Invasive vs. Non-Invasive Neural Interfaces: A 2025 Technical and Clinical Analysis for Biomedical Research
This article provides a comprehensive analysis of invasive and non-invasive neural interfaces, tailored for researchers and drug development professionals.
Invasive vs. Non-Invasive Neural Interfaces: A 2025 Technical and Clinical Analysis for Biomedical Research
Abstract
This article provides a comprehensive analysis of invasive and non-invasive neural interfaces, tailored for researchers and drug development professionals. It explores the foundational principles, from the biophysics of signal acquisition to the latest material and algorithmic innovations. The content details current methodologies and applications in clinical trials and therapeutic development, examines persistent technical challenges and optimization strategies, and offers a critical, evidence-based comparison of interface modalities. The goal is to equip scientific audiences with the insights needed to select appropriate technologies, navigate the development landscape, and contribute to the future of neurotechnology.
Core Principles and Neurotechnology Foundations: From Biophysics to Modern Systems
Neural interfaces, often termed brain-computer interfaces (BCIs) or brain-machine interfaces (BMIs), represent a revolutionary class of technologies that enable direct communication between the brain and external devices. These systems can translate neural activity into commands for controlling computers, prosthetic limbs, or other machines, bypassing traditional neuromuscular pathways [1] [2]. The fundamental value of these interfaces lies in their potential to restore function for individuals with disabilities—such as allowing paralyzed persons to control robotic arms or communicate through synthesized speech—and in their capacity to provide new tools for neuroscience research and therapeutic interventions [3] [4].
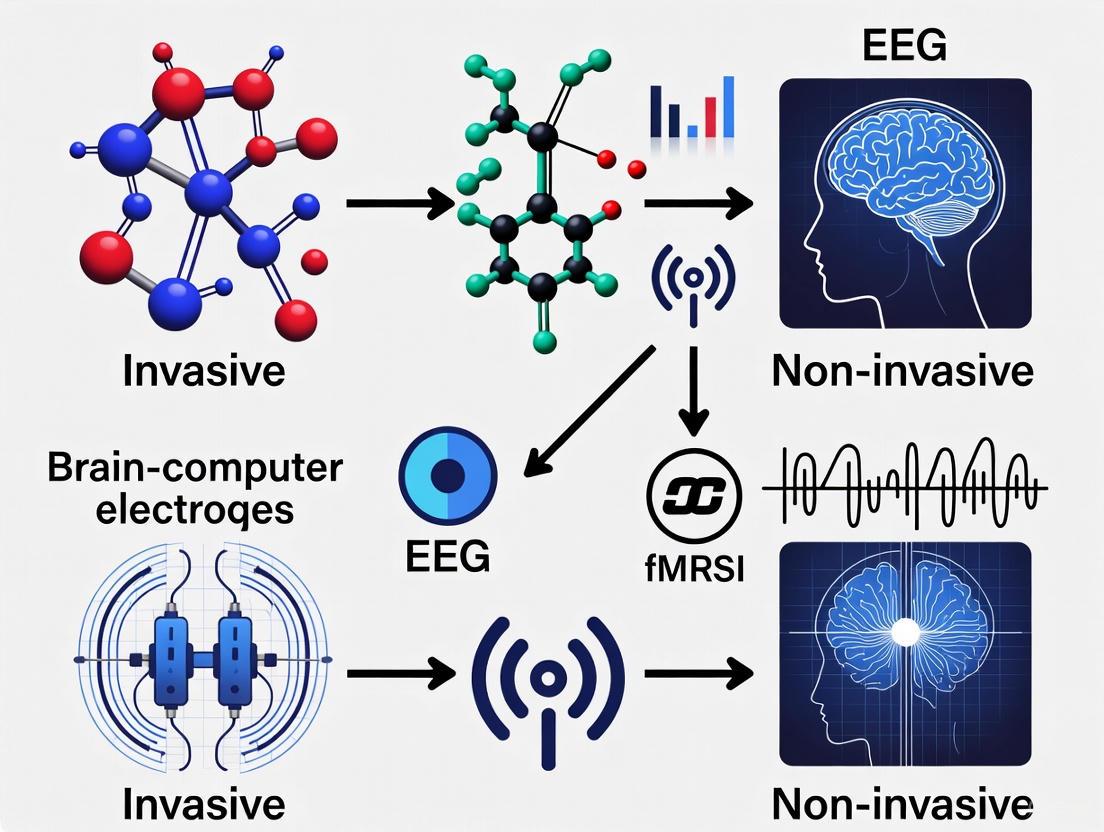
The field categorizes neural interfaces primarily by their level of invasiveness, which directly correlates with their signal quality, spatial resolution, and associated risks. Invasive interfaces are surgically implanted and directly interface with brain tissue, offering high-fidelity signals but carrying greater medical risks. Partially-invasive (or minimally-invasive) interfaces are located inside the skull but not within brain tissue, representing a middle ground. Non-invasive interfaces record from outside the skull, avoiding surgical risks entirely but obtaining lower-resolution signals [5] [6]. This spectrum of approaches enables researchers and clinicians to select appropriate technologies based on specific application requirements, balancing signal quality with safety considerations. The subsequent sections provide a detailed comparative analysis of these paradigms, supported by experimental data and methodological descriptions to inform researchers and drug development professionals.
Comparative Analysis of Neural Interface Technologies
Performance and Signal Characteristics
The performance characteristics of neural interfaces vary significantly across the invasiveness spectrum, influencing their suitability for different applications. The table below summarizes key quantitative metrics and attributes for the three primary paradigms.
Table 1: Performance Comparison of Neural Interface Paradigms
| Parameter | Invasive Interfaces | Partially-Invasive Interfaces | Non-Invasive Interfaces |
|---|---|---|---|
| Spatial Resolution | Micrometer scale (single neurons) [6] | Millimeter scale (neural populations) [5] | Centimeter scale (broad regions) [6] |
| Temporal Resolution | Millisecond precision (kHz range) [6] | Millisecond precision [5] | Tens of milliseconds (100 Hz typical for dry EEG) [6] |
| Signal-to-Noise Ratio | High [6] | Moderate to High [5] | Low to Moderate [5] [6] |
| Information Transfer Rate | High (e.g., speech decoding at 62 WPM) [1] | Moderate to High [5] | Low to Moderate (e.g., 20.9 WPM for sEMG handwriting) [7] |
| Key Signals Recorded | Action Potentials (APs), Local Field Potentials (LFPs) [6] | Electrocorticography (ECoG) [5] | EEG, MEG, fNIRS, sEMG [7] [5] |
| Primary Applications | Restoring motor function, speech decoding, complex device control [3] [4] | Motor restoration, epilepsy monitoring, research [5] | Basic device control, neurostimulation, research, wellness [7] [5] |
| Surgical Risk Profile | High (requires brain implantation) [4] | Moderate (requires craniotomy but not brain penetration) [5] | None [5] |
Signal Source and Technical Characteristics
Understanding the biological sources and technical aspects of the signals each interface type captures is crucial for appropriate selection in research and clinical settings.
Table 2: Signal Sources and Technical Specifications
| Interface Type | Biological Signal Sources | Recording Techniques | Penetration Depth | Typical Coverage |
|---|---|---|---|---|
| Invasive | Extracellular action potentials, local field potentials from cortical layers [6] | Utah arrays, intracortical electrodes, Neuropixels [5] [4] | Direct brain tissue contact [6] | Focal, limited to implant location [6] |
| Partially-Invasive | Cortical surface potentials, electrocorticography (ECoG) [5] | ECoG grids, WIMAGINE implant, Stentrode [5] | Brain surface (epidural or subdural) [5] | Regional, covers implanted grid area [5] |
| Non-Invasive | Post-synaptic currents (EEG), magnetic fields (MEG), hemodynamic responses (fNIRS), muscle potentials (sEMG) [7] [5] [6] | EEG caps, MEG systems, fNIRS headbands, sEMG wristbands [7] [5] | Superficial (through skull and scalp) [6] | Whole-brain or broad regions [6] |
Invasive interfaces provide access to the richest neural signals, including action potentials from individual neurons and local field potentials that reflect the integrated activity of local neuronal populations [6]. Partially-invasive techniques like ECoG capture signals from the cortical surface, offering a balance between signal quality and reduced invasiveness [5]. Non-invasive methods face the fundamental challenge of signal attenuation and spatial blurring as neural signals pass through the meninges, cerebrospinal fluid, skull, and scalp [6]. For instance, EEG primarily detects synchronized post-synaptic potentials from pyramidal neurons, but the skull acts as a strong low-pass filter, attenuating high-frequency components and reducing spatial resolution [6].
Recent advancements in non-invasive approaches include surface electromyography (sEMG) interfaces that decode neuromuscular signals at the wrist. One study demonstrated a generic non-invasive neuromotor interface using an sEMG wristband that achieved handwriting transcription at 20.9 words per minute and gesture decoding with greater than 90% accuracy across participants without person-specific training [7]. This represents a significant advancement in non-invasive interface performance, though still below the bandwidth of invasive systems capable of decoding speech at up to 62 words per minute [1].
Experimental Protocols and Methodologies
Protocol for Invasive Intracortical Recording
The following methodology outlines a standard approach for obtaining high-resolution neural signals using invasive intracortical interfaces, based on established practices in the field [5] [6]:
Surgical Implantation: Under sterile conditions and general anesthesia, perform a craniotomy to expose the dura mater over the target brain region. For motor control applications, the primary motor cortex is typically targeted. Implant multi-electrode arrays (such as Utah arrays or custom flexible arrays) using pneumatic insertion or controlled mechanical insertion to a depth of approximately 1-1.5mm to access cortical layers containing pyramidal neurons [6]. Secure the array to the skull using medical-grade titanium plates and cement.
Neural Signal Acquisition: Connect the implanted array to a percutaneous connector or wireless transmitter. For acute experiments, use wired connections to high-channel-count acquisition systems (e.g., Blackrock Neurotech systems). For chronic implants, utilize fully implanted wireless systems. Set sampling rates to 30 kHz per channel to adequately capture action potentials (300-5000 Hz band) and local field potentials (0.5-300 Hz band) [6]. Apply appropriate referencing schemes to minimize common-mode noise.
Signal Processing and Decoding: Implement a real-time processing pipeline beginning with bandpass filtering (300-5000 Hz for spikes, 0.5-300 Hz for LFPs). For spike detection, apply amplitude thresholding based on the root-mean-square of the signal. Perform spike sorting using principal component analysis or template matching algorithms to isolate single-unit activity [6]. Decode movement intentions using population vector algorithms or neural network models trained on the relationship between neural firing patterns and movement parameters [5] [6].
Closed-Loop Control Implementation: Establish a real-time control loop with update rates of 10-100 Hz. Map decoded movement intentions to prosthetic device commands using kinematic models. Provide visual feedback to users to facilitate neuroplasticity and improve control proficiency over time [6].
Protocol for Non-Invasive sEMG Interface
This protocol details the methodology for implementing a non-invasive surface electromyography (sEMG) interface for gesture decoding and computer control, based on recent research [7]:
Hardware Setup and Data Collection: Utilize a dry-electrode, multichannel sEMG wristband (sEMG-RD) with a high sample rate (2 kHz) and low-noise design (2.46 μVrms). Ensure proper sizing for participant wrist circumference with electrode spacing approaching the spatial bandwidth of EMG signals (5-10 mm) [7]. Position the electrode gap to align with the ulna bone where muscle density is reduced. Collect training data by prompting participants to perform specific gestures, wrist control tasks, and handwriting while recording sEMG activity and corresponding labels.
Signal Preprocessing and Time Alignment: Process raw sEMG signals using a real-time processing engine to reduce online-offline shift. Apply a time-alignment algorithm to precisely align prompter labels with actual gesture onset times, accounting for participant reaction time and compliance variations [7]. Filter signals to remove motion artifacts and power line interference.
Model Training and Validation: Train neural network models on data collected from a diverse participant population (hundreds to thousands of participants). Use the collected sEMG data as input and the aligned behavioral labels as supervision. Implement data augmentation techniques to improve model robustness across anatomical variations and sensor placements [7]. Validate model performance on held-out participants to assess cross-user generalization.
Closed-Loop Performance Evaluation: Evaluate the system in closed-loop tasks including continuous navigation (measuring target acquisitions per second), discrete gesture detection (gesture detections per second), and handwriting transcription (words per minute) [7]. For handwriting, prompt participants to hold their fingers together as if holding a writing implement and "write" prompted text while the system decodes the sEMG signals into text.
Visualization of Experimental Workflows
The following diagrams illustrate key experimental workflows and signal pathways for different neural interface paradigms.
Diagram 1: Invasive interface workflow with closed-loop feedback
Diagram 2: Non-invasive sEMG interface workflow for computer control
The Scientist's Toolkit: Research Reagent Solutions
This section details essential materials, reagents, and tools used in neural interface research, providing investigators with a practical resource for experimental planning.
Table 3: Essential Research Tools for Neural Interface Development
| Category | Specific Tools/Reagents | Research Function | Example Applications |
|---|---|---|---|
| Electrode Materials | Platinum-iridium alloys, Graphene, Conductive polymers [3] | Neural signal transduction with biocompatibility | Chronic implants, ECoG grids, stent electrodes [3] [5] |
| Signal Acquisition Systems | Blackrock Neurotech systems, OpenBCI, Ripple Neuro systems [8] [9] | Multi-channel neural data acquisition with precise temporal resolution | Preclinical research, human clinical trials [5] [9] |
| Decoding Algorithms | Spike sorting algorithms, Deep learning networks (CNN, RNN), Transfer learning methods [5] | Translating neural signals to intended commands | Real-time prosthetic control, speech decoding [5] [1] |
| Surgical Implantation Tools | Stereotactic frames, Pneumatic inserters, MRI/CT guidance systems [3] | Precise electrode placement with minimal tissue damage | Utah array implantation, depth electrode placement [3] [6] |
| Calibration & Testing Protocols | Behavioral prompting systems, Time-alignment algorithms, Cross-validation methods [7] | System performance evaluation and optimization | Gesture decoding validation, handwriting recognition tests [7] |
The selection of appropriate materials and tools significantly impacts neural interface performance and longevity. For invasive interfaces, electrode materials must balance electrical properties with biocompatibility to minimize immune response and signal degradation over time [3]. Platinum-iridium alloys offer excellent corrosion resistance, while graphene and conductive polymers provide flexibility that reduces mechanical mismatch with neural tissue [3]. For signal acquisition, commercial systems like those from Blackrock Neurotech support high-channel-count recordings essential for decoding complex intentions from neural populations [9].
In decoding algorithms, recent advances in deep learning have improved the performance of both invasive and non-invasive systems. Convolutional neural networks can extract spatial patterns from multi-electrode arrays, while recurrent neural networks model temporal dependencies in neural signals [5]. Transfer learning techniques are particularly valuable for non-invasive systems, enabling models trained on large participant populations to generalize to new users with minimal calibration [7] [5]. For non-invasive sEMG interfaces, the development of time-alignment algorithms has been crucial for precisely matching prompts with actual muscle activity during training data collection [7].
The neural interface spectrum encompasses technologies with complementary strengths tailored to different applications. Invasive systems provide unparalleled signal resolution for restoring complex functions like movement and communication in severe paralysis, while partially-invasive approaches offer a favorable risk-benefit profile for specific clinical applications. Non-invasive interfaces present the safest option for basic control applications, wellness monitoring, and research involving healthy participants.
Future progress will likely focus on improving the performance and accessibility of all interface types. For invasive approaches, developments in biocompatible materials and wireless technology may reduce risks and extend functional lifespan [3] [4]. Partially-invasive techniques like the Stentrode and high-density ECoG continue to narrow the performance gap with fully invasive approaches [5]. Non-invasive methods are benefiting from advanced signal processing and large-scale data collection to improve cross-user generalization [7]. Additionally, optical neural interfaces represent an emerging alternative that may offer high spatial resolution with decreased invasiveness, though this technology remains primarily in preclinical development [10].
The optimal neural interface paradigm depends critically on the specific application requirements and risk-benefit considerations. This comparison provides researchers and clinicians with evidence-based guidance for selecting appropriate technologies and methodologies to advance both fundamental neuroscience and clinical applications.
The field of neural interfaces research is fundamentally divided by the biophysical properties of the signals that these tools acquire. Understanding the origin, characteristics, and limitations of electrophysiological and hemodynamic signals is crucial for selecting the appropriate technology for specific scientific or clinical applications, from basic neuroscience to drug development. This guide provides a structured comparison of four core signal acquisition modalities—EEG, ECoG, intracortical, and fNIRS—framed within the critical context of the invasive versus non-invasive trade-off. We dissect their underlying biophysical principles, summarize their performance metrics in comparative tables, and detail experimental protocols that leverage their complementary strengths.
Biophysical Origins and Signal Characteristics
Neural signals can be broadly categorized into those measuring electrical activity directly and those measuring the metabolic consequences of that activity.
Electrophysiological Signals (EEG, ECoG, Intracortical)
Electrophysiological signals originate from the transient flow of ions across neuronal membranes. Action Potentials are all-or-nothing, millisecond-duration signals that propagate along a neuron's axon, representing the primary unit of neuronal communication [11]. Field Potentials, in contrast, are slower, graded signals resulting from the summation of postsynaptic potentials (EPSPs and IPSPs) from thousands to millions of synchronously active neurons [11] [12]. The spatial scale of recording determines the signal type accessible to a given modality.
- Intracortical Signals: Recorded via microelectrodes implanted directly into the brain tissue, these signals provide the highest resolution. They can capture single-unit activity (SUA), representing action potentials from individual neurons, and multi-unit activity (MUA), alongside local field potentials (LFPs), which are low-frequency components (<300 Hz) reflecting summed synaptic activity [11] [13].
- ECoG Signals: Electrocorticography (ECoG) electrodes are placed on the surface of the brain, beneath the skull. They primarily capture LFPs from a larger population of neurons than intracortical electrodes, with a spatial resolution of 1-10 mm [13]. ECoG offers a balance, providing signals with higher spatial resolution and signal-to-noise ratio than non-invasive methods but without penetrating the brain tissue [5].
- EEG Signals: Electroencephalography (EEG) is recorded from electrodes on the scalp. The electrical signals generated by cortical pyramidal neurons must propagate through the meninges, skull, and scalp, which act as resistive and capacitive layers that severely blur the signal. Consequently, EEG reflects the synchronized activity of millions of neurons, providing excellent temporal resolution (milliseconds) but poor spatial resolution (several centimeters) [12].
The following diagram illustrates the pathway of electrical signal generation and acquisition for these modalities.
Diagram 1: Pathway from neuronal activity to acquired electrophysiological signals.
Hemodynamic Signals (fNIRS)
Functional Near-Infrared Spectroscopy (fNIRS) measures an indirect correlate of neural activity based on neurovascular coupling—the mechanism by which neural activity triggers a localized hemodynamic response [14] [12]. When a brain region becomes active, it consumes oxygen, leading to a complex cascade that increases cerebral blood flow to deliver oxygenated hemoglobin (HbO). fNIRS uses near-infrared light (600-1000 nm) shined through the scalp to measure concentration changes of HbO and deoxygenated hemoglobin (HbR) in the cortical capillaries [14] [12]. This hemodynamic response is slower than electrical signals, unfolding over seconds, which limits fNIRS's temporal resolution but provides good spatial resolution for a non-invasive technique.
Comparative Performance Data
The biophysical origins of these signals directly translate into their performance characteristics, as summarized in the tables below.
Table 1: Technical specifications and performance metrics of neural signal acquisition modalities.
| Metric | EEG | ECoG | Intracortical | fNIRS |
|---|---|---|---|---|
| Spatial Resolution | ~1-3 cm [12] | 1-10 mm [13] | 50-500 μm [11] [13] | ~1-2 cm [15] |
| Temporal Resolution | ~1-100 ms [12] | ~1-10 ms [5] | <1 ms [11] | ~0.1-1 s [15] [12] |
| Invasiveness | Non-invasive | Invasive (subdural) | Invasive (intraparenchymal) | Non-invasive |
| Primary Signal | Scalp potentials | Cortical surface potentials | Action potentials & LFPs | HbO/HbR concentration |
| Signal Origin | Summed postsynaptic potentials [12] | Summed postsynaptic potentials | Single-unit & multi-unit activity [11] | Hemodynamic response [14] |
| Typical Bandwidth | 0.1-100 Hz [16] | 0-500 Hz [13] | 0.1-7,000 Hz (SUA: 300-7,000 Hz) [13] | ~0.01-0.3 Hz [14] |
Table 2: Suitability for applications and practical considerations in research and clinical settings.
| Consideration | EEG | ECoG | Intracortical | fNIRS |
|---|---|---|---|---|
| Key Clinical Applications | Epilepsy monitoring, sleep disorders, brain injury [16] [9] | Epilepsy focus mapping, surgical planning [17] | Motor prosthetics for paralysis [5] [17] | Cognitive neuroscience, neurodevelopment [14] |
| Key Research Applications | Cognitive neuroscience, brain-state monitoring [12] | Motor control BCIs, basic communication [13] | Fine motor control, complex language decoding [13] | Neurovascular coupling, bedside monitoring [18] |
| Signal Stability | Moderate (prone to artifacts) | High | Degrades over time (glial scarring) [13] | High |
| Relative Cost | Low | High | Very High | Moderate [12] |
| Portability | High (wearable systems) | Low | Very Low | High [12] |
Experimental Protocols for Multimodal Integration
No single modality provides a complete picture of brain function. The following protocols illustrate how combining these tools can yield synergistic insights.
Protocol: Investigating Cognitive Load in Dynamic Environments
This protocol, adapted from a Frontiers study, uses a dual-task paradigm to study cognitive load and stress [14].
- Objective: To investigate the effects of complex, dynamically changing environments on cognitive load, affective state, and performance.
- Subjects: 30 healthy human participants.
- Task: Participants play three versions of Tetris (Easy constant, Hard constant, Ramp difficulty) while simultaneously performing an Auditory Reaction Task (ART) [14].
- Signal Acquisition:
- fNIRS: Measures HbO and HbR concentration changes in the prefrontal cortex to index cognitive load via hemodynamic response [14].
- EEG: Recorded from scalp electrodes to track mental fatigue through power band shifts (e.g., increased Delta power) and provide millisecond-resolution brain dynamics [14].
- ECG/EDA: Recorded to assess physiological stress response.
- Performance Metrics: Tetris score and ART reaction time/accuracy.
- Subjective Reports: Self-reports of valence, enjoyment, and perceived workload.
- Analysis:
- fNIRS: General linear model analysis to compare HbO/HbR changes between task conditions.
- EEG: Time-frequency analysis to quantify band power changes (Delta, Theta, Alpha, Beta).
- Correlation: Perform multimodal correlation between fNIRS activation, EEG spectral features, and performance metrics.
This protocol leverages fNIRS's spatial localization of cortical load and EEG's sensitivity to rapid state changes like fatigue, providing a comprehensive assessment unavailable to either modality alone [14].
Protocol: Concurrent fNIRS-EEG for Motor Imagery BCI
This protocol outlines a standard pipeline for developing a more robust Brain-Computer Interface (BCI) [12] [18].
- Objective: To improve the classification accuracy of motor imagery (e.g., imagining hand movement) for BCI control by integrating electrical and hemodynamic data.
- Signal Acquisition:
- A custom-built helmet or cap with co-registered EEG electrodes and fNIRS optodes over the motor cortex [18].
- EEG is recorded continuously.
- fNIRS records changes in HbO and HbR from channels covering the same cortical area.
- Experimental Paradigm:
- A cue-based block design where participants perform cued motor imagery (e.g., left hand vs. right hand) interspersed with rest periods.
- Data Processing & Fusion:
- Preprocessing: Independent Component Analysis (ICA) for EEG artifact removal [16] and Modified Beer-Lambert Law for fNIRS to convert light intensity to HbO/HbR concentration [12].
- Feature Extraction:
- EEG: Extract event-related desynchronization/synchronization (ERD/ERS) in the Mu (8-12 Hz) and Beta (13-30 Hz) rhythms.
- fNIRS: Extract the mean HbO concentration during the task blocks.
- Data Fusion: A common approach is feature-level fusion, where the extracted EEG and fNIRS features are concatenated into a single feature vector for classification [12].
- Classification: The fused feature vector is fed into a classifier (e.g., Support Vector Machine - SVM or Linear Discriminant Analysis - LDA) to discriminate between the different motor imagery tasks.
The fusion of EEG's rapid onset and fNIRS's spatially specific response has been shown to improve classification accuracy and reduce BCI calibration time compared to unimodal systems [12] [18].
The following workflow diagram visualizes the stages of this multimodal experimental protocol.
Diagram 2: Workflow for a concurrent fNIRS-EEG Brain-Computer Interface experiment.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key materials and equipment for setting up experiments with the featured modalities.
| Item | Function/Description | Exemplary Use Case |
|---|---|---|
| Integrated fNIRS-EEG Cap | A flexible cap with co-registered EEG electrodes and fNIRS optode holders for simultaneous data acquisition [18]. | Concurrent fNIRS-EEG studies (Section 4.2). |
| 3D-Printed Custom Helmet | A rigid, subject-specific helmet for precise and stable positioning of EEG and fNIRS components, improving data quality [18]. | Studies requiring high spatial accuracy and minimal motion artifact. |
| ECoG Grid (e.g., WIMAGINE) | An implantable ECoG grid system designed for chronic, stable recording from the cortical surface [5]. | Long-term BCI studies for restoring motor function. |
| Intracortical Array (e.g., Utah Array) | A microelectrode array implanted into the brain tissue to record single- and multi-unit activity [5]. | High-precision motor control studies for advanced neuroprosthetics. |
| Independent Component Analysis (ICA) | A computational algorithm for separating artifacts (e.g., eye blinks, muscle activity) from neural signals in EEG data [16]. | Standard preprocessing step for EEG analysis. |
| Modified Beer-Lambert Law (MBLL) | The fundamental algorithm used in fNIRS to convert measured light attenuation into changes in HbO and HbR concentration [12]. | Essential for all fNIRS data analysis. |
The evolution of Brain-Computer Interfaces (BCIs) hinges on overcoming fundamental engineering and biological constraints embodied by three critical performance benchmarks: spatial resolution, temporal resolution, and signal-to-noise ratio (SNR). These parameters form a delicate triage that defines a neural interface's capability to accurately interpret brain activity, and they are directly influenced by the choice between invasive and non-invasive approaches. Spatial resolution refers to the smallest distinguishable distance between two neural activity sources, determining whether an interface can differentiate individual neuron firing or broader regional activation. Temporal resolution represents the smallest measurable time interval between neural events, dictating how precisely an interface can track the rapid dynamics of brain signaling. Signal-to-noise ratio quantifies the strength of relevant neural signals against background interference, ultimately determining decoding accuracy and reliability [19] [20].
The central thesis in BCI research posits that invasiveness level dictates performance characteristics across these three benchmarks. Invasive interfaces, by physically penetrating the skull and often contacting neural tissue directly, achieve superior performance across all three parameters but introduce surgical risks, potential for tissue response, and long-term stability challenges. Non-invasive interfaces, operating outside the skull, offer greater safety and accessibility but face fundamental physical limitations in signal acquisition that constrain their ultimate performance ceiling [8] [17] [1]. This comparison guide provides an objective analysis of how current neural interface technologies perform across these key benchmarks, supported by experimental data and methodological details to inform research and development decisions.
Performance Benchmark Comparison of Neural Interface Technologies
The table below provides a quantitative comparison of key performance characteristics across major neural interface technologies, highlighting the clear trade-offs between invasive and non-invasive approaches.
Table 1: Performance Characteristics of Neural Interface Technologies
| Technology | Spatial Resolution | Temporal Resolution | Signal-to-Noise Ratio | Primary Applications |
|---|---|---|---|---|
| Intracortical Electrodes | Single neuron (~0.05 mm) [21] | Excellent (<1 ms) [21] | Very High (direct neural contact) [1] | Motor prosthetics, speech decoding [22] [1] |
| ECoG | Mesoscale (1-10 mm) [8] | Excellent (<1 ms) [8] | High (subdural placement) [8] | Epilepsy monitoring, motor BCIs [17] |
| EEG | Low (10-20 mm) [8] [1] | Good (~10-100 ms) [17] | Low (signal attenuation through skull) [1] [7] | Brain monitoring, basic BCIs, research [8] [17] |
| fNIRS | Low (10-20 mm) [8] | Poor (seconds) [8] | Low (hemodynamic response lag) [8] | Brain monitoring, neurofeedback [8] [17] |
| fMRI | High (1-3 mm) [23] [20] | Poor (1-3 seconds) [23] | Variable (BOLD sensitivity) [23] [20] | Research, surgical planning [23] |
| sEMG | Muscle group level [7] | Excellent (<1 ms) [7] | High (amplified neural signals in muscle) [7] | Neuromotor interfaces, prosthesis control [7] |
Table 2: Market Forecast and Application Focus (2025-2045) [8]
| Segment | Forecasted CAGR | Primary Drivers | Key Challenges |
|---|---|---|---|
| Non-Invasive (Medical) | 8.4% (overall market) | Assistive technology, neurological disorder management | Signal quality, spatial resolution limitations |
| Non-Invasive (Consumer) | 8.4% (overall market) | AR/VR headsets, wellness monitoring | Performance vs. accessibility trade-offs |
| Invasive (Assistive) | 8.4% (overall market) | Severe paralysis, communication restoration | Surgical risks, long-term stability, biocompatibility |
| Invasive (Research) | 8.4% (overall market) | Neuroscience understanding, algorithm development | Regulatory hurdles, tissue response |
Experimental Protocols and Methodologies
Deep Neural Network Decoding for Intracortical Interfaces
Objective: To develop a BCI decoding framework that maintains high accuracy without daily recalibration, addressing stability challenges in invasive interfaces [22].
Methodology:
- Participant: 27-year-old male with C5 AIS A tetraplegia implanted with a 96-channel microelectrode array in the hand and arm area of left primary motor cortex [22].
- Task Design: Participant performed a four-movement imagination task (index extension, index flexion, wrist extension, wrist flexion) in response to visual cues across 80 sessions over 865 days [22].
- Neural Features: Mean wavelet power (MWP) values calculated from raw voltage for each of the 96 channels over 100-ms bins [22].
- Decoder Architecture: Deep neural network (NN) with three configurations:
- Fixed NN (fNN): Initial model calibrated using 40 sessions without updating
- Supervised NN (sNN): Updated daily with explicit training labels
- Unsupervised NN (uNN): Updated daily without explicit labels using inferred movement timing [22]
- Comparison Models: Support vector machine (SVM), linear discriminant analysis (LDA), and naive Bayes decoders retrained daily [22].
Key Results: The supervised NN (sNN) demonstrated significantly higher accuracy than daily-retrained SVM (mean difference 6.35±2.47%, p=3.69×10⁻⁸), with 37/40 sessions achieving >90% accuracy. The unsupervised NN (uNN) maintained performance for over a year without supervised recalibration, outperforming the daily-retrained SVM by 6.12±2.68% [22].
High-Resolution fMRI for BCI Applications
Objective: To investigate the effects of spatial and temporal resolution on fMRI sensitivity and its implications for fMRI-based BCIs [23].
Methodology:
- Imaging Parameters: 7T fMRI during ankle-tapping task across range of spatial (1.5×1.5×1.5mm³ to standard resolutions) and temporal resolutions (500ms to standard TR) [23].
- Metrics: Temporal signal-to-noise ratio (tSNR), observed percent signal change (%∆S), volumes of significant activation, Z-scores, and decoding performance of linear classifiers [23].
- Analysis: Compared BOLD sensitivity measures across resolution combinations to determine optimal parameters for functional network imaging [23].
Key Results: At highest spatial resolution (1.5×1.5×1.5mm³), increasing temporal resolution yielded 22% increase in %∆S (p=0.006) and 9% improvement in decoding performance (p=0.015) despite 29% decrease in tSNR (p<0.001). This demonstrates BOLD sensitivity can be significantly improved with temporal resolution when spatial resolution is sufficiently high [23].
Non-Invasive Surface EMG Neuromotor Interface
Objective: To develop a generic non-invasive neuromotor interface with high performance and cross-user generalization [7].
Methodology:
- Platform: Dry-electrode, multichannel sEMG wristband with high sample rate (2 kHz) and low noise (2.46 μVrms), manufactured in four sizes for anatomical variation [7].
- Participants: 162-6,627 participants across tasks (wrist control, discrete-gesture detection, handwriting) for training generic models [7].
- Data Collection: Supervised training with sEMG activity and prompt timestamps, with post-hoc time-alignment algorithm to account for reaction time variations [7].
- Tasks: Continuous navigation (wrist control), discrete gesture detection (9 distinct gestures), and handwriting (20.9 words per minute) [7].
Key Results: The generic sEMG decoding models achieved cross-user generalization with 0.66 target acquisitions per second in continuous navigation, 0.88 gesture detections per second in discrete tasks, and handwriting at 20.9 words per minute without person-specific training [7].
Technical Foundations: Resolution and SNR Relationships
Spatial Resolution Fundamentals
In MRI and related imaging modalities, spatial resolution is determined by the relationship between k-space coverage and image properties. The nominal spatial resolution (Δx, Δy) is inversely related to the overall extent of k-space coverage (Wx, Wy):
Δx = 1/Wx, Δy = 1/Wy [19]
Where k-space represents the spatial frequency domain of the image, with the central region containing low spatial frequency information (overall contrast) and peripheral regions containing high spatial frequency information (fine details and edges) [19] [24]. The fundamental limitation emerges from k-space truncation, where finite sampling necessarily loses high spatial frequency information, leading to Gibbs ringing artifacts and reduced image sharpness [19] [24]. This physical constraint manifests differently across BCI modalities: invasive interfaces minimize truncation effects by closer proximity to neural sources, while non-invasive approaches suffer from inherent spatial low-pass filtering by biological tissues [8] [1].
Temporal Resolution and SNR Trade-Offs
The relationship between temporal resolution, spatial resolution, and SNR presents a fundamental challenge across neural interface technologies. In fMRI, increasing temporal resolution (shorter TR) typically decreases tSNR due to T1-relaxation effects, while increasing spatial resolution decreases net magnetization per voxel [23]. However, research demonstrates that at sufficiently high spatial resolution, increasing temporal resolution can improve overall BOLD sensitivity despite tSNR reductions, indicating complex interactions between these parameters [23].
In electrophysiological methods including EEG and intracortical recording, temporal resolution is generally superior but faces different SNR challenges. The table below summarizes key relationships and optimization strategies across interface types.
Table 3: Resolution and SNR Optimization Strategies
| Technology | Primary SNR Limitations | Optimization Strategies |
|---|---|---|
| Intracortical Electrodes | Tissue response, glial scarring, electrode degradation [21] [1] | Flexible substrates, biocompatible materials, adaptive algorithms [8] [22] |
| EEG | Skull attenuation, distance from sources, environmental noise [8] [1] | Dry electrodes, sensor arrays, advanced signal processing, reference schemes [8] |
| fMRI | Physiological noise, thermal noise, BOLD sensitivity [23] [20] | Higher field strengths, array coils, parallel imaging, optimized sequences [23] |
| sEMG | Electrode-skin interface, motion artifacts, cross-talk [7] | High-density arrays, anatomical conformity, adaptive fitting [7] |
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Essential Research Materials for Neural Interface Development
| Item | Function | Example Applications |
|---|---|---|
| Microelectrode Arrays | Record action potentials from neuronal populations | Intracortical BCIs, motor decoding studies [21] [22] |
| Dry Electrodes | Enable convenient EEG acquisition without conductive gel | Consumer neurotechnology, wearable BCIs [8] |
| fNIRS Systems | Measure blood oxygenation changes using near-infrared light | Brain monitoring, neurofeedback training [8] [17] |
| High-Density sEMG Arrays | Record myoelectric potentials from multiple muscle regions | Neuromotor interfaces, gesture decoding [7] |
| Deep Neural Network Frameworks | Decode neural signals with high accuracy and adaptability | Motor intention decoding, speech reconstruction [22] |
| Biocompatible Substrates | Improve long-term stability of implanted interfaces | Chronic neural implants, reducing tissue response [8] [1] |
| Quantum Sensors | Enable wearable MEG with improved sensitivity | Next-generation non-invasive BCIs [8] |
The future of neural interface technology lies in breaking the current resolution-SNR-invasiveness trade-offs through multidisciplinary innovation. Promising directions include the development of miniaturized, biocompatible invasive interfaces that reduce tissue response while maintaining high signal quality, and next-generation non-invasive technologies like quantum-enabled sensors (OPM-MEG) that approach invasive-level performance without surgical risks [8] [1]. Advanced decoding algorithms, particularly deep learning approaches that can extract more information from limited signals, will further bridge the performance gap between modalities [22] [7].
The clinical translation pathway will likely see invasive interfaces addressing severe neurological conditions where benefits justify surgical risks, while non-invasive technologies expand into broader consumer and therapeutic applications [8] [17] [1]. As both trajectories advance, the fundamental benchmarks of spatial resolution, temporal resolution, and signal-to-noise ratio will remain the critical metrics driving progress in this rapidly evolving field.
For over two decades, the Utah Array has served as the gold standard for invasive cortical recording and stimulation, underpinning critical advances in brain-computer interfaces (BCIs) and neuroscience research [25] [26]. With its high-channel count and superior signal-to-noise ratio, it has empowered researchers to perform intricate studies of neural networks at an unprecedented level of detail [25]. However, the relentless pursuit of understanding the brain's complex circuitry has fueled a strong drive toward developing modern high-channel-count neuroelectronic interfaces [27]. This evolution is marked by a transition from passive electrode arrays to systems incorporating novel materials and active transduction mechanisms, enabling recordings from thousands of channels simultaneously [27]. This guide objectively compares the performance of the established Utah Array against the capabilities of emerging high-density systems, framing the discussion within the broader scientific debate on invasive versus non-invasive neural interfaces.
Performance Comparison: Utah Array vs. Modern High-Channel-Count Systems
The following tables summarize key quantitative metrics and functional characteristics, providing a direct comparison between the traditional Utah Array and modern high-channel-count technologies.
Table 1: Quantitative Performance and Physical Specifications
| Parameter | Utah Array | Modern High-Channel-Count Systems |
|---|---|---|
| Channel Count (per device) | 96 - 128 electrodes per array; up to 1024 channels per system [25] [26] | Thousands of channels [27] |
| Electrode Pitch | 400 µm [25] | Significantly reduced (enabled by novel materials and active electronics) [27] |
| Standard Electrode Lengths | 0.5 - 1.5 mm (Research); 1.0 - 1.5 mm (Clinical) [25] | Customizable for specific targets |
| Impedance Range | Platinum: 20-800 kΩ; SIROF/IrOx: 1-80 kΩ [25] | Optimized for high-density, addressable arrays [27] |
| Typical Recorded Signals | Action Potentials (spikes), Local Field Potentials (LFPs) [25] [6] | Action Potentials, Local Field Potentials, with higher spatial resolution [27] |
| Long-Term Human Implantation | Over 8 years and counting (documented) [28] [26] | Primarily in research and development stages [27] |
Table 2: Functional Characteristics and Applications
| Characteristic | Utah Array | Modern High-Channel-Count Systems |
|---|---|---|
| Key Advantage | Longevity and Safety: Extensive safety profile with decades of human use; FDA-cleared for short-term monitoring [26] | Spatio-temporal Resolution: High-density design allows for recording from vast neuronal populations [27] |
| Primary Limitation | Channel Count Cap: Practical limit for chronic stability in humans; higher counts risk tissue damage [26] | Clinical Translation: Long-term stability and biocompatibility in humans still under investigation [27] |
| Material Failure Mode | Metal corrosion (Pt, IrOx); insulation cracking/delamination of Parylene-C [28] | Under evaluation; focus on novel, robust biomaterials [27] |
| Biological Failure Mode | Meningeal encapsulation; glial sheath formation; neuronal loss [28] | Tissue reaction to higher density implants is a critical research area [27] |
| Ideal Application | Chronic human BCI for neuroprosthetics, communication [25] [26] [29] | Fundamental neuroscience research, high-fidelity sensory mapping [27] |
The Invasive vs. Non-Invasive Neural Interface Context
The evolution toward higher channel counts in invasive interfaces must be understood within the broader dichotomy of invasive versus non-invasive BMI strategies. Invasive BCIs, like the Utah Array and its successors, record signals directly from the cortical surface or within the brain tissue, capturing signals such as action potentials and local field potentials (LFPs) with high spatial and temporal resolution [6] [30]. In contrast, non-invasive techniques, such as electroencephalography (EEG), record from the scalp and are limited to measuring aggregated, low-frequency neuronal activity that has been attenuated by the skull and scalp [6].
Table 3: Invasive vs. Non-Invasive Signal Characteristics
| Feature | Invasive (e.g., Utah Array & Modern Systems) | Non-Invasive (e.g., EEG) |
|---|---|---|
| Spatial Resolution | High (microns to millimeters) [30] | Low (centimeters) [6] |
| Temporal Resolution | High (capable of detecting single-neuron spikes) [30] | Lower (skull acts as a low-pass filter) [6] |
| Signal-to-Noise Ratio | High, robust against artifacts [30] | Lower, susceptible to noise [6] |
| Signal Source | Input, local processing, and output of cortical areas [6] | Primarily post-synaptic currents from pyramidal neurons [6] |
| Information Transfer Rate | Inherently higher [6] | Lower [6] |
| Clinical Risk | Requires surgery; higher initial risk [30] | Risk-free [6] |
The following diagram illustrates the fundamental anatomical and signal resolution relationships that define this technological landscape.
Anatomical and Signal Relationship of Neural Interfaces
Experimental Protocols for Assessing Neural Interface Performance
Evaluating the performance and longevity of invasive microelectrode arrays involves standardized experimental protocols, both in preclinical and clinical settings. The methodologies below are critical for generating the comparative data presented in this guide.
Chronic Electrophysiological Recording in Human BCI Trials
Objective: To assess the long-term stability and quality of neural signal recording from implanted arrays in human participants for brain-computer interface control [28].
Methodology:
- Implantation: Utah Arrays are surgically implanted into the target brain region (e.g., motor cortex) under an Investigational Device Exemption (IDE) from the FDA and with local IRB approval [28].
- Signal Acquisition: Neural data (action potentials and LFPs) are recorded daily or weekly using a dedicated neural signal processing system (e.g., from Blackrock Neurotech). The system amplifies, filters, and digitizes the signals from each electrode [25].
- Performance Metrics:
- Signal Amplitude: The peak-to-peak voltage of recorded action potentials is tracked over time. An initial increase is often observed post-implantation, followed by a gradual decline in the following months and years [28].
- Impedance Measurement: Electrode impedance is monitored regularly, as it can indicate tissue encapsulation or material degradation [28].
- BCI Control Tasks: Participants perform tasks such as controlling a cursor on a screen or a robotic arm. Decoding algorithms (e.g., Kalman filters, population vector algorithms) translate neural activity into control commands. Performance is measured by metrics like success rate, information transfer rate, and task completion time [30].
- Data Analysis: Recording quality is correlated with the duration of implantation and post-explant findings related to tissue reaction and material integrity [28].
Post-Explant Material and Histological Analysis
Objective: To characterize the material degradation of explanted electrode arrays and the biological tissue response, and to correlate these findings with recorded electrophysiological performance [28].
Methodology:
- Explantation: Arrays are surgically removed from human or animal subjects after a predetermined implantation period.
- Tissue Encapsulation Analysis:
- Optical Microscopy: Provides an initial assessment of the extent of fibrous tissue growth on the array substrate and around electrode shanks [28].
- Two-Photon Microscopy (TPM): Allows for high-resolution, three-dimensional imaging of the tissue sheath surrounding individual electrodes, revealing its thickness and density [28].
- Material Degradation Analysis:
- Scanning Electron Microscopy (SEM): Used to examine the physical integrity of electrode tips and insulation at high magnification, revealing cracks, delamination, or corrosion [28].
- Energy-Dispersive X-ray Spectroscopy (EDS): Performed in conjunction with SEM to determine the elemental composition of electrode materials, identifying loss of conductive coating (e.g., iridium from IrOx tips) or contamination [28].
- Correlation with Performance: Findings from explant analysis are directly compared with the chronic recording data from the same array to identify factors influencing signal decline [28].
The workflow for this comprehensive analysis is depicted below.
Post-Explant Analysis Workflow
The Scientist's Toolkit: Key Research Reagents and Materials
This table details essential materials and solutions used in experiments featuring the Utah Array and high-channel-count systems, which are crucial for replicating studies and understanding the underlying technology.
Table 4: Essential Research Materials and Reagents
| Item | Function / Description | Example Use Case |
|---|---|---|
| Utah Electrode Array (UEA) | A 10x10 grid of silicon microelectrodes; the gold-standard device for chronic cortical recording and stimulation [25] [26]. | Fundamental platform for intracortical BCI research in humans and animal models [25] [29]. |
| Platinum (Pt) Electrode Tips | A stable, biocompatible metal for recording; standard option for the UEA with higher impedance [25] [28]. | Chronic recording of neural signals without the intent for aggressive stimulation [28]. |
| Sputtered Iridium Oxide (SIROF or IrOx) Electrode Tips | A coating with lower impedance and higher charge injection capacity, ideal for both recording and electrical stimulation [25] [28]. | Arrays intended for bidirectional BCIs, providing both control and sensory feedback via intracortical microstimulation (ICMS) [28]. |
| Parylene-C | A biocompatible polymer used as insulation for the electrode shanks and wires, preventing current leakage and signal crosstalk [25] [28]. | Standard insulation material for chronic neural implants; integrity is critical for long-term function [28]. |
| Neural Signal Processor | A specialized hardware system for amplifying, filtering, and digitizing signals from hundreds of electrode channels in real-time [25]. | Acquiring raw neural data for BCI control and scientific analysis [25] [30]. |
| Decoding Algorithms (e.g., Kalman Filter) | Computational methods that translate recorded neural population activity into predicted movement intentions or device commands [30]. | Enabling real-time, closed-loop control of external devices such as computer cursors and robotic limbs [30]. |
The journey from the Utah Array to modern high-channel-count systems represents a pivotal evolution in neurotechnology. The Utah Array established a robust, clinically viable platform, demonstrating that long-term, high-fidelity interfacing with the human brain is possible. Its documented safety and efficacy profile remains its most significant advantage for therapeutic applications [26]. In contrast, emerging high-density technologies promise unparalleled resolution for mapping neural circuits, a drive fueled by the demands of basic science rather than immediate clinical application [27]. The choice between these invasive technologies, and indeed the broader choice between invasive and non-invasive approaches, is not a matter of superiority but of alignment with research goals. The future lies not in one technology prevailing over another, but in the continued, parallel development of both—refining the proven clinical workhorse while pioneering the next-generation tools needed to unravel the brain's deepest mysteries.
The field of neural interfaces is undergoing a profound transformation, moving from simple read-out devices to sophisticated bidirectional systems that blur the line between biology and technology. This evolution is characterized by three interconnected macro-trends: the development of closed-loop systems that enable real-time bidirectional communication, the emergence of neuroadaptive technologies that dynamically respond to cognitive states, and the creation of biohybrid interfaces that improve biological integration through cellular and tissue engineering. These trends are reshaping the fundamental paradigm of human-machine interaction, offering new pathways to treat neurological disorders, restore lost function, and potentially enhance human capabilities.
The trajectory of neural interface development is fundamentally framed by the trade-offs between invasive and non-invasive approaches. Invasive systems (implanted inside the skull) provide unparalleled signal resolution and precision, enabling control of complex prosthetics and communication at near-conversational speeds for paralyzed individuals [1]. Non-invasive systems (worn on the scalp or skin) offer greater safety and accessibility, dominating current market applications, but are limited by lower signal fidelity due to signal attenuation through the skull and other tissues [31] [32]. The emerging macro-trends discussed in this guide are advancing both pathways, each with distinct advantages, challenges, and appropriate applications for researchers and drug development professionals to consider.
Closed-Loop Systems: Bidirectional Neural Communication
Core Concept and Comparative Advantage
Closed-loop brain-computer interfaces (BCIs) represent a significant leap beyond first-generation systems. Unlike open-loop interfaces that only record neural signals (output) or only stimulate the brain (input), closed-loop systems create a dynamic feedback cycle where neural activity is continuously decoded, and the system responds with tailored stimulation or other feedback in real time [1]. This self-adjusting loop mirrors the brain's own operational principles, leading to more stable and effective interventions.
The fundamental value proposition for researchers is the system's ability to detect and respond to physiological states as they occur. For instance, in managing epilepsy, a closed-loop system can detect the onset of a seizure from neural signatures and deliver immediate electrical stimulation to abort it, a stark contrast to continuous, non-contingent stimulation [33]. This responsive approach is not only more therapeutically efficient but also reduces the cumulative exposure to electrical stimulation, potentially minimizing side effects and extending device battery life.
Experimental Protocols and Performance Data
A primary application of closed-loop systems is in adaptive neurostimulation for movement disorders. A typical experimental protocol for Parkinson's disease involves:
- Signal Acquisition: Implanted depth electrodes (e.g., in the subthalamic nucleus) continuously record local field potentials (LFPs).
- Biomarker Identification: Specific oscillatory patterns in the beta band (13-30 Hz) are established as biomarkers for hypokinetic motor states (bradykinesia and rigidity).
- Real-Time Processing: The embedded processor runs a decoding algorithm that quantifies the power of this beta-band activity.
- Adaptive Stimulation: When the beta power exceeds a predefined threshold, the system automatically triggers high-frequency deep brain stimulation (DBS). The stimulation amplitude may be titrated proportionally to the biomarker's intensity.
- Feedback Loop: As beta power normalizes, stimulation is reduced or ceased, preventing over-stimulation and allowing for natural neural activity [33].
The performance of this approach is superior to traditional open-loop DBS. The table below summarizes key comparative metrics.
Table 1: Performance Comparison: Open-Loop vs. Closed-Loop Deep Brain Stimulation
| Performance Metric | Open-Loop DBS | Closed-Loop aDBS |
|---|---|---|
| Stimulation Duty Cycle | Continuous (100%) | Intermittent (~30-60%) |
| Therapeutic Efficacy | Effective, but can fluctuate | More consistent symptom suppression |
| Side Effect Profile | Higher risk of speech/balance impairment | Reduced side effects due to targeted stimulation |
| Energy Consumption | Higher | Significantly lower, extends battery life |
| Adaptability to State | None; static parameters | Dynamic adjustment to patient's real-time need |
Another critical protocol involves motor rehabilitation after spinal cord injury or stroke. Here, the closed loop decodes motor intention from the cortical signals, drives a prosthetic limb or functional electrical stimulation (FES) of paralyzed muscles, and provides somatosensory feedback through cortical stimulation, creating a bridge that promotes neuroplasticity and recovery [33] [34].
System Workflow and Signaling Pathways
The following diagram illustrates the core operational workflow of a closed-loop neural interface, showing the continuous cycle of signal processing, decoding, and adaptive response that defines this technology.
Closed-Loop Neural Interface Workflow
Neuroadaptive Technologies: AI Systems that Respond to Cognitive State
Core Concept and Comparative Advantage
Neuroadaptive technology represents a paradigm shift in human-computer interaction (HCI). These systems use passive BCIs to monitor a user's cognitive and emotional states in real-time—such as attention, cognitive load, and fatigue—and allow the AI system to dynamically adapt its behavior accordingly [35]. While closed-loop systems often focus on direct neurological intervention, neuroadaptive tech aims for seamless, context-aware collaboration between human and machine.
The strategic advantage for applied research lies in moving beyond explicit commands to implicit, context-driven interaction. For example, in a drug development setting, a neuroadaptive system could monitor researchers' focus levels during long data analysis sessions and automatically adjust interface complexity or trigger breaks to reduce error rates. This technology is particularly relevant for addressing the "AI alignment problem," where AI systems can be designed to optimize for not just task completion but also for human well-being and ethical values by responding to affective states [35].
Experimental Protocols and Performance Data
A common protocol for developing a neuroadaptive system involves enhancing sustained attention in critical tasks:
- Signal Acquisition: A non-invasive EEG headset (e.g., a dry-electrode system) records brain activity, focusing on metrics like the theta/beta ratio and P300 event-related potentials, which are correlated with attention and workload.
- Baseline Calibration: The user's individual EEG signatures for states of "high focus" and "distraction" are established during a calibration task.
- Real-Time Classification: Machine learning models (e.g., Support Vector Machines or deep learning networks) classify the user's cognitive state on a second-by-second basis.
- System Adaptation: The connected software adapts based on the decoded state. For instance, if "high cognitive load" is detected, the system might simplify its display. If "drowsiness" is detected in a driver monitoring system, it could trigger an alert [31] [35].
The performance of these systems is gauged by improvements in human performance and reduction in error, rather than pure bit-rate communication.
Table 2: Performance Metrics for Neuroadaptive vs. Static Systems
| Performance Metric | Static System | Neuroadaptive System |
|---|---|---|
| User Error Rate | Baseline | Reduced by 15-30% in high-load tasks |
| Task Completion Time | Baseline | Improved efficiency in complex tasks |
| User Experience | Passive interaction | More intuitive, less frustrating |
| Bandwidth for Control | High (irrelevant) | Low (but highly relevant information) |
| Safety in Monitoring | N/A | Can predict lapses in attention ~ |
The trade-off is clear: while invasive interfaces like Neuralink aim for high-bandwidth data transfer, neuroadaptive systems prioritize the relevance of information over its volume, capturing critical condensed decisions related to values and moral reasoning that occur at much lower bit rates [35].
Biohybrid Interfaces: Enhancing Integration with Biology
Core Concept and Comparative Advantage
Biohybrid neural interfaces represent the cutting edge of biomimetic design, aiming to overcome the most significant barrier to chronic implant stability: the foreign body reaction (FBR). These interfaces incorporate living biological components—such as cells, tissues, or bioactive molecules—into the device structure to create a more seamless and functional integration with host neural tissue [33] [36].
The core value for long-term translational research is the potential for dramatically improved biocompatibility and long-term signal stability. Traditional rigid implants (e.g., silicon, platinum) trigger a chronic inflammatory response, leading to glial scar formation that insulates the electrode and degrades signal quality over weeks or months [36]. Biohybrid approaches seek to trick the body into accepting the device as a more natural part of its environment, thereby mitigating the FBR and preserving the viability of surrounding neurons.
Experimental Protocols and Performance Data
Research in biohybrid interfaces spans multiple innovative strategies. A prominent protocol involves creating a "living electrode":
- Scaffold Fabrication: A soft, porous conductive scaffold is fabricated using materials like conductive hydrogels (e.g., PEDOT:PSS), soft elastomers (e.g., PDMS), or flexible meshes.
- Functionalization: The scaffold is coated with bioactive cues, such as cell-adhesion peptides (e.g., RGD, laminin) or anti-inflammatory drugs (e.g., dexamethasone).
- Cell Seeding: The scaffold is seeded with neural progenitor cells or supportive cells like astrocytes. These cells proliferate and form a living layer on the electrode.
- Implantation: The biohybrid construct is implanted into the target neural tissue.
- Integration: The living layer on the device promotes integration with the host tissue, encouraging neuronal ingrowth and reducing the activation of microglia and astrocytes that lead to scarring [33] [36].
Performance data from animal models is promising. The table below contrasts traditional implants with advanced biohybrid designs.
Table 3: Comparative Performance of Traditional vs. Biohybrid Neural Implants
| Performance Metric | Traditional Rigid Implant | Biohybrid / Biomimetic Implant |
|---|---|---|
| Chronic Signal Amplitude | Degrades by ~40-70% over 6 months | Maintains >80% amplitude over 6 months |
| Electrode Impedance | Increases significantly over time | Remains more stable |
| Neuronal Density at Interface | Reduced by ~40% | Near-normal density preserved |
| Glial Scar Thickness | Significant (tens of micrometers) | Greatly reduced or minimal |
| Long-term Biocompatibility | Poor | Excellent |
Other protocols include the development of "regenerative electrodes" that release neurotrophic factors like BDNF to promote neuron survival and the use of stent-like electrodes (e.g., Stentrode) that are implanted via blood vessels, avoiding direct brain tissue penetration altogether [33] [37].
Key Research Reagent Solutions
The development of biohybrid interfaces relies on a specialized toolkit of materials and biological factors.
Table 4: Essential Research Reagents for Biohybrid Interface Development
| Reagent Category | Specific Examples | Primary Function in Research |
|---|---|---|
| Conductive Polymers | PEDOT:PSS, Polypyrrole (PPy) | Form soft, electroactive coatings and scaffolds to reduce impedance and improve signal transduction. |
| Biomaterial Scaffolds | Polyimide, PDMS, SU-8, Hydrogels (e.g., GelMA) | Provide flexible, biocompatible substrates and encapsulation for electrodes. |
| Bioactive Coatings | Laminin, RGD peptides, L1 neural adhesion protein | Promote neuron adhesion and neurite outgrowth directly on the implant surface. |
| Controlled Release Systems | Dexamethasone-loaded hydrogels, BDNF-eluting coatings | Deliver anti-inflammatories or neurotrophic factors locally to suppress FBR and support neurons. |
| Cell Sources | Neural progenitor cells, Induced Pluripotent Stem Cell (iPSC)-derived neurons/glia | Create living, biologically active layers on devices to facilitate host integration. |
Integrated Discussion and Future Outlook
The convergence of closed-loop, neuroadaptive, and biohybrid technologies points toward a future of increasingly sophisticated and symbiotic neural interfaces. The most advanced systems on the horizon will likely be closed-loop, biohybrid implants that not only read and write neural information with high fidelity but are also fully integrated into the biological fabric of the brain, operating stably for decades. Meanwhile, non-invasive neuroadaptive technology will become woven into the fabric of everyday life, creating computing environments that are responsive to our cognitive and emotional needs.
The strategic choice between invasive and non-invasive approaches remains, and will continue to be, dictated by the risk-benefit calculus of the application. Invasive systems, propelled by advances in biohybrid design, will dominate in restoring function for severe neurological injuries and disorders [1] [37]. Non-invasive systems, enhanced by more powerful AI decoding, will expand in consumer wellness, mental health, and human-computer interaction [7] [32]. As these macro-trends evolve, they will not only provide researchers with powerful new tools but also necessitate proactive engagement with the profound ethical and regulatory questions they raise concerning data privacy, identity, and equity.
Research and Clinical Translation: Methodologies and Therapeutic Applications
Brain-Computer Interfaces (BCIs) represent a revolutionary technology that enables direct communication between the brain and external devices, bypassing traditional neuromuscular pathways. Within the broader thesis of neural interface research, the fundamental distinction between invasive and non-invasive approaches revolves around the critical trade-off between signal fidelity and clinical risk. Invasive BCIs, which involve surgically implanted electrodes that directly interface with brain tissue, offer unparalleled access to high-resolution neural signals but require neurosurgical intervention. In contrast, non-invasive approaches, such as electroencephalography (EEG), provide safer and more accessible platforms but contend with significant signal attenuation caused by the skull and scalp [38] [6].
This comparison guide objectively analyzes the performance of invasive BCIs against non-invasive alternatives, focusing specifically on their application in restoring motor function and communication for individuals with paralysis. The assessment is grounded in experimental data and clinical outcomes, providing researchers and drug development professionals with a clear evidence-based framework for evaluating these technologies. The core performance differentiator lies in the fundamental electrophysiology: invasive interfaces record detailed neural signals such as action potentials (APs) and local field potentials (LFPs), while non-invasive systems like EEG capture a spatially blurred and low-pass-filtered version of this activity, primarily from pyramidal neurons [6]. This biological reality creates an inherent performance gap that next-generation technologies are striving to narrow.
Performance Comparison: Invasive vs. Non-Invasive BCIs
The following tables synthesize quantitative data from clinical studies and commercial systems to compare the performance of invasive and non-invasive BCIs across key metrics and application-specific outcomes.
Table 1: Fundamental Signal and Performance Characteristics
| Performance Metric | Invasive BCI | Non-Invasive BCI |
|---|---|---|
| Spatial Resolution | Single neuron level (micrometers) [6] | Centimetre-scale resolution [38] |
| Temporal Resolution | Very High (up to several kHz) [6] | Lower (limited to <~90 Hz for EEG) [6] |
| Signal-to-Noise Ratio | High [38] | Low to Moderate, susceptible to EMG noise [38] |
| Information Transfer Rate | High (~100-200 bits/min) [38] | Low (~5-25 bits/min) [38] |
| Typical Control Latency | Low (enables real-time control) [39] | Higher due to signal processing demands [39] |
| Key Signal Types | Action Potentials (APs), Local Field Potentials (LFPs) [6] | EEG, MEG, fNIRS [8] [39] |
Table 2: Application-Specific Outcomes in Paralysis
| Application & Outcome | Invasive BCI Performance | Non-Invasive BCI Performance |
|---|---|---|
| Prosthetic/Arm Control | Multi-fingered robotic arm control for grasping and manipulation [1] [40] | Limited to simple, discrete commands for device control [39] |
| Communication Speed | Speech decoding up to 62 words per minute [1]; 97% accuracy [41] | P300-based spelling devices with slower rates (~5-10 words/min) [42] [39] |
| Somatosensory Feedback | Bidirectional systems enabling sensation restoration via cortical microstimulation [6] | Largely unidirectional; feedback is typically visual or auditory [6] |
| Clinical Target Population | Severe paralysis (e.g., Locked-In Syndrome, tetraplegia) [38] [40] | Moderate to severe paralysis, rehabilitation [38] [43] |
| Motor Function Recovery | Enables control of complex exoskeletons [44] | BCI-guided therapy shows 30-50% motor improvement in stroke rehab [43] |
Experimental Protocols and Methodologies
A critical evaluation of BCI performance requires an understanding of the underlying experimental methods. The following section details the protocols for key experiments that have established benchmarks for invasive BCI applications.
Protocol 1: Speech Decoding for Communication Restoration
Objective: To restore fluent communication in patients with paralysis or locked-in syndrome by decoding neural signals directly related to speech motor intention into text or synthetic speech [1] [41].
- Neural Signal Acquisition: A high-density electrode array (e.g., Utah Array or similar implant) is surgically placed over the cortical region responsible for speech motor control. This array records action potentials and local field potentials from populations of neurons [41] [6].
- Data Collection & Training: The patient is asked to attempt to speak or imagine speaking words and sentences. During this process, high-resolution neural data is recorded simultaneously with the intended speech output (or the text the patient intends to generate). This creates a large, labelled dataset mapping neural patterns to specific phonemes, words, or articulatory gestures [1].
- Decoder Training: Machine learning models (e.g., recurrent neural networks or linear decoders) are trained on the collected dataset. The model learns to map the complex neural activity patterns to the intended speech elements [1] [41].
- Real-Time Decoding: For communication, the trained decoder translates newly recorded neural signals into text or drives a speech synthesizer in real-time, allowing the patient to communicate at near-conversational speeds. Performance is validated by measuring output accuracy (e.g., word error rate) and information transfer rate (words per minute) [41].
Protocol 2: Robotic Arm Control for Motor Restoration
Objective: To enable individuals with tetraplegia to control a multi-degree-of-freedom robotic arm or prosthetic limb for performing activities of daily living [40] [6].
- Surgical Implantation: A microelectrode array (e.g., Utah Array) is implanted into the hand and arm area of the patient's primary motor cortex. This allows for recording from individual neurons tuned to specific movement directions, forces, and grips [40] [6].
- Neural Tuning Characterization: The patient observes or imagines performing various arm and hand movements. The firing rates of recorded neurons are analyzed to create a "tuning model" that correlates neural activity with specific movement parameters (e.g., velocity, position, grip type) [6].
- Closed-Loop System Calibration: The patient engages in closed-loop calibration, using their neural activity to control a cursor on a screen. This process allows the decoder algorithm to refine its parameters and for the patient's brain to adapt to the interface, a phenomenon known as neuroplasticity [6].
- Task Performance & Validation: The patient progresses to controlling a robotic arm to perform functional tasks, such as reaching for and grasping objects. Performance is quantitatively assessed using metrics like success rate, task completion time, and the number of degrees of freedom successfully controlled. The ultimate validation is the restoration of independent action, such as self-feeding [40].
BCI Closed-Loop Workflow: This diagram illustrates the core operational loop of an invasive BCI system for restoring function, highlighting the integration of neural signal decoding and sensory feedback.
The Scientist's Toolkit: Key Research Reagents & Materials
Successful development and experimentation in invasive BCI research rely on a suite of specialized materials and technological components. The table below details these essential tools and their functions.
Table 3: Essential Research Materials for Invasive BCI Development
| Tool / Material | Function in Research & Development |
|---|---|
| Microelectrode Arrays (e.g., Utah Array, Neuropixels) | The primary physical interface with the brain; designed to record extracellular action potentials and local field potentials from populations of neurons with high fidelity [8] [6]. |
| Hermetic Encapsulation | Provides a biocompatible, protective barrier around the implant electronics, shielding them from the corrosive biological environment and preventing moisture ingress to ensure long-term stability [41]. |
| Neural Signal Acquisition ASIC | An Application-Specific Integrated Circuit (e.g., 128-channel acquisition chip) that performs front-end amplification, filtering, and analog-to-digital conversion of weak neural signals directly at the source, minimizing noise [41]. |
| Biocompatible Substrates (e.g., Polyimide, SU-8, Graphene) | Flexible and durable materials used for thin-film electrodes and implant substrates to minimize tissue damage, scarring, and the chronic immune response, thereby improving signal longevity [41] [40]. |
| Cortical Microstimulation Circuitry | Enables bidirectional functionality by delivering precise, low-current electrical pulses to neural tissue, thereby restoring sensory feedback (artificial sensation) or modulating neural circuits for therapeutic purposes [6]. |
| Decoder Algorithms (e.g., Kalman Filters, RNNs) | Machine learning models that translate raw, high-dimensional neural data into intended movement kinematics (velocity, grip force) or discrete commands (phonemes, letters) in real-time [1] [6]. |
BCI Technology Trade-offs: A logical breakdown of the core advantages, constraints, and resultant application profiles that distinguish invasive and non-invasive BCI approaches.
The objective comparison of performance data solidifies the position of invasive BCIs as the superior solution for restoring complex motor functions and high-bandwidth communication in cases of severe paralysis. Their ability to decode single-neuron activity and deliver bidirectional communication via cortical stimulation provides a level of control and feedback that non-invasive systems cannot currently match, as evidenced by achievements in robotic arm control and rapid speech decoding [1] [40] [6]. The primary trade-off remains the requirement for neurosurgery and the associated risks, which are diminishing with improved surgical techniques and more biocompatible materials [6].
The future of neural interfaces will likely not be a victory for one modality over the other, but a coexistence shaped by application-specific needs. Invasive interfaces are poised to address the most severe neurological disorders and serve as a platform for foundational neuroscience discovery. Concurrently, advances in non-invasive technologies like high-density EEG and wearable magnetoencephalography (MEG) are expected to expand their utility in rehabilitation, consumer applications, and as a screening tool for potential invasive implant candidates [8] [39]. For researchers and clinicians, this evolving landscape underscores the importance of a nuanced understanding of both invasive and non-invasive paradigms to effectively develop and deploy these transformative technologies.
The field of neural interfaces is undergoing a transformative shift from invasive to non-invasive approaches, driven by advancements in technology and a growing understanding of neural mechanisms. While invasive neural interfaces provide high spatial resolution and signal quality, they require surgical implantation, carrying risks of infection, tissue damage, and other complications [17]. In contrast, non-invasive interfaces offer safer, more accessible alternatives for clinical monitoring and therapeutic intervention, though they have historically faced challenges with signal quality and spatial resolution [17]. This evolution is particularly evident in three key clinical areas: epilepsy monitoring, stroke rehabilitation, and neurostimulation therapy.
The fundamental distinction between these approaches lies in their method of interaction with the nervous system. Invasive interfaces, such as stereoelectroencephalography (SEEG) and subdural electrodes (SDE), require surgical placement directly in or on brain tissue [45]. These methods provide superior signal quality for localizing seizure origins but are associated with higher infection rates (1.8% for SDE versus 0.3% for SEEG) and other surgical risks [45]. Non-invasive modalities leverage external sensors or stimulators to record or modulate brain activity through the scalp, making them suitable for long-term monitoring and broader patient populations [17].
This review comprehensively compares the product performance and experimental efficacy of non-invasive modalities against both invasive alternatives and other non-invasive approaches across epilepsy monitoring, stroke rehabilitation, and neurostimulation therapy, providing researchers with objective data for clinical and research applications.
Epilepsy Monitoring: From Invasive Localization to Non-Invasive Detection
Comparative Efficacy of Invasive Monitoring Techniques
For patients with drug-resistant epilepsy (DRE) requiring surgical evaluation, invasive monitoring remains the gold standard for precise seizure focus localization. A recent meta-analysis of 81 studies comparing the two primary invasive modalities reveals important clinical trade-offs:
Table 1: Comparison of Invasive Epilepsy Monitoring Techniques [45]
| Parameter | Stereoelectroencephalography (SEEG) | Subdural Electrodes (SDE) | P-value |
|---|---|---|---|
| Operative Time | 185 minutes | 164 minutes | 0.50 |
| Inpatient Monitoring Time | 8.9 days | 8.7 days | 0.81 |
| Seizure Focus Identification | 95.4% | 91.9% | 0.25 |
| Subsequent Resective Surgery | 74.0% | 85.6% | <0.01 |
| Overall Adverse Events | 8.0% | 10.6% | 0.22 |
| Infection Rate | 0.3% | 1.8% | <0.01 |
| Seizure Freedom Post-Resection | 62.7% | 63.4% | 0.87 |
This analysis demonstrates that while SDE leads to higher rates of subsequent resective surgery, it carries a significantly higher infection risk compared to SEEG [45]. Both modalities eventually achieve equivalent seizure freedom outcomes, informing clinical risk-benefit decisions.
Emerging Non-Invasive Monitoring and Intervention
For broader epilepsy management, non-invasive approaches offer promising alternatives for seizure detection and reduction, particularly valuable for long-term monitoring and patients who are not candidates for invasive procedures.
Wearable EEG Monitoring Systems Research into wearable EEG devices demonstrates the potential for long-term, non-invasive epilepsy monitoring. One development platform implemented seizure detection algorithms on a parallel ultra-low-power (PULP) embedded system, achieving 300 hours of continuous monitoring on a 300 mAh battery [46]. Employing subject-specific approaches with 4 temporal channels and an 8-second window size, these systems reached 100% sensitivity with zero false positives, meeting critical patient and caregiver requirements for reliable home monitoring [46].
Non-Invasive Neuromodulation Therapies For treatment, several non-invasive neuromodulation techniques show potential for reducing seizure frequency in DRE:
Table 2: Non-Invasive Neuromodulation for Drug-Resistant Epilepsy [47]
| Technique | Proposed Mechanism | Evidence Level | Key Efficacy Findings |
|---|---|---|---|
| Transcranial Direct Current Stimulation (tDCS) | Modulates cortical excitability with weak direct current | Meta-analysis of RCTs | Significant reduction in seizure frequency at 4 weeks (MD=-4.72) and 8 weeks (MD=-3.39) |
| Transcutaneous Vagus Nerve Stimulation (tVNS) | Indirect brain modulation via peripheral nerve stimulation | Meta-analysis of 3 RCTs (n=280) | Significant mean difference in seizure reduction (MD=-3.29) vs control |
| Repetitive Transcranial Magnetic Stimulation (rTMS) | Magnetic field induction of electrical currents in cortex | Systematic review | Mixed results across trials; insufficient evidence for definitive conclusions |
| Low-Intensity Focused Ultrasound (LI-FUS) | Precise stimulation of deep brain structures | Pilot safety studies | No tissue damage detected; efficacy studies ongoing |
A systematic review protocol registered in PROSPERO (CRD42023446051) aims to further investigate the efficacy, safety, and optimal stimulation parameters for these non-invasive neuromodulation techniques, highlighting the ongoing development in this field [47].
Stroke Rehabilitation: Harnessing Neuroplasticity with Non-Invasive Stimulation
Evidence Synthesis for Motor Recovery
Non-invasive brain stimulation (NIBS) represents a promising adjuvant strategy to enhance conventional rehabilitation for stroke-related motor impairments. An umbrella review of 56 meta-analyses provides comprehensive evidence within the International Classification of Functioning, Disability and Health (ICF) framework, focusing specifically on repetitive transcranial magnetic stimulation (rTMS) and transcranial direct current stimulation (tDCS) [48].
Table 3: NIBS Efficacy for Stroke Motor Recovery by ICF Domain [48]
| ICF Domain | Technique | Effect Size (SMD) | Certainty of Evidence | Key Outcomes |
|---|---|---|---|---|
| Body Structure/ Function | rTMS | -0.32 to -0.97 | Low to Moderate | Improved upper-limb motor impairment, general neurological function |
| Body Structure/ Function | tDCS | -0.22 to -1.54 | Very Low | Small effects on motor impairment; large effects in small trial subsets |
| Activity | rTMS | -0.82 | Moderate | Consistent benefits for activities of daily living (ADL) |
| Activity | tDCS | -0.31 | Very Low | Small effects on upper-limb activity; inconsistent ADL effects |
| Activity | rTMS | -0.35 to -0.97 | Low to Moderate | Variable effects on mobility from small to large |
The review concluded that rTMS was more frequently associated with moderate to large effect sizes for body structure/function outcomes, while tDCS demonstrated smaller effects supported by very low certainty evidence due to significant heterogeneity, imprecision, and protocol variability [48].
Comparative Neurostimulation Approaches
Beyond tDCS and rTMS, other stimulation modalities are being investigated for stroke rehabilitation:
Vagus Nerve Stimulation (VNS) Following a positive phase 3 sham-controlled trial in 2021, the FDA approved a VNS device for patients in the chronic stage of ischemic stroke with persistent moderate to severe upper extremity impairment [49]. While the benefit is considered modest and requires pairing with intensive rehabilitation, it represents a significant milestone for non-invasive stroke therapy.
Novel Rehabilitation Technologies Advanced technologies are complementing neurostimulation for motor recovery:
- Robotic therapy: Provides high-intensity, task-specific training but has shown limited efficacy for severely impaired patients [49].
- Virtual reality (VR) therapy: A meta-review of 57 systematic reviews concluded that VR can improve upper and lower limb function, balance, gait, and possibly cognition [49]. Advantages include relatively low cost, enhanced patient engagement, and minimal side effects.
Neurostimulation Therapy: Expanding Applications Beyond Stroke and Epilepsy
Non-Invasive Neurostimulation for Insomnia
The application of non-invasive neurostimulation has expanded to sleep disorders, particularly insomnia, where it offers advantages over pharmacological approaches that can cause cognitive impairment, adverse events, and long-term dependence [50]. Recent research has identified several promising modalities:
Table 4: Non-Invasive Neurostimulation Modalities for Insomnia [50]
| Technique | Mechanism of Action | Advantages | Disadvantages |
|---|---|---|---|
| Transcranial Magnetic Stimulation (TMS) | Magnetic fields induce electrical currents affecting cortical excitability | Causes prolonged neuroplastic changes | Contraindicated in CNS diseases; high cost |
| Transcranial Electrical Stimulation (tES) | Weak electrical current modulates neural activity | Adjustable, reversible parameters; includes tDCS/tACS | Effects typically reversible after stimulation ceases |
| Transcutaneous Auricular Vagus Nerve Stimulation (taVNS) | Stimulates auricular vagus nerve branches affecting multiple brain regions | Non-invasive, safe, and convenient | Limited long-term efficacy data |
| Virtual Reality (VR) | Computer-generated sensory replacement and interaction | Less time-consuming, cost-effective, fewer safety concerns | Requires user compliance and equipment access |
| Biofeedback | Provides physiological data to teach self-regulation skills | No dependence or withdrawal; can be used independently | Slower effects similar to physical exercise |
Emerging Technologies and Home-Use Devices
The neurostimulation landscape is rapidly evolving with technological advancements:
- Transcranial focused ultrasound (tFUS): Can target cortical, subcortical, and deep brain regions with high precision [49].
- Home-use neurofeedback devices: Consumer-grade devices like Sens.ai, Muse, and Mendi are making neurofeedback more accessible, though most maintain wellness rather than clinical classifications [51].
- Photobiomodulation therapy: Uses light stimulation to modulate neural activity [50].
Experimental Protocols and Methodologies
Standardized Protocols for Non-Invasive Neuromodulation
To ensure reproducibility and comparability across studies, rigorous experimental protocols are essential. For non-invasive neuromodulation in drug-resistant epilepsy, a standardized systematic review protocol has been developed with the following key methodological components [47]:
Search Strategy Framework
- Databases: Comprehensive searches across PubMed, OVID Embase, OVID Medline, and Web of Science
- Timeframe: Studies published from January 1, 1985, to May 22, 2024, with ongoing updates
- Keywords: Structured searches using controlled vocabulary and Boolean operators for each intervention type
Eligibility Criteria
- Study Designs: Randomized control trials, cohort studies, and case-control studies
- Participants: Human participants with drug-resistant epilepsy exclusively
- Interventions: Specific non-invasive techniques (rTMS, tDCS, tACS, LI-FUS, tVNS, TNS) as primary interventions
Outcome Measures
- Primary Efficacy: Seizure reduction measured by mean/median change in seizure frequency and responder rate
- Safety Profile: Percentage of patients reporting specified adverse events
- Stimulation Parameters: Optimal protocol settings for each intervention type
This systematic review protocol (PROSPERO CRD42023446051) enables rigorous comparison across stimulation methods using consistent methodology [47].
Research Reagent Solutions and Experimental Tools
Table 5: Essential Research Materials for Non-Invasive Neural Interface Studies
| Item | Function/Application | Examples/Specifications |
|---|---|---|
| EEG Recording Systems | Neural signal acquisition for monitoring and neurofeedback | Systems with 7-19 electrodes; dry vs. wet electrode options [51] |
| Transcranial Magnetic Stimulator | Non-invasive brain stimulation using magnetic fields | rTMS systems with stimulation intensity at 80-120% motor threshold [50] |
| Transcranial Electrical Stimulators | Neuromodulation via weak electrical currents | tDCS/tACS devices with 1-2 mA current intensity [50] |
| Transcutaneous Vagus Nerve Stimulators | Peripheral nerve stimulation for central effects | taVNS devices with electrodes placed in external auditory canal [50] |
| Virtual Reality Systems | Immersive environments for rehabilitation and therapy | Head-worn devices with motion tracking sensors [50] |
| Biofeedback Systems | Physiological signal monitoring for self-regulation | Respiratory, cardiovascular, neuromuscular, and neurofeedback modalities [50] |
Signaling Pathways and Workflow Visualization
Non-Invasive Neuromodulation Mechanisms
The therapeutic effects of non-invasive neuromodulation techniques involve complex neural pathways and mechanisms. The following diagram illustrates the primary signaling pathways through which these interventions achieve their clinical effects:
Non-Invasive Neuromodulation Signaling Pathways
Clinical Research Workflow for Therapeutic Development
The development and validation of non-invasive neural interfaces follows a systematic research pathway from concept to clinical application:
Therapeutic Development Research Workflow
The evolution of neural interfaces reflects a continuing tension between the superior precision of invasive approaches and the safety and accessibility of non-invasive alternatives. In epilepsy monitoring, invasive techniques like SEEG and SDE remain essential for surgical planning, with SEEG demonstrating a superior safety profile for infection risk [45]. However, emerging non-invasive technologies show promise for long-term monitoring and seizure detection [46]. In stroke rehabilitation, rTMS has accumulated more substantial evidence supporting its benefits, particularly for activities of daily living, while tDCS shows potential but with lower certainty of evidence [48]. For neurostimulation therapy across conditions like insomnia, the non-invasive modality portfolio has expanded significantly, offering multiple mechanisms for modulating neural function without surgical risks [50].
Future directions point toward increasingly personalized parameter optimization, technological miniaturization for home-based use, and integration with other therapeutic modalities. As the field advances, the distinction between invasive and non-invasive approaches may blur with the development of minimally invasive technologies that balance precision with safety. For researchers and clinicians, selection of neural interface strategies must be guided by specific clinical questions, patient characteristics, and the evolving evidence base comparing both efficacy and risk profiles across this rapidly developing therapeutic landscape.
The integration of neural interfaces into drug development represents a paradigm shift in how researchers identify therapeutic biomarkers and monitor treatment efficacy. These sophisticated systems, which facilitate direct communication between the brain and external devices, are increasingly critical for evaluating neuroactive compounds in both clinical and preclinical settings [52]. The fundamental divergence between invasive and non-invasive approaches creates a strategic trade-off between signal fidelity and practical implementation that directly impacts their application in pharmaceutical research [38] [53]. Invasive neural interfaces, implanted directly into brain tissue or on its surface, provide unparalleled access to neural signals with high spatial and temporal resolution, enabling researchers to detect subtle neurophysiological changes in response to drug candidates [38] [53]. Conversely, non-invasive approaches such as electroencephalography (EEG) and functional near-infrared spectroscopy (fNIRS) offer safer, more scalable alternatives for longitudinal studies, though with reduced signal quality [38] [8].
Within drug development pipelines, these technologies serve dual purposes. First, they enable the identification of quantifiable biomarkers—electrophysiological patterns, hemodynamic responses, or oscillatory dynamics—that correlate with disease states and treatment responses [52]. Second, they provide direct windows into central nervous system drug effects, allowing researchers to monitor pharmacodynamics with unprecedented temporal precision [54]. This capability is particularly valuable for assessing drugs targeting neurological and psychiatric disorders, where traditional biomarkers often lack the sensitivity to detect early efficacy signals [54]. As the neurotechnology landscape evolves, with the overall brain-computer interface market forecast to grow to over US$1.6 billion by 2045, pharmaceutical researchers are positioned to leverage these advances for more efficient, targeted drug development [8].
Comparative Analysis of Neural Interface Technologies
The selection of appropriate neural interface technology for drug development requires careful consideration of technical specifications, application requirements, and practical constraints. Invasive systems typically provide superior signal quality but introduce additional surgical and safety considerations, while non-invasive approaches offer greater accessibility at the cost of signal resolution [38]. This fundamental trade-off directly impacts their utility across different stages of the drug development pipeline, from early preclinical target engagement studies to large-scale clinical trials.
Table 1: Technical Comparison of Neural Interface Technologies for Drug Development
| Parameter | Invasive BCIs | Semi-Invasive BCIs | Non-Invasive BCIs |
|---|---|---|---|
| Spatial Resolution | Highest (single neuron level) [38] | Moderate (neural population level) [38] | Lowest (regional brain activity) [38] |
| Temporal Resolution | <1 ms (action potentials) [53] | ~10 ms (local field potentials) [53] | ~100 ms (EEG) to seconds (fNIRS) [8] |
| Signal Quality | Highest signal-to-noise ratio [38] | Moderate signal-to-noise ratio [38] | Lowest signal-to-noise ratio [38] |
| Information Transfer Rate | ~100-200 bits/minute [38] | ~40-60 bits/minute [38] | ~5-25 bits/minute [38] |
| Surgical Risk | High (requires brain surgery) [38] | Moderate (requires craniotomy) [38] | None [38] |
| Long-term Stability | Limited (scar tissue formation) [38] [53] | Better than invasive [38] | Highest [38] |
| Ideal Drug Development Application | High-precision biomarker discovery [53] | Chronic toxicity monitoring [38] | Large-scale clinical trials [37] |
Table 2: Suitability for Drug Development Applications
| Application | Invasive BCIs | Semi-Invasive BCIs | Non-Invasive BCIs |
|---|---|---|---|
| Biomarker Identification | Excellent for single-neuron biomarkers [53] | Good for localized population biomarkers [38] | Limited to macro-scale biomarkers [38] |
| Target Engagement Verification | Direct measurement of drug effects on specific circuits [53] | Good regional assessment [38] | Indirect inference from surface signals [52] |
| Treatment Efficacy Monitoring | Limited by surgical risks for long-term use [38] | Suitable for medium-term monitoring [38] | Ideal for repeated measures [37] |
| Preclinical Research | Extensive use in animal models [53] | Limited use in specialized models [38] | Challenging due to species differences [8] |
| Clinical Trials | Restricted to severe conditions (e.g., paralysis) [38] | Intermediate scope [38] | Broad applicability across indications [37] |
From a drug development perspective, each neural interface category offers distinct advantages. Invasive systems, particularly those using depth electrodes or high-density microarrays, enable researchers to detect drug-induced changes in specific neuronal populations with millisecond precision—critical for characterizing fast-acting neurotherapeutics [53]. Semi-invasive approaches, such as electrocorticography (ECoG), provide a balanced solution for monitoring regional drug effects over weeks to months, making them suitable for chronic toxicity studies [38]. Non-invasive technologies offer the practical advantage of rapid deployment across multiple study sites, enabling standardized efficacy assessment in large-scale clinical trials [37] [8]. The choice between these technologies ultimately depends on the specific research question, with each providing complementary insights into drug effects on neural systems.
Experimental Approaches for Biomarker Identification
Methodologies for Neural Biomarker Discovery
The identification of neural biomarkers for drug development employs specialized experimental protocols designed to capture disease-relevant neural signatures and their modulation by therapeutic interventions. For invasive approaches, the gold standard methodology involves stereotactic implantation of electrode arrays—such as the Utah Array or Neuropixels probes—into target brain regions associated with specific disease pathologies [53]. Following surgical recovery, researchers record baseline neural activity, including action potentials from individual neurons and local field potentials from neuronal populations, while subjects engage in cognitive tasks or during resting state [53]. Drug candidates are then administered, and changes in neural firing patterns, oscillatory dynamics, and network connectivity are quantified using advanced signal processing techniques.
Non-invasive biomarker identification follows a similar conceptual framework but utilizes fundamentally different acquisition technologies. High-density EEG systems with 64-256 electrodes capture electrical activity from the scalp surface, while fNIRS devices measure hemodynamic responses through infrared sensors [8]. Functional MRI (fMRI) provides complementary information about drug-induced changes in blood oxygenation levels with excellent spatial resolution [52]. The experimental workflow typically involves repeated testing sessions to establish baseline variability, followed by acute or chronic drug administration periods to identify reproducible neurophysiological signatures of target engagement [54].
Neural Biomarker Identification Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Neural Interface Experiments
| Item | Function | Application Notes |
|---|---|---|
| Multielectrode Arrays (Utah Array, Neuropixels) | Record action potentials and local field potentials [53] | Invasive studies requiring single-neuron resolution [53] |
| EEG Cap Systems (wet/dry electrodes) | Scalp surface potential measurement [8] | Non-invasive human studies; dry electrodes enable longer recordings [8] |
| fNIRS Headsets | Hemodynamic response monitoring via infrared [8] | Complementary to EEG; better spatial resolution [8] |
| Signal Amplifiers & DACs | Neural signal conditioning and digitization [53] | Critical for maintaining signal fidelity across all modalities [53] |
| Stereotactic Frames | Precise electrode implantation [38] | Essential for invasive animal and human studies [38] |
| Biocompatible Coatings | Reduce tissue response to implants [53] | Improve long-term signal stability in chronic studies [53] |
| Spike Sorting Software | Identify individual neurons from recorded data [53] | Essential for invasive biomarker discovery [53] |
| Spectral Analysis Tools | Quantify oscillatory power in frequency bands [53] | Standard for EEG and LFP analysis across modalities [53] |
Successful execution of neural biomarker studies requires specialized equipment and computational resources. For invasive approaches, microelectrode arrays with high channel counts (256-1000+ electrodes) enable researchers to capture distributed neural representations of drug effects across multiple brain regions simultaneously [53]. Signal integrity must be maintained through high-performance acquisition systems with appropriate sampling rates (≥30 kHz for action potentials, ≥1 kHz for local field potentials) and minimal electrical noise [53]. Non-invasive studies benefit from recent advances in dry electrode technology, which eliminate the need for conductive gels and reduce setup time—particularly advantageous for clinical trials requiring efficient multisite data collection [8].
Computational resources represent an equally critical component of the modern neural biomarker pipeline. Machine learning algorithms, particularly deep learning networks, have demonstrated remarkable capability in decoding complex neural patterns associated with drug effects [53] [31]. These systems can identify subtle multivariate signatures that escape detection by conventional statistical approaches, potentially revealing novel biomarker combinations that predict treatment response [31]. The integration of artificial intelligence with neural interfaces is creating unprecedented opportunities for biomarker discovery in drug development [31].
Treatment Efficacy Monitoring Protocols
Methodologies for Longitudinal Efficacy Assessment
Monitoring treatment efficacy through neural interfaces employs specialized protocols designed to track neurophysiological changes throughout therapeutic interventions. For chronic conditions requiring long-term medication, non-invasive approaches offer particular utility through repeated measurements without cumulative risk [37]. The standard methodology involves establishing a pre-treatment baseline through multiple recording sessions to account for natural variability in neural signals [54]. Following treatment initiation, patients undergo periodic monitoring using consistent experimental conditions—typically combining resting-state recordings with task-based assessments relevant to the target disorder (e.g., working memory tasks for cognitive impairment, emotion recognition tasks for mood disorders) [54].
Invasive monitoring protocols, while limited to specialized populations, provide unparalleled insight into neurotherapeutic mechanisms. The BrainGate clinical trial, for instance, has demonstrated the feasibility of long-term intracortical recording in humans, showing that stable neural signals can be obtained for over 1000 days in some participants [52]. These chronic interfaces enable continuous, high-fidelity tracking of drug effects on neural circuits, capturing dynamics that would be inaccessible through intermittent clinic visits [52]. Such approaches are particularly valuable for establishing pharmacokinetic-pharmacodynamic relationships for CNS drugs, where the timing of neural effects relative to drug concentration is critical for understanding mechanisms of action [54].
Treatment Efficacy Monitoring Protocol
Data Analysis and Interpretation Framework
The interpretation of neural efficacy data requires sophisticated analytical approaches that account for the multidimensional nature of neural signals. For both invasive and non-invasive data, analytical pipelines typically include time-frequency decomposition to quantify oscillatory activity in relevant frequency bands (delta, theta, alpha, beta, gamma), functional connectivity analysis to assess drug effects on network organization, and event-related potential/field analysis for task-based paradigms [53] [54]. The critical analytical challenge involves distinguishing true drug-related neural changes from spontaneous fluctuations and non-specific factors such as alertness, motivation, or practice effects.
Machine learning approaches are increasingly employed to address this challenge through multivariate pattern analysis that identifies complex neural signatures predictive of clinical outcomes [53] [31]. These methods can integrate information across multiple neural features (oscillatory power, connectivity, spatial patterns) to generate composite efficacy metrics with greater sensitivity than individual measures [31]. For pharmaceutical developers, these advanced analytical capabilities enable more efficient trial designs through early identification of promising compounds and precise dose selection based on neural response curves [54].
The convergence of neural interface technology with artificial intelligence is creating particularly powerful frameworks for treatment efficacy assessment. Companies like Synchron have demonstrated integration of neural data with AI platforms such as NVIDIA's Holoscan, enabling real-time analysis of neural signals during therapeutic interventions [37]. Such systems can potentially identify efficacy signals earlier than conventional clinical endpoints, accelerating drug development timelines for neurological and psychiatric conditions [37] [31].
Comparative Performance Data: Invasive vs. Non-Invasive Approaches
Quantitative Performance Metrics
The selection between invasive and non-invasive neural interfaces for specific drug development applications requires careful consideration of empirical performance data. Direct comparisons reveal stark trade-offs between signal quality, information content, and practical implementation across technology categories. These differences directly impact their utility for various stages of pharmaceutical research, from early biomarker discovery to large-scale clinical trials.
Table 4: Experimental Performance Comparison Across Neural Interface Types
| Performance Metric | Invasive BCIs | Semi-Invasive BCIs | Non-Invasive BCIs |
|---|---|---|---|
| Spatial Resolution | 50-400 μm (individual neurons) [38] | 1-10 mm (neural populations) [38] | 10-20 mm (brain regions) [38] |
| Temporal Resolution | <1 ms (action potentials) [53] | 5-10 ms (local field potentials) [38] | 1-100 ms (EEG) to seconds (fNIRS) [8] |
| Signal-to-Noise Ratio | Highest (direct neural contact) [38] | High (minimal tissue attenuation) [38] | Moderate to low (skull attenuation) [38] |
| Target Engagement Detection Sensitivity | Can detect drug effects on single neurons [53] | Identifies regional drug effects [38] | Limited to larger-scale drug effects [52] |
| Participant Tolerance | Poor (surgical implantation required) [38] | Moderate (requires craniotomy) [38] | Excellent (non-invasive) [37] |
| Multisite Deployment Feasibility | Low (specialized surgical centers) [38] | Moderate (medical centers) [38] | High (clinical research sites) [37] |
Table 5: Drug Development Application Performance
| Application Scenario | Invasive BCIs | Semi-Invasive BCIs | Non-Invasive BCIs |
|---|---|---|---|
| Preclinical Mechanism Studies | Excellent (direct circuit-level analysis) [53] | Good (regional analysis) [38] | Limited (indirect measures only) [8] |
| Phase I Target Engagement | Limited to special populations [38] | Emerging capability [38] | Established capability [37] |
| Large-scale Clinical Trials | Not feasible [38] | Limited feasibility [38] | Standard approach [37] |
| Chronic Safety Monitoring | Limited by tissue response [53] | Suitable for medium-term [38] | Ideal for long-term monitoring [37] |
| Biomarker Qualification | High precision for circuit biomarkers [53] | Moderate precision [38] | Population-level biomarkers only [52] |
Strategic Implementation Considerations
Beyond technical specifications, the implementation of neural interfaces in drug development programs requires consideration of practical, regulatory, and ethical factors. Invasive approaches, while offering superior signal quality, face significant regulatory hurdles and ethical considerations that limit their application to severe conditions with few alternative monitoring options [38] [53]. The surgical procedures required for implantation carry risks of infection, hemorrhage, and neurological deficits that must be carefully weighed against potential scientific benefits [38]. Additionally, the long-term stability of invasive interfaces remains challenging due to the brain's foreign body response, which can lead to signal degradation over timescales relevant to chronic drug studies [53].
Non-invasive systems address many of these limitations through substantially improved safety profiles and greater participant acceptability [37]. However, they introduce their own methodological challenges, particularly regarding signal standardization across sessions and sites [8]. Movement artifacts, electrode impedance variations, and environmental noise can significantly impact data quality, requiring rigorous quality control procedures during clinical trials [8]. Recent advances in dry electrode technology and hardware miniaturization are addressing these challenges, making non-invasive neural interfaces increasingly practical for large-scale pharmaceutical studies [8].
The emerging category of semi-invasive interfaces, including endovascular approaches developed by companies like Synchron, offers a promising middle ground with improved signal quality compared to non-invasive methods while avoiding the major risks of fully invasive implants [37]. These devices, implanted via blood vessels rather than open brain surgery, demonstrate the ongoing innovation in neural interface technology that may eventually overcome current trade-offs between signal quality and safety [37]. For pharmaceutical researchers, this evolving landscape offers an expanding toolkit for assessing CNS drug effects with increasing precision and practicality.
The integration of neural interfaces into drug development pipelines represents a transformative approach to biomarker identification and treatment efficacy monitoring. The comparative analysis presented in this guide demonstrates that invasive and non-invasive technologies offer complementary strengths, with selection criteria dependent on specific research questions, development stages, and practical constraints. Invasive systems provide unparalleled resolution for mechanistic studies and precision biomarker discovery, while non-invasive approaches enable scalable efficacy assessment across diverse patient populations [38] [37].
For pharmaceutical developers, strategic implementation requires matching technology capabilities to specific development objectives. Early-stage programs targeting novel neural mechanisms may benefit from invasive approaches in preclinical models or highly selected patient populations to establish proof-of-concept and identify sensitive biomarkers [53]. As programs advance toward larger clinical trials, non-invasive technologies provide practical tools for monitoring treatment effects across multiple sites [37]. The ongoing innovation in neural interface technology, particularly in semi-invasive approaches and AI-enhanced signal processing, promises to further enhance their utility in drug development [37] [31].
As these technologies continue to evolve, their integration into standard drug development practice offers the potential for more efficient evaluation of neurotherapeutics, with neural biomarkers providing early efficacy signals that can accelerate decision-making. Companies that strategically leverage these tools across their development portfolios will be positioned to advance more effective CNS treatments with greater precision and efficiency.
Neural decoding—the process of interpreting brain activity to infer stimuli, intent, or behavior—represents a critical frontier in neuroscience and neuroengineering. The evolution of this field is inextricably linked to the ongoing debate between two technological paradigms: invasive neural interfaces, which provide high-fidelity signals from implanted electrodes, and non-invasive systems, which prioritize safety and accessibility by measuring brain activity from outside the skull [38] [55]. This comparison guide examines how advanced machine learning, particularly multimodal and self-supervised approaches, is reshaping this landscape by enhancing decoding capabilities across both interface types.
Each interface category presents a distinct set of trade-offs. Invasive systems offer unparalleled signal quality with high spatial and temporal resolution, capturing individual neuron activity but requiring complex brain surgery and carrying risks of tissue damage and scar formation [38] [55]. Non-invasive alternatives, while safer and more accessible, contend with significantly lower signal-to-noise ratios due to skull interference and limited capacity to record from deep brain structures [38]. Recent innovations in artificial intelligence are not merely incrementally improving decoding algorithms but are fundamentally transforming how we leverage the respective advantages of each interface type, enabling researchers to extract more meaningful information than previously thought possible from neural signals.
Comparative Performance Analysis of Neural Decoding Approaches
The decoding performance gap between invasive and non-invasive interfaces remains substantial, though machine learning advances are pushing the boundaries of what each can achieve. The table below summarizes key quantitative differences in their decoding capabilities:
Table 1: Performance comparison of invasive vs. non-invasive neural interfaces for decoding
| Performance Metric | Invasive Interfaces | Non-Invasive Interfaces |
|---|---|---|
| Signal Quality | Highest signal-to-noise ratio; records single neuron activity [38] | Lowest signal-to-noise ratio due to skull interference [38] |
| Information Transfer Rate | ~100-200 bits/minute [38] | ~5-25 bits/minute [38] |
| Spatial Resolution | Precise; pinpoints specific brain regions [38] | Reduced; blurs brain activity patterns [38] |
| Temporal Resolution | Millisecond precision for neural spiking activity | Limited by signal conduction through tissue and bone |
| Decoding Applications | Advanced prosthetic control, communication for severe disabilities [38] | Consumer-grade applications, rehabilitation, cognitive monitoring [38] |
Beyond this fundamental divide, specific algorithmic innovations demonstrate markedly different performance characteristics. The recently introduced Neural Encoding and Decoding at Scale (NEDS) framework exemplifies cutting-edge capabilities. As a multimodal, multi-task model, NEDS employs a novel masking strategy during training that alternates between neural, behavioral, within-modality, and cross-modality masking [56]. This approach enables simultaneous encoding (predicting neural activity from behavior) and decoding (predicting behavior from neural activity), achieving state-of-the-art performance in both tasks when pretrained on multi-animal data and fine-tuned on new subjects [56].
Table 2: Performance of advanced neural decoding algorithms and architectures
| Algorithm/Architecture | Interface Compatibility | Key Innovation | Reported Performance |
|---|---|---|---|
| NEDS (Neural Encoding and Decoding at Scale) [56] | Primarily invasive (tested on Neuropixels data) | Multi-task masking for bidirectional neural-behavior translation | State-of-the-art for both encoding and decoding; emergent brain region prediction from embeddings |
| Boosted Neural Min-Sum (NMS) Decoder [57] | Not specific | Novel training with uncorrected vectors, block-wise training, dynamic weight sharing | Meets 6G xURLLC requirement (FER below 10⁻⁹) for LDPC codes |
| EEG-Deformer [58] | Non-invasive (EEG) | Dense convolutional transformer architecture | Enhanced BCI performance for EEG-based applications |
| REI-Net [58] | Non-invasive (Motor Imagery EEG) | Reference Electrode Standardization + 3D CNN | Improved motor imagery classification accuracy |
For non-invasive systems, deep learning architectures are demonstrating remarkable improvements in overcoming inherent signal limitations. EEG-Deformer, which utilizes a dense convolutional transformer architecture, and REI-Net, which combines reference electrode standardization with 3D convolutional neural networks, both show significant enhancements in classification accuracy for electroencephalography (EEG)-based brain-computer interfaces [58]. These approaches leverage the capacity of deep networks to learn complex spatial-temporal patterns from noisy, low-resolution signals, effectively expanding the functional capabilities of non-invasive systems.
Experimental Protocols and Methodologies
The NEDS Framework: A Protocol for Multimodal Decoding
The NEDS (Neural Encoding and Decoding at Scale) framework represents a paradigm shift in neural decoding methodology by unifying encoding and decoding within a single, multimodal architecture. The experimental protocol for implementing and validating NEDS involves several critical stages:
Dataset Curation: Utilizing large-scale, standardized datasets is fundamental. The International Brain Laboratory (IBL) repeated site dataset, which includes Neuropixels recordings from 83 mice performing the same visual decision-making task, serves as an ideal foundation. This dataset provides neural recordings targeting the same five brain regions across multiple subjects, enabling effective multi-animal training [56].
Model Architecture: NEDS implements a multimodal transformer where each modality (neural activity and behavior) is tokenized independently and processed through a shared transformer backbone. This architecture allows the model to learn rich, cross-modal representations [56].
Multi-Task Masking Strategy: The core innovation involves a novel training regimen that alternates between different masking patterns: neural masking (predicting neural activity from behavior), behavioral masking (predicting behavior from neural activity), within-modality masking, and cross-modality masking. This approach forces the model to learn the bidirectional relationships between neural activity and behavior [56].
Training and Validation: The protocol involves pretraining on data from multiple animals (e.g., 73 animals) followed by fine-tuning on held-out subjects. Performance is benchmarked on decoding key task variables including whisker motion, wheel velocity, choice, and the "block" prior [56].
The following workflow diagram illustrates the experimental structure of the NEDS framework:
Signal Processing Pipelines for Non-Invasive Interfaces
For non-invasive neural decoding, particularly with EEG, the experimental protocol requires extensive signal preprocessing to overcome inherent noise and limitations. The standard methodology includes:
Filtering and Preprocessing: Raw neural signals are typically contaminated with noise and artifacts. Band-pass filtering (e.g., 1-40 Hz for EEG) removes low-frequency drifts and high-frequency noise. Notch filtering eliminates 50/60 Hz power line interference. Techniques like Independent Component Analysis (ICA) and Principal Component Analysis (PCA) are employed for artifact removal (e.g., eye blinks, muscle activity) [59].
Time-Frequency Analysis: To analyze spectral power over time, methods like Short-Time Fourier Transform (STFT), Continuous Wavelet Transform (CWT), or Hilbert-Huang Transform (HHT) are applied. These techniques help identify frequency bands (alpha: 8-12 Hz, beta: 13-30 Hz, theta: 4-8 Hz) associated with different cognitive states [59].
Spatial Analysis: Source localization techniques, including Minimum Norm Estimation (MNE) and beamforming, estimate the location of neural sources based on scalp-recorded signals. Functional connectivity analysis (coherence analysis, phase-locking value) studies connections between brain regions [59].
Machine Learning Implementation: After preprocessing, both traditional algorithms (Linear Discriminant Analysis, Support Vector Machines) and deep learning approaches (Convolutional Neural Networks, Recurrent Neural Networks) are trained for specific decoding tasks. Evaluation metrics including accuracy, precision, recall, and F1-score, with cross-validation ensuring generalizability [59].
Implementing advanced neural decoding requires a sophisticated toolkit spanning hardware, software, and data resources. The following table catalogs essential components for establishing a capable research pipeline:
Table 3: Essential research reagents and resources for neural decoding research
| Resource Category | Specific Examples | Function/Purpose |
|---|---|---|
| Recording Hardware | Neuropixels probes, Utah arrays, Michigan electrodes, EEG systems with dry/wet electrodes [38] [8] | Acquire neural signals at appropriate spatial/temporal resolution and invasiveness level |
| Public Datasets | International Brain Laboratory (IBL) repeated site dataset [56] | Provide standardized, large-scale neural and behavioral data for model development |
| Signal Processing Tools | Band-pass/notch filters, Independent Component Analysis (ICA), time-frequency analysis (STFT, CWT) [59] | Remove noise, extract meaningful features from raw neural signals |
| Machine Learning Frameworks | Transformer architectures, CNN/RNN models, Boosted Neural Min-Sum decoders [56] [58] [57] | Implement decoding algorithms for neural-behavioral mapping |
| Evaluation Metrics | Accuracy, precision, recall, F1-score, frame error rate (FER) [59] [57] | Quantify decoding performance and model reliability |
| Specialized Software | EEG-Deformer, REI-Net, NEDS framework implementations [56] [58] | Provide specialized architectures for specific decoding tasks |
The selection of appropriate recording hardware represents a fundamental strategic decision with significant methodological implications. Invasive systems like Neuropixels probes offer high-density recording capabilities targeting specific brain regions with single-neuron resolution, but require surgical expertise and raise biocompatibility concerns [56] [55]. Non-invasive EEG systems are more accessible but necessitate more sophisticated signal processing to extract meaningful information from noise-prone signals [38] [59]. Recent innovations in dry electrodes are reducing barriers to EEG adoption by eliminating the need for conductive gels, facilitating longer recording sessions and consumer applications [8].
The following diagram illustrates the architectural overview of a modern neural decoding pipeline, showing how these components interact:
The rapid advancement of machine learning for neural decoding is reshaping, but not eliminating, the fundamental trade-offs between invasive and non-invasive interfaces. While invasive systems continue to provide superior signal quality and decoding performance for clinically critical applications, non-invasive approaches are closing the capability gap through algorithmic innovations that more effectively extract meaningful information from noisy signals [38] [58].
The emergence of multimodal frameworks like NEDS demonstrates that future progress may depend less on choosing between interface paradigms and more on developing approaches that can leverage the unique advantages of each [56]. For researchers and drug development professionals, this suggests a strategic imperative: invest in flexible decoding architectures that can adapt to multiple data sources rather than optimizing for a single interface type. Such an approach will be essential for advancing both basic neuroscience and therapeutic applications across the spectrum of neurological disorders.
The field of neural interfaces is defined by a fundamental trade-off between signal fidelity and invasiveness. Invasive Brain-Computer Interfaces (BCIs), which are implanted directly into brain tissue, provide unparalleled access to high-frequency neural data but carry surgical risks and long-term biocompatibility challenges. Non-invasive interfaces, which record signals from outside the skull, offer greater safety and accessibility but are constrained by lower spatial resolution and signal strength due to skull attenuation [38] [16]. This guide objectively analyzes recent human trials from leading organizations, framing their performance and methodologies within this central thesis to provide researchers and drug development professionals with a clear, data-driven comparison.
The following table summarizes the core capabilities and recent findings from key human trials active in 2025.
Table 1: Overview of Recent Neural Interface Human Trials (2025)
| Organization/Entity | Interface Type & Key Hardware | Stated Primary Application | Reported Trial Outcomes & Performance Metrics |
|---|---|---|---|
| CEBSIT & Huashan Hospital [60] | Invasive (China's BCI)• Ultra-flexible, high-density electrodes• Coin-sized implant (Ø26mm, <6mm thick) | Motor function replacement for tetraplegia | • Patient able to control computer, play games post-training [60]• Stable operation with no infection or electrode failure reported post-March 2025 implant [60] |
| Neuralink [61] | Invasive (N1 Implant)• 1024 electrodes across 64 threads | Controlling digital devices for quadriplegia | • Five patients in trial "controlling digital and physical devices with their thoughts" as of June 2025 [61] |
| Synchron [61] | Minimally Invasive (Stentrode)• Endovascular electrode array delivered via jugular vein | Communication for paralysis | • Allowed patients with paralysis to control a computer, including texting [61]• No serious adverse events after 12 months in a four-patient trial [61] |
| Precision Neuroscience [61] | Minimally Invasive (Layer 7)• Ultra-thin cortical surface array | Communication for ALS | • FDA 510(k) clearance in April 2025 for implantation durations up to 30 days [61] |
| Nature-Described sEMG Platform [7] | Non-Invasive (sEMG)• Dry-electrode, multi-channel wristband | Generic human-computer interaction | • Handwriting transcription at 20.9 words per minute [7]• >90% classification accuracy for held-out participants in offline evaluation [7] |
Comparative Analysis of Interface Performance and Applications
A critical comparison of recent trial data reveals distinct performance profiles and application suitability for invasive and non-invasive approaches. The following table synthesizes quantitative and qualitative findings across key dimensions.
Table 2: Comparative Analysis of Invasive vs. Non-Invasive Interfaces Based on Recent Trials
| Comparison Dimension | Invasive & Minimally Invasive Interfaces | Non-Invasive Interfaces |
|---|---|---|
| Signal Quality & Information Transfer | Very High. Direct neural signal access; supports high bandwidth for real-time control [38] [16]. | Lower. Signals attenuated by skull and tissues; lower spatial resolution and bandwidth [38] [7] [16]. |
| Primary Medical Application (from Trials) | Restoring motor function and communication for severe disabilities (tetraplegia, ALS) [60] [61]. | Rehabilitation, assistive technologies, and generic human-computer interaction [38] [7]. |
| Key Surgical & Safety Considerations | Invasive: Requires craniotomy; risks include infection, hemorrhage, and tissue scarring [38] [61]. Minimally Invasive: Lower risk; Synchron's Stentrode avoids brain tissue [61]. | No surgical risks. Safe for widespread and repeated use [38] [7]. |
| Long-Term Stability & Biocompatibility | Limited long-term stability; potential for scar tissue formation that degrades signal quality [38]. CEBSIT's ultra-flexible electrodes designed to mitigate this [60]. | High long-term stability as no foreign object is implanted [38]. |
| Example Performance Metric | Patient with tetraplegia skillfully operating racing games and chess via thought [60]. | Wristband decoding handwriting at 20.9 WPM, generalizing across users [7]. |
| Regulatory & Commercial Status | In clinical trials; aiming for first market approvals (e.g., CEBSIT targets 2028) [60]. Precision's Layer 7 cleared for 30-day use [61]. | Some consumer-grade and research systems already available; lower regulatory barrier [38] [31]. |
Deep Dive: Experimental Protocols and Methodologies
Protocol for an Invasive BCI Clinical Trial (e.g., CEBSIT/Neuralink Model)
The general protocol for an invasive BCI trial, as reflected in recent reports, involves several critical phases [38] [60] [61].
- Participant Selection: Recruits individuals with severe motor impairments (e.g., tetraplegia from spinal cord injury or amyotrophic lateral sclerosis) who have provided informed consent [38] [60].
- Surgical Implantation:
- Craniotomy: A section of the skull is removed to access the brain [38].
- Dura Mater Incision: A small opening is created in the protective membrane covering the brain [38].
- Electrode Array Implantation: Using stereotactic guidance for precision, an electrode array (e.g., CEBSIT's flexible mesh or Neuralink's N1) is implanted into the targeted brain region, typically the motor cortex [38] [60]. Wires are routed under the scalp to a skull-mounted connector or a sealed, coin-sized unit [38] [60].
- Signal Acquisition & Processing: The implanted device records neural signals, such as action potentials (single neuron activity) and local field potentials (group neuron activity) [38]. These signals are transmitted wirelessly to an external decoder.
- Decoder Calibration & Training: In the weeks following surgery, the patient performs mental tasks (e.g., imagining hand movements) while the system records the corresponding neural patterns. Machine learning models are trained to map these patterns to intended output commands [60].
- Closed-Loop Task Performance: The patient practices controlling an external device (e.g., computer cursor, gaming interface) in real-time, creating a feedback loop that allows both the user and the decoding algorithm to adapt and improve [60].
The workflow for this protocol is summarized in the following diagram:
Protocol for a Non-Invasive Surface EMG (sEMG) Study
The recent Nature study describing a high-performance non-invasive neuromotor interface provides a robust protocol for non-invasive signal acquisition and decoding [7].
- Hardware Setup: Participants don a dry-electrode, multi-channel sEMG recording band on the dominant wrist. The device streams data wirelessly via Bluetooth [7].
- Data Collection Paradigm: Participants perform prompted tasks while software records both sEMG activity and precise task labels.
- Wrist Control: Participants control a cursor, with wrist angles tracked by motion capture as ground truth [7].
- Discrete-Gesture Detection: Participants perform one of nine distinct gestures (e.g., finger pinches, thumb swipes) in a randomized order [7].
- Handwriting: Participants hold fingers together as if holding a pen and "write" prompted text in the air [7].
- Signal Preprocessing: Raw sEMG signals are processed with a real-time engine to reduce online-offline shift. A time-alignment algorithm is applied to precisely align prompter labels with actual gesture events, accounting for participant reaction time [7].
- Model Training with Large-Scale Data: Unlike bespoke invasive decoders, this approach uses data collected from thousands of consenting participants to train generic neural network models that generalize across people without user-specific calibration [7].
- Closed-Loop Performance Evaluation: The system is tested in real-time tasks, with key metrics including target acquisitions per second for navigation and words per minute for handwriting transcription [7].
The workflow for this non-invasive protocol is summarized below:
The Scientist's Toolkit: Essential Research Reagents & Materials
The following table details key materials and their functions as derived from the methodologies of the featured trials and studies, providing a resource for researchers designing similar experiments.
Table 3: Key Research Reagents and Materials for Neural Interface Studies
| Item | Function/Application | Example from Case Studies |
|---|---|---|
| High-Density Electrode Array | Records neural electrical activity; higher channel counts enable higher information bandwidth [60] [61]. | Neuralink's N1 (1024 electrodes), CEBSIT's ultra-flexible array, Paradromics' Connexus (421 electrodes) [60] [61]. |
| sEMG Sensor Array | Records electrical signals from muscle units at the skin surface, providing a non-invasive window into motor intent [7]. | The multi-channel, dry-electrode wristband with high sample rate (2 kHz) and low noise described in the Nature study [7]. |
| Stereotactic Surgical System | Provides precise 3D guidance for implanting electrodes into specific brain targets during surgery [38]. | Used in invasive BCI trials (e.g., CEBSIT, Neuralink) to target the motor cortex or other regions [38] [60]. |
| Neural Signal Decoder (Software) | Machine learning/Algorithms that translate raw neural or sEMG signals into intended device commands [7] [16]. | The generic neural networks trained on data from thousands of participants for the sEMG interface [7]. |
| Biocompatible Substrate | The material forming the electrode array; flexibility and small size reduce immune response and improve long-term stability [60]. | CEBSIT's electrodes, noted for being over 100 times more flexible than previous designs, to minimize tissue damage [60]. |
| Endovascular Delivery System | Enables minimally invasive implantation of electrodes via the blood vessels, avoiding open brain surgery [61]. | The catheter-based system used to deliver and place Synchron's Stentrode in the superior sagittal sinus [61]. |
Navigating Technical Hurdles: Optimization Strategies for Signal Stability and Biocompatibility
The evolution of Brain-Computer Interfaces (BCIs) presents a fundamental dichotomy between performance and biological integration. Invasive neural interfaces, which penetrate brain tissue or reside on its surface, offer unparalleled signal quality and specificity for both recording neural activity and providing therapeutic stimulation [5] [62]. However, their long-term functional stability is severely compromised by the body's natural immune response to foreign materials—a challenge that remains a primary bottleneck in clinical translation [63] [62]. This foreign body response triggers inflammation, activates glial cells (microglia and astrocytes), and ultimately leads to the formation of an insulating scar tissue around the implant [62]. This scar not only physically isolates the electrode but significantly increases electrical impedance, degrading signal-to-noise ratio and stimulating efficacy over time [62]. The core of this problem often lies in the mechanical mismatch between rigid, conventional electrode materials (like silicon or platinum) and the soft, dynamic environment of neural tissue, which has a Young's modulus ranging from 1 to 10 kPa [62].
Consequently, the pursuit of long-term implant stability has catalyzed innovation at the intersection of materials science, bioengineering, and neurobiology. Researchers are developing a new generation of neural interfaces designed to harmonize with the biological environment rather than simply resist it. This guide provides a comparative analysis of the leading material-based strategies—from advanced drug-releasing coatings to flexible conductive substrates—that are actively being tested to overcome the biocompatibility challenge. The success of these approaches is critical for the future of invasive BCIs, enabling chronic applications in restorative neuroscience, such as controlling robotic prostheses, restoring communication, and treating neurological disorders [5] [64].
Comparative Analysis of Material Innovation Strategies
The following section objectively compares the performance, key features, and experimental evidence for several prominent strategies aimed at improving the biocompatibility and chronic stability of neural implants.
Table 1: Comparison of Material Innovation Strategies for Neural Implants
| Strategy | Key Materials & Examples | Proposed Mechanism of Action | Reported Efficacy & Experimental Data | Noted Limitations |
|---|---|---|---|---|
| Anti-inflammatory Drug Coatings | Dexamethasone covalently bound to Polyimide [63] | Localized, slow release of potent anti-inflammatory drug to suppress the immune response during the critical post-implantation period. | • Significant reduction in inflammation-related signals in immune cells in vitro [63].• Animal tests: Dexamethasone-releasing implants showed a marked reduction in immune reactions and scar tissue formation [63].• Release Duration: Sustained release over at least two months [63]. | Long-term effects of drug depletion and potential for tissue remodeling beyond the release period require further study. |
| Soft & Flexible Conductive Polymers | Poly(3,4-ethylenedioxythiophene) (PEDOT), other conductive polymers, soft nanocomposites [62] [65] | Reduction of mechanical mismatch at the tissue-device interface minimizes micromotion-induced damage and chronic inflammation. | • Evolution from rigid substrates to flexible conductive polymers and biodegradable bioactive scaffolds [65].• Mechanical Property Target: Young's modulus close to neural tissue (1-10 kPa) [62].• Improved conformal contact with tissue, leading to more stable signal acquisition. | Can present challenges in surgical implantation; long-term stability of electrical properties in vivo is an active area of research. |
| Surface Topography & Biofunctionalization | Micro- and nano-textured surfaces; bioactive molecule coatings [62] [65] | Surface textures and immobilized bioactive signals promote better integration with host tissue and discourage glial scar encapsulation. | • Advanced micro-textured shells shown to improve integration and reduce capsular contracture in other implant models [66].• Aim: Promote neuronal attachment over glial cell attachment. | Optimization of specific feature sizes and densities for neural tissue is complex; reproducibility at scale. |
| Novel Minimally Invasive Form Factors | Stentrode (endovascular electrode) [5] | Avoids direct penetration of brain parenchyma by recording from within a blood vessel, thereby evading the severe foreign body response. | • FDA approval for human BCI use [5].• Successful control of computer cursor tasks in patients demonstrated [5]. | Recording coverage is limited by vessel location; primarily targets motor cortex areas adjacent to large vessels. |
Detailed Experimental Protocols for Key Innovations
To facilitate replication and critical evaluation, this section details the experimental methodologies behind two of the most promising strategies from the comparison table.
Protocol: Covalent Binding of Dexamethasone to Polyimide
This protocol is based on the recent work by Turrin et al., 2025, which serves as a prime example of a targeted drug-delivery approach [63].
- Surface Activation: The polyimide substrate of the neural electrode is first subjected to a plasma or chemical oxidation treatment. This process creates reactive functional groups (e.g., hydroxyl or carboxyl groups) on the otherwise inert polymer surface.
- Chemical Functionalization: The activated surface is then immersed in a solution containing a coupling agent, such as a silane derivative, which possesses one end that binds to the surface groups and another end that presents a reactive moiety (e.g., an amine-reactive group) for drug attachment.
- Drug Conjugation: Dexamethasone is chemically modified to display a compatible functional group. The modified dexamethasone is then reacted with the functionalized polyimide surface under controlled conditions (specific pH, temperature, and duration) to form a stable covalent bond.
- Washing and Characterization: The coated implant is thoroughly washed with solvents to remove any unbound, physisorbed drug molecules. The success of the coating procedure is validated through:
- Surface Analysis: Techniques like X-ray Photoelectron Spectroscopy (XPS) to confirm the chemical composition of the surface.
- Drug Release Kinetics: In vitro elution studies in phosphate-buffered saline (PBS) at 37°C, with periodic measurement of dexamethasone concentration via High-Performance Liquid Chromatography (HPLC) to confirm sustained release over weeks.
- In vivo Validation: The final coated devices are implanted in animal models (e.g., rodents). After a predetermined period (e.g., 6-12 weeks), histological analysis of the brain tissue surrounding the implant is performed. This involves staining for specific cell types to quantify the presence of astrocytes (GFAP stain), microglia (Iba1 stain), and neurons (NeuN stain) to assess the extent of glial scarring and neuronal survival compared to uncoated controls [63].
Protocol: Fabrication and Implantation of Flexible Neural Probes
This protocol outlines the general workflow for creating and testing soft neural interfaces, as highlighted in reviews of the field [62] [65].
- Substrate Selection and Patterning: A flexible polymer such as polyimide, parylene-C, or a biodegradable elastomer is selected as the substrate. Microfabrication techniques, including photolithography and laser ablation, are used to pattern the thin-film polymer into the desired shank and electrode site geometry.
- Conductive Trace Deposition: A thin metal layer (e.g., Gold, Platinum) or a conductive polymer (e.g., PEDOT:PSS) is deposited and patterned onto the substrate to form the conductive traces and recording/stimulation sites.
- Insulation Layer and Encapsulation: A second layer of the flexible polymer is deposited to insulate the conductive traces, with openings etched at the recording sites. A final, hermetic encapsulation layer (e.g., silicon carbide, alumina) is often applied over the entire device, except for the electrode sites, to protect the electronics from the corrosive biological environment—a key failure point for chronic implants [62] [67].
- Mechanical Characterization: The stiffness (Young's modulus) of the fabricated probe is measured using techniques like nanoindentation or tensile testing to verify its compliance with neural tissue.
- Implantation Strategy: Due to their flexibility, these probes often require a temporary rigid shuttle or a biodegradable stiffener (e.g., silk, sugar) to facilitate reliable insertion into the brain tissue without buckling.
- Functional Validation: The performance of the flexible implants is assessed chronically over weeks to months. Key metrics include:
- Electrophysiological Recording: Monitoring the amplitude and signal-to-noise ratio of recorded neural signals (spikes and local field potentials) over time.
- Stimulating Efficacy: Measuring the impedance and charge-injection capacity of the electrode sites during electrical stimulation.
- Histological Correlation: Post-mortem histology is correlated with the electrical data to confirm that stable signals correspond with reduced glial scarring and closer proximity of neuronal cell bodies to the electrode sites [62].
Visualizing the Foreign Body Response and Mitigation Strategies
The following diagram illustrates the biological challenge of the Foreign Body Response (FBR) and the primary points of intervention for the material strategies discussed.
Diagram 1: The Foreign Body Response and Material Mitigation Pathways. This chart visualizes the key stages of the immune-mediated reaction to an implanted neural electrode, culminating in signal-degrading scar tissue. The green nodes and arrows indicate how advanced material strategies directly target and interrupt this detrimental pathway.
The mechanism of a drug-releasing coating, a key strategy, involves a carefully engineered release profile to intervene at the critical early stages of the FBR, as shown below.
Diagram 2: Sustained Drug Release Mechanism for Biocompatibility. This diagram outlines the functional principle of a drug-eluting neural implant, where a therapeutic agent is released locally over a prolonged period to quell the inflammatory response and achieve a stable tissue interface.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Reagents for Biocompatibility Research
| Item Name | Function/Description | Relevance to Biocompatibility Research |
|---|---|---|
| Polyimide Substrates | A durable, biocompatible polymer commonly used as a flexible substrate for neural microelectrodes. | Serves as a base material for flexible implants, reducing mechanical mismatch. Can be chemically modified for drug binding [63] [62]. |
| Dexamethasone | A potent synthetic glucocorticoid (anti-inflammatory drug). | The active pharmaceutical ingredient in drug-releasing coatings. It suppresses the activation and proliferation of glial cells (microglia, astrocytes) [63]. |
| Conductive Polymers (PEDOT:PSS) | Organic polymers that conduct electricity, often used as a coating on electrode sites. | Improve the electrical characteristics of electrodes (lower impedance, higher charge injection). Their softer, more hydrogel-like nature is more tissue-compliant than rigid metals [62]. |
| Primary Antibodies (GFAP, Iba1, NeuN) | Antibodies used in immunohistochemistry to label specific cell types in fixed tissue. | GFAP labels astrocytes, Iba1 labels microglia—key markers of the glial scar. NeuN labels neuronal nuclei. Essential for quantifying the foreign body response histologically [63] [62]. |
| Silane Coupling Agents | Bifunctional molecules that can form a covalent bridge between an inorganic surface (e.g., metal oxide on polyimide) and an organic molecule (e.g., drug). | Enable the stable, covalent attachment of bioactive molecules like dexamethasone to the implant surface, preventing rapid burst release [63]. |
The innovations in biocompatible materials are not occurring in isolation but are fundamentally shaping the trajectory and potential applications of invasive neural interfaces. The choice between invasive and non-invasive BCIs often involves a trade-off between signal fidelity and biocompatibility/safety [5]. Non-invasive approaches like EEG are safe and accessible but suffer from limited spatial resolution and signal strength [5] [8]. In contrast, invasive interfaces, such as the Utah Array or emerging flexible probes, offer high-resolution data crucial for complex tasks like dexterous control of robotic arms [5] [64] or speech decoding [5].
The material strategies detailed in this guide are what make the long-term viability of these high-performance invasive interfaces feasible. By directly addressing the foreign body response, they extend the functional lifespan of implants, thereby enhancing the return on the inherent risk and cost of invasive surgery. This progress expands the scope of invasive BCIs from short-term proof-of-concept studies toward reliable, chronic therapeutic and assistive devices for conditions like spinal cord injury and ALS [63] [64]. The ultimate goal is a seamless integration of biology and technology, where an implant is not merely tolerated by the nervous system but is accepted as a stable and permanent conduit for bidirectional communication. The continued convergence of advanced materials, sophisticated drug delivery, and intelligent device design is steadily turning this goal into a clinical reality.
Invasive Brain-Computer Interfaces (BCIs) represent a transformative technology for restoring function in patients with severe neurological conditions, yet their long-term efficacy is fundamentally challenged by biological responses to implanted devices. The core issue lies in the brain's natural defense mechanisms: following electrode implantation, the body initiates a complex tissue response that often leads to scar tissue formation, progressively degrading signal quality over time. This phenomenon of signal degradation poses a significant barrier to the clinical viability and commercial adoption of chronic neural implants [52] [68].
The foreign body response unfolds through a predictable sequence: protein adsorption on the implant surface, activation of microglia and astrocytes, recruitment of inflammatory cells, and ultimately, the formation of a fibrotic capsule that physically separates electrodes from their target neurons [38]. This insulating layer attenuates neural signals, increases electrical impedance, and diminishes the signal-to-noise ratio essential for high-fidelity decoding. Consequently, even meticulously implanted electrodes can experience progressively deteriorating performance, necessitating frequent recalibration or explaining procedures [61]. Understanding and mitigating this tissue response is therefore not merely a biological curiosity but an engineering imperative for next-generation neurotechnologies.
This review examines the multifaceted strategies emerging to address this challenge, located within the broader scientific discourse comparing invasive and non-invasive neural interfaces. While non-invasive approaches (EEG, fNIRS, MEG) circumvent implantation risks entirely, they remain constrained by fundamentally lower spatial resolution and signal fidelity [69] [8]. The strategic imperative for invasive BCIs is to preserve their superior signal quality while achieving the long-term stability required for chronic clinical applications. The following sections analyze technological innovations, experimental methodologies, and material science advances collectively aiming to resolve this central trade-off.
Comparative Analysis of BCI Technologies and Tissue Response
The neural interface landscape spans a spectrum of invasiveness, each tier presenting distinct trade-offs between signal fidelity, long-term stability, and surgical risk. Understanding these trade-offs is essential for contextualizing tissue response mitigation strategies.
Table 1: Comparison of BCI Modalities by Invasiveness and Signal Characteristics
| BCI Category | Implantation Site | Signal Quality | Information Transfer Rate | Primary Tissue Response Challenges |
|---|---|---|---|---|
| Invasive | Within brain tissue | Highest (single neuron resolution) | ~100-200 bits/minute | Chronic glial scarring, inflammation, electrode degradation [38] |
| Semi-Invasive | Brain surface (beneath skull) | Moderate (local field potentials) | ~40-60 bits/minute | Meningeal response, subdural fibrosis [38] |
| Non-Invasive | Scalp surface | Lowest (attenuated by skull) | ~5-25 bits/minute | Minimal (skin irritation only) [38] [16] |
Invasive approaches, while offering unparalleled signal resolution, face the most significant biological integration challenges. The foreign body response to penetrating electrodes involves multiple phases: initial blood-brain barrier disruption, activation of microglia (the brain's resident immune cells), recruitment of astrocytes, and eventual formation of a dense glial scar that insulates electrodes from nearby neurons [38] [68]. This process not only reduces signal amplitude but can also trigger neurodegenerative changes in the immediate microenvironment. The signal degradation timeline typically follows a predictable trajectory, with the most pronounced decline occurring within the first 3-6 months post-implantation, though the specific timecourse varies substantially based on device characteristics and implantation technique [61].
Different invasive BCI platforms have developed distinct architectural approaches to mitigate these responses, with varying levels of documented success in human trials:
Table 2: Tissue Response Mitigation in Commercial Invasive BCI Platforms
| BCI Platform | Architectural Approach | Electrode Characteristics | Documented Tissue Response |
|---|---|---|---|
| Neuralink | Ultra-fine polymer threads | 1024 electrodes across 64 threads | Limited human data; designed to minimize displacement [61] [68] |
| Blackrock Neurotech | Utah array | Rigid silicon microelectrodes | Chronic glial scarring observed in long-term implants [61] |
| Precision Neuroscience | Cortical surface film | Electrode array on flexible substrate | Avoids penetration; minimal parenchymal disruption [61] |
| Synchron | Endovascular stent | Stent-electrode array in blood vessels | Avoids brain tissue penetration; no direct scarring [61] [68] |
The comparison reveals an emerging trend: next-generation interfaces are prioritizing minimally disruptive form factors that either dramatically reduce device footprint or avoid parenchymal penetration altogether. This strategic shift acknowledges that the biological response, rather than purely electronic considerations, often constitutes the limiting factor for chronic BCI performance [61] [68].
Methodological Approaches for Investigating Tissue Response
Research into BCI tissue response employs sophisticated methodological approaches spanning computational modeling, material science, and experimental neuroscience. These methodologies enable researchers to quantify the relationship between device characteristics and biological outcomes, informing the development of next-generation interfaces.
Computational Modeling of Signal Degradation
Advanced computational approaches now enable researchers to simulate the effects of tissue response on signal quality. The Multiscale Fusion enhanced Spiking Neural Network (MFSNN) represents a particularly innovative framework that addresses the challenge of data distribution shifts in chronic neural recordings [70]. This method explicitly models how features extracted from neural signals evolve over time as electrode-tissue interactions change, allowing decoders to maintain performance despite progressive signal degradation. The MFSNN architecture incorporates temporal convolutional networks and channel attention mechanisms to identify stable neural features resilient to the scar-induced signal alterations, effectively discriminating neural activity from increasing noise contamination [70].
The experimental workflow for evaluating these models typically follows a standardized protocol:
- Chronic Implantation: Arrays are implanted in animal models (typically non-human primates or rodents) for extended periods (6-18 months)
- Longitudinal Recording: Neural signals are regularly acquired during structured behavioral tasks
- Histological Analysis: Post-explanation tissue examination quantifies glial fibrillary acidic protein (GFAP) expression and neuronal density around electrodes
- Correlative Modeling: Computational models map histological findings to signal quality metrics across the implant duration
This methodology has revealed that the most significant signal alterations occur not from bulk impedance changes but from the progressive insulation of electrodes from active neurons, effectively increasing the recording distance and filtering high-frequency neural components [70].
Material Science and Biocompatibility Testing
Parallel to computational approaches, material science investigations systematically evaluate how device physical properties influence tissue integration. Standardized testing protocols assess:
- Surface topography at nano-scale dimensions and its effect on protein adsorption
- Material stiffness relative to brain tissue and its impact on chronic micromotion-induced inflammation
- Chemical composition and leachables that may provoke immune responses
The emerging consensus indicates that softer, smaller devices with surface features that mimic the extracellular matrix produce significantly reduced glial activation compared to conventional rigid interfaces [61]. These findings have driven innovation in flexible electronics, dissolvable coatings, and bioactive interfaces that actively modulate the host response. Validation typically involves quantitative immunohistochemistry comparing marker expression (Iba1 for microglia, GFAP for astrocytes) around test versus control devices, providing objective metrics of biocompatibility improvement [68].
Signaling Pathways in Tissue Response and Experimental Workflow
The cellular response to implanted electrodes follows a well-defined signaling cascade that presents multiple intervention points for therapeutic modulation. Understanding this pathway is essential for developing targeted mitigation strategies.
Diagram: Signaling pathway of tissue response to implanted electrodes and intervention points. Gold nodes represent mitigation strategies that target specific stages of the response.
The experimental workflow for investigating these pathways combines electrophysiology, histology, and molecular biology techniques in a longitudinal design:
Diagram: Standard experimental workflow for evaluating tissue response to invasive BCIs. Green nodes represent critical assessment phases.
This methodological framework enables researchers to establish causal relationships between specific device parameters, the resulting cellular response, and ultimate functional outcomes. The combination of real-time signal monitoring with post-mortem histological validation provides a comprehensive picture of the device-tissue interface evolution over time [70] [68].
Research Reagent Solutions for BCI Tissue Response Studies
Investigating tissue response to implanted BCIs requires specialized reagents and materials designed to quantify biological reactions and signal quality metrics. The following table details essential research tools employed in this field:
Table 3: Essential Research Reagents and Materials for BCI Tissue Response Studies
| Reagent/Material | Function/Application | Experimental Utility |
|---|---|---|
| Iba1 Antibodies | Immunohistochemical staining of activated microglia | Quantifies innate immune response magnitude and distribution around implants [68] |
| GFAP Antibodies | Labels reactive astrocytes in glial scar formation | Measures astrocytic encapsulation thickness and density [68] |
| NeuN Antibodies | Identifies viable neuronal cell bodies | Assesses neuronal survival and density in peri-implant regions [68] |
| Flexible Polymer Substrates | Base material for minimally disruptive electrodes | Reduces mechanical mismatch; decreases chronic inflammation [61] |
| Anti-inflammatory Coatings | Device surface functionalization | Modulates local immune response; minimizes scar formation [68] |
| Channel Attention Algorithms | Computational feature identification in neural data | Identifies stable neural signals amidst progressive degradation [70] |
| Spiking Neural Networks | Brain-inspired signal decoding architecture | Enables energy-efficient processing of high-dimensional neural data [70] |
These research tools enable standardized quantification of the tissue response across different experimental conditions and device architectures. The combination of molecular markers for specific cell types with computational approaches for signal analysis provides a multi-modal assessment framework that captures both biological and functional outcomes [70] [68]. This methodological standardization is crucial for comparing results across studies and establishing validated benchmarks for device biocompatibility.
The challenge of signal degradation in invasive BCIs represents a complex interplay between materials science, neurobiology, and signal processing. While the foreign body response remains a significant obstacle, current research demonstrates multiple promising pathways toward more stable neural interfaces. The strategic integration of flexible materials that minimize mechanical mismatch, bioactive surfaces that modulate cellular responses, and adaptive algorithms that compensate for signal evolution collectively point toward a future of chronically reliable BCIs. As these technologies mature, the distinction between biological and engineered systems will increasingly blur, potentially enabling seamless integration between neural tissue and implanted devices. The continued convergence of interdisciplinary expertise will be essential to translate these promising approaches into clinically viable solutions that maintain their performance over decades of service.
Brain-Computer Interfaces (BCIs) represent a revolutionary technology enabling direct communication between the human brain and external devices [31]. Within this field, a fundamental dichotomy exists between invasive approaches, which require surgical implantation of electrodes directly into brain tissue, and non-invasive approaches, which measure neural signals from outside the skull [38] [5]. Non-invasive BCIs, primarily using techniques like electroencephalography (EEG), offer the significant advantages of safety, accessibility, and avoidance of surgical risks [38] [52]. However, these benefits come at a cost: non-invasive systems are fundamentally limited by low signal resolution due to the signal-blunting effect of the skull and persistent contamination from physiological clutter, such as blood flow, heart rate, and respiration [38] [71]. This article examines the current state of research and the innovative strategies being developed to overcome these central challenges, thereby optimizing the performance and broadening the applications of non-invasive neural interfaces within the broader context of invasive versus non-invasive BCI research.
Core Challenges in Non-Invasive Neural Interfacing
The performance gap between invasive and non-invasive neural interfaces stems from two primary, interconnected challenges that corrupt signal quality and limit information transfer rates.
Low Signal Resolution: The human skull acts as a formidable low-pass filter, severely attenuating and spatially smearing the electrical signals generated by neural activity [38] [5]. This results in a significantly lower signal-to-noise ratio (SNR) compared to invasive methods. While invasive BCIs can record the firing of individual neurons (action potentials), non-invasive EEG is limited to recording the summed, large-scale electrical activity of millions of neurons [38]. Consequently, the spatial resolution of non-invasive systems is drastically reduced, making it difficult to pinpoint the precise origin of neural signals.
Physiological Clutter: A major source of noise in non-invasive recordings comes from the body itself. These so-called "physiological artifacts" include the electrical activity of the heart (ECG), muscle contractions (EMG), eye movements (EOG), and the hemodynamic pulsations from blood flow and respiration [71]. This clutter is often orders of magnitude stronger than the neural signals of interest, making their separation a primary focus of signal processing research. One research team explicitly noted the difficulty of identifying novel neural signals due to this "competing noise from physiological clutter" [71].
Table 1: Fundamental Challenges of Non-Invasive BCIs
| Challenge | Impact on Signal | Comparative Performance to Invasive BCIs |
|---|---|---|
| Low Signal Resolution | Attenuated and spatially blurred signals; lower Signal-to-Noise Ratio (SNR). | Spatial Resolution: Scalp-level (cm) vs. single-neuron (µm) [38].Information Transfer Rate: ~5-25 bits/min (Non-Invasive) vs. ~100-200 bits/min (Invasive) [38]. |
| Physiological Clutter | Contamination from heartbeat, muscle activity, and blood flow obscures target neural signals [71]. | Signal is recorded at the source (Invasive) vs. through multiple interfering biological filters (Non-Invasive) [38] [5]. |
Emerging Solutions and Experimental Approaches
Researchers are employing a multi-faceted strategy to overcome these limitations, combining novel sensor technologies, advanced signal processing algorithms, and hybrid measurement approaches.
Hardware and Sensor Innovations
At the hardware level, improvements focus on capturing cleaner signals at their source. A significant trend is the development of high-density, dry-electrode EEG systems that are more user-friendly and accessible than traditional wet-electrode caps [8]. Furthermore, researchers are exploring non-electrical modalities. A team from Johns Hopkins, for instance, developed a digital holographic imaging system designed to detect "the tiny tissue deformations that occur during brain activity," representing a novel signal type that is less susceptible to traditional electrical interference [71].
Another promising avenue is the move towards hybrid systems that combine neural signals with other data streams. Surface Electromyography (sEMG) has emerged as a powerful non-invasive method for decoding motor intention from the electrical activity of muscles, which are the final output of motor neural pathways. A recent landmark study described a highly sensitive sEMG wristband that achieved a handwriting decoding rate of 20.9 words per minute with out-of-the-box generalization across users, demonstrating performance previously associated only with invasive systems [7].
Algorithmic and Data Processing Advances
The "big data" problem in BCI is being addressed with modern artificial intelligence. Machine learning, particularly deep learning models, are now essential for feature extraction and classification of noisy neural signals [5] [72]. These models are trained on massive, crowdsourced datasets to improve their robustness and user-independence [7]. For example, the same sEMG study collected data from thousands of participants to build models that generalize effectively across different anatomies and recording sessions, directly addressing the challenges of signal variability [7].
The following diagram illustrates a modern, AI-driven processing workflow for a non-invasive BCI system, showing how raw signals are transformed into device commands.
Comparative Performance Data
The efficacy of these optimization strategies is demonstrated by quantitative performance benchmarks across various BCI tasks. The table below compares the state-of-the-art in non-invasive systems with established invasive benchmarks, highlighting the closing gap in certain applications.
Table 2: Performance Comparison: Invasive vs. Optimized Non-Invasive BCIs
| Application / Task | Invasive BCI Performance | Optimized Non-Invasive BCI Performance | Key Technologies & Notes |
|---|---|---|---|
| Communication (Text/Writing) | Imagined handwriting decoded at ~90 characters/min [5]. | sEMG-decoded handwriting at 20.9 words per minute (WPM) [7]. | Surface EMG (sEMG) on the wrist; generalizes across users without personalization [7]. |
| Discrete Gesture Control | High-speed control of robotic arms and prosthetics [38]. | 0.88 gesture detections per second with high accuracy [7]. | High-density sEMG wristband combined with neural network decoders [7]. |
| Continuous Navigation/Control | Precise control of computer cursors and robotic limbs [38]. | 0.66 target acquisitions per second in a continuous navigation task [7]. | Decoding of wrist angle velocity from sEMG (error < 13°/s) [7]. |
| Signal Fidelity | Records single-neuron action potentials and local field potentials [38]. | Novel systems capturing "tiny tissue deformations" from brain activity [71]. | Digital holographic imaging to mitigate physiological clutter; represents a new signal modality [71]. |
Detailed Experimental Protocol: A Template for Optimization
To illustrate the practical application of these solutions, what follows is a synthesized experimental protocol representative of cutting-edge non-invasive BCI research, drawing from the methodologies described in the search results.
Aims and Hypothesis
- Primary Aim: To develop and validate a generic, high-performance non-invasive neuromotor interface for human-computer interaction.
- Hypothesis: That a combination of high-fidelity hardware and AI-driven, data-intensive modeling can overcome traditional limitations of low resolution and physiological clutter, enabling cross-user generalization without per-person calibration [7].
Methodology
Participant Recruitment and Hardware
- Participants: Recruit an anthropometrically and demographically diverse cohort of participants (e.g., numbering in the thousands) to ensure model robustness and generalization [7].
- Hardware: Utilize a high-density, dry-electrode sensor array. For neuromotor interfaces, a multi-channel, wireless sEMG band is placed on the dominant wrist. Key specifications should include [7]:
- High Sample Rate: 2 kHz or greater.
- Low Noise: <2.5 μVrms.
- Multiple Device Sizes: To accommodate varying anatomies and ensure consistent electrode-skin contact.
Data Collection Paradigm
Participants perform a series of prompted tasks while neural/neuromotor data and precise label timestamps are recorded.
- Task 1: Continuous Navigation: Participants control a cursor using wrist movements, with motion capture providing ground-truth labels for model training [7].
- Task 2: Discrete Gesture Detection: Participants perform a set of distinct gestures (e.g., finger pinches, thumb swipes) in a randomized order with variable intervals to capture a range of signal patterns [7].
- Task 3: Handwriting: Participants "air-write" prompted text while wearing the sEMG sensor, generating data for decoding complex, fine-motor intentions [7].
Signal Processing and Model Training
- Time-Alignment: Implement an algorithm to post-hoc align prompt labels with the actual onset of gestures, accounting for user reaction time and ensuring clean training data [7].
- Feature Extraction & Model Training: Train deep neural networks on the collected dataset. The architecture should be designed to map sEMG patterns to the corresponding prompts or continuous control signals. A key focus is on creating models that are trained across the entire participant pool to enforce cross-user generalization [7].
The workflow for this large-scale, data-driven approach is visualized below.
Key Research Reagent Solutions
Table 3: Essential Materials and Reagents for Advanced Non-Invasive BCI Research
| Item / Solution | Function / Role in Research | Specification Example |
|---|---|---|
| High-Density sEMG Band | Records electrical signals from muscle units as a proxy for motor neural commands. | Dry electrodes; 2 kHz sampling; <2.5 μVrms noise; multiple sizes for anatomical fit [7]. |
| Digital Holographic Imaging System | Captures novel neural signals based on mechanical tissue deformations, bypassing electrical clutter [71]. | Designed to mitigate physiological noise from blood flow and respiration [71]. |
| AI/Deep Learning Models | Extracts features and decodes intent from noisy, complex signal data. | Neural networks (e.g., CNNs, Transformers) trained on large-scale participant data [7]. |
| Data Collection & Alignment Software | Presents tasks, records data, and ensures precise time-alignment between prompts and neural signals. | Custom engine with real-time processing and post-hoc time-alignment algorithms [7]. |
The frontier of non-invasive neural interfacing is being rapidly advanced by a concerted attack on the dual problems of low resolution and physiological clutter. While invasive BCIs continue to offer the highest signal fidelity for a limited number of clinical patients, the optimized non-invasive systems detailed here are achieving unprecedented levels of performance, in some cases rivaling the functional output of their invasive counterparts [7]. Through innovations in hardware like high-density sEMG and holographic imaging, coupled with the power of data-intensive AI models, the field is systematically overcoming its historical limitations. The resulting "generic" interfaces that work robustly across diverse users without calibration represent a paradigm shift, promising to accelerate the integration of BCIs from specialized medical therapy into broader areas of human-computer interaction.
The field of neural interfaces is grappling with a data deluge. As of 2025, invasive brain-computer interfaces (BCIs) have transitioned from laboratory curiosities to a burgeoning neurotechnology industry, with multiple companies initiating human trials [61]. This transition is underpinned by a relentless increase in the channel count of neural recording systems, which in turn generates unprecedented data processing demands. Modern high-density implants, such as Neuralink's Telepathy system, now incorporate 65,536 electrodes, while Paradromics' Connexus BCI uses a modular array with 421 electrodes and an integrated wireless transmitter [61]. These systems generate raw data throughput approaching 491 Mbits/sec from 1,024 electrodes alone, creating a significant bottleneck between data acquisition and meaningful interpretation [73].
This article analyzes the hardware and software solutions developed to overcome this data processing bottleneck, framing the discussion within the broader context of invasive versus non-invasive neural interfaces research. For neuroscientists and drug development professionals, understanding these technological foundations is crucial for designing experiments, interpreting neural data, and developing novel therapeutic approaches. The solutions emerging represent interdisciplinary collaborations between neuroscience, electrical engineering, and computer science—particularly in the domain of artificial intelligence (AI).
Table: Representative High-Channel-Count Neural Interfaces and Their Data Characteristics
| Company/System | Interface Type | Electrode Count | Key Data Processing Features | Primary Applications |
|---|---|---|---|---|
| Neuralink (Telepathy) | Invasive (intracortical) | 65,536 electrodes (1,024 per thread) | On-chip preprocessing, custom spike-sorting algorithms, wireless data transmission [61] [73] | Motor control for paralysis, computer control |
| Paradromics (Connexus) | Invasive (intracortical) | 421 electrodes | Integrated wireless transmitter, modular array design [61] | Speech restoration, communication |
| Synchron (Stentrode) | Minimally invasive (endovascular) | Not specified | Endovascular placement, eliminates open-brain surgery [61] | Digital device control for paralysis |
| Blackrock Neurotech | Invasive (intracortical) | Varies (Utah array) | Developing Neuralace flexible lattice, chronic implantation experience [61] | Research applications, motor control |
| Precision Neuroscience (Layer 7) | Minimally invasive (epicortical) | Not specified | Ultra-thin electrode array, conforms to cortical surface [61] | Communication for ALS patients |
Hardware Solutions: From Electrodes to Processors
Advanced Electrode Technologies and Biocompatibility
The first stage of the data processing pipeline begins at the electrode-tissue interface. Traditional rigid electrodes, such as the Utah array, create significant mechanical mismatch with brain tissue (Young's modulus of ~1-10 kPa versus silicon at ~102 GPa), leading to chronic inflammation, scar tissue formation, and signal degradation over time [62]. This biocompatibility challenge directly impacts data quality and longevity in high-channel-count systems.
Next-generation solutions focus on flexible, biocompatible materials that minimize foreign body response. Neuralink employs ultra-thin polymer threads (5 microns in diameter) to reduce tissue damage [73], while Precision Neuroscience has developed an ultra-thin electrode array that conforms to the cortical surface without penetrating brain tissue [61]. Blackrock Neurotech is pursuing a flexible lattice design called Neuralace for less invasive cortical coverage [61]. These material innovations are crucial for maintaining stable signal quality—the foundation for all subsequent data processing—over extended implantation periods.
Integrated Circuit Design and On-Chip Processing
To manage the enormous data flow from thousands of recording sites, modern BCIs implement sophisticated integrated circuits with significant on-chip preprocessing capabilities. This approach dramatically reduces the volume of data that must be transmitted wirelessly, conserving power and bandwidth while minimizing heat generation in sensitive neural tissue.
The Neuralink system exemplifies this approach with its N1 chip, fabricated on a 40 nm CMOS process node, which performs initial analog front-end processing including amplification, filtering, and analog-to-digital conversion [73]. This on-chip preprocessing is essential given the raw data throughput of approximately 491 Mbits/sec from 1,024 electrodes sampling at 30 kHz with 16-bit resolution [73]. Similar design principles are employed across high-channel-count systems, with variations in implementation based on specific application requirements and power constraints.
Diagram Title: Neural Data Processing Pipeline in High-Channel-Count Systems
Wireless Data Transmission Challenges
After on-chip processing, reduced data must be transmitted externally for further analysis. This wireless transmission presents significant engineering challenges related to power consumption, data rate, and thermal management. Current systems typically employ custom protocols optimized for the specific data characteristics of neural signals, balancing bandwidth requirements with safety considerations for chronic implantation.
Manufacturing these hybrid systems—combining flexible biocompatible polymers with ultra-fine metal traces and micro-electromechanical assembly—requires specialized processes such as polymer thread fabrication via spin-coating or extrusion, automated robotic insertion systems with micron-scale precision, and rigorous sterilization protocols [73]. These manufacturing complexities directly influence the scalability and commercial viability of high-channel-count neural interfaces.
Software Solutions: Algorithms and AI for Neural Decoding
Signal Processing Pipelines and Feature Extraction
The software pipeline for processing neural data typically involves multiple stages: signal registration, digitization, preprocessing, feature extraction, classification/decoding, and command execution [74]. For invasive systems, the initial processing stages often focus on spike sorting—the challenging task of identifying and classifying action potentials from individual neurons amidst noisy multi-unit recordings.
High-channel-count systems benefit from advanced spike-sorting algorithms that can leverage information across multiple electrodes to resolve individual neurons more accurately. These algorithms must operate in near-real-time (with latencies under 0.25 seconds for applications like speech decoding) while adapting to non-stationary neural signals that change over time due to factors such as electrode drift or neural plasticity [61] [62]. The development of robust, adaptive signal processing pipelines remains an active research area, particularly for clinical applications where reliability is paramount.
Deep Learning and Adaptive Decoders
Artificial intelligence, particularly deep learning, has revolutionized neural decoding for high-channel-count systems. Convolutional neural networks (CNNs) such as EEGNet—originally developed for non-invasive EEG data—have been adapted for use with invasive recordings, demonstrating superior performance in decoding complex neural patterns [75]. These networks can automatically learn hierarchical representations from raw or minimally processed neural signals, capturing subtle temporal and spatial patterns that may be missed by traditional feature engineering approaches.
Transfer learning and fine-tuning approaches have proven particularly valuable in neural interface applications. As demonstrated in a 2025 study on finger movement decoding, fine-tuning a pre-trained base model with session-specific data significantly improved performance, with two-way ANOVA showing substantial improvements across sessions for both binary (F = 14.455, p = 0.001) and ternary (F = 24.590, p < 0.001) classification paradigms [75]. This adaptability is crucial for handling inter-session variability and maintaining decoding performance over extended periods.
Table: Performance Comparison of Decoding Approaches for Individual Finger Movements
| Decoding Approach | Interface Type | Classification Task | Accuracy/Performance | Key Algorithm |
|---|---|---|---|---|
| Individual finger movement decoding [75] | Non-invasive (EEG) | 2-finger MI tasks | 80.56% accuracy | EEGNet with fine-tuning |
| Individual finger movement decoding [75] | Non-invasive (EEG) | 3-finger MI tasks | 60.61% accuracy | EEGNet with fine-tuning |
| Intracortical finger decoding [75] | Invasive (ECoG) | Individual finger movement | Higher precision than non-invasive | Shallow feed-forward neural network |
| Speech decoding [61] | Invasive (intracortical) | Word inference from neural activity | 99% accuracy with <0.25s latency | Deep learning with neural data |
Real-Time Processing Frameworks
Several software frameworks have been developed specifically for BCI research and applications, providing infrastructure for real-time data acquisition, processing, and visualization. Platforms such as BCI2000, OpenViBE, NeuroPype, and BCILAB implement real-time emulation modes that enable system testing with new paradigms and algorithms [74]. These frameworks must support stringent timing requirements while providing flexibility for research innovation—a challenging balance that becomes increasingly difficult with higher channel counts.
For invasive systems in particular, the processing pipeline is often distributed across multiple hardware platforms, with computationally intensive decoding algorithms potentially running on external computers rather than implantable hardware. This division necessitates careful optimization to minimize latency throughout the system, particularly for closed-loop applications where timely feedback is critical for learning and control.
Comparative Analysis: Invasive vs. Non-Invasive Approaches
The data processing bottleneck manifests differently across the spectrum of neural interface approaches. Invasive systems provide unprecedented signal quality and spatial resolution but face biocompatibility challenges and surgical constraints. Non-invasive approaches like EEG offer greater accessibility but contend with significantly lower signal-to-noise ratios and spatial resolution limited by volume conduction effects [62] [75].
This fundamental tradeoff directly influences data processing strategies. Invasive systems must handle enormous data volumes from individual neuron monitoring but can implement more precise decoding algorithms. Non-invasive systems work with noisier, more spatially blurred signals but benefit from greater channel count scalability without surgical constraints. Interestingly, some researchers question whether the extreme data rates of invasive systems are always necessary, given psychophysical evidence that human behavior operates at surprisingly low information rates—perhaps 10-50 bits per second for complex tasks like speech [76].
Diagram Title: Invasive vs. Non-Invasive Neural Interfaces Tradeoffs
The choice between invasive and non-invasive approaches ultimately depends on the application requirements. For restoring motor control or communication in severely paralyzed individuals, the superior performance of invasive interfaces may justify the surgical risks. As of mid-2025, human trials with invasive BCIs have demonstrated capabilities such as controlling digital devices, texting with thoughts alone, and achieving speech decoding at 99% accuracy with latencies under 0.25 seconds [61]. For applications such as neurofeedback training or basic assistive control, non-invasive approaches may offer sufficient performance without implantation risks.
Experimental Protocols and Methodologies
Benchmarks for Evaluating Processing Performance
Standardized evaluation methodologies are essential for comparing data processing approaches across different neural interface systems. Key metrics include decoding accuracy (often reported as classification accuracy for discrete tasks or correlation coefficients for continuous variables), latency (the delay between neural activity and output generation), and adaptability (performance maintenance over time despite neural non-stationarities) [74].
For motor decoding tasks, benchmark paradigms often involve controlling computer cursors, robotic limbs, or virtual avatars. In speech decoding, metrics include word error rate, vocabulary size, and decoding speed. A 2025 study on individual finger movement decoding used both binary (thumb vs. pinky) and ternary (thumb vs. index vs. pinky) classification tasks with majority voting accuracy as the primary performance metric [75]. These standardized assessments enable direct comparison between different hardware and software approaches.
Case Study: Individual Finger Movement Decoding
A July 2025 study published in Nature Communications provides a detailed experimental protocol for evaluating neural decoding algorithms. The researchers implemented a real-time noninvasive robotic control system using movement execution and motor imagery of individual finger movements to drive robotic finger motions [75]. The methodology included:
- Participants: 21 able-bodied experienced BCI users
- Experimental Design: One offline familiarization session followed by two online sessions each for finger ME and MI tasks
- Signal Acquisition: EEG recordings using standard scalp electrodes
- Processing Pipeline: EEGNet-8.2 architecture for real-time decoding with fine-tuning mechanism
- Feedback: Both visual (on-screen color indicators) and physical (robotic hand movement)
- Performance Assessment: Majority voting accuracy calculated as percentage of trials where predicted class matched true class
This comprehensive protocol illustrates the sophisticated methodologies required to evaluate data processing approaches for high-channel-count systems, balancing experimental control with ecological validity.
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Research Tools for Neural Data Processing
| Tool/Category | Specific Examples | Function/Purpose | Representative Use Cases |
|---|---|---|---|
| Signal Processing Frameworks | BCI2000, OpenViBE, NeuroPype, BCILAB [74] | Real-time data acquisition, processing, and visualization | Implementing and testing decoding algorithms in real-time scenarios |
| Deep Learning Architectures | EEGNet, ViSNet, Equiformer, Deep Potential (DP) [77] [75] | Automated feature learning from raw neural data | Decoding individual finger movements, speech recognition from neural signals |
| Transfer Learning Approaches | Fine-tuning mechanisms, pre-trained models [75] | Adapting models to individual users and sessions | Addressing inter-session variability, reducing calibration time |
| Biocompatible Materials | Flexible polymers (parylene C, polyimide), conducting polymers [62] [73] | Improving electrode-tissue interface, reducing foreign body response | Chronic implantation, maintaining signal stability |
| Wireless Communication Systems | Custom protocols, integrated transmitters [61] [73] | Transmitting processed neural data externally | Enabling untethered operation, reducing infection risk |
| Spike Sorting Algorithms | Various customized approaches | Identifying and classifying action potentials from individual neurons | Neural population analysis, single-neuron decoding |
Future Directions and Research Opportunities
The relentless progression of high-channel-count neural interfaces ensures that data processing will remain a critical challenge and opportunity for innovation. Several promising directions are emerging, including the development of more sophisticated AI architectures specifically designed for neural data characteristics, the integration of neuromorphic computing approaches for ultra-efficient processing, and the creation of adaptive systems that co-evolve with the user's brain [74] [62].
Of particular interest is the potential for bidirectional interfaces that not record from but also stimulate neural tissue, creating closed-loop systems for therapeutic applications. These systems present additional processing challenges, as they must interpret neural activity and generate appropriate stimulation patterns in real time, often with strict power constraints. Advances in algorithm efficiency, particularly through edge computing approaches, will be essential for realizing the full potential of these sophisticated neural interfaces.
For researchers and drug development professionals, understanding these technological foundations is increasingly important for designing rigorous experiments and interpreting neural data accurately. As the field progresses, collaboration between neuroscience, engineering, and computer science will be essential for developing solutions to the data processing bottleneck—ultimately enabling new approaches to understanding and treating neurological disorders.
For researchers and drug development professionals, the choice between invasive and non-invasive neural interfaces extends beyond signal fidelity to fundamental questions of long-term system reliability. The core trade-off is stark: invasive brain-computer interfaces (BCIs) provide unparalleled signal quality for precise neurological research but face significant biological and mechanical durability challenges, while non-invasive systems offer superior safety and stability at the cost of spatial resolution and signal strength [38] [5]. This hardware reliability directly impacts data consistency in longitudinal studies and clinical trials, making durability and power strategies critical design considerations.
The stability of the hardware-brain interface presents the primary challenge for chronic implantation. Invasive devices must contend with the brain's immune response, including glial scarring that insulates electrodes and degrades signal quality over time [38] [72]. Meanwhile, non-invasive systems battle the signal-to-noise ratio inherent in measuring neural activity through the skull, compounded by day-to-day application variability [5]. Wireless power systems further complicate this landscape, balancing transfer efficiency against thermal and size constraints. This guide compares these approaches through experimental data to inform selection criteria for research applications requiring sustained neural recording or stimulation.
Comparative Analysis of Interface Reliability and Performance
The tables below synthesize key performance metrics and reliability characteristics from current research and commercial systems, providing a quantitative basis for comparison.
Table 1: Performance and Reliability Metrics by BCI Type
| Parameter | Invasive BCIs | Semi-Invasive BCIs (ECoG) | Non-Invasive BCIs (EEG) |
|---|---|---|---|
| Signal Quality | Records single neuron activity (action potentials); Highest signal-to-noise ratio [38] | Detects local field potentials; Moderate signal quality [38] | Records large-scale brain activity; Lowest signal-to-noise ratio due to skull interference [38] [5] |
| Spatial Resolution | Precise; can pinpoint specific brain regions [38] | Lower than invasive; cannot isolate single neurons [38] | Reduced; blurs brain activity patterns [38] |
| Information Transfer Rate | Highest bit rates (~100-200 bits/minute) [38] | Moderate bit rates (~40-60 bits/minute) [38] | Lowest bit rates (~5-25 bits/minute) [38] |
| Typical Longevity & Stability | Limited long-term stability; body may reject foreign object; signal degradation from scar tissue [38] [72] | Improved long-term stability compared to invasive; reduced scarring [38] | Highest long-term stability; no surgical risks or tissue damage [38] |
| Primary Failure Modes | Scar tissue formation, device failure/malfunction, infection [38] | Infection (though less than invasive), device migration [38] | Sensitivity to external noise (muscle movement, electrical devices) [38] [5] |
Table 2: Wireless Power and Hardware Durability Strategies
| Strategy Category | Invasive/Semi-Invasive Approach | Non-Invasive Approach | Key Research Findings |
|---|---|---|---|
| Power Delivery | Fully implantable systems with wireless power transfer (WPT) via inductive coupling or near-infrared optical links [72] [78] | External batteries; no implantation challenges [38] | Recent WPT systems achieve up to 86.7% efficiency with ~5% voltage fluctuation using machine learning-optimized designs [79] |
| Material Biocompatibility | Flexible materials (graphene, soft polymers, ultrathin films) to minimize immune response and scarring [72] | Dry electrodes for ergonomic design and user comfort [8] | Flexible, conformal electrodes significantly reduce chronic immune response, improving signal stability [72] |
| System Durability | Focus on miniaturization, encapsulation, and reducing power consumption to ~1.1mW for chronic use [72] | Consumer-grade designs prioritizing ease of use and portability [38] [52] | Miniaturization and low-power chips (e.g., Neuralink's N1 Implant) enable fully implanted wireless systems [52] |
Experimental Protocols for Assessing Reliability
To evaluate the long-term reliability claims for different neural interfaces, researchers employ standardized experimental protocols. The following workflows detail key methodologies for assessing material biocompatibility and wireless power efficiency.
Protocol 1: Chronic Biocompatibility and Signal Stability Testing
Objective: To quantify the foreign body response and signal degradation over time for implanted neural interfaces [72].
Methodology Details:
- Implantation: Devices are implanted in rodent or non-human primate models using stereotactic surgery [38]. Test groups include devices with different material properties (e.g., rigid silicon vs. flexible graphene-based electrodes) [72].
- Signal Recording: Neural data (single-unit activity, local field potentials) is recorded daily. The Signal-to-Noise Ratio (SNR) is calculated by comparing the amplitude of neural spikes to the background noise floor [38].
- Histological Analysis: After a predetermined period (typically 12+ weeks), brain tissue is sectioned and stained. Glial Fibrillary Acidic Protein (GFAP) labels astrocytes, and Ionized Calcium-Binding Adapter Molecule 1 (IBA1) labels microglia. The thickness of the GFAP-positive scar capsule around the implant is quantified [72].
- Data Correlation: A correlation analysis between SNR decay over time and glial scar thickness establishes the relationship between biological response and functional decline.
Protocol 2: Wireless Power Transfer Efficiency and Stability
Objective: To measure the efficiency and thermal performance of wireless power systems for neural interfaces under realistic load conditions [79] [78].
Methodology Details:
- System Setup: The WPT system consists of an external transmitter coil and a receiver coil embedded in a phantom material that simulates the electrical and thermal properties of human tissue [78].
- Load Testing: The electrical load on the receiver is dynamically varied using a programmable circuit to mimic the changing power demands of a real BCI (e.g., from sleep mode to active stimulation) [79].
- Efficiency Calculation: Input power ((P{in})) to the transmitter and output power ((P{out})) from the receiver are measured simultaneously with high-precision power analyzers. Efficiency ((η)) is calculated as: (η = (P{out} / P{in}) \times 100\%).
- Stability Metrics: Voltage fluctuation is measured as the percentage deviation from the target output voltage. Thermal performance is assessed using infrared imaging of the receiver coil to ensure temperature increases remain within safe biological limits (typically <2°C rise) [79].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Materials and Reagents for Neural Interface Reliability Research
| Item Name | Function/Application | Relevance to Reliability |
|---|---|---|
| Flexible Graphene Electrodes | Conformal neural recording interfaces [72] | High flexibility reduces mechanical mismatch with brain tissue, minimizing chronic immune response and scar tissue formation [72]. |
| Utah & Michigan Arrays | Standard for high-density invasive neural recording [38] [8] | Provide benchmark performance data but are prone to scar-tissue induced signal degradation; used as a control in longevity studies [38]. |
| GFAP & IBA1 Antibodies | Histological staining for astrocytes and microglia [72] | Enable quantification of glial scar formation, the primary biological failure mode for invasive interfaces [72]. |
| Dry EEG Electrodes | Non-invasive signal acquisition without conductive gel [8] | Improve usability and consistency for repeated daily applications in long-term non-invasive BCI studies [8]. |
| Inductive Power Coils | Wireless power transfer for implanted devices [78] | Key component for testing the efficiency and thermal safety of fully implantable, long-duration BCI systems [79] [78]. |
The divergence in reliability strategies between invasive and non-invasive neural interfaces presents researchers with a critical, application-dependent choice. Invasive interfaces are advancing toward chronic reliability through material science innovations like flexible graphene electrodes and sophisticated wireless power systems, making them suitable for long-term, high-fidelity research on specific neural circuits despite inherent biological challenges [72]. Conversely, non-invasive interfaces leverage their inherent safety and stability for longitudinal studies where daily reapplication is feasible and supreme signal quality is not the primary requirement [38] [5].
For the research and drug development professional, the selection framework extends beyond initial performance. It must incorporate the planned duration of the study, the required consistency of the signal, and the institutional capacity to support the respective hardware systems. As wireless power efficiency approaches the 90% benchmark with minimal fluctuation [79], and as biocompatible materials mitigate the foreign body response [72], the horizon for long-term, reliable neural interfacing looks increasingly promising for both fundamental neuroscience and therapeutic development.
Critical Analysis and Validation: A Comparative Assessment of Interface Modalities
The evolution of Brain-Computer Interface (BCI) and neuromotor interface technology has bifurcated into two primary methodologies: invasive techniques, which involve surgical implantation of electrodes directly into or onto brain tissue, and non-invasive techniques, which utilize external sensors to detect neural activity through the skull and scalp [80]. This divergence presents a critical strategic decision for researchers and clinicians, particularly when selecting interfaces for specific clinical applications such as communication for paralyzed individuals, motor restoration, or epilepsy management.
The core trade-off is fundamental: invasive interfaces provide high-fidelity neural signals but introduce surgical risks and long-term biocompatibility challenges, whereas non-invasive interfaces offer greater safety and accessibility but often face limitations in signal resolution and robustness [6] [15]. The global BCI market reflects this duality, with the medical segment currently representing the largest application area and projected to grow significantly [80]. This guide provides an objective, data-driven comparison of the performance of these two approaches, framing the discussion within the broader thesis that the future of neural interfaces may lie in hybrid systems that optimize the trade-off between signal quality and invasiveness [80].
The following tables summarize key performance metrics for invasive and non-invasive interfaces across major clinical application domains, based on recent state-of-the-art demonstrations.
Table 1: Performance Comparison for Communication & Motor Control Applications
| Clinical Application | Interface Type & Technology | Key Performance Metric | Reported Performance | Notable Study/System |
|---|---|---|---|---|
| Handwriting Decoding | Invasive (Intracortical) | Texting Speed (Words per Minute) | ~90 WPM [7] | High-performance invasive BCI [7] |
| Non-invasive (sEMG Wristband) | Texting Speed (Words per Minute) | 20.9 WPM (+16% with personalization) [7] | Generic sEMG Interface [7] | |
| Discrete Gesture Control | Invasive (Intracortical) | Gesture Detection Rate (per second) | High (Precise rates vary by study) [5] | Robotic arm control systems [5] |
| Non-invasive (sEMG Wristband) | Gesture Detection Rate (per second) | 0.88 detections/sec [7] | Generic sEMG Interface [7] | |
| Continuous Navigation | Invasive (Intracortical) | Target Acquisition Rate (per second) | High for complex control [5] | Cortical control of computer cursor [5] |
| Non-invasive (sEMG Wristband) | Target Acquisition Rate (per second) | 0.66 acquisitions/sec [7] | Generic sEMG Interface [7] | |
| Prosthetic Control | Invasive (ECoG) | Classification Accuracy for Motor Tasks | >90% accuracy [5] | WIMAGINE system for exoskeletons [5] |
| Non-invasive (EEG) | Classification Accuracy for Motor Tasks | 65-75% accuracy [80] | Motor Imagery-based BCIs [16] |
Table 2: General Performance Characteristics and Clinical Suitability
| Parameter | Invasive Interfaces (e.g., ECoG, Intracortical) | Non-Invasive Interfaces (e.g., EEG, sEMG) |
|---|---|---|
| Spatial Resolution | Single neuron level (micrometers) [6] | ~1-10 cm (scalp-level) [6] [15] |
| Temporal Resolution | Millisecond precision [5] | Millisecond precision (EEG) [16] |
| Signal-to-Noise Ratio | High [5] [15] | Low to Moderate [5] [15] |
| Information Transfer Rate | High [6] | Low to Moderate [6] |
| Typical Clinical Use Case | Severe paralysis, complex prosthetic control [5] [16] | Basic communication, stroke rehab, epilepsy monitoring [16] |
| Primary Risk Profile | Surgical risks (infection, tissue damage), long-term stability [81] [15] | Minimal risk; limitations in signal robustness [15] |
| User Acceptance | Lower due to invasiveness [6] | Higher due to safety and accessibility [6] |
Detailed Experimental Protocols
To contextualize the performance data, this section details the experimental methodologies behind key recent studies for both invasive and non-invasive approaches.
Non-Invasive Surface EMG (sEMG) Protocol for Handwriting and Gesture Decoding
A landmark 2025 study demonstrated a high-performance, generic non-invasive neuromotor interface using surface electromyography (sEMG) [7].
- Signal Acquisition: Researchers developed a dry-electrode, multichannel sEMG wristband (sEMG-RD) that is wireless, comfortable, and can be donned in seconds. The device was manufactured in four sizes to accommodate diverse wrist anatomies and featured a high sample rate (2 kHz) and low-noise design (2.46 μVrms) to capture subtle electrical potentials at the wrist, including putative motor unit action potentials (MUAPs) during low-movement conditions [7].
- Data Collection & Behavioral Prompting: Data was collected from a large and anthropometrically diverse cohort of participants (162 to 6,627 across different tasks). Participants wore the sEMG band on their dominant wrist and were prompted by custom software to perform specific tasks:
- Handwriting Task: Participants held their fingers together as if gripping a pen and "wrote" prompted text in the air [7].
- Discrete-Gesture Task: A prompter instructed participants to perform one of nine distinct gestures (e.g., finger pinches, thumb swipes) in a randomized order [7].
- Wrist Control Task: Participants controlled a cursor, with wrist position tracked via motion capture for training data [7].
- Signal Processing and Decoding: A real-time processing engine recorded sEMG activity and prompt timestamps. A time-alignment algorithm was used post-hoc to infer the actual gesture event times, accounting for participant reaction time. The sEMG data was used to train neural network models for decoding. The study highlighted the use of large-scale data to build generic models that generalize across users and the potential for personalization to improve performance further [7].
Invasive Intracortical BCI Protocol for Speech and Motor Decoding
Invasive BCI protocols, often tested in clinical trials with a limited number of participants, focus on achieving high-fidelity control.
- Signal Acquisition: Invasive protocols typically utilize electrodes implanted directly into the brain tissue, such as the Utah Array, or placed on the cortical surface (ECoG). These electrodes record neural signals like single-unit activity (SUA), multi-unit activity (MUA), and local field potentials (LFP) with high spatial and temporal resolution. For motor decoding, electrodes are often targeted at regions like the primary motor cortex or the posterior parietal cortex [5] [6].
- Experimental Task Design:
- Motor Control: Participants with paralysis are trained to control a computer cursor or robotic arm by imagining limb movements. The BCI system decodes these movement intentions from the recorded neural activity in real-time [5].
- Speech Decoding: Recent high-profile studies have participants attempt to speak or imagine speaking. The invasive arrays record the rich neural activity from speech-related motor cortices, which is then decoded into text or synthesized speech at high speeds [7] [5].
- Signal Processing and Decoding: The high-bandwidth signals from hundreds of electrodes require sophisticated processing. Decoding involves spike sorting to identify individual neurons and the application of complex machine learning algorithms (e.g., deep learning) to map neural firing patterns to intended outputs. A critical aspect of invasive BCI operation is closed-loop feedback, where the user adapts their neural activity based on the system's output, and the system itself adapts to the user's evolving neural patterns [6].
Signaling Pathways and System Workflows
The fundamental difference in the origin and pathway of the signals acquired by each interface type underpins their performance characteristics.
Diagram 1: Neural Signal Pathways for Invasive vs. Non-Invasive Interfaces
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of BCI research requires a suite of specialized hardware and software solutions. The table below details key components.
Table 3: Essential Research Tools for Neural Interface Development
| Tool Category | Specific Examples & Models | Primary Function in Research |
|---|---|---|
| Invasive Electrodes | Utah Array (Blackrock Neurotech), Neuropixels [5] [9] | High-density recording of single and multi-unit neural activity from the cortical surface or within brain tissue. |
| Minimally Invasive Implants | WIMAGINE (ECoG) [5], Stentrode (Endovascular) [5] | Record from the cortical surface or from within blood vessels, offering a balance between signal quality and invasiveness. |
| Non-Invasive Biosensors | High-density EEG caps, Dry EEG electrodes [8], sEMG wristbands [7] | Record electrical activity from the scalp (EEG) or muscles (sEMG) without surgical intervention. |
| Data Acquisition Systems | Intan Technologies RHD, Blackrock Neurotech systems [9] | Amplify, filter, and digitize analog neural signals from electrodes for processing. |
| Signal Processing Software | EEGLAB, BCILAB, FieldTrip, custom Python/ML pipelines [5] [16] | Preprocess data (filtering, artifact removal), extract features, and classify/decode neural signals. |
| Calibration & Prompting Software | Custom behavioral prompting systems [7] | Guide participants through standardized tasks (e.g., gesture performance) to generate labeled training data for decoding models. |
The direct performance comparison reveals a clear but nuanced landscape. Invasive neural interfaces remain the undisputed leader for the most demanding clinical applications, such as high-speed communication and dexterous prosthetic control, where their superior signal quality translates directly into higher information transfer rates and more complex control [7] [5] [6]. However, this comes at the cost of significant surgical risks and challenges with long-term signal stability.
Conversely, non-invasive interfaces, particularly with recent breakthroughs in sEMG and the application of deep learning to EEG, are rapidly closing the performance gap for a wide range of applications [7] [16]. Their paramount advantages of safety, accessibility, and higher user acceptance make them suitable for broader deployment in rehabilitation, basic communication, and monitoring. The choice between invasive and non-invasive technology is not a matter of which is universally better, but which is optimal for a specific clinical need, weighing the requirement for precision against considerations of risk and accessibility. The future of the field, aligned with the broader thesis of neural interface research, points toward hybrid systems that leverage the strengths of both approaches to create more powerful and practical solutions for patients.
Brain-computer interfaces (BCIs) represent a revolutionary technology that establishes a direct communication pathway between the brain and external devices, creating what researchers term a "non-muscular channel" for interaction [82]. The fundamental challenge in BCI design lies in balancing the degree of surgical invasiveness against the quality of neural signals obtained, a trade-off that dictates both clinical risk and functional performance. Neural interfaces exist along a continuum of invasiveness, with fully invasive devices implanted directly into brain tissue, semi-invasive systems placed on the brain surface or within natural body cavities, and non-invasive approaches that operate entirely external to the skull [38].
This comparison guide examines the risk-benefit profiles across this spectrum, focusing specifically on how surgical interventions correlate with signal fidelity metrics critical for research and clinical applications. The relationship between these factors is not merely linear but involves complex interactions between biomedical engineering, neurosurgical techniques, and neural decoding algorithms. Understanding these trade-offs is essential for researchers selecting appropriate methodologies for specific applications, from basic neuroscience investigations to restorative neurotechnologies for patients with paralysis, amyotrophic lateral sclerosis, or other severe neurological disorders [83] [37].
Comparative Analysis of Neural Interface Technologies
Technical Performance Metrics
Table 1: Quantitative Comparison of Neural Interface Technologies
| Parameter | Non-Invasive BCIs | Semi-Invasive BCIs | Fully Invasive BCIs |
|---|---|---|---|
| Spatial Resolution | Low (cm-scale) [38] | Moderate (mm-scale) [38] | High (μm-scale) [38] |
| Temporal Resolution | Moderate (∼10-100 ms) [8] | High (∼1-10 ms) [8] | Very High (sub-millisecond) [8] |
| Signal-to-Noise Ratio | Low (skull attenuation) [38] | Moderate [38] | High [38] |
| Information Transfer Rate | 5-25 bits/minute [38] | 40-60 bits/minute [38] | 100-200 bits/minute [38] |
| Typical Signal Types | EEG, MEG, fNIRS [8] | ECoG, local field potentials [38] [81] | Single-unit activity, multi-unit activity [38] [81] |
| Penetration Depth | Superficial cortical areas [38] | Cortical surface and local regions [38] | Deep brain structures possible [81] |
Table 2: Surgical Risk and Practical Implementation Factors
| Factor | Non-Invasive BCIs | Semi-Invasive BCIs | Fully Invasive BCIs |
|---|---|---|---|
| Surgical Procedure | None [38] | Craniotomy required [38] | Complete craniotomy with dura mater penetration [38] |
| Infection Risk | None [38] | Moderate [38] | High (can lead to meningitis/brain abscess) [38] |
| Tissue Damage Risk | None [38] | Low (minimal brain contact) [83] | High (direct brain penetration) [38] |
| Long-Term Stability | High (no biological rejection) [38] | Moderate (reduced scar formation) [38] | Low (scarring, immune response) [38] |
| Ethical Concerns | Minimal [38] | Moderate [38] | Significant (brain alteration, identity issues) [38] |
| Regulatory Pathway | Less stringent [8] | Moderately stringent [8] | Highly stringent [8] |
Performance and Functional Outcomes
Performance metrics across BCI types reveal a consistent pattern where increased invasiveness correlates with enhanced functional capabilities. A recent systematic review and individual patient meta-analysis of invasive BCIs in humans demonstrated median task performance accuracy of 76.00% for cursor control tasks, 80.00% for motor tasks, and 93.27% for communication tasks across 214 patients [84]. These performance levels substantially exceed what is typically achievable with non-invasive systems, particularly for complex tasks requiring fine motor control or rapid communication.
The Chinese Academy of Sciences team reported that their invasive BCI system completes the entire process of neural signal extraction, movement intent interpretation, and control command generation within tens of milliseconds, faster than the blink of an eye, enabling real-time control of external devices [83]. This temporal performance is critical for applications requiring seamless interaction, such as controlling prosthetic limbs or communicating through thought-driven interfaces.
Experimental Protocols and Methodologies
Signal Acquisition Protocols
Non-Invasive BCI Methodology:
- Electrode Placement: Application of 64-256 electrodes according to the international 10-20 system using conductive gel or dry electrode technologies [8]
- Signal Acquisition: Recording of electrocortical activity through the skull and scalp, typically capturing postsynaptic potentials with amplitudes of 10-100 μV [8]
- Preprocessing: Application of spatial filters (Laplacian, common average reference), bandpass filtering (0.5-60 Hz for ERPs, 8-30 Hz for motor imagery), and artifact removal techniques including independent component analysis [82]
- Feature Extraction: Time-frequency analysis using wavelet transforms or autoregressive modeling, followed by dimensionality reduction techniques [82]
Semi-Invasive BCI Methodology:
- Surgical Implantation: Craniotomy with placement of electrode grids (e.g., ECoG arrays) on the cortical surface without penetrating brain tissue [38]
- Signal Acquisition: Recording of local field potentials and cortical surface activity with higher spatial resolution than non-invasive methods [81]
- Feature Extraction: Analysis of high-frequency gamma oscillations (70-200 Hz) which correlate with neuronal firing rates and provide superior control signals [38]
Fully Invasive BCI Methodology:
- Surgical Implantation: Stereotactic guidance for precise placement of microelectrode arrays (e.g., Utah Array) into targeted brain regions [38]
- Signal Acquisition: Recording of single-unit and multi-unit activity with sampling rates typically exceeding 30 kHz to capture action potential waveforms [85]
- Spike Sorting: Application of algorithms such as principal component analysis or wavelet-based feature extraction to classify individual neurons [81]
- Decoding: Implementation of Kalman filters, recurrent neural networks, or support vector machines to translate neural activity into control commands [84]
Performance Validation Protocols
Standardized assessment methodologies are critical for comparing BCI performance across different interface types. The field has developed several validation protocols:
Communication Task Protocol:
- Setup: Matrix-based spelling interface or imagined speech decoding paradigm [84]
- Metrics: Characters per minute, accuracy rate, information transfer rate [38]
- Testing Paradigm: Copy spelling (replicating predefined phrases) or free spelling tasks [84]
Motor Control Task Protocol:
- Setup: 2D or 3D cursor control, robotic arm manipulation, or prosthetic device control [84]
- Metrics: Path efficiency, task completion time, target acquisition accuracy [84]
- Testing Paradigm: Center-out reaching tasks or activities of daily living simulation [83]
Clinical Assessment Protocol:
- Metrics: Quality of life measures, independence scales, and functional independence measures [37]
- Long-term Tracking: Signal stability over time, device reliability, adverse event monitoring [84]
Visualizing the Risk-Benefit Relationship
BCI Risk-Benefit Trade-off Relationships
The diagram above illustrates the fundamental relationships between invasiveness and key performance metrics across the BCI spectrum. As we move from non-invasive to fully invasive approaches, signal fidelity and information transfer rates increase proportionally, while surgical risks correspondingly elevate and clinical adoption potential decreases due to procedural complexity and regulatory hurdles [38].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for Neural Interface Studies
| Item | Function | Example Specifications |
|---|---|---|
| Flexible Microelectrodes | Neural signal acquisition with minimal tissue damage | Ultra-flexible electrodes (∼1% hair diameter) [83] |
| Graphene-Based Sensors | High-resolution neural recording with biocompatibility | Graphene electrodes for real-time multi-region activity capture [72] |
| ECoG Grid Arrays | Cortical surface recording for semi-invasive approaches | High-density electrode grids (256+ contacts) [38] |
| Utah Microelectrode Arrays | Intracortical recording for fully invasive BCIs | 96-256 microelectrodes, 1-1.5mm length [8] |
| Biocompatible Encapsulants | Long-term protection of implanted electronics | Parylene-C, silicone elastomers for chronic implants [72] |
| Neural Signal Processors | Real-time signal amplification and filtering | 30kHz sampling, programmable filter settings [85] |
| Spike Sorting Algorithms | Identification and classification of individual neurons | PCA, wavelet analysis, or template matching techniques [81] |
| Machine Learning Decoders | Translation of neural signals to device commands | Recurrent neural networks, Kalman filters [84] |
| Stereo-tactic Navigation Systems | Precise surgical placement of invasive electrodes | Sub-millimeter accuracy for targeted implantation [83] |
The selection of an appropriate neural interface technology requires careful consideration of the trade-offs between surgical risk and signal fidelity. Non-invasive BCIs offer the lowest risk profile and are suitable for basic neuroscience research, cognitive monitoring, and applications where the highest signal quality is not essential [38]. Semi-invasive approaches provide an intermediate solution with enhanced signal quality while mitigating some risks associated with fully penetrating brain tissue [72]. Fully invasive BCIs deliver superior signal quality and performance for the most demanding applications, including dexterous prosthetic control and communication restoration for severely disabled individuals, but require acceptance of significant surgical risks and potential long-term stability issues [83].
Future directions in neural interface development focus on overcoming these trade-offs through technological innovations, including flexible bioelectronics that minimize tissue damage [83], advanced signal processing that extracts more information from less invasive recordings [85], and closed-loop systems that adapt to the user's changing neural patterns [72]. As these technologies mature, the risk-benefit calculus will continue to evolve, potentially enabling new research paradigms and therapeutic applications that are currently limited by existing technological constraints.
The field of neural interfaces represents a groundbreaking convergence of neuroscience, engineering, and artificial intelligence, creating direct communication pathways between the brain and external devices. This technological domain has evolved into two primary research and development trajectories: invasive interfaces that require surgical implantation into brain tissue and non-invasive systems that operate externally to the skull. The fundamental distinction lies in the trade-off between signal fidelity and accessibility—invasive methods provide unparalleled access to neural signals but introduce surgical risks and regulatory complexity, while non-invasive approaches offer greater safety and scalability at the cost of signal resolution [38] [5].
This analysis examines the current market landscape, key players, investment patterns, and regulatory pathways shaping both technological approaches. Understanding these dimensions is crucial for researchers, investors, and drug development professionals navigating this rapidly evolving field, where technological capabilities are advancing while ethical considerations and regulatory frameworks continue to develop [37] [31].
The brain-computer interface market demonstrates robust growth driven by increasing neurological disorder prevalence, technological advancements, and substantial investment inflows. Market projections consistently indicate significant expansion across multiple forecasting horizons, with varying growth rates reflecting different methodological approaches and market segment definitions.
Table 1: Global BCI Market Size Projections
| Source | Base Year Value | Projection Year | Projected Value | CAGR | Market Segmentation |
|---|---|---|---|---|---|
| Spherical Insights [86] | $2.87B (2024) | 2035 | $15.14B | 16.32% | Includes all BCI types |
| Strait Research [87] | $2.83B (2025) | 2033 | $8.73B | 15.13% | Includes all BCI types |
| Fact.MR [88] | $324M (2025) | 2035 | $1.33B | 15.2% | Wireless neural interfaces only |
Regional adoption patterns reveal distinct centers of innovation and market growth. North America, particularly the United States, currently dominates with approximately 39.86% market share, driven by advanced healthcare infrastructure, concentration of key players (Neuralink, Synchron, Blackrock Neurotech), and substantial research funding [86] [87]. The Asia-Pacific region demonstrates the fastest growth rate, fueled by increasing healthcare investments, government-supported research initiatives, and a large patient population. Countries including China, Japan, and South Korea are making significant investments in BCI research, with China establishing a $56 million research center at Fudan University specifically focused on BCI applications for restoring sight and mobility [86] [87].
Technology Comparison: Invasive vs. Non-Invasive Approaches
The core technological divide in neural interfaces centers on the method of signal acquisition, with distinct trade-offs in signal quality, risk profile, and application suitability.
Table 2: Technical Performance Comparison of BCI Approaches
| Parameter | Invasive BCIs | Semi-Invasive BCIs | Non-Invasive BCIs |
|---|---|---|---|
| Signal Quality | Highest (single neuron resolution) [38] | Moderate (local field potentials) [38] | Lowest (skull attenuation) [38] [5] |
| Spatial Resolution | Highest (micrometer scale) [38] | Moderate (millimeter scale) [38] | Lowest (centimeter scale) [38] |
| Temporal Resolution | Millisecond precision [38] | Millisecond precision [38] | Millisecond precision (EEG) [5] |
| Information Transfer Rate | 100-200 bits/minute [38] | 40-60 bits/minute [38] | 5-25 bits/minute [38] |
| Surgical Risk | Highest (brain surgery required) [38] | Moderate (craniotomy required) [38] | None [38] |
| Long-term Stability | Limited (scar tissue formation) [38] | Better than invasive [38] | Highest [38] |
Invasive Neural Interfaces
Invasive systems are implanted directly into brain tissue, typically targeting specific regions such as the motor cortex for movement control or speech centers for communication restoration. These interfaces provide the highest signal-to-noise ratio and spatial resolution, enabling decoding of individual neuron activity (action potentials) [38]. The surgical implantation process involves craniotomy, opening of the dura mater, and precise electrode array placement using stereotactic guidance [38]. Chronic challenges include potential tissue damage, scar formation that can degrade signal quality over time, and infection risk [38] [5].
Non-Invasive Neural Interfaces
Non-invasive approaches primarily utilize electroencephalography (EEG), functional near-infrared spectroscopy (fNIRS), or magnetoencephalography (MEG) to record neural activity through the skull [38] [5]. These systems benefit from no surgical risks, easier application, and minimal ethical concerns, but contend with significantly attenuated and noisy signals due to skull interference [38] [5]. Recent advancements in dry electrodes, AI-powered signal processing, and wearable form factors are improving the usability and performance of non-invasive systems [8] [88].
Semi-Invasive Approaches
Occupying a middle ground, semi-invasive interfaces such as electrocorticography (ECoG) and endovascular electrodes (Stentrode) are positioned beneath the skull but not within brain tissue [38] [5]. These approaches offer better signal quality than non-invasive methods while reducing surgical risks compared to fully invasive implants. The Stentrode, developed by Synchron, represents a particularly innovative approach utilizing blood vessels as natural pathways to position electrodes near cortical regions, demonstrating the feasibility of minimally disruptive implantation techniques [37] [5].
Figure 1: BCI Signal Processing Workflow and Technology Trade-offs
Key Players and Competitive Landscape
The neural interface ecosystem comprises established medical device companies, well-funded startups, and research institutions, each pursuing distinct technological approaches and market segments.
Table 3: Key Players in the Neural Interface Market
| Company/Institution | Primary Approach | Key Technology | Funding/Status | Target Applications |
|---|---|---|---|---|
| Neuralink [86] [52] | Invasive | N1 Implant with 1024 electrodes | $680M raised; Human trials ongoing | Paralysis, communication |
| Blackrock Neurotech [86] [52] | Invasive | NeuroPort Array | 30+ human implants | Paralysis, ALS, communication |
| Paradromics [86] | Invasive | Connexus Direct Data Interface | DARPA funding; 2025 human trials planned | Communication (ALS, stroke) |
| Precision Neuroscience [86] | Semi-invasive | Layer 7 Cortical Interface | $102M raised | Paralysis, communication |
| Synchron [86] [37] | Semi-invasive | Stentrode (endovascular) | Gates/Bezos backing; FDA approval for study | Paralysis, device control |
| Kernel [86] | Non-invasive | Kernel Flow (light-based) | $100M+ raised | Wellness, cognitive monitoring |
| MindMaze [86] | Non-invasive | EEG with VR integration | Approved in US/EU hospitals | Neurorehabilitation |
The competitive landscape reveals distinct strategic positioning across the invasiveness spectrum. Invasive interface companies (Neuralink, Blackrock Neurotech, Paradromics) typically target severe neurological conditions where high-fidelity control justifies surgical intervention, focusing on medical applications with potential for breakthrough device designation [86]. Semi-invasive approaches (Synchron, Precision Neuroscience) aim to balance performance and safety, potentially addressing broader patient populations through reduced surgical complexity [86] [37]. Non-invasive players (Kernel, MindMaze, various EEG companies) target both medical and consumer markets, with applications ranging from clinical rehabilitation to wellness monitoring [86] [31].
Traditional medical device companies including Medtronic, Boston Scientific, and Abbott Laboratories are leveraging their regulatory experience and distribution networks to establish presence in the neuromodulation and neural monitoring segments, often through incremental innovations rather than disruptive BCI platforms [88].
Funding Trends and Investment Landscape
Investment in neural interface technologies has accelerated dramatically, with distinct funding patterns across technological approaches and development stages.
Venture Capital and Private Investment
Private funding has concentrated on invasive and semi-invasive approaches with clear medical applications. Neuralink leads with approximately $680 million raised across multiple rounds, while Precision Neuroscience secured over $100 million in its latest funding round [86] [87]. These substantial investments reflect confidence in the potential for BCIs to address severe neurological conditions and establish new therapeutic paradigms. Synchron has attracted backing from prominent technology leaders including Bill Gates and Jeff Bezos, signaling cross-industry recognition of the field's potential [86].
Government and Institutional Funding
Public funding continues to play a crucial role in foundational research and high-risk development. The U.S. BRAIN Initiative, launched in 2013, has established multiple industry partnerships with companies including Inscopix, Blackrock Microsystems, and Ripple Neuro to advance neural interface technology [9]. Defense applications represent another significant funding source, with DARPA supporting companies including Paradromics for communication restoration technologies [86]. European support mechanisms include grants from the European Innovation Council, such as the funding awarded to Onward Medical for developing ARC-BCI therapy for stroke recovery [87].
Investment Distribution Trends
Analysis of funding patterns reveals disproportionate investment in invasive technologies relative to their current market share, reflecting investor anticipation of transformative medical applications and potential for high returns despite longer regulatory pathways. Non-invasive technologies typically secure smaller funding rounds but target larger total addressable markets including consumer wellness and gaming applications [8] [31].
Regulatory Pathways and Approval Status
Regulatory frameworks for neural interfaces vary by technology classification, with distinct pathways for invasive medical devices versus non-invasive systems.
United States FDA Framework
The U.S. Food and Drug Administration has established regulatory pathways for different BCI categories through its Center for Devices and Radiological Health (CDRH). Invasive BCIs typically pursue the Pre-Market Approval (PMA) pathway, requiring extensive clinical data to demonstrate safety and effectiveness for specific medical indications [37]. The FDA has granted Breakthrough Device designation to multiple invasive BCI companies including Paradromics and Precision Neuroscience, accelerating development and review processes for technologies addressing unmet medical needs [86] [87].
Synchron's Stentrode became the first permanently implanted BCI to receive FDA approval for an early feasibility study in the United States, establishing an important regulatory precedent for endovascular approaches [86]. Neuralink received FDA approval for initial human trials in 2024, focusing initially on patients with quadriplegia [86] [52].
Regional Regulatory Variations
European markets operate under the Medical Device Regulation (MDR) framework, with CE marking indicating conformity with safety and performance standards. MindMaze's neurorehabilitation system has received regulatory approval for hospital use in both the U.S. and Europe, demonstrating the feasibility of multi-regional regulatory strategy for non-invasive medical BCIs [86].
Asian regulatory bodies are developing frameworks tailored to regional healthcare priorities, with China implementing policies to accelerate BCI development as part of national technology initiatives [31] [87].
Figure 2: Regulatory Pathway for Invasive Neural Interfaces
Research Methodologies and Experimental Protocols
Rigorous experimental design is essential for validating neural interface performance and securing regulatory approval. Standardized protocols have emerged across key application domains.
Motor Intent Decoding and Prosthetic Control
Objective: To assess the ability of a BCI system to translate motor cortex activity into control signals for external devices [5].
Protocol:
- Participant Selection: Patients with spinal cord injury, ALS, or stroke with preserved cognitive function; healthy controls for non-invasive system development [5].
- Task Design:
- Motor Imagery: Participants imagine limb movements without physical execution
- Attempted Movement: Patients with paralysis attempt actual movements
- Visual Cueing: On-screen prompts guide movement timing and type [5]
- Data Acquisition:
- Invasive: Utah arrays or microelectrodes implanted in motor cortex
- Non-invasive: High-density EEG systems with 64-128 channels [5]
- Signal Processing:
- Bandpass filtering (0.5-300 Hz for invasive, 0.1-100 Hz for EEG)
- Common average referencing to reduce noise
- Artifact removal using independent component analysis [5]
- Feature Extraction:
- Time-domain: Signal amplitude, velocity
- Frequency-domain: Band power in mu (8-12 Hz) and beta (13-30 Hz) rhythms [5]
- Decoding Algorithms:
- Support vector machines for classification tasks
- Kalman filters or deep learning networks for continuous decoding [5]
- Performance Metrics:
- Information transfer rate (bits/minute)
- Task completion accuracy and timing
- Fitts' law testing for motor control applications [5]
Speech Decoding and Communication Restoration
Objective: To decode intended speech from neural signals for patients with communication impairments [5] [87].
Protocol:
- Participant Selection: Patients with ALS, brainstem stroke, or locked-in syndrome [87].
- Task Design:
- Overt Speech: Participants speak actual words (healthy controls or patients with residual speech)
- Covert Speech: Participants imagine speaking without vocalization
- Auditory Stimuli: Listening to words or sentences [5]
- Data Acquisition:
- Invasive: Electrodes implanted in speech-related cortical areas (inferior frontal gyrus, sensorimotor cortex)
- Non-invasive: High-temporal resolution EEG or MEG [5]
- Neural Features:
- High-frequency broadband power (70-150 Hz) from ECoG
- Low-frequency signals (<30 Hz) for phonetic feature extraction [5]
- Decoding Approaches:
- Acoustic feature regression (formant frequencies, spectral content)
- Classification-based approaches for small vocabulary
- Sequence-to-sequence models for continuous speech [5]
- Validation Metrics:
Table 4: Essential Research Reagents and Materials for BCI Development
| Category | Specific Examples | Function/Application | Considerations |
|---|---|---|---|
| Electrode Technologies | Utah Array, Neuropixels, Micro-ECoG grids | Neural signal acquisition | Biocompatibility, chronic stability, channel count [9] [5] |
| Non-invasive Sensors | Wet electrodes, Dry electrodes, fNIRS optodes | Scalp-based signal recording | Electrode-skin impedance, setup time, comfort [8] [5] |
| Signal Acquisition Systems | Neural signal processors, Amplifiers, AD converters | Signal conditioning and digitization | Sampling rate, noise floor, wireless capability [88] [5] |
| Implant Materials | Silicon, Polyimide, Parylene-C, Iridium oxide | Biocompatible encapsulation and contacts | Foreign body response, long-term stability [9] |
| Decoding Algorithms | SVM, CNN, RNN, Kalman filters, Transfer learning | Neural signal interpretation | Computational efficiency, adaptive capability [5] |
| Validation Tools | Phantom heads, Bench-top test systems, Computational models | System performance verification | Signal fidelity simulation, automated testing [5] |
Future Outlook and Strategic Implications
The neural interface landscape continues to evolve along multiple dimensions, with significant implications for research direction, investment priorities, and clinical application.
Technology Development Trajectories
Invasive interfaces are progressing toward higher channel counts, improved biocompatibility, and wireless operation. Companies including Neuralink and Paradromics are developing systems with thousands of recording channels to capture more detailed neural population activity [86]. Materials science innovations focus on reducing foreign body response and improving long-term signal stability through flexible, tissue-like electrodes [9].
Non-invasive technologies are benefiting from advancements in dry electrodes, miniaturization, and integration with augmented reality platforms. The emergence of wearable MEG systems and quantum-enhanced sensors promises significant improvements in spatial resolution for non-invasive approaches [8] [88].
Clinical Translation and Commercialization
Near-term clinical applications will continue focusing on severe neurological conditions where the risk-benefit ratio justifies invasive intervention. The increasing availability of minimally invasive approaches such as Synchron's Stentrode may expand patient eligibility for implanted systems [37]. Non-invasive technologies are positioned for broader adoption in neurorehabilitation, cognitive assessment, and mental health monitoring [86] [31].
Regulatory harmonization efforts will be crucial for global market development, particularly as companies seek multi-regional clinical trials and commercialization strategies. The establishment of standardized performance metrics and validation protocols will accelerate regulatory review and clinical adoption [37].
Research Priorities and Knowledge Gaps
Key research priorities include improving long-term stability of invasive interfaces, enhancing information transfer rates for non-invasive systems, and developing adaptive decoding algorithms that maintain performance across sessions and behavioral states. The integration of neural interfaces with neuromodulation approaches represents another promising direction, creating closed-loop systems that can both read from and write to the nervous system [5].
Significant knowledge gaps remain in understanding neural plasticity in response to chronic interface use, optimizing human learning for BCI control, and developing comprehensive frameworks for ethical implementation across diverse cultural contexts [37] [31]. Addressing these challenges will require sustained interdisciplinary collaboration between neuroscientists, engineers, clinicians, and ethicists.
Strengths, Weaknesses, Opportunities, and Threats (SWOT) Analysis for Each Technology Class
The field of neural interfaces is undergoing a period of unprecedented acceleration, marked by a clear dichotomy between invasive and non-invasive technology classes. Invasive Brain-Computer Interfaces (iBCIs) require surgical implantation of electrodes directly onto or into brain tissue, while non-invasive approaches record neural signals through the scalp [8] [5]. This guide provides an objective SWOT analysis and performance comparison of these distinct technological pathways, contextualized within the broader thesis of their application in clinical and research settings. The analysis is designed to inform researchers, scientists, and drug development professionals about the current state-of-the-art, enabling informed decisions on technology selection for specific investigative or therapeutic goals. The content is framed around experimental data and standardized protocols to ensure a rigorous, evidence-based comparison.
Invasive neural interfaces, such as intracortical electrode arrays and minimally invasive Stentrodes, offer high-fidelity signal acquisition by physically accessing neural tissue [72] [5]. Non-invasive interfaces, primarily using electroencephalography (EEG) and emerging methods like digital holographic imaging, acquire signals through the skull, prioritizing safety and accessibility at the cost of signal resolution [5] [89]. A recent systematic review and individual patient meta-analysis of iBCIs provides robust performance benchmarks, showing a median task performance accuracy of 93.27% for communication tasks, 80.00% for motor tasks, and 76.00% for cursor control tasks across 214 patients [84]. In contrast, a state-of-the-art non-invasive interface using surface electromyography (sEMG) demonstrated handwriting transcription at 20.9 words per minute and high gesture classification accuracy in a continuous control task [7]. The following table summarizes key quantitative performance metrics and characteristics for a direct comparison.
Table 1: Performance and Characteristics of Invasive vs. Non-Invasive Neural Interfaces
| Metric | Invasive Interfaces | Non-Invasive Interfaces |
|---|---|---|
| Communication Task Performance | 93.27% median accuracy (Cursor control: 76.00%) [84] | 20.9 words per minute (sEMG) [7] |
| Spatial Resolution | Single-neuron / Multi-unit activity (High) [5] | Scalp-level signals (Low) [5] [89] |
| Temporal Resolution | Millisecond precision (High) [72] | Millisecond to second scale (Moderate to High) [8] |
| Signal-to-Noise Ratio | High [5] | Low, susceptible to physiological clutter [5] [89] |
| Clinical Trial Scope (as of 2024) | 93 studies, 214 patients in systematic review [84] | Scalable to 1,000s of participants for data collection [7] |
| Target Applications | Restoration of motor function, speech decoding, complex device control [72] [84] | Assistive technology, neurorehabilitation, consumer wellness, research [8] [7] |
SWOT Analysis
Invasive Neural Interfaces
Table 2: SWOT Analysis of Invasive Neural Interfaces
| Strengths | Weaknesses |
|---|---|
| • High-Fidelity Signals: Capable of recording single-neuron and multi-unit activity with high spatial and temporal resolution, enabling complex decoding for speech and motor control [72] [84] [5].• High Performance: Demonstrated high accuracy in clinical tasks, such as over 93% for communication, making them suitable for severe disabilities [84].• Direct Brain Access: Enables precise closed-loop stimulation and interaction with specific neural circuits [72]. | • Surgical Risks & Invasiveness: Implantation requires craniotomy or endovascular surgery, carrying inherent risks of infection, bleeding, and tissue damage [72] [90].• Biotic Response & Longevity: Chronic immune response (gliosis, scarring) can degrade signal quality over time, limiting long-term reliability and stability [72] [90].• Limited Scalability & High Cost: High surgical and hardware costs, coupled with specialized clinical requirements, restrict widespread adoption [88] [84]. |
| Opportunities | Threats |
| • Restoring Critical Functions: Potential to restore independence for individuals with quadriplegia, ALS, and locked-in syndrome by enabling control of computers and assistive devices [37] [68].• Treatment of Neurological Disorders: Emerging applications in treating conditions like depression, addiction, and epilepsy via targeted neuromodulation [72].• Technological Miniaturization: Advances in flexible, bio-compatible materials (e.g., graphene, ultra-thin films) and wireless systems are improving safety and portability [72] [90]. | • Stringent Regulatory Hurdles: The path to FDA and other regulatory approvals is complex and lengthy, requiring extensive clinical trials to prove safety and efficacy [88] [68].• Ethical and Privacy Concerns: Raises critical issues regarding informed consent, data privacy, identity, and agency, demanding robust ethical frameworks [68].• Commercialization Challenges: High development costs, technical complexities, and the need for specialized surgical expertise can slow translation to market [88] [90]. |
Non-Invasive Neural Interfaces
Table 3: SWOT Analysis of Non-Invasive Neural Interfaces
| Strengths | Weaknesses |
|---|---|
| • Safety & Accessibility: No surgical risk, making them suitable for a broader population and enabling rapid deployment in research and consumer settings [8] [5].• Ease of Use & Scalability: Systems like high-density EEG and sEMG wristbands can be donned quickly, facilitating large-scale data collection from thousands of participants [8] [7].• Consumer & Research Adoption: Lower cost and minimal risk support applications in wellness, cognitive monitoring, and human-computer interaction research [8] [88]. | • Limited Signal Resolution: Signals are attenuated and blurred by the skull and scalp, resulting in lower spatial resolution and signal-to-noise ratio compared to invasive methods [5] [89].• Lower Information Transfer Rate: Bandwidth is insufficient for decoding complex motor commands or imagined speech with high precision [72] [5].• Susceptibility to Artifact: Vulnerable to contamination from muscle movement, eye blinks, and other physiological signals, complicating signal processing [5] [89]. |
| Opportunities | Threats |
| • Broad Therapeutic Applications: Significant potential in neurorehabilitation (e.g., post-stroke motor recovery), cognitive training, and management of mental health conditions [37] [5].• Integration with Consumer Tech: Convergence with AR/VR headsets, hearables, and wearable wellness devices creates large market opportunities [8] [88].• Novel Signal Discovery: Research into new signal modalities, such as tissue deformation measured via digital holographic imaging, could revolutionize non-invasive sensing [89]. | • Performance Plateau: Fundamental physical barriers (skull) may limit the ability to achieve the fidelity required for high-bandwidth applications, regardless of algorithmic advances [5].• Market Fragmentation: Proliferation of consumer-grade devices with unvalidated claims can erode scientific credibility and user trust [8].• Data Privacy & Standardization: Lack of standardized data protocols and the collection of sensitive neural data raise significant privacy and cybersecurity concerns [88]. |
Experimental Protocols and Methodologies
Protocol for Assessing Invasive BCI Performance (Based on Systematic Review)
A recent systematic review and individual patient meta-analysis established a standardized methodology for evaluating iBCI performance in human subjects [84].
Objective: To quantitatively assess the performance of various iBCI systems in restoring motor, communication, and sensory functions. Methodology:
- Literature Search: A comprehensive search of databases (Medline, EMBASE, PubMed, Cochrane) from inception until April 13, 2024, was conducted.
- Study Selection: Included primary studies reporting the use of iBCIs in human subjects to restore function. Excluded studies without quantitative performance metrics or those not involving human implants.
- Data Extraction: Key endpoints were extracted for each study, including:
- Electrode Type: (e.g., Utah Array, Stentrode, ECoG grids).
- Decoder Algorithm: (e.g., Kalman filters, Recurrent Neural Networks).
- BCI Effector: The device being controlled (e.g., computer cursor, robotic arm, speech synthesizer).
- Task Performance: Accuracy, information transfer rate, and speed for specific tasks (cursor control, motor tasks, communication).
- Data Synthesis: A narrative synthesis of hardware and software trends was performed. An Individual Patient Data (IPD) meta-analysis was conducted to identify factors significantly affecting iBCI performance. Key Findings: The analysis of 93 studies involving 214 patients provided the performance benchmarks cited in Table 1, highlighting the superiority of recurrent neural network decoders and the challenges of portability and chronic use [84].
Protocol for a Generic Non-Invasive Neuromotor Interface
A landmark 2025 study detailed the development of a high-performance, generalizable non-invasive interface using surface electromyography (sEMG) [7].
Objective: To create a non-invasive neuromotor interface for human-computer interaction that generalizes across users without per-person calibration. Methodology:
- Hardware Platform: A dry-electrode, multichannel sEMG wristband (sEMG-RD) was developed with high sample rate (2 kHz) and low noise (2.46 μVrms). The device was manufactured in four sizes to fit a range of wrist anatomies.
- Data Collection at Scale: Data were collected from a large and anthropometrically diverse cohort of participants (162 to 6,627 individuals, depending on the task). Participants performed three primary tasks while wearing the sEMG band:
- Wrist Control: Controlling a cursor using wrist angles tracked by motion capture.
- Discrete-Gesture Detection: Performing nine distinct gestures in a randomized order.
- Handwriting: "Writing" prompted text in the air while holding fingers together.
- Model Training and Generalization: Neural networks were trained on the aggregated data. A critical focus was on testing cross-user and cross-session generalization, comparing the performance of generic models against single-participant models.
- Closed-Loop Evaluation: Performance was tested in real-time (online) on computer-based tasks, measuring target acquisitions per second for continuous control and words per minute for handwriting. Key Findings: The generic sEMG decoding models achieved a handwriting rate of 20.9 WPM and high gesture detection rates without user-specific calibration, demonstrating the feasibility of a high-bandwidth, non-invasive interface that works out-of-the-box [7].
Signaling Pathways and Experimental Workflows
The following diagrams illustrate the core workflows and signal pathways for both invasive and non-invasive neural interfaces, based on the experimental protocols described above.
Invasive BCI Signal Decoding Pathway
Invasive BCI Signal Decoding Pathway: This workflow depicts the high-fidelity pathway from neural signal to device control, characteristic of invasive interfaces.
Non-Invasive sEMG Interface Workflow
Non-Invasive sEMG Interface Workflow: This workflow highlights the scalable data-driven approach used to develop a generic model for non-invasive interaction.
The Scientist's Toolkit: Research Reagent Solutions
This section details key materials and technologies essential for conducting research in neural interfaces, as featured in the cited experiments and broader field development.
Table 4: Essential Research Tools for Neural Interface Development
| Tool / Material | Function in Research |
|---|---|
| Utah Array / Neuropixels | Invasive microelectrode arrays for high-density recording of single-neuron and multi-unit activity in cortical regions. A cornerstone of iBCI research [84] [5]. |
| Stentrode | A minimally invasive endovascular electrode array implanted via blood vessels. Used to record cortical signals without open-brain craniotomy [72] [5]. |
| Dry sEMG Electrodes | Contact sensors in wearable wristbands that acquire myographic signals without conductive gel. Enable comfortable, long-duration recording for non-invasive interface studies [7]. |
| Digital Holographic Imaging (DHI) | An optical system using laser interferometry to detect nanometer-scale tissue deformations associated with neural activity. A novel modality for future non-invasive BCI [89]. |
| Recurrent Neural Networks (RNNs) | A class of deep learning decoder algorithms particularly effective for processing time-series neural data, improving the performance of both invasive and non-invasive BCIs [84] [7]. |
| WIMAGINE Device | An implantable, wireless ECoG grid system designed for chronic recording from the surface of the brain. Used in research to restore walking ability [5]. |
| Flexible Polymer / Graphene Electrodes | Biocompatible, soft substrate electrodes that minimize immune response and improve long-term signal stability in chronic invasive implants [72] [90]. |
The field of neural interfaces has long been divided between invasive and non-invasive approaches, each with distinct trade-offs. Invasive Brain-Computer Interfaces (BCIs), which require surgical implantation of electrodes directly into neural tissue, provide unparalleled signal quality with high spatial and temporal resolution, enabling recording from individual neurons and precise modulation of specific brain circuits [30]. These systems can achieve millimeter-scale precision and millisecond temporal resolution, capturing both action potentials and local field potentials (LFPs) [91]. However, this comes at the cost of increased medical risks, including surgical complications, potential tissue response, and higher accessibility barriers [30] [91].
In contrast, non-invasive approaches such as electroencephalography (EEG), functional near-infrared spectroscopy (fNIRS), and magnetoencephalography (MEG) offer safer, more accessible alternatives but have traditionally faced fundamental limitations in signal-to-noise ratio and spatial resolution [39] [91]. These methods record through the scalp and skull, which act as biological filters that attenuate and spatially blur neural signals [91]. The recent breakthrough from Johns Hopkins University Applied Physics Laboratory (APL) represents a potential paradigm shift in this landscape, introducing a novel signal source—neural tissue deformation—that may overcome these historical constraints [89].
Breakthrough Technology: Digital Holographic Imaging for Neural Recording
The Johns Hopkins APL team has developed a Digital Holographic Imaging (DHI) system that identifies and validates a previously unexplored neural signal: the tiny tissue deformations that occur during neural activity [89]. This mechanical manifestation of brain activity represents a fundamental departure from traditional electrical or hemodynamic measurement approaches. The system operates by actively illuminating neural tissue with a laser and precisely recording the light scattered from the tissue using a specialized camera [89]. This information is processed to form a complex image from which magnitude and phase information can be extracted to spatially resolve changes in brain tissue velocity at the nanometer scale [89].
The key innovation lies in detecting mechanical displacements of only tens of nanometers in height that correspond to neural firing events [89]. This mechanical coupling between electrical activity and tissue movement provides an entirely new information channel for assessing brain function. Researchers described the challenge as a "remote sensing problem," where they needed to detect this minute neural signal within a complex, cluttered environment filled with competing physiological noise from blood flow, heart rate, and respiratory activity [89].
Experimental Protocol and Validation
The validation of this novel signal required a rigorous multi-year experimental approach:
- System Development: Researchers built a custom DHI system with nanometer-scale sensitivity capable of capturing tiny tissue velocity changes [89].
- Signal Correlation: The team conducted numerous fundamental tests to ensure the detected tissue deformation signals were truly correlated with neuronal firing events, distinguishing them from physiological clutter [89].
- Noise Mitigation: Advanced signal processing techniques were developed to separate neural deformation signals from competing noise sources including pulsatile blood flow, cardiac rhythms, and respiratory patterns [89].
- Ancillary Benefit Discovery: During noise mitigation, researchers discovered that the physiological "clutter" itself could provide valuable insights into overall brain health, including the ability to noninvasively record intracranial pressure—a measurement that traditionally requires drilling through the skull [89].
The DHI system's ability to simultaneously monitor neural activity and clinically relevant physiological parameters represents a significant advantage over existing technologies, providing both functional and physiological information from a single measurement platform [89].
Comparative Analysis: Non-Invasive Neural Recording Technologies
Table 1: Performance Comparison of Neural Recording Technologies
| Technology | Spatial Resolution | Temporal Resolution | Primary Signal Source | Key Advantages | Principal Limitations |
|---|---|---|---|---|---|
| Digital Holographic Imaging (DHI) | High (theoretically cellular) | High (ms potential) | Neural tissue deformation | Novel signal source; noninvasive intracranial pressure monitoring | Early development stage; technical complexity |
| Electroencephalography (EEG) | Low (cm-scale) | High (ms) | Post-synaptic potentials | Whole-brain coverage; low cost; established methodology | Limited spatial resolution; skull attenuation effects |
| Functional MRI (fMRI) | High (mm-scale) | Low (seconds) | Hemodynamic (BOLD) response | Excellent spatial resolution; widespread availability | Indirect neural measure; poor temporal resolution |
| Electrocorticography (ECoG) | High (mm-scale) | High (ms) | Cortical field potentials | High signal quality; clinical applicability | Invasive (subdural/epidural); limited coverage |
| Intracortical Microelectrodes | Very high (single neuron) | Very high (ms) | Action potentials & LFPs | Gold standard resolution; single-unit recording | Highly invasive; tissue response; surgical risk |
Table 2: Signal Characteristics and Applications Comparison
| Parameter | DHI | EEG | fNIRS | ECoG | Intracortical |
|---|---|---|---|---|---|
| Signal Origin | Tissue deformation | Pyramidal neuron postsynaptic currents | Hemodynamic changes | Cortical field potentials | Neuronal spiking & LFPs |
| Penetration Depth | Full cortical depth | Superficial layers | Cortical surface | Cortical surface | All implant depths |
| Temporal Resolution | Potentially ms (theoretical) | Millisecond | Seconds | Millisecond | Sub-millisecond |
| Spatial Resolution | High (theoretically cellular) | ~1-3 cm | ~1 cm | 1 mm - 1 cm | 50-500 μm |
| Signal Fidelity | High (direct mechanical coupling) | Low (skull filtering) | Moderate (indirect measure) | Very high | Highest |
| Clinical Translation | Early research phase | Widespread clinical use | Emerging clinical use | Established (epilepsy) | Limited (research focus) |
Technical Implementation and Research Toolkit
Digital Holographic Imaging Workflow
The experimental workflow for DHI-based neural recording involves a sophisticated integration of optical hardware and computational processing, as shown in the following diagram:
Research Reagent Solutions
Table 3: Essential Research Materials for High-Resolution Neural Interface Development
| Research Tool | Function/Purpose | Example Applications |
|---|---|---|
| Digital Holographic Imaging System | Records nanometer-scale tissue deformation from neural activity | Novel signal validation; non-invasive intracranial pressure monitoring [89] |
| Microelectrode Arrays (MEAs) | Records action potentials and LFPs from neuronal populations | Invasive BCI motor control; high-fidelity neural decoding [30] [91] |
| High-Density EEG Systems | Records electrical activity from scalp surface | Clinical epilepsy monitoring; cognitive state assessment [39] [91] |
| fNIRS Systems | Measures hemodynamic changes via light absorption | Mobile brain imaging; developmental neuroscience studies [9] |
| Graph Neural Networks (GNN) | Analyzes molecular structure for drug response prediction | Drug discovery; molecular property prediction [92] |
| Neuromorphic Computing Platforms | Brain-inspired computing for neural disorder modeling | Drug development; neurological disease simulation [93] |
Implications for Drug Discovery and Development
The advancement of non-invasive high-resolution neural recording technologies intersects with parallel progress in artificial intelligence and computational modeling, creating new paradigms for neurological drug development. Neuromorphic computing—computational systems inspired by the brain's structure and function—provides a transformative framework for modeling neurological disorders in drug development [93]. These systems can simulate complex neural circuits affected by conditions like Alzheimer's, Parkinson's, and epilepsy, potentially overcoming limitations of traditional animal models that have contributed to high failure rates in late-stage clinical trials for neurological therapies [93].
The integration of deep learning approaches with high-resolution neural data further enhances drug discovery capabilities. Graph Neural Networks (GNNs) have demonstrated particular promise in molecular property prediction and drug-target interaction analysis [92]. These networks naturally preserve molecular structural information, enabling more accurate prediction of drug response and revealing comprehensive mechanisms of action between drugs and their targets [92]. The explainable graph-based drug response prediction (XGDP) approach not only enhances prediction accuracy but also identifies salient functional groups of drugs and their interactions with significant genes in cancer cells [92].
For researchers and pharmaceutical developers, these technological advances create new opportunities to:
- Utilize high-resolution neural data to identify precise biomarkers for neurological conditions
- Employ neuromorphic models to simulate drug effects on pathological neural circuits
- Leverage explainable AI to understand drug mechanism of action at molecular levels
- Develop more targeted therapeutic interventions with potentially higher success rates
The validation of novel neural signals through approaches like digital holographic imaging represents a significant milestone in the evolution of non-invasive neural interfaces. While the technology remains in early development, its potential to bridge the critical gap between invasive and non-invasive approaches could fundamentally reshape the landscape of neural interface research and applications [89]. The DHI system's additional capability to monitor clinically relevant parameters like intracranial pressure further enhances its value proposition for both research and clinical translation [89].
The broader field of neural interfaces continues to advance rapidly, with invasive approaches maintaining superiority for high-information-content applications like controlling complex robotic arms [30], while non-invasive methods are becoming increasingly sophisticated for both research and clinical applications such as communication aids for locked-in patients and cognitive state monitoring [39]. The emerging synergy between neural interface technologies and advanced computational approaches like neuromorphic computing and explainable AI promises to accelerate progress across both domains [93] [92].
For the research community, the critical challenges ahead include:
- Validating the DHI approach in human subjects and clinical populations
- Further refining signal processing techniques to enhance signal-to-noise ratio
- Developing standardized experimental protocols for novel signal validation
- Establishing correlation metrics between tissue deformation signals and specific neural functions
- Integrating multi-modal data streams to create comprehensive brain activity maps
As these technologies mature, they hold the potential to not only advance basic neuroscience knowledge but also transform clinical practice in neurology, psychiatry, and pharmaceutical development, ultimately enabling more effective interventions for the approximately one billion people worldwide affected by neurological disorders [93].
Conclusion
The choice between invasive and non-invasive neural interfaces is not a binary one but a strategic decision based on the specific application, required signal fidelity, and acceptable risk profile. Invasive systems currently offer unparalleled resolution for restoring complex functions in severe neurological disorders, while non-invasive technologies are rapidly advancing and offer a safer, more scalable path for broader clinical and research applications. Future directions will be shaped by breakthroughs in materials science to improve biocompatibility, sophisticated AI for powerful signal decoding, and the maturation of closed-loop systems that both read from and write to the nervous system. For researchers and drug developers, this evolving landscape presents unprecedented opportunities to develop novel therapeutics, identify precise neurological biomarkers, and ultimately redefine treatment paradigms for millions of patients with neurological conditions.
References
- 1. Brain-Computer Interfaces : Exploring the Last Frontier [https://www.byfounders.vc/insights/brain-computer-interfaces]
- 2. and Challenges | by Sam | Medium Neural Interfaces Benefits [https://medium.com/@ossamaabbas1999/neural-interfaces-benefits-and-challenges-de220188bf9f]
- 3. Unlocking the Brain's Secrets [https://www.numberanalytics.com/blog/ultimate-guide-invasive-neural-interfaces-neuroengineering]
- 4. JMIR Neurotechnology - Invasive Brain-Computer Interfaces ... [https://neuro.jmir.org/2024/1/e60151]
- 5. Non-Invasive Brain-Computer Interfaces: State of the Art and Trends - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11861396/]
- 6. Frontiers | Invasive . vs - Non Signals for... Invasive Neuronal [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2016.00295/full]
- 7. A generic non - invasive neuromotor interface for... | Nature [https://www.nature.com/articles/s41586-025-09255-w?error=cookies_not_supported&code=b21007fc-3659-495e-9d2e-f0cd4d54b6cc]
- 8. Brain Computer Interfaces -2045: Technologies, Players, Forecasts 2025 [https://www.idtechex.com/en/research-report/brain-computer-interfaces/1024]
- 9. Invasive and Non-Invasive Neural Interfaces: Forecasts and Applications 2018-2028: IDTechEx [https://www.idtechex.com/en/research-report/invasive-and-non-invasive-neural-interfaces-forecasts-and-applications-2018-2028/573]
- 10. Current Review of Optical Neural Interfaces for Clinical Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8400671/]
- 11. Types of neural signals: action potentials and field potentials [https://fiveable.me/brain-computer-interfaces/unit-3/types-neural-signals-action-potentials-field-potentials/study-guide/ZfTITXFngYgMZwNv]
- 12. Concurrent fNIRS and EEG for Brain Function Investigation: A Systematic, Methodology-Focused Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9371171/]
- 13. of Comparison and ECoG signals | Fiveable intracortical [https://fiveable.me/brain-computer-interfaces/unit-5/comparison-ecog-intracortical-signals/study-guide/ahyTx7o9wtbS31R2]
- 14. Frontiers | fNIRS , EEG , ECG, and GSR reveal an effect of complex... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1459653/full]
- 15. Diving Deeper into BCI Technologies: Non-Invasive vs .... | Medium [https://shashank-goyal-blogs.medium.com/diving-deeper-into-bci-technologies-non-invasive-vs-invasive-modalities-4cd55f74ab12]
- 16. Recent applications of EEG-based brain-computer-interface in the medical field | Military Medical Research | Full Text [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-025-00598-z]
- 17. Uncovered Neural Interfaces [https://www.numberanalytics.com/blog/comprehensive-guide-neural-interfaces-neuropsychology]
- 18. Strategic Integration: A Cross-Disciplinary Review of the fNIRS-EEG Dual-Modality Imaging System for Delivering Multimodal Neuroimaging to Applications - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11506513/]
- 19. Spatial, Temporal Resolution and Signal-to-Noise Ratio | SpringerLink [https://link.springer.com/chapter/10.1007/978-3-319-22141-0_4]
- 20. The influence of spatial resolution and smoothing on the detectability of resting-state and task fMRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5736131/]
- 21. The Science of Neural Interface Systems - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2921719/]
- 22. Meeting brain–computer interface user performance expectations using a deep neural network decoding framework | Nature Medicine [https://www.nature.com/articles/s41591-018-0171-y]
- 23. 7T-fMRI: Faster temporal yields optimal BOLD sensitivity... resolution [https://pubmed.ncbi.nlm.nih.gov/28286317/]
- 24. Spatial, Temporal Resolution and Signal-to-Noise Ratio | Thoracic Key [https://thoracickey.com/spatial-temporal-resolution-and-signal-to-noise-ratio/]
- 25. , Electrodes | Products | Blackrock Neurotech Utah Array [https://blackrockneurotech.com/products/utah-array/]
- 26. How the Utah is advancing BCI science Array [https://www.medicaldesignandoutsourcing.com/utah-array-brain-computer-interface-blackrock-neurotech/]
- 27. Novel transducers for high - channel - count neuroelectronic recording... [https://pubmed.ncbi.nlm.nih.gov/34695765/]
- 28. Frontiers | Explant Analysis of Utah Electrode Arrays Implanted in... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2021.759711/full]
- 29. Clinical applications of penetrating neural and interfaces ... Utah [https://pubmed.ncbi.nlm.nih.gov/27762237/]
- 30. Modulating Brain Activity with Invasive Brain–Computer Interface: A Narrative Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856340/]
- 31. The Neuro- Interface Generation: How Brain-Computer... | Medium [https://medium.com/@raktims2210/the-neuro-interface-generation-how-brain-computer-interfaces-are-transforming-human-ai-strategy-67a17b093d49]
- 32. Mind and machine: The state of neurotech in [https://www.insights.onegiantleap.com/blogs/mind-and-machine-the-state-of-neurotech-in-2025/]
- 33. Bio-inspired electronics: Soft, biohybrid, and “living” neural interfaces | Nature Communications [https://www.nature.com/articles/s41467-025-57016-0]
- 34. The Future of Neural Control [https://www.numberanalytics.com/blog/future-of-neural-control]
- 35. Neuralink, Passive BCIs And The Future Of Neuroadaptive Technology [https://www.forbes.com/councils/forbestechcouncil/2024/11/14/neuralink-passive-bcis-and-the-future-of-neuroadaptive-technology/]
- 36. Biohybrid neural interfaces: improving the biological integration of neural implants - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10720954/]
- 37. -led approaches to Tech could address global health... neural interfaces [https://www.weforum.org/stories/2025/01/brain-computer-interfaces-healthcare/]
- 38. Types of BCIs: invasive , semi- invasive , and non - invasive | Fiveable [https://fiveable.me/brain-computer-interfaces/unit-1/types-bcis-invasive-semi-invasive-non-invasive/study-guide/Wz8G1AecOttsxslK]
- 39. - Non Brain-Computer Invasive : State of the Art and Trends Interfaces [https://pubmed.ncbi.nlm.nih.gov/39186407/]
- 40. Unlocking the Brain's Secrets [https://www.numberanalytics.com/blog/ultimate-guide-invasive-bci]
- 41. Brain-Computer Chip: Ushering in the First Year of Commercialization [https://eu.36kr.com/en/p/3423925429816962]
- 42. Brain-computer interfaces: communication and restoration of... [https://pubmed.ncbi.nlm.nih.gov/17234696/]
- 43. Brain-computer Interface Chip in the Real World: 5 Uses You'll Actually... [https://www.linkedin.com/pulse/brain-computer-interface-chip-real-world-5-uses-youll-314zc]
- 44. How new technologies enable the human-machine economy | EY - Global [https://www.ey.com/en_gl/megatrends/how-emerging-technologies-are-enabling-the-human-machine-hybrid-economy]
- 45. Frontiers | Seizure outcomes and complications associated with stereoelectroencephalography versus subdural electrodes for invasive monitoring in epilepsy surgery: a meta-analysis [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1619288/full]
- 46. [2106.08008] Towards Long-term Non-invasive Monitoring for Epilepsy via Wearable EEG Devices [https://arxiv.org/abs/2106.08008]
- 47. - Non neuromodulation for the treatment of drug-resistant... invasive [https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-025-02981-2]
- 48. Frontiers | Non-invasive brain stimulation for stroke-related motor impairment and disability: an umbrella review of systematic review and meta-analysis [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1633986/full]
- 49. The Evolution of Poststroke Recovery: Advances and Challenges [https://www.medscape.com/viewarticle/evolution-poststroke-recovery-advances-and-challenges-2025a10006bf]
- 50. The Latest Advances in Non - Invasive for Insomnia... Neurostimulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12089259/]
- 51. 15+ Top Neurofeedback Devices Review 2025: Pro Brain Training At Home [https://outliyr.com/best-home-neurofeedback-devices-machines]
- 52. Neurotechnology & Brain-Computer Interfaces in 2025 - Ambula Healthcare [https://www.ambula.io/neurotechnology-brain-computer-interfaces-in-2025/]
- 53. The Neurotech Revolution [https://www.numberanalytics.com/blog/neurotech-revolution-invasive-neural-interfaces]
- 54. of cognitive and memory decline in psychotropic Biomarkers users drug [https://link.springer.com/article/10.1007/s00702-024-02837-4]
- 55. Revolutionizing brain‒computer interfaces: overcoming biocompatibility challenges in implantable neural interfaces | Journal of Nanobiotechnology | Full Text [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03573-x]
- 56. Encoding and Neural at Scale Decoding [https://arxiv.org/html/2504.08201v3]
- 57. Boosted Neural : Achieving Extreme Reliability of... | CoLab Decoders [https://colab.ws/articles/10.1109%2Fjsac.2025.3531553]
- 58. March 2025 Highlights - Journal of Biomedical and Health Informatics (JBHI) [https://www.embs.org/jbhi/articles/march-2025-highlights/]
- 59. the Brain Decoding [https://www.numberanalytics.com/blog/quantitative-methods-neural-decoding]
- 60. China's first invasive brain-computer interface clinical trial launched... [https://www.globaltimes.cn/page/202506/1336164.shtml]
- 61. BCIs in 2025: Trials, Progress, and Challenges [https://andersenlab.com/blueprint/bci-challenges-and-opportunities]
- 62. Revolutionizing brain‒computer interfaces: overcoming biocompatibility challenges in implantable neural interfaces - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12243264/]
- 63. Novel method to improve the biocompatibility and chronic stability of... [https://www.news-medical.net/news/20250630/Novel-method-to-improve-the-biocompatibility-and-chronic-stability-of-neural-electrode-implants.aspx]
- 64. Neural Interfaces for Robotics and Prosthetics: Current Trends [https://www.mdpi.com/2224-2708/14/6/105]
- 65. Multidimensional advances in neural interface technology for peripheral nerve repair: From material innovation to clinical translation - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S2590006425006623]
- 66. What’s New in Breast Implant Technology in 2025 ? [https://www.acibadembeautycenter.com/en/blog/what-s-new-in-breast-implant-technology-in-2025]
- 67. Recent advances in neural interfaces-Materials chemistry to clinical translation - PubMed [https://pubmed.ncbi.nlm.nih.gov/34690420/]
- 68. Frontiers | Neuralink’s brain-computer interfaces: medical innovations and ethical challenges [https://www.frontiersin.org/journals/human-dynamics/articles/10.3389/fhumd.2025.1553905/full]
- 69. Brain Computer Interface ( BCI ) Research Report 2025 -2035: EEG... [https://finance.yahoo.com/news/brain-computer-interface-bci-research-090400037.html]
- 70. Frontiers | Multiscale fusion enhanced spiking neural network for... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1551656/full]
- 71. Breakthrough in noninvasive brain activity recording by... | LinkedIn [https://www.linkedin.com/posts/johns-hopkins-university-applied-physics-laboratory_a-new-path-to-noninvasive-brain-computer-activity-7364010597513846785-6WUS]
- 72. : Brain Tech Transforming Connectivity Neural Interfaces 2025 [https://infotribes.com/neural-interfaces-2025-brain-computer-tech/]
- 73. Neuralink's $650M Series E: Accelerating the Future of Brain ... [https://applyingai.com/2025/07/neuralinks-650m-series-e-accelerating-the-future-of-brain-computer-interfaces/]
- 74. Neural–Computer Interfaces: Theory, Practice, Perspectives [https://www.mdpi.com/2076-3417/15/16/8900]
- 75. EEG-based brain-computer interface enables real-time ... [https://www.nature.com/articles/s41467-025-61064-x]
- 76. The speed of human thought, and its implications for brain- ... [https://www.paradromics.com/blog/the-speed-of-human-thought-and-its-implications-for-brain-computer-interfaces]
- 77. EMFF-2025: a general neural network potential for ... [https://www.nature.com/articles/s41524-025-01809-w]
- 78. Frontiers | Advanced Technologies in Wireless ... Neural Interfaces [https://www.frontiersin.org/research-topics/64295/advanced-technologies-in-wireless-neural-interfaces-from-animal-models-to-human-applications]
- 79. Japanese power breakthrough could be 'step toward a fully wireless society' | Live Science [https://www.livescience.com/technology/japanese-power-breakthrough-could-be-step-toward-a-fully-wireless-society]
- 80. Comparative accuracy of invasive versus non-invasive Brain-Computer Interfaces approaches [https://eureka.patsnap.com/report-comparative-accuracy-of-invasive-versus-non-invasive-brain-computer-interfaces-approaches]
- 81. Unlocking the Brain's Secrets [https://www.numberanalytics.com/blog/ultimate-guide-invasive-neural-interfaces-brain-computer-interfaces]
- 82. Signal acquisition of brain–computer interfaces: A medical-engineering crossover perspective review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11955058/]
- 83. Chinese Research Team Launches Clinical Trial for Invasive Brain-computer Interface----Chinese Academy of Sciences [https://english.cas.cn/newsroom/cas_media/202506/t20250616_1045625.shtml]
- 84. The state-of-the-art of invasive brain-computer interfaces in humans: a systematic review and individual patient meta-analysis - PubMed [https://pubmed.ncbi.nlm.nih.gov/39978072/]
- 85. Data Compression versus Signal in Wired-OR... Fidelity Tradeoff [https://dbi2.nl/publications/scientific-publications/publication-1]
- 86. Top 10 Brain-Computer Interface Companies in 2025 [https://www.sphericalinsights.com/blogs/top-10-companies-leading-the-brain-computer-interface-market-in-2025-key-players-statistics-future-trends-2024-2035]
- 87. Brain Computer Interfaces Market Size, Trends & Growth Graph by 2033 [https://straitsresearch.com/report/brain-computer-interfaces-market]
- 88. Wireless Neural Market Insights Interfaces to 2035 2025 [https://www.factmr.com/report/wireless-neural-interfaces-market]
- 89. A New Path to Noninvasive Brain-Computer Interface | Johns Hopkins University Applied Physics Laboratory [https://www.jhuapl.edu/news/news-releases/241114-noninvasive-brain-computer-interface]
- 90. Translational opportunities and challenges of invasive electrodes for neural interfaces - PubMed [https://pubmed.ncbi.nlm.nih.gov/37081142/]
- 91. Invasive vs. Non-Invasive Neuronal Signals for Brain-Machine Interfaces: Will One Prevail? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4921501/]
- 92. Drug discovery and mechanism prediction with explainable graph neural networks | Scientific Reports [https://www.nature.com/articles/s41598-024-83090-3]
- 93. Neuromorphic computing for modeling neurological and psychiatric disorders: implications for drug development | Artificial Intelligence Review [https://link.springer.com/article/10.1007/s10462-024-10948-3]