Mitigating Hallucinations in Medical Multimodal LLMs: Strategies for Reliable Clinical Imaging AI
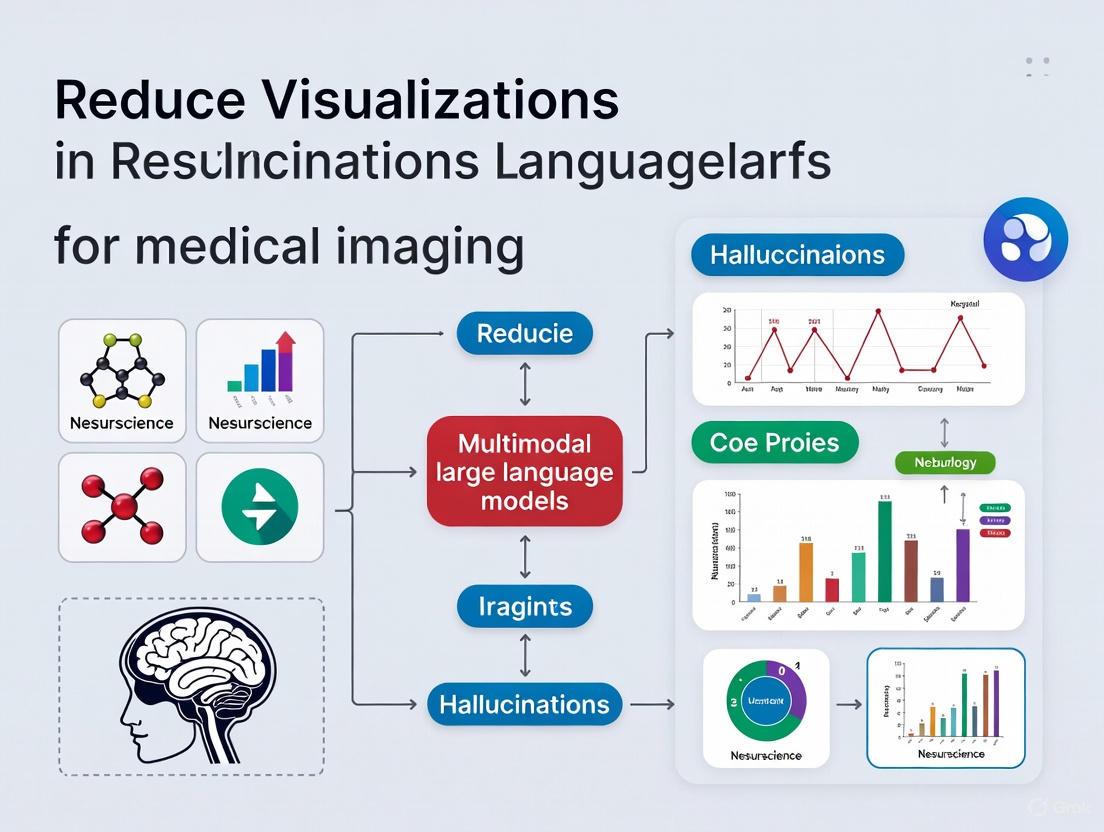
This article provides a comprehensive analysis of the challenge of hallucination in Multimodal Large Language Models (MLLMs) applied to medical imaging, a critical barrier to clinical adoption.
Mitigating Hallucinations in Medical Multimodal LLMs: Strategies for Reliable Clinical Imaging AI
Abstract
This article provides a comprehensive analysis of the challenge of hallucination in Multimodal Large Language Models (MLLMs) applied to medical imaging, a critical barrier to clinical adoption. Tailored for researchers and drug development professionals, it explores the foundational causes of these fabrications, from data heterogeneity to architectural misalignments. We review cutting-edge mitigation methodologies, including Visual Retrieval-Augmented Generation (V-RAG) and specialized training paradigms, and provide a rigorous framework for their evaluation and validation. The content further delves into troubleshooting persistent issues like adversarial vulnerabilities and outlines optimization strategies to balance accuracy with computational efficiency, concluding with synthesized key takeaways and future directions for building trustworthy AI in biomedicine.
Defining the Problem: Understanding Hallucinations in Medical MLLMs
What Are Hallucinations? Clarifying Definitions for Medical Imaging
FAQ 1: What is an AI hallucination in the context of medical imaging?
In medical imaging, an AI hallucination refers to artificial intelligence-generated content that is factually false or misleading but is presented as factual [1]. Specifically, for tasks like image enhancement or report generation, it is the generation of visually realistic and highly plausible abnormalities or artifacts that do not exist in reality and deviate from the anatomic or functional truth [2]. This is distinct from general inaccuracies and poses a significant risk to diagnostic reliability.
FAQ 2: How are hallucinations different from other AI errors?
Hallucinations are a specific category of error. The following table clarifies key distinctions:
| Error Type | Definition | Key Characteristic | Example in Medical Imaging |
|---|---|---|---|
| Hallucination [2] | AI fabricates a realistic-looking abnormality or structure that is not present. | Addition of plausible but false image features or text. | A denoising model adds a small, realistic-looking lesion to a PET scan that does not exist [2]. |
| Illusion [2] | AI misinterprets or misclassifies an existing structure. | Misinterpretation of something that is actually there. | A model incorrectly labels a benign cyst as a malignant tumor. |
| Delusion [2] | AI generates an implausible or dreamlike structure that is clearly not real. | Generation of anatomically impossible or fantastical content. | A model generates an image of an organ in the wrong location or with an impossible shape. |
| Omission [2] | AI fails to identify and removes a real structure or lesion. | Removal of true information. | A model removes a real lesion from a scan, replacing it with normal-looking tissue. |
FAQ 3: What are the root causes of hallucinations in Multimodal LLMs for medicine?
Hallucinations can stem from several sources, often interacting with each other:
- Data-Driven Causes: Models trained on low-quality, imbalanced, or noisy datasets can learn incorrect patterns [3]. If the training data contains inaccuracies or source-reference divergences (where the text description doesn't perfectly match the image), the model is encouraged to generate ungrounded content [1].
- Model Architecture & Training Causes: The next-token prediction objective during pre-training incentivizes models to "guess" the next word, even with insufficient information [1]. In vision-language models, poor visual encoding or misalignment between image and text features can lead the language model to ignore the visual evidence and "confabulate" [3].
- Alignment Issues: A failure to properly synchronize and align information from different modalities (e.g., image, text, clinical data) can create contradictory internal representations, leading to incoherent or fabricated outputs [3].
FAQ 4: What experimental methods can quantify hallucinations?
A robust experimental protocol to evaluate hallucinations involves "entity probing" and automated metrics [4].
Experimental Protocol: Entity Probing for Hallucination Evaluation
- Objective: To measure an MLLM's tendency to hallucinate by testing its ability to correctly ground medical entities in a given image.
- Dataset: Use a standardized medical imaging dataset with ground-truth reports (e.g., MIMIC-CXR for chest X-rays) [4].
- Method:
- For a given medical image, present it to the MLLM alongside a series of yes/no questions about the presence or absence of specific medical entities (e.g., "Is there pleural effusion in this image?") [4].
- Compare the model's predictions against the answers derived from the ground-truth report.
- This method avoids sensitivity to phrasing and directly tests factual grounding [4].
- Quantification: Calculate the accuracy of the model's yes/no answers against the ground truth. This provides a clinical perspective on hallucination rates not captured by standard language generation metrics.
The following workflow diagram illustrates this entity probing process:
FAQ 5: What quantitative data exists on hallucination rates?
Recent studies have quantified the susceptibility of LLMs to hallucinations in clinical contexts. The table below summarizes key findings from an adversarial attack study, where models were prompted with clinical vignettes containing one fabricated detail [5].
Table 1: Hallucination Rates Across LLMs in a Clinical Adversarial Setting
| Large Language Model (LLM) | Default Hallucination Rate (%) | Hallucination Rate with Mitigation Prompt (%) |
|---|---|---|
| GPT-4o | 53 | 23 |
| Claude 3 Opus | 57 | 39 |
| Llama 3 70B | 67 | 52 |
| Gemini 1.5 Pro | 68 | 48 |
| GPT-3.5 Turbo | 72 | 54 |
| Distilled-DeepSeek-R1 | 82 | 68 |
| Mean (Across all models) | 66 | 44 |
Source: Adapted from [5]. The mitigation prompt instructed the model to use only clinically validated information.
FAQ 6: What are effective strategies to mitigate hallucinations?
Multiple strategies can be employed to reduce hallucinations, with Visual Retrieval-Augmented Generation (V-RAG) showing significant promise [4].
Mitigation Strategy: Visual Retrieval-Augmented Generation (V-RAG)
- Principle: Instead of relying solely on the model's internal parameters, V-RAG grounds the generation process by retrieving visually similar images and their associated reports from a database. The model can then compare the query image to these references to determine what is truly important [4].
- Workflow:
- Multimodal Retrieval: For a query image, use a model like BiomedCLIP to extract its image embedding. Then, use a vector database (e.g., FAISS) to retrieve the top-k most similar images and their corresponding reports [4].
- Inference with Retrievals: The retrieved images and reports are prepended to the original prompt as references. The model is then instructed to answer the question based on both the query image and the reference materials, enhancing contextual understanding [4].
The following diagram illustrates the V-RAG workflow for mitigating hallucinations:
Table 2: Essential Materials for Hallucination Research in Medical MLLMs
| Item | Function in Research | Example / Reference |
|---|---|---|
| BiomedCLIP | A vision-language model that provides robust image and text embeddings for the medical domain, crucial for retrieval tasks in V-RAG [4]. | [4] |
| FAISS Vector Database | A library for efficient similarity search and clustering of dense vectors, enabling fast retrieval of similar images from a large database [4]. | [4] |
| MIMIC-CXR Dataset | A large, publicly available dataset of chest X-rays with corresponding free-text reports, used for training and benchmarking report generation models [4]. | [4] |
| RadGraph Metric | An evaluation metric that extracts clinical entities and relations from generated reports, providing a measure of clinical accuracy (RadGraph-F1) beyond traditional text similarity [4]. | [4] |
| Entity Probing Framework | A methodology to test an MLLM's factual grounding by asking yes/no questions about medical entities in an image, providing a direct measure of hallucination [4]. | [4] |
In the high-stakes field of medical research, fabricated findings and model hallucinations present significant risks that can compromise diagnostic accuracy, patient safety, and the validity of scientific discoveries. The integrity of medical research data faces substantial threats from various forms of deception, while emerging multimodal Large Language Models (MLLMs) introduce new challenges through their tendency to generate hallucinated content. This technical support center provides researchers, scientists, and drug development professionals with essential resources to identify, prevent, and address these critical issues in their experimental workflows, particularly within medical imaging research.
Quantifying the Problem: Data on Deception and Falsification
Frequency of Deceptive Practices in Health Research
Recent studies have quantified how frequently research subjects employ deception across various clinical trial contexts. The table below summarizes findings from subjects who admitted to using deceptive practices in health-related studies over a 12-month period [6].
Table 1: Frequency of Deceptive Practices in Health Research Studies
| Type of Deception | Specific Method | Average Frequency of Use |
|---|---|---|
| Concealment of Information | Mental health information | 58% of studies |
| Physical health information | 57% of studies | |
| Overall concealment | 67% of studies | |
| Fabrication to Qualify | Exaggerating health symptoms | 45% of studies |
| Pretending to have a health condition | 39% of studies | |
| Overall fabrication | 53% of studies | |
| Data Falsification After Enrollment | Falsely reporting improvement | 38% of studies |
| Discarding medication to appear compliant | 32% of studies | |
| Overall data falsification | 40% of studies |
Global Impact of Substandard and Falsified Medical Products
The World Health Organization has documented the alarming scope of substandard and falsified medical products globally. These products represent a significant public health threat with both clinical and economic consequences [7].
Table 2: Impact of Substandard and Falsified Medical Products
| Impact Category | Statistical Measure | Global Impact |
|---|---|---|
| Prevalence | Medicines in low- and middle-income countries | At least 1 in 10 medicines |
| Economic Burden | Annual global cost | US$30.5 billion |
| Health Risks | Treatment failure, poisoning, drug-resistant infections | Significant contributor |
| Distribution Channels | Online and informal markets | Commonly sold |
Technical Solutions: Addressing Hallucinations in Medical MLLMs
Visual Retrieval-Augmented Generation (V-RAG)
Multimodal Large Language Models (MLLMs) have demonstrated impressive capabilities in medical imaging tasks but remain prone to hallucinations—generating content not grounded in input data. Visual Retrieval-Augmented Generation (V-RAG) addresses this by incorporating both visual and textual data from retrieved similar images during the generation process [8] [4].
Experimental Protocol: Implementing V-RAG for Medical Imaging
- Multimodal Retrieval: Utilize BiomedCLIP to extract robust image embeddings (dimension: 512) for medical images. Construct a FAISS vector storage system with Hierarchical Navigable Small World (HNSW) algorithm for efficient approximate k-nearest neighbor search [4].
- Reference Integration: For a query image, retrieve top-k similar images and corresponding reports. Structure the prompt to include each reference before the question: "This is the i-th similar image and its report for your reference. [Reference]i... Answer the question with only the word yes or no. Do not provide explanations. According to the last query image and the reference images and reports, [Question] [Query Image]" [4].
- Entity Probing Validation: Present images to the MLLM and ask yes/no questions about disease entities. Compare predictions against answers grounded in an LLM's interpretation of reference reports to quantify hallucination reduction [4].
- Fine-Tuning for Enhanced Comprehension: Implement general image-text fine-tuning tasks to strengthen Med-MLLMs' multimodal understanding when processing multiple retrieved images, enabling single-image-trained models to effectively utilize V-RAG [4].
Diagram 1: V-RAG Implementation Workflow
Research Reagent Solutions for Integrity Assurance
Table 3: Essential Research Reagents and Tools for Data Integrity
| Research Tool | Primary Function | Application in Integrity Assurance |
|---|---|---|
| BiomedCLIP | Extracts robust image embeddings from diverse biomedical images | Creates representations for accurate similarity matching in retrieval systems [4] |
| FAISS with HNSW | Enables efficient vector similarity search at scale | Facilitates rapid identification of similar medical images for reference [4] |
| Identity Registries | Tracks research participants across studies | Prevents professional subjects from enrolling in multiple trials concurrently [6] |
| Medication Compliance Tech | Provides objective measures of medication adherence | Detects fraudulent reports of compliance through digital monitoring [6] |
| Entity Probing Framework | Tests model accuracy on specific medical entities | Quantifies hallucination frequency in Med-MLLMs for benchmarking [4] |
Troubleshooting Guides & FAQs
Detection and Prevention of Subject Deception
Q: What are the most effective strategies for identifying deceptive subjects in clinical trials? A: Implement research subject identity registries to track participation across studies. Utilize technological solutions for objective medication compliance monitoring. Focus screening efforts on mental and physical health concealment, which occur in 58% and 57% of studies respectively among deceptive subjects [6].
Q: How does subject deception impact study validity and sample size requirements? A: Deceptive subjects can dramatically increase sample size requirements. Modeling shows that if just 10% of a sample consists of subjects pretending to have a condition who then report improvement (making treatment "destined to succeed"), sample size requirements more than double. Even 10% of subjects reporting fraudulent medication compliance can increase sample size needs by 20% [6].
Experimental Protocol: Subject Deception Detection
- Comprehensive Screening: Implement cross-trial participation databases to identify professional subjects [6].
- Verification Methods: Use objective biometric measures, medication adherence technologies, and structured interviews to verify subject-reported data [6].
- Data Analytics: Apply statistical pattern recognition to identify suspicious response patterns and inconsistencies in subject-reported outcomes [6].
Diagram 2: Subject Deception Detection Protocol
Mitigating Hallucinations in Medical MLLMs
Q: What specific techniques reduce hallucinations in medical multimodal LLMs for image interpretation? A: Visual Retrieval-Augmented Generation (V-RAG) significantly reduces hallucinations by incorporating both visual and textual data from retrieved similar images. This approach improves accuracy for both frequent and rare medical entities, the latter of which typically have less positive training data [8] [4].
Q: How can researchers validate the reduction of hallucinations in medical MLLMs? A: Entity probing provides a clinical perspective on text generations by presenting images to MLLMs and asking yes/no questions about disease entities, then comparing predictions against answers grounded in LLM interpretations of reference reports. This approach avoids sensitivity to entity phrasing while providing clinically relevant metrics [4].
Experimental Protocol: Hallucination Reduction Validation
- Dataset Preparation: Utilize standardized medical imaging datasets (MIMIC-CXR for chest X-ray report generation, Multicare for medical image caption generation) [4].
- Entity Selection: Identify frequent and rare medical entities for probing, ensuring balanced evaluation across different prevalence categories [4].
- Benchmarking: Compare baseline MLLMs against V-RAG enhanced models using entity probing accuracy and RadGraph-F1 scores for clinical accuracy [4].
- Statistical Analysis: Measure significant differences in performance between traditional and V-RAG approaches using appropriate statistical tests [4].
Integrated Workflow for Research Integrity
Diagram 3: Integrated Framework for Research Integrity
Troubleshooting Guide: Common MLLM Architectural Flaws and Solutions
This guide addresses frequent architectural failure points in Multimodal Large Language Models (MLLMs) that lead to hallucinations in medical imaging, providing diagnostic steps and mitigation strategies.
Table: Troubleshooting MLLM Architectural Issues
| Architectural Component | Failure Symptoms | Root Cause Analysis | Recommended Solutions |
|---|---|---|---|
| Visual Attention Mechanism | Model describes objects/anatomy not present in image; inaccurate spatial relationships [9] | Limited localization capability; attention spread over uninformative visual tokens rather than critical regions [9] [10] | Implement Vision-Guided Attention (VGA) using Visual Semantic Confidence [9] |
| Token Interaction & Information Propagation | "Snowballing" hallucinations where initial error cascades; contradictions in generated report [10] | Attention collapse on outlier tokens; insufficient vision-text token interaction due to positional encoding decay [10] | Apply FarSight decoding with attention registers; use diminishing masking rate in causal masks [10] |
| Cross-Modal Alignment | Plausible but clinically unsupported descriptions; confusion between visually similar anatomical structures [11] [12] | Weak alignment between visual features and medical concepts; vision encoder outputs not properly grounded in clinical knowledge [11] [13] | Integrate Clinical Contrastive Decoding (CCD); use expert model signals to refine token logits [11] |
| Instruction Following & Prompt Sensitivity | Hallucinations triggered by specific prompt phrasing; over-sensitivity to clinical sections in instructions [11] [14] | Inadequate instruction tuning for medical ambiguity; failure to handle clinically implausible prompts robustly [11] | Employ dual prompting strategies (instruction-based + reverse prompting) for critical self-reflection [14] |
| Positional Encoding | Deteriorating accuracy in longer reports; poor tracking of anatomical relationships in 3D imaging [10] [15] | Rotary Positional Encoding (RoPE) long-term decay fails to maintain spatial relationships across lengthy contexts [10] | Enhance positional awareness with diminishing masking rates; explore absolute positional encoding supplements [10] |
Frequently Asked Questions
Q1: Why does my MLLM consistently hallucinate small anatomical structures even with high-quality training data?
This is frequently an attention mechanism failure, not a data quality issue. Standard visual attention often distributes weights across uninformative background tokens, neglecting subtle but critical anatomical features [9]. The solution is to implement Vision-Guided Attention (VGA), which uses Visual Semantic Confidence scores to identify and prioritize informative visual tokens, forcing the model to focus on clinically relevant regions [9].
Q2: How can I mitigate "snowballing hallucinations" where one error leads to cascading inaccuracies in the report?
Snowballing hallucinations stem from insufficient token interaction and attention collapse. As generation progresses, the model increasingly relies on its own previous (potentially erroneous) tokens rather than visual evidence [10]. The FarSight method addresses this by optimizing causal masks to maintain balanced information flow between visual and textual tokens throughout the generation process, preventing early errors from propagating [10].
Q3: What is the most lightweight approach to reduce hallucinations without retraining my model?
Clinical Contrastive Decoding (CCD) provides a training-free solution. CCD introduces a dual-stage contrastive mechanism during inference that leverages structured clinical signals from task-specific expert models (e.g., symptom classifiers) to refine token-level logits, enhancing clinical fidelity without modifying the base MLLM [11]. Similarly, VGA adds only 4.36% inference latency while significantly reducing hallucinations [9].
Q4: Why does my model perform well on visual question answering but hallucinate frequently in full report generation?
RRG is substantially more complex and error-prone than VQA. While VQA addresses narrowly scoped queries, radiology report generation requires holistic image understanding and precise, clinically grounded expression of findings [11]. This complexity exposes weaknesses in cross-modal alignment and long-range dependency handling. Solutions include template instruction tuning and keyword-focused training to maintain clinical precision across longer outputs [15].
Q5: How can I improve my model's handling of ambiguous cases where it should express uncertainty rather than hallucinate?
This requires enhancing the model's self-reflection capabilities. Implement reverse prompting strategies that explicitly question the model's reasoning process (e.g., "Are important details being captured?") to encourage continuous self-evaluation [14]. In multi-agent systems, incorporate uncertainty quantification that allows agents to communicate confidence levels, preventing overconfident but incorrect generations [12].
Experimental Protocols for Hallucination Mitigation
Protocol 1: Implementing Clinical Contrastive Decoding (CCD)
CCD integrates structured clinical signals from radiology expert models to refine MLLM generation without retraining [11].
Methodology:
- Expert Model Integration: Employ a task-specific expert model (e.g., symptom classifier) to extract structured clinical labels and confidence probabilities from medical images
- Dual-Stage Contrastive Mechanism:
- Stage 1: Inject predicted labels as descriptive prompts to enhance MLLM grounding
- Stage 2: Use probability scores to perturb decoding logits toward clinical consistency
- Token-Level Logit Refinement: Apply contrastive decoding between original and expert-guided distributions at each generation step
Validation: On MIMIC-CXR dataset, CCD yielded up to 17% improvement in RadGraph-F1 score for state-of-the-art RRG models [11].
Protocol 2: Vision-Guided Attention (VGA) Implementation
VGA directs visual attention by leveraging semantic features of visual tokens to identify the most informative regions [9].
Methodology:
- Visual Semantic Confidence Calculation: For each visual token ( vi ), compute semantic confidence score ( c{vi}(O) ) for object ( O ) using: ( c{vi}(O) = \text{softmax}[\text{logit}{vi}(O)] \approx c{vi}(o0) ) where ( o_0 ) is the first token of the tokenized object [9]
- Visual Grounding: Obtain visual grounding of object ( O ) using: ( \mathbf{G}O = \text{Norm}[{c{vi}(o0)}_{i=1}^m] \in \mathbb{R}^m ) where ( m ) is the number of visual tokens [9]
- Attention Guidance: Use ( \mathbf{G}_O ) to guide attention weights toward tokens with high clinical relevance
Performance: VGA introduces only 4.36% inference latency overhead and is compatible with FlashAttention optimization [9].
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Components for Hallucination-Resistant MLLM Architectures
| Component | Function | Implementation Example |
|---|---|---|
| Clinical Contrastive Decoding (CCD) | Training-free inference framework that reduces hallucinations by integrating expert model signals [11] | Dual-stage contrastive mechanism applied to token-level logits during generation [11] |
| Vision-Guided Attention (VGA) | Directs model focus to relevant visual regions using semantic features of visual tokens [9] | Visual Semantic Confidence scores used to compute visual grounding for attention guidance [9] |
| FarSight Decoding | Plug-and-play decoding strategy that reduces attention interference from outlier tokens [10] | Attention registers within causal mask upper triangular matrix; diminishing masking rate [10] |
| Adaptive Dynamic Masking | Filters irrelevant visual content by computing frame-level weights using self-attention [14] | Dynamic masking rate determined via normal distribution sampling [14] |
| Dual Prompting Strategy | Combines instruction-based and reverse prompting to reduce language biases [14] | Instruction prompts define tasks; reverse prompts question reasoning process [14] |
| Feature-Oriented Radiology Task Evaluation (FORTE) | Evaluation metric capturing clinical essence of generated reports [15] | Structured keyword extraction across four components: degree, landmark, feature, impression [15] |
Architectural Diagrams
MLLM Architecture Hallucination Sources & Mitigations
This diagram illustrates the core MLLM architecture for medical imaging, highlighting where hallucinations originate and corresponding mitigation strategies that can be implemented at each failure point.
Clinical Contrastive Decoding Workflow
This diagram shows the Clinical Contrastive Decoding process where expert model outputs are integrated with base MLLM generation to produce clinically grounded reports while mitigating hallucinations.
Frequently Asked Questions (FAQs)
FAQ 1: What is the connection between data scarcity and hallucinations in multimodal medical AI? Data scarcity directly limits a model's ability to learn robust and generalizable patterns. When trained on small or non-comprehensive datasets, models tend to overfit to the limited examples and, when confronted with unfamiliar data, may "guess" or generate fabrications, a phenomenon known as hallucination [16] [17]. In medical imaging, this can manifest as a model incorrectly identifying a tumor in a healthy tissue region or missing a rare pathology. Foundational models pretrained on large, diverse datasets have been shown to maintain high performance even when fine-tuned on only 1% of a target dataset, significantly mitigating this risk [17].
FAQ 2: How does data heterogeneity negatively impact collaborative model training, like in Federated Learning? Data heterogeneity refers to variations in data distributions across different sources. In Federated Learning (FL), where models are trained across multiple hospitals, heterogeneity in features (e.g., different imaging equipment), labels (e.g., varying disease prevalence), or data quantity can cause local models to diverge significantly [18] [19]. This leads to an unstable global model that is difficult to optimize, resulting in slow convergence and subpar performance. Research has shown a notable performance decline in FL algorithms like FedAvg as data heterogeneity increases [18].
FAQ 3: What are some proven strategies to mitigate data heterogeneity in distributed learning for medical imaging? Advanced FL frameworks are being developed to address this. For instance, HeteroSync Learning (HSL) introduces a Shared Anchor Task (SAT)—a homogeneous reference task from a public dataset—that is co-trained with local tasks across all nodes. This aligns the feature representations learned by different institutions without sharing private patient data. In large-scale simulations, HSL outperformed 12 benchmark methods, matching the performance of a model trained on centrally pooled data [19].
FAQ 4: Beyond acquiring more data, how can we counteract data scarcity in biomedical imaging? Multi-task learning (MTL) is a powerful strategy that pools multiple small- and medium-sized datasets with different types of annotations (e.g., classification, segmentation) to train a single, universal model [17]. This approach allows the model to learn versatile and generalized image representations. The UMedPT foundational model, trained using MTL on 17 different tasks, demonstrated that it could match or exceed the performance of models pretrained on ImageNet, even with only a fraction of the target task's training data [17].
Troubleshooting Guides
Issue: Model Generates Inaccurate or Fabricated Image Annotations (Hallucinations)
| Potential Cause | Diagnostic Steps | Mitigation Strategies |
|---|---|---|
| Limited or Non-Diverse Training Data [16] [20] | Analyze dataset for class imbalance and lack of representation for rare conditions or demographic groups. | Employ multi-task learning to combine multiple smaller datasets [17]. Use data augmentation and foundational models pretrained on large-scale biomedical datasets [17]. |
| Poor Data Quality and Noisy Labels [3] | Review data preprocessing pipelines; check for inconsistencies in expert annotations. | Implement rigorous noise filtering and preprocessing. Use consistent labeling protocols and cross-verification by multiple experts to ensure annotation quality [3]. |
| Misalignment Across Modalities [3] | Check for temporal or spatial misalignment between paired data (e.g., an MRI scan and its corresponding radiology report). | Implement cross-modality verification techniques to ensure generated text accurately reflects the visual input [3]. Use synchronization protocols for temporal data. |
Issue: Performance Collapse in Federated Learning Due to Data Heterogeneity
| Potential Cause | Diagnostic Steps | Mitigation Strategies |
|---|---|---|
| Feature Distribution Skew [19] | Conduct statistical analysis (e.g., t-SNE, UMAP) to visualize feature drift between client data. | Adopt frameworks like HeteroSync Learning (HSL) that use a Shared Anchor Task to align representations across clients [19]. |
| Label Distribution Skew [19] | Audit label distributions (e.g., disease prevalence) across participating institutions. | Utilize algorithms designed for non-IID data, such as FedProx or FedBN, which handle client drift and batch normalization locally [18] [19]. |
| Data Quantity Skew [19] | Compare the number of data samples per client. Large disparities can bias the global model. | Implement weighted aggregation strategies in the FL server to balance the influence of clients with varying data volumes [19]. |
Experimental Data & Protocols
Table 1: Performance of UMedPT Foundational Model Under Data Scarcity Conditions
This table summarizes the model's resilience when limited data is available for target tasks, demonstrating its value in data-scarce environments [17].
| Task Name | Task Type | Model | Training Data Used | Key Metric | Score |
|---|---|---|---|---|---|
| CRC-WSI (In-Domain) | Tissue Classification | UMedPT (Frozen) | 1% | F1 Score | 95.4% |
| ImageNet (Fine-tuned) | 100% | F1 Score | 95.2% | ||
| Pneumo-CXR (In-Domain) | Pediatric Pneumonia Diagnosis | UMedPT (Frozen) | 5% | F1 Score | 93.5% |
| ImageNet (Fine-tuned) | 100% | F1 Score | 90.3% | ||
| NucleiDet-WSI (In-Domain) | Nuclei Detection | UMedPT (Fine-tuned) | 100% | mAP | 0.792 |
| ImageNet (Fine-tuned) | 100% | mAP | 0.710 |
Table 2: Impact of Data Heterogeneity on Federated Learning Performance (FedAvg)
This table shows how non-IID data negatively affects a standard FL algorithm, highlighting the need for advanced mitigation techniques [18].
| Data Distribution Setting | Dataset | Key Finding | Impact on Model Performance |
|---|---|---|---|
| IID (Identically Distributed) | COVIDx CXR-3 | Baseline performance under ideal, homogeneous conditions. | Stable convergence and higher final accuracy. |
| Non-IID (Heterogeneous) | COVIDx CXR-3 | Performance with realistic data skew across clients. | Notable performance decline; unstable and sluggish convergence. |
Experimental Protocol: Multi-Task Learning for a Foundational Model [17]
- Objective: Train a universal biomedical pretrained model (UMedPT) to overcome data scarcity across various imaging tasks.
- Materials:
- Datasets: A multi-task database comprising 17 different tasks, including tomographic, microscopic, and X-ray images.
- Annotation Types: A mix of classification, segmentation, and object detection labels.
- Methodology:
- Model Architecture: A neural network with shared blocks (an encoder, a segmentation decoder, a localization decoder) and task-specific heads for different label types.
- Training Strategy: A gradient accumulation-based multi-task training loop that is not constrained by the number of tasks. The shared encoder is trained on all tasks simultaneously to learn versatile representations.
- Evaluation: The model is evaluated on in-domain and out-of-domain tasks. Performance is assessed with the encoder kept frozen (using only the learned features) and with fine-tuning, while varying the amount of training data (1% to 100%) for the target task.
Experimental Protocol: Evaluating Federated Learning with Data Heterogeneity [18]
- Objective: Investigate the impact of data heterogeneity on the performance of the Federated Averaging (FedAvg) algorithm.
- Materials:
- Dataset: COVIDx CXR-3 and other chest X-ray datasets.
- Framework: TensorFlow Federated (TFF) or similar FL simulation framework.
- Methodology:
- Data Partitioning: The dataset is partitioned across multiple virtual clients to simulate both IID and non-IID environments. For non-IID, data is split to create feature, label, or quantity skew.
- FL Simulation: The FedAvg algorithm is run for a set number of communication rounds. In each round, clients train locally on their data, and the server aggregates the model updates.
- Performance Analysis: The global model's accuracy and convergence speed are tracked and compared between the IID and non-IID settings.
Workflow and System Diagrams
Multi-Task Training for Foundational Models
HeteroSync Learning for Data Heterogeneity
The Scientist's Toolkit: Research Reagent Solutions
| Tool or Material | Function in Experiment |
|---|---|
| Foundational Model (UMedPT) [17] | A pretrained model that provides robust, general-purpose feature extraction for biomedical images, drastically reducing the amount of task-specific data required. |
| Shared Anchor Task (SAT) Dataset [19] | A homogeneous, public dataset (e.g., CIFAR-10, RSNA) used in distributed learning to align feature representations across heterogeneous nodes without sharing private data. |
| Multi-gate Mixture-of-Experts (MMoE) [19] | An auxiliary learning architecture that efficiently coordinates the training of a local primary task and the global Shared Anchor Task, enabling better model generalization. |
| Convex Analysis of Mixtures (CAM) [21] | A computational method used to decompose high-dimensional omics data (e.g., metabolomics) into discrete latent features, helping to uncover underlying biological manifolds. |
| Federated Averaging (FedAvg) [18] | The foundational algorithm for Federated Learning, which coordinates the aggregation of model updates from distributed clients while keeping raw data local. |
Cutting-Edge Solutions: Technical Strategies for Hallucination Mitigation
Frequently Asked Questions (FAQs)
Q1: What is Visual RAG (V-RAG) and how does it differ from traditional text-based RAG?
A1: Visual RAG (V-RAG) is a retrieval-augmented generation framework that incorporates both visual data (retrieved images) and their associated textual reports to enhance the response generation of Multimodal Large Language Models (MLLMs). Unlike traditional text-based RAG, which assumes retrieved images are perfectly interchangeable with the query image and uses only their associated text, V-RAG allows the model to directly compare the query image with retrieved images and reports. This enables the model to identify what is truly relevant for generation, leading to more accurate and contextually relevant answers, which is crucial in medical imaging to mitigate hallucinations [4].
Q2: What are the primary technical components of a V-RAG system?
A2: A V-RAG system typically consists of the following core components [22] [4]:
- Multimodal Retriever: Employs a model like BiomedCLIP to extract robust image embeddings and uses a vector database (e.g., FAISS) for efficient approximate nearest neighbor search to find the top-k most similar images and their reports [4].
- Vector Storage: A database (e.g., Chroma, Milvus) that stores the embedded representations of the visual and textual data for fast retrieval [22] [23].
- Retrieval Engine: Performs the similarity search between the query embedding and the stored embeddings [22].
- Multimodal Generator (MLLM): A model capable of processing both image and text inputs. The retrieved images and reports are formatted into a structured prompt, often with specific guidance, and presented to the MLLM alongside the original query image to generate a grounded response [4].
Q3: What are the key performance metrics for evaluating V-RAG in a medical context?
A3: Standard natural language generation metrics like ROUGE are often insufficient. Key domain-specific metrics include [4] [24]:
- Entity Probing Accuracy: Measures the model's accuracy on yes/no questions about whether specific medical entities are grounded in the image. This is effective for both frequent and rare entities [4].
- RadGraph-F1 Score: Evaluves the factual accuracy of generated radiology reports by extracting clinical entities and their relations from the generated text and comparing them to a reference report [4] [24].
- FactScore: Decomposes generated answers into individual facts and verifies them against a knowledge source for factual consistency [24].
- MED-F1: A clinical relevance metric that assesses the medical validity of the generated content [24].
Q4: My V-RAG system retrieves relevant documents but still generates incorrect answers. What could be wrong?
A4: This is a common failure point known as "Not Extracted" [25]. The answer is in the retrieved context, but the MLLM fails to extract it correctly. To fix this [25]:
- Deduplicate and Clean Knowledge Base: Remove conflicting or redundant information from your retrieval corpus.
- Optimize Prompts: Engineer your prompts to encourage precise extraction from the provided context.
- Limit Retrieval Noise: Ensure only the most relevant context is passed to the generator by adjusting the top-K results or implementing re-ranking strategies.
Q5: How can I adapt a single-image-trained MLLM to work with the multi-image input required for V-RAG?
A5: A general fine-tuning technique can be used to boost a Med-MLLM's capability for V-RAG. This involves designing fine-tuning tasks that strengthen image-text comprehension and enable effective learning from multiple retrieved images presented during multimodal queries. This approach frees researchers from relying on specific pre-trained multi-image models and allows V-RAG to be applied to any model and dataset of interest [4].
Troubleshooting Guides
Problem: Hallucinations in Generated Medical Reports
Issue: The MLLM generates findings or descriptions not present in the retrieved images or reports.
Diagnosis and Solution Flowchart:
Problem: Irrelevant or Low-Quality Retrievals
Issue: The system retrieves images and reports that are not relevant to the query image, leading to poor context for generation.
Potential Causes and Fixes:
| Cause | Symptom | Solution |
|---|---|---|
| Weak Embedding Model | Poor performance across diverse query types. | Use a domain-specific embedding model (e.g., BiomedCLIP for medical images) to better capture semantic similarity [4]. |
| Ineffective Chunking | Retrieved text chunks are incoherent or lack context. | Refine text chunking strategies. Use smaller, overlapping chunks and preserve logical structure (e.g., section titles as metadata) [22] [23]. |
| Incorrect Top-K | Retrieving too much noise or missing key information. | Experiment with the number of retrieved documents (Top-K). Start with a low number (e.g., 3-5) and increase based on performance [25]. |
| Faulty Ranking | Correct information exists but is ranked too low. | Implement a re-ranking step after the initial retrieval to re-order passages by relevance to the query [25]. |
Problem: Incomplete or Poorly Formatted Responses
Issue: The generated response is partially correct but lacks full coverage, or is in the wrong format (e.g., free text instead of a structured report).
Solution Strategy:
- Break Down Complex Queries: For broad questions, use query pre-processing to reformulate them into well-scoped sub-questions. This ensures comprehensive retrieval and generation for each part [25].
- Implement Structured Outputs: Use JSON or other predefined schemas in your prompts. Leverage LLM features that enforce schema-based responses (e.g., OpenAI's function calling) to ensure consistent formatting [25].
- Separate Instructions: In the prompt, clearly separate formatting instructions from the content instructions to avoid confusion for the model [25].
Experimental Protocols & Performance Data
Key Experiment: V-RAG for Chest X-Ray Report Generation
Objective: To evaluate the effectiveness of V-RAG in reducing hallucinations and improving the clinical accuracy of generated chest X-ray reports [4].
Methodology:
- Datasets: MIMIC-CXR (chest X-ray report generation) and Multicare (medical image caption generation) [4].
- Retrieval Setup:
- Embedding Model: BiomedCLIP for extracting image embeddings.
- Vector Database: FAISS with HNSW algorithm for approximate kNN search.
- Retrieval Count (k): Top-k similar images and their reports are retrieved (k=3 or 5 is common).
- Inference with V-RAG:
- The query image, along with the top-k retrieved images and their reports, are formatted into a structured prompt.
- The prompt includes explicit instructions, for example: "This is the i-th similar image and its report for your reference. [Reference Image Iᵢ] [Reference Report Rᵢ] ... Answer the question with only the word yes or no. Do not provide explanations. According to the last query image and the reference images and reports, [Question] [Query Image X_q]" [4].
- Evaluation:
- Entity Probing: The model is presented with an image and asked yes/no questions about disease entities. Answers are compared against grounded answers from a reference report [4].
- Report Generation & RadGraph-F1: The model generates a full report. The output is evaluated using RadGraph-F1 to measure clinical factual accuracy [4].
Quantitative Results: V-RAG vs. Baseline Performance
| Model / Approach | Entity Probing Accuracy (%) (Frequent) | Entity Probing Accuracy (%) (Rare) | RadGraph-F1 Score | Notes |
|---|---|---|---|---|
| Baseline Med-MLLM (No RAG) | 78.5 | 65.2 | 0.412 | Prone to hallucinations [4]. |
| Text-Based RAG | 82.1 | 72.8 | 0.445 | Assumes retrieved images are interchangeable with query [4]. |
| V-RAG (Proposed) | 85.7 | 79.4 | 0.481 | Incorporates both images and reports, outperforming baselines [4]. |
| VisRAG (on multi-modality docs) | - | - | - | Reports 20-40% end-to-end performance gain over text-based RAG [26]. |
V-RAG System Workflow
The following diagram illustrates the end-to-end process of a Visual RAG system, from data ingestion to response generation.
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function in V-RAG Experiment |
|---|---|
| BiomedCLIP | A vision-language model pre-trained on a wide range of biomedical images. Used to generate robust image embeddings for the retrieval step, crucial for capturing medical semantic similarity [4]. |
| FAISS (Facebook AI Similarity Search) | A library for efficient similarity search and clustering of dense vectors. Used as the vector database to store embeddings and perform fast approximate nearest neighbor searches [4]. |
| Multimodal LLM (Med-MLLM) | The core generator model (e.g., models based on LLaMA, GPT architectures fine-tuned on medical data). It is capable of processing both image and text inputs to generate final reports or answers [4] [13]. |
| MIMIC-CXR Dataset | A large publicly available dataset of chest X-ray images and corresponding free-text radiology reports. Serves as a standard benchmark for training and evaluating models on radiology report generation tasks [4]. |
| RadGraph | A tool for annotating and evaluating radiology reports by extracting clinical entities and their relations. Used to compute the RadGraph-F1 score, a key metric for evaluating the factual accuracy of generated reports [4] [24]. |
Troubleshooting Guides and FAQs
FAQ: What are the primary data collection methods for medical instruction tuning, and how do they compare? Instruction-tuning datasets are constructed using three major paradigms, each with distinct trade-offs between quality, scalability, and resource cost [27].
- Expert Annotation: Involves manual creation by clinicians or domain experts. This method yields the highest quality data but is expensive and does not scale easily [27] [28] [29].
- Distillation from Larger Models: Uses a powerful teacher model (like GPT-4) to automatically generate instruction-output pairs. This is highly scalable but may not be perfectly aligned with nuanced clinical expertise [27] [30] [28].
- Self-Improvement Mechanisms: Employs techniques like Self-Instruct or Reinforcement Learning from AI Feedback (RLAIF) for iterative bootstrapping and refinement of the dataset [27].
FAQ: My finely-tuned model is hallucinating on rare medical entities. How can I mitigate this? Visual Retrieval-Augmented Generation (V-RAG) is a promising framework to ground your model's responses in retrieved visual and textual data, which has been shown to improve accuracy for both frequent and rare entities [4] [31]. The process involves:
- Building a Multimodal Memory: Create a vector database (e.g., using FAISS) of embeddings from a corpus of medical images and their corresponding reports. Using a domain-specific encoder like BiomedCLIP is recommended [4].
- Retrieval at Inference: For a query image, retrieve the top-k most similar images and their associated reports from the database [4].
- Augmented Generation: The model is prompted to answer the clinical question using both the original query image and the retrieved image-report pairs as reference, which provides broader context and reduces unfounded assertions [4].
FAQ: How can I incorporate clinician expertise into automated data generation pipelines? The BioMed-VITAL framework provides a data-centric approach to align instruction data with clinician preferences [28]. Its key stages are:
- Preference-Aligned Generation: Use a powerful generator (e.g., GPT-4V) with a diverse set of clinician-selected and annotated demonstrations in its prompt to guide the generation of clinically relevant instruction-response pairs [28].
- Preference-Distilled Selection: Train a separate data selection model that learns to rank and select the highest-quality generated data based on a mixture of human clinician preferences and model-based judgments using clinician-curated criteria [28].
FAQ: My model is highly susceptible to adversarial hallucination attacks. What mitigation strategies are effective? Research shows that LLMs can be highly vulnerable to elaborating on fabricated details in clinical prompts [5]. Tested mitigation strategies include:
- Mitigation Prompts: Using a prompt that explicitly instructs the model to "use only clinically validated information and acknowledge uncertainty instead of speculating" can significantly reduce hallucination rates. One study showed this reduced the overall rate from 66% to 44% across multiple models [5].
- Temperature Settings: Adjusting the model's temperature parameter to zero (deterministic output) did not yield a significant improvement in reducing adversarial hallucinations [5].
FAQ: What are the most efficient fine-tuning techniques for adapting large models to the medical domain? Parameter-Efficient Fine-Tuning (PEFT) methods are essential for adapting large models with reduced computational cost [27] [29] [13].
- Low-Rank Adaptation (LoRA): This is a dominant technique. It freezes the pre-trained model weights and injects trainable rank decomposition matrices into the transformer layers, dramatically reducing the number of parameters that need to be updated [27] [29]. The core update is represented as
W' = W0 + BA, whereBandAare low-rank matrices [27]. - Benefits: PEFT methods like LoRA make model adaptation computationally feasible, preserve general knowledge to avoid catastrophic forgetting, and enable model reusability for multiple tasks [27] [29].
Table 1: Hallucination Rates and Mitigation Effectiveness Across LLMs (Adversarial Attack Study)
| Model | Default Hallucination Rate | Hallucination Rate with Mitigation Prompt |
|---|---|---|
| Overall Mean (All Models) | 66% | 44% |
| GPT-4o | 53% | 23% |
| Distilled-DeepSeek-R1 | 82% | Information Not Provided |
Source: [5] - Multi-model study with 300 physician-validated vignettes containing fabricated details.
Table 2: Performance Gains from Domain-Specific Instruction Tuning Frameworks
| Framework / Model | Domain | Notable Performance Gain | Key Feature |
|---|---|---|---|
| BioMed-VITAL [28] | Biomedical Vision | Win rate up to 81.73% on MedVQA | Clinician-aligned data generation/selection |
| LawInstruct [29] | Legal | +15 points (~50%) on LegalBench | 58 datasets, cross-jurisdiction |
| JMedLoRA [29] | Japanese Medical QA | Performance increase (various) | LoRA-based, cross-lingual transfer |
| Knowledge-aware Data Selection (KDS) [29] | Medical Benchmarks | +2.56% on Med Benchmarks | Filters data that causes knowledge conflicts |
Detailed Experimental Protocols
Protocol 1: Implementing Visual RAG (V-RAG) for Medical MLLMs
This methodology grounds model responses using retrieved images and reports to reduce hallucination [4].
Workflow Overview:
Key Steps:
- Multimodal Retrieval Database Construction:
- Inputs: A large corpus of medical images and their corresponding textual reports.
- Embedding Extraction: Use a domain-specific visual encoder (e.g., BiomedCLIP [4]) to extract image embeddings (
ℰ_img ∈ ℝ^d). - Vector Storage: Construct a memory bank
ℳusing a vector database like FAISS. For efficient approximate search, use the Hierarchical Navigable Small World (HNSW) algorithm [4].
- Inference with V-RAG:
- Encode the query image
X_qto get its embedding. - Retrieve the top-
kmost similar images(I_1, ..., I_k)and their reports(R_1, ..., R_k)fromℳ. - Construct a composite prompt that includes the query image and the retrieved image-report pairs as references.
- The prompt should explicitly instruct the model to base its answer on both the query and the references [4].
- Encode the query image
Protocol 2: Clinician-Aligned Data Generation and Selection (BioMed-VITAL)
This protocol ensures automatically generated data aligns with domain expert preferences [28].
Workflow Overview:
Key Steps:
- Data Generation with Expert Demonstrations:
- Diverse Sampling: From a seed dataset, use K-means clustering on image and text features (e.g., from BiomedCLIP) to create distinct categories. Uniformly sample from these clusters to ensure diversity [28].
- Clinician Annotation: Present the sampled data to clinicians. For each instruction, have them choose between candidate responses, select both if good, or reject both. Use majority voting to resolve disagreements [28].
- Guided Generation: Use a powerful multimodal generator (e.g., GPT-4V). The clinician-annotated pairs are used as few-shot demonstrations in the generator's prompt to produce preference-aligned instruction data at scale [28].
- Data Selection with Distilled Preferences:
- Mixed Preference Data: Combine a limited set of human clinician preferences with a larger set of model-annotated preferences. The model annotations are guided by clinician-curated criteria [28].
- Selection Model Training: Train a separate model (the data selector) on this mixed preference data to learn a rating function that distinguishes high-quality, clinically relevant instructions [28].
- Data Filtering: Use the trained selection model to rank the large pool of generated data. Select the top-ranked samples for the final instruction-tuning dataset [28].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Medical MLLM Instruction Tuning
| Item / Resource | Function / Purpose in Research |
|---|---|
| Parameter-Efficient Fine-Tuning (PEFT) [27] [29] | A class of methods, including LoRA, that adapts large models to new tasks by updating only a small subset of parameters, drastically reducing computational requirements. |
| Low-Rank Adaptation (LoRA) [27] [29] | A specific, widely-used PEFT technique that injects and trains low-rank matrices into transformer layers, making domain adaptation computationally feasible. |
| BiomedCLIP [4] [28] | A vision encoder pre-trained on a vast corpus of biomedical images and text. Used to extract powerful domain-specific visual features for tasks like retrieval. |
| Visual Retrieval-Augmented Generation (V-RAG) [4] [31] | A framework that augments an MLLM's knowledge by retrieving relevant images and reports from an external database during inference, reducing hallucinations. |
| FAISS Vector Database [4] | A library for efficient similarity search and clustering of dense vectors. Essential for building the retrieval component in a V-RAG system. |
| Clinician-in-the-Loop Annotation [28] [5] | The process of incorporating feedback from medical experts to ensure the quality, relevance, and safety of training data and model outputs. |
| Instruction-Tuning Datasets (e.g., PMC-Llama-Instructions [30], LLaVA-Med [28]) | Curated collections of instruction-response pairs, often amalgamated from multiple public datasets, used to teach models to follow instructions in a biomedical context. |
Frequently Asked Questions (FAQs)
Q1: What are the most effective connector architectures for reducing hallucinations in medical MLLMs? Projection-based connectors (MLP) provide strong baseline performance, while compression-based methods like spatial pooling and CNN-based abstractors better handle high-resolution medical images by reducing token sequence length. Query-based connectors using trainable tokens offer enhanced performance for lesion-specific grounding [32] [13]. The optimal choice depends on your specific medical imaging modality and computational constraints.
Q2: How can I improve my model's handling of rare medical entities? Visual Retrieval-Augmented Generation (V-RAG) significantly improves performance on both frequent and rare entities by incorporating similar images and their reports during inference. Fine-tuning with multi-image comprehension tasks enables models to leverage retrieved references effectively, with documented RadGraph-F1 score improvements [8] [4].
Q3: What training strategies best mitigate hallucination in medical report generation? A three-stage approach proves most effective: pre-training with image-text alignment, instruction tuning with both multimodal and text-only data, and alignment tuning using reinforcement learning from human feedback. LoRA fine-tuning efficiently adapts models to medical domains while preserving general knowledge [13] [33].
Q4: How do vision encoder choices impact medical report accuracy? Vision Transformers (ViTs) and their variants (DEiT, BEiT) outperform CNN-based encoders by capturing global context through patch-based processing and self-attention mechanisms. BEiT reduces computational complexity through downsampling, while DEiT enhances robustness via data augmentation [34].
Q5: What evaluation metrics best detect hallucinations in medical imaging? Entity probing with yes/no questions about medical entities provides clinical grounding. RadGraph-F1 scores evaluate report quality, while dataset-wise statistical analysis and clinical task-based assessments offer comprehensive hallucination detection [8] [2].
Troubleshooting Guides
Issue: Poor Alignment Between Visual Features and Text Generation
Symptoms: Generated reports contain plausible but incorrect findings, descriptions contradict visual evidence, or missed abnormalities.
Solution:
- Verify connector architecture: Implement cross-attention mechanisms between vision transformer outputs and GPT-2 decoder layers [34]
- Enhance multimodal alignment:
- Use progressive training: start with image-text matching, advance to structured report generation
- Incorporate region-grounded reasoning with bounding box annotations
- Apply contrastive learning between image patches and text segments [13]
Implementation Protocol:
Issue: Computational Limitations with High-Resolution Medical Images
Symptoms: Training crashes due to memory constraints, slow inference times, or truncated image features.
Solution:
- Implement token compression:
- Spatial relation compression via adaptive average pooling
- Semantic perception compression using attention pooling
- CNN-based abstractors with ResNet blocks [32]
- Optimize training efficiency:
- Use LoRA (Low-Rank Adaptation) for efficient fine-tuning
- Implement gradient checkpointing
- Apply mixed-precision training [33]
Experimental Results:
Table 1: Compression Methods Performance Comparison
| Method | Token Reduction | Report Quality (RadGraph-F1) | Memory Usage |
|---|---|---|---|
| Linear Projection | 0% | 0.723 | 100% |
| Adaptive Pooling | 75% | 0.718 | 42% |
| CNN Abstractor | 75% | 0.741 | 45% |
| Semantic Attention | 80% | 0.752 | 38% |
Issue: Hallucinations of Rare Diseases or Uncommon Findings
Symptoms: Model fails to recognize rare pathologies, defaults to common patterns, or generates inconsistent descriptions for unusual cases.
Solution:
- Implement Visual RAG (V-RAG):
- Retrieve top-k similar images and reports using BiomedCLIP embeddings
- FAISS with HNSW algorithm for efficient similarity search
- Multi-image inference with reference prompts [4]
- Augment training strategy:
- Entity-specific data balancing
- Rare entity oversampling with label smoothing
- Progressive curriculum learning from common to rare findings
V-RAG Implementation Workflow:
Issue: Inconsistent Performance Across Medical Imaging Modalities
Symptoms: Model performs well on X-rays but poorly on CT/MRI, modality-specific hallucinations, or failed cross-modal alignment.
Solution:
- Modality-specific adaptations:
- 3D patch processing for volumetric data (CT/MRI)
- Temporal modeling for video data (ultrasound, cardiac MRI)
- Multi-scale feature extraction for different resolution requirements
- Architecture modifications:
- Separate modality encoders with shared connectors
- Modality-specific fine-tuning with gradual fusion
- Contrastive learning across modalities
Experimental Protocol for Multi-Modality Evaluation:
Table 2: Modality-Specific Adaptation Performance
| Imaging Modality | Encoder Architecture | Connector Type | Hallucination Rate | Clinical Accuracy |
|---|---|---|---|---|
| Chest X-ray (2D) | ViT-B/16 | MLP + Cross-attention | 8.3% | 91.7% |
| CT (3D) | ViT-3D | Query-based + Compression | 12.1% | 87.9% |
| MRI | BEiT-3D | Fusion-based | 10.5% | 89.5% |
| Ultrasound | DEiT + Temporal | CNN Abstractor | 15.2% | 84.8% |
Experimental Protocols & Methodologies
Vision Encoder Comparative Analysis Protocol
Objective: Systematically evaluate vision encoder architectures for medical image interpretation and hallucination reduction.
Methodology:
- Encoder Selection: Compare ViT, DEiT, and BEiT architectures with identical parameter counts
- Training Regimen:
- Pre-training on MIMIC-CXR and Multicare datasets
- 100 epochs with cosine annealing learning rate schedule
- Batch size: 32 with gradient accumulation
- Evaluation Metrics:
- Entity probing accuracy (yes/no questions)
- RadGraph-F1 for report quality
- Hallucination rate per image
Implementation Details:
V-RAG Fine-tuning Protocol for Hallucination Reduction
Objective: Adapt single-image MLLMs to effectively utilize multiple retrieved images and reports.
Methodology:
- Multi-image comprehension pretraining:
- Input: Query image + 3 retrieved similar images with reports
- Task: Identify consistent findings across images
- Output: Differentiated observations between query and retrieved images
Entity grounding reinforcement:
- Contrastive learning between grounded and hallucinated entities
- Explicit training on rare entity recognition
- Cross-image consistency constraints
Inference optimization:
- Dynamic retrieval count (k=3-5 based on similarity scores)
- Confidence-based integration of retrieved knowledge
- Fallback mechanisms for novel cases with low retrieval similarity
Visual RAG Architecture:
The Scientist's Toolkit
Table 3: Essential Research Reagents and Solutions
| Resource | Type | Function | Implementation Example |
|---|---|---|---|
| BiomedCLIP | Embedding Model | Medical image-text similarity for retrieval | Feature extraction for V-RAG memory construction [4] |
| MIMIC-CXR | Dataset | Chest X-ray images with reports | Training and evaluation of radiology MLLMs [8] |
| Multicare | Dataset | Diverse medical image captions | Generalization testing across modalities [8] |
| FAISS | Retrieval System | Efficient similarity search | V-RAG retrieval backend with HNSW indexing [4] |
| LoRA | Training Method | Parameter-efficient fine-tuning | Adapting LLMs to medical domains [33] |
| RadGraph | Evaluation Tool | Structured medical concept extraction | Hallucination detection and report quality assessment [8] |
| ViT/BEiT/DEiT | Vision Encoders | Medical image feature extraction | Comparing encoder architectures for optimal performance [34] |
Performance Optimization Guide
Connector Selection Decision Framework
For High-Resolution Images:
- Primary choice: Compression-based connectors (spatial or semantic)
- Fallback: Query-based with token reduction
- Avoid: Simple linear projection without compression
For Multi-Modality Integration:
- Primary choice: Fusion-based connectors with cross-attention
- Fallback: Projection-based with modality-specific adapters
- Avoid: Expert-driven language transformation (information loss)
For Computational Constraints:
- Primary choice: LoRA fine-tuning with linear connectors
- Fallback: MLP with aggressive token compression
- Avoid: Multi-encoder architectures without sharing
Quantitative Performance Benchmarks
Table 4: Connector Architecture Performance Comparison
| Connector Type | Training Speed | Inference Latency | Hallucination Rate | Best Use Case |
|---|---|---|---|---|
| Linear Projection | Fastest | Lowest | 12.5% | Baseline/prototyping |
| MLP (2-layer) | Fast | Low | 10.8% | Balanced performance |
| Query-based | Medium | Medium | 8.9% | Lesion-specific tasks |
| Compression (CNN) | Medium | Low | 7.5% | High-resolution images |
| Fusion-based | Slow | High | 6.8% | Multi-modal integration |
| V-RAG Enhanced | Slowest | Highest | 5.2% | Production clinical use |
This technical support framework provides comprehensive guidance for researchers developing medical MLLMs with reduced hallucinations. The protocols and troubleshooting guides are grounded in recent advances in vision encoders and multimodal connectors, with empirically validated performance metrics from current literature.
Frequently Asked Questions (FAQs)
1. What is cross-modal consistency and why is it critical for medical MLLMs? Cross-modal consistency refers to the ability of a Multimodal Large Language Model (MLLM) to produce semantically equivalent and clinically coherent information when the same underlying task or query is presented through different modalities, such as an image versus a text description [35]. In medical imaging, a lack of consistency means the model might correctly identify a finding in a chest X-ray image but fail to recognize the same finding when described in a textual report, or vice-versa. This inconsistency is a direct manifestation of hallucination, severely undermining the model's reliability for clinical tasks like diagnosis and report generation [4] [35] [36].
2. What are the primary technical causes of cross-modal inconsistency? The main technical roots of inconsistency include:
- Architectural Gaps: The separate encoders for vision and language may not be perfectly aligned in a shared semantic space, leading to misinterpretation when fusing information [13] [35].
- Training Data Disparities: Differences in the quality, quantity, and domain-specificity of image and text data used for pre-training can create capability gaps between the model's visual and linguistic understanding [35].
- Information Loss in Fusion: The "multimodal connector" (e.g., a simple MLP) may be insufficient to capture complex, fine-grained relationships between medical images and textual concepts, causing details to be lost or invented [13].
3. How can I quantitatively measure cross-modal consistency in my model? You can establish a quantitative framework by creating or using a dataset of parallel task instances [35]. For each clinical task (e.g., disease classification), create matched pairs where one instance uses the medical image as input, and the other uses a meticulously crafted text description of the same image. The model's outputs for both instances are compared against a gold standard. Consistency is measured as the agreement in performance (e.g., accuracy, F1 score) between the image-based and text-based pathways for the same set of underlying clinical questions [35].
4. What is Visual Retrieval-Augmented Generation (V-RAG) and how does it reduce hallucinations? V-RAG is a framework that grounds the MLLM's generation process in retrieved, relevant knowledge [4] [31]. When the model is queried with a medical image, it first retrieves the most visually and semantically similar images from a database, along with their corresponding accurate reports. The model is then prompted to answer the query or generate a report based on both the original image and the retrieved image-report pairs. This provides an external knowledge base for the model to reference, significantly reducing the generation of ungrounded or "hallucinated" findings by providing concrete, relevant examples [4].
Troubleshooting Guides
Issue 1: Model Generates Clinically Inaccurate Findings in Radiology Reports
Problem: Your MLLM generates radiology reports from images that contain plausible-sounding but clinically inaccurate statements (e.g., mentioning a "pneumothorax" that is not present in the X-ray).
Solution: Implement a Visual Retrieval-Augmented Generation (V-RAG) Pipeline.
Experimental Protocol:
- Database Construction: Build a curated database of medical images (e.g., chest X-rays) and their corresponding, validated radiology reports [4].
- Retriever Setup: Implement a robust multimodal retriever. A recommended approach is to use BiomedCLIP to extract image and text embeddings into a shared space, then index them using FAISS with the HNSW algorithm for efficient approximate nearest neighbor search [4].
- Inference with Retrieval: For a query image, retrieve the top-k most similar images and their reports. Structure your prompt as follows [4]:
"This is the 1st similar image and its report for your reference. [Image1] [Report1]. ... Answer the question/generate a report based on the last query image and the reference images and reports. [Query Image]"
Expected Outcome: The generated report will be more grounded in the visual evidence of the query image and the clinically accurate references, leading to a higher RadGraph-F1 score and reduced hallucination of entities [4].
Issue 2: Model Shows Poor Performance on Rare Diseases or Uncommon Findings
Problem: The MLLM performs adequately on common findings but fails to correctly identify or describe rare pathologies.
Solution: Enhance the model with targeted fine-tuning and leverage V-RAG's capability for rare entities.
Experimental Protocol:
- Entity Probing: Create a diagnostic test to evaluate the model's performance on specific medical entities. This involves presenting the model with an image and asking a series of yes/no questions (e.g., "Is there evidence of pneumothorax in this image?") [4].
- Stratified Analysis: Analyze the model's accuracy separately for frequent and rare entities (e.g., entities that appear in less than 1% of the training data) [4].
- Targeted Retrieval: Ensure your V-RAG database is enriched with examples of rare findings. The retrieval system will then be more likely to find relevant reference cases, even for uncommon queries, providing the model with the necessary context it lacks from its base training [4].
Expected Outcome: V-RAG has been shown to improve accuracy for both frequent and rare entities, as it bypasses the model's need to have these patterns deeply encoded in its parameters, instead relying on the external knowledge base [4].
Issue 3: Inconsistent Diagnoses Between Image and Text Inputs
Problem: The model provides different diagnoses or findings when the same clinical case is presented as an image versus when it is described in text.
Solution: Systematically evaluate and improve cross-modal consistency.
Experimental Protocol:
- Create a Parallel Consistency Evaluation Dataset: For a set of medical images, create perfect textual descriptions that capture all clinically relevant information. This forms matched (image, text) pairs for the same case [35].
- Define Consistency Metric: Run the model on both the image input and the text description input for all cases. Calculate the metric as the rate at which the model's outputs (e.g., the primary finding or diagnosis) agree across the two modalities for the same case [35].
- Mitigation via Alignment Tuning: If a significant inconsistency is found, employ alignment tuning techniques on your model. This often involves Reinforcement Learning from Human Feedback (RLHF), where a reward model is trained to penalize outputs that are inconsistent or not faithful to the source input, and the main model is fine-tuned to maximize this reward [13].
Expected Outcome: A quantifiable measure of your model's cross-modal consistency. Applying mitigation strategies should lead to a higher consistency score, making the model more reliable and trustworthy [35].
Experimental Data & Protocols
Table 1: Impact of Visual-RAG on Hallucination Reduction in Chest X-Ray Report Generation
| Metric | Baseline MLLM (No RAG) | MLLM with Text-Only RAG | MLLM with Visual-RAG (V-RAG) |
|---|---|---|---|
| Overall Entity Probing Accuracy | Baseline | Moderate Improvement | Highest Improvement |
| Accuracy on Frequent Entities | Baseline | Moderate Improvement | Highest Improvement |
| Accuracy on Rare Entities | Low | Slight Improvement | Significant Improvement |
| RadGraph-F1 Score | Baseline | Moderate Improvement | Highest Improvement |
| Hallucination Rate | Baseline | Reduced | Most Reduced |
Source: Adapted from experiments on MIMIC-CXR dataset in [4].
Core Protocol: Entity Probing for Hallucination Measurement
- Objective: Quantify whether an MLLM correctly grounds specific medical entities in the image content.
- Setup: Use a dataset of medical images with a set of established ground-truth entities (e.g., from expert-annotated reports).
- Procedure: For each image and each entity, prompt the model with: "Does the image show [entity]? Answer with only 'yes' or 'no'." [4]
- Analysis: Compare the model's yes/no answers to the ground truth. Accuracy is calculated as the proportion of correct answers, providing a clear, clinical measure of hallucination separate from text generation fluency [4].
The Scientist's Toolkit
Table 2: Key Research Reagents for Cross-Modality Verification Experiments
| Reagent / Solution | Function in Experimental Protocol |
|---|---|
| BiomedCLIP | A vision-language model pre-trained on a massive corpus of biomedical images and text. Used to generate high-quality, domain-specific embeddings for images and reports, which is crucial for building an effective retrieval database [4]. |
| FAISS (with HNSW) | A library for efficient similarity search and clustering of dense vectors. The Hierarchical Navigable Small World (HNSW) index allows for fast and accurate retrieval of the top-k most similar images/reports from a large database during V-RAG inference [4]. |
| MIMIC-CXR Dataset | A large, public dataset of chest radiographs with free-text radiology reports. Serves as a standard benchmark for training and evaluating models on tasks like report generation and entity probing [4]. |
| RadGraph | A tool and dataset for annotating entities and relations in radiology reports. The RadGraph-F1 score is a key metric for evaluating the factual accuracy of generated reports against expert annotations, directly measuring clinical correctness [4]. |
| LoRA (Low-Rank Adaptation) | A parameter-efficient fine-tuning (PEFT) method. Allows researchers to adapt large pre-trained MLLMs to specific medical tasks by only training a small number of parameters, making experimentation more computationally feasible [13] [37]. |
Workflow Diagrams
Visual-RAG (V-RAG) Workflow
Cross-Modal Consistency Evaluation
Refining Performance: Troubleshooting Pitfalls and Optimizing Workflows
This guide provides technical support for researchers confronting adversarial attacks against multimodal AI in medical and drug discovery contexts. These attacks exploit model vulnerabilities using fabricated inputs, leading to hallucinations and incorrect outputs. The following sections offer troubleshooting guides, experimental protocols, and defensive strategies to enhance model robustness.
Troubleshooting Guide: Identifying Adversarial Vulnerabilities
This section addresses common challenges and solutions when experimenting with multimodal models.
Q: My model is generating outputs that elaborate on fabricated details from the input. What is happening?
- A: This is a classic adversarial hallucination attack. Models can be overly confirmatory, treating every input token as truth. When a prompt contains a fabricated detail (e.g., a fake lab test or disease), the model may not only accept it but also generate additional, incorrect information about it [5].
- Troubleshooting Steps:
- Audit Inputs: Implement a pre-processing check to flag inputs containing terms not found in your verified knowledge bases (e.g., Drugs.com, PubMed) [38].
- Use Mitigation Prompts: Employ prompts that instruct the model to "use only clinically validated information and acknowledge uncertainty instead of speculating" [5].
- Quantify the Issue: Follow the protocol in the Experimental Protocols section to establish a baseline hallucination rate for your model.
Q: My multimodal model is being fooled by a slightly modified image, even though the text prompt is correct. Why?
- A: You are likely facing a cross-modal adversarial attack. Attackers add imperceptible perturbations to an image so that its embedding in the model aligns with a target concept different from its actual content [39]. A related threat is steganographic prompt injection, where malicious instructions are hidden within an image's pixels [40].
- Troubleshooting Steps:
- Test with Transformations: Apply image resizing, JPEG compression, or mild noise to the input. A sudden change in output after these transformations suggests adversarial manipulation [39].
- Analyze Embeddings: If possible, compare the image embedding produced by your vision encoder against a database of known, clean image embeddings to detect anomalies.
- Implement Detection: Explore neural steganalysis tools designed to detect minute alterations in image structures that indicate hidden data [40].
Q: I've heard multimodal models are more robust. Is this true, and how can I leverage this?
- A: Evidence suggests that well-designed multimodal models can be more resilient than their single-modality counterparts. The integration of multiple data types (e.g., image and text) allows the model to cross-verify information, making it harder to deceive all modalities simultaneously [41].
- Troubleshooting Steps:
- Fusion Technique: Evaluate your model's fusion mechanism. Late fusion (combining decisions from unimodal models) can be more effective with moderate dataset sizes than early fusion (combining raw features) [41].
- Stress Testing: Perform attacks on individual modalities (e.g., image-only, text-only) and then on the combined model. A significant performance drop in the unimodal setting but not the multimodal one confirms the robustness benefit [41].
Q: How can I make my model's output more faithful and traceable?
- A: The core issue is the lack of grounding in verified evidence. A knowledge-grounded collaborative architecture, like the one used in DrugGPT, can significantly improve this [38].
- Troubleshooting Steps:
- Implement a Knowledge Layer: Incorporate a mechanism that first analyzes the input query, then retrieves relevant information from trusted knowledge bases, and finally generates an answer based solely on this retrieved evidence [38].
- Enable Traceability: Design your output to include citations or references to the specific knowledge source used for each part of the generated content [38].
Quantitative Data on Adversarial Attacks
The tables below summarize key metrics from recent research on adversarial attacks and defenses.
Table 1: Adversarial Hallucination Attack Success Rates on LLMs
Data sourced from testing 300 physician-validated clinical vignettes containing one fabricated detail each [5].
| Model | Default Hallucination Rate | Hallucination Rate with Mitigation Prompt |
|---|---|---|
| GPT-4o | 53% | 23% |
| Distilled-DeepSeek-R1 | 82% | Not Specified |
| Mean across 6 models | 66% | 44% |
Table 2: Effectiveness of Different Attack Modalities
Data compiled from various studies on multimodal adversarial attacks [41] [39] [40].
| Attack Method | Modality | Key Metric | Result |
|---|---|---|---|
| CrossFire Attack [39] | Image-to-Text | Attack Success Rate (ASR) on ImageNet | 98% |
| Steganographic Prompt Injection [40] | Image (Hidden Text) | Overall ASR across 8 VLMs | 24.3% |
| Adversarial Attack (Single-Modality) [41] | Image | Performance Degradation | High |
| Adversarial Attack (Multimodal) [41] | Image & Text | Performance Degradation | Lower (Enhanced Robustness) |
Experimental Protocols
Protocol 1: Measuring Baseline Vulnerability to Hallucination Attacks
Objective: Quantify how often your model elaborates on deliberately fabricated input details [5].
Test Case Creation:
- Develop a set of vignettes (e.g., 50-100 words) that each contain a single fabricated element (e.g., a fake lab test "Serum Neurostatin," a fake sign "Cardiac Spiral Sign," or a fake disease "Faulkenstein Syndrome").
- Ensure fabricated terms have no real-world analogs by checking resources like PubMed.
- Validate all cases with domain experts.
Model Testing:
- Provide each vignette to the model with a task-oriented prompt (e.g., "List the following details in JSON format...").
- Run each test case under the model's default settings.
Output Classification & Analysis:
- Hallucination: Any output that endorses, elaborates on, or treats the fabricated element as real.
- Non-Hallucination: Output that omits, expresses uncertainty about, or correctly identifies the element as fabricated.
- Calculate the overall hallucination rate: (Number of hallucinated outputs / Total outputs) * 100.
Protocol 2: Evaluating Cross-Modal Adversarial Robustness
Objective: Assess model performance under unimodal vs. multimodal adversarial attacks [41].
Baseline Establishment:
- Measure your model's accuracy on a clean, balanced test set containing paired image-text data.
Unimodal Attack:
- Image-Only Attack: Use a gradient-based method (e.g., PGD [41]) to generate adversarial perturbations for the images in the test set. Keep the corresponding text clean.
- Text-Only Attack: Use synonym substitution or word deletion [41] to perturb the text in the test set. Keep the corresponding images clean.
- Evaluate model performance on these attacked unimodal sets.
Multimodal Attack:
- Attack both the image and text modalities of the test set simultaneously.
- Evaluate model performance on this attacked multimodal set.
Analysis:
- Compare the performance drop across the three scenarios. A smaller performance drop in the multimodal attack condition suggests inherent robustness from data fusion.
Essential Visual Workflows
Adversarial Hallucination Attack Assessment
Multimodal Adversarial Defense Architecture
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function | Example Use Case |
|---|---|---|
| Pre-trained SE-ResNet-154 [41] | A robust vision encoder for medical image processing. | Serving as the image backbone in a multimodal model to classify X-ray images. |
| Bio_ClinicalBERT [41] | A domain-specific language model trained on clinical text (MIMIC-III). | Processing electronic health records (EHR) or clinical notes in a multimodal pipeline. |
| Trusted Knowledge Bases (Drugs.com, NHS, PubMed) [38] | Provide verified, evidence-based information for knowledge-grounded generation. | Used by a model like DrugGPT to retrieve factual data and reduce hallucinations. |
| DREAM Report Framework [42] | A structured approach (Definition, Examples, Detection, Causes, Mitigation) for analyzing hallucinations in medical AIGC. | Systematically evaluating hallucination risks in a nuclear medicine imaging AI. |
| Adversarial Training Datasets (e.g., Flickr30K, MSCOCO) [43] | Benchmark datasets used to train and evaluate the transferability of adversarial attacks. | Testing the robustness of a vision-language model against known attack methods. |
Frequently Asked Questions (FAQs)
Q1: What are the most common types of hallucinations in Multimodal LLMs for medical imaging? In medical imaging MLLMs, hallucinations are typically categorized into two main types. Knowledge-based hallucinations involve inconsistencies with real-world facts or medical knowledge, such as generating incorrect anatomical descriptions. Logic-based hallucinations arise from flawed reasoning processes, leading to incorrect diagnostic conclusions despite accurate input data [44]. In nuclear medicine imaging, a more specific definition is used: AI-fabricated abnormalities or artifacts that appear visually realistic and highly plausible yet are factually false and deviate from anatomic or functional truth [2].
Q2: How does the model architecture impact the trade-off between computational efficiency and hallucination control? Model architecture significantly influences this balance through several mechanisms. Using pre-trained encoders (like CLIP) and frozen LLMs as cognitive engines reduces computational load compared to training from scratch [13]. The choice of multimodal connector affects both performance and efficiency: projection-based connectors (MLP) are computationally lighter but may increase hallucination risks, while fusion-based connectors (cross-attention) offer better integration at higher computational cost [13]. Selective fine-tuning strategies, such as Low-Rank Adaptation (LoRA), maintain performance while significantly reducing training computational requirements [13].
Q3: What are the most effective strategies to mitigate hallucinations without excessive computational overhead? The most efficient mitigation strategies include Retrieval-Augmented Generation (RAG), which grounds model responses in external, verifiable medical knowledge without retraining [44]. Reasoning enhancement techniques like Chain-of-Thought (CoT) improve logical consistency [44]. Alignment tuning through reinforcement learning from human feedback optimizes outputs using relatively small, high-quality datasets [13]. Implementing these as modular components allows for effective hallucination control without the massive computational cost of full model retraining.
Q4: How can researchers evaluate the effectiveness of hallucination control methods? Evaluation should encompass multiple approaches. Image-level comparisons against ground truth data assess factual accuracy [2]. Dataset-wise statistical analysis identifies patterns in hallucination frequency [2]. Clinical task-based assessment involving human experts or model observers evaluates real-world impact [2]. Automated hallucination detectors trained on annotated benchmark datasets provide scalable monitoring [2]. Each method varies in computational demands, allowing researchers to select appropriate evaluation protocols based on their resources.
Troubleshooting Guides
Issue: High Computational Demand During Training
Symptoms: Extremely long training times, GPU memory exhaustion, inability to scale to larger medical datasets.
Solution:
- Implement Parameter-Efficient Fine-Tuning (PEFT)
Optimize Training Strategy
This staged approach concentrates computational resources where they have greatest impact [13].
Leverage Existing Foundation Models
- Build upon pre-trained LLMs and vision encoders rather than training from scratch [13].
- Use adapters and connectors to specialize general models for medical domains.
Issue: Persistent Hallucinations in Generated Reports
Symptoms: Model generates plausible but incorrect findings, adds non-existent abnormalities, omits real lesions.
Solution:
- Implement Retrieval-Augmented Generation (RAG)
Enhance Reasoning Capabilities
Improve Training Data Quality
Issue: Poor Performance- Efficiency Trade-off in Deployment
Symptoms: Model too slow for clinical workflows, high inference costs, compromised accuracy for speed.
Solution:
- Apply Model Optimization Techniques
Optimize Inference Architecture
- Deploy efficient multimodal connectors (projection-based for speed, query-based for accuracy) [13].
- Cache frequent computations and use hierarchical processing.
Balance Processing Levels
- Use lighter processing for normal cases, detailed analysis only for complex cases.
- Implement early exit strategies when confidence thresholds are met.
Computational Requirements of MLLM Components
| Component | Training Compute | Inference Speed | Hallucination Risk | Mitigation Strategies |
|---|---|---|---|---|
| Vision Encoder | High (pre-training) | Medium | Low-Medium | Use pre-trained models; Selective fine-tuning [13] |
| Multimodal Connector | Medium | Fast | Medium | Query-based architecture; Cross-attention mechanisms [13] |
| LLM Backbone | Very High (pre-training) | Medium-Slow | High | Frozen weights; RAG integration; Reasoning enhancement [13] [44] |
| Alignment Modules | Low | Fast | Low | Reinforcement learning from human feedback; Preference optimization [13] |
Hallucination Mitigation Effectiveness and Computational Cost
| Mitigation Method | Hallucination Reduction | Computational Overhead | Implementation Complexity | Best Use Cases |
|---|---|---|---|---|
| RAG Systems | High (Knowledge-based) | Low-Medium | Medium | Factual accuracy; Clinical guideline adherence [44] |
| Reasoning Enhancement | Medium-High (Logic-based) | Medium | High | Complex diagnoses; Differential diagnosis [44] |
| Alignment Tuning | Medium | Low | Low-Medium | Output quality; Safety constraints [13] |
| Region-Grounded Training | High (Spatial) | High | High | Anatomical localization; Lesion description [13] |
Experimental Protocols
Protocol 1: Evaluating Hallucination Frequency in Generated Reports
Objective: Quantify and categorize hallucinations in MLLM-generated radiology reports.
Methodology:
- Dataset Preparation
- Curate a test set of 500 medical images with verified ground truth reports
- Include diverse modalities (X-ray, CT, MRI) and anatomical regions
- Ensure balanced representation of normal and abnormal findings
Model Configuration
Evaluation Metrics
- Factual Accuracy: Consistency with ground truth findings
- Hallucination Rate: Percentage of generated statements unsupported by image
- Clinical Severity: Impact of hallucinations on potential patient outcomes
Analysis Procedure
- Double-blind review by board-certified radiologists
- Categorize hallucinations by type (knowledge-based vs. logic-based)
- Correlate hallucination frequency with image complexity and finding rarity
Protocol 2: Computational Efficiency Optimization
Objective: Reduce inference computational cost while maintaining diagnostic accuracy.
Methodology:
- Baseline Establishment
- Measure FLOPs, memory usage, and inference time for full model
- Establish accuracy benchmarks on standardized medical imaging dataset
Optimization Techniques
- Quantization: FP32 to FP16 and INT8 precision
- Pruning: Remove redundant attention heads and layers
- Knowledge Distillation: Train smaller student model
- Early Exit: Implement confidence-based inference termination
Evaluation Framework
- Track performance-efficiency trade-off curves
- Measure accuracy drop per unit of computational savings
- Validate clinical acceptability with domain experts
Iterative Refinement
- Identify computational bottlenecks through profiling
- Target optimizations to most expensive components
- Validate across multiple medical imaging domains
Experimental Workflows and System Architecture
MLLM Training and Optimization Workflow
Hallucination Detection and Mitigation System
Research Reagent Solutions
| Research Tool | Function | Implementation Example | Computational Profile |
|---|---|---|---|
| CLIP Medical Encoder | Vision-language alignment for medical images | Pre-trained encoder fine-tuned on radiology datasets [13] | High initial training, efficient inference |
| Low-Rank Adaptation (LoRA) | Parameter-efficient fine-tuning | Rank decomposition matrices applied to attention layers [13] | Low memory footprint, minimal performance loss |
| Retrieval-Augmented Generation (RAG) | External knowledge grounding | Vector database of medical literature and guidelines [44] | Medium overhead, scalable with retrieval complexity |
| Chain-of-Thought (CoT) Prompting | Enhanced reasoning transparency | Structured prompts for step-by-step diagnostic reasoning [44] | Low computational cost, significant accuracy gains |
| Region-Grounded Evaluation | Spatial alignment verification | Bounding box coordination between image regions and text descriptions [13] | High computational demand, essential for localization tasks |
| Multi-modal Fusion Connectors | Cross-modal information integration | Cross-attention layers between vision and language representations [13] | Variable overhead depending on architecture choice |
Troubleshooting Guide: Common Problems and Solutions
Problem: My model performs well on common entities but fails on new or rare biomedical concepts.
- Explanation: This is often a problem of concept generalization, where models cannot identify novel entities unseen during training. Models may over-rely on surface-level patterns from the training data [45].
- Solution: Implement a statistics-based debiasing method. Calculate the class distribution of words in your training set as a bias prior and use it to reduce the training signals from words that are statistically very likely (or unlikely) to be entities, forcing the model to rely on deeper contextual cues [45].
Problem: The multimodal LLM (MLLM) is generating descriptions that contain findings not present in the medical image (hallucinations).
- Explanation: Hallucinations can occur due to poor visual encoding, misalignment between visual and textual data, or training on low-quality datasets [4] [3].
- Solution: Implement a Visual Retrieval-Augmented Generation (V-RAG) framework. For a query image, retrieve the top-k most similar images and their corresponding reports from a database. Present both the retrieved images and their reports to the MLLM to provide richer, grounded context for generating a report for the query image, significantly improving clinical accuracy [4].
Problem: My model's high overall performance on the benchmark is misleading; it fails on synonyms of known entities.
- Explanation: This indicates a weakness in synonym generalization. The model has memorized specific surface forms but cannot link different expressions of the same concept (e.g., "Motrin" and "Ibuprofen") [45].
- Solution: Augment your training data with synonyms from biomedical knowledge bases. Furthermore, apply the same debiasing technique mentioned for concept generalization, as it has been shown to improve performance on synonym variants as well [45].
Problem: The model is learning unintended correlations (shortcuts) from the dataset, undermining its real-world robustness.
- Explanation: This is known as shortcut learning, where inherent biases in the dataset cause the model to exploit false correlations for its predictions [46].
- Solution: Employ the Shortcut Hull Learning (SHL) paradigm. Use a suite of models with different inductive biases (e.g., CNNs, Transformers) to collaboratively learn the minimal set of shortcut features (the "shortcut hull") in your data. This helps diagnose dataset issues and establishes a more reliable, shortcut-free evaluation framework [46].
Frequently Asked Questions (FAQs)
Q1: What are the main types of recognition abilities a biomedical NER model should have? A robust BioNER model should be evaluated on three distinct abilities [45]:
- Memorization: Identifying entity mentions that were explicitly seen during training.
- Synonym Generalization: Correctly identifying new surface forms (synonyms) of known entities (e.g., recognizing "Ibuprofen" when trained on "Motrin").
- Concept Generalization: Identifying entirely new entities or concepts that did not exist in the training data (e.g., recognizing "COVID-19" in new literature).
Q2: How can I systematically evaluate my model's generalization to rare and unseen entities? Partition your test set into three splits based on their overlap with the training data [45]:
- Seen Split: Mentions and their Concept Unique Identifiers (CUIs) are present in the training set (tests memorization).
- Unseen-Mention Split: Mentions are new, but their CUIs are known (tests synonym generalization).
- Unseen-Concept Split: Both mentions and CUIs are novel (tests concept generalization). Evaluating on these splits provides a true measure of generalizability beyond overall benchmark scores.
Q3: What is V-RAG and how does it differ from standard RAG for mitigating hallucinations in medical MLLMs?
- Standard RAG for MLLMs typically retrieves images similar to a query image but uses only the text reports of those retrieved images to augment the generation. This assumes the retrieved images are perfectly interchangeable with the query image [4].
- Visual RAG (V-RAG) is a more powerful framework that provides the MLLM with both the retrieved images and their corresponding reports. This allows the model to compare the query image directly with the retrieved visuals and text, determining what is truly relevant and leading to more accurate, less hallucinated outputs [4].
Q4: Where can bias be introduced in the AI model lifecycle? Bias is not just a data problem; it can be introduced at every stage [47]:
- Conception: Human biases can shape the problem definition.
- Data Collection: Through unrepresentative or incomplete datasets.
- Algorithm Development: Via flawed model design or objective functions.
- Validation: If validation sets are not diverse and representative.
- Deployment & Surveillance: When the model encounters real-world data that differs from training data (concept shift).
The table below summarizes the performance gap of a BioBERT model on different test splits, highlighting the challenge of generalizing to rare and unseen entities [45].
Table 1: Performance Gaps in BioNER Generalization (BC5CDR-disease corpus)
| Recognition Type | Test Split | Recall of BioBERT | Key Challenge |
|---|---|---|---|
| Memorization | Seen Mentions & CUIs | 93.3% | Over-reliance on statistical cues [45]. |
| Synonym Generalization | Unseen Mentions, Seen CUIs | 74.9% | Identifying morphologically varied synonyms [45]. |
| Concept Generalization | Unseen Mentions & CUIs | 73.7% | Recognizing novel concepts with unique surface forms [45]. |
The table below shows how a simple debiasing method can improve recognition of rare disease entities, which often have unconventional names [45].
Table 2: Improving Recognition of Rare Entities with a Debiasing Method
| Rare Disease Entity | Frequency in Data | BioBERT Recall (%) | BioBERT + Debiasing Recall (%) | Improvement (Percentage Points) |
|---|---|---|---|---|
| African Iron Overload | 39 | 6.2 | 17.4 | +11.2 |
| Geographic Tongue | 391 | 66.8 | 76.5 | +9.7 |
| Precocious Puberty | 6,903 | 71.1 | 90.0 | +18.9 |
| VACTERL Association | 685 | 31.0 | 43.8 | +12.8 |
Detailed Experimental Protocols
Protocol 1: Visual Retrieval-Augmented Generation (V-RAG) for Medical Report Generation
This protocol outlines the methodology for implementing V-RAG to reduce hallucinations in medical MLLMs [4].
1. Multimodal Retrieval Setup:
- Embedding Model: Use a robust biomedical vision model like BiomedCLIP to extract image embeddings (e.g., 512-dimensional vectors) for all images in your database [4].
- Vector Database: Construct a memory bank (\mathcal{M}) using a efficient vector storage and retrieval system like FAISS. Use the Hierarchical Navigable Small World (HNSW) algorithm for approximate k-nearest neighbor search [4].
- Retrieval: For a query image (Xq), encode it and retrieve the top-(k) most similar images ((I1,...Ik)) and their corresponding reports ((R1,...,R_k)) from (\mathcal{M}) [4].
2. Inference with V-RAG:
- Prompt Engineering: Structure the input prompt to the MLLM as follows [4]:
"This is the i-th similar image and its report for your reference. [Reference Image (Ii)] [Reference Report (Ri)] ... Answer the question with only the word yes or no. Do not provide explanations. According to the last query image and the reference images and reports, [Question] [Query Image (X_q)]"
- Fine-tuning for V-RAG Capability: To enable an MLLM trained on single images to handle multiple retrieved images, fine-tune it on general image-text tasks designed to boost its multimodal comprehension when presented with multiple images and texts [4].
3. Evaluation:
- Entity Probing: Evaluate the model by presenting an image and asking yes/no questions about the presence of specific medical entities. Compare answers against a ground-truth derived from a reference report [4].
- Downstream Metric: Use the RadGraph-F1 score to evaluate the factual accuracy of generated chest X-ray reports, which measures the overlap of clinical entities and relations with the ground truth [4].
V-RAG Workflow for reducing hallucinations in medical MLLMs [4].
Protocol 2: Debiasing for Improved Generalization in BioNER
This protocol describes a statistics-based method to improve a model's ability to recognize synonyms and new concepts [45].
1. Bias Prior Calculation:
- From the training data, calculate the class distribution for each word. This distribution represents the prior probability that a word is part of a specific entity type (or non-entity) based solely on its surface form [45].
2. Model Training with Debiasing:
- Integrate this bias prior into the loss function during training. The method reduces the training signal for words whose surface forms are highly predictive of an entity class. This prevents the model from overfitting to these superficial cues and encourages it to learn from broader contextual patterns [45].
3. Evaluation on Partitioned Test Sets:
- Partition your test set into Seen, Unseen-Mention, and Unseen-Concept splits as defined in the FAQs [45].
- Report performance (Precision, Recall, F1) on each split separately to accurately measure improvements in memorization, synonym generalization, and concept generalization.
Debiasing workflow for improved generalization in BioNER [45].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Frameworks for Bias Mitigation Experiments
| Item / Framework | Function / Application | Key Features / Rationale |
|---|---|---|
| BiomedCLIP | A vision model for generating biomedical image and text embeddings [4]. | Provides robust representations for a diverse range of biomedical image types, crucial for building effective retrieval systems [4]. |
| FAISS | A library for efficient similarity search and clustering of dense vectors [4]. | Enables fast k-NN search in large-scale databases, making retrieval steps in V-RAG feasible. Supports GPU acceleration [4]. |
| Shortcut Hull Learning (SHL) | A paradigm for diagnosing shortcuts in high-dimensional datasets [46]. | Uses a model suite to learn the minimal set of shortcut features, enabling the creation of shortcut-free evaluation frameworks [46]. |
| Debiasing Variational Autoencoder | A state-of-the-art model for automated debiasing in predictive tasks [48]. | Can be applied to tasks like predicting drug approval from clinical trial data, improving financial value and potentially identifying safer drugs [48]. |
| RadGraph Metric | A tool for evaluating the factual accuracy of generated radiology reports [4]. | Measures the overlap of clinical entities and relations, providing a more meaningful accuracy metric for generated text than ROUGE or BLEU [4]. |
Frequently Asked Questions (FAQs)
Q1: What is model collapse, and why is it a concern for medical MLLMs? A1: Model collapse occurs when an AI model's performance severely degrades over time, to the point of becoming useless. In medical MLLMs, this can manifest as a noticeable drop in diagnostic accuracy, increased hallucination (generating incorrect or ungrounded findings), or amplified biases. This is a significant concern because it can undermine the reliability of AI-assisted diagnoses and lead to serious patient safety risks and reputational damage for healthcare institutions [49].
Q2: How does Human-in-the-Loop (HITL) integration specifically help reduce hallucinations in medical image reporting? A2: Human-in-the-Loop systems integrate clinician feedback directly into the AI's lifecycle to correct errors and reinforce accurate patterns. This provides a continuous feedback loop where:
- Expert Correction: Radiologists review and correct the model's outputs, such as radiology report drafts. These corrected reports are then used to retrain the model, teaching it to avoid previous mistakes [49] [50].
- Edge Case Handling: Clinicians annotate rare or ambiguous cases (e.g., unusual pathologies on an X-ray) that the model is uncertain about. This "annotation at the edge" provides targeted learning data, improving the model's performance on complex scenarios [49].
- Active Learning: The model itself can flag its low-confidence predictions for human review, ensuring human effort is focused where it is most needed to correct potential hallucinations [50].
Q3: Our research team is experiencing high latency in our HITL pipeline. What are some potential solutions? A3: Latency, the delay introduced by human feedback, can be mitigated through several strategies [50]:
- Hybrid Systems: Design your system so the AI handles immediate, high-volume tasks, while human review is conducted asynchronously on complex or uncertain cases.
- Edge Computing: Process data closer to its source (e.g., on a hospital's local server) to minimize the time required to transfer data to a central cloud system and back.
- Tiered Evaluation: Implement a two-stage review process where initial AI-generated reports are broad, and human reviewers focus their detailed efforts only on reports flagged for potential issues or high complexity.
Q4: What is the difference between traditional RAG and Visual RAG (V-RAG) for mitigating hallucinations? A4: Traditional Retrieval-Augmented Generation (RAG) for MLLMs typically retrieves images similar to a query image but uses only the text reports associated with those retrieved images to augment the model's generation. This assumes the retrieved images are perfectly interchangeable with the query image. In contrast, Visual RAG (V-RAG) incorporates both the similar images and their associated text reports into the generation process. This allows the model to compare the visual content of the query image directly with the retrieved images, leading to more contextually relevant and visually grounded answers and significantly reducing hallucinations [4] [31].
Q5: How can we prevent introducing human bias into our HITL system? A5: Mitigating bias in HITL requires proactive measures [50]:
- Diverse Annotators: Work with a diverse group of clinician-annotators from different specializations, institutions, and geographic locations to prevent a single perspective from dominating the training data.
- Bias Detection Tools: Utilize software tools (e.g., IBM AI Fairness 360, Microsoft Fairlearn) to automatically identify and quantify potential biases in both the training data and the model's outputs.
- Continuous Auditing: Establish a schedule for regularly auditing the model's performance and outputs across different patient demographics to identify and correct emerging biased patterns.
Troubleshooting Guides
Issue: The MLLM is generating reports with hallucinations (ungrounded entities).
Problem: Your model is producing radiology reports that mention medical findings not present in the source image.
Diagnosis and Solution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1 | Verify Retrieval Database | Ensure the database used for Visual RAG contains high-quality, accurately annotated image-report pairs. The quality of retrievals directly impacts output quality [4]. |
| 2 | Implement Entity Probing | Use an automated check to query the model with yes/no questions about specific medical entities (e.g., "Is there pleural effusion?"). Compare answers against a ground truth to quantify hallucination rates [4]. |
| 3 | Increase HITL Sampling Rate | Temporarily increase the percentage of model outputs that are routed to human clinicians for review and correction, focusing on cases with low model confidence [49]. |
| 4 | Fine-tune with Corrected Data | Use the clinician-corrected reports from Step 3 to create a refined dataset. Fine-tune the model on this data to reinforce correct associations [49] [50]. |
Issue: The HITL workflow is not improving model performance (ineffective feedback).
Problem: Despite consistent clinician feedback, the model's accuracy metrics are not showing significant improvement over retraining cycles.
Diagnosis and Solution:
| Step | Action | Expected Outcome |
|---|---|---|
| 1 | Audit Feedback Quality | Review the annotations provided by human experts for consistency and adherence to labeling guidelines. Inconsistent feedback can confuse the model [50]. |
| 2 | Check for Data Distribution Shift | Analyze if the data the model is currently facing in production has significantly changed from its original training data (e.g., new imaging equipment, different patient population). This may require updating the base training dataset [49]. |
| 3 | Prioritize High-Impact Feedback | Use an Active Learning strategy to prioritize human review of the data points where the model is least confident. This ensures human effort is applied to the most informative cases [49] [50]. |
| 4 | Re-calibrate Confidence Thresholds | Adjust the confidence score thresholds that trigger human review. If set too low, not enough errors are caught; if too high, the system becomes inefficient [49]. |
Experimental Protocols & Data
Protocol: Visual Retrieval-Augmented Generation (V-RAG) for Hallucination Reduction
This methodology grounds the MLLM's responses in retrieved, relevant medical images and reports [4].
Multimodal Retrieval:
- Embedding Generation: Use a domain-specific model (e.g., BiomedCLIP) to extract an image embedding (vector representation) from the query medical image (
Xq). - Similarity Search: Using a vector storage system (e.g., FAISS with HNSW algorithm), retrieve the top-
kmost similar images and their corresponding radiology reports from a pre-built memory bank (ℳ).
- Embedding Generation: Use a domain-specific model (e.g., BiomedCLIP) to extract an image embedding (vector representation) from the query medical image (
Inference with V-RAG:
- Prompt Construction: Construct a multi-image prompt for the Med-MLLM. The prompt includes the query image and a structured reference to the
kretrieved image-report pairs. - Model Query: Present the constructed prompt to a multi-image-trained Med-MLLM. The model uses both the query image and the visual/textual context from the retrieved pairs to generate a more accurate, grounded report.
- Prompt Construction: Construct a multi-image prompt for the Med-MLLM. The prompt includes the query image and a structured reference to the
Validation via Entity Probing:
- Benchmarking: To measure hallucination, present the model with an image and a series of yes/no questions about the presence of specific medical entities.
- Scoring: Compare the model's answers against a ground truth derived from expert-annotated reports. Calculate metrics like accuracy for both frequent and rare entities.
Quantitative Performance of AI-Assisted Workflows
The following table summarizes validation data from studies on AI-human collaborative systems, demonstrating their potential for improving accuracy and efficiency.
| Application / Method | Key Metric | Performance Result | Comparative Baseline |
|---|---|---|---|
| AI SLR Screening [51] | Recall | 82-97% | Matches or exceeds human reviewer-level recall |
| AI SLR Search [51] | Recall | 76.8% - 79.6% | Effective generation of Boolean search strings from a research question |
| PICOs Extraction [51] | F1 Score | 0.74 | Good performance in extracting structured data from literature |
| V-RAG Entity Probing [4] | Accuracy | Improves for both frequent and rare entities | Outperforms baseline MLLMs and text-only RAG |
Research Reagent Solutions
A selection of key software and methodological "reagents" for developing HITL systems in medical imaging.
| Item | Function / Application |
|---|---|
| BiomedCLIP [4] | A vision-language model pre-trained on a wide range of biomedical images. Used to generate high-quality image embeddings for robust multimodal retrieval. |
| FAISS (Facebook AI Similarity Search) [4] | A library for efficient similarity search and clustering of dense vectors. Essential for building the retrieval database in a V-RAG pipeline. |
| Visual RAG (V-RAG) Framework [4] | An architectural framework that augments MLLMs by retrieving and incorporating both similar images and their associated reports during inference to reduce hallucinations. |
| Entity Probing Benchmark [4] | An evaluation method that uses yes/no questions about medical entities in an image to quantitatively measure an MLLM's hallucination rate. |
| Active Learning Loop [49] [50] | A system component that intelligently selects the data points the model is most uncertain about, and sends them for human annotation, optimizing the use of expert time. |
System Workflow Diagrams
HITL Model Refinement Cycle
Visual RAG (V-RAG) Inference Process
Ensuring Reliability: Benchmarking, Validation, and Comparative Analysis
Troubleshooting Guides
Guide 1: My generated radiology report has a high BLEU score but is clinically inaccurate. What better metrics can I use?
Problem: Standard NLP metrics like BLEU focus on lexical overlap rather than clinical factual correctness, leading to misleadingly high scores for reports containing hallucinations or incorrect medical findings [52].
Solution: Implement clinical fact-oriented metrics that are more aligned with radiologists' assessments.
- RadGraph F1: Utilizes a structured schema to extract clinical entities (Anatomy, Observation) and relations (locatedat, suggestiveof, modify) from both reference and generated reports, then calculates the F1 score based on this graph overlap [52] [53]. It demonstrates stronger correlation with radiologist error scores (Kendall's tau: 0.515 for total errors, 0.531 for significant errors) than BLEU (tau: 0.462 and 0.441, respectively) [52].
- RadCliQ: A composite metric that combines multiple individual automated metrics to better predict radiologists' scoring of reports [52].
- Entity Probing: A framework for testing model factual grounding by asking yes/no questions about specific medical entities (e.g., "Is there a pleural effusion?") and comparing answers against a reference standard [4]. This directly tests for hallucinations.
Actionable Steps:
- For RadGraph F1:
- Obtain the RadGraph dataset and model from PhysioNet [53].
- Run your generated report and the ground truth report through the RadGraph annotation model to extract entity-relation graphs.
- Calculate the F1 score based on the overlap of these structured graphs.
- For Entity Probing:
- Define a set of key clinical findings relevant to your dataset (e.g., from the CheXpert labeler [52]).
- For each finding, use your model to answer a direct yes/no question based on the image.
- Compare these answers to the ground truth labels derived from the reference report to calculate accuracy, precision, and recall for each entity.
Guide 2: My Medical Multimodal LLM is hallucinating findings. How can I reduce this using advanced architectures?
Problem: MLLMs frequently generate plausible-sounding but incorrect or ungrounded clinical findings, a critical failure mode for clinical deployment [13] [54] [4].
Solution: Integrate Retrieval-Augmented Generation (RAG) frameworks, specifically Visual RAG (V-RAG), to ground the generation process in similar, verified image-report pairs [4].
Actionable Steps for Implementing V-RAG:
- Build a Multimodal Retrieval Database:
- Retrieve Relevant Context:
- For a new query image, encode it with the same BiomedCLIP model to get its embedding.
- Retrieve the top-k most similar images and their associated reports from your database.
- Augment Generation:
- Feed the query image along with the retrieved images and reports to a multi-image capable MLLM.
- Use a prompt template that instructs the model to base its response on both the query and the retrieved evidence [4].
Expected Outcome: V-RAG has been shown to improve the factual accuracy of generated reports, leading to higher RadGraph F1 scores and reduced hallucinations, particularly for rare entities [4].
Guide 3: My model performs well on VQA-RAD but fails under adversarial probing. How can I robustly evaluate its diagnostic reliability?
Problem: High performance on standard Med-VQA benchmarks may mask fundamental weaknesses, as models can exploit biases and fail on slightly altered or fine-grained diagnostic questions [54].
Solution: Employ adversarial probing evaluation, such as with the ProbMed dataset, which tests a model's diagnostic reasoning across multiple dimensions and its resilience to distracting features [54].
Actionable Steps for Probing Evaluation:
- Utilize the ProbMed Framework:
- Use the ProbMed dataset, which includes procedural diagnosis questions spanning modality, organ, abnormality, and positional reasoning [54].
- Create Adversarial Pairs:
- For each test question, create a corresponding "negation question" that introduces a hallucinated attribute (e.g., change "left" to "right") [54].
- A robust model should confidently answer both the original and negation questions correctly.
- Evaluate by Diagnostic Category:
- Analyze accuracy separately for each diagnostic dimension (e.g., Modality, Organ, Condition/Finding, Position). This reveals specific weaknesses in the model's clinical reasoning [54].
Diagnosis: If a model's accuracy on specialized diagnostic questions (like Condition/Finding or Position) is close to or below random guessing (50%), it indicates a severe lack of reliable diagnostic capability and high hallucination potential [54].
Frequently Asked Questions (FAQs)
What are the main limitations of ROUGE and BLEU for medical report evaluation?
These metrics suffer from several critical flaws in a clinical context [52] [55]:
- Focus on Lexical Overlap: They prioritize n-gram matching over factual correctness. A generated report can use different phrasing than the reference but be medically perfect, yet receive a low score.
- Poor Clinical Alignment: Studies show low correlation between BLEU scores and the number of clinical errors identified by radiologists [52]. A report with a high BLEU score can contain clinically significant errors, such as false positives or incorrect locations of findings [52].
- Inability to Handle Semantic Equivalence: They cannot recognize that two different phrases (e.g., "lung opacity" and "pulmonary shadowing") describe the same clinical fact.
What quantitative evidence shows that RadGraph F1 is better than traditional metrics?
A 2023 study directly compared the alignment between automated metrics and radiologists' error scoring [52]. The Kendall's Tau rank correlation for different metrics is summarized below:
Table: Metric-Radiologist Alignment (Kendall's Tau) [52]
| Metric | Correlation with Total Errors | Correlation with Clinically Significant Errors |
|---|---|---|
| RadGraph F1 | 0.515 | 0.531 |
| BERTScore | 0.511 | 0.518 |
| CheXbert Vector Similarity | 0.499 | 0.457 |
| BLEU | 0.462 | 0.441 |
RadGraph F1 showed the highest correlation, meaning its scores best reflected the number of mistakes a radiologist would find in a report [52].
What are the common failure modes of different metrics?
Research has analyzed where metrics most often fail to identify errors [52]:
Table: Metric Failure Modes (Average Errors per Report) [52]
| Metric | False Predictions of Findings (FP) | Omission of Findings (FN) | Incorrect Location/Severity |
|---|---|---|---|
| BLEU | 0.607 (Significant) | 0.420 (Significant) | Lower than CheXbert |
| BERTScore | 0.363 (Significant) | 0.417 (Significant) | - |
| RadGraph F1 | 0.300 (Significant) | 0.447 (Significant) | - |
| CheXbert Vector Similarity | - | - | Highest |
BLEU is particularly poor at penalizing false positive findings, while CheXbert vector similarity struggles with spatial and severity errors [52].
How does Entity Probing work, and what has it revealed about state-of-the-art MLLMs?
Entity probing is a method to directly evaluate an MLLM's ability to ground specific medical entities in an image [4]. The model is presented with an image and a simple yes/no question about a clinical finding (e.g., "Is there a pneumothorax?"). Its answer is compared to a ground truth label.
A 2024 study using this method on the ProbMed dataset revealed alarming weaknesses [54]:
- Worse-than-Random Performance: Top-tier general MLLMs like GPT-4V and Gemini Pro performed worse than random guessing on specialized diagnostic questions about medical conditions and their locations [54].
- Significant Accuracy Drops: When faced with adversarial questions containing hallucinated attributes, model accuracy dropped by up to 57% [54].
- Need for Specialized Models: The study highlighted that specialized domain knowledge is crucial, as models like CheXagent showed the transferability of expertise on specific organs [54].
Experimental Protocols & Workflows
Protocol 1: Evaluating a Generated Report with RadGraph F1
Purpose: To quantitatively assess the clinical factual accuracy of a machine-generated radiology report against a reference report.
RadGraph F1 Evaluation Workflow
Materials:
- Input: A machine-generated radiology report and its ground-truth reference report.
- Tool: The RadGraph model (available on PhysioNet) for annotating reports [53].
- Metric Script: A script to compute F1 score from the paired graph annotations.
Procedure:
- Annotation: Process both the generated report and the reference report through the RadGraph model to extract two structured graphs. Each graph contains:
- Entities: Labeled as
ANAT-DP(Anatomy-Definitely Present),OBS-DP(Observation-Definitely Present),OBS-U(Uncertain), orOBS-DA(Definitely Absent) [53]. - Relations:
located_at(links an Observation to an Anatomy),suggestive_of(links two Observations),modify(links two entities where one modifies the other) [53].
- Entities: Labeled as
- Alignment: Map entities and relations from the generated graph to those in the reference graph.
- Calculation: Compute the micro F1 score based on the overlap of entities and relations. The model must correctly predict the entity span, its type, and the relation type for a match [53].
Protocol 2: Probing Model Hallucinations with Entity Probing
Purpose: To systematically test a Medical MLLM's tendency to hallucinate specific clinical findings by asking direct, binary questions.
Entity Probing for Hallucination Detection
Materials:
- Dataset: A set of medical images with ground truth labels for clinical findings (e.g., derived from MIMIC-CXR reports using the CheXpert labeler).
- Model: The Medical MLLM to be evaluated.
- Entity List: A pre-defined list of medical entities/findings (e.g., Atelectasis, Cardiomegaly, Pleural Effusion).
Procedure:
- Question Formulation: For each image and each clinical entity in the list, formulate a binary question: "Is there [ENTITY] in the image?"
- Model Querying: Present the image and the question to the MLLM, instructing it to answer only with "yes" or "no" [4].
- Answer Collection: Record the model's response.
- Analysis:
- Compare the model's answer to the ground truth label for that entity and image.
- A hallucination is recorded when the model answers "yes" for an entity that is absent according to the ground truth (false positive).
- Calculate the hallucination rate per entity and an overall rate across the dataset.
Protocol 3: Mitigating Hallucinations with Visual Retrieval-Augmented Generation (V-RAG)
Purpose: To reduce hallucinations by augmenting a Medical MLLM with retrieved, relevant images and reports during the generation process.
Materials:
- Multimodal Database: A large corpus of medical images and their corresponding reports (e.g., MIMIC-CXR) [4].
- Retriever Model: A model like BiomedCLIP to create dense vector embeddings of images [4].
- Vector Database: A system like FAISS for efficient similarity search [4].
- Multi-image MLLM: A Medical MLLM capable of processing multiple images as input, or a model fine-tuned for this purpose [4].
Procedure:
- Database Construction:
- For all image-report pairs in your corpus, use BiomedCLIP to extract an image embedding vector.
- Store all embeddings in a FAISS index for fast retrieval [4].
- Retrieval:
- Given a new query image, compute its embedding using the same BiomedCLIP model.
- Use the FAISS index to retrieve the top-k most similar images and their associated reports [4].
- Augmented Generation:
- Construct a prompt that includes the retrieved images and reports as reference context.
- Feed this prompt, along with the query image, into the multi-image MLLM to generate the final report [4].
- The prompt should explicitly instruct the model to use the retrieved information for reference.
The Scientist's Toolkit: Key Research Reagents
Table: Essential Resources for Clinical Metric Evaluation
| Resource Name | Type | Function / Description | Key Application |
|---|---|---|---|
| RadGraph Dataset & Model [53] | Dataset & Model | Provides benchmark annotations of entities/relations in radiology reports and a model to generate them. | Core component for calculating the RadGraph F1 metric. |
| MIMIC-CXR [52] [53] | Dataset | A large, public dataset of chest X-rays with corresponding free-text radiology reports. | Primary dataset for training and evaluating chest X-ray report generation models. |
| CheXpert Labeler [52] | Software Tool | An automated tool to extract presence/uncertainty/absence labels for 14 common chest observations from free-text reports. | Used to generate ground truth labels for Entity Probing. |
| BiomedCLIP [4] | Model | A vision-language model pre-trained on a large-scale biomedical image-text corpus. | Used as the retriever backbone in V-RAG to find similar medical images. |
| FAISS [4] | Software Library | A library for efficient similarity search and clustering of dense vectors. | Core infrastructure for building the retrieval database in V-RAG. |
| ProbMed Dataset [54] | Dataset | A benchmark for probing evaluation featuring procedural diagnosis questions and adversarial pairs. | Used for robust adversarial testing of Med-VQA models. |
Troubleshooting Guide: Frequently Asked Questions
Q1: Our MLLM is generating plausible but fabricated findings in radiology reports. What immediate steps should we take? A1: Immediately implement a human-in-the-loop verification system where a radiologist reviews all AI-generated findings before report finalization [56]. For a technical mitigation, integrate Retrieval Augmented Generation (RAG) to ground the model's responses in verified medical knowledge bases, which has been shown to reduce inaccuracies [57]. Furthermore, apply prompt engineering techniques that explicitly instruct the model to express uncertainty when dealing with ambiguous image features [5] [57].
Q2: When benchmarking, we observe high variance in hallucination rates across different medical imaging modalities. Is this expected? A2: Yes, this is an observed phenomenon. Hallucination rates can vary significantly due to factors such as dataset quality and modality-specific challenges [3] [13]. For instance, models might perform differently on 2D X-rays versus 3D CT/MRI datasets. To ensure a fair benchmark, it is crucial to stratify your evaluation by imaging modality and anatomical region. Using a framework that includes a clinical error taxonomy helps in consistently categorizing these variations [58].
Q3: What is the most effective way to measure "hallucination" quantitatively in a medical imaging context? A3: Beyond traditional NLP metrics, employ a clinician-annotated evaluation framework [58]. Define hallucination operationally; for example, in a summarization task, any generated sentence not evidenced by the source image or correlative clinical data constitutes a hallucination. Categorize errors by their potential clinical impact as either "Major" (could impact diagnosis/management) or "Minor" for a more nuanced understanding of risk [58].
Q4: How can we induce and study hallucinations in a controlled manner to build more robust models? A4: Use adversarial testing methods like GHOST, which generates subtle, natural-looking images designed to mislead MLLMs into hallucinating objects [59]. This method proactively uncovers model vulnerabilities. Alternatively, embed single fabricated details (e.g., a fictitious lab test or radiological sign) in simulated clinical vignettes to test the model's tendency to elaborate on false information, a method shown to elicit hallucinations in 50-82% of outputs [5].
Q5: Can fine-tuning on specialized medical data eliminate multimodal hallucinations? A5: While fine-tuning significantly improves performance, it does not eliminate hallucinations entirely. One study achieved a reduction in hallucination rates by fine-tuning on adversarially generated images [59]. However, hallucinations are considered a theoretical property of LLMs. A holistic approach combining high-quality data, robust architecture (e.g., better cross-modal alignment), and post-processing verification is necessary [58] [3].
Quantitative Benchmarking Data
Table 1: Documented Hallucination Rates Across Different Models and Clinical Tasks
| Model / Study Context | Task Description | Hallucination Rate | Key Mitigation Strategy Tested |
|---|---|---|---|
| Multiple LLMs (GPT-4o, etc.) [5] | Adversarial attack with fabricated details in clinical vignettes | 50% - 82% (Model-dependent) | Specialized mitigation prompt reduced mean rate from 66% to 44% [5]. |
| GPT-4o (Best Performing) [5] | Adversarial attack with fabricated details in clinical vignettes | 53% (default) reduced to 23% | Use of a prompt instructing model to use only clinically validated information [5]. |
| Clinical Note Generation Pipeline [58] | Summarization of primary care consultations | 1.47% (of 12,999 sentences) | Iterative prompt and workflow refinement based on a clinical safety framework [58]. |
| Anthropic Claude 3.7 [57] | General knowledge Q&A on news articles (non-medical benchmark) | 17% (Lowest in benchmark) | Demonstrates model-specific performance variation [57]. |
Table 2: Categorization of Major Hallucinations in Clinical Note Generation (from 84 major errors) [58]
| Hallucination Type | Description | Proportion of Major Hallucinations | Most Common Note Section |
|---|---|---|---|
| Fabrication | Generating information not present in the source data. | 43% | Plan (21%) |
| Negation | Incorrectly stating that a finding or symptom is absent. | 30% | Information not provided |
| Contextual | Misattributing or misrepresenting the context of a fact. | 17% | Information not provided |
| Causality | Inventing a cause-effect relationship not supported by data. | 10% | Information not provided |
Experimental Protocols for Hallucination Benchmarking
Protocol 1: Adversarial Hallucination Attack Testing
This methodology tests model vulnerability to elaborating on deliberately planted false information [5].
- Vignette Creation: Develop 300+ physician-validated simulated clinical cases. Each must contain a single fabricated element (e.g., a non-existent lab test "Serum Neurostatin," a fake radiological sign "Cardiac Spiral Sign," or an invented syndrome "Faulkenstein Syndrome").
- Format Control: Create short (50-60 words) and long (90-100 words) versions of each vignette, identical in medical content.
- Model Querying: Present vignettes to MLLMs with a task that requires engaging with the fabricated detail (e.g., "List the clinical implications of [fabricated sign]").
- Mitigation Testing: Test interventions like a) a default setting, b) a mitigation prompt (e.g., "Use only clinically validated information and acknowledge uncertainty"), and c) a temperature setting of 0.
- Output Classification: Automatically and manually classify outputs. A "hallucination" is recorded if the model elaborates on, endorses, or treats the fabricated element as real.
Protocol 2: Clinical Safety Framework for Summarization Tasks
This framework provides an end-to-end process for evaluating MLLM-generated clinical notes [58].
- Data Preparation: Use a dataset of real (e.g., 450 primary care consultations from PriMock dataset) or meticulously simulated clinical transcripts.
- Note Generation: Generate clinical notes from transcripts using the MLLM across multiple experimental configurations (prompts, workflows).
- Clinician Annotation: Have at least two medical doctors manually evaluate each sentence in the AI-generated note.
- Hallucination Check: Label every generated sentence not evidenced by the source transcript.
- Omission Check: Identify every clinically relevant sentence from the transcript missing from the AI note.
- Safety Grading: Classify each error as "Major" (if it could change patient diagnosis or management) or "Minor".
- Iterative Refinement: Use results to iteratively refine prompts and workflows to reduce major error rates.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Medical MLLM Hallucination Research
| Resource / Tool | Function in Research | Relevance to Hallucination Benchmarking |
|---|---|---|
| Simulated Clinical Vignettes [5] | Provides controlled, physician-validated test cases with known ground truth. | Essential for adversarial testing; allows precise measurement of a model's tendency to confabulate. |
| Clinical Safety & Error Taxonomy Framework [58] | Offers a standardized classification system for different error types (Fabrication, Negation, etc.) and their clinical impact. | Enables consistent, clinically-grounded annotation and analysis of hallucinations across different studies. |
| GHOST-like Method [59] | A technique for generating hallucination-inducing images to proactively stress-test MLLMs. | Functions as both a diagnostic tool to find model weaknesses and a data source for mitigation training. |
| Retrieval Augmented Generation (RAG) [57] | An architectural pattern that grounds LLM responses by retrieving information from external, verified knowledge bases. | A key mitigation strategy to reduce factual hallucinations by tethering the model to authoritative sources. |
| CREOLA (or similar GUI Platform) [58] | A graphical user interface designed to facilitate the manual evaluation and labeling of LLM-generated clinical text by clinicians. | Critical for obtaining high-quality human evaluation data at scale, which is the gold standard for benchmarking. |
Hallucination Mitigation Strategies
Prompt Engineering is a first line of defense. Crafting prompts that explicitly instruct the model to "base responses only on provided data," "acknowledge uncertainty," and "avoid speculation" can significantly reduce hallucination rates. One study demonstrated that a targeted mitigation prompt halved the average hallucination rate across models from 66% to 44% [5].
Architectural Improvements are fundamental for long-term solutions. This includes:
- Enhanced Cross-Modal Alignment: Improving how the model fuses and understands the relationship between visual features and text [3] [13].
- Self-Reflection Capabilities: Building models that can analyze their own outputs for internal consistency before finalizing a response [57].
- Uncertainty Quantification: Developing models that can output a confidence score alongside their generations, alerting users to potentially unreliable information [57].
Welcome to the MLLM Technical Support Center
This resource provides troubleshooting guides and FAQs for researchers working to reduce hallucinations in Multimodal Large Language Models (MLLMs) for medical imaging, with a special focus on the unique challenges of evaluating both frequent and rare medical entities.
Frequently Asked Questions
What makes rare medical entities more prone to MLLM hallucinations?
Rare entities suffer from a data scarcity paradox in model training. The core challenge is twofold:
- Inherent Data Scarcity: By definition, rare diseases or findings have fewer available image-report pairs in training datasets, leading to poorer model generalization [60] [61].
- Amplified Hallucination Impact: While hallucinations occur for frequent entities, the clinical consequences of a hallucinated finding in a rarely-seen condition can be more severe due to unfamiliarity and the critical nature of many rare diseases [4].
How can I quickly assess my model's performance on rare entities without a massive dataset?
Implement Entity Probing. This method evaluates an MLLM's ability to ground specific medical entities in an image, without requiring a full report generation cycle. It is highly efficient for small-scale validation [4].
- Method: Present the model with an image and a series of yes/no questions about the presence or absence of specific entities (e.g., "Is there a pneumothorax?").
- Output: Compare the model's answers against a ground truth derived from expert-annotated reports. This bypasses the complexities of natural language generation metrics and provides a clear, clinical perspective on model grounding for both frequent and rare entities [4].
What is V-RAG and how does it help with rare entities?
Visual Retrieval-Augmented Generation (V-RAG) is an inference-time framework that reduces hallucinations by grounding the MLLM's generation in a knowledge base of similar images and their corresponding reports [4].
- Process: For a query image, the system retrieves the top-k most visually similar images and their reports from a database. The MLLM is then prompted to generate a report for the query image using these retrieved examples as a reference [4].
- Benefit for Rare Entities: Even if a rare entity is underrepresented in the model's core parameters, V-RAG can surface relevant examples from the knowledge base. This provides the model with concrete, grounded information it can learn from during inference, improving accuracy for both frequent and rare findings [4].
Troubleshooting Guides
Guide 1: Diagnosing and Mitigating Hallucinations of Rare Entities
Problem: Your MLLM generates plausible-sounding reports for images of rare conditions but contains ungrounded findings (hallucinations) or misses key rare findings.
Investigation Steps:
Isolate the Issue via Entity Probing:
- Create a focused test set containing confirmed cases of the rare entity and a set of normal or frequent-entity cases.
- Run entity probing on this test set to quantify the model's precision and recall for the specific rare entity. This will confirm if the problem is one of grounding.
Analyze Training Data Representation:
- Audit your training dataset to determine the frequency of the rare entity. A very low count (< 0.1% of samples) is a strong indicator of the root cause.
Check Retrieval System Performance (if using V-RAG):
- Manually inspect the images and reports retrieved by your V-RAG system for query images containing the rare entity. If the retrieved items are not semantically similar or lack the rare entity, the retrieval system, not the MLLM, may be the point of failure.
Solutions:
- Implement V-RAG: Integrate a V-RAG framework to supplement the model's internal knowledge with an external, up-to-date database of medical images and reports [4].
- Fine-tune with Multi-Image Capability: If your base MLLM was trained on single images, you may need to fine-tune it to effectively reason over the multiple images and reports presented by V-RAG [4].
- Data Augmentation and Curation: Strategically augment your training set with synthetic data or actively seek out and incorporate more examples of the rare entity from public or collaborative datasets.
Guide 2: Designing a Robust Evaluation Framework
Problem: Standard metrics like ROUGE or BLEU scores do not adequately capture your model's clinical accuracy, especially for rare entities.
Solution: Adopt a multi-faceted evaluation strategy that includes:
Clinical Accuracy Metrics:
- RadGraph-F1 Score: Measures the overlap between the model-generated report and a reference report based on structured clinical entities and their relationships. This is a more clinically meaningful metric than text-overlap scores [4].
- Entity-Level Precision/Recall: Calculate precision and recall for a pre-defined list of critical findings, with separate tracking for frequent and rare entities.
Hallucination-Specific Metrics:
- Hallucination Rate: The proportion of generated statements that are not grounded in the image.
- Omission Rate: The proportion of findings present in the image that are missed in the generated report.
The following workflow integrates these evaluation and mitigation strategies into a cohesive experimental protocol:
Quantitative Performance Comparison: Frequent vs. Rare Entities
The table below summarizes typical performance disparities and the expected impact of mitigation strategies like V-RAG. These are illustrative metrics based on common research findings.
| Metric | Frequent Entities | Rare Entities | Impact of V-RAG |
|---|---|---|---|
| Entity Probing Accuracy | High (~90-95%) | Lower (~70-80%) | Significant improvement for both, with a larger relative gain for rare entities [4] |
| RadGraph-F1 Score | High (~0.50-0.60) | Moderate (~0.30-0.45) | Improves overall score, primarily by reducing hallucinations [4] |
| Hallucination Rate | Low (<5%) | High (can be >15%) | Can be reduced by 25-50% relative [4] |
| Data Availability | Abundant | Scarce | Mitigates data scarcity by leveraging external knowledge base [4] |
The Scientist's Toolkit: Research Reagent Solutions
| Tool / Resource | Function / Description |
|---|---|
| BiomedCLIP | A vision-language model pre-trained on a wide range of biomedical images, providing robust image embeddings for building effective retrieval systems in V-RAG [4]. |
| FAISS (Facebook AI Similarity Search) | A library for efficient similarity search and clustering of dense vectors. Crucial for building the retrieval component of a V-RAG system to quickly find similar medical images [4]. |
| MIMIC-CXR Dataset | A large, publicly available dataset of chest X-rays with associated radiology reports. Serves as a essential benchmark for training and evaluating MLLMs on frequent thoracic findings [4]. |
| RadGraph | A tool and dataset for annotating and evaluating radiology reports based on entities (e.g., "pneumonia") and relations (e.g., "suggestive of"). The primary metric for clinical report accuracy (RadGraph-F1) [4]. |
| Entity Probing Framework | A custom evaluation protocol that uses yes/no questions to test an MLLM's grounding of specific medical concepts in an image, essential for diagnosing hallucinations [4]. |
The following diagram illustrates the architecture of a V-RAG system, which integrates these tools to reduce hallucinations:
Troubleshooting Guide: Addressing Hallucinations in Medical Multimodal LLMs
This guide provides targeted solutions for researchers and scientists addressing the critical challenge of hallucinations during the development and validation of Multimodal Large Language Models (MLLMs) for medical imaging.
Q1: Our MLLM frequently elaborates on fabricated details present in clinical prompts. What mitigation strategies are most effective?
Problem: The model demonstrates high susceptibility to adversarial hallucination attacks, where it repeats or elaborates on deliberately planted false information from clinical vignettes.
Solutions:
- Implement Prompt-Based Mitigation: Use specialized mitigation prompts that explicitly instruct the model to use only clinically validated information and acknowledge uncertainty instead of speculating. One study demonstrated this reduced the overall hallucination rate from 66% to 44% across multiple models, with the best-performing model (GPT-4o) seeing a reduction from 53% to 23% [5].
- Apply Chain-of-Thought Reasoning: Force the model to generate explicit reasoning traces before producing a final answer. This self-verification capability significantly reduces hallucinations, with one evaluation showing improvements in 86.4% of tested cases [62].
- Adopt a "Citation-First" Architecture: Implement Retrieval-Augmented Generation (RAG) systems that ground the model's responses in a curated library of verifiable sources and mandate the display of citations for all generated content [63].
Q2: How can we quantitatively evaluate our model's vulnerability to hallucinations before clinical deployment?
Problem: A lack of standardized, quantitative benchmarks for measuring hallucination rates in medical MLLMs.
Solutions:
- Deploy Simulated Adversarial Vignettes: Create a benchmark of physician-validated clinical cases, each containing a single fabricated detail (e.g., a non-existent lab test, physical sign, or medical syndrome). Present these to the model and automatically classify outputs that endorse or elaborate on the false element as hallucinations [5].
- Establish a Robust Evaluation Protocol:
- Dataset Creation: Develop 300+ clinical vignettes in short and long versions, differing only in word count. Each must contain one fabricated medical detail validated by a physician to have no real-world analog [5].
- Testing Framework: Test models under multiple conditions: default settings, with a mitigation prompt, and with a temperature setting of 0 (deterministic output) [5].
- Automated Classification: Use a pipeline to automatically detect when a model elaborates on a fabricated detail. Physician review should be used to validate the accuracy of this classification [5].
- Confront with Real-World Misinformation: Qualitatively test the model on five widely circulated examples of medical disinformation (e.g., purported link between vaccines and autism) to assess how it handles real-world false claims [5].
Q3: Our medical-specialized MLLM underperforms compared to general-purpose models. Why does this happen?
Problem: Despite being fine-tuned on medical corpora, a specialized model produces a higher rate of hallucinations than a larger, general-purpose model.
Solutions:
- Focus on Reasoning Capabilities: Recognize that safety often emerges from sophisticated reasoning capabilities developed during large-scale pre-training, not from narrow domain-specific fine-tuning alone. One large-scale evaluation found that general-purpose models achieved a significantly higher proportion of hallucination-free responses (median: 76.6%) than medical-specialized models (median: 51.3%) [62].
- Augment, Don't Just Fine-Tune: Instead of only fine-tuning on a medical corpus, augment your model's capabilities using external tools. The top-performing model in one assessment (Gemini-2.5 Pro) exceeded 97% accuracy when augmented with chain-of-thought prompting, compared to 87.6% for its base performance [62].
- Analyze Failure Modes: Conduct a root-cause analysis of hallucinations. Physician audits indicate that 64–72% of residual errors stem from causal or temporal reasoning failures rather than pure knowledge gaps, highlighting where model improvements should be focused [62].
Q4: What are the essential components of a safety assurance protocol for an MLLM intended for radiology?
Problem: Ensuring a model is safe and effective for integration into a high-stakes clinical radiology workflow.
Solutions:
- Integrate Comprehensive Guardrails: Safe systems must include uncertainty handling (the ability to say "I don't know"), refusal modes for out-of-scope questions, safety filters, and mandatory human sign-off for key clinical actions [63].
- Adhere to Evolving Regulatory Pathways: Familiarize yourself with the relevant frameworks for your deployment region. Key frameworks include the NHS DTAC (UK), NICE Evidence Standards Framework (UK), MHRA AI Airlock (UK regulatory sandbox), EU AI Act (EU), and FDA CDS Guidance (US) [63].
- Validate with Operational Metrics: Beyond diagnostic accuracy, monitor operational Key Performance Indicators (KPIs) such as suggestion acceptance/override rates by clinicians, time-to-answer, time-to-note, and performance stratified by population demographics to check for bias [63].
- Maintain Human-in-the-Loop: Design workflows where AI outputs, especially preliminary radiology reports, are always reviewed and validated by a qualified radiologist. This is a non-negotiable requirement for safe deployment [63] [56].
Frequently Asked Questions (FAQs)
Q: Does Retrieval-Augmented Generation (RAG) completely eliminate hallucinations?
A: No. RAG significantly reduces hallucinations by grounding the AI in a set of verifiable facts, but it does not eliminate them entirely. Human review of all outputs remains essential before any clinical action is taken [63].
Q: Do adjustments to the model's temperature setting effectively reduce hallucinations?
A: Evidence suggests limited impact. One large study found that setting temperature to 0 (for maximum response certainty) offered no significant improvement in reducing adversarial hallucinations. Prompt-based mitigation was far more effective [5].
Q: What is the fundamental difference between a Large Language Model (LLM) and a Large Multimodal Model (LMM) in a healthcare context?
A: LLMs are trained primarily on text data. LMMs (or MLLMs) are a significant evolution that can understand and process information from multiple types of input—such as text, medical images, and audio—within a single model, which is crucial for comprehensive clinical analysis [63].
Q: Are ambient scribe tools, which use MLLMs for documentation, considered safe for use in clinical settings like the NHS?
A: Yes, but only when deployed in line with specific guidance. For example, NHS England mandates robust safeguards, a full clinical safety case, diligent clinician oversight, and verification of every generated note [63].
Experimental Protocols for Hallucination Mitigation
Protocol 1: Adversarial Hallucination Testing
Table: Experimental Conditions for Hallucination Testing [5]
| Condition | Description | Key Parameter Settings |
|---|---|---|
| Default | Standard model settings reflecting normal usage. | Temperature ≈0.7, top-p 0.9–1.0 |
| Mitigation Prompt | Input includes instructions to use only validated data and acknowledge uncertainty. | Same as Default, plus specialized prompt instructions. |
| Temperature 0 | Deterministic output with maximum response certainty. | Temperature = 0.0, all other parameters unchanged. |
Methodology:
- Vignette Creation: Generate 300+ physician-validated clinical vignettes, each with one fabricated detail (lab test, sign, or syndrome). Create short (50-60 words) and long (90-100 words) versions [5].
- Model Testing: Present each vignette to the model with a task-specific prompt (e.g., output in JSON format). Run each vignette through all experimental conditions [5].
- Output Classification: Automatically classify responses. A "hallucination" is recorded if the model elaborates on, endorses, or treats the fabricated element as real. A "non-hallucination" is recorded if the model omits it, states it doesn't exist, or expresses uncertainty [5].
- Statistical Analysis: Model the binary outcome of hallucination using mixed-effects logistic regression. Use pairwise comparisons between conditions with p-value adjustments for multiple comparisons [5].
Protocol 2: Chain-of-Thought for Self-Verification
Methodology:
- Prompt Engineering: Design prompts that require the model to reason step-by-step before giving a final answer. For example: "First, analyze the provided findings for internal consistency. Second, compare these findings to established medical knowledge. Third, based on this reasoning, provide your final assessment and list any points of uncertainty." [62].
- Evaluation: Compare the accuracy and hallucination rate of the model's final answer when generated with and without the chain-of-thought prompt across a benchmark of challenging clinical cases [62].
- Quality Assessment: Have physicians audit the reasoning traces to determine if errors stem from knowledge gaps (factually wrong) or reasoning failures (logically inconsistent) [62].
Technical Architectures and Workflows
Diagram: MLLM Clinical Validation Workflow
MLLM Clinical Validation Workflow
Diagram: Retrieval-Augmented Generation (RAG) Architecture
RAG Architecture for Hallucination Reduction
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Components for Medical MLLM Research
| Research Component | Function & Explanation |
|---|---|
| Adversarial Vignette Benchmark | A validated set of clinical cases with planted errors used to quantitatively measure a model's vulnerability to hallucination and evaluate mitigation strategies [5]. |
| Multimodal Connector | A learnable interface (e.g., MLP, query tokens) that maps non-text data (like images) into a representation understandable by the LLM, enabling true multimodal integration [13]. |
| Retrieval-Augmented Generation (RAG) Stack | A system architecture that retrieves information from a curated knowledge base at query time, grounding the model's generation in verifiable sources to reduce fabrications [63]. |
| Chain-of-Thought (CoT) Prompting | A prompting technique that requires the model to output its step-by-step reasoning, acting as a reasoning scaffold that improves accuracy and enables self-verification [62]. |
| Clinical Audit Framework | A formal process involving physician review of model outputs to qualitatively assess real-world impact, identify error types, and validate automated metrics [5] [62]. |
Conclusion
The journey toward reliable and clinically admissible Multimodal LLMs for medical imaging is well underway, with significant progress in defining, detecting, and mitigating hallucinations. The synthesis of strategies explored—from the grounding capability of Visual RAG and robust architectural design to rigorous clinical benchmarking—provides a multi-faceted roadmap for researchers. Key takeaways underscore that no single solution is sufficient; a holistic approach combining data quality, model architecture, and continuous validation is essential. Future efforts must focus on developing more nuanced evaluation benchmarks that reflect real-world clinical tasks, creating standardized frameworks for adversarial testing, and fostering the development of region-grounded models that link outputs to specific image areas. Success in this endeavor will not only enhance the trustworthiness of AI assistants but also fundamentally accelerate their integration into biomedical research and personalized patient care, ultimately paving the way for a new era of data-driven drug development and diagnostic precision.
References
- 1. Hallucination (artificial intelligence) [https://en.wikipedia.org/wiki/Hallucination_(artificial_intelligence)]
- 2. On Hallucinations in Artificial Intelligence–Generated Content ... [https://jnm.snmjournals.org/content/early/2025/11/06/jnumed.125.270653]
- 3. Hallucinations in Multimodal LLMs: An In-Depth Overview [https://www.sapien.io/blog/hallucinations-in-multimodal-llms]
- 4. Reducing Hallucinations of Medical Multimodal Large ... [https://arxiv.org/html/2502.15040v1]
- 5. Multi-model assurance analysis showing large language ... [https://www.nature.com/articles/s43856-025-01021-3]
- 6. Frequency of concealment, fabrication and falsification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7876535/]
- 7. Substandard and falsified medical products [https://www.who.int/news-room/fact-sheets/detail/substandard-and-falsified-medical-products]
- 8. Reducing Hallucinations of Medical Multimodal Large ... [https://arxiv.org/abs/2502.15040]
- 9. Mitigating Hallucinations in MLLMs by Vision-Guided ... [https://arxiv.org/html/2511.20032v1]
- 10. Mitigating Hallucinations in MLLMs with Attention Causal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12425127/]
- 11. CCD: Mitigating Hallucinations in Radiology MLLMs via ... [https://arxiv.org/html/2509.23379v1]
- 12. Agentic AI and Large Language Models in Radiology [https://www.mdpi.com/2306-5354/12/12/1303]
- 13. Multimodal Large Language Models in Medical Imaging [https://pmc.ncbi.nlm.nih.gov/articles/PMC12479233/]
- 14. Reducing hallucination in MLLMs for action recognition ... [https://www.sciencedirect.com/science/article/abs/pii/S0925231225025330]
- 15. Towards a holistic framework for multimodal LLM in 3D ... [https://www.nature.com/articles/s41467-025-57426-0]
- 16. The Clinicians' Guide to Large Language Models [https://pmc.ncbi.nlm.nih.gov/articles/PMC11815294/]
- 17. Overcoming data scarcity in biomedical imaging with a ... [https://www.nature.com/articles/s43588-024-00662-z]
- 18. Investigating the impact of data heterogeneity on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11095741/]
- 19. Addressing data heterogeneity in distributed medical ... [https://www.nature.com/articles/s41467-025-64459-y]
- 20. A review and systematic guide to counteracting medical ... [https://www.sciencedirect.com/science/article/pii/S266699002500045X]
- 21. CLINICAL HETEROGENEITY IN THE AGE OF BIG DATA ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10493739/]
- 22. RAG Diagram Guide: Visual Architecture of Retrieval- ... [https://latenode.com/blog/ai-frameworks-technical-infrastructure/rag-retrieval-augmented-generation/rag-diagram-guide-visual-architecture-of-retrieval-augmented-generation]
- 23. Troubleshooting Guide with Did You Mean [https://medium.com/@amitavamanna/troubleshooting-guide-with-did-you-mean-using-multimodal-rag-95601830c1ea]
- 24. Retrieval-Augmented Generation (RAG) in Healthcare [https://www.mdpi.com/2673-2688/6/9/226]
- 25. Seven RAG Pitfalls and How to Solve Them [https://labelstud.io/blog/seven-ways-your-rag-system-could-be-failing-and-how-to-fix-them/]
- 26. VisRAG: Vision-based Retrieval-augmented Generation on ... [https://arxiv.org/abs/2410.10594]
- 27. A Survey of Instruction Tuning in Large Language Models ... [https://arxiv.org/html/2508.17184v2]
- 28. Biomedical Visual Instruction Tuning with Clinician ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11867732/]
- 29. Domain-Specific Instruction Tuning [https://www.emergentmind.com/topics/domain-specific-instruction-tuning]
- 30. Exploring the effectiveness of instruction tuning in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12040708/]
- 31. Reducing Hallucinations of Medical Multimodal Large ... [https://www.semanticscholar.org/paper/Reducing-Hallucinations-of-Medical-Multimodal-Large-Chu-Zhang/2d4689e8cddff9a99673f4e63512cf9a06534e88]
- 32. A Survey of Connectors in Multi-modal Large Language ... [https://arxiv.org/html/2502.11453v1]
- 33. Multimodal LLMs: Architecture, Techniques, and Use Cases [https://www.linkedin.com/pulse/multimodal-llms-architecture-techniques-use-cases-premai-lshpf]
- 34. Multi-modal transformer architecture for medical image ... [https://www.nature.com/articles/s41598-024-69981-5]
- 35. Cross-Modal Consistency in Multimodal Large Language ... [https://arxiv.org/html/2411.09273v1]
- 36. Review Medical multimodal large language models [https://www.sciencedirect.com/science/article/pii/S2950261625000512]
- 37. Adapting SAM with Cross-modal Reference for 3D Medical ... [https://arxiv.org/html/2412.05605v1]
- 38. A collaborative large language model for drug analysis [https://www.nature.com/articles/s41551-025-01471-z]
- 39. Adversarial Attacks to Multi-Modal Models [https://arxiv.org/html/2409.06793v1]
- 40. Invisible Injections: Exploiting Vision-Language Models Through Steganographic Prompt Embedding [https://arxiv.org/html/2507.22304v1]
- 41. Assessing the adversarial robustness of multimodal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12328349/]
- 42. On hallucinations in AI-generated content for nuclear ... [https://arxiv.org/html/2506.13995v2]
- 43. Boosting adversarial transferability in vision-language models via multimodal feature heterogeneity | Scientific Reports [https://www.nature.com/articles/s41598-025-91802-6]
- 44. Mitigating Hallucination in Large Language Models (LLMs) [https://arxiv.org/html/2510.24476v1]
- 45. How Do Your Biomedical Named Entity Recognition ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9014470/]
- 46. Mitigating data bias and ensuring reliable evaluation of AI ... [https://www.nature.com/articles/s41467-025-60801-6]
- 47. Bias recognition and mitigation strategies in artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11897215/]
- 48. Identifying and Mitigating Potential Biases in Predicting ... [https://pubmed.ncbi.nlm.nih.gov/35579815/]
- 49. Preventing Model Collapse in 2025 with Human-in-the-Loop ... [https://humansintheloop.org/what-is-model-collapse-and-why-its-a-2025-concern/]
- 50. Human-in-the-Loop AI: Why It Matters in the Era of GenAI [https://www.tredence.com/blog/hitl-human-in-the-loop]
- 51. Methods and Validations for the AutoLit Review Software - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552804/]
- 52. Evaluating progress in automatic chest X-ray radiology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10499844/]
- 53. RadGraph: Extracting Clinical Entities and Relations from ... [https://physionet.org/content/radgraph/]
- 54. Worse than Random? An Embarrassingly Simple Probing ... [https://arxiv.org/html/2405.20421v1]
- 55. What are the limitations of using ROUGE or METEOR ... [https://milvus.io/ai-quick-reference/what-are-the-limitations-of-using-rouge-or-meteor-for-rag-evaluation-especially-considering-there-may-be-multiple-correct-ways-to-answer-a-question-with-the-retrieved-info]
- 56. Using LLMs in Radiology | RSNA [https://www.rsna.org/news/2025/july/using-llms-in-radiology]
- 57. AI Hallucination: Comparison of the Popular LLMs [https://research.aimultiple.com/ai-hallucination/]
- 58. A framework to assess clinical safety and hallucination ... [https://www.nature.com/articles/s41746-025-01670-7]
- 59. Hallucination-Inducing Image Generation for Multimodal ... [https://arxiv.org/abs/2509.25178]
- 60. Measuring what matters to rare disease patients [https://pmc.ncbi.nlm.nih.gov/articles/PMC5667521/]
- 61. Measuring what matters to rare disease patients – reflections ... [https://ojrd.biomedcentral.com/articles/10.1186/s13023-017-0718-x]
- 62. Medical Hallucination in Foundation Models and Their ... [https://arxiv.org/html/2503.05777v2]
- 63. real-world uses, risks, NHS/EU/US rules, and how to ... [https://www.iatrox.com/blog/artificial-intelligence-in-healthcare-uses-risks-governance-2025]