram 1: Experimental workflow for hybrid EEG-fNIRS
Data Analysis and Fusion Strategies
Multimodal Integration Approaches
The integration of EEG and fNIRS data occurs at three primary levels, each with distinct advantages and implementation considerations:
Parallel Data Analysis involves independent processing of each modality with subsequent correlation of findings. This approach maintains the integrity of each signal's unique characteristics and is often employed in initial exploratory studies. For BCI applications, parallel analysis typically involves training separate classifiers for EEG and fNIRS features, with a meta-classifier (e.g., weighted voting) making the final decision [81]. Studies have demonstrated that this approach can improve classification accuracy by approximately 5% compared to single-modality systems [76].
Informed Data Analysis uses information from one modality to constrain or guide the analysis of the other, creating a more physiologically grounded integration:
- fNIRS-informed EEG analysis: The activation maps derived from fNIRS provide spatial constraints for EEG source localization, an otherwise ill-posed inverse problem. This combination enhances the accuracy of identifying neural generators of electrical activity [81].
- EEG-informed fNIRS analysis: EEG features (e.g., event-related potentials or band power changes) serve as regressors in the General Linear Model (GLM) analysis of fNIRS data, offering a more precise model of the expected hemodynamic response than standard boxcar functions [81].
Feature-Level Fusion creates a unified feature vector by concatenating temporally aligned features from both modalities before classification. This method requires careful normalization to address the different scales and temporal characteristics of EEG and fNIRS data [76] [80]. For example, one might combine EEG band power (alpha, beta) with fNIRS HbO/HbR concentration means and slopes, followed by dimension reduction techniques to manage the high feature dimensionality [76].
Decision-Level Fusion maintains separate classification pathways for each modality, combining their outputs at the final decision stage. The Dempster-Shafer Theory (DST) of evidence has emerged as an advanced framework for this approach, effectively modeling and combining uncertainties from both modalities [82]. Recent implementations using Dirichlet distribution parameter estimation for uncertainty quantification have achieved classification accuracies of 83.26% for motor imagery tasks [82].
Advanced Computational Frameworks
Transfer learning has recently been applied to address the critical challenge of cross-subject generalization in hybrid BCIs, particularly for clinical populations. A novel framework incorporating a Wasserstein metric-driven source domain selection method quantifies inter-subject neural distribution divergence, enabling effective knowledge transfer from normal subjects to ICH patients [80]. This approach achieved 74.87% mean classification accuracy on patient data when trained with optimally selected normal templates, significantly outperforming conventional models [80].
Deep learning architectures are increasingly being designed specifically for heterogeneous neural data. For EEG, spatiotemporal features can be extracted using dual-scale temporal convolution and depthwise separable convolution, while fNIRS signals benefit from spatial convolution across channels combined with gated recurrent units (GRUs) to capture temporal dynamics [82]. Hybrid attention mechanisms further enhance model sensitivity to salient neural patterns across both modalities [82].
Table 2: Performance Comparison of Fusion Strategies in Motor Imagery Classification
| Fusion Method | Key Features | Reported Accuracy | Advantages | Limitations |
|---|---|---|---|---|
| Parallel Analysis with Meta-Classifier [76] | Separate EEG & fNIRS feature extraction, LDA classifiers, meta-decision | ~5% improvement over single modality | Maintains modality-specific strengths, relatively simple implementation | Limited cross-modal integration, may not capture synergistic relationships |
| Feature-Level Fusion with JMI Optimization [76] | Band power (EEG), HbO/HbR (fNIRS), Joint Mutual Information feature selection | Improved performance in force/speed MI discrimination | Enables rich feature interaction, can discover novel cross-modal patterns | High dimensionality requires robust feature selection, sensitive to temporal alignment |
| Decision-Level Fusion with Dempster-Shafer Theory [82] | Dirichlet distribution for uncertainty modeling, two-layer evidence reasoning | 83.26% (3.78% improvement over baseline) | Effectively handles modality uncertainty, robust to missing data | Computationally complex, requires careful parameter tuning |
| Transfer Learning with Wasserstein Metric [80] | Neural distribution divergence quantification, cross-subject adaptation | 74.87% (normal to ICH patient transfer) | Addresses clinical population variability, improves generalizability | Requires comprehensive source domain dataset |
Implementation and Practical Applications
The Scientist's Toolkit: Essential Research Reagents and Materials
Implementing a hybrid EEG-fNIRS research program requires specific hardware, software, and analytical tools. The following table details essential components and their functions based on current research practices:
Table 3: Essential Research Toolkit for Hybrid EEG-fNIRS Investigations
| Component | Specification/Example | Function/Purpose |
|---|---|---|
| EEG Amplifier | g.HIamp (g.tec), 32+ channels, 256+ Hz sampling | Records electrical brain activity with millisecond temporal resolution |
| fNIRS System | NirScan (Danyang Huichuang), 32 sources, 30 detectors | Measures hemodynamic responses via near-infrared light absorption |
| Hybrid Cap | Custom design with integrated EEG electrodes & fNIRS optodes | Ensures proper co-registration and consistent scalp coupling for both modalities |
| Stimulation Software | E-Prime 3.0, PsychToolbox | Presents standardized paradigms and sends synchronization markers |
| Data Analysis Platforms | MATLAB, Python (MNE, PyTorch) | Preprocessing, feature extraction, and multimodal fusion algorithms |
| Synchronization Interface | Custom trigger interface, Lab Streaming Layer (LSL) | Aligns EEG and fNIRS data streams with sub-second precision |
| Clinical Assessment Tools | Fugl-Meyer Assessment (FMA-UE), Modified Barthel Index (MBI) | Quantifies patient motor function and independence for correlation with neural data |
Clinical Applications and Validation
Hybrid EEG-fNIRS systems have demonstrated particular promise in neurorehabilitation, where they address critical limitations of conventional unimodal approaches. For intracerebral hemorrhage (ICH) patients, these systems can detect residual motor planning capabilities despite significant structural damage, enabling more targeted rehabilitation strategies [79] [80]. The HEFMI-ICH dataset revealed fundamental differences in neural activation patterns between normal subjects and ICH patients, with patients showing reduced α/β event-related desynchronization (ERD) in contralateral sensorimotor cortex during motor imagery tasks [80].
Beyond motor rehabilitation, hybrid systems show potential for various clinical applications:
- Disorders of Consciousness: Detecting residual cognitive function in minimally conscious states through combined analysis of evoked potentials and hemodynamic responses [83].
- Epilepsy Monitoring: Improved localization of seizure foci by combining EEG's temporal precision with fNIRS's spatial specificity [77].
- Neurodevelopmental Disorders: Characterizing atypical neurovascular coupling in conditions like ADHD and autism spectrum disorder [77] [83].
- Neuroprosthetics: Creating more robust control systems for assistive devices by simultaneously decoding movement intention and monitoring cognitive load [78] [62].
The field of hybrid EEG-fNIRS BCIs continues to evolve rapidly, with several emerging trends shaping its future trajectory. Miniaturization and wireless technology are making these systems more practical for real-world applications beyond laboratory settings [62] [77]. Advanced deep learning architectures specifically designed for heterogeneous temporal data are improving classification performance while reducing reliance on manual feature engineering [80] [82]. The development of standardized analysis pipelines and shared public datasets like HEFMI-ICH is addressing reproducibility challenges and accelerating methodological innovation [79].
Technical challenges remain, particularly in achieving seamless hardware integration with optimized ergonomics, managing the computational demands of real-time multimodal processing, and establishing robust protocols for cross-subject and cross-population generalization [80] [77]. The integration of additional biosignals such as eye tracking, electromyography (EMG), and electrodermal activity may further enhance the capabilities of multimodal systems [78].
In conclusion, hybrid EEG-fNIRS approaches represent a significant advancement in non-invasive BCI technology, offering a more comprehensive characterization of brain function by leveraging the complementary strengths of electrophysiological and hemodynamic signals. As technical integration becomes more sophisticated and analytical methods more powerful, these systems are poised to transform both fundamental neuroscience research and clinical practice in neurology and neurorehabilitation. The continued refinement of multimodal frameworks will be essential for unlocking the full potential of non-invasive BCIs and addressing the complex challenges of neurological disorders.
Wireless and Portable Systems for Real-World Deployment
The evolution of brain-computer interfaces (BCIs) from laboratory settings to real-world applications is critically dependent on the advancement of wireless and portable systems. Non-invasive BCIs, which primarily use technologies like electroencephalography (EEG), offer a safe and practical method for brain monitoring outside clinical environments [2]. The transition to portable platforms enables their use in daily life, expanding applications from medical rehabilitation to cognitive enhancement and entertainment [3]. This shift is driven by innovations in dry electrodes, wearable hardware, and advanced signal processing algorithms that combat the challenges of signal degradation and environmental artifacts inherent in mobile use [2]. This section explores the core technologies enabling this transition and the systemic requirements for effective real-world BCI deployment.
Core Technologies and Signal Acquisition Methods
The performance of wireless portable BCIs hinges on the selection of appropriate signal acquisition technologies. The table below summarizes the key technical attributes of prominent non-invasive methods.
Table 1: Comparison of Non-Invasive BCI Signal Acquisition Technologies
| Technology | Spatial Resolution | Temporal Resolution | Portability & Cost | Primary Strengths | Primary Limitations |
|---|---|---|---|---|---|
| Electroencephalography (EEG) | Low (cm) | High (ms) | High portability, relatively low cost [2] | High temporal resolution, cost-effective, established for BCI [2] [8] | Signal degradation from skull, sensitive to motion artifacts and external noise [2] [3] |
| Functional Near-Infrared Spectroscopy (fNIRS) | Medium (cm) | Low (seconds) | Growing portability, moderate cost | Better motion artifact resistance than EEG, measures hemodynamic response | Lower temporal resolution, limited penetration depth |
| Wearable Magnetoencephalography (MEG) | High (mm) | High (ms) | Emerging portability, currently high cost [8] | High spatiotemporal resolution | Typically requires shielded environments; new wearable versions are emerging [8] |
EEG remains the most widely used platform for portable non-invasive BCIs due to its excellent temporal resolution, relative affordability, and established form factors for head-worn devices [2]. Its primary challenge for real-world deployment is vulnerability to motion artifacts and electromagnetic interference, which necessitates sophisticated hardware and software solutions for noise cancellation [2] [84]. Innovations in dry electrodes eliminate the need for conductive gels, improving user convenience and enabling longer-term use, though they often face challenges with higher contact impedance compared to traditional wet electrodes [8]. Hybrid systems, such as those combining EEG with near-infrared spectroscopy (NIRS), are gaining traction for providing complementary information and improving classification accuracy for complex tasks like motor imagery [84].
System Architecture and Workflow of a Portable BCI
A portable BCI system follows a structured pipeline from signal acquisition to the execution of commands. The entire process must be optimized for low latency and power efficiency to function effectively in real-world conditions.
The workflow illustrates the three critical stages of a portable BCI system. The Signal Acquisition stage is facilitated by wireless headsets employing dry electrodes for usability [8]. The Signal Processing stage employs machine learning (ML) algorithms for feature extraction and classification; modern approaches utilize deep learning and transfer learning to improve performance across users and sessions [3]. The final Device Control & Feedback stage creates a closed-loop system where user feedback is essential for adaptation and learning, enabling control of complex devices such as robotic arms and virtual reality (VR) environments [3] [7].
Experimental Protocols and Methodologies
Robust experimental protocols are essential for validating the performance of wireless BCI systems. The following table outlines key components and methodologies used in BCI research, particularly for applications like controlling assistive devices or neurofeedback training.
Table 2: Essential Research Reagents and Materials for BCI Experimentation
| Item Category | Specific Examples | Function & Application in BCI Research |
|---|---|---|
| Recording Hardware | Wireless EEG headsets with dry electrodes; Hybrid EEG-fNIRS systems [84] | Acquire neural signals with minimal setup time and high user comfort for real-world deployment [8] [84] |
| Software & Algorithms | Open-source BCI toolboxes (e.g., BCILAB, OpenBMI); Deep learning models (CNNs, RNNs) [3] | Signal processing, artifact removal, feature extraction, and classification of brain states in real-time or offline analysis [3] |
| Paradigm Stimulation | Motor Imagery (MI) tasks; P300 evoked potentials; Steady-State Visual Evoked Potentials (SSVEP) | Elicit specific, classifiable brain patterns for BCI control [3] [84] |
| External Control Devices | Robotic arms; Wheelchairs; Virtual Reality (VR) interfaces [3] [7] | Serve as actuating endpoints for BCI commands, enabling restoration of function or immersive training environments [3] |
A representative protocol for a Motor Imagery (MI)-based BCI study involves several key phases. First, participants don a wireless EEG system, and a calibration session is conducted where users imagine specific movements (e.g., left hand or right hand movement). During this, data is recorded to train a user-specific model. Next, in the online control phase, the system decodes the user's real-time intent, translating it into commands for an external device like a robotic arm or a cursor on a screen [3]. Critical to the success of this protocol is the implementation of artifact removal techniques to handle noise from blinks, eye movements, and muscle activity, which is more prevalent in mobile settings [84]. The system provides continuous visual or haptic feedback to the user, creating a closed-loop interface that facilitates learning and improves performance over time [3].
Key Challenges and Future Directions
Despite significant progress, wireless portable BCIs face several hurdles for widespread real-world deployment. Signal quality remains a primary concern, as motion artifacts and environmental noise can severely degrade performance [2]. Solving the "ground truth" problem in artifact correction is an active area of research [84]. Furthermore, user variability in the ability to control BCIs—a phenomenon known as "BCI inefficiency"—requires more adaptive algorithms that can personalize to the user's neural patterns [84].
Future development is focused on several key areas. Improved hardware, including more robust dry electrodes and low-power electronics, will enhance comfort and battery life [8]. Advanced ML algorithms, particularly deep learning and transfer learning, are being developed to create more robust and adaptive decoders that require less user-specific training [3]. The integration of BCIs with other bio-signals, such as electromyography (EMG) and eye-tracking, in hybrid systems provides a more comprehensive intent-recognition framework [8]. Finally, the fusion of BCIs with consumer augmented and virtual reality (AR/VR) headsets presents a significant near-term opportunity for mainstream adoption, moving beyond medical applications into communication, entertainment, and cognitive enhancement [2] [8]. The market forecast for BCI technologies reflects this growth, with projections indicating the overall market will surpass $1.6 billion by 2045 [8].
Addressing Technical Limitations and Enhancing BCI Performance
The skull represents the most significant biological barrier to high-fidelity brain-computer interfacing. Its primary function—to protect the delicate neural tissue within—directly contradicts the requirements of non-invasive neural recording, which depends on the clear transmission of electrical signals. This chapter dissects the biophysical nature of the skull barrier, quantifying its impact on signal quality and exploring the methodological and technological innovations designed to overcome it. As non-invasive BCIs transition from laboratory curiosities to tools with real-world clinical and consumer applications, a rigorous understanding of these challenges is paramount for researchers and developers aiming to push the boundaries of what is possible without surgical intervention [2] [3].
The Biophysics of Signal Attenuation
At its core, the challenge of the skull barrier is one of volume conduction. Electrical potentials generated by synchronized neuronal activity must travel from their cortical sources through several layers of tissue—the cerebrospinal fluid (CSF), the dura and arachnoid mater, the skull itself, and the scalp—before they can be measured at the surface. Each of these tissues has distinct electrical properties that degrade the signal.
The skull is particularly problematic due to its low electrical conductivity and high resistivity compared to both neural tissue and scalp. The precise conductivity ratio is critical for accurate head modeling. While traditional three-sphere head models (brain, skull, scalp) often use a brain-to-skull conductivity ratio of 1:1/80, more recent in vivo measurements suggest this ratio should be closer to 1:1/15 [85]. This indicates that the skull's attenuation effect, while still substantial, may be less severe than previously modeled in earlier simulations. The thickness of the skull is also not uniform; it can vary by a factor of six across different areas of the same skull, with the temporal region being significantly thinner than the frontal or parietal bones [85]. This natural variation directly impacts signal fidelity, making some brain areas inherently easier to monitor non-invasively than others.
Table 1: Electrical Properties and Impact of Head Tissues on Signal Quality
| Tissue Layer | Typical Conductivity (S/m) | Impact on Neural Signals |
|---|---|---|
| Brain / CSF | ~0.33 (High) | Minimal signal attenuation; high conductivity. |
| Skull | ~0.0042 - 0.022 (Very Low) | Major source of signal attenuation and spatial blurring. |
| Scalp | ~0.33 (High) | Minimal attenuation, but introduces muscular and other biological artifacts. |
The combined effect of these tissues is a significant degradation of the original neural signal. Scalp-recorded electroencephalography (EEG) signals experience substantial attenuation and spatial blurring. The electrical potentials are smeared as they pass through the resistive skull, reducing the effective spatial resolution of non-invasive EEG to the order of centimeters, compared to the millimeter or sub-millimeter resolution afforded by invasive intracortical electrodes [66] [3]. Furthermore, the signal-to-noise ratio (SNR) is drastically reduced, as the tiny microvolt-level signals of interest must be distinguished from noise amplified by the same high-gain amplifiers.
Figure 1: Signal Degradation Pathway from Cortex to Scalp. The skull barrier is the primary site of signal attenuation and spatial blurring.
Quantitative Analysis of the Skull's Impact
Research using sophisticated computational models has precisely quantified the skull's effect on scalp potentials. A key finding is that the drop in electrical potential within the bone is directly dependent on its thickness [85]. One simulation study using a three-dimensional resistor mesh model of the head found that the introduction of a hole in the skull, bypassing this resistive layer, can increase the maximum potential value measured at the scalp by a factor of 11.5 [85]. This dramatic result underscores the sheer magnitude of the skull's impedance.
Furthermore, failing to account for the skull's inherent anisotropy (directional dependence of conductivity) and inhomogeneity (variations in thickness and conductivity) can lead to source localization errors of approximately 1 cm in EEG inverse modeling [85]. This is a critical consideration for BCIs that aim to decode activity from specific cortical regions, as misattributing a signal's origin can severely compromise decoding accuracy and system performance.
Table 2: Impact of Skull Properties on EEG Signal Fidelity
| Skull Property | Quantitative Impact | Consequence for BCI |
|---|---|---|
| Low Conductivity | Brain-to-skull conductivity ratio of ~1:1/15 to 1:1/80 [85]. | Severe attenuation of signal amplitude. |
| Variable Thickness | Varies by a factor of 3-6 across the skull [85]. | Inconsistent signal quality across different brain regions. |
| Presence of Holes | Can increase scalp potential by a factor of 11.5 [85]. | Creates localized "hot spots" of high-fidelity signal. |
| Anisotropy & Inhomogeneity | Can induce source localization errors of ~1 cm [85]. | Reduces accuracy of decoding algorithms. |
Methodologies for Modeling and Experimental Investigation
Investigating the skull barrier requires a combination of computational modeling and empirical validation.
4.1 Computational Head Modeling Advanced numerical techniques are used to solve the "forward problem" of predicting scalp potentials from known neural sources.
- Finite Element Method (FEM) and Finite Difference Method (FDM): These methods split the head volume into thousands or millions of small elements (voxels), each assigned specific electrical properties derived from anatomical MRI scans. This allows for highly realistic modeling of complex tissue geometries, including anisotropic skull conductivity and local thickness variations [85].
- Resistor Mesh Models: An alternative approach uses a 3D mesh of resistors to model the head, where the value of each resistor represents the local geometric and electrical properties. This method is particularly adept at easily introducing and studying local modifications, such as skull holes or regions of varying thickness [85].
The workflow for such investigations typically involves:
- Image Segmentation: Processing high-resolution MRI scans to identify and label different tissues (gray matter, white matter, CSF, skull, scalp).
- Mesh Generation: Creating a 3D computational mesh from the segmented volumes.
- Assignment of Electrical Properties: Applying known or estimated conductivity values to each tissue type in the mesh.
- Forward Simulation: Calculating the scalp potentials that would result from a simulated dipole source in the cortex.
- Inverse Solution (Optional): Using the model to estimate the location of a neural source based on a given scalp potential map, thereby quantifying localization errors.
Figure 2: Workflow for Computational Modeling of Skull Barrier Effects.
4.2 Experimental Reagents and Materials The following toolkit is essential for research in this domain: Table 3: Research Reagent Solutions for Investigating the Skull Barrier
| Research Tool | Function & Explanation |
|---|---|
| High-Density EEG Systems (128-256 channels) | Increases spatial sampling to improve source localization accuracy and mitigate spatial blurring caused by the skull [85] [86]. |
| Anatomical MRI Data | Provides the essential structural dataset for building patient-specific realistic head models, including precise skull geometry and thickness mapping. |
| Tissue Conductivity Phantoms | Gel- or saline-based models with known electrical properties used to validate and calibrate computational models against empirical measurements. |
| Stimulus Presentation Software | Precisely controls visual/auditory stimuli for Evoked Potential studies (e.g., P300), generating time-locked neural responses used to validate model predictions [87]. |
Emerging Strategies and Technological Solutions
The field is responding to the skull barrier challenge with innovations in signal processing, sensor technology, and alternative modalities.
5.1 Advanced Signal Processing and Machine Learning Modern deep learning algorithms are proving highly effective at denoising EEG signals and decoding user intent despite low SNR. These models can learn to isolate neural patterns of interest from the background noise, including artifacts and the smearing effects of volume conduction [3]. Transfer learning techniques are also being developed to adapt models to new users more quickly, reducing the lengthy calibration times traditionally associated with non-invasive BCIs [3].
5.2 Hardware and Sensor Innovations Improvements in electrode technology are focusing on enhancing the quality of the signal at the point of acquisition.
- Dry Electrodes: These eliminate the need for conductive gel, enabling quicker setup and improving user comfort for long-term wearables. They are a key development for consumer BCI applications [8].
- High-Density Arrays: Using 64, 128, or more electrodes provides denser spatial sampling, which, when combined with advanced source localization algorithms, can help "de-blur" the scalp signals and provide a more accurate reconstruction of underlying brain activity [85].
5.3 Hybrid and Novel Modalities Researchers are exploring other non-invasive modalities that are less affected by the skull or that provide complementary information.
- Functional Near-Infrared Spectroscopy (fNIRS): This measures hemodynamic activity (blood oxygenation) in response to neural firing. While it has a lower temporal resolution than EEG, light in the near-infrared spectrum penetrates the skull more easily, and the signal is less susceptible to electrical interference [8].
- Magnetoencephalography (MEG): MEG measures the magnetic fields induced by neural electrical activity. Since magnetic fields are less distorted by the skull and scalp than electrical potentials, MEG offers superior spatial resolution. The traditional barrier has been the need for bulky, cryogenically cooled sensors in a shielded room, but the emergence of wearable, optically-pumped magnetometer (OPM)-based MEG systems may eventually make this a more viable option for BCI [8].
- Endovascular (Stentrode) and ECoG Approaches: While minimally invasive, technologies like the Stentrode—an electrode array implanted within a blood vessel—represent a compromise. They avoid penetrating brain tissue but record from inside the skull, thereby bypassing the signal attenuation of the bone entirely and offering a higher-fidelity signal than purely non-invasive methods [62] [3].
The skull barrier remains a fundamental, biophysically-grounded challenge that defines the performance limits of non-invasive BCIs. It imposes a hard constraint on the spatial resolution and signal-to-noise ratio achievable with current technologies. However, through quantitative modeling, we can precisely characterize its effects, and through a multi-pronged strategy encompassing advanced computational algorithms, improved hardware, and innovative signal acquisition methods, the field is making steady progress in mitigating these limitations. The future of non-invasive BCI lies not in a single silver bullet, but in the intelligent integration of these diverse approaches to extract the richest possible information from the attenuated signals that successfully traverse the protective bone of the skull.
Advanced Signal Processing for Artifact Removal and Noise Reduction
Electroencephalography (EEG), a cornerstone of non-invasive Brain-Computer Interface (BCI) technology, is plagued by a fundamental challenge: the recorded electrical activity is invariably contaminated by artifacts and noise, which severely obstructs the analysis of the underlying neural signals [88]. These unwanted signals can originate from a myriad of sources, both physiological and environmental, leading to a low signal-to-noise ratio (SNR) that complicates the interpretation of brain activity and can bias clinical diagnosis [88] [43]. For non-invasive BCIs to achieve reliable performance in both clinical applications, such as neurorehabilitation for stroke and spinal cord injury patients, and emerging consumer domains, advanced signal processing techniques for effective artifact removal are not merely beneficial—they are essential [89] [10].
The pursuit of robust artifact removal methodologies is a critical enabler for the broader thesis on non-invasive BCI technologies. It directly impacts the feasibility, accuracy, and real-world applicability of these systems, forming the foundation upon which reliable BCI operation is built.
Characterization and Typology of EEG Artifacts
A comprehensive understanding of artifact types is a prerequisite for selecting and developing effective removal strategies. These artifacts are broadly categorized into extrinsic and intrinsic types [88].
- Extrinsic Artifacts: These originate from external sources and include instrumentation artifacts (e.g., faulty electrodes, high electrode impedance, and cable movement) and environmental artifacts (e.g., powerline interference at 50/60 Hz). While often preventable through proper experimental procedure and simple filtering, they remain a common practical challenge [88].
- Intrinsic (Physiological) Artifacts: These arise from the subject's own body and represent the most significant challenge for artifact removal due to their complex nature and spectral overlap with neural signals of interest. The major types are:
- Ocular Artifacts: Generated by eye movements and blinks, these artifacts have a large amplitude and propagate over the scalp. Their frequency is similar to EEG signals, making them particularly difficult to remove without distorting neural data [88].
- Muscle Artifacts (EMG): Caused by the contraction of various muscle groups (e.g., jaw clenching, swallowing), these artifacts have a broad frequency distribution (0 Hz to >200 Hz) and can mask underlying brain activity. Their removal is notoriously challenging [88].
- Cardiac Artifacts (ECG): These artifacts, which include pulse and electrical activity from the heart, can be introduced when electrodes are placed near blood vessels. While the characteristic pattern of ECG can sometimes facilitate its removal, its regularity can also be mistaken for neural phenomena [88].
Table 1: Major Physiological Artifacts in EEG Recordings
| Artifact Type | Source | Frequency Characteristics | Primary Challenge for Removal |
|---|---|---|---|
| Ocular (EOG) | Eye movements & blinks | Similar to EEG bands, high amplitude | Spectral overlap and large amplitude obscures neural signals [88]. |
| Muscle (EMG) | Head, neck, jaw muscle activity | Broadband (0 - >200 Hz) | Widespread spectral contamination that overlaps with key EEG rhythms [88]. |
| Cardiac (ECG) | Heart electrical activity & pulse | ~1.2 Hz (pulse), characteristic pattern | Regular pattern can be misinterpreted as neural activity; requires reference [88]. |
Signal Processing Techniques for Artifact Removal
A wide array of signal processing techniques has been developed to tackle the problem of artifacts, ranging from classical statistical methods to modern deep-learning approaches.
Conventional and Classical Methods
Classical methods form the historical foundation of artifact removal and are still in use today, often serving as a benchmark for newer algorithms.
- Regression Methods: This is a traditional technique that operates under the assumption that each EEG channel is a cumulative sum of pure neural data and a scaled version of the artifact [88]. It requires exogenous reference channels (e.g., EOG, ECG) to estimate and subsequently subtract the artifactual component from the EEG signal. A significant limitation is the problem of bidirectional interference, where the reference channel itself may be contaminated by cerebral activity, leading to the unwanted removal of neural signals [88].
- Blind Source Separation (BSS): BSS methods, particularly Independent Component Analysis (ICA), are among the most commonly used algorithms for artifact removal [88]. ICA works by decomposing multi-channel EEG data into statistically independent components. Artifactual components (e.g., those linked to eye blinks or muscle activity) can be visually or automatically identified and removed before the signal is reconstructed. Its effectiveness relies on having a sufficient number of EEG channels and the statistical independence of sources [88].
- Wavelet Transform and Empirical Mode Decomposition (EMD): These are signal decomposition techniques that break down the EEG signal into different frequency sub-bands or intrinsic mode functions, respectively [88]. Artifacts are removed by thresholding or discarding the components associated with noise, after which the signal is reconstructed. These methods are particularly useful for dealing with non-stationary signals like EEG [88].
AI and Deep Learning-Based Approaches
The limitations of conventional methods have spurred the adoption of deep learning, which offers a data-driven approach capable of learning complex, non-linear relationships between noisy and clean EEG signals.
- Generative Adversarial Networks (GANs): GANs have emerged as a powerful framework for artifact removal. A typical GAN for this task consists of a Generator that takes noisy EEG as input and attempts to produce a clean version, and a Discriminator that learns to distinguish between the generator's output and ground-truth clean EEG [90]. This adversarial training process forces the generator to produce increasingly realistic, artifact-free signals.
- Hybrid Deep Learning Models: Recent research focuses on enhancing GANs by integrating networks that can capture temporal dependencies. For instance, the AnEEG model incorporates Long Short-Term Memory (LSTM) layers into a GAN architecture [90]. LSTMs are a type of recurrent neural network exceptionally well-suited for processing time-series data like EEG, as they can learn long-range contextual information and temporal dynamics critical for accurate artifact separation [90]. Other advanced architectures, such as GCTNet, combine GANs with Convolutional Neural Networks (CNNs) and Transformer networks to capture both spatial and global temporal dependencies in the EEG data [90].
Table 2: Comparison of Key Artifact Removal Techniques
| Method | Underlying Principle | Key Advantages | Key Limitations |
|---|---|---|---|
| Regression | Linear subtraction of artifact estimated from reference channels. | Simple, computationally efficient. | Requires reference channels; prone to over-correction and removing neural signals [88]. |
| ICA | Separates signals into statistically independent components. | Does not require reference channels; effective for ocular and some muscle artifacts [88]. | Requires multi-channel EEG; manual component selection can be subjective; struggles with source dependencies. |
| Wavelet/EMD | Decomposes signal into time-frequency components for thresholding. | Effective for non-stationary signals and transient artifacts. | Choosing optimal thresholds and base functions can be complex; can introduce reconstruction artifacts. |
| Deep Learning (e.g., GAN-LSTM) | Learns a non-linear mapping from noisy to clean EEG using trained models. | Data-driven; can model complex noise patterns; no need for manual intervention post-training. | Requires large, labeled datasets for training; computationally intensive; risk of overfitting [90]. |
Experimental Protocols and Methodological Workflows
Implementing advanced artifact removal requires a structured experimental pipeline. Below is a detailed protocol for a typical deep learning-based approach, as exemplified by the AnEEG model [90].
Protocol: GAN-LSTM for EEG Artifact Removal
Objective: To remove ocular and muscle artifacts from raw multichannel EEG data using a Generative Adversarial Network integrated with Long Short-Term Memory (LSTM) layers.
Materials and Dataset:
- EEG Data: The protocol requires a dataset containing paired recordings of artifact-contaminated EEG and corresponding ground-truth clean EEG. Publicly available datasets like EEG DenoiseNet or the MIT-BIH Arrhythmia Dataset (for semi-simulated data) can be used [90].
- Computing Environment: A workstation with a powerful GPU (e.g., NVIDIA RTX series) is recommended to handle the computational load of training deep learning models.
- Software Stack: Python with deep learning libraries such as TensorFlow or PyTorch, along with standard scientific computing packages (NumPy, SciPy).
Experimental Workflow:
Data Preprocessing:
- Bandpass Filtering: Apply a bandpass filter (e.g., 1-45 Hz) to remove slow drifts and high-frequency noise outside the range of interest.
- Re-referencing: Re-reference the EEG data to a common average reference.
- Segmentation: Segment the continuous EEG data into epochs of a fixed length (e.g., 2-second segments).
- Normalization: Normalize the data from each channel to have zero mean and unit variance to stabilize the training process.
Model Architecture Definition (GAN-LSTM):
- Generator Network: Design a generator that takes a noisy EEG epoch as input. The architecture should include:
- Input layer matching the dimensions of the EEG epoch (channels × time points).
- Multiple LSTM layers (e.g., two layers with 50 units each) to capture temporal dependencies.
- A fully connected output layer with a linear activation function to reconstruct the clean EEG epoch [90].
- Discriminator Network: Design a discriminator that classifies inputs as "real" (clean EEG) or "fake" (generated EEG). The architecture could be a 1D Convolutional Neural Network (CNN) or a dense network, ending with a sigmoid activation function for binary classification [90].
- Generator Network: Design a generator that takes a noisy EEG epoch as input. The architecture should include:
Model Training:
- Loss Functions: Implement a composite loss function for the generator, typically a weighted sum of:
- Adversarial Loss: The binary cross-entropy loss from the discriminator, encouraging the generator to "fool" the discriminator.
- Content Loss: The Mean Squared Error (MSE) between the generated EEG and the ground-truth clean EEG, ensuring the output is structurally similar to the target [90].
- Training Loop: Train the model in an alternating fashion:
- Train the Discriminator with a batch of real clean EEG (labeled "1") and a batch of generated EEG from the generator (labeled "0").
- Train the Generator to produce outputs that the Discriminator will classify as "real".
- Loss Functions: Implement a composite loss function for the generator, typically a weighted sum of:
Validation and Quantitative Analysis:
- Use a held-out test set to evaluate the model's performance.
- Calculate standard quantitative metrics to confirm effectiveness [90]:
- Normalized Mean Square Error (NMSE) and Root Mean Square Error (RMSE): Lower values indicate better agreement with the original clean signal.
- Correlation Coefficient (CC): Higher values indicate a stronger linear relationship with the ground truth.
- Signal-to-Noise Ratio (SNR) and Signal-to-Artifact Ratio (SAR): Higher values indicate superior artifact removal and signal quality preservation.
The following workflow diagram illustrates the core closed-loop process of a BCI system, highlighting the central role of the signal processing and artifact removal stage.
Diagram 1: BCI Closed-Loop System with Artifact Removal. This workflow shows the essential stages of a non-invasive BCI, emphasizing the critical preprocessing and artifact removal step that enables reliable feature extraction and device control.
The Scientist's Toolkit: Research Reagent Solutions
The following table details key hardware, software, and algorithmic "reagents" essential for conducting research in advanced EEG artifact removal.
Table 3: Essential Research Reagents for Advanced EEG Artifact Removal
| Category | Item/Technique | Function & Application |
|---|---|---|
| Hardware & Data | High-density EEG Systems (e.g., 64+ channels) | Provides spatial resolution necessary for source separation techniques like ICA. |
| Dry Electrode Headsets | Enables more convenient, long-term monitoring; a focus of innovation for consumer BCI [91] [8]. | |
| Public EEG Datasets (e.g., EEG DenoiseNet, PhysioNet) | Provides standardized, labeled data for training and benchmarking machine learning models [90]. | |
| Algorithms & Models | Independent Component Analysis (ICA) | A classic BSS method for isolating and removing artifactual components from multi-channel data [88]. |
| Generative Adversarial Network (GAN) | A deep learning framework for learning to generate clean EEG from noisy inputs in a data-driven manner [90]. | |
| Long Short-Term Memory (LSTM) Network | A type of RNN added to models like AnEEG to capture temporal dependencies in EEG time-series data [90]. | |
| Software & Libraries | TensorFlow / PyTorch | Open-source libraries for building, training, and deploying deep learning models. |
| MNE-Python | A comprehensive open-source Python package for exploring, visualizing, and analyzing human neurophysiological data. | |
| EEGLAB / FieldTrip (MATLAB) | Established MATLAB toolboxes offering extensive functionalities for EEG processing, including ICA. |
The evolution of signal processing from conventional regression and ICA to sophisticated deep learning models represents a paradigm shift in addressing the perennial challenge of artifacts in non-invasive BCI. While classical methods remain valuable, AI-driven approaches like GAN-LSTM hybrids demonstrate superior capability in handling complex, non-linear artifacts while preserving the integrity of neural information [90]. This progress is critical for unlocking the full potential of non-invasive BCIs, enhancing their reliability in clinical applications such as motor rehabilitation after stroke and spinal cord injury, and paving the way for broader adoption in assistive technology and beyond [89] [10]. As the field advances, the integration of these advanced signal processing techniques will continue to be a cornerstone of the ongoing review and comparison of non-invasive BCI technologies, pushing the boundaries of what is possible in human-computer interaction.
Adaptive Calibration and Personalization Techniques for Individual Variability
In non-invasive Brain-Computer Interface (BCI) technology, the "one-size-fits-all" paradigm is a fundamental limitation. Individual variability in neuroanatomy, cognitive strategies, and signal-to-noise characteristics necessitates a shift toward adaptive calibration and personalization techniques. These methods are crucial for developing robust BCIs that can function reliably across diverse user populations in both clinical and research settings. The core challenge lies in creating systems that can dynamically adjust to a user's unique neural signature, thereby improving classification accuracy, reducing calibration time, and enhancing overall usability [41].
The pursuit of personalization is driven by the significant performance variations observed across users, a phenomenon often termed "BCI illiteracy" or "inefficiency." For individuals with severe motor impairments, this problem is compounded by "negative plasticity"—maladaptive neural changes that degrade the attentional and cognitive processes exploited by BCI systems [41]. Consequently, adaptive calibration is not merely a convenience but a prerequisite for viable assistive technologies. This technical guide examines the core algorithms, experimental protocols, and implementation frameworks that address individual variability in non-invasive BCIs, providing researchers with methodologies to enhance system robustness and accessibility.
Technical Approaches to Personalization
Machine Learning and Adaptive Algorithms
Modern personalization techniques leverage advanced machine learning to create user-specific models that evolve over time. The following table summarizes key algorithmic approaches and their applications:
Table 1: Machine Learning Techniques for BCI Personalization
| Technique | Mechanism | Application in BCI | Reported Efficacy |
|---|---|---|---|
| Reinforcement Learning (RL) with Error-Related Potentials (ErrPs) | Uses ErrP signals—generated when a user perceives a system error—as intrinsic feedback to reinforce or adjust the decoder's policy in real-time [41]. | Continuous adaptation of classifier parameters during online BCI control. | Enables long-term calibration without explicit user training sessions. |
| Transfer Learning & Domain Adaptation | Maps data from existing users (source domain) to fit a new user (target domain) with minimal calibration. Frameworks like SSVEP-DAN (Domain Adaptation Network) align feature distributions [41]. | Rapid setup for new users by leveraging pre-existing datasets from other subjects. | Reduces calibration time; SSVEP-DAN maintains high ITR with new users. |
| Deep Learning & Self-Attention Networks | Models complex, non-linear EEG patterns. Hybrid CNN-Attention networks (e.g., CNNATT) capture temporal and feature dependencies for robust decoding [41]. |
Continuous variable decoding (e.g., hand force) and cognitive state monitoring. | Achieves high decoding accuracy (e.g., ~65% for tactile classification) [41]. |
| Ensemble Methods | Combines multiple classifiers (e.g., LSTM-CNN-Random Forest) to improve generalization and stability against variable signal quality [41]. | Complex control tasks, such as prosthetic arm manipulation with the BRAVE system. | Reported accuracies as high as 96% for intent decoding [41]. |
| Online Recursive Classifiers | Models like MarkovType use a Partially Observable Markov Decision Process (POMDP) to recursively update belief states, balancing speed and accuracy [41]. |
Discrete BCIs, such as rapid serial visual presentation (RSVP) typing systems. | High symbol recognition accuracy (>85%) with optimized information transfer rate [41]. |
Signal Processing and Feature Extraction
The personalization pipeline begins with signal processing tailored to individual electrophysiological characteristics. Spatial filtering optimization, such as user-specific Common Spatial Patterns (CSP), is a critical step. The CSP algorithm finds spatial filters w that maximize the variance ratio between two classes (e.g., left-hand vs. right-hand motor imagery):
Here, C1 and C2 are the covariance matrices of the respective classes [41]. Adaptive versions of CSP update these filters based on incoming user data.
Furthermore, adaptive filtering techniques like Recursive Least Squares (RLS) are employed for robust denoising. These filters continuously adjust their parameters to suppress artifacts (e.g., EMG, EOG) specific to a user's typical noise profile [41]. This results in a cleaner signal from which personalized features—such as logarithmic band-power variances from user-specific frequency bands or wavelet coefficients—can be extracted for more reliable classification.
Experimental Protocols and Methodologies
Core Calibration Workflow
A standardized yet flexible protocol is essential for evaluating adaptive calibration techniques. The following diagram outlines a generalized experimental workflow for collecting user-specific data and implementing personalized models.
Detailed Protocol Description
Participant Recruitment and Screening: Recruit subjects representing target variability (e.g., age, clinical condition). For spinal cord injury (SCI) patients, document injury level (e.g., cervical, thoracic) and severity using the American Spinal Injury Association (ASIA) Impairment Scale (AIS A-E) [10]. Ethical approval and informed consent are mandatory.
Initial Signal Acquisition and Paradigm Explanation:
- Equipment Setup: Fit a multi-channel EEG cap (e.g., 64-channel scientific-grade system or a 14-channel headset like Emotiv EPOC+). Apply electrode gel for low impedance (< 10 kΩ). Configure auxiliary data streams for fNIRS or MEG if using a hybrid system [41].
- Task Instruction: Explain the BCI paradigm (e.g., motor imagery, P300 speller) using standardized instructions and demonstration.
Baseline Calibration Session:
- Protocol: Conduct a structured session where the user performs repetitive, cue-based trials. For motor imagery, this may involve 40-50 trials per class (e.g., imagining left-hand vs. right-hand movement), each trial lasting 4-8 seconds with inter-trial rest periods [41].
- Data Recording: Record raw EEG signals (e.g., 250 Hz sampling rate, 0.5-60 Hz bandpass filter). Mark trial onsets and event triggers precisely.
Feature Extraction and Initial Model Training:
- Preprocessing: Apply user-specific filters: a notch filter (50/60 Hz) and a bandpass filter tailored to the individual's prominent rhythm range (e.g., 8-30 Hz for motor imagery). Perform artifact removal using Independent Component Analysis (ICA), with components flagged for rejection based on a user-specific template [41].
- Modeling: Extract user-discriminative features (e.g., CSP patterns, power spectral density). Train an initial classifier (e.g., Linear Discriminant Analysis or Support Vector Machine) on this user's calibration data.
Online Adaptive Session:
- Procedure: The user operates the BCI in a closed-loop setting with real-time feedback (e.g., moving a cursor, controlling a wheelchair in a digital twin simulation) [41].
- Adaptation Mechanism: The system incorporates feedback, such as Error-Related Potentials (ErrPs), to trigger model updates. For example, an ErrP detected after an incorrect cursor movement is used as a negative reinforcement signal for the RL agent, which then adjusts the decoder's policy [41].
Model Update and Performance Evaluation:
- Quantitative Metrics: Calculate performance metrics after each block or session:
- Classification Accuracy: Percentage of correct commands.
- Information Transfer Rate (ITR): Bits per minute, factoring in accuracy and speed.
- Task Completion Time: For control tasks (e.g., pick-and-place with a robotic arm) [92].
- Update Frequency: Decide on an update strategy: incremental update after every trial, batch update after a session, or triggered update upon ErrP detection.
- Quantitative Metrics: Calculate performance metrics after each block or session:
Long-term Stability Assessment: Conduct follow-up sessions over days or weeks to track performance. Retrain or fine-tune the model as needed to compensate for non-stationarities in the neural signals (e.g., due to learning, fatigue, or changes in electrode impedance) [41].
The Scientist's Toolkit: Research Reagent Solutions
Implementing adaptive BCI systems requires a suite of hardware, software, and methodological "reagents." The following table details essential components.
Table 2: Essential Research Reagents for Adaptive BCI Experiments
| Item Name / Category | Specification / Example | Primary Function in Personalization |
|---|---|---|
| High-Density EEG Systems | 64+ channel systems (e.g., from BrainVision, g.tec). Dry electrode caps (e.g., from Wearable Sensing) [41]. | Captures detailed spatial patterns of brain activity. Dry electrodes improve usability for frequent, long-term calibration sessions. |
| Hybrid BCI Modalities | Combined EEG-fNIRS systems (e.g., CNNATT framework) [41]. |
Provides complementary neural data (electrical + hemodynamic), improving decoding robustness and creating a richer user profile for adaptation. |
| Standardized Electrode Gel | SignaGel (Parker Laboratories) or similar. | Ensures stable, low-impedance electrical contact, which is critical for obtaining clean signals necessary for building accurate user models. |
| BCI Software Platforms | OpenBCI, BCILAB, or custom Python/MATLAB toolboxes with real-time processing capabilities. | Provides the computational environment for implementing and testing adaptive filtering, feature extraction, and machine learning algorithms. |
| Calibration Paradigm Software | Custom scripts for P300 speller, motor imagery cues (e.g., using Psychtoolbox or PsychoPy). | Presents standardized, yet customizable, tasks to elicit user-specific neural responses for the initial calibration and subsequent model updates. |
| Error-Related Potential (ErrP) Detector | A trained classifier (e.g., SVM) within the real-time processing pipeline that identifies characteristic ErrP waveforms [41]. | Provides an implicit feedback signal for unsupervised adaptive algorithms, enabling continuous, user-driven calibration. |
| Transcranial Alternating Current Stimulation (tACS) | Non-invasive neurostimulation device (e.g., from Neuroelectrics) [93]. | Potential to modulate brain rhythms (e.g., enhance alpha waves) to create a more consistent neural state for calibration, though this is an emerging technique. |
System Architecture and Implementation
Conceptual Framework for an Adaptive BCI
A fully adaptive BCI system integrates the components and protocols described into a cohesive architecture. The following diagram illustrates the information flow and decision logic within such a personalized system.
Quantitative Outcomes and Efficacy
The ultimate validation of any personalization technique lies in its measurable impact on BCI performance. A 2025 meta-analysis of non-invasive BCI interventions for Spinal Cord Injury (SCI) patients provides compelling quantitative evidence. The analysis, which included 9 studies (4 RCTs and 5 self-controlled trials) with 109 patients, demonstrated that personalized BCI interventions had a statistically significant positive impact on core functional domains compared to control groups [10].
Table 3: Quantitative Outcomes of Personalized BCI Interventions from a 2025 Meta-Analysis
| Functional Domain | Standardized Mean Difference (SMD) | 95% Confidence Interval | P-value | Evidence Grade |
|---|---|---|---|---|
| Motor Function | 0.72 | [0.35, 1.09] | < 0.01 | Medium |
| Sensory Function | 0.95 | [0.43, 1.48] | < 0.01 | Medium |
| Activities of Daily Living (ADL) | 0.85 | [0.46, 1.24] | < 0.01 | Low |
Source: Adapted from [10]. SMD values indicate the magnitude of improvement, where 0.8 is considered a large effect.
Furthermore, the meta-analysis revealed a critical modifying factor: the stage of the injury. Subgroup analyses showed that BCI interventions initiated during the subacute stage of SCI produced statistically stronger effects on motor function, sensory function, and ADL compared to interventions for patients in the slow chronic stage [10]. This underscores the importance of tailoring not only the algorithm but also the therapeutic application timeline to individual patient characteristics.
Adaptive calibration and personalization represent the frontier of practical non-invasive BCI research. By moving beyond static decoders and embracing machine learning techniques that account for individual variability and temporal non-stationarities, the field is poised to deliver systems that are robust, accessible, and effective. The experimental protocols and technical frameworks outlined in this guide provide a roadmap for developing the next generation of personalized BCIs. Future progress hinges on the continued integration of sophisticated AI with high-quality signal acquisition, ultimately leading to technologies that seamlessly adapt to the unique and dynamic human brain.
Flexible Electrode Designs and Improved Skin-Electrode Interface
The performance of non-invasive Brain-Computer Interfaces (BCIs) is fundamentally constrained by the quality of the electrophysiological signal acquisition at the skin-electrode interface. Flexible electrodes represent a paradigm shift from traditional rigid electrodes, offering enhanced comfort, superior biocompatibility, and reduced susceptibility to motion artifacts [71]. These advancements are critical for transitioning BCIs from laboratory settings to reliable, long-term use in clinical, research, and consumer environments. This technical guide examines the current state of flexible electrode designs, their material compositions, operational principles, and the experimental methodologies used to quantify their performance, providing a foundation for their role in next-generation non-invasive BCI systems.
Classification and Materials of Flexible Electrodes
Flexible electrodes for non-invasive BCIs can be categorized based on their operational principle and physical structure. The core advantage of these designs lies in their use of compliant materials that conform to the curvilinear surfaces of the head, thereby improving contact stability and signal integrity [71].
Dry Electrodes: These electrodes operate without conductive gel, prioritizing user-friendliness and portability. Their primary drawback is higher skin-contact impedance, which can degrade signal quality. Innovations focus on topological features to enhance contact. Microneedle Array Electrodes (MAEs) incorporate microscopic projections that gently penetrate the outermost layer of the skin (the stratum corneum) to achieve lower impedance and reduce motion artifacts [71]. These are often fabricated from polymers like polystyrene or SU-8 and designed to flex with the skin's surface. Other forms include comb-shaped and bristle electrodes, which use specific geometrical patterns to maintain stable contact across curved and often hairy regions of the scalp [71].
Semi-Dry Electrodes: A hybrid solution, semi-dry electrodes feature internal reservoirs that release a minimal amount of liquid electrolyte (e.g., saline) upon application to the skin. This mechanism bridges the gap between the high signal quality of wet electrodes and the convenience of dry electrodes [71]. Common designs utilize micro-seepage technology, employing materials like polyurethane (PU) sponges or superporous hydrogels (e.g., polyacrylamide/polyvinyl alcohol or PAM/PVA) to absorb and controllably release the electrolyte. A key engineering challenge is ensuring uniform pressure and consistent, reliable seepage over the long term [71].
Wet/Hydrogel Electrodes: As the traditional gold standard for signal quality, wet electrodes use a hydrogel film saturated with an electrolyte to create a stable conductive bridge between the skin and the electrode metal (typically Ag/AgCl) [71]. Recent material science innovations have led to advanced hydrogels. These include formulations integrated with carbon nanotubes and cellulose for high water absorption and mechanical strength, and elastic hydrogel-elastomer sensors that offer strong adhesion and inherent resistance to motion artifacts, making them suitable for portable BCIs [71]. Hydrogel-based claw electrodes are a specific design that effectively penetrates hair to achieve low-impedance contact with the scalp [71].
Table 1: Comparison of Non-Invasive Flexible Electrode Types
| Electrode Type | Key Materials | Interface Mechanism | Advantages | Disadvantages |
|---|---|---|---|---|
| Dry Electrodes | Conductive polymers, Polystyrene, SU-8 [71] | Direct skin contact; Microneedles penetrate stratum corneum | Portability, ease of use, no gel preparation, stable for long-term use [71] | High contact impedance, sensitive to motion, signal quality can be variable [71] |
| Semi-Dry Electrodes | PU Sponge, PAM/PVA Hydrogel [71] | Controlled release of internal electrolyte (e.g., saline) | Good signal quality, simpler setup than wet electrodes, user-friendly | Potential for uneven electrolyte release, long-term reliability requires validation [71] |
| Wet/Hydrogel Electrodes | Ag/AgCl, Hydrogels with CNT/Cellulose [71] | Hydrogel film acts as an electrolyte-soaked buffer | Excellent signal quality, low and stable impedance, established gold standard [71] | Time-consuming setup, gel can dry out causing signal drift, potential for skin irritation [71] |
Experimental Protocols for Performance Validation
Rigorous experimental validation is essential for characterizing the performance of flexible electrode designs. The following protocols outline standard methodologies for assessing key metrics.
Protocol for Electrode-Skin Impedance and Signal Quality Characterization
Objective: To quantitatively measure the electrode-skin contact impedance and the quality of the recorded electrophysiological signals under controlled conditions [94].
Materials and Setup:
- EEG Acquisition System: A clinical-grade data acquisition device, such as a NuAmps amplifier (Compumedics, Neuroscan, Inc.) [94].
- Electrode Cap: A multi-channel cap (e.g., 30-channel LT 37 cap) equipped with the test flexible electrodes [94].
- Reference Electrodes: Standard Ag/AgCl electrodes for reference (e.g., right mastoid) and ground placements [94].
- Impedance Meter: A device capable of measuring impedance at standard frequencies (e.g., 10-100 Hz).
- Subject Preparation: Participants are seated in a comfortable chair in a controlled environment.
Procedure:
- Subject Preparation: Fit the electrode cap onto the subject according to the international 10-20 system. For wet and semi-dry electrodes, apply gel or activate the electrolyte release mechanism as per design.
- Impedance Measurement: Before EEG recording, measure the impedance at each electrode. Impedance should be stabilized below a threshold, typically < 5 kΩ, to ensure quality signal acquisition [94].
- EEG Data Acquisition: Record EEG signals while the subject performs standardized paradigms (e.g., steady-state visual evoked potentials (SSVEP) or P300 tasks). Use a sampling rate of 250 Hz or higher, and apply appropriate band-pass filtering (e.g., 0.1-40 Hz for P300) [94].
- Signal Quality Analysis:
- Signal-to-Noise Ratio (SNR): Calculate the SNR by comparing the power of the target signal (e.g., P300 peak) to the power of the background noise in non-target segments.
- Task Performance: For BCI applications, calculate classification accuracy by comparing the number of correct target identifications to the total number of trials. Statistical significance can be assessed using χ² tests, where, for example, 32 hits in 50 trials (64% accuracy) may correspond to a significance level of p=0.05 [94].
Protocol for Long-Term Stability and Comfort Assessment
Objective: To evaluate the performance and user comfort of flexible electrodes over extended wearing periods.
Materials and Setup: Similar to Protocol 3.1, with the addition of subjective user feedback forms.
Procedure:
- Baseline Recording: Conduct an initial EEG recording session following the steps in Protocol 3.1.
- Extended Wear Phase: Instruct the subject to wear the cap for a prolonged period (e.g., 4-8 hours), engaging in normal, sedentary activities.
- Intermittent Testing: At regular intervals (e.g., hourly), repeat a short, standardized EEG recording (e.g., a 5-minute P300 paradigm) without adjusting the cap or electrodes.
- Data Analysis:
- Impedance Drift: Track changes in electrode-skin impedance over time.
- Signal Stability: Calculate the variation in SNR and noise floor across testing intervals.
- Artifact Presence: Quantify the power of artifacts related to motion (e.g., from head turns) or electrochemical instability.
- Subjective Feedback: After the test, subjects rate comfort, skin irritation, and overall wearability on a standardized scale (e.g., 1-10).
Performance Metrics and Material Considerations
Quantifying the performance of flexible electrodes involves multiple, interrelated metrics. Insights from chronic invasive electrode studies highlight the critical link between physical integrity and function. One study of 980 explanted intracortical microelectrodes found that despite greater observed physical degradation, electrodes made of Sputtered Iridium Oxide Film (SIROF) were twice as likely to record neural activity than traditional Platinum (Pt) electrodes, as measured by Signal-to-Noise Ratio (SNR) [95]. Furthermore, for SIROF, impedance at 1 kHz significantly correlated with all physical damage metrics, recording metrics, and stimulation performance, establishing it as a reliable indicator of in vivo degradation [95]. This underscores the importance of material choice not just for flexibility, but for electrochemical resilience.
Table 2: Key Performance Metrics for Flexible Electrode Assessment
| Performance Metric | Target Value / Ideal Characteristic | Measurement Technique |
|---|---|---|
| Skin-Electrode Impedance | Stable and < 5-10 kΩ at 10-100 Hz [94] | Impedance spectroscopy meter |
| Signal-to-Noise Ratio (SNR) | Maximized; High enough for target detection (e.g., P300) [95] | Analysis of recorded EEG during evoked potentials |
| Motion Artifact Resilience | Minimal signal deviation during subject movement | Accelerometer data correlated with EEG noise power |
| Long-Term Stability | Minimal drift in impedance and SNR over >4 hours | Repeated measures over time (Protocol 3.2) |
| Biocompatibility & Comfort | No skin irritation; high subjective comfort score | Subject feedback surveys, visual skin inspection |
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and reagents used in the development and testing of flexible electrodes for non-invasive BCIs.
Table 3: Essential Research Reagents and Materials for Flexible BCI Electrodes
| Item Name | Function/Application | Specific Examples & Notes |
|---|---|---|
| Conductive Polymers | Base material for dry and semi-dry electrodes; provides flexibility and electrical conductivity [71] | PEDOT:PSS; often combined with stretchable substrates. |
| Hydrogels | Acts as the ionic-conducting interface for wet electrodes; can be engineered for specific properties [71] | PAM/PVA for semi-dry reservoirs; Ag/AgCl-filled gels for wet electrodes; composites with CNT/cellulose for strength [71]. |
| Microneedle Templates | Fabrication of microneedle array electrodes (MAEs) to penetrate the stratum corneum [71] | Polymers like polystyrene or SU-8, shaped into comb, bristle, or pillar geometries [71]. |
| Electrolyte Solutions | Ionic bridge for semi-dry and wet electrode operation [71] | Phosphate-buffered saline (PBS) or specialized isotonic solutions for micro-seepage systems. |
| Signal Acquisition System | Hardware for recording, amplifying, and digitizing EEG signals from the electrodes [94] | Clinical-grade EEG systems (e.g., NuAmps by Compumedics) with >16-bit ADC and Bluetooth capability [94]. |
| Impedance Spectroscopy Meter | Quantifying the electrical properties of the skin-electrode interface [95] | Used to measure impedance magnitude and phase across a frequency range (e.g., 1 Hz - 1 kHz) [95]. |
The future of flexible electrodes in non-invasive BCIs is oriented toward solving remaining challenges in manufacturability, reliability, and seamless integration. Key research thrusts include developing simple, cost-effective, and scalable manufacturing methods to produce high-density electrode arrays [71]. There is also a strong focus on creating ever more reliable and user-friendly systems that can be donned and doffed easily for daily use, potentially integrating flexible electrodes directly into consumer-grade headsets, hearables, and augmented/virtual reality devices [8]. Continued exploration of novel materials, such as graphene and other two-dimensional materials, alongside advanced fabrication techniques like printing and lithography, will be crucial to unlocking the full potential of flexible electrodes [71]. The ultimate goal is to establish a stable, high-fidelity, and comfortable skin-electrode interface that makes non-invasive BCIs a robust tool for communication, rehabilitation, and cognitive enhancement.
Workflow Diagram
The following diagram illustrates the standard development and validation workflow for a new flexible electrode design, from material selection to performance benchmarking.
Real-Time Feedback and Error Correction Mechanisms
Non-invasive Brain-Computer Interfaces (BCIs) establish a direct communication pathway between the brain and external devices, bypassing conventional neuromuscular channels [2]. Within this closed-loop system, real-time feedback and error correction mechanisms constitute critical technological components that significantly enhance performance and usability. These systems transform raw neural signals into executable commands while continuously adapting to the user's intentions and cognitive state [2] [96]. For non-invasive BCIs, particularly those using electroencephalography (EEG), implementing effective feedback and correction presents substantial technical challenges due to signal degradation, noise interference, and the non-stationary nature of brain signals [2] [97].
The fundamental importance of these mechanisms stems from their dual role: they provide users with sensory information about the system's current state (feedback) while autonomously detecting and compensating for misinterpreted commands (error correction). This dual functionality creates a collaborative learning environment where both the human user and the machine intelligence co-adapt, leading to progressively more intuitive and efficient interaction [96] [97]. As non-invasive BCIs evolve toward practical applications in healthcare, rehabilitation, and human-computer interaction, sophisticated feedback and error correction systems become increasingly essential for bridging the gap between laboratory demonstrations and real-world usability [2] [96].
Neural Mechanisms and Signal Processing for Error Detection
The human brain spontaneously generates distinctive neural patterns when it perceives errors or unexpected outcomes. These Error-Related Potentials (ErrPs) are event-related potentials that occur approximately 100-500 milliseconds after an error is detected [98] [97]. Recent research has demonstrated that ErrPs contain rich information beyond simple binary error detection, including continuous data about the magnitude and direction of perceived deviations from intended actions [98].
From a signal processing perspective, ErrPs are detected through multi-channel EEG recordings followed by sophisticated machine learning algorithms. The conventional approach has treated ErrP detection as a binary classification problem, distinguishing between correct and erroneous trials [98]. However, emerging research demonstrates the feasibility of regressing continuous error information from error-related brain activity, enabling more nuanced and naturalistic correction mechanisms [98]. This advanced approach uses multi-output convolutional neural networks to decode ongoing target-feedback discrepancies in a pseudo-online fashion, significantly improving correlations between corrected feedback and target trajectories [98].
The neural basis for these signals primarily involves the anterior cingulate cortex (ACC), which plays a key role in performance monitoring and conflict detection. When recorded non-invasively via EEG, ErrPs manifest as a characteristic waveform sequence: an initial negative deflection peaking around 100ms (N100), followed by a positive peak around 250ms (P300), and subsequent negative deflection around 400ms (N400) [98]. The precise timing and amplitude of these components provide critical features for automated error detection systems and vary based on error severity and context [98].
Table: Key Components of Error-Related Potentials in EEG
| Component | Latency (ms) | Polarity | Neural Generator | Functional Significance |
|---|---|---|---|---|
| N100 | 80-150 | Negative | Anterior Cingulate Cortex | Early error detection |
| P300 | 200-300 | Positive | Parietal Cortex | Attention allocation to error |
| N400 | 300-500 | Negative | Anterior Cingulate Cortex | Error evaluation and processing |
Modalities and Implementation of Real-Time Feedback
Effective feedback systems in non-invasive BCIs translate decoded neural commands into perceptual cues that users can intuitively interpret. The choice of feedback modality significantly influences both performance and user experience, with multimodal approaches generally yielding superior results compared to unimodal presentations [99].
Visual Feedback Modalities
Visual feedback represents the most established modality in BCI systems, typically implemented as two-dimensional cursor control tasks [99]. In motor imagery BCIs, users learn to modulate sensorimotor rhythms to control cursor movement on a screen, with the visual representation providing continuous information about decoding accuracy. Advanced implementations map this visual feedback to specific applications, such as representing vowel production through formant frequency visualization [99]. Research demonstrates that when visual feedback meaningfully corresponds to task goals—rather than serving as generic biofeedback—it significantly enhances performance metrics including accuracy, distance to target, and movement time [99].
Auditory Feedback Modalities
Auditory feedback provides an alternative or complementary modality that offers particular advantages for applications where visual attention must be directed elsewhere. Early auditory BCI implementations used generic audio signals such as pitch or volume to indicate BCI state [99]. However, recent approaches have developed more intuitive auditory mappings, such as real-time formant frequency speech synthesizers that generate vowel sounds corresponding to decoded neural commands [99]. This content-relevant auditory feedback creates a more naturalistic interface, especially for communication applications where the auditory output directly corresponds to the intended action [99].
Multimodal Feedback Integration
Multimodal feedback combines visual, auditory, and sometimes haptic information to create a richer, more robust feedback environment. Research consistently demonstrates that combined audiovisual feedback leads to superior performance compared to either unimodal condition alone [99]. In a comprehensive study comparing unimodal auditory, unimodal visual, and combined audiovisual feedback for vowel production tasks, the multimodal condition produced the greatest performance across all metrics including percent accuracy, distance to target, and movement time [99]. The effectiveness of multimodal feedback appears to depend critically on the meaningful integration of information across modalities rather than simply duplicating the same information through different channels [99].
Table: Comparison of Feedback Modalities in Non-Invasive BCIs
| Feedback Modality | Implementation Examples | Advantages | Limitations | Typical Performance Metrics |
|---|---|---|---|---|
| Visual | 2D cursor control, formant frequency visualization, target highlighting | High spatial precision, intuitive for spatial tasks | Requires visual attention, may cause fatigue | Accuracy: 70-85%, Movement time: 3-5s to target [99] |
| Auditory | Formant speech synthesis, pitch modulation, spatial audio | Eyes-free operation, natural for communication | Lower information density, environmental interference | Accuracy: 60-75%, Improved user engagement [99] |
| Multimodal | Combined cursor and speech feedback, visual+audio+tactile | Robust to single modality failure, enhanced learning | Increased system complexity, potential cognitive load | Accuracy: 80-90%, Significant performance improvement [99] |
Error Correction Mechanisms and Adaptive Algorithms
Error correction in non-invasive BCIs has evolved from simple binary classifiers to sophisticated adaptive systems that leverage multiple information sources to improve accuracy and robustness. These mechanisms can be broadly categorized into explicit error detection using ErrPs and implicit adaptation through machine learning.
Error-Related Potential (ErrP) Integration
The most direct approach to error correction involves detecting ErrPs as they naturally occur during BCI operation. When the system identifies a neural signature indicating user-perceived error, it can trigger compensatory actions including command cancellation, trajectory correction, or system recalibration [98]. Recent advances have demonstrated that continuous error regression—rather than binary classification—enables more nuanced corrections that account for both the direction and magnitude of perceived errors [98]. In practical implementation, this approach uses multi-output convolutional neural networks to decode target-feedback discrepancies from cortical activity, then applies this information to adjust the initially displayed feedback, resulting in significantly improved correlations between corrected feedback and target trajectories [98].
Reinforcement Learning for Adaptive BCIs
Reinforcement learning (RL) provides a powerful framework for developing self-adapting BCI systems that continuously improve through interaction with the user [97]. In RL-driven BCIs, the system learns optimal control policies by receiving rewards for successful actions and penalties for errors. A novel approach implements dual RL agents that dynamically adapt to EEG non-stationarities by incorporating ErrP signals and motor imagery patterns [97]. This framework enables the BCI to adjust its decoding parameters in response to changing mental states or signal characteristics, maintaining robust performance across sessions and users [97]. Validation studies using motor imagery datasets and fast-paced game environments demonstrate that RL agents can effectively learn control policies from user interactions, though task design complexity remains a critical consideration for real-world implementation [97].
Deep Learning and Fine-Tuning Approaches
Deep neural networks, particularly convolutional architectures like EEGNet, have revolutionized decoding capabilities in non-invasive BCIs [44]. These models automatically learn hierarchical representations from raw EEG signals, capturing subtle patterns associated with specific motor intentions or cognitive states. Implementation typically involves a two-stage process: initial base model training on aggregate data followed by session-specific fine-tuning using transfer learning [44]. This approach effectively addresses inter-session variability, a major challenge in non-invasive BCI systems. In finger-level robotic control tasks, fine-tuning significantly enhanced performance across binary and ternary classification paradigms, with repeated measures ANOVA showing substantial improvements between sessions (F = 14.455, p = 0.001 for binary; F = 24.590, p < 0.001 for ternary) [44].
Experimental Protocols and Methodologies
Rigorous experimental protocols are essential for developing and validating real-time feedback and error correction systems in non-invasive BCIs. The following methodologies represent current best practices across different application domains.
Motor Imagery BCI with Multimodal Feedback
This protocol evaluates feedback modalities in a motor imagery BCI for vowel production [99]:
Participant Preparation and Screening:
- Recruit native speakers without neurological impairments
- Apply 64-channel EEG system according to 10-10 international standard
- Place ground electrode at FPz, reference to left earlobe
- Record electrooculogram for artifact monitoring
Training Phase Protocol:
- Present thirty repetitions of each vowel stimulus in random order
- Use kinesthetic motor imagery: left-hand for vowel /u/, right-hand for /ɐ/, bilateral feet for /i/
- Provide modality-specific feedback according to experimental group (auditory, visual, or audiovisual)
- Estimate Kalman filter decoder parameters from training data
Online Testing Protocol:
- Present target vowel for 1.5 seconds followed by one-second blank interval
- Implement six-second response period with real-time feedback
- Begin with formant values at vowel space center (neutral sound)
- Instruct participants to initiate motor imagery to move decoded formants toward target
- Provide breaks of 3-5 seconds between trials
- Complete four runs of thirty trials each (ten trials per stimulus)
Data Collection Metrics:
- Percent accuracy of target acquisition
- Movement time to reach and maintain target
- Distance to target throughout trial
- Electrode impedance monitoring throughout session
Finger-Level Robotic Control with Error Correction
This protocol enables real-time robotic hand control at individual finger level using error-corrected motor imagery [44]:
System Setup and Calibration:
- Implement EEGNet-8.2 architecture for real-time decoding
- Configure robotic hand with individual finger actuators
- Establish continuous decoding pipeline with 128Hz sampling rate
Participant Training Protocol:
- Conduct offline session for task familiarization and base model training
- Implement two online sessions each for motor execution and motor imagery
- Assign right hand as dominant hand for all participants
- Map finger movements: thumb, index, and pinky to robotic counterparts
Online Testing with Progressive Adaptation:
- Provide dual feedback: visual (target color change) and physical (robotic finger movement)
- Begin feedback one second after trial onset
- Use base model for first 8 runs of each task
- Apply fine-tuned model for subsequent 8 runs using same-day data
- Implement online smoothing to stabilize control outputs
Performance Evaluation:
- Calculate majority voting accuracy across trial segments
- Compute precision and recall for each finger class
- Perform two-way repeated measures ANOVA for session comparisons
- Visualize feature representation discriminability across sessions
Experimental Protocol for BCI Feedback Studies
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Materials for BCI Feedback and Error Correction Studies
| Component | Specifications | Function/Purpose | Example Implementation |
|---|---|---|---|
| EEG Acquisition System | 64-channel active electrodes, g.HIAmp, reference to earlobes | Records electrical brain activity from scalp | 64 electrodes placed per 10-10 system, ground at FPz [99] |
| Signal Processing Library | EEGNet, Kalman filters, convolutional neural networks | Extracts features and decodes neural signals | EEGNet-8.2 for finger movement classification [44] |
| Feedback Actuators | Formant speech synthesizer, robotic hand, visual display | Provides real-time sensory feedback to user | Formant synthesizer (Snack Sound Toolkit) [99] |
| Error Detection Algorithm | Multi-output CNN, ErrP regression models | Identifies error-related brain potentials | Continuous error regression from cortical activity [98] |
| Adaptive Learning Framework | Reinforcement learning agents, fine-tuning mechanisms | Enables system adaptation to user and signal changes | Dual RL agents incorporating ErrPs and motor imagery [97] |
| Experimental Control Software | Psychophysics Toolbox, OpenVibe, custom MATLAB/Python | Prescribes trial structure and records responses | Randomized trial presentation with breaks [99] |
Technical Implementation and System Architecture
Implementing robust real-time feedback and error correction requires a sophisticated system architecture that balances computational efficiency with decoding accuracy. The core technical challenge lies in processing high-dimensional EEG signals within tight latency constraints to enable truly interactive control.
Signal Processing Pipeline
The standard processing pipeline begins with analog-to-digital conversion of multi-channel EEG signals, typically at sampling rates between 128-1000 Hz with 16-24 bit resolution [100]. Subsequent digital filtering removes line noise (50/60 Hz) and isolates frequency bands of interest, commonly implementing bandpass filters between 0.5-40 Hz for ErrP detection and 8-30 Hz for sensorimotor rhythms [100]. Artifact removal algorithms then identify and compensate for ocular, muscular, and motion artifacts using techniques like independent component analysis or regression-based approaches [2].
For error correction systems, the processed signals feed into parallel decoding pathways: one for primary intent recognition (e.g., motor imagery classification) and another for continuous error monitoring [98] [97]. This dual-path architecture enables real-time correction by comparing the primary command stream with simultaneously decoded error signals. Implementation typically employs a multi-output convolutional neural network that performs both classification and regression tasks, extracting spatial-temporal features from raw EEG while maintaining computational efficiency for real-time operation [98].
Hardware Considerations and Optimization
As BCIs transition toward portable and clinical applications, hardware constraints become increasingly important. Recent analysis reveals a counterintuitive relationship in BCI hardware design: increasing the number of channels can simultaneously reduce power consumption per channel through hardware sharing while increasing the Information Transfer Rate by providing more input data [100]. For EEG and ECoG decoding circuits, power consumption is dominated by signal processing complexity rather than data acquisition itself [100].
Effective hardware implementations must balance multiple constraints including input data rate (IDR), classification latency, and power efficiency. Empirical studies indicate that achieving a target classification rate requires a specific IDR that can be estimated during system design [100]. Optimization strategies include leveraging fixed-point arithmetic, implementing application-specific integrated circuits (ASICs) for common operations like filtering and feature extraction, and employing hardware-sharing techniques that maximize resource utilization across multiple channels [100].
Dual-Path Architecture for BCI Error Correction
Performance Metrics and Evaluation Frameworks
Comprehensive evaluation of feedback and error correction mechanisms requires multidimensional assessment spanning technical performance, usability, and clinical relevance. While classification accuracy remains a fundamental metric, it provides an incomplete picture of real-world system effectiveness [96].
Technical Performance Metrics
Information Transfer Rate (ITR) measures the communication bandwidth achieved by a BCI system, incorporating both speed and accuracy into a single value [100]. Modern systems target ITRs between 20-50 bits/minute for practical applications. Correlation coefficients between intended and executed trajectories provide critical insights for continuous control tasks, with successful error correction systems demonstrating significant improvements in these correlations after implementation [98]. Temporal precision metrics evaluate system latency, with effective error correction requiring complete processing within 100-500ms to align with natural human response timing [98].
For error correction specifically, false positive and negative rates in ErrP detection must be balanced, as excessive false positives unnecessarily interrupt operation while false negatives permit uncorrected errors to persist [98]. Additionally, correction effectiveness quantifies how accurately the system compensates for detected errors, measured by the similarity between post-correction outputs and intended commands [98].
User-Centered Evaluation
Beyond technical metrics, comprehensive evaluation must incorporate user experience measures including usability, user satisfaction, and cognitive load [96]. These qualitative assessments capture aspects like frustration levels, mental fatigue, and perceived control that significantly influence long-term adoption. Emerging evaluation frameworks emphasize the importance of ecological validity, testing systems in environments that approximate real-world conditions rather than optimized laboratory settings [96].
Effective evaluation follows a tiered approach, beginning with offline analysis to identify promising algorithms, progressing to online closed-loop testing with able-bodied participants, and culminating in longitudinal studies with target patient populations [96]. This iterative process acknowledges the significant performance discrepancies that often emerge between offline simulations and online operation, making online evaluation the gold standard for assessing real-world viability [96].
Addressing User Training and BCI Illiteracy Challenges
Brain-Computer Interface (BCI) illiteracy represents one of the most significant barriers to the widespread adoption of non-invasive BCI technologies. This phenomenon refers to the inability of a substantial portion of users—estimated between 15% to 30%—to produce the specific, distinguishable brain patterns necessary to reliably control a BCI system [101] [102]. For these individuals, achieving the desired control over external devices through motor imagery or other cognitive tasks remains elusive even after standard training periods. The core of this challenge lies in the substantial inter-subject variability in EEG signals, which arises from differences in brain anatomy, cognitive strategies, and neurophysiological responses [102]. This variability makes it difficult to develop universal BCI systems that perform consistently across all users, thereby limiting the technology's real-world applicability in both clinical and non-clinical settings.
The implications of BCI illiteracy extend beyond mere inconvenience. In therapeutic contexts, such as spinal cord injury rehabilitation, where non-invasive BCIs show promise for improving motor function (SMD = 0.72), sensory function (SMD = 0.95), and activities of daily living (SMD = 0.85), the inability to effectively use these systems could deny patients potential benefits [10]. Similarly, in educational applications where BCIs have demonstrated potential for improving concentration and skill acquisition—such as a documented 15% average improvement in accuracy in musical training tasks—BCI illiteracy could create inequities in access to these emerging learning technologies [103]. Addressing this challenge is therefore critical for ensuring the equitable and effective deployment of BCI systems across diverse user populations.
Quantitative Landscape of BCI Performance and Illiteracy
Understanding the scope and impact of BCI illiteracy requires examining performance data across user populations. The following table synthesizes key quantitative findings from recent research on BCI performance and the illiteracy challenge:
Table 1: BCI Performance Metrics and Illiteracy Statistics
| Metric Category | Specific Metric | Value or Range | Context and Implications |
|---|---|---|---|
| Illiteracy Prevalence | Estimated affected population | 15-30% of users [101] [102] | A significant minority unable to achieve control with standard systems |
| Performance Threshold | Classification accuracy threshold for "illiteracy" | Below 70% [102] | Benchmark for identifying struggling users |
| Rehabilitation Effect Sizes | Motor function improvement (SMD) | 0.72 [95% CI: 0.35,1.09] [10] | Medium effect size showing clinical potential |
| Sensory function improvement (SMD) | 0.95 [95% CI: 0.43,1.48] [10] | Medium effect size in sensory domains | |
| Activities of daily living (SMD) | 0.85 [95% CI: 0.46,1.24] [10] | Low to medium effect size for functional outcomes | |
| Training Efficacy | Accuracy improvement with feedback | Average 15% improvement [103] | Demonstrates trainability of BCI skills |
Beyond these quantitative measures, the temporal dimension of BCI illiteracy reveals additional insights. Research indicates that BCI performance is not static but can evolve with appropriate training interventions. For instance, co-adaptive learning approaches have demonstrated that some initially "illiterate" users can achieve successful control within 3-6 minutes of adaptation through properly structured training protocols [101]. Furthermore, subgroup analyses have revealed that patients in subacute stages of spinal cord injury show statistically stronger responses to BCI interventions compared to those in slow chronic stages, suggesting that timing of intervention may affect outcomes [10]. These findings underscore the dynamic nature of BCI literacy and the importance of personalized, adaptive approaches to training.
Technical Approaches to Overcoming BCI Illiteracy
Machine Learning and Adaptive Algorithms
Modern approaches to addressing BCI illiteracy heavily leverage advanced machine learning techniques that create a symbiotic relationship between the user and the system. Co-adaptive learning represents a foundational strategy in this domain, where both the user and the algorithm continuously adapt to each other during the feedback process [101] [102]. In practical implementation, this begins with a subject-independent classifier that operates on simple features (band-power in alpha and beta frequencies), then progressively transitions to more complex, subject-optimized features including subject-specific narrow frequency bands and Common Spatial Pattern (CSP) filters [101]. The linear discriminant analysis (LDA) classifier is typically updated using recursive-least-square algorithms with update coefficients between 0.015-0.05, balancing stability with adaptability to the user's evolving neural patterns [101].
Another significant approach involves multi-kernel learning, which aims to make feature distributions more similar across users while maximizing category separability [102]. However, these conventional ML methods often rely on assumptions of linear separability and same feature space, and can struggle with the high-dimensional nature of EEG data [102]. The following table compares the primary technical approaches to addressing BCI illiteracy:
Table 2: Technical Solutions for BCI Illiteracy
| Technical Approach | Core Methodology | Advantages | Limitations and Challenges |
|---|---|---|---|
| Co-adaptive Learning [101] [102] | Continuous mutual adaptation of user and classifier | Rapid performance acquisition (3-6 mins); Works with novice users | Requires sophisticated algorithm design; Multiple adaptation levels needed |
| Subject-to-Subject Style Transfer [102] | Transferring discrimination styles from experts to illiterates | Addresses inter-subject variability directly; Improved performance for illiterates | Risk of negative transfer; Requires expert subject data |
| Domain Adaptation [102] | Extracting common domain-invariant features from multiple subjects | Leverages multi-subject data; Potential for robust general models | Requires large labeled datasets; Susceptible to negative transfer |
| Deep Learning Models [102] | Using neural networks for feature extraction and classification | Handles high-dimensional data well; Reduced need for handcrafted features | Data-hungry; Computationally intensive; Less interpretable |
Subject-to-Subject Semantic Style Transfer
A particularly promising approach for addressing BCI illiteracy is the Subject-to-Subject Semantic Style Transfer Network (SSSTN), which operates at the feature level to bridge the performance gap between expert and illiterate users [102]. This method uses continuous wavelet transform to convert high-dimensional EEG data into images as input. The process involves three key stages: first, training a separate classifier for each subject; second, transferring the distribution of class discrimination styles from a source subject (BCI expert) to target subjects (BCI illiterates) through a specialized style loss function while preserving class-relevant semantic information via a modified content loss; and finally, merging classifier predictions from both source and target subjects using ensemble techniques [102].
This approach has demonstrated improved classification performance on standard datasets (BCI Competition IV-2a and IV-2b), particularly for users who previously struggled with BCI control [102]. The method's effectiveness stems from its ability to address the fundamental challenge of inter-subject variability without requiring extensive labeled data from multiple subjects, which has been a limitation of conventional domain adaptation methods. The visual representation below illustrates the workflow and core mechanisms of this approach:
Standardized Experimental Protocols for User Training
Structured Training Framework
Effective addressing of BCI illiteracy requires systematic training protocols that extend beyond technical algorithms alone. A comprehensive framework divides user training into two critical periods: the introductory period (before BCI interaction) and the BCI interaction period (during active use) [104]. The introductory period is particularly crucial as it establishes the user's mental model, understanding, and confidence with the system. Research demonstrates that BCI performance can be significantly influenced by methodologies employed during this preliminary phase, highlighting the need for standardized approaches that optimize user preparedness [104].
During the BCI interaction period, the design of the interface itself—including its form (2D, 3D, size, color) and modality (visual, auditory, haptic)—requires careful consideration based on principles of perceptual affordance [104]. Studies show that motor neurons can be triggered simply by observing certain objects, with neural reactions varying based on object properties like size and location. Surprisingly, these effects of perceptual affordance have not been systematically investigated in BCI contexts, representing a promising area for future research [104]. The lack of standardization in both introductory procedures and interface designs currently makes it difficult to reproduce experiments, predict outcomes, and compare results across studies.
Co-Adaptive Training Methodology
The co-adaptive training methodology represents a sophisticated approach that guides users from initial subject-independent classifiers to fully optimized subject-specific systems. The typical implementation involves three progressive levels of adaptation:
Level 1 (Runs 1-3): Initial operation using a pre-trained subject-independent classifier based on simple features (band-power in alpha and beta frequencies from Laplacian channels at C3, Cz, C4). During this phase, the LDA classifier undergoes supervised adaptation after each trial using recursive-least-square algorithms with update coefficients of 0.015 for covariance matrix updates and 0.05 for class-specific mean estimation [101].
Level 2 (Runs 4-6): Transition to more complex feature sets including subject-specific narrow frequency bands and Common Spatial Pattern (CSP) filters. The system automatically selects an optimized frequency band based on data from the first three runs, with channel selection constrained to include two positions each from areas over left hand, right hand, and foot regions. Classifiers are recalculated after each trial using the last 100 trials, incorporating both CSP channels and repeatedly selected Laplacian channels [101].
Level 3 (Runs 7-8): Final phase employing unsupervised adaptation where CSP filters calculated from runs 4-6 remain static, but the classifier bias is adapted by updating the pooled mean after each trial without class label distinction. This provides an unbiased measure of BCI performance while maintaining system adaptability [101].
This structured yet flexible approach has demonstrated success in helping previously illiterate users gain significant control over BCI systems, with some users developing characteristic sensory motor idle rhythms during the course of a single session that were absent at the beginning [101].
Essential Research Reagents and Tools
Implementing effective solutions for BCI illiteracy requires specific methodological tools and computational resources. The following table catalogues key research reagents and their functions in developing and testing BCI training protocols:
Table 3: Essential Research Reagents and Computational Tools for BCI Illiteracy Research
| Research Reagent / Tool | Category | Function and Application | Implementation Notes |
|---|---|---|---|
| Linear Discriminant Analysis (LDA) [101] [102] | Classification Algorithm | Core classifier for motor imagery tasks; Adaptable via recursive updates | Often used with shrinkage regularization for high-dimensional features |
| Common Spatial Patterns (CSP) [101] | Feature Extraction | Optimizes spatial filters for discriminative feature extraction | Identifies patterns that maximize variance between classes |
| Continuous Wavelet Transform [102] | Signal Processing | Converts temporal EEG signals to time-frequency representations | Creates image-like inputs for deep learning approaches |
| Subject-to-Subject Semantic Style Transfer Network (SSSTN) [102] | Deep Learning Architecture | Transfers classification style from experts to novices | Uses style and content losses to preserve semantics |
| Recursive-Least-Square Algorithm [101] | Adaptive Filtering | Updates classifier parameters during online operation | Enables real-time adaptation with forgetting factor |
| BCI Competition IV-2a/2b Datasets [102] | Benchmark Data | Standardized datasets for method validation | Enables comparative performance assessment |
| Shrinkage Covariance Estimation [101] | Regularization Technique | Stabilizes covariance matrix estimation with limited data | Addresses small sample size issues in adaptive settings |
These tools collectively enable researchers to implement the sophisticated adaptive systems necessary to address BCI illiteracy. The combination of traditional machine learning approaches like LDA with emerging deep learning techniques like style transfer networks represents the current state of the art in making BCI technology accessible to broader user populations.
The challenge of BCI illiteracy remains a significant but addressable barrier to the widespread adoption of non-invasive brain-computer interfaces. Current evidence suggests that through integrated approaches combining co-adaptive algorithms, structured training protocols, and advanced transfer learning methods, a substantial proportion of initially struggling users can achieve functional BCI control. The quantitative improvements demonstrated in rehabilitation outcomes—particularly for motor and sensory functions in spinal cord injury patients—highlight the practical importance of overcoming this challenge [10].
Future research directions should focus on several key areas: first, the development of more sophisticated cross-subject validation frameworks to better predict individual performance; second, the integration of multimodal feedback and perceptual affordance principles into training protocols; and third, the creation of standardized benchmarking datasets and metrics specifically designed for evaluating BCI illiteracy solutions [104]. Additionally, exploring the neural correlates of successful versus unsuccessful BCI control may provide neurophysiological markers that could guide personalized training approaches. As these technical advances mature, they promise to make non-invasive BCI technology more accessible and effective across diverse applications from clinical rehabilitation to educational enhancement, ultimately fulfilling the potential of direct brain-computer communication for broader user populations.
Power Management and Computational Efficiency Optimization
The evolution of non-invasive Brain-Computer Interfaces (BCIs) is fundamentally constrained by power consumption and computational efficiency, particularly for wearable, battery-operated, or implantable applications. Effective power management is not merely an engineering consideration but a critical enabler for practical, long-duration BCI deployment in clinical, research, and consumer settings. This guide analyzes the core principles and state-of-the-art techniques for optimizing these parameters, focusing on hardware-software co-design strategies that balance computational demands with strict energy budgets. The pursuit of efficiency is driving innovation across the signal processing chain, from novel low-power circuits and optimized machine learning algorithms to system-level architectural choices that minimize data movement and processing overhead [105]. As the BCI market is forecasted to grow to over US$1.6 billion by 2045, advancements in efficiency will be pivotal for widespread adoption [8].
Core Power and Performance Metrics for BCI Systems
Quantifying the performance and efficiency of BCI systems requires a standardized set of metrics. These benchmarks allow for direct comparison between different technological approaches and provide clear goals for optimization efforts.
Table 1: Key Performance and Power Metrics for BCI Systems
| Metric | Description | Importance for Optimization |
|---|---|---|
| Information Transfer Rate (ITR) | The speed at which information is communicated from the brain to an external device, typically measured in bits per minute [105]. | A primary measure of BCI performance; optimization aims to increase ITR without a proportional increase in power. |
| Input Data Rate (IDR) | The rate of data inflow from the recording electrodes, determined by the number of channels, sampling rate, and bit resolution [105]. | A major driver of system power; reducing the effective IDR through processing is a key goal. |
| Power per Channel (PpC) | The power consumption attributable to a single data acquisition and processing channel [105]. | Enables fair comparison between systems with different channel counts; lower PpC is critical for scalability. |
| Classification Rate / Decision Rate (DR) | The frequency at which the system outputs a classified brain state or command [105]. | Determines the system's responsiveness; must be optimized against latency and power constraints. |
| Energy per Classification | The total energy consumed to process sensor data and produce a single output classification. | A holistic efficiency metric that encompasses hardware and algorithmic performance. |
Counter-intuitively, research has shown a negative correlation between Power per Channel (PpC) and Information Transfer Rate (ITR). This indicates that increasing the number of channels can, through efficient hardware sharing, simultaneously reduce the PpC while providing more input data to boost the ITR [105]. This principle underscores the importance of system-level design over isolated component optimization.
Hardware-Level Optimization Strategies
The physical layer of a BCI system, encompassing the electrodes, analog front-end, and data conversion hardware, presents the first and most critical opportunity for power savings.
Electrode Technology and Data Acquisition
The choice of electrode technology directly impacts signal quality and system complexity. While traditional wet electrodes (using electrolyte gel) provide excellent signal quality, they require preparation time and are less suitable for long-term use. Dry electrodes are an emerging solution that reduces setup burden and improves user comfort for wearable applications [8]. Furthermore, the spatial resolution and signal source differ significantly between non-invasive and invasive methods, which in turn affects power demands. Electroencephalography (EEG) signals, recorded from the scalp, are averaged over a large number of neurons and are susceptible to noise, necessitating sophisticated filtering and processing. In contrast, invasive methods like Microelectrode Arrays (MEAs) capture precise, single-neuron activity but require complex, high-channel-count implantable systems [105].
Low-Power Circuit Design for On-Chip Decoding
For battery-powered, miniaturized medical devices, general-purpose microprocessors consume too much power. The field is therefore moving toward custom, application-specific integrated circuits (ASICs) and Systems-on-Chip (SoCs) [105].
Table 2: Hardware Optimization Techniques for Low-Power BCI Decoding
| Technique | Implementation | Impact on Power and Performance |
|---|---|---|
| Analog Feature Extraction | Performing initial signal processing (e.g., filtering, feature detection) in the analog domain before analog-to-digital conversion [105]. | Dramatically reduces the power and data load on the digital signal processor and ADC. |
| Hardware Sharing | Leveraging the empirical finding that a higher number of channels can reduce PpC. Resources like arithmetic logic units (ALUs) and memory are shared across multiple channels [105]. | Lowers overall power consumption (PpC) while increasing data input, potentially boosting ITR. |
| Mixed-Signal SoCs | Integrating analog acquisition, digital processing, and sometimes wireless communication on a single chip to minimize off-chip data transfer [105]. | Reduces the size, weight, and power (SWaP) of the entire system, which is crucial for implantable and wearable devices. |
| Adaptive Sampling | Dynamically adjusting the sampling rate or resolution based on the current state of the brain signal or the task demands. | Saves power during periods of low-information brain activity or when high precision is not required. |
Analysis of state-of-the-art decoding circuits reveals that for non-invasive BCIs like EEG and ECoG, the power consumption is dominated by the complexity of the digital signal processing rather than the data acquisition itself [105]. This highlights the critical need for efficient algorithms and processing architectures.
Algorithmic and Computational Optimizations
The software and algorithmic layer offers extensive opportunities to reduce computational load, thereby enabling the use of lower-power hardware.
Signal Processing and Machine Learning
The core computational burden lies in translating raw, noisy brain signals into clean, actionable commands. Key optimization strategies include:
- Feature Extraction and Selection: Instead of processing all available data, algorithms identify the most informative features from the brain signals (e.g., specific frequency band powers from EEG). Dimensionality reduction techniques like Principal Component Analysis (PCA) or Linear Discriminant Analysis (LDA) are commonly used to reduce the data load for the subsequent classification stage [2] [105].
- Efficient Classification Models: While deep neural networks offer high performance, they are computationally expensive. For many BCI applications, simpler models like Linear Discriminant Analysis (LDA) and Support Vector Machines (SVM) provide a favorable balance between accuracy and computational cost, making them suitable for low-power implementations [2] [105].
- Online Model Adaptation: The ability to update the decoding model in real-time to adapt to the user's changing brain signals (a phenomenon known as "non-stationarity") is a key research area. Circuits that enable such online updates, like the one described by Zhong et al. for SSVEP-based drone control, prevent performance degradation over time without requiring a full, power-intensive retraining [105].
The following diagram illustrates the optimized signal decoding workflow that incorporates these power-saving techniques.
Experimental Protocols for Evaluating BCI Efficiency
To validate new power management techniques, researchers employ standardized experimental protocols that measure both performance and power consumption. The following workflow outlines a standard methodology for such evaluations.
Detailed Methodology for Power-Performance Correlation
This protocol provides a framework for generating comparable data on BCI system efficiency.
BCI Paradigm Selection: Choose a well-established BCI paradigm for benchmarking, such as:
- P300: An event-related potential elicited by a rare or significant stimulus, commonly used for spellers [106].
- Motor Imagery (MI): The imagination of movement, which modulates sensorimotor rhythms in the EEG, used for continuous control [105] [106].
- Steady-State Visually Evoked Potentials (SSVEP): Responses to visual stimuli flickering at a constant frequency, allowing for high-ITR control [105].
System Implementation: Develop the BCI system prototype, incorporating the optimization technique under investigation (e.g., a new low-power classifier, analog feature extraction circuit, or hardware-sharing architecture).
Performance Benchmarking: Establish baseline performance metrics without power constraints. This includes measuring the system's Accuracy (%) and Information Transfer Rate (ITR in bits/min) under controlled conditions [105].
Power Measurement Setup: Integrate a high-precision power meter into the system's power supply line. For multi-channel systems, it is critical to measure both total system power and, where possible, the Power per Channel (PpC). The device should be tested under its intended operating voltage.
Controlled Task Execution: Recruit participants to perform a predefined series of BCI tasks (e.g., a calibration session followed by a goal-oriented task like controlling a cursor or spelling). During these tasks, simultaneously log performance data (accuracy, timing) and detailed power consumption data.
Data Analysis and Correlation: Analyze the collected data to establish the relationship between performance and power. Key analyses include:
- Plotting ITR against PpC to confirm or refute the observed negative correlation [105].
- Calculating the Energy per Classification by dividing the average power during a trial by the classification rate.
- Comparing the performance-power trade-off of the new optimized system against a reference, non-optimized system.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential components and tools for developing and testing power-efficient non-invasive BCIs.
Table 3: Essential Research Tools for Power-Efficient BCI Development
| Item / Reagent | Function in Research & Development |
|---|---|
| Dry EEG Electrodes | Enable longer-term, more user-friendly recordings compared to wet electrodes, facilitating research into practical, wearable BCI systems [8]. |
| Low-Power SoC/FPGA Platforms | Provide a reconfigurable hardware platform for prototyping and deploying custom low-power signal processing algorithms and on-chip decoders [105]. |
| Linear Discriminant Analysis (LDA) | A computationally lightweight classification algorithm that serves as a high-performance baseline for comparing the efficiency of more complex models [105]. |
| Input Data Rate (IDR) Estimator | A model or script to estimate the data rate from channel count, sampling rate, and resolution. This is crucial for sizing and power-balancing new BCI systems [105]. |
| WCAG 2.1 Contrast Checkers | Tools (e.g., WebAIM's Contrast Checker) to validate visual stimuli in paradigms like P300 or SSVEP, ensuring they are accessible and effective for all users, which is critical for robust experimental design [107]. |
| Power Meter & Profiling Software | Essential instrumentation for measuring power consumption at the system, component, and channel level during experimental validation [105]. |
Ensuring Long-Term System Stability and Reliability
For researchers and clinicians deploying non-invasive Brain-Computer Interfaces (BCIs), ensuring long-term system stability and reliability presents a formidable scientific challenge. Unlike their invasive counterparts, which record neural activity directly from the cortex, non-invasive systems acquire signals through the skull, resulting in inherent limitations in signal-to-noise ratio (SNR) and spatial resolution [67]. The electrophysiological properties of the extracellular space, cerebrospinal fluid, skull, and scalp collectively act as a spatial low-pass filter, attenuating and distorting the electrical fields generated by neural currents before they reach scalp electrodes [67]. This tutorial provides a technical framework for characterizing, monitoring, and improving the stability of non-invasive BCI systems, with a focus on methodologies applicable to clinical research and therapeutic development.
The reliability of a non-invasive BCI is contingent upon the stable acquisition of key neural signals. The most common signals targeted for BCI control include the P300 event-related potential, sensorimotor rhythms (SMR), steady-state evoked potentials (SSEP), and the contingent negative variation (CNV) [106]. The integrity of these signals is compromised by several technical and biological factors.
First, the signal composition itself is a limitation. Non-invasive techniques like electroencephalography (EEG) are primarily sensitive to post-synaptic extracellular currents from pyramidal neurons, which must superimpose across a large, confined area to be detectable at the scalp. This makes them less sensitive to the activity of small neuronal clusters compared to invasive methods [67]. Furthermore, biological tissues act as a low-pass filter, generally attenuating high-frequency neural activity (>90 Hz) to a level buried in background noise [67].
Second, instability arises from multiple operational domains:
- Signal Quality Degradation: Electrode impedance can fluctuate due to skin preparation, drying electrolyte gel, or user movement [106] [8].
- User State Variability: User's cognitive state, fatigue, and level of adaptation introduce significant variance in neural signals [108].
- Environmental Noise: Ambient electromagnetic noise from power lines and electronic equipment can corrupt sensitive electrophysiological recordings [108].
Table 1: Key Performance Benchmarks for Non-Invasive BCI Signals
| Neural Signal | Typical Spatial Resolution | Typical Temporal Resolution | Primary Stability Challenges |
|---|---|---|---|
| P300 Event-Related Potential | Low (Scalp-level) | High (Milliseconds) | Sensitivity to user attention and oddball stimulus probability [106] |
| Sensorimotor Rhythms (SMR) | Low to Moderate | High | User learning effects; susceptibility to muscle artefact [106] [67] |
| Steady-State Evoked Potentials | Low (Scalp-level) | High | Signal amplitude and stability dependent on stimulus properties [106] |
| Contingent Negative Variation (CNV) | Low (Scalp-level) | High | Dependency on user expectation and readiness [106] |
A Framework for Quantifying and Monitoring Stability
A rigorous, data-driven approach is essential for quantifying long-term stability. This involves tracking key metrics across multiple experimental sessions.
Key Performance Indicators (KPIs)
Researchers should systematically monitor the following KPIs:
- Information Transfer Rate (ITR): A composite measure of accuracy and speed, typically in bits per minute. A declining ITR indicates system degradation [67].
- Signal-to-Noise Ratio (SNR): Calculated for specific event-related potentials or frequency bands. A stable or improving SNR suggests robust signal acquisition [67].
- Classification Accuracy: The core metric for most BCIs. Tracking accuracy over time, both within and across sessions, is fundamental [10] [108].
- Electrode Impedance: Should be logged continuously or at regular intervals to identify deteriorating electrode contact [8].
Experimental Protocols for Longitudinal Assessment
To objectively assess stability, controlled longitudinal studies are required. The following protocol provides a template for such an assessment, adaptable for different BCI paradigms.
Protocol 1: Longitudinal BCI Stability Assessment
- Objective: To evaluate the intra- and inter-session stability of a non-invasive BCI system's performance and signal characteristics over a predefined period (e.g., 3 months).
- Participant Recruitment: Recruit a cohort of end-users (e.g., patients with Spinal Cord Injury or healthy controls). A systematic review of BCI for SCI suggests medium-level evidence for improved motor and sensory function, highlighting the importance of stable performance for clinical application [10].
- Baseline Session:
- Perform standardized skin preparation and electrode placement (e.g., following the 10-20 system) [106].
- Record resting-state EEG (eyes-open, eyes-closed) for 5 minutes to establish baseline noise floors and connectivity patterns.
- Conduct a standardized BCI calibration task (e.g., a motor imagery or P300 speller task).
- Intervention/Training Phase: Participants undergo a defined number of BCI training or usage sessions per week, using the experimental paradigm.
- Data Collection Points: During each session, record:
- Continuous Impedance Values: From all active electrodes.
- Raw EEG Data: From all tasks.
- Task Performance Metrics: Including trial-by-trial accuracy, timing, and ITR.
- Data Analysis:
- Compute within-session and between-session variance for all KPIs.
- Use statistical process control (SPC) charts to monitor for significant deviations in SNR and accuracy.
- Perform test-retest reliability analysis on features extracted from the resting-state and task data.
Diagram 1: Stability Assessment Workflow
Methodologies for Enhancing System Reliability
Improving reliability requires a multi-pronged approach addressing hardware, software, and user interaction.
Advanced Signal Acquisition and Processing
- Adaptive Noise Cancellation: Implement algorithms that dynamically model and subtract environmental and physiological artifacts (e.g., from eye movements or muscle activity) [108]. The integration of optical modalities like functional Near-Infrared Spectroscopy (fNIRS) with EEG can create a hybrid system that is less susceptible to motion artifacts, thereby improving robustness [108].
- Feature Adaptation: Decoder recalibration is critical. Algorithms should be designed to track non-stationarities in the neural signal, either by using adaptive classifiers that update their parameters in the background or by scheduling periodic explicit recalibration sessions [108].
- Dry Electrode Technology: While traditional wet electrodes require conductive gel which can dry out, emerging dry electrode designs offer improved long-term usability and comfort, though they often come with a trade-off of higher baseline impedance [8]. Material innovations in this area are a key research focus for improving stability.
Robust Experimental and User-Focused Design
- User Training and Neurofeedback: A BCI system is a co-adaptive loop. Providing users with effective neurofeedback allows them to learn to modulate their brain signals more consistently, which directly improves system stability [106]. This is particularly relevant for Motor Imagery (MI)-based BCIs, where user aptitude varies [108].
- Paradigm Design: For evoked potentials like the P300, designing a robust and engaging stimulus presentation paradigm can help maintain user attention over long sessions, reducing performance drift [106].
Protocol 2: Closed-Loop Adaptive Decoder Calibration
This protocol outlines a method for maintaining decoder performance in the face of non-stationary neural signals.
- Objective: To stabilize BCI performance by implementing a closed-loop system that adapts the decoding algorithm to gradual changes in neural signal features.
- System Setup: Utilize a BCI software framework that supports online signal processing and classifier output, such as the open-source framework mentioned in [108], which enables human-in-the-loop model training and real-time EEG classification.
- Initial Model Training: Collect a high-quality dataset during a user-specific calibration session to train an initial decoder.
- Online Operation:
- During BCI use, continuously extract feature vectors from the streaming neural data.
- Maintain a rolling buffer of recent feature vectors and their corresponding decoder outputs/outcomes.
- Periodically, use this recent data to compute a updated version of the decoder model. This can be done via a dynamic weighted algorithm that gives more importance to recent data points.
- Stability Check: Implement a change-point detection algorithm to prevent the model from adapting to spurious noise. Only significant and persistent shifts in the feature distribution should trigger a major model update.
Diagram 2: Adaptive Calibration Logic
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and tools for building and maintaining a reliable non-invasive BCI research platform.
Table 2: Essential Research Toolkit for Non-Invasive BCI Stability
| Item / Solution | Function & Relevance to Stability | Technical Notes |
|---|---|---|
| High-Density EEG Systems (64+ channels) | Enables source localization to mitigate spatial distortion and better isolate neural signals from noise [106] [67]. | Critical for research; commercial systems may use fewer electrodes (e.g., 8) to reduce setup burden [106]. |
| Electrolyte Gel & Abrasive Skin Prep | Maintains low and stable electrode-skin impedance, the foundation of high-quality signal acquisition [106]. | Gel drying is a major source of signal decay in long sessions. |
| Hybrid fNIRS-EEG Systems | Provides complementary hemodynamic (fNIRS) and electrophysiological (EEG) data, improving robustness against motion artifacts and enabling validation across modalities [108]. | fNIRS is noted for its portability and high spatial resolution, making it a growing sub-segment [36]. |
| Open-Source BCI Software Frameworks | Supports real-time stimulus control, online EEG classification, and human-in-the-loop model training, which is essential for implementing adaptive decoders [108]. | Enhances reproducibility and allows for customization of stability protocols. |
| Dry EEG Electrodes | Eliminates the need for gel, improving setup time and long-term comfort for users, which can reduce fatigue-related performance decay [8]. | Performance can be variable and dependent on specific design and fit; an area of active innovation. |
Achieving long-term stability and reliability in non-invasive BCIs is a multifaceted endeavor that requires rigorous attention to signal acquisition, processing, and user interaction. By adopting a framework of continuous monitoring using defined KPIs, implementing adaptive algorithms to handle neural non-stationarities, and leveraging advancements in hybrid imaging and electrode technology, researchers can significantly enhance the robustness of their systems. This reliability is the critical bridge that will translate the promising efficacy observed in controlled lab settings, such as improvements in motor function for Spinal Cord Injury patients [10], into effective and dependable real-world clinical and research applications.
Evidence-Based Assessment and Performance Benchmarking
The validation of therapeutic interventions through meta-analysis represents the highest standard of evidence-based medicine in clinical neuroscience. For brain-computer interface (BCI) technologies, which stand at the intersection of neuroscience, engineering, and clinical practice, rigorous synthesis of emerging evidence is particularly crucial. This review focuses exclusively on non-invasive BCI approaches—defined by their external placement and absence of surgical implantation—which offer distinct advantages in safety and accessibility while facing unique challenges in signal fidelity and clinical efficacy [6].
The fundamental mechanism of non-invasive BCI operation involves a closed-loop system where neural signals are acquired, processed, and translated into commands that enable patient interaction with external devices or provide therapeutic feedback. This process creates a real-time neurofeedback mechanism that promotes neuroplasticity—the brain's inherent capacity to reorganize neural pathways in response to experience and injury [10] [62]. The therapeutic potential of this technology is particularly relevant for neurological disorders where traditional interventions have reached plateaued effectiveness.
This technical review examines the current state of clinical validation for non-invasive BCIs through comprehensive analysis of recent meta-analyses, with particular focus on spinal cord injury and stroke rehabilitation. We present synthesized quantitative evidence, detailed methodological protocols, and analytical frameworks to assess the translation of BCI technologies from laboratory demonstrations to clinically validated therapeutics.
Quantitative Synthesis of Therapeutic Efficacy
Recent meta-analyses have provided quantitative assessments of non-invasive BCI efficacy across multiple neurological domains. The tabulated results below represent synthesized evidence from randomized controlled trials (RCTs) and self-controlled studies, highlighting effect sizes and evidence quality.
Table 1: Meta-Analysis Findings for Non-Invasive BCI in Spinal Cord Injury Rehabilitation
| Functional Domain | Studies (Patients) | Standardized Mean Difference (SMD) | 95% Confidence Interval | Evidence Quality (GRADE) |
|---|---|---|---|---|
| Motor Function | 9 (109) | 0.72 | [0.35, 1.09] | Moderate |
| Sensory Function | 9 (109) | 0.95 | [0.43, 1.48] | Moderate |
| Activities of Daily Living | 9 (109) | 0.85 | [0.46, 1.24] | Low |
Data extracted from a 2025 meta-analysis of non-invasive BCI interventions for spinal cord injury (SCI) shows consistent positive effects across functional domains, with particularly strong benefits for sensory function (SMD = 0.95) [10]. The analysis included 4 randomized controlled trials and 5 self-controlled trials, with all outcomes reaching statistical significance (p < 0.01) with low heterogeneity (I² = 0%) [10].
Table 2: Network Meta-Analysis of Upper Limb Rehabilitation Interventions Post-Stroke
| Intervention | Surface Under Cumulative Ranking Curve (SUCRA) | Mean Difference vs. Conventional Therapy | 95% Confidence Interval |
|---|---|---|---|
| BCI-FES + tDCS | 98.9 | 9.26 | [2.19, 9.83] |
| BCI-FES | 73.4 | 6.01 | [2.19, 9.83] |
| tDCS | 33.3 | -0.48 | [-2.72, 14.82] |
| FES | 32.4 | 2.16 | [2.17, 5.53] |
| Conventional Therapy | 12.0 | Reference | - |
A 2025 network meta-analysis of 13 studies (777 subjects) directly compared intervention efficacy for upper limb recovery post-stroke, ranking combined BCI-FES with tDCS as most effective (SUCRA = 98.9) [109]. BCI-FES alone also demonstrated significant advantages over conventional therapy (MD = 6.01, 95% CI: [2.19, 9.83]) [109].
Methodological Frameworks in BCI Meta-Analysis
Search Strategy and Study Selection
Recent high-quality meta-analyses employed comprehensive, systematic search strategies across multiple electronic databases. The typical approach includes:
- Database Coverage: PubMed/MEDLINE, Web of Science, Scopus, Cochrane Central Register of Controlled Trials, Embase, and regional databases (CNKI, Wanfang, VIP for Chinese literature) [10] [109].
- Search Timeframe: From database inception through February/April 2025, with regular updates until the final analysis date [10].
- Boolean Search Logic: Complex query structures combining terms:
("brain-computer interface" OR BCI OR "brain-machine interface") AND ("spinal cord injury" OR stroke) AND ("rehabilitation" OR "recovery")with field-specific adaptations [10] [109].
The study selection process follows the PRISMA guidelines with a predefined PICOS framework:
- Participants: Spinal cord injury patients or stroke survivors with motor impairment
- Interventions: Non-invasive BCI systems, often combined with adjunctive therapies (FES, tDCS)
- Comparators: Conventional therapy, sham stimulation, or other active interventions
- Outcomes: Standardized functional measures (FMA-UE, ASIA scores, SCIM)
- Study Design: Randomized controlled trials or self-controlled trials
Quality Assessment and Statistical Analysis
Methodological quality assessment utilizes Cochrane Risk of Bias tool for randomized trials, evaluating sequence generation, allocation concealment, blinding, incomplete outcome data, selective reporting, and other potential biases [10].
Statistical methodologies in recent meta-analyses include:
- Effect Size Calculation: Standardized mean differences (Hedges' g) for continuous outcomes with 95% confidence intervals
- Heterogeneity Quantification: I² statistic with random-effects models preferred when I² > 50%
- Network Meta-Analysis: Bayesian framework using gemtc package in R, evaluating consistency between direct and indirect evidence
- Publication Bias Assessment: Funnel plot symmetry tests and Egger's regression test
- Evidence Quality Grading: GRADE framework evaluating risk of bias, inconsistency, indirectness, imprecision, and publication bias
Figure 1: Methodological Workflow for BCI Meta-Analysis
Technical Implementation & Signaling Pathways
Non-Invasive BCI Modalities and Mechanisms
Non-invasive BCIs utilize various signal acquisition technologies, each with distinct operating principles and clinical applications:
- Electroencephalography (EEG): Measures electrical activity from scalp surface using electrodes (wet or dry). Provides excellent temporal resolution but limited spatial resolution [8] [6].
- Functional Near-Infrared Spectroscopy (fNIRS): Uses light to detect hemodynamic responses correlated with neural activity. Better spatial resolution than EEG but slower temporal response [8].
- Magnetoencephalography (MEG): Detects magnetic fields generated by neural currents. Offers high spatiotemporal resolution but requires shielded environments [8].
The therapeutic mechanism of non-invasive BCIs in neurological rehabilitation involves creating closed-loop feedback systems that promote targeted neuroplasticity. When integrated with functional electrical stimulation (FES) or other adjunctive therapies, these systems establish complete sensorimotor loops that reinforce damaged neural pathways [109].
Figure 2: BCI-Mediated Therapeutic Pathway for Neurological Recovery
Table 3: Essential Research Resources for Non-Invasive BCI Implementation
| Resource Category | Specific Examples | Research Application & Function |
|---|---|---|
| Signal Acquisition | Dry EEG electrodes, fNIRS optodes, MEG magnetometers | Neural signal capture with varying spatiotemporal resolution and invasiveness tradeoffs [8] |
| Data Processing Platforms | EEGLAB, FieldTrip, MNE-Python, BCI2000 | Signal preprocessing, feature extraction, and classification pipeline implementation [62] |
| Stimulator Systems | Functional electrical stimulation (FES), transcranial direct current stimulation (tDCS) | Effector mechanisms for closed-loop intervention and neuromodulation [109] |
| Outcome Assessment | Fugl-Meyer Assessment (FMA), ASIA Impairment Scale, Spinal Cord Independence Measure (SCIM) | Standardized quantification of functional recovery across motor, sensory, and daily living domains [10] [109] |
| Statistical Analysis | R Statistics, Stata, Bayesian frameworks (gemtc) | Meta-analytic synthesis, network analysis, and evidence quality grading [10] [109] |
Discussion and Clinical Translation
Efficacy Patterns and Moderating Factors
The quantitative synthesis of evidence reveals consistent positive effects of non-invasive BCIs across neurological conditions, with effect sizes generally in the moderate to large range (SMD 0.72-0.95) [10]. Subgroup analyses from recent meta-analyses indicate potentially stronger effects in subacute versus chronic stages of spinal cord injury, suggesting a critical window for intervention [10]. This temporal pattern aligns with known neuroplasticity mechanisms, where the brain demonstrates heightened adaptability in early recovery phases.
For stroke rehabilitation, the superior ranking of combined BCI-FES with tDCS (SUCRA = 98.9) suggests synergistic effects between different neuromodulation approaches [109]. This multimodal effect likely arises from simultaneous targeting of peripheral neuromuscular pathways (via FES) and central cortical excitability (via tDCS), while BCI provides intention-driven closed-loop integration.
Limitations and Evidence Gaps
Despite promising results, significant limitations temper clinical translation:
- Evidence Quality: Most domains show low to moderate quality evidence according to GRADE framework, with limited high-quality RCTs [10].
- Methodological Heterogeneity: Varied BCI paradigms, stimulation parameters, and outcome measures complicate cross-study comparisons.
- Sample Size Limitations: Many studies include small participant cohorts (total n=109 across 9 studies in SCI meta-analysis) [10].
- Long-Term Effects: Limited data on durability of benefits beyond immediate post-intervention period.
Recent analyses explicitly caution against immediate clinical application, instead characterizing findings as "preliminary and hypothetical" until validated by larger RCTs [10].
The meta-analytic evidence synthesized in this review demonstrates consistent, positive effects of non-invasive BCIs for neurological rehabilitation, with moderate to large effect sizes across functional domains. The highest efficacy appears associated with multimodal approaches that combine BCI with complementary interventions like FES and tDCS, particularly when implemented during subacute recovery phases.
While these findings support continued investment and investigation in non-invasive BCI technologies, the current evidence base remains insufficient for widespread clinical implementation. Future research priorities should include standardized protocols, larger multicenter trials, longer-term follow-up assessments, and individualized parameter optimization to advance non-invasive BCIs from promising investigational tools to established clinical therapeutics.
In non-invasive Brain-Computer Interface (BCI) research, quantitative performance metrics are essential for evaluating system efficacy, comparing technological approaches, and guiding clinical translation. Information Transfer Rate (ITR), measured in bits per minute (bit/min or bpm), and Classification Accuracy, expressed as a percentage, serve as the two paramount benchmarks for assessing BCI performance [41]. ITR comprehensively captures the speed, accuracy, and number of available classes in a single value, providing a measure of communication bandwidth, while classification accuracy reflects the system's fundamental reliability in interpreting user intent [3] [41]. The optimization of these metrics is a central focus in BCI development, driving advancements in signal acquisition hardware, processing algorithms, and experimental paradigms [3] [2]. This document provides an in-depth technical examination of these core metrics, their interrelationship, state-of-the-art values, and the methodological frameworks used to achieve them.
Defining the Core Metrics
Classification Accuracy
Classification accuracy is the most immediate measure of BCI performance, representing the proportion of correct classifications made by the system over a given number of trials.
- Definition: It is calculated as the ratio of correctly classified trials to the total number of trials. For multi-class paradigms, this is often extended to the overall accuracy across all classes.
- Significance: High accuracy is critical for user acceptance and practical application, as frequent errors can lead to user frustration and render a system unusable [41]. It is the foundational element upon which ITR is built.
- Technical Influences: Accuracy is heavily influenced by the quality of the recorded neural signal, the efficacy of signal processing and feature extraction methods (e.g., Common Spatial Patterns for motor imagery), and the choice of classification algorithm [110] [41].
Information Transfer Rate (ITR)
ITR, also known as Bit Rate, quantifies the amount of information communicated per unit time, typically bits per minute. It provides a more holistic view of system performance than accuracy alone by incorporating speed and the number of possible choices.
- Standard Formula (for a P300 Speller):
( B = \frac{{\log2 N + P \log2 P + (1-P) \log_2 (\frac{{1-P}}{{N-1}})}}{{}} ) × (60/T) bits/min
Where:
- ( N ) = Number of classes or targets
- ( P ) = Classification Accuracy (0 to 1)
- ( T ) = Time per selection (in seconds)
- Significance: ITR allows for direct comparison between different BCI paradigms (e.g., a 2-class motor imagery system vs. a 36-class P300 speller) [41]. It is the preferred metric for evaluating the practical utility of a BCI for communication or control tasks.
- Dependencies: ITR increases with higher accuracy, a greater number of classes, and a faster selection speed. However, these factors are often in tension; for example, increasing speed (( T )) can reduce accuracy (( P )), and a larger ( N ) can make classification more difficult.
State-of-the-Art Performance and Benchmarking
Performance varies significantly based on the BCI paradigm, the modality used, and the user's level of training. The following tables summarize reported performance metrics across different non-invasive BCI categories.
Table 1: Performance Metrics by BCI Paradigm
| BCI Paradigm | Reported Classification Accuracy | Reported ITR (bits/min) | Key Applications |
|---|---|---|---|
| P300 Speller | >85% [41] | Varies based on N and T | Communication, typing systems [106] [41] |
| Motor Imagery (MI) | Up to 96% with advanced ensemble methods [41] | Varies; highly user-dependent | Prosthetic control, neurorehabilitation [110] [41] |
| Steady-State Visually Evoked Potential (SSVEP) | High (often >90%) [106] | Can be among the highest for non-invasive BCIs [106] | High-speed control, selection tasks |
| Rapid Serial Visual Presentation (RSVP) | >85% symbol recognition [41] | Optimized for speed-accuracy balance [41] | High-speed typing, target identification |
Table 2: Performance by Signal Modality and User Group
| Modality / User Group | Typical Performance Range | Notable Advances & Challenges |
|---|---|---|
| EEG (General) | Wide range; from ~70% to >95% accuracy depending on paradigm and user [2] [41] | Portable and cost-effective. Suffers from low spatial resolution and signal-to-noise ratio [2]. |
| fNIRS | Moderate accuracy; slower ITR due to hemodynamic response lag [8] | More resistant to motion artifacts. Suitable for hybrid systems with EEG to improve robustness [41]. |
| MEG | High spatial and temporal resolution potential [41] | Used for non-invasive speech decoding. Limited by equipment complexity and cost [8] [41]. |
| Severely Motor-Impaired Users | Performance can be degraded due to "negative plasticity" [41] | A key translational challenge. Requires adaptive algorithms and personalized paradigms to maintain usability [41]. |
Experimental Protocols for High-Performance BCI
Achieving high ITR and accuracy requires a rigorously controlled experimental workflow, from data acquisition to the final output of a command.
Standardized Experimental Workflow
The following diagram outlines the universal processing pipeline for a non-invasive BCI system.
Detailed Methodological Breakdown
Signal Acquisition & Pre-processing:
- Acquisition: Neural signals are recorded using multi-channel devices. Research-grade EEG often uses 64 electrodes, while commercial systems may use fewer (e.g., 14 in Emotiv EPOC+) to reduce setup burden [106] [41]. EEG signals are characterized by specific frequency bands (delta, theta, alpha, beta, gamma) and event-related potentials (P300, SSVEPs) [41].
- Pre-processing: This critical step improves the signal-to-noise ratio. It involves:
- Amplification: EEG signals (≈100 µV) are amplified by approximately 10,000x [41].
- Filtering: Band-pass filtering isolates relevant frequency bands, and notch filtering removes power line interference.
- Artifact Removal: Advanced methods like Independent Component Analysis (ICA) are used to separate and remove artifacts from eye movements (EOG) and muscles (EMG) [41].
Feature Extraction & Classification:
- Feature Extraction: Informative features are distilled from the pre-processed signals. For Motor Imagery BCIs, Common Spatial Pattern (CSP) is a potent and widely used algorithm that maximizes the variance between two classes [110]. The optimization problem is formulated as: ( \operatorname{argmax}w \frac{w^\top C1 w}{w^\top (C1+C2) w} ), where ( C1 ) and ( C2 ) are the covariance matrices of the two classes [41]. Other methods include time-frequency decomposition using wavelet transforms.
- Classification: Machine learning models map the extracted features to control commands. Linear Discriminant Analysis (LDA) and Support Vector Machines (SVM) are widely used [110]. Deep learning approaches, including Convolutional Neural Networks (CNNs) like EEGNet, are increasingly employed for their ability to learn complex features directly from data [41]. Ensemble methods (e.g., LSTM-CNN-Random Forest hybrids) have demonstrated accuracies as high as 96% in complex tasks like prosthetic arm control [41].
Adaptation and Real-Time Processing:
- A key challenge is the non-stationary nature of EEG signals. Adaptive algorithms and transfer learning strategies are used to address signal variability over time and across users, reducing the need for frequent and lengthy user-specific calibration [41]. Reinforcement learning agents that utilize error-related potentials as feedback are an emerging solution for online adaptation [41].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Solutions for BCI Experimentation
| Item / Solution | Function in BCI Research | Technical Notes |
|---|---|---|
| High-Density EEG Systems | Primary data acquisition for electrical brain activity. | 64+ channels common in research [106] [41]. Provides high temporal resolution essential for capturing rapid neural dynamics [106]. |
| Dry Electrodes | Enable faster set-up and improve user comfort compared to traditional wet (gel) electrodes. | A key innovation for consumer and long-term use; material biocompatibility and signal quality are active research areas [8]. |
| Electrode Caps (10-20 System) | Standardized placement of EEG electrodes on the scalp. | Ensures consistent positioning across subjects and sessions; letters (F, C, P, O, T) denote brain areas, numbers denote lateralization [106]. |
| fNIRS Hardware | Measures hemodynamic responses via near-infrared light for an alternative neural signal source. | Offers moderate spatial resolution and is less susceptible to motion artifacts, making it suitable for hybrid EEG+fNIRS systems [8] [41]. |
| Open-Source BCI Toolboxes | Provide standardized pipelines for data processing, feature extraction, and classification. | Crucial for reproducibility and accelerating research. Examples include toolboxes for EEG processing and BCI experiment control [3]. |
| ICA Algorithm Software | Statistically separates neural signals from artifacts (e.g., eye blinks, muscle activity). | A critical pre-processing step for improving the signal-to-noise ratio before feature extraction [41]. |
| Common Spatial Pattern (CSP) Code | Extracts discriminative spatial features for Motor Imagery paradigms. | A cornerstone algorithm for MI-BCI; many optimized and regularized variants exist [110] [41]. |
| Deep Learning Frameworks | Enable the implementation of complex models like EEGNet, CNNs, and LSTMs for classification. | Used to push the boundaries of decoding accuracy from complex, high-dimensional neural data [41]. |
Brain-Computer Interfaces (BCIs) represent a transformative technology that establishes a direct communication pathway between the brain and external devices, bypassing conventional neuromuscular channels [2]. This field is fundamentally divided into two methodological approaches: invasive interfaces, which require surgical implantation of electrodes directly onto or into the brain tissue, and non-invasive interfaces, which record neural signals from outside the skull [8] [6]. For researchers and drug development professionals, understanding this dichotomy is crucial for designing appropriate studies and evaluating therapeutic applications.
The central challenge in BCI development has been the inherent trade-off between signal fidelity and practical accessibility. Invasive BCIs provide high-resolution data but carry surgical risks and are limited to small patient populations. Non-invasive BCIs offer greater safety and accessibility but historically suffered from inferior signal quality due to signal attenuation by the skull and scalp [2] [41]. However, recent advancements in sensor technology, signal processing algorithms, and artificial intelligence are rapidly bridging this performance gap, opening new possibilities for both clinical applications and basic neuroscience research.
Fundamental Technical Divergences
The core distinction between invasive and non-invasive methods stems from their physical relationship to neural tissue and the resulting implications for signal acquisition.
Invasive BCI Approaches
Invasive interfaces are characterized by their direct contact with the brain, typically involving microelectrode arrays implanted into the cortex. These systems record action potentials and local field potentials with high spatial and temporal resolution, providing rich datasets for decoding neural intent [6] [62].
- Surgical Implementation: Traditional approaches like the Utah Array require craniotomy for implantation, which can trigger immune responses, scarring, and inflammation—a limitation quantified by the "butcher ratio" (neurons killed relative to those recorded from) [6].
- Novel Form Factors: Recent innovations aim to minimize tissue damage. Precision Neuroscience's "Layer 7" array is designed to be minimally invasive, resting on the cortical surface, while Synchron's Stentrode takes an endovascular approach, delivered via blood vessels [38] [62].
Non-Invasive BCI Approaches
Non-invasive techniques acquire signals through the skull, eliminating surgical risk but introducing signal degradation. The electrical conductivity of the skull (approximately 0.01–0.02 S/m) is an order of magnitude lower than that of the scalp (0.1-0.3 S/m), resulting in significant signal attenuation—particularly for low-frequency components like Delta and Theta waves [70].
Primary non-invasive modalities include:
- Electroencephalography (EEG): Measures electrical activity via scalp electrodes with high temporal resolution but limited spatial resolution [2] [41].
- Functional Near-Infrared Spectroscopy (fNIRS): Uses light to measure hemodynamic responses correlated with neural activity, offering moderate spatial and temporal resolution [8] [41].
- Magnetoencephalography (MEG): Detects magnetic fields associated with neuronal currents, providing high resolution but typically requiring bulky, shielded environments [8] [41].
Table 1: Comparative Analysis of BCI Signal Acquisition Modalities
| Modality | Spatial Resolution | Temporal Resolution | Invasiveness | Key Advantages | Primary Limitations |
|---|---|---|---|---|---|
| Invasive (ECoG/Arrays) | ~1 mm | ~1 ms | High (Surgical implantation) | High signal-to-noise ratio, Broad bandwidth | Surgical risks, Tissue response, Limited long-term stability |
| EEG | ~10 mm | ~10-100 ms | Non-invasive | Portable, Cost-effective, High temporal resolution | Signal attenuation through skull, Sensitive to artifacts |
| fNIRS | ~5-10 mm | ~1-5 seconds | Non-invasive | Less sensitive to artifacts, Tolerates some movement | Indirect measure (hemodynamic), Lower temporal resolution |
| MEG | ~2-3 mm | ~1 ms | Non-invasive | High spatial & temporal resolution | Expensive, Bulky equipment requiring shielding |
Quantitative Performance Benchmarks
The performance gap between invasive and non-invasive approaches can be quantified across multiple dimensions, including information transfer rates (ITR), decoding accuracy, and clinical outcomes.
Communication and Control Performance
Invasive systems currently demonstrate superior performance for complex control tasks. Blackrock Neurotech has achieved typing speeds of 90 characters per minute through direct neural decoding [38]. Speech decoding from cortical signals has reached remarkable accuracy levels of 99% with latencies under 0.25 seconds in research settings [62].
Non-invasive systems have traditionally lagged in performance, particularly for continuous control applications. However, recent innovations are substantially narrowing this gap. A 2025 UCLA study incorporating an AI copilot with a 64-channel EEG cap demonstrated a 3.9-fold performance improvement in cursor and robotic arm control tasks for a paralyzed participant with a T5 spinal cord injury [111]. The study critically reported that the participant could not complete the tasks without AI assistance, highlighting the transformative potential of hybrid intelligence systems.
Clinical Efficacy Metrics
Recent meta-analyses have quantified the therapeutic potential of non-invasive BCIs for neurological conditions. A systematic review of 9 studies involving 109 spinal cord injury patients found significant effect sizes for non-invasive BCI interventions across multiple functional domains [10]:
- Motor function: SMD = 0.72, 95% CI: [0.35,1.09], P < 0.01
- Sensory function: SMD = 0.95, 95% CI: [0.43,1.48], P < 0.01
- Activities of daily living: SMD = 0.85, 95% CI: [0.46,1.24], P < 0.01
Subgroup analyses revealed stronger effects in subacute versus chronic spinal cord injury patients, suggesting intervention timing may influence outcomes [10]. While promising, the review authors noted these conclusions remain preliminary due to limited sample sizes and recommended larger randomized controlled trials before widespread clinical adoption.
Table 2: Market Forecast and Adoption Trends for BCI Technologies
| Metric | Non-Invasive BCI | Invasive BCI | Overall BCI Market |
|---|---|---|---|
| 2024 Market Size | Component of overall $2.87B BCI market [38] | Component of overall $2.87B BCI market [38] | $2.87 billion [38] |
| Projected 2035 Market Size | Significant component of projected growth | Smaller revenue share but high impact | $15.14 billion [38] |
| CAGR (2025-2035) | 9.35% (estimated for non-invasive segment) [111] | 1.49% (estimated for invasive segment) [111] | 16.32% [38] |
| Forecasted 2045 Revenue | Expected to comprise majority share | Smaller but growing segment | >$1.6 billion [8] |
| Primary Adoption Drivers | Safety, Accessibility, Consumer applications, Neurorehabilitation | Medical necessity for severe disabilities, High-fidelity control | Increasing neurological disorders, Aging population, Technological advances |
Technological Innovations Narrowing the Gap
Advanced Signal Processing and AI Integration
Modern machine learning approaches are dramatically enhancing non-invasive BCI capabilities. The UCLA team implemented a convolutional neural network-Kalman filter (CNN-KF) architecture that significantly improves real-time decoding of noisy EEG data [111]. This hybrid approach combines CNN's feature extraction capabilities with Kalman filtering's strength in estimating unknown variables from noisy time-series data.
Other innovative algorithms include:
- Adaptive Transfer Learning: Frameworks like SSVEP-DAN (Domain Adaptation Network) transform source user data to new user templates, substantially reducing calibration requirements [41].
- Multimodal Data Fusion: Hybrid systems integrating complementary modalities (e.g., EEG + fNIRS) demonstrate improved decoding performance and robustness compared to unimodal approaches [41].
- Ensemble Methods: Architectures like LSTM-CNN-RF (Long Short-Term Memory - Convolutional Neural Network - Random Forest) ensembles have achieved 96% accuracy in complex decoding tasks [41].
Novel Sensing Modalities
Breakthroughs in sensor technology are enabling higher-resolution non-invasive neural recording. Researchers at Johns Hopkins APL have developed a Digital Holographic Imaging (DHI) system that detects nanometer-scale tissue deformations occurring during neural activity [9]. This approach represents a fundamentally new signal acquisition method that could potentially overcome limitations of traditional modalities.
Flexible Brain Electronic Sensors (FBES) represent another frontier, with materials innovations enabling:
- Enhanced biocompatibility and conformal contact with scalp or brain tissue
- Improved signal-to-noise ratios through better skin-sensor coupling
- Multidimensional, multilevel physiological signal monitoring [70]
Recent investigations into alternative signal acquisition pathways include in-ear EEG sensors that leverage proximity to the central nervous system via the cochlea, with one study demonstrating 95% offline accuracy for SSVEP classification [70].
Experimental Protocols and Methodologies
Protocol: AI-Enhanced Non-Invasive BCI for Motor Control
This protocol is adapted from the UCLA study demonstrating significant performance improvements in non-invasive BCI control [111].
Research Objective: To evaluate the efficacy of an AI copilot system in enhancing non-invasive BCI performance for continuous control tasks.
Participant Selection:
- Include both healthy participants and individuals with relevant neurological conditions (e.g., spinal cord injury)
- Sample size: 3 healthy participants + 1 paraplegic participant (as reported in foundational study)
Equipment and Reagents:
- 64-channel EEG cap with conductive gel or dry electrodes
- Signal amplification system with sampling rate ≥256 Hz
- Data acquisition system with real-time processing capability
- Robotic arm or cursor control interface
- AI processing unit with CNN-Kalman Filter implementation
Experimental Procedure:
- EEG Setup: Apply EEG cap according to 10-20 international system, ensuring impedance <5 kΩ for all electrodes.
- Calibration Phase: Record 5 minutes of resting-state activity followed 10 minutes of motor imagery tasks for decoder calibration.
- Task Paradigm: Implement center-out reaching tasks where participants mentally control cursor movement toward visual targets.
- AI Integration: Deploy CNN-KF architecture for continuous decoding of movement intention and trajectory.
- Copilot Assistance: Implement AI copilot to interpret user intent and refine executed commands based on task context.
- Performance Assessment: Quantify success rate, path efficiency, and completion time across multiple trials with and without AI assistance.
Data Analysis:
- Compare task performance metrics between AI-assisted and unassisted conditions
- Compute information transfer rate (ITR) using standard formulae
- Perform statistical analysis (e.g., paired t-tests) to determine significance of AI enhancement
Protocol: Digital Holographic Imaging for Non-Invasive Neural Recording
This protocol outlines the methodology for the Johns Hopkins APL breakthrough in non-invasive neural signal detection [9].
Research Objective: To validate neural tissue deformation as a novel signal for non-invasive high-resolution brain activity recording.
Equipment:
- Digital Holographic Imaging (DHI) system with laser illumination source
- High-sensitivity camera capable of detecting nanometer-scale displacements
- Vibration isolation table
- Animal preparation setup (for initial validation studies)
- Signal processing unit for resolving physiological clutter (blood flow, heart rate, respiration)
Experimental Workflow:
- System Calibration: Align DHI system and validate nanometer-scale displacement sensitivity using reference materials.
- Signal Isolation: Implement advanced filtering algorithms to distinguish neural signals from physiological clutter.
- Validation: Correlate tissue deformation signals with simultaneous direct neural recordings (in animal models) or with behavioral outputs.
- Signal Processing: Apply recursive estimation methods to extract neural activity patterns from complex background interference.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Reagents for Advanced BCI Research
| Item | Specifications | Research Function | Example Applications |
|---|---|---|---|
| Dry EEG Electrodes | Flexible, non-gel contacts with high conductivity materials (e.g., graphene, polymer composites) | Enable long-term monitoring without skin irritation | Consumer neurotechnology, Ambulatory monitoring, Longitudinal studies |
| fNIRS Optodes | Near-infrared light sources (690-850 nm) and detectors with specific spacing (25-35 mm) | Measure hemodynamic responses through neurovascular coupling | Cognitive state monitoring, Motor imagery paradigms, Clinical rehabilitation |
| Flexible Brain Electronic Sensors (FBES) | Conformable substrates with integrated electrode arrays, stretchable conductors | Improve skin-contact interface for enhanced signal quality | Wearable BCI, Continuous health monitoring, Electronic skin applications |
| Utah Array & Derivatives | 100-1000+ microelectrodes on rigid or flexible substrates | High-resolution neural recording for invasive applications | Basic neuroscience, Motor decoding, Speech neuroprosthetics |
| CNN-Kalman Filter Algorithm | Custom software implementation for real-time signal processing | Decode noisy neural signals and predict intended movements | AI-enhanced BCI, Robotic arm control, Cursor navigation |
| Digital Holographic Imaging System | Laser illumination with nanometer-scale displacement detection | Novel non-invasive detection of neural tissue deformations | Fundamental signal validation, Next-generation non-invasive BCI |
The distinction between invasive and non-invasive BCI technologies is becoming increasingly nuanced as innovations in materials science, artificial intelligence, and sensor design progressively bridge the historical performance gap. For the research community, several promising directions emerge:
Multimodal Integration: Combining complementary sensing modalities (e.g., EEG + fNIRS + eye tracking) offers synergistic benefits for robust neural decoding [8] [41]. This approach leverages the temporal resolution of EEG with the spatial advantages of other modalities.
Adaptive Brain-Computer Interfaces: Systems that continuously learn and adapt to individual users' changing neural patterns can maintain performance over extended periods without recalibration [41]. Reinforcement learning approaches using error-related potentials as feedback signals represent a particularly promising avenue.
Biocompatible Materials Development: Advances in flexible, biocompatible materials are critical for both minimally invasive implants and high-performance non-invasive sensors [70]. Solutions that overcome the skull barrier without penetration remain a primary challenge.
Ethical and Privacy-Preserving BCI: As neural interfaces advance, protecting sensitive brain data becomes paramount. Perturbation-based algorithms that mask private information while preserving utility represent an emerging research frontier [41].
The trajectory of BCI development suggests a future where non-invasive systems may achieve performance levels once exclusive to invasive approaches, particularly for applications beyond severe disabilities. The overall BCI market is forecast to grow to over $1.6 billion by 2045, with non-invasive technologies capturing an increasing share [8]. For researchers and clinical professionals, this evolving landscape presents unprecedented opportunities to develop transformative neurotechnologies that balance performance with practicality, ultimately expanding access to brain-computer communication.
Comparative Analysis of EEG, fNIRS, and MEG for Specific Applications
Non-invasive Brain-Computer Interfaces (BCIs) and neuroimaging techniques are revolutionizing neuroscience research and clinical practice. Electroencephalography (EEG), functional Near-Infrared Spectroscopy (fNIRS), and Magnetoencephalography (MEG) stand as the three primary non-invasive modalities for measuring brain activity, each with distinct operational principles and performance characteristics. The convergence of these technologies is creating powerful multimodal tools for a more comprehensive understanding of brain function, crucial for applications ranging from drug development to the diagnosis of neurological and psychiatric disorders. This whitepaper provides a comparative analysis of EEG, fNIRS, and MEG, detailing their technical specifications, experimental protocols, and synergistic potential within a non-invasive BCI framework. The selection of an appropriate neuroimaging modality—or a combination thereof—is paramount for researchers and drug development professionals aiming to precisely identify biomarkers, evaluate treatment efficacy, and elucidate underlying circuit deficits [77] [112].
Technical Specifications and Performance Benchmarking
The core technologies of EEG, fNIRS, and MEG measure fundamentally different physiological phenomena: electrical potentials, hemodynamic responses, and magnetic fields, respectively.
- EEG records the brain's electrical activity from the scalp surface, resulting from the summed post-synaptic potentials of neurons. It offers millisecond-level temporal resolution, allowing it to track the rapid dynamics of brain function. However, its spatial resolution is limited (approximately 2 cm) because the electrical signals are attenuated and blurred as they pass through the skull and other tissues [77] [113].
- fNIRS measures hemodynamic changes by detecting light attenuation in the brain tissue. It tracks concentration changes in oxygenated (HbO) and deoxygenated hemoglobin (HbR), providing an indirect measure of neural activity with a spatial resolution superior to EEG. Its temporal resolution is limited by the slow hemodynamic response, occurring over seconds [77] [114].
- MEG captures the magnetic fields generated by intraneuronal electrical currents. These fields are largely undistorted by the skull and scalp. Traditional MEG systems use Superconducting Quantum Interference Devices (SQUIDs) requiring cryogenic cooling. A newer technology, Optically Pumped Magnetometer (OPM)-MEG, uses laser-pumped quantum sensors that operate at room or body temperature, enabling more flexible, on-scalp configurations that enhance signal strength [115] [112].
Table 1: Technical Benchmarking of Non-Invasive Neuroimaging Modalities
| Parameter | EEG | fNIRS | SQUID-MEG | OPM-MEG |
|---|---|---|---|---|
| Measured Signal | Electrical potentials on scalp [77] | Hemodynamic (HbO/HbR) changes [77] | Magnetic fields from intraneuronal currents [112] | Magnetic fields from intraneuronal currents [112] |
| Temporal Resolution | Excellent (Milliseconds) [77] [113] | Poor (Seconds) [77] | Excellent (Milliseconds) [112] | Excellent (Milliseconds) [112] |
| Spatial Resolution | Low (~2 cm) [113] | Fair (Superior to EEG) [77] | Good [77] | Better than SQUID-MEG [112] |
| Invasiveness | Non-invasive | Non-invasive | Non-invasive | Non-invasive |
| Tolerance to Movement | Moderate | Moderate | Low (requires immobilization) [112] | High (movement-tolerant) [112] |
| Portability & Cost | High portability, low cost [77] | High portability, relatively low cost [77] [113] | Low portability, very high cost [77] | Emerging, potential for better portability and lower cost than SQUID-MEG [112] |
| Key Advantage | Direct neural electrical activity, high temporal resolution, low cost | Direct hemodynamic response, good spatial resolution, portable | Excellent spatiotemporal resolution, signals unaffected by tissue [112] | Superior signal strength, flexible sensor placement, no cryogenics [115] [112] |
| Key Limitation | Low spatial resolution, sensitive to artifacts | Low temporal resolution, measures indirect neural activity | High cost, bulky, restricts movement [112] | New technology, can be sensitive to external magnetic fields [112] |
Experimental Protocols and Methodologies
A critical application of these technologies is in developing robust BCIs. The following outlines a standard protocol for a multimodal experiment, such as one investigating semantic decoding or motor imagery.
Multimodal BCI Experimental Workflow
The diagram below illustrates the generalized workflow for a simultaneous EEG-fNIRS-MEG experiment, from setup to data fusion.
Detailed Protocol: Semantic Decoding with EEG-fNIRS
This protocol is adapted from a study investigating the decoding of imagined semantic categories (animals vs. tools) using simultaneous EEG-fNIRS [113].
- Participants: Recruit right-handed native speakers to control for language-related variability. Ensure normal or corrected-to-normal vision. Obtain informed consent.
- Stimuli: Prepare a set of images representing the target semantic categories (e.g., 18 animals and 18 tools). Images should be standardized (e.g., grayscaled, uniform size, white background) [113].
- Mental Tasks:
- Silent Naming: Participants silently name the displayed object in their mind.
- Visual Imagery: Participants visualize the object in their mind.
- Auditory Imagery: Participants imagine the sounds associated with the object.
- Tactile Imagery: Participants imagine the feeling of touching the object.
- Each task should be performed for a fixed duration (e.g., 3-5 seconds) following a visual cue, with randomized order across blocks [113].
- Data Acquisition:
- EEG: Record using a standard electrode cap (e.g., 29 positions based on the 10-20 system). Impedance should be kept below 5 kΩ [116] [113].
- fNIRS: Integrate optodes (sources and detectors) into the same cap as the EEG electrodes. Precise scalp localization and consistent optode-scalp coupling are critical [77] [113].
- Synchronization: Use a unified processor to acquire EEG and fNIRS signals simultaneously, ensuring precise temporal alignment [77].
- Data Analysis:
- Preprocessing: For EEG, apply band-pass filtering and artifact removal (e.g., for eye blinks). For fNIRS, convert raw light intensity into HbO and HbR concentration changes using the Modified Beer-Lambert Law [77] [117].
- Feature Extraction: Extract multi-domain features. For EEG, this includes time-domain (e.g., ERPs), frequency-domain (e.g., band powers), and time-frequency features. For fNIRS, features include mean, peak, slope, and variance of HbO/HbR trajectories [117].
- Fusion and Classification: Employ a multi-level progressive learning framework. First, select optimal features using an algorithm like Atomic Search Optimization. Then, fuse the selected EEG and fNIRS features and feed them into a classifier (e.g., Support Vector Machine). This approach has achieved classification accuracies over 96% for motor imagery and mental arithmetic tasks [117].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Materials and Equipment for Multimodal BCI Research
| Item | Function / Description | Example Application in Protocol |
|---|---|---|
| EEG Electrode Cap | A headcap with integrated electrodes (Ag/AgCl) for recording electrical activity from standard scalp positions (10-20 system). | Recording electrical brain activity during mental tasks. Integrated caps with pre-cut holes for fNIRS optodes are available [77]. |
| fNIRS Optodes | Sources (laser diodes or LEDs) that emit near-infrared light and detectors (photodiodes) that measure light intensity after tissue penetration. | Measuring hemodynamic changes in the cortex by placing optodes over regions of interest (e.g., prefrontal cortex for executive function) [77] [113]. |
| OPM-MEG Sensors | Compact, room-temperature quantum sensors containing a vapor cell (e.g., Rubidium) that measures magnetic fields. Replaces bulky SQUID sensors. | Flexible, on-scalp MEG recording that is tolerant to head movement, ideal for pediatric or clinical populations [115] [112]. |
| Data Acquisition System | A central microcontroller that amplifies analog signals, performs analog-to-digital conversion, and synchronizes data streams from multiple modalities. | Simultaneously acquiring and digitizing EEG and fNIRS signals with high temporal precision for later fusion [77]. |
| Customized Helmets | 3D-printed or thermoplastic helmets molded to an individual's head shape. | Ensuring consistent and optimal placement of and pressure on both EEG electrodes and fNIRS optodes, improving data quality and reproducibility [77]. |
| Stimulus Presentation Software | Software (e.g., PsychoPy, Presentation) to display visual/auditory cues and record participant responses with precise timing. | Presenting the sequence of images (animals/tools) and task instructions to the participant in a controlled manner [113]. |
Application-Specific Modality Selection and Fusion Strategies
The choice of modality is dictated by the specific research question. The complementary nature of these signals makes their fusion particularly powerful.
- EEG-dominated Applications: Ideal for investigating high-speed neural dynamics, such as detecting Event-Related Potentials (ERPs) like the P300 for matrix spellers, monitoring sleep stages, or tracking seizure activity in epilepsy with high temporal precision [2] [116].
- fNIRS-dominated Applications: Excellent for long-term, portable monitoring in naturalistic settings. It is well-suited for studying brain function in populations that find fMRI/MEG challenging (e.g., infants, patients with movement disorders) and for tasks where EEG artifacts are unavoidable [77].
- MEG-dominated Applications: Superior for precise source localization of neural activity, such as pinpointing the epileptogenic focus in pre-surgical epilepsy evaluation or studying the functional organization of the sensory and motor cortices. OPM-MEG is particularly promising for mapping deep brain structures like the hippocampus [116] [112].
- Multimodal Fusion: Combining modalities overcomes individual limitations. For instance, EEG's poor spatial resolution is compensated by fNIRS or MEG. Conversely, fNIRS's slow hemodynamic response can be complemented by EEG's millisecond precision. Studies consistently show that multimodal systems (EEG-fNIRS, MEG-EEG) achieve significantly higher classification accuracy and robustness in BCI applications than any single modality alone [115] [117] [116]. A 2022 study demonstrated that a fusion of EEG and fNIRS using multi-domain features and progressive machine learning achieved over 96% accuracy in classifying motor imagery, significantly outperforming unimodal approaches [117].
EEG, fNIRS, and MEG each offer a unique window into brain function, with trade-offs between temporal resolution, spatial resolution, and practical applicability. The future of non-invasive neuroimaging lies not in selecting a single superior technology, but in strategically combining these complementary modalities. The emergence of wearable technologies like OPM-MEG and integrated EEG-fNIRS systems is pushing the field toward more flexible, powerful, and clinically viable tools. For researchers and drug developers, this multimodal approach provides a more comprehensive platform for identifying neural biomarkers, understanding neurovascular coupling, validating therapeutic mechanisms of action, and ultimately developing next-generation BCIs for communication and rehabilitation.
Regulatory Landscape and FDA Clearance Pathways
The regulatory landscape for Brain-Computer Interface (BCI) technologies represents a critical framework for ensuring safety and efficacy as these innovative neurotechnologies transition from research laboratories to clinical and consumer applications. For researchers and development professionals, understanding the U.S. Food and Drug Administration (FDA) pathways is essential for successful translation of non-invasive BCI devices. These regulatory frameworks balance the need for rigorous safety assessment with the urgency of bringing transformative neurotechnologies to patients with neurological conditions. The FDA oversees neural-interface regulation primarily through the Center for Devices and Radiological Health (CDRH), which classifies devices based on risk level, invasiveness, and intended use [118].
Non-invasive BCIs, which typically utilize technologies such as electroencephalography (EEG), functional near-infrared spectroscopy (fNIRS), and magnetoencephalography (MEG), generally fall into lower risk categories compared to their invasive counterparts [8] [118]. This classification significantly impacts the regulatory pathway, with most non-invasive systems classified as Class II devices, while implantable BCIs typically fall into the Class III category [118]. The growing importance of non-invasive approaches is underscored by recent innovations in dry electrode technology and advanced signal processing algorithms that have substantially improved signal acquisition quality, making these systems increasingly viable for both medical and consumer applications [8] [119].
FDA Device Classification and Regulatory Pathways
Classification Framework
The FDA's medical device classification system is based on risk, with the level of regulatory control increasing with the potential risk to patients. For BCI technologies, this classification directly correlates with the device's invasiveness and intended use.
Table: FDA Device Classification for BCI Technologies
| Device Class | Risk Level | BCI Examples | Regulatory Controls |
|---|---|---|---|
| Class I | Low to Moderate | Basic research-use EEG headsets | General controls (e.g., labeling, manufacturing practices) |
| Class II | Moderate to High | Non-invasive EEG-based medical systems, diagnostic BCIs | General controls and special controls (e.g., performance standards, post-market surveillance) |
| Class III | High | Implantable BCIs, cortical implants | General controls and premarket approval (PMA) requiring clinical evidence |
Approval Pathways for Non-Invasive BCI
For non-invasive BCI technologies targeting medical applications, three primary regulatory pathways exist:
510(k) Clearance - This pathway requires demonstration of substantial equivalence to an existing legally marketed predicate device [118]. For non-invasive BCI systems, this typically involves comparing technological characteristics with previously cleared EEG-based systems for neurodiagnostic monitoring or rehabilitation applications. The 510(k) pathway is generally efficient for incremental innovations in non-invasive BCI technology.
De Novo Classification - This route is available for novel, moderate-risk devices with no existing predicate [118]. The De Novo process provides a pathway to classify new types of non-invasive BCI systems that incorporate innovative sensing technologies or novel intended uses not previously cleared by the FDA. This pathway is particularly relevant for emerging non-invasive approaches such as wearable MEG and high-density fNIRS systems [8].
Investigational Device Exemption (IDE) - For clinical investigations aimed at collecting safety and effectiveness data for FDA review, an IDE allows the device to be used in a clinical study [118]. The IDE must be approved before beginning a study that will contribute to a Premarket Approval (PMA) or a PMA Supplement application.
Table: Documentational Requirements for FDA Submission
| Submission Type | Clinical Data Requirements | Technical Documentation | Typical Review Timeline |
|---|---|---|---|
| 510(k) | Typically not required; may include performance bench testing | Substantial equivalence comparison; electrical safety and electromagnetic compatibility data | 90 days |
| De Novo | May require limited clinical data for novel technologies | Description of novel technological features; risk analysis; performance testing | 120 days |
| PMA | Extensive clinical data from controlled investigations | Complete device description; manufacturing information; comprehensive bench testing | 180 days |
Experimental Protocols for BCI Validation
Clinical Validation Framework
Robust clinical validation is fundamental to regulatory approval for medical BCI devices. The following protocol outlines a standardized approach for evaluating the efficacy of non-invasive BCI systems for motor function rehabilitation in spinal cord injury (SCI) patients, based on recent systematic methodologies [10].
Study Design: A randomized controlled trial (RCT) or self-controlled trial design is recommended, with participants stratified by SCI severity using the American Spinal Injury Association (ASIA) Impairment Scale (grades A-E) [10].
Participant Selection:
- Inclusion Criteria: Diagnosed SCI patients (any severity level), stable medical condition, ≥3 months post-injury, and ability to provide informed consent.
- Exclusion Criteria: Severe cognitive impairment, uncontrolled epilepsy, significant head injury history, or contraindications for BCI use.
- Sample Size: Recent meta-analyses have included approximately 109 patients across multiple studies to achieve statistical power [10].
Intervention Protocol:
- BCI System Configuration: Non-invasive EEG-based system with minimum 16-channel setup, sampled at ≥250 Hz with appropriate impedance control (<50 kΩ).
- Session Parameters: Minimum 20 sessions, 45-60 minutes each, conducted 3-5 times weekly.
- Feedback Mechanism: Real-time visual or tactile feedback based on motor imagery decoding.
- Control Group: Receives conventional rehabilitation therapy or sham BCI training.
Outcome Measures and Assessment Schedule
Standardized outcome measures are critical for demonstrating clinical efficacy in regulatory submissions.
Table: Primary Outcome Measures for BCI Clinical Trials
| Functional Domain | Assessment Tool | Administration Time | Key Metrics |
|---|---|---|---|
| Motor Function | ASIA Motor Score [10] | Baseline, 4 weeks, 8 weeks, post-intervention | Upper Extremity Motor Score (UEMS), Lower Extremity Motor Score (LEMS) |
| Sensory Function | ASIA Sensory Score [10] | Baseline, 4 weeks, 8 weeks, post-intervention | Light touch, pinprick scores |
| Activities of Daily Living | Spinal Cord Independence Measure (SCIM) [10] | Baseline, post-intervention | Self-care, respiration, mobility |
| Manual Ability | Graded Redefined Assessment of Strength, Sensibility, and Prehension (GRASSP) [10] | Baseline, post-intervention | Strength, sensibility, prehension |
Data Analysis and Statistical Methods
Regulatory submissions require rigorous statistical analysis plans. For BCI trials, key considerations include:
- Primary Efficacy Analysis: Comparison of change scores from baseline to post-intervention between groups using analysis of covariance (ANCOVA) adjusting for baseline values.
- Subgroup Analyses: Stratification by injury characteristics (complete vs. incomplete SCI), injury level (cervical, thoracic), and time since injury (subacute vs. chronic) [10].
- Signal Processing Metrics: Evaluation of BCI performance including accuracy, information transfer rate (ITR), and signal-to-noise ratio (SNR) [119].
- Safety Analysis: Comprehensive reporting of all adverse events, with special attention to seizure incidence, skin irritation from electrodes, and fatigue-related issues.
Recent meta-analyses have demonstrated that non-invasive BCI interventions can significantly impact patients' motor function (SMD = 0.72, 95% CI: 0.35-1.09), sensory function (SMD = 0.95, 95% CI: 0.43-1.48), and activities of daily living (SMD = 0.85, 95% CI: 0.46-1.24) [10].
Regulatory Decision Pathway
The following workflow visualizes the key decision points in selecting and navigating the appropriate FDA regulatory pathway for a non-invasive BCI device.
Global Regulatory Considerations
While this guide focuses on FDA pathways, researchers developing non-invasive BCI technologies for global markets must consider international regulatory frameworks:
European Union (EU): Under the Medical Device Regulation (MDR) 2017/745, non-invasive BCI devices are typically classified as Class IIa or IIb [118]. Manufacturers must undergo assessment by a Notified Body and submit a Clinical Evaluation Report demonstrating conformity with general safety and performance requirements.
Asia-Pacific Regions:
- Japan (PMDA): Requires local testing and clinical evaluation for moderate to high-risk devices [118].
- China (NMPA): Demands clinical trials and local type testing before approval, with specific cybersecurity requirements for connected BCI devices [118].
- Australia (TGA): Conformity assessment required for all medical devices, with implantable systems facing stricter requirements [118].
Harmonized Standards: Compliance with international standards facilitates global market access. Key standards include:
- ISO 13485: Quality management systems for medical devices
- ISO 10993: Biological evaluation of medical devices (particularly relevant for wearable components)
- IEC 60601-1: Medical electrical equipment safety
- IEC 80601-2-78: Particular requirements for basic safety and essential performance of medical robots
The Scientist's Toolkit: Research Reagents and Materials
Successful BCI development and regulatory approval requires carefully selected research materials and methodologies. The following table outlines essential components for non-invasive BCI research systems.
Table: Essential Research Materials for Non-Invasive BCI Development
| Component Category | Specific Examples | Research Function | Regulatory Considerations |
|---|---|---|---|
| Electrode Technologies | Wet electrodes (Ag/AgCl), Dry electrodes, Multi-electrode arrays [8] | Neural signal acquisition with optimal signal-to-noise ratio | Biocompatibility testing (ISO 10993) for skin contact |
| Signal Acquisition Systems | EEG amplifiers, fNIRS detectors, MEG sensors [8] | Capture of electrophysiological signals or hemodynamic responses | Electrical safety certification (IEC 60601-1) |
| Signal Processing Algorithms | Machine learning classifiers, Deep neural networks, Filtering algorithms [119] | Decoding of neural signals into device commands | Algorithm validation documentation |
| Calibration Tools | Phantom heads, Signal simulators, Standardized tasks [119] | System calibration and performance verification | Traceable calibration standards |
| Data Management Systems | Secure databases, Encryption tools, Audit trails | Storage and management of neural data | HIPAA/GDPR compliance for data security |
Emerging Trends and Future Directions
The regulatory landscape for non-invasive BCI technologies continues to evolve in response to technological advancements:
Breakthrough Device Program: This FDA initiative provides expedited access to devices that provide more effective treatment or diagnosis of life-threatening or irreversibly debilitating conditions [118]. Certain non-invasive BCI technologies for severe neurological disorders may qualify for this program.
Software as a Medical Device (SaMD): As AI and machine learning components become more integral to BCI functionality, regulatory frameworks specifically addressing adaptive algorithms and locked vs. unlocked algorithms are emerging [118].
Digital Endpoints: Regulatory acceptance of novel digital biomarkers derived from BCI data is increasing, potentially accelerating clinical validation for certain indications [10].
Post-Market Surveillance Requirements: Following regulatory clearance, manufacturers must implement robust post-market surveillance systems including:
- Unique Device Identification (UDI) implementation
- Adverse event reporting
- Periodic Safety Update Reports (PSURs) in the EU
- Cybersecurity monitoring for connected systems [118]
The future regulatory landscape will likely see increased harmonization across international jurisdictions and the development of specialized frameworks for consumer-grade neurotechnologies that blur the line between medical devices and wellness products.
Standardization Challenges in BCI Research and Clinical Translation
Brain-Computer Interface (BCI) technology represents a revolutionary advancement in human-computer interaction, establishing a direct communication pathway between the brain and external devices [87]. As of 2025, BCI technology stands at a critical juncture, transitioning from laboratory research and clinical trials toward potential real-world applications and commercialization [62] [120]. This transition has exposed significant standardization challenges that impact every facet of BCI development, from basic research methodologies to clinical implementation and regulatory approval.
The fundamental operation of a BCI system involves a multi-stage pipeline: signal acquisition, processing and decoding, output generation, and feedback [62]. Each stage presents unique standardization hurdles that affect the reliability, reproducibility, and safety of BCI technologies. These challenges are particularly pronounced in non-invasive approaches, which face additional complications from signal degradation and external noise [2]. As the field progresses, establishing comprehensive standards has become essential for translating BCI technology from research laboratories into clinically viable applications that can improve patient outcomes in neurological disorders [121].
Core Standardization Challenges in BCI Development
Evaluation Methodology Inconsistencies
A fundamental challenge in BCI standardization is the lack of consistent evaluation methodologies across research and clinical domains. The discrepancy between offline model performance and online closed-loop operation represents a critical hurdle in assessing true BCI efficacy [87]. Offline analysis, while useful for preliminary algorithm development, fails to capture the dynamic interaction between the user and the system during real-time operation.
Comprehensive evaluation must extend beyond traditional metrics like classification accuracy and bit rate to include usability, user satisfaction, and functional efficacy [87]. These qualitative measures are essential for determining practical utility but resist easy standardization due to the highly individualized nature of BCI interaction. Furthermore, establishing standardized protocols for evaluating the medical efficacy of BCIs in treating neurological conditions requires rigorous evidence-based research and objective assessment criteria that are still under development [122].
Signal Acquisition and Data Quality Variability
The absence of standardized signal acquisition protocols introduces significant variability in data quality, complicating cross-study comparisons and technology transfer. Non-invasive techniques, particularly electroencephalography (EEG), face challenges with signal-to-noise ratio and susceptibility to artifacts from muscle movement, eye blinks, and environmental interference [2]. The table below summarizes key signal acquisition challenges across different BCI modalities:
Table 1: Signal Acquisition Challenges in Major BCI Modalities
| BCI Modality | Key Technical Challenges | Standardization Gaps |
|---|---|---|
| Scalp EEG | Signal attenuation by skull, low spatial resolution, sensitivity to artifacts | Electrode placement protocols, impedance standards, artifact rejection criteria |
| fNIRS | Indirect hemodynamic measurement, slow temporal response | Source-detector placement, physiological noise removal algorithms |
| Invasive ECoG | Surgical risk, long-term signal stability, biocompatibility | Biocompatibility testing protocols, signal stability metrics |
| Endovascular | Limited signal bandwidth, long-term vessel compatibility | Deployment procedures, signal quality validation |
The proliferation of different electrode technologies, including wet and dry electrodes, further complicates standardization efforts [8]. Each electrode type exhibits distinct electrical properties, signal stability characteristics, and susceptibility to noise, creating barriers to comparing results across studies and systems.
Decoding Algorithm and Performance Benchmarking
The lack of standardized benchmarking frameworks for BCI decoding algorithms presents another major challenge. While international BCI data competitions have attempted to address this issue, their focus has primarily been on offline analysis rather than closed-loop online performance [87]. The transition from offline analysis to online system implementation represents a "qualitative leap" that introduces numerous variables not captured in traditional benchmarking approaches.
Algorithm performance varies significantly across individuals and even within the same user across different sessions due to factors such as fatigue, attention fluctuations, and neural plasticity [120]. This variability necessitates user-specific calibration and adaptation mechanisms that resist standardization. Furthermore, the distributed and dynamic nature of neural representations means that even simple actions involve complex network interactions across multiple brain regions, complicating the development of universal decoding approaches [120].
Clinical Translation and Efficacy Assessment
The translation of BCI technology from research to clinical practice faces standardization hurdles in efficacy assessment and clinical validation. Unlike pharmaceutical interventions, BCI systems involve complex human-machine interactions that defy evaluation through traditional randomized controlled trials alone [122]. Establishing standardized endpoints and assessment timelines for BCI-mediated rehabilitation remains challenging due to the highly individualized nature of recovery trajectories.
The clinical translation pipeline requires standardization at multiple stages, including patient selection criteria, intervention protocols, outcome measures, and long-term efficacy assessment. Each neurological condition targeted by BCI therapy—such as stroke, spinal cord injury, or ALS—presents unique assessment challenges that necessitate condition-specific standardization approaches [121].
Standardized Experimental Protocols for BCI Research
Online Closed-Loop Evaluation Framework
To address the disconnect between offline analysis and real-world performance, a standardized framework for online closed-loop evaluation has been proposed as the "gold standard" for BCI validation [87]. This framework emphasizes the importance of real-time system operation with human-in-the-loop feedback, providing a more accurate assessment of practical BCI performance.
The protocol involves iterative cycles of online testing followed by offline analysis, with each cycle informing system improvements [87]. This approach captures the adaptive nature of BCI interaction, where both the user and the system co-adapt during learning and operation. Standardized metrics for online evaluation should include:
- Effectiveness: The accuracy and precision with which users can achieve specific goals
- Efficiency: The mental and physical resources expended to achieve these goals
- User Satisfaction: The subjective experience and acceptability of the system
The following workflow diagram illustrates the standardized protocol for online BCI system evaluation:
Cross-System Performance Benchmarking
Standardized benchmarking requires carefully designed experimental protocols that enable meaningful comparisons across different BCI systems and approaches. These protocols should control for variables such as user population characteristics, task complexity, feedback modalities, and training duration. Key elements of a standardized benchmarking protocol include:
- Participant stratification based on neurological status, age, and BCI experience
- Standardized tasks with multiple difficulty levels to assess performance scalability
- Fixed training schedules with predetermined session durations and intervals
- Control conditions to account for learning effects and non-BCI factors
- Multi-dimensional assessment including performance metrics, user experience measures, and physiological indicators
The implementation of such protocols across research sites would facilitate meta-analyses and technology transfer, accelerating the overall development of the field.
Quantitative Analysis of BCI Research Landscape
Bibliometric analysis reveals significant growth in BCI research, with 1,431 publications on BCI technology in rehabilitation between 2004 and 2024 [55]. This expanding research landscape underscores the urgency of addressing standardization challenges to ensure coherent progress. The table below summarizes publication trends and collaborative networks in BCI research:
Table 2: Bibliometric Analysis of BCI Research (2004-2024)
| Metric Category | Specific Measure | Value or Finding |
|---|---|---|
| Publication Volume | Total Publications | 1,431 |
| Contributing Countries | 79 countries | |
| Leading Country (Publications) | China (398 publications) | |
| Leading Country (Citations) | USA (10,501 citations) | |
| Collaboration Networks | Total Connections | 444 collaborative links |
| Highest Betweenness Centrality | USA (0.35) | |
| Research Institutions | 1,281 institutions | |
| Research Focus | Primary Applications | Stroke rehabilitation, spinal cord injury, motor restoration |
| Emerging Technologies | Deep learning, hybrid BCI systems, cloud-based platforms |
The data reveals substantial global research activity with strong collaborative networks, particularly centered around the United States, which demonstrates the highest betweenness centrality despite China leading in publication volume [55]. This quantitative analysis highlights the need for standardization frameworks that can accommodate diverse research approaches while enabling meaningful comparisons across studies and systems.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful BCI research and development requires carefully selected materials and technologies tailored to specific research objectives. The following table outlines essential components of the BCI research toolkit, along with their functions and implementation considerations:
Table 3: Essential Research Materials for BCI Development
| Research Material | Function/Purpose | Implementation Considerations |
|---|---|---|
| EEG Electrodes (Wet/Dry) | Signal acquisition from scalp surface | Electrode impedance, signal stability, setup time, user comfort |
| fNIRS Optodes | Hemodynamic activity monitoring | Source-detector separation, penetration depth, temporal resolution |
| Utah Array & Neuralace | Invasive neural signal recording | Biocompatibility, channel count, long-term stability, surgical implantation |
| Stentrode | Endovascular signal recording | Minimally invasive placement, signal quality, long-term safety |
| BCI2000/OpenVibe | Signal processing platforms | Algorithm development, real-time processing, modular architecture |
| Standardized Paradigms | Experimental task protocols | SSVEP, P300, Motor Imagery, cross-system compatibility |
| Validation Datasets | Algorithm benchmarking | Publicly available datasets, standardized formats, labeled data quality |
Each component must be selected based on the specific research goals, target application, and patient population. The growing availability of standardized platforms and validation datasets represents significant progress in addressing the field's standardization challenges.
Implementation Framework for Standardized BCI Development
To address the multifaceted standardization challenges in BCI research and clinical translation, a comprehensive implementation framework is necessary. This framework should coordinate efforts across technical, clinical, and regulatory domains to establish coherent standards that support innovation while ensuring safety and efficacy.
The following diagram illustrates the multi-domain standardization framework required for effective BCI translation:
Interdisciplinary Collaboration Infrastructure
Successful standardization requires establishing formal collaboration infrastructures that bring together stakeholders from academia, industry, clinical practice, and regulatory bodies. These infrastructures should facilitate:
- Consensus development on core terminology, metrics, and methodologies
- Reference dataset creation for algorithm validation and benchmarking
- Interlaboratory studies to validate methods across different settings
- Standardized reporting guidelines for publications and regulatory submissions
- Shared repository development for protocols, software, and validation tools
Such infrastructures are particularly important for addressing emerging challenges in neural data privacy, informed consent procedures, and long-term safety monitoring [120].
Regulatory Science and Translation Pathway
The pathway from BCI research to clinical application requires harmonization between regulatory science and clinical practice. Standardization efforts should focus on:
- Predicate device identification for substantial equivalence determinations
- Performance standard development for safety and effectiveness
- Clinical trial design standardization for specific neurological conditions
- Real-world evidence collection frameworks for post-market surveillance
- Quality management systems appropriate for neurotechnology development
Regulatory agencies have begun addressing these needs through initiatives like the FDA's leapfrog guidance for implanted BCI devices [123], but significant work remains to create a comprehensive regulatory framework that keeps pace with technological innovation while ensuring patient safety.
Standardization challenges present significant barriers to the clinical translation of BCI technologies, affecting signal acquisition, data processing, algorithm development, efficacy assessment, and regulatory approval. Addressing these challenges requires coordinated efforts across technical, clinical, and regulatory domains to establish frameworks that support innovation while ensuring reliability, safety, and efficacy. The development of standardized evaluation methodologies, particularly for online closed-loop systems, represents a critical priority for the field. As BCI technology continues to evolve toward clinical application and commercial viability, overcoming these standardization hurdles will be essential for realizing the full potential of neurotechnology to transform patient care and human-computer interaction.
Brain-Computer Interfaces (BCIs) represent a transformative technology establishing a direct communication pathway between the brain and external devices [2]. For researchers and clinical professionals, the fundamental challenge lies in balancing the clinical benefits against the substantial technical implementation hurdles. This analysis examines the cost-benefit landscape of non-invasive BCI technologies, focusing on quantitative efficacy data, technical benchmarks, and implementation frameworks relevant to medical research and therapeutic development.
Non-invasive BCIs, primarily using electroencephalography (EEG) and functional near-infrared spectroscopy (fNIRS), offer significant safety advantages over invasive methods by eliminating surgical risks [6] [124]. However, they face inherent signal quality limitations that directly impact their clinical utility across various applications including neurorehabilitation, communication restoration, and sensory deficit treatment [2] [61]. This review systematically evaluates this tradeoff through structured data comparison, experimental protocol analysis, and technical implementation roadmaps.
Quantitative Clinical Utility Assessment
Therapeutic Efficacy Metrics
Recent meta-analyses and clinical trials provide quantitative evidence for BCI efficacy, particularly in neurological rehabilitation. The following table summarizes key findings from systematic reviews of non-invasive BCI interventions:
Table 1: Clinical Efficacy of Non-Invasive BCI Interventions for Spinal Cord Injury (Based on Meta-Analysis of 9 Studies, n=109) [10]
| Functional Domain | Standardized Mean Difference (SMD) | 95% Confidence Interval | P-value | Evidence Grade |
|---|---|---|---|---|
| Motor Function | 0.72 | [0.35, 1.09] | < 0.01 | Medium |
| Sensory Function | 0.95 | [0.43, 1.48] | < 0.01 | Medium |
| Activities of Daily Living | 0.85 | [0.46, 1.24] | < 0.01 | Low |
Subgroup analyses revealed that intervention timing significantly impacts outcomes. Patients with subacute spinal cord injuries demonstrated statistically stronger improvements across all functional domains compared to those with chronic injuries, highlighting the importance of treatment timing in clinical implementation [10].
Communication Restoration Performance
For patients with motor speech impairments such as ALS, communication restoration represents a critical application. Performance metrics for emerging systems demonstrate the rapid evolution of this technology:
Table 2: Performance Benchmarks for BCI Communication Systems
| Technology/Company | Information Transfer Rate (bits/min) | Words Per Minute | Application Context | Reference |
|---|---|---|---|---|
| Cognixion Axon-R Nucleus | 30 (equating to ~30 choices/min) | Variable (with AI augmentation) | ALS communication with AR interface | [125] |
| Blackrock Neurotech | N/A | 90 characters/minute | Paralysis/ALS communication | [38] |
| Advanced Speech Decoders | N/A | ~290 words (total vocabulary) | Speech decoding from neural signals | [62] |
The integration of generative AI in systems like Cognixion's introduces complexity in traditional metrics like words-per-minute, as a single binary choice can generate extensive text, potentially inflating this measure beyond its functional communication value [125].
Technical Implementation Framework
BCI Signal Processing Pathway
The technical implementation of non-invasive BCIs follows a structured signal processing pipeline with distinct stages that introduce specific computational requirements and potential signal degradation points. The following diagram visualizes this pathway:
BCI Signal Processing Pipeline
This workflow illustrates the closed-loop nature of modern BCI systems, where neurofeedback enables user adaptation and potentially enhances performance over time—a critical consideration for clinical trial design and rehabilitation protocols [62] [10].
Technology Comparison and Selection Framework
The fundamental tradeoff between signal quality and accessibility dictates clinical implementation decisions. The following table benchmarks major non-invasive and minimally invasive technologies against key implementation criteria:
Table 3: Technical Implementation Benchmarking of BCI Technologies [126] [2] [124]
| Technology | Spatial Resolution | Temporal Resolution | Portability | Setup Complexity | Signal Fidelity | Primary Clinical Applications |
|---|---|---|---|---|---|---|
| EEG (traditional) | Low (cm) | High (ms) | High | High (gel electrodes) | Low | Sleep monitoring, basic neurofeedback |
| Dry EEG | Low (cm) | High (ms) | High | Medium | Low to Medium | Wellness, cognitive monitoring, communication |
| fNIRS | Medium (1-2 cm) | Low (seconds) | Medium | Medium | Medium | Rehabilitation, music imagery, binary communication |
| Wearable MEG | High (mm) | High (ms) | Low | Very High | High | Research settings with shielding |
| Endovascular (Stentrode) | High (mm) | High (ms) | High | Very High (surgical) | High | Paralysis, communication restoration |
| Cortical Surface (Layer 7) | Very High (mm) | Very High (ms) | High | Very High (surgical) | Very High | Speech restoration, motor control |
Synchron's Stentrode represents a hybrid approach, offering higher signal quality through a minimally invasive endovascular procedure that avoids open brain surgery, potentially improving the risk-benefit profile for certain patient populations [62] [6].
Experimental Implementation Protocols
Clinical Trial Design Considerations
Recent BCI trials have established methodological frameworks that balance regulatory requirements with patient-centered outcomes:
4.1.1 Communication Restoration Protocol (Cognixion)
- Patient Population: Mid- to late-stage ALS patients with motor speech impairments, requiring caregiver support for device operation [125].
- Device Configuration: Integrated system combining occipital EEG sensors with Apple Vision Pro augmented reality display presenting frequency-specific visual stimuli [125].
- Outcome Measures:
- Primary: Information Transfer Rate (bits/minute)
- Secondary: System Usability Scale (SUS), quality of life measures
- Exploratory: Caregiver burden assessment
- Implementation Challenge: Participant recruitment difficulties due to disease rarity (25,000-30,000 ALS patients in U.S.) and heterogeneity necessitates multi-regional trial designs [125].
4.1.2 Motor Function Rehabilitation Protocol (Spinal Cord Injury)
- Intervention Structure: Non-invasive BCI-driven neurofeedback training targeting sensorimotor rhythms [10].
- Session Parameters: Variable protocols across studies, typically involving multiple sessions per week over several weeks.
- Assessment Timeline: Acute (post-intervention) and retention (follow-up) measurements using standardized scales including ASIA motor scores, Berg Balance Scale, and Spinal Cord Independence Measure [10].
- Key Finding: Significantly stronger effect sizes in subacute versus chronic SCI patients, informing patient selection criteria [10].
Research Reagent Solutions
The following table details essential research components for BCI experimental implementation:
Table 4: Essential Research Materials and Platforms for BCI Investigation
| Component Category | Specific Examples | Research Function | Implementation Considerations |
|---|---|---|---|
| Signal Acquisition | EEG electrode systems (wet, dry), fNIRS optodes, MEG sensors | Neural signal recording | Dry electrodes reduce setup time but may compromise signal quality; fNIRS avoids electrical artifacts but has slower temporal response [124] |
| Data Acquisition Platforms | Blackrock Neurotech systems, custom FPGA solutions | Signal digitization and initial processing | High-channel count systems require substantial data handling capabilities; sampling rates must balance temporal resolution with storage needs [126] |
| Stimulus Presentation | AR displays (Apple Vision Pro), visual stimulus projectors | Paradigm delivery for evoked responses | Integrated systems like Cognixion's combine stimulation and recording in one device [125] |
| Signal Processing Libraries | Python MNE, EEGLAB, Cloud-based AI services | Feature extraction and classification | Deep learning approaches require substantial training datasets but show promise for decoding complexity [62] [6] |
| Output Controllers | Robotic limbs, functional electrical stimulation, communication interfaces | Effector devices for BCI output | Must match the control capabilities of the BCI system; simplicity often enhances reliability [61] [10] |
Market Implementation Economics
The commercial landscape for BCIs reflects both the significant potential and substantial implementation barriers. The overall BCI market is forecast to grow from $2.87 billion in 2024 to over $15.14 billion by 2035, representing a CAGR of 16.32% [38]. Invasive approaches currently dominate high-functionality applications, but non-invasive technologies are expected to capture significant market share in consumer and wellness sectors [126].
Geographic implementation varies significantly, with Asia-Pacific leading in market demand due to healthcare infrastructure development and attractive manufacturing environments, while North America shows the fastest growth driven by concentrated BCI startup activity (over 87 BCI startups in the United States alone) and high research investment [38]. This geographic distribution influences clinical trial site selection and resource allocation for multi-center studies.
Regulatory pathways continue to evolve, with the FDA establishing specialized committees including representatives from companies including Precision Neuroscience and Neuralink to debate appropriate efficacy measures, focusing on metrics like information transfer rate versus words-per-minute for communication devices [125].
The cost-benefit analysis of non-invasive BCIs reveals a technology class with demonstrated clinical utility but significant implementation complexity. Quantitative evidence supports efficacy in motor, sensory, and communication domains, though effect sizes vary substantially based on patient factors and implementation protocols. The tradeoff between signal fidelity and accessibility remains the fundamental determinant of clinical application suitability.
For researchers and drug development professionals, optimal implementation requires careful matching of technology capabilities to specific clinical use cases, with consideration of patient population characteristics, outcome measurement strategies, and economic constraints. As signal processing algorithms and sensor technologies continue to advance, the balance may shift toward non-invasive methods for an expanding range of applications, potentially transforming neurorehabilitation and human-computer interaction paradigms.
User Experience and Usability Studies in Patient Populations
The integration of non-invasive Brain-Computer Interface (BCI) technologies into clinical practice requires rigorous evaluation of user experience (UX) and usability within patient populations. For researchers and drug development professionals, understanding these factors is critical for developing effective, adoptable, and safe neurotechnologies. This technical guide examines UX and usability methodologies, metrics, and experimental protocols essential for evaluating non-invasive BCIs in clinical research settings, framed within a broader thesis on BCI technology review and comparison. The core challenge lies in adapting traditional UX principles to the unique constraints of patients with spinal cord injuries (SCI) and other neurological disorders, where motor, sensory, and cognitive impairments can significantly impact interaction paradigms [10] [2].
Non-invasive BCI systems, particularly those using electroencephalography (EEG), offer a promising pathway for functional recovery and quality-of-life enhancement without the risks associated with surgical implantation [2] [8]. This guide provides a structured approach for conducting robust usability studies that can generate high-quality evidence for clinical validation and technology adoption.
Quantitative Outcomes of BCI Interventions
A meta-analysis of non-invasive BCI interventions for Spinal Cord Injury (SCI) patients provides critical quantitative evidence for their therapeutic potential. The following table summarizes the standardized mean differences (SMDs) and evidence quality for core functional domains based on 9 studies involving 109 SCI patients [10].
Table 1: Meta-Analysis of BCI Efficacy on Core Functional Domains in SCI
| Functional Domain | Number of Studies | SMD (95% CI) | P-value | I² | GRADE Evidence Level |
|---|---|---|---|---|---|
| Motor Function | 9 | 0.72 (0.35, 1.09) | < 0.01 | 0% | Medium |
| Sensory Function | 9 | 0.95 (0.43, 1.48) | < 0.01 | 0% | Medium |
| Activities of Daily Living (ADL) | 9 | 0.85 (0.46, 1.24) | < 0.01 | 0% | Low |
Subgroup analyses from this meta-analysis revealed that patients in the subacute stage of SCI demonstrated statistically stronger improvements across all three domains compared to those in the slow chronic stage [10]. This highlights a potential critical window for BCI intervention and underscores the importance of considering injury chronicity as a key modifier in UX study design and patient recruitment.
Beyond these core outcomes, usability studies should capture data on technology acceptance, cognitive load, and fatigue, as these subjective metrics are crucial for long-term adoption. The next table outlines key subjective and performance metrics relevant to a comprehensive BCI usability assessment.
Table 2: Key Metrics for BCI Usability Assessment in Patient Populations
| Metric Category | Specific Metric | Assessment Method | Clinical Relevance |
|---|---|---|---|
| System Performance | Information Transfer Rate (ITR) | Calculation from accuracy & speed | Quantifies communication bandwidth |
| Classification Accuracy | Percentage of correct commands | Measures system reliability | |
| User Performance | Task Completion Time | Time measurement per task | Assesses practical efficiency |
| Error Rate | Frequency of incorrect commands | Induces user frustration | |
| Subjective Usability | System Usability Scale (SUS) | Standardized questionnaire | Global usability perception |
| NASA-TLX | Workload assessment | Quantifies cognitive fatigue | |
| Quebec User Evaluation of Satisfaction with assistive Technology (QUEST) | Structured interview | Measures user satisfaction |
Experimental Protocols for BCI Usability
Hybrid P300/SSVEP BCI Protocol
A rigorously tested protocol for patients with disorders of consciousness, which is also applicable to SCI populations, involves a hybrid P300/SSVEP BCI [94]. This protocol is particularly valuable for assessing usability in users with varying levels of cognitive and motor function.
- GUI and Stimuli: The interface presents two frontal-view facial photographs (the patient's own face and a stranger's face), each embedded in a static photo-frame. The photographs flicker at different frequencies (6.0 Hz and 7.5 Hz) to evoke Steady-State Visual Evoked Potentials (SSVEPs) [94].
- Trial Structure: Each trial begins with an 8-second audiovisual instruction. A 10-second stimulation period follows, during which the two photographs flicker, and their frames flash simultaneously in a pseudorandom order (each flashing 5 times for 200ms with 800ms intervals) to evoke P300 potentials. A 4-second feedback period then provides both visual (tick or cross) and auditory (applause for success) feedback [94].
- Data Processing: For P300 detection, EEG signals are filtered (0.1–10 Hz), and segments from 10 channels (0–600ms after each flash) are down-sampled and concatenated to form a feature vector. A Support Vector Machine (SVM) classifier is applied. For SSVEP detection, signals are filtered (4–20 Hz), and a weighted sum of segments from 8 electrodes is processed via discrete Fourier transform to calculate a power ratio at the target frequencies [94].
- Usability Adaptation: This protocol's design, which includes personalized stimuli (the patient's own face) and multi-sensory feedback, directly enhances user engagement and provides a robust framework for testing UX parameters.
Motor Imagery-Based BCI Protocol
For motor function rehabilitation in SCI, kinaesthetic motor imagery (KMI) protocols are highly relevant. These can be implemented using platforms like OpenViBE, which provides a comprehensive software environment for EEG acquisition, signal processing, and feedback [127].
- Paradigm: A standard Graz BCI protocol for foot kinaesthetic motor imagery is employed. Users imagine the kinesthetic sensation of foot movement without executing actual motion.
- Signal Processing Focus: The key analytic method is the quantification of Event-Related Desynchronization (ERD) and Synchronization (ERS) patterns in the sensorimotor rhythms (mu and beta bands) over the primary sensorimotor cortex.
- Application: This protocol is a potential tool for the control of wearable lower-limb devices and rehabilitation equipment, making its usability directly relevant to restoring mobility. The platform's online processing capability is essential for providing real-time feedback, a critical component for user learning and engagement [127].
BCI Signaling and Experimental Workflows
Non-Invasive BCI Signal Pathway
The following diagram visualizes the core signal processing pathway that underpins most non-invasive BCI systems, from signal acquisition to the execution of a command. This pathway is fundamental to understanding the points where usability can be impacted by technical performance.
Usability Experiment Workflow
A methodologically sound usability study for BCI in patient populations requires a structured experimental workflow. The following diagram outlines the key phases from participant screening to data analysis.
The Scientist's Toolkit: Research Reagent Solutions
This section details essential materials and computational tools used in contemporary non-invasive BCI research, providing a quick reference for scientists designing usability studies.
Table 3: Essential Research Materials and Tools for BCI Usability Studies
| Item Name / Category | Specification / Example | Primary Function in BCI Research |
|---|---|---|
| EEG Acquisition System | NuAmps device (Compumedics Neuroscan); Emotiv EPOC; BrainProducts ActiCap | Multi-channel EEG signal recording with specific sampling rates (e.g., 250 Hz) and impedance management (< 5 kΩ) [94] [128]. |
| Electrode Cap | 30-channel LT 37 cap; 16-channel EPOC cap; 32-channel ActiCap | Holds electrodes in standardized positions according to the International 10-20 system for consistent signal acquisition [94] [128]. |
| Signal Processing & BCI Platform | OpenViBE; BCILAB; Custom MATLAB/Python toolboxes | Provides a software environment for real-time signal processing, feature extraction (ERD/ERS), classifier training, and experimental scenario design [127]. |
| Classification Algorithms | Support Vector Machine (SVM); Common Spatial Patterns (CSP); Bayesian Classifiers | Translates pre-processed EEG features into identifiable commands or states. SVM is noted for performance with small training datasets [94] [128]. |
| Paradigm Stimulation Software | Custom applications using Psychtoolbox (MATLAB) or PsychoPy (Python) | Presents visual/auditory stimuli (e.g., for P300, SSVEP) with precise timing control essential for evoked potential studies [94]. |
| Subjective Assessment Tools | System Usability Scale (SUS); NASA-TLX; Quebec User Evaluation of Satisfaction with assistive Technology (QUEST) | Standardized questionnaires and interviews to quantify user perception, cognitive workload, and satisfaction with the BCI system [10]. |
User experience and usability studies are paramount for translating non-invasive BCI technologies from laboratory demonstrations to clinically impactful tools. The quantitative data shows promising effects on motor, sensory, and daily living functions in SCI patients, particularly when intervention occurs in the subacute phase [10]. The field is progressing through advancements in dry electrodes, improved signal processing algorithms, and more sophisticated hybrid BCI paradigms that combine multiple control signals (e.g., P300 + SSVEP) to improve reliability and user experience [2] [8].
Future research must focus on longitudinal usability studies to understand learning curves and long-term adoption barriers. Furthermore, developing standardized, validated UX metrics specifically for BCI will enable more meaningful cross-study comparisons. As the technology matures, the integration of BCI with other assistive technologies and its application in broader clinical contexts will continue to present new challenges and opportunities for UX research, ultimately driving the development of more intuitive, effective, and patient-centered neurotechnologies.
Conclusion
Non-invasive BCIs represent a rapidly advancing frontier in neurotechnology with significant potential to transform biomedical research and clinical practice. Current evidence demonstrates their established value in neurorehabilitation, particularly for spinal cord injury and stroke recovery, while emerging applications in cognitive enhancement and neurodegenerative disease monitoring show considerable promise. The field is progressing toward higher-fidelity signal acquisition through innovations like flexible electronic sensors, digital holographic imaging, and advanced machine learning algorithms that continuously narrow the performance gap with invasive approaches. Future directions will likely focus on multimodal integration, personalized adaptive systems, and miniaturized wireless platforms that enable real-world deployment beyond laboratory settings. For researchers and drug development professionals, non-invasive BCIs offer unprecedented opportunities for quantifying neurological function, monitoring therapeutic responses, and developing novel digital biomarkers. However, realizing this potential requires addressing persistent challenges in signal quality standardization, regulatory harmonization, and demonstrating cost-effectiveness in healthcare ecosystems. The convergence of non-invasive BCI with artificial intelligence and personalized medicine approaches positions this technology as a cornerstone of next-generation neurological research and therapeutic development.
References
- 1. 1.2 Fundamental principles and components of BCIs [https://fiveable.me/brain-computer-interfaces/unit-1/fundamental-principles-components-bcis/study-guide/i7OZVBcnnTkaAYWw]
- 2. The history, current state and future possibilities of the non- ... [https://www.sciencedirect.com/science/article/pii/S2590093525000049]
- 3. Non-Invasive Brain-Computer Interfaces: State of the Art and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11861396/]
- 4. Summary of over Fifty Years with Brain-Computer Interfaces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7824107/]
- 5. Physical principles of brain–computer interfaces and their ... [https://www.sciencedirect.com/science/article/abs/pii/S0370157321001095]
- 6. The Past, Present And Future Of Brain-Computer Interfaces [https://www.forbes.com/sites/robtoews/2025/10/05/these-are-the-startups-merging-your-brain-with-ai/]
- 7. Non-Invasive BCI-VR Applied Protocols as Intervention ... [https://www.mdpi.com/1424-8220/25/5/1342]
- 8. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/en/research-report/brain-computer-interfaces/1024]
- 9. A New Path to Noninvasive Brain-Computer Interface [https://www.jhuapl.edu/news/news-releases/241114-noninvasive-brain-computer-interface]
- 10. The impact of non-invasive brain-computer interface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12642192/]
- 11. Biophysical and physiological origins of blood oxygenation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3390806/]
- 12. Human Neocortical Neurosolver (HNN), a new software ... [https://elifesciences.org/articles/51214]
- 13. Current implications of EEG and fNIRS as functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11629311/]
- 14. Comparative analysis of signal quality and usability for a ... [https://www.sciencedirect.com/science/article/pii/S2467981X25000289]
- 15. A Comparison of Physiological Signal Analysis Techniques ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4945646/]
- 16. Non-Invasive Brain-Computer Interfaces: State of the Art and ... [https://pubmed.ncbi.nlm.nih.gov/39186407/]
- 17. Investigating the interaction between EEG and fNIRS [https://www.sciencedirect.com/science/article/pii/S1877750324002096]
- 18. Benchmarking the utility of dry-electrode ... [https://www.nature.com/articles/s41598-025-18184-7]
- 19. Recent Advances in Portable Dry Electrode EEG [https://pmc.ncbi.nlm.nih.gov/articles/PMC12389868/]
- 20. A Comparison of Electrodes: Dry, Wet and Soft [https://www.brainaccess.ai/a-comparison-of-electrodes-dry-wet-and-soft/]
- 21. Why Brain Wearables Are Making Traditional EEG Labs ... [https://globalrph.com/2025/10/why-brain-wearables-are-making-traditional-eeg-labs-obsolete-in-2025/]
- 22. Brain–Computer Interfacing Using Functional Near-Infrared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8534036/]
- 23. fNIRS-based brain-computer interfaces: a review [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2015.00003/full]
- 24. Applications of Functional Near-Infrared Spectroscopy (fNIRS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11188690/]
- 25. How fNIRS technology enables hemodynamic response [https://www.thinkiesystem.com/blog/how-fnirs-technology-enables-hemodynamic-response?srsltid=AfmBOopp8yFZv34cTqdh023n18Rz0_15pqJH7CkEoHJHjuZFioAHUnm5]
- 26. A temporal comparison of BOLD, ASL, and NIRS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2692693/]
- 27. Functional Near-Infrared Imaging for Biomedical Applications [https://www.intechopen.com/chapters/1195745]
- 28. The top BCI stories of 2025 so far [https://www.massdevice.com/top-bci-stories-2025-so-far/]
- 29. Recent Progress in Wearable Brain–Computer Interface (BCI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10880169/]
- 30. Trends for wearable and noninvasive Brain–Computer ... [https://www.sciencedirect.com/science/article/pii/S0956566325001952]
- 31. Breakthrough in Noninvasive Brain-Computer Interfaces ... [https://www.impactlab.com/2024/11/21/breakthrough-in-noninvasive-brain-computer-interfaces-paves-the-way-for-mind-controlled-devices/]
- 32. Outlook for Noninvasive Brain-Computer Interfaces for AI [https://etcjournal.com/2025/09/21/outlook-for-noninvasive-brain-computer-interfaces-for-ai/]
- 33. 7T-fMRI: Faster Temporal Resolution Yields Optimal BOLD ... [https://pubmed.ncbi.nlm.nih.gov/28286317/]
- 34. What is BCI? | How brain-computer interfaces redefine ... [https://www.paradromics.com/insights/what-is-bci]
- 35. BETA: A Large Benchmark Database Toward SSVEP-BCI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7324867/]
- 36. Non-Invasive BCI Market Size, Analysis, Growth Outlook ... [https://www.forinsightsconsultancy.com/reports/non-invasive-bci-market]
- 37. Brain Computer Interface (BCI) Research Report 2025-2035 [https://finance.yahoo.com/news/brain-computer-interface-bci-research-090400037.html]
- 38. Top 10 Brain-Computer Interface Companies in 2025 [https://www.sphericalinsights.com/blogs/top-10-companies-leading-the-brain-computer-interface-market-in-2025-key-players-statistics-future-trends-2024-2035]
- 39. Review of Performance Improvement of a Noninvasive Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10984355/]
- 40. Top 10 Global Brain-Computer Interface (BCI) Companies ... [https://alltechmagazine.com/top-10-global-brain-computer-interface-bci-companies-in-2025/]
- 41. Non-Invasive Brain–Computer Interfaces [https://www.emergentmind.com/topics/non-invasive-brain-computer-interfaces-bcis]
- 42. Triboelectric nanogenerators for neural data interpretation [https://pubmed.ncbi.nlm.nih.gov/41281720/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=1V_PRf-wigmvSPfOUX24LRPUd9z0ARqsOWLr2f-R0beykJ_kU&fc=None&ff=20251126084739&v=2.18.0.post22+67771e2]
- 43. Advancing Brain-Computer Interface Closed-Loop Systems for ... [https://biomedeng.jmir.org/2025/1/e72218]
- 44. EEG-based brain-computer interface enables real-time ... [https://www.nature.com/articles/s41467-025-61064-x]
- 45. Triboelectric Nanogenerators for Neural Data Interpretation [https://www.frontiersin.org/journals/computational-neuroscience/articles/10.3389/fncom.2025.1691017/abstract]
- 46. A Survey on Advancements in Neural Signal Processing ... [https://arxiv.org/html/2503.00580v2]
- 47. Non-Invasive BCI in Focus: Growth Trajectories and ... [https://www.datainsightsmarket.com/reports/non-invasive-bci-1676871]
- 48. Neural decoding reliability: Breakthroughs and potential of ... [https://www.sciencedirect.com/science/article/pii/S1571064525001265]
- 49. AI co-pilot boosts noninvasive brain-computer interface by ... [https://newsroom.ucla.edu/releases/ai-brain-computer-interface-interprets-user-intent-ucla]
- 50. fMRI Brain Decoding and Its Applications in Brain–Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8869956/]
- 51. Towards decoding individual words from non-invasive ... [https://www.nature.com/articles/s41467-025-65499-0]
- 52. An empirical comparison of neural networks and machine ... [https://www.nature.com/articles/s41598-020-60932-4]
- 53. Decoding neuronal networks: A Reservoir Computing ... [https://www.sciencedirect.com/science/article/pii/S0893608024009870]
- 54. Motor imagery-based brain–computer interface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11134735/]
- 55. Knowledge mapping and research trends of brain-computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11557533/]
- 56. A multi-paradigm EEG dataset for studying upper limb ... [https://www.nature.com/articles/s41597-025-06147-6]
- 57. Paradigm Design [https://bio-protocol.org/exchange/minidetail?id=10265900&type=30]
- 58. A study of motor imagery EEG classification based on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307489/]
- 59. Feature Extraction and Classification of Motor Imagery EEG ... [https://www.mdpi.com/2071-1050/16/15/6627]
- 60. Motor Imagery Tasks Based Electroencephalogram ... [https://www.sciencedirect.com/science/article/pii/S2772528623000134]
- 61. Application and future directions of brain-computer ... [https://www.sciencedirect.com/science/article/pii/S2589238X2500083X]
- 62. BCIs in 2025: Trials, Progress, and Challenges [https://andersenlab.com/blueprint/bci-challenges-and-opportunities]
- 63. Advancing Brain-Computer Interface Closed-Loop Systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12588595/]
- 64. Unveiling the upper-limb functional recovery mechanisms ... [https://www.nature.com/articles/s41598-025-23267-6]
- 65. Reviewing 2025's Most Promising Cognitive Enhancement ... [https://ericker.com/blog/cognitive-enhancement-research.html]
- 66. How does invasive vs non-invasive BCI compare? [https://synapse.patsnap.com/article/how-does-invasive-vs-non-invasive-bci-compare]
- 67. Invasive vs. Non-Invasive Neuronal Signals for Brain- ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2016.00295/full]
- 68. Practice effects on digital cognitive assessment tools [https://pmc.ncbi.nlm.nih.gov/articles/PMC12412751/]
- 69. A Symbols Based BCI Paradigm for Intelligent Home ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9781197/]
- 70. Flexible brain electronic sensors advance wearable ... [https://www.nature.com/articles/s44385-025-00029-7]
- 71. Flexible Electrodes in BCI: Types and Future [https://www.allpcb.com/allelectrohub/flexible-electrodes-in-bci-types-and-future]
- 72. Recent Progress in Flexible Wearable Sensors for Real- ... [https://www.mdpi.com/2072-666X/16/10/1124]
- 73. Wireless EEG monitoring system with wearable self ... [https://www.sciencedirect.com/science/article/abs/pii/S1385894725062825]
- 74. Recent advancements in wearable sensors: integration with ... [https://pubs.rsc.org/en/content/articlehtml/2025/ra/d5ra00167f]
- 75. All-in-one self-powered wearable biosensors systems [https://www.sciencedirect.com/science/article/pii/S0927796X25000117]
- 76. Multi-Modal Integration of EEG-fNIRS for Brain-Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5651279/]
- 77. A Cross-Disciplinary Review of the fNIRS-EEG Dual-Modality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11506513/]
- 78. Brain–computer interfaces: the innovative key to unlocking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11392146/]
- 79. HEFMI-ICH: a hybrid EEG-fNIRS motor imagery dataset for ... [https://www.nature.com/articles/s41597-025-06100-7]
- 80. A Novel Transfer Learning‐Based Hybrid EEG‐fNIRS Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12631896/]
- 81. Multimodal fNIRS-EEG measurements — Analysis ... [https://www.artinis.com/blogpost-all/multimodal-fnirs-eeg-measurements-analysis-approaches]
- 82. EEG–fNIRS signal integration for motor imagery ... [https://www.sciencedirect.com/science/article/pii/S2772528625000299]
- 83. Breakthrough BCI Applications in Medicine [https://www.frontiersin.org/research-topics/6300/breakthrough-bci-applications-in-medicine/magazine]
- 84. Editorial: Methods and protocols in Brain-Computer ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2024.1447973/full]
- 85. Effects of skull thickness, anisotropy, and inhomogeneity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6872130/]
- 86. Performance Measurement for Brain-Computer or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4185283/]
- 87. Comprehensive evaluation methods for translating BCI into ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2024.1429130/full]
- 88. Removal of Artifacts from EEG Signals: A Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6427454/]
- 89. Short-term BCI intervention enhances functional brain ... [https://www.sciencedirect.com/science/article/pii/S2213158225000427]
- 90. AnEEG: leveraging deep learning for effective artifact ... [https://www.nature.com/articles/s41598-024-75091-z]
- 91. Noise To Signal: Cuban Backs Synaptrix Labs Non- ... [https://www.forbes.com/sites/naveenrao/2025/10/24/noise-to-signal-cuban-backs-synaptrix-labs-non-invasive-bci-platform/]
- 92. AI Co-Pilot Boosts Noninvasive Brain-Computer Interface ... [https://samueli.ucla.edu/ai-co-pilot-boosts-noninvasive-brain-computer-interface-by-interpreting-user-intent/]
- 93. Brain-Computer Interfaces: Exploring the Last Frontier [https://www.byfounders.vc/insights/brain-computer-interfaces]
- 94. Brain-computer interface experiments [https://bio-protocol.org/exchange/minidetail?id=6046861&type=30]
- 95. Quantifying physical degradation alongside recording and ... [https://www.sciencedirect.com/science/article/pii/S1742706125001151]
- 96. Comprehensive evaluation methods for translating BCI into ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11188342/]
- 97. Error-related Potential driven Reinforcement Learning for ... [https://arxiv.org/abs/2502.18594]
- 98. Improving non-invasive trajectory decoding via neural ... [https://pubmed.ncbi.nlm.nih.gov/39231465/]
- 99. A Non-Invasive Brain-Computer Interface for Real-Time ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5906041/]
- 100. Comparison metrics and power trade-offs for BCI motor ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1547074/full]
- 101. Towards a Cure for BCI Illiteracy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2874052/]
- 102. Bridging the BCI illiteracy gap: a subject-to- ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2023.1194751/full]
- 103. Exploring the Potential of BCI in Education: An Experiment ... [https://www.mdpi.com/2078-2489/16/4/261]
- 104. Standardization of protocol design for user training in EEG- ... [https://pubmed.ncbi.nlm.nih.gov/33217745/]
- 105. Comparison metrics and power trade-offs for BCI motor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11936894/]
- 106. Behind the Scenes of Noninvasive Brain–Computer Interfaces [https://pmc.ncbi.nlm.nih.gov/articles/PMC7288588/]
- 107. Best Practices for Accessible Color Contrast in UX [https://developerux.com/2025/07/28/best-practices-for-accessible-color-contrast-in-ux/]
- 108. Editorial: Methods and protocols in Brain-Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11288932/]
- 109. Efficacy of brain–computer interface with functional ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1643536/full]
- 110. Signal processing techniques for motor imagery brain ... [https://www.sciencedirect.com/science/article/pii/S2590005619300037]
- 111. AI Copilot Boosts Brain-Computer Interface's Performance [https://www.psychologytoday.com/us/blog/the-future-brain/202509/ai-copilot-boosts-brain-computer-interfaces-performance]
- 112. Applications of OPM-MEG for translational neuroscience [https://www.nature.com/articles/s41398-024-03047-y]
- 113. Simultaneous EEG and fNIRS recordings for semantic ... [https://www.nature.com/articles/s41597-025-04967-0]
- 114. Techniques Advances and Clinical Applications in Fused ... [https://www.frontiersin.org/research-topics/8182/techniques-advances-and-clinical-applications-in-fused-eeg-fnirs/magazine]
- 115. A simultaneous MEG-EEG-fNIRS acquisition system [https://www.sciencedirect.com/science/article/pii/S1053811922005377]
- 116. A Comparative Study on the Detection of Covert Attention ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2017.00575/full]
- 117. Improved classification performance of EEG-fNIRS ... [https://pubmed.ncbi.nlm.nih.gov/35992956/]
- 118. Regulatory Pathways for Neural-Interface Devices - MediGear [https://medigear.uk/blog/what-are-the-regulatory-pathways-for-neural-interface-devices]
- 119. Comparative accuracy of invasive versus non- ... [https://eureka.patsnap.com/report-comparative-accuracy-of-invasive-versus-non-invasive-brain-computer-interfaces-approaches]
- 120. Ethical imperatives in the commercialization of brain- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12553070/]
- 121. A brain-computer interface roadmap for diagnosing and ... [https://www.the-innovation.org/article/doi/10.59717/j.xinn-inform.2025.100016]
- 122. Several inaccurate or erroneous conceptions and misleading ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11004276/]
- 123. 7 brain-computer interface companies you need to know [https://www.massdevice.com/brain-computer-interface-bci-companies/]
- 124. The Promise and Challenges of Brain–Computer Interfaces [https://www.technologynetworks.com/informatics/articles/the-promise-and-challenges-of-braincomputer-interfaces-397268]
- 125. Non-Invasive Brain-Computer Interface Trial Balances ... [https://www.clinicalleader.com/doc/non-invasive-brain-computer-interface-trial-balances-regulatory-requirements-with-patient-needs-0001]
- 126. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/tw/research-report/brain-computer-interfaces/1024]
- 127. Motor imagery based EEG features visualization for BCI ... [https://www.sciencedirect.com/science/article/pii/S1877050918313358]
- 128. Brain-Computer Interface Based on Generation of Visual Images [https://pmc.ncbi.nlm.nih.gov/articles/PMC3112189/]