Evaluating Neurotechnology Safety and Efficacy: A Comprehensive Framework for Researchers and Developers
This article provides a comprehensive framework for the safety and efficacy evaluation of neurotechnologies, from foundational concepts to advanced validation strategies.
Evaluating Neurotechnology Safety and Efficacy: A Comprehensive Framework for Researchers and Developers
Abstract
This article provides a comprehensive framework for the safety and efficacy evaluation of neurotechnologies, from foundational concepts to advanced validation strategies. Tailored for researchers, scientists, and drug development professionals, it explores the current regulatory landscape, innovative testing methodologies like sandbox environments, and comparative analyses of electrical stimulation and pharmacological agents. The content addresses critical challenges in the field, including navigating regulatory pathways for direct-to-consumer devices and implantable systems, and offers insights into optimizing clinical trial design and post-market surveillance to ensure the reliable and ethical translation of neurotechnologies into clinical practice.
Neurotechnology Fundamentals: Core Principles and the Regulatory Landscape
The field of neurotechnology is undergoing a rapid transformation, evolving from a specialized research discipline into a burgeoning industry poised to revolutionize medicine and human-machine interaction. At its core, neurotechnology encompasses a spectrum of tools designed to monitor, analyze, and modulate neural activity. This spectrum ranges from non-invasive systems that record brain activity through the skull to fully implanted devices that interface directly with neural tissue. Brain-Computer Interfaces (BCIs) form a critical segment of this spectrum, operating as systems that measure central nervous system activity and convert it into artificial outputs that replace, restore, enhance, supplement, or improve natural neural outputs [1]. These systems create a real-time bidirectional information gateway between the brain and external devices, offering unprecedented potential for restoring function in patients with neurological disorders and injuries [2].
Understanding the technical capabilities, applications, and limitations of each category within the neurotechnology spectrum is essential for researchers, clinicians, and developers aiming to advance the field or apply these tools in therapeutic contexts. The choice between non-invasive, semi-invasive, and invasive technologies involves careful trade-offs between signal fidelity, risk tolerance, and intended application. This guide provides a structured comparison of these modalities, supported by current experimental data and methodological protocols, to inform evidence-based evaluation of their safety and efficacy.
Categorizing the Neurotechnology Spectrum
Neurotechnologies are fundamentally categorized based on their physical relationship to neural tissue, which directly determines their signal quality, surgical risk, and suitable applications. The three primary categories are:
Non-invasive BCIs: Placed on the scalp or skin surface external to the skull. These systems record large-scale brain activity (e.g., via EEG, fMRI, fNIRS) without penetrating the body, minimizing surgical risks and ethical concerns but suffering from lower signal quality due to skull interference and susceptibility to external noise [3].
Semi-invasive BCIs: Positioned on the brain surface beneath the skull (epidural or subdural). This approach offers better signal quality than non-invasive methods by detecting local field potentials without piercing brain tissue, but still requires craniotomy for electrode placement [3].
Invasive BCIs: Implanted directly into brain tissue, penetrating the cortex. These systems provide the highest signal quality by recording single neuron activity (action potentials) with precise spatial resolution, but require complex brain surgery that carries risks of infection, tissue damage, and scar formation [2] [3].
Table 1: Fundamental Characteristics of BCI Approaches
| Characteristic | Non-invasive BCI | Semi-invasive BCI | Invasive BCI |
|---|---|---|---|
| Spatial Resolution | Low (scales to centimeters) | Moderate (millimeter scale) | High (micron scale for single neurons) |
| Temporal Resolution | Moderate (milliseconds) | High (milliseconds) | Very High (sub-millisecond) |
| Signal-to-Noise Ratio | Lowest | Moderate | Highest |
| Surgical Risk | None | Moderate (craniotomy required) | High (brain penetration) |
| Long-term Stability | Highest | Moderate | Limited (scarring, signal degradation) |
| Information Transfer Rate | Lowest (~5-25 bits/minute) | Moderate (~40-60 bits/minute) | Highest (~100-200 bits/minute) |
| Primary Signal Types | EEG, MEG, fNIRS, fMRI | ECoG, sEEG | Single/Multi-unit spikes, Local Field Potentials |
Technical Performance and Market Landscape
Performance Benchmarks and Clinical Applications
The technical performance differences between BCI categories translate directly into their clinical applications and efficacy. Non-invasive systems have found significant utility in stroke rehabilitation, where a 2025 umbrella review of systematic analyses demonstrated that BCI-combined treatment can improve upper limb motor function and quality of daily life for stroke patients, particularly those in the subacute phase, with good safety profiles [4]. However, these systems face challenges including signal interference from noise, "BCI illiteracy" where a significant proportion of users struggle to achieve effective control, and substantial variation in therapeutic efficacy across patients [5].
Invasive BCIs have demonstrated remarkable capabilities in restoring communication for severely paralyzed individuals. Recent research presented at Neuroscience 2025 documented a paralyzed man with ALS who used a chronic intracortical BCI independently at home for over two years, controlling his home computer, working full-time, and communicating more than 237,000 sentences with up to 99% word output accuracy at approximately 56 words per minute [6]. This exemplifies the high-performance potential of invasive approaches for severe disabilities.
Semi-invasive approaches offer a middle ground, with technologies like Precision Neuroscience's "Layer 7" ultra-thin electrode array designed to slip between the skull and brain with minimal invasiveness. This approach aims to capture high-resolution signals without piercing brain tissue, and in April 2025 received FDA 510(k) clearance for commercial use with implantation durations of up to 30 days, initially focused on enabling communication for patients with ALS [1].
Table 2: Current Market Leaders and Their Technological Approaches
| Company/Institution | Technology Type | Key Technology | Primary Application Focus | Development Status (2025) |
|---|---|---|---|---|
| Neuralink | Invasive | Ultra-high-bandwidth implantable chip with thousands of micro-electrodes | Severe paralysis, communication | Human trials with 5 participants [1] |
| Synchron | Semi-invasive | Stentrode (endovascular, delivered via blood vessels) | Paralysis, computer control | Clinical trials, partnership with Apple and NVIDIA [1] |
| Blackrock Neurotech | Invasive | Neuralace (flexible lattice electrode), Utah array | Paralysis, communication | Expanding trials, including in-home tests [1] |
| Precision Neuroscience | Semi-invasive | Layer 7 (ultra-thin electrode array on brain surface) | Communication for ALS | FDA 510(k) cleared for up to 30 days implantation [1] |
| Paradromics | Invasive | Connexus BCI (modular array with 421 electrodes) | Speech restoration | First-in-human recording, planning clinical trial [1] |
| Johns Hopkins APL | Non-invasive | Digital holographic imaging (records neural tissue deformations) | Fundamental research, future BCI applications | Preclinical validation [7] |
Market Outlook and Adoption Trends
The neurotechnology market is experiencing significant growth, driven by increasing investment and technological advancement. According to industry analysis, the global BCI market is forecast to grow to over US$1.6 billion by 2045, representing a compound annual growth rate of 8.4% since 2025 [8]. The addressable market in healthcare alone is substantial, with an estimated 5.4 million people in the United States living with paralysis that impairs their ability to use computers or communicate [1]. Initial market growth is driven primarily by applications in paralysis, rehabilitation, and prosthetics.
Private investment in neurotechnology has surged, with Neuralink reportedly raising over $650 million to date, and Paradromics securing more than $105 million in venture funding plus $18 million from NIH and DARPA grants as of February 2025 [1]. This funding landscape reflects strong confidence in the commercial potential of advanced BCI technologies, particularly invasive and semi-invasive approaches aimed at addressing severe neurological disabilities.
Experimental Protocols and Methodologies
Protocol: Non-Invasive Brain-Spine Interface for Motor Rehabilitation
Recent research has demonstrated innovative approaches to combining non-invasive technologies for rehabilitation. A 2025 study published in the Journal of NeuroEngineering and Rehabilitation developed and evaluated a non-invasive brain-spine interface (BSI) using EEG and transcutaneous spinal cord stimulation (tSCS) for motor rehabilitation [9].
Objective: To detect movement intention from EEG correlates and use this to trigger spinal cord stimulation timed with voluntary effort, creating a closed-loop rehabilitation system.
Participant Recruitment: 17 unimpaired participants (10 male, 7 female, average age 25.8 ± 3.9 years) with no acute or chronic pain conditions, neurological diseases, or implanted metal [9].
Experimental Setup:
- EEG data recorded at 500 Hz using a wireless 32-channel headset positioned over central-medial areas according to the 10-10 system.
- Electromyography (EMG) signals recorded at 1482 Hz using wireless surface electrodes placed bilaterally on lower limb muscles.
- Participants performed cued right knee extensions, imagined movements, and uncued movements.
Signal Processing and Decoding:
- Initiation of knee extension was associated with event-related desynchronization in central-medial cortical regions at frequency bands between 4-44 Hz.
- A linear discriminant analysis (LDA) decoder using μ (8-12 Hz), low β (16-20 Hz), and high β (24-28 Hz) frequency bands was implemented.
- The decoder achieved an average area under the curve (AUC) of 0.83 ± 0.06 during cued movement tasks offline.
Closed-Loop Implementation:
- With real-time decoder-modulated tSCS, the neural decoder performed with an average AUC of 0.81 ± 0.05 on cued movement and 0.68 ± 0.12 on uncued movement.
- The system successfully provided closed-loop control of tSCS timed with movement intention [9].
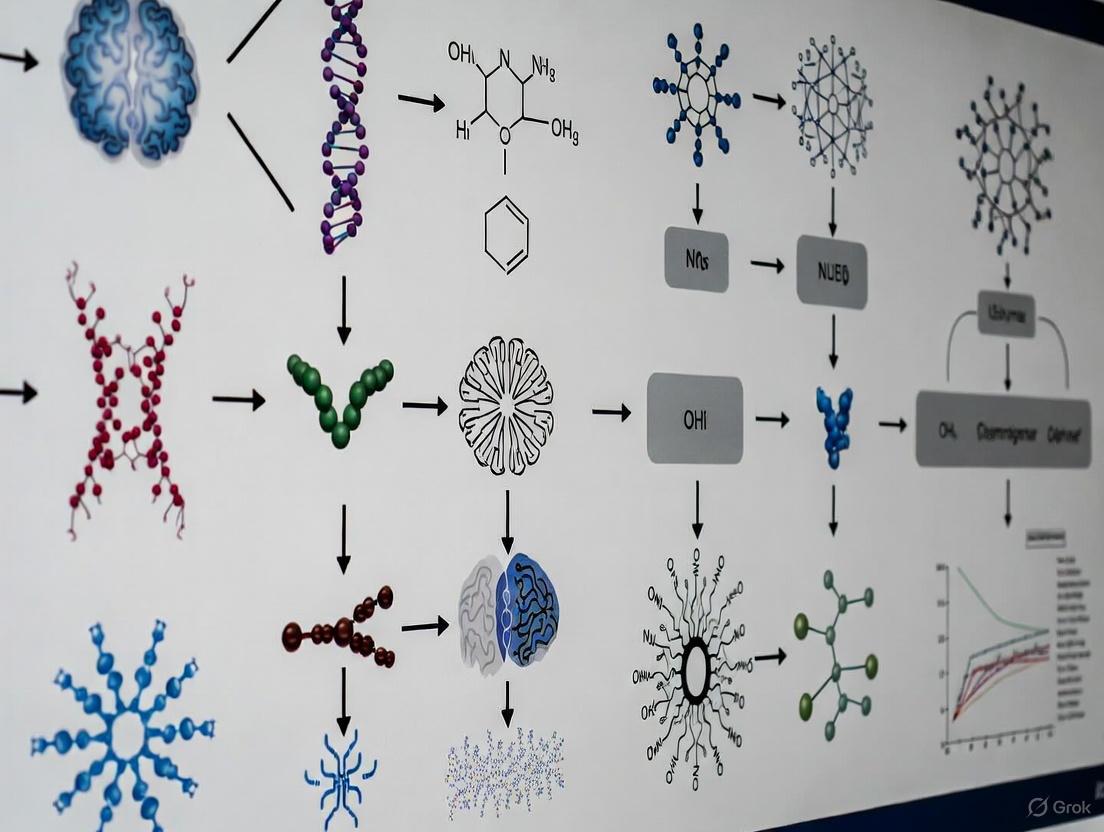
The following workflow diagram illustrates the experimental setup and closed-loop control system:
Diagram 1: Workflow of non-invasive brain-spine interface experimental protocol for motor rehabilitation.
Protocol: Intracortical Microstimulation for Somatosensory Restoration
For invasive approaches, intracortical microstimulation (ICMS) has emerged as a promising technique for restoring tactile sensations. A foundational study presented at Neuroscience 2025 provided crucial long-term safety and efficacy data [6].
Objective: To evaluate the safety and stability of ICMS via microelectrode interfaces in the somatosensory cortex over extended periods.
Participant Profile: Five participants implanted with microelectrode arrays in the somatosensory cortex, receiving millions of electrical stimulation pulses over a combined 24 years.
Methodology:
- Microelectrode arrays were chronically implanted in the somatosensory cortex.
- Electrical stimulation parameters were carefully controlled to evoke tactile sensations without causing tissue damage.
- Subjective reports of sensation quality and location were collected.
- Neural interface stability and electrode functionality were monitored regularly.
Results:
- ICMS evoked high-quality, stable tactile sensations in the hand without serious adverse effects.
- More than half of the electrodes continued to function reliably after 10 years in one participant.
- This study represents the most extensive evaluation of ICMS in humans and establishes that ICMS is safe over long periods [6].
The signaling pathway for this invasive approach can be visualized as follows:
Diagram 2: Bidirectional signaling pathway for invasive intracortical microstimulation and recording.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for BCI Development and Evaluation
| Category | Specific Tool/Reagent | Research Function | Example Application |
|---|---|---|---|
| Signal Acquisition | gNautilus 32-channel EEG headset (gTec) | Records cortical activity from scalp surface | Non-invasive BCI for motor intention detection [9] |
| Microelectrode arrays (Utah array, Neuropixels) | Records single-neuron activity in cortex | High-fidelity neural decoding for speech and movement [1] [6] | |
| Trigno Avanti wireless EMG sensors (Delsys) | Records muscle activity for validation | Correlating neural decoding with actual movement [9] | |
| Signal Processing | BCI2000 software platform | General-purpose BCI research platform | Real-time signal processing and experiment control [9] |
| Linear Discriminant Analysis (LDA) decoder | Classifies neural signals into intended commands | Detecting movement onset from sensorimotor rhythms [9] | |
| Kalman filter, Bayesian decoders | Estimates continuous movement parameters | Predicting movement trajectory from motor cortex activity [2] | |
| Neuromodulation | DS8R constant current stimulator (Digitimer) | Precisely controls electrical stimulation amplitude | Transcutaneous spinal cord stimulation [9] |
| Intracortical microstimulation arrays | Provides focal electrical stimulation to neural tissue | Restoring artificial touch sensations [6] | |
| Experimental Control | NI-DAQ digital input/output board (National Instruments) | Synchronizes multiple data acquisition systems | Temporal alignment of EEG, EMG, and stimulus markers [9] |
| Digital pulse train generator (DG2A, Digitimer) | Precisely times stimulation delivery | Ensuring accurate closed-loop stimulation timing [9] | |
| 3-(Pyridin-3-yl)prop-2-enamide | 3-(Pyridin-3-yl)prop-2-enamide | RUO | Supplier | 3-(Pyridin-3-yl)prop-2-enamide for research. Explore its applications in kinase & cancer studies. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| (4-Nitro-benzyl)-phosphonic acid | (4-Nitro-benzyl)-phosphonic Acid | High Purity | (4-Nitro-benzyl)-phosphonic acid for RUO. A phosphatase & kinase research tool. High-purity, for biochemical studies only. Not for human, veterinary, or household use. | Bench Chemicals |
Safety and Efficacy Evaluation Framework
Risk-Benefit Analysis Across the Spectrum
Each category within the neurotechnology spectrum presents distinct safety considerations that must be balanced against potential efficacy. Non-invasive systems demonstrate favorable safety profiles, with a 2025 umbrella review of BCI for stroke rehabilitation confirming good safety, particularly for subacute stroke patients [4]. The primary limitations relate to efficacy rather than safety, including signal quality issues and variable patient responsiveness.
Semi-invasive approaches moderate risk while improving signal quality. The Stentrode by Synchron, which is delivered via blood vessels, reported no serious adverse events or blood vessel blockages in a four-patient trial after 12 months, with the device staying in place [1]. This suggests acceptable safety for carefully selected patients.
Invasive technologies carry the highest risks but offer superior performance. The most extensive safety evaluation of intracortical microstimulation in humans demonstrated maintained safety over a combined 24 years across five participants, with more than half of electrodes continuing to function reliably after 10 years in one participant [6]. However, invasive implants always carry risks of infection, hemorrhage, and neurological deficits, with tissue scarring potentially limiting long-term stability [3].
Emerging Innovations and Future Directions
The neurotechnology field continues to evolve with innovations addressing current limitations. Johns Hopkins APL researchers have demonstrated a breakthrough in non-invasive, high-resolution recording using digital holographic imaging to detect neural tissue deformations at nanometer scale, potentially enabling future non-invasive BCIs with improved signal quality [7]. Similarly, magnetomicrometry—implanting small magnets in muscle tissue tracked by external magnetic field sensors—has shown potential for more intuitive prosthetic control than traditional neural approaches [6].
The BRAIN Initiative has outlined a comprehensive vision spanning from 2016-2026, focusing initially on technology development and shifting toward integrating technologies to make fundamental discoveries about brain function [10]. This coordinated effort continues to drive innovation across the neurotechnology spectrum.
The neurotechnology spectrum encompasses complementary toolsets with distinct risk-benefit profiles suited to different applications and patient populations. Non-invasive systems offer safety and accessibility for rehabilitation and basic research, while invasive approaches provide unprecedented fidelity for severe disabilities. Semi-invasive technologies represent a promising middle ground, with recent regulatory approvals signaling their growing clinical viability. As the field advances, ethical considerations around neural enhancement, data privacy, and appropriate use of brain data will require ongoing attention from the research community [10]. The continued convergence of engineering, neuroscience, and clinical medicine across this spectrum promises to transform our approach to neurological disorders and human-machine interaction in the coming decades.
The Imperative of Rigorous Safety and Efficacy Evaluation
The rapid emergence of neurotechnology represents a paradigm shift in neurology and psychiatry, offering unprecedented potential for treating debilitating conditions. By 2026, the neurotechnology market is estimated to be worth £14 billion, reflecting substantial investment and innovation in this sector [11]. These technologies, defined by their direct connection with the nervous system, interface with the most complex and least understood organ in the human body [12]. The powerful capabilities of neurotechnology—to both read from and write into the brain—create an ethical and clinical imperative for rigorous safety and efficacy evaluation before these interventions can be responsibly integrated into clinical practice [12]. This evaluation framework must balance the promise of life-changing therapeutic benefits with meticulous assessment of risks, from physical safety to profound ethical considerations surrounding mental privacy and personal identity [12] [13].
The Expanding Neurotechnology Landscape
Neurotechnology encompasses a diverse range of invasive and non-invasive approaches, from well-established deep brain stimulation (DBS) to emerging closed-loop systems and brain-computer interfaces (BCIs). A recent horizon scan identified 81 unique neurotechnologies in development, with 23 targeting mental health conditions, 31 focused on healthy aging, and 42 addressing physical disability [11]. This scan revealed that the majority (79%) of these technologies do not yet have FDA approval, and most (77.4%) remain in earlier stages of development (pilot/feasibility studies), with only 22.6% at pivotal or post-market stages [11].
The table below illustrates the current development landscape across key application areas:
Table 1: Neurotechnology Development Pipeline by Therapeutic Area
| Therapeutic Area | Technologies in Development | FDA Approval Status | Development Stage |
|---|---|---|---|
| Mental Health | 23 | 21% approved | Mostly early-stage |
| Healthy Aging | 31 | Limited approval | Mixed stages |
| Physical Disability | 42 | Emerging approvals | Later-stage focus |
Data synthesized from horizon scan of 81 neurotechnologies [11]
Digital elements are common features across these technologies, including software, apps, and connectivity to other devices. Interestingly, despite the prominence of AI in discussions of neurotechnology, only three of the 81 identified technologies had an identifiable AI component [11]. This disconnect between technological hype and current capabilities underscores the need for realistic evaluation frameworks.
Comparative Efficacy Analysis: Methodologies and Metrics
Endovascular Treatments for Intracranial Stenosis
Symptomatic intracranial atherosclerotic stenosis (sICAS) is a common cause of ischemic stroke, particularly among Asian, Black, and Hispanic populations [14]. A recent single-center study compared the safety and efficacy of different endovascular treatments in 154 patients with sICAS, providing robust comparative data on bare metal stents (BMS), drug-coated balloons (DCB), and drug-eluting stents (DES) [14].
Experimental Protocol: The study involved patients with ≥70% stenosis of major intracranial arteries who experienced TIA or stroke despite maximal medical therapy. Patients were assigned to BMS, DCB, or DES groups based on lesion characteristics and operator experience. All patients received pre-procedural aggressive medical therapy including antiplatelet agents and statins. Technical success was defined as residual stenosis ≤30% after angioplasty. Primary endpoints included incidence of in-stent restenosis (ISR) at 6 months, periprocedural complications, stroke recurrence rates, and modified Rankin scores (mRS) at multiple timepoints [14].
Table 2: Comparative Outcomes for Different Endovascular Treatments
| Treatment Modality | Periprocedural Complications | 6-Month Restenosis Rate | Stroke Recurrence During Follow-up |
|---|---|---|---|
| Bare Metal Stent (BMS) | 11.3% | 35.2% | 7.0% (5/71 patients) |
| Drug-Coated Balloon (DCB) | 8.0% | 6.0% | 2.0% (1/50 patients) |
| Drug-Eluting Stent (DES) | 6.1% | 9.1% | 3.0% (1/33 patients) |
Data from study of 154 patients with symptomatic intracranial atherosclerotic stenosis [14]
Multivariate logistic regression analysis identified both endovascular treatment strategy and vessel distribution as significant independent risk factors for ISR within 6 months, with DES and DCB demonstrating superior performance compared to BMS [14].
Gene Therapy for Spinal Muscular Atrophy
The Phase III STEER trial investigated intrathecal onasemnogene abeparvovec (OAV101 IT), an investigational gene replacement therapy for spinal muscular atrophy (SMA), providing a robust example of rigorous efficacy evaluation in neuromodulation [15].
Experimental Protocol: This registrational study employed a sham-controlled design in treatment-naïve patients with SMA Type 2, aged 2 to <18 years, who could sit but had never walked independently. A total of 126 patients were randomized to receive either OAV101 IT (n=75) or a sham procedure (n=51). The primary endpoint was change from baseline to 52 weeks in Hammersmith Functional Motor Scale Expanded (HFMSE) score, a gold standard for SMA-specific assessment of motor function. At the end of the 52-week period, all eligible patients crossed over to receive the active treatment [15].
Key Efficacy Results: The trial met its primary endpoint, with OAV101 IT demonstrating a statistically significant 2.39-point improvement on the HFMSE compared to 0.51 points in the sham group (overall difference: 1.88 points; P=0.0074). All secondary endpoints consistently favored OAV101 IT, though they did not achieve statistical significance due to the pre-planned multiple testing procedure [15].
A companion Phase IIIb STRENGTH study evaluated OAV101 IT in patients who had discontinued previous SMA treatments (nusinersen or risdiplam), demonstrating stabilization of motor function over 52 weeks of follow-up, with an increase from baseline in HFMSE least squares total score of 1.05 [15].
Safety Assessment Frameworks Across Modalities
Long-Term Safety Profiling
Comprehensive safety evaluation requires extended follow-up periods to identify potential long-term risks. The five-year safety and efficacy outcomes of ofatumumab in patients with relapsing multiple sclerosis exemplify this approach [16].
Experimental Protocol: Safety was analyzed in 1,969 participants who received at least one dose of ofatumumab across multiple trial phases (ASCLEPIOS I/II, APLIOS, APOLITOS, or ALITHIOS). Researchers tracked exposure-adjusted incidence rates of adverse events, serious adverse events, serious infections, and malignancies over the five-year period [16].
Safety Outcomes: The analysis revealed consistent exposure-adjusted incidence rates per 100 patient-years for adverse events (124.65), serious adverse events (4.68), serious infections (1.63), and malignancies (0.32) through five years of follow-up, with no new safety signals identified. With ofatumumab treatment up to five years, over 80% of patients remained free of 6-month confirmed disability worsening [16].
Ethical Dimensions of Safety in Closed-Loop Systems
Closed-loop (CL) neurotechnology, which dynamically adapts to patients' neural states in real-time, introduces unique safety considerations that extend beyond conventional physical risks. A scoping review of 66 clinical studies involving CL systems revealed significant gaps in how ethical dimensions of safety are addressed [13].
Methodological Framework: The review analyzed peer-reviewed research on human participants to evaluate both the presence and depth of ethical engagement. The analysis employed thematic coding to identify key ethical themes, including beneficence (maximizing benefits while minimizing risks) and nonmaleficence (avoiding harm) [13].
Findings on Safety Reporting: Among the 66 reviewed studies, 56 addressed adverse effects, ranging from minor discomfort to severe complications requiring device removal. However, ethical considerations were typically addressed only implicitly, folded into technical or procedural discussions without structured analysis. Only one study included a dedicated assessment of ethical considerations, suggesting that ethics is not currently a central focus in most ongoing clinical trials of CL systems [13].
The review identified a concerning gap between regulatory compliance and meaningful ethical reflection, particularly regarding psychological safety, personal identity, and mental privacy. This highlights the need for safety evaluation frameworks that address both physical and ethical dimensions of risk [13].
Essential Research Reagents and Methodologies
Rigorous evaluation of neurotechnologies requires specialized research reagents and methodologies tailored to assess both functional outcomes and safety parameters across diverse neurological conditions.
Table 3: Essential Research Reagents and Methodologies for Neurotechnology Evaluation
| Research Tool | Application | Function in Evaluation |
|---|---|---|
| Hammersmith Functional Motor Scale Expanded (HFMSE) | Spinal Muscular Atrophy | Gold standard assessment of motor function and disease progression [15] |
| Modified Rankin Scale (mRS) | Stroke and Intracranial Stenosis | Evaluates disability levels and functional independence in daily activities [14] |
| Responsive Neurostimulation (RNS) System | Epilepsy | Closed-loop system detecting epileptiform activity and delivering targeted stimulation [13] |
| Digital Subtraction Angiography (DSA) | Intracranial Stenosis | Visualizes blood vessels to quantify stenosis degree and guide interventions [14] |
| Quality of Life in Epilepsy (QOLIE) Inventory | Epilepsy and Neurostimulation | Assesses quality of life impact beyond seizure frequency reduction [13] |
| Local Field Potentials (LFPs) | Adaptive Deep Brain Stimulation | Neural signals used as biomarkers for real-time adjustment of stimulation parameters [13] |
The selection of appropriate assessment tools must align with the specific neurotechnology and condition being studied. For motor function evaluation in SMA, the HFMSE provides validated, disease-specific metrics [15]. For vascular interventions, DSA offers precise anatomical visualization, while the mRS captures functional outcomes relevant to patients' daily lives [14]. In closed-loop systems, LFPs serve as critical biomarkers enabling real-time adaptation of therapeutic parameters [13].
The imperative for rigorous safety and efficacy evaluation in neurotechnology stems from both the profound potential benefits and significant risks associated with interfacing directly with the human nervous system. As the field expands rapidly—with dozens of technologies in development across mental health, healthy aging, and physical disability—robust evaluation frameworks must evolve in parallel [11]. The comparative data presented in this analysis demonstrate that methodological rigor, including controlled trial designs, standardized outcome measures, long-term safety monitoring, and comprehensive ethical oversight, is essential for responsible innovation [15] [14] [13]. Future development must bridge the identified gap between regulatory compliance and meaningful ethical reflection, particularly as technologies advance toward more sophisticated closed-loop systems and brain-computer interfaces [12] [13]. Only through such comprehensive evaluation can we ensure that neurotechnologies deliver on their promise to transform treatment for neurological and psychiatric disorders while safeguarding the fundamental aspects of human identity and autonomy.
The rapid advancement of neurotechnologies presents unprecedented opportunities for treating neurological disorders and restoring human function, while simultaneously creating complex regulatory challenges across international jurisdictions. Devices that interface directly with the central or peripheral nervous system can decode mental activity, with recent studies demonstrating astonishing capabilities—from decoding attempted speech in paralyzed patients with 97.5% accuracy to reconstructing visual imagery directly from brain scans [17]. These technological breakthroughs operate within a divergent global regulatory landscape, where the United States Food and Drug Administration (FDA) and European Union Medical Device Regulation (MDR) represent two dominant but significantly different frameworks for ensuring safety and efficacy [18] [19]. Simultaneously, the emergence of "neuro-rights" as a legal concept reflects growing international concern about protecting mental privacy and neural data integrity [20] [17]. For researchers, scientists, and drug development professionals working in neurotechnology, navigating these parallel pathways of device regulation and data protection requires careful strategic planning from the earliest stages of development through post-market surveillance.
Comparative Analysis: FDA vs. MDR Regulatory Frameworks
Fundamental Structural Differences
The FDA and EU MDR employ fundamentally different regulatory architectures, though both utilize risk-based classification systems. The FDA operates a centralized review process where the agency itself makes all approval decisions, while the MDR relies on a decentralized system where independent Notified Bodies conduct conformity assessments [21]. This structural difference creates varying timelines and consistency in review, as different Notified Bodies may interpret requirements slightly differently [21].
Philosophically, the frameworks also diverge in their core approaches. The FDA focuses primarily on whether a device is safe and effective for its intended use, often relying on substantial equivalence to existing predicates [21]. In contrast, the MDR takes a more performance-based approach, emphasizing clinical evaluation, post-market surveillance, and lifecycle safety even for moderate-risk devices [21].
Classification Systems Compared
Although both systems are risk-based, their classification structures differ significantly, leading to potential mismatches for specific neurotechnology devices:
Table 1: FDA vs. MDR Device Classification and Regulatory Pathways
| Aspect | US FDA | EU MDR |
|---|---|---|
| Risk Classes | Class I, II, III [18] | Class I, IIa, IIb, III [18] |
| Classification Basis | Intended use and product code [18] | 22 classification rules in Annex VIII [18] |
| Class I Devices | Most exempt from 510(k) but subject to General Controls [18] | Only standard Class I can be self-certified; sterile/measuring/reusable require Notified Body [18] |
| Class II/IIa Devices | Typically requires 510(k) demonstrating substantial equivalence [21] | Requires Notified Body assessment with clinical evidence [21] |
| Class III Devices | Premarket Approval (PMA) with clinical evidence [18] | Extensive clinical evaluation and Notified Body review [19] |
| Software Classification | Standalone software may be Class I [18] | Software typically Class IIa or higher [18] |
| Review Body | FDA directly reviews all submissions [19] | Notified Bodies conduct conformity assessments [19] |
Clinical Evidence Requirements
Clinical evidence requirements represent another significant divergence between the two frameworks. Under the MDR, clinical evaluation is an ongoing process throughout the device lifecycle, with particular emphasis on real-world clinical data and post-market clinical follow-up (PMCF) [19]. The FDA, in contrast, places greater emphasis on pre-market clinical trials, particularly for high-risk devices under the PMA pathway [19].
For neurotechnology devices specifically, the MDR typically requires Clinical Evaluation Reports (CER) for all Class III and some Class IIb devices, whereas the FDA does not require CER for most devices qualifying for 510(k) submission [19]. This discrepancy can significantly impact development timelines and resource allocation for neurotechnology companies planning regulatory strategy.
Emerging Neuro-Rights and Neural Data Protection Frameworks
The Expanding Definition of Neural Data
The regulatory landscape for neurotechnologies extends beyond device safety and efficacy to encompass emerging concerns about mental privacy and neural data protection. Neural data is uniquely sensitive because it can reveal intimate thoughts, memories, mental states, emotions, and health conditions—sometimes forecasting future behavior or health risks without conscious recognition by the individual [17]. The definition of neural data continues to evolve, generally encompassing information generated by measuring activity in both the central and peripheral nervous systems, whether obtained electrically, chemically, or via other means [17].
Internationally, prominent examples of neuro-rights legislation include Chile's pioneering 2021 constitutional amendment that protects "cerebral activity and the information drawn from it" as a constitutional right, which led to a 2023 Supreme Court ruling ordering a company to delete a consumer's neural data [17]. At the United Nations, a 2025 report by the Special Rapporteur on the right to privacy called for the development of a model law on neurotechnologies and neurodata processing to protect fundamental human rights [20].
United States Regulatory Landscape for Neural Data
The United States currently lacks comprehensive federal neural data protection legislation, but several important developments are shaping this emerging landscape:
Table 2: US Neural Data Privacy Legislation Overview
| Jurisdiction | Status | Key Provisions | Definition of Neural Data |
|---|---|---|---|
| Federal (MIND Act) | Proposed (Oct 2025) [22] | Directs FTC to study neural data processing, identify regulatory gaps, and make recommendations [22] | Information obtained by measuring activity of central or peripheral nervous system [22] |
| Colorado | Enacted [23] | Includes neural data in "sensitive data" requiring opt-in consent for collection/processing [23] | Information generated by measuring nervous system activity that can be processed with device assistance [23] |
| California | Enacted [23] | Includes neural data in "sensitive personal information" with limited opt-out rights [23] | Excludes data inferred from non-neural information [23] |
| Other States | Proposed (CT, IL, MA, MN, MT, VT) [23] | Varying approaches from opt-in consent to processing restrictions [23] | Definitions vary, with some including and excluding peripheral data [22] |
The proposed federal Management of Individuals' Neural Data Act of 2025 (MIND Act) would direct the Federal Trade Commission to study the collection, use, storage, transfer, and other processing of neural data, which "can reveal thoughts, emotions, or decision-making patterns" [22]. The Act would not immediately create new regulations but would establish a framework for future oversight, recognizing both the risks and beneficial uses of neurotechnology in medical, scientific, and assistive applications [22].
Ethical Implementation and Compliance Strategies
For researchers and developers, compliance with emerging neuro-rights frameworks requires implementing robust data governance protocols that align with both existing regulations and anticipated legislation. Key considerations include:
- Data Minimization: Collect only neural data strictly necessary for the intended medical or research purpose [23]
- Informed Consent: Develop transparent consent processes that explain neural data collection, use, and storage in comprehensible language [20]
- Security Safeguards: Implement enhanced cybersecurity protections for neural data storage and transfer [22]
- Purpose Limitation: Use neural data only for the purpose for which it was originally collected [23]
A 2024 analysis of thirty direct-to-consumer neurotechnology companies revealed significant privacy practice gaps, with all companies taking possession of users' neural data, most retaining unfettered access rights, and many permitting broad sharing with third parties [17]. These findings highlight the urgent need for standardized ethical practices across the industry.
Safety and Efficacy Evaluation Methodologies for Neurotechnology
Multidimensional Assessment Framework
Evaluating the safety and efficacy of neurotechnologies requires multifaceted considerations at cellular, circuit, and system levels, including neuroinflammation, cell-type specificity, neural circuitry adaptation, systemic functional effects, electrode material safety, and electrical field distribution [24]. Given the complexity of the nervous system, comprehensive assessment requires innovative methodologies across the preclinical-to-clinical continuum.
Table 3: Neurotechnology Safety and Efficacy Assessment Methods
| Method Type | Key Applications | Typical Metrics | Considerations for Neurotechnology |
|---|---|---|---|
| In silico Modeling | Electrical field prediction, parameter optimization [24] | Field distribution, current density, thermal effects | Limited by biological complexity; requires validation |
| In vitro Systems | Electrode material degradation, cytotoxicity [24] | Cell viability, material integrity, inflammatory markers | May not recapitulate neural tissue complexity |
| In vivo Animal Models | Tissue response, functional outcomes, behavioral effects [24] | Histopathology, neural signals, behavioral tasks | Species differences may limit translatability |
| Clinical Trials | Human safety and efficacy [25] | Adverse events, performance metrics, patient-reported outcomes | Limited parameter exploration; focused on benefit-risk |
Recent advances in electrical stimulation safety assessment have revealed the importance of considering bidirectional interactions—how neural tissue changes impact stimulation effectiveness, how electrical parameters affect electrode integrity, and how electrode degradation alters electrical field distribution [24]. These complex interactions necessitate sophisticated testing protocols that extend beyond traditional characterization methods.
Representative Experimental Protocol: Flow Diverter Evaluation
A May 2025 prospective multicenter observational study of a mechanical balloon-based flow diverter for intracranial aneurysms demonstrates a comprehensive approach to neurotechnology evaluation [25]. The study enrolled 128 patients with unruptured intracranial aneurysms between September 2019 and November 2021, employing the following methodology:
Primary Efficacy Endpoints:
- Immediate implantation success rate
- Successful aneurysm occlusion rate (Raymond I-II or OKM C-D) at 12-month follow-up
- Complete occlusion rate (Raymond I or OKM D) at 12-month follow-up
- Parent artery stenosis rate (>50%) at follow-up
Primary Safety Endpoints:
- All-cause mortality
- Adverse events (AEs) and neurological AEs
- Serious adverse events (SAEs)
- Incidence of cerebral hemorrhage
The study reported a 100% deployment success rate, with 91.4% of patients achieving successful occlusion and 85.9% achieving complete occlusion at 12 months, while safety outcomes included no mortalities or cerebral hemorrhage, with 4.69% neurological adverse events and 3.1% serious adverse events [25]. This comprehensive endpoint structure exemplifies the dual focus on both technical performance and patient safety required for neurotechnology evaluation.
Essential Research Reagents and Materials
Neurotechnology safety and efficacy research requires specialized reagents and materials for comprehensive evaluation:
Table 4: Essential Research Reagents for Neurotechnology Evaluation
| Reagent/Material | Application | Function in Evaluation |
|---|---|---|
| Primary Neuronal Cultures | In vitro safety testing [24] | Assess cytotoxicity and neuronal response to stimulation |
| Multi-electrode Arrays | In vitro and in vivo electrophysiology [24] | Record neural activity and network responses |
| Immunohistochemistry Kits | Tissue analysis [24] | Evaluate neuroinflammation and tissue damage markers |
| Electrode Materials | Device development [24] | Test biocompatibility and electrical properties |
| Conducting Polymers | Electrode coating [24] | Improve interface properties and reduce impedance |
| fMRI Contrast Agents | Large animal and human studies [17] | Visualize neural activity and connectivity changes |
| EEG/ERP Systems | Non-invasive assessment [17] | Measure brain activity patterns and responses |
| Biomechanical Testers | Material durability [24] | Evaluate device integrity under physiological conditions |
| Cytokine Assays | Inflammation monitoring [24] | Quantify neuroinflammatory responses to implantation |
| AI-Decoding Algorithms | Neural signal interpretation [17] | Translate neural data to intended outputs or commands |
Integrated Regulatory Strategy for Global Neurotechnology Development
For neurotechnology developers targeting global markets, an integrated regulatory strategy that addresses both device approval and data protection requirements is essential. Key strategic considerations include:
- Early Classification Analysis: Conduct parallel FDA and MDR classification assessments during initial design phases, paying particular attention to software components and invasive/non-invasive distinctions [18] [19]
- Clinical Evidence Planning: Develop clinical evaluation strategies that satisfy both FDA pre-market trial requirements and MDR's ongoing post-market clinical follow-up expectations [19]
- Neural Data Protections: Implement privacy-by-design principles that comply with both existing frameworks (like Colorado and California laws) and anticipated federal guidance [23]
- Quality Management Integration: Transition to Quality Management System Regulation (QMSR) aligning with ISO 13485:2016 to streamline compliance with both FDA and MDR requirements [26]
- Post-Market Surveillance: Establish robust systems that address both EU requirements for Periodic Safety Update Reports (PSUR) and FDA adverse event reporting [18]
The regulatory pathway selection should consider not only time-to-market but also long-term compliance requirements. While FDA approval may offer faster entry for some moderate-risk devices through 510(k) pathways, the comprehensive clinical evidence required under MDR, though more resource-intensive initially, may provide competitive advantages in global markets [21].
Navigating the complex interplay between FDA device regulations, MDR requirements, and emerging neuro-rights frameworks presents significant challenges for neurotechnology researchers and developers. The divergent classification systems, clinical evidence expectations, and review processes between major markets necessitate early strategic planning and ongoing compliance vigilance. Simultaneously, the rapidly evolving landscape of neural data protection requires proactive implementation of ethical data practices that respect mental privacy while enabling beneficial medical applications. By adopting integrated development approaches that address safety, efficacy, and data protection in parallel—rather than sequentially—neurotechnology innovators can position themselves for sustainable success across global markets while maintaining public trust in these transformative technologies.
The rapid advancement of neurotechnology presents a dual frontier of therapeutic promise and significant safety challenges. As implantable devices such as deep brain stimulation (DBS) systems and closed-loop neurotechnologies become increasingly sophisticated, a comprehensive understanding of their risk profiles becomes essential for researchers, clinicians, and developers. The integration of artificial intelligence and adaptive algorithms in these systems introduces novel safety considerations that extend beyond traditional surgical risks to encompass psychological, identity, and data privacy dimensions [27] [28]. This analysis systematically compares safety risks across multiple neurotechnologies, providing structured experimental data and methodologies to inform safety efficacy evaluation in neurotechnology research.
Comparative Safety Risk Profiles of Major Neurotechnologies
Table 1: Quantitative Safety Data for Implantable Neurotechnologies
| Device Type | Most Common Surgical Complications | Most Common Device-Related Issues | Reported Psychological Effects | Frequency of Serious Adverse Events |
|---|---|---|---|---|
| Deep Brain Stimulation (DBS) | Infections (1-8%), lead misplacement [29] | High impedance, battery problems, unintended stimulation changes [29] | Worsening anxiety/depression, manic symptoms (in rare cases) [29] | 27% of high-risk devices recalled; serious psychological events in subset of patients [29] |
| Vagus Nerve Stimulation (VNS) | Surgical complications, infection [29] | High impedance, incorrect frequency delivery, battery issues [29] | Voice alteration, laryngeal adverse effects (187 reports out of 12,725 issues) [29] | 449 death reports among 5,888 complications (2011-2021); causality not always established [29] |
| Spinal Cord/Dorsal Root Ganglion Stimulation | Lead migration, pocket pain, muscle spasms [29] | Device-related complications (almost 50% of reports) [29] | Not prominently reported | Surgical revision required in majority of complications; serious events like epidural hematomas (<0.2%) [29] |
| Responsive Neurostimulation (RNS) | Surgical site infections, implantation complications [28] | System removal required in some cases [28] | Not systematically assessed in most studies | 8 of 66 reviewed studies reported system removal [28] |
Table 2: Psychological and Identity-Related Safety Concerns
| Psychological Risk Domain | Reported Prevalence | Contextual Factors | Assessment Methodologies |
|---|---|---|---|
| Personality Changes | Limited evidence for widespread negative changes; some reports of positive restorative effects [30] | Often related to adjustment to symptom relief rather than direct device effects [30] | Qualitative interviews, standardized personality inventories [30] |
| Impact on Identity/Authenticity | Majority report unchanged or restored pre-disorder identity; rare cases of alienation [30] | Mediated by thorough pre-surgical evaluation and post-operative care [30] | Prospective studies with pre/post assessment; feelings of autonomy and control measures [30] |
| Autonomy & Agency Concerns | Increased feelings of control and self-regulation reported in many patients post-DBS [30] | Related to regaining functional capabilities rather than loss of agency [30] | Neuroethics scales, patient-reported outcomes, authenticity measures [30] |
Experimental Protocols for Safety Assessment
MAUDE Database Analysis Methodology
The FDA's Manufacturer and User Facility Device Experience (MAUDE) database provides critical post-market surveillance data for neurotechnology safety assessment. A standardized protocol for analyzing this data involves:
Data Extraction: Collect all reports for specific device codes over defined time periods (typically 5-10 years for sufficient power) [29].
Categorization Framework: Classify adverse events into:
- Device malfunctions (hardware/software failures)
- Procedural complications (surgical and implantation-related)
- Clinical adverse events (psychological, neurological, systemic)
- Patient complaints (subjective experiences) [29]
Causality Assessment: Differentiate between device-related events and those with unclear relationship to the device.
Statistical Analysis: Calculate frequencies, proportions, and trends over time while acknowledging limitations of voluntary reporting systems.
This methodology was applied in a VNS analysis spanning 2011-2021 that identified 5,888 complications, enabling quantification of laryngeal adverse effects as the eighth most common vagus nerve problem [29].
Long-Term Safety Monitoring Protocol
The BrainGate clinical trial exemplifies rigorous long-term safety assessment for implanted brain-computer interfaces:
Duration: Implants maintained for extended periods (average over 2 years in BrainGate) to identify delayed complications [29].
Safety Endpoints: Monitor for:
- Device explantation requirements
- Death or permanently increased disability
- Infection rates (particularly intracranial)
- Unanticipated adverse device events [29]
Systematic Documentation: Use standardized reporting forms for all adverse events regardless of perceived relationship to device.
Independent Adjudication: Utilize data safety monitoring boards to evaluate event causality.
This protocol established the safety of the BrainGate system with no explantation-requiring events, no intracranial infections, and no device-related deaths or permanent disabilities among 14 participants over a 17-year period [29].
Sandbox Testing for Predictive Safety Validation
Researchers have proposed "sandbox" environments for predictive safety testing of neurotechnologies before human implantation:
Figure 1: Sandbox testing workflow for neurotechnology safety validation.
The experimental workflow involves:
Model Development: Create computational simulations of neural circuitry and tissue-electrode interfaces based on biophysical principles [27].
Device Integration: Interface actual device hardware or software with simulated biological environments.
Scenario Testing: Expose the device to simulated edge cases, rare neural states, and failure modes that would be unethical or impractical to test in humans [27].
Iterative Refinement: Use results to modify device parameters and algorithms to minimize identified risks.
This approach enables identification of latent failure modes and optimization of safety measures while reducing dependency on animal and early human trials [27].
Research Reagent Solutions for Neurotechnology Safety Research
Table 3: Essential Research Tools for Safety Assessment
| Research Tool Category | Specific Examples | Research Application in Safety Assessment |
|---|---|---|
| Adverse Event Databases | FDA MAUDE database, Medical Device Recalls database [29] | Post-market surveillance; identification of rare complications; trend analysis across device types and time periods |
| Standardized Assessment Scales | QOLIE-31, QOLIE-89 (Quality of Life in Epilepsy), neuroethics scales [28] [13] | Quantifying impact on quality of life; standardizing psychological and identity-related outcome measures across studies |
| Computational Modeling Platforms | Virtual patient avatars, in silico neural networks, digital twins [27] | Simulating device-tissue interactions; predicting long-term effects; testing safety parameters in simulated environments |
| Clinical Trial Safety Endpoints | Procedure-related complications, system removal rates, serious adverse event frequency [28] [29] | Standardized safety monitoring in clinical studies; comparison across device platforms and patient populations |
Emerging Safety Paradigms and Research Gaps
The evolution of closed-loop neurotechnologies introduces unique safety challenges that conventional frameworks inadequately address. Current clinical studies demonstrate significant gaps in systematic ethical and safety assessment, with only 1 of 66 reviewed studies including dedicated ethical evaluation [28] [13]. Most ethical considerations remain implicit in technical discussions rather than receiving structured analysis.
The emerging "sandbox" approach represents a paradigm shift toward proactive safety engineering for neurotechnologies. By creating isolated testing environments where devices can be rigorously evaluated against simulated biological variability and edge cases, developers can identify and mitigate risks before human trials [27]. This methodology is particularly valuable for adaptive systems incorporating machine learning, whose behavior may evolve in unpredictable ways post-deployment.
Future safety research must address critical gaps including:
- Long-term effects of continuous neural monitoring and stimulation
- Standardized assessment of identity and agency impacts
- Cybersecurity vulnerabilities in connected neurodevices
- Equity in safety profiles across diverse patient populations [28] [12]
Comprehensive safety efficacy evaluation requires integration of quantitative device performance data, systematic psychological assessment, and robust post-market surveillance to balance therapeutic innovation with responsible development.
The direct-to-consumer (DTC) neurotechnology market represents a rapidly expanding sector at the intersection of neuroscience, consumer electronics, and digital health. These products, which interface with the nervous system to monitor, stimulate, or modulate neural activity, are increasingly marketed directly to consumers without requiring physician intermediaries [31] [32]. The global neurotechnology market is projected to reach significant value, with some estimates exceeding $50 billion by 2034, fueled by advances in neuroscience, materials science, and artificial intelligence [33] [32]. This growth reflects increasing consumer interest in technologies that promise cognitive enhancement, mental wellness monitoring, and alternative therapeutic interventions.
Unlike medically approved neurotechnologies that undergo rigorous clinical validation and regulatory scrutiny, most DTC products occupy a regulatory gray zone [34]. Manufacturers often market these devices as "wellness" products rather than medical devices, thereby bypassing the stringent premarket approval processes required for medical claims [31] [34]. This regulatory positioning creates significant challenges for evaluating product efficacy and safety, leaving consumers with limited protection against unsubstantiated claims and potential harms [34] [32]. The situation parallels historical challenges with dietary supplements, where limited premarket oversight has resulted in markets flooded with products of dubious effectiveness [31].
Efficacy Assessment: Methodological Frameworks and Comparative Performance
Evaluating DTC neurotechnology efficacy requires understanding both the scientific foundations of these technologies and the methodological limitations of consumer-grade implementations. The translation from laboratory research to consumer products often involves significant compromises in design, application, and validation that undermine efficacy claims.
Comparative Performance Analysis of Major DTC Neurotechnology Categories
Table 1: Efficacy Evidence and Limitations Across DTC Neurotechnology Categories
| Product Category | Stated Claims & Applications | Evidence Base | Key Efficacy Limitations |
|---|---|---|---|
| Consumer EEG Devices (e.g., NeuroSky) | Mental state monitoring (focus, stress, meditation) [31] | Laboratory EEG research; limited independent validation of consumer devices [31] | Different electrode configurations and placement by users vs. research-grade systems; classification algorithms often proprietary and unvalidated; potential for erroneous feedback causing psychological harm [31] |
| Transcranial Direct Current Stimulation (tDCS) | Cognitive enhancement, mood improvement [31] | Mixed results in controlled studies; debate about cognitive effects [35] | Questionable applicability of laboratory findings to consumer devices; variability in electrode placement; small effect sizes in meta-analyses; skin burns reported [31] |
| Cognitive Training Applications (e.g., Lumosity) | Improved memory, attention, generalizable cognitive benefits [31] | Some task-specific improvements; limited transfer to untrained cognitive domains [31] | Narrow training effects that often fail to generalize to real-world cognitive tasks; questionable practical significance of statistically significant improvements [31] |
| Mental Health Apps (e.g., meditation, mood tracking) | Stress reduction, mental health management [31] | Variable study quality; potential placebo effects [31] | Lack of professional support structures; uncertain efficacy compared to standard care; privacy concerns with sensitive data [31] [34] |
Experimental Protocols for Efficacy Evaluation
Rigorous assessment of DTC neurotechnology efficacy requires standardized methodologies that can validate manufacturer claims and identify potential limitations. The following experimental frameworks represent best practices for evaluating these technologies.
Protocol for Neurofeedback and EEG Device Validation
Objective: To evaluate the classification accuracy and signal reliability of consumer EEG devices in detecting claimed mental states (e.g., focus, stress, meditation) compared to research-grade systems [31].
Methodology:
- Participant Recruitment: N=40 healthy adults (balanced gender, 18-65 years)
- Equipment Setup: Simultaneous recording with consumer device (test unit) and research-grade EEG system (reference standard)
- Task Protocol:
- Resting State Baseline: 5 minutes eyes open, 5 minutes eyes closed
- Focused Attention: 20-minute continuous performance task with varying difficulty levels
- Stress Induction: 15-minute timed arithmetic task with social evaluation component
- Meditation: 15-minute guided mindfulness practice
- Data Analysis:
- Correlation of band power (alpha, beta, theta, gamma) between systems across conditions
- Comparison of mental state classification accuracy using manufacturer algorithms vs. research-grade feature extraction
- Test-retest reliability assessment across two sessions separated by 7 days
Validation Metrics: Inter-device correlation coefficients (>0.8 target), classification accuracy (>80% target), within-subject consistency (intraclass correlation coefficient >0.7) [31].
Protocol for Neurostimulation Cognitive Effects
Objective: To assess the impact of consumer tDCS devices on cognitive performance in domains matching marketing claims (e.g., working memory, attention) [31] [35].
Methodology:
- Study Design: Randomized, double-blind, sham-controlled trial with crossover design
- Participants: N=60 healthy adults (stratified by age and baseline cognitive performance)
- Intervention:
- Active Stimulation: Manufacturer-recommended parameters (e.g., 2mA for 20 minutes, electrode placement Fp3/Fp4)
- Sham Stimulation: Identical setup with 30-second ramp-up/down and no sustained stimulation
- Outcome Measures (assessed pre-, immediately post-, and 24 hours post-stimulation):
- Working Memory: N-back task (2-back, 3-back)
- Attention: Continuous performance task (reaction time, variability, commission errors)
- Executive Function: Task-switching paradigm (mixing costs, switch costs)
- Safety Monitoring: Skin assessment, adverse effect questionnaire, dropout rates
Statistical Analysis: Mixed-effects models accounting for period, sequence, and treatment effects; minimal clinically important difference thresholds established a priori [35].
Regulatory Landscape: Current Frameworks and Identified Gaps
The regulatory environment for DTC neurotechnologies remains fragmented, with significant variations in oversight approaches across jurisdictions and product categories. This regulatory patchwork creates challenges for consistent consumer protection and reliable product evaluation.
Comparative Analysis of Regulatory Approaches
Table 2: Regulatory Frameworks and Limitations for DTC Neurotechnologies
| Regulatory Mechanism | Scope & Authority | Key Strengths | Identified Insufficiencies |
|---|---|---|---|
| FDA Medical Device Regulation | Products making medical claims (disease treatment/diagnosis) [31] | Rigorous premarket review for safety and effectiveness; established classification system (I, II, III) based on risk [31] | "Wellness" products can bypass regulation by limiting claims; 2019 guidance clarified non-enforcement for low-risk wellness products [31] [34] |
| Federal Trade Commission (FTC) Oversight | Deceptive advertising practices [31] | Can take action against false marketing claims; has pursued cases against brain training companies [31] | Reactive rather than proactive approach; requires demonstrated deception; limited resources to monitor thousands of products [31] [34] |
| EU Medical Device Regulation (MDR) | Medical devices and certain non-medical devices per Annex XVI [32] | Broader scope than FDA in some areas; includes some non-medical brain stimulation equipment [32] | Still evolving implementation; distinction between medical and wellness uses creates potential gaps [32] |
| Self-Regulation & Working Groups | Industry standards and independent evaluations [31] | Flexibility to adapt to rapidly changing technologies; can provide consumer education [31] | Limited enforcement power; potential conflicts of interest; variable adoption [31] |
Regulatory Pathways and Decision Framework
The following diagram illustrates the complex regulatory pathways and decision points that determine the oversight level for neurotechnologies, highlighting where regulatory gaps emerge:
Regulatory Pathway Decision Flow
This diagram illustrates how most DTC neurotechnologies bypass rigorous FDA oversight by making only wellness claims, falling into a regulatory gap with primarily reactive FTC protection against deceptive marketing [31] [34].
Research Toolkit: Essential Methodologies and Reagents
Comprehensive evaluation of DTC neurotechnologies requires specialized research tools and methodologies to assess both their technical performance and biological effects.
Key Research Reagent Solutions
Table 3: Essential Research Materials for DTC Neurotechnology Evaluation
| Research Tool Category | Specific Examples & Applications | Function in Evaluation |
|---|---|---|
| Reference Standard Recording Systems | Research-grade EEG (e.g., 256-channel systems), fMRI, MEG [31] [12] | Provide gold-standard measurement of neural activity for validating consumer device signal accuracy [31] |
| Behavioral Task Platforms | Cognitive test batteries (CANTAB, NIH Toolbox), specialized paradigms (N-back, flanker, Stroop) [31] | Objective assessment of cognitive claims (memory, attention) under controlled conditions [31] |
| Biomarker Assays | Plasma pTau-181, pTau-217, GFAP, neurofilament light chain (NfL) [36] | Assessment of potential neurobiological effects in clinical populations; used in recent Alzheimer's device trials [36] |
| Signal Processing Tools | Open-source algorithms (EEGLAB, FieldTrip), custom classification pipelines [31] | Independent analysis of neural data quality and feature extraction validity [31] |
| Safety Assessment Materials | Skin impedance measurement tools, adverse effect structured interviews, thermal cameras [31] [35] | Objective evaluation of physical safety parameters and side effect profiles [31] |
| (R)-2-Phenylpropylamide | (R)-2-Phenylpropylamide | High-Purity Chiral Reagent | High-purity (R)-2-Phenylpropylamide for research. A key chiral building block for asymmetric synthesis & medicinal chemistry. For Research Use Only. Not for human or veterinary use. |
| Benzamide, N,N,4-trimethyl- | Benzamide, N,N,4-trimethyl-, CAS:14062-78-3, MF:C10H13NO, MW:163.22 g/mol | Chemical Reagent |
Experimental Workflow for Comprehensive Device Evaluation
The following diagram outlines a systematic approach for evaluating DTC neurotechnologies, incorporating both technical validation and assessment of functional claims:
Comprehensive Device Evaluation Workflow
This workflow emphasizes the multi-phase approach necessary to thoroughly evaluate DTC neurotechnologies, from technical validation through functional assessment and safety profiling [31] [35] [36].
The DTC neurotechnology market presents significant challenges regarding efficacy validation and regulatory oversight. Current evidence suggests substantial gaps between marketing claims and scientifically demonstrated effects across multiple product categories [31]. These efficacy concerns are exacerbated by a regulatory framework that permits many products to reach consumers without rigorous premarket evaluation [31] [34].
Addressing these challenges requires a multi-faceted approach including enhanced regulatory clarity, independent evaluation mechanisms, and standardized methodological frameworks for device assessment [31] [32]. The development of an independent working group to evaluate DTC neurotechnologies—similar to models proposed in the literature—could provide much-needed objective assessment while balancing innovation promotion and consumer protection [31]. Furthermore, increased funding for research specifically examining the safety and efficacy of consumer neurotechnologies would help address current evidence gaps and inform both regulatory policy and consumer decision-making [31].
As the neurotechnology landscape continues to evolve at a rapid pace, establishing robust, scientifically-grounded evaluation frameworks becomes increasingly urgent to ensure that consumer products deliver meaningful benefits while minimizing potential harms.
Advanced Methodologies for Testing and Clinical Translation
The evaluation of safety and efficacy represents a critical foundation in the development of neurotechnologies and therapeutic agents. Traditional preclinical approaches have historically relied on a sequential pipeline progressing from in vitro (in glass) studies to in vivo (in living organism) animal testing. However, the landscape of biomedical research is undergoing a profound transformation driven by technological innovation. The emergence of sophisticated in silico (computational) modeling and advanced, human-relevant in vitro systems is rewriting the rules of preclinical research [37]. These innovative models offer unprecedented opportunities to understand complex biological mechanisms, enhance predictive accuracy, and adhere to ethical principles, thereby accelerating the translation of novel neurotechnologies from bench to bedside. This guide provides a comparative analysis of these three pillars—in silico, in vitro, and in vivo—within the context of neurotechnology safety and efficacy evaluation, supporting a broader thesis that integrated, human-relevant approaches are essential for future progress.
Model Definitions and Core Characteristics
The modern preclinical toolkit encompasses three distinct but complementary methodologies. In silico models use computer simulations to model biological systems, from molecular drug-target interactions to whole-organ physiology [38] [37]. In vitro models involve studying biological components, such as cells or tissues, in a controlled laboratory environment outside their native context [39]. In vivo models involve studying biological processes within a living organism, typically an animal model, to assess integrated system-level responses [40] [39].
Table 1: Core Characteristics of Preclinical Models
| Feature | In Silico Models | In Vitro Models | In Vivo Models |
|---|---|---|---|
| Definition | Computer-based simulations of biological processes [38] [37] | Cells or tissues studied in an artificial, non-living environment [39] | Studies conducted within a living organism [40] |
| Typical Applications | Target-drug dynamics, disease progression modeling, toxicity prediction, pharmacokinetics [38] [37] | Drug screening, molecular pathway analysis, basic cell behavior, co-culture studies [40] [41] | System-level efficacy, toxicity, pharmacokinetics, behavioral studies, complex disease phenotypes [40] |
| Fundamental Principle | Computational abstraction and simulation of biology | Isolation and control of biological variables | Preservation of full biological complexity |
| Key Strength | High-throughput, mechanistic insight, can simulate unobservable processes [38] | High control over variables, amenable to human-derived cells, often high-throughput [39] | Provides full physiological context; historical gold standard for system-level prediction [40] [39] |
| Inherent Limitation | Dependent on quality of input data and model assumptions; can be a "black box" [38] [37] | Simplified environment; lacks systemic interactions [41] [39] | Species differences; ethical concerns; high cost and low throughput [40] [37] [39] |
Comparative Analysis in Neurotechnology and Drug Development
Each model class offers a unique set of advantages and limitations, making them suited for different stages of the research and development pipeline.
In Silico Approaches
In silico modeling has shifted from a complementary tool to a critical component in early-stage development pipelines [38]. In neurotechnology, these models are used to simulate the safety and efficacy of electrical stimulation devices by modeling neuronal and non-neuronal responses at cellular, circuit, and system levels [24]. For drug development, target-drug dynamic simulations use molecular docking, molecular dynamics simulations, and AI-augmented models to predict how a therapeutic agent interacts with its biological target [38].
Key Advantages:
- Mechanistic Insight: Techniques like molecular dynamics simulations can reveal interaction patterns (e.g., hydrogen bonds, binding site flexibility) that static experiments cannot capture, allowing for early refinement of drug leads [38].
- Speed and Cost-Efficiency: Virtual screening of large compound libraries can drastically reduce the number of molecules that require synthesis and wet-lab testing, accelerating lead prioritization [38].
- Predictive ADMET: AI models are increasingly effective at predicting a compound's absorption, distribution, metabolism, excretion, and toxicity (ADMET) profiles, helping to weed out problematic candidates early [38].
- Scalability and Ethics: Computational models can evaluate millions of compounds and reduce reliance on animal testing, aligning with the 3R (Replacement, Reduction, Refinement) principles [38] [37].
Key Limitations:
- Model Accuracy: Predictions are highly dependent on the quality of input data. Many targets lack high-resolution structures, and using homology models can lead to inaccurate results [38].
- Computational Cost: While molecular docking is relatively cheap, accurate molecular dynamics or free energy calculations require substantial computational resources [38].
- Data Bias: AI/machine learning models can be biased if trained on limited or non-representative datasets, particularly for under-studied targets, leading to over-optimistic predictions [38].
- Regulatory Hurdles: Regulatory agencies often require reproducible experimental data, and the acceptance of in silico data as primary evidence is still evolving, though this is changing rapidly [38] [37].
In Vitro Approaches
In vitro models range from simple two-dimensional (2D) monolayer cell cultures to advanced three-dimensional (3D) systems like spheroids, organoids, and organ-on-a-chip devices [40] [41] [39]. In neurotechnology, these models are crucial for testing the biocompatibility of implant materials and understanding cellular responses to electrical stimulation [24] [41].
Key Advantages:
- High Control and Throughput: Researchers maintain precise control over the cellular environment (nutrients, temperature, etc.), making these systems ideal for high-throughput drug screening and mechanistic studies [40] [39].
- Use of Human Cells: Advanced models like Organ-Chips can be constructed with human cells, circumventing the issue of species translatability that plagues animal models [39].
- Bridging the Gap: Advanced 3D in vitro models, such as organoids and Organ-Chips, expose cells to biomechanical forces, fluid flow, and heterogeneous cell populations, encouraging more in vivo-like behavior and improving translational value [41] [39].
Key Limitations:
- Simplified Environment: Even advanced 3D models cannot fully recapitulate the systemic complexity of a living organism, including integrated immune, endocrine, and neural networks [40] [41].
- Artificial Mutations: Immortalized cell lines, commonly used in 2D culture, may develop mutations that cause them to behave abnormally, reducing their predictive power [39].
In Vivo Approaches
In vivo models, typically in animals, remain the gold standard for assessing complex outcomes like behavior, systemic toxicity, and therapeutic efficacy in an intact organism [40] [39]. They are essential for studying phenomena such as neuroinflammation, circuit-level neural adaptation, and systemic functional effects of neuromodulation [24].
Key Advantages:
- Full Physiological Context: Provides the most accurate representation of how cells and tissues function within a complete, living system, accounting for metabolism, immune responses, and organ-organ interactions [39].
- Complex Phenotypes: Ideal for studying complex disease processes, such as tumor heterogeneity and metastasis, which are difficult to model in vitro [40].
Key Limitations:
- Species Differences: Genetic and physiological differences between animals and humans can erode the predictive accuracy of these models, particularly in preclinical drug safety testing [37] [39].
- Ethical and Regulatory Concerns: The use of animals in research is fraught with ethical considerations and is subject to increasingly stringent regulatory requirements [40] [37].
- High Cost and Low Throughput: Animal studies are expensive, labor-intensive, and low-throughput, making them unsuitable for large-scale screening [40].
Table 2: Quantitative Comparison of Model Performance and Utility
| Criterion | In Silico Models | Simple 2D In Vitro | Advanced 3D In Vitro | In Vivo Models |
|---|---|---|---|---|
| Relative Cost | Low (after development) | Low [39] | Moderate [41] | Very High [40] [37] |
| Throughput | Very High (can screen millions) [38] | High [39] | Moderate [41] | Low |
| Human Relevance | Variable (depends on data and model) | Low to Moderate [39] | High (if using human cells) [41] [39] | Low to Moderate (due to species differences) [39] |
| Regulatory Acceptance | Growing (e.g., FDA Modernization Act 2.0) [37] | Established for specific endpoints | Emerging | Established gold standard [40] |
| Data Output | Predictive simulations & KPIs | Cellular viability, toxicity, pathway data | Complex cell-cell interactions, tissue-level responses | Systemic efficacy, toxicity, behavioral data [40] |
| Example Neurotech Application | Simulating electrical field distribution & neural activation [24] | Testing electrode material cytotoxicity on neuronal cell lines [24] [41] | 3D co-culture of neurons/glia to model implant-associated infection [41] | Evaluating seizure reduction or motor function recovery post-stimulation |
Experimental Protocols and Methodologies
Protocol for In Silico Target-Drug Dynamics
This protocol outlines the steps for simulating drug binding to a biological target, a key application in central nervous system (CNS) drug discovery [38].
- Target Preparation: Obtain a high-resolution 3D structure of the target protein (e.g., a neuronal receptor) from a protein data bank. If an experimental structure is unavailable, create a homology model using a related template, and verify the model against known ligands [38].
- Ligand Preparation: Generate 3D structures of the small molecule drug candidates. Assign appropriate bond orders, formal charges, and optimize the geometry using molecular mechanics force fields.
- Molecular Docking: Define the binding site on the target protein. Use docking software (e.g., AutoDock Vina, Glide) to computationally predict the preferred orientation (pose) and binding affinity of each ligand within the binding site.
- Molecular Dynamics (MD) Simulation: Subject the top-ranked docking poses to MD simulation. Place the protein-ligand complex in a solvated box with ions, and use a force field (e.g., AMBER, CHARMM) to simulate atomic movements over time (nanoseconds to microseconds). This assesses the stability of the binding pose and captures conformational changes [38].
- Free Energy Calculations: For the most stable complexes, perform more computationally intensive calculations (e.g., Free Energy Perturbation, FEP) to obtain a quantitative estimate of the binding free energy, which correlates more closely with experimental binding affinity [38].
- Validation: Cross-validate predictions with small-scale experimental data (e.g., a binding assay) whenever possible to guide and correct the computational models [38].
Protocol for Establishing a 3D In Vitro Model for Implant-Associated Infection
This protocol is relevant for testing the safety of neural implants by modeling bacterial infection at the material-tissue interface [41].
- Scaffold Selection and Preparation: Choose a 3D scaffold material that mimics the implant environment (e.g., a hydrogel or a rigid scaffold like ß-TCP). Sterilize the scaffold (e.g., UV light, ethanol, autoclave) and pre-condition it with cell culture medium.
- Cell Seeding: Seed relevant human cell types onto the scaffold. For a neural implant model, this could involve co-culturing neurons, astrocytes, and microglia. Cells can be mixed with the scaffold material before gelling or seeded on top.
- Tissue Maturation: Culture the 3D construct in an appropriate medium, potentially using a bioreactor or transwell system to provide nutrient exchange and mechanical cues, for a period sufficient for the cells to form tissue-like structures [41].
- Bacterial Challenge: Introduce a relevant bacterial strain (e.g., Staphylococcus aureus) at a predetermined multiplicity of infection (MOI) to the surface of the 3D model to simulate contamination.
- Co-Culture and Analysis: Co-culture cells and bacteria for a set duration. Analyze the outcome using a combination of methods [41]:
- Cell Viability Assays: e.g., Live/Dead staining.
- Molecular Methods: qPCR to measure cytokine expression from host cells and bacterial load.
- Microscopy/Histology: Confocal microscopy or histological staining to visualize biofilm formation and host-cell integration.
Workflow for Integrated Model Validation
The most powerful modern approaches integrate multiple models. The following diagram illustrates a workflow for validating an in silico prediction using a tiered experimental approach, a key concept in the evolving regulatory landscape.
Diagram 1: A sequential workflow for validating in silico predictions. This reduces animal use and refines hypotheses before in vivo testing.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Reagent Solutions for Preclinical Models
| Item | Function/Application | Example in Context |
|---|---|---|
| Molecular Docking Software (e.g., AutoDock Vina, Glide) | Predicts binding orientation and affinity of a small molecule to a protein target [38]. | Screening a compound library against a neuronal ion channel target. |
| Molecular Dynamics Software (e.g., GROMACS, NAMD) | Simulates the physical movements of atoms and molecules over time, assessing the stability of a protein-ligand complex [38]. | Observing conformational changes in a receptor upon drug binding. |
| 3D Scaffold Materials (e.g., Hydrogels, ß-TCP) | Provides a three-dimensional structure for cells to grow on, mimicking the natural extracellular matrix [41]. | Creating a 3D brain-on-a-chip model to test neural electrode integration. |
| Organ-on-a-Chip (Organ-Chip) | Microfluidic devices containing living human cells that emulate the structure and function of human tissues and organs [39]. | Modeling the blood-brain barrier to assess drug permeability for neurological diseases. |
| Patient-Derived Organoids | 3D mini-organs derived from human stem cells that recapitulate key aspects of the source organ's complexity [40]. | Studying disease-specific neural development or screening personalized therapies. |
| Genetically Engineered Mouse Models | Animals with modified genes to study the function of a specific gene or to model a human disease [40]. | Investigating the role of a specific gene in a neurodegenerative disease like Parkinson's. |
| 4-Methylcyclohexane-1,3-diamine | 4-Methylcyclohexane-1,3-diamine, CAS:13897-55-7, MF:C7H16N2, MW:128.22 g/mol | Chemical Reagent |
| N-Allyl-4-chloroaniline | N-Allyl-4-chloroaniline|CAS 13519-80-7 |
The paradigm of preclinical research is shifting from a reliance on sequential, siloed models toward an integrated, human-relevant framework. In silico models offer unparalleled speed and mechanistic insight, advanced in vitro systems bridge the gap between traditional cell culture and whole organisms, and in vivo models remain crucial for understanding system-level complexity. The future of neurotechnology safety and efficacy evaluation lies not in choosing one model over another, but in strategically combining them. Hybrid workflows that leverage AI-driven simulations, human cell-based advanced in vitro models, and targeted in vivo validation will dominate the next decade of research [38] [37]. As regulatory science evolves to accept this multi-faceted evidence, failure to employ these integrated methodologies may not merely be seen as outdated—it may be considered an ethical and scientific shortcoming [37].
The Role of Sandbox Environments for Implantable Neurotechnology Validation
Implantable neurotechnologies, such as invasive Brain-Computer Interfaces (iBCIs) and neural prostheses, represent a frontier in medical science with the potential to restore functions for individuals with neurological disorders. However, their path to clinical use is obstructed by technical, ethical, and regulatory complexities. Regulatory sandboxes have emerged as a promising controlled environment to test these innovative products under a tailored, supervised regime, aiming to balance accelerated innovation with rigorous safety and efficacy evaluation [42] [27]. This guide objectively compares the sandbox approach against traditional validation pathways, providing a structured analysis for researchers and development professionals.
Comparative Frameworks for Neurotechnology Validation
The table below compares the core characteristics of the sandbox approach against traditional regulatory pathways for implantable neurotechnology validation.
Table 1: Comparison of Validation Pathways for Implantable Neurotechnologies
| Characteristic | Regulatory Sandbox Approach | Traditional Regulatory Pathway |
|---|---|---|
| Core Functional Rationale | To sustain and shape novel technologies; participatory and adaptive development [42]. | To verify compliance with predefined standards [42]. |
| Process Design | Iterative, circular procedures with continuous feedback loops [42]. | Linear proceedings from application to decision [42]. |
| Regulatory Flexibility | Allows for derogation from specific legal obligations to test scientific outcomes while preserving overarching objectives [42]. | Strict adherence to existing regulatory requirements with limited flexibility. |
| Primary Objective | Enable innovation and development while addressing medical, ethical, and socio-economic challenges [42]. | Verify safety and efficacy based on established, often rigid, benchmarks. |
| Risk Management | Adaptive, supervised long-term risk management integrated into the development process [42]. | Primarily pre-market risk assessment, with post-market surveillance. |
| Stakeholder Involvement | Highly participatory, systematically involving innovators, patients, clinicians, and ethicists [42]. | Limited, often confined to interactions between the manufacturer and regulatory authority. |
The validation of medical devices, including neurotechnologies, is a growing field, with the global market for validation and verification services projected to experience a robust compound annual growth rate (CAGR) from 2025 to 2033 [43]. This underscores the critical importance of establishing robust validation frameworks.
Experimental Protocols and Methodologies in Sandboxes
Sandboxes enable the use of sophisticated experimental protocols that are less feasible in traditional clinical trials. The methodologies below are foundational for validating implantable neurotechnologies within these controlled environments.
Protocol 1: In-Silico Validation Using Digital Twins
Objective: To uncover latent failure modes and optimize control algorithms using computational models before human implantation [27].
- Step 1 – Model Creation: Develop patient-specific digital avatars (digital twins) that replicate intricate electrophysiological phenomena, tailored to reflect inter-individual variability and pathological heterogeneity [27] [44].
- Step 2 – Scenario Simulation: Simulate a multitude of brain states, environmental stimuli, and pathological scenarios within the sandboxed testbed [27].
- Step 3 – Device Interaction: Run the neuroimplant's algorithms (e.g., adaptive control or machine learning models) in interaction with the digital twin.
- Step 4 – Performance Quantification: Quantify device responses over an extensive operational space to measure stability, efficacy, and safety margins [27].
- Step 5 – Iterative Refinement: Use the results to refine the device's software and hardware configurations in an iterative loop.
Protocol 2: Cybersecurity Stress Testing
Objective: To proactively identify and harden vulnerabilities in wireless, connected neuroimplants against adversarial threats [27].
- Step 1 – Threat Modeling: Identify potential attack vectors, such as unauthorized access to the device's communication protocol or manipulation of neural data.
- Step 2 – Controlled Environment Setup: Conduct tests within the isolated sandbox ecosystem, ensuring no risk to patients [27].
- Step 3 – Penetration Testing: Aggressively model and test cybersecurity threats, attempting to hijack device control or disrupt its function.
- Step 4 – Firmware Hardening: Update device firmware and communication interfaces to mitigate identified vulnerabilities.
- Step 5 – Validation Retesting: Repeat testing to validate the effectiveness of the security patches.
Protocol 3: Closed-Loop System Adaptive Algorithm Validation
Objective: To ensure the behavioral predictability and safety of autonomous or adaptive neurodevices that dynamically adjust their operation [27].
- Step 1 – Baseline Performance Establishment: Define safety margins and performance benchmarks for the device under controlled, static conditions.
- Step 2 – Real-World Variability Introduction: Expose the device to simulated real-world variability, such as fluctuating neural signals or changing patient conditions.
- Step 3 – Algorithmic Response Monitoring: Monitor the device’s evolving operational modes to check if it remains within pre-approved safety margins [27].
- Step 4 – Feedback Loop Adjustment: If the device approaches or breaches safety limits, adjust the control algorithms and retest.
- Step 5 – Long-Term Stability Assessment: Run extended simulations to assess long-term algorithm stability and prevent performance degradation.
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key materials and tools essential for conducting rigorous validation experiments for implantable neurotechnologies.
Table 2: Essential Research Reagents and Solutions for Neurotechnology Validation
| Research Reagent/Material | Core Function in Validation |
|---|---|
| Digital Twin Software Platforms | Creates virtual patient avatars for safe, high-fidelity simulation of device-tissue interaction and prediction of long-term performance [27] [44]. |
| Neuromorphic Computing Hardware | Provides biologically inspired, energy-efficient computing architectures for real-time signal processing and closed-loop feedback in neurohybrid interfaces [44]. |
| Biocompatible Interface Materials | Novel material strategies (e.g., for electrodes) engineered for seamless neural interfacing, minimizing foreign body response and improving signal-to-noise ratio [44]. |
| Monte Carlo Simulation Software | Models survival curves and device longevities under a variety of fictitious patient pool conditions, helping personalize device choice [45]. |
| Open-Source Neural Signal Software | Tools like EEGLAB, OpenViBE, and BCI2000 enable accessible processing and analysis of neural data, crucial for algorithm development [44]. |
| 1-Butanone, 3-hydroxy-1-phenyl- | 1-Butanone, 3-hydroxy-1-phenyl-, CAS:13505-39-0, MF:C10H12O2, MW:164.2 g/mol |
| Isopropyl cyanoacrylate | Isopropyl Cyanoacrylate | High-Purity Research Grade |
Visualizing the Sandbox Workflow and Its Adaptive Regulatory Process
The following diagram illustrates the iterative, participant-driven workflow of a regulatory sandbox for implantable neurotechnology, highlighting its circular and adaptive nature.
Sandbox Adaptive Regulatory Process: This diagram visualizes the non-linear, feedback-driven workflow of a regulatory sandbox, emphasizing its core participatory, adaptive, and supervised characteristics [42].
Regulatory sandboxes represent a paradigm shift in how implantable neurotechnologies can be validated. Unlike traditional pathways focused on compliance, sandboxes offer a participatory, adaptive, and supervised environment [42]. This framework facilitates rigorous testing through advanced methodologies like digital twins and cybersecurity stress tests, enabling researchers to address the unique technical and ethical challenges of iBCIs. For the field to advance responsibly, the adoption of such innovative validation environments is not just beneficial but essential for balancing transformative innovation with unwavering patient safety.
Clinical trial design for neurodevices presents a unique set of challenges and considerations distinct from pharmaceutical development. Neurotechnologies—defined as health technologies that enable a direct connection between technical components and the nervous system—represent a rapidly emerging field with vast potential within healthcare [46]. The global neurotechnology market is estimated to be worth GBP £14 billion by 2026, driven by the ageing demographic and the growing prevalence of neurological disorders [46]. Unlike pharmacological interventions, neurodevices require multifaceted evaluation encompassing not only biological responses but also device integrity, electrical field distribution, and long-term biocompatibility.
The complexity of the nervous system necessitates that safety and efficacy evaluations for neurodevices extend across cellular, circuit, and system levels [35]. Our understanding of the safety and effectiveness of established methods like electrical stimulation remains limited to minimal data collected from traditional electrodes at a sparse set of stimulation paradigms using conventional characterization tools [35]. This foundational gap constrains the available stimulation parameter range and potentially limits therapeutic options for many novel stimulation devices or applications. This article examines the structured pathway of clinical development for neurodevices through feasibility, pivotal, and long-term safety studies, providing researchers with evidence-based frameworks for generating robust clinical evidence.
Feasibility and Pilot Studies
Objectives and Design Considerations
Feasibility studies for neurodevices serve as critical preliminary investigations to establish initial safety profiles, determine practical implementation parameters, and assess the viability of proceeding to larger-scale trials. These studies typically focus on technical performance, surgical implantation techniques (for invasive devices), and initial biomarker validation. According to a recent horizon scan of neurotechnology innovations, 77.4% of developing neurotechnologies are at these pilot/feasibility stages, highlighting their crucial role in the development pipeline [46].
These early-phase studies must evaluate both neuronal and non-neuronal responses to neurostimulation, including effects on glial cells, vascular systems, and overall tissue health [35]. For invasive neuromodulation devices such as deep brain stimulation (DBS) systems, feasibility studies must specifically assess targeting accuracy, electrode integrity, and initial parameter settings. The primary objectives include establishing preliminary safety parameters, refining inclusion/exclusion criteria, determining optimal endpoints, and assessing the feasibility of recruitment and retention strategies.
Methodological Framework
Comprehensive feasibility assessment for neurodevices requires a multi-modal approach combining various evaluation methods:
Table: Key Methodological Components of Neurodevice Feasibility Studies
| Method Type | Primary Applications | Data Outputs |
|---|---|---|
| In silico Modeling | Predicting electrical field distribution, parameter optimization | Computational models of stimulus spread and neural activation |
| In vitro Testing | Material safety, electrode degradation assessment | Biocompatibility, material integrity under stimulation |
| In vivo Studies | Neural tissue response, behavioral effects | Histological changes, neuronal/glial activation, functional outcomes |
| Clinical Pilot Trials | Initial human safety, preliminary efficacy | Adverse event profiles, biomarker validation, dose-response relationships |
Innovative methods for evaluating safety and efficacy include molecular, neurochemical, and neuropeptide measurements resulting from electrical stimulation (such as stimulated dopamine release), and original findings in biological responses, including neuronal, glial, vascular, and behavioral changes [35]. These multifaceted assessments are particularly crucial for understanding the biological mechanisms underlying both safety and efficacy of the stimulation.
Essential Research Reagents and Tools
Table: Research Reagent Solutions for Neurodevice Feasibility Studies
| Reagent/Tool Category | Specific Examples | Primary Research Function |
|---|---|---|
| Electrode Materials | Metal electrodes, conducting polymer electrodes, carbon fiber microelectrodes | Neural signal recording and electrical stimulation delivery |
| Biomarker Assays | pTau-181, pTau-217, GFAP, Neurofilament light chain (NfL) | Assessing neurochemical responses and potential tissue damage |
| Neural Interface Systems | Glassy carbon electrodes, microdialysis probes, in vivo fiber photometry | Real-time monitoring of neural activity and neurochemical release |
| Computational Modeling Tools | Finite element analysis software, neural activation models | Predicting electrical field distribution and optimizing stimulus parameters |
Pivotal Study Design
Controlled Trial Methodologies
Pivotal studies for neurodevices represent the definitive stage of clinical evidence generation, designed to provide substantial evidence of safety and effectiveness for regulatory approval. These trials typically employ randomized controlled designs, though neurodevices present unique blinding challenges—particularly for invasive interventions where sham surgery may raise ethical concerns [47]. Adaptive trial designs are increasingly employed, particularly for closed-loop systems that dynamically adjust stimulation parameters based on real-time neural feedback [28].
The complexity of pivotal neurodevice trials is exemplified by recent advances in closed-loop systems. These adaptive neurotechnologies continuously monitor physiological inputs, process data through advanced algorithms, and dynamically adjust outputs in real-time to achieve desired outcomes [28]. This approach enables not only precise control and enhanced efficacy but also personalized treatment tailored to each patient's momentary physiological state. The FDA-approved responsive neurostimulation (RNS) system for epilepsy exemplifies this approach, utilizing intracranial electroencephalography (iEEG) to detect epileptiform activity and deliver targeted stimulation to prevent seizures [28].
Endpoint Selection and Regulatory Considerations
Endpoint selection for neurodevice pivotal trials requires careful alignment with both clinical meaningfulness and regulatory expectations. Co-primary endpoints often combine performance-based functional measures with patient-reported outcomes, particularly for conditions where disease progression varies significantly even within the same diagnosis [47]. Recent neurodevice trials have increasingly incorporated biomarker endpoints alongside clinical measures, as demonstrated in the AR1001 trial for Alzheimer's disease which examined plasma biomarkers pTau-181, pTau-217, Aβ42/40 ratio, GFAP, and NfL alongside cognitive and global impression scales [36].
Engaging regulatory agencies early through pre-IND meetings or scientific advice procedures is crucial for pivotal trial success. Both the FDA and EMA have provided guidance on how natural history data and external controls can support approval pathways when traditional trial designs are not feasible [47]. The FDA's 2019 draft guidance on natural history studies and its 2023 draft guidance on externally controlled trials provide clear frameworks for sponsors, while the EMA has demonstrated flexibility through tools like Scientific Advice and PRIME scheme for accelerated development in areas of high need [47].
Statistical Considerations and Innovative Designs
Rare neurological disease trials present particular statistical challenges, often requiring innovative approaches to control groups. When randomized controls are impractical or unethical, external comparators built from patient registries, medical chart data, or prior trial datasets provide a credible alternative [47]. Statistical methods like propensity score matching and covariate adjustment are crucial to address baseline imbalances and minimize bias in these designs.
Recent approvals illustrate the successful application of these innovative designs. Brineura (cerliponase alfa) was approved for CLN2 Batten disease based on a single-arm trial whose outcomes were benchmarked against untreated natural history controls, while eteplirsen for DMD received accelerated approval using increased dystrophin as a surrogate endpoint with supportive functional data from historical controls [47]. These cases highlight the importance of planning these strategies from the beginning, ensuring data sources, comparison methods, and documentation satisfy regulatory requirements.
Long-Term Safety and Post-Market Surveillance
Study Design and Methodological Framework
Long-term safety studies for neurodevices extend beyond traditional clinical trial timelines to capture rare adverse events, device durability concerns, and chronic tissue responses. These studies are particularly critical for implantable neurodevices where tissue-electrode interfaces evolve over time, potentially impacting both safety and efficacy [35]. Our current understanding of long-term neural tissue responses to electrical stimulation is limited to minimal data collected from traditional electrodes, constraining our knowledge of chronic stimulation effects [35].
Post-market surveillance for neurodevices should encompass comprehensive assessment of multiple dimensions: neuroinflammation, cell-type specificity, neural circuitry adaptation, systemic functional effects, stimulation electrode geometry, electrode material stability, and electrical field distribution changes over time [35]. Additionally, considerations must be given to interactions among different factors, including how neural tissue changes impact the effectiveness of preset stimulation, how electrical stimulation parameters affect electrode integrity, and how electrode degradation changes electrical field distribution.
Monitoring Protocols and Outcome Measures
Robust long-term safety monitoring requires standardized protocols for assessing both device performance and biological responses. Key safety endpoints include electrode impedance stability, lead integrity, generator function, and battery longevity. Biological monitoring should encompass serial neurological examinations, neuroimaging assessments for tissue changes, and systematic documentation of neurological and psychiatric adverse events.
For closed-loop systems, additional considerations include monitoring algorithm performance, sensor accuracy drift over time, and stability of neural signal detection [28]. The continuous real-time recording and processing of neural data in these systems raises important challenges for privacy and the patients' right to be informed about when and how their data are collected and processed [28]. These concerns require transparent communication, informed consent procedures tailored to adaptive systems, and principled deliberation on how to balance privacy protection with device functionality.
Ethical Considerations in Neurodevice Trials
Unique Ethical Challenges
Neurodevice clinical trials raise distinctive ethical considerations that extend beyond conventional medical device research. A recent scoping review of ethical gaps in closed-loop neurotechnology revealed that despite the prominence of these systems in neuroethical discourse, explicit ethical assessments remain rare in clinical studies [28]. Ethical issues are typically addressed only implicitly, folded into technical or procedural discussions without structured analysis [28].
The integration of artificial intelligence in closed-loop neurotechnologies raises concerns about their potential impact on patients' sense of self and identity, as these systems can autonomously modulate neural activity in ways that may blur the distinction between voluntary and externally driven actions [28]. The extent to which patients perceive these interventions as an extension of their own agency or as an external influence remains largely unexplored, warranting further investigation [28]. Additionally, issues related to equitable access to advanced neurotechnologies add another layer of complexity, as these applications are often resource-intensive and require specialized expertise, potentially exacerbating existing healthcare disparities [28].
Implementing Ethical Frameworks
Addressing these ethical challenges requires more than regulatory compliance; it demands transparent communication, informed consent procedures tailored to adaptive systems, and principled deliberation on how to balance competing values [28]. From an ethical standpoint, resolving concerns around neural data privacy requires more than regulatory compliance; it demands transparent communication, informed consent procedures tailored to adaptive systems, and principled deliberation on how to balance privacy protection with device functionality through frameworks such as proportionality and least-infringement [28].
Investigators should implement comprehensive ethical frameworks that address the unique aspects of neurodevice research. These include ongoing consent processes for adaptive systems that evolve in functionality, clear data governance policies for neural data, and systematic assessment of perceived agency and identity effects. Furthermore, ethical oversight should extend to post-market surveillance phases, ensuring that long-term effects on personality, cognition, and quality of life are monitored and addressed.
Clinical trial design for neurodevices requires sophisticated, multi-stage approaches that address both technological and biological complexities. The development pathway from feasibility studies through pivotal trials to long-term safety monitoring demands specialized methodologies tailored to the unique characteristics of neural interfaces. As the field advances toward increasingly adaptive, closed-loop systems that dynamically respond to neural states, trial designs must evolve accordingly, incorporating comprehensive safety monitoring, innovative control strategies, and robust ethical frameworks.
Future directions in neurodevice trials will likely see greater integration of real-world evidence, digital endpoints, and advanced analytics. The continued development of this promising therapeutic domain depends on generating clinically meaningful, ethically robust, and scientifically valid evidence across the device lifecycle. By implementing the structured approaches outlined in this review, researchers can contribute to the responsible advancement of neurotechnologies that offer significant benefits for patients with neurological and psychiatric disorders.
The evaluation of neurotechnologies—ranging from non-invasive neuromodulation devices to implanted brain-computer interfaces—requires a multifaceted approach to endpoint selection that captures neural, functional, and behavioral dimensions of treatment effects. Endpoint selection represents a critical methodological decision that directly influences a trial's ability to demonstrate therapeutic efficacy and safety. In neurotechnology development, this process is particularly complex due to the intricate relationship between neural circuit activity and resulting behavioral or functional manifestations [13]. The choice of appropriate endpoints must balance scientific rigor with clinical relevance, while also considering practical constraints in measurement feasibility, reliability, and sensitivity to change.
Recent analyses reveal that neurotechnology trials are evolving in their endpoint strategies, moving beyond traditional clinical measures to incorporate novel biomarkers and patient-centered outcomes [48] [49]. This evolution reflects growing recognition that neural interventions may produce benefits across multiple domains of functioning, requiring comprehensive assessment strategies. Furthermore, emerging closed-loop neurotechnologies that dynamically adapt to neural states introduce additional complexity to endpoint selection, as their effects may be non-linear and context-dependent [13]. This comparison guide examines the current landscape of endpoint selection in neurotechnology research, providing a structured framework for comparing different assessment approaches across neural, functional, and behavioral domains.
Comparative Analysis of Endpoint Categories
Table 1: Comparison of Neural Outcome Endpoints in Neurotechnology Research
| Endpoint Category | Specific Measures | Technological Requirements | Research Contexts | Strengths | Limitations |
|---|---|---|---|---|---|
| Electrophysiological | Local field potentials (LFPs), intracranial EEG (iEEG), beta-band oscillations | Implanted recording electrodes, amplifiers, signal processing systems | Adaptive deep brain stimulation for Parkinson's disease, responsive neurostimulation for epilepsy [13] | Direct neural readouts, high temporal resolution, objective quantification | Invasive methods required for some measures, signal interpretation complexity |
| Neuroimaging-Based | fMRI connectivity, PET receptor binding, structural MRI volumes | MRI/PET scanners, analysis software, standardized acquisition protocols | Target engagement studies, dose-finding trials, mechanistic investigations | Spatial localization, network-level analysis, non-invasive options | Cost, accessibility constraints, indirect neural activity measures |
| Circuit Engagement | Evoked potentials, stimulation-locked responses, network oscillation patterns | Stimulation-capable devices, synchronized recording systems | Closed-loop neurostimulation, target verification studies [13] | Causal evidence of engagement, pathway-specific assessment | Technical complexity, device-specific implementation |
Table 2: Comparison of Functional and Behavioral Outcome Endpoints
| Domain | Endpoint Examples | Assessment Methods | Psychometric Properties | Clinical Relevance |
|---|---|---|---|---|
| Motor Function | UPDRS-III, Tremor Rating Scales, Purdue Pegboard | Clinical assessment, performance timing, accelerometry | Established reliability, sensitivity to change in movement disorders | Direct impact on activities of daily living, patient-observable benefits |
| Cognitive Function | MMSE, MoCA, Processing Speed Tasks, Working Memory Tests | Neuropsychological testing, computerized assessment | Variable sensitivity to change, practice effects possible | Impacts functional independence, workplace performance, safety |
| Mental Health | HAM-D, MADRS, Y-BOCS, PANSS | Clinician-rated interviews, self-report questionnaires | Well-validated in specific populations, subject to rater bias | Direct targeting of disorder core symptoms, regulatory acceptance |
| Quality of Life | QOLIE-31, NEI-VFQ, disease-specific QoL measures | Patient-reported outcomes, structured interviews | Captures patient perspective, may reflect multiple domains of benefit | Holistic assessment of treatment impact, values-based care alignment |
| Global Function | Clinical Global Impression, Global Assessment of Functioning | Clinician judgment, anchor-based assessment | Integrative but subjective, limited granularity | Regulatory familiarity, practical significance interpretation |
Table 3: Endpoint Usage Trends in Neurological Trials (2020-2022)
| Endpoint Type | Frequency in Phase II Trials | Trend Compared to 2017-2019 | Primary Applications |
|---|---|---|---|
| Time-to-Event Outcomes | 73% of trials [48] [49] | Stable prevalence | Progression-free survival in glioblastoma, time to clinical worsening |
| Objective Response Rate | 8% of trials (significantly decreased, p=0.022) [48] [49] | Significant decrease from previous period | Limited use in brain tumors due to RECIST limitations |
| Performance Outcomes | 17-22% of trials as primary endpoints [49] | Increasing diversity of specific measures | Functional capacity, cognitive performance, motor function |
| Patient-Reported Outcomes | 14% of trials as secondary endpoints [49] | Growing incorporation | Quality of life, symptom burden, treatment satisfaction |
Methodological Protocols for Endpoint Assessment
Electrophysiological Signal Processing Pipeline
The quantification of neural activity endpoints requires standardized processing methodologies to ensure reproducibility and cross-study comparability. The electrophysiological assessment protocol for local field potentials in adaptive deep brain stimulation trials typically follows a multi-stage pipeline [13]. Raw neural signals are first preprocessed to remove artifacts using notch filters (50/60 Hz line noise) and band-pass filters appropriate to the frequency band of interest (e.g., 13-35 Hz for beta oscillations in Parkinson's disease). Feature extraction then computes time-domain or frequency-domain metrics, with common approaches including power spectral density analysis, burst detection algorithms, or cross-frequency coupling measures. These features are subsequently normalized to baseline recording periods obtained during defined behavioral states. For closed-loop systems, additional steps involve implementing detection thresholds that trigger stimulation adjustments when neural features deviate from predefined targets. The entire processing chain requires validation against clinical outcomes to establish clinically meaningful effect sizes for neural endpoints.
Behavioral Task Implementation Framework
Behavioral assessment protocols must balance experimental control with ecological validity, particularly when evaluating cognitive or motor functions in patient populations. Standardized implementation includes equipment calibration, standardized instruction scripts, practice trials to ensure task understanding, and consistent environmental conditions across testing sessions. For serial assessments, time-of-day matching helps control for circadian fluctuations in performance. Quality control procedures should include monitoring for practice effects, particularly in cognitively impaired populations, and implementing alternate test forms when possible. Data collection typically includes both accuracy and reaction time measures, as these can dissociate under different intervention effects. In clinical trial contexts, rater training and certification programs ensure consistent administration and scoring across sites, with periodic reliability checks to prevent rater drift.
Visualization of Endpoint Selection Framework
Diagram 1: Neurotechnology endpoint framework and relationships
Research Reagent Solutions for Endpoint Assessment
Table 4: Essential Research Materials and Platforms for Endpoint Assessment
| Category | Specific Tools/Platforms | Primary Application | Key Features | Implementation Considerations |
|---|---|---|---|---|
| Neurophysiology Platforms | RNS System (NeuroPace), Activa PC+S (Medtronic) | Continuous neural monitoring, responsive stimulation [13] | Intracranial recording, closed-loop capability, chronic implantation | Surgical implantation required, specialized programming expertise |
| Behavioral Testing Software | NIH Toolbox, CANTAB, Psychology Experiment Builder | Standardized cognitive assessment, cross-study comparability | Normative data, alternate forms, automated scoring | Licensing costs, hardware compatibility, administration time |
| Clinical Rating Instruments | UPDRS, HAM-D, Y-BOCS, PANSS | Disorder-specific symptom severity | Structured administration guidelines, established validity | Rater training requirements, potential subjectivity, translation needs |
| Data Analysis Environments | MATLAB EEG Toolbox, Python MNE, FMRIB Software Library | Signal processing, statistical analysis, visualization | Open-source options, customization capability, publication-ready outputs | Computational resources, programming expertise, version control |
| Patient-Reported Outcome Systems | Neuro-QoL, PROMIS, REDCap ePRO | Quality of life, symptom tracking, functional status | Electronic administration, real-time data capture, multilingual options | Regulatory compliance (21 CFR Part 11), patient burden, missing data protocols |
The translation of scientific discoveries from laboratory research into real-world clinical treatments is a critical pathway for improving human health, yet it remains a significant challenge. Translational neuroscience, in particular, has witnessed tremendous advances driven by innovations in understanding brain cell types, novel molecular tools for monitoring neural activity, and groundbreaking hardware like large-scale neural recording probes [50]. Despite this progress, therapeutic options for brain diseases often lag behind fundamental discoveries, creating a well-documented "valley of death" between research and clinical application [51]. The process of clinical translation is a multi-stage journey that can take years to decades, involving rigorous testing to establish both safety and effectiveness of new interventions [52]. In neurotechnology, this challenge is particularly acute due to the complexity of the nervous system and the rapid evolution of technical capabilities, from sophisticated brain-computer interfaces to innovative neuromodulation devices [35] [12]. This guide objectively examines the current landscape of translational strategies, comparing methodological approaches and providing a framework for researchers and drug development professionals to navigate the complex pathway from laboratory discovery to clinical implementation.
The Translational Pathway: From Concept to Clinic
The journey from basic research to clinical application follows a structured pathway designed to systematically evaluate safety and efficacy. This process begins with basic research to understand fundamental mechanisms of disease and progresses through increasingly rigorous stages of testing.
Stages of Clinical Translation
Basic Research: The foundation of the translational pipeline begins in the laboratory with fundamental research to understand how living organisms work from the cellular level to whole organisms, and what goes wrong in disease or injury. Scientists develop testable hypotheses, perform experiments, analyze results, and draw conclusions about scientific principles that may underlie potential medical discoveries [52].
Preclinical Research: Building upon basic research findings, preclinical studies apply this knowledge to develop potential treatments using laboratory models of disease, including cells, lab-grown tissues, organoids, and animals. This stage should include external peer review, publication in scientific journals, and reproduction of results—ideally by an independent laboratory—before advancing to human testing [52].
Clinical Research: After demonstrating likely safety and effectiveness in preclinical models, researchers seek permission from regulatory authorities and ethical review boards to conduct clinical trials in humans. These regulated studies are designed to establish whether a potential new treatment reliably produces the intended medical benefit and is safe for patients [52].
Regulatory Approval and Implementation: Following successful clinical trials, regulatory agencies like the FDA (U.S. Food and Drug Administration) or EMA (European Medicines Agency) review the complete data set to determine if effectiveness and safety have been formally demonstrated for approval in clinical practice [52].
Technology Transfer Mechanisms
Beyond the scientific pathway, successful translation requires effective technology transfer—the transmittal of developed ideas, products, or techniques from a research environment to practical application. Several models exist to facilitate this process:
The Agricultural Extension Model: Considered one of the most successful federal agency models, this approach involves a research system, county extension agents, and state extension specialists. Notably, the U.S. Department of Agriculture spends approximately the same amount on technology transfer as on agricultural research, whereas most federal agencies spend only about 4-5% of research funding on transfer and diffusion activities [53].
Specialized Technology Transfer Offices: Many research organizations employ dedicated technology transfer officers who facilitate the process through patents, licensing arrangements, and other legal matters. Laws such as the Technology Transfer Act of 1986 have been particularly significant for government laboratories and private organizations [53].
VA Technology Transfer Program: The Department of Veterans Affairs maintains a Technology Transfer Section within its Rehabilitation Research and Development Program that funds prototype development with manufacturers and evaluates prototypes in VA medical centers, with positive evaluations leading to approved technology purchases [53].
Table: Key Legislation and Programs Supporting Technology Transfer
| Mechanism | Description | Impact |
|---|---|---|
| Technology Transfer Act of 1986 | Amends the Stevenson-Wydler Act of 1980 regarding government laboratories and private organizations | Considered most significant legislation for government lab technology transfer [53] |
| Small Business Innovative Research (SBIR) | Provides start-up funding to small companies developing technologies from agency-funded research | Stimulates commercialization of research developments [53] |
| VA Technology Transfer Section | Unit within VA Rehabilitation Research and Development Program that facilitates technology transfer | Funds prototype development and evaluation in VA medical centers [53] |
Comparative Analysis of Neurotechnology Translation
Classification and Evaluation of Neurotechnologies
Neurotechnology encompasses a broad spectrum of interventions that interface with the nervous system, ranging from non-invasive devices to implanted systems. These technologies can be categorized based on their mechanism of action, invasiveness, and primary application.
Table: Comparative Analysis of Neurotechnology Modalities
| Technology Type | Key Applications | Regulatory Status | Safety Considerations | Efficacy Evidence |
|---|---|---|---|---|
| Deep Brain Stimulation (DBS) | Parkinson's disease, essential tremor, dystonia, OCD [12] | FDA approved (1997-2009) [12] | Surgical risks, device-related complications, stimulation-induced side effects | Strong clinical trial evidence for motor symptoms in movement disorders [12] |
| Implantable Brain-Computer Interfaces (BCI) | Quadriparesis from spinal cord injury, brainstem stroke, motor neuron disease [12] | Experimental (Brain Gate trial), first human trials (Neuralink) [12] | Neural tissue damage, neuroinflammation, electrode integrity, long-term stability [35] | Early feasibility data showing signal decoding and communication capability [12] |
| Electrical Stimulation Devices | Neurological diseases, sensory and motor function restoration [35] | Varied based on application and risk profile | Neural tissue damage, electrode degradation, glial responses, parameter-dependent toxicity [35] | Limited to traditional electrodes and sparse parameter sets; novel approaches under investigation [35] |
| Cochlear Implants | Hearing restoration [12] | Established clinical use | Surgical risks, device failure, infection | Strong long-term evidence for auditory rehabilitation [12] |
Methodological Frameworks for Safety and Efficacy Evaluation
The evaluation of neurotechnologies requires specialized methodologies that address the unique challenges of interfacing with the nervous system. Recent advances have expanded our understanding of the multifaceted considerations necessary for comprehensive safety and efficacy assessment.
Key Methodological Approaches:
Multiscale Biological Response Assessment: Comprehensive evaluation requires examining neuronal and non-neuronal responses to electrical stimulation at cellular, circuit, and system levels. This includes assessment of neuroinflammation, cell-type specificity, neural circuitry adaptation, and systemic functional effects [35].
Material-Biology Interaction Studies: The safety of materials used in electrical stimulation devices requires specialized evaluation, including how electrode degradation would change electrical field distribution and how neural tissue changes impact stimulation effectiveness [35].
Advanced Biomarker Integration: Incorporating molecular, neurochemical, and neuropeptide measurements as results of electrical stimulation (such as stimulated dopamine release) provides objective indicators of biological effects and potential therapeutic mechanisms [35].
Longitudinal Safety Monitoring: Particularly for implanted devices and cell-based therapies, long-term safety must be determined since transplanted cells or chronic implants may remain for many years in patients' bodies, requiring extended follow-up [52].
Experimental Design and Methodologies
Standardized Protocols for Translation Readiness
The transition from preclinical to clinical research requires rigorous experimental designs that generate predictive data for human applications. The following workflow illustrates a standardized protocol for translational research in neurotechnology:
Diagram: Translational Research Workflow from Discovery to Implementation
Clinical Trial Framework: A Case Study in Alzheimer's Disease
Recent advances in clinical trial methodology are exemplified by a phase 2 randomized, placebo-controlled study on the efficacy and safety of AR1001, a phosphodiesterase-5 inhibitor, in patients with mild-to-moderate Alzheimer's disease [36]. This trial demonstrates key elements of modern neurotechnology evaluation:
Trial Design Parameters:
- Design: Randomized, double-blind, placebo-controlled phase 2 trial
- Participants: 210 adults aged 55-80 years with mild-to-moderate dementia
- Intervention: Once daily oral administration of placebo, 10 mg AR1001, or 30 mg AR1001 for 26 weeks
- Primary Endpoints: Changes in Alzheimer's Disease Assessment Scale-cognitive subscale (ADAS-Cog 13) and Alzheimer's Disease Cooperative Study-Clinical Global Impression of Change (ADCS-CGIC)
- Biomarker Assessment: Levels of plasma biomarkers pTau-181, pTau-217, Aβ42/40 ratio, glial fibrillary acidic protein (GFAP), and neurofilament light chain (NfL)
Key Findings and Implications: The study demonstrated that AR1001 was safe and well tolerated, with similar safety profiles compared to placebo. While primary efficacy endpoints were not met after 26 weeks of treatment, participants receiving 30 mg AR1001 showed favorable changes in AD-related plasma biomarkers compared to placebo [36]. This highlights the growing importance of biomarker integration in clinical trials, even when primary clinical endpoints are not achieved.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful translation requires carefully selected research tools and materials that ensure reproducible and clinically relevant results. The following table details key research reagent solutions essential for neurotechnology development and evaluation.
Table: Essential Research Reagents and Materials for Neurotechnology Translation
| Research Reagent/Material | Function/Application | Translation Relevance |
|---|---|---|
| Neuropixels Probes | High-density neural recording probes for stable, long-term brain recordings [50] | Enables large-scale neural activity monitoring with clinical-grade stability |
| Stem Cell-Derived Organoids | In vitro models of brain development and disease [50] | Provides human-relevant systems for drug screening and disease modeling |
| Voltage-Sensitive Fluorescent Indicators | Genetically encoded voltage indicators with enhanced sensitivity for unitary synaptic events [50] | Allows monitoring of neural activity at synaptic resolution |
| Conducting Polymer Electrodes | Advanced electrode materials for improved neural interfacing [35] | Enhances signal quality and reduces tissue response in implanted devices |
| Carbon Fiber Microelectrodes | Miniaturized electrodes for precise neural recording and stimulation [35] | Enables targeted neural circuit interrogation with minimal tissue damage |
| Phosphodiesterase-5 Inhibitors | Small molecule compounds for targeting intracellular signaling pathways [36] | Exemplifies drug repurposing strategies for neurological disorders |
| Plasma Biomarker Panels | Multiplex assays for pTau-181, pTau-217, GFAP, NfL [36] | Provides objective, measurable endpoints for clinical trial assessment |
| Dimethyl vinyl phosphate | Dimethyl vinyl phosphate, CAS:10429-10-4, MF:C4H9O4P, MW:152.09 g/mol | Chemical Reagent |
| Thallium(III) chloride | Thallium(III) Chloride | High-Purity Reagent | High-purity Thallium(III) Chloride for research applications. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Data Management and Analysis Frameworks
Quantitative Data Analysis in Translational Research
The increasing complexity and scale of data in neurotechnology requires sophisticated analysis approaches. Quantitative data analysis transforms raw numerical information into actionable insights through mathematical, statistical, and computational techniques [54].
Essential Quantitative Analysis Methods:
Descriptive Statistics: Initial data summarization using measures of central tendency (mean, median, mode) and dispersion (range, variance, standard deviation) to describe dataset characteristics [54].
Inferential Statistics: Using sample data to make generalizations about larger populations through hypothesis testing, t-tests, ANOVA, and regression analysis [54].
Cross-Tabulation: Analyzing relationships between categorical variables through contingency table analysis, particularly useful for survey data and demographic comparisons [54].
Gap Analysis: Comparing actual performance against potential or benchmarks to identify improvement areas and measure strategy effectiveness [54].
Data Visualization for Translational Science
Effective data visualization is crucial for communicating complex relationships in translational research. The following visualization techniques are particularly valuable for neurotechnology development:
Diagram: Data Analysis and Visualization Workflow for Translational Research
Visualization Selection Framework:
Comparison Analysis: Bar charts and grouped bar charts effectively compare quantities across categories or sub-categories [55].
Trend Analysis: Line charts and area charts display changes over continuous time intervals, showing trends and cumulative effects [55].
Relationship Analysis: Scatter plots and bubble charts illustrate correlations between variables and identify patterns or outliers [55].
Distribution Analysis: Box plots and histograms visualize data spread, central tendency, and variability across datasets [55].
Emerging Strategies and Future Directions
Addressing Translational Bottlenecks
Significant challenges remain in translating basic neuroscience discoveries into clinical applications. Key obstacles include the selection of appropriate study readouts and endpoints, standardization of experimental models and assessments, and development of personalized treatment strategies [51]. Strategic solutions include:
Refined Endpoint Development: Establishing more sensitive clinical endpoints combined with biomarkers capable of predicting treatment responses in human patients [51].
Precision-Based Approaches: Implementing clearly defined experimental procedures that closely match clinical conditions and ensure efficient therapeutic responses through personalized medicine strategies [51].
Cross-Disciplinary Collaboration: Enhancing communication between experimental neuroscientists and clinicians with shared understanding and common language [51].
Responsible Innovation in Neurotechnology
As neurotechnologies advance in capability and complexity, ethical and governance considerations become increasingly important. The Organisation for Economic Co-operation and Development (OECD) has identified five systemic changes to accelerate responsible neurotechnology development [12]:
Responsible Research: Encouraging consideration of ethical, legal, and social issues (ELSI) through collaboration between all stakeholders, including patients and funders.
Anticipatory Governance: Proactively establishing ethical and regulatory frameworks before technologies are widely deployed.
Open Innovation: Promoting collaboration between public and private stakeholders to share assets and mitigate investment risks.
Avoiding Neuro-Hype: Controlling unproven claims through evidence-based policies and realistic communication about capabilities.
Access and Equity: Addressing socioeconomic disparities and ensuring global access to innovations, particularly in resource-limited settings.
The future of neurotechnology translation will likely be shaped by increasingly sophisticated brain-computer interfaces, robotics, and memory modulation technologies, all requiring robust translational frameworks to safely bridge the gap between laboratory discoveries and clinical applications that improve patient lives [12].
Addressing Evaluation Challenges and Optimizing Protocols
Invasive Brain-Computer Interface (BCI) systems represent a transformative frontier in neurotechnology, offering unprecedented potential for restoring function in individuals with severe neurological conditions. These systems, which involve implanting electrodes directly into brain tissue, face significant challenges across three critical domains: surgical implantation, long-term hardware reliability, and cybersecurity vulnerabilities. The convergence of advances in material science, surgical techniques, and cryptographic security has created new pathways for risk mitigation in BCI systems. This review synthesizes current experimental data and safety outcomes from leading BCI platforms to objectively compare risk profiles and protective strategies, providing a framework for evaluating neurotechnology safety within clinical and research contexts. Understanding these interrelated risk domains is essential for researchers, regulatory bodies, and developers working to translate invasive BCIs from experimental trials to clinically viable therapeutics.
Surgical Risk Profiles and Mitigation Strategies
Surgical implantation represents the initial and most immediate risk domain for invasive BCIs. Current approaches vary significantly in their surgical methodologies, each presenting distinct risk-benefit profiles. Open craniotomy procedures used for platforms like Neuralink and Blackrock Neurotech's Utah Array provide direct cortical access but carry risks of dural damage, cortical bleeding, and cerebrospinal fluid leakage [1]. In contrast, minimally invasive techniques such as Synchron's Stentrode, delivered via neurovascular catheters through the jugular vein, avoid open brain surgery altogether but present potential complications including vessel perforation, thrombosis, and device migration [1]. Precision Neuroscience's "brain film" approach attempts to balance these concerns by inserting ultra-thin electrode arrays through a subdural slit, minimizing cortical penetration while maintaining high signal fidelity [1].
Table: Comparative Surgical Risk Profiles of Leading Invasive BCI Platforms
| BCI Platform | Surgical Approach | Key Surgical Risks | Mitigation Strategies | Clinical Evidence |
|---|---|---|---|---|
| Neuralink | Open craniotomy with robotic insertion | Cortical bleeding, dural damage, infection | Robotic precision, antibiotic coatings | Limited human trial data (n=5 reported) [1] |
| Synchron | Endovascular (jugular vein catheterization) | Vessel perforation, thrombosis, device migration | Nitinol self-expanding stent, endothelialization | 4-patient trial: no serious adverse events at 12 months [1] |
| Blackrock Neurotech | Open craniotomy with manual array placement | Cortical trauma, glial scarring, signal degradation | Biocompatible materials, surgical experience | Years of research use; long-term scarring documented [1] |
| Precision Neuroscience | Minimally invasive subdural insertion | Dural leakage, cortical compression, array displacement | Ultra-thin flexible film, <1 hour procedure | FDA 510(k) clearance for up to 30 days implantation [1] |
| Paradromics | Open cranotomy with modular array placement | Cortical damage, infection, meningeal irritation | Modular design, surgical techniques familiar to neurosurgeons | First-in-human recording in epilepsy surgery patient [1] |
Experimental data from recent clinical trials provides quantitative safety profiles for these approaches. The Synchron Stentrode demonstrated an exemplary safety record in a four-patient trial, with zero serious adverse events reported over 12 months of continuous implantation [1]. This endovascular approach leverages the body's natural healing response, as the device becomes endothelialized and incorporated into the venous wall. In contrast, traditional open approaches show higher initial risk profiles but offer established long-term track records. Blackrock Neurotech's Utah Array, despite concerns about long-term glial scarring, has demonstrated functional stability in excess of 5 years in some research participants [1]. Emerging platforms like Precision Neuroscience aim to reduce surgical morbidity further, with procedures reportedly requiring less than 60 minutes of operating time compared to multi-hour craniotomies [1].
Surgical risk mitigation extends beyond the initial procedure to encompass long-term biocompatibility. Materials engineering has become crucial for reducing foreign body responses and maintaining signal fidelity. Flexible substrates, bioactive coatings, and reduced device footprints represent key innovation areas. Experimental protocols for assessing biocompatibility typically include histopathological analysis of neural tissue response in animal models, electrochemical impedance spectroscopy to monitor electrode degradation, and long-term tracking of signal-to-noise ratios in human participants [1] [56]. These methodologies provide critical data for evaluating the tissue-device interface and guiding iterative improvements in hardware design.
Hardware Reliability and Biocompatibility Challenges
The physical hardware of invasive BCIs presents formidable challenges for long-term reliability and biocompatibility. These systems must operate reliably within the harsh biological environment of the human brain while maintaining stable neural interfaces over decades. Current data reveals significant variation in hardware performance across leading BCI platforms, with important implications for both safety and efficacy.
Table: Comparative Hardware Performance and Failure Modes in Invasive BCI Systems
| BCI Platform | Electrode Technology | Key Failure Modes | Signal Longevity Data | Biocompatibility Solutions |
|---|---|---|---|---|
| Neuralink | 96 flexible polymer threads with 3072 electrodes | Thread retraction, encapsulation, broken leads | Limited public data; initial reports show stable recordings | Biocompatible polymer encapsulation, microscopic threads |
| Blackrock Neurotech | Utah Array (96-128 rigid silicon electrodes) | Glial scarring, encapsulation, electrode degradation | >5 years in some cases with degraded signal quality | Parylene-C coating, established materials profile |
| Precision Neuroscience | Flexible thin-film cortical surface array | Delamination, compression injury, limited penetration | FDA clearance for 30 days; long-term data limited | Conformable surface contact, minimal tissue displacement |
| Paradromics | Modular 421-electrode array with wireless transmitter | Connector failure, module malfunction, heating effects | Initial human testing underway | Integrated wireless to reduce failure points |
| Synchron | Stentrode nitinol electrode array on stent | Endothelial overgrowth, signal attenuation, vessel occlusion | 12-month stable recording demonstrated in humans | Self-expanding stent design promotes incorporation |
Signal stability represents a critical hardware performance metric, with degradation occurring through multiple mechanisms. The foreign body response triggers glial scarring that insulates electrodes from target neurons, progressively reducing signal quality [1]. Blackrock Neurotech's rigid Utah arrays demonstrate this challenge, with histopathological studies showing progressive glial fibrillary acidic protein (GFAP) positive astrocyte encapsulation over implantation periods [1]. Flexible electrode designs from Neuralink and Precision Neuroscience aim to mitigate this response by reducing mechanical mismatch with brain tissue, though long-term human data remains limited. Accelerated aging tests in simulated physiological conditions provide preliminary reliability data, with protocols typically involving cyclic voltammetry, electrochemical impedance spectroscopy, and accelerated lifetime testing at elevated temperatures [56].
Hardware reliability extends beyond the electrode-tissue interface to encompass complete system integrity. Connector failures, insulation degradation, and electronic component malfunction represent common failure points in chronic implants. Paradromics addresses these challenges through a modular design that localizes potential failure domains, while Synchron's completely internalized design eliminates transcutaneous connections that represent infection pathways [1]. Experimental methodologies for evaluating hardware reliability include accelerated lifecycle testing that subjects components to mechanical stress equivalent to years of implantation, hermeticity testing for moisture barrier efficacy, and thermal profiling to ensure safe operation within neural tissue [56].
The experimental protocol for assessing BCI hardware biocompatibility typically involves multiple phases. In vitro cytotoxicity testing follows ISO 10993-5 standards using fibroblast or neural cell cultures exposed to material extracts. In vivo assessment in animal models (typically rodents or primates) involves histopathological evaluation at multiple timepoints, quantifying neuronal density, glial activation, and inflammatory markers around implants. Functional testing in both animals and human participants tracks signal quality metrics including signal-to-noise ratio, unit yield, and stimulation efficacy over time [1] [56]. These standardized methodologies enable direct comparison across platforms and inform iterative design improvements.
Cybersecurity Vulnerabilities and Defense Frameworks
As invasive BCIs evolve toward greater connectivity and functionality, they face emerging cybersecurity threats that represent unprecedented risks to neural integrity and privacy. The direct brain-computer connection creates attack surfaces that could potentially enable malicious actors to access, manipulate, or damage neural tissue and cognitive processes. Analysis of current BCI architectures reveals several critical vulnerability domains requiring robust countermeasures.
Brain tapping attacks target the signal acquisition phase, intercepting neural data transmissions to extract sensitive information including emotions, preferences, and potentially even concrete thoughts [57]. This represents a fundamental privacy violation, as neural data reflects the most intimate aspects of human experience. Misleading stimuli attacks manipulate the input pathway, delivering malicious signals to the brain that could influence perceptions, emotions, or even motor actions without user consent [57]. Such attacks could potentially hijack neurally controlled vehicles or weapons systems, with catastrophic consequences. Adversarial machine learning attacks target BCI classification algorithms by injecting manipulated inputs during training or deployment, potentially causing misclassification of user intent with serious safety implications [57].
Experimental evidence of BCI vulnerabilities, while limited in public literature, demonstrates the plausibility of these threats. Cybersecurity researchers have successfully demonstrated vulnerabilities in implanted medical devices like pacemakers and insulin pumps, establishing precedent for connected medical device exploits [58]. In BCI-specific research, experiments have shown the feasibility of reconstructing perceptual experiences from neural data and inducing erroneous motor commands through manipulated feedback [57]. These findings underscore the critical need for robust security frameworks in commercial BCI systems.
Defense strategies employ multi-layered security approaches. End-to-end encryption protects neural data in transit, while hardware-based secure elements provide tamper-resistant key storage and cryptographic operations [58]. Continuous authentication mechanisms verify user identity through biometric neural patterns, preventing unauthorized device access. Adversarial training of machine learning models improves resilience against manipulated inputs, and real-time anomaly detection monitors for unusual neural patterns indicative of attack [57]. These security measures must be balanced against power constraints and computational limitations inherent in implanted devices.
Table: BCI Cybersecurity Framework: Threats, Experimental Evidence, and Countermeasures
| Threat Vector | Experimental Demonstration | Potential Impact | Proposed Countermeasures | Regulatory Considerations |
|---|---|---|---|---|
| Brain Data Interception | Reconstruction of visual stimuli from EEG; Inference of emotional states | Privacy violation, identity theft, discrimination | End-to-end encryption, differential privacy, data minimization | GDPR neural data protections; "Neuro-rights" legislation |
| Malicious Neural Stimulation | Induced erroneous movements in animal models; Altered decision-making | Physical harm, behavior manipulation, psychological distress | Input validation, stimulation limits, emergency stop | Medical device safety standards; Stimulation safety limits |
| Adversarial ML Attacks | Decreased BCI classification accuracy via manipulated training data | System malfunction, safety compromise, loss of control | Adversarial training, ensemble methods, anomaly detection | Algorithm transparency requirements; Independent validation |
| Device Hijacking | Demonstrated exploits of connected medical devices (pacemakers, insulin pumps) | Complete system control, ransom attacks, physical harm | Secure boot, hardware roots of trust, regular security updates | Mandatory security patches; Vulnerability disclosure policies |
Regulatory frameworks for BCI cybersecurity remain underdeveloped, though emerging guidelines from the FDA and international bodies increasingly address connected medical device security [57]. The proposed "neuro-rights" framework, including mental privacy, personal identity, and free will protections, would establish foundational legal protections against neural data exploitation [58]. However, significant gaps remain between current regulations and the unique challenges posed by direct brain-computer connections, highlighting the need for specialized security standards in neurotechnology.
Experimental Protocols for Safety and Efficacy Evaluation
Robust evaluation of invasive BCI systems requires standardized experimental protocols that objectively assess safety, efficacy, and reliability across multiple domains. These methodologies enable direct comparison between platforms and provide critical data for regulatory approval and clinical adoption. The following section outlines key experimental approaches for evaluating BCI systems across surgical, hardware, and security domains.
Biocompatibility assessment follows ISO 10993 standards, evaluating tissue response through histopathological analysis in animal models. Standard protocols involve implanting devices or materials in subcutaneous, intramuscular, or neural tissues for periods ranging from 1-52 weeks [1]. Explanation followed by tissue sectioning and staining for neurons (NeuN), astrocytes (GFAP), microglia (Iba1), and macrophages (CD68) enables quantification of the foreign body response. Metrics include neuronal density within proximity to implants, glial scarring thickness, and inflammatory cell counts. These standardized methodologies allow direct comparison of tissue response across different BCI materials and designs.
Electrochemical performance evaluation characterizes the electrode-tissue interface through standardized metrics. Cyclic voltammetry establishes safe voltage windows by scanning potentials typically between -0.6V to 0.8V vs. Ag/AgCl at scan rates of 0.1 V/s. Electrochemical impedance spectroscopy measures interface impedance across frequencies from 1 Hz to 100 kHz, with lower impedance generally indicating better charge transfer capability. Accelerated aging tests subject electrodes to extreme conditions including elevated temperature, voltage cycling, and mechanical stress equivalent to years of implantation [56]. These protocols provide quantitative data on electrode stability and predicted lifespan.
Signal fidelity assessment employs standardized benchmarks to evaluate recording and stimulation capabilities. For recording, signal-to-noise ratio, unit yield (detectable neurons per channel), and sorting stability are tracked over time. Stimulation efficacy is evaluated through evoked potential magnitude, charge transfer requirements, and spatial resolution. Standardized testing protocols include presentation of controlled sensory stimuli or recording during specific motor tasks to establish baseline performance metrics [1] [56]. These methodologies enable objective comparison across BCI platforms and components.
Security validation employs specialized testing frameworks adapted from cybersecurity practice. Penetration testing evaluates system vulnerabilities through controlled attacks on communication channels, authentication mechanisms, and data processing pipelines. Fuzz testing subjects BCI input channels to malformed data to identify potential crash or exploit scenarios. Side-channel analysis examines unintended information leakage through power consumption, electromagnetic emissions, or timing variations [57] [58]. These security evaluation protocols are increasingly incorporated into pre-clinical testing regimens for connected BCI systems.
Research Reagent Solutions for BCI Evaluation
Table: Essential Research Reagents and Materials for BCI Safety and Efficacy Testing
| Reagent/Material | Specific Function | Experimental Application | Example Vendor/Product |
|---|---|---|---|
| Anti-GFAP Antibody | Astrocyte marker for glial scarring quantification | Immunohistochemical staining of explanted neural tissue | Abcam (ab7260), MilliporeSigma (G3893) |
| Anti-NeuN Antibody | Neuronal nuclear marker for neuronal density assessment | Quantification of neuronal survival near implant interface | MilliporeSigma (MAB377), Cell Signaling (12943) |
| Anti-Iba1 Antibody | Microglia/macrophage marker for inflammatory response | Evaluation of neuroinflammatory response to implants | Fujifilm (019-19741), Abcam (ab178846) |
| Parylene-C | Biocompatible polymer coating for neural electrodes | Insulation and protection of implanted electrode arrays | Specialty Coating Systems, KISCO |
| Nitinol | Shape memory alloy for self-expanding stent electrodes | Minimally invasive delivery of endovascular BCIs | Johnson Matthey, SAES Smart Materials |
| Polyimide | Flexible polymer substrate for thin-film electrodes | Creating conformable cortical surface arrays | DuPont (Kapton), UBE |
| Agarose Gel | Tissue phantom for electrode testing | Simulating electrical properties of neural tissue | Thermo Fisher Scientific, Sigma-Aldrich |
| Artificial Cerebrospinal Fluid | Electrochemical testing medium | Mimicking ionic composition of brain environment | Harvard Apparatus, Tooris Bioscience |
Invasive BCI technology stands at a pivotal juncture, with multiple platforms demonstrating feasibility in early human trials while facing significant challenges in surgical risk, hardware reliability, and cybersecurity. The comparative analysis presented herein reveals distinct risk-benefit profiles across current approaches, with open craniotomy methods offering established track records but higher initial morbidity, while minimally invasive techniques show promising safety profiles but more limited long-term data. Hardware reliability remains constrained by the foreign body response and material degradation, though flexible substrates and biocompatible coatings show promise for extending functional lifespan. Cybersecurity emerges as a critical concern as BCIs become more connected, requiring multi-layered protection strategies for neural data privacy and system integrity. Standardized experimental protocols enable objective comparison across platforms and inform iterative safety improvements. As the field advances toward broader clinical application, continued focus on mitigating risks across these three domains will be essential for realizing the transformative potential of invasive BCIs while ensuring patient safety and trust.
Overcoming Hurdles in Direct-to-Consumer and Wellness Neurotechnology Oversight
The direct-to-consumer (DTC) neurotechnology market is experiencing rapid growth, with consumer-focused firms now constituting 60% of the global neurotechnology landscape and outnumbering medical applications since 2018 [59]. This expansion has created a significant regulatory challenge: while medical neurodevices must undergo rigorous safety and efficacy evaluation through established pathways like the FDA Premarket Approval (PMA), consumer wellness products operate in a regulatory grey zone [60] [59]. These products often leverage similar base technologies as medical devices but reach consumers without clinical trials or comprehensive safety assessments, creating potential risks to human rights, mental privacy, and neural integrity [60] [12]. This comparison guide examines the current oversight landscape, evaluates emerging assessment methodologies, and provides researchers with standardized frameworks for evaluating the safety and efficacy of these rapidly proliferating technologies.
Table: Key Differences Between Medical and Consumer Neurotechnology Oversight
| Evaluation Dimension | Medical Neurotechnology | Consumer Wellness Neurotechnology |
|---|---|---|
| Regulatory Pathway | FDA PMA/510(k), EU MDR Class III | General product safety laws, limited specific regulation [60] |
| Pre-market Evidence Requirements | Clinical trials for safety/efficacy, biocompatibility testing | No mandatory clinical trials; limited safety data [59] |
| Post-market Surveillance | Mandatory reporting systems | Voluntary reporting, limited oversight |
| Mental Impact Assessment | Risk-benefit analysis for patients | No standardized assessment protocols [60] |
| Data Privacy Standards | HIPAA protected health information | Variable protection, commercial data use possible [12] [59] |
Regulatory Framework Comparison: Global Oversight Approaches
The current regulatory landscape for consumer neurotechnology is characterized by significant jurisdictional variation and emerging ethical concerns. In the United States, non-medical neurodevices generally fall outside FDA jurisdiction unless they make specific medical claims, placing them primarily under general consumer protection laws with minimal specialized oversight [60]. The European Union has taken a more cautious approach by classifying non-invasive non-medical brain stimulation devices in the highest risk category under the Medical Device Regulation (MDR), though implementation for implantable consumer devices remains deferred [60]. This regulatory patchwork creates substantial challenges for researchers and developers working across international markets.
A critical development in addressing these gaps is the proposed Mental Impact Assessment, a comprehensive screening protocol designed to systematically evaluate adverse mental effects under realistic use conditions [60]. This assessment framework addresses growing concerns about potential cognitive deskilling, emotional instability, and privacy vulnerabilities that may arise from chronic use of consumer neurotechnology [60]. Some researchers have further advocated for a precautionary moratorium on implantable non-medical devices until such assessments are fully developed and ethical concerns regarding mental integrity and privacy are resolved [60].
Table: Comparative Regulatory Status by Technology Type
| Technology Category | Medical Context Regulation | Consumer Context Regulation | Key Oversight Gaps |
|---|---|---|---|
| Implantable BCIs | FDA PMA, EU MDR Class III | No specific regulation in most jurisdictions [60] | Long-term safety, psychological effects, privacy |
| Non-invasive Stimulation | FDA De Novo, EU MDR Class II/III | EU MDR Class III (non-medical), US: general product safety [60] | Real-world efficacy, misuse potential, cognitive effects |
| Neuroimaging/EEG | FDA 510(k), CE Mark as medical device | General product safety laws only [60] | Data privacy, interpretation accuracy, over-reliance |
| Wearable Neurotech | Subject to medical claims regulation | Consumer electronics framework | Habit formation, unintended behavioral modification |
Experimental Methodologies for Safety and Efficacy Evaluation
Mental Impact Assessment Protocol
The proposed Mental Impact Assessment represents a methodological framework for systematically evaluating potential adverse effects of consumer neurotechnologies. The protocol should be implemented under realistic use conditions and include the following key components:
Cognitive Function Testing: Comprehensive assessment of potential cognitive deskilling effects, particularly on attention, working memory, and executive function, using standardized neuropsychological batteries administered before, during, and after technology use [60]. Testing should evaluate both short-term effects (immediately after use) and potential long-term adaptations (after 30-90 days of regular use).
Emotional Stability Monitoring: Systematic evaluation of effects on emotional regulation and well-being using validated self-report measures (DASS-21, PANAS) combined with physiological markers (HRV, cortisol levels) across diverse user populations [60]. Particular attention should be paid to vulnerable populations including children, adolescents, and individuals with pre-existing mental health conditions.
Neural Privacy Safeguards: Assessment of data collection practices and potential vulnerabilities for unauthorized neural data access, including evaluation of encryption standards, anonymization protocols, and potential for re-identification of neural data [60] [12]. Testing should simulate realistic attack vectors to identify potential privacy vulnerabilities.
Robotic-Assisted Rehabilitation Methodology
A recent feasibility study demonstrates rigorous methodology for evaluating neurotechnology safety and efficacy in a clinical context, providing a template for consumer device assessment [61]. The experimental protocol included:
Participant Selection and Randomization: 11 adults with hand hemiparesis following recent stroke were randomized into experimental and control groups using a computer-generated block randomization method to ensure unbiased allocation [61]. Inclusion criteria specified specific functional limitations (FMA-Hand<14) while exclusion criteria eliminated those with minimal motor recovery or inability to provide consent.
Intervention Protocol: The experimental group received ten 30-minute sessions of robotic-assisted hand rehabilitation exercise (RAHRE) over two weeks, incorporating four distinct hand opening and closing exercises with personalized assistance or resistance levels using the Dexmo glove coupled with virtual reality software [61]. The control group received conventional rehabilitation alone.
Outcome Measures: Standardized functional assessments including Action Research Arm Test (ARAT), Fugl-Meyer Assessment for the Upper Extremity (FMA-UE), Box and Block Test, and ABILHAND were administered pre- and post-intervention by blinded assessors [61]. Safety was evaluated through continuous monitoring of discomfort, pain, spasticity, and soft tissue integrity.
Feasibility Metrics: Attendance rate (96%), compliance rate (95%), repetitions per session (median 260), active training time (median 24:39 minutes), and required therapist support were quantitatively tracked throughout the intervention period [61].
Mental Impact Assessment Experimental Workflow
Key Research Challenges and Methodological Considerations
Researchers face significant hurdles in establishing robust safety and efficacy frameworks for consumer neurotechnology. These challenges necessitate careful methodological consideration:
Long-Term Effect Uncertainty: The medium and long-term effects of recurrent non-medical brain stimulation on mental processes remain largely unknown, with limited longitudinal data on potential neurological adaptations or dependency development [60]. Research protocols should incorporate extended observation periods and multiple follow-up assessments to identify potential delayed effects.
Signal Specificity Limitations: Current stimulation technologies demonstrate limited spatial and temporal selectivity, complicating isolation of specific neural circuits and creating potential for off-target effects [24] [62]. Advanced imaging and electrophysiological monitoring should be incorporated to precisely map stimulation effects.
Closed-Loop System Complexity: Development of responsive neurotechnology systems capable of adapting to real-time neural feedback requires sophisticated algorithms with limited validation in diverse populations [62]. Research should prioritize transparency in algorithmic decision-making and include rigorous testing across different user demographics.
Cognitive Liberty Concerns: Technologies capable of modifying thought patterns, behaviors, or emotional states raise fundamental questions about identity and personal agency that require both ethical analysis and empirical study [12] [62]. Research protocols should include qualitative assessment of user experience and perceived autonomy impacts.
Table: Research Reagent Solutions for Neurotechnology Evaluation
| Research Tool Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Electrophysiology Platforms | High-density EEG, ECoG arrays, sEEG | Neural signal acquisition and processing | Signal-to-noise ratio, spatial resolution, mobility limitations [63] |
| Stimulation Technologies | TMS, tDCS, TPS, low-field magnetic stimulation | Controlled neural modulation | Parameter optimization, dosing precision, sham protocols [62] |
| Imaging Modalities | fMRI, fNIRS, functional ultrasound (fUS) | Brain activity mapping and connectivity analysis | Temporal resolution, artifact rejection, accessibility [12] [63] |
| Biomechanical Sensors | Dexmo glove, force transducers, accelerometers | Motor function quantification | Calibration protocols, measurement validity, real-world applicability [61] |
| Computational Tools | Machine learning classifiers, network neuroscience algorithms, multimodal data fusion | Data analysis and pattern recognition | Model interpretability, generalizability, computational demands [63] |
Future Directions and Standardization Initiatives
The evolving regulatory and research landscape for consumer neurotechnology necessitates continued methodological development and standardization. Promising initiatives include the OECD's international standards for responsible neurotechnology innovation, which emphasize anticipatory governance, open innovation, and equitable access [12]. The NIH Blueprint MedTech program provides funding mechanisms and specialized support to accelerate development of novel neurotechnologies through structured pathways from proof-of-concept to first-in-human testing [64]. Additionally, research-grade consumer devices are increasingly incorporating standardized data formats and API access to facilitate independent validation studies.
Neurotechnology Development Funding Pathway
For researchers working in this rapidly evolving field, establishing standardized evaluation protocols that address both technical performance and potential psychosocial impacts will be essential. Priorities should include developing validated biomarkers for cognitive and emotional effects, creating open-source reference datasets for algorithm validation, and establishing cross-disciplinary committees to address the unique ethical dimensions of consumer neurotechnology. As these technologies continue to converge with artificial intelligence and integrate into mainstream consumer products, the scientific community plays a critical role in ensuring their development prioritizes user wellbeing alongside technological innovation.
Optimizing Electrical Stimulation Parameters for Safety and Efficacy
Electrical stimulation represents a cornerstone of neurotechnology, offering therapeutic interventions for a range of neurological, musculoskeletal, and sensory disorders. This technology operates through the delivery of controlled electrical impulses to neural tissues, modulating neuronal activity to restore function or alleviate symptoms. The global electrical stimulation devices market, valued at $7.75 billion in 2024 and projected to reach $12.13 billion by 2029, reflects the growing clinical adoption and technological advancement in this field [65]. The expanding application spectrum encompasses deep brain stimulation for movement disorders, spinal cord stimulation for pain management, neuromuscular electrical stimulation (NMES) for muscle rehabilitation, and retinal prostheses for visual restoration.
The fundamental challenge in electrical stimulation therapeutics lies in balancing efficacy with safety. Efficacy depends on achieving sufficient activation of target neural pathways, while safety requires minimizing tissue damage, premature fatigue, and off-target effects. Current research focuses extensively on parameter optimization—including waveform characteristics, stimulation intensity, frequency, and duration—to maximize this therapeutic window. As the field progresses toward more sophisticated neuromodulation devices, particularly implantable electrodes that offer higher spatial accuracy, the biological responses to electrical stimulation at cellular, circuit, and system levels require deeper characterization [24].
Comparative Analysis of Electrical Stimulation Modalities
Table 1: Comparison of Electrical Stimulation Modalities and Applications
| Stimulation Type | Primary Applications | Key Efficacy Findings | Safety Profile | Optimal Parameters |
|---|---|---|---|---|
| Neuromuscular Electrical Stimulation (NMES) | Fibromyalgia rehabilitation, muscle strength recovery | Superior to conventional treatment alone for pain reduction (p=0.015) and posture improvement (p=0.014) in fibromyalgia [66] | Well-tolerated; minimal adverse events | 6-week treatment duration; combined with conventional therapy |
| Functional Electrical Stimulation (FES) | Rehabilitation after neurological impairment, restoration of motor function | Accurate motion tracking; reduced muscle fatigue in optimal control paradigms [67] | Early muscle fatigue remains limitation | Optimal control algorithms; pulse width or intensity modulation |
| Transcutaneous Electrical Nerve Stimulation (TENS) | Rheumatoid arthritis pain management, chronic intractable pain | Effective for pain alleviation and functional recovery in RA [68] | Non-invasive; favorable safety profile | At least 4 weeks duration; 20min/session minimum |
| Epiretinal Stimulation | Visual restoration in retinal degeneration | Shorter phase durations (500μs) lower activation thresholds; longer durations (1000-1500μs) confine cortical spread [69] | Charge density limits prevent tissue damage | Frequency-dependent response attenuation (1Hz vs. 10-20Hz) |
| Belt-Type Electrical Stimulation (B-SES) | Preventing disuse syndrome in frail elderly hemodialysis patients | Increased thigh muscle cross-sectional area; improved intramuscular fat composition [70] | Safe for frail elderly; no elevated inflammatory markers | 20Hz frequency; 12-week duration; 40min sessions during dialysis |
Table 2: Stimulation Parameter Effects on Physiological Responses
| Parameter | Physiological Effect | Impact on Efficacy | Impact on Safety |
|---|---|---|---|
| Phase Duration | Shorter durations (500μs) reduce activation thresholds [69] | Enhances neural activation efficiency | Reduces total charge delivery, improving safety margin |
| Frequency | High frequencies (10-20Hz) attenuate cortical responses versus low frequency (1Hz) [69] | Affects sustained response maintenance | May accelerate muscle fatigue with repeated activation |
| Interphase Interval | Limits extension of cortical responses [69] | Improves spatial precision of activation | Preposes current spread to non-target areas |
| Stimulation Intensity | Directly correlates with muscle contraction strength and perceived sensation | Essential for achieving therapeutic threshold | Higher intensities associated with tissue discomfort and damage risk |
| Session Duration | Cumulative effects on muscle adaptation and neural plasticity | Longer interventions (6-12 weeks) show significant functional improvements [66] [70] | Extended sessions may increase fatigue and skin irritation risk |
Experimental Protocols for Parameter Optimization
Protocol 1: Visual Cortex Activation in Retinal Degeneration Models
The optimization of epiretinal prosthesis parameters requires systematic investigation of cortical responses to retinal stimulation. A recent study established a comprehensive protocol for evaluating parameter effects on visual cortex activation in both healthy Long-Evans (LE) and retinal degenerated (F1) rats [69].
Methodology: Animals were anesthetized and prepared with a bipolar concentric stimulating electrode (75μm diameter, Pt/Ir) inserted through the sclera into the ventral-temporal region of the retina. Electrode-retinal impedance (5-8 kΩ) was monitored in real-time using a potentiostat to maintain consistent electrode-epiretinal distance. A 4×4 grid electrode array (16 electrodes, 400μm inter-tip distance) was inserted approximately 800-950μm deep into the primary visual cortex (V1) contralateral to the stimulated eye to record local field potentials (LFPs).
Stimulation Parameters Tested: Researchers systematically varied (1) phase duration (500μs, 1000μs, 1500μs), (2) frequency (1Hz, 10Hz, 20Hz), and (3) interphase interval (presence/absence) while recording electrically evoked potentials (EEPs) in the visual cortex. Charge-balanced biphasic pulses were delivered, and cortical responses were analyzed for activation thresholds and spatial spread.
Key Findings: Shorter phase durations (500μs) elicited V1 activation at lower charge thresholds. Longer phase durations (1000-1500μs) and inclusion of an interphase interval resulted in more confined spread of cortical activation. Responses to repetitive stimulation were significantly attenuated at high frequencies (10-20Hz) compared to low frequency stimulation (1Hz) [69].
Protocol 2: Neuromuscular Electrical Stimulation in Fibromyalgia
A randomized controlled study investigated the effects of NMES combined with conventional treatment (CT) versus CT alone in 40 female fibromyalgia patients over 6 weeks [66].
Methodology: Participants were randomized to either NMES+CT or CT alone groups. The NMES group received electrical stimulation applied to key muscle groups in addition to standard conventional therapy. Assessments included pain intensity (Visual Analog Scale), sleep quality (Pittsburg Sleep Quality Index), quality of life (Fibromyalgia Impact Questionnaire), and posture (New York Posture Rating Chart) at baseline and post-treatment.
Stimulation Parameters: While the specific NMES parameters (frequency, pulse duration) were not detailed in the available abstract, the treatment duration was 6 weeks with regularly applied sessions [66].
Key Findings: The NMES+CT group demonstrated significantly greater improvements in pain intensity (p=0.015) and posture (p=0.014) compared to the CT alone group. Both groups showed significant within-group improvements across multiple outcomes, but the between-group difference was most pronounced for pain and postural measures, suggesting specific benefits of NMES for these domains [66].
Protocol 3: Optimal Control-Driven Functional Electrical Stimulation
A scoping review of 52 studies examined optimal control approaches for FES, which aim to improve motion precision and reduce muscle fatigue [67].
Methodology: The review analyzed both in silico (25 studies) and in vivo (27 studies) investigations, encompassing 94 participants (predominantly healthy young males). Studies typically employed FES models that modulated pulse width or intensity to track joint angle during single-joint lower-limb movements. Optimal control problems (OCP) primarily addressed joint tracking and FES activation dynamics.
Key Findings: Optimal control-driven FES can produce accurate motions and reduce fatigue, though the technology remains at approximately Technology Readiness Level (TRL) 5. Significant challenges include lack of consensus on modeling approaches, inconvenient model identification protocols, and limited validation in diverse patient populations. Only six in vivo studies demonstrated reduced fatigue through optimal control approaches [67].
Signaling Pathways and Experimental Workflows
Diagram 1: Parameter Optimization Logic Flow (Title: Electrical Stimulation Parameter Optimization Framework)
Diagram 2: Visual Cortex Activation Protocol (Title: Retinal Stimulation Experimental Workflow)
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Research Materials for Electrical Stimulation Studies
| Item | Function | Example Specifications | Application Context |
|---|---|---|---|
| Bipolar Concentric Electrode | Delivers focal electrical stimulation to target tissue | Pt/Ir, 75μm diameter [69] | Retinal stimulation studies |
| Grid Electrode Array | Records multidimensional electrophysiological responses | 4×4 grid, 16 electrodes, 400μm inter-tip distance [69] | Cortical mapping of evoked potentials |
| Potentiostat | Monitors electrode-tissue interface impedance | AC sinusoid signal at 100kHz, 10-mV (r.m.s.) [69] | Real-time electrode positioning verification |
| Belt-Type Electrodes | Provides distributed stimulation across large muscle groups | Multi-electrode configuration for trunk and limbs [70] | Whole-body neuromuscular stimulation |
| Therapeutic Electrical Stimulator | Generates controlled stimulation waveforms | G-TES system; 20Hz frequency, 250μs pulse width [70] | Clinical applications in frail populations |
| Data Acquisition System | Records and processes electrophysiological signals | Micro1401 CED system; 25kHz sampling rate [69] | High-fidelity signal capture for analysis |
| Impedance Monitoring System | Ensures consistent electrode-tissue contact | Real-time measurement during electrode placement [69] | Quality control in experimental setups |
| 3-Amino-4-hydroxybenzonitrile | 3-Amino-4-hydroxybenzonitrile, CAS:14543-43-2, MF:C7H6N2O, MW:134.14 g/mol | Chemical Reagent | Bench Chemicals |
The optimization of electrical stimulation parameters represents an evolving frontier in neurotechnology, with significant implications for therapeutic efficacy and patient safety. Current evidence demonstrates that systematic parameter manipulation—including phase duration, frequency, interphase intervals, and treatment duration—can substantially influence physiological outcomes across diverse applications from retinal prostheses to musculoskeletal rehabilitation. The growing understanding of neural responses to electrical stimulation, coupled with advancements in electrode technology and optimal control algorithms, promises to enhance the precision and effectiveness of these interventions.
Future research directions should address several critical gaps identified in this analysis. First, standardized reporting of stimulation parameters across studies would facilitate meta-analyses and cross-study comparisons. Second, the development of patient-specific optimization protocols based on individual neurophysiology could maximize therapeutic outcomes. Third, longitudinal studies examining long-term safety and adaptive responses to chronic stimulation are needed, particularly for implantable devices. Finally, the translation of optimal control approaches from laboratory demonstrations to clinical practice requires addressing current limitations in model identification and validation [67]. As the field progresses, these advances will strengthen the evidence base for electrical stimulation therapies and expand their clinical utility across a broadening spectrum of neurological and musculoskeletal disorders.
Clinical trials, particularly in the specialized field of neurotechnology, face a complex array of operational and scientific challenges that can compromise their successful execution and the validity of their findings. The convergence of technological innovation, regulatory evolution, and methodological complexity has created an environment where researchers must adeptly troubleshoot critical aspects of trial design and management. Within this context, three fundamental areas consistently demand strategic attention: patient recruitment, endpoint measurement, and data integrity. Failures in any of these domains can result in costly delays, inconclusive results, or failed trials, with studies revealing that 80% of clinical studies fail to meet their enrollment deadlines, while recruitment costs consume 40% of all trial expenditures [71]. For trial sponsors, every month of delay can cost an additional $1 million, and a failed clinical trial can represent a loss of $800 million to $1.4 billion [71]. This guide systematically compares contemporary solutions across these three critical domains, providing researchers with evidence-based frameworks for optimizing trial performance within neurotechnology safety and efficacy evaluation.
Patient Recruitment: From Traditional Barriers to Digital Solutions
Comparative Analysis of Modern Patient Recruitment Strategies
Traditional patient recruitment methods, reliant on physician referrals and local advertising, increasingly prove inadequate for modern clinical trials, especially in neurotechnology where specific patient phenotypes are often required. These conventional approaches are characterized by geographic limitations, low patient awareness, and inefficient screening processes that lead to screen failure rates exceeding 80% for complex trials [71]. Digital recruitment strategies have emerged to address these bottlenecks, leveraging technology to reach broader, more targeted populations while improving efficiency.
Table 1: Quantitative Comparison of Patient Recruitment Strategies
| Strategy | Reported Impact on Enrollment | Time Efficiency Gain | Relative Cost | Key Advantages |
|---|---|---|---|---|
| AI-Powered Pre-Screening | Increases by 30-50% [71] | Reduces screening time by 60% [71] | High initial, lower long-term | Precision targeting, reduced screen failures |
| Digital Advertising (Social/Search) | 40% higher conversion than traditional [72] | Cuts initial recruitment phase by 50% [72] | Medium, highly scalable | Demographic targeting, real-time optimization |
| Patient Matching Platforms | 25-35% of total enrollment [72] | Steady stream of pre-qualified candidates | Variable per platform | Access to motivated, trial-seeking patients |
| Healthcare Provider Referrals | 64% of patients prefer this route [72] | Slow but high-quality leads | Low direct cost | Built on established trust, higher retention |
| Decentralized Clinical Trial Models | Improves rural access by 200% [73] | Reduces participant burden significantly | High infrastructure | Geographic diversity, improved retention |
The transformation toward digital-first recruitment is underscored by several technological shifts. Leading organizations now leverage predictive analytics, real-time monitoring, and advanced attribution modeling to continually enhance recruiting performance instead of simply tracking enrollment [74]. The regulatory acceptance of remote and hybrid trial models during the COVID-19 pandemic has reshaped patient expectations and created lasting opportunities for researchers to reach participants beyond their local regions [74]. Furthermore, the professionalization of recruitment operations within research organizations recognizes that effective recruitment requires dedicated expertise, not just clinical knowledge or good intentions [74].
Experimental Protocol for Implementing Digital Recruitment
Protocol Title: Multi-Channel Digital Recruitment Framework for Neurotechnology Trials
Objective: To systematically evaluate and implement a coordinated digital recruitment strategy for a neurotechnology clinical trial targeting patients with social anxiety disorder, maximizing enrollment efficiency and participant diversity.
Methodology:
Patient Population Analysis: Conduct preliminary research to understand target demographic characteristics, online behavior patterns, and primary concerns related to their condition. This foundational step informs messaging strategy and channel selection [72].
Channel Selection and Integration: Deploy a balanced multi-channel approach:
- Targeted Social Media Advertising: Utilize Facebook and Instagram ads targeting users aged 18-70 with interests related to anxiety treatments, mental health wellness, and relevant support groups. Ads should feature relatable imagery and focus on the condition rather than overly emphasizing the clinical trial aspect [72].
- Search Engine Optimization: Develop a dedicated, mobile-optimized landing page with clear calls-to-action ("Apply now" or "Learn more"), comprehensive trial information, and eligibility criteria. Optimize page content with keywords potential participants use when seeking health information online (e.g., "new social anxiety treatments," "clinical trials for anxiety") [72].
- Patient Matching Platforms: List the trial on established platforms like ResearchMatch to access individuals actively seeking clinical trial opportunities [72].
- Electronic Health Record (EHR) Mining: Implement AI-powered algorithms to identify potentially eligible patients through secure analysis of de-identified EHR data based on trial inclusion/exclusion criteria [71].
Pre-Screening and Consent: Deploy an AI-powered pre-screening chatbot on the landing page to conduct initial eligibility assessments 24/7, collecting basic information and providing immediate feedback to potential participants while reducing administrative burden [71].
Performance Monitoring: Establish key metrics including cost per eligible lead, screen failure rate, and enrollment rate by channel. Use real-time analytics to continuously refine advertising spend and messaging based on performance data [74].
Expected Outcomes: Implementation of this protocol should reduce recruitment timelines by approximately 40%, decrease screen failure rates below 30%, and yield a participant pool that better represents the target population demographically and geographically [71].
Digital Recruitment Workflow: This diagram illustrates the sequential workflow for implementing a digital recruitment strategy, from initial planning through continuous optimization.
Research Reagent Solutions for Patient Recruitment
Table 2: Essential Tools for Modern Patient Recruitment
| Solution Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| AI-Patient Matching Platforms | Deep 6 AI, Antidote [73] | Accelerates identification of eligible patients from EHR and real-world data | Requires data integration capabilities; addresses data privacy |
| Decentralized Clinical Trial (DCT) Platforms | Science 37, Medable [73] | Enables remote participation and data collection | Reduces geographic barriers; requires regulatory compliance |
| Digital Advertising Platforms | Google Display Ads, Meta Business Suite [72] | Targets potential participants based on demographics, interests, and online behavior | Enables A/B testing; needs IRB-approved language |
| Patient Facing Technology | E-Consent platforms, Patient portals [74] | Facilitates remote informed consent and ongoing engagement | Improves accessibility; must maintain human touchpoints |
| Analytics and Attribution Tools | Real-time recruitment dashboards [74] | Tracks channel performance and enrollment metrics | Enables data-driven optimization; requires data standardization |
Endpoint Measurement: Strategic Selection and Multiplicity Management
Advanced Endpoint Frameworks for Neurotechnology Trials
Endpoint selection and analysis present particular challenges in neurotechnology trials, where efficacy signals may be subtle, multidimensional, or evolve over varying timeframes. The complexity is further compounded when supporting regulatory claims for multiple clinical endpoints and dose regimens due to issues of multiplicity and sample size constraints [75]. Joint Primary Endpoints (JPEs) offer a compelling strategy to address these challenges by combining multiple clinically meaningful endpoints into a composite measure, thereby enhancing the sensitivity to detect treatment effects in complex neurological conditions [75].
Recent methodological advancements include robust two-stage gatekeeping frameworks designed to test two hierarchically ordered families of hypotheses. These approaches employ novel truncated closed testing procedures in the first stage, enhancing flexibility and adaptability in evaluating primary endpoints while strategically propagating a controlled fraction of the error rate to the second stage for assessing secondary endpoints [75]. This ensures rigorous control of the global family-wise Type I error rate across both stages, which is particularly crucial in neurotechnology trials where multiple outcome domains (e.g., cognitive, functional, biomarker) must be assessed comprehensively.
Table 3: Comparison of Endpoint Configurations in Neurotechnology Trials
| Endpoint Strategy | Statistical Considerations | Regulatory Acceptability | Therapeutic Context | Key Limitations |
|---|---|---|---|---|
| Single Primary Endpoint | Straightforward sample size calculation; no multiplicity adjustment needed | High - clearly interpretable | Conditions with a single dominant efficacy measure | May miss multidimensional treatment effects |
| Joint Primary Endpoints (JPE) | Requires predefined hierarchical testing; controls Type I error [75] | Medium-High with proper statistical planning | Complex disorders like Alzheimer's or Parkinson's | Complex interpretation if components disagree |
| Multiple Co-Primary Endpoints | Requires strong control of family-wise error rate; larger sample size | Medium with rigorous multiplicity control | When treatment must demonstrate benefit on all measures | High statistical hurdle; potentially underpowered |
| Composite Endpoints | Combates multiple outcomes into single measure; requires component validation | Medium - depends on clinical relevance | Conditions where individual outcomes are inadequate | Masking of effects on individual components |
| Primary with Secondary Hierarchical Testing | Gatekeeping procedures control alpha spending across endpoints [75] | High with predefined testing hierarchy | Most neurotechnology applications | Testing stops when hierarchy is breached |
The application of these sophisticated endpoint strategies is illustrated in recent neurological trials. For example, a phase 2 study of AR1001 in Alzheimer's disease utilized co-primary efficacy endpoints (changes in ADAS-Cog13 and ADCS-CGIC) while also examining multiple secondary endpoints and plasma biomarkers [36]. Although the primary endpoints were not met, the trial detected favorable changes in AD-related plasma biomarkers (pTau-181, pTau-217, and GFAP), demonstrating how comprehensive endpoint strategies can provide valuable insights even when primary objectives are not achieved [36].
Experimental Protocol for Implementing Joint Primary Endpoints
Protocol Title: Gatekeeping Procedure for Joint Primary Endpoints in Neurotechnology Trials
Objective: To implement a statistically robust methodology for evaluating joint primary endpoints while controlling family-wise error rate and efficiently assessing secondary endpoints in a neurotechnology clinical trial.
Methodology:
Endpoint Definition and Hierarchical Structuring:
- Define two joint primary endpoints (e.g., cognitive performance and functional independence in dementia trials).
- Establish a predefined hierarchical testing order for the endpoints based on clinical importance.
- Define secondary endpoint families (e.g., quality of life measures, biomarker changes).
Statistical Analysis Plan:
- Employ a two-stage gatekeeping procedure with a truncated closed testing principle for the primary endpoint family [75].
- Set significance levels for each hypothesis in the hierarchy, typically starting with α = 0.05 for the first endpoint.
- Pre-specify the alpha propagation rule to determine how much alpha will be passed to subsequent endpoints in the hierarchy.
Analysis Execution:
- Test the first primary endpoint at the full significance level (e.g., α = 0.05).
- If significant, proceed to the second primary endpoint using predetermined alpha allocation rules.
- Upon success on primary endpoints, utilize the recycled alpha from the gatekeeping procedure to test ordered secondary endpoints while maintaining strong control over family-wise error rate [75].
Interpretation and Reporting:
- Clearly document the testing hierarchy and any modifications to alpha levels throughout the procedure.
- Report both statistically significant and non-significant results within the predefined framework.
- Interpret findings in the context of the hierarchical testing sequence, acknowledging that failure at any stage terminates the testing procedure for subsequent endpoints.
Expected Outcomes: This protocol provides a statistically rigorous approach to evaluate multiple endpoints while controlling Type I error inflation, leading to more reliable conclusions about treatment effects across multiple domains of neurotechnology efficacy.
Endpoint Testing Hierarchy: This diagram visualizes the sequential gatekeeping procedure for testing joint primary and secondary endpoints while controlling family-wise error rate.
Research Reagent Solutions for Endpoint Measurement
Table 4: Essential Tools for Advanced Endpoint Assessment
| Solution Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| Clinical Outcome Assessments (COAs) | ADAS-Cog, MMSE, LSAS [76] [36] | Standardized measurement of patient-reported, observer-reported, and performance outcomes | Requires validation in target population; cultural adaptation |
| Digital Biomarkers | Wearable sensors, Mobile cognitive testing [73] | Provides continuous, objective measurement of neurological function | Needs technical validation; regulatory acceptance evolving |
| Statistical Analysis Platforms | R, SAS with multiplicity procedures [75] | Implements complex statistical methods for endpoint analysis | Requires specialized statistical expertise; predefined SAP |
| Biomarker Assay Kits | pTau-181, pTau-217, GFAP, NfL immunoassays [36] | Quantifies pathological biomarkers in biofluids | Needs analytical validation; standardized protocols essential |
| Data Collection Systems | EDC systems with eCOA integration | Captures endpoint data consistently across sites | Requires training; ensures data quality and compliance |
Data Integrity: From Collection to Reporting in the Regulatory Landscape
Comparative Framework for Data Integrity Management
Data integrity remains foundational to clinical trial credibility, particularly in neurotechnology where subtle treatment effects demand exceptional data quality. Recent analyses reveal that while improvements have occurred following the 2017 FDAAA Final Rule, many trials remain non-compliant with reporting requirements, with significant variability across organization types [77]. Large industry sponsors typically report results information more consistently, largely due to established regulatory affairs departments, while academic medical centers (AMCs) often struggle with timely reporting despite their critical role in the research ecosystem [77].
The data integrity landscape in 2025 is shaped by several regulatory developments. The finalization of ICH E6(R3) emphasizes proportionate, risk-based quality management, data integrity across all modalities, and clear sponsor-investigator oversight [78]. The EU Clinical Trials Regulation (CTR), fully applicable as of January 31, 2025, requires all EU trials to operate under the centralized CTIS portal, increasing public transparency and enforcing stricter timelines [78]. Simultaneously, FDA guidance on decentralized trials, AI, and digital health technology has codified requirements for model validation, transparency, and governance [78].
Table 5: Data Integrity Challenge and Solution Comparison
| Data Integrity Challenge | Traditional Approach | Modern Solution | Impact on Data Quality |
|---|---|---|---|
| Incomplete ClinicalTrials.gov Reporting | Manual compliance tracking | Centralized institutional processes with dedicated resources [77] | Improves scientific transparency and reduces reporting bias |
| Inconsistent Data Collection | Paper source documents followed by EDC entry | Electronic data capture (EDC) with automated checks | Reduces transcription errors and missing data |
| Inadequate Monitoring | 100% source data verification | Risk-based quality management (RBQM) [78] | Focuses resources on highest risk areas; more efficient |
| Poor Protocol Compliance | Manual protocol adherence checks | Structured machine-readable protocols (ICH M11) [78] | Enhances consistency across sites; enables automation |
| Data Security Vulnerabilities | Physical security and basic access controls | Blockchain technology, federated learning systems [73] [71] | Enhances security while maintaining data utility |
The transformation toward automated, risk-based data integrity systems represents a significant shift from traditional approaches. Rather than applying uniform monitoring intensity across all trial aspects, risk-based quality management (RBQM) must now be integrated throughout the study lifecycle, not just applied to monitoring activities [78]. This includes centralized monitoring techniques that use statistical surveillance to identify unusual data patterns across sites, as well as targeted on-site monitoring focused on critical data and processes.
Experimental Protocol for Implementing Risk-Based Data Integrity
Protocol Title: Risk-Based Data Integrity Framework for Neurotechnology Trials
Objective: To implement a comprehensive, proportionate approach to data quality management that prioritizes resources toward the highest risks to data integrity and participant safety in neurotechnology trials.
Methodology:
Risk Assessment and Triage:
- Conduct preliminary risk assessment during protocol development identifying critical data points and processes most vulnerable to integrity issues.
- Categorize risks based on potential impact on participant safety and trial conclusions.
- Develop a risk-based monitoring plan that allocates resources according to identified risks.
Centralized Monitoring Implementation:
- Establish centralized statistical surveillance to detect unusual data patterns across sites using key risk indicators (KRIs).
- Implement automated checks for data ranges, consistency, and plausibility within the EDC system.
- Utilize visualization tools to identify site-level deviations and data trends requiring investigation.
Targeted On-Site Activities:
- Focus on-site monitoring on critical activities including informed consent documentation, IP accountability, and serious adverse event reporting.
- Verify source data for primary efficacy endpoints and key safety parameters rather than 100% source data verification.
- Conduct targeted training based on centralized monitoring findings to address specific deficiencies.
Transparency and Reporting Compliance:
- Implement automated tracking systems for regulatory reporting deadlines from trial initiation.
- Prepare results summaries concurrently with database lock to facilitate timely ClinicalTrials.gov submission.
- Conduct pre-submission quality control reviews to ensure complete and accurate results reporting.
Expected Outcomes: This protocol reduces monitoring costs by 20-30% while improving data quality focus, ensures timely reporting compliance, and creates a defensible audit trail demonstrating comprehensive data integrity oversight.
Risk-Based Data Integrity Process: This diagram outlines the continuous cycle of risk assessment, centralized monitoring, and targeted intervention for maintaining data integrity.
Research Reagent Solutions for Data Integrity
Table 6: Essential Tools for Ensuring Data Integrity
| Solution Category | Specific Examples | Primary Function | Implementation Considerations |
|---|---|---|---|
| Electronic Data Capture (EDC) Systems | Commercial EDC with audit trails | Captures clinical data electronically with full provenance | Requires 21 CFR Part 11 compliance; user training |
| Clinical Trial Management Systems (CTMS) | CTMS with compliance tracking | Manakes trial operations and tracking | Should integrate with EDC and reporting systems |
| Risk-Based Quality Management Platforms | Centralized monitoring systems | Statistical surveillance of data quality across sites | Needs predefined risk indicators and thresholds |
| Regulatory Submission Portals | ClinicalTrials.gov, EU CTIS [77] [78] | Official channels for trial registration and results reporting | Requires dedicated resources and processes |
| Data Standardization Tools | CDISC SDTM/ADaM converters [78] | Transforms data into regulatory-compliant formats | Early planning reduces rework; needs expertise |
In the specialized field of neurotechnology, the continuous evolution of software presents a unique set of challenges and imperatives. Implantable neuromodulation devices, which treat neurological diseases and restore sensory and motor function, rely on sophisticated software for operation, data analysis, and therapy delivery [35]. The safety and efficacy of these devices are paramount, as they directly impact patient health and clinical outcomes. While hardware innovations like novel electrode materials and designs progress, the software controlling these systems requires diligent management to ensure long-term reliability and robust data security. This guide objectively compares the security and reliability postures of maintained versus outdated software environments within neurotechnology research and deployment, providing a framework for evaluating performance in this critical domain.
The Quantifiable Risks of Outdated Software
The decision to delay or forgo software updates is often a calculated risk. However, data reveals that this calculation frequently underestimates the true probability and impact of a security incident. The following statistics illuminate common patching practices and the associated vulnerabilities.
Table 1: Software Patching Statistics and Associated Risks
| Metric | Finding | Source |
|---|---|---|
| Organizations with severe vulnerabilities | 57% of organizations operated web servers with a known, severe vulnerability after a fix was available. | [79] |
| Attacks via unpatched software | 32% of cyberattacks exploit unpatched software vulnerabilities. | [80] |
| Breach prevention via patching | 80% of data breaches could have been prevented by timely patching or configuration updates. | [81] |
| Time to close vulnerabilities | Organizations take an average of 67 days to close a discovered vulnerability. | [81] |
| Exploitation speed | 25% of Common Vulnerabilities and Exposures (CVEs) are exploited on the same day they are published. | [80] |
| Use of legacy systems | 58% of organizations run on legacy systems that are no longer supported with patches. | [81] |
For neurotechnology devices, these risks are magnified. A security breach could lead to unauthorized access to sensitive patient neural data or, in a worst-case scenario, manipulation of therapy delivery. Furthermore, the "patching paradox" is evident: despite organizations planning to hire more personnel for vulnerability response, simply adding staff does not resolve the underlying challenges of manual processes and prioritization difficulties [81]. The core reasons for update delays are multifaceted, including fear of updates "breaking" critical systems (72% of managers), the high cost and time required for manual updates, and a reluctance to accept ancillary functionality changes that accompany security patches [81] [80].
Comparative Analysis: Updated vs. Outdated Systems Security Posture
A direct comparison of updated and outdated systems reveals a stark contrast in security, reliability, and operational efficiency. This comparison is critical for risk assessment in neurotechnology research, where device integrity directly influences experimental validity and patient safety.
Table 2: Security Posture Comparison: Updated vs. Outdated Systems
| Aspect | Updated Systems | Outdated Systems |
|---|---|---|
| Attack Surface | Minimized through timely patching of known vulnerabilities. | Expanded by an accumulation of unpatched, known vulnerabilities. |
| Exploitability | Significantly reduced; attackers must find novel, unpatched flaws. | Highly exploitable; attackers use automated tools for known flaws. |
| Vendor Support | Full security support and patch availability from the manufacturer. | No support or patches after End-of-Life (EOL), creating permanent risks. |
| Data Security | Protected by the latest cryptographic standards and security protocols. | Relies on weak, compromised algorithms (e.g., old TLS, SHA-1). |
| Operational Stability | Risk of rare update failures (as with CrowdStrike) but generally stable. | High risk of disruption from cyberattacks exploiting known weaknesses. |
| Compliance Status | Typically aligns with data protection and medical device regulations. | High risk of failing audits and violating regulatory requirements. |
The fundamental reason for the increased risk in outdated systems is the presence of unpatched known vulnerabilities. Once a flaw is publicly disclosed in databases like the Common Vulnerabilities and Exposures (CVE), it provides a roadmap for attackers [80]. Outdated software, by definition, contains these identified but unaddressed weaknesses. In neurotechnology, this could translate to vulnerabilities in the software that controls neural modulation parameters or collects high-fidelity neural data, potentially compromising both safety and efficacy research data [35].
Experimental Protocols for Evaluating Update Impact and System Security
To objectively assess the impact of software updates and the risks of outdated systems, researchers and IT professionals employ a range of methodologies. The following protocols detail key experiments cited in the comparative analysis.
Protocol 1: Vulnerability Window and Exploitability Assessment
This protocol quantifies the risk window between a patch release and its deployment, a critical metric for any system handling sensitive data.
- Objective: To measure the time an asset remains vulnerable to known exploits after a patch is available and to assess its actual exploitability.
- Methodology:
- Asset Inventory & CVE Mapping: Maintain a real-time inventory of all software assets and their versions. Subscribe to CVE feeds from sources like the National Vulnerability Database (NVD) and vendor-specific security advisories.
- Patch Deployment Timing: For a defined period (e.g., 6 months), record the time of publication for every relevant patch and the time of its successful deployment across test and production environments.
- Exploitability Testing: In an isolated test environment, deploy unpatched systems. Utilize platforms like Metasploit or publicly available Proof-of-Concept (PoC) exploit code to attempt to compromise the system for each unpatched CVE classified as "Critical" or "High" severity.
- Data Collection: Record the "vulnerability window" (deployment time minus patch release time) for each patch. Document the success rate of exploit attempts, the level of access gained, and the time required for a successful compromise.
- Analysis: Calculate the mean and median vulnerability windows. Corregate the success rate of exploits against the age of the unpatched vulnerability. This data provides empirical evidence for the risk of update delays, showing that, as noted in the statistics, a significant proportion of vulnerabilities are exploited rapidly after publication [80].
Protocol 2: Safety and Efficacy of Update-Induced System Changes
This protocol is paramount for neurotechnology, where any system change must be evaluated for its impact on the device's primary function.
- Objective: To verify that a software update does not adversely affect the safety or performance of a neuromodulation device or the research data it generates.
- Methodology:
- Pre-Update Baseline Establishment: Conduct a full suite of functional, performance, and safety tests on the stable system before update application. This includes:
- Therapy Accuracy: Measuring the fidelity of electrical stimulation output (e.g., waveform, amplitude, frequency) against predefined parameters.
- Data Integrity: Verifying the accuracy and completeness of recorded neural signals or other biomarker data.
- System Stability: Documenting baseline metrics for uptime and resource utilization (CPU, memory).
- Controlled Update Application: Apply the software update in a controlled test environment that mirrors the production setup as closely as possible.
- Post-Update Validation Testing: Repeat the exact same battery of tests conducted during the baseline establishment.
- Long-Term Monitoring: Continue monitoring for aberrant behavior or performance degradation over a predefined period (e.g., 30 days).
- Pre-Update Baseline Establishment: Conduct a full suite of functional, performance, and safety tests on the stable system before update application. This includes:
- Data Collection: Collect quantitative data on stimulation parameters, signal-to-noise ratios in neural recordings, system resource usage, and any functional errors or crashes.
- Analysis: Compare pre- and post-update data using statistical methods to identify significant deviations. This process helps mitigate the primary fear of updates "breaking stuff," a concern cited by 72% of managers [81]. It provides a scientific basis for approving or rejecting an update.
The Scientist's Toolkit: Key Research Reagent Solutions
Managing software evolution in a research environment requires a set of specialized tools and resources. The following table details essential "research reagents" for maintaining software integrity and security.
Table 3: Essential Research Reagent Solutions for Software Management
| Item | Function & Explanation |
|---|---|
| Vulnerability Scanner | Automatically scans software assets to identify known vulnerabilities (CVEs), misconfigurations, and outdated components. This replaces manual tracking and is fundamental for risk assessment. |
| Patch Management Platform | Automates the deployment of software updates across multiple endpoints or servers. Tools like Heimdal can reduce the patch deployment window to within hours of release, addressing the time-cost of manual updates [81]. |
| Configuration Management DB | A database that tracks all hardware and software configuration items. It is essential for understanding dependencies and assessing the impact of updates, preventing unforeseen system conflicts. |
| Isolated Test Environment | A hardware and software replica of the production research environment. It is critical for conducting Protocol 2 (Safety and Efficacy) without risking the live research setup or data. |
| CVE/NVD Feeds | Subscriptions to real-time feeds from the National Vulnerability Database and other sources. These provide the raw intelligence on newly discovered threats relevant to the software inventory. |
| Software Bill of Materials | A nested inventory of all components and dependencies within a software product. It is crucial for identifying risks from vulnerable third-party libraries, such as those highlighted in the OWASP Top 10 [80]. |
Strategic Mitigation for Long-Term Reliability
Addressing the challenges of software evolution requires a strategic shift from reactive to proactive management. Key mitigation strategies include:
- Implementing Robust Patch Management: Move beyond manual processes to automated patch management solutions. This directly addresses the primary cost and coordination challenges, with some tools capable of deploying patches within hours [81]. Policies should prioritize patches based on severity and exploitability, not just on a fixed calendar.
- Managing End-of-Life (EOL) Software: Proactively identify and plan for the retirement of software components reaching EOL. Where replacement is not immediately feasible, implement compensating controls such as strict network segmentation to isolate vulnerable systems and virtual patching using intrusion detection/prevention systems to block exploit attempts [80].
- Cultivating a Security-Aware Culture: Technical controls are insufficient without organizational buy-in. Training and clear communication can help overcome the reluctance to update based on fear of functionality changes or operational disruption [80].
In the context of neurotechnology safety and efficacy evaluation, managing device evolution through software updates is not an IT overhead but a foundational component of research integrity and patient safety. The data clearly demonstrates that updated systems provide a significantly more secure, reliable, and compliant foundation for research and clinical deployment than their outdated counterparts. By adopting the experimental protocols and strategic mitigations outlined in this guide, researchers and developers can make informed, evidence-based decisions that ensure the long-term reliability and security of their critical neuromodulation technologies.
Comparative Analysis and Validation Frameworks for Neurotherapies
This guide provides an objective, data-driven comparison between five third-generation anti-seizure medications (ASMs) and two non-invasive brain stimulation (NIBS) techniques for the treatment of refractory epilepsy. The analysis is framed within the critical context of neurotechnology safety and efficacy evaluation, providing researchers and drug development professionals with a synthesis of comparative performance metrics, detailed experimental methodologies, and essential research tools. The data reveals a clear efficacy hierarchy among these interventions, underscoring the importance of safety and efficacy profiling in advancing neurotherapeutic development.
Comparative Efficacy and Safety Data
The following tables synthesize quantitative data on efficacy and safety from a recent network meta-analysis encompassing 45 studies [82] [83]. The outcomes are primarily measured against placebo for patients with refractory epilepsy (seizures uncontrolled by one or more concomitant ASMs).
Table 1: Comparative Efficacy of Third-Generation ASMs and NIBS
| Intervention | Full Name | Change in Seizure Frequency from Baseline (vs. Placebo) | ≥50% Responder Rate (vs. Placebo) | Ranking for Seizure Frequency Reduction (SUCRA) | Ranking for 50% Responder Rate (SUCRA) |
|---|---|---|---|---|---|
| ESL | Eslicarbazepine acetate | Significant decrease [82] | Significantly higher [82] | 1st (Best) [82] | - |
| CNB | Cenobamate | Significant decrease [82] | Significantly higher [82] | - | 1st (Best) [82] |
| LCM | Lacosamide | Significant decrease [82] | Significantly higher [82] | Among most effective [82] | - |
| BRV | Brivaracetam | Significant decrease [82] | Significantly higher [82] | - | - |
| PER | Perampanel | Significant decrease [82] | Significantly higher [82] | - | - |
| rTMS | Repetitive Transcranial Magnetic Stimulation | Significant decrease (less effective than ASMs) [82] | - | - | - |
| tDCS | Transcranial Direct Current Stimulation | Significant decrease (less effective than ASMs) [82] | - | - | - |
Table 2: Comparative Safety Profile of Third-Generation ASMs and NIBS
| Intervention | Treatment-Emergent Adverse Events (TEAEs) vs. Placebo | Safety Ranking (SUCRA) / Notes |
|---|---|---|
| BRV | Associated with fewer adverse events (p<0.05) [82] | 1st (Best Tolerated) [82] |
| CNB, ESL, LCM, PER | Associated with fewer adverse events (p<0.05) [82] | - |
| rTMS | Safety confirmed [82] | Generally safe, no significant side effects or complications [82] |
| tDCS | Safety confirmed [82] | Generally safe, painless, and non-invasive [82] |
Detailed Experimental Protocols
The comparative data presented above is derived from a specific methodological framework. Understanding this framework is crucial for interpreting the results and designing future studies.
Network Meta-Analysis Protocol
The foundational evidence for this guide comes from a systematic review and network meta-analysis [82] [83].
- Study Design Inclusion: The analysis included randomized, double-blind, placebo-controlled, add-on studies. Other cohort studies were included if they achieved a Newcastle-Ottawa scale (NOS) quality score of ≥5 [82] [83].
- Participant Criteria: Patients were diagnosed with refractory epilepsy, defined by the International League Against Epilepsy (ILAE) as seizures uncontrolled by the appropriate choice and use of two ASMs. Concomitant ASMs were required to be stable before and throughout the trial period [82] [83].
- Intervention & Control: The interventions were add-on therapies to a patient's stable ASM regimen. The active interventions included five third-generation ASMs (BRV, CNB, ESL, LCM, PER) and two NIBS techniques (rTMS, tDCS). The common control was placebo [82] [83].
- Outcome Measures:
- Statistical Analysis: A random-effects model was used to incorporate heterogeneity. Efficacy and safety were ranked for each intervention using the Surface Under the Cumulative Ranking Curve (SUCRA), a percentage that represents the relative position of each treatment [82] [83].
Mechanism of Action Protocols
The biological rationale for these therapies stems from their distinct mechanisms of action.
- Brivaracetam (BRV): Binds to synaptic vesicle glycoprotein 2A (SV2A) in the brain, which is involved in regulating neurotransmitter release [82].
- Eslicarbazepine Acetate (ESL) & Lacosamide (LCM): Both selectively modulate voltage-gated sodium channels, stabilizing hyperexcitable neuronal membranes and inhibiting repetitive neuronal firing [84].
- Perampanel (PER): A selective non-competitive antagonist of the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) glutamate receptor, thereby reducing excitatory neurotransmission [84].
- Cenobamate (CNB): Exhibits a dual mechanism: it blocks voltage-gated sodium channels and is a positive allosteric modulator of GABAA receptors, enhancing inhibitory neurotransmission [84].
- Repetitive Transcranial Magnetic Stimulation (rTMS): Uses a rapidly changing magnetic field to induce an electric current in a targeted brain area. The effect on cortical excitability is frequency-dependent:
- Transcranial Direct Current Stimulation (tDCS): Applies a weak, constant direct current to the scalp via electrodes to modulate cortical excitability.
The Scientist's Toolkit: Research Reagent Solutions
This section details key materials and methodological tools essential for conducting rigorous research in this field.
Table 3: Essential Reagents and Tools for ASM & NIBS Research
| Item Name | Function / Rationale | Example Application in Context |
|---|---|---|
| Stable ASM Regimen | Foundation of add-on therapy trials; ensures any change in seizure frequency is attributable to the investigational intervention. | Required protocol in included RCTs: concomitant ASMs kept stable before and during trial [82]. |
| Placebo Control | Gold-standard for blinding and controlling for placebo effect; critical for establishing efficacy and safety. | Used in all included double-blind studies for both ASM (pill) and NIBS (sham stimulation) arms [82]. |
| Seizure Diary | Primary tool for collecting patient-reported outcome data on seizure frequency and type. | Source data for calculating "change in seizure frequency" and "50% responder rate" [82] [83]. |
| Cochrane Risk of Bias Tool | Standardized tool for assessing methodological quality and potential biases in randomized controlled trials (RCTs). | Used to evaluate the risk of bias in the included RCTs [82] [83]. |
| Newcastle-Ottawa Scale (NOS) | Tool for assessing the quality of non-randomized studies, such as cohort studies. | Used to include higher-quality cohort studies (NOS ≥5) [82] [83]. |
| SUCRA (Statistical Analysis) | Provides a numerical ranking (0-100%) of where each treatment stands relative to others in the network. | Used to rank interventions for efficacy and safety outcomes (e.g., ESL ranked 1st for seizure reduction) [82]. |
| Sham Stimulation Coil | Placebo device for NIBS that mimics the sound and sensation of real rTMS/tDCS without delivering the full neural stimulus. | Essential for blinding participants in controlled trials evaluating rTMS and tDCS [82]. |
Validation Frameworks for Brain-Computer Interfaces (BCIs) and Neuromodulation Devices
Brain-Computer Interfaces (BCIs) and neuromodulation devices represent a transformative frontier in neurotechnology, requiring rigorous validation frameworks to ensure their safety and efficacy. A BCI is fundamentally a system that measures brain activity and converts it in real-time into functionally useful outputs, changing the ongoing interactions between the brain and its external or internal environments [1]. As of 2025, these systems are transitioning from laboratory experiments into clinical trials and early commercial applications, making robust validation methodologies more critical than ever [1].
Validation of these neurotechnologies occurs across multiple domains, including technical performance, clinical efficacy, safety profiles, and user acceptability. The convergence of BCIs with artificial intelligence has accelerated the development of more accurate decoders, with some speech BCIs now achieving 99% accuracy with latency under 0.25 seconds - performance metrics that were unthinkable just a decade ago [1]. This rapid advancement necessitates equally sophisticated validation frameworks that can keep pace with innovation while ensuring patient safety and reliable performance.
Comparative Performance Analysis of Major BCI Platforms
The current BCI landscape features multiple approaches with varying levels of invasiveness, technical specifications, and validation milestones. The table below summarizes the key performance metrics and validation status of leading platforms as of 2025.
Table 1: Performance Comparison of Major Implantable BCI Platforms
| Company/Platform | Approach & Invasiveness | Key Technical Specifications | Current Validation Status (as of 2025) | Primary Clinical Targets |
|---|---|---|---|---|
| Neuralink [1] | Intracortical array; Fully invasive | Ultra-high-bandwidth chip with thousands of micro-electrodes | FDA clearance (2023); 5 patients in ongoing trials | Severe paralysis; digital device control |
| Synchron Stentrode [1] | Endovascular; Minimally invasive | Electrode array delivered via blood vessels | 4-patient trial completed; >80% acceptability among neurosurgeons [85]; Planning pivotal trial | Paralysis; computer control |
| Blackrock Neurotech [1] | Intracortical array; Fully invasive | Utah array & Neuralace flexible lattice | Years of academic research; expanding in-home trials | Paralysis; communication |
| Paradromics [1] | Intracortical array; Fully invasive | Connexus BCI with 421 electrodes | First-in-human recording (June 2025); full trial planned late 2025 | Speech restoration |
| Precision Neuroscience [1] | Epithelial array; Minimally invasive | Layer 7 ultra-thin "brain film" | FDA 510(k) cleared (April 2025); 30-day implantation | ALS communication |
Beyond these commercial platforms, non-invasive neuromodulation techniques are also advancing rapidly. A 2025 umbrella review of 18 systematic reviews and meta-analyses found that BCI-combined treatment can significantly improve upper limb motor function and quality of daily life for stroke patients, demonstrating good safety, particularly in the subacute phase [4]. However, the same review noted that effects on improving speech function, lower limb motor function, and long-term outcomes require further evidence through multicenter, long-term follow-up studies [4].
Experimental Protocols for BCI Validation
Clinical Trial Design for Efficacy Assessment
Validating BCIs requires specialized experimental protocols that account for both technical performance and clinical outcomes. For motor rehabilitation in stroke patients, the most robust validation comes from randomized controlled trials with standardized outcome measures.
The key methodological components include:
Population Definition: Clear inclusion/exclusion criteria, typically focusing on patients with specific conditions such as stroke with motor deficits, ALS, or spinal cord injuries. Studies often stratify participants by condition chronicity (acute, subacute, chronic) [4].
Intervention Protocol: BCI systems are typically integrated with functional electrical stimulation (FES) or robotic devices in closed-loop paradigms. Sessions usually last 60-90 minutes, occurring 3-5 times weekly for 4-12 weeks [4].
Control Groups: Active controls may receive sham BCI (random or pre-recorded feedback) or dose-matched conventional therapy [4].
Outcome Measures: Primary outcomes often include Fugl-Meyer Assessment (FMA) for upper extremity motor function and Modified Barthel Index (MBI) for activities of daily living. Secondary outcomes may include electrophysiological measures (EEG-based motor-related cortical potentials) and neuroimaging metrics (fMRI connectivity) [4].
Statistical Analysis: Intention-to-treat analysis with appropriate adjustments for multiple comparisons. Effect sizes are calculated with 95% confidence intervals [4].
Safety and Adverse Event Monitoring
Safety validation follows standardized frameworks for reporting adverse events, with special attention to device-related serious adverse events (SAEs). In invasive BCIs, monitoring includes surgical complications (hemorrhage, infection), device-related issues (migration, failure), and long-term risks (tissue response, scarring) [1] [85]. For the Synchron Stentrode, a 4-patient trial reported no serious adverse events or blood vessel blockages at 12-month follow-up, demonstrating an acceptable safety profile for the minimally invasive approach [1].
Table 2: Standardized Efficacy Metrics from BCI Clinical Studies
| Domain | Primary Assessment Tools | Typical Effect Sizes in Rehabilitation | Evidence Strength |
|---|---|---|---|
| Upper Limb Motor Function | Fugl-Meyer Assessment (FMA) [4] | Significant improvements, especially in subacute stroke [4] | Moderate (multiple systematic reviews) |
| Activities of Daily Living | Modified Barthel Index (MBI) [4] | Improved scores post-BCI training [4] | Moderate |
| Neuromodulation Target Engagement | EEG Motor-Related Cortical Potentials [4] | Increased contralateral activity | Emerging |
| User Acceptability | Technology Acceptability Scales [85] | >80% for restorative uses; divided for augmentation [85] | Limited (single specialty survey) |
| Long-Term Efficacy | Retention of gains at 3-6 month follow-up [4] | Mixed evidence; requires more study [4] | Limited |
Signaling Pathways and Experimental Workflows
The validation of BCIs requires understanding both the technical workflow of the systems and the neural pathways they engage. The following diagrams illustrate these critical processes.
BCI System Workflow
The fundamental operational pipeline of a BCI system follows a consistent pattern across different platforms, with variations in implementation based on the specific technology.
Neural Pathways in BCI-Mediated Rehabilitation
BCI systems for motor rehabilitation engage specific neural pathways that underlie recovery processes. The mechanism involves promoting neuroplasticity through Hebbian learning principles.
The Scientist's Toolkit: Essential Research Reagents and Materials
Validating BCI technologies requires specialized tools, reagents, and equipment. The following table details key components of the BCI research toolkit.
Table 3: Essential Research Toolkit for BCI Validation Studies
| Tool/Reagent Category | Specific Examples | Research Function | Validation Role |
|---|---|---|---|
| Signal Acquisition Systems | EEG systems, ECoG grids, Intracortical microelectrode arrays [1] [86] | Capture neural electrical activity | Signal fidelity, signal-to-noise ratio |
| Signal Processing Tools | MATLAB Toolboxes (EEGLAB, FieldTrip), Python (MNE, Scikit-learn) [86] | Preprocessing, artifact removal, feature extraction | Algorithm performance, reproducibility |
| Neuromodulation Devices | TMS, tDCS, tACS, TMAES systems [87] | Provide targeted neural stimulation | Target engagement, dose-response |
| Behavioral Task Suites | PsychToolbox, Presentation, Unity-based environments | Present standardized stimuli and record responses | Functional efficacy, user performance |
| Biomarker Assays | ELISA kits, RNA sequencing, immunohistochemistry reagents | Assess molecular and cellular responses | Safety, mechanistic understanding |
| Clinical Outcome Measures | FMA, ARAT, MBI scales [4] | Quantify functional improvements | Clinical efficacy, regulatory endpoints |
| Data Sharing Platforms | OpenNeuro, GIN, BCI Competitions | Enable reproducibility and benchmarking | Cross-validation, methodological rigor |
Emerging Frontiers and Validation Challenges
As BCI technology advances, validation frameworks must evolve to address new challenges and applications. Several key areas represent particularly dynamic frontiers in neurotechnology validation.
Non-Invasive Multi-Target Stimulation
Recent advances in non-invasive neuromodulation present novel validation challenges. Techniques like transcranial magneto-acoustic electrical stimulation (TMAES) enable multi-target electrical stimulation with high spatial resolution (approximately 5.1 mm focal point size) at depth, without implantation [87]. However, validating the precision and efficacy of these approaches requires sophisticated phantoms and computational models that can accurately represent the complex electromagnetic and acoustic properties of neural tissue.
Ethical and Social Validation Frameworks
Beyond technical and clinical validation, BCIs introduce profound ethical considerations that require specialized assessment frameworks. Surveys of neurosurgical teams reveal that acceptability of invasive BCI exceeds 80% for restorative applications but is divided for augmentation purposes in healthy populations [85]. This highlights the need for comprehensive ethical frameworks that address emerging concerns about mental privacy, cognitive liberty, and potential misuse such as "brain hacking" [12]. The Organization for Economic Co-operation and Development (OECD) has established international standards for responsible innovation in neurotechnology, emphasizing anticipatory governance and equitable access as core validation principles [12].
Regulatory Science and Real-World Evidence
The regulatory pathway for BCIs is evolving rapidly, with the FDA establishing specialized review processes for neurotechnologies. The transition from feasibility studies to pivotal trials represents a critical validation milestone, as demonstrated by companies like Synchron planning their pivotal trial in 2025 [1]. Post-market surveillance and real-world evidence generation are becoming increasingly important components of the validation lifecycle, particularly for detecting rare adverse events and understanding long-term performance in diverse patient populations.
The validation of Brain-Computer Interfaces and neuromodulation devices requires a multifaceted framework that addresses technical performance, clinical efficacy, safety, and ethical considerations. As the field progresses from proof-of-concept studies to clinical implementation, robust validation methodologies become increasingly critical. The current evidence base, while promising, reveals significant gaps in long-term outcomes and standardization across platforms. Future validation efforts should prioritize multicenter collaborations, standardized outcome measures, long-term follow-up, and comprehensive ethical frameworks to ensure that these transformative technologies deliver on their potential while maintaining the highest standards of safety and efficacy. The rapid pace of innovation demands equally agile validation approaches that can keep pace with technological advancement while protecting patient welfare.
The rapid advancement of neurotechnology presents a dual frontier of unprecedented therapeutic potential and significant safety considerations. For researchers and drug development professionals, a critical step in navigating this landscape is a rigorous, evidence-based comparison of the safety profiles between two fundamental approaches: implantable and non-invasive neurotechnologies. These technologies differ not only in their mechanism of action but also in the nature and severity of their associated risks, which directly influences their application in clinical trials and therapeutic development. This guide provides an objective comparison of their safety and performance, supported by experimental data and detailed methodologies, to inform ethical and scientific decision-making in research and development.
Table 1: Comparative Safety and Performance Profiles of Neurotechnologies
| Feature | Implantable Neurotechnology | Non-Invasive Neurotechnology |
|---|---|---|
| Invasiveness & Primary Risks | Surgical implantation; risks of hemorrhage, infection, and tissue damage [60] [88]. | Non-surgical; generally low risk of serious adverse events [89]. |
| Typical Adverse Events | Seizures, pain at implant site, device failure requiring explantation [88]. | Mild tingling, itching, redness at electrode site; headache; fatigue [89]. |
| Long-Term Safety & Stability | Uncertain long-term effects; risk of glial scarring, signal degradation; device obsolescence requires revision surgery [60] [88]. | Well-tolerated over time; no known long-term tissue damage; effects are typically transient [89]. |
| Signal Fidelity & Performance | High spatial and temporal resolution; records from specific neuronal populations [90]. | Lower spatial resolution and signal-to-noise ratio; records aggregate neural activity [90]. |
| Information Transfer Rate | High, suitable for complex control (e.g., prosthetic limbs, typing) [90]. | Lower, suitable for simpler applications (e.g., neurofeedback, basic control) [90]. |
| Regulatory Status | Stringent medical device regulation; active debate on moratorium for non-medical uses [60] [91]. | Varied; some non-invasive devices are highly regulated as medical devices, others fall under general product safety laws [60]. |
Detailed Experimental Protocols and Data
Protocol: Safety and Tolerability of NIBS in a Pediatric Population with Cerebral Palsy
Objective: To evaluate the safety and effectiveness of Non-Invasive Brain Stimulation (NIBS), including tDCS and rTMS, on mobility and balance in children with Cerebral Palsy (CP) [89].
Methodology:
- Study Design: Systematic review and meta-analysis of 16 Randomized Controlled Trials (RCTs).
- Participants: 346 children with CP, aged 3–14 years.
- Intervention: NIBS protocols (tDCS or rTMS) targeting motor cortex areas. Control groups received sham stimulation.
- Safety Measures: Adverse events were systematically recorded and categorized. Risk Difference (RD) was calculated for adverse events between active and sham stimulation groups.
- Outcome Measures: Gross Motor Function Measure (GMFM) scores, gait velocity, and stride length were assessed immediately post-intervention and at one-month follow-up.
Key Safety Results: The meta-analysis found no significant difference in the risk of adverse events between active and sham stimulation groups (Risk Difference = 0.16, 95% CI −0.01–0.33). Reported adverse events were mild and transient, including tingling and redness under the electrodes for tDCS, and headache for rTMS. The study concluded that NIBS is safe and well-tolerated in pediatric populations [89].
Protocol: Cognitive and Functional Benefits of Invasive vs. Non-Invasive Sensory Feedback
Objective: To compare the cognitive benefits and performance of a non-invasive electro-cutaneous sensory feedback system against an invasive intraneural system in transfemoral amputees [92].
Methodology:
- Study Design: Comparative study in functionality-matched amputees.
- Participants: Two transfemoral amputees using a non-invasive (NI) system compared to two matched subjects using an invasive (I) intraneural system.
- Intervention:
- NI System: Delivered electro-cutaneous stimulation to the thigh, providing remapped feedback on touch and knee angle.
- I System: Used implanted electrodes in residual nerves to evoke somatotopic (natural) sensations in the phantom foot.
- Calibration: Measured the perceptual threshold, comfortable charge range, and Just Noticeable Difference (JND) for stimulus intensity.
- Cognitive Task: A dual motor and cognitive task was used to assess cognitive integration and load.
Key Performance Results:
- Stimulation Parameters: The charge required for perception was significantly higher for the NI system (1.107 ± 0.070 µC) compared to the I system (15.1 ± 3.1 nC). The NI system also had a significantly higher average Weber fraction, indicating poorer sensitivity to changes in stimulus intensity [92].
- Functional & Cognitive Outcomes: The non-invasive system induced similar improvements in dual-task performance as the invasive system, suggesting it can reduce cognitive load. However, it failed to improve prosthesis embodiment and was less performant in evoking intuitive, recognizable sensations [92].
Safety Evaluation Pathways for Neurotechnology
The following diagram outlines the key decision-making workflow for evaluating the safety and applicability of implantable versus non-invasive neurotechnologies, based on the risks and criteria discussed.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Analytical Tools for Neurotechnology Research
| Tool / Material | Function in Research | Safety & Efficacy Context |
|---|---|---|
| Multi-electrode Arrays (e.g., Utah Array) | Implanted for high-resolution recording of action potentials and local field potentials (LFPs) in animal and human studies [90]. | Enables high-fidelity data but carries risk of tissue damage and signal degradation over the long term [88] [90]. |
| Transcranial Direct Current Stimulation (tDCS) | Non-invasive technique to modulate cortical excitability using low-intensity electrical currents via scalp electrodes [89]. | Considered safe and well-tolerated; common adverse events are mild skin irritation and tingling [89]. |
| Repetitive Transcranial Magnetic Stimulation (rTMS) | Non-invasive method using magnetic fields to induce electrical currents in targeted cortical regions [89]. | A safe intervention with a low incidence of adverse events, such as headache; requires monitoring for rare risk of seizures [89]. |
| Electroencephalography (EEG) | Non-invasive recording of electrical activity from the scalp, representing aggregate post-synaptic currents [90]. | Risk-free in terms of surgery; primary limitation is lower spatial resolution and signal-to-noise ratio compared to invasive methods [90]. |
| Just Noticeable Difference (JND) Paradigms | Psychophysical method to quantify the minimal detectable change in a stimulus, such as electrical charge for sensory feedback [92]. | Critical for calibrating devices to be above perception threshold but below discomfort levels, directly impacting user safety and acceptability [92]. |
| Adverse Event Reporting Standardization | Systematic framework (e.g., risk difference calculations in meta-analyses) for collecting and reporting safety data across clinical trials [89]. | Allows for objective, pooled analysis of safety profiles and is essential for establishing the risk-benefit ratio of a technology [89]. |
The intersection of neurology and cardiology has unveiled patent foramen ovale (PFO) as a significant comorbidity in patients suffering from migraine, particularly migraine with aura. PFO, a remnant cardiac atrial communication present in approximately 25% of the adult population, has been implicated in allowing venous blood-borne microemboli or vasoactive substances to bypass pulmonary filtration and trigger cortical events like migraines [93] [94]. Consequently, percutaneous PFO closure has emerged as an invasive therapeutic strategy for medication-refractory migraine.
The core of this intervention lies in the occluder device deployed to seal the cardiac defect. Traditional nitinol (nickel-titanium alloy) metallic occluders (MOs), while effective, carry the lifelong risk of complications such as nickel allergy, device erosion, and thrombus formation [93] [95]. The next generation of biodegradable occluders (BOs) seeks to mitigate these long-term risks. Composed of materials like polydioxanone (PDO) and poly-L-lactic acid (PLLA), BOs provide a temporary scaffold that supports native tissue endothelialization before degrading into biologically benign byproducts, leaving no permanent implant [93] [95].
This guide provides a comparative evaluation of these material paradigms within the context of neurotechnology safety and efficacy research, synthesizing current clinical data, experimental methodologies, and material considerations for a scientific audience.
Performance Comparison: Efficacy and Safety Data
Recent clinical studies directly comparing biodegradable and metallic occluders demonstrate comparable short-term efficacy in migraine symptom relief, while highlighting distinct safety and prognostic profiles.
Table 1: Comparative Clinical Efficacy of Occluders in Migraine Relief
| Efficacy Metric | Biodegradable Occluder (BO) | Metallic Occluder (MO) | P-value |
|---|---|---|---|
| Post-op MIDAS Score (Mean ± SD) | 10.45 ± 9.19 | 11.32 ± 9.62 | 0.453 [93] [94] |
| Post-op Monthly Migraine Days (Mean ± SD) | 2.09 ± 1.58 days | 1.87 ± 1.43 days | 0.506 [93] [94] |
| Pre- vs. Post-op Improvement (MIDAS & Attack Days) | Statistically Significant (p<0.05) [93] [94] | Statistically Significant (p<0.05) [93] [94] | N/A |
| Primary Endpoint Definition | Complete elimination or ≥50% reduction in monthly migraine attack days [93] [94] | Same as BO [93] [94] | N/A |
Table 2: Comparative Safety and Prognostic Profile
| Characteristic | Biodegradable Occluder (BO) | Metallic Occluder (MO) |
|---|---|---|
| Material Composition | PDO skeleton & PLLA membranes [95] | Nickel-Titanium Alloy (Nitinol) [95] |
| Long-Term Presence | Fully degrades and is absorbed; no permanent implant [93] | Permanent implant [93] |
| Key Long-Term Risks | Theoretically lower risk of long-term erosion, allergy, and thrombosis [93] | Nickel allergy, device erosion, atrioventricular block, heart perforation [93] [95] |
| Perioperative Safety | No significant complications reported; limited mild adverse events [93] [94] | No significant complications reported; limited mild adverse events [93] [94] |
| Independent Predictors of Post-op Relief | Pre-op MIDAS, monthly attacks, RLS at rest, Platelet Crit (PCT) [93] [94] | Pre-op MIDAS, monthly attacks, RLS at rest, Platelet Crit (PCT), C-reactive Protein (CRP) [93] [94] |
Experimental Protocols and Methodologies
Robust evaluation of occluder materials relies on standardized clinical trial designs and diagnostic protocols. The following section details key methodologies cited in contemporary research.
Clinical Trial Design: The BioMetal Trial Protocol
The ongoing BioMetal trial (NCT06203873) is a prospective, multicenter, single-blind, randomized controlled superiority study designed to provide high-quality evidence comparing BO and MO [95].
- Objective: To compare the efficacy and safety of a BO (MemoSorb) versus a MO in patients with PFO and medication-refractory migraine with aura [95].
- Study Population: 400 participants, aged ≥18 and <65 years, will be enrolled across approximately 20 centers in China and randomized 1:1 to the BO or MO group [95].
- Key Inclusion Criteria:
- Diagnosis of migraine with aura per International Classification of Headache Disorders, 3rd edition (ICHD-3) criteria.
- ≥4 migraine days per month on average during a 3-month baseline.
- Refractory to at least three preventive medication categories.
- PFO with significant right-to-left shunt (RLS) (≥ grade 2 upon Valsalva) confirmed by transesophageal echocardiography (TEE) and contrast TEE (cTEE) [95].
- Primary Endpoint: Change in monthly migraine days at 12 months compared to baseline [95].
- Blinding: Single-blind design with blinded endpoint evaluation [95].
Diagnostic and Shunt Assessment Workflow
Pre-procedural identification of suitable candidates requires precise anatomical and functional assessment of the PFO and the associated shunt.
PFO and Shunt Assessment Workflow
Efficacy and Safety Endpoint Assessment
Post-procedural monitoring employs standardized tools to quantify therapeutic outcomes and adverse events.
- Efficacy Endpoints:
- Migraine Disability Assessment (MIDAS) Questionnaire: A 5-item questionnaire assessing headache-related disability over 3 months, scored as: 0-5 (little/no disability), 6-10 (mild), 11-20 (moderate), ≥21 (severe) [93] [94].
- Monthly Migraine Days (MMDs): The number of days with migraine headache per month, collected via patient headache diaries. Treatment response is defined as complete cessation or a ≥50% reduction in MMDs [93] [94] [95].
- Safety Endpoints:
Mechanisms and Material Science
The fundamental differences between occluder types stem from their material properties and biological interactions, which dictate long-term safety and biocompatibility.
Mechanisms of Action and Failure
Understanding how PFO closure alleviates migraine and how devices can potentially fail or cause adverse effects is critical for material evaluation.
Mechanisms of PFO Closure and Device-Specific Effects
The Scientist's Toolkit: Key Reagents and Materials
Table 3: Essential Research Reagents and Materials for PFO Occluder Studies
| Item | Function/Description | Example Use in Context |
|---|---|---|
| MemoSorb BO | A biodegradable PFO occluder made from a PDO skeleton and PLLA occluder membranes [95]. | The investigational device in the BioMetal trial; represents the biodegradable material class [95]. |
| AMPLATZER PFO Occluder | A widely studied and used nitinol (MO) device [95]. | The active comparator device in pivotal trials (PRIMA, PREMIUM) and the reference for metallic occluders [95]. |
| Transesophageal Echocardiogram (TEE) | An ultrasound probe inserted into the esophagus to obtain high-resolution images of the heart's structure, including the atrial septum [93] [95]. | Used to confirm the anatomical presence of a PFO and guide device placement [95]. |
| Contrast TEE (cTEE) | Agitated saline contrast injected during TEE to functionally assess and grade the severity of a right-to-left shunt [93] [95]. | Critical for patient selection; a shunt grade of ≥2 (10+ microbubbles) is a typical inclusion criterion [95]. |
| Migraine Disability Assessment (MIDAS) | A validated 5-item questionnaire for quantifying headache-related disability [93] [94]. | Primary tool for assessing the functional impact of migraine pre- and post-operatively in clinical studies [93]. |
The evolution of PFO occluders from permanent metallic implants to biodegradable scaffolds represents a significant advancement in neuro-interventional technology, aligning with the core principles of biocompatibility and long-term patient safety. Current evidence indicates that while biodegradable and metallic occluders demonstrate comparable efficacy in reducing migraine burden at one year, their risk profiles are distinctly different.
Metallic occluders carry established, albeit low, risks associated with lifelong nickel-titanium exposure. In contrast, biodegradable occluders offer a theoretically superior safety profile by eliminating permanent foreign material, but their long-term performance and degradation kinetics require further validation through rigorous, prospective trials like BioMetal.
For researchers and clinicians, the choice of material involves a nuanced trade-off. The optimal selection may be patient-specific, considering factors such as age, nickel allergy status, and biomarker levels (e.g., CRP). The ongoing research and development in this field, including the integration of shape-memory polymers (SMPs) and other advanced material technologies [96] [97], promise a future of increasingly sophisticated and patient-tailored neuro-vascular implants.
Leveraging Real-World Evidence and Post-Market Surveillance for Continuous Validation
The evaluation of neurotechnologies does not end with pre-market randomized controlled trials. Real-world evidence (RWE) and post-market surveillance (PMS) have become critical components for the continuous validation of safety and efficacy throughout a product's lifecycle. RWE is derived from the analysis of real-world data (RWD) collected outside of traditional clinical trials, including electronic health records, claims data, patient-generated data, and registry information [98]. For neurotechnology, this continuous validation approach is particularly vital due to the complex, evolving nature of neurological conditions and the personalized response to interventions.
The global RWE solutions market is projected to grow from USD 2.7 billion in 2024 to USD 4.5 billion by 2035, reflecting increased adoption across healthcare sectors [98]. This growth is especially relevant for neurotechnology, where post-market surveillance provides essential insights into long-term device performance, rare adverse events, and effectiveness across diverse patient populations that may not have been fully represented in initial clinical studies [99] [100].
Comparative Frameworks: RWE and PMS Approaches
Data Source Comparisons for Neurotechnology Evaluation
Table 1: Comparative Analysis of Real-World Data Sources for Neurotechnology Validation
| Data Source | Key Applications in Neurotechnology | Strengths | Limitations |
|---|---|---|---|
| Electronic Health Records (EHRs) | Patient population characterization, treatment patterns, comorbidities | Rich clinical detail, longitudinal data | Variable data quality, documentation inconsistencies |
| Claims Data | Healthcare utilization, economic outcomes, safety signals | Large populations, standardized coding | Limited clinical granularity, coding inaccuracies |
| Disease Registries | Natural history studies, long-term outcomes in specific conditions | Disease-specific data collection, curated variables | Potential selection bias, limited generalizability |
| Patient-Generated Data (Wearables, Apps) | Functional status, quality of life, daily symptom tracking | High-frequency data, patient perspective | Validation challenges, data standardization issues |
| Medical Device Reports (e.g., MAUDE) | Safety signal detection, device performance issues | Mandatory reporting, large volume | Passive surveillance, underreporting, incomplete data |
Methodological Approaches for Evidence Generation
Table 2: Methodological Frameworks for RWE Generation in Neurotechnology
| Methodological Approach | Primary Use Cases | Regulatory Acceptance | Key Considerations |
|---|---|---|---|
| Prospective Observational Studies | Natural disease progression, treatment patterns | Moderate-High | Protocol registration, pre-specified analysis plans |
| Registry-Based Studies | Long-term safety, comparative effectiveness | Moderate-High | Data quality assurance, representative sampling |
| Pragmatic Clinical Trials | Effectiveness in routine care, implementation research | High | Balance between internal validity and generalizability |
| Active Surveillance Programs | Safety signal detection, risk minimization | Moderate | Systematic data collection, automated signal detection |
| Electronic Phenotyping | Patient identification, cohort creation | Moderate | Algorithm validation, accuracy assessment |
Experimental Data and Case Studies
Case Study: Post-Market Surveillance of Prescription Digital Therapeutics
A recent pharmacovigilance study of the FDA's MAUDE database through April 2025 identified only two adverse event reports associated with 13 FDA-cleared prescription digital therapeutics (PDTs), highlighting both the potential safety profile of these interventions and the limitations of passive surveillance systems [100].
Experimental Protocol: MAUDE Database Analysis
- Data Source: FDA's Manufacturer and User Facility Device Experience (MAUDE) database
- Search Period: Through April 30, 2025
- Identification Method: Device-specific product codes for 13 FDA-cleared PDTs
- Screening Process: Manual review for relevance and data extraction
- Data Extraction Elements: Device name, product code, event type, patient demographics, outcomes, narrative description
- Inclusion Criteria: Reports involving cleared, prescription-only PDTs authorized by FDA
- Exclusion Criteria: Over-the-counter, investigational, or non-prescription software products
Results Interpretation: The two identified reports included one injury (Somryst PDT used in a patient with contraindicated seizure disorder) and one malfunction (EndeavorRx perceived ineffectiveness). The limited number of reports must be interpreted cautiously given known underreporting in passive surveillance systems [100].
Case Study: Robotic-Assisted Neurorehabilitation
A 2025 feasibility study evaluated a robotic-assisted hand rehabilitation exercise (RAHRE) program for adults with hand hemiparesis following recent stroke, demonstrating the application of real-world evidence generation in neurorehabilitation [61].
Experimental Protocol: RAHRE Feasibility Study
- Study Design: Prospective intervention feasibility study with pre- and post-evaluations
- Participants: 11 adults with hand hemiparesis post-stroke undergoing intensive neurorehabilitation
- Intervention: 10 additional 30-minute sessions of RAHRE program over 2 weeks alongside conventional rehabilitation
- Technology: Dexmo soft robotic glove coupled with btrained virtual environment software
- Primary Outcomes: Feasibility (attendance, compliance, repetitions), safety (discomfort, adverse effects)
- Functional Assessments: Action Research Arm Test (ARAT), Fugl-Meyer Assessment for Upper Extremity (FMA-UE), Box and Block Test, ABILHAND
- Analysis: Generalized linear mixed models for repeated measures
Key Findings: The experimental group achieved 96% attendance rate with median 2543 additional movement repetitions and no adverse effects, supporting the feasibility and safety of technology-enhanced neurorehabilitation [61].
Signaling Pathways and Workflow Diagrams
RWE and PMS Workflow for Neurotechnology Validation
Table 3: Essential Research Reagent Solutions for Neurotechnology RWE Studies
| Tool Category | Specific Solutions | Research Application |
|---|---|---|
| RWE Analytics Platforms | AETION Evidence Platform, IQVIA RWE Solutions, Flatiron Health Platform | Analyze longitudinal RWD to generate evidence on safety, effectiveness, and value of neurotechnologies |
| Data Integration Tools | OMOP Common Data Model, Sentinel Initiative System, DARWIN EU | Harmonize disparate data sources to create standardized datasets for analysis |
| Statistical Software | SAS, R, Python | Perform advanced statistical analyses including propensity score matching, marginal structural models |
| Terminology Standards | MedDRA, SNOMED CT, ICD-10 | Standardize coding of adverse events, medical conditions, and procedures |
| Signal Detection Tools | WHO Uppsala Monitoring Centre system, FDA Sentinel Signal Management | Identify potential safety signals from large-scale healthcare data |
| Patient-Reported Outcome Measures | Neuro-QoL, PROMIS, disease-specific instruments | Capture patient perspectives on treatment benefits and harms |
Implementation Framework and Future Directions
The integration of artificial intelligence and machine learning is revolutionizing RWE analytics, enabling the extraction of deeper insights from complex neurological datasets [98]. Predictive models can identify patient subgroups that respond differentially to neurotechnologies, while natural language processing facilitates the extraction of unstructured clinical information from EHRs. These technological advances are particularly relevant for neurotechnologies, where treatment effects may be modulated by individual patient characteristics, disease subtypes, and technical device factors.
The future of neurotechnology validation will be shaped by emerging regulatory frameworks that formally incorporate RWE into decision-making processes. Between 2020 and 2024, the proportion of FDA approvals containing RWE increased from approximately 5-10% to nearly 50% [98]. This trend is complemented by initiatives such as the European Medicines Agency's DARWIN EU, which provides coordinated access to healthcare data across member states. For researchers and developers, these developments underscore the importance of designing comprehensive evidence generation strategies that integrate pre-market clinical data with robust post-market surveillance and real-world effectiveness studies.
Conclusion
The safe and effective development of neurotechnology demands a multifaceted and adaptive approach that integrates robust foundational science, innovative and regulated testing methodologies, proactive troubleshooting, and rigorous comparative validation. The emergence of new frameworks, such as regulatory sandboxes and international 'neuro-rights,' highlights the dynamic nature of the field. Future directions must prioritize the creation of independent evaluation bodies to guide public and professional understanding, the development of standardized, transparent validation protocols, and a continued ethical focus on cognitive liberty and mental privacy. For biomedical and clinical research, this means embracing collaborative models that accelerate the translation of reliable, patient-centered neurotechnologies from the laboratory to the clinic, ultimately improving outcomes for individuals with neurological disorders.
References
- 1. BCIs in 2025: Trials, Progress, and Challenges [https://andersenlab.com/blueprint/bci-challenges-and-opportunities]
- 2. Modulating Brain Activity with Invasive Brain–Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856340/]
- 3. 1.3 Types of BCIs: invasive, semi-invasive, and non-invasive [https://fiveable.me/brain-computer-interfaces/unit-1/types-bcis-invasive-semi-invasive-non-invasive/study-guide/Wz8G1AecOttsxslK]
- 4. Efficacy and safety of brain–computer interface for stroke ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11922947/]
- 5. Progress in the combined application of Brain-Computer ... [https://www.sciencedirect.com/science/article/abs/pii/S1388245725012350]
- 6. A new era of brain-computer interfaces: Restored touch ... [https://www.eurekalert.org/news-releases/1106526]
- 7. A New Path to Noninvasive Brain-Computer Interface [https://www.jhuapl.edu/news/news-releases/241114-noninvasive-brain-computer-interface]
- 8. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/en/research-report/brain-computer-interfaces/1024]
- 9. Development and evaluation of a non-invasive brain-spine ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-025-01628-6]
- 10. BRAIN 2025: A Scientific Vision - BRAIN Initiative - NIH [http://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 11. A Horizon Scan of Neurotechnology Innovations - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12110900/]
- 12. The grand challenge at the frontiers of neurotechnology ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10827995/]
- 13. Ethical gaps in closed-loop neurotechnology: a scoping ... [https://www.nature.com/articles/s41746-025-01908-4]
- 14. Comparison of safety and efficacy of different endovascular ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1539127/full]
- 15. New Novartis Phase III data demonstrate meaningful ... [https://www.novartis.com/news/media-releases/new-novartis-phase-iii-data-demonstrate-meaningful-efficacy-and-safety-results-intrathecal-onasemnogene-abeparvovec-broad-patient-population-sma]
- 16. Five-Year Safety and Efficacy Outcomes with Ofatumumab ... [https://pubmed.ncbi.nlm.nih.gov/40652442/]
- 17. Mental privacy: navigating risks, rights and regulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC12287510/]
- 18. US FDA vs EU MDR: Device Classification Differences [https://cmcmedicaldevices.com/us-fda-vs-eu-mdr-key-differences-in-medical-device-classification/]
- 19. EU MDR vs FDA: what are the main differences and ... [https://spyro-soft.com/blog/healthcare/eu-mdr-vs-fda-what-are-the-main-differences-and-similarities]
- 20. UN expert calls for model law on neurotechnologies to ... [https://www.ohchr.org/en/press-releases/2025/10/un-expert-calls-model-law-neurotechnologies-protect-right-privacy]
- 21. FDA vs. EU-MDR: Key Differences in Medical Device ... [https://mdsdenmark.dk/fda-vs-eu-mdr-key-differences-in-medical-device-regulations/]
- 22. U.S. Senators Propose "MIND Act" to Study and ... [https://www.dwt.com/blogs/privacy--security-law-blog/2025/10/senate-mind-act-neural-data-ftc-regulation]
- 23. Neural Data Privacy Regulation: What Laws Exist and ... [https://www.arnoldporter.com/en/perspectives/advisories/2025/07/neural-data-privacy-regulation]
- 24. Safety and Efficacy Evaluation of Electrical Stimulation ... [https://www.frontiersin.org/research-topics/25537/safety-and-efficacy-evaluation-of-electrical-stimulation-devices-for-neural-modulation/magazine?trk]
- 25. Efficacy and safety of a new mechanical balloon-based ... [https://pubmed.ncbi.nlm.nih.gov/40425281/]
- 26. Top 5 Upcoming FDA and EU Regulations - MEDIcept [https://www.medicept.com/top-5-upcoming-fda-and-eu-regulations-what-to-know-for-2025/]
- 27. Why Sandboxes Matter in Implantable Neurotechnology [https://bioengineer.org/why-sandboxes-matter-in-implantable-neurotechnology/]
- 28. Ethical gaps in closed-loop neurotechnology: a scoping review [https://pmc.ncbi.nlm.nih.gov/articles/PMC12334599/]
- 29. A Discussion of Safety in Medical Neurotechnology [https://medium.com/neurotechx/a-discussion-of-safety-in-medical-neurotechnology-38a9fb6222b4]
- 30. The Potential Harms of Speculative Neuroethics Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC10593500/]
- 31. Oversight of direct-to-consumer neurotechnologies [https://pmc.ncbi.nlm.nih.gov/articles/PMC6629579/]
- 32. Mind the Gap: Regulating Neurotechnologies in ... [https://petrieflom.law.harvard.edu/2025/05/27/mind-the-gap-regulating-neurotechnologies-in-the-consumer-age/]
- 33. Neurotechnology Market Size, Share & Industry Forecast ... [https://www.mordorintelligence.com/industry-reports/neurotechnology-market]
- 34. Assessing current mechanisms for the regulation of direct- ... [https://www.sciencedirect.com/science/article/abs/pii/S2589295920300199]
- 35. Safety and Efficacy Evaluation of Electrical Stimulation ... [https://www.frontiersin.org/research-topics/25537/safety-and-efficacy-evaluation-of-electrical-stimulation-devices-for-neural-modulation/magazine]
- 36. A phase 2 randomized, placebo-controlled study on the ... [https://pubmed.ncbi.nlm.nih.gov/40912996/]
- 37. In Silico Research Is Rewriting the Rules of Drug Development [https://pmc.ncbi.nlm.nih.gov/articles/PMC12070237/]
- 38. Pros And Cons Of In Silico Target-Drug Dynamics [https://www.drugdiscoveryonline.com/doc/pros-and-cons-of-in-silico-target-drug-dynamics-0001]
- 39. In Vitro vs In Vivo: A History of Modern Cell Culture [https://emulatebio.com/in-vitro-vs-in-vivo-cell-culture/]
- 40. a comprehensive review of in vitro and in vivo experimental ... [https://pubmed.ncbi.nlm.nih.gov/40632186/]
- 41. Better models, better treatment? a systematic review of ... [https://www.frontiersin.org/journals/bioengineering-and-biotechnology/articles/10.3389/fbioe.2025.1569211/full]
- 42. Making the case for sandboxes in implantable ... [https://www.nature.com/articles/s41467-025-65584-4]
- 43. Medical Device Validation & Verification 2025-2033 Trends [https://www.archivemarketresearch.com/reports/medical-device-validation-verification-783269]
- 44. Neural vs Neuromorphic Interfaces: Where Are We Standing? [https://pmc.ncbi.nlm.nih.gov/articles/PMC12512108/]
- 45. Cardiac implantable electronic devices' longevity [https://pmc.ncbi.nlm.nih.gov/articles/PMC12478916/]
- 46. A Horizon Scan of Neurotechnology Innovations [https://www.mdpi.com/1660-4601/22/5/811]
- 47. Smarter Trial Designs for Rare Neurological Disease Trials [https://tfscro.com/resources/rare-neurological-disease-trials-smarter-design-with-natural-history-external-controls-and-real-world-evidence/]
- 48. Trends in Efficacy Endpoints in Phase II Glioblastoma Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC11898451/]
- 49. Trends in Efficacy Endpoints in Phase II Glioblastoma Trials [https://www.preprints.org/manuscript/202501.1164/v1]
- 50. The future of neurotechnology: From big data to translation [https://www.sciencedirect.com/science/article/abs/pii/S0896627325001370]
- 51. Most prominent challenges in translational neuroscience ... [https://www.explorationpub.com/Journals/en/Article/1006106]
- 52. Clinical Translation - About Stem Cells [https://www.aboutstemcells.org/info/clinical-translation]
- 53. Translating Research into Practical Applications - NCBI - NIH [https://www.ncbi.nlm.nih.gov/books/NBK233565/]
- 54. Top 6 Visualizations for Quantitative Data Analysis Methods [https://chartexpo.com/blog/quantitative-data-analysis-methods]
- 55. Visualizing Quantitative Data: Best Experience [https://powerdrill.ai/blog/visualizing-quantitative-data-best-experience]
- 56. Brain-Computer Interfaces: Exploring the Last Frontier [https://www.byfounders.vc/insights/brain-computer-interfaces]
- 57. Brain computer interface is growing but what are the risks? [https://www.weforum.org/stories/2024/06/the-brain-computer-interface-market-is-growing-but-what-are-the-risks/]
- 58. Invasive BCIs: What's At Stake If Your Brain Gets Hacked? [https://aicompetence.org/invasive-bcis-what-if-brain-gets-hacked/]
- 59. Neurotech consumer market atlas - How the sector is ... [https://cfg.eu/neurotech-market-atlas/]
- 60. A Moratorium on Implantable Non-Medical Neurotech Until ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12521269/]
- 61. Poststroke Neurorehabilitation Using a Soft Robotic Glove ... [https://neuro.jmir.org/2025/1/e69750]
- 62. Neurotechnologies: The Next Technology Frontier [https://brain.ieee.org/topics/neurotechnologies-the-next-technology-frontier/]
- 63. 2025 IEEE Brain Discovery & Neurotechnology Workshop [https://brain.ieee.org/2025-ieee-brain-discovery-neurotechnology-workshop/]
- 64. Blueprint Neurotech [https://blueprintneurotech.org/]
- 65. Electrical Stimulation Devices Global Market Report 2025 [https://www.thebusinessresearchcompany.com/report/electrical-stimulation-devices-global-market-report]
- 66. Comparison of the effects of neuromuscular electrical ... [https://pubmed.ncbi.nlm.nih.gov/40826799/]
- 67. Optimal control-driven functional electrical stimulation [https://www.sciencedirect.com/science/article/pii/S0010482525016658]
- 68. a protocol for systematic review and network meta-analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11987110/]
- 69. Optimizing electrical stimulation parameters to enhance ... [https://www.nature.com/articles/s41598-025-08657-0]
- 70. Safety and efficacy of belt-type electrical stimulation for ... [https://www.frontiersin.org/journals/rehabilitation-sciences/articles/10.3389/fresc.2025.1559077/full]
- 71. Clinical Trial Digital Patient Recruitment: Top 5 for 2025 [https://lifebit.ai/blog/clinical-trial-digital-patient-recruitment/]
- 72. Top 10 Clinical Trial Recruitment Strategies for 2025 - Patiro [https://www.patiro.com/insights/top-10-clinical-trial-recruitment-strategies-for-2025]
- 73. Top Patient Recruitment Companies Transforming Clinical ... [https://www.lindushealth.com/blog/top-patient-recruitment-companies-transforming-clinical-trials-in-2025]
- 74. The New Playbook for Clinical Trial Patient Recruitment [https://www.openclinica.com/blog/the-new-playbook-for-clinical-trial-patient-recruitment/]
- 75. Multiple Comparisons Procedures for Analyses of Joint ... [https://pubmed.ncbi.nlm.nih.gov/40140702/]
- 76. A Study to Evaluate the Efficacy and Safety of ENX-102 in ... [https://www.centerwatch.com/clinical-trials/listings/NCT07193563/a-study-to-evaluate-the-efficacy-and-safety-of-enx-102-in-participants-with-social-anxiety-disorder]
- 77. FDA Closing the Clinical Trial Reporting Gap for Research ... [https://www.fda.gov/news-events/fda-voices/fda-focuses-closing-clinical-trial-reporting-gap-research-integrity]
- 78. Clinical Research in 2025: Key Shifts, Challenges, and ... [https://blog.cloudbyz.com/resources/clinical-research-in-2025-key-shifts-challenges-and-whats-next]
- 79. Why Companies Shouldn't Delay Software Updates—Even ... [https://www.library.hbs.edu/working-knowledge/why-companies-shouldnt-delay-software-updates-even-after-crowdstrikes-flaw]
- 80. Outdated Software: The Cybersecurity Time Bomb ... [https://www.baytechconsulting.com/blog/outdated-software-the-cybersecurity-time-bomb-organizations-ignore]
- 81. Software Patching Statistics: Common Practices [https://heimdalsecurity.com/blog/software-patching-statistics-practices-vulnerabilities/]
- 82. The efficacy and safety of third-generation antiseizure ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1307296/full]
- 83. The efficacy and safety of third-generation antiseizure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10804851/]
- 84. Clinical Practice Guidelines for the Administration of Third ... [https://www.sciencedirect.com/science/article/abs/pii/S1059131125002961]
- 85. Neurosurgical Team Acceptability of Brain–Computer Interfaces [https://pmc.ncbi.nlm.nih.gov/articles/PMC10444691/]
- 86. A Comprehensive Survey of Brain–Computer Interface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180781/]
- 87. The simulation and experimental validation of a novel ... [https://www.nature.com/articles/s41598-024-61571-9]
- 88. Neuralink's brain-computer interfaces: medical innovations ... [https://www.frontiersin.org/journals/human-dynamics/articles/10.3389/fhumd.2025.1553905/full]
- 89. Safety and effectiveness of non-invasive brain stimulation on ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12087172/]
- 90. Invasive vs. Non-Invasive Neuronal Signals for Brain-Machine ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4921501/]
- 91. The MIND Act: Balancing Innovation and Privacy in ... [https://www.cooley.com/news/insight/2025/2025-09-25-the-mind-act-balancing-innovation-and-privacy-in-neurotechnology]
- 92. Cognitive benefits of using non-invasive compared to ... [https://www.nature.com/articles/s41598-022-21057-y]
- 93. The safety, efficacy, and influencing factors of ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1677536/full]
- 94. The safety, efficacy, and influencing factors of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12541255/]
- 95. study design and rationale of BioMetal Trial - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344936/]
- 96. Recent advances in shape memory polymers for ... [https://www.sciencedirect.com/science/article/pii/S259018342500016X]
- 97. Percutaneous delivery and degradation of a shape ... [https://www.sciencedirect.com/science/article/abs/pii/S0142961222005907]
- 98. World's Top 50 Real-World Evidence Solutions Market ... [https://www.sphericalinsights.com/blogs/world-s-top-50-real-world-evidence-solutions-market-companies-2025-industry-intelligence-report-by-spherical-insights-2024-2035]
- 99. Real World Evidence Solutions Research and Forecast ... [https://finance.yahoo.com/news/real-world-evidence-solutions-research-140000088.html]
- 100. Postmarket Safety Surveillance of FDA-Cleared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12136109/]