Improving fMRI Test-Retest Reliability: A Comprehensive Guide for Biomarker Development and Clinical Translation
This article provides a comprehensive examination of test-retest reliability in functional magnetic resonance imaging (fMRI) for researchers and drug development professionals. Converging evidence indicates poor to moderate reliability for common fMRI measures, with meta-analyses reporting mean intraclass correlation coefficients (ICCs) of 0.397 for task-based activation and 0.29 for edge-level functional connectivity. We explore foundational concepts of reliability measurement, methodological factors influencing consistency, optimization strategies for improving reliability, and validation approaches across different contexts. The content synthesizes recent evidence on how analytical decisions, acquisition parameters, and processing pipelines impact reliability, providing practical guidance for enhancing fMRI's utility in clinical trials and biomarker development.
Improving fMRI Test-Retest Reliability: A Comprehensive Guide for Biomarker Development and Clinical Translation
Abstract
This article provides a comprehensive examination of test-retest reliability in functional magnetic resonance imaging (fMRI) for researchers and drug development professionals. Converging evidence indicates poor to moderate reliability for common fMRI measures, with meta-analyses reporting mean intraclass correlation coefficients (ICCs) of 0.397 for task-based activation and 0.29 for edge-level functional connectivity. We explore foundational concepts of reliability measurement, methodological factors influencing consistency, optimization strategies for improving reliability, and validation approaches across different contexts. The content synthesizes recent evidence on how analytical decisions, acquisition parameters, and processing pipelines impact reliability, providing practical guidance for enhancing fMRI's utility in clinical trials and biomarker development.
Understanding fMRI Reliability: Why It Matters for Clinical and Research Applications
The Critical Importance of Reliability in fMRI Biomarker Development
FAQs: Understanding fMRI Reliability
What does "test-retest reliability" mean in the context of fMRI? Test-retest reliability refers to the consistency of fMRI measurements when the same individual is scanned under the same conditions at different time points. It is essential for ensuring that observed brain activity patterns are stable traits of the individual rather than random noise. High reliability is particularly crucial for studies investigating individual differences in brain function, as it directly impacts the ability to detect brain-behavior relationships [1].
Why is the reliability of fMRI biomarkers a major concern? Poor reliability drastically reduces effect sizes and statistical power for detecting associations with behavioral measures or clinical conditions. This reduction can lead to failures in replicating findings and undermines the utility of fMRI for predictive and individual-differences research. Essentially, even with large sample sizes, a biomarker with poor reliability will struggle to detect true effects [1].
Can fMRI measures be highly reliable? Yes, but it depends heavily on what is being measured. While the average activity in individual brain regions often shows poor reliability, multivariate measures—which combine patterns of activity across multiple brain areas using machine learning—can demonstrate good to excellent reliability. For example, some multivariate neuromarkers for conditions like cardiovascular risk or pain have shown same-day test-retest reliabilities above 0.70 [2].
Do all biomarkers need high long-term test-retest reliability? No. This is a common misconception. The U.S. Food and Drug Administration identifies several biomarker categories. Some, like prognostic biomarkers, require long-term stability. Others, such as diagnostic, monitoring, or pharmacodynamic biomarkers, are designed to detect dynamic states and therefore require low within-person measurement error but not necessarily high stability across weeks or months [2].
Troubleshooting Guides: Addressing Common Reliability Challenges
Problem: Poor reliability in individual brain regions
Symptoms
- Low intraclass correlation coefficients (ICCs) for task-related activation in regions of interest.
- Inconsistent brain-behavior correlations across studies.
- Inability to replicate findings in longitudinal studies.
Solutions
- Shift to Multivariate Measures: Instead of relying on single regions, use machine learning to create patterns distributed across multiple brain areas. These neuromarkers can show significantly higher reliability [2].
- Increase Data Per Participant: Collect more data per individual. Studies have shown that reliability increases with scan duration. For resting-state functional connectivity, longer scans (e.g., 20-30 minutes) substantially improve phenotypic prediction accuracy [3].
- Optimize Task Design: Simpler tasks and block designs (compared to event-related designs) may yield more reliable activation, especially in regions with stronger overall activation [1].
Problem: High within-subject variability across scanning runs
Symptoms
- Large differences in activation patterns for the same individual within a single scanning session.
- Low split-half reliability estimates.
Solutions
- Minimize Motion: Subject movement has a pronounced negative effect on reliability. Implement rigorous motion correction protocols during preprocessing. One study found that participants with the lowest motion had reliability estimates 2.5 times higher than those with the highest motion [1].
- Employ Advanced Denoising: Use techniques like multirun spatial ICA (e.g., FIX denoising) to ameliorate the impact of subject movement and other noise sources [1].
- Ensure Adequate Trial Count: For event-related designs, ensure a sufficient number of trials. For error-related brain activity, achieving stable estimates typically requires 6-8 error trials for fMRI measures and 4-6 trials for ERP measures [4].
Problem: Low reliability in multicenter studies
Symptoms
- Inconsistent results across different scanners and sites.
- Poor generalizability of biomarkers.
Solutions
- Account for Scanner and Protocol Effects: A 2025 multicenter study revealed hierarchical variations in functional connectivity, with significant contributions from scanner, protocol, and participant factors. Use statistical models that can account for these sources of variance [5].
- Utilize Ensemble Classifiers: Machine learning approaches like ensemble sparse classifiers can suppress site-related variances and prioritize disease-related signals, improving the reliability of diagnostic biomarkers in multicenter settings [5].
- Implement Harmonized Protocols: When possible, use standardized imaging protocols across sites to minimize protocol-related variability [5].
Quantitative Data on fMRI Reliability
Table 1: Summary of Reported fMRI Reliability Metrics
| Measure Type | Average Reliability (ICC) | Key Influencing Factors | Reference |
|---|---|---|---|
| Task-fMRI (Regional Activity) | 0.088 (short-term), 0.072 (long-term) | Motion, task design, developmental stage | [1] |
| Edge-Level Functional Connectivity | 0.29 (pooled mean) | Network type (within-network > between-network), scan length | [6] |
| Multivariate fMRI Biomarkers | 0.73 - 0.82 (examples) | Machine learning method, number of features | [2] |
| Error-Processing fMRI | Stable with 6-8 trials | Number of error trials, sample size (~40 participants) | [4] |
Table 2: Effect of Scan Duration on Phenotypic Prediction Accuracy
| Total Scan Duration (Sample Size × Scan Time) | Prediction Accuracy (Cognitive Factor Score) | Recommendation |
|---|---|---|
| Low (e.g., 200 pts × 14 min) | ~0.33 | Under-powered |
| Medium (e.g., 700 pts × 14 min) | ~0.45 | Improved, but not cost-optimal |
| High (e.g., 200 pts × 58 min) | ~0.40 | Improved, but less efficient than larger N |
| Optimal (Theoretical) | Highest | ~30 min scan time per participant is most cost-effective [3] |
Experimental Protocols for Reliability Optimization
Protocol: Assessing and Improving Task-fMRI Reliability
This protocol is based on methodologies used to evaluate the Adolescent Brain Cognitive Development (ABCD) Study data [1].
Data Acquisition:
- Tasks: Use well-established paradigms such as the Stop Signal Task (SST) for response inhibition, Monetary Incentive Delay (MID) for reward processing, and nBack for working memory.
- Design: Include two runs per task within the same session to assess within-session reliability.
- Duration: Each run should be approximately 5 minutes. However, for new studies, consider longer runs if focused on individual differences.
Reliability Analysis:
- Model: Use Linear Mixed-Effect models (LME) to estimate reliability, controlling for confounds like scanner site and family structure.
- Metric: Calculate the ratio of non-scanner related stable variance to all variances.
- Motion Quantification: Include rigorous motion quantification as a covariate, as it is a major source of unreliable variance.
Denoising Pipeline:
- Apply advanced denoising techniques, such as multirun spatial ICA followed by FIX cleaning, to reduce the impact of motion and other artifacts.
Protocol: Developing a Reliable Multivariate Biomarker
This protocol is derived from commentaries and studies on multivariate neuromarkers [2] [5].
Feature Extraction: Do not rely on average activity in pre-defined ROIs. Instead, extract activation estimates from a whole-brain map or a large set of brain regions.
Machine Learning Training:
- Algorithm: Use sparse machine learning algorithms (e.g., ensemble sparse classifiers) or kernel ridge regression.
- Validation: Employ nested cross-validation to avoid overfitting. The outer loop assesses generalizability, while the inner loop optimizes model hyperparameters.
- Feature Selection: The algorithm should weight and select features (connections or voxels) that are most stable and diagnostic, effectively suppressing unreliable variance [5].
Reliability Assessment:
- Calculate test-retest reliability (e.g., using intraclass correlation) of the resulting continuous biomarker score across separate sessions in a hold-out sample, not just its classification accuracy.
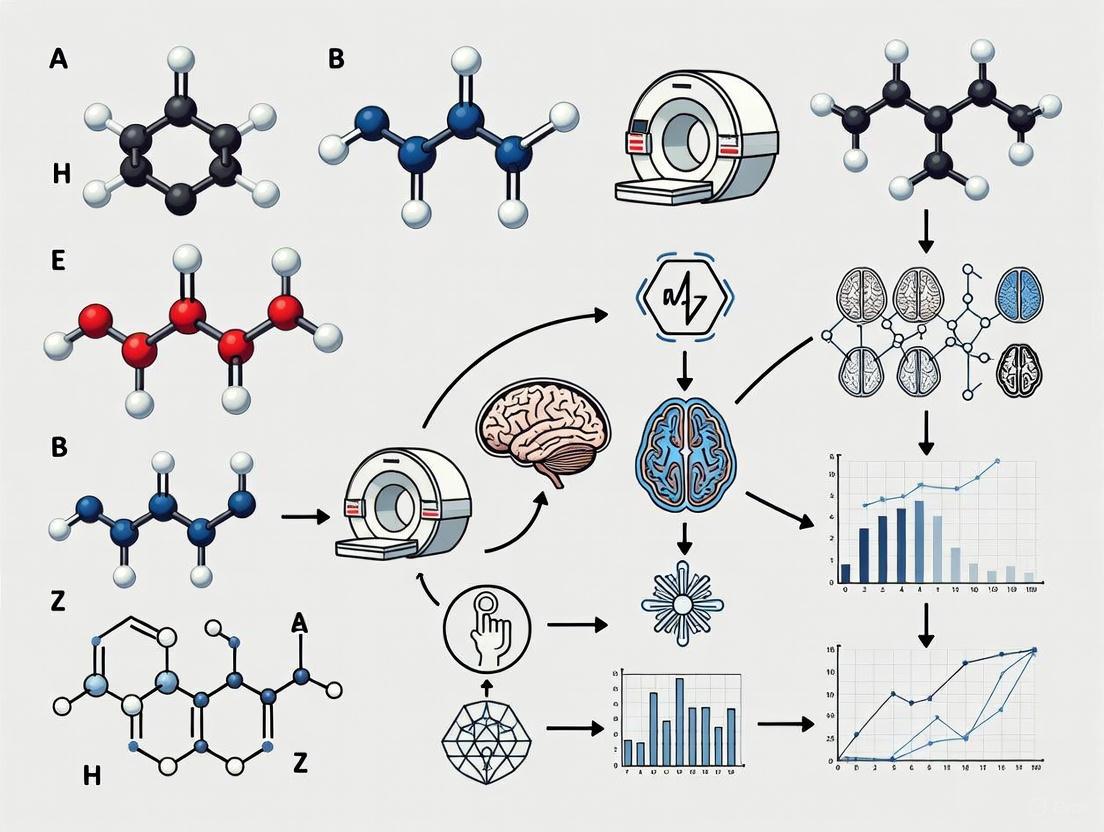
Workflow and Pathway Diagrams
The Scientist's Toolkit
Table 3: Essential Resources for fMRI Reliability Research
| Tool / Resource | Function | Example / Note |
|---|---|---|
| Linear Mixed-Effects (LME) Models | Statistical analysis that partitions variance and estimates reliability while controlling for confounds (site, family). | Preferred over simple ICC for complex, multi-site datasets like ABCD [1]. |
| Multivariate Machine Learning | Creates reliable biomarkers by integrating signals across many brain voxels or connections. | Kernel Ridge Regression, Ensemble Sparse Classifiers [2] [5]. |
| Advanced Denoising Pipelines | Removes non-neural noise from fMRI data to improve signal quality. | Multirun Spatial ICA combined with FIX [1]. |
| Traveling Subjects Dataset | A dataset where the same subjects are scanned across multiple sites and scanners. | Critical for quantifying and correcting for scanner-related variance in multicenter studies [5]. |
| Optimal Scan Time Calculator | A tool to help design cost-effective studies by balancing sample size and scan duration. | Available online based on findings from [3]. |
Troubleshooting Guide: Common fMRI Reliability Challenges
FAQ 1: How reliable are common task-fMRI and functional connectivity measures?
The Problem: Many researchers assume that widely used fMRI measures possess inherent reliability suitable for individual-differences research or clinical biomarker development. However, quantitative synthesis of the evidence reveals significant reliability challenges.
The Evidence: Meta-analytic evidence demonstrates that both task-fMRI and resting-state functional connectivity measures show concerningly low test-retest reliability in their current implementations:
Table: Meta-Analytic Evidence of fMRI Reliability
| fMRI Measure Type | Pooled Mean Reliability (ICC) | Quality of Reliability | Sample Size | Citation |
|---|---|---|---|---|
| Common Task-fMRI Measures | ICC = 0.397 | Poor | 90 experiments (N=1,008) | [7] |
| Resting-State Functional Connectivity (Edge-Level) | ICC = 0.29 | Poor | 25 studies | [8] |
| HCP Task-fMRI (11 common tasks) | ICC = 0.067 - 0.485 | Poor | N=45 | [7] |
ICC = Intraclass Correlation Coefficient. ICC quality thresholds: <0.4 = Poor; 0.4-0.59 = Fair; 0.6-0.74 = Good; ≥0.75 = Excellent.
The Solution: Recognize that standard fMRI measures were primarily designed to detect robust within-subject effects and group-level averages, not to precisely measure individual differences [9]. When planning studies focused on individual variability, explicitly select and optimize paradigms for reliability rather than simply adopting traditional cognitive neuroscience tasks.
FAQ 2: What factors most significantly impact fMRI reliability, and how can I control for them?
The Problem: Uncontrolled methodological and physiological variables introduce noise, reducing the signal-to-noise ratio of reliable individual differences in the BOLD signal.
The Evidence: Research has identified several key factors that systematically influence reliability estimates:
Table: Factors Influencing fMRI Reliability and Practical Recommendations
| Factor Category | Impact on Reliability | Evidence-Based Recommendation |
|---|---|---|
| Data Quantity | Reliability increases with more data per subject [9]. | Implement extended aggregation: acquire more trials, more scans, or longer resting-state scans per participant. |
| Functional Networks | Reliability varies across brain systems [8]. | Focus analyses on networks with higher inherent reliability (e.g., Frontoparietal, Default Mode) or account for network-specific reliability in models. |
| Subject State | Eyes-open, awake, active recordings show higher reliability than resting states [8]. | Standardize and monitor participant state (e.g., alertness) during scanning. |
| Test-Retest Interval | Shorter intervals generally yield higher reliability [8]. | Minimize time between repeated scans for reliability assessments. |
| Physiological Confounds | The BOLD signal is influenced by vascular physiology, not just neural activity [10]. | Measure and control for heart rate, blood pressure, respiration, and caffeine intake. Consider multi-echo fMRI to better isolate BOLD from noise. |
| Preprocessing & Analysis | Specific pipelines can introduce bias or spurious correlations [11]. | Use validated pipelines (e.g., with surrogate data methods). For connectivity, consider full correlation-based measures with shrinkage. |
The Solution: Adopt a "precision fMRI" (pfMRI) framework that prioritizes data quality and quantity per individual. Proactively control for known sources of physiological and methodological variance through experimental design and advanced processing techniques [9] [12].
Diagram: An Integrated Workflow for Improving fMRI Reliability. The red path highlights a sample protocol prioritizing reliability at each stage.
FAQ 3: Can I use fMRI for clinical trials or drug development given these reliability concerns?
The Problem: The pharmaceutical industry seeks objective biomarkers for CNS drug development, but the unreliable nature of many fMRI measures hinders their regulatory acceptance and clinical utility.
The Evidence:
- Regulatory agencies like the FDA and EMA require demonstrated precision, reproducibility, and a clear context of use for any biomarker in drug development [13].
- While fMRI has potential roles in demonstrating target engagement, dose-response relationships, and disease modification, no fMRI biomarker has yet been fully qualified for regulatory decision-making [13] [14].
- The fundamental limitation is that poor test-retest reliability establishes a low upper limit for a measure's predictive validity [8] [9].
The Solution:
- For trials using fMRI, invest in extensive site standardization and operator training to minimize technical variability.
- Focus on fMRI paradigms that show modifiable and reproducible readouts in the context of the specific drug's mechanism.
- Collect data supporting the biomarker's validity within a specific context of use (e.g., patient stratification, pharmacodynamic response) [13].
The Scientist's Toolkit: Essential Reagents & Materials
Table: Key Methodological Solutions for Reliable fMRI
| Tool Category | Specific Example | Primary Function | Key Benefit |
|---|---|---|---|
| Acquisition Hardware | Ultra-High Field Scanners (7T+) | Increases BOLD contrast-to-noise ratio and spatial resolution [12]. | Enables single-subject mapping of fine-scale functional architecture. |
| Pulse Sequences | Multi-Echo fMRI | Acquires data at multiple echo times, allowing for better separation of BOLD signal from noise [9]. | Improves sensitivity and specificity through advanced denoising. |
| Processing Algorithms | Multi-Echo Independent Component Analysis (ME-ICA) | Identifies and removes non-BOLD noise components from fMRI data [9]. | Significantly enhances functional connectivity reliability. |
| Analysis Framework | Reliability Modeling | Statistically models known sources of measurement error to derive more reliable latent variables [9]. | Increases validity of individual differences measurements. |
| Experimental Design | Naturalistic Paradigms (e.g., movie-watching) | Presents dynamic, engaging stimuli that modulate brain states more consistently than rest [15]. | Can yield more robust and reliable individual difference measures. |
| Data Aggregation | Precision fMRI (pfMRI) Protocols | Involves collecting large amounts of data per individual (e.g., >100 mins) [9] [12]. | Allows random noise to average out, revealing stable individual patterns. |
Interpreting Intraclass Correlation Coefficients (ICCs) in Neuroimaging Contexts
Frequently Asked Questions
What does the ICC quantify in fMRI research? The Intraclass Correlation Coefficient (ICC) quantifies test-retest reliability by measuring the proportion of total variance in fMRI data that can be attributed to stable differences between individuals [16]. It is a dimensionless statistic bracketed between 0 and 1 [17].
Why is my voxel-wise or edge-level ICC considered 'poor'? Meta-analyses have demonstrated that univariate fMRI measures inherently exhibit low test-retest reliability at the voxel or individual edge level. The pooled mean ICC for functional connectivity edges is 0.29, classified as 'poor' [6]. Similarly, task-based activation often shows poor reliability [16].
My data shows a strong group-level effect, but poor ICC. Is this possible? Yes. A strong group-level effect (high mean activation) indicates a consistent response across participants but does not guarantee that the measure can reliably differentiate between individuals, which is what ICC assesses [17].
How can I improve the ICC reliability of my fMRI measure? You can improve reliability by using shorter test-retest intervals, acquiring more data per subject, analyzing stronger and more robust BOLD signals (e.g., within-network cortical edges), and choosing appropriate analytical approaches such as using beta coefficients instead of contrast scores [16] [18] [6].
Should I use a 'consistency' or 'agreement' ICC model? This choice depends on your research question [19]. Use an agreement ICC (e.g., ICC(2,1)) when the absolute values and measurement scales are consistent across sessions and you care about absolute agreement. Use a consistency ICC (e.g., ICC(3,1)) when you are only interested in whether the relative ranking of subjects is preserved across sessions, even if the mean of the measurements shifts [16] [19].
Is reliability (ICC) the same as validity? No. Reliability provides an upper bound for validity, but they are distinct concepts [16]. A measure can be reliable but not valid (e.g., a thermometer that consistently reads 0°C is reliable but not valid). The ultimate goal is a measure that is both reliable and valid [16] [17].
Troubleshooting Low ICC Values
This guide helps you diagnose and address common causes of low reliability in fMRI studies.
| Troubleshooting Step | Description | Key References |
|---|---|---|
| 1. Inspect Your Measure | For task-based fMRI, calculate ICC using beta coefficients from your GLM, not difference scores (contrasts). Contrasts have low between-subject variance, which artificially deflates ICC [18]. | [18] |
| 2. Optimize Study Design | Use shorter test-retest intervals (e.g., days or weeks instead of months). Ensure participants are in similar states (e.g., both eyes-open awake). Collect more data per subject (longer scans/more runs) [16] [6]. | [16] [6] |
| 3. Enhance Signal Quality | Focus analyses on brain regions with stronger, more reliable signals (e.g., cortical regions vs. subcortical). Prioritize within-network connections over between-network connections for connectivity studies [18] [6]. | [18] [6] |
| 4. Check ICC Model Selection | Ensure you are using an ICC model that correctly accounts for the facets (sources of error) in your design. For most test-retest studies with sessions considered a random sample, ICC(2,1) is a robust starting point [16] [19]. | [16] [19] |
| 5. Consider Multivariate Methods | Univariate measures (single voxels/edges) are often unreliable. Explore multivariate approaches like brain-based predictive models or network-level analyses (e.g., ICA), which can aggregate signal and improve both reliability and validity [16]. | [16] |
Quantitative Data and Methodologies
| fMRI Measure | Pooled Mean ICC | Reliability Classification | Key Context |
|---|---|---|---|
| Functional Connectivity (Edge-Level) | 0.29 (95% CI: 0.23 - 0.36) | Poor | Based on a meta-analysis of 25 studies [6]. |
| Task-Based Activation | Low (varies) | Poor | Multiple converging reports and a meta-analysis confirm generally poor reliability for univariate measures [16]. |
| Structural MRI | Relatively High | Fair/Good | Structural measures are generally more reliable than functional measures [16]. |
ICC Interpretation Guidelines
| ICC Range | Conventional Interpretation | Implication for fMRI |
|---|---|---|
| < 0.40 | Poor | Limited utility for discriminating between individuals at a single measurement level [16] [18]. |
| 0.40 - 0.59 | Fair | May be acceptable for group-level inferences, but caution is advised for individual-level applications [18]. |
| 0.60 - 0.74 | Good | Suitable for many research contexts, including some individual differences studies [16]. |
| ≥ 0.75 | Excellent | Indicates a measure stable enough for clinical applications or tracking individual changes over time [16]. |
Experimental Factors Influencing ICC
The following table summarizes factors that have been empirically shown to influence the test-retest reliability of fMRI measures [16] [6].
| Factor | Effect on Reliability | Practical Recommendation |
|---|---|---|
| Test-Retest Interval | Shorter intervals generally yield higher ICC. | Minimize the time between scanning sessions where possible [16] [6]. |
| Paradigm/State | Active tasks often show higher reliability than resting state. "Eyes open" rest is more reliable than "eyes closed" [6]. | Prefer active tasks for individual differences research. Standardize the awake state during rest [16] [6]. |
| Data Quantity | More within-subject data (longer scan times, more runs) improves reliability. | Acquire as much data as feasibly possible per subject [6]. |
| Signal Strength | Stronger BOLD responses and higher magnitude functional connections are more reliable. | Focus on robust, well-characterized signals and networks [18] [6]. |
| Analytical Choice | Using beta coefficients is more reliable than using contrast scores. Multivariate patterns can be more reliable than univariate ones [18]. | Use beta coefficients for task reliability; explore multivariate methods [16] [18]. |
| Brain Region | Cortical regions and within-network connections are typically more reliable than subcortical regions and between-network connections [18] [6]. | Be aware of regional limitations; cortical signals are generally more reliable [18]. |
The Scientist's Toolkit
Key Research Reagents and Computational Solutions
| Item Name | Function/Brief Explanation |
|---|---|
| ICC Analysis Toolbox | A MATLAB toolbox for calculating various reliability metrics, including different ICC models, Kendall's W, RMSD, and Dice coefficients [20]. |
| ISC Toolbox | A toolbox for performing Inter-Subject Correlation analysis, which can be used to assess reliability in naturalistic fMRI paradigms [21]. |
| Beta Coefficients (β) | The raw parameter estimates from a first-level GLM, representing the strength of task-related activation. Preferred over contrast scores for reliability analysis [18]. |
| Intra-Class Effect Decomposition (ICED) | A structural equation modeling framework that decomposes reliability into multiple orthogonal error sources (e.g., session, day, site), providing a nuanced view of measurement error [17]. |
| Independent Component Analysis (ICA) | A data-driven multivariate method to identify coherent functional networks. Network-level measures derived from ICA can show higher reliability than voxel-wise analyses [18]. |
Workflow for a Reliability-Focused fMRI Analysis
The following diagram outlines a recommended workflow for designing and analyzing a test-retest fMRI study with reliability in mind.
Logical Relationship Between Variance, Reliability, and Validity
This diagram illustrates the core statistical concepts behind the ICC and its relationship to validity, helping to clarify common points of confusion.
FAQs: Core Concepts and Definitions
Q1: What is the practical difference between test-retest and between-site reliability?
- Test-Retest Reliability assesses the consistency of measurements when the same individual is scanned repeatedly on the same scanner under similar conditions. It confirms that a protocol can produce stable results for an individual over time [22] [23].
- Between-Site Reliability assesses the consistency of measurements across different scanners and locations. It is essential for determining if data from multiple sites in a multicenter study can be meaningfully merged [22] [24]. High between-site reliability is often harder to achieve than test-retest reliability due to additional variance introduced by different hardware and software [22].
Q2: Why is multisession data acquisition often recommended?
Employing multiple scanning sessions or runs significantly improves reliability. This is analogous to the Spearman-Brown prediction formula in classical test theory, where increasing the number of measurements enhances reliability [22]. Averaging across multiple runs helps to average out random noise, leading to more stable and reproducible estimates of the brain's signal [22] [25].
Q3: How does the choice of fMRI metric influence reliability?
The type of measure extracted from the fMRI data is a critical factor. Studies have found that:
- Percent Signal Change (PSC) often shows higher reliability than measures like contrast-to-noise ratio (CNR), which have an estimate of noise in the denominator [22].
- Multivariate patterns derived from machine learning can exhibit good-to-excellent reliability, whereas the average activation in a single brain region is often much less reliable [2].
- Median values from a Region of Interest (ROI) are typically more reliable than maximum values, as the latter can be unduly influenced by outliers [22].
Troubleshooting Guides
Guide 1: Addressing Poor Between-Site Reliability
Problem: Data collected from different MRI scanners are inconsistent, preventing effective data pooling in a multicenter study.
Solutions:
- Increase ROI Size: Using larger, functionally-derived Regions of Interest (ROIs) can help compensate for anatomical and functional misalignment across sites, markedly improving between-site reliability [22].
- Adjust for Smoothness Differences: Differences in image reconstruction filters can lead to varying image smoothness between scanners. Statistically adjusting for these smoothness differences has been shown to increase reliability for certain metrics [22].
- Harmonize Acquisition Protocols: Use standardized sequences and parameters across all sites. Ensure all sites undergo rigorous quality assurance testing. A study using Siemens scanners across sites demonstrated that a harmonized protocol could yield excellent reliability for quantitative metrics like R1 and MTR [26].
Guide 2: Improving Test-Retest Reliability of Functional Connectivity
Problem: Resting-state functional connectivity (RSFC) measures show poor consistency across scanning sessions.
Solutions:
- Increase Scan Duration: Reliability asymptotically increases with more data. Aim for longer scan durations (e.g., 10-15 minutes or more) per session to substantially improve reliability [23] [27] [25].
- Focus on Stronger Connections and Specific Networks: Reliability is positively associated with connection strength. Analyses focused on established, stronger connections within known brain subnetworks (e.g., the default-mode network) are generally more reliable than analyses of the whole brain or weak connections [28] [23].
- Control for Head Motion: Head motion is a major source of artefactual variance. Implement strict motion control and correction protocols during both data acquisition and preprocessing [29] [25].
- Consider Task-Based Paradigms: For brain networks engaged by a specific task, using that task during the fMRI scan (instead of rest) can enhance FC reliability within those specific networks by increasing the signal variability related to the function of interest [25].
Guide 3: Optimizing Acquisition Sequences for Reliability
Problem: An advanced, high-resolution multiband fMRI sequence is yielding low signal-to-noise ratio (SNR) and unreliable results.
Solutions:
- Prioritize SNR over Extreme Resolution: Small voxel sizes (e.g., 2 mm isotropic) drastically reduce SNR. For standard volumetric analyses that include spatial smoothing, a slightly larger voxel size (e.g., 2.5-3 mm) can provide a better SNR/reliability balance, especially if total scan time per subject is limited [30].
- Optimize Repetition Time (TR): Very short TRs (e.g., < 1 second) reduce T1-weighting and can lower SNR. A TR in the range of 1-1.5 seconds is often a good compromise for conventional BOLD fMRI studies [30].
- Use Multiband Acceleration Judiciously: High multiband acceleration factors can introduce artefacts and signal dropout in medial temporal and subcortical regions. Use the minimum acceleration factor necessary to achieve your target TR and coverage to mitigate these issues [30].
The following table summarizes reliability findings for various fMRI metrics and conditions from the cited literature.
Table 1: Reliability Benchmarks for Different fMRI Metrics
| Modality / Metric | Reliability Type | ICC / Correlation Value | Interpretation & Context |
|---|---|---|---|
| Task-fMRI (Sensorimotor) | Between-Site (Initial) | Low ICC | Strong site and site-by-subject variance [22] |
| Task-fMRI (Sensorimotor) | Between-Site (Optimized) | Increased by 123% | After ROI size increase, smoothness adjustment, and more runs [22] |
| Quantitative R1, MTR, DWI | Between-Site | ICC > 0.9 | Excellent reliability with a harmonized multisite protocol [26] |
| Resting-State FC | Between-Site | ICC ~ 0.4 | Moderate reliability [26] |
| Structural Connectivity (SC) | Test-Retest | CoV: 2.7% | Highest reproducibility among connectivity estimates [28] |
| Functional Connectivity (FC) | Test-Retest | CoV: 5.1% | Lower reproducibility than structural connectivity [28] |
| Edge-Level RSFC (Aphasia) | Test-Retest | Fair Median ICC | With 10-12 min scans; better in subnetworks than whole brain [23] |
| ABCD Task-fMRI | Test-Retest | Avg: 0.088 | Poor reliability in children; motion had a pronounced negative effect [29] |
| Multivariate fMRI Biomarkers | Test-Retest | r = 0.73 - 0.82 | Good-to-excellent same-day reliability [2] |
| Brain-Network Temporal Variability | Test-Retest | ICC > 0.4 | At least moderate reliability with optimized window parameters [27] |
Abbreviations: ICC (Intraclass Correlation Coefficient); CoV (Coefficient of Variation); R1 (Longitudinal Relaxation Rate); MTR (Magnetization Transfer Ratio); DWI (Diffusion Weighted Imaging); FC (Functional Connectivity); RSFC (Resting-State Functional Connectivity.
Multicenter Reliability Study (fBIRN Phase 1) [22] [24]
- Objective: To estimate test-retest and between-site reliability of fMRI assessments.
- Subjects: Five healthy males scanned at 10 different MRI scanners on two separate occasions.
- Task: A simple block-design sensorimotor task.
- Analysis: FIR deconvolution with FMRISTAT to derive impulse response functions. Six functionally-derived ROIs covering visual, auditory, and motor cortices were used.
- Key Dependent Variables: Percent signal change (PSC) and contrast-to-noise ratio (CNR).
- Reliability Assessment: Intraclass correlation coefficients (ICCs) derived from a variance components analysis.
Visual Workflow: Pathway to Reliable fMRI
Diagram Title: Pathway to Reliable fMRI
The Scientist's Toolkit
Table 2: Essential Reagents and Solutions for fMRI Reliability Research
| Tool / Solution | Primary Function | Application Note |
|---|---|---|
| Intraclass Correlation Coefficient (ICC) | Quantifies measurement agreement and consistency [22]. | Use ICC(2,1) for absolute agreement between sites/scanners when merging data is the goal [22] [26]. |
| Functionally-Defined ROIs | Spatially constrained regions for signal extraction. | Larger ROIs improve between-site reliability by mitigating misalignment [22]. |
| Multiband fMRI Sequences | Accelerates data acquisition [26] [30]. | Use judiciously; high acceleration factors can reduce SNR and cause signal dropout [30]. |
| Variance Components Analysis | Decomposes sources of variability in data [22]. | Critical for identifying whether variance stems from subject, site, session, or their interactions. |
| Temporal Signal-to-Noise Ratio (tSNR) | Measures quality of BOLD time series [25]. | A key factor influencing functional connectivity reliability; varies across the brain and with tasks [25]. |
| Harmonized Acquisition Protocol | Standardizes scanning parameters across sites [26]. | Foundation for any successful multicenter study to ensure data comparability [26]. |
FAQs: Addressing Researcher Questions on fMRI Reliability
What does "test-retest reliability" mean in the context of fMRI? Test-retest reliability refers to the extent to which an fMRI measurement produces a similar value when repeated under similar conditions. It is a numerical representation of the consistency of your measurement tool. High reliability is crucial for drawing meaningful conclusions about individual differences and for the development of clinical biomarkers [25] [18].
My task-based fMRI results have poor reliability at the individual level. Is this normal? This is a common challenge, but it is not an insurmountable flaw of fMRI as a whole. Reports of poor individual-level reliability are often tied to specific analytical choices, such as using contrast scores (difference between two task conditions) instead of beta coefficients (a direct measure of functional activation from a single condition). Contrasts can have low between-subject variance and introduce error, leading to suppressed reliability estimates. Switching to beta coefficients has been shown to yield higher Intraclass Correlation Coefficient (ICC) values [18].
I use resting-state fMRI. Is it immune to reliability issues? No. While resting-state fMRI (rsfMRI) is a powerful tool, its reliability can be compromised by statistical artifacts. Standard preprocessing steps, particularly band-pass filtering (e.g., 0.009–0.08 Hz), can introduce biases that inflate correlation estimates and increase false positives. The reliability of functional connectivity measurements is also fundamentally constrained by factors like scan length and head motion [25] [11].
Can I improve the reliability of my existing dataset? Yes, a primary method is through extended data aggregation. The reliability of fMRI measures asymptotically increases with a greater number of timepoints acquired. If your dataset includes multiple task or rest runs, concatenating them can boost your reliability estimates [25] [15].
Is fMRI reliable enough for use in drug development? It has significant potential but meets challenges. For fMRI to be widely adopted in clinical trials, its readouts must be both reproducible and modifiable by pharmacological agents. While no fMRI biomarker has yet been fully qualified by regulatory agencies like the FDA or EMA, consortia are actively working toward this goal. Its value is highest for providing objective data on central nervous system (CNS) penetration, target engagement, and pharmacodynamic effects in early-phase trials [13] [31].
Troubleshooting Guides: Diagnosing and Solving Reliability Problems
Problem: Low ICC in Task-Based fMRI Analysis
Symptoms: Low Intraclass Correlation Coefficient (ICC) values (e.g., below 0.4, which is considered "poor") when assessing test-retest reliability for individual brain regions [18].
Diagnosis Checklist:
- Are you using contrast scores? Check your first-level model. Using a contrast of Condition A vs. Condition B is common but problematic for reliability.
- Is your scan length too short? Reliability increases with more data. A typical 10-minute scan is often insufficient for robust individual differences research [25] [15].
- Is the task engaging the regions you are analyzing? Reliability is not uniform across the brain; it is highest in regions strongly activated by the task [25] [18].
Solutions:
- Use Beta Coefficients: For reliability analysis, extract β coefficients from your first-level General Linear Model (GLM) for a single condition of interest, rather than a contrast. One study found this simple switch significantly increased ICC values [18].
- Adopt Multivariate Measures: Instead of relying on the average signal from a single region of interest (ROI), use multivariate pattern analysis or brain-state classifiers. These measures, optimized with machine learning, can show good-to-excellent reliability, even when single-region measures fail [2].
- Aggregate More Data: Collect more data per participant. If possible, design studies with longer scan times or multiple sessions. "Precision fMRI" studies may use 5+ hours of data per person to achieve high-fidelity individual brain maps [15].
Problem: Inconsistent Resting-State Functional Connectivity Results
Symptoms: High variation in functional connectivity matrices between sessions for the same participant; connectivity strengths that are not reproducible.
Diagnosis Checklist:
- Check your band-pass filter settings. The standard frequency filters (e.g., 0.009–0.08 Hz) can artificially inflate correlation estimates and lead to false positives [11].
- Review data quality. High head motion is a primary confound that systematically alters the functional connectome and reduces measurement validity [25].
- Consider the signal-to-noise ratio. Regions with low temporal signal-to-noise ratio (tSNR), such as the orbitofrontal cortex, have inherently lower reliability [25].
Solutions:
- Statistical Correction: Adjust your preprocessing pipeline. Align your sampling rate with the analyzed frequency band and consider using surrogate data methods to account for autocorrelation, which helps control for false positives [11].
- Robust Denoising: Implement advanced denoising techniques, such as multi-echo ICA, which can help separate BOLD signal from non-BOLD noise more effectively [15].
- Increase Scan Duration: Just as with task-based fMRI, the reliability of functional connectivity measures improves with longer scan times. Aim for acquisitions longer than 10 minutes [25].
Quantitative Data on fMRI Reliability
Table 1: Reliability Coefficients of Different fMRI Measures
This table summarizes the range of test-retest reliability (often measured by ICC) for common fMRI measures, highlighting how the choice of measure impacts reliability.
| fMRI Measure | Typical Reliability (ICC Range) | Key Influencing Factors |
|---|---|---|
| Univariate Task Activation (single ROI) | Poor to Fair (0.1 - 0.5) [2] [18] | Scan length, task design, head motion, analytical approach (contrasts vs. betas) |
| Multivariate Pattern Analysis | Good to Excellent (0.7 - 0.9+) [2] | Pattern stability, machine learning model, amount of training data |
| Resting-State Functional Connectivity | Variable (Poor to Good) [25] | Scan length, network location, head motion, preprocessing pipeline |
| Network-Level Analysis (ICA) | Generally higher than voxel-wise [18] | Data-driven approach, stability of large-scale networks |
Table 2: Impact of Experimental Factors on Reliability
This table outlines how specific design and methodological choices can either degrade or enhance the reliability of your fMRI data.
| Factor | Impact on Reliability | Evidence-Based Recommendation |
|---|---|---|
| Scan Length | Positive asymptotic relationship [25] [15] | Aggregate data across longer scans or multiple sessions (e.g., >30 mins total). |
| Task vs. Rest | Region-specific effect [25] | Use tasks that strongly engage your network of interest; reliability there will be higher than at rest. |
| Analytical Variable (Beta vs. Contrast) | Beta coefficients > Contrasts [18] | Use β coefficients from first-level GLM for reliability calculations on single conditions. |
| Signal Variability (tSD) | Strong positive driver [25] | Temporal standard deviation (tSD) of the BOLD signal is a key marker; higher tSD often associates with higher reliability. |
Experimental Protocols for Reliability
Protocol: Assessing Test-Retest Reliability with ICC
Purpose: To quantitatively evaluate the consistency of an fMRI measure within the same individuals across multiple sessions.
Materials: fMRI dataset with at least two scanning sessions per participant, acquired under identical or very similar conditions (e.g., same scanner, sequence, and task).
Methodology:
- Data Acquisition: Acquire your fMRI data (task or rest) across two or more sessions. The time between sessions (e.g., same day, weeks apart) should be chosen based on the stability you wish to measure.
- Preprocessing: Process all data through a standardized, robust pipeline (e.g., including motion correction, normalization, and for rsfMRI, careful filtering).
- Feature Extraction: For the measure of interest (e.g., amygdala activation during an emotion task), extract the values for each participant at each session.
- Critical Step: Extract β coefficients for a specific condition, not contrast scores, to maximize between-subject variance [18].
- Statistical Analysis: Calculate the Intraclass Correlation Coefficient (ICC). The ICC(2,1) form is commonly used, which partitions variance into between-subject and within-subject components. Values are interpreted as:
- Poor: < 0.4
- Fair: 0.4 - 0.59
- Good: 0.6 - 0.74
- Excellent: > 0.75 [18]
Protocol: Precision fMRI for Individual Brain Mapping
Purpose: To create highly reliable functional brain maps for individual participants, suitable for clinical biomarker discovery or brain-behavior mapping.
Materials: Access to an MRI scanner; participants willing to undergo extended scanning.
Methodology:
- Study Design: Plan for densely sampled data. This involves collecting many hours of fMRI data per participant, spread across multiple sessions (e.g., 10 sessions of 1+ hour each) [15].
- Data Collection: Acquire a mixture of data types, including multiple task states (engaging different systems) and resting-state data. This allows for comprehensive mapping.
- Data Processing: Process data at the individual level, avoiding group-level averaging that obscures individual differences. Use surface-based analysis and custom registration for optimal alignment [15].
- Data Aggregation: Concatenate all fMRI time series (from both task and rest) for each participant. This massive aggregation drives reliability into the high asymptotic range.
- Validation: Use split-half reliability (e.g., correlating connectomes from sessions 1-5 with sessions 6-10) to confirm the high fidelity of the individual maps [25].
Visualizing the Pathways to Reliability
Diagram: Factors Determining fMRI Reliability
The Scientist's Toolkit: Essential Reagents & Materials
Table 3: Key Research Reagent Solutions for Reliability
| Tool / Material | Function | Role in Enhancing Reliability |
|---|---|---|
| Densely-Sampled Datasets (e.g., Midnight Scan Club) | Provides a benchmark and testbed for reliability methods. | Enables the study of reliability asymptotic limits and region-specific task effects [25]. |
| Multivariate Pattern Analysis | A class of machine learning algorithms applied to brain activity patterns. | Extracts more reliable, distributed brain signatures than univariate methods, improving biomarker potential [2]. |
| Multi-echo fMRI Sequence | An acquisition sequence that collects data at multiple echo times. | Allows for superior denoising (e.g., via multi-echo ICA), isolating BOLD signal from non-BOLD noise [15]. |
| Intraclass Correlation (ICC) | A statistical model quantifying test-retest reliability. | The standard metric for assessing measurement consistency; crucial for evaluating new methods [18]. |
| Independent Component Analysis (ICA) | A data-driven method to separate neural networks from noise. | Improves reliability by identifying coherent, large-scale networks that are stable across sessions [18]. |
Methodological Strategies for Enhancing fMRI Reliability in Experimental Designs
A guide to enhancing the reliability and power of your fMRI research
This resource addresses frequently asked questions on optimizing key fMRI acquisition parameters, framed within the broader goal of improving test-retest reliability in neuroimaging research. The guidance synthesizes recent empirical findings to help researchers, scientists, and drug development professionals design more powerful, reproducible, and cost-effective studies.
Frequently Asked Questions
Q1: How does scan duration impact prediction accuracy and reliability in brain-wide association studies (BWAS)?
Longer scan durations significantly improve phenotypic prediction accuracy and data reliability. A 2025 large-scale study in Nature demonstrated that prediction accuracy increases with the total scan duration (calculated as sample size × scan time per participant) [3].
The study, analyzing 76 phenotypes across nine datasets, found that for scans up to 20 minutes, accuracy increases linearly with the logarithm of the total scan duration [3].
- Cost-Benefit Analysis: When accounting for overhead costs per participant (e.g., recruitment), longer scans can be more economical than larger sample sizes for improving prediction performance. The research indicates that 10-minute scans are cost-inefficient, and 30-minute scans are, on average, the most cost-effective, yielding 22% savings over 10-minute scans [3].
- Practical Recommendation: The study recommends a scan time of at least 30 minutes for resting-state whole-brain BWAS. For task-fMRI, the most cost-effective scan time may be shorter, while for subcortical-to-whole-brain BWAS, it may be longer [3].
Q2: What are the key temporal factors in session planning that can influence fMRI reliability?
The timing of your scan session is not arbitrary; several temporal factors can modulate resting-state brain connectivity and topology, potentially confounding results.
A study of over 4,100 adolescents found that the time of day, week, and year of scanning were correlated with topological properties of resting-state connectomes [32].
- Time of Day: Scanning later in the day was negatively correlated with multiple whole-brain and network-specific topological properties (with the exception of a positive correlation with modularity). These effects, while spatially extensive, were generally small [32].
- Time of Week and Year: Being scanned on a weekend (vs. a school day) or during summer vacation (vs. the school year) was associated with topological differences, particularly in visual, somatomotor, and temporoparietal networks. The effect sizes varied from small to large [32].
- Impact on Cognition: Including these scan time parameters in models eliminated some associations between connectome properties and performance on cognitive tasks, suggesting they should be treated as confounders in analyses relating brain function to behavior [32].
Q3: Which analytical measures provide better test-retest reliability for task-based fMRI?
The choice of which neural activation measure to use in reliability calculations has a substantial impact on the resulting Intraclass Correlation Coefficient (ICC).
Research indicates that using β coefficients from a first-level General Linear Model (GLM) provides higher test-retest reliability than using contrasts (difference scores between conditions) [18].
- Rationale: Contrasts often have low between-subject variance and the two measures being subtracted are highly correlated, introducing error and resulting in lower reliability estimates [18].
- Empirical Support: A 2022 study found that ICC values were higher when calculated using β coefficients for both voxel-wise and network-level (ICA) analyses. Using contrasts may underlie the low reliability estimates frequently reported in the literature [18].
Q4: How should I approach the trade-off between sample size and scan duration per participant?
Sample size and scan time are initially interchangeable but with diminishing returns. Investigators must often choose between scanning more participants for a shorter time or fewer participants for a longer time [3].
The following workflow outlines a data-driven approach to planning your study parameters, based on empirical models:
A theoretical model shows that prediction accuracy increases with both sample size (N) and total scan duration. For a fixed total scanning time (e.g., 6,000 minutes), prediction accuracy decreases as scan time per participant increases, but the reduction is modest for shorter scan times [3].
- Key Insight: While longer scans can compensate for smaller sample sizes (and vice versa), the required increase in scan time becomes progressively larger as the duration extends. Sample size is ultimately more important for generalizability, but longer scans can be a cost-effective way to boost prediction power [3].
- Resource for Planning: An online reference is available for future study design based on this model: Optimal Scan Time Calculator [3].
The table below summarizes key quantitative relationships derived from empirical studies to aid in experimental design and parameter selection.
| Relationship | Empirical Finding | Practical Implication | Source |
|---|---|---|---|
| Scan Duration vs. Prediction Accuracy | Accuracy increases with the logarithm of total scan duration (Sample Size × Scan Time). Diminishing returns observed, especially beyond 20-30 min. | For a fixed budget, longer scans (≥20 min) are initially interchangeable with a larger sample size for boosting accuracy. | [3] |
| Optimal Cost-Effective Scan Time | On average, 30-minute scans are the most cost-effective, yielding 22% cost savings over 10-minute scans. | 10-minute scans are cost-inefficient. Overshooting the optimal scan time is cheaper than undershooting it. | [3] |
| Sample Size vs. Scan Time Trade-off | For a fixed 6,000 min of total scan time, prediction accuracy decreases as scan time per participant increases. | When total resource is fixed, a larger sample size with shorter scans generally yields higher accuracy than a small sample with very long scans. | [3] |
The Scientist's Toolkit: Essential Reagents & Materials
The following table details key methodological "reagents" and considerations for designing an fMRI study with high test-retest reliability.
| Item / Solution | Function / Role in Experiment | Technical Notes |
|---|---|---|
| Optimal Scan Time Calculator | An online tool to model the trade-off between sample size and scan duration for maximizing prediction power. | Based on empirical models from large datasets (ABCD, HCP). Use for study planning and power analysis [3]. |
| β Coefficients (GLM) | A direct measure of functional activation for a single task condition; used as a superior input for test-retest reliability (ICC) calculations. | Provides higher ICC values than contrast scores due to greater between-subject variance [18]. |
| ICC(2,1) | A specific intraclass correlation coefficient model used to assess test-retest reliability, reflecting absolute agreement with a random facet for raters (sessions). | A recommended starting point for estimating the reliability of single measurements in fMRI [16]. |
| Scan Time Covariates | Variables related to the timing of the scan session that should be included in statistical models to control for confounding variance. | Includes time of day, day of week (school vs. weekend), and time of year (school vs. vacation) [32]. |
| Phantom Scans | Regular quality assurance (QA) scans on a standardized object to monitor scanner stability and identify hardware-related artefacts over time. | Critical for longitudinal and multi-site studies to ensure measurement consistency [33]. |
Detailed Experimental Protocols
Protocol 1: Designing a BWAS with Optimal Scan Duration
This protocol is adapted from the large-scale analysis published in Nature (2025) [3].
- Define Phenotype and Dataset: Select the phenotypic trait for prediction and choose an appropriate dataset (e.g., resting-state or task-fMRI from HCP, ABCD, etc.).
- Calculate Functional Connectivity: For each participant, calculate a whole-brain functional connectivity matrix (e.g., 419x419) using the first T minutes of fMRI data. Vary T from short (e.g., 2 min) to the maximum available in intervals (e.g., 2 min).
- Predict Phenotype: Use a machine learning model (e.g., Kernel Ridge Regression) with the connectivity matrices as features to predict the phenotype. Employ a nested cross-validation procedure.
- Systematically Vary Parameters: Repeat the prediction across different training sample sizes (N) and scan durations (T).
- Model the Relationship: Fit a logarithmic or theoretical model to the resulting prediction accuracies to characterize the relationship between N, T, and accuracy. Use this model or the provided online calculator to determine the optimal scan time and sample size for a new study.
Protocol 2: Assessing Test-Retest Reliability with ICC
This protocol guides the measurement of fMRI reliability, drawing from best practices in the field [16] [18].
- Data Acquisition: Collect fMRI data from participants at two separate time points (test and retest). The interval should be chosen based on the research question (e.g., short-term for scanner stability, long-term for developmental traits).
- Image Processing & First-Level Analysis: Preprocess the data (motion correction, normalization, etc.). For task-based data, run a first-level GLM for each participant and session to obtain β coefficient maps for conditions of interest.
- Define the Measure of Interest: Extract the neural measure for reliability assessment. For univariate analysis, this could be the mean β value from an ROI. For functional connectivity, it could be the correlation strength of a specific edge or network.
- Choose an ICC Model: Select an appropriate ICC model. ICC(2,1) is often a robust choice for assessing absolute agreement between sessions, modeling the session facet as random [16].
- Calculate and Interpret ICC: Compute the ICC for the measure across participants. Interpret values using established benchmarks: poor (<0.4), fair (0.4-0.59), good (0.6-0.74), excellent (≥0.75) [16].
Troubleshooting Guide: Frequently Asked Questions
Smoothing Kernel Selection
1. How does the size of the smoothing kernel affect my functional connectivity results?
Smoothing kernel size directly modifies functional connectivity networks and network parameters by altering node connections. Studies show different kernel sizes (0-10mm FWHM) produce varying effects on resting-state versus task-based fMRI analyses [34].
Table 1: Effects of Smoothing Kernel Size on Group-Level fMRI Metrics [34]
| Kernel Size (FWHM) | Effect on Functional Networks | Impact on Signal-to-Noise Ratio | Effect on Spatial Specificity |
|---|---|---|---|
| 0mm (no smoothing) | Maximum spatial specificity | Lowest SNR | No blurring |
| 2-4mm | Minimal network alteration | Moderate SNR improvement | Mild blurring |
| 6-8mm | Balanced network enhancement | Good SNR improvement | Moderate blurring |
| 10mm+ | Significant network modification | Highest SNR | Substantial blurring |
Research indicates that kernel selection represents a trade-off: larger kernels improve SNR and group-level analysis sensitivity but reduce spatial specificity and may obscure small activation regions, which is particularly problematic for clinical applications like presurgical planning [35] [36].
2. What is the recommended smoothing kernel for clinical applications requiring high spatial specificity?
For clinical applications where individual-level accuracy is critical (e.g., presurgical planning), use minimal smoothing (2-4mm FWHM) or adaptive spatial smoothing methods [36]. The standard 8mm kernel often used in neuroscience group studies is inappropriate for clinical applications where individual variability must be preserved [36]. Advanced methods like Deep Neural Networks (DNNs) can provide adaptive spatial smoothing that incorporates brain tissue properties for more accurate characterization of brain activation at the individual level [35].
Motion Correction Strategies
3. What are the main types of motion artifacts in fMRI, and how do they affect data quality?
Motion artifacts represent one of the greatest challenges in fMRI, causing two primary problems [37]:
- Spatial misalignment: Voxels represent different brain locations over time, complicating time-series analysis
- Signal artifacts: Motion disrupts EPI acquisition assumptions, creating large-magnitude signal changes that can dwarf biological signals of interest
Table 2: Motion Correction Strategies and Their Applications
| Strategy Type | Method Examples | Best Use Cases | Limitations |
|---|---|---|---|
| Prospective Correction | Real-time position updating, navigator echoes [37] | High-motion populations, children | Not widely available, requires specialized sequences |
| Retrospective Correction | Rigid-body registration, FSL MCFLIRT, SPM realign [38] | Standard research protocols | Cannot fully correct spin-history effects |
| Physiological Noise Correction | RETROICOR, CompCor [39] | Studies sensitive to cardiac/respiratory effects | Requires additional monitoring equipment |
| Advanced Methods | Multi-echo fMRI, fieldmap correction [39] | High-quality data acquisition | Increased acquisition and processing complexity |
4. How can I improve test-retest reliability through motion correction?
Optimizing your preprocessing pipeline significantly impacts test-retest reliability. Key strategies include [40]:
- Implementing rigorous motion parameter regression (6-24 parameters)
- Incorporating noise regressors from white matter and CSF signals
- Applying global signal regression cautiously, as it impacts connectivity measures
- Using high-pass filtering to remove low-frequency drifts
Research shows that preprocessing optimization can improve intra-class correlation coefficients (ICC) from modest levels (0.5-0.6) to more reliable values, though the optimal pipeline depends on your specific research goals [40].
Pipeline Optimization
5. How do I balance smoothing and motion correction in my preprocessing pipeline?
Create an optimized, standardized pipeline that maintains consistency across all subjects [34]:
- Perform quality assurance before any processing to identify fatal artifacts [41]
- Apply slice timing correction to account for acquisition time differences between slices [38]
- Implement rigid-body motion correction using a standardized reference volume [38]
- Choose smoothing parameters based on your specific research question and need for spatial specificity [36]
- Apply consistent parameters across all subjects in your study [34]
Experimental Protocols for Method Validation
Protocol 1: Evaluating Smoothing Kernel Impact
Objective: Systematically assess how kernel size affects your specific data and research question [34].
Methodology:
- Process identical dataset with multiple kernel sizes (0, 2, 4, 6, 8, 10mm FWHM)
- For each kernel size, calculate:
- Graph theory metrics (betweenness centrality, global/local efficiency, clustering coefficient)
- Principal Component Analysis parameters (kurtosis, skewness)
- Independent Component Analysis components
- Compare network structures and connectivity patterns across kernel sizes
- Select kernel that optimizes SNR while preserving spatial specificity needed for your hypothesis
Protocol 2: Motion Correction Quality Assessment
Objective: Validate motion correction efficacy and identify residual motion artifacts [37] [40].
Methodology:
- Extract six rigid-body motion parameters (3 translation, 3 rotation)
- Calculate framewise displacement (FD) and DVARS metrics
- Identify motion-contaminated volumes exceeding threshold (typically FD > 0.2-0.5mm)
- Implement censoring (scrubbing) or include motion parameters as regressors
- Verify correction efficacy by examining:
- Residual motion-related correlations in denoised data
- Relationship between motion and connectivity measures
- Group differences in motion parameters that may confound results
Research Reagent Solutions
Table 3: Essential Tools for fMRI Preprocessing Optimization
| Tool Category | Specific Solutions | Function | Implementation Considerations |
|---|---|---|---|
| Preprocessing Pipelines | fMRIPrep, SPM, FSL, AFNI | Automated standardized preprocessing | fMRIPrep provides consistent, reproducible processing [42] |
| Spatial Smoothing Tools | Gaussian filtering, Adaptive DNN methods [35] | Noise reduction, SNR improvement | DNN methods preserve spatial specificity better than isotropic smoothing [35] |
| Motion Correction Methods | MCFLIRT (FSL), Realign (SPM), RETROICOR [39] | Head motion artifact reduction | RETROICOR specifically targets physiological noise from cardiac/respiratory cycles [39] |
| Quality Metrics | Framewise displacement, DVARS, tSNR | Quantify data quality and preprocessing efficacy | Critical for identifying problematic datasets and validating corrections |
Workflow Visualization
fMRI Preprocessing Decision Pathway
Smoothing Kernel Selection Guide
FAQs on Paradigm Selection and Optimization
FAQ 1: What is the fundamental difference between a blocked and an event-related design?
A blocked design presents a condition continuously for an extended time interval (a block) to maintain cognitive engagement, with different task conditions alternating over time [43]. In contrast, an event-related design presents discrete, short-duration events. These events can be presented with randomized timing and order, allowing for the analysis of individual trial responses and reducing a subject's expectation effects [43]. A "rapid" event-related design uses an inter-stimulus-interval (ISI) shorter than the duration of the hemodynamic response function (HRF), which is typically 10-12 seconds [43].
FAQ 2: Which design has higher statistical power for detecting brain activation?
Blocked designs are historically recognized for their high detection power and robustness [43]. They produce a relatively large blood-oxygen-level-dependent (BOLD) signal change compared to baseline [43]. However, some direct comparisons, particularly in patient populations like those with brain tumors, have found that rapid event-related designs can provide maps with more robust activations in key areas like language cortex, suggesting comparable or even higher detection power in certain clinical applications [43].
FAQ 3: How does paradigm choice impact test-retest reliability, a critical issue in fMRI research?
Converging evidence demonstrates that standard univariate fMRI measures, including voxel- and region-level task-based activation, show poor test-retest reliability as measured by intraclass correlation coefficients (ICC) [16]. This is a major challenge for the field. The reliability of task-based activation can be influenced by task type [16]. Optimizing task design is therefore cited as an urgent need to improve the utility of fMRI for studying individual differences, including in drug development [29].
FAQ 4: For a pre-surgical language mapping study, which design is more sensitive?
A study comparing designs for a vocalized antonym generation task in brain tumor patients found a relatively high degree of discordance between blocked and event-related activation maps [43]. In general, the event-related design provided more robust activations in putative language areas, especially for the patients. This suggests that event-related designs may generate more sensitive language maps for pre-surgical planning [43].
FAQ 5: What are the key trade-offs I should consider when choosing a design?
The table below summarizes the core trade-offs between the two design types.
Table 1: Key Characteristics of Blocked vs. Event-Related fMRI Designs
| Characteristic | Blocked Design | Event-Related Design |
|---|---|---|
| Detection Power | High, robust [43] | Can be comparable or higher in some contexts [43] |
| BOLD Signal Change | Large relative to baseline [43] | Smaller for individual events |
| Trial Analysis | Not suited for single-trial analysis | Allows analysis of individual trial responses [43] |
| Subject Expectancy | More susceptible to expectation effects | Less sensitive to habituation and expectation [43] |
| Head Motion | More sensitive to head motion [43] | Less sensitive to head motion [43] |
| HRF Estimation | Not designed for precise HRF estimation | Effective at estimating the hemodynamic impulse response [43] |
Troubleshooting Common Experimental Issues
Issue 1: My fMRI activation maps are unreliable across sessions.
- Potential Cause: Low test-retest reliability of univariate measures is a known, widespread challenge in fMRI [16] [29].
- Solutions:
- Consider Multivariate Approaches: Some evidence suggests multivariate approaches may improve both reliability and validity [16].
- Minimize Head Motion: Motion has a pronounced negative effect on reliability. Ensure participants are comfortably restrained and use real-time motion correction if available. Studies show the lowest motion quartile of participants can have reliability estimates 2.5 times higher than the highest motion quartile [29].
- Optimize Design Timing: For event-related designs, use a jittered ISI to help de-convolve overlapping hemodynamic responses and improve statistical efficiency [43].
- Increase Session Length: Acquiring more data per subject can improve signal-to-noise ratio and reliability.
Issue 2: I need to isolate the brain's response to a specific, brief cognitive event.
- Potential Cause: A blocked design averages activity over a long period, making it unsuitable for parsing discrete cognitive processes.
- Solution: Switch to an event-related design. This paradigm is specifically suited for detecting transient variations in the hemodynamic response to individual trials or trial types, allowing you to model the brain's response to isolated events [43] [16].
Issue 3: My participants are becoming habituated or predicting the task sequence.
- Potential Cause: The predictable nature of a standard blocked design can lead to habituation and anticipation effects, which may confound the neural signal of interest.
- Solution: Implement a rapid event-related design with a jittered ISI. The randomized order and timing of trials help to minimize these confounding effects [43].
Issue 4: I am working with a clinical population that has difficulty performing tasks for long periods.
- Potential Cause: Blocked designs often require sustained cognitive engagement over 20-30 second periods, which can be challenging for some patient groups.
- Solution: An event-related design may be more tolerable. The presentation of brief, discrete trials can be easier for patients to handle, and the design is generally less sensitive to head motion, which is a common issue in clinical populations [43].
Experimental Protocols for Paradigm Comparison
Protocol: Direct Comparison of Blocked and Event-Related Designs for Language fMRI
This protocol is adapted from a study investigating design efficacy for pre-surgical planning [43].
1. Task Paradigm:
- Task: Vocalized antonym generation.
- Stimuli: Visually presented words.
- Control Condition: Vocalized reading of visually presented words.
2. Experimental Designs:
- Blocked Design: Alternating 30-second task blocks and 30-second control blocks.
- Event-Related Design: Rapid presentation of individual trial events (e.g., 3-second duration) with a jittered inter-stimulus-interval (ISI) randomized around a mean of 5-6 seconds.
3. Image Acquisition:
- Scanner: 3.0 Tesla MRI system.
- Sequence: Single-shot gradient-echo echo-planar imaging (EPI) for BOLD fMRI.
- Parameters: TR=2000 ms, TE=40 ms, flip angle=90°, voxel size=2×2×4 mm³.
- Structural Scan: High-resolution T1-weighted 3D-SPGR sequence.
4. Data Analysis:
- Preprocessing: Standard pipeline including motion correction, spatial smoothing, and normalization.
- Statistical Modeling:
- Blocked Design: Use a boxcar regressor convolved with a hemodynamic response function (HRF) to model task vs. control periods.
- Event-Related Design: Model each trial as a discrete event convolved with the HRF.
- Comparison Metrics:
- Visual Inspection: Qualitatively assess activation maps for robustness and coverage in putative language areas (e.g., Broca's and Wernicke's).
- Laterality Index: Calculate a quantitative measure of language lateralization for each design.
- Clinical Concordance: Compare fMRI results with gold-standard invasive maps from Wada testing or intra-operative cortical stimulation, if available [43].
The Scientist's Toolkit
Table 2: Essential Research Reagents and Materials for fMRI Paradigm Development
| Item Name | Function / Description | Key Considerations |
|---|---|---|
| 3.0 Tesla MRI Scanner | High-field magnetic resonance imaging system for BOLD fMRI data acquisition. | Higher field strength provides improved signal-to-noise ratio [43]. |
| Echo-Planar Imaging (EPI) | Fast MRI sequence for capturing rapid whole-brain images during task performance. | Essential for measuring the temporal dynamics of the BOLD signal [43]. |
| Stimulus Presentation Software | Software to deliver visual, auditory, or other stimuli to the participant in the scanner. | Must be capable of precise timing synchronization with the scanner's TR and support jittered designs. |
| Response Recording Device | Apparatus (e.g., button box, fMRI-compatible microphone) to record participant behavior. | Critical for monitoring task performance and ensuring engagement; must be MRI-safe [43]. |
| High-Resolution Structural Sequence | T1-weighted 3D sequence (e.g., SPGR, MPRAGE) for anatomical reference. | Used for spatial normalization and localization of functional activations [43]. |
| Jittered ISI Protocol | A trial presentation sequence with randomized intervals between stimuli. | A key component of rapid event-related designs to improve efficiency and de-convolve HRFs [43]. |
Workflow and Signaling Diagrams
Blocked vs. Event-Related Design Workflow
fMRI Reliability Optimization Pathway
Contrast Selection and Parameterization Approaches for Improved Consistency
Frequently Asked Questions
Q1: Why is the test-retest reliability of my fMRI task activations poor, and how can contrast selection improve it? Poor test-retest reliability can stem from several factors related to how brain activity is modeled and contrasted. To improve consistency, focus on selecting contrasts that capture stable, trait-like neural responses. Research indicates that the magnitude and type of contrast significantly impact reliability. For instance, contrasts modeled on the average BOLD response to a specific event (e.g., a simple decision vs. baseline) typically show greater reliability than those using parametrically modulated regressors (e.g., responses weighted by risk level) [44]. Furthermore, ensure your model includes key parameters known to affect analytical variability, such as appropriate motion regressors and hemodynamic response function (HRF) modeling [45].
Q2: What specific parameters in my subject-level GLM most impact the consistency of my results across sessions? Your choices in the General Linear Model (GLM) at the subject level are critical. Key parameters identified as major sources of analytical variability include [45]:
- Spatial Smoothing: The size of the smoothing kernel (FWHM) affects signal-to-noise and spatial specificity.
- Motion Regressors: The number of motion parameters included as nuisance regressors (e.g., 6, 24, or none) can significantly alter results.
- HRF Modeling: The presence or absence of HRF derivatives (temporal and/or dispersion) in the model flexibly accounts for variations in the hemodynamic response timing and shape. The combination of these choices, along with the software package used (e.g., FSL or SPM), can lead to substantially different group-level results, impacting the consistency of your findings [45].
Q3: How can I design an fMRI task to maximize its long-term reliability for a longitudinal or clinical trial study? To maximize long-term reliability, choose a task with minimal practice effects so that behavioral performance and neural correlates remain stable over time. For example, a probabilistic classification learning task has shown high long-term (13-month) test-retest reliability in frontostriatal activation because the specific materials to be learned can be changed across sessions, limiting performance gains from practice [46]. Additionally, select task contrasts that have been empirically demonstrated to show good reliability, such as the decision period in a risk-taking task (e.g., the Balloon Analogue Risk Task), which often shows higher reliability than outcome evaluation periods [44].
Troubleshooting Guides
Issue: Low Intra-class Correlation (ICC) in Key ROIs
Problem: The brain activation in your regions of interest (ROIs) is not stable across multiple scanning sessions for the same participants, leading to low ICC values.
Solution:
- Verify Contrast Design: Re-evaluate your primary contrast. Use a categorical "task vs. baseline" contrast instead of a parametrically modulated one if you are in the early stages of establishing reliability [44].
- Optimize ROI Definition:
- Define your ROIs based on significant group-level activations from an independent localizer task or dataset, rather than using an entire anatomical parcel. Using only the significantly activated vertices within a parcel has been shown to improve reliability [44].
- If using a pre-defined parcellation, ensure the regions are functionally relevant to your task.
- Control for Motion: Rigorously account for participant motion, as it has a documented moderate negative effect on test-retest reliability. Include a comprehensive set of motion parameters (e.g., 24 regressors: 6 rigid-body, their derivatives, and squares) in your subject-level GLM [45] [44].
- Check Analytical Pipeline: Ensure consistency in your processing pipeline across all sessions. Use containerized computing (e.g., Docker/Singularity) to guarantee identical software environments and versions [45].
Issue: High Analytical Variability Across Research Teams
Problem: Different research groups analyzing the same dataset arrive at different conclusions due to varying analytical pipelines.
Solution:
- Standardize Critical Parameters: Based on large-scale comparisons, explicitly define and report these parameters in your methods [45]:
- Software (FSL, SPM, AFNI)
- Spatial smoothing kernel size (e.g., 5mm or 8mm FWHM)
- Number of motion regressors (0, 6, or 24)
- HRF modeling (with or without derivatives)
- Provide Unthresholded Maps: Share unthresholded statistical maps to facilitate direct comparison and meta-analysis across studies, as thresholding can exaggerate small differences [45] [46].
- Use Public Datasets for Benchmarking: Leverage publicly available datasets like the HCP Multi-Pipeline dataset to benchmark your pipeline's performance against a range of common analytical choices [45].
Data and Metrics Tables
Table 1: Test-Retest Reliability (ICC) of fMRI Tasks in Selected Brain Regions
| Brain Region | Task (Contrast) | ICC Value | Retest Interval | Key Influencing Factor |
|---|---|---|---|---|
| Left Anterior Insula [44] | BART (Decision Period) | 0.54 | ~6 months | Contrast type (decision > baseline) |
| Right Caudate [44] | BART (Outcome Period) | 0.63 | ~6 months | Event type (outcome processing) |
| Right Fusiform [44] | BART | 0.66 (Familiality) | ~6 months | High magnitude of activation |
| Frontostriatal Network [46] | Probabilistic Classification Learning | High (Group Concordance) | 13 months | Task with minimal practice effects |
| Parietal, Occipital, Temporal Lobes [44] | BART | Good (Mean ICC ~0.17, range 0-.8) | ~6 months | General regional sensitivity |
Table 2: Impact of GLM Parameter Choices on Analytical Variability
| GLM Parameter | Common Options | Impact on Results & Reliability |
|---|---|---|
| Spatial Smoothing [45] | 5mm FWHM, 8mm FWHM | Larger kernels increase signal-to-noise but reduce spatial specificity; a key driver of result variability. |
| Motion Regressors [45] | 0, 6 (rotations & translations), 24 (6 + derivatives + squares) | The number included can significantly alter activation maps; 24 regressors provide more comprehensive noise control. |
| HRF Modeling [45] | Canonical only, With temporal derivatives, With dispersion derivatives | Including derivatives accounts for timing differences, improving model fit but increasing analytical flexibility. |
| Software Package [45] | FSL, SPM, AFNI | Different algorithms and default settings across software are a major source of variability in final results. |
Experimental Protocols
Protocol 1: Evaluating Parameter Choices with the HCP Multi-Pipeline Dataset
Objective: To systematically investigate how analytical choices at the subject-level impact the consistency of group-level fMRI results [45].
Methodology:
- Data: Use the raw task-fMRI data (e.g., motor task) from a large public dataset like the HCP Young Adult (N=1080) [45].
- Pipeline Implementation: Implement multiple analysis pipelines using a workflow system like Nipype to ensure interoperability. The pipelines should vary on these key parameters [45]:
- Software: SPM and FSL.
- Smoothing: FWHM of 5mm and 8mm.
- Motion Regressors: 0, 6, and 24.
- HRF Derivatives: Presence (1) or absence (0).
- Analysis: Run all 24 (2x2x3x2) pipeline combinations on the dataset. Compute group-level statistics for each pipeline and a specific contrast (e.g., "right hand tap vs. baseline").
- Evaluation: Compare the resulting group-level statistic maps to quantify the variability introduced by each parameter choice.
Protocol 2: Assessing Test-Retest Reliability for a Novel Task
Objective: To determine the long-term test-retest reliability of neural activations for a task intended for use in longitudinal studies or clinical trials [44] [46].
Methodology:
- Participant Recruitment: Recruit a cohort of participants (e.g., N=20-30). Including monozygotic twins can allow for additional assessment of familiality [44].
- Scanning Sessions: Schedule two identical scanning sessions separated by a clinically relevant interval (e.g., 6-12 months). The task should be designed to minimize practice effects [46].
- Data Acquisition & Preprocessing: Acquire task-fMRI data using a standardized protocol. Preprocess all data through a single, fixed pipeline (e.g., using fMRIPrep) to minimize variability from preprocessing steps.
- Subject-Level Analysis: For a specific contrast of interest, extract the parameter estimates (e.g., beta weights) or percent signal change from your pre-defined ROIs for each participant at both time points.
- Reliability Analysis: Calculate the Intra-class Correlation Coefficient (ICC) for each ROI to quantify the consistency of the activation measures between the two sessions. ICC values can be interpreted as: <0.4 Poor; 0.4-0.59 Fair; 0.6-0.74 Good; >0.75 Excellent [44].
The Scientist's Toolkit
| Tool / Resource | Function / Purpose | Example Use Case |
|---|---|---|
| HCP Multi-Pipeline Dataset [45] | Provides pre-computed statistical maps from 24 different pipelines on 1,080 subjects. | Benchmarking your analytical pipeline; studying sources of analytical variability. |
| Nipype [45] | A Python-based framework for creating interoperable and reproducible fMRI analysis workflows. | Implementing and comparing multiple analysis pipelines that combine different software tools (FSL, SPM). |
| NeuroDocker [45] | A tool for generating containerized and reproducible neuroimaging computing environments. | Ensuring that your analysis pipeline runs identically across different computing systems, enhancing reproducibility. |
| Intra-class Correlation (ICC) [44] [46] | A statistical measure used to quantify test-retest reliability of continuous measures. | Determining the stability of fMRI activation measures in an ROI across multiple scanning sessions. |
| FSL & SPM [45] | Widely used software packages for fMRI data analysis, each with different algorithms and default settings. | Performing standard GLM-based analysis of task-fMRI data; their comparison highlights analytical variability. |
What is the recommended window width and step length for a balance of reliability and sensitivity?
The selection of window width and step length is a critical trade-off between capturing meaningful brain dynamics and ensuring the statistical reliability of the computed connectivity metrics. Based on recent test-retest reliability studies, the following parameters are recommended:
| Parameter | Recommended Value | Effect on Reliability | Key Findings |
|---|---|---|---|
| Window Width | ~100 seconds (e.g., 139 TRs for TR=0.72s) | Moderate to High | A 100-second width provided at least moderate whole-brain reliability (ICC > 0.4). Longer windows (e.g., 150s) can decrease reliability [27]. |
| Step Length | ~40 seconds (e.g., 56 TRs for TR=0.72s) | Minimal Impact | Test-retest reliability was not significantly altered by different step lengths when the window width was fixed [27]. |
| Scan Duration | ≥ 15 minutes | Significant Impact | Shorter total fMRI scan durations markedly reduce the reliability of dFC metrics. Approximately 15 minutes of data is recommended for reliable state prevalence measures [47] [27]. |
How do these parameters affect the test-retest reliability of dFC metrics?
The reliability of different dFC metrics is not uniform. When using a sliding-window approach, some metrics demonstrate much higher test-retest reliability than others.
- State Prevalence is Most Reliable: In a two-state model, the prevalence of a brain state (the fraction of time spent in that state) has been identified as the most reliable parameter, with Intraclass Correlation Coefficient (ICC) values around 0.5 for ~15 minutes of data [47].
- Lower Reliability for Other Metrics: Parameters such as mean dwell time (the average time spent in a state before switching) have been found to be much less reliable [47].
- Temporal Variability is Moderately Reliable: The temporal variability of a network (how much its connectivity profile fluctuates over time) has shown at least moderate test-retest reliability (ICC > 0.4) across the whole brain and in most networks when using the recommended parameters above [27].
Beyond the sliding window, what other factors influence dFC reliability?
Optimizing your pipeline extends beyond window parameters. The following factors systematically impact the reliability and validity of your dFC results:
- Data Preprocessing: Common band-pass filters (e.g., 0.009–0.08 Hz) can inflate correlation estimates and increase false positives if not used with appropriate downsampling [11]. The controversial step of Global Signal Regression (GSR) also affects reliability, and its use should be justified and reported [47] [48].
- Brain Parcellation: The choice of brain atlas (e.g., AAL with 90 nodes vs. Power with 264 nodes) can influence results. However, one study found that atlas choice had no significant effect on the reliability of a two-state model's parameters [47] [27].
- Connectivity Metric: While Pearson's correlation is the default, benchmarking studies show that other pairwise statistics, such as precision (inverse covariance), can yield higher structure-function coupling and better alignment with other neurophysiological networks [49].
- Data Centering: Within-subject centering of data has been shown to reduce the reliability of dFC parameters [47].
Experimental Protocol for Parameter Optimization
To systematically evaluate window width and step length in your own data, follow this experimental workflow:
Step-by-Step Methodology:
- Data Preparation: Begin with fully preprocessed resting-state fMRI data from a test-retest dataset (e.g., the Human Connectome Project). Ensure minimal artifacts and proper denoising [27].
- Parameter Sampling: Systematically vary the window width and step length across a realistic range. A robust design includes at least three different values for each parameter (e.g., window widths of 50s, 100s, 150s; step lengths of 20s, 40s, 60s) [27].
- dFC Construction: For each parameter combination, apply the sliding-window technique to construct dynamic functional connectivity matrices. Use a consistent connectivity measure (e.g., Pearson correlation) for this initial comparison.
- Metric Extraction: From the dynamic matrices, calculate your dFC metric of interest, such as brain-state prevalence or temporal variability [47] [27].
- Reliability Calculation: Compute the Intraclass Correlation Coefficient (ICC) for each dFC metric across the test and retest sessions for every parameter set. The ICC quantifies the consistency of measurements between sessions [47] [27].
- Optimal Parameter Selection: Identify the parameter combination (window width and step length) that yields the highest ICC value for the most critical dFC metrics in your study.
- Validation: Confirm the stability and generalizability of your chosen parameters by applying them to a separate, independent dataset or a held-out portion of your sample [48].
The Scientist's Toolkit: Essential Research Reagents
| Tool Name | Function / Role in dFC Analysis |
|---|---|
| Human Connectome Project (HCP) Dataset | Provides high-quality, test-retest resting-state fMRI data for method development and validation [27]. |
| Sliding-Window Algorithm | The core method for segmenting continuous fMRI data into time-varying connectivity matrices [27]. |
| Intraclass Correlation Coefficient (ICC) | The key statistical measure for quantifying test-retest reliability of dFC metrics [47] [27]. |
| Brain Parcellation Atlas (e.g., AAL, Power) | Defines the network nodes by partitioning the brain into regions of interest [27]. |
| PySPI Package | A software library that enables the computation of a vast library of 239 pairwise interaction statistics beyond Pearson correlation, allowing for the optimization of the connectivity metric itself [49]. |
| Portrait Divergence (PDiv) | An information-theoretic measure used to compare whole-network topologies, useful for evaluating pipeline reliability beyond individual edges or metrics [48]. |
Troubleshooting Guide: Common Issues and Solutions
| Problem Area | Specific Issue | Potential Causes | Recommended Solutions |
|---|---|---|---|
| Data Reliability | Poor test-retest reliability (ICC) of univariate measures [16] | High within-subject variance, short test-retest intervals, analytical choices (e.g., using contrast scores) [16] [18] | Use beta coefficients from GLM instead of contrast scores; employ multivariate approaches; optimize preprocessing [18] [50]. |
| Site & Scanner Effects | Systematic differences in data between sites [5] | Different scanner manufacturers, imaging protocols, and head coils [5] [51] | Implement traveling-subject studies; use standardized quality control (QC) phantoms; harmonize imaging protocols across sites [5] [51]. |
| Functional Connectivity Variability | High within-subject across-run variation in rsFC [5] | Physiological noise, participant state (e.g., arousal, attention), and protocol differences [5] | Use longer (e.g., 10-minute) resting-state scans; employ machine-learning algorithms that can suppress irrelevant variability [5]. |
| Analytical Reproducibility | Inability to reproduce published results | Insufficient methodological details in published papers; use of different analysis software/options [52] | Adhere to reporting guidelines (e.g., COBIDAS); use standardized preprocessing pipelines (e.g., fMRIPrep); share analysis code and data [52] [53]. |
Frequently Asked Questions (FAQs)
Q1: What is the most critical first step in planning a multicenter fMRI study? The most critical step is protocol harmonization. This involves standardizing the MRI acquisition sequences, scanner hardware where possible, and participant setup (e.g., head coil, stimulus presentation systems) across all sites. Early studies demonstrated that even with identical scanner models, factors like stimulus luminance and auditory delivery must be matched to ensure compatibility [51].
Q2: Our study found low intraclass correlation coefficients (ICCs) for task activation. Does this mean our measure is invalid? Not necessarily. While reliability provides an upper bound for validity, the two are distinct concepts [16]. A measure can be valid but unreliable if it is noisy, much like a noisy thermometer that gives the correct reading on average. Focus on improving reliability through analytical choices, but note that low ICC attenuates the observed correlation with other variables and increases the sample size needed to detect effects [16] [50].
Q3: How can we statistically account for scanner and site effects in our analysis? Including "site" as a covariate or random factor in your statistical model is a common approach. Furthermore, traveling-subject studies, where the same participants are scanned across all sites, are the gold standard for quantifying and correcting for site-related variance [5] [51]. Recent multivariate machine-learning methods can also actively suppress site-related variance while enhancing disease-related signals [5].
Q4: Which should I use to calculate reliability: beta coefficients or contrast values? Evidence suggests using beta coefficients from your first-level general linear model (GLM). Contrasts (difference scores) tend to have lower between-subject variance and higher error, which artificially deflates reliability estimates (ICC values) [18]. Using beta coefficients for a single condition typically yields higher and more accurate reliability.
Q5: What are the key methodological details we must report for our multicenter study? Comprehensive reporting is essential for reproducibility [52]. Key details include:
- Participants: Detailed inclusion/exclusion criteria and demographic information.
- Task: Precise description of the paradigm, including stimulus timing, delivery, and participant instructions.
- Acquisition: Full MRI scanner and sequence parameters (e.g., TR, TE, voxel size, FOV, manufacturer, model, software version).
- Analysis: The software used (with version), preprocessing steps, statistical models (including the precise regressors and contrasts), and methods for multiple comparison correction.
- Normalization: The specific atlas or template used (e.g., MNI, not just "Talairach space") [52].
Quantitative Data on Multicenter Variability
The following table summarizes the magnitude of different sources of variation found in a large-scale multicenter resting-state fMRI study, which helps prioritize mitigation efforts [5].
Table: Hierarchy of Functional Connectivity Variations in Multicenter Studies
| Source of Variation | Median Magnitude (BMB Dataset) | Description & Impact |
|---|---|---|
| Unexplained Residuals | 0.160 | Largely attributed to within-subject, across-run variation (e.g., physiological state, attention). This is often the largest noise component [5]. |
| Participant Factor (Individual Differences) | 0.107 | Represents genuine, stable differences between people. This is the signal of interest in many studies and should be maximized [5]. |
| Scanner Factor | 0.026 | Systematic differences introduced by different scanner manufacturers and models [5]. |
| Protocol Factor | 0.016 | Differences due to acquisition protocols (e.g., sequence parameters). Harmonization can minimize this [5]. |
Standardized Experimental Protocol for Site Compatibility
This protocol is designed to be implemented across multiple scanning sites to ensure data compatibility.
Objective: To acquire task-based and resting-state fMRI data with minimal site-specific variance.
Materials:
- Identical or comparable 3T MRI scanners (preferred).
- Standardized quality control phantom (e.g., cylindrical MRI phantom).
- Harmonized EPI sequence parameters (TR, TE, flip angle, voxel size, FOV).
- Projector or display system with calibrated luminance.
- MRI-compatible headphones.
Pre-Study Procedure: Site Harmonization [51]
- Phantom Scans: All sites perform daily QC phantom scans using the standardized EPI sequence for at least one week. Analyze for system noise (NRMS, PTP) and stability.
- Traveling Subjects: Scan a small cohort of "traveling subjects" (e.g., 3-5 participants) at all participating sites. Use this data to quantify and adjust for site effects in the main study.
Data Acquisition Protocol:
- Structural Scan: Acquire a high-resolution T1-weighted image.
- Resting-State fMRI:
- Duration: 10 minutes with eyes open [5].
- Instructions: Participants should fixate on a cross and not think of anything in particular.
- Task-Based fMRI (Example: Blocked Motor/Visual Task [51]):
- Design: Alternating 20-second blocks of task and rest.
- Motor Task: Auditory-paced button pressing (1 Hz).
- Visual Task: Presentation of a flashing checkerboard.
- Instructions: Provide identical written and verbal instructions to all participants at all sites.
Data Analysis & Reliability Assessment:
- Preprocessing: Use a robust, standardized pipeline like fMRIPrep [53] to ensure consistency.
- First-Level Model: For task data, model the BOLD response using a canonical HRF. Extract beta coefficients for conditions of interest [18].
- Reliability Calculation: Calculate the Intraclass Correlation Coefficient (ICC) – specifically ICC(2,1) for absolute agreement of single measures – for key brain regions or connections [16].
Workflow and Relationship Diagrams
Diagram 1: Standardization Workflow for Multicenter fMRI Studies.
Diagram 2: Machine Learning Inverts Variation Hierarchy.
The Scientist's Toolkit: Essential Research Reagents & Materials
| Tool / Resource | Function in Multicenter Studies | Key Considerations |
|---|---|---|
| Standardized QA Phantom | Monitors scanner stability and noise performance over time [51]. | Use a consistent phantom model across sites. Track metrics like NRMS and PTP noise. |
| fMRIPrep Pipeline | Provides a robust, standardized platform for preprocessing both task and resting-state fMRI data [53]. | Promotes reproducibility; handles diverse data inputs; generates quality control reports. |
| Traveling Subject Data | Gold standard for directly quantifying and correcting for intersite variance [5] [51]. | Logistically challenging; crucial for validating that site effects are smaller than effects of interest. |
| ICC Analysis Scripts | Quantifies test-retest reliability of fMRI measures (activation/connectivity) [16]. | Choose the appropriate ICC model (e.g., ICC(2,1)); use beta coefficients, not contrasts, for calculation [18]. |
| Reporting Guidelines (COBIDAS) | Checklist for comprehensive methodological reporting to ensure reproducibility [52]. | Critical for meta-analyses and database mining; should detail acquisition, preprocessing, and analysis. |
Practical Solutions for Overcoming Common fMRI Reliability Challenges
Troubleshooting Guides
Physiological Noise Correction
Issue: My fMRI data, particularly in brainstem and subcortical regions, shows high physiological noise from cardiac and respiratory cycles, reducing temporal signal-to-noise ratio (tSNR).
Solution: Implement a physiological noise model using the RETROICOR method.
- Detailed Protocol: Based on a 2025 study comparing implementations for multi-echo fMRI data [39]:
- Data Acquisition: Collect cardiac and respiratory signals simultaneously with your fMRI data using a pulse oximeter and breathing belt.
- Model Construction: Use the recorded physiological data to create noise regressors. The RETROICOR algorithm models the noise as a Fourier series based on the phase of the cardiac and respiratory cycles.
- Integration into Pipeline: Incorporate the noise regressors into your general linear model (GLM) for denoising. You can apply RETROICOR to individual echo times (
RTC_ind) or to the composite data after combining echoes (RTC_comp); both approaches show comparable efficacy [39]. - Validation: Check the improvement in temporal SNR (tSNR) and metrics like signal fluctuation sensitivity (SFS) in affected regions.
Table 1: RETROICOR Efficacy Across Acquisition Parameters (Adapted from [39])
| Multiband Factor | Flip Angle | tSNR Improvement with RETROICOR |
|---|---|---|
| 4 | 45° | Significant improvement |
| 6 | 45° | Significant improvement |
| 6 | 20° | Notable improvement |
| 8 | 20° | Limited improvement; acquisition quality degraded |
Denoising Pipeline Selection
Issue: I am unsure which denoising pipeline to use for my resting-state fMRI data to best remove artifacts while preserving neural signals of interest.
Solution: Adopt a standardized, multi-metric approach to select a denoising strategy.
- Detailed Protocol: A 2025 benchmarking study proposed a robust framework for comparing pipelines [54]:
- Apply Multiple Pipelines: Process your data in parallel with several denoising strategies. Common options include:
- Regression of mean signals from White Matter (WM) and Cerebrospinal Fluid (CSF).
- Global Signal Regression (GSR).
- ACompCor.
- Calculate Quality Metrics: Compute a set of metrics for each pipeline to quantify performance:
- Artifact Removal: Framewise Displacement (FD), DVARS.
- Signal Preservation: Temporal Signal-to-Noise Ratio (tSNR).
- Resting-State Network Identifiability: Quantitative metrics for network spatial sharpness and identifiability.
- Use a Summary Index: Combine the metrics into a single summary performance index to identify the pipeline that offers the best compromise between noise removal and signal preservation. The cited study found that a pipeline combining WM/CSF regression and GSR often performed best [54].
- Apply Multiple Pipelines: Process your data in parallel with several denoising strategies. Common options include:
Improving Analysis Reliability
Issue: The test-retest reliability of my task-fMRI results is poor, especially at the individual level.
Solution: Optimize your analytical approach by using beta coefficients and multivariate models.
- Detailed Protocol:
- Use Beta Coefficients for ICC Calculation: When assessing reliability for a task, calculate the Intraclass Correlation Coefficient (ICC) using the β coefficients from your first-level GLM instead of condition contrasts. A 2022 study demonstrated that β coefficients yield higher ICC values because they have greater between-subject variance and avoid the high error inherent in subtracting two correlated condition values [18].
- Leverage Multivariate Predictive Models: For resting-state functional connectivity, move beyond the reliability of single connections. Use multivariate predictive models (e.g., ridge regression, connectome-based predictive modeling) that aggregate information across many brain features. A 2021 study showed that the predicted outcomes of these models have substantially higher test-retest reliability than individual functional connections [55].
Table 2: Reliability (ICC) of fMRI Measures [18] [55]
| fMRI Measure | Typical ICC Range | Interpretation |
|---|---|---|
| Individual task activation contrast (voxel) | Often < 0.4 | Poor reliability |
| Task β coefficient (voxel) | Higher than contrasts | Improved reliability |
| Individual functional connection | Often < 0.4 | Poor reliability |
| Multivariate model prediction | 0.6 - 0.75 (for best methods) | Good reliability |
Addressing Motion-Related Global Signal Changes
Issue: After using multi-echo ICA (ME-ICA) to remove motion artifacts, I am concerned about whether to perform Global Signal Regression (GSR).
Solution: ME-ICA is effective at removing motion artifacts, but the decision to apply GSR requires careful consideration.
- Detailed Protocol:
- Apply ME-ICA: Use multi-echo fMRI acquisition combined with ME-ICA processing. This method effectively differentiates BOLD from non-BOLD signals and removes spurious, distance-dependent effects caused by head motion [56].
- Evaluate GSR Cautiously: Be aware that while some argue GSR can remove residual motion-associated respiratory effects after ME-ICA, this is not empirically definitive. GSR can distort correlation patterns and remove neural signal of interest [56].
- Recommendation: The consensus is to discourage the routine implementation of GSR following ME-ICA. Consider alternative, more targeted denoising approaches if necessary [56].
Frequently Asked Questions
Q1: What is the most reliable measure for task-based fMRI? For calculating test-retest reliability, using the β coefficient from a first-level general linear model is more reliable than using condition contrasts. Contrasts (difference scores) have low between-subject variance and introduce error, leading to underestimation of true reliability [18].
Q2: How does magnetic field strength affect physiological noise? Physiological noise increases with the square of the main field strength (B0), while the signal only increases linearly. This means that at higher field strengths (e.g., 7T), physiological noise can become the dominant source of noise, especially in areas like the brainstem. However, the benefits of higher BOLD contrast and spatial resolution at ultra-high fields can still be advantageous [57].
Q3: Can "noise" in the fMRI signal ever be clinically useful? Yes. Emerging research shows that systemic low-frequency oscillations (sLFOs), traditionally treated as physiological noise, carry biologically meaningful information. For example, sLFO amplitude has been linked to drug abstinence, dependence severity, and cue-induced craving, offering a potential complementary biomarker for clinical studies [58].
Q4: My scan protocol uses high multiband acceleration. Will RETROICOR still work? A 2025 study confirms RETROICOR's compatibility with accelerated acquisitions. The benefits are particularly notable with moderate acceleration factors (e.g., MB4 and MB6). While the highest acceleration (e.g., MB8) can degrade overall data quality, RETROICOR can still be applied, though its benefits may be more limited [39].
The Scientist's Toolkit
Table 3: Essential Research Reagents & Solutions for fMRI Reliability
| Item | Function / Explanation |
|---|---|
| Multi-Echo fMRI Sequence | Acquires multiple images at different echo times (TEs), enabling advanced denoising like ME-ICA to separate BOLD signal from non-BOLD artifacts [56] [39]. |
| RETROICOR Algorithm | A method for modeling and removing signal fluctuations caused by the cardiac and respiratory cycles from the fMRI time series, using externally recorded physiological data [39] [57]. |
| Physiological Monitors | A pulse oximeter (for cardiac cycle) and breathing belt (for respiratory cycle) are required to collect the data needed for RETROICOR [57]. |
| Standardized Pipeline Software | Tools like the HALFpipe provide a containerized, standardized workflow for fMRI preprocessing and denoising, reducing analytical flexibility and improving reproducibility [54]. |
| Multivariate Predictive Models | Machine learning models (e.g., Ridge Regression, SVR) that aggregate information across many brain features to predict an outcome, resulting in higher test-retest reliability than single features [55]. |
Frequently Asked Questions (FAQs)
Q1: Why should I consider using a Finite Impulse Response (FIR) model over a canonical hemodynamic response model?
A1: The primary advantage of an FIR model is its flexibility. Unlike a canonical model, which is biased toward a specific, predetermined shape, the FIR model is shape-unconstrained [59]. This allows it to capture the true hemodynamic response more accurately, especially in brain regions (e.g., prefrontal cortex, subcortical areas) or clinical populations where the response may differ from the canonical shape derived from visual and auditory stimuli [59] [60]. This flexibility is crucial for improving the validity of your analysis and can reveal more subtle aspects of the BOLD response, such as differences in the latency of the signal rise between conditions [59].
Q2: Why is the choice of hemodynamic model important for improving test-retest reliability in fMRI studies?
A2: Test-retest reliability is a basic precursor for the clinical adoption of fMRI [61]. Mis-specification of the BOLD response's shape introduces noise and inefficiency into single-subject reactivity estimates, which directly lowers reliability [61]. Using a more accurate model, like FIR or Gamma Variate, that better fits the individual's actual hemodynamic response can enhance the signal-to-noise ratio of your estimates, leading to more stable and reproducible results across scanning sessions [61] [60].
Q3: What is a common challenge when implementing a Gamma Variate model, and how can it be addressed?
A3: A significant challenge is that Gamma Variate fitting is inherently noisy [62]. The model is often fit using only the first portion of the contrast uptake curve to avoid contamination from recirculation effects, which means it is estimated from a limited data sample [62]. To address this, it is recommended to generate and inspect a goodness-of-fit map (e.g., a χ²-map) to identify voxels or regions where the model provides a poor fit to the data [62].
Q4: How do I specify contrasts for an FIR model, given it produces multiple parameter estimates per condition?
A4: Contrast specification in FIR models is more complex because the response for a single condition is characterized across several time lags [63]. A common and valid approach is to define your contrast to test the sum across the multiple time lags [63]. This involves creating a contrast vector that adds together the beta weights for all the delays (e.g., 1, 2, and 3) that belong to the same experimental condition. This tests the overall response to that condition across the modeled time window.
Troubleshooting Guides
Poor Test-Retest Reliability with FIR Models
| Problem | Potential Causes | Solutions |
|---|---|---|
| Poor test-retest reliability of FIR model estimates. | 1. Low statistical power from dividing already noisy data into finer time-point estimates [59].2. Group-level analysis involves a large number of statistical tests, increasing the risk of false positives if not properly controlled [59].3. Unmodeled time-varying noise sources (e.g., head motion, state anxiety) [61]. | 1. Ensure your design has sufficient trials to robustly estimate the response at each delay.2. At the group level, carefully select a specific time-point or a small subset of time-points to test your hypothesis, and apply rigorous multiple comparison correction [59].3. Statistically control for sources of variance like motion parameters and physiological measures (e.g., heart rate) [61] [64]. |
Implementation and Fit Issues with Gamma Variate Models
| Problem | Potential Causes | Solutions |
|---|---|---|
| High variance or poor goodness-of-fit in Gamma Variate model parameters. | 1. The model is fitted only on the initial portion of the first-pass bolus, making it sensitive to noise [62].2. The selected parameters (A, α, β, etc.) are not optimal for your data.3. The model itself may be mis-specified for the underlying physiological process. | 1. Always generate and consult a goodness-of-fit map (χ²-map) to assess model performance and interpret parameter maps with caution [62].2. Use a symbolic equation to model the Gamma Variate function and ensure coefficients are pre-defined and appropriate for your data [65].3. Consider alternative models, such as the single compartment recirculation (SCR) model, if Gamma Variate fitting performs poorly [62]. |
Comparative Performance of Hemodynamic Modeling Techniques
The following table summarizes key characteristics and reported performance metrics for FIR and Gamma Variate models, based on simulation and empirical studies.
| Model | Key Features | Reported ICC / Reliability | Best Use Cases |
|---|---|---|---|
| Finite Impulse Response (FIR) | Unconstrained shape; models response at discrete time lags; flexible [59] [63]. | Can improve reliability vs. canonical models when optimized [61]. Useful for quantifying latency [60]. | Exploring HRF shape in new regions/populations; studying response latency and duration [59] [60]. |
| Gamma Variate | Parametric model; can fit onset, rise/fall slope, and magnitude; can correct for recirculation [61] [62]. | Including temporal derivatives can provide larger test-retest reliability values [61]. | DSC perfusion imaging; when a smooth, parametric estimate of the HRF is needed [62]. |
| Canonical HRF (with derivatives) | Constrained shape; typically includes timing and dispersion derivatives to account for small shifts [61]. | The use of derivatives can improve reliability by accounting for individual differences in timing [61]. | Standard task-fMRI when the canonical shape is a reasonable assumption; high-power studies focused on amplitude. |
Test-Retest Reliability Benchmarks in fMRI
This table presents established guidelines and commonly reported values for test-retest reliability in fMRI, providing context for evaluating your own results.
| Reliability Index | Value Range | Interpretation | Context from Literature |
|---|---|---|---|
| Intraclass Correlation (ICC) | < 0.400.40 - 0.590.60 - 0.74> 0.75 | PoorFairGoodExcellent | Considered the standard index for fMRI reliability [61] [66]. Fair reliability (≥0.4) is suggested for scientific purposes, while excellent reliability (≥0.75) is required for clinical use [66]. |
| Single-Subject Time Course Reproducibility (Correlation) | ~0.26 (conventional pipeline)~0.41 (optimized pipeline) | LowFair | Conventional preprocessing pipelines yield low single-subject reproducibility. One study showed optimized Savitzky-Golay filtering could improve it to a fair level [66]. |
| Group-Level fMRI (Meta-Analysis) | ICC = ~0.40 (task-based)ICC = ~0.29 (resting-state) | Poor to Fair | Recent meta-analyses suggest that group-level reproducibility for both task and resting-state fMRI is currently below the threshold required for clinical applications [66]. |
Experimental Protocols
Protocol for Implementing an FIR Analysis
This protocol outlines the key steps for setting up and executing a Finite Impulse Response analysis, using common fMRI software packages.
Objective: To estimate the hemodynamic response to a task condition without assuming a fixed shape, thereby improving the accuracy of latency and duration measurements.
Procedure:
- Preprocessing: Preprocess your fMRI data (motion correction, slice-timing correction, normalization, etc.) as you would for a standard GLM analysis [59].
- Model Specification: In your statistical software (SPM, FSL, AFNI), specify the design matrix using the FIR model. Set the
hrf_modelto 'fir' and define thefir_delays. For example, with a TR of 2 seconds, delays of [1, 2, 3, 4, 5] would model the response across a 10-second window [63]. - Contrast Specification: This is a critical and more complex step. To test for an overall response to a condition, you must create a contrast that sums the beta weights across all delays for that condition [63]. For a condition named "A" modeled with 3 delays, this would be a contrast vector of [1, 1, 1] for the three columns corresponding to "A" and zeros elsewhere.
- Group-Level Analysis: Analyze the FIR estimates at the group level. This can be done by:
- Averaged Response: Using the contrast that sums across delays to test for the overall presence of a response.
- Time-Point Analysis: Selecting one or a few specific, hypothesis-driven time-points (e.g., the time-to-peak) for group comparison to minimize the number of tests [59].
Workflow for FIR Analysis Implementation
The diagram below illustrates the key stages and decision points in a typical FIR analysis pipeline.
The Scientist's Toolkit: Research Reagent Solutions
This table lists essential computational tools and methodological "reagents" for implementing advanced fMRI modeling techniques.
| Tool / Solution | Function | Example Use Case / Note |
|---|---|---|
| FIR Basis Set | A set of binary regressors that capture the BOLD signal at discrete time lags after stimulus onset. | Used to model the hemodynamic response without assuming its shape. Implemented in SPM, FSL, and AFNI [63]. |
| Gamma Variate Function | A parametric function of the form S(t) = A(t−to)α e−(t−to)/β used to model the first-pass hemodynamic response. | Used in DSC perfusion imaging and task-fMRI to estimate onset, magnitude, and width of the HRF while correcting for recirculation [61] [62]. |
| Savitzky-Golay Filter | A digital filter that can smooth data while preserving signal features, improving time-course reproducibility. | An optimized post-processing filter that can improve single-subject test-retest reliability from poor (r=0.26) to fair (r=0.41) [66]. |
| Intraclass Correlation (ICC) | A statistical measure of test-retest reliability, quantifying the consistency of measurements across sessions. | The standard metric for assessing fMRI reliability. Values above 0.4 are considered "fair" and a minimum for scientific use [61] [66]. |
| Goodness-of-Fit Map (χ²-map) | A voxel-wise map showing how well the chosen model fits the observed data. | Critical for diagnosing poor model fit, especially for noisy models like the Gamma Variate [62]. |
Region of Interest (ROI) Selection Strategies Based on Reliability Metrics
Troubleshooting Guides
FAQ 1: What is the most reliable method for defining Regions of Interest (ROIs) for language fMRI?
Issue: Researchers encounter low test-retest reliability in language mapping studies, leading to inconsistent results across scanning sessions.
Solution: Evidence strongly supports using subject-specific functional ROIs (fROIs) over standardized anatomical ROIs (aROIs). A 2025 study directly comparing these approaches found that subject-specific fROIs yielded significantly larger effect sizes and higher reliability across sessions [67] [68].
Recommended Protocol:
- Acquire functional data using a robust language paradigm (e.g., sentence reading vs. nonword reading)
- Define functional partitions based on group-level activation patterns
- Within these group-constrained partitions, identify subject-specific active regions for each individual
- Use these individualized fROIs for subsequent analysis
This approach accounts for inter-individual anatomical and functional variability, increasing sensitivity and functional resolution [67] [68].
FAQ 2: How does ROI selection strategy affect reliability in clinical populations with brain disorders?
Issue: Researchers working with post-stroke aphasia patients question whether reliability findings from healthy populations generalize to clinical groups.
Solution: For clinical populations like people with aphasia, focus analyses on established cognitive and language subnetworks rather than whole-brain networks. A 2025 study in adults with chronic aphasia found that reliability was better in most subnetworks compared to the whole brain [23].
Key Considerations for Clinical Populations:
- Ensure sufficiently long scan durations (10-12 minutes)
- Focus on stronger functional connections, which demonstrate higher reliability
- Consider hemispheric differences; in aphasia, right hemisphere edges may show higher reliability than left hemisphere or inter-hemispheric connections [23]
FAQ 3: What is the impact of different statistical thresholds on ROI-based reliability?
Issue: The choice of statistical thresholds for defining functional ROIs is somewhat arbitrary and affects reliability metrics.
Solution: Using a predefined set of ROIs reduces the dependency on arbitrary statistical thresholds. The signal change across all voxels within a given ROI determines activity levels rather than threshold-dependent activation maps [67] [68].
Implementation Guide:
- Use anatomically-defined ROIs based on meta-analyses of language topology OR
- Employ functional ROIs derived from group activation patterns
- For subject-specific fROIs, define individual masks within group-constrained functional partitions [67] [68]
Table 1: Comparative Reliability of Different ROI Selection Approaches
| ROI Type | Population | Reliability Metric | Performance | Key Findings |
|---|---|---|---|---|
| Subject-specific fROIs [67] [68] | Healthy adults (n=24) | Effect size & test-retest reliability | Significantly larger effect sizes and higher reliability | More sensitive to individual functional anatomy; recommended for short scan protocols |
| Anatomical ROIs [67] [68] | Healthy adults (n=24) | Effect size & test-retest reliability | Lower effect sizes and reliability | Less sensitive to individual variability; better anatomical interpretability |
| Language Subnetworks [23] | Post-stroke aphasia (n=14) | Intraclass Correlation Coefficient (ICC) | Better reliability than whole-brain | Fair reliability at 10-12 min scan duration; affected by connection strength |
| Whole-Brain Networks [23] | Post-stroke aphasia (n=14) | Intraclass Correlation Coefficient (ICC) | Lower reliability than subnetworks | Fair median reliability; influenced by inter-node distance and hemisphere |
Table 2: Factors Influencing ROI Reliability Across Studies
| Factor | Effect on Reliability | Evidence |
|---|---|---|
| Scan Duration [23] | Positive association | Longer scans (10-12 min) provide fair reliability in aphasia |
| Connection Strength [23] | Positive association | Stronger edges show higher reliability in multiple connectivity types |
| Inter-node Distance [23] | Weak negative relationship | Shorter distances slightly associated with better reliability |
| Hemisphere [23] | Variable effects | Right hemisphere edges more reliable in post-stroke aphasia |
| Analysis Method [67] [68] | Significant impact | Subject-specific fROIs outperform anatomical ROIs |
| Data Amount [69] | Critical for rest | Resting-state has higher reliability at lower data amounts (<5 min) |
Experimental Protocols
Protocol 1: Subject-Specific Functional ROI Definition
Application: Language mapping for presurgical planning
Procedure:
- Participant Preparation: Screen for neurological conditions, medication use, and MRI contraindications
- Task Design: Implement block design with language tasks (e.g., sentence reading vs. nonword reading)
- Data Acquisition:
- Use 3T MRI scanner with standard parameters (TR=1500ms, TE=30ms, flip angle=72°)
- Acquire 235 volumes per run (~6 minutes)
- Include two sessions on different days with two runs per session
- ROI Definition:
- Create group-constrained functional partitions from healthy controls
- For each participant, define individual fROIs within these functional partitions
- Compare with anatomical ROIs from automated cortical parcellation
- Analysis:
- Preprocess with standard pipelines (motion correction, spatial smoothing, normalization)
- Calculate effect sizes and test-retest reliability for both ROI types
Protocol 2: Reliability Assessment in Clinical Populations
Based on: [23]
Application: Resting-state functional connectivity in post-stroke aphasia
Procedure:
- Participant Selection: Adults with chronic aphasia due to left-hemisphere stroke
- Scan Protocol:
- Acquire two resting-state fMRI scans several days apart (no intervention between)
- Use extended scan durations (10-12 minutes)
- ROI Strategy:
- Define whole-brain network and multiple cognitive/language subnetworks
- Assess edges (connections) within and between networks
- Reliability Analysis:
- Compute Intraclass Correlation Coefficients (ICCs) for every edge
- Calculate median ICCs for whole brain and subnetworks
- Examine relationships with connectivity strength, inter-node distance, and hemisphere
Methodological Workflows
Diagram 1: ROI selection methodology workflow
Diagram 2: Factors influencing ROI reliability
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Application | Specifications |
|---|---|---|
| 3T MRI Scanner [67] [68] | Data acquisition for functional imaging | Standardized parameters: TR=1500ms, TE=30ms, flip angle=72° |
| Language Paradigm Software [67] [68] | Stimulus presentation and response collection | Presentation Software, block design implementation |
| Cortical Parcellation Atlas [67] [68] | Anatomical ROI definition | Automated labeling (e.g., Destrieux atlas) |
| fMRI Processing Pipeline [67] [68] | Data preprocessing and analysis | FMRIB Software Library (FSL) with FEAT processing |
| Group Functional Templates [67] [68] | Subject-specific fROI definition | Predefined functional partitions from healthy controls |
| Reliability Analysis Tools [23] | Test-retest reliability quantification | Intraclass Correlation Coefficient (ICC) calculations |
What is within-subject variability in fMRI?
Within-subject variability refers to fluctuations in an individual's brain activity measurements across repeated fMRI scanning sessions. These fluctuations can be substantial, with studies showing individual activation levels can vary up to half the size of the group mean activation level, even when task performance and group-level activation patterns remain highly stable [70]. This variability presents a significant challenge for studies seeking to detect experimental effects across measurements or use fMRI for biomarker discovery.
Why is understanding state effects crucial for fMRI reliability?
The human brain is not a static system, and fMRI signals are markedly influenced by transient neural states that can change over minutes, hours, or days. Natural variations in arousal, perceptual state, attention, mind-wandering, and mood can substantially shape fMRI connectivity and activation measures [71]. These state-related neural influences introduce unwanted variance that can reduce the test-retest reliability of fMRI measurements if not properly accounted for in experimental design and analysis.
Troubleshooting Guides
FAQ: Addressing Common Experimental Challenges
Q1: Why do my fMRI results show poor test-retest reliability despite consistent task performance? Even with stable task performance, underlying neural processing can vary due to multiple state factors:
- Arousal fluctuations: Individuals can lose wakefulness within minutes of an fMRI scan, especially during resting-state paradigms [72]
- Carryover effects: Altered connectivity associated with task performance can persist post-task and affect subsequent measurements [71]
- Cognitive state variations: Natural fluctuations in attention, mind-wandering, and internal thought processes can modulate fMRI signals [71]
- Analytical choices: Using difference scores (contrasts) rather than β coefficients from GLM analyses can artificially reduce reliability estimates [18]
Q2: Which brain states most significantly impact fMRI reliability? Multiple interrelated states contribute to reliability challenges:
- Arousal/vigilance: Systematic differences in arousal levels occur across subjects and populations due to anxiety, sleep quality, and disease states [71]
- Autonomic state: Brain-body interactions and peripheral autonomic activity can influence BOLD responses [71] [73]
- Affective state: Anxiety and other emotional states produce widespread global effects on fMRI signals [73]
- Cognitive states: Attention, expectation, and task engagement vary within and across sessions
Q3: How can I distinguish state-related variability from trait measures in clinical populations?
- Collect state measures: Incorporate continuous monitoring (e.g., pupil diameter, heart rate) or experience sampling to gauge ongoing cognitive and affective processes [71]
- Use multivariate approaches: Pattern-based measures often show better reliability than univariate region-of-interest approaches [2]
- Control for global effects: The global mean fMRI signal contains valuable information about state and trait anxiety, rather than being merely a confound [73]
Q4: What practical steps can improve reliability in drug development studies?
- Standardize timing: Conduct scans at consistent times of day to minimize diurnal variations [71]
- Monitor state continuously: Implement pupillometry, heart rate monitoring, or experience sampling during scans [71]
- Pre-scan preparation: Standardize instructions regarding sleep, caffeine, and medication use prior to scanning
- Optimize tasks: Use engaging paradigms that maintain vigilance and minimize mind-wandering
Reliability Improvement Protocol
Table: Strategies to Mitigate Specific Sources of Variability
| Source of Variability | Impact on Reliability | Recommended Solutions |
|---|---|---|
| Vigilance/Arousal Fluctuations | Alters global signal amplitude and functional connectivity patterns [72] | Use engaging tasks; monitor with eyelid tracking or pupillometry; consider caffeine standardization [72] |
| Analytical Approach | Univariate measures show poor reliability (ICC=0.067-0.485) [7] | Use β coefficients instead of contrasts; employ multivariate pattern analysis [18] [2] |
| Cognitive/Affective State | Modulates network connectivity and activation strength [71] | Implement experience sampling; measure state anxiety; use tasks less susceptible to internal state |
| Brain-Body Interactions | Affects global signal via autonomic nervous system [71] [73] | Monitor heart rate and respiration; account for global signal in analyses [73] |
| Session Timing Effects | Introduces unwanted between-session variance [16] | Standardize inter-session intervals; shorter intervals (e.g., same-day) improve reliability [16] |
Experimental Protocols & Methodologies
Standardized Protocol for Controlling State Effects
Objective: To minimize the impact of state-related variability on fMRI measurements in longitudinal or clinical trials.
Pre-Scan Preparation:
- Participant Instructions: Standardize instructions regarding sleep (7-9 hours), caffeine/alcohol consumption (abstain 12 hours), and medication use prior to scanning
- State Assessment: Administer brief questionnaires for anxiety (State-Trait Anxiety Inventory), sleep quality (Pittsburgh Sleep Quality Index), and current alertness
- Habituation: Allow 10-15 minutes for scanner habituation while explaining procedures to reduce anxiety
During-Scan Monitoring:
- Vigilance Tracking: Implement eye-tracking for percent eyelid closure as a proxy for vigilance [72]
- Physiological Monitoring: Record heart rate and respiration for brain-body interaction assessments [73]
- Task Design: Incorporate engaging tasks with performance metrics to maintain consistent cognitive engagement
Data Acquisition Parameters:
- Sequence Optimization: Use standardized sequences with minimal noise characteristics
- Session Timing: Conduct repeat scans at consistent times of day to control for diurnal variations [71]
- Adequate Sampling: Acquire sufficient data per participant (≥15-20 minutes) to improve reliability [2]
Analytical Framework for State-Related Variance
Table: Analytical Approaches for Improving Reliability
| Methodological Challenge | Traditional Approach | Recommended Improvement | Expected Benefit |
|---|---|---|---|
| Measuring Neural Activation | Use task contrasts (Condition A - Condition B) | Use β coefficients from first-level GLM | Higher ICC values due to greater between-subject variance [18] |
| Accounting for Global Signal | Global signal regression as standard confound removal | Treat global signal as potential source of information; use partial correlation approaches | Retains valuable state-related information; improves anxiety biomarker detection [73] |
| Functional Connectivity Estimation | Static connectivity measures across entire scan | Dynamic connectivity with state-based stratification; frame-wise vigilance estimation | Reduces contamination from vigilance fluctuations; improves reliability [71] [72] |
| Individual Differences Measurement | Univariate region-of-interest approaches | Multivariate pattern analysis; machine learning classifiers | Good-to-excellent reliability (Spearman-Brown rs = 0.73-0.82) [2] |
Visual Guide to State Effects
Relationship Between Factors Affecting fMRI Reliability
Factors Influencing fMRI Reliability
Experimental Workflow for Controlling State Effects
Workflow for Controlling State Effects
The Scientist's Toolkit
Table: Key Reagents and Tools for State-Effects Research
| Tool Category | Specific Examples | Primary Function | Considerations for Use |
|---|---|---|---|
| Vigilance Monitoring | Eye-tracking (% eyelid closure), EEG-based metrics (α/θ ratio), Pupillometry | Quantify arousal fluctuations during scanning | Eye-tracking compatible with MRI; EEG requires specialized equipment; pupillometry affected by lighting [72] |
| Physiological Recording | Heart rate monitoring, Respiration belts, Skin conductance | Capture brain-body interactions and autonomic state | Standard MRI-compatible physiological monitoring systems; sync with fMRI acquisition [71] [73] |
| State Assessment Tools | State-Trait Anxiety Inventory (STAI), Profile of Mood States (POMS), Visual Analog Scales (VAS) | Measure pre-scan and post-scan subjective state | Brief forms preferable; administer immediately before/after scanning; consider computerized adaptation |
| Analytical Software | FIRMM (Framework for Integrated MRI Monitoring), FSL, SPM, AFNI, Connectome Workbench | Real-time monitoring and state-informed processing | FIRMM provides real-time motion and data quality metrics; standard packages offer preprocessing pipelines |
| Multivariate Analysis Tools | Pattern classification algorithms, Machine learning toolkits (scikit-learn, PRONTO) | Improve reliability through multivariate approaches | Requires programming expertise; cross-validation essential; larger sample sizes beneficial [2] |
| Global Signal Methods | Global signal regression, Global signal as covariate, Partial correlation approaches | Account for widespread state-related signal changes | Decision has theoretical implications; global signal may contain valuable clinical information [73] |
Quantitative Reference Guide
Reliability Benchmarks Across Methodological Approaches
Table: Comparative Reliability of Different fMRI Measures
| fMRI Measure Type | Typical ICC Range | Key Influencing Factors | Recommended Applications |
|---|---|---|---|
| Univariate Task Activation | 0.067 - 0.485 [7] | Brain region, task design, contrast vs. β coefficients [18] | Group-level analyses; hypothesis generation |
| Resting-State Functional Connectivity | 0.2 - 0.6 [16] | Scan length, vigilance control, global signal regression [71] | Group comparisons; network identification |
| Multivariate Pattern Measures | 0.73 - 0.82 [2] | Sample size, feature selection, cross-validation | Biomarker development; individual differences |
| Structural MRI Measures | 0.7 - 0.9 [16] | Sequence parameters, processing pipeline | Longitudinal studies; individual tracking |
| β Coefficients (vs. Contrasts) | Significantly higher than contrasts [18] | Between-subject variance, GLM specification | Individual differences research; clinical applications |
Sample Size Implications for Reliable Detection
Table: Impact of Within-Subject Variation on Study Design
| Within-Subject Variation Level | Small Effect Size | Medium Effect Size | Large Effect Size |
|---|---|---|---|
| Low Stability (High σw) | N > 50 | N = 25-35 | N = 15-20 |
| Medium Stability | N = 30-40 | N = 15-25 | N = 10-15 |
| High Stability (Low σw) | N = 20-30 | N = 10-15 | N < 10 |
Note: σw refers to within-subject standard deviation of BOLD signal changes. Sample sizes estimated for 80% power in repeated-measures designs [70].
Frequently Asked Questions
FAQ: What is the minimum recommended fMRI scan duration for reliable individual-level prediction? For most brain-wide association studies, scan times of at least 20 minutes are recommended. While sample size and scan time are initially interchangeable for achieving prediction accuracy, 30-minute scans are typically the most cost-effective, yielding up to 22% cost savings compared to 10-minute scans [3].
FAQ: Why is test-retest reliability rarely reported in fMRI depression studies? Many fMRI studies for clinical prediction or treatment in Major Depressive Disorder (MDD) rarely mention reliability metrics. One possible reason is that reported reliability is often below acceptable thresholds (with ICCs around 0.50, which is below "good" reliability thresholds), making researchers hesitant to report it [61].
FAQ: How can I improve the test-retest reliability of my fMRI data?
- Optimize BOLD signal parameterization by evaluating indices like average amplitude and timing/shape of the BOLD response curve in addition to its canonical amplitude [61]
- Examine voxel-wise reliability within ROIs by reporting median voxelwise ICCs within regions of interest [61]
- Account for individual and clinical features such as state anxiety and rumination which can affect neural activation [61]
- Test reliability in relevant clinical populations rather than only healthy controls [61]
FAQ: What quality checks should I perform on raw fMRI data? Always inspect both anatomical and functional images for problems like scanner spikes, incorrect orientation, poor contrast, or excessive motion. For functional images, check for sudden jerky movements by viewing the time-series as a movie, and watch for distortions in areas like the orbitofrontal cortex [74].
fMRI Scan Duration vs. Prediction Accuracy
| Scan Duration | Prediction Accuracy | Cost Efficiency | Recommended Use Cases |
|---|---|---|---|
| ≤10 minutes | Lower accuracy | 22% less cost-effective than 30min | Pilot studies, limited budgets |
| 20 minutes | Linear increase with log total duration | Good balance | Initial BWAS, large samples |
| 30 minutes | High accuracy | Most cost-effective | Optimal for most scenarios |
| >30 minutes | Diminishing returns | Cheaper to overshoot than undershoot | Subcortical-to-whole-brain BWAS |
Test-Retest Reliability Classifications (ICC Metrics)
| ICC Value Range | Reliability Classification | Typical fMRI Performance |
|---|---|---|
| <0.40 | Poor | Often found in regional fMRI activity |
| 0.40-0.59 | Fair | Lower end of reported range |
| 0.60-0.74 | Good | Upper end of reported range |
| >0.75 | Excellent | Rarely achieved in fMRI studies |
Experimental Protocols & Methodologies
Optimizing Test-Retest Reliability in fMRI
Principle R1: Optimize Indices of Task-Related Reactivity
- Evaluate BOLD response using gamma variate models that yield parameters for onset, rise and fall slopes, and magnitude of hemodynamic responses
- Include temporal and dispersion derivatives to account for individual differences in peak response timing and HRF length
- Use alternate parameterization methods including canonical amplitude, area under the curve (via Finite Impulse Response basis), and peak amplitude [61]
Principle R2: Voxel-Wise Reliability Examination
- Compute median voxelwise ICCs within regions of interest
- Create indices that inherit solely from reliable voxels to increase psychometric properties
- Identify and promote regions or voxels with stronger psychometric properties [61]
Principle R3: Account for Individual and Clinical Features
- Control time-varying noise sources through experimental design (instrumentation, time of day, motion, instructions, practice effects)
- Statistically control for clinical features like state anxiety and rumination that account for neural activation
- Account for within-individual changes in symptomatology across time [61]
Principle R4: Examine Reliability in Relevant Populations
- Test reliability in treatment-seeking patients rather than only healthy controls
- Use paradigms that address clinical phenomenology that may be reliable in clinical populations but not controls
- Consider that heterogeneous samples can produce different ICCs even with same within-subject reliability [61]
Data Quality Assessment Protocol
Anatomical Image Inspection [74]
- Check for ripples indicating excessive subject motion
- Identify abnormal intensity differences within grey or white matter that may indicate pathologies
- Report artifacts according to laboratory protocols
Functional Image Inspection [74]
- Check for extremely bright or dark spots in grey or white matter
- Identify image distortions like abnormal stretching or warping
- Quantify motion by viewing time-series as a movie to detect sudden jerky movements
Experimental Workflows
fMRI Data Processing Workflow
The Scientist's Toolkit: Research Reagent Solutions
| Tool/Resource | Function | Application Context |
|---|---|---|
| ICC (Intraclass Correlation) | Indexes test-retest reliability through rank ordering of values across days [61] | Standard metric for fMRI reliability assessment |
| BIDS (Brain Imaging Data Structure) | Standardized file organization and nomenclature system for neuroimaging data [74] [75] | Data sharing across labs and software platforms |
| Voxel-Wise Reliability Analysis | Identifies reliable voxels within ROIs by calculating median ICC values [61] | Improving psychometric properties of fMRI measures |
| Gamma Variate Models | Parameterizes BOLD response with onset, rise/fall slopes, and magnitude parameters [61] | Accounting for individual differences in hemodynamic responses |
| Finite Impulse Response (FIR) | Models BOLD response via multiple regression of delta functions across TRs [61] | Calculating area under curve and peak amplitude |
| FSL/Fsleyes | FSL's image viewer for inspecting anatomical and functional images [74] | Quality checking raw fMRI data for artifacts and motion |
| Reliability Toolbox | Add-on package for SPM that computes ICC metrics [61] | Calculating test-retest reliability for fMRI data |
Multivariate Approaches vs. Univariate Methods for Improved Reliability
Frequently Asked Questions (FAQs)
Q1: What is the fundamental difference between univariate and multivariate functional connectivity?
A: Univariate functional connectivity is calculated by first averaging the timecourses of all voxels within a brain region to create a single representative signal, and then computing the correlation (typically using Pearson's correlation) between these averaged signals from different regions. In contrast, multivariate functional connectivity (measured with methods like multivariate distance correlation) analyzes the relationships between the full, voxel-wise timecourses from two regions without averaging them first. This approach preserves the spatial patterns of activity within each node, capturing more complex dependencies and resulting in higher test-retest reliability and stronger behavioral predictions [76] [77].
Q2: My fMRI data is limited to short scan times. How can I improve reliability?
A: For studies with very short scan times (e.g., under 5 minutes), resting-state data may initially show higher reliability [69]. However, you can adopt several strategies to enhance reliability:
- Use Multivariate Methods: Switching from univariate to multivariate connectivity measures can boost reliability even with shorter datasets [76] [77].
- Employ Subject-Specific Functional ROIs: Defining regions of interest (ROIs) based on individual functional localizers significantly increases effect sizes and reliability compared to using standardized anatomical atlases, which is particularly beneficial for short paradigms common in clinical settings [67].
- Consider Movie-Watching Paradigms: For slightly longer acquisitions, movie-watching fMRI can improve data quality by reducing head motion and drowsiness, and often enhances the ability to discriminate between individuals [69].
Q3: How does scan duration affect the prediction of individual behaviors or traits?
A: Prediction accuracy for individual traits increases with the total scan duration, which is the product of the number of participants and the scan time per participant. Initially, sample size and scan time are somewhat interchangeable. However, a key study found diminishing returns for scan times beyond 20-30 minutes. For optimal cost-effectiveness in brain-wide association studies, the evidence suggests that scan times of at least 30 minutes are most recommended [3]. The relationship between total scan duration and prediction accuracy follows a logarithmic pattern, meaning gains in accuracy become progressively smaller with each additional minute of scanning [3].
A: Multicenter studies face a hierarchy of functional connectivity variations. From largest to smallest median magnitude, these are:
- Within-Subject, Across-Run Variation: The variability in a single participant's connectivity across different scanning sessions.
- Individual Differences: Variation between different participants.
- Disorder-Related Effects: Changes in connectivity associated with a clinical condition.
- Scanner and Protocol Differences: Technical variations introduced by different MRI machines or imaging parameters [5]. Machine learning algorithms, particularly ensemble sparse classifiers, can help manage this variability by prioritizing disease-related effects and suppressing irrelevant individual and within-subject variations [5].
Troubleshooting Guides
Problem: Low Test-Retest Reliability of Functional Connectivity Measures
Symptoms: High variability in connectivity values for the same subject across repeated scans, poor fingerprinting accuracy, weak correlation between brain features and behavioral measures.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Insufficient Scan Time | Check the length of your functional runs. If under 10 minutes, this is a likely contributor. | Aim for longer scan times. For prediction tasks, ~30 minutes per participant is optimal for cost-effective accuracy [3]. If long scans are impossible, use multivariate methods to maximize signal from shorter data [77]. |
| Suboptimal Acquisition State | Determine if participants were at rest. High mind-wandering or drowsiness can increase within-subject variance. | Consider using a movie-watching paradigm. It constrains cognition, reduces head motion, and can enhance the discriminability of individual connectomes, especially in visual and temporal brain regions [69]. |
| Use of Anatomical ROIs | Check if your analysis uses a standardized anatomical atlas on data with individual anatomical variability. | Switch to subject-specific functional ROIs (fROIs). This method defines ROIs based on individual functional localizer scans, improving sensitivity and reliability [67]. |
| Outdated Univariate Connectivity Metric | Review your analysis pipeline for the use of simple Pearson's correlation between averaged regional timecourses. | Adopt a multivariate connectivity measure like Multivariate Distance Correlation. It captures richer, within-region information and demonstrates higher edge-level and connectome-level reliability [76] [77]. |
Problem: Poor Individual-Level Phenotypic Prediction
Symptoms: Machine learning models fail to predict cognitive scores or clinical status from connectome data with meaningful accuracy.
| Possible Cause | Diagnostic Steps | Solution |
|---|---|---|
| Underpowered Study Design | Evaluate your total scan duration (Sample Size × Scan Time per Participant). Compare it to established benchmarks [3]. | Increase the total scan duration. The logarithmic model shows prediction accuracy is strongly tied to this product (R² = 0.89) [3]. Prioritize increasing sample size if scan time is already ≥30 minutes. |
| High Uncontrolled Variability | Analyze the variance components in your data, especially from multicenter designs. | Apply ensemble sparse classifiers in your machine learning pipeline. These methods are designed to suppress non-disease-related variations (individual differences, scanner effects) and amplify the disorder-related signal [5]. |
| Low Discriminability of Connectomes | Perform a connectome fingerprinting analysis. Low accuracy indicates poor separation of individuals. | Use multivariate connectivity for fingerprinting. It improves the unique identification of individuals from their brain data, which is foundational for predicting individual traits [77]. |
Experimental Protocols & Workflows
Protocol 1: Calculating Multivariate Functional Connectivity
This protocol details the steps to compute multivariate functional connectivity using Multivariate Distance Correlation, an approach proven to enhance reliability [77].
Key Research Reagents & Solutions
| Item | Function & Brief Description |
|---|---|
| Preprocessed fMRI Data | Cleaned BOLD time series data, with artifacts and noise removed. This is the fundamental input for all connectivity analysis. |
| Brain Parcellation Atlas | A map dividing the brain into distinct regions (e.g., Glasser's MMP). Provides the nodes for network analysis. |
| Multivariate Distance Correlation Algorithm | A statistical software script/package that calculates the multivariate dependency between all voxel timecourses in two regions, without averaging. |
| High-Performance Computing Cluster | Computational resources for handling the intensive calculations of voxel-wise connectivity matrices. |
Step-by-Step Methodology:
- Data Preparation: Start with preprocessed fMRI data (e.g., from FSL or HCP pipelines), which includes motion correction, slice-timing correction, and regression of nuisance signals (white matter, CSF, motion parameters) [77].
- Extract Voxel-wise Timecourses: For each brain region defined by your chosen atlas, extract the full, un-averaged timecourse for every voxel within its boundaries.
- Compute Pairwise Connectivity: For every pair of brain regions (A and B), compute the multivariate distance correlation. This metric assesses the dependency between the multivariate set of voxel timecourses in Region A and the set in Region B.
- Build Connectivity Matrices: Assemble the results into a symmetric connectivity matrix where each element represents the multivariate connectivity strength between two regions.
- Validation: Assess the reliability of the resulting matrices using test-retest intraclass correlation (ICC) or connectome fingerprinting and compare against univariate methods [77].
Protocol 2: Implementing a Movie-watching fMRI Paradigm
This protocol outlines how to set up a movie-fMRI acquisition to improve data quality and individual discriminability [69].
Step-by-Step Methodology:
- Stimulus Selection: Choose engaging movie clips with continuous narrative or semantic content. Note that high identification accuracies have been found even when different movies are used across scans [69].
- Presentation Setup: Use presentation software (e.g., Presentation, PsychoPy) to display the movie on a screen visible to the participant via a mirror on the head coil.
- Data Acquisition: Acquire fMRI data using standard BOLD imaging sequences. The naturalistic stimulus helps maintain alertness and reduce head motion, particularly in challenging populations [69].
- Preprocessing: Apply standard fMRI preprocessing. Additionally, you may model the movie stimulus timing as a regressor of no interest if the goal is to isolate intrinsic connectivity rather than stimulus-evoked activity.
- Analysis for Discriminability: Calculate functional connectivity matrices (preferably using multivariate methods) during the movie-watching state. Apply a connectome fingerprinting algorithm to test the accuracy of identifying individuals across scanning sessions [69].
Visualized Workflows & Pathways
Analytical Workflow: Univariate vs. Multivariate Connectivity
The diagram below illustrates the key procedural differences between univariate and multivariate functional connectivity analysis, highlighting where multivariate methods capture additional information.
Factors Affecting Functional Connectivity Reliability
This diagram outlines the hierarchy of factors that contribute to variability in functional connectivity measurements, particularly in multicenter studies.
Validation Frameworks and Comparative Reliability Across fMRI Modalities
Troubleshooting Guides
FAQ 1: Which fMRI paradigm provides more reliable functional connectivity for predicting individual behavioral differences?
Answer: Evidence indicates that task-based functional connectivity (FC) often demonstrates superior reliability and greater power for predicting individual behavioral differences compared to resting-state FC.
- Underlying Cause: The cognitive engagement during a task can elicit more consistent and robust brain network configurations. The FC associated with the task model fit (the part of the brain's activity time course directly explained by the task design) is a key driver of this improved reliability and behavioral prediction [78].
- Solution: When the research goal involves linking brain connectivity to individual differences in behavior or cognition, incorporating task-based fMRI paradigms is recommended. The choice of task should be content-specific, meaning it should probe cognitive constructs similar to the behavior you aim to predict [78].
FAQ 2: How does scan length impact the test-retest reliability of resting-state functional connectivity?
Answer: The reliability of resting-state functional connectivity is significantly influenced by scan length, with longer scans generally yielding higher reliability, though with diminishing returns.
- Underlying Cause: FC metrics are calculated from correlation statistics, which become more accurate and stable with an increasing number of data points (longer time series) [25] [79].
- Solution:
- Minimum Duration: Aim for a minimum of 10-13 minutes of resting-state data to achieve good intra-session reliability [79].
- Diminishing Returns: Gains in reliability across different sessions (intersession reliability) tend to diminish after about 9-12 minutes [79].
- Practical Balance: While longer scans are better, you must balance the gain in reliability against practical constraints like participant fatigue, which can increase head motion [25].
FAQ 3: What are common physiological confounds that reduce fMRI reliability, and how can they be mitigated?
Answer: Participant states such as sleep/drowsiness and uncontrolled head motion are major sources of noise that reduce the test-retest reliability of fMRI metrics.
- Underlying Cause: The unconstrained nature of the resting state makes it vulnerable to drowsiness, which alters functional connectivity patterns [64]. Head motion introduces systematic artifacts that can inflate or distort connectivity measures [25] [64].
- Solution:
- Combatting Sleep: Monitor alertness using physiological measures like heart rate variability (HRV) during the scan. Excluding data segments marked as "sleepy" can significantly improve reliability [64].
- Reducing Motion: Use tasks to increase participant engagement and reduce head motion compared to rest [25]. Implement rigorous motion correction during data preprocessing and regress out motion parameters [64].
Experimental Protocols & Methodologies
This section provides detailed methodologies from key studies cited in this guide, serving as a reference for robust experimental design.
Protocol 1: Dense Sampling for FC Reliability Analysis
- Source: Midnight Scan Club (MSC) Dataset [25]
- Objective: To investigate regional effects of tasks on FC reliability with high precision.
- Participants: 10 healthy adults.
- Design:
- Each participant completed 12 separate scanning sessions.
- Acquired approximately 5 hours of resting-state fMRI and 6 hours of task fMRI data per subject.
- Tasks were designed to engage specific cognitive systems.
- Analysis: FC reliability was quantified using test-retest correlation (split-half) and intraclass correlation. Signal properties like temporal standard deviation (tSD) were analyzed for their relationship with reliability.
Protocol 2: Optimizing Resting-State Scan Length and Condition
- Source: [79] [80]
- Objective: To determine the effect of scan length and resting instruction on reliability.
- Participants: 25 healthy adults.
- Design:
- Participants were scanned at three time points (two same-day, one ~3 months later).
- At each session, three 10-minute resting-state scans were acquired under different instructions: Eyes Closed (EC), Eyes Open (EO), and Eyes Fixated on a cross (EF).
- Data from these scans were concatenated to create time series of varying lengths (3 to 27 minutes) for analysis.
- Analysis: Intraclass correlation (ICC) was used to assess test-retest reliability for different scan lengths and conditions across major brain networks.
Protocol 3: Isolating Task-Related Connectivity for Behavioral Prediction
- Source: [78]
- Objective: To test whether the improvement in behavioral prediction from task-based FC is driven by the task design itself.
- Data: Used data from the Adolescent Brain Cognitive Development (ABCD) Study, including resting-state fMRI and three task fMRI paradigms.
- Analysis:
- For each task, the fMRI time course was decomposed using a general linear model (GLM) into:
- Task Model Fit: The fitted time course based on task condition regressors.
- Task Model Residual: The remaining signal not explained by the task.
- Functional connectivity was computed for the original time course, the task model fit, and the residual.
- The power of these FC matrices to predict behavioral measures was compared against resting-state FC.
- For each task, the fMRI time course was decomposed using a general linear model (GLM) into:
The following tables summarize key quantitative findings on fMRI reliability from the search results.
Table 1: Impact of Scan Length on Resting-State FC Reliability (ICC) [79]
| Scan Length | Intrasession Reliability | Intersession Reliability |
|---|---|---|
| 5 minutes | Moderate | Moderate |
| 9-12 minutes | High (Plateau) | High (Peak) |
| 12-16 minutes | High (Plateau) | Diminishing |
| >27 minutes | No major gain | No major gain |
Note: ICC, Intraclass Correlation Coefficient. Intrasession: reliability within the same scanning session. Intersession: reliability across sessions separated by days or months.
Table 2: Comparative Reliability of fMRI Paradigms and Factors
| Paradigm / Factor | Key Reliability Finding | Primary Reference |
|---|---|---|
| Task vs. Rest | Tasks enhance FC reliability and signal variability in task-engaged regions, but can dampen it elsewhere. | [25] |
| Behavioral Prediction | FC from the task model fit outperforms resting-state FC in predicting individual cognitive performance. | [78] |
| Resting Condition | Eyes fixated (EF) showed significantly greater reliability for DMN and attention networks than eyes closed (EC). | [80] |
| Signal Property | Temporal Standard Deviation (tSD) is a strong, positive driver of FC reliability. | [25] |
Experimental Workflow & Signaling Pathways
The following diagram illustrates the core decision-making workflow for optimizing fMRI reliability based on research objectives, integrating factors like paradigm choice, scan length, and physiological monitoring.
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 3: Key Resources for fMRI Reliability Research
| Item | Function in Research | Example/Note |
|---|---|---|
| High-Density Datasets | Provide extensive data per subject for precise reliability estimation and novel analysis. | Midnight Scan Club (MSC) [25]; Human Connectome Project (HCP) [81] |
| Task Paradigms | Engage specific cognitive systems to elicit robust and behaviorally relevant network states. | Working Memory, Inhibitory Control (e.g., Go/No-Go), Sensory Tasks [25] [78] |
| Physiological Monitors | Record data to identify and remove confounding physiological noise. | ECG for Heart Rate Variability (sleep detection) [64]; Pulse Oximeter, Respiratory Belt |
| Advanced Analysis Tools | Decompose fMRI signals and compute reliability metrics. | General Linear Model (GLM) [78]; Dictionary Learning/Sparse Representation [81]; Intraclass Correlation (ICC) [25] [79] [80] |
| Motion Correction Software | Identify and correct for head motion artifacts in fMRI time series. | Volume registration tools (e.g., in AFNI, FSL) [79] [80] |
FAQs on Reliability in Clinical vs. Healthy Cohorts
Q1: Why might the test-retest reliability of an fMRI measure differ between a patient population and a healthy control group?
Reliability can differ due to several key factors:
- Between-Subject Variability: The Intraclass Correlation Coefficient (ICC), a standard metric for reliability, is proportional to between-subject variability. Clinical populations often show greater heterogeneity in brain responses compared to the more homogeneous responses typically found in healthy, young control groups. This increased variability in a clinical sample can lead to higher ICC estimates, even if the within-subject reliability is similar [61].
- State-Dependent Fluctuations: Patients with disorders like major depression may experience within-individual changes in symptomatology (e.g., state anxiety, rumination) across scanning sessions. These clinical state fluctuations can introduce additional within-subject variance that is not typically present in stable control participants, potentially reducing reliability if not accounted for [61].
- Task Relevance: Paradigms designed to probe processes central to a clinical disorder (e.g., emotion regulation in depression) may engage neural circuits more consistently and reliably in the patient population for whom the process is salient, compared to healthy controls [61] [82].
Q2: What analytical choices can improve the reliability of task-fMRI in clinical studies?
- Use Beta Coefficients over Contrasts: Calculating ICCs using β coefficients from a first-level general linear model (GLM) provides a more direct measure of functional activation and often yields higher reliability than using difference scores (contrasts). Contrasts can have low between-subject variance and high error, leading to underestimation of true reliability [18].
- Optimize the BOLD Signal Model: Instead of relying solely on a canonical hemodynamic response function (HRF), using models that account for individual differences in timing and shape, such as a gamma variate model or Finite Impulse Response (FIR) models, can reduce noise and improve reliability estimates [61].
- Focus on Significantly Activated Voxels: Within a pre-defined Region of Interest (ROI), creating an index based only on voxels that show significant task-related activation at the group level, rather than all voxels in the anatomical parcel, can yield higher reliability [44].
Q3: Which brain regions often show sufficiently high reliability for use in clinical biomarker studies?
While reliability is task- and population-dependent, some regions consistently show fair-to-good reliability, particularly in cortical areas. Core regions within well-defined networks are often strong candidates [44] [82].
- High-Reliability Regions: The left anterior insula (during decision-making), the right caudate (during outcome processing), and regions in the dorsolateral and ventrolateral prefrontal cortex (during emotion regulation) have been reported to show good reliability (ICCs > 0.5) [44] [82].
- General Trend: Cortical regions typically demonstrate higher test-retest reliability than subcortical regions [18].
Quantitative Data on fMRI Reliability
The following tables summarize key quantitative findings on fMRI reliability from the literature, highlighting the range of ICC values you might expect and how they are influenced by various factors.
Table 1: Summary of Reported Test-Retest Reliability (ICC) Across fMRI Modalities
| fMRI Modality | Typical ICC Range | Reported Mean ICC | Key Findings |
|---|---|---|---|
| Task-based fMRI | Poor to Good (0.0 - 0.8) [44] | ~0.50 regionally [61] | Reliability is highly region- and task-specific. Parietal, occipital, and temporal regions often show higher reliability [44]. |
| Resting-State Functional Connectivity (Edge-Level) | Poor [6] | 0.29 (95% CI: 0.23 - 0.36) [6] | Stronger, within-network, cortical connections are more reliable. Shorter test-retest intervals improve reliability [6]. |
| Amplitude of Low-Frequency Fluctuations (ALFF) | Moderate [83] | 0.68 (for between-subject differences) [83] | Achieves moderate test-retest reliability but replicability across independent datasets can be low [83]. |
Table 2: Impact of Experimental and Analytical Factors on Reliability
| Factor | Impact on Reliability | Evidence |
|---|---|---|
| Sample Characteristics | Higher between-subject variability in clinical cohorts can increase ICC. | Heterogeneous clinical samples can produce different ICCs than healthy controls, even with the same within-subject reliability [61]. |
| Individual-Level Data | Increasing scan time per subject markedly improves replicability. | Adding individual-level data (e.g., from 10 to ~40 mins) improved peak replicability from ~30% to over 90% for some contrasts, even with modest sample sizes (n=23) [84]. |
| Analytical Measure | Using β coefficients yields higher ICCs than contrast scores. | ICC values were consistently higher when calculated from β coefficients compared to task contrasts in an emotion processing task [18]. |
| Region Definition | Using only significant voxels within an ROI improves reliability. | ROIs defined by significantly activated vertices showed greater reliabilities than those defined by a whole anatomical parcel [44]. |
Experimental Protocol for Assessing Reliability in Clinical Cohorts
This section provides a detailed methodological guide for a study designed to evaluate the test-retest reliability of a task-based fMRI measure in a clinical population compared to healthy controls.
Objective: To determine and compare the test-retest reliability of neural activity in pre-specified regions of interest (ROIs) during a clinically-relevant task in individuals with Major Depressive Disorder (MDD) and a matched healthy control (HC) group.
Population & Design:
- Participants: Recruit two groups: a treatment-seeking MDD group and a demographically-matched HC group. Aim for a sample size of at least 20-25 per group, based on data suggesting this is a minimum for reliable estimates with sufficient individual-level data [84].
- Study Design: A longitudinal design with two scanning sessions. For the MDD group, the test-retest interval should be short (e.g., 1-2 weeks) to minimize the impact of symptomatic fluctuation, yet long enough to avoid habituation. For HCs, a similar interval is acceptable. Collect at least 40 minutes of task data per participant across the sessions to ensure sufficient individual-level data [84].
fMRI Acquisition & Task:
- Scanner Parameters: Use a multiband acquisition sequence (e.g., MB factor 4) to improve temporal resolution and signal-to-noise ratio, which has been associated with higher test-retest reliability for cortical measures [85].
- Task Paradigm: Employ a well-established, slow event-related task that robustly engages the neural circuitry relevant to the clinical population (e.g., an emotional word labeling task for depression) [61].
Data Analysis Workflow: The following diagram outlines the core analytical pipeline for assessing reliability.
Calculating Reliability:
- Parameter Estimation: For each participant and session, model the BOLD response using a flexible model (e.g., Gamma variate function or FIR) to optimize the signal estimate [61]. Extract the parameter of interest (e.g., peak amplitude, area under the curve) for each pre-defined ROI.
- Intraclass Correlation Coefficient (ICC): Calculate the voxel-wise ICC(3,1) for each ROI within each group (MDD and HC) separately. The ICC(3,1) is a common choice that assumes the same scanner is used across sessions [61] [44]. Report the median voxel-wise ICC within each ROI [61].
- Statistical Comparison: Formally compare the median ICC values for each ROI between the MDD and HC groups using appropriate statistical tests (e.g., permutation tests) to determine if reliability is significantly different.
The Scientist's Toolkit: Key Reagents & Materials
Table 3: Essential Resources for fMRI Reliability Research
| Item / Resource | Function / Purpose | Example / Note |
|---|---|---|
| Reliability Toolbox | Software to compute psychometric metrics like ICC for fMRI data. | The "reliability toolbox" for SPM allows computation of ICC metrics not natively supported by main software packages [61]. |
| Flexible Basis Functions | To model the BOLD response more accurately at the individual level. | Gamma variate models or the use of temporal and dispersion derivatives in AFNI's 3dDeconvolve or SPM can account for individual differences in HRF timing and shape [61]. |
| Validated Clinical Task | A task paradigm known to engage neural circuits relevant to the clinical disorder. | For depression, an emotional word labeling or face-matching task can be used to probe amygdala and prefrontal reactivity [61]. |
| Multiband fMRI Sequence | Accelerates data acquisition, improving temporal resolution and coverage. | A multiband factor of 4 (with or without in-plane acceleration) has been shown to provide high test-retest reliability for cortical networks [85]. |
| High-Quality T1-Weighted Image | For accurate anatomical reference and spatial normalization. | A magnetization-prepared rapid acquisition gradient echo (MPRAGE) sequence is standard for detailed structural imaging. |
FAQs on Multiverse Analysis in fMRI Research
Q1: What is a multiverse analysis and why is it important for fMRI reliability? A multiverse analysis involves systematically testing research questions across the vast set of all plausible, defensible data preprocessing and analysis pipelines [86]. This approach is crucial for fMRI test-retest reliability research because it directly addresses the "replication crisis" in neuroimaging by quantifying how variable analytical choices impact results. It moves beyond a single analysis path to examine the robustness of findings across many potential methodological decisions [86] [87].
Q2: What is the typical scope of analytical variability in graph-based fMRI analysis? In graph-based fMRI analysis alone, researchers have identified 61 distinct analytical steps, 17 of which involve debatable parameter choices [86]. The three primary levels of analytical flexibility are:
- Inclusion/Exclusion of specific processing steps
- Parameter Tuning within each step
- Sequencing of the analytical steps [86]
Q3: Which preprocessing steps are particularly controversial in fMRI pipelines? Among the most contentious preprocessing steps are scrubbing (removing motion-corrupted volumes), global signal regression, and spatial smoothing [86]. Each of these decisions can significantly impact final results and requires careful consideration in multiverse frameworks.
Q4: How can multiverse analysis benefit fMRI in drug development? Implementing multiverse approaches can enhance the utility of fMRI in drug development by providing a more comprehensive understanding of a pharmacological agent's effects across multiple analysis pipelines [13]. This is particularly valuable for establishing dose-response relationships and demonstrating normalization of disease-related fMRI signals, which are important for regulatory submissions [13].
Troubleshooting Guides for Multiverse Experiments
Problem: Inconsistent Results Across Pipelines
Symptoms: Large variations in effect sizes or statistical significance when different defensible pipelines are applied to the same dataset.
Solutions:
- Implement Systematic Pipeline Documentation: Create a detailed decision tree mapping all possible analytical choices. Studies have shown that flexible analytical pipelines can produce inconsistent results [87].
- Increase Sample Size: Evidence suggests that thousands of subjects may be needed to achieve reproducible brain-behavior associations with univariate approaches [87]. For multivariate prediction algorithms, samples as small as 100 subjects may produce replicable results [87].
- Apply Multivariate Methods: Use multivariate approaches like Connectome-Based Predictive Modeling (CPM), which have shown success in explaining individual differences among adolescents in substance use studies [87].
Problem: Excessive Computational Demands
Symptoms: Multiverse analyses becoming computationally prohibitive due to the combinatorial explosion of pipeline options.
Solutions:
- Strategic Sampling of Pipeline Space: Rather than testing all possible combinations, prioritize testing the most defensible and commonly used parameter settings based on systematic reviews of the literature [86].
- Leverage High-Performance Computing: Implement distributed computing approaches to parallelize pipeline executions.
- Utilize Interactive Tools: Use decision support applications like METEOR (developed for graph-fMRI analysis) which provide educational value and facilitate access to design well-informed robustness analyses [86].
Problem: Head Motion Artifacts in Developmental or Clinical Populations
Symptoms: Motion-related contaminants disproportionately affecting data quality, particularly challenging in developmental studies or populations with movement disorders.
Solutions:
- Implement Robust Motion Correction: Apply standard rigid-body transformation methods (three directions of translation and three axes of rotation) with a single functional volume as reference [38].
- Incorporate Prospective Correction: Use navigator echoes and real-time motion correction during data acquisition when possible [38].
- Apply Data Scrubbing Strategically: Identify and remove motion-corrupted volumes using graphical and semi-automated methods to identify outlier data [38], while testing the impact of different scrubbing thresholds in your multiverse framework.
Problem: Low Temporal Signal-to-Noise Ratio (tSNR)
Symptoms: Poor quality data limiting detection of true effects across all pipeline variants.
Solutions:
- Implement Multi-echo fMRI Acquisition: Acquire several echoes after a single excitation to enable calculation of T2* and combination of echoes to enhance BOLD contrast sensitivity [88].
- Apply Advanced Denoising Algorithms: Use state-of-the-art denoising methods like total variation (TV) minimization, which has been shown to produce denoised echoes with superior signal-to-noise and contrast-to-noise ratios compared to current methods (3dDespike, tedana, NORDIC) [88].
- Optimize Spatial Smoothing: Apply Gaussian spatial smoothing with full width half maximum (FWHM) typically set to 4-6 mm for single subject studies and 6-8 mm for multi-subject analyses [38], while testing these parameters in your multiverse.
Methodological Protocols for Multiverse Analysis
Standardized fMRI Preprocessing Steps
Table: Essential fMRI Preprocessing Steps and Common Variants
| Processing Step | Purpose | Common Variants/Parameters |
|---|---|---|
| Slice Timing Correction | Corrects for acquisition time differences between slices [38] | Data shifting vs. model shifting; interpolation methods [38] |
| Motion Correction | Aligns volumes to correct for head movement [38] | Rigid-body transformation; reference volume selection [38] |
| Temporal Filtering | Removes low-frequency drifts and high-frequency noise [38] | High-pass filter cutoffs; low-pass filter application [38] |
| Spatial Smoothing | Improves SNR by averaging adjacent voxels [38] | Gaussian kernel FWHM: 4-6mm (single subject) vs. 6-8mm (group) [38] |
| Global Signal Regression | Removes global signal fluctuations | Inclusion vs. exclusion [86] |
| Distortion Correction | Corrects for magnetic field inhomogeneities [38] | Field mapping; unwarping; z-shimming [38] |
Experimental Protocol: Implementing a Multiverse Analysis
Define the Analytical Space
Implement Quality Assurance
Execute Parallel Processing Pipelines
- Generate all reasonable combinations of analytical choices
- Implement efficient computing framework to handle multiple pipelines
Analyze Result Robustness
- Assess consistency of findings across the analytical multiverse
- Identify which analytical choices most strongly influence results
Report and Visualize
- Document all tested pipelines and their results
- Utilize visualization tools like METEOR for interactive exploration of analytical choices [86]
Quantitative Data on Analytical Variability
Table: Documented Variability in fMRI Analytical Choices
| Analysis Domain | Number of Variable Steps | Number of Contentious Parameters | Key Sources of Variability |
|---|---|---|---|
| Graph-fMRI Analysis | 61 steps [86] | 17 debatable parameters [86] | Scrubbing, global signal regression, spatial smoothing [86] |
| fMRI Drug Cue Reactivity | 38 consensus items [89] | 7 major categories [89] | Participant characteristics, craving assessment, scanning preparation [89] |
The Scientist's Toolkit: Essential Research Reagents
Table: Key Analytical Tools for Multiverse fMRI Analysis
| Tool/Resource | Function/Purpose | Application Context |
|---|---|---|
| METEOR App | Decision support application for accessing analytical choices [86] | Educational tool for designing robustness analyses [86] |
| Contrast Subgraph Method | Algorithm for extracting differential connectivity patterns [90] | Identifying altered functional connectivity in ASD [90] |
| TV-Minimizing Algorithm | Denoising method for multi-echo BOLD time series [88] | Improving signal-to-noise and contrast-to-noise ratios [88] |
| ENIGMA Addiction Checklist | 38-item checklist for FDCR studies [89] | Standardizing methods reporting in cue reactivity studies [89] |
| Cortical Grid Approach | Regular 2D grids for cortical depth analysis [91] | Investigating laminar structures in human brain [91] |
| Multi-echo fMRI Acquisition | Protocol for acquiring several echoes after single excitation [88] | Enabling quantitative T2* analysis and improved BOLD sensitivity [88] |
Workflow Visualization: Multiverse Analysis Implementation
Multiverse Analysis Workflow
Analytical Decision Points in fMRI Preprocessing
fMRI Preprocessing Decision Points
Between-Site Reliability Validation in Multicenter Clinical Trials
Troubleshooting Guides
Q1: Our multicenter fMRI study shows poor between-site reliability (ICC < 0.4). What are the primary factors we should investigate and correct?
A: Poor between-site reliability often stems from systematic differences in data acquisition and processing. Focus on these key areas:
- Scanner-Specific Smoothness: Differences in image reconstruction algorithms, particularly the application of apodization (k-space) filters during reconstruction, can lead to significant variations in image smoothness across sites. This was identified as a major contributor to site-related variance [22].
- Insufficient Data per Subject: The number of task runs or amount of resting-state data acquired per subject can be a limiting factor. Reliability can be theoretically increased by averaging more runs, analogous to increasing the number of test items in classical test theory [22].
- Region of Interest (ROI) Size and Definition: The size of the ROIs used to extract signal can impact reliability. ROIs that are too small may not adequately capture the primary activation across different sites and field strengths, particularly given differences in geometric distortion [22].
- Subject Physiological State (for resting-state fMRI): For resting-state studies, the subject's alertness level is a critical confound. Drowsiness and sleep during the scan significantly alter functional connectivity metrics and reduce test-retest reliability. These periods can be identified using heart rate variability (HRV) measures derived from simultaneous electrocardiogram (ECG) recordings [92].
Solution Protocol:
- Quantify Smoothness: Calculate the Full-Width at Half-Maximum (FWHM) of the data from each scanner.
- Statistical Adjustment: Incorporate smoothness as a covariate in your group-level statistical model to adjust for these differences [22].
- Increase Data Yield: Where feasible, increase the number of task runs or the duration of resting-state scans per subject per site.
- Optimize ROIs: Use larger, functionally-derived ROIs to improve reliability, balancing the need for anatomical specificity [22].
- Monitor Alertness: For resting-state studies, record cardiac pulse via ECG or a pulse oximeter. Calculate HRV metrics like RMSSD (Root Mean Square of Successive Differences) to identify and exclude volumes where the subject was likely drowsy or asleep [92].
Q2: How can we improve the test-retest reliability of the BOLD signal itself for clinical prediction studies?
A: Standard modeling of the BOLD signal can introduce noise. To improve reliability for individual-level clinical applications:
- Optimize the HRF Model: The canonical hemodynamic response function (HRF) may not fit all individuals or brain regions equally well. Mis-specification of the BOLD response shape introduces noise and reduces reliability [50].
- Use Voxel-Wise Reliability Mapping: Within a predefined ROI, reliability can be heterogeneous. Instead of using the mean signal from the entire ROI, identify and use only the most reliable voxels to create a composite measure [50].
- Account for Clinical State: Within-individual changes in clinical symptomatology (e.g., anxiety, rumination) between scan sessions can be a source of variance. Statistically controlling for these time-varying clinical features can improve the reliability of the underlying neural signal [50].
Solution Protocol:
- Employ Flexible HRF Modeling: Use a Finite Impulse Response (FIR) model or a gamma variate model that estimates parameters for onset-delay, rise-decay rate, and height. This accounts for individual differences in the timing and shape of the hemodynamic response [50].
- Calculate Voxel-Wise ICC: Within your ROI, compute the ICC for every voxel across your test-retest data.
- Create a "Reliability-Masked" ROI: Discard voxels with poor reliability (e.g., ICC < 0.4) and use the median or mean signal from the remaining, high-ICC voxels for subsequent analysis [50].
- Collect and Covary State Measures: Administer behavioral or clinical state questionnaires (e.g., rumination, anxiety scales) immediately before or after each scan. Include these scores as covariates of no interest in your model.
Q3: What is an acceptable threshold for Intraclass Correlation Coefficient (ICC) to deem a measure reliable enough for multicenter trials?
A: While interpretations can vary, a commonly used benchmark in the fMRI literature is based on Cicchetti and Sparrow's guidelines [22] [16].
The table below summarizes these qualitative interpretations:
| ICC Value | Interpretation |
|---|---|
| < 0.40 | Poor |
| 0.40 – 0.59 | Fair |
| 0.60 – 0.74 | Good |
| ≥ 0.75 | Excellent |
Important Considerations:
- Context is Key: These are general guidelines. Some experts advocate for more stringent cutoffs (e.g., >0.75) for clinical applications [50].
- ICC Depends on Your Sample: The ICC is proportional to between-subject variability. A heterogeneous sample (e.g., mixing patients and controls) can produce a higher ICC than a homogeneous sample, even with the same level of within-subject measurement error [50] [16].
- Type of ICC Matters: Ensure you are using the appropriate form of ICC. For merging data across sites, an ICC that measures "absolute agreement" (e.g., ICC(2,1)) is often most relevant, as it is sensitive to systematic differences between scanners [22] [16].
Frequently Asked Questions (FAQs)
Q1: What is the difference between test-retest reliability and between-site reliability?
A: Both concepts are related but distinct components of measurement reliability:
- Test-Retest Reliability assesses the stability of a measurement within the same scanner and site over time. It quantifies how consistent the results are when the same subject is scanned on different days [22].
- Between-Site Reliability assesses the consistency of measurements across different scanners and sites. It determines whether data from different institutions can be literally merged for analysis. A measure can have high test-retest reliability at each individual site but poor between-site reliability if systematic differences exist between scanners [22] [93].
Q2: Can we achieve high between-site reliability even with different scanner manufacturers and field strengths?
A: Yes, though it requires careful calibration. Studies have shown that even with different hardware, site-related variance can be minimized. One study found that with identical imaging hardware and software, site did not play a significant role, and between-subject differences accounted for nearly 10 times more variance than site effects [93]. The key is to identify and control for the major sources of variance, such as smoothness differences and reconstruction filters, as outlined in the troubleshooting guides above [22].
Q3: Our study involves a clinical population. Should we assess reliability in a separate healthy control group?
A: No, for clinical applications, it is highly recommended to assess reliability within the relevant clinical population. The psychometric properties of an fMRI measure can differ between healthy controls and patients. A task or region that is reliable in healthy individuals may not be reliable in a patient group, and vice versa. Furthermore, the higher between-subject variability often found in clinical samples can positively influence ICC estimates [50].
Key Multicenter Reliability Validation Protocol
This protocol is adapted from the FBIRN Phase 1 study, which established best practices for multicenter fMRI reliability [22] [24].
- Traveling Subjects Cohort: A small group of subjects (e.g., n=5) travel to and are scanned at all participating sites.
- Scanning Schedule: Each subject is scanned at each site on two separate occasions (e.g., on consecutive days) to allow for both between-site and test-retest reliability assessment.
- Standardized Task: A simple, robust paradigm (e.g., a block-design sensorimotor or visual task) is performed by subjects at all sites.
- Data Analysis for Reliability:
- Preprocessing: Use a standardized preprocessing pipeline across all data.
- ROI Analysis: Extract the signal from pre-defined, functionally-derived ROIs.
- Dependent Variables: Calculate dependent variables like Percent Signal Change (PSC) or Contrast-to-Noise Ratio (CNR).
- Variance Components Analysis: Perform a variance components analysis to partition the total variance into components attributable to subjects, sites, sessions, and their interactions.
- Calculate ICC: Compute Intraclass Correlation Coefficients (ICC) for both between-site and test-retest reliability from the variance components.
The following table summarizes the improvements in between-site reliability achievable through specific methodological optimizations, as demonstrated in the FBIRN study [22].
| Methodological Factor | Impact on Between-Site Reliability | Notes |
|---|---|---|
| Increasing ROI Size | Marked Improvement | Larger ROIs are less sensitive to misalignment and differential distortion across sites. |
| Adjusting for Smoothness | Marked Improvement | Correcting for FWHM differences between scanners removes a major source of systematic variance. |
| Averaging Multiple Task Runs | Theoretical & Empirical Improvement | Adding a second, third, or fourth run progressively increases reliability. |
| Combined Optimizations | 123% increase for 3T scanners | Applying multiple optimizations in sequence has a cumulative, positive effect on reliability. |
The Scientist's Toolkit: Key Research Reagents & Materials
| Item | Function in Reliability Validation |
|---|---|
| Standardized Functional Localizer Task | A simple, robust task (e.g., sensorimotor, visual) used across all sites to define ROIs and assess basic signal reliability [22]. |
| Structural MPRAGE Sequence | A high-resolution T1-weighted anatomical scan used for subject registration and spatial normalization. |
| ECG Recording System | For recording cardiac pulse during resting-state fMRI; used to derive Heart Rate Variability (HRV) metrics to identify and exclude periods of drowsiness [92]. |
| Smoothness (FWHM) Estimation Tool | Software to calculate the Full-Width at Half-Maximum of the processed fMRI data, which is a critical covariate for correcting between-site differences [22]. |
| Variance Components Analysis Software | Statistical tools (e.g., in R, SPSS, or specialized toolboxes) to decompose variance and calculate ICC(2,1) for absolute agreement [22] [16]. |
| Flexible Basis Functions (FIR, Gamma) | Alternative to the canonical HRF in model-based analysis; improves fit and reliability by accounting for individual differences in hemodynamic timing [50]. |
Workflow Diagrams
Between-Site Reliability Optimization Workflow
Signal Reliability Improvement Protocol
Frequently Asked Questions (FAQs)
Q: What are the established minimum reliability thresholds for clinical fMRI applications? A: Reliability is typically quantified using Intraclass Correlation Coefficients (ICCs), with specific thresholds established for different application contexts [94]:
- ICC < 0.40: Considered poor reliability; insufficient for any clinical or scientific use
- ICC 0.40-0.59: Considered fair reliability; meets minimum standard for scientific research
- ICC 0.60-0.74: Considered good reliability; may serve as an ancillary diagnostic tool alongside other clinical methods
- ICC ≥ 0.75: Considered excellent reliability; required for standalone clinical diagnostic use
Most current task-fMRI and resting-state fMRI measures fall into the "poor" range for single-subject reproducibility, with average ICC values around 0.26 for time courses and 0.44 for connectivity measures, necessitating methodological improvements to reach clinical utility [94].
Q: Why does my fMRI data show adequate group-level reliability but poor single-subject test-retest reliability? A: This common discrepancy occurs because group-level analyses benefit from averaging across participants, which reduces random error components. Single-subject measurements contain more unexplained variability from factors such as:
- State-dependent cognitive processes (attention, fatigue, emotional state)
- Head motion artifacts, particularly problematic in clinical populations
- Hemodynamic response variability between sessions
- Insufficient scan duration to characterize stable individual patterns
Recent studies report single-subject time course reproducibility around r = 0.26 with conventional pipelines, far below the clinical threshold [94]. This fundamentally limits the detectable connectivity strength in individual analyses.
Q: What paradigm choices can improve functional connectivity reliability? A: Naturalistic paradigms (e.g., movie viewing) demonstrate significantly higher test-retest reliability compared to resting-state conditions:
Table: Reliability Comparison Across fMRI Paradigms
| Paradigm Type | Key Characteristics | Reported Reliability Improvement | Best Use Cases |
|---|---|---|---|
| Resting-State | Unconstrained, no task | Baseline reliability | Clinical populations unable to perform tasks |
| Naturalistic (e.g., movie viewing) | Ecological validity, implicit behavioral constraints | ~50% increase in reliability across various connectivity measures [95] | Higher-order networks (default mode, attention), clinical longitudinal studies |
| Task-Based | Targeted cognitive engagement, performance measures | Variable; depends on task design and number of trials | Specific cognitive systems, brain-behavior associations |
Natural viewing paradigms improve reliability by providing more consistent cognitive states across sessions and reducing unwanted confounds like excessive head motion [95].
Q: How does data quality impact the reproducibility of my findings? A: Data quality has a profound impact on reproducibility. In studies of people with aphasia, better data quality significantly improved agreement in individual-level analyses [23]. Motion has a particularly pronounced effect – participants in the lowest motion quartile showed reliability 2.5 times higher than those in the highest motion quartile in task-fMRI studies [29]. For functional connectivity, scan duration is crucial: fair reliability (median ICCs) was achieved at longer scan durations of 10-12 minutes compared to shorter acquisitions [23].
Troubleshooting Guides
Problem: Poor Single-Subject Test-Retest Reliability
Symptoms:
- High within-subject variability across scanning sessions
- ICC values consistently below 0.40 for key connectivity measures
- Inability to replicate individual connectivity patterns over time
Solution: Implement optimized filtering frameworks Conventional preprocessing pipelines often yield insufficient reproducibility for clinical applications. Systematic filtering approaches can significantly enhance time course reproducibility:
Table: Filtering Protocol for Enhanced Reliability
| Processing Step | Conventional Approach | Optimized Approach | Expected Improvement |
|---|---|---|---|
| Filter Type | Gaussian or HRF filters (often removed in modern SPM) | Savitzky-Golay (SG) filters with optimized parameters [94] | Better noise removal while preserving cognitive signals |
| Parameter Optimization | Fixed, canonical parameters | Data-driven optimization using subject-specific HRFs [94] | Customized to individual BOLD response characteristics |
| Autocorrelation Control | Not explicitly addressed | Empirical derivation from predictor time courses [94] | Maintains acceptable autocorrelation levels for event-related designs |
| Connectivity Enhancement | Standard GLM denoising | Combined SG filtering + GLM-based data cleaning [94] | Improves connectivity correlations from r = 0.44 to r = 0.54 |
Implementation protocol:
- Calculate subject-specific hemodynamic response function by averaging task-related signal changes
- Determine optimal SG filter parameters (window size, polynomial order) using brute-force optimization
- Apply optimized SG filter to time courses while monitoring autocorrelation levels
- Validate that filtered time courses maintain cognitive signals in task-related frequency bands
This approach has demonstrated improvement of average time course reproducibility from r = 0.26 to r = 0.41, moving from "poor" to "fair" reliability [94].
Problem: Inconsistent Functional Connectivity Findings
Symptoms:
- Variable connectivity patterns across similar analyses
- Poor agreement between different analysis pipelines
- Literature reports with contradictory connectivity findings
Solution: Standardize connectivity measurement and preprocessing The choice of pairwise interaction statistic dramatically impacts connectivity findings. Benchmarking studies reveal substantial variation across 239 different pairwise statistics [49]:
Optimal pairwise statistics by application:
- Structure-function coupling: Precision-based statistics, stochastic interaction, imaginary coherence
- Individual fingerprinting: Covariance, precision, and distance measures
- Brain-behavior prediction: Precision-based and covariance-based statistics
Critical preprocessing considerations:
- Band-pass filtering: Standard filters (0.009-0.08 Hz, 0.01-0.10 Hz) can introduce biases that increase correlation estimates between independent time series [96]
- Sampling rates: Adjust sampling rates to align with analyzed frequency band to avoid distorted correlation coefficients [96]
- Multiple comparisons: Conventional corrections may fail with filtered data; surrogate data methods better control Type I errors [96]
Recommended workflow:
- Select pairwise statistics aligned with research question (covariance for general use, precision for direct connections)
- Adjust sampling rate to match frequency band of interest
- Use surrogate data methods for multiple comparison correction
- Report exact pairwise statistic and preprocessing parameters for reproducibility
Problem: Analytical Variability Across Research Teams
Symptoms:
- Different research groups obtaining divergent results from identical datasets
- Low agreement on hypothesis testing outcomes
- Challenges in replicating published findings
Solution: Adopt standardized preprocessing frameworks and reporting standards The NARPS study demonstrated that 70 expert teams testing identical hypotheses on the same dataset produced divergent conclusions, primarily due to methodological variability [97].
Standardization strategies:
- Implement BIDS and BIDS-Apps: Use Brain Imaging Data Structure for consistent data organization and BIDS Apps for standardized pipeline execution [97]
- Adopt NiPreps: Utilize NeuroImaging PREProcessing tools that provide standardized, containerized preprocessing environments [97]
- Embrace containerization: Use platforms like Neurodesk that encapsulate complete software environments with persistent DOIs for long-term reproducibility [98]
Reporting requirements:
- Document all preprocessing steps using COBIDAS checklist or similar frameworks
- Share complete analysis code in containerized formats
- Specify exact software versions and parameters for all processing steps
Multi-lab analysis experiments demonstrate that standardized approaches can achieve 80% agreement on group-level results even when analytical flexibility exists [99].
The Scientist's Toolkit
Table: Essential Resources for Reliability Optimization
| Tool/Resource | Function | Application Context | Access Information |
|---|---|---|---|
| NiPreps | Standardized, containerized preprocessing pipelines | fMRI, dMRI, and other neuroimaging modalities; ensures consistent preprocessing across studies [97] | Open-source; available with BIDS compliance |
| BIDS & BIDS-Derivatives | Consistent data organization and formatting | Data sharing, archiving, and pipeline interoperability; critical for multi-site studies [97] | Community standard; validator tools available |
| Neurodesk | Containerized analysis environments | Reproducible workflows across computing platforms; enables exact replication of analysis environments [98] | Open-source platform with versioned containers |
| Savitzky-Golay Filter Framework | Enhanced time course reproducibility | Single-subject applications; clinical settings requiring high test-retest reliability [94] | Custom implementation with parameter optimization |
| SPI Benchmarking Suite | Evaluation of pairwise interaction statistics | Functional connectivity studies; method selection for specific research questions [49] | PySPI package for comprehensive benchmarking |
Experimental Workflows
Standardized Reliability Assessment Protocol
Factors Influencing fMRI Reliability
Conclusion
The evidence consistently demonstrates that fMRI test-retest reliability requires careful methodological attention to reach thresholds suitable for clinical applications and individual-differences research. Key takeaways include the superiority of specific acquisition parameters (moderate window widths, sufficient scan durations), analytical decisions (larger smoothing kernels, appropriate contrast selection), and processing approaches that collectively enhance reliability without sacrificing validity. Future directions should focus on developing standardized reliability reporting practices, validating multivariate approaches that show promise for improved psychometric properties, and establishing reliability benchmarks specific to clinical populations and applications. For drug development professionals, these advancements are crucial for transforming fMRI from a research tool into a validated biomarker capable of predicting treatment outcomes and monitoring intervention effects in clinical trials.
References
- 1. Reliability and Stability Challenges in ABCD Task fMRI Data [https://pmc.ncbi.nlm.nih.gov/articles/PMC9017319/]
- 2. Functional MRI Can Be Highly Reliable, but It Depends on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8258303/]
- 3. Longer scans boost prediction and cut costs in brain-wide ... [https://www.nature.com/articles/s41586-025-09250-1]
- 4. Neuroimaging Measures of Error-Processing [https://pmc.ncbi.nlm.nih.gov/articles/PMC4860744/]
- 5. Computational mechanisms of neuroimaging biomarkers ... [https://www.nature.com/articles/s41380-025-03134-6]
- 6. A decade of test-retest reliability of functional connectivity [https://www.sciencedirect.com/science/article/pii/S1053811919307487]
- 7. What Is the Test - Retest of Common Task- Reliability ... Functional MRI [https://pubmed.ncbi.nlm.nih.gov/32489141/]
- 8. A decade of test-retest reliability of functional connectivity [https://pmc.ncbi.nlm.nih.gov/articles/PMC6907736/]
- 9. Striving toward translation: strategies for reliable fMRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8363569/]
- 10. Current Challenges in Translational and Clinical fMRI and ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2019.00924/full]
- 11. The diagnostic potential of resting state functional MRI [https://www.sciencedirect.com/science/article/pii/S1053811925003374]
- 12. High-resolution fMRI at 7 Tesla: challenges, promises and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8018601/]
- 13. The role of fMRI in drug development - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC5931333/]
- 14. What is the value of human FMRI in CNS drug development? [https://www.sciencedirect.com/science/article/abs/pii/S1359644610002953]
- 15. Striving toward translation: strategies for reliable fMRI ... [https://www.sciencedirect.com/science/article/abs/pii/S1364661321001297]
- 16. A guide to the measurement and interpretation of fMRI test- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7875178/]
- 17. Assessing reliability in neuroimaging research through ... [https://elifesciences.org/articles/35718]
- 18. Test-Retest Reliability of fMRI During an Emotion ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2022.859792/full]
- 19. Tutorial on use of intraclass correlation coefficients for ... [https://www.spiedigitallibrary.org/journals/Tutorial-on-use-of-intraclass-correlation-coefficients-for-assessing-intertest/volume-20/issue-05/050801/Tutorial-on-use-of-intraclass-correlation-coefficients-for-assessing-intertest/10.1117/1.JBO.20.5.050801.full]
- 20. Tools for test-retest FMRI studies [https://github.com/ekmolloy/fmri_test-retest]
- 21. isc-toolbox: Inter-subject correlation analysis for fMRI in ... [https://www.nitrc.org/forum/forum.php?thread_id=15594&forum_id=7013]
- 22. Test–retest and between‐site reliability in a multicenter fMRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3670112/]
- 23. Test-retest reliability of edge-level resting-state functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12581729/]
- 24. Test-retest and between-site reliability in a multicenter fMRI ... [https://pubmed.ncbi.nlm.nih.gov/17636563/]
- 25. How do tasks impact the reliability of fMRI functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10884875/]
- 26. Multisite reliability and repeatability of an advanced brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6636359/]
- 27. Brain-Network Temporal Variability in Resting-State fMRI [https://www.preprints.org/manuscript/202510.2046]
- 28. Test-retest reproducibility of structural and proxy estimates ... [https://www.sciencedirect.com/science/article/pii/S1053811925005610]
- 29. Reliability and stability challenges in ABCD task fMRI data [https://www.sciencedirect.com/science/article/pii/S1053811922001756]
- 30. Multiband acquisition sequences for fMRI: Proceed with ... [https://apertureneuro.org/article/91292-multiband-acquisition-sequences-for-fmri-proceed-with-caution]
- 31. Use of functional imaging across clinical phases in CNS ... [https://www.nature.com/articles/tp201343]
- 32. Modulatory effects of fMRI acquisition time of day, week ... [https://www.sciencedirect.com/science/article/pii/S1053811923006109]
- 33. Protocol for magnetic resonance imaging acquisition, quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8412227/]
- 34. Spatial Smoothing Effect on Group-Level Functional ... [https://www.mdpi.com/1424-8220/23/13/5866]
- 35. A deep neural network for adaptive spatial smoothing of ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1554769/full]
- 36. Consensus recommendations for clinical functional MRI ... [https://apertureneuro.org/article/128149-consensus-recommendations-for-clinical-functional-mri-applied-to-language-mapping]
- 37. Functional MRI [https://www.sciencedirect.com/science/article/abs/pii/B9780128244609000212]
- 38. What are the steps for preprocessing fMRI data? [https://mriquestions.com/data-pre-processing.html]
- 39. Correction of Physiological Artifacts in Multi‐Echo fMRI Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12183604/]
- 40. Optimization of rs-fMRI Pre-processing for Enhanced ... [https://www.sciencedirect.com/science/article/abs/pii/S105381191500395X]
- 41. FAQ - Frequently Asked Questions [https://fmriprep.org/en/stable/faq.html]
- 42. What's new — fmriprep version documentation [https://fmriprep.org/en/25.1.4/changes.html]
- 43. Comparison of blocked and event-related fMRI designs for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3036974/]
- 44. Test-retest reliability of fMRI-measured brain activity during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7846028/]
- 45. a derived dataset to investigate analytical variability in fMRI [https://www.nature.com/articles/s41597-025-05247-7]
- 46. Long-term test–retest reliability of functional MRI in a ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1630684/]
- 47. Test-retest reliability of dynamic functional connectivity ... [https://pubmed.ncbi.nlm.nih.gov/40161977/]
- 48. Systematic evaluation of fMRI data-processing pipelines for ... [https://www.nature.com/articles/s41467-024-48781-5]
- 49. Benchmarking methods for mapping functional connectivity ... [https://www.nature.com/articles/s41592-025-02704-4]
- 50. Importance of test–retest reliability for promoting fMRI ... [https://www.nature.com/articles/s41398-021-01507-3]
- 51. Investigation and validation of intersite fMRI studies using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2785504/]
- 52. Guidelines for reporting an fMRI study - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2287206/]
- 53. fMRIPrep: A Robust Preprocessing Pipeline for fMRI Data ... [https://fmriprep.org/]
- 54. Multi‐Metric Approach for the Comparison of Denoising ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12044599/]
- 55. Boost in Test–Retest Reliability in Resting State fMRI with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8599720/]
- 56. Multiecho fMRI denoising effectively removes head motion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6765232/]
- 57. Frontiers | Physiological Noise in Brainstem fMRI [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2013.00623/full]
- 58. Systemic physiological "noise" in fMRI has clinical relevance [https://pubmed.ncbi.nlm.nih.gov/40909822/]
- 59. Finite Impulse Response (FIR) - Andy's Brain Book! [https://andysbrainbook.readthedocs.io/en/latest/FIR/FIR_Overview.html]
- 60. Modeling the hemodynamic response function in fMRI [https://www.sciencedirect.com/science/article/abs/pii/S1053811908012056]
- 61. Importance of test–retest reliability for promoting fMRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8272717/]
- 62. DSC: Recirculation Effects [https://mriquestions.com/dsc-recirculation.html]
- 63. Analysis of an fMRI dataset with a Finite Impule Response ... [https://nilearn.github.io/stable/auto_examples/04_glm_first_level/plot_fir_model.html]
- 64. Improving the Test-Retest Reliability of Resting State fMRI ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2017.00249/full]
- 65. two-gamma-variate fitting - MATLAB Answers [https://www.mathworks.com/matlabcentral/answers/886074-two-gamma-variate-fitting]
- 66. Towards clinical applicability of fMRI via systematic filtering [https://pmc.ncbi.nlm.nih.gov/articles/PMC12068634/]
- 67. Subject-specific Functional ROIs Enhance Reliability in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12552277/]
- 68. Subject-specific Functional ROIs Enhance Reliability in ... [https://link.springer.com/article/10.1007/s00062-025-01534-3]
- 69. Comparing reliability-based measures of functional ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319993/]
- 70. - Within variation in BOLD- subject signal changes across... fMRI [https://pubmed.ncbi.nlm.nih.gov/18538585/]
- 71. State-related neural influences on fMRI connectivity estimation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8815005/]
- 72. Vigilance Effects in Resting-State fMRI [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.00321/full]
- 73. Global effects in fMRI reveal brain markers of state and trait ... [https://www.medrxiv.org/content/10.1101/2025.07.15.25331571v1]
- 74. fMRI Tutorial #3: Looking at the Data - Andy's Brain Book! [https://andysbrainbook.readthedocs.io/en/latest/fMRI_Short_Course/fMRI_03_LookingAtTheData.html]
- 75. Tutorial 1: fMRI Data Structures [http://www.newbi4fmri.com/tutorial-1-data]
- 76. Multivariate approaches improve the reliability and validity of ... [https://pubmed.ncbi.nlm.nih.gov/31039408/]
- 77. Multivariate approaches improve the reliability and validity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6591084/]
- 78. Task fMRI paradigms may capture more behaviorally ... [https://www.sciencedirect.com/science/article/pii/S1053811923000939]
- 79. The effect of scan length on the reliability of resting-state ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4104183/]
- 80. The effect of resting condition on resting-state fMRI reliability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4003890/]
- 81. Characterizing and Differentiating Task-based and Resting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4559495/]
- 82. Test-retest reliability of emotion regulation networks using ... [https://www.sciencedirect.com/science/article/pii/S1053811921001944]
- 83. Reproducibility of R‐fMRI metrics on the impact of different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6866539/]
- 84. fMRI replicability depends upon sufficient individual-level ... [https://www.nature.com/articles/s42003-019-0378-6]
- 85. Test-retest reliability of time-varying patterns of brain ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2022.980280/full]
- 86. The multiverse of data preprocessing and analysis in graph ... [https://www.sciencedirect.com/science/article/pii/S0149763424003154]
- 87. Task and resting state fMRI modelling of brain-behavior ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12593242/]
- 88. Smooth dynamic T 2 * mapping in fMRI based on a novel ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1544748/full]
- 89. A methodological checklist for fMRI drug cue reactivity ... [https://www.nature.com/articles/s41596-021-00649-4]
- 90. Contrast subgraphs catch patterns of altered functional ... [https://www.nature.com/articles/s41598-025-04932-2]
- 91. High resolution data analysis strategies for mesoscale human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5745233/]
- 92. Improving the Test-Retest Reliability of Resting State fMRI by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5420587/]
- 93. Investigation and validation of intersite fMRI studies using the ... [https://experts.illinois.edu/en/publications/investigation-and-validation-of-intersite-fmri-studies-using-the-/]
- 94. Towards clinical applicability of fMRI via systematic filtering [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0321088]
- 95. Test–retest reliability of functional connectivity networks during ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6867176/]
- 96. The diagnostic potential of resting state functional MRI - PubMed [https://pubmed.ncbi.nlm.nih.gov/40554035/]
- 97. Standardized Preprocessing in Neuroimaging: Enhancing ... [https://link.springer.com/protocol/10.1007/978-1-0716-4260-3_8]
- 98. Toward the future of scientific publishing through ... [https://apertureneuro.org/article/143700-toward-the-future-of-scientific-publishing-through-reproducible-research-artefacts-enabled-by-neurodesk]
- 99. fNIRS reproducibility varies with data quality, analysis ... [https://www.nature.com/articles/s42003-025-08412-1]