Multimodal LLMs for Brain MRI Sequence Classification: A Comprehensive Review for Biomedical Researchers
This article provides a comprehensive analysis of the application of Multimodal Large Language Models (MLLMs) in classifying brain MRI sequences, a critical task for medical imaging workflows and AI-driven diagnostics.
Multimodal LLMs for Brain MRI Sequence Classification: A Comprehensive Review for Biomedical Researchers
Abstract
This article provides a comprehensive analysis of the application of Multimodal Large Language Models (MLLMs) in classifying brain MRI sequences, a critical task for medical imaging workflows and AI-driven diagnostics. We explore the foundational principles enabling MLLMs to process and interpret radiological images, detail the current methodologies and real-world applications being developed, and critically examine performance benchmarks from recent comparative studies. The content further addresses significant challenges such as model hallucinations and sequence misclassifications, presenting emerging optimization strategies. Designed for researchers, scientists, and drug development professionals, this review synthesizes validation data and outlines a forward-looking perspective on the integration of MLLMs into clinical and biomedical research pipelines, emphasizing the balance between technological potential and the necessity for robust, clinically-safe implementation.
The Rise of Multimodal AI in Radiology: Core Principles and Clinical Promise
Multimodal Large Language Models (MLLMs) represent a significant evolution in artificial intelligence, extending the capabilities of text-only large language models (LLMs) to process and integrate diverse data types. In clinical medicine, particularly in visually intensive disciplines like radiology, MLLMs can concurrently process various imaging types (e.g., CT, MRI, X-ray) alongside textual data such as radiology reports and clinical notes from electronic health records (EHRs) [1]. Their core capability lies in integrating and aligning this heterogeneous information across modalities, often mapping them into a shared representational space [1]. This synergy allows for a more comprehensive understanding than unimodal approaches permit, enabling complex cross-modal tasks such as radiology report generation (RRG) from images and visual question answering (VQA) that incorporates both imaging and clinical context [1]. This document frames the exploration of MLLMs within the specific research context of brain MRI sequence classification, providing application notes and detailed experimental protocols for researchers and drug development professionals.
Technical Foundations of MLLMs
Core Architectural Components
A typical MLLM architecture comprises several key components [1]:
- Modality-Specific Encoders: These transform complex data types—such as images, audio, and video—into simpler, meaningful representations. Pre-trained models, like Contrastive Language-Image Pre-training (CLIP), are often employed to align visual data with corresponding textual descriptions [1].
- Multimodal Connector: This is a learnable interface that bridges the modality gap between non-text data (e.g., images) and natural language. It translates the outputs of specialized encoders into a format interpretable by the LLM. Connector types include projection-based (using multi-layer perceptrons), query-based (using trainable tokens), and fusion-based (using cross-attention mechanisms) [1].
- Pre-trained LLM: This serves as the cognitive backbone, providing powerful reasoning capabilities acquired from training on vast text corpora. The LLM processes the fused multimodal information to generate coherent responses [1].
Standardized Training Pipeline
MLLMs are typically developed through a sequential, multi-stage training pipeline [1]:
- Pre-training: A multimodal connector learns to align visual and textual representations using large-scale image-text pairs.
- Instruction Tuning: The model is fine-tuned with diverse natural language instructions and multimodal inputs to reliably follow complex directives.
- Alignment Tuning: The model's outputs are optimized to better reflect human preferences, often through reinforcement learning from human feedback (RLHF), to improve response quality and reliability and reduce hallucinations [1].
Quantitative Performance in Brain MRI Sequence Classification
Evaluating the ability of MLLMs to recognize fundamental image characteristics, such as MRI sequences, is a critical first step before deploying them in complex clinical scenarios. A recent comparative analysis tested three advanced MLLMs—ChatGPT-4o, Claude 4 Opus, and Gemini 2.5 Pro—on a set of 130 brain MRI images without pathological findings, representing 13 standard MRI series [2]. The models were prompted in a zero-shot setting to identify the modality, anatomical region, imaging plane, contrast-enhancement status, and specific MRI sequence [2].
Table 1: Performance Accuracy of MLLMs on Basic Brain MRI Identification Tasks (n=130 images)
| Task | ChatGPT-4o | Claude 4 Opus | Gemini 2.5 Pro |
|---|---|---|---|
| Modality identification | 130/130 (100.00%) | 130/130 (100.00%) | 130/130 (100.00%) |
| Anatomical region recognition | 130/130 (100.00%) | 130/130 (100.00%) | 130/130 (100.00%) |
| Imaging plane classification | 130/130 (100.00%) | 129/130 (99.23%) | 130/130 (100.00%) |
| Contrast-enhancement status | 128/130 (98.46%) | 124/130 (95.38%) | 128/130 (98.46%) |
| MRI sequence classification | 127/130 (97.69%) | 95/130 (73.08%) | 121/130 (93.08%) |
The data reveals that while all models excelled at basic recognition tasks, performance varied significantly in the more complex task of specific MRI sequence classification, which was the study's primary outcome (p < 0.001) [2]. ChatGPT-4o achieved the highest accuracy (97.69%), followed by Gemini 2.5 Pro (93.08%), and Claude 4 Opus (73.08%) [2]. The most frequent misclassifications involved Fluid-attenuated Inversion Recovery (FLAIR) sequences, often confused with T1-weighted or diffusion-weighted sequences [2]. Claude 4 Opus showed particular difficulty with Susceptibility-Weighted Imaging (SWI) and Apparent Diffusion Coefficient (ADC) sequences [2]. It is crucial to note that Gemini 2.5 Pro exhibited occasional hallucinations, generating irrelevant clinical details such as "hypoglycemia" and "Susac syndrome," which underscores a significant risk for clinical use [2].
Other studies corroborate the potential of LLMs in this domain. A GPT-4-based classifier outperformed both convolutional neural network (CNN) and string-matching methods on 1490 brain MRI sequences, achieving an accuracy of 0.83 with high sensitivity and specificity [3]. Furthermore, addressing the challenge of domain shift—where models perform poorly on data that deviates from the training set, such as between adult and pediatric MRI data—requires specialized approaches. One study found that a hybrid CNN-Transformer model (MedViT), especially when combined with expert domain knowledge adjustments, achieved high accuracy (0.905) in classifying pediatric MRI sequences after being trained on adult data, demonstrating enhanced robustness [4].
Experimental Protocols for MLLM Evaluation
Protocol 1: Zero-Shot MRI Sequence Classification
This protocol outlines the methodology for evaluating MLLMs on brain MRI sequence classification, as derived from the comparative study [2].
1. Objective: To assess and compare the zero-shot performance of MLLMs in classifying brain MRI sequences and other fundamental image characteristics.
2. Materials:
- Image Dataset: 130 brain MRI images from adult patients without pathological findings, representing 13 standard MRI series (e.g., axial T1w, T2w, FLAIR, DWI, ADC, SWI, and contrast-enhanced variants) [2].
- Data Preparation: Export single representative slices in high-quality JPEG format (minimum resolution 994 × 1382 pixels) without compression, cropping, annotations, or visual post-processing [2].
- Models: Access to the most up-to-date versions of MLLMs such as ChatGPT-4o, Gemini 2.5 Pro, and Claude 4 Opus via their official web interfaces [2].
3. Procedure:
- Image Upload: For each of the 130 images, initiate a new chat session to prevent in-context adaptation. Individually upload the image to the MLLM [2].
- Standardized Prompting: Use the following exact English prompt in a zero-shot setting [2]:
"This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: What type of radiological modality is this examination? Which anatomical region does this examination cover? What is the imaging plane (axial, sagittal, or coronal)? Is this a contrast-enhanced image or not? If this image is an MRI, what is the specific MRI sequence? If it is not an MRI, write 'Not applicable.' Please number your answers clearly."
- Response Collection: Record the model's responses for all questions.
4. Data Analysis:
- Ground Truth and Scoring: Two radiologists, in consensus, independently review and classify each response as "correct" or "incorrect" based on established ground truth [2].
- Statistical Analysis: Calculate accuracy for each task. For the primary outcome (MRI sequence classification), use Cochran's Q test for overall comparison between models, followed by pairwise McNemar tests with Bonferroni correction. Compute macro-averaged F1 scores and Cohen's kappa coefficients [2].
- Hallucination Monitoring: Document any model-generated statements unrelated to the input image or prompt context [2].
Protocol 2: Mitigating Domain Shift in Sequence Classification
This protocol addresses the challenge of applying a model trained on one dataset (e.g., adult MRIs) to another with different characteristics (e.g., pediatric MRIs) [4].
1. Objective: To enhance the robustness of a pre-trained MRI sequence classification model when applied to a new domain (e.g., pediatric data) using a hybrid architecture and expert domain knowledge.
2. Materials:
- Datasets:
- Models: A pre-trained hybrid CNN-Transformer model like MedViT, which is designed for medical images and expects 3-channel RGB input [4].
3. Procedure:
- Model Pre-training: Train the MedViT model on the source (adult) dataset across all available MRI sequence classes (e.g., T1, T2, CT1, FLAIR, ADC, SWI, DWI variants, T2*/DSC) [4].
- Baseline Testing: Evaluate the pre-trained model's performance directly on the target (pediatric) test dataset to establish a baseline performance under domain shift [4].
- Expert Domain Knowledge Adjustment: Analyze the target dataset to identify which sequence labels from the source are present or absent. Adjust the model's final classification layer or decision-making process to ignore labels absent from the target dataset, effectively re-aligning the classification task [4].
- Final Evaluation: Re-evaluate the adjusted model's performance on the target dataset [4].
4. Data Analysis:
- Report accuracy with 95% confidence intervals.
- Compare the performance of the hybrid model (MedViT) against benchmark models (e.g., ResNet-18) with and without expert adjustment to quantify improvement [4].
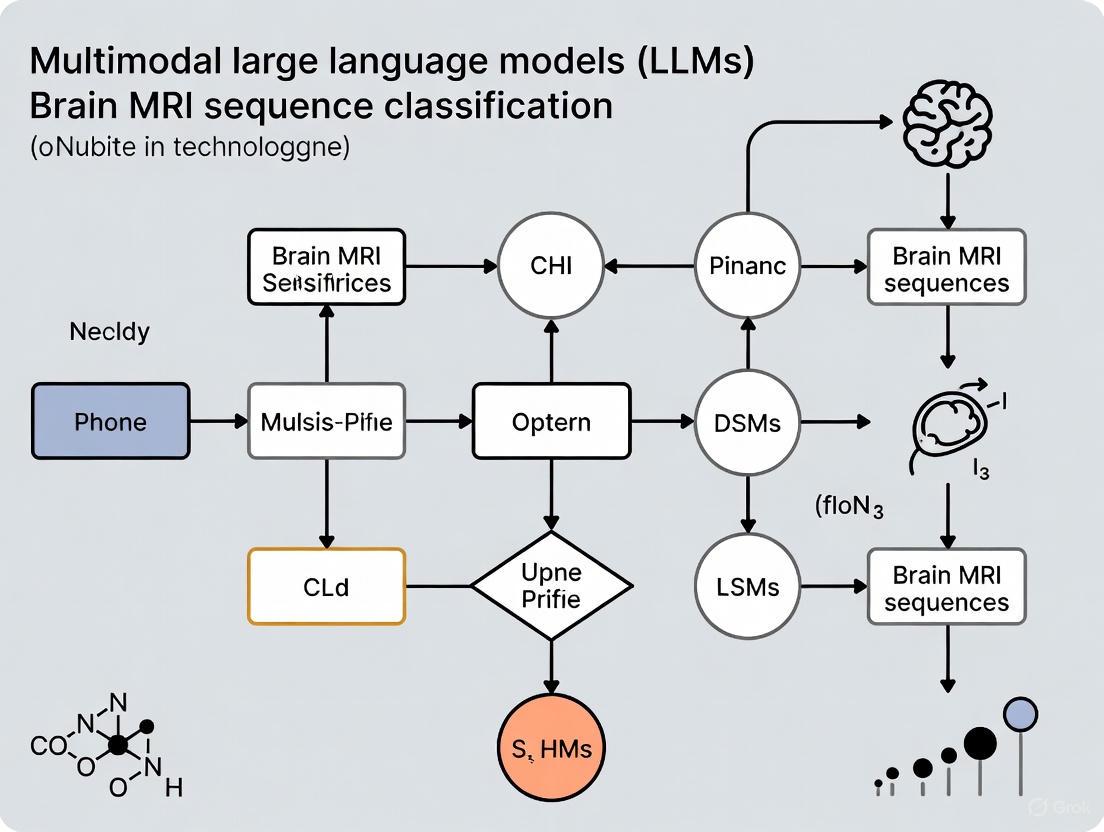
Workflow Visualization for MLLM Evaluation and Application
The following diagram illustrates the logical workflow for evaluating an MLLM on MRI sequence classification, as detailed in the experimental protocols.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 2: Essential Materials for MLLM Research in Brain MRI Classification
| Item Name | Function/Description | Example/Reference |
|---|---|---|
| Multimodal LLMs | Core AI models capable of processing both images and text for classification and query-answering tasks. | ChatGPT-4o (OpenAI), Gemini 2.5 Pro (Google), Claude 4 Opus (Anthropic) [2]. |
| Curated Brain MRI Datasets | High-quality, labeled image sets for model training, testing, and benchmarking. Essential for evaluating domain shift. | Adult glioblastoma cohorts [4], pediatric CNS tumor datasets (e.g., MNP 2.0) [4], the Natural Scenes Dataset (NSD) for fundamental research [5]. |
| Expert Annotators | Radiologists who provide ground truth labels for images and evaluate model outputs, crucial for validation and identifying hallucinations. | Board-certified radiologists performing consensus review [2] [4]. |
| Hybrid Deep Learning Models | Specialized neural networks that combine architectural strengths (e.g., CNNs and Transformers) to handle medical image specifics and domain shift. | MedViT (CNN-Transformer hybrid) [4]. |
| Statistical Analysis Software | Tools for performing rigorous statistical comparisons of model performance and calculating reliability metrics. | SPSS, Python (with scikit-learn for stratified data splitting) [2] [4]. |
| Adherence to WCAG Contrast Guidelines | A framework for ensuring sufficient visual contrast in generated diagrams and outputs, promoting accessibility and clarity. | WCAG 2.1, Contrast Ratio of at least 4.5:1 for normal text [6] [7]. |
The integration of vision and language processing represents a paradigm shift in medical image analysis, particularly for complex tasks such as brain MRI sequence classification. Modern Multimodal Large Language Models (MLLMs) architecturally unify visual information from medical scans with textual context for sophisticated diagnostic reasoning. These systems fundamentally rely on three core components: a vision encoder that processes pixel-level image data, a large language model (LLM) that handles textual understanding and generation, and a connector that creates a semantic bridge between these two modalities. The precision of this integration is especially critical in neuroimaging, where subtle variations in MRI sequences—such as T1-weighted, T2-weighted, FLAIR, and diffusion-weighted imaging—carry distinct clinical significance for diagnosing neurological conditions, brain tumors, and traumatic injuries [2] [8].
Architecturally, MLLMs face the significant challenge of overcoming the inherent modality gap between dense, high-dimensional image data and discrete textual tokens. Current research explores various fusion strategies—early, intermediate, and late fusion—to optimize alignment between visual features and linguistic concepts [9]. In specialized medical applications, these architectures are increasingly evaluated on comprehensive benchmarks like OmniBrainBench, which assesses model performance across 15 brain imaging modalities and 15 multi-stage clinical tasks, from anatomical identification to therapeutic planning [10]. The continuous refinement of these architectural blueprints is essential for developing clinically reliable AI systems that can assist researchers and clinicians in complex diagnostic workflows.
Core Architectural Components
Vision Encoders
Vision encoders serve as the foundational component for processing visual input, transforming raw image pixels into structured, high-dimensional feature representations. In medical MLLMs, vision encoders are typically built upon pre-trained models like Vision Transformers (ViTs) or Convolutional Neural Networks (CNNs), which extract hierarchically organized features from medical images [8] [9]. For brain MRI analysis, specialized encoders such as BioMedCLIP—a vision transformer pre-trained on 15 million biomedical image-text pairs from the PMC dataset—demonstrate enhanced performance by leveraging domain-specific pre-training. This specialized training allows the encoder to recognize clinically relevant patterns in structural MRI data, which is particularly valuable when working with limited annotated medical datasets [8].
The technical implementation often involves processing high-resolution medical images by dividing them into patches, which are then linearly embedded and processed through transformer blocks with self-attention mechanisms. Advanced architectures employ techniques like the AnyRes strategy, which handles variable image resolutions through tiled views with resolution-aware aggregation, crucial for analyzing medical images with diverse aspect ratios and resolutions [11]. For instance, a SigLIP2 vision encoder with patch-16 configuration can process a 384×384 pixel input to produce 576 visual tokens, effectively balancing computational efficiency with feature richness for complex MRI sequence recognition tasks [11].
Connector Modules
Connector modules function as the critical architectural bridge between visual and textual modalities, translating the high-dimensional output from vision encoders into a format comprehensible to language models. These components address the fundamental challenge of modality alignment, ensuring that visual features can effectively inform linguistic reasoning processes [9]. Common connector implementations include lightweight Multi-Layer Perceptrons (MLPs), cross-attention mechanisms, and more sophisticated query-based transformers like Q-Former, which uses learnable query embeddings to extract the most semantically relevant visual features for text generation [9].
The Q-Former architecture, as employed in models like BLIP-2, represents a particularly advanced connector approach, consisting of two transformer submodules: an image transformer for visual feature extraction and a text transformer serving as both encoder and decoder. This architecture employs self-attention layers that allow learnable queries to interact with each other and cross-attention layers that enable interaction with frozen image features, effectively creating a trainable bottleneck that distills the most text-relevant visual information [9]. With approximately 188 million parameters, Q-Former provides a balanced mechanism for modality fusion without requiring full retraining of the vision or language components, making it particularly suitable for medical applications where computational resources may be constrained [9].
Large Language Models
Large Language Models form the reasoning core of multimodal architectures, processing the fused visual-textual representations to generate coherent, contextually appropriate responses. In medical MLLMs, LLMs like PubMedBERT, Qwen, and other transformer-based models provide the linguistic understanding and clinical reasoning capabilities necessary for tasks such as generating radiology reports, answering diagnostic questions, or classifying MRI sequences [11] [8]. These models, often pre-trained on extensive biomedical corpora, bring domain-specific knowledge that enhances their ability to handle specialized medical terminology and clinical concepts.
In unified architectures like SOLO, a single transformer model processes both visual patches and text tokens, eliminating the need for separate encoders and complex fusion mechanisms. This approach simplifies the overall architecture while maintaining competitive performance on medical vision-language tasks [12]. However, most current medical MLLMs maintain a heterogeneous architecture where the LLM component remains primarily frozen or lightly fine-tuned to preserve its linguistic capabilities while adapting to visual inputs through the connector module. This design allows researchers to leverage powerful pre-trained LLMs without the prohibitive computational cost of end-to-end training, making advanced multimodal AI more accessible for clinical research applications [9].
Quantitative Performance Analysis
Table 1: Performance Comparison of Multimodal LLMs on Brain MRI Classification Tasks
| Model | Modality Identification Accuracy | Anatomical Region Accuracy | Imaging Plane Classification | Contrast-Enhancement Status | MRI Sequence Classification |
|---|---|---|---|---|---|
| ChatGPT-4o | 100% | 100% | 100% | 98.46% | 97.69% |
| Gemini 2.5 Pro | 100% | 100% | 100% | 98.46% | 93.08% |
| Claude 4 Opus | 100% | 100% | 99.23% | 95.38% | 73.08% |
Recent comprehensive evaluations of multimodal LLMs on brain MRI analysis reveal significant performance variations across models and tasks. As shown in Table 1, all major proprietary models achieve perfect or near-perfect accuracy in basic recognition tasks including modality identification and anatomical region recognition. However, performance diverges markedly in more complex tasks such as MRI sequence classification, where ChatGPT-4o leads at 97.69% accuracy, followed by Gemini 2.5 Pro at 93.08%, with Claude 4 Opus trailing significantly at 73.08% [2]. This performance gradient underscores the critical importance of specialized architectural optimizations for fine-grained medical image interpretation.
Error analysis reveals consistent patterns in model limitations, with fluid-attenuated inversion recovery (FLAIR) sequences frequently misclassified as T1-weighted or diffusion-weighted sequences across all models. Claude 4 Opus demonstrates particular difficulties with susceptibility-weighted imaging (SWI) and apparent diffusion coefficient (ADC) sequences, suggesting specific weaknesses in its visual processing capabilities for these sequence types [2]. Additionally, Gemini 2.5 Pro exhibits occasional hallucinations, generating clinically irrelevant details such as "hypoglycemia" and "Susac syndrome" without prompt justification, highlighting ongoing challenges in maintaining clinical relevance and avoiding confabulation in diagnostic contexts [2].
Table 2: Domain-Specific vs. General MLLMs on Medical Benchmarks
| Model Category | Example Models | Strengths | Limitations |
|---|---|---|---|
| Medical-Specialized MLLMs | Glio-LLaMA-Vision, BiomedCLIP | Domain-specific pre-training, better clinical alignment | Narrower scope, limited general knowledge |
| General-Purpose MLLMs | GPT-4o, Gemini 2.5 Pro | Broad knowledge base, strong reasoning | Higher hallucination rates in specialized domains |
| Open-Source MLLMs | VARCO-VISION-2.0, SOLO | Customizability, transparency | Lower overall performance on complex clinical tasks |
Beyond sequence classification, specialized medical MLLMs demonstrate promising results on disease-specific diagnostic tasks. For instance, fine-tuned biomedical foundation models achieve high accuracy in headache disorder classification from structural MRI data, with models reaching 89.96% accuracy for migraine versus healthy controls, 88.13% for acute post-traumatic headache (APTH), and 83.13% for persistent post-traumatic headache (PPTH) [8]. Similarly, specialized models like Glio-LLaMA-Vision show robust performance in molecular prediction, radiology report generation, and visual question answering for adult-type diffuse gliomas, providing a practical paradigm for adapting general-domain LLMs to specific medical applications [13]. These results collectively indicate that while general-purpose MLLMs offer strong baseline performance, domain-specific adaptation remains essential for clinically reliable applications.
Experimental Protocols for MRI Sequence Classification
Dataset Preparation and Curation
Protocol for assembling a comprehensive brain MRI dataset begins with collecting images from diverse sources, including clinical PACS systems and public repositories like the IXI dataset. A representative study utilized 130 brain MRI images from adult patients without pathological findings, encompassing 13 standard MRI sequences with 10 images per sequence [2]. Critical sequences should include axial T1-weighted (T1w), axial T2-weighted (T2w), axial fluid-attenuated inversion recovery (FLAIR), coronal FLAIR, sagittal FLAIR, coronal T2w, sagittal T1w, axial susceptibility-weighted imaging (SWI), axial diffusion-weighted imaging (DWI), axial apparent diffusion coefficient (ADC), and contrast-enhanced variants of T1w across multiple planes [2].
Each image must undergo rigorous preprocessing: export in high-quality JPEG format with minimum resolution of 994×1382 pixels, without compression, cropping, or visual post-processing. All annotations, arrows, or textual markings should be removed to prevent model cheating, while preserving original resolution and anatomical proportions [2]. For model evaluation, a standardized selection approach ensures consistency—for each MRI series, a single representative slice should be selected at an anatomical level where critical structures like the lateral ventricles are clearly visible, ensuring each image reflects typical visual characteristics of its respective sequence [2].
Model Training and Fine-tuning Procedures
Effective training protocols for medical MLLMs typically employ multi-stage curricula that progressively build multimodal capabilities. The VARCO-VISION-2.0 training pipeline exemplifies this approach with four distinct stages [11]. Stage 1 involves feature alignment pre-training, where only the connector module (typically an MLP) is trained to project visual features into the language model's embedding space, while both vision encoder and LLM remain frozen. This stage uses filtered image-caption pairs to learn robust input-output alignment without explicit text prompts [11].
Stage 2 advances to basic supervised fine-tuning with all model components trained jointly in single-image settings at relatively low resolutions to reduce computational overhead. This stage focuses on building broad world knowledge and visual-textual understanding through curated captioning datasets covering real-world images, charts, and tables, often with in-house recaptioning to enhance accuracy and consistency [11]. Stage 3 implements advanced supervised fine-tuning with higher-resolution image processing and support for multi-image scenarios. This critical phase expands the dataset to include specialized tasks like document-based question answering with strategies to minimize hallucination, such as creating QA pairs from document text before generating corresponding synthetic images with different templates [11].
Evaluation Metrics and Validation Methods
Comprehensive evaluation protocols for MRI sequence classification employ multiple accuracy metrics across progressively challenging tasks. The primary evaluation should include five distinct classification tasks: imaging modality identification, anatomical region recognition, imaging plane classification, contrast-enhancement status determination, and specific MRI sequence classification [2]. Formal statistical comparisons using Cochran's Q test and pairwise McNemar tests with Bonferroni correction are essential for determining significant performance differences between models, particularly for the primary outcome of sequence classification accuracy [2].
Beyond basic accuracy calculations, robust evaluation should include macro-averaged F1 scores and Cohen's kappa coefficients to assess inter-class performance consistency and agreement with ground truth. For contrast-enhancement classification, binary classification metrics including sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) with corresponding 95% confidence intervals provide a more nuanced performance picture [2]. To ensure evaluation stability, bootstrap resampling (1000 iterations) should be applied with 95% confidence intervals reported for each MRI sequence and model. Additionally, systematic analysis of misclassifications through confusion matrices and error heatmaps reveals consistent patterns of model confusion between specific sequence types [2].
Architectural Workflows and Signaling Pathways
Diagram 1: End-to-End MRI Sequence Classification Workflow. This architecture illustrates the complete pipeline from medical image input to clinical report generation, highlighting the three core components and their interactions.
The architectural workflow for brain MRI sequence classification follows a structured pipeline that transforms raw image data into clinically actionable information. As shown in Diagram 1, the process begins with input images being partitioned into standardized patches, typically 512×512 pixels, which are processed through a vision encoder such as SigLIP2 or BioMedCLIP [11] [8]. These specialized encoders extract hierarchical visual features using transformer architectures pre-trained on biomedical datasets, enabling robust pattern recognition for medical imaging characteristics. The resulting high-dimensional visual feature vectors then pass to the connector module, which performs critical modality alignment functions.
The connector module, implemented as Q-Former or multi-layer perceptron, acts as a feature bottleneck that distills the most semantically relevant visual information for language processing [9]. Through cross-attention mechanisms, the connector creates fused representations in a joint embedding space where visual and textual concepts become aligned. These unified representations are then processed by the large language model component, which leverages its pre-trained linguistic capabilities and biomedical knowledge to perform the final sequence classification. The LLM generates specific sequence identifications (T1w, T2w, FLAIR, etc.) along with confidence assessments, ultimately producing a comprehensive text report that integrates visual findings with clinical context [2] [13].
Research Reagent Solutions
Table 3: Essential Research Tools for Multimodal MRI Research
| Research Tool | Function | Example Implementations |
|---|---|---|
| Vision Encoders | Extracts visual features from medical images | SigLIP2 (patch-16), BioMedCLIP, Vision Transformers (ViT) |
| Connector Modules | Bridges visual and linguistic modalities | Q-Former, MLP Adapters, Cross-Attention Layers |
| Large Language Models | Processes fused representations for reasoning | PubMedBERT, Qwen, LLaMA, GPT series |
| Training Frameworks | Provides infrastructure for model development | Hugging Face Transformers, vLLM, PyTorch |
| Medical Benchmarks | Evaluates model performance on clinical tasks | OmniBrainBench, Brain Tumor VQA, VQA-RAD |
| Data Augmentation Tools | Enhances dataset diversity and size | AnyRes strategy, synthetic data generation |
The development of effective multimodal architectures for brain MRI classification requires a specialized toolkit of research reagents. As detailed in Table 3, these essential components include vision encoders specifically pre-trained on biomedical imagery, such as BioMedCLIP, which provides significant advantages over general-purpose encoders by leveraging contrastive language-image pretraining on 15 million biomedical image-text pairs [8]. Connector modules like Q-Former with approximately 188 million parameters serve as critical bridges between visual and linguistic modalities, using learnable query embeddings to extract the most text-relevant visual information while keeping computational requirements manageable [9].
Specialized training frameworks including Hugging Face Transformers and vLLM provide essential infrastructure for developing and deploying medical MLLMs, ensuring compatibility with established ecosystems while enabling production-scale inference [11]. Comprehensive evaluation benchmarks like OmniBrainBench—covering 15 imaging modalities, 9,527 clinically verified VQA pairs, and 31,706 images—offer rigorous testing environments that simulate real clinical workflows across anatomical identification, disease diagnosis, lesion localization, prognostic assessment, and therapeutic management [10]. Additionally, advanced data augmentation strategies such as the AnyRes technique, which handles variable image resolutions through tiled views with resolution-aware aggregation, help address the data scarcity challenges common in medical imaging research [11].
The Critical Role of Accurate MRI Sequence Classification in Clinical and Research Workflows
Accurate Magnetic Resonance Imaging (MRI) sequence classification is a foundational prerequisite for both advanced clinical workflows and large-scale research. Different MRI sequences, such as T1-weighted (T1w), T2-weighted (T2w), and Fluid-Attenuated Inversion Recovery (FLAIR), provide unique and complementary tissue contrasts essential for diagnosis and quantitative analysis [14]. The absence of standardized naming conventions in DICOM headers, coupled with confounding annotations and institutional protocol variations, frequently renders metadata unreliable [14] [15]. This necessitates labor-intensive manual correction, creating a significant bottleneck. The emergence of sophisticated Artificial Intelligence (AI) methodologies, particularly deep learning and multimodal Large Language Models (LLMs), is poised to revolutionize this domain by enabling precise, automated classification, thereby enhancing diagnostic reliability and accelerating research pipelines.
The Clinical and Research Imperative for Accurate Classification
In clinical practice, erroneous sequence identification can directly impact patient care. The hanging protocol, which automates image arrangement for radiologist review, is entirely dependent on correct sequence labels [15]. Misclassification can lead to misdiagnosis, for instance, by confusing pathology-highlighting sequences like FLAIR with others [2]. In research, especially large multicenter studies, consistent sequence grouping is critical for creating labeled datasets to train robust deep learning models [3] [4]. Inconsistent data confounds analysis and undermines the validity of findings.
A significant challenge is domain shift, where a model trained on data from one source (e.g., adult populations, specific scanner brands) experiences a performance drop when applied to another (e.g., pediatric data, different institutions) [4]. One study demonstrated that a model achieving high accuracy on adult MRI data saw reduced performance when tested on pediatric data, a deficit mitigated by using advanced hybrid architectures and expert domain knowledge to adjust for protocol differences [4].
Quantitative Performance of Modern Classification Approaches
Modern approaches for MRI sequence classification primarily involve Convolutional Neural Networks (CNNs) and Multimodal Large Language Models (MLLMs). The table below summarizes the performance of various state-of-the-art methods as reported in recent literature.
Table 1: Performance of Automated MRI Sequence Classification Models
| Model / Approach | Reported Accuracy | Key Strengths | Test Context |
|---|---|---|---|
| MRISeqClassifier (Deep Learning Toolkit) [14] | 99% | Highly efficient with small, unrefined datasets; uses lightweight models & ensemble voting. | Brain MRI |
| ChatGPT-4o (Multimodal LLM) [2] | 97.7% | High accuracy in sequence, plane, and contrast-status classification. | Brain MRI |
| Gemini 2.5 Pro (Multimodal LLM) [2] | 93.1% | Excellent performance, but noted for occasional clinical hallucinations. | Brain MRI |
| Claude 4 Opus (Multimodal LLM) [2] | 73.1% | Lower performance, struggled with SWI and ADC sequences. | Brain MRI |
| MedViT (CNN-Transformer Hybrid) [4] | 89.3% - 90.5% | Superior robustness against domain shift (e.g., adult to pediatric data). | Multicenter Brain MRI |
| 3D DenseNet-121 Ensemble [15] | F1: 99.5% (Siemens)F1: 86.5% (Philips, OOD) | High performance on vendor-specific data; OOD robustness. | Body MRI (Chest, Abdomen, Pelvis) |
| GPT-4-based LLM Classifier [3] | 0.83 (Accuracy) | Provides interpretable classifications, enhancing transparency. | Brain MRI |
Analysis of Model Performance
The data reveals that specialized deep learning models like MRISeqClassifier and 3D DenseNet-121 can achieve exceptional accuracy (exceeding 99%) in controlled or vendor-specific environments [14] [15]. However, their performance can degrade on out-of-distribution (OOD) data, as seen with the drop in F1 score on Philips scanner data, highlighting the domain shift challenge [15].
Among multimodal LLMs, performance varies significantly. ChatGPT-4o demonstrates remarkable capability, nearing the performance of specialized models [2]. A critical caveat with LLMs is the phenomenon of hallucination, where models generate plausible but incorrect information, such as inventing irrelevant clinical details [2]. This underscores the necessity for expert human oversight in clinical applications.
Experimental Protocols for MRI Sequence Classification
To ensure reproducible and valid results, adherence to standardized experimental protocols is essential. The following sections detail key methodologies.
Protocol A: Evaluating Multimodal LLMs on Brain MRI
This protocol is adapted from a comparative analysis of LLMs [2].
Dataset Curation:
- Source: Collect images from a Picture Archiving and Communication System (PACS).
- Content: Include 130 brain MRI images from adult patients without pathological findings.
- Sequences: Ensure representation of 13 standard series (e.g., Axial T1w, T2w, FLAIR; Coronal/Sagittal FLAIR; SWI; DWI; ADC; contrast-enhanced T1w in multiple planes).
- Selection Criteria: Choose a single representative slice per series where anatomical landmarks (e.g., lateral ventricles) are clearly visible.
- Format: Export images as high-quality JPEG without compression, cropping, annotations, or post-processing.
Model Prompting and Evaluation:
- Setup: Use a zero-shot prompting approach in a new chat session for each image to prevent in-context adaptation.
- Standardized Prompt: > "This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: 1. What type of radiological modality is this examination? 2. Which anatomical region does this examination cover? 3. What is the imaging plane (axial, sagittal, or coronal)? 4. Is this a contrast-enhanced image or not? 5. If this image is an MRI, what is the specific MRI sequence? If it is not an MRI, write 'Not applicable.' Please number your answers clearly."
- Ground Truth: Two radiologists independently review and classify LLM responses as "correct" or "incorrect" in consensus.
- Metrics: Calculate accuracy for all tasks. For sequence classification (the primary outcome), use Cochran's Q test for overall comparison and pairwise McNemar tests with Bonferroni correction. Also compute macro-averaged F1 scores and Cohen’s kappa.
Figure 1: LLM evaluation workflow for brain MRI sequence classification.
Protocol B: Training a Deep Learning Model for Multicenter Data
This protocol addresses the challenge of domain shift, as explored in recent studies [4].
Data Preparation and Preprocessing:
- Training Data: Utilize a large, retrospective multicenter brain MRI dataset (e.g., 63,327 sequences from 2179 patients across 249 hospitals).
- Classes: Define sequence classes for training (e.g., T1, T2, CT1, FLAIR, ADC, SWI, DWI variants, T2*/DSC).
- Test Data: Use a separate dataset introducing domain shift (e.g., a pediatric CNS tumor MRI dataset from 51 centers).
- Preprocessing: Resize images (e.g., 200x200 pixels). Apply data augmentation (e.g., Gaussian noise). Normalize intensity. For 3D models, copy the midslice to all three RGB channels if required by the architecture.
Model Training and Expert Adjustment:
- Architecture Selection: Compare a benchmark CNN (e.g., ResNet-18) against a hybrid CNN-Transformer model (e.g., MedViT).
- Training: Use stratified sampling for train/validation splits. Train with Adam optimizer, cross-entropy loss, and class weights to handle imbalance.
- Expert Domain Knowledge Integration: Analyze the target test dataset. If it contains fewer sequence classes than the training data, adjust the model's final classification layer or decision-making process to ignore unused classes, aligning the task with the new domain.
Table 2: Key Research Reagents and Computational Tools
| Item / Resource | Function / Description | Application Example |
|---|---|---|
| MRISeqClassifier [14] | A deep learning toolkit tailored for small, unrefined MRI datasets. | Precise sequence classification with high data efficiency. |
| MedViT [4] | A hybrid CNN-Transformer architecture for medical image classification. | Handling domain shift in multicenter studies. |
| ResNet-18/50/101 [4] [15] | Convolutional Neural Networks for image feature extraction and classification. | Benchmark models for sequence classification tasks. |
| 3D DenseNet-121 [15] | A 3D convolutional network ensemble for volumetric data. | Body MRI sequence classification. |
| Multimodal LLMs (ChatGPT-4o, etc.) [2] | Pre-trained models capable of joint image-text understanding and zero-shot classification. | Direct image-based classification without task-specific training. |
| PyTorch / MONAI [4] | Open-source frameworks for deep learning in healthcare imaging. | Model development, training, and data augmentation. |
Figure 2: Deep learning training protocol to handle domain shift.
Accurate MRI sequence classification is a critical enabler for modern radiology and computational research. While specialized deep learning models offer high precision, their vulnerability to domain shift requires strategic mitigation through advanced architectures like MedViT and the incorporation of expert knowledge. Multimodal LLMs, particularly ChatGPT-4o, present a powerful, flexible alternative with impressive zero-shot performance, though their potential for hallucination necessitates rigorous validation and clinical oversight. The future of this field lies in leveraging the respective strengths of these technologies—combining the robustness of purpose-built models with the adaptability and intuitive reasoning of LLMs—to build fully reliable, automated workflows that enhance diagnostic confidence and fuel scientific discovery.
Multimodal Large Language Models (MLLMs) represent a significant evolution in medical artificial intelligence, extending traditional text-based LLMs by integrating and processing diverse data modalities including medical images, clinical notes, and electronic health records [1]. In medical imaging, these models combine large language models with advanced computer vision modules, mapping heterogeneous data into a shared representational space to enable comprehensive understanding of clinical contexts [1]. This technological advancement is particularly transformative for visually intensive disciplines like radiology, where MLLMs demonstrate promising capabilities in tasks ranging from automatic radiology report generation to visual question answering and interactive diagnostic support [1] [2]. The rapid development of MLLMs reflects several converging technological innovations: the evolution of transformer-based LLMs, parallel advances in vision transformers (ViTs) for medical imaging modalities, sophisticated multimodal learning strategies, and the availability of high-performance computing infrastructure [1]. This review comprehensively examines the current state-of-the-art MLLMs in medical imaging, with particular focus on their application to brain MRI sequence classification research, providing structured analysis of quantitative performance, experimental methodologies, and practical implementation frameworks.
Technical Foundations of Medical MLLMs
Architectural Paradigms
MLLM architectures typically comprise four key components: modality-specific encoders, a multimodal connector, a pre-trained LLM backbone, and optional generative modules [1]. The encoders transform high-dimensional inputs (e.g., images) into streamlined feature representations, with contrastive language-image pre-training (CLIP) being a popular choice for aligning visual data with textual descriptions [1]. The multimodal connector serves as a critical learnable interface that bridges the modality gap between non-text data and natural language, and can be categorized into four main types:
- Projection-based connectors employ multi-layer perceptrons (MLPs) to transform visual data into representations alignable with language [1].
- Query-based connectors utilize specialized trainable "query tokens" to extract salient visual details from images [1].
- Fusion-based connectors facilitate feature-level integration through cross-attention mechanisms, establishing direct interactions between visual and language representations [1].
- Expert-driven language transformations convert non-linguistic data directly into text through specialized models, though this approach risks information loss for complex data [1].
The pre-trained LLM serves as the "cognitive engine," maintaining its text-centric reasoning capabilities while processing the aligned multimodal inputs [1].
Training Strategies
Medical MLLMs are typically developed through three sequential stages [1]:
- Pre-training: The multimodal connector learns to align visual and textual representations, often using autoregressive captioning on image-text pairs. Selective fine-tuning of the vision encoder enables more precise cross-modal alignment [1].
- Instruction Tuning: The model is fine-tuned using datasets containing diverse natural language instructions and multimodal inputs, teaching it to follow complex clinical directives reliably. This stage often employs parameter-efficient methods like Low-Rank Adaptation (LoRA) [1] [16].
- Alignment Tuning: The model's outputs are optimized to better reflect human clinical preferences, typically through reinforcement learning from human feedback (RLHF), helping reduce hallucination risks and improve response quality [1].
Performance Benchmarking in Brain MRI Analysis
Quantitative Comparison of State-of-the-Art MLLMs
Recent comparative studies have evaluated the performance of advanced MLLMs on fundamental brain MRI interpretation tasks, with particular focus on sequence classification accuracy. The table below summarizes key performance metrics from a comprehensive evaluation using 130 brain MRI images across 13 standard sequences [2] [17].
Table 1: Performance Comparison of General-Purpose MLLMs on Brain MRI Classification Tasks
| Model | Modality Identification | Anatomical Region Recognition | Imaging Plane Classification | Contrast-Enhancement Status | MRI Sequence Classification |
|---|---|---|---|---|---|
| ChatGPT-4o | 130/130 (100%) | 130/130 (100%) | 130/130 (100%) | 128/130 (98.46%) | 127/130 (97.69%) |
| Gemini 2.5 Pro | 130/130 (100%) | 130/130 (100%) | 130/130 (100%) | 128/130 (98.46%) | 121/130 (93.08%) |
| Claude 4 Opus | 130/130 (100%) | 130/130 (100%) | 129/130 (99.23%) | 124/130 (95.38%) | 95/130 (73.08%) |
Statistical analysis revealed significant differences in MRI sequence classification accuracy (p < 0.001), with ChatGPT-4o demonstrating superior performance (97.69%) followed closely by Gemini 2.5 Pro (93.08%), while Claude 4 Opus trailed substantially (73.08%) [2]. The most frequent misclassifications involved fluid-attenuated inversion recovery (FLAIR) sequences, often confused with T1-weighted or diffusion-weighted sequences [2]. Claude 4 Opus showed particular difficulties with susceptibility-weighted imaging (SWI) and apparent diffusion coefficient (ADC) sequences [2].
Domain-Specific Medical MLLMs
Beyond general-purpose models, several specialized medical MLLMs have demonstrated advanced capabilities in brain image analysis:
Table 2: Performance of Domain-Specific MLLMs in Medical Imaging Tasks
| Model | Specialization | Key Innovation | Reported Performance |
|---|---|---|---|
| BrainGPT [18] | 3D Brain CT Report Generation | Clinical Visual Instruction Tuning (CVIT) | FORTE F1-score: 0.71; 74% of reports indistinguishable from human-written ground truth in Turing test |
| Infi-Med-3B [16] | General Medical Reasoning | Resource-efficient fine-tuning with 150K medical data | Matches or surpasses larger SOTA models (Qwen2.5-VL-7B, InternVL3-8B) while using only 3B parameters |
| Glio-LLaMA-Vision [13] | Glioma Analysis | Adapted from general-domain LLMs for specific medical domain | Promising performance in molecular subtype prediction, radiology report generation, and VQA for adult-type diffuse gliomas |
| VGRefine [19] | Medical Visual Grounding | Inference-time attention refinement | State-of-the-art performance across 6 diverse Med-VQA benchmarks (over 110K VQA samples) without additional training |
Specialized models like BrainGPT address unique challenges in volumetric medical image interpretation through innovative approaches like Clinical Visual Instruction Tuning (CVIT), which enhances medical domain knowledge by incorporating structured clinical-defined QA templates and categorical keyword guidelines [18]. The Infi-Med framework demonstrates that resource-efficient approaches with careful data curation can achieve competitive performance while reducing computational demands [16].
Experimental Protocols for Brain MRI Sequence Classification
Standardized Evaluation Methodology
A rigorously validated experimental protocol for benchmarking MLLM performance on brain MRI sequence classification has been established in recent literature [2] [17]:
Dataset Curation:
- Collect 130 brain MRI images from adult patients without pathological findings
- Include 13 representative MRI sequences: axial T1-weighted (T1w), axial T2-weighted (T2w), axial FLAIR, coronal FLAIR, sagittal FLAIR, coronal T2w, sagittal T1w, axial SWI, axial DWI, axial ADC, contrast-enhanced axial T1w, contrast-enhanced coronal T1w, and contrast-enhanced sagittal T1w
- Select a single representative slice for each series at an anatomical level where lateral ventricles are clearly visible
- Export images in high-quality JPEG format (minimum resolution: 994 × 1382 pixels) without compression, cropping, or visual post-processing
- Ensure no annotations, arrows, or textual markings are present on images
Experimental Procedure:
- Upload each image individually using official web interfaces of respective MLLMs
- Utilize a standardized English prompt in a zero-shot setting: "This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: What type of radiological modality is this examination? Which anatomical region does this examination cover? What is the imaging plane (axial, sagittal, or coronal)? Is this a contrast-enhanced image or not? If this image is an MRI, what is the specific MRI sequence? If it is not an MRI, write 'Not applicable.' Please number your answers clearly."
- Initiate a new session for each prompt by clearing chat history to prevent in-context adaptation
- Conduct all evaluations within a defined timeframe using the most up-to-date model versions available
Outcome Measures and Statistical Analysis:
- Primary outcome: MRI sequence classification accuracy
- Secondary outcomes: accuracy in modality identification, anatomical region recognition, imaging plane classification, and contrast-enhancement status determination
- Calculate accuracy as the proportion of correct responses
- Analyze differences in model performance for MRI sequence classification using Cochran's Q test for overall comparison, followed by pairwise McNemar tests with Bonferroni correction where appropriate
- Compute macro-averaged F1 scores and Cohen's kappa coefficients to evaluate inter-class performance consistency and agreement with ground truth
- Perform bootstrap resampling (1000 iterations) to provide stability estimates for sequence-specific accuracy
Specialized Assessment Frameworks
For comprehensive evaluation of radiology report generation, the Feature-Oriented Radiology Task Evaluation (FORTE) framework provides a structured approach to assess clinical essence beyond traditional metrics [18]. FORTE evaluates four essential keyword components in diagnostic radiology sentences: degree, landmark, feature, and impression [18]. The protocol involves:
- Sentence Pairing: Decompose multisentence paragraphs into smaller semantic granularity to relieve sequential constraints between report input and generated output
- Negation Removal: Filter out irrelevant image descriptions to enhance alignment between generated content and evaluation scores
- Structured Keyword Extraction: Assess medical content through a categorized system that addresses multi-semantic context, recognizes synonyms, and enables transferability across modalities
Visualization of MLLM Architectures and Workflows
Typical MLLM Architecture for Medical Imaging
MLLM Training Pipeline
Brain MRI Sequence Classification Workflow
Critical Datasets for Medical MLLM Research
Table 3: Essential Datasets for Medical MLLM Development and Evaluation
| Dataset | Modalities | Body Organ | Primary Use Cases | Sample Size |
|---|---|---|---|---|
| 3D-BrainCT [18] | 3D CT, Text Reports | Brain | 3D CT report generation, Visual instruction tuning | 18,885 text-scan pairs |
| BraTS [20] | MRI (T1, T2, T1c, FLAIR) | Brain | Brain tumor segmentation & classification | Yearly updates (2012-2023) |
| ADNI [20] | sMRI, fMRI, PET | Brain | Alzheimer's disease classification | Longitudinal data (2004-2027) |
| MIMIC-CXR [16] | Chest X-ray, Reports | Chest | Radiology report generation, VQA | Large-scale (varies) |
| VQA-RAD [16] | Medical Images, QA Pairs | Multiple | Visual question answering | 11,000+ questions |
| MultiMedBench [16] | Multimodal Clinical Data | Multiple | Multimodal data synthesis, Reasoning | Comprehensive |
Computational Frameworks and Model Architectures
Foundation Models:
- LLaVA-Med: Specialized for biomedical domains, demonstrating success in single-slice CT and X-ray report generation [18]
- Med-PaLM Multimodal: Google Research's model showing preliminary success in medical multimodal tasks [18]
- Otter: General foundation model that can be adapted for medical use through clinical visual instruction tuning [18]
Evaluation Frameworks:
- FORTE (Feature-Oriented Radiology Task Evaluation): Specialized evaluation system that captures clinical essence by assessing degree, landmark, feature, and impression components in generated reports [18]
- Traditional NLP Metrics: BLEU, METEOR, ROUGE-L, CIDEr - though these show limited correlation with clinical quality [18]
- Clinical Consistency Metrics: Turing-test like evaluations with physician raters, keyword recall rates, and negation removal analysis [18]
Implementation Tools:
- Low-Rank Adaptation (LoRA): Parameter-efficient fine-tuning method that reduces computational demands while maintaining performance [1] [16]
- Reinforcement Learning from Human Feedback (RLHF): Critical for aligning model outputs with clinical preferences and reducing hallucinations [1]
- Chain-of-Thought (CoT) Annotations: Enhance model reasoning capabilities through step-by-step reasoning processes [16]
Application Notes for Brain MRI Sequence Classification Research
Practical Implementation Considerations
Data Preprocessing Protocols:
- Ensure high-quality image exports (minimum 994 × 1382 pixels) without compression artifacts
- Maintain original resolution and anatomical proportions
- Implement rigorous anonymization procedures to remove patient identifiers
- Standardize image selection criteria (e.g., clear visualization of lateral ventricles for brain MRI)
- Establish ground truth labeling through consensus reading by multiple expert radiologists
Model Selection Guidelines:
- For sequence classification tasks: ChatGPT-4o demonstrates highest accuracy (97.69%) based on current evidence [2]
- For resource-constrained environments: Consider specialized smaller models like Infi-Med-3B that maintain competitive performance [16]
- For 3D volume analysis: BrainGPT with Clinical Visual Instruction Tuning provides specialized capability for volumetric data [18]
- For visual grounding tasks: Implement attention refinement approaches like VGRefine to address inadequate visual grounding in medical images [19]
Limitations and Mitigation Strategies
Hallucination Management: Recent studies report concerning instances of model hallucinations, including Gemini 2.5 Pro generating irrelevant clinical details such as "hypoglycemia" and "Susac syndrome" without supporting image evidence [2]. Mitigation strategies include:
- Implementation of alignment tuning with clinical expert feedback
- Incorporation of uncertainty quantification in model outputs
- Development of hybrid systems that combine MLLMs with traditional computer vision approaches for verification
- Establishing rigorous human-in-the-loop validation protocols for clinical deployment
Visual Grounding Enhancement: Systematic investigations reveal that medical MLLMs often fail to ground their predictions in clinically relevant image regions, unlike their performance with natural images [19]. The VGRefine method addresses this through inference-time attention distribution refinement, achieving state-of-the-art performance across diverse Med-VQA benchmarks without requiring additional training [19].
Evaluation Methodologies: Traditional NLP metrics frequently fail to capture clinical essence and show poor correlation with diagnostic quality [18]. The FORTE framework provides a structured alternative focusing on clinical relevance through categorized keyword extraction that addresses multi-semantic context, recognizes synonyms, and enables transferability across imaging modalities [18].
Future Research Directions
The evolution of medical MLLMs for brain MRI analysis will likely focus on several critical frontiers: developing robust foundation models pre-trained on large-scale medical datasets, incorporating region-grounded reasoning to link model outputs to specific image regions, establishing comprehensive evaluation frameworks that better capture clinical utility, and creating strategies for safe effective integration into clinical workflows [1]. Particular attention should be directed toward overcoming current limitations in 3D medical image interpretation, enhancing visual grounding capabilities, and reducing hallucination risks through improved training methodologies and validation frameworks [18] [19]. As these technologies mature, rigorous clinical validation and thoughtful implementation will be essential to realizing their potential as trusted AI partners in medical imaging.
Implementing MLLMs: From Protocol Selection to Automated Report Generation
Multimodal large language models (MLLMs) represent a transformative advancement in artificial intelligence, capable of processing and interpreting both visual and textual data. Within the specialized domain of brain MRI sequence classification, two distinct methodological paradigms have emerged: zero-shot prompting of generalist foundation models and the deployment of fine-tuned specialist models. Zero-shot prompting leverages the broad capabilities of pre-trained models without additional task-specific training, while fine-tuning adapts these models to specialized domains through targeted training on curated datasets. This article examines both approaches within the context of brain MRI research, providing a comprehensive analysis of their comparative strengths, limitations, and optimal application scenarios.
Performance Comparison in Brain MRI Classification
Quantitative Performance Metrics
Recent comparative studies reveal significant performance differences between zero-shot and fine-tuned approaches across various brain MRI classification tasks. The table below summarizes key findings from empirical evaluations:
Table 1: Performance comparison of LLM approaches in brain MRI classification tasks
| Model Type | Specific Model | Task Description | Performance Metric | Result |
|---|---|---|---|---|
| Zero-Shot MLLM | ChatGPT-4o | MRI sequence classification | Accuracy | 97.69% [2] |
| Zero-Shot MLLM | Gemini 2.5 Pro | MRI sequence classification | Accuracy | 93.08% [2] |
| Zero-Shot MLLM | Claude 4 Opus | MRI sequence classification | Accuracy | 73.08% [2] |
| Fine-Tuned Specialist | Japanese BERT (Fine-tuned) | Brain MRI report classification | Accuracy | 97.00% [21] |
| Fine-Tuned Specialist | Brainfound | Automatic report generation | FORTE F1-Score | 0.71 [18] |
| Fine-Tuned Specialist | Brainfound | Multiple-choice questions | Accuracy advantage over GPT-4V | +47.68% [22] |
| Fine-Tuned Specialist | FG-PAN | Zero-shot brain tumor subtype classification | State-of-the-art performance | Achieved [23] |
Task-Specific Performance Analysis
The performance gap between approaches varies significantly based on task complexity. For fundamental recognition tasks including modality identification, anatomical region recognition, and imaging plane classification, zero-shot models achieve near-perfect accuracy (99-100%) comparable to specialist models [2]. However, for more specialized tasks such as specific MRI sequence classification and clinical report generation, fine-tuned models demonstrate superior performance, particularly in capturing domain-specific nuances and clinical terminology [2] [18].
Notably, zero-shot models exhibit specific weakness patterns in brain MRI classification. The most frequent misclassifications involve distinguishing between fluid-attenuated inversion recovery (FLAIR) sequences and T1-weighted or diffusion-weighted sequences [2]. Furthermore, models like Claude 4 Opus show particular difficulties with susceptibility-weighted imaging (SWI) and apparent diffusion coefficient (ADC) sequences [2].
Experimental Protocols
Protocol 1: Zero-Shot Evaluation of Multimodal LLMs for MRI Sequence Classification
This protocol outlines the methodology for assessing pre-trained multimodal LLMs on brain MRI sequence classification without additional training [2].
Table 2: Research reagents and materials for zero-shot MRI classification
| Item | Specification | Purpose |
|---|---|---|
| Brain MRI Dataset | 130 images, 13 standard MRI series from adult patients without pathological findings | Evaluation benchmark |
| Model Interfaces | Official web interfaces of ChatGPT-4o, Claude 4 Opus, Gemini 2.5 Pro | Model access |
| Standardized Prompt | Predefined English text with specific questions about modality, anatomy, plane, contrast, sequence | Consistent evaluation |
| Statistical Analysis | Cochran's Q test, McNemar test with Bonferroni correction | Performance comparison |
Procedure:
Dataset Curation:
- Select 130 brain MRI images representing 13 standard MRI series (including axial T1-weighted, T2-weighted, FLAIR, SWI, DWI, ADC, and contrast-enhanced variants)
- Ensure images are from adult patients without pathological findings
- Export images in high-quality JPEG format (minimum resolution: 994 × 1382 pixels) without compression, cropping, or annotations [2]
Model Setup:
- Access each model (ChatGPT-4o, Claude 4 Opus, Gemini 2.5 Pro) through their official web interfaces
- Initiate new sessions for each prompt to prevent in-context adaptation [2]
Prompting Strategy:
- Use standardized zero-shot prompt: "This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: What type of radiological modality is this examination? Which anatomical region does this examination cover? What is the imaging plane (axial, sagittal, or coronal)? Is this a contrast-enhanced image or not? If this image is an MRI, what is the specific MRI sequence? If it is not an MRI, write 'Not applicable.' Please number your answers clearly." [2]
Evaluation:
- Two radiologists independently review and classify responses as "correct" or "incorrect" through consensus
- Define hallucinations as statements unrelated to the input image or prompt context
- Calculate accuracy for each classification task
- Perform statistical analysis using Cochran's Q test for overall comparison and McNemar tests with Bonferroni correction for pairwise comparisons [2]
Figure 1: Zero-shot evaluation workflow for MRI sequence classification
Protocol 2: Fine-Tuning Specialist Models for Brain MRI Report Classification
This protocol details the methodology for creating specialist models through fine-tuning on domain-specific data, adapted from approaches used for brain MRI report classification [21] and foundation model development [18] [22].
Table 3: Research reagents and materials for fine-tuning specialist models
| Item | Specification | Purpose |
|---|---|---|
| Base Model | Pretrained Japanese BERT (110M parameters) or similar foundation model | Starting point for fine-tuning |
| Training Dataset | 759 brain MRI reports (nontumor, posttreatment, pretreatment tumor cases) | Task-specific training |
| Validation Dataset | 284 brain MRI reports | Hyperparameter tuning |
| Test Dataset | 164 brain MRI reports | Final evaluation |
| Computational Resources | Workstation with NVIDIA GeForce RTX 3090 GPU, 128GB RAM | Model training |
| Fine-tuning Framework | Python 3.10.13, Transformers library 4.35.2 | Implementation environment |
Procedure:
Dataset Preparation:
- Collect brain MRI reports from Picture Archiving and Communication System (PACS) and teaching file systems
- Categorize reports into three groups: nontumor (group 1), posttreatment tumor (group 2), and pretreatment tumor (group 3)
- Divide data into training (759 reports), validation (284 reports), and test (164 reports) sets
- Ensure reports are anonymized and contain no personal data [21]
Model Configuration:
- Initialize with pretrained base model (e.g., BERT-base-Japanese with 12 layers, 768 hidden dimensions, 12 attention heads)
- Configure model for sequence classification using AutoModelForSequenceClassification class
- Set hyperparameters empirically based on validation performance (e.g., 10 epochs) [21]
Fine-Tuning Process:
- Conduct multiple training sessions (e.g., 15 repetitions) with same hyperparameters to account for randomness
- Fine-tune model on training dataset, validating after each epoch
- Select final model based on highest performance on validation dataset [21]
Evaluation:
- Assess selected model on independent test dataset
- Compare model performance against human radiologists (6 and 1 years of experience)
- Measure time required for classification task
- Use McNemar test to compare sensitivity, specificity, and accuracy between model and human readers [21]
Figure 2: Fine-tuning protocol for specialist model development
The Scientist's Toolkit: Essential Research Reagents
Implementing effective brain MRI classification systems requires carefully selected resources and methodologies. The following table catalogs essential research reagents and their applications:
Table 4: Essential research reagents for brain MRI classification research
| Category | Item | Specification/Example | Application |
|---|---|---|---|
| Datasets | Brain MRI Images | 130 images, 13 sequences, normal findings [2] | Zero-shot evaluation |
| Brain MRI Reports | 759 training, 284 validation, 164 test reports [21] | Fine-tuning specialist models | |
| BraTS 2020 | Multi-modal MRI scans with expert annotations [24] | Glioma classification benchmarks | |
| 3D-BrainCT | 18,885 text-scan pairs [18] | 3D report generation training | |
| BrainCT-3M & BrainMRI-7M | 3M CT and 7M MRI images with reports [22] | Large-scale foundation model training | |
| Models | General MLLMs | ChatGPT-4o, Claude 4 Opus, Gemini 2.5 Pro [2] | Zero-shot classification |
| Fine-tuned Specialists | Brainfound, BrainGPT, FG-PAN [18] [22] [23] | Domain-specific applications | |
| Vision-Language Models | CLIP, FLAVA, ALIGN [23] | Zero-shot classification backbone | |
| Evaluation Metrics | Traditional NLP | BLEU, METEOR, ROUGE [18] | Report quality assessment |
| Clinical Evaluation | FORTE (Feature-Oriented Radiology Task Evaluation) [18] | Clinical essence measurement | |
| Statistical Tests | Cochran's Q, McNemar tests [2] | Performance comparison |
Discussion and Implementation Guidelines
Approach Selection Framework
The choice between zero-shot and fine-tuned approaches depends on several factors, including task complexity, data availability, and performance requirements. The following diagram illustrates the decision process for selecting the appropriate methodological approach:
Figure 3: Decision framework for selecting methodological approaches
Performance and Resource Trade-offs
The selection between methodological approaches involves balancing multiple factors:
Zero-Shot Prompting Advantages:
- Immediate deployment without training requirements [2]
- Lower computational costs and infrastructure needs
- Broad generalization across diverse task types [2]
- Access to cutting-edge capabilities through API-based models
Fine-Tuned Specialist Advantages:
- Superior performance on specialized tasks (up to 97.69% vs. 73.08% for complex sequence classification) [2] [21]
- Reduced hallucinations and improved clinical reliability [2] [18]
- Domain-specific optimization for particular use cases [22] [23]
- Data efficiency once fine-tuned, with potential for continuous improvement
Emerging Trends and Future Directions
Recent research indicates several promising developments in both approaches:
Advanced Fine-Tuning Techniques: Methods like Clinical Visual Instruction Tuning (CVIT) demonstrate significant improvements in generating clinically sensible reports, with BrainGPT achieving a 0.71 FORTE F1-score and 74% of reports being indistinguishable from human-written ground truth [18].
Hybrid Approaches: Frameworks like FG-PAN combine zero-shot classification with fine-grained patch-text alignment, achieving state-of-the-art performance in brain tumor subtype classification without extensive labeled data [23].
Foundation Model Scaling: Evidence suggests that simply scaling model size improves alignment with human brain activity more than instruction tuning, indicating the importance of architectural decisions in model development [25].
The methodological divide between zero-shot prompting and fine-tuned specialist models represents a fundamental consideration in developing AI systems for brain MRI sequence classification. Zero-shot approaches offer practicality and broad applicability for fundamental recognition tasks, while fine-tuned specialists deliver superior performance for complex, clinically significant classification challenges. The optimal approach depends on specific use case requirements, with emerging hybrid methodologies offering promising pathways to leverage the strengths of both paradigms. As multimodal LLMs continue to evolve, the strategic selection and implementation of these methodological approaches will play a crucial role in advancing brain MRI research and clinical applications.
Automating MRI Protocol Selection and Design with Multi-Agent LLM Systems
The integration of Large Language Models into radiology represents a paradigm shift, moving beyond narrative report generation to tackle complex, procedural tasks. The automation of Magnetic Resonance Imaging protocol selection and design, a critical yet time-consuming process in the clinical workflow, stands as a prime candidate for this transformation. Traditional protocoling consumes a significant portion of radiologists' time—approximately 6.2% to 17% of their work shift—and is prone to human error, with studies indicating that over 37% of protocoling-related issues are amenable to automation [26] [27]. Early machine learning approaches demonstrated feasibility but often struggled with institutional specificity and the nuanced reasoning required for protocol selection. The advent of Multimodal LLMs and sophisticated AI architectures, particularly Multi-Agent LLM Systems, now offers a path toward more intelligent, context-aware, and autonomous solutions. These systems can process complex clinical indications, integrate institutional guidelines, and even generate pulse sequences, thereby promising to enhance efficiency, standardize protocols, reduce errors, and free up expert radiologists for higher-level diagnostic duties. This document outlines the application notes and experimental protocols for implementing such systems, with a specific focus on brain MRI within the broader context of multimodal LLM research for sequence classification.
Research into AI-driven MRI protocoling spans traditional machine learning, convolutional neural networks, and the latest large language models. The tables below summarize the performance of various approaches, providing a benchmark for the current state of the technology.
Table 1: Performance of Traditional Machine Learning and Deep Learning Models in Automated Protocoling
| Model Type | Modality | Task | Dataset Size | Number of Protocols/Sequences | Reported Accuracy | Citation |
|---|---|---|---|---|---|---|
| Support Vector Machine | MRI & CT | Protocol Selection | ~700,000 reports | 293 (MRI) | 86.9% (MRI) | [28] |
| Convolutional Neural Network | Prostate MRI | DCE Sequence Decision | 300 training, 100 validation | Binary (bpMRI vs. mpMRI) | AUC: 0.88 | [29] |
| ResNet-18 | Brain MRI | Sequence Classification | 10,771 exams, 43,601 MRIs | 9 sequence classes | Benchmark for domain shift | [4] |
| MedViT (CNN-Transformer) | Brain MRI | Sequence Classification under Domain Shift | 10,771 exams (Adult) → 2,383 (Pediatric) | 6 sequence classes | 0.905 (after expert adjustment) | [4] |
Table 2: Performance of Large Language Models in MRI Protocoling and Sequence Recognition
| Model | Task | Key Enhancement | Performance | Comparison | Citation |
|---|---|---|---|---|---|
| GPT-4o | Brain MRI Sequence Recognition | Zero-shot prompting | 97.7% sequence accuracy | Outperformed other MLLMs | [17] |
| Gemini 2.5 Pro | Brain MRI Sequence Recognition | Zero-shot prompting | 93.1% sequence accuracy | Occasional hallucinations | [17] |
| Claude 4 Opus | Brain MRI Sequence Recognition | Zero-shot prompting | 73.1% sequence accuracy | Lower accuracy on SWI/ADC | [17] |
| GPT-4o | Neuroradiology Protocol Selection | Retrieval-Augmented Generation (RAG) | 81% sequence prediction accuracy | Matched radiologists (81% ± 0.21, P=0.43) | [27] |
| LLaMA 3.1 405B | Neuroradiology Protocol Selection | Retrieval-Augmented Generation (RAG) | 70% sequence prediction accuracy | Lower than GPT-4o (P<0.001) | [27] |
| Multi-Agent LLM System | MR Exam Design | Multi-Agent Framework | Demonstrated feasibility | Automated protocol/sequence design from health record | [13] |
Experimental Protocols for Multi-Agent LLM Systems in MRI Protocoling
Protocol 1: Implementing a Multi-Agent LLM System with RAG for Protocol Selection
1. Objective: To establish and validate a multi-agent LLM system capable of accurately selecting institution-specific MRI brain protocols based on a patient's clinical presentation, leveraging Retrieval-Augmented Generation to ensure recommendations adhere to local guidelines.
2. Background: A primary challenge in automated protocoling is the lack of standardization across institutions. LLMs, in their base form, lack knowledge of local protocols and are prone to hallucination. A study by Wagner et al. demonstrated that a context-aware, RAG-based pipeline can streamline protocol selection, minimizing manual input and training needs [13].
3. Materials and Reagents:
- Computing Hardware: Workstation with high-speed internet connection and/or access to cloud computing services (e.g., AWS, Google Cloud) for running LLM APIs.
- Software & Libraries: Python 3.12+, LangChain framework, Replicate API (for open-source models like LLaMA), OpenAI API.
- LLMs: Proprietary model (e.g., GPT-4o) and/or a powerful open-source model (e.g., LLaMA 3.1 405B).
- Embedding Model: OpenAI's "text-embedding-ada-002" or an equivalent open-source model.
- Data: A curated, institution-specific protocol guideline document (PDF or text format) detailing all available brain MRI protocols and their corresponding sequences.
4. Workflow Procedure:
- Step 1: Data Preprocessing. Convert the institutional protocol guideline PDF into plain text. Use a recursive character text splitter (e.g., from LangChain) to segment the document into chunks of ~400 characters with no overlap, ensuring each protocol is a distinct unit [27].
- Step 2: Vector Database Creation. Use the chosen embedding model to convert each text chunk into a vector representation. Store all vectors in a vector database (e.g., FAISS, Chroma) to enable efficient similarity search [27].
- Step 3: Multi-Agent System Design.
- Agent A: "Clinical Indication Interpreter": This agent's role is to extract key clinical entities from the free-text clinical question (e.g., "rule out multiple sclerosis," "evaluate for acute stroke"). It summarizes the patient's presentation into structured keywords.
- Agent B: "Protocol Retriever": This agent takes the keywords from Agent A and queries the vector database. It retrieves the top K (e.g., 4) most relevant protocol guidelines based on semantic similarity [27].
- Agent C: "Protocol Selector & Justifier": This final agent receives the retrieved protocol guidelines and the original clinical question. It is prompted to select the single most appropriate protocol from the retrieved options and output the MRI sequences exactly as listed. It can also be instructed to provide a brief justification for its selection.
- Step 4: Integration and Prompting. Integrate the agents using a scripting framework like LangChain. The temperature parameter for all LLM calls should be set low (e.g., 0.1) to ensure deterministic and reproducible outputs [27].
- Step 5: Validation. Perform a retrospective evaluation using a dataset of historical clinical questions with known, expert-selected protocol ground truths. Calculate token-based symmetric accuracy to compare the model's output against the ground truth [27].
Diagram 1: Multi-Agent RAG Workflow for MRI Protocol Selection
Protocol 2: Experimental Validation of LLM Performance in Sequence Classification
1. Objective: To quantitatively evaluate and compare the performance of advanced Multimodal LLMs in recognizing fundamental features of brain MRI sequences from images, including modality, anatomical region, plane, contrast status, and specific sequence type.
2. Background: Before MLLMs can be trusted with protocol design, their foundational ability to recognize basic imaging features must be established. Salbas et al. conducted a comparative analysis of ChatGPT-4o, Claude 4 Opus, and Gemini 2.5 Pro, highlighting significant performance variations and the critical issue of model hallucination [17].
3. Materials:
- Dataset: 130 brain MRI images from adult patients without pathological findings, representing 13 standard MRI series (e.g., T1, T2, FLAIR, DWI, ADC, SWI) [17].
- Models: Access to the MLLMs to be tested (e.g., ChatGPT-4o, Claude 4 Opus, Gemini 2.5 Pro via their respective APIs).
- Statistical Software: R or Python with libraries for statistical testing (e.g., scipy, statsmodels).
4. Workflow Procedure:
- Step 1: Dataset Curation. Ensure the image dataset is clean and accurately labeled by a expert radiologist. Each image should have a ground truth label for modality, anatomical region, imaging plane, contrast-enhancement status, and MRI sequence.
- Step 2: Zero-Shot Prompting. For each image in the dataset, present the image to each MLLM with a standardized, zero-shot prompt. An example prompt: "Identify the following for this brain MRI image: 1) Modality, 2) Anatomical region, 3) Imaging plane, 4) Contrast-enhancement status (contrast-enhanced or non-contrast), and 5) Specific MRI sequence." [17].
- Step 3: Response Collection and Parsing. Collect the model responses and parse them into structured data. Automated scripts can be used to extract the answers for each category.
- Step 4: Accuracy Calculation. For each model and each feature category, calculate the classification accuracy by comparing the model's output to the ground truth.
- Step 5: Statistical Analysis. Use Cochran's Q test to determine if there are statistically significant differences in performance between the models. Follow up with pairwise McNemar tests with Bonferroni correction to identify which model pairs differ significantly [17].
- Step 6: Hallucination Analysis. Manually review all incorrect classifications and note any instances where the model generated irrelevant or incorrect clinical details (e.g., mentioning specific syndromes like "Susac syndrome" when not present) [17].
Protocol 3: Mitigating Domain Shift in Automated Sequence Classification
1. Objective: To enhance the robustness of deep learning-based MRI sequence classifiers when applied to data from a different domain (e.g., pediatric vs. adult patients, different scanner vendors), using hybrid architectures and expert domain knowledge.
2. Background: Deep learning models for sequence classification often experience a performance drop due to domain shift. A study by Mahmutoglu et al. showed that a hybrid CNN-Transformer model (MedViT) combined with expert domain knowledge adjustments significantly improved accuracy on a pediatric dataset after being trained on adult data [4].
3. Materials:
- Datasets:
- Models: A benchmark CNN (e.g., ResNet-18), a hybrid CNN-Transformer model (e.g., MedViT).
- Software: PyTorch or TensorFlow, MONAI library for medical imaging AI.
4. Workflow Procedure:
- Step 1: Model Training. Pre-train both the ResNet-18 and MedViT models on the adult source dataset to classify the available sequence types (e.g., T1, T2, CT1, FLAIR, ADC, SWI, etc.).
- Step 2: Baseline Testing. Evaluate the pre-trained models directly on the pediatric target dataset without any modification. This establishes the baseline performance under domain shift.
- Step 3: Expert Domain Knowledge Adjustment. Analyze the target dataset to identify:
- Label Distribution Changes: Which sequence classes are present/absent compared to the source data?
- Sequence Characteristics: Are there qualitative differences in how sequences appear in pediatric vs. adult brains?
- Adjust the model's final classification layer to only output probabilities for the classes present in the target domain, ignoring unused classes from the source [4].
- Step 4: Fine-Tuning (Optional). If sufficient labeled data is available in the target domain, perform fine-tuning of the pre-trained models. Alternatively, use the model with adjusted output classes as-is.
- Step 5: Performance Evaluation. Compare the accuracy, precision, recall, and F1-score of the benchmark model, the hybrid model, and the hybrid model with expert adjustments on the pediatric test set.
Diagram 2: Mitigating Domain Shift in Sequence Classification
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Resources for Developing Automated MRI Protocoling Systems
| Tool/Resource | Type | Primary Function | Example/Reference |
|---|---|---|---|
| GPT-4o / LLaMA 3.1 | Large Language Model | Core reasoning engine for interpreting clinical questions and making protocol decisions. | [17] [27] |
| LangChain | Software Framework | Orchestrates multi-agent workflows, manages prompts, and integrates with vector databases. | [27] |
| Vector Database (e.g., FAISS, Chroma) | Data Structure | Enables efficient semantic search and retrieval of institutional protocol guidelines for RAG. | [27] |
| Text Embedding Model (e.g., text-embedding-ada-002) | AI Model | Converts text-based protocols into numerical vectors, enabling similarity comparison. | [27] |
| MedViT | Hybrid CNN-Transformer Model | Robust medical image classification, particularly effective under domain shift conditions. | [4] |
| Institutional Protocol Guidelines (PDF/Text) | Data | The domain-specific knowledge base that grounds the LLM and prevents hallucination. | [27] |
| DICOM Metadata | Data | Provides standardized, though sometimes unreliable, information for sequence labeling. | [4] |
| Bayesian Optimization Pipeline | Optimization Algorithm | A generalizable framework for designing and optimizing MRI sequence parameters. | [30] |
| SeqGPT | Specialized LLM | Demonstrates the capability of LLMs to generate MRI pulse sequences based on text prompts. | [13] |
Application Notes: The Expanding Role of MLLMs in Brain MRI
Multimodal Large Language Models (MLLMs) are advancing the analysis of brain MRI beyond simple classification tasks into complex cognitive domains including Radiology Report Generation (RRG) and Visual Question Answering (VQA). These applications represent a significant evolution from unimodal image analysis to integrated systems capable of synthesizing imaging data with clinical context to generate comprehensive reports and answer diagnostic queries.
The integration of MLLMs into brain MRI workflows addresses several critical limitations of traditional AI systems. While conventional deep learning models excel at specific classification tasks, they operate in isolation from the broader clinical context and generate restricted outputs lacking the comprehensiveness of radiologist-written reports [18] [1]. MLLMs bridge this gap by combining the visual processing capabilities of computer vision with the contextual understanding and generative capacity of large language models, enabling more holistic clinical decision support [1].
Table 1: Performance Comparison of MLLM Applications in Brain MRI
| Application | Model Name | Dataset | Key Metric | Performance | Comparative Baseline |
|---|---|---|---|---|---|
| RRG (3D CT) | BrainGPT | 3D-BrainCT (18,885 pairs) | FORTE F1-Score | 0.71 average | N/A |
| Turing Test Pass Rate | 74% | Human-written reports | |||
| VQA (3D mpMRI) | mpLLM | Multi-parametric Brain MRI | Average Accuracy | +5.3% | Strong medical VLM baselines |
| Sequence Classification | ChatGPT-4o | 130 Brain MRI Images | Sequence Accuracy | 97.7% | Claude 4 Opus (73.1%) |
| Gemini 2.5 Pro | 130 Brain MRI Images | Sequence Accuracy | 93.1% | ChatGPT-4o (97.7%) | |
| Differential Diagnosis | GPT-4 (PerplexityAI) | 40 Challenging Brain MRI Cases | Diagnostic Accuracy | 61.4% | Conventional search (46.5%) |
Clinical Implementation Challenges
Despite promising results, deploying MLLMs in clinical brain MRI workflows presents significant challenges. Hallucinations remain a critical concern, with studies reporting instances where models generate plausible but incorrect findings or invent irrelevant clinical details [2] [17]. One study noted Gemini 2.5 Pro occasionally hallucinated irrelevant clinical details such as "hypoglycemia" and "Susac syndrome" [17]. Effective human-AI collaboration protocols are essential, as research identifies inaccurate case descriptions by users (9.2% of cases) and insufficient contextualization of LLM responses as significant barriers to optimal performance [31].
Experimental Protocols
Protocol 1: BrainGPT for 3D Radiology Report Generation
Data Preparation and Curation
- Dataset Composition: Curate the 3D-BrainCT dataset containing 18,885 text-scan pairs with comprehensive lesion details including degree, spatial landmarks, and diagnostic impressions of both neuronal and vascular CT features [18].
- Annotation Standards: Structure reports in a list-by-list format focusing on differential diagnoses, ensuring inclusion of essential radiology descriptors (degree, landmark, feature, impression) that outweigh grammatical filler words [18].
- Preprocessing: Apply sentence pairing to decompose multi-sentence paragraphs into smaller semantic granularity, significantly improving traditional metric scores by an average of 5.28 points in METEOR and 114 points in CIDEr-R [18].
Model Architecture and Training
- Base Model: Utilize Otter foundation model as the starting point for development [18].
- Fine-tuning Approaches: Implement four clinical visual instruction tuning (CVIT) conditions:
- Plain Instruction: Basic role definition as radiology assistant
- In-context Example Instruction: 3-shot examples added to plain instruction
- Template Instruction: Structured clinical-defined QA templates
- Keyword Instruction: Categorical guidelines focused on keywords [18]
- Training Strategy: Employ a three-stage training approach comprising pre-training, instruction tuning, and alignment tuning to progressively improve cross-modal understanding and reasoning capabilities [1].
Evaluation Methodology
- FORTE Assessment: Implement Feature-Oriented Radiology Task Evaluation (FORTE) with four components: degree (0.661), landmark (0.706), feature (0.693), and impression (0.779) F1-scores [18].
- Turing Test: Conduct human evaluation where radiologists assess whether reports are generated by AI or humans, with BrainGPT achieving 74% indistinguishability from human-written reports [18].
- Clinical Validation: Externally validate diagnostic accuracy and linguistic style on the CQ500 dataset with 11 physician raters [18].
Protocol 2: mpLLM for Visual Question Answering on Multiparametric 3D Brain MRI
Data Preparation and Synthesis
- Dataset Creation: Develop the first clinically validated VQA dataset for 3D brain multiparametric MRI (mpMRI) through collaboration with medical experts [32] [33].
- Synthetic VQA Generation: Implement a synthetic visual question answering protocol that generates medically relevant VQA pairs from segmentation annotations to address limited image-text paired supervision [32] [33].
- Modality Integration: Process multiple interrelated 3D modalities including T1-weighted, T2-weighted, FLAIR, DWI, ADC, and contrast-enhanced sequences through a unified architecture [32].
Model Architecture
- Mixture-of-Experts Framework: Implement a prompt-conditioned hierarchical mixture-of-experts (MoE) architecture that routes across modality-level and token-level projection experts [32] [33].
- Efficient Training: Design the system to enable efficient training without image-report pretraining, reducing computational demands [32].
- Modality Fusion: Develop specialized mechanisms to fuse multiple interrelated 3D modalities, allowing the model to leverage complementary information across different MRI sequences [32] [34].
Evaluation and Validation
- Performance Benchmarking: Evaluate against strong medical Vision-Language Model baselines across multiple mpMRI datasets, demonstrating 5.3% average improvement [32].
- Ablation Studies: Conduct comprehensive ablations highlighting the importance of modality-level and token-level experts and prompt-conditioned routing [32] [33].
- Clinical Validation: Collaborate with medical experts for clinical validation of generated responses, ensuring medical relevance and accuracy [32].
Protocol 3: Human-AI Collaboration for Brain MRI Differential Diagnosis
Experimental Design
- Case Selection: Curate 40 brain MRI cases with challenging but definitive diagnoses, confirmed either histopathologically (42.5%) or by independent agreement of two neuroradiologists with clinical follow-up (57.5%) [31].
- Reader Recruitment: Enroll six radiology residents with average neuroradiology experience of 6.3 months (range: 2-11 months) to simulate realistic clinical scenarios [31].
- Crossover Design: Randomize cases into two groups with readers using conventional internet search for one set and LLM-assisted search (PerplexityAI with GPT-4) for the other, ensuring each case is examined with both workflows in equal frequency [31].
Implementation Protocol
- LLM Interface: Utilize PerplexityAI for its ability to access real-time web content and indicate information sources, with GPT-4 as the underlying LLM [31].
- Training Session: Conduct 10-15 minute training sessions using three sample brain MRI cases to ensure familiarity with LLM operation and functionality [31].
- Prompting Strategy: Provide sample prompts including case details (age range, sex, symptoms, MRI findings) with explicit instruction to name the most likely differential diagnoses, while allowing participants to explore alternative approaches [31].
Evaluation Metrics
- Diagnostic Accuracy: Employ binary scoring (correct/incorrect) and numeric scoring (0-3 based on rank of correct diagnosis) systems [31].
- Efficiency Metrics: Measure interpretation times using time-tracking software and record confidence levels on a 5-point Likert scale for each case [31].
- Error Analysis: Review LLM logs to quantify queries, categorize content, identify hallucinations, and classify inaccurate user inputs [31].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Materials and Computational Resources for MLLM Experiments in Brain MRI
| Resource Category | Specific Solution | Function/Purpose | Example Implementation |
|---|---|---|---|
| Datasets | 3D-BrainCT | 18,885 text-scan pairs for training RRG models | BrainGPT development [18] |
| Brain mpMRI VQA Dataset | First clinically validated VQA dataset for multiparametric 3D brain MRI | mpLLM training and validation [32] | |
| Foundation Models | Otter Model | Base foundation model for medical MLLM development | BrainGPT fine-tuning [18] |
| CLIP Encoders | Pre-trained vision encoders for visual feature extraction | Multimodal connector training [1] | |
| Evaluation Frameworks | FORTE | Feature-Oriented Radiology Task Evaluation for clinical essence measurement | BrainGPT assessment [18] |
| Synthetic VQA Protocol | Generates medically relevant VQA from segmentation annotations | Data augmentation for mpLLM [32] | |
| Architectural Components | Mixture-of-Experts | Prompt-conditioned hierarchical routing for multiple modalities | mpLLM architecture [32] |
| Multimodal Connectors | Bridge modality gap between non-text data and natural language | Projection-based, query-based, fusion-based connectors [1] |
The integration of MLLMs for RRG and VQA in brain MRI represents a paradigm shift from passive classification tools to active collaborative partners in radiological practice. Current research demonstrates that these models can generate clinically sensible reports and answer complex diagnostic questions with accuracy approaching human performance in specific domains. The successful implementation of specialized evaluation frameworks like FORTE addresses the critical limitation of traditional metrics in capturing clinical essence.
Future development should focus on enhancing region-grounded reasoning to link model outputs to specific image regions, developing robust foundation models pre-trained on large-scale medical datasets, and establishing comprehensive strategies for the safe integration of MLLMs into clinical practice. As these technologies mature, they hold significant potential to serve as trusted AI partners that augment radiologist expertise while maintaining essential human oversight in the diagnostic process.
Multimodal Large Language Models (MLLMs) represent a transformative advancement in medical artificial intelligence, capable of interpreting complex medical imagery and generating preliminary radiology reports. This case study examines the application of frameworks like BrainGPT for generating clinically-sensible reports from 3D brain CT scans, with direct relevance to brain MRI sequence classification research. The integration of specialized training techniques and novel evaluation metrics addresses critical challenges in clinical deployment, offering a roadmap for reliable implementation in neuroimaging.
Table 1: Core Challenges and Solutions in Medical MLLMs for 3D Neuroimaging
| Challenge | Description | BrainGPT Framework Solution |
|---|---|---|
| Data Complexity | 2D datasets cannot capture complex 3D neurovascular anatomy; "sharpshooter fallacy" in slice selection [18] [35] | Curation of a large-scale 3D-BrainCT dataset (18,885 text-scan pairs) [18] |
| Model Capacity | Standard MLLMs struggle with volumetric 3D data and clinical reasoning [18] [1] | Clinical Visual Instruction Tuning (CVIT) on Otter model foundation [18] [35] |
| Evaluation Fidelity | Traditional NLP metrics (BLEU, ROUGE) fail to capture clinical essence and information density [18] [35] | Feature-Oriented Radiology Task Evaluation (FORTE) [18] |
Background and Significance
The transition from unimodal to multimodal AI represents a paradigm shift in medical imaging analysis. While convolutional neural networks excelled at isolated image recognition tasks, they operated in isolation from the rich contextual information available in clinical practice [1]. MLLMs bridge this gap by integrating diverse data sources—including radiologic images (e.g., CT, MRI), clinical notes, and laboratory results—into a unified analytical framework [1]. This capability is particularly valuable in radiology, where practitioners naturally synthesize information across multiple modalities during diagnostic reasoning [1].
In the specific domain of brain imaging, the ability to accurately describe lesion degree, size, and location is paramount for diagnosis and treatment planning [18]. Early MLLM applications demonstrated promising results in 2D radiology report generation (RRG) for chest X-rays, but their performance in volumetric 3D neuroimaging remained largely unexplored until recently [18]. The BrainGPT framework represents a significant advancement in this domain, specifically addressing the unique challenges of 3D brain CT interpretation through a holistic approach encompassing dataset curation, model tuning, and evaluation [18].
Experimental Protocols and Methodologies
Dataset Curation and Preprocessing
The foundation for training robust medical MLLMs lies in high-quality, clinically representative datasets. The BrainGPT framework utilized a curated 3D-BrainCT dataset comprising 18,885 text-scan pairs collected from Taipei Veterans General Hospital (2010-2022) [18] [35]. This dataset includes scans from 9,689 patients with Alzheimer's disease (average age >82 years), encompassing normal brains, past infarcts, chronic conditions, and acute lesions, thereby capturing the diversity of real-world diagnostic scenarios [35].
Key Protocol Steps:
- Volumetric Data Handling: Instead of single slices, each data point includes 24 consecutive CT slices, preserving 3D contextual information [35].
- Structured Reporting: Ground truth reports follow a standardized list-by-list format focusing on differential diagnoses, emphasizing key radiology descriptors over grammatical filler words [18].
- Data Triplet Formation: For model training, data is structured as triplets containing (1) the set of 24 slices, (2) an instruction, and (3) the corresponding ground truth report [35].
Model Architecture and Training
BrainGPT is built upon the open-source Otter model, which itself is based on the OpenFlamingo architecture [35]. This architecture was selected for its multi-image captioning capability and support for in-context learning.
Table 2: BrainGPT Architectural Components
| Component | Implementation | Role | Training Status |
|---|---|---|---|
| Visual Encoder | OpenAI's CLIP ViT/L14 [35] | Extracts meaningful visual features from 24 input slices | Frozen |
| Multimodal Connector | Perceiver Resampler [35] | Maps visual features into tokens processable by the LLM | Trainable |
| Language Model | LLaMA-7B [35] | Elaborates text and visual tokens; generates report | Frozen (only cross-gated attention layers trained) |
The core innovation in BrainGPT's training is Clinical Visual Instruction Tuning (CVIT), which enhances the model's medical domain knowledge through structured clinical guidance [18]. This approach was compared against Regular Visual Instruction Tuning (RVIT) under different conditions:
- RVIT-Plain: Basic instruction establishing the model's role as a radiology assistant [35].
- RVIT-Example: Plain instruction augmented with 3 in-context examples of high-quality reports [35].
- CVIT-Template: Instruction with structured clinical QA templates guiding the report format [35].
- CVIT-Keyword: Instruction with categorical guidelines focusing on specific clinical elements (Degree, Landmark, Feature, Impression) [18] [35].
Evaluation Methods and Metrics
Comprehensive evaluation of generated reports requires both traditional natural language processing (NLP) metrics and clinically-grounded assessment:
Traditional NLP Metrics:
- BLEU (Bilingual Evaluation Understudy): Measures n-gram overlap with reference reports [35].
- METEOR (Metric for Evaluation of Translation with Explicit ORdering): Word-to-word matching considering synonyms [35].
- ROUGE-L (Recall-Oriented Understudy for Gisting Evaluation): Assesses longest common subsequence [35].
- CIDEr-R (Robust Consensus-based Image Description): Computes cosine similarity of TF-IDF vectors, capturing keyword usage frequency [18].
Clinical Relevance Metrics:
- FORTE (Feature-Oriented Radiology Task Evaluation): A novel evaluation scheme that extracts and categorizes clinical keywords into four essential components [18]:
- Degree: Intensity or state of findings (e.g., mild, chronic)
- Landmark: Anatomical location (e.g., periventricular, midline)
- Feature: Observed abnormalities (e.g., hemorrhage, atrophy)
- Impression: Clinical diagnosis or summary (e.g., arteriosclerotic encephalopathy)
- Turing Test: Human evaluation where physician raters distinguish between AI-generated and human-written reports [18].
BrainGPT Workflow and Evaluation
Results and Performance Analysis
Quantitative Performance Metrics
BrainGPT demonstrated significant improvements in report generation quality across both traditional and clinical metrics.
Table 3: BrainGPT Performance on Traditional and Clinical Metrics
| Metric / Model Type | Baseline Otter | BrainGPT-Plain (RVIT) | BrainGPT-Keyword (CVIT) |
|---|---|---|---|
| Traditional Metrics (after Sentence Pairing) [18] [35] | |||
| BLEU-4 | ~0 | ~15 | ~20.38 |
| CIDEr-R | ~5.9 | ~125.86 | ~211.77 |
| FORTE F1-Scores (Clinical Evaluation) [18] | |||
| Degree | N/A | N/A | 0.661 |
| Landmark | N/A | N/A | 0.706 |
| Feature | N/A | N/A | 0.693 |
| Impression | N/A | N/A | 0.779 |
| Average FORTE F1-Score | N/A | N/A | 0.710 |
| Human Evaluation [18] | |||
| Turing Test Pass Rate | N/A | N/A | ~74% |
The progression from baseline Otter to advanced CVIT models (BrainGPT-keyword) shows substantial improvement in clinical content quality. The CIDEr-R metric, which captures keyword usage through TF-IDF weighting, showed the most dramatic improvement, increasing from 5.9 (baseline) to 211.77 (BrainGPT-keyword) [18] [35]. This indicates significantly enhanced usage of clinically relevant terminology in the CVIT-tuned models.
Comparison with Alternative Approaches
Sentence Pairing for Enhanced Evaluation: A notable methodological innovation involved decomposing multisentence reports into smaller semantic units through sentence pairing. This technique dramatically improved traditional metric scores by an average of 5.28 points in METEOR, 6.48 points in ROUGE-L, and 114 points in CIDEr-R, revealing the limitations of evaluating full paragraphs against reference reports [18].
Keyword-Based Assistance Paradigm: Complementary research demonstrates that AI assistance can significantly reduce reporting time. One study showed that when radiologists provided structured keywords instead of writing full reports, AI could generate complete reports with 72% primary diagnosis accuracy while reducing reporting time by approximately 28% [36].
Performance in MRI Sequence Classification: Recent evaluations of general-purpose MLLMs in brain MRI tasks show varying capabilities. In classifying 13 standard MRI sequences from 130 images, ChatGPT-4o achieved 97.7% accuracy, Gemini 2.5 Pro 93.1%, and Claude 4 Opus 73.1%, with most errors involving FLAIR sequence misclassification [2]. This demonstrates the specialized challenge of medical image interpretation even for advanced models.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Resources for Medical MLLM Research
| Resource / Component | Function / Application | Implementation Example |
|---|---|---|
| Otter Model Framework [35] | Open-source foundation model supporting multi-image inputs and in-context learning | Base architecture for BrainGPT |
| OpenFlamingo Architecture [35] | Enables processing of interleaved image-text inputs | Backbone of Otter model |
| CLIP ViT/L14 Visual Encoder [35] | Extracts visual features from medical images | Pre-trained encoder for processing CT slices |
| Perceiver Resampler [35] | Maps visual features to language model space | Multimodal connector |
| LLaMA-7B Language Model [35] | Provides linguistic reasoning capabilities | Frozen LLM in BrainGPT |
| 3D-BrainCT Dataset [18] | Large-scale volumetric CT dataset with paired reports | Training and evaluation data |
| FORTE Evaluation Framework [18] | Clinically-grounded assessment metric | Measures diagnostic quality of generated reports |
Implementation Protocol for Brain MRI Research
Adapting the BrainGPT framework for brain MRI sequence classification research requires specific methodological adjustments:
Protocol: Adapting BrainGPT for MRI Sequence Analysis
Step 1: Data Preparation and Curation
- Collect multi-sequence MRI studies with corresponding radiology reports
- Ensure representation of all major sequences: T1-weighted, T2-weighted, FLAIR, DWI, ADC, SWI, and contrast-enhanced variants [2]
- Annotate sequences with standardized terminology and plane information (axial, sagittal, coronal)
Step 2: Model Selection and Configuration
- Implement architecture based on OpenFlamingo with CLIP visual encoder
- Modify input processing to handle MRI sequences rather than CT slices
- Maintain CVIT approach with sequence-specific instruction templates
Step 3: Specialized Instruction Tuning
- Develop MRI-specific keyword categories:
- Sequence Type: T1w, T2w, FLAIR, DWI, etc.
- Contrast Status: Pre-contrast vs. post-contrast
- Anatomical Plane: Axial, sagittal, coronal
- Pathological Correlation: Signal characteristics, restriction, enhancement
Step 4: Evaluation and Validation
- Implement FORTE-style evaluation with sequence-specific keywords
- Include expert radiologist review for hallucination detection
- Conduct sequence classification accuracy assessment using confusion matrices
Adapting BrainGPT for MRI Sequence Analysis
The BrainGPT framework demonstrates that generating clinically-sensible radiology reports from 3D neuroimaging data is achievable through a holistic approach combining specialized dataset curation, clinical visual instruction tuning, and robust evaluation metrics. The achieved FORTE F1-score of 0.71 and 74% Turing test pass rate establish a new benchmark for medical MLLM performance [18].
For brain MRI sequence classification research, this framework offers:
- A validated methodology for adapting MLLMs to volumetric neuroimaging
- Clinical Visual Instruction Tuning as a powerful approach for incorporating domain knowledge
- FORTE evaluation as a robust alternative to traditional NLP metrics
- A pathway toward reliable AI-assisted radiology reporting that maintains diagnostic accuracy while reducing interpretation time
Future research directions should focus on expanding these techniques to multi-modal neuroimaging (combining MRI, CT, and clinical data), enhancing spatial reasoning capabilities for precise lesion localization, and developing more sophisticated methods for detecting and mitigating hallucinated content in generated reports.
Navigating Challenges: Hallucinations, Data Heterogeneity, and Performance Optimization
Identifying and Mitigating Clinical Hallucinations and Inaccurate Outputs
Multimodal large language models (MLLMs) represent a significant evolution in medical artificial intelligence (AI), demonstrating particular promise in radiology by integrating diverse data sources such as clinical text and radiologic images ranging from 2D X-rays to 3D CT and MRI [1]. In the specific context of brain MRI sequence classification research, these models can function as trusted AI partners, assisting with tasks ranging from automatic protocol generation to interactive diagnostic support [1]. However, their clinical deployment is challenged by a critical vulnerability: the tendency to generate hallucinations, which are fluent, confident, but factually incorrect outputs that can mislead clinical decisions [37]. In high-stakes domains like neuroradiology, where an inaccurate sequence recommendation or a misclassified finding could impact patient diagnosis and treatment, identifying and mitigating these hallucinations is paramount for ensuring patient safety and model trustworthiness. This document provides detailed application notes and experimental protocols to support researchers in this endeavor, framed within the broader scope of multimodal LLM research for brain MRI.
Defining and Quantifying the Hallucination Problem
In medical imaging, hallucinations are not merely inaccuracies but are more specifically defined as AI-fabricated abnormalities or artifacts that appear visually realistic and highly plausible, yet are factually false and deviate from anatomic or functional truth [38]. For brain MRI sequence classification and analysis, this can manifest in two primary directions:
- Image-to-Text Hallucinations: The model generates radiology reports or sequence classifications that contain findings unsupported by the input image. A critical example in brain MRI is the misestimation or failure to detect midline shift, a clinically significant finding indicating potential mass effect from hemorrhage or tumor [37].
- Text-to-Image Hallucinations: The model synthesizes brain MRI images that are anatomically implausible or contain features inconsistent with the clinical prompt [37]. For instance, a model might generate an image labeled as a "brain MRI" that shows a fracture, which is anatomically impossible for this imaging modality [37].
The quantitative impact of these hallucinations is non-trivial. The following table summarizes performance data from recent studies evaluating LLMs in radiology protocoling tasks, highlighting both baseline error rates and the significant improvements achievable with mitigation strategies like Retrieval-Augmented Generation (RAG).
Table 1: Quantitative Performance of LLMs in Radiology Protocoling Tasks
| Study Focus | Model(s) Evaluated | Performance Metric | Baseline Performance (without RAG) | Enhanced Performance (with RAG) |
|---|---|---|---|---|
| General MRI Protocoling [39] | LLaMA 3.1 405B | Sequence Prediction Accuracy | 38% | 70% |
| Contrast Media Prediction Accuracy | 77% | 94% | ||
| GPT-4o | Sequence Prediction Accuracy | 43% | 81% | |
| Contrast Media Prediction Accuracy | 79% | 92% | ||
| Brain MRI Protocoling [40] | o3-mini | Accuracy Index (Sum of redundant/missing sequences) | 2.65 ± 1.61 | 1.94 ± 1.25 |
| GPT-4o | Accuracy Index | 3.11 ± 1.83 | 2.23 ± 1.48 |
Experimental Protocols for Hallucination Assessment
Rigorous evaluation is the cornerstone of identifying hallucinations. The following protocol provides a framework for assessing MLLMs in brain MRI sequence classification tasks.
Protocol: Hallucination Detection in Image-to-Text Tasks
Objective: To systematically identify and categorize hallucinations in MLLM-generated brain MRI reports or sequence classifications.
Materials:
- Curated Dataset: A set of brain MRI studies (e.g., 150 cases) with corresponding, verified clinical questions [40].
- Ground Truth Establishment: Reference standards (e.g., MRI sequences, radiology reports) defined by at least two board-certified neuroradiologists. Inter-rater agreement (e.g., Cohen’s κ) should be calculated to ensure consistency [40].
- Model(s) for Evaluation: The MLLM(s) under investigation (e.g., GPT-4o, o3-mini, open-source alternatives) [40].
Methodology:
- Prompt Engineering: Develop a standardized base prompt that clearly defines the task. For example: "You are a senior neuroradiologist tasked with defining a brain MRI protocol for a given clinical case. Include only clinically relevant sequences, avoid redundant or unnecessary sequences" [40]. The prompt can be iteratively refined using a small set of hold-out cases.
- Model Inference: Execute the model(s) for all cases in the dataset. Use a low temperature setting (e.g., 0 or 0.1) to ensure deterministic outputs and high reproducibility [39] [40].
- Output Analysis: Compare model outputs against the ground truth. The analysis should focus on:
- Factual Hallucinations: Outputs that contradict established medical knowledge (e.g., suggesting an inappropriate sequence for a clinical indication).
- Faithfulness Hallucinations: Outputs that violate the source input (e.g., omitting a critical sequence explicitly mentioned in the clinical guidelines provided in the prompt).
- Omissions: Critical elements present in the ground truth that are missing from the model's output [37].
- Quantitative Evaluation: Calculate metrics such as:
- Accuracy Index: The sum of redundant and missing sequences, which provides a granular view of protocoling errors [40].
- Token-based Symmetric Accuracy: For comparing the overlap between predicted and ground-truth sequences [39].
- Statistical Tests: Use paired t-tests or McNemar tests to compare performance between models or conditions [39] [40].
Protocol: Mitigation via Retrieval-Augmented Generation (RAG)
Objective: To enhance the accuracy and reduce the hallucination rate of an MLLM by grounding its responses in institution-specific, authoritative knowledge.
Materials:
- Knowledge Base: Institutional protocol guidelines (e.g., a PDF document detailing 63 different MRI protocols) [39].
- Embedding Model: A model such as OpenAI's "text-embedding-ada-002" to convert text into vector representations [39].
- Vector Database: A database to store and query the embedded text chunks.
Methodology:
- Data Preprocessing: Segment the protocol guidelines into manageable paragraphs or chunks using a text splitter (e.g., with a 400-character limit and no overlap) [39].
- Vectorization and Storage: Use the embedding model to convert each text chunk into a vector and store them in the vector database.
- RAG-Augmented Prompting:
- For a given clinical question, perform a similarity search in the vector database to retrieve the top K (e.g., 4) most relevant protocol chunks [39].
- Construct a prompt that includes the patient's clinical question and the retrieved, context-specific protocol information.
- Instruct the model to select the appropriate protocol from the retrieved options, forcing it to ground its decision in the provided documentation [39].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for Hallucination Research
| Item Name | Function/Description | Example/Reference |
|---|---|---|
| Clinical Dataset | A curated, often retrospective, set of brain MRI cases with clinical questions. Essential for training and evaluation. | 150 brain MRI cases derived from local imaging request forms [40]. |
| Ground Truth Annotations | Expert-validated labels (e.g., sequences, reports) against which model outputs are compared. | Protocols defined by board-certified neuroradiologists [40]. |
| Vector Database | Stores embedded chunks of institutional knowledge for efficient retrieval in a RAG pipeline. | Used to store embedded protocol guidelines for similarity search [39]. |
| Embedding Model | Converts text into numerical vector representations, enabling semantic similarity search. | OpenAI's "text-embedding-ada-002" [39]. |
| Structured Output Parser | Ensures model outputs adhere to a predefined schema (e.g., JSON), enabling programmatic analysis. | Used to parse LLM-generated protocols into a structured JSON format [40]. |
| Statistical Analysis Package | For performing significance tests and calculating performance metrics and inter-rater reliability. | Used for paired t-tests and McNemar tests [39] [40]. |
Workflow Visualization
The following diagram illustrates the logical workflow and system architecture for a RAG-enhanced MLLM system designed to mitigate hallucinations in brain MRI protocoling.
RAG System for Hallucination Mitigation
The accompanying diagram outlines the hallucination assessment workflow, from the initial clinical question to the final evaluation against expert-defined ground truth.
Hallucination Assessment Workflow
The integration of multimodal large language models (MLLMs) into radiology represents a transformative advancement with the potential to revolutionize medical image analysis. Within the specific domain of brain MRI interpretation, the fundamental task of accurately identifying basic imaging sequences serves as a critical foundation for any subsequent diagnostic application. Research demonstrates that while these models show remarkable proficiency in general image recognition, their performance varies significantly when classifying specific MRI sequences, particularly Fluid-Attenuated Inversion Recovery (FLAIR), Susceptibility-Weighted Imaging (SWI), and Apparent Diffusion Coefficient (ADC) sequences [2]. This challenge is not merely academic; misclassification of these critical sequences can lead to incorrect image interpretation pipelines, potentially compromising diagnostic accuracy in clinical and research settings. The susceptibility of MLLMs to misclassify FLAIR as T1-weighted or diffusion-weighted sequences, alongside difficulties in recognizing SWI and ADC sequences, represents a significant bottleneck that must be addressed to ensure reliable implementation in medical environments [2]. This application note examines the common pitfalls in MLLM-based classification of these crucial sequences and provides detailed protocols to enhance classification accuracy within the broader context of multimodal LLM research for brain MRI analysis.
Quantitative Performance Landscape of MLLMs in Sequence Classification
Recent comprehensive evaluations have quantified the performance disparities among leading MLLMs in brain MRI sequence classification. A 2025 comparative analysis tested ChatGPT-4o, Claude 4 Opus, and Gemini 2.5 Pro using 130 brain MRI images representing 13 standard sequences in a zero-shot prompting scenario [2] [17]. The results revealed striking differences in model capabilities, particularly for the challenging sequence classifications that form the focus of this analysis.
Table 1: Overall Performance of MLLMs in Brain MRI Sequence Classification Tasks
| Model | Modality Identification | Anatomical Region Recognition | Imaging Plane Classification | Contrast-Enhancement Status | MRI Sequence Classification |
|---|---|---|---|---|---|
| ChatGPT-4o | 130/130 (100%) | 130/130 (100%) | 130/130 (100%) | 128/130 (98.46%) | 127/130 (97.69%) |
| Gemini 2.5 Pro | 130/130 (100%) | 130/130 (100%) | 130/130 (100%) | 128/130 (98.46%) | 121/130 (93.08%) |
| Claude 4 Opus | 130/130 (100%) | 130/130 (100%) | 129/130 (99.23%) | 124/130 (95.38%) | 95/130 (73.08%) |
Statistical analysis using Cochran's Q test revealed statistically significant differences in MRI sequence classification performance (p < 0.001), with ChatGPT-4o demonstrating superior accuracy, followed by Gemini 2.5 Pro, and Claude 4 Opus showing substantially lower performance [2].
Table 2: Sequence-Specific Misclassification Patterns in MLLMs
| MRI Sequence | ChatGPT-4o Accuracy | Gemini 2.5 Pro Accuracy | Claude 4 Opus Accuracy | Most Common Misclassifications |
|---|---|---|---|---|
| FLAIR | 97.7% | 93.1% | 73.1% | T1-weighted, Diffusion-weighted |
| SWI | High | Moderate | Low | Not specified |
| ADC | High | Moderate | Low | Not specified |
The most frequent misclassifications involved FLAIR sequences, which were often incorrectly identified as T1-weighted or diffusion-weighted sequences [2]. Claude 4 Opus exhibited particular difficulties with SWI and ADC sequences, while Gemini 2.5 Pro occasionally produced hallucinations, including irrelevant clinical details such as "hypoglycemia" and "Susac syndrome" in its responses [2].
Experimental Protocols for Evaluating Sequence Classification
Standardized Image Dataset Curation Protocol
To ensure consistent evaluation of MLLM performance in sequence classification, researchers should adhere to a standardized dataset curation protocol:
- Image Selection: Collect brain MRI images from adult patients without pathological findings to eliminate confounding factors. A minimum of 10 single-slice images per sequence type is recommended for statistical power [2].
- Sequence Representation: Include all major sequence types: axial T1-weighted (T1w), axial T2-weighted (T2w), axial FLAIR, coronal FLAIR, sagittal FLAIR, coronal T2w, sagittal T1w, axial SWI, axial diffusion-weighted imaging (DWI), axial ADC, contrast-enhanced axial T1w, contrast-enhanced coronal T1w, and contrast-enhanced sagittal T1w [2].
- Image Quality Control: Export images in high-quality JPEG format with minimum resolution of 994 × 1382 pixels without compression, cropping, or visual post-processing. Ensure no annotations, arrows, or textual markings are present on images to prevent model bias [2].
- Anatomical Standardization: Select representative slices at anatomical levels where key structures (e.g., lateral ventricles) are clearly visible, ensuring each image reflects typical visual characteristics of its respective sequence [2].
MLLM Testing and Evaluation Framework
A rigorous testing protocol is essential for obtaining reliable performance metrics:
- Prompt Standardization: Use consistent zero-shot prompts across all model evaluations: "This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: What type of radiological modality is this examination? Which anatomical region does this examination cover? What is the imaging plane (axial, sagittal, or coronal)? Is this a contrast-enhanced image or not? If this image is an MRI, what is the specific MRI sequence? If it is not an MRI, write 'Not applicable.' Please number your answers clearly." [2]
- Session Management: Initiate a new session for each prompt by clearing chat history to prevent in-context adaptation, where models might alter response strategies based on previous answers [2].
- Evaluation Methodology: Have two radiologists independently review and jointly classify LLM responses as "correct" or "incorrect" through consensus. Define hallucinations as statements unrelated to the input image or prompt context [2].
- Statistical Analysis: Calculate accuracy for each classification task. Use Cochran's Q test for overall comparison of MRI sequence classification performance, followed by pairwise McNemar tests with Bonferroni correction where appropriate. Compute macro-averaged F1 scores and Cohen's kappa coefficients to evaluate inter-class performance consistency and agreement with ground truth [2].
Diagram 1: Experimental workflow for evaluating MLLM performance in MRI sequence classification
Technical Characteristics and Classification Challenges of Key Sequences
FLAIR (Fluid-Attenuated Inversion Recovery) Sequences
FLAIR sequences represent a particular challenge for MLLMs due to their visual similarity to other sequences. FLAIR is a specialized T2-weighted technique that nulls the cerebrospinal fluid (CSF) signal, providing superior visualization of periventricular lesions and cortical pathology. The characteristic appearance of dark ventricles alongside bright parenchymal signal creates a potential for confusion with T1-weighted sequences (which also show dark CSF) and diffusion-weighted sequences (which may show similar contrast in certain pathologies) [2]. This visual ambiguity explains why FLAIR sequences were most frequently misclassified as T1-weighted or diffusion-weighted sequences in the evaluation studies [2].
SWI (Susceptibility-Weighted Imaging) Sequences
SWI presents unique technical characteristics that contribute to its misclassification challenges. SWI is generated from gradient-echo (GRE) pulse sequences that are exquisitely sensitive to differences in tissue susceptibility due to their inability to refocus spins dephased by magnetic field inhomogeneities [41]. Modern SWI sequences incorporate several distinctive features: they are typically acquired in 3D mode (rather than 2D), allowing thinner slices and smaller voxel sizes; they use flow compensation in all three directions to reduce artifacts; and they employ parallel imaging to reduce acquisition time [41]. A key characteristic of SWI is the independent processing and display of both magnitude and phase information, which are combined for diagnostic purposes [41] [42]. The phase data undergoes sophisticated processing including digital high-pass filtering to remove low-frequency fluctuations and additional local phase correction algorithms to reduce artifacts at the skull base [41]. The resulting susceptibility-weighted image represents a complex combination of magnitude and phase information that can be challenging for MLLMs to distinguish from other GRE-based sequences, particularly for models like Claude 4 Opus which demonstrated lower accuracy in SWI identification [2].
ADC (Apparent Diffusion Coefficient) Sequences
ADC sequences derived from diffusion-weighted imaging present classification difficulties due to their quantitative nature and specific clinical applications. ADC maps provide quantitative measurement of water molecule diffusion, with lower values indicating restricted diffusion typically associated with acute ischemia, high cellularity tumors, or abscesses [43]. In glioma evaluation, ADC values have demonstrated significant differences between low-grade and high-grade gliomas, with high-grade gliomas typically showing lower ADC values due to increased cellularity [43]. The quantitative grayscale representation of water diffusion coefficients creates a distinct appearance that nevertheless can be confused with other quantitative maps or even conventional T2-weighted images by MLLMs, particularly evidenced by Claude 4 Opus's lower accuracy in ADC sequence identification [2].
Diagram 2: Technical challenges in classifying FLAIR, SWI, and ADC sequences
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Resources for MLLM MRI Sequence Classification Studies
| Resource Category | Specific Resource | Function/Application | Technical Specifications |
|---|---|---|---|
| Multimodal LLMs | ChatGPT-4o (OpenAI) | High-accuracy baseline for sequence classification | Demonstrated 97.69% accuracy in sequence classification [2] |
| Multimodal LLMs | Gemini 2.5 Pro (Google) | Comparative model with moderate hallucination risk | 93.08% sequence accuracy; occasional irrelevant clinical details [2] |
| Multimodal LLMs | Claude 4 Opus (Anthropic) | Lower-performance benchmark for challenging sequences | 73.08% sequence accuracy; difficulties with SWI and ADC [2] |
| MRI Data Sources | Institutional PACS | Source of validated medical images for testing | 130 brain MRI images, 13 sequence types, no pathological findings [2] |
| Evaluation Framework | Standardized Prompt Template | Ensures consistent zero-shot testing across models | Specific text prompt for medical image evaluation [2] |
| Statistical Tools | Cochran's Q Test | Determines significant differences in model performance | p < 0.001 for sequence classification differences [2] |
| Clinical Validation | Radiologist Consensus | Ground truth establishment for model responses | Two radiologists reviewing responses jointly [2] |
Mitigation Strategies for Enhanced Classification Accuracy
Based on the identified pitfalls and performance patterns, several strategic approaches can enhance MLLM classification accuracy for challenging sequences:
- Ensemble Modeling: Combine the strengths of different MLLMs by implementing weighted voting systems that prioritize ChatGPT-4o for sequence classification while leveraging other models for complementary tasks.
- Sequence-Specific Fine-tuning: Develop specialized classification modules for problematic sequences (particularly FLAIR, SWI, and ADC) using transfer learning approaches with curated image datasets.
- Multi-feature Analysis: Incorporate quantitative image features beyond visual analysis, including texture parameters, signal intensity ratios, and spatial frequency characteristics that distinguish ambiguous sequences.
- Clinical Context Integration: Implement retrieval-augmented generation (RAG) architectures that provide clinical context to reduce hallucinations and improve classification rationale, as demonstrated in emerging research [13].
- Rigorous Validation Protocols: Establish standardized evaluation frameworks with radiologist consensus validation, similar to the methodology that revealed the significant performance differences in current models [2].
The implementation of these mitigation strategies requires careful consideration of the specific research context and application requirements. For clinical deployment applications, the highest accuracy standards must be maintained with ChatGPT-4o currently representing the most reliable base model. For research environments focused on method development, the comparative analysis of lower-performing models may provide valuable insights into failure modes and improvement opportunities.
The accurate classification of FLAIR, SWI, and ADC sequences represents a critical challenge in the application of multimodal LLMs to brain MRI analysis. Significant performance disparities exist among current state-of-the-art models, with ChatGPT-4o demonstrating superior classification accuracy (97.69%) compared to Gemini 2.5 Pro (93.08%) and Claude 4 Opus (73.08%) [2]. The consistent misclassification patterns, particularly for FLAIR sequences being confused with T1-weighted or diffusion-weighted sequences, highlight specific areas requiring methodological refinement. The occurrence of hallucinations in some models further underscores the necessity of rigorous validation and expert oversight in clinical implementations. As research in this domain advances, the development of sequence-specific classification enhancements, ensemble approaches, and standardized evaluation protocols will be essential for achieving the reliability required for clinical decision support systems. The comprehensive experimental protocols and analytical frameworks presented in this application note provide a foundation for further investigation and development in this rapidly evolving field.
Multimodal Large Language Models (MLLMs) represent a significant evolution in medical artificial intelligence (AI), enabling concurrent processing and integration of heterogeneous data modalities including various magnetic resonance imaging (MRI) types alongside textual clinical data [1]. In brain MRI sequence classification and analysis, two advanced optimization strategies have demonstrated substantial improvements in model performance and clinical applicability: Clinical Visual Instruction Tuning (CVIT) and Retrieval-Augmented Generation (RAG). CVIT enhances medical domain knowledge through specialized instruction tuning, while RAG frameworks integrate external medical knowledge bases to improve diagnostic precision by leveraging established clinical expertise [18] [44]. These methodologies address critical challenges in medical AI implementation, including domain-specific adaptation, reduction of model hallucination, and enhancement of diagnostic accuracy for complex neurological conditions.
The integration of these strategies within brain MRI research pipelines enables more accurate sequence classification, improved differential diagnosis, and generation of clinically relevant reports. This technical note provides detailed application protocols and implementation frameworks for CVIT and RAG, supported by experimental data and practical workflows for research and clinical implementation.
Clinical Visual Instruction Tuning (CVIT): Protocols and Applications
Core Principles and Implementation Framework
Clinical Visual Instruction Tuning (CVIT) represents a specialized approach to adapting foundation multimodal models for medical domains through structured, clinically-informed instruction sets. Unlike generic visual instruction tuning, CVIT incorporates medical taxonomy, structured reporting templates, and clinical reasoning pathways to enhance model outputs' diagnostic relevance [18] [35]. The fundamental architecture typically maintains a pre-trained visual encoder (such as CLIP ViT), a perceiver resampler for visual feature alignment, and a large language model, with strategic fine-tuning of cross-attention mechanisms while freezing most foundational parameters to preserve general knowledge [35].
Table 1: CVIT Instruction Types and Clinical Applications
| Instruction Type | Key Components | Clinical Applications | Report Quality Impact |
|---|---|---|---|
| Plain Instruction | Basic role definition as radiology assistant | General image description tasks | Baseline performance |
| In-Context Example Instruction | 3-shot examples added to plain instructions | Pattern recognition for common findings | Improved style consistency |
| Template Instruction | Structured clinical QA templates | Standardized reporting formats | Enhanced organizational structure |
| Keyword Instruction | Categorical guidelines focused on keywords | Detailed differential diagnosis | Highest clinical relevance and keyword density |
Implementation of CVIT follows a structured workflow beginning with dataset curation of paired image-text clinical data, followed by instruction template design, model fine-tuning with parameter-efficient methods, and rigorous clinical validation. The BrainGPT implementation demonstrated that CVIT-augmented models significantly outperform baseline models in clinical keyword usage and diagnostic accuracy, with template and keyword instructions showing particular strength in generating clinically coherent reports [18].
Experimental Protocol: CVIT for Brain MRI Report Generation
Materials and Reagents
- Hardware: High-performance computing cluster with A100 GPUs (minimum 4 for efficient training)
- Software: Python 3.8+, PyTorch 2.0+, Transformers library, OpenFlamingo or Otter model framework
- Data: Curated brain MRI dataset with paired images and radiology reports (minimum 5,000 pairs recommended)
- Annotation: Domain expert radiologists for template design and validation
Methodology
- Data Preparation and Curation
- Collect brain MRI studies with corresponding radiology reports
- Anonymize all patient data following HIPAA/comparable guidelines
- Preprocess images: normalize intensities, resize to uniform dimensions (e.g., 224×224), extract representative slices from 3D volumes
- Clean and structure report text: remove identifiers, standardize terminology, segment into findings and impression sections
Instruction Template Design
- Develop structured prompt templates incorporating clinical reasoning pathways
- Define keyword categories relevant to brain MRI: anatomical landmarks, pathological features, severity descriptors, clinical impressions
- Create in-context learning examples demonstrating optimal reporting patterns
- Validate templates with domain experts for clinical appropriateness
Model Fine-Tuning
- Initialize with base multimodal model (e.g., Otter based on OpenFlamingo architecture)
- Freeze visual encoder (CLIP ViT-L/14) and language model (LLaMA-7B) parameters
- Train perceiver resampler and cross-attention layers using low-rank adaptation (LoRA)
- Employ gradual curriculum: begin with plain instructions, progress to template-based, then keyword-enhanced instructions
- Training parameters: batch size 4-8, learning rate 2e-4, cosine scheduler, warmup ratio 0.03
Validation and Evaluation
- Quantitative metrics: FORTE score (analyzing degree, landmark, feature, and impression components)
- Qualitative assessment: expert radiologist evaluation of report clinical utility
- Turing-test evaluation: blinded assessment distinguishing AI-generated from human reports
Retrieval-Augmented Generation (RAG) for Enhanced Diagnostic Accuracy
Architectural Framework and Clinical Implementation
Retrieval-Augmented Generation (RAG) frameworks address critical limitations in standalone LLMs by integrating external medical knowledge bases to enhance diagnostic precision and reduce hallucination. In brain MRI applications, RAG systems combine multimodal data embedding, vector database retrieval, and context-aware generation to provide clinically grounded interpretations [45] [44]. The AlzheimerRAG implementation demonstrates how cross-modal attention fusion techniques can effectively integrate textual and visual data processing, efficiently indexing and accessing vast amounts of biomedical literature to enhance diagnostic accuracy for complex neurological conditions [45].
The fundamental RAG architecture for brain MRI applications comprises four core components: (1) multimodal embedding systems that encode both visual features and textual descriptions into a shared semantic space, (2) vector databases storing curated medical knowledge, (3) retrieval mechanisms employing similarity search to identify relevant clinical references, and (4) generative components that incorporate retrieved context to produce clinically accurate outputs. The Adaptive RAG-Assisted MRI Platform (ARAMP) demonstrated significant improvements in brain metastasis detection, with sensitivity increasing from 0.84 to 0.98 post-RAG integration [44].
Table 2: RAG Framework Performance in Clinical Studies
| Application | Knowledge Base | Retrieval Method | Performance Metrics | Clinical Impact |
|---|---|---|---|---|
| AlzheimerRAG | PubMed articles on Alzheimer's | Cross-modal attention fusion | Improved performance on BioASQ, PubMedQA benchmarks | Accurate synthesis of domain-specific information |
| ARAMP | 5 authoritative medical references | FAISS vector similarity search | Sensitivity: 0.98, Inference Similarity: 67.45% | Improved brain metastasis detection |
| MRI Protocoling | Institutional protocol guidelines | LangChain text splitting + embedding | Sequence prediction: 81%, Contrast: 92% accuracy | Protocol selection comparable to radiologists |
Experimental Protocol: Multimodal RAG for Brain MRI Analysis
Materials and Reagents
- Vector Database: ChromaDB or FAISS for efficient similarity search
- Embedding Models: BiomedCLIP or domain-specific text encoders
- Knowledge Sources: Curated medical literature (PubMed, institutional guidelines)
- Integration Framework: LangChain for pipeline orchestration
Methodology
- Knowledge Base Construction
- Collect domain-specific medical literature: clinical guidelines, radiology textbooks, structured reporting templates
- Process institutional protocols: convert PDF guidelines to structured text, segment by anatomical region and clinical indication
- Implement data cleaning: remove formatting artifacts, standardize terminology, resolve abbreviations
- Chunk documents: recursive character text splitting with 400-600 character chunks, minimal overlap
Multimodal Embedding Generation
- Image encoding: extract features from brain MRI sequences using medical vision transformers
- Text encoding: generate embeddings for clinical questions, findings, and knowledge base content
- Fusion strategy: combine image and text embeddings using weighted summation (e.g., 0.6×image + 0.4×text)
- Dimensionality: 512-768 dimension vectors for balanced performance and efficiency
Vector Database Implementation
- Initialize vector store: ChromaDB or FAISS with cosine similarity indexing
- Populate with embeddings: store multimodal representations of knowledge base content
- Implement adaptive retrieval: dynamic top-K selection based on query complexity (typically 4-7 similar cases)
- Configure metadata filtering: enable filtering by source, date, confidence level
RAG Integration and Inference
- Develop retrieval pipeline: integrate similarity search with confidence thresholding
- Implement prompt engineering: structure context incorporation with explicit citation
- Configure generation parameters: temperature 0.1 for low variability, top-p sampling for diversity control
- Include explanation mechanisms: generate reasoning traces for clinical transparency
Integrated CVIT-RAG Framework for Brain MRI Classification
Synergistic Implementation Protocol
The integration of CVIT and RAG creates a powerful framework for brain MRI sequence classification and analysis, combining the domain-specific tuning of CVIT with the evidence-based grounding of RAG. The MMed-RAG system for MGMT promoter methylation status prediction demonstrates this synergy, achieving 69.2% accuracy in glioblastoma characterization by fusing MRI features with clinical context through retrieval-augmented reasoning [46].
Experimental Protocol: Integrated CVIT-RAG for Brain Tumor Classification
Data Preprocessing Pipeline
- DICOM to standard format conversion: extract middle slices from 3D volumes
- Multi-sequence alignment: co-register T1, T1CE, T2, FLAIR sequences
- Intensity normalization: standardize values across scanners and protocols
- Feature extraction: radiomic features (intensity, texture, shape)
Multimodal Knowledge Base Development
- Curate tumor imaging guidelines: response assessment criteria (RANO), diagnostic pathways
- Annotate exemplar cases: confirmed diagnoses with imaging correlates
- Structure retrieval content: segment by tumor type, molecular signature, imaging characteristics
- Implement hierarchical indexing: enable multi-level similarity matching
Dual-Phase Model Training
Phase 1: CVIT with structured reporting templates
- Instruction design: incorporate radiology lexicon, reporting structure
- Fine-tuning: focus on cross-modal attention layers
- Validation: FORTE metrics for clinical relevance
Phase 2: RAG integration for evidence grounding
- Retrieval mechanism: implement similarity search with clinical context
- Fusion methodology: cross-modal attention between query and retrieved evidence
- Confidence calibration: implement certainty estimation for recommendations
Validation Framework
- Diagnostic accuracy: sensitivity, specificity, AUC for classification tasks
- Clinical utility: expert evaluation of report comprehensiveness and relevance
- Retrieval quality: precision@K for knowledge base access
- Hallucination reduction: measure factual consistency in generated texts
Table 3: Performance Comparison of AI Approaches in Brain MRI Analysis
| Method | Accuracy | F1-Score | Clinical Explainability | Implementation Complexity |
|---|---|---|---|---|
| Zero-Shot CLIP | 41.0% | 36.8% | Low | Low |
| Fine-Tuning Only | 63.2% | 63.3% | Medium | Medium |
| MMed-RAG (CVIT+RAG) | 69.2% | 67.8% | High | High |
| Human Radiologist | 85-90% (est.) | 85-90% (est.) | Native | N/A |
Table 4: Essential Research Reagents and Computational Resources
| Resource Category | Specific Tools/Solutions | Function/Purpose | Implementation Notes |
|---|---|---|---|
| Multimodal Models | Otter (OpenFlamingo), LLaVA-Med, BiomedCLIP | Foundation MLLMs for medical adaptation | Select based on modality support and clinical task requirements |
| Vector Databases | ChromaDB, FAISS, Pinecone | Efficient similarity search and retrieval | ChromaDB recommended for research prototypes; FAISS for scale |
| Medical Knowledge Bases | PubMed Central, Institutional Guidelines, Radiology Teaching Files | Domain knowledge for RAG grounding | Requires curation and structuring for optimal retrieval |
| Instruction Templates | Structured Reporting Templates, Clinical QA Pairs | CVIT implementation for clinical alignment | Domain expert validation essential for clinical appropriateness |
| Evaluation Frameworks | FORTE (Feature-Oriented Radiology Task Evaluation), Traditional NLP Metrics | Performance assessment for clinical relevance | FORTE captures clinical essence better than traditional metrics |
| Feature Extraction | PyRadiomics, MONAI, Custom CNN Architectures | Quantitative imaging biomarker extraction | Essential for radiogenomic applications and precision medicine |
The integration of Clinical Visual Instruction Tuning and Retrieval-Augmented Generation represents a paradigm shift in brain MRI sequence classification research. CVIT provides the clinical framing and domain-specific reasoning capabilities, while RAG ensures evidence-based grounding and access to current medical knowledge. The experimental protocols outlined herein provide researchers with practical frameworks for implementing these advanced methodologies in neuroimaging research.
Future development directions include dynamic retrieval optimization, where the system automatically adjusts the retrieval strategy based on query complexity and uncertainty, and federated RAG implementations that enable multi-institutional knowledge sharing while preserving data privacy. Additionally, the emerging capability of foundation models for multimodal MRI synthesis guided by textual imaging metadata, as demonstrated by TUMSyn, presents promising avenues for data augmentation and resolution enhancement in resource-constrained settings [47].
As these technologies mature, their integration into clinical workflows holds significant potential for enhancing diagnostic accuracy, reducing interpretation variability, and ultimately improving patient outcomes in neurological disorders. The protocols and applications detailed in this technical note provide a foundation for continued innovation at the intersection of artificial intelligence and neuroimaging.
The development of sophisticated multimodal large language models (LLMs) for brain MRI sequence classification is critically constrained by the scarcity of large, accurately annotated datasets. The process of generating expert-curated radiology reports is both time-consuming and expensive, creating a significant data bottleneck that impedes research progress and clinical application. This challenge is particularly acute in specialized domains or for rare conditions where data is inherently limited. Within this context, the strategic generation of pseudo-reports and the utilization of weakly paired datasets have emerged as transformative methodologies for bypassing these constraints and enabling the training of robust models without exhaustive manual annotation efforts [13].
Recent research demonstrates that these approaches are not merely stopgap measures but represent a fundamental shift in how we leverage available data. As highlighted in a 2025 review of deep learning for brain tumor analysis, maximizing potential in report-limited environments without additional training is crucial for advancing the field [48]. The application of pseudo-reports allows researchers to synthesize the informational value of structured radiology reports from limited examples, thereby creating the scale of labeled data required for training complex models like vision-language segmentation models (VLSM) [13]. Concurrently, weakly paired datasets—where images and text reports are associated but not perfectly aligned at a fine-grained level—provide a rich, if noisy, source of information that can be algorithmically refined.
This document provides detailed Application Notes and Protocols for implementing these data-enhancement strategies, specifically framed within multimodal LLM research for brain MRI. It is intended to equip researchers, scientists, and drug development professionals with the practical methodologies needed to accelerate their model development pipelines, ultimately contributing to more accurate diagnostic tools and personalized treatment strategies in neuro-oncology.
Application Notes
Core Concepts and Definitions
- Pseudo-Reports: Automatically generated textual descriptions of brain MRI scans that mimic the structure and content of expert radiology reports. These are used as supervisory signals for training vision-language models when genuine annotated reports are scarce. They are synthesized by algorithms to capture key observations such as tumor presence, sequence type, and anatomical features [13].
- Weakly Paired Datasets: Collections of brain MRI scans and their corresponding radiology reports where the alignment between specific imaging findings and text passages is not explicitly guaranteed or meticulously annotated. The pairing exists at the whole-exam or whole-study level, requiring models to learn correlations without direct, pixel-level or lesion-specific text labels [13].
- Vision-Language Segmentation Model (VLSM): A deep learning architecture that processes both visual (MRI scans) and textual (reports or pseudo-reports) data to perform pixel-level segmentation of pathological features. The integration of text provides contextual guidance, improving segmentation accuracy and specificity [13].
Performance Analysis of a Pseudo-Report Generation Approach
A seminal study presented at the ISMRM 2025 Annual Meeting detailed a novel pseudo-report generation approach designed to maximize the utility of VLSMs in environments with limited genuine reports. The research was conducted on a weakly paired stroke dataset and yielded significant performance improvements, demonstrating the practical efficacy of this strategy [13].
Table 1: Quantitative Performance of Pseudo-Report Enhanced VLSM on a Stroke Dataset
| Metric | Image-Only Model | VLSM with Only 10% Genuine Reports | VLSM with Pseudo-Reports (Using 10% Genuine Reports) |
|---|---|---|---|
| Segmentation Accuracy (DSC) | Baseline | Lower than Pseudo-Report | Outperforms Image-Only Model |
| False Positive Reduction | Baseline | Moderate Improvement | More Effective Reduction |
| Data Efficiency | N/A | Low | High (Leverages weak labels) |
Key Findings:
- The model leveraging pseudo-reports, trained with only 10% of the genuine reports available, successfully outperformed conventional image-only segmentation models [13].
- A primary benefit observed was a more effective reduction in false positives compared to other methods, indicating that the text guidance from pseudo-reports helps the model discount irrelevant image features [13].
- This approach provides a highly practical clinical benefit by enhancing segmentation efficiency without the need for a fully annotated, large-scale dataset, thus directly addressing the core data bottleneck [13].
Experimental Protocols
Protocol 1: Generating Pseudo-Reports for a Weakly Paired Brain MRI Dataset
Objective: To create a large-scale corpus of pseudo-reports from a weakly paired dataset of brain MRI scans and their corresponding radiology reports, enabling the training of a vision-language model.
Materials:
- Hardware: High-performance computing workstation with multiple GPUs (e.g., NVIDIA A100 or H100).
- Software: Python 3.8+, PyTorch or TensorFlow, Natural Language Processing libraries (e.g., Hugging Face Transformers), DICOM image processing libraries (e.g., PyDICOM, SimpleITK).
- Dataset: A weakly paired dataset of brain MRI volumes (e.g., T1, T2, FLAIR, T1CE) and their corresponding textual radiology reports.
Procedure:
- Data Preprocessing:
- Image Processing: Convert DICOM files to NIfTI format. Perform skull-stripping, intensity normalization (e.g., Z-score), and co-registration of all sequences to a common space (e.g., MNI152).
- Text Processing: De-identify radiology reports. Perform standard NLP preprocessing: tokenization, lowercasing, and removal of stop words and punctuation.
Model Fine-Tuning for Report Generation:
- Select a pre-trained multimodal LLM (e.g., a vision transformer encoder coupled with a language decoder like LLaMA or GPT-2).
- Train the model on the available genuine paired data (even if limited) to establish a baseline understanding of mapping imaging features to textual descriptions. The training objective is a text-generation loss, where the model learns to predict the next token in the report sequence given the image and the previous tokens.
Pseudo-Report Synthesis:
- For each MRI scan in the broader, weakly paired dataset (including those without reports), use the fine-tuned model from Step 2 to generate a synthetic radiology report.
- Employ beam search or nucleus sampling during generation to ensure fluent and diverse text output.
- This step effectively expands the labeled training set from a small number of genuine image-report pairs to a large number of image-pseudo-report pairs.
Validation:
- Engage a panel of radiologists or trained experts to blindly evaluate a random subset of the generated pseudo-reports against their genuine counterparts (where available). Use metrics like clinical accuracy, relevance, and completeness on a Likert scale (1-5).
- The final output is a large-scale, strongly paired dataset of MRI scans and high-quality pseudo-reports ready for downstream VLSM training.
Diagram 1: Pseudo-report generation workflow.
Protocol 2: Training a Vision-Language Segmentation Model (VLSM) with Pseudo-Reports
Objective: To train a VLSM for precise brain tumor (e.g., glioma) segmentation using the dataset augmented with pseudo-reports.
Materials:
- Dataset: The strongly paired dataset of MRI scans and pseudo-reports generated in Protocol 1.
- Hardware/Software: Same as Protocol 1, with additional libraries for image segmentation (e.g., MONAI, nnUNet).
Procedure:
- Model Architecture Setup:
- Implement a VLSM architecture. This typically consists of:
- A Visual Encoder (e.g., a 3D U-Net or Vision Transformer) to extract hierarchical image features from the MRI volumes.
- A Text Encoder (e.g., a pre-trained BERT or ClinicalBERT model) to encode the paired pseudo-report into a text embedding.
- A Fusion Module that integrates image and text features, often via cross-attention or concatenation in a latent space.
- Implement a VLSM architecture. This typically consists of:
Training with Text Guidance:
- The model is trained with a combined loss function:
- ( \mathcal{L}{total} = \mathcal{L}{Dice} + \lambda \mathcal{L}_{Cross-Entropy} )
- The primary segmentation loss (( \mathcal{L}_{Dice} )) is computed between the model's predicted segmentation mask and the ground-truth manual segmentation (available for a subset of scans).
- The text guidance is implicit in the fusion mechanism; the model learns to attend to image regions that are relevant to the descriptions in the pseudo-report.
- The model is trained with a combined loss function:
Evaluation:
- Evaluate the trained VLSM on a held-out test set with expert-validated segmentations.
- Use standard segmentation metrics: Dice Similarity Coefficient (DSC), Hausdorff Distance, and Sensitivity/Specificity.
- Compare its performance against an ablated model trained without text guidance (i.e., an image-only model) to quantify the benefit of the pseudo-reports.
Diagram 2: VLSM training architecture with pseudo-reports.
The Scientist's Toolkit
Table 2: Essential Research Reagents and Computational Materials
| Item | Function/Application in Research | Example/Specification | ||||||
|---|---|---|---|---|---|---|---|---|
| Pre-trained Multimodal LLM | Serves as the foundational model for generating pseudo-reports. Provides initial language and vision understanding. | Models like LLaMA-Vision, BioMed-VLP, or a fine-tuned GPT for radiology. | ||||||
| Weakly Paired Brain MRI Dataset | The raw material containing the images and text from which knowledge is extracted and synthesized. | Public datasets (e.g., BraTS with clinical descriptions) or institutional PACS data. | ||||||
| Visual Encoder (3D CNN/ViT) | Extracts spatial and contextual features from volumetric MRI data, forming the visual understanding branch of the VLSM. | Architectures such as 3D U-Net, EfficientNet-3D, or Vision Transformer (ViT). | ||||||
| Text Encoder | Processes the pseudo-reports into dense numerical representations (embeddings) that capture semantic meaning. | Pre-trained language models like BERT, RoBERTa, or their clinical variants (e.g., ClinicalBERT). | ||||||
| Fusion Module | The critical component that integrates features from the visual and textual encoders, enabling the model to link image regions with descriptive text. | Cross-attention layers, feature concatenation, or tensor fusion networks. | ||||||
| Segmentation Decoder | Translates the fused multimodal features into a pixel-level segmentation mask, identifying tumor sub-regions. | Typically the decoder arm of a U-Net-like architecture. | ||||||
| Dice Loss Function | A robust loss function for optimizing model performance on class-imbalanced medical image segmentation tasks. | ( \mathcal{L}_{Dice} = 1 - \frac{2 \times | X \cap Y | }{ | X | + | Y | } ) |
Benchmarking Performance: A Rigorous Comparative Analysis of Leading MLLMs
The deployment of multimodal large language models (MLLMs) in medical imaging, particularly for brain MRI analysis, faces a significant validation challenge: traditional Natural Language Processing (NLP) metrics are insufficient for capturing clinical diagnostic quality. These conventional metrics, including BLEU, ROUGE, and METEOR, were primarily designed for general machine translation and text summarization tasks, focusing on n-gram overlap and lexical similarity rather than clinical accuracy and completeness [49]. This limitation becomes critically apparent in radiology report generation (RRG), where diagnostic fidelity—the precise identification of pathological features, their locations, and clinical significance—far outweighs grammatical perfection or lexical variation.
The Feature-Oriented Radiology Task Evaluation (FORTE) framework emerges as a specialized solution to this challenge. FORTE is a novel evaluation scheme specifically engineered to capture the clinical essence of AI-generated radiology reports [49] [50] [51]. Unlike traditional metrics that assess surface-level text similarity, FORTE operates by decomposing radiology reports into four clinically essential keyword components—degree, landmark, feature, and impression—then evaluating the model's performance in accurately generating these critical elements. This paradigm shift in evaluation methodology enables researchers to quantitatively measure whether AI systems capture diagnostically relevant information, moving beyond superficial textual comparisons to assess genuine clinical utility.
FORTE's Technical Architecture and Implementation
Component-Based Evaluation Structure
FORTE's analytical power derives from its structured decomposition of radiology reports into semantically distinct clinical categories. Each category targets a specific dimension of diagnostic information essential for clinical decision-making [49]:
- Degree: Quantifies the extent, size, or severity of pathological findings (e.g., "small," "severe," "progressive").
- Landmark: Identifies the precise anatomical location of abnormalities (e.g., "right frontal lobe," "cerebellar vermis").
- Feature: Describes the pathological characteristics and observations (e.g., "edema," "mass effect," "restricted diffusion").
- Impression: Captures the overall diagnostic interpretation and clinical significance (e.g., "consistent with acute infarction," "neoplasm cannot be excluded").
This categorical approach enables granular performance assessment across different aspects of radiological interpretation, revealing specific strengths and limitations in MLLM capabilities that would remain obscured by traditional metrics.
Quantitative Scoring Methodology
FORTE employs an F1-score based evaluation for each component category, balancing precision (correct identification of relevant features) and recall (completeness in identifying all relevant features) [49]. The framework utilizes term frequency-inverse document frequency (TF-IDF) principles to weight the importance of different radiological terms, giving higher value to specific, clinically significant terminology over common radiological phrases. This approach effectively measures how well MLLMs utilize diagnostically meaningful vocabulary in their generated reports.
Table 1: FORTE Performance Benchmark in Brain CT Report Generation
| Evaluation Component | F1-Score | Precision | Recall |
|---|---|---|---|
| Degree | 0.661 | Not Reported | Not Reported |
| Landmark | 0.706 | Not Reported | Not Reported |
| Feature | 0.693 | Not Reported | Not Reported |
| Impression | 0.779 | Not Reported | Not Reported |
| Overall Average | 0.710 | Not Reported | Not Reported |
Data sourced from BrainGPT validation studies on 3D-BrainCT dataset (n=18,885 text-scan pairs) [49]
The implementation of FORTE typically involves a structured pipeline: (1) report preprocessing with sentence pairing and negation removal to enhance alignment; (2) automated extraction and categorization of key terms using clinical ontologies; (3) matching against ground truth annotations from expert radiologists; and (4) calculation of component-specific and aggregate performance scores [49].
Experimental Protocol for FORTE Implementation
Materials and Computational Setup
Table 2: Essential Research Reagents and Computational Resources
| Resource Category | Specific Examples | Function in FORTE Implementation |
|---|---|---|
| Medical Imaging Datasets | 3D-BrainCT (18,885 text-scan pairs) [49], Kaggle Brain Tumor MRI Dataset [52] | Provides paired image-report data for training and validation |
| MLLM Architectures | BrainGPT (CVIT-tuned) [49], GPT-4o, Claude 4 Opus, Gemini 2.5 Pro [2] | Base models for radiology report generation and sequence classification |
| Evaluation Frameworks | FORTE Python Implementation, Traditional NLP Metrics (BLEU, ROUGE, CIDEr) [49] | Enables comparative performance assessment |
| Clinical Validation Tools | Turing-like Test Framework, Radiologist Annotation Platform [49] | Facilitates human evaluation of report quality |
| Computational Infrastructure | High-Memory GPU Clusters, 3D CNN Compatible Systems [49] [53] | Supports processing of volumetric medical imaging data |
Step-by-Step FORTE Implementation Protocol
Phase 1: Dataset Preparation and Preprocessing
- Data Curation: Assemble a comprehensive dataset of brain MRI studies with corresponding radiology reports. The 3D-BrainCT dataset exemplifies the scale required, with 18,885 text-scan pairs [49].
- Report Annotation: Engage board-certified radiologists to annotate ground truth reports according to FORTE categories (degree, landmark, feature, impression). Establish inter-rater reliability metrics to ensure annotation consistency.
- Sentence Pairing: Decompose lengthy report paragraphs into individual sentences corresponding to specific observations. Research indicates this step alone can increase traditional metric scores by an average of 5.28 points in METEOR and 6.48 points in ROUGE-L [49].
- Negation Removal: Implement natural language processing techniques to identify and standardize negated findings (e.g., "no mass effect" → "mass effect: absent") to improve matching accuracy.
Phase 2: Model Training and Fine-Tuning
- Baseline Establishment: Implement current state-of-the-art MLLMs (e.g., Otter) as baseline models before clinical fine-tuning [49].
- Clinical Visual Instruction Tuning (CVIT): Apply specialized fine-tuning approaches that enhance medical domain knowledge:
- Template Instruction: Incorporate structured clinical QA templates
- Keyword Instruction: Emphasize categorical guidelines focused on diagnostically critical terminology [49]
- Anatomy-Aware Training: Utilize spatial attention mechanisms similar to those employed in 3D CNN architectures for brain age estimation to enhance localization capabilities [53].
Phase 3: Evaluation and Validation
- Automated FORTE Scoring: Compute component-specific F1 scores for generated reports against expert-annotated ground truth.
- Traditional Metric Comparison: Calculate conventional NLP metrics (BLEU, ROUGE, CIDEr) to demonstrate FORTE's advantages.
- Human Evaluation: Implement Turing-like tests where radiologists assess whether reports were generated by AI or human experts. In validation studies, 74% of BrainGPT-generated reports were indistinguishable from human-written ground truth [49].
- Cross-Dataset Validation: Test generalizability using external datasets (e.g., CQ500) to evaluate performance consistency across different institutions and populations.
FORTE Implementation Workflow: A three-phase protocol for implementing the FORTE framework in brain MRI research.
FORTE Validation in Brain MRI Sequence Classification
Integration with Multimodal LLM Research
The application of FORTE extends naturally to brain MRI sequence classification, where MLLMs must demonstrate proficiency in both recognizing technical sequence parameters and generating clinically accurate interpretations. Recent studies evaluating multimodal LLMs (GPT-4o, Claude 4 Opus, Gemini 2.5 Pro) on brain MRI sequence identification reveal critical performance variations—with sequence classification accuracy ranging from 73.1% to 97.7% across models [2]. These findings highlight the necessity for evaluation frameworks like FORTE that can discern clinically meaningful differences in model performance beyond basic recognition tasks.
FORTE's component-based approach aligns with the hierarchical complexity of MRI interpretation, where accurate sequence identification constitutes only the foundational layer of clinical assessment. The framework enables researchers to evaluate whether models can not only identify a T2-weighted FLAIR sequence, for instance, but also correctly interpret hyperintense lesions, localize them to specific neuroanatomical regions, assess their clinical significance, and generate appropriate differential diagnoses—all essential elements of radiologic practice.
Comparative Performance Analysis
Table 3: FORTE vs. Traditional Metrics in Evaluating MLLM Performance
| Evaluation Metric | Sensitivity to Clinical Quality | Granular Component Analysis | Correlation with Diagnostic Accuracy | Implementation Complexity |
|---|---|---|---|---|
| FORTE | High | Yes (4 components) | Strong | Moderate |
| BLEU | Low | No | Weak | Low |
| ROUGE-L | Low | No | Weak | Low |
| METEOR | Low-Moderate | No | Moderate | Low |
| CIDEr | Moderate | No | Moderate | Moderate |
Comparative analysis based on validation studies from BrainGPT development [49]
Research demonstrates that while traditional metrics often fail to reflect clinical utility, FORTE scores show strong correlation with diagnostic accuracy and radiologist assessments. In development of BrainGPT, traditional metrics showed minimal sensitivity to increasingly sophisticated clinical instruction tuning methods, whereas FORTE scores progressively improved with advanced Clinical Visual Instruction Tuning (CVIT) approaches [49]. This differential sensitivity makes FORTE particularly valuable for optimizing MLLMs toward clinical applicability rather than mere textual fluency.
Advanced Applications and Research Directions
Integration with Emerging MLLM Architectures
The FORTE framework provides an essential validation component for cutting-edge MLLM architectures specifically designed for medical imaging applications. Models like Glio-LLaMA-Vision, which performs molecular prediction, radiology report generation, and visual question answering for adult-type diffuse gliomas, require evaluation metrics that transcend traditional NLP scores [13]. Similarly, SeqGPT, which generates MRI pulse sequences, needs assessment frameworks that can evaluate both technical correctness and clinical relevance [13].
FORTE's modular design enables adaptation to these specialized applications through component customization. For stroke classification tasks, FORTE components could be weighted to emphasize vascular territories and diffusion-perfusion mismatches [54]. For brain tumor characterization, components could prioritize molecular markers, enhancement patterns, and mass effect quantification. This flexibility ensures FORTE's continued relevance as MLLM capabilities expand into increasingly specialized clinical domains.
Protocol for FORTE-Enhanced Model Optimization
For researchers aiming to optimize MLLMs using FORTE metrics, we recommend this iterative refinement protocol:
- Baseline Assessment: Evaluate current model performance using both FORTE components and traditional metrics.
- Component Gap Analysis: Identify which FORTE categories (degree, landmark, feature, impression) show the largest performance gaps compared to expert benchmarks.
- Targeted Fine-Tuning: Implement specialized training regimens addressing specific deficiencies:
- For weak "landmark" performance: Enhance anatomical localization through spatial attention mechanisms [53]
- For weak "impression" performance: Incorporate diagnostic reasoning chains through chain-of-thought prompting
- Hallucination Mitigation: Implement retrieval-augmented generation (RAG) techniques to reduce factual inaccuracies, a known issue in general-purpose MLLMs [2] [13]
- Validation Cycle: Re-assess using FORTE metrics and iterate until clinical performance plateaus.
FORTE Component Structure: The four evaluative components of FORTE with their performance benchmarks and clinical applications.
The FORTE framework represents a paradigm shift in how the medical AI research community evaluates and validates multimodal LLMs for brain MRI applications. By moving beyond traditional NLP scores to capture clinically essential elements of radiological interpretation, FORTE addresses the critical gap between technical performance and diagnostic utility. As MLLMs continue to evolve in capabilities—from basic sequence recognition to comprehensive report generation and clinical decision support—robust, clinically-grounded evaluation frameworks like FORTE will become increasingly essential for ensuring these advanced AI systems deliver genuine value in patient care settings.
The implementation protocols, validation methodologies, and optimization strategies outlined in this document provide researchers with a comprehensive toolkit for integrating FORTE into their MLLM development pipelines. Through widespread adoption of clinically meaningful evaluation metrics, the research community can accelerate the development of AI systems that not only achieve impressive technical benchmarks but also demonstrate tangible improvements in diagnostic accuracy, workflow efficiency, and ultimately, patient outcomes.
Within the broader thesis on multimodal large language models (MLLMs) for brain MRI sequence classification research, this document establishes application notes and protocols. The ability to accurately classify MRI sequences is a foundational competency, as misidentification can lead to incorrect clinical interpretation [2]. This analysis provides a structured comparison of three advanced MLLMs—ChatGPT-4o (OpenAI), Gemini 2.5 Pro (Google), and Claude 4 Opus (Anthropic)—focusing on their performance in recognizing basic imaging features and specific brain MRI sequences, thereby offering researchers a clear understanding of their current capabilities and limitations [2] [17].
A direct comparative study evaluated the models using 130 brain MRI images representing 13 standard sequences in a zero-shot prompting setting [2]. The table below summarizes their performance across five critical classification tasks.
Table 1: Model Performance on Fundamental Brain MRI Recognition Tasks
| Classification Task | ChatGPT-4o | Claude 4 Opus | Gemini 2.5 Pro |
|---|---|---|---|
| Modality Identification | 100% | 100% | 100% |
| Anatomical Region Recognition | 100% | 100% | 100% |
| Imaging Plane Classification | 100% | 99.23% | 100% |
| Contrast-Enhancement Status | 98.46% | 95.38% | 98.46% |
| MRI Sequence Classification | 97.69% | 73.08% | 93.08% |
For the primary task of MRI sequence classification, statistical analysis using Cochran’s Q test revealed a statistically significant difference in model performance (p < 0.001) [2]. Pairwise comparisons confirmed that ChatGPT-4o and Gemini 2.5 Pro significantly outperformed Claude 4 Opus [2].
It is crucial to note that model performance can vary significantly with different tasks and datasets. A separate, larger-scale study involving 35,711 MRI slices reported different absolute accuracy figures for pathology and sequence prediction, though it confirmed the challenging nature of these visual tasks [55]. Furthermore, another study highlighted that ChatGPT-4o's diagnostic accuracy is highly dependent on input, dropping to as low as 19.90% in "image-only" conditions and rising to over 80% when clinical context and diagnostic options are provided [56].
Detailed Experimental Protocol
The following protocol is adapted from the comparative study by Salbas et al. to ensure reproducible evaluation of MLLMs on brain MRI sequence classification [2].
Materials and Setup
- Model Versions: The most up-to-date versions of ChatGPT-4o, Claude 4 Opus, and Gemini 2.5 Pro available at the time of testing. All evaluations should be completed within a short, defined period to avoid confounding effects from model updates.
- Dataset Curation:
- Source: Collect brain MRI images from a Picture Archiving and Communication System (PACS).
- Content: Include images from adult patients without pathological findings to focus the evaluation on sequence recognition rather than pathology detection.
- Sequences: Ensure representation of key sequences. The referenced study used 10 images each of 13 sequences, including Axial T1-weighted (T1w), T2-weighted (T2w), FLAIR, DWI, ADC, SWI, and contrast-enhanced T1w in multiple planes [2].
- Anonymization: Remove all patient-identifiable information and metadata from images.
- Format: Export images in high-quality JPEG or PNG format without annotations, arrows, or text overlays, preserving original resolution.
Prompting and Data Collection
- Prompt Design: Use a standardized, zero-shot prompt in English to ensure consistency. The prompt should clearly state the research purpose and request specific information. For example: > "This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: > 1. What type of radiological modality is this examination? > 2. Which anatomical region does this examination cover? > 3. What is the imaging plane (axial, sagittal, or coronal)? > 4. Is this a contrast-enhanced image or not? > 5. If this image is an MRI, what is the specific MRI sequence? If it is not an MRI, write 'Not applicable.' > Please number your answers clearly."
- Session Management: Initiate a new, separate session (clearing chat history) for each image query. This prevents in-context adaptation, where a model's response could be influenced by previous interactions in the same session [2].
- Data Recording: Systematically record all model responses in a structured format (e.g., a spreadsheet) for subsequent analysis.
Analysis and Validation
- Ground Truth: Establish a ground truth for all images, verified by at least two board-certified radiologists in consensus.
- Performance Metrics: Calculate accuracy for each task (number of correct responses / total responses). For the primary task of sequence classification, use statistical tests like Cochran's Q test for overall model comparison and McNemar tests with Bonferroni correction for pairwise analysis [2].
- Error Analysis: Log all misclassifications and analyze patterns (e.g., which sequences are frequently confused). Document instances of hallucination, defined as the model generating information unrelated to the input image or prompt context [2] [57].
Experimental Workflow Visualization
The following diagram illustrates the step-by-step experimental procedure for a standardized model evaluation.
The Scientist's Toolkit: Research Reagent Solutions
This table details the key "research reagents" or essential components required to conduct a robust evaluation of MLLMs for brain MRI classification.
Table 2: Essential Research Materials and Their Functions
| Item | Function/Description | Research Purpose |
|---|---|---|
| Curated Brain MRI Dataset | A set of anonymized, high-quality brain images with verified sequence types and no pathologies. | Serves as the standardized input stimulus to benchmark model performance objectively. |
| Standardized Prompt Protocol | A pre-defined, unambiguous text prompt in English, used consistently across all models. | Ensures experimental consistency and reproducibility by eliminating prompt variability as a confounding factor. |
| Radiologist-Consensus Ground Truth | Expert-validated labels for modality, anatomy, plane, contrast, and sequence for every image. | Provides the gold standard against which model outputs are measured for accuracy. |
| Statistical Analysis Scripts | Code for calculating accuracy, Cochran's Q test, McNemar test, and confidence intervals. | Enables quantitative, statistically sound comparison of model performances and significance testing. |
| Model Access APIs/Interfaces | Official web interfaces or APIs for the MLLMs (ChatGPT-4o, Claude 4 Opus, Gemini 2.5 Pro). | The platform through which models are queried and responses are collected. |
The comparative data indicates that while current MLLMs like ChatGPT-4o and Gemini 2.5 Pro show high proficiency in basic MRI image recognition and specific sequence classification, Claude 4 Opus lags in this particular visual task [2]. However, all models are prone to limitations, including hallucinations and a heavy reliance on clinical context for complex diagnostic tasks [2] [56].
For the research community, these findings underscore that MLLMs are not yet ready for autonomous clinical application in image interpretation. Their strength currently lies in acting as a powerful assistive tool. Research shows that a human-AI collaborative workflow, where radiologists use LLMs for differential diagnosis support, can significantly improve diagnostic accuracy compared to conventional methods [57]. Future work should focus on rigorous external validation, developing strategies to mitigate hallucinations, and exploring advanced fine-tuning techniques like Clinical Visual Instruction Tuning (CVIT) to enhance the clinical reasoning capabilities of these models [18].
Within the field of medical imaging informatics, the accurate classification of brain Magnetic Resonance Imaging (MRI) sequences is a critical prerequisite for building labeled datasets essential to deep learning research and clinical workflows. Traditional approaches, primarily Convolutional Neural Networks (CNNs) and string-matching of Digital Imaging and Communications in Medicine (DICOM) headers, have long been employed for this task. However, the recent emergence of Multimodal Large Language Models (MLLMs), which can process and interpret both text and images, presents a new paradigm. This application note provides a comparative analysis of these methodologies, summarizing recent performance data, detailing experimental protocols, and outlining essential research tools to guide researchers and scientists in selecting appropriate technologies for brain MRI sequence classification.
Performance Comparison & Quantitative Analysis
Recent studies directly comparing MLLMs, CNNs, and string-matching classifiers reveal a nuanced performance landscape. The quantitative findings are summarized in the table below.
Table 1: Performance Comparison of MRI Sequence Classification Models
| Model Type | Specific Model | Reported Accuracy | Key Strengths | Key Limitations |
|---|---|---|---|---|
| Multimodal LLM | GPT-4-based LLM [3] | 0.83 (Sensitivity & Specificity also high) | High accuracy, model interpretability, minimizes false positives [3] | Performance varies significantly by specific model [17] |
| Multimodal LLM | ChatGPT-4o [17] [58] | 0.977 (97.7%) | Excellent on imaging plane & contrast-enhancement status [17] [58] | Occasional hallucinations (e.g., adding irrelevant clinical details) [17] |
| Multimodal LLM | Gemini 2.5 Pro [17] [58] | 0.931 (93.1%) | Excellent on imaging plane & contrast-enhancement status [17] [58] | Occasional hallucinations [17] |
| Multimodal LLM | Claude 4 Opus [17] [58] | 0.731 (73.1%) | N/A | Lower accuracy, particularly on SWI and ADC sequences [17] |
| CNN / Hybrid CNN | MedViT (Hybrid) [4] | 0.893 - 0.905 (After expert adjustment) | Robust to domain shift (e.g., adult to pediatric data) [4] | Performance degrades under significant domain shift without adaptation [4] |
| CNN | Custom 3D CNN [59] | 0.80 (Glioma Classification) | Superior spatial understanding for segmentation tasks [59] | Limited to image data, requires large labeled datasets |
| Traditional Method | String-Matching [3] | Lower than LLM & CNN (exact value not reported) | Simple to implement, fast | Unreliable due to non-standardized DICOM metadata [3] [4] |
The data indicates that top-performing MLLMs like ChatGPT-4o can surpass both traditional CNNs and string-matching in classification accuracy under controlled conditions [3] [17]. However, CNN-based architectures, particularly hybrid models like MedViT, demonstrate superior robustness against domain shift—a critical challenge in multicenter studies where imaging protocols, scanner types, and patient demographics (e.g., adult vs. pediatric) vary [4]. A significant weakness observed in some MLLMs is their tendency to produce confabulations or "hallucinations," inventing clinical details not present in the images, which raises concerns for clinical deployment [17].
Detailed Experimental Protocols
To ensure reproducible and comparable results, researchers should adhere to standardized experimental protocols. The following sections detail the methodologies used for evaluating MLLMs and CNN-based models.
Protocol for MLLM Evaluation (Zero-Shot)
This protocol is adapted from studies evaluating MLLMs like ChatGPT-4o and Gemini 2.5 Pro [17] [58].
- Objective: To evaluate the zero-shot capability of MLLMs in identifying basic image characteristics and specific MRI sequences.
- Dataset:
- Composition: 130 brain MRI images from adult patients without pathological findings.
- Sequence Coverage: 13 standard series, including T1w (axial, sagittal, contrast-enhanced), T2w (axial, coronal), FLAIR (axial, coronal, sagittal), DWI, ADC, and SWI.
- Standards: A single representative slice per series, exported in high-quality JPEG format with no annotations, compression, or cropping. Resolution should be preserved (e.g., minimum 994 × 1382 pixels) [17] [58].
- Prompting Strategy:
- Use a standardized, structured prompt in English.
- Initiate a new chat session for each image to prevent in-context adaptation.
- Example Prompt: "This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: 1. What type of radiological modality is this examination? 2. Which anatomical region does this examination cover? 3. What is the imaging plane (axial, sagittal, or coronal)? 4. Is this a contrast-enhanced image or not? 5. If this image is an MRI, what is the specific MRI sequence? If it is not an MRI, write 'Not applicable.' Please number your answers clearly." [17] [58]
- Evaluation:
- Responses are independently reviewed by two radiologists in consensus and classified as "correct" or "incorrect."
- Primary metric: Accuracy for sequence classification. Secondary metrics: Accuracy for modality, plane, and contrast-enhancement status.
- Analyze misclassification patterns and note any hallucinations [17] [58].
Figure 1: Experimental workflow for zero-shot MLLM evaluation.
Protocol for CNN-Based Model Training & Evaluation
This protocol is synthesized from studies using CNNs and hybrid models for sequence classification and tumor analysis [59] [4] [60].
- Objective: To train and evaluate a CNN or CNN-Transformer model for MRI sequence classification, assessing its performance and robustness to domain shift.
- Dataset:
- Preprocessing & Augmentation:
- Model Training:
- Models: Pre-trained ResNet-18 or a hybrid architecture like MedViT.
- Training Loop: Use stratified k-fold cross-validation. Train for ~200 epochs with Adam optimizer and cross-entropy loss. Apply class weighting to handle imbalance [4].
- Domain Shift Mitigation:
- Strategy: Incorporate expert domain knowledge to adjust the model's decision-making process for the target domain (e.g., ignoring labels not present in the pediatric test set) [4].
- Evaluation:
- Primary metrics: Accuracy, Specificity, Sensitivity with 95% confidence intervals.
- Compare performance on in-domain test sets versus out-of-domain (domain-shift) test sets [4].
Figure 2: CNN-based model training and domain shift evaluation workflow.
The Scientist's Toolkit: Research Reagents & Materials
The following table lists key resources and their functions for conducting research in brain MRI sequence classification.
Table 2: Essential Research Materials and Resources
| Resource Name | Type | Function in Research | Example/Reference |
|---|---|---|---|
| BraTS Dataset | Imaging Dataset | Benchmark dataset for glioma classification, segmentation, and model training; contains multi-modal MRI scans. [59] [61] | BraTS 2020 [59] |
| OmniBrainBench | Benchmark & VQA Dataset | Comprehensive benchmark for evaluating MLLMs across 15 imaging modalities and 15 clinical tasks in brain imaging. [10] | 9,527 VQA pairs, 31,706 images [10] |
| ResNet-18 / MedViT | Deep Learning Model | Pre-trained architectures for image classification. MedViT, a CNN-Transformer hybrid, shows robustness to domain shift. [4] | MedViT achieved 0.905 accuracy [4] |
| DICOM Metadata | Data Source | Source of information for string-matching classifiers, though often unreliable due to a lack of standardization. [4] | DICOM headers [3] [4] |
| Gaussian Filter / Noise | Preprocessing Tool | Used to blur images and reduce high-frequency noise, or as a data augmentation technique to improve model robustness. [4] [60] | Gaussian noise (mean=0, std=0.1) [4] |
| Stratified K-Fold Cross-Validation | Evaluation Technique | Reduces overfitting risk and ensures reliable performance estimates by maintaining class distribution across data splits. [4] [62] | 5-fold cross-validation [62] |
In the evaluation of diagnostic tools, particularly within the innovative field of multimodal Large Language Models (LLMs) for brain MRI sequence classification, sensitivity and specificity are foundational metrics for assessing clinical reliability. Sensitivity, or the true positive rate, measures a test's ability to correctly identify patients with a condition. Specificity, or the true negative rate, measures its ability to correctly identify patients without the condition [63] [64]. These prevalence-independent metrics are intrinsic properties of a test, providing a core understanding of its performance separate from the population it is applied to [63] [65]. In the context of AI-driven medical image analysis, a profound understanding of the interplay between sensitivity and specificity is critical for validating model outputs and ensuring their safe integration into clinical workflows, such as the diagnostic and treatment planning continuum for neurological disorders [10].
Core Definitions and Calculations
The mathematical definitions for sensitivity and specificity are derived from a 2x2 contingency table that cross-references the test results with the true disease status, as established by a gold standard [63] [64].
Sensitivity is defined as the probability of a positive test result given that the patient truly has the disease. It is calculated as the number of true positives divided by the sum of true positives and false negatives [63] [66].
Sensitivity = True Positives / (True Positives + False Negatives)Specificity is defined as the probability of a negative test result given that the patient is well. It is calculated as the number of true negatives divided by the sum of true negatives and false positives [63] [66].
Specificity = True Negatives / (True Negatives + False Positives)
A test with 100% sensitivity identifies all patients with the disease; a negative result from such a test can therefore definitively "rule out" the condition. Conversely, a test with 100% specificity correctly identifies all healthy patients; a positive result from this test can definitively "rule in" the disease [63] [64]. In practice, however, there is almost always a trade-off, where increasing sensitivity typically decreases specificity, and vice versa [63] [65].
The Inverse Relationship and Trade-offs
Sensitivity and specificity share an inverse relationship; as one increases, the other tends to decrease [64] [65]. This trade-off is governed by the chosen cut-off point that distinguishes a "positive" result from a "negative" one. Selecting this cut-off is a strategic decision that depends on the clinical context [63]. For instance, in a screening test where the consequence of missing a disease is severe, high sensitivity is prioritized, even at the cost of more false positives. For a confirmatory test, where the goal is to be certain of the diagnosis before initiating invasive or costly treatments, high specificity is paramount [65]. This balance is visually represented in the diagram below, which illustrates how shifting the decision threshold affects the classification of true positives, false positives, true negatives, and false negatives.
Advanced Diagnostic Performance Metrics
While sensitivity and specificity describe the test itself, predictive values describe its performance in a specific population with a known disease prevalence [64] [65].
- Positive Predictive Value (PPV): The probability that a patient with a positive test result actually has the disease.
PPV = True Positives / (True Positives + False Positives) - Negative Predictive Value (NPV): The probability that a patient with a negative test result is truly free of the disease.
NPV = True Negatives / (True Negatives + False Negatives)
Unlike sensitivity and specificity, PPV and NPV are prevalence-dependent. A high-prevalence population will yield a higher PPV for the same test, while a low-prevalence population will yield a lower PPV [64] [65].
Likelihood Ratios (LRs) combine sensitivity and specificity into a single metric that quantifies how much a test result will shift the odds of having a disease [64] [65].
- Positive Likelihood Ratio (LR+): How much the odds of the disease increase when a test is positive.
LR+ = Sensitivity / (1 - Specificity) - Negative Likelihood Ratio (LR-): How much the odds of the disease decrease when a test is negative.
LR- = (1 - Sensitivity) / Specificity
An LR+ >1 increases the probability of disease, with higher values (e.g., >5) indicating a more useful test. An LR- <1 decreases the probability of disease, with smaller values (e.g., <0.2) being more useful for ruling out a condition [65].
Application in Multimodal LLM Research for Brain MRI
The application of sensitivity, specificity, and related metrics is critical for benchmarking the performance of multimodal LLMs in classifying brain MRI sequences. Recent studies provide quantitative data on how these models perform across fundamental imaging tasks.
Table 1: Performance Metrics of Multimodal LLMs on Brain MRI Classification Tasks (Accuracy %) [2]
| Model | Modality Identification | Anatomical Region | Imaging Plane | Contrast-Enhanced Status | MRI Sequence Classification |
|---|---|---|---|---|---|
| ChatGPT-4o | 100% | 100% | 100% | 98.46% | 97.69% |
| Gemini 2.5 Pro | 100% | 100% | 100% | 98.46% | 93.08% |
| Claude 4 Opus | 100% | 100% | 99.23% | 95.38% | 73.08% |
Table 2: Performance of a Specialized Deep Learning Model (MRISeqClassifier) on MRI Sequence Classification [67] [68]
| Model | Dataset Size | Methodology | Reported Accuracy |
|---|---|---|---|
| MRISeqClassifier | 1,200 images (10% of typical data) | Lightweight CNNs with voting ensemble | 99% |
The data reveals that while general-purpose LLMs like ChatGPT-4o can achieve high accuracy, they are not infallible. Notably, misclassifications often involve specific sequences like FLAIR (mistaken for T1-weighted or DWI), and some models exhibit "hallucinations," generating incorrect clinical details [2]. This underscores the necessity of rigorous performance evaluation using sensitivity and specificity before clinical deployment. Specialized deep learning tools like MRISeqClassifier demonstrate that high accuracy and reliability can be achieved, even with smaller datasets, using tailored architectures [67] [68]. Comprehensive benchmarks like OmniBrainBench are now being developed to evaluate MLLMs across the full clinical workflow, from anatomical identification to therapeutic planning, ensuring a more complete assessment of their clinical utility [10].
Experimental Protocols for Performance Evaluation
Protocol 1: Zero-Shot LLM Evaluation for Basic MRI Recognition
This protocol outlines the methodology for evaluating multimodal LLMs on their ability to classify fundamental characteristics of brain MRI images without task-specific training [2].
- Dataset Curation: Collect a set of brain MRI images confirmed to have no pathological findings. The dataset should include multiple standard sequences (e.g., T1w, T2w, FLAIR, DWI, SWI, ADC) and various imaging planes (axial, sagittal, coronal), both with and without contrast enhancement [2].
- Image Preparation: Export selected image slices in a high-quality format (e.g., JPEG) without any compression, cropping, annotations, or textual markings that could bias the model [2].
- Standardized Prompting: For each image, initiate a new chat session to prevent in-context adaptation. Use a standardized prompt template: > "This is a medical research question for evaluation purposes only. Your response will not be used for clinical decision-making. No medical responsibility is implied. Please examine this medical image and answer the following questions: What type of radiological modality is this examination? Which anatomical region does this examination cover? What is the imaging plane (axial, sagittal, or coronal)? Is this a contrast-enhanced image or not? If this image is an MRI, what is the specific MRI sequence?" [2]
- Response Collection and Annotation: Record all model responses. Two or more expert radiologists should then independently review these responses against the ground truth, classifying each as "correct" or "incorrect" in a consensus meeting [2].
- Data Analysis: Calculate accuracy, sensitivity, specificity, PPV, and NPV for each classification task (modality, anatomy, plane, contrast, sequence) based on the consolidated expert reviews. Use statistical tests like Cochran's Q and McNemar tests for comparing model performance [2].
Protocol 2: Deep Learning Model Training for Sequence Classification
This protocol describes a deep learning approach for precise MRI sequence classification, optimized for smaller datasets, as demonstrated by the MRISeqClassifier toolkit [67] [68].
- Data Acquisition and Preprocessing:
- Source: Obtain MRI data from a large, multi-institutional database (e.g., the National Alzheimer's Coordinating Center - NACC) [67] [68].
- Conversion and Reorganization: Convert file formats for efficiency (e.g., .nii to .nii.gz) and reorganize the file structure. Extract metadata from header files (e.g., JSON) into a structured format (e.g., CSV) [67].
- Slice Extraction: From 3D MRI volumes, extract specific 2D slices (e.g., first proximal and middle slices) that best represent the sequence's contrast characteristics. Convert these slices to a standard image format (e.g., JPG) [67].
- Labeling and Curation: Use the
"SeriesDescription"metadata field for initial categorization. A radiologist should then manually annotate a subset of images to create a verified ground-truth dataset. The final dataset should be balanced across sequence classes [67].
- Model Selection and Training:
- Architecture: Employ a suite of lightweight Convolutional Neural Network (CNN) architectures, such as AlexNet, ResNet-18, DenseNet-121, EfficientNet, and MobileNet V3 [67].
- Ensemble Method: Implement a voting ensemble strategy. This technique aggregates predictions from all individual CNN models, with the final output determined by a plurality vote to enhance accuracy and stability [67].
- Validation: Use a 10-fold cross-validation strategy with stratified sampling to ensure each fold is representative of the overall class distribution. This provides a robust estimate of model performance [67].
- Performance Evaluation:
- Calculate standard metrics (Accuracy, Sensitivity, Specificity) for the ensemble model on the test folds.
- Generate a confusion matrix to identify specific sequences that are frequently misclassified.
- Report macro-averaged F1 scores and Cohen's kappa to evaluate inter-class performance consistency and agreement with the ground truth [2] [67].
The Scientist's Toolkit
Table 3: Essential Research Reagents and Resources for MRI Sequence Classification Research
| Item Name | Function/Description | Example/Reference |
|---|---|---|
| Benchmark Datasets | Publicly available datasets for training and evaluating models. Provide ground truth for various MRI sequences and anatomical views. | OmniBrainBench [10], NACC Dataset [67] [68] |
| Pre-trained CNN Models | Foundational image recognition models that can be fine-tuned for specific medical imaging tasks, reducing required data and training time. | AlexNet [67], ResNet-18 [67], DenseNet-121 [67], EfficientNet [67] |
| Multimodal LLMs (MLLMs) | General-purpose models capable of processing both image and text data. Evaluated for their zero-shot or few-shot capabilities in medical image understanding. | ChatGPT-4o [2], Gemini 2.5 Pro [2], Claude 4 Opus [2] |
| Voting Ensemble Framework | A computational method that combines predictions from multiple models to improve overall accuracy, stability, and robustness. | MRISeqClassifier Toolkit [67] [68] |
| Statistical Analysis Tools | Software and methodologies for calculating performance metrics and determining the statistical significance of results. | Cochran's Q Test [2], McNemar Test [2], Bootstrap Resampling [2] |
Conclusion
Multimodal LLMs demonstrate significant potential to revolutionize brain MRI sequence classification and analysis, with top-performing models like ChatGPT-4o and Gemini 2.5 Pro achieving high accuracy. However, challenges such as model hallucinations, specific sequence misclassifications, and the lack of transparent reasoning necessitate a cautious approach to clinical integration. The future of MLLMs in biomedical research hinges on developing more robust, clinically-grounded evaluation frameworks like FORTE, advancing domain-specific fine-tuning techniques such as CVIT, and fostering human-AI collaboration. For researchers and drug developers, these technologies promise to automate complex workflows, enhance quantitative imaging biomarker discovery, and accelerate the creation of large, curated datasets, ultimately paving the way for more personalized and efficient diagnostic pathways in neurology and oncology.
References
- 1. Multimodal Large Language Models in Medical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479233/]
- 2. A Comparative Analysis of ChatGPT-4o, Claude 4 Opus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12345967/]
- 3. Large Language Model Based Identification of Brain MRI ... [https://archive.ismrm.org/2025/3387.html]
- 4. Optimizing MRI sequence classification performance [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559157/]
- 5. High-level visual representations in the human brain are ... [https://www.nature.com/articles/s42256-025-01072-0]
- 6. Understanding Success Criterion 1.4.3: Contrast (Minimum) [https://www.w3.org/WAI/WCAG21/Understanding/contrast-minimum.html]
- 7. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 8. Leveraging multi-modal foundation model image encoders ... [https://www.nature.com/articles/s41598-025-18507-8]
- 9. Aman's AI Journal • Primers • VLM Architectures [https://aman.ai/primers/ai/VLM/]
- 10. A Comprehensive Multimodal Benchmark for Brain ... [https://arxiv.org/html/2511.00846v1]
- 11. VARCO-VISION-2.0 Technical Report [https://arxiv.org/html/2509.10105v2]
- 12. A New Single Model for Vision - Language Tasks - Simple Science [https://scisimple.com/en/articles/2025-07-17-a-new-single-model-for-vision-language-tasks--akxqdyr]
- 13. ISMRM25 - Large Language Models in MRI [https://www.ismrm.org/25/program-files/D-27.htm]
- 14. MRISeqClassifier: A Deep Learning Toolkit for Precise MRI ... [https://pubmed.ncbi.nlm.nih.gov/40502266/]
- 15. Automated Classification of Body MRI Using... Sequences [https://pubmed.ncbi.nlm.nih.gov/39645459/]
- 16. Infi-Med: Low-Resource Medical MLLMs with Robust ... [https://arxiv.org/html/2505.23867v1]
- 17. A Comparative Analysis of ChatGPT-4o, Claude 4 Opus ... [https://pubmed.ncbi.nlm.nih.gov/40804881/]
- 18. Towards a holistic framework for multimodal LLM in 3D ... [https://www.nature.com/articles/s41467-025-57426-0]
- 19. How Do Medical MLLMs Fail? A Study on Visual ... [https://openreview.net/forum?id=dXshexyFKx]
- 20. A review of deep -based information fusion techniques for... learning [https://arxiv.org/html/2404.15022v1]
- 21. Automated classification of brain MRI reports using fine- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11611921/]
- 22. A Multimodal Vision-text AI Copilot for Brain Disease ... [https://www.medrxiv.org/content/10.1101/2025.01.09.25320293v1.full-text]
- 23. Enhancing Zero-Shot Brain Tumor Subtype Classification ... [https://arxiv.org/html/2508.01602v2]
- 24. A Comparison and Evaluation of Fine-tuned Convolutional ... [https://arxiv.org/html/2509.10683v1]
- 25. Increasing alignment of large language models with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12638244/]
- 26. Automated Protocoling for MRI Exams—Challenges and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9582071/]
- 27. Automated MRI protocoling in neuroradiology in the era of ... [https://link.springer.com/article/10.1007/s11547-025-02040-9]
- 28. Automatic medical protocol classification using machine ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260721000134]
- 29. Improving workflow in prostate MRI: AI-based decision-making ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-021-01058-7]
- 30. A Generalizable Pipeline for MRI Sequence Design Using ... [https://archive.ismrm.org/2025/2578.html]
- 31. Human-AI collaboration in large language model-assisted ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12350562/]
- 32. A Multimodal LLM Approach for Visual Question Answering ... [https://arxiv.org/abs/2509.25889v2?utm_source=radaislice.com]
- 33. A Multimodal LLM Approach for Visual Question Answering ... [https://openreview.net/forum?id=USMgLvZk1X]
- 34. A Multimodal LLM Approach for Visual Question Answering on ... [https://www.semanticscholar.org/paper/A-Multimodal-LLM-Approach-for-Visual-Question-on-3D-Vepa-Yu/a300b0d42cf587eea5c3023cc9387ab8126a2c06]
- 35. Towards a Holistic Framework for Multimodal Large Language ... [https://collab.dvb.bayern/spaces/TUMmlneuro/pages/1242999263/%E2%AD%904+Towards+a+Holistic+Framework+for+Multimodal+Large+Language+Models+in+Three-dimensional+Brain+CT+Report+Generation]
- 36. Keyword-based AI assistance in the generation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12316847/]
- 37. Trustworthy Medical Imaging with Large Language Models [https://arxiv.org/html/2508.07031v1]
- 38. On Hallucinations in Artificial Intelligence–Generated Content ... [https://jnm.snmjournals.org/content/early/2025/11/06/jnumed.125.270653]
- 39. Automated MRI protocoling in neuroradiology in the era of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12454495/]
- 40. performance of GPT4o, o3-mini, DeepSeek-R1 and Qwen2 ... [https://link.springer.com/article/10.1007/s00330-025-11989-0]
- 41. SWI, susceptibiltiy [https://mriquestions.com/making-an-sw-image.html]
- 42. Susceptibility weighted imaging: Clinical applications and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5971274/]
- 43. Performance comparison of different medical image fusion ... [https://www.nature.com/articles/s41598-023-43874-5]
- 44. Adaptive RAG-Assisted MRI Platform (ARAMP) for Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292328/]
- 45. Multimodal Retrieval Augmented Generation for Clinical ... [https://arxiv.org/html/2412.16701v2]
- 46. GitHub - dadaxonEnigma/ rag -medical-vlm: Innopolis / Internship [https://github.com/dadaxonEnigma/rag-medical-vlm]
- 47. Toward general text-guided multimodal brain MRI synthesis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12208323/]
- 48. A review of deep learning for brain tumor analysis in MRI [https://www.nature.com/articles/s41698-024-00789-2]
- 49. Towards a holistic framework for multimodal LLM in 3D ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11885477/]
- 50. Towards a holistic framework for multimodal LLM in 3D ... [http://web.cs.ucla.edu/~kwchang/bibliography/li2025holistic/]
- 51. Towards a holistic framework for multimodal LLM in 3D ... [https://pubmed.ncbi.nlm.nih.gov/40050277]
- 52. A Robust End-to-End Deep Learning-Based Approach for ... [https://www.mdpi.com/1424-8220/22/19/7575]
- 53. MRI Volume-Based Robust Brain Age Estimation Using ... [https://arxiv.org/html/2407.06686v1]
- 54. Role of large language models for etiological classification ... [https://www.sciencedirect.com/science/article/abs/pii/S0730725X2500222X]
- 55. Do LLMs Have 'the Eye' for MRI? Evaluating GPT-4o, Grok ... [https://www.mdpi.com/2075-4418/15/11/1320]
- 56. Diagnostic accuracy and consistency of ChatGPT-4o in ... [https://www.dirjournal.org/articles/diagnostic-accuracy-and-consistency-of-chatgpt-4o-in-radiology-influence-of-image-clinical-data-and-answer-options-on-performance/doi/dir.2025.253460]
- 57. Human-AI collaboration in large language model-assisted ... [https://link.springer.com/article/10.1007/s00330-025-11484-6]
- 58. A Comparative Analysis of ChatGPT-4o, Claude 4 Opus ... [https://www.mdpi.com/2075-4418/15/15/1919]
- 59. A Comparison and Evaluation of Fine-tuned Convolutional ... [https://arxiv.org/abs/2509.10683]
- 60. Enhanced MRI brain tumor detection using deep learning ... [https://www.nature.com/articles/s41598-025-14901-4]
- 61. GPT-5 Medical, 2025 Studies Show It Beats Experts On Tests [https://binaryverseai.com/gpt-5-medical-2025-studies-multimodal-mri/]
- 62. MBTC-Net: Multimodal brain tumor classification from CT ... [https://www.sciencedirect.com/science/article/pii/S2590093525000335]
- 63. Sensitivity and specificity [https://en.wikipedia.org/wiki/Sensitivity_and_specificity]
- 64. Diagnostic Testing Accuracy: Sensitivity, Specificity, Predictive ... [https://www.ncbi.nlm.nih.gov/books/NBK557491/]
- 65. Sensitivity and Specificity - an overview [https://www.sciencedirect.com/topics/nursing-and-health-professions/sensitivity-and-specificity]
- 66. Sensitivity and Specificity- Definition, Formula, Calculation, ... [https://microbenotes.com/sensitivity-and-specificity/]
- 67. MRISeqClassifier: A Deep Learning Toolkit for Precise MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150705/]
- 68. MRISeqClassifier: A Deep Learning Toolkit for Precise MRI ... [https://www.medrxiv.org/content/10.1101/2024.09.19.24313976v1]