Ensuring Reliability in Brain Imaging: From Scanner to Statistical Analysis
This article provides a comprehensive framework for assessing the reliability of brain imaging methodologies, crucial for researchers and drug development professionals.
Ensuring Reliability in Brain Imaging: From Scanner to Statistical Analysis
Abstract
This article provides a comprehensive framework for assessing the reliability of brain imaging methodologies, crucial for researchers and drug development professionals. It explores foundational concepts of reliability and reproducibility in neuroimaging, examines both traditional and deep learning-based analytical methods, identifies key sources of error with optimization strategies, and presents comparative validation approaches for different tools and sequences. By synthesizing current evidence and best practices, this review aims to enhance the rigor and reproducibility of structural MRI analyses in both research and clinical trial contexts.
Understanding Brain Imaging Reliability: Core Concepts and Reproducibility Challenges
In the field of quantitative brain imaging, the derivation of robust and reproducible biomarkers is paramount for both research and clinical applications, such as tracking neurodegenerative disease progression or assessing treatment efficacy. The reliability of these measurements, whether obtained from magnetic resonance imaging (MRI) or other automated segmentation software, is fundamentally assessed through specific statistical metrics. This guide provides an objective comparison of two predominant reliability metrics—the Intraclass Correlation Coefficient (ICC) and the Coefficient of Variation (CV)—framed within the context of brain imaging reliability assessment. Furthermore, it explores the concept of significant bits in the context of image standardization, which bridges the gap between metric evaluation and technical implementation. Supporting experimental data from published studies are synthesized to illustrate their application and performance.
Conceptual Foundations and Mathematical Definitions
Intraclass Correlation Coefficient (ICC)
The ICC is a measure of reliability that describes how strongly units in the same group resemble each other. In the context of reliability analysis, it is used to assess the consistency or reproducibility of quantitative measurements made by different observers or devices measuring the same quantity [1].
In a random effects model framework, the ICC is defined as the ratio of the between-subject variance to the total variance. The one-way random effects model is often expressed as: ( Y{ij} = \mu + \alphaj + \epsilon{ij} ) where ( Y{ij} ) is the i-th observation in the j-th subject, ( \mu ) is the overall mean, ( \alphaj ) are the random subject effects with variance ( \sigma{\alpha}^2 ), and ( \epsilon{ij} ) are the error terms with variance ( \sigma{\epsilon}^2 ). The population ICC is then [1]: ( \text{ICC} = \frac{\sigma{\alpha}^2}{\sigma{\alpha}^2 + \sigma_{\epsilon}^2} )
A critical consideration is that several forms of ICC exist. Shrout and Fleiss, for example, described multiple ICC forms applicable to different experimental designs [2]. The selection of the appropriate ICC form (e.g., based on "model," "type," and "definition") must be guided by the research design, specifically whether the same or different raters assess all subjects, and whether absolute agreement or consistency is of interest [3]. Koo and Li (2016) provide a widely cited guideline suggesting that ICC values less than 0.5 indicate poor reliability, values between 0.5 and 0.75 indicate moderate reliability, values between 0.75 and 0.9 indicate good reliability, and values greater than 0.90 indicate excellent reliability [3].
Coefficient of Variation (CV)
The Coefficient of Variation (CV) is a standardized measure of dispersion, defined as the ratio of the standard deviation ( \sigma ) to the mean ( \mu ), often expressed as a percentage [4]: ( \text{CV} = \frac{\sigma}{\mu} \times 100\% )
In reliability assessment, particularly for laboratory assays or measurement devices, the within-subject coefficient of variation (WSCV) is often more appropriate than the typical CV. The WSCV is defined as ( \theta = \sigmae / \mu ), where ( \sigmae ) is the within-subject standard deviation. This metric specifically determines the degree of closeness of repeated measurements taken on the same subject under the same conditions [5]. A key advantage of the CV is that it is a dimensionless number, allowing for comparison between data sets with different units or widely different means [4]. However, a notable disadvantage is that when the mean value is close to zero, the coefficient of variation can approach infinity and become highly sensitive to small changes in the mean [4].
Relationship to Significant Bits and Image Standardization
While "significant bits" is not a standard statistical metric like ICC or CV, the concept relates directly to image pre-processing and standardization, which underpins the reliability of any subsequent quantitative feature extraction. In MRI-based radiomics, the lack of standardized intensity values across machines and protocols is a major challenge [6]. The process of grey-level discretization, which clusters similar intensity levels into a fixed number of bins (bits), is a critical pre-processing step that influences the stability of second-order texture features [6]. Using a fixed bin number (e.g., 32 bins) is a form of relative discretization that helps manage the bit depth of the analyzed data, thereby contributing to more reliable and reproducible radiomics features by reducing the impact of noise and non-biological intensity variations.
Comparative Analysis of Reliability Metrics
Table 1: Comparison of Reliability Metrics in Brain Imaging
| Metric | Primary Use Case | Interpretation Range | Key Strengths | Key Limitations |
|---|---|---|---|---|
| ICC | Assessing reliability/agreement between raters or devices. | 0 to 1 (or -1 to 1 for some forms). Values >0.9 indicate excellent reliability [3]. | Accounts for both within- and between-subject variance; can handle multiple raters [1]. | Multiple forms exist, requiring careful selection [3]; can be influenced by population heterogeneity [5]. |
| CV / WSCV | Quantifying reproducibility of a single instrument or within-subject variability. | 0% to infinity. Smaller values indicate better reproducibility [5]. | Dimensionless, allows comparison across different measures [4]; intuitive interpretation. | Sensitive to small mean values [4]; does not directly assess agreement between raters. |
The choice between ICC and WSCV depends on the specific research question. The ICC is particularly useful when the goal is to differentiate among subjects, as a larger heterogeneity among subjects (with a constant or smaller random error) increases the ICC [5]. In contrast, the WSCV is a pure measure of reproducibility, determining the degree of closeness of repeated measurements on the same subject, irrespective of between-subject variation [5]. This makes the WSCV particularly valuable for assessing the intrinsic performance of a measurement device.
Experimental Protocols for Reliability Assessment
Test-Retest Dataset Acquisition for Brain MRI
A foundational step for assessing the reliability of brain imaging metrics is the creation of a robust test-retest dataset. A standard protocol involves acquiring multiple scans from the same subjects across different sessions.
Methodology from a Publicly Available Dataset [7]:
- Subjects: 3 healthy subjects.
- Scanning Sessions: 20 sessions per subject over 31 days.
- Scans per Session: 2 T1-weighted scans per session, with subject repositioning between scans.
- Scanner and Protocol: 3T GE MR750 scanner using the Alzheimer's Disease Neuroimaging Initiative (ADNI) T1-weighted imaging protocol (accelerated sagittal 3D IR-SPGR).
- Data Processing: All 120 3D volumes were processed using FreeSurfer (v5.1) to obtain volumetric data for structures like the lateral ventricles, hippocampus, and amygdala.
This design allows for the separate calculation of intra-session (within the same day) and inter-session (between days) reliability, capturing variability from repositioning, noise, and potential day-to-day biological changes.
Protocol for Comparing Dependent Reliability Coefficients
When comparing the reproducibility of two different measurement devices or platforms used on the same set of subjects, the reliability coefficients (like the WSCV) are dependent. A specialized statistical approach is required for this comparison.
Methodology for Comparing Two Dependent WSCVs [5]:
- Model: A one-way random effects model is fitted for each instrument: ( x{ijl} = \mul + bi + e{ijl} ), where ( x{ijl} ) is the j-th measurement on the i-th subject by the l-th instrument, ( \mul ) is the mean for instrument ( l ), ( bi ) is the random subject effect, and ( e{ijl} ) is the random error.
- Parameter of Interest: The within-subject coefficient of variation for each instrument is ( \thetal = \sigmal / \mu_l ).
- Statistical Tests: The hypothesis of equality of two dependent WSCVs (( H0: \theta1 = \theta_2 )) can be tested using several methods:
This methodology was applied, for instance, to compare the reproducibility of gene expression measurements from Affymetrix and Amersham microarray platforms [5].
Standardization Pipeline for MRI-Based Radiomics
To ensure the reliability of radiomics features in brain MRI, a standardized pre-processing pipeline is critical to mitigate the impact of different scanners and protocols.
Methodology from a Multi-Scanner Radiomics Study [6]:
- Datasets: Two independent datasets, one including 20 patients with gliomas scanned on two different MR devices (1.5T and 3.0T).
- Pre-processing Steps:
- Intensity Normalization: Three methods were evaluated (Nyul, WhiteStripe, Z-Score). The Z-Score method (subtracting the mean and dividing by the standard deviation of the image or ROI) was recommended for first-order features.
- Grey-Level Discretization: Two methods were evaluated (Fixed Bin Size, Fixed Bin Number). A Fixed Bin Number of 32 was recommended as a good compromise.
- Reliability Assessment: The robustness of first-order and second-order (textural) features across the two acquisitions was analyzed using the ICC and the Concordance Correlation Coefficient (CCC). A feature was considered robust if both ICC and CCC were greater than 0.80.
Table 2: Key Materials and Reagents for Reliability Experiments in Brain MRI
| Item Name | Function / Description | Example in Protocol |
|---|---|---|
| 3T MRI Scanner | High-field magnetic resonance imaging for structural brain data. | GE MR750 3T scanner [7]; Siemens MAGNETOM Trio [8]. |
| ADNI Phantom | Quality assurance phantom for scanner calibration and stability. | Used for regular quality assurance tests [7]. |
| T1-Weighted MPRAGE Sequence | High-resolution 3D structural imaging sequence. | ADNI-recommended protocol [7]; Slight parameter variations in multi-session studies [8]. |
| Automated Segmentation Software | Software for automated quantification of brain structure volumes. | FreeSurfer (v5.1) [7]. |
| Intensity Normalization Algorithm | Algorithm to standardize MRI intensities across different scans. | Z-Score, Nyul, WhiteStripe methods [6]. |
Experimental Data and Performance Comparison
Test-Retest Reliability of Brain Volume Measurements
Application of the test-retest protocol on 3 subjects (40 scans each) yielded the following coefficients of variation for various brain structures, demonstrating the range of reproducibility achievable with automated segmentation software [7]:
Table 3: Test-Retest Reliability of Brain Volume Measurements using FreeSurfer [7]
| Brain Structure | Coefficient of Variation (CV) - Pooled Average |
|---|---|
| Caudate | 1.6% |
| Putamen | 2.3% |
| Amygdala | 3.0% |
| Hippocampus | 3.3% |
| Pallidum | 3.6% |
| Lateral Ventricles | 5.0% |
| Thalamus | 6.1% |
The study also found that inter-session variability (CVt) significantly exceeded intra-session variability (CVs) for lateral ventricle volume (P<0.0001), indicating the presence of day-to-day biological variations in this structure [7].
Impact of Standardization on Feature Reliability
The radiomics standardization study provided quantitative data on how pre-processing impacts the robustness of imaging features [6]:
- First-Order Features: Without intensity normalization, no first-order features were robust (ICC/CCC > 0.8) across T1w-gd and T2w-flair sequences. After applying the Nyul normalization method, 16 out of 18 first-order features became robust for the T1w-gd sequence, and 8 out of 18 for the T2w-flair sequence.
- Classification Performance: For a tumour grade classification task using first-order features from T1w-gd images, intensity normalization significantly increased the mean balanced accuracy from 0.67 (no normalization) to 0.82 (using Z-Score or Nyul normalization).
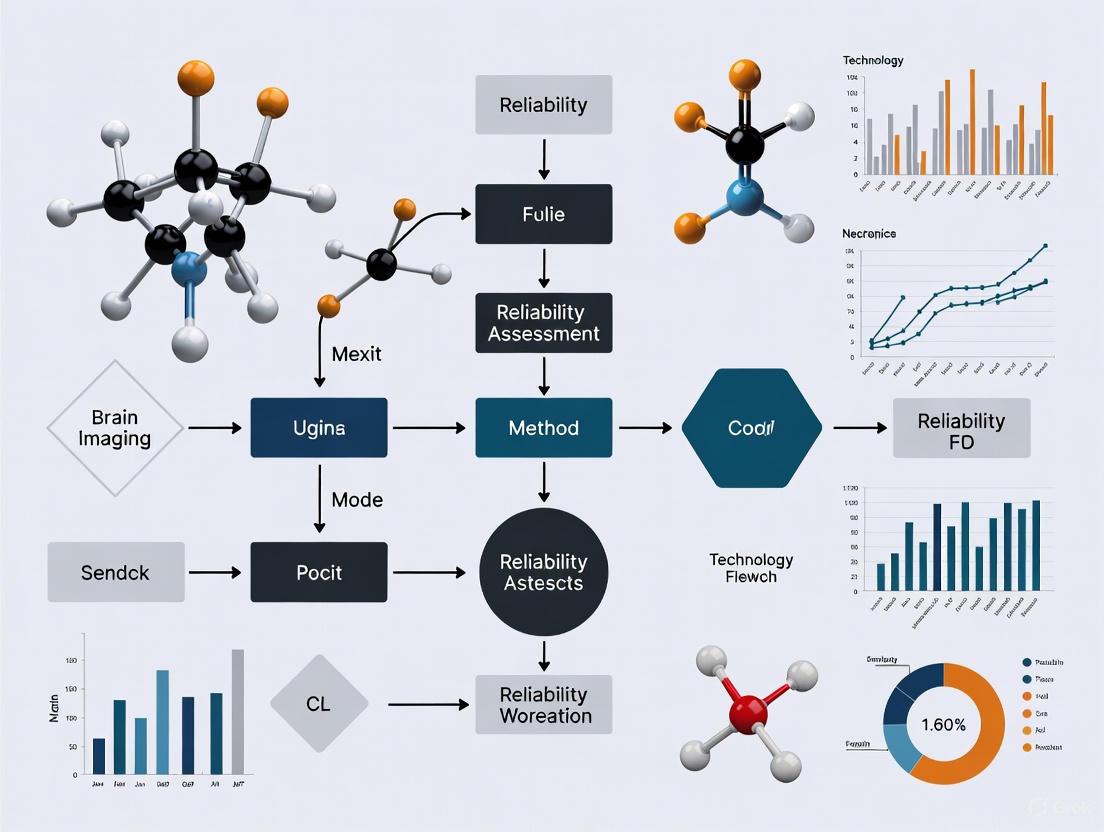
Workflow for Reliability Assessment
The following diagram illustrates the logical workflow for assessing the reliability of a brain imaging measurement, integrating the concepts of experimental design, metric selection, and standardization.
Diagram 1: Workflow for Assessing Reliability of Brain Imaging Measurements
The objective comparison of ICC and Coefficient of Variation reveals distinct and complementary roles for these metrics in brain imaging reliability assessment. The ICC is the measure of choice for evaluating agreement between different raters or scanners, while the WSCV is superior for quantifying the intrinsic reproducibility of a single measurement device. Experimental data from test-retest studies show that even with automated segmentation, the reliability of volumetric measurements varies substantially across different brain structures. Furthermore, the critical role of image standardization—conceptually related to managing significant bits through discretization—has been quantitatively demonstrated to significantly improve the robustness of derived image features. A rigorous approach to reliability assessment, incorporating appropriate experimental design, metric selection, and standardization protocols, is therefore foundational for generating trustworthy quantitative biomarkers in brain imaging research and drug development.
In the pursuit of establishing functional magnetic resonance imaging (fMRI) as a reliable tool for clinical applications and longitudinal research, understanding and quantifying sources of variance is paramount. The reliability of fMRI measurements is fundamentally challenged by multiple factors that can be broadly categorized as scanner-related, session-related, and biological. These sources of variance collectively influence the reproducibility of findings and the ability to detect genuine neurological effects amid technical noise. This guide systematically compares how these factors impact fMRI reliability, supported by experimental data and methodologies from contemporary research. The broader thesis context emphasizes that without properly accounting for these variance components, the development of fMRI-based biomarkers for drug development and clinical diagnostics remains substantially hindered.
Quantifying Reliability in fMRI Research
Key Reliability Metrics
In fMRI research, reliability is quantified using several statistical metrics, each with distinct interpretations and applications. The most commonly used include:
- Intraclass Correlation Coefficient (ICC): This metric reflects the strength of agreement between repeated measurements and is essential for assessing between-person differences. ICC values range from 0 (no reliability) to 1 (perfect reliability), with values below 0.4 considered poor, 0.4-0.59 fair, 0.60-0.74 good, and above 0.75 excellent [9]. ICC is particularly valuable in psychometrics for gauging individual differentiation.
- Coefficient of Variation (CV): Representing the ratio of variability to the mean measurement, CV expresses measurement precision normalized to the scale metric. In physics-oriented applications, lower CV values indicate greater precision in detecting a specific quantity [10].
- Overlap Metrics (Dice/Jaccard): These measure the spatial similarity of activation maps between sessions, reflecting reproducibility of spatial patterns in thresholded statistical maps [11].
These metrics offer complementary insights—ICC is preferred for individual differences research, while CV better reflects measurement precision in technical validation.
Advanced Reliability Assessment Frameworks
The Intra-Class Effect Decomposition (ICED) framework extends traditional reliability analysis by using structural equation modeling to decompose reliability into orthogonal error sources associated with different measurement characteristics (e.g., session, day, scanner) [10]. This approach enables researchers to quantify specific variance components, make inferences about error sources, and optimize future study designs. ICED is particularly valuable for complex longitudinal studies where multiple nested sources of variance exist.
Inter-Scanner Variability
Scanner-related factors introduce substantial variance in fMRI measurements, particularly in multi-center studies. Hardware differences (magnetic field homogeneity, gradient performance, RF coils), software variations (reconstruction algorithms), and acquisition parameter implementations all contribute to this variability.
Table 1: Inter-Scanner Reliability of Resting-State fMRI Metrics
| fMRI Metric | Intra-Scanner ICC | Inter-Scanner ICC | Notes |
|---|---|---|---|
| Amplitude of Low Frequency Fluctuation (ALFF) | 0.48-0.72 | 0.31-0.65 | Greater sensitivity to BOLD signal intensity differences |
| Regional Homogeneity (ReHo) | 0.45-0.68 | 0.28-0.61 | Less dependent on signal intensity |
| Degree Centrality (DC) | 0.35-0.58 | 0.15-0.42 | Shows worst reliability both intra- and inter-scanner |
| Percent Amplitude of Fluctuation (PerAF) | 0.51-0.75 | 0.42-0.68 | Reduces BOLD intensity influence, improving inter-scanner reliability |
Data from [12] demonstrate that inter-scanner reliability is consistently worse than intra-scanner reliability across all voxel-wise whole-brain metrics. Degree centrality shows particularly poor reliability, while PerAF offers improved performance by correcting for BOLD signal intensity variations.
Scanner Type and Harmonization Approaches
Differences in scanner manufacturers and models significantly impact measurements. One study directly comparing GE MR750 and Siemens Prisma scanners found systematic differences in relative BOLD signal intensity attributable to magnetic field inhomogeneity variations [12]. These differences directly affect metrics like ALFF that depend on absolute signal intensity.
Harmonization techniques have been developed to mitigate scanner effects:
- NeuroCombat: A widely used method that applies Empirical Bayes approaches to remove additive and multiplicative scanner effects from neuroimaging data, originally adapted from genomics batch effect correction [13].
- LongCombat: An extension of NeuroCombat designed for longitudinal studies that accounts for within-subject correlations across timepoints [13].
Experimental data from diffusion MRI studies demonstrate that these harmonization methods can reduce both intra- and inter-scanner variability to levels comparable to scan-rescan variability within the same scanner [13].
Scan Length and Temporal Stability
Session-related factors encompass variations across different scanning sessions, including scan length, time between sessions, and physiological state changes. Research demonstrates that scan length significantly influences resting-state fMRI reliability.
Table 2: Impact of Scan Length on Resting-State fMRI Reliability
| Scan Duration (minutes) | Intrasession Reliability | Intersession Reliability | Practical Recommendations |
|---|---|---|---|
| 3-5 | 0.35-0.55 | 0.25-0.45 | Below optimal range for most applications |
| 9-12 | 0.65-0.78 | 0.60-0.72 | Recommended for intersession studies |
| 13-16 | 0.72-0.82 | 0.68-0.75 | Plateau for intrasession reliability |
| >27 | 0.75-0.85 | 0.70-0.78 | Diminishing returns for practical use |
Data from [14] indicate that increasing scan length from 5 to 13 minutes substantially improves both reliability and similarity metrics. Reliability gains follow a nonlinear pattern, with intersession improvements diminishing after 9-12 minutes and intrasession reliability plateauing around 12-16 minutes. This relationship is driven by both increased number of data points and longer temporal sampling.
Task and Experimental Design
The cognitive paradigm and experimental design significantly impact session-to-session reliability. Studies simultaneously comparing multiple tasks have found substantial variation in reliability across paradigms:
- Motor tasks generally show higher reliability (ICC: 0.60-0.75) due to reduced cognitive strategy variations [11].
- Complex cognitive tasks (e.g., working memory, emotion regulation) demonstrate moderate reliability (ICC: 0.40-0.65) due to variable cognitive strategies across sessions [15].
- Block designs typically yield higher reliability than event-related designs for basic sensory and motor tasks [15].
- Contrast type influences reliability, with task-versus-rest contrasts generally more reliable than subtle within-task comparisons [15].
One study directly comparing episodic recognition and working memory tasks found that the interaction between task and design significantly influenced reliability, emphasizing that no single combination optimizes reliability for all applications [15].
Physiological and State Factors
Biological variance encompasses both trait individual differences and state-dependent fluctuations that affect fMRI measurements:
- Head motion: Even when within acceptable thresholds (e.g., <2mm), subtle motion differences between sessions contribute significantly to reliability limitations, accounting for approximately 30-40% of single-session variance in thresholded t-maps [11].
- Cardiac and respiratory pulsations: These introduce cyclic noise that can be misattributed as neural activity, particularly in regions near major vessels [14].
- Cognitive/emotional state: Variations in attentional focus, anxiety, rumination, or mind-wandering between sessions affect BOLD activity patterns [9].
- Vasomotion: Spontaneous oscillations in blood vessel diameter introduce cyclicity in BOLD signals that can be misrepresented as functional connectivity [16].
The cyclic nature of biological signals introduces autocorrelation that violates independence assumptions in standard statistical tests, potentially increasing false positive rates in functional connectivity analyses [16].
Clinical Population Considerations
Biological variance manifests differently in clinical populations, potentially affecting reliability estimates. For example, patients with major depressive disorder may show different reliability patterns due to symptom fluctuation, medication effects, or disease-specific vascular differences [9]. Importantly, ICC values are proportional to between-subject variability, meaning that heterogeneous samples (including both patients and controls) can produce higher ICCs even with identical within-subject reliability [9].
Experimental Protocols for Assessing Variance Components
Test-Retest fMRI Protocols
Robust assessment of variance components requires carefully designed test-retest experiments:
Participant Selection and Preparation
- Recruit subjects representative of the target population (e.g., patients for clinical applications) [9]
- Match groups for age, sex, and other relevant demographic factors
- Standardize instructions across sessions regarding eye status (open/closed), cognitive engagement, and alertness
Data Acquisition Parameters
- Use consistent scanning parameters across sessions: TR/TE, flip angle, voxel size, FOV [12]
- Implement physiological monitoring: cardiac, respiratory, and galvanic skin response where possible [14]
- Control for time-of-day effects when feasible [17]
Session Timing Considerations
- For intra-session reliability: 20-60 minute intervals between scans [15]
- For inter-session reliability: Days to weeks between scans, matching intended application intervals [9]
- For longitudinal studies: Months between scans to assess stability over clinically relevant intervals [9]
Processing Pipelines and Statistical Analysis
Preprocessing Steps
- Motion correction using Friston-24 parameter model [12]
- Physiological noise removal (RETROICOR for cardiac/respiratory effects) [14]
- Nuisance regression (white matter, CSF signals, motion parameters) [14]
- Spatial normalization to standard templates (e.g., MNI space) [12]
- Band-pass filtering (typically 0.01-0.1 Hz) with appropriate downsampling to avoid inflation of correlation estimates [16]
Analytical Approaches
- For ROI-based analyses: Extract mean time series from predefined regions
- For voxel-wise analyses: Compute metrics across whole brain
- For connectivity analyses: Apply Fisher's Z-transformation to correlation coefficients to improve normality [14]
- Implement surrogate data methods to account for autocorrelation effects [16]
Visualization of Variance Components in fMRI
This visualization illustrates the complex interplay between major variance sources in fMRI measurements, highlighting how scanner, session, and biological factors collectively influence measurement reliability. The color-coded framework helps researchers identify potential sources of variance in their specific experimental context.
The Scientist's Toolkit: Essential Methods for Variance Control
Table 3: Research Reagent Solutions for fMRI Variance Assessment
| Tool/Method | Primary Function | Application Context | Key References |
|---|---|---|---|
| NeuroCombat/LongCombat | Harmonization of multi-scanner data | Multi-center studies, longitudinal designs | [13] |
| ICED Framework | Decomposition of variance components | Experimental design optimization | [10] |
| RETROICOR | Physiological noise correction | Cardiac/respiratory artifact removal | [14] |
| PerAF (Percent Amplitude of Fluctuation) | BOLD intensity normalization | Inter-scanner reliability improvement | [12] |
| Surrogate Data Methods | Autocorrelation-robust hypothesis testing | False positive control in connectivity | [16] |
| FIR/Gamma Variate Models | Flexible HRF modeling | Improved task reactivity estimation | [9] |
| Phantom QA Protocols | Scanner performance monitoring | Variance attribution analysis | [17] |
| 8-Bromo-7-methoxycoumarin | 8-Bromo-7-methoxycoumarin, CAS:172427-05-3, MF:C10H7BrO3, MW:255.06 g/mol | Chemical Reagent | Bench Chemicals |
| 2-(5-Bromothiophen-2-yl)quinoxaline | 2-(5-Bromothiophen-2-yl)quinoxaline|2-Thienylquinoxaline Reagent | Bench Chemicals |
Understanding and mitigating sources of variance in fMRI is essential for advancing the technique's application in clinical trials and drug development. Scanner-related factors introduce systematic biases that can be addressed through harmonization techniques like NeuroCombat. Session-related factors, particularly scan length and task design, can be optimized based on the specific reliability requirements of a study. Biological factors present both challenges and opportunities, as they represent both noise and signals of interest in clinical applications. The future of fMRI reliability assessment lies in comprehensive approaches that simultaneously account for multiple variance sources through frameworks like ICED, improved experimental design, and advanced statistical methods that properly account for the complex nature of fMRI data. Researchers should select reliability optimization strategies based on their specific application, whether for individual differentiation, group comparisons, or longitudinal monitoring of treatment effects.
The Reproducibility Crisis in Neuroimaging and Numerical Uncertainty
Recent evidence has revealed a significant reproducibility crisis in neuroimaging, threatening the validity of findings and their application in areas like drug development. This crisis stems from multiple sources, but a critical and often underestimated factor is numerical uncertainty within analytical pipelines. When researchers analyze brain-imaging data, they employ complex processing pipelines to derive findings on brain function or pathologies. Recent work has demonstrated that seemingly minor analytical decisions, small amounts of numerical noise, or differences in computational environments can lead to substantial differences in the final results, thereby endangering the trust in scientific conclusions [18]. This variability is not merely a theoretical concern; studies like the Neuroimaging Analysis Replication and Prediction Study (NARPS) have shown that when 70 independent teams were tasked with testing the same hypotheses on the same dataset, their conclusions showed poor agreement, primarily due to methodological variability in their analysis pipelines [19]. The instability of results can range from perfectly stable to highly unstable, with some results having as few as zero to one significant digits, indicating a profound lack of reliability [18]. This article explores the roots of this crisis, quantifies the impact of numerical uncertainty, and compares solutions aimed at enhancing the reliability of neuroimaging research for scientists and drug development professionals.
Quantifying the Problem: Numerical Uncertainty and Its Impact
Experimental Evidence of Numerical Instability
Direct experimentation has illuminated how numerical uncertainty propagates through analytical pipelines. In one key study, researchers instrumented a structural connectome estimation pipeline with Monte Carlo Arithmetic to introduce random noise throughout the computation process. This method allowed them to evaluate the reliability of the resulting brain networks (connectomes) and the robustness of their features [18]. The findings were alarming: the stability of results ranged from perfectly stable (i.e., all digits of data significant) to highly unstable (i.e., zero to one significant digits) [18]. This variability directly impacts downstream analyses, such as the classification of individual differences, which is crucial for both basic cognitive neuroscience and clinical applications in drug development.
Key Metrics for Assessing Reliability
In neuroimaging, reliability is typically assessed using two primary metrics, which represent different but complementary conceptions of signal and noise. The table below summarizes these core metrics and findings from key studies.
Table 1: Key Metrics for Assessing Reliability and Experimental Findings
| Metric | Definition | Interpretation | Experimental Findings |
|---|---|---|---|
| Coefficient of Variation (CV) | ( CVi = \frac{\sigmai}{mi} ) where (\sigmai) is within-object variability and (m_i) is the mean [10]. | Measures precision of measurement for a single object (e.g., a phantom or participant). A lower CV indicates higher precision [10]. | In simulation studies, CV can remain low (good precision) even when the Intra-class Correlation Coefficient (ICC) is low, showing that a measure can be precise but poor for detecting between-person differences [10]. |
| Intra-class Correlation Coefficient (ICC) | ( ICC = \frac{\sigmaB^2}{\sigmaW^2 + \sigmaB^2} ) where (\sigmaB^2) is between-person variance and (\sigma_W^2) is within-person variance [10]. | Measures consistency in assessing between-person differences. Ranges from 0-1; higher values indicate better reliability for group studies [10]. | A high ICC indicates that the measure reliably discriminates among individuals, which is fundamental for studies of individual differences in brain structure or function [10]. |
| Stability (Significant Digits) | The number of digits in a result that remain unchanged despite minor numerical perturbations [18]. | Direct measure of numerical robustness. More significant digits indicate greater stability and lower numerical uncertainty [18]. | Results from connectome pipelines showed variability from "perfectly stable" (all digits significant) to "highly unstable" (0-1 significant digits) [18]. |
The distinction between CV and ICC is critical. A physicist or engineer focused on measuring a phantom might prioritize a low CV, indicating high precision. In contrast, a psychologist or clinical researcher studying individual differences in a population requires a high ICC, which shows that the measurement can reliably distinguish one person from another. A measurement can be precise (low CV) but still be poor for detecting individual differences (low ICC) if the between-person variability is small relative to the within-person variability [10].
The Multifactorial Nature of the Reproducibility Crisis
The reproducibility crisis in neuroimaging is not due to a single cause but arises from a confluence of factors. Evidence for this crisis includes an absence of replication studies in published literature, the failure of large systematic projects to reproduce published results, a high prevalence of publication bias, the use of questionable research practices that inflate false positive rates, and a documented lack of transparency and completeness in reporting methods, data, and analyses [20]. Within this broader context, analytical variability is a major contributor.
Experimental Protocol: Assessing Reliability with ICED
To systematically assess reliability and decompose sources of error, researchers have developed methods like Intra-class Effect Decomposition (ICED). This protocol uses structural equation modeling of data from a repeated-measures design to break down reliability into orthogonal sources of measurement error associated with different characteristics of the measurements, such as session, day, or scanning site [10].
Protocol Steps:
- Study Design: Implement a repeated-measures design where each participant is scanned multiple times. The design should encompass the potential sources of variability of interest (e.g., different sessions on the same day, different days, different scanners in a multi-site study).
- Data Collection: Collect neuroimaging data according to the designed protocol. This could involve structural, functional, or diffusion-weighted MRI.
- Model Specification: Using a structural equation modeling framework, specify a path diagram that represents the different nested sources of variance (e.g., runs nested within sessions, sessions nested within days).
- Variance Decomposition: The ICED model estimates the magnitude of the variance components associated with each specified factor (e.g., day, session, participant).
- Reliability Estimation and Interpretation: The variance components are used to calculate ICC and understand the relative contribution of each factor to the total measurement error. This helps researchers identify the largest sources of unreliability and informs the planning of future studies [10].
Table 2: Decomposing Sources of Variability in Neuroimaging
| Source of Variability | Description | Impact on Reproducibility |
|---|---|---|
| Numerical Uncertainty | Instability in results due to computational environment, rounding errors, or algorithmic implementation [18]. | Leads to impactful variability in derived brain networks, with stability ranging from 0 to all digits being significant [18]. |
| Methodological Choices | Decisions in preprocessing and analysis pipelines (e.g., software tool, parameter settings) [19]. | The primary driver of divergent results in the NARPS study, where 70 teams analyzing the same data reached different conclusions [19]. |
| Data Acquisition | Variability across scanning sessions, days, sites, or scanners [10]. | A major source of measurement error that can be quantified using frameworks like ICED, affecting both CV and ICC [10]. |
| Insufficient Reporting | Lack of transparency and completeness in describing methods and analyses [20]. | Undermines the ability to replicate or reproduce findings, even when checklists like COBIDAS are used [19]. |
The following diagram illustrates the core conceptual relationship between different data and methodology choices and their impact on research conclusions, which was starkly revealed by studies like NARPS.
Figure 1: How One Dataset Can Lead to Many Conclusions. A single input dataset, when processed through different methodological choices and subjected to numerical uncertainty, can yield a wide range of results and divergent scientific conclusions.
Solutions and Comparative Analysis
Standardization and Open Science Practices
A multi-pronged approach is required to combat the reproducibility crisis, focusing on standardization, transparency, and the adoption of robust tools.
- Standardize Preprocessing with Tools like NiPreps: Initiatives such as the NeuroImaging PREProcessing toolS (NiPreps) provide standardized, automated preprocessing pipelines for various modalities (e.g., fMRIPrep for fMRI). These tools leverage the Brain Imaging Data Structure (BIDS) for input and output, ensuring consistency, reducing analytical variability, and improving the reliability of the resulting "scores" for subsequent analysis [19].
- Adopt the Brain Imaging Data Structure (BIDS): BIDS provides a consistent framework for organizing neuroimaging data and metadata. This standardization is critical for implementing reproducible research, maximizing data shareability, and ensuring proper data archiving. It also enables the development of BIDS Apps—portable pipeline containers that operate consistently on any BIDS-formatted dataset [19].
- Share Research Plans, Code, and Data: Reproducible research practices advocate for three key steps: (1) sharing research plans via pre-registration; (2) organizing and sharing data in BIDS-formatted repositories like OpenNeuro; and (3) organizing and sharing code using version control (e.g., Git) and containerization (e.g., Docker, Singularity) to capture the exact computational environment [20] [21].
- Quantify and Report Reliability: Researchers should move beyond qualitative statements about reliability and routinely quantify it using appropriate metrics like ICC and CV for their specific context. Frameworks like ICED allow for a nuanced understanding of different error sources, which is invaluable for planning longitudinal studies or multi-site trials [10].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key tools and resources that form the foundation for reproducible and reliable neuroimaging research.
Table 3: Essential Research Reagent Solutions for Reproducible Neuroimaging
| Tool/Resource | Category | Primary Function |
|---|---|---|
| BIDS (Brain Imaging Data Structure) [19] | Data Standard | Provides a consistent framework for structuring data directories, naming conventions, and metadata specifications, enabling data shareability and pipeline interoperability. |
| NiPreps (e.g., fMRIPrep) [19] | Standardized Pipeline | Provides robust, standardized preprocessing workflows for different neuroimaging modalities, reducing analytical variability and improving reliability. |
| DataLad [21] [20] | Data Management | A free and open-source distributed data management system that keeps track of data, ensures reproducibility, and supports collaboration. |
| Docker/Singularity [21] [20] | Containerization | Creates portable and reproducible software environments, ensuring that analyses run identically across different computational systems. |
| Git/GitHub [20] | Version Control | Tracks changes in code and analysis scripts, facilitating collaboration and ensuring the provenance of analytical steps. |
| ICED Framework [10] | Reliability Assessment | Uses structural equation modeling to decompose reliability into specific sources of measurement error (e.g., session, site) for improved study design. |
| OpenNeuro [19] | Data Repository | A public repository for sharing BIDS-formatted neuroimaging data, promoting open data and facilitating re-analysis. |
| 4-Methoxy-6-nitroindole | 4-Methoxy-6-nitroindole|CAS 175913-41-4 | 4-Methoxy-6-nitroindole (CAS 175913-41-4) is a versatile nitro- and methoxy-substituted indole building block for pharmaceutical and agrochemical research. For Research Use Only. Not for human or veterinary use. |
| Cis-2-Amino-cyclohex-3-enecarboxylic acid | Cis-2-Amino-cyclohex-3-enecarboxylic Acid | RUO | High-purity Cis-2-Amino-cyclohex-3-enecarboxylic acid for peptide research. For Research Use Only. Not for human or veterinary use. |
The workflow for implementing a reproducible neuroimaging study, integrating these various tools and practices, can be summarized as follows.
Figure 2: A Reproducible Neuroimaging Workflow. A sequential workflow integrating modern tools and practices to enhance the reproducibility and reliability of neuroimaging research from start to finish.
The reproducibility crisis in neuroimaging, significantly driven by numerical uncertainty and analytical variability, presents a formidable challenge to the field. However, it also affords an opportunity to increase the robustness of findings by adopting more rigorous methods. The experimental evidence is clear: numerical instability can lead to impactful variability in brain networks, and methodological choices can dramatically alter research conclusions. For researchers and drug development professionals, the path forward requires a cultural and technical shift towards standardization, transparency, and rigorous reliability assessment. By leveraging standardized pipelines like NiPreps, organizing data with BIDS, sharing code and data openly, and routinely quantifying reliability with frameworks like ICED, the neuroimaging community can build a more robust, reliable, and reproducible foundation for understanding the brain.
Multicenter studies are indispensable in brain imaging research for accelerating participant recruitment and enhancing the generalizability of findings. However, they introduce a complex interplay between statistical power and technical variance. This guide objectively compares the performance of different study designs and analytical tools in managing this balance. We present empirical data on variance components in functional MRI, evaluate the reliability of automated brain volumetry software, and analyze the statistical foundations of design effects. Framed within the broader thesis of brain imaging method reliability, this analysis provides researchers, scientists, and drug development professionals with evidence-based recommendations for optimizing multicenter study design and execution.
In multicenter brain imaging studies, the total observed variance in neuroimaging metrics can be partitioned into several distinct components. Understanding these components is critical for designing powerful studies and interpreting their results accurately. A foundational study dissecting variance in a multicentre functional MRI study identified that in activated regions, the total variance partitions as follows: between-subject variance (23% of total), between-centre variance (2%), between-paradigm variance (4%), within-session occasion (paradigm repeat) variance (2%), and residual (measurement) error (69%) [22].
This variance partitioning reveals that measurement error constitutes the largest fraction, underscoring the significance of technical reliability. Furthermore, the surprisingly small between-centre contribution suggests that well-controlled multicentre studies can be conducted without major compensatory increases in sample size. A separate study on scan-rescan reliability further emphasizes that the choice of software has a stronger effect on volumetric measurements than the scanner itself, highlighting another critical dimension of technical variance [23].
Quantifying the Statistical Power of Multicenter Designs
The statistical power of a multicenter study is fundamentally influenced by its design, which dictates how the center effect is handled statistically. The core concept for quantifying this is the design effect (Deff), defined as the ratio of the variance of an estimator (e.g., a treatment effect) in the actual multicenter design to its variance under a simple random sample assumption [24].
The Design Effect Formula
For a multicenter study comparing two groups on a continuous outcome, the design effect can be approximated by the formula: Deff ≈ 1 + (S - 1)Ï
In this formula:
- Ï is the intraclass correlation coefficient (ICC), measuring the correlation between data from two subjects in the same center.
- S is a statistic that quantifies the heterogeneity of group distributions across centers (i.e., the association between the group variable and the center) [24].
The value of the Deff directly determines the gain or loss of power:
- Deff < 1: Indicates a gain in power. The multicenter design is more efficient than a simple random sample.
- Deff > 1: Indicates a loss in power. The sample size must be inflated to compensate for the clustering effect.
- Deff = 1: Indicates no net change in power.
Power Implications Across Study Designs
The application of the design effect formula to common research designs reveals how power is differentially affected.
Table 1: Design Effects and Power Implications in Different Multicenter Study Designs
| Study Design | Description | Design Effect (Deff) | Power Implication |
|---|---|---|---|
| Stratified Individually Randomized Trial | Randomization is balanced and stratified per center; equal group sizes within centers. | Deff = 1 - Ï | Gain in Power |
| Multicenter Observational Study | Group distributions are identical across all centers (i.e., constant proportion in group 1). | Deff = 1 - Ï | Gain in Power |
| Cluster Randomized Trial | Entire centers (clusters) are randomized to a single treatment group. | Deff ≈ 1 + [(m - 1)Ï] | Loss of Power |
| Matched Pair Design | A special case of stratification with 1 subject per group in each "center" (e.g., a pair). | Deff = 1 - Ï | Gain in Power |
Key: Ï = Intraclass Correlation Coefficient; m = mean cluster size.
The key insight is that power loss is not an inevitable consequence of a multicenter design. A loss occurs primarily when the grouping variable is strongly associated with the center, as in cluster randomized trials. In contrast, when the group distribution is balanced across centers—through stratification or natural occurrence—the design effect shrinks, leading to a gain in power [24].
Technical Variance in Brain MRI Analysis: A Software Comparison
Technical variance, introduced by different imaging hardware and processing software, is a major threat to the reliability of multicenter brain imaging studies. A recent scan-rescan reliability assessment evaluated seven automated brain volumetry tools across six scanners in twelve subjects [23].
Experimental Protocol for Reliability Assessment
The methodology for assessing technical variance was as follows:
- Subjects: Twelve healthy volunteers.
- Scanning Protocol: Each subject was scanned on six different scanners twice within a 2-hour period on the same day (scan-rescan).
- Software Analysis: The T1-weighted structural images from all scanning sessions were processed through seven different volumetry tools: AssemblyNet, AIRAscore, FreeSurfer, FastSurfer, syngo.via, SPM12, and Vol2Brain.
- Outcome Measures: The primary outputs were gray matter volume, white matter volume, and total brain volume.
- Statistical Analysis: The study employed:
- Generalized Estimating Equations (GEE): To model the significant effects of software and scanner on volumetric measurements.
- Coefficient of Variation (CV): Calculated as a percentage to quantify scan-rescan reliability. A lower CV indicates higher reliability.
- Bland-Altman Analysis: To assess the limits of agreement between methods.
Comparative Reliability of Volumetry Software
The results provide a direct performance comparison of the different software solutions, which is critical for selecting tools in multicenter research.
Table 2: Scan-Rescan Reliability of Brain Volumetry Software Across Multiple Scanners
| Software Tool | Median CV for Gray Matter (%) | Median CV for White Matter (%) | Median CV for Total Brain Volume (%) | Relative Performance |
|---|---|---|---|---|
| AssemblyNet | < 0.2% | < 0.2% | 0.09% | High Reliability |
| AIRAscore | < 0.2% | < 0.2% | 0.09% | High Reliability |
| FreeSurfer | > 0.2% | > 0.2% | > 0.2% | Lower Reliability |
| FastSurfer | > 0.2% | > 0.2% | > 0.2% | Lower Reliability |
| syngo.via | > 0.2% | > 0.2% | > 0.2% | Lower Reliability |
| SPM12 | > 0.2% | > 0.2% | > 0.2% | Lower Reliability |
| Vol2Brain | > 0.2% | > 0.2% | > 0.2% | Lower Reliability |
The GEE models showed a statistically significant effect (p < 0.001) of both software and scanner on all volumetric measurements, with the software effect being stronger than the scanner effect [23]. This finding underscores that the choice of processing pipeline is a more critical decision than scanner model for minimizing technical variance. While Bland-Altman analysis showed no systematic bias, the limits of agreement varied significantly between methods, meaning that the degree of expected disagreement between measurements depends heavily on the software used.
The Researcher's Toolkit for Multicenter Studies
Success in multicenter brain imaging research relies on a suite of methodological, statistical, and computational tools.
Table 3: Essential Research Reagents and Solutions for Multicenter Brain Imaging
| Item / Solution | Category | Function / Purpose |
|---|---|---|
| Stratified Randomization | Study Design | Balances group distributions across centers to minimize Deff and maximize statistical power [24]. |
| Intraclass Correlation Coefficient (ICC) | Statistical Metric | Quantifies the degree of correlation of data within centers; essential for power calculations [24]. |
| Design Effect (Deff) Formula | Statistical Tool | Predicts the impact of the multicenter design on statistical power and required sample size [24]. |
| High-Reliability Volumetry (e.g., AssemblyNet) | Software Tool | Provides consistent and reliable brain volume measurements across different scanning sessions and scanners, reducing technical variance [23]. |
| Convolutional Neural Networks (CNNs) | Software Tool | Offers lower numerical uncertainty in tasks like MRI registration and segmentation compared to traditional tools like FreeSurfer, enhancing reproducibility [25]. |
| Generalized Estimating Equations (GEE) | Statistical Model | A robust method for analyzing clustered data (e.g., subjects within centers) that provides valid inferences even with misspecified correlation structures. |
| Coefficient of Variation (CV) | Metric | A standardized measure (percentage) of scan-rescan reliability used to compare the precision of different measurement tools [23]. |
| 4-Bromo-3-oxo-n-phenylbutanamide | 4-Bromo-3-oxo-N-phenylbutanamide | Research Chemical | 4-Bromo-3-oxo-N-phenylbutanamide for research use only (RUO). A versatile beta-keto amide building block for organic synthesis and medicinal chemistry. |
| Azobenzene, 4-(phenylazo)- | Azobenzene, 4-(phenylazo)-|High-Purity Azo Compound | High-purity Azobenzene, 4-(phenylazo)- for research applications in photopharmacology and smart materials. For Research Use Only. Not for human or veterinary use. |
Integrated Workflow: From Study Design to Result Interpretation
The relationship between key decisions in a multicenter study and their impact on the final results can be visualized as a workflow where managing statistical and technical variance is paramount. The following diagram synthesizes this process:
Diagram: Impact of Design and Tool Choices on Multicenter Study Outcomes. This workflow illustrates how initial choices in study design and software selection directly influence statistical power and technical variance, thereby determining the ultimate reliability of the study's findings.
The successful execution of a multicenter brain imaging study requires a deliberate and informed balance between statistical power and technical variance. Based on the empirical data and theoretical frameworks presented, the following conclusions and recommendations are offered:
- Prioritize Balanced Designs: To maximize statistical power, employ study designs that balance the group distribution across centers, such as stratified individually randomized trials. This approach transforms the center effect from a source of noise into a factor that increases efficiency, yielding a design effect below 1 [24].
- Select Software for Minimal Variance: The choice of analysis software has a demonstrably greater impact on measurement variance than the choice of scanner. To ensure reliable longitudinal and cross-sectional comparisons, commit to using the same high-reliability software tool (e.g., one with a CV < 0.2%) throughout a study [23].
- Quantify and Account for Variance: During the planning phase, use the design effect formula to perform accurate sample size calculations, incorporating realistic estimates of the ICC. Furthermore, the knowledge that measurement error is the largest component of total variance in fMRI [22] argues for protocols that include task repetition within sessions to improve signal-to-noise ratio.
- Embrace Methodological Consistency: The strongest guarantee of reliable results in multicenter research is the consistent application of the same scanner and software combination across all sites and sessions [23]. This practice minimizes technical variance, ensuring that observed changes in brain measures are more likely to reflect true biological effects rather than methodological inconsistencies.
By integrating these principles—leveraging balanced designs for power, selecting tools for minimal technical variance, and enforcing methodological consistency—researchers can harness the full potential of multicenter studies to generate robust, reproducible, and clinically meaningful findings in brain imaging research.
Impact of Hydration, Menstrual Cycle, and Daily Biological Fluctuations
The reliability of brain imaging measurements is fundamental to their application in both clinical diagnostics and neuroscience research. A significant challenge in achieving this reliability is accounting for inherent biological variability. Fluctuations in physiological states, driven by factors such as hydration status and the menstrual cycle, can alter brain measurements obtained through magnetic resonance imaging (MRI), magnetoencephalography (MEG), and functional MRI (fMRI). These fluctuations, if unaccounted for, can introduce confounding variability that mimics or obscures pathological changes, potentially compromising longitudinal study results and clinical trial outcomes. This guide systematically compares the effects of these biological factors on brain imaging metrics, providing researchers and drug development professionals with experimental data and methodologies to improve measurement accuracy.
The Menstrual Cycle: Hormonal Effects on Brain Structure and Function
Quantitative Fluctuations in Neural Oscillations
The menstrual cycle, characterized by rhythmic fluctuations of estradiol and progesterone, induces measurable changes in spontaneous neural activity. A 2021 MEG study quantitatively demonstrated cycle-dependent alterations in resting-state cortical activity [26].
Table 1: Menstrual Cycle Effects on Spectral MEG Parameters (MP vs. OP)
| Spectral Parameter | Change During Menstrual Period (MP) | Brain Regions Involved | Statistical Significance |
|---|---|---|---|
| Median Frequency | Decreased | Global | Significant (p < 0.05) |
| Peak Alpha Frequency | Decreased | Global | Significant (p < 0.05) |
| Shannon Spectral Entropy | Increased | Global | Significant (p < 0.05) |
| Theta Oscillatory Intensity | Decreased | Right Temporal Cortex, Right Limbic System | Significant (p < 0.05) |
| High Gamma Oscillatory Intensity | Decreased | Left Parietal Cortex | Significant (p < 0.05) |
The study found that the median frequency and peak alpha frequency of the power spectrum were significantly lower during the menstrual period (MP), while Shannon spectral entropy was higher [26]. These parameters are established biomarkers for functional brain diseases, indicating that the menstrual cycle is a confounding factor that must be controlled for in clinical MEG interpretations.
Phase-Dependent Shifts in Brain Activation and Connectivity
Beyond spectral properties, the menstrual cycle modulates regional brain activation and large-scale network communication. A 2019 fMRI study investigating spatial navigation and verbal fluency found that, despite no significant performance differences, brain activation patterns shifted dramatically between cycle phases [27].
Table 2: Menstrual Cycle Phase Effects on Brain Activation and Connectivity
| Cycle Phase | Hormonal Profile | Neural Substrate Affected | Observed Effect on Brain Activity |
|---|---|---|---|
| Pre-ovulatory (Follicular) | High Estradiol | Hippocampus | Boosts hippocampal activation [27] |
| Mid-Luteal | High Progesterone | Fronto-Striatal Circuitry | Boosts frontal & striatal activation; increased inter-hemispheric decoupling [27] |
| Luteal Phase | High Progesterone | Whole-Brain Turbulent Dynamics | Higher information transmission across spatial scales [28] |
The study demonstrated that estradiol and progesterone exert distinct, and often opposing, effects on brain networks. Estradiol enhances hippocampal activation, whereas progesterone boosts fronto-striatal activation and leads to inter-hemispheric decoupling, which may help down-regulate hippocampal influence [27]. Furthermore, a 2021 dense-sampling study using a turbulent dynamics framework showed that the luteal phase is characterized by significantly higher whole-brain information transmission across spatial scales compared to the follicular phase, affecting default mode, salience, somatomotor, and attention networks [28].
Experimental Protocol for Controlling Menstrual Cycle Effects
Study Design: To systematically investigate menstrual cycle effects, the protocol from Pritschet et al. (2019) is exemplary [27]. The study involved scanning participants multiple times across their naturally cycling menstrual cycle.
- Participants: 36 healthy, naturally cycling women with no history of psychological, endocrinological, or neurological illness.
- Cycle Phase Determination: Sessions were scheduled during:
- Menses (Days 2-6): Low estradiol and progesterone.
- Pre-ovulatory Phase (2-3 days before expected ovulation): High estradiol, low progesterone. Confirmed via commercial ovulation tests detecting the luteinizing hormone (LH) surge.
- Mid-Luteal Phase (3-10 days after ovulation): High progesterone, medium estradiol. Confirmed via ovulation tests and subsequent menstruation onset.
- Hormone Assay: Multiple saliva samples were collected per session via unstimulated passive drool, immediately frozen, and later analyzed for estradiol and progesterone concentrations after centrifugation to remove particulate matter.
- fMRI Acquisition: A 3T Siemens scanner was used. The protocol included a T2*-weighted multi-band EPI sequence for resting-state fMRI (TR=720 ms, TE=37 ms, voxel size=2mm³, multiband factor=8). A high-resolution T1-weighted MPRAGE structural scan was also acquired.
- Cognitive Tasks: Participants performed spatial navigation and verbal fluency tasks during scanning to probe brain activation underlying specific cognitive functions.
Hydration Status: Effects on Brain Physiology and Measurement
Cognitive and Mood Consequences of Dehydration
The brain is approximately 75% water, making it highly sensitive to changes in hydration status [29]. Even mild dehydration, defined as a 1-2% loss of body water content, can significantly impair cognitive function and mood.
Table 3: Cognitive and Mood Effects of Mild Dehydration (1-2% Body Water Loss)
| Domain Affected | Specific Impairment | Supporting Evidence |
|---|---|---|
| General Cognition | Slower reaction times, reduced attention span, cognitive sluggishness | Journal of Nutrition (2011) [29] |
| Mood | Increased fatigue, headaches, concentration difficulties, heightened irritability | British Journal of Nutrition (2011) [29] |
| Memory & Learning | Impaired short-term memory and reduced ability to concentrate | Frontiers in Human Neuroscience (2013) [29] |
| Neural Efficiency | Increased neural activity required for the same cognitive tasks, leading to mental fatigue | The Journal of Neuroscience (2014) [29] |
Notably, studies suggest women may be more sensitive to dehydration-induced cognitive and mood changes than men, reporting more headaches, fatigue, and concentration difficulties under mild dehydration [30]. Furthermore, rehydration after a 24-hour fluid fast improved mood but did not fully restore vigor and fatigue levels, indicating that the effects of significant fluid deprivation can be prolonged [30].
Impact of Hydration on Brain Volume and Water Content Measurements
Despite the clear cognitive effects, the impact of hydration on structural MRI measures of brain volume is a point of methodological importance. A 2016 JMRI study specifically addressed whether physiological hydration changes affect brain total water content (TWC) and volume [31].
- Experimental Protocol: Twenty healthy volunteers were scanned four times on a 3T scanner:
- Day 1: Baseline scan.
- Day 2: Hydrated scan after consuming 3L of water over 12 hours.
- Day 3 (a): Dehydrated scan after a 9-hour overnight fast.
- Day 3 (b): Reproducibility scan one hour later.
- Measurements: Body weight and urine specific gravity were recorded. MRI sequences included T2 relaxation (for TWC), inversion recovery (for T1), and 3D T1-weighted (for brain volumes). TWC was calculated with corrections and normalized to ventricular CSF.
- Findings: Despite objective signs of dehydration (increased urine specific gravity, decreased body weight), the study found no measurable change in total brain water content within any of the 14 regions examined or in overall brain volume between the hydrated and dehydrated states [31].
This suggests that within a range commonly encountered in clinical settings (e.g., overnight fasting), brain TWC and volume as measured by standard MRI protocols are relatively stable. This is a critical insight for designing longitudinal neuroimaging studies.
Implications for Reliability Assessment in Brain Imaging Research
The Scientist's Toolkit: Key Research Reagent Solutions
Table 4: Essential Materials and Methods for Controlling Biological Variability
| Item / Solution | Function in Research | Application Example |
|---|---|---|
| Salivary Hormone Assay Kits | To non-invasively measure fluctuating levels of estradiol and progesterone for precise cycle phase confirmation. | Used to pool multiple saliva samples per session for accurate hormone level correlation with neural data [27]. |
| Urine Specific Gravity Refractometer | To provide an objective, immediate measure of hydration status at the time of scanning. | Served as a key biomarker (along with body weight) to confirm hydration state intervention in a dehydration-MRI study [31]. |
| Commercial Ovulation Test Kits (LH Surge Detection) | To objectively pinpoint the pre-ovulatory phase in naturally cycling women, moving beyond self-report. | Critical for scheduling the pre-ovulatory scan with high temporal precision in a multi-phase cycle study [27]. |
| Automated Segmentation Software (e.g., FreeSurfer) | To provide reliable, quantitative volumetric data for brain structures across multiple time points with minimal manual intervention. | Used to process 120 T1-weighted volumes for test-retest analysis of subcortical structure volume reliability [7]. |
| Standardized MRI Phantoms (e.g., ADNI Phantom) | To monitor scanner stability and performance over time, separating biological variability from instrumental drift. | Employed for regular quality assurance and scanner stability checks throughout a long-term test-retest study [7]. |
| 3-Hydroxy-4-methylpyridine | 3-Hydroxy-4-methylpyridine | Vitamin B6 Intermediate | High-purity 3-Hydroxy-4-methylpyridine for research. A key pyridoxine analog for studying enzyme cofactors & metabolism. For Research Use Only. Not for human or veterinary use. |
| (S)-4-Aminovaleric acid | (S)-4-Aminovaleric Acid | High-Purity GABA Analog | High-purity (S)-4-Aminovaleric Acid, a selective GABA receptor agonist. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. |
Best Practices for Experimental Design
Integrating the findings on these biological fluctuations leads to several key recommendations for enhancing the reliability of brain imaging data:
- Control for the Menstrual Cycle: In studies involving premenopausal women, the cycle should be a controlled variable. For cross-sectional studies, participants should be scanned in a consistent phase (e.g., early follicular/menses). For longitudinal studies or clinical trials, repeated scans of the same individual should be scheduled in the same cycle phase to minimize hormone-driven variance [26] [27] [32].
- Standardize Hydration Protocols: While brain volume may be resilient to short-term fasting, the clear cognitive and mood effects of dehydration suggest that standardizing hydration instructions (e.g., avoiding significant dehydration) prior to scanning is prudent, especially for task-based fMRI, MEG, or EEG studies where cognitive performance is a metric [30] [29].
- Implement Rigorous Test-Retest Designs: As demonstrated in publicly available test-retest datasets [7] [8], estimating the intra- and inter-session variability of your chosen imaging metrics is crucial. This establishes a benchmark for determining whether observed longitudinal changes exceed normal physiological fluctuations.
- Report and Covary: Transparently report participant information including cycle phase and hydration instructions. Where full control is not feasible, measure and include these factors (e.g., hormone levels) as covariates in statistical models to account for their variance.
Hydration status and the menstrual cycle represent significant sources of biological variability that can impact functional brain measurements, including oscillatory activity, network activation, and cognitive performance. While structural brain volume appears robust to minor hydration shifts, the functional consequences are pronounced. The hormonal fluctuations of the menstrual cycle systematically alter both global spectral properties and region-specific brain activation, with estradiol and progesterone exerting distinct neuromodulatory effects. Acknowledging and controlling for these factors through careful experimental design, phase-specific scheduling, and the use of objective biomarkers is not merely a methodological refinement but a necessity for ensuring the reliability, reproducibility, and ultimate validity of brain imaging data in neuroscience research and drug development.
Analytical Approaches: From Traditional Pipelines to Deep Learning Solutions
In the fields of neuroscience and drug development, the ability to reliably quantify brain structure and function from magnetic resonance imaging (MRI) is paramount. Automated segmentation software provides essential tools for extracting meaningful biological information from raw MRI data, enabling researchers to track disease progression, evaluate treatment efficacy, and understand fundamental brain processes. The reliability of these tools directly impacts the validity of research findings and the success of clinical trials. Among the most established traditional software tools are Statistical Parametric Mapping (SPM) and FreeSurfer, which employ distinct processing philosophies and algorithms for brain image analysis [33] [34]. This guide provides an objective comparison of their performance based on published experimental data, focusing on their application in reliability assessment research critical for researchers and drug development professionals.
FreeSurfer is a comprehensive open-source software suite developed at the Martinos Center for Biomedical Imaging, Harvard-MGH. Its primary strength lies in cortical and subcortical analysis, utilizing surface-based models to measure cortical thickness, surface area, and curvature [34]. The software creates detailed models of the gray-white matter boundary and pial surface, enabling precise quantification of cortical architecture.
Statistical Parametric Mapping (SPM), developed at University College London's Wellcome Trust Centre for Neuroimaging, is a MATLAB-based software that employs a mass-univariate, voxel-based approach [34]. SPM's segmentation and normalization algorithms use a unified generative model that combines tissue classification, bias correction, and image registration within the same framework, making it particularly effective for voxel-based morphometry (VBM) studies [35].
Performance Comparison: Quantitative Experimental Data
Segmentation Accuracy and Volumetric Precision
Multiple independent studies have evaluated the performance of automated segmentation tools against ground truth data, using both simulated digital phantoms and real MRI datasets with expert manual segmentations.
Table 1: Segmentation Accuracy Compared to Ground Truth
| Software | Gray Matter Volume Deviation | White Matter Volume Deviation | Data Source | Experimental Conditions |
|---|---|---|---|---|
| SPM5 | ~10% from reference [35] | ~10% from reference [35] | BrainWeb Digital Phantom | 3% noise, 0% intensity inhomogeneity |
| FreeSurfer | >10% from reference [35] | >10% from reference [35] | BrainWeb Digital Phantom | 3% noise, 0% intensity inhomogeneity |
| FSL | ~10% from reference [35] | ~10% from reference [35] | BrainWeb Digital Phantom | 3% noise, 0% intensity inhomogeneity |
| SPM | Highest accuracy [36] | N/A | IBSR Real MRI Data | Compared to expert segmentations |
| VBM8 | Very high accuracy [36] | N/A | IBSR Real MRI Data | Compared to expert segmentations |
| FreeSurfer | Lowest accuracy [36] | N/A | IBSR Real MRI Data | Compared to expert segmentations |
Reliability and Reproducibility Metrics
Test-retest reliability is crucial for longitudinal studies in drug development where tracking changes over time is essential. Different software packages demonstrate varying reliability performance.
Table 2: Reliability Performance Metrics
| Software | Within-Segmenter Reliability | Between-Segmenter Reliability | Test-Retest Consistency | Experimental Context |
|---|---|---|---|---|
| FreeSurfer | High reliability [36] | Discrepancies up to 24% [35] | High reliability [37] | Real T1 images from same subject scanned twice [36] |
| SPM | N/A | Discrepancies up to 24% [35] | N/A | Real T1 images from same subject scanned twice [36] |
| FSL | Poor reliability [36] | Discrepancies up to 24% [35] | N/A | Real T1 images from same subject scanned twice [36] |
| VBM8 | Very high reliability [36] | N/A | N/A | Real T1 images from same subject scanned twice [36] |
Performance in Clinical Populations
Studies evaluating software performance in specific patient populations reveal important considerations for clinical research and drug development applications.
Table 3: Performance in Neurological and Psychiatric Disorders
| Software | Alzheimer's Disease/MCI | ALS with Frontotemporal Dementia | General Notes on Clinical Application |
|---|---|---|---|
| SPM | Recommended for limited image quality or elderly brains [38] | GM volume changes not significant in SPM [39] | Underestimates GM, overestimates WM with increasing noise [38] |
| FreeSurfer | Calculates largest GM, smallest WM volumes [38] | Similar pattern to FSL VBM results [39] | Calculates smaller brain volumes with increasing noise [38] |
| FSL | Calculates smallest GM volumes [38] | GM changes similar to FreeSurfer cortical measures [39] | Increased WM, decreased GM with image inhomogeneity [38] |
Experimental Protocols: Methodologies for Reliability Assessment
Digital Phantom Validation Studies
The BrainWeb simulated brain database from the Montreal Neurological Institute provides a critical resource for validation studies, offering MRI datasets with varying image quality based on known "gold-standard" tissue segmentation masks [36] [35].
Protocol Summary:
- Data Source: Twenty simulated T1-weighted MRI images from BrainWeb with known ground truth segmentations [36]
- Image Quality Variations: Systematic manipulation of noise levels (0-9%) and intensity inhomogeneity (0-40%) [35]
- Processing Pipeline: Identical preprocessing applied across all software platforms
- Validation Metric: Dice similarity coefficient comparing automated segmentation with ground truth [36]
- Statistical Analysis: Quantitative comparison of volumetric deviations from reference values [35]
This approach allows researchers to assess both within-segmenter (same method, varying image quality) and between-segmenter (same data, different methods) comparability under controlled conditions.
Real MRI Data Validation with Expert Segmentations
Protocol Summary:
- Data Source: Internet Brain Segmentation Repository (IBSR) providing 18 real T1-weighted MR images with expert manual segmentations [36]
- Processing: Each software package processes images using default recommended parameters
- Validation Metric: Overlap measures (Dice coefficient) between automated and manual segmentations
- Additional Metrics: Volume difference ratios, false positive/negative rates [36]
- Statistical Analysis: Correlation coefficients, intraclass correlation coefficients for reliability assessment
Longitudinal Reliability Assessment
Protocol Summary:
- Data Acquisition: Repeated scanning of the same subject with minimal time interval (test-retest design)
- Processing: Identical processing pipelines applied to all scans
- Metrics: Coefficient of variation, intraclass correlation coefficients for volumetric measurements
- Analysis: Comparison of within-subject variability between software platforms [37]
Processing Streams: Architectural Workflows
The fundamental differences between FreeSurfer and SPM emerge from their distinct processing philosophies, which can be visualized through their workflow architectures.
The diagram above illustrates the fundamental architectural differences between FreeSurfer's surface-based stream and SPM's voxel-based stream. FreeSurfer emphasizes precise cortical surface modeling through a sequence of topological operations, while SPM focuses on voxel-wise statistical comparisons through spatial normalization and tissue classification.
Table 4: Essential Resources for Brain Imaging Reliability Research
| Resource | Type | Function in Research | Relevance to Software Comparison |
|---|---|---|---|
| BrainWeb Database | Simulated MRI Data | Provides digital brain phantoms with known ground truth for validation [36] | Enables controlled assessment of accuracy under varying image quality conditions [35] |
| IBSR Data | Real MRI with Expert Segmentations | Offers real clinical images with manual tracings for benchmarking [36] | Allows validation of automated methods against human expert performance |
| OASIS Database | Large-Scale Neuroimaging Database | Provides diverse dataset for testing generalizability [35] | Enables assessment of performance across different populations and scanners |
| UK Biobank Pipeline | Automated Processing Pipeline | Demonstrates large-scale application of processing methods [33] | Illustrates real-world implementation challenges and solutions |
| DARTEL | SPM Algorithm | Improved spatial normalization using diffeomorphic registration [39] | Enhances SPM's registration accuracy for longitudinal studies |
| Threshold Free Cluster Enhancement (TFCE) | FSL Statistical Method | Improves statistical inference in neuroimaging [39] | Highlights impact of statistical methods on final results |
The experimental data reveals that software selection involves significant trade-offs between accuracy, reliability, and methodological approach. FreeSurfer demonstrates advantages for cortical analysis and longitudinal reliability, while SPM shows strengths in statistical parametric mapping and handling of challenging image quality. For drug development professionals tracking subtle changes in clinical trials, FreeSurfer's test-retest reliability may be particularly valuable. For researchers investigating voxel-wise structural differences across populations, SPM's VBM approach may be preferable. Critically, studies consistently show that between-software differences can reach 20-24%, comparable to disease effects, necessitating consistent software use throughout a study [39] [35]. The emerging generation of deep-learning tools like FastSurfer offers promising directions for combining the accuracy of traditional methods with significantly improved processing speed [37].
In the fields of neuroscience and clinical neurology, the quantitative analysis of brain structure through magnetic resonance imaging (MRI) has become an indispensable tool for understanding brain anatomy, diagnosing neurological disorders, and monitoring disease progression. For these measurements to have scientific and clinical value, they must be both accurate and highly reliable. The advent of Convolutional Neural Networks (CNNs) and other deep learning architectures has revolutionized two fundamental computational tasks in brain image analysis: image registration (the spatial alignment of different brain images to a common coordinate system) and image segmentation (the delineation of specific brain structures or regions of interest). These tasks are foundational for everything from longitudinal studies tracking brain atrophy to surgical planning for tumor resection.
This revolution is occurring within the critical context of brain imaging method reliability assessment research. As quantitative imaging biomarkers play an increasingly prominent role in both research and clinical trials, understanding the reliability and reproducibility of these measurements becomes paramount. This article provides a comparative analysis of CNN-based approaches against traditional methodologies for brain image registration and segmentation, with a specific focus on empirical performance data and experimental protocols that inform their reliability.
Performance Comparison: CNNs vs. Traditional Methods
Quantitative Reliability in Segmentation Tasks
Multiple studies have systematically evaluated the performance of automated segmentation tools, providing crucial data on their reliability. A 2025 scan-rescan reliability assessment examined seven volumetry tools across six scanners, measuring the coefficient of variation (CV) for gray matter (GM), white matter (WM), and total brain volume (TBV) measurements. The CV quantifies the relative variability of measurements, with lower values indicating higher reliability [40].
Table 1: Scan-Rescan Reliability of Brain Volume Measurements Across Software Tools
| Segmentation Software | Type | Gray Matter CV (%) | White Matter CV (%) | Total Brain Volume CV (%) |
|---|---|---|---|---|
| AssemblyNet | AI-based | <0.2% | <0.2% | 0.09% |
| AIRAscore | AI-based | <0.2% | <0.2% | - |
| FastSurfer | CNN-based | <1.0% | <0.2% | - |
| FreeSurfer | Traditional | <1.0% | - | - |
| SPM12 | Traditional | <1.0% | - | - |
| syngo.via | Traditional | <1.0% | - | - |
| Vol2Brain | Traditional | <1.0% | - | - |
The data reveals that AI-based tools, particularly AssemblyNet and AIRAscore, achieved superior reliability with median CV values below 0.2% for both GM and WM, significantly outperforming traditional software. The study concluded that software choice had a stronger effect on measurement variability than the scanner hardware itself (p < 0.001) [40].
Numerical Uncertainty in Registration and Segmentation
A 2025 study specifically assessed the numerical uncertainty of CNNs in brain MRI analysis, comparing them to the traditional FreeSurfer pipeline ("recon-all"). Numerical uncertainty refers to potential errors in calculations arising from computational systems, which can impact reproducibility across different execution environments. The research employed Random Rounding, a stochastic arithmetic technique, to quantify this uncertainty in tasks of non-linear registration (using SynthMorph CNN) and whole-brain segmentation (using FastSurfer CNN) [25].
Table 2: Numerical Uncertainty Comparison Between CNN and Traditional Methods
| Task | Metric | CNN Model | Performance | Traditional Method (FreeSurfer) |
|---|---|---|---|---|
| Non-linear Registration | Significant Bits (higher is better) | SynthMorph | 19 bits on average | 13 bits on average |
| Whole-Brain Segmentation | Sørensen-Dice Score (0-1, higher is better) | FastSurfer | 0.99 on average | 0.92 on average |
The results demonstrated that CNN predictions were substantially more accurate numerically than traditional image-processing results. The higher number of significant bits in registration and superior Dice scores in segmentation suggest better reproducibility of CNN results across different computational environments, a critical factor for multi-center research studies and clinical trials [25].
Experimental Protocols for Reliability Assessment
Scan-Rescan Reliability Protocol
The assessment of segmentation reliability requires a rigorous experimental design that controls for multiple sources of variability. A landmark test-retest dataset established a protocol that has been widely adopted in the field [7].
Experimental Design:
- Subjects: Multiple healthy volunteers (e.g., 3 subjects in the original study).
- Scanning Sessions: Multiple sessions (e.g., 20) over a defined period (e.g., 31 days).
- Intra-session Acquisitions: Two scans per session with subject repositioning between scans.
- Scanner Protocol: Standardized protocol (e.g., Alzheimer's Disease Neuroimaging Initiative (ADNI) T1-weighted protocol).
- Data Analysis: Processing with consistent software version and computing environment.
Key Metrics:
- Coefficient of Variation (CV): Calculated for both intra-session (CVs) and inter-session (CVt) measurements.
- Statistical Models: Generalized estimating equations (GEE) to evaluate effects of software, scanner, and session on measurements.
This protocol allows researchers to separate measurement variability due to the segmentation method itself from biological variations occurring day to day, providing a comprehensive assessment of a tool's reliability [40] [7].
Multi-Atlas Registration Validation Protocol
For registration tasks, validation often involves assessing the accuracy of propagating anatomical labels from an atlas to target images. A 2023 study on MR-CT multi-atlas registration guided by CNN segmentation outlined a comprehensive protocol [41].
Experimental Workflow:
- Data Preparation: Collect paired MR and CT brain images with manual segmentations of key structures (e.g., ventricles, brain parenchyma).
- CNN Segmentation: Train and validate CNN models (e.g., nnU-Net) to automatically segment guidance structures.
- Registration: Perform multi-atlas registration using similarity measures (e.g., Normalized Gradient Fields - NGF) with guidance from segmented structures.
- Validation: Quantify registration accuracy using Dice Similarity Coefficient (DSC) between propagated labels and ground truth.
This study demonstrated that using CNN-derived segmentations as guidance for registration achieved high accuracy (mean Dice values of 0.87 for ventricles and 0.98 for brain parenchyma), closely matching the performance when using manual segmentations (0.92 and 0.99 respectively) [41].
The following diagram illustrates the logical relationship and workflow between these key reliability assessment methodologies:
Implementing and validating CNN-based registration and segmentation methods requires familiarity with key software tools, datasets, and validation metrics. The following table summarizes essential "research reagent solutions" used in the featured studies.
Table 3: Essential Research Resources for CNN-Based Brain Image Analysis
| Resource Category | Specific Tools / Metrics | Application & Function |
|---|---|---|
| CNN Segmentation Tools | FastSurfer, AssemblyNet, SynthMorph | Automated segmentation of brain structures from MRI data |
| Traditional Software (Benchmark) | FreeSurfer, FSL, SPM | Established pipelines for comparison and validation studies |
| Performance Metrics | Dice Coefficient/Sørensen-Dice Score, Hausdorff Distance, Coefficient of Variation (CV) | Quantifying segmentation accuracy and measurement reliability |
| Registration Metrics | Significant Bits, Normalized Mutual Information (NMI) | Assessing numerical precision and alignment accuracy in registration |
| Validation Datasets | ADNI Phantom, RSNA Intracranial Hemorrhage Dataset, BraTS Challenges | Standardized data for training and benchmarking algorithms |
| Experimental Protocols | Scan-rescan reliability assessment, Multi-atlas registration validation | Standardized methods for evaluating algorithm performance and reliability |
The deep learning revolution has fundamentally transformed brain image registration and segmentation, with CNN-based approaches demonstrating superior reliability and reduced numerical uncertainty compared to traditional methods. The empirical data consistently shows that CNNs achieve higher reproducibility across different scanning environments and computational platforms, as evidenced by lower coefficients of variation in segmentation tasks (<0.2% for leading AI tools vs. >0.2% for traditional software) and higher significant bits in registration tasks (19 vs. 13 bits). These advancements are particularly significant within the context of brain imaging method reliability assessment, where precise, reproducible measurements are essential for both scientific discovery and clinical application.
As the field continues to evolve, standardized experimental protocols—including scan-rescan reliability assessments and multi-atlas registration validation—provide critical frameworks for objectively evaluating new methodologies. The continued development and validation of CNN-based tools promises to further enhance the reliability of brain imaging analyses, ultimately advancing both neuroscience research and clinical care for neurological disorders.
Magnetic Resonance Imaging (MRI) is a powerful, non-invasive diagnostic tool, but its clinical utility and application in research are often limited by prolonged acquisition times. Accelerated MRI techniques are therefore critical for improving patient comfort, reducing motion artifacts, and increasing throughput. Among the most significant advancements are Parallel Imaging (PI) and Compressed Sensing (CS), which exploit different principles to shorten scan times. More recently, artificial intelligence (AI) and machine learning have been integrated with these methods, pushing the boundaries of acceleration further [42] [43].
This guide provides an objective comparison of these accelerated sequencing families, focusing on their underlying mechanisms, performance metrics, and experimental validation. The context is framed within the reliability assessment of brain imaging methods, providing drug development professionals and scientists with a clear understanding of the trade-offs and capabilities of each technology.
Technical Foundations and Comparison
Core Acceleration Mechanisms
Parallel Imaging (PI) techniques, such as GRAPPA (GeneRalized Autocalibrating Partially Parallel Acquisitions) and SENSE (SENSitivity Encoding), utilize the spatial sensitivity information from multiple receiver coils in a phased array to reconstruct an image from undersampled k-space data. GRAPPA operates in k-space by estimating missing data points using autocorrelation lines, while SENSE operates in the image domain to unfold aliased images using known coil sensitivity maps [44] [42]. The acceleration factor in PI is ultimately limited by the number of coils and the geometry of the coil array, with higher factors leading to noise amplification and a reduction in the signal-to-noise ratio (SNR).
Compressed Sensing (CS) theory leverages the inherent sparsity of MR images in a transform domain (e.g., wavelet or temporal Fourier). It allows for the reconstruction of images from highly undersampled, pseudo-random k-space acquisitions that generate incoherent aliasing artifacts, which appear as noise. A non-linear, iterative reconstruction is then used to enforce both data consistency and sparsity in the chosen transform domain [42] [45]. CS does not require coil sensitivity maps and its acceleration potential is governed by the image's sparsity.
AI-Assisted/Deep Learning Reconstruction represents the latest evolution. These methods use deep neural networks, often trained on vast datasets of fully-sampled images, to learn the mapping from undersampled k-space or aliased images to high-quality reconstructions. AI can be used as a standalone reconstructor or integrated within traditional CS and PI frameworks to improve their performance and speed [46] [43].
Quantitative Performance Comparison
The following tables summarize key performance characteristics and experimental data from cited studies comparing these acceleration techniques.
Table 1: Technical and Performance Characteristics of Acceleration Techniques
| Feature | Parallel Imaging (e.g., GRAPPA) | Compressed Sensing (CS) | AI-Assisted Compressed Sensing |
|---|---|---|---|
| Underlying Principle | Spatial sensitivity of receiver coils [42] | Sparsity & incoherent undersampling [42] | Learned mapping from undersampled to full data [43] |
| Primary Domain | k-space (GRAPPA) or Image domain (SENSE) [42] | Transform domain (e.g., Wavelet) [42] | Image and/or k-space domain [43] |
| Key Limitation | Noise amplification, g-factor penalty [47] | Limited by sparsity; iterative reconstruction can be slow [45] | Generalizability; requires large training datasets [46] |
| Typical Acceleration Factor | 2-3 [48] | 5-8 and higher [48] [45] | 10+ [43] |
| Impact on SNR | Decreases with acceleration factor [47] | Better preserved at moderate acceleration [47] | Can improve or better preserve SNR [43] |
| Reconstruction Speed | Very fast | Slower (iterative) | Fast after initial training [43] |
Table 2: Experimental Data from Comparative Studies
| Study & Modality | Comparison | Key Quantitative Findings | Clinical/Qualitative Findings |
|---|---|---|---|
| 4D Flow MRI (Phantom) [48] | GRAPPA (R=2,3,4) vs. CS (R=7.6) vs. Fully Sampled | Good agreement for flow rates; trend to overestimate peak velocities vs. CFD. CS (R=7.6) scan time: ~5.5 min. | All sequences showed artifacts inherent to PC-MRI; eddy-current correction was crucial. |
| Brain & Pelvic MRI (Patient) [47] | CS vs. CAIPIRINHA (PI) | CS provided significantly higher SNR (e.g., 7% signal gain for T1) [47]. | CS-T1 was qualitatively superior; CS-T2-FLAIR was equivalent; pelvic T2 was equivalent. |
| Nasopharyngeal Carcinoma MRI [43] | AI-CS vs. PI | ACS exam time significantly shorter (p<0.0001). SNR and CNR significantly higher with ACS (p<0.005). | Lesion detection, margin sharpness, and overall quality were higher for ACS (p<0.0001). |
| Cardiac Perfusion MRI [45] | k-t SPARSE-SENSE (CS+PI) vs. GRAPPA | Combined CS+PI enabled 8-fold acceleration. | Combined method presented similar temporal fidelity and image quality to 2-fold GRAPPA. |
Experimental Protocols for Key Comparisons
To ensure the reliability of data used in comparative studies, rigorous experimental protocols are essential. The following methodologies are commonly employed in the field.
Phantom Validation Studies
Phantom studies provide a controlled environment for validating quantitative accuracy.
- Phantom Setup: A custom-made, MRI-compatible flow phantom with a pulsatile pump system is used to mimic physiological flow conditions, such as those found in the aorta. The fluid is designed to mimic the viscosity and relaxation times of blood [48] [44].
- Reference Standard: The flow rate from the pump is measured using an ultrasonic flowmeter, providing a ground truth for validation [48] [44]. For static phantoms (e.g., Magphan), known geometrical patterns and contrast inserts serve as the reference [47].
- Data Acquisition: Multiple accelerated sequences (e.g., GRAPPA with R=2,3,4 and CS with high acceleration factors) are run on the same phantom setup. A fully sampled, non-accelerated acquisition is often performed as an internal reference [48].
- Data Analysis: Voxel-wise comparisons (e.g., Bland-Altman analysis, L2-norm) are conducted for velocity fields in 4D flow. For structural imaging, quantitative metrics like SNR and CNR are calculated in specific regions of interest (ROIs) and compared to the reference standard [48] [47].
Patient Study Protocols
Patient studies assess clinical performance and diagnostic confidence.
- Population and Design: Prospective or retrospective studies with patients referred for a specific clinical indication (e.g., nasopharyngeal carcinoma or knee injury). Institutional review board approval and patient consent are obtained [43] [49].
- Scanning Protocol: Each patient undergoes scanning with both the accelerated protocol under investigation (e.g., AI-CS) and the conventional or reference protocol (e.g., PI) during the same session. The order of sequences is randomized to control for biases like contrast timing [47] [43].
- Image Analysis:
- Quantitative: SNR and CNR are measured by placing ROIs on lesions and background tissues [47] [43].
- Qualitative: Expert radiologists and clinicians, blinded to the reconstruction technique, rate the images on criteria such as lesion detection, sharpness, artifacts, and overall diagnostic confidence using Likert scales [47] [43].
- Reference Standard: For diagnostic performance, surgical findings (e.g., arthroscopy for knee studies) often serve as the reference standard to calculate sensitivity and specificity [49].
Visualization of Principles and Workflows
Technical Principles and Data Flow
The following diagram illustrates the fundamental operational differences and data flow between Parallel Imaging and Compressed Sensing.
Figure 1. Comparison of fundamental workflows for Parallel Imaging (PI) and Compressed Sensing (CS). PI relies on coil sensitivity maps to reconstruct images, while CS uses iterative algorithms to enforce sparsity and data consistency.
Experimental Validation Workflow
A standard methodology for validating accelerated sequences, particularly in phantom studies, is outlined below.
Figure 2. Generic workflow for experimental validation of accelerated MRI sequences. The process begins with establishing a ground truth in a controlled phantom setup or with a reference standard in patients, followed by acquisition, reconstruction, and multi-faceted analysis.
The Scientist's Toolkit
This section details key reagents, tools, and software essential for conducting research in accelerated MRI sequence development and validation.
Table 3: Essential Research Tools for Accelerated MRI Studies
| Tool / Reagent | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| Flow Phantom | Physical Hardware | Provides a controlled, reproducible environment with known flow dynamics for quantitative validation [48] [44]. | Testing accuracy of 4D flow MRI sequences against computational fluid dynamics or ultrasonic flowmeter data [48]. |
| AI-Assisted Reconstruction Software (e.g., AiCE, ACS) | Software | Integrates deep learning models into the reconstruction pipeline to improve image quality from highly undersampled data [43]. | Reducing scan time for T2-weighted FSE brain sequences while maintaining or improving SNR and CNR [43]. |
| Imaging Phantom (e.g., Magphan) | Physical Hardware | Contains standardized structures and contrast inserts for evaluating geometric accuracy, resolution, and SNR [47]. | Comparing the SNR performance and artifact levels of different acceleration techniques across the field-of-view [47]. |
| k-t SPARSE-SENSE Framework | Algorithm/Software | Combines compressed sensing (sparsity in temporal Fourier domain) with parallel imaging (SENSE) for high acceleration in dynamic MRI [45]. | Enabling high-resolution, whole-heart coverage in first-pass cardiac perfusion imaging with 8-fold acceleration [45]. |
| Implicit Neural Representations (INR) | Algorithm/Software | Models continuous k-space signals, offering compatibility with arbitrary sampling patterns for efficient non-Cartesian reconstruction [50] [51]. | Patient-specific optimization for reconstructing undersampled non-Cartesian k-space data in abdominal imaging [51]. |
| 1,5-Diazecane-6,10-dione | 1,5-Diazecane-6,10-dione | High-Purity Research Chemical | 1,5-Diazecane-6,10-dione: A versatile macrocyclic precursor for chemical biology & drug discovery. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
| Propene-1-D1 | Propene-1-D1 | Deuterated Propene | | Propene-1-D1, a deuterium-labeled propene. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals |
The landscape of accelerated MRI is diverse, with Parallel Imaging and Compressed Sensing representing distinct yet complementary approaches. PI is a mature technology with predictable performance at low acceleration factors, while CS and, more notably, AI-driven methods push the boundaries of what is possible, achieving diagnostic-quality images at significantly higher acceleration factors.
For researchers assessing the reliability of brain imaging methods, the choice of acceleration technique involves careful consideration of trade-offs. PI may be sufficient for standard protocols where moderate acceleration is needed. In contrast, CS and AI-CS are preferable for advanced applications requiring high acceleration or improved image quality, such as in oncological imaging or detailed hemodynamic studies [48] [43]. The emerging trend of combining these techniques with machine learning, including innovative approaches like Implicit Neural Representations (INR), points toward a future where highly personalized, patient-specific rapid MRI becomes a clinical reality, thereby enhancing its utility in both diagnostic and drug development settings [50] [51].
The integration of structural magnetic resonance imaging (sMRI), diffusion tensor imaging (DTI), and quantitative MRI techniques represents a paradigm shift in neuroimaging, moving from subjective qualitative assessment to data-driven, quantitative brain analysis. This multimodal approach leverages the complementary strengths of each imaging modality to provide a comprehensive view of brain anatomy, connectivity, and microstructural organization. While sMRI offers detailed visualization of cortical and subcortical anatomy, DTI provides unique insights into white matter architecture and structural connectivity by measuring the directional dependence of water diffusion in neural tissues [52]. The quantitative parameters derived from these techniques serve as sensitive biomarkers for detecting subtle alterations in brain structure and integrity across various neurological conditions, from neurodegenerative diseases to brain tumors [53] [54].
The clinical and research value of multimodal integration lies in its ability to capture different aspects of brain organization within a unified framework. Structural MRI serves as the anatomical reference, providing metrics like cortical thickness and regional volumes, while DTI-derived parameters such as fractional anisotropy (FA) and mean diffusivity (MD) reflect white matter integrity and organization [52]. Advanced integration frameworks, particularly those incorporating deep learning and machine learning approaches, have demonstrated superior performance compared to single-modality analyses across various diagnostic and prognostic tasks in neurology and neurosurgery [55] [56]. This comparative guide examines the technical capabilities, experimental protocols, and performance metrics of integrated structural and DTI approaches against standalone alternatives, providing researchers and clinicians with evidence-based insights for method selection in brain imaging reliability assessment.
Technical Specifications and Imaging Parameters
Fundamental Principles of Structural MRI and DTI
Structural MRI techniques, particularly T1-weighted volumetric imaging, form the foundation of multimodal integration by providing high-resolution anatomical reference data. These sequences enable precise segmentation of brain tissue into gray matter, white matter, and cerebrospinal fluid based on signal intensity differences [53]. Common clinical protocols include magnetization-prepared rapid gradient-echo (MPRAGE) for Siemens scanners and spoiled gradient echo (SPGR) for General Electric systems, typically requiring 3-5 minutes acquisition time without intravenous contrast [53]. The quantitative output includes regional brain volumes, cortical thickness measurements, and whole-brain atrophy indices, which are compared against normative databases to determine statistical deviations.
Diffusion Tensor Imaging extends conventional diffusion-weighted imaging by modeling the directional dependence of water diffusion in biological tissues [52]. The technique employs a tensor model to characterize anisotropic diffusion, typically requiring diffusion-weighted images acquired along at least 6-30 non-collinear directions with b-values ranging from 700-1000 s/mm² (up to 3000 s/mm² for advanced models) [52] [54]. The fundamental quantitative parameters derived from DTI include fractional anisotropy, which reflects the degree of directional preference in water diffusion; mean diffusivity, representing the overall magnitude of diffusion; and axial/radial diffusivity, which provide directional specificity to white matter alterations [52]. The biological basis for these parameters stems from the fact that in organized white matter tracts, water diffuses more freely parallel to axon bundles than perpendicular to them, creating directional asymmetry that the tensor model quantifies [52].
Table 1: Core Technical Parameters of Structural MRI and DTI
| Parameter | Structural MRI | Diffusion Tensor Imaging (DTI) |
|---|---|---|
| Primary Contrast | Tissue T1/T2 relaxation times | Directional water diffusion |
| Key Quantitative Metrics | Regional volumes, cortical thickness | Fractional anisotropy (FA), mean diffusivity (MD) |
| Acquisition Time | 3-5 minutes (volumetric) | 5-10 minutes (30 directions) |
| Spatial Resolution | 0.8-1mm isotropic | 2-2.5mm isotropic |
| Main Clinical Applications | Neurodegenerative disease monitoring, surgical planning | White matter mapping, tractography, microstructural assessment |
| Key Limitations | Insensitive to microstructural changes | Limited by complex fiber crossings, sensitivity to motion |
Advanced Integration Frameworks
Multimodal integration strategies have evolved from simple visual correlation to sophisticated computational frameworks that combine imaging features across spatial and temporal dimensions. Early integration approaches relied on feature concatenation or statistical fusion, but contemporary methods leverage deep learning architectures specifically designed for cross-modal analysis [55] [56]. Transformer-3D CNN hybrid models with cross-modal attention mechanisms have demonstrated particular efficacy, achieving segmentation accuracy of Dice coefficient 0.92 in glioma analysis [55]. Graph neural networks (GNNs) provide another powerful framework, structuring multimodal data within unified graph representations where nodes represent brain regions and edges encode structural or functional connections [57]. These frameworks employ masking strategies to differentially weight neural connections, facilitating meaningful integration of disparate imaging data while preserving network topology [57].
The integration process typically involves several standardized steps: image preprocessing and quality control, registration to common anatomical space, feature extraction from each modality, cross-modal feature fusion using specialized algorithms, and finally, model training for specific predictive or classification tasks [55] [56]. Attention mechanisms have proven particularly valuable in these pipelines, enabling models to dynamically prioritize diagnostically relevant features across modalities and providing intrinsic interpretability to the integration process [56]. As these frameworks continue to mature, they increasingly incorporate biological constraints and neuroanatomical priors to ensure that the integrated models reflect plausible neurobiological mechanisms rather than purely statistical associations.
Comparative Performance Analysis
Diagnostic Accuracy in Neuro-Oncology
In neuro-oncology, the combination of structural MRI and DTI has demonstrated superior performance for predicting molecular markers in gliomas compared to either modality alone. A comprehensive study evaluating IDH mutation status in CNS WHO grade 2-4 glioma patients found that combined structural and DTI features achieved an area under the curve (AUC) of 0.846, significantly outperforming standalone structural MRI (AUC = 0.72) or DTI alone [54]. Similarly, for predicting MGMT promoter methylation status in diffuse gliomas, integrated structural MRI with dynamic contrast-enhanced (DCE) and DTI features achieved an AUC of 0.868 on test datasets, surpassing the diagnostic performance of two radiologists with 1 and 5 years of experience, respectively [58]. The quantitative improvement with multimodal integration was consistent across metrics, with sensitivity improvements of 15-20% over single-modality approaches while maintaining specificity.
Deep learning frameworks further enhance these diagnostic capabilities. A CNN-SVM differentiable model incorporating both DTI and structural images achieved a 23% improvement in IDH mutation prediction (AUC = 0.89) compared to conventional radiomics approaches (DeLong test, p < 0.001) [55]. This performance advantage extends to clinical translation, with multimodal models predicting glioma recurrence 3-6 months earlier than conventional imaging and tracing metastatic brain tumor primary lesions with 87.5% accuracy [55]. The integration of demographic data, particularly patient age, with multimodal imaging features provides additional diagnostic value, further enhancing model specificity from 0.567 to 0.617 without compromising sensitivity [54].
Table 2: Performance Comparison in Neuro-Oncology Applications
| Application | Modality Combination | Performance Metrics | Comparison to Single Modality |
|---|---|---|---|
| IDH Mutation Prediction | Structural MRI + DTI | AUC: 0.846-0.89 [54] [55] | 23% improvement over structural MRI alone [55] |
| MGMT Promoter Methylation | Structural MRI + DCE + DTI | AUC: 0.868 [58] | Outperformed radiologist assessment |
| Glioma Segmentation | T2-FLAIR + DSC-PWI + DTI | Dice: 0.91 [55] | 9% improvement over single modality |
| Glioma Recurrence Prediction | Multimodal MRI + DL | 3-6 months earlier detection [55] | Clinical lead time advantage |
Applications in Neurodegenerative and Neuroinflammatory Disorders
Multimodal integration of structural and diffusion imaging has demonstrated particular value in characterizing neurodegenerative and neuroinflammatory conditions, where microstructural alterations often precede macroscopic atrophy. In Alzheimer's disease, combined structural parameters ( hippocampal volume, cortical thickness) with DTI metrics of white matter integrity improve classification accuracy between healthy controls, mild cognitive impairment, and Alzheimer's dementia by 12-15% compared to structural measures alone [59] [53]. The integration also enables more precise tracking of disease progression, with multimodal models identifying atrophic patterns in subcortical structures and white matter tracts that are not apparent on structural imaging alone [53].
For optic neuritis, a common manifestation of neuroinflammatory conditions like multiple sclerosis, the combination of structural MRI, DTI of the optic nerves, and optical coherence tomography (OCT) provides comprehensive assessment of anterior visual pathway integrity [60]. DTI parameters such as fractional anisotropy reduction in the optic radiations correlate strongly with retinal nerve fiber layer thinning measured by OCT (r = 0.62, p < 0.001), enabling more accurate prediction of visual recovery and relapse risk [60]. In Parkinson's disease, integrated T1 and T2 structural MRI with diffusion imaging using a dual interaction network achieved diagnostic accuracy of 93.11% for early diagnosis and 89.85% for established disease, significantly outperforming single-modality approaches [61].
The predictive value of multimodal integration extends to pre-symptomatic disease detection. A machine learning model combining structural MRI parameters with accelerometry data from wearable devices achieved an AUC of 0.819 for predicting incident neurodegenerative diseases in the UK Biobank cohort, substantially outperforming models using either data type alone (AUC = 0.688 without MRI) [59]. Feature importance analysis revealed that 18 of the 20 most predictive features were structural MRI parameters, highlighting their central role in multimodal predictive frameworks [59].
Experimental Protocols and Methodologies
Standardized Acquisition Protocols
Reproducible multimodal integration requires strict standardization of image acquisition parameters across modalities and scanning sessions. For structural MRI, high-resolution 3D T1-weighted sequences are essential, with recommended parameters including: repetition time (TR) = 510-600 ms, echo time (TE) = 30-37 ms, flip angle = 10°, isotropic voxel size = 1mm³, matrix size = 256×256, and field of view (FOV) = 256×232 mm² [58] [53]. Consistent positioning and head immobilization are critical to minimize motion artifacts, with scan times typically ranging from 3-5 minutes depending on specific sequence optimization.
DTI acquisition requires single-shot spin-echo echo-planar imaging sequences with parameters optimized for diffusion weighting: TR = 7600-9400 ms, TE = 70-84 ms, b-values = 1000-3000 s/mm², 30 diffusion encoding directions, FOV = 236×236 mm², matrix size = 128×128, and slice thickness = 2-2.5mm [54] [52]. The b-value selection represents a balance between diffusion contrast and signal-to-noise ratio, with higher b-values providing better diffusion weighting but reduced signal. For clinical applications, b-values of 1000 s/mm² are standard, while research protocols often employ multi-shell acquisitions with b-values up to 3000 s/mm² to enable more complex microstructural modeling [52]. The total acquisition time for a comprehensive multimodal protocol including structural MRI, DTI, and optional functional sequences typically ranges from 25-35 minutes [54].
Cross-scanner harmonization presents significant challenges in multicenter studies, with phantom studies demonstrating up to 30% T2 signal intensity variance between 1.5T and 3T scanners from different manufacturers [55]. Implementation of N4 bias field correction combined with histogram matching reduces interscanner intensity discrepancies to <5%, while motion compensation neural networks (MoCo-Net) achieve submillimeter registration accuracy (0.4 mm error) [55]. These preprocessing steps are essential for ensuring that quantitative parameters derived from different scanners can be meaningfully compared and integrated.
Data Processing and Feature Extraction Workflows
Processing pipelines for multimodal integration follow a structured workflow beginning with quality control and preprocessing, followed by feature extraction, and culminating in integrated analysis. For structural MRI, processing typically includes noise reduction, intensity inhomogeneity correction, brain extraction, and tissue segmentation into gray matter, white matter, and cerebrospinal fluid [53]. Volumetric quantification then employs atlas-based parcellation to compute regional volumes and cortical thickness measurements, which are compared against age- and sex-matched normative databases [53].
DTI processing involves more complex computational steps, beginning with correction for eddy currents and head motion, followed by tensor estimation to derive voxel-wise maps of fractional anisotropy, mean diffusivity, axial diffusivity, and radial diffusivity [52]. Tractography algorithms then reconstruct white matter pathways based on the principal diffusion directions, enabling quantification of tract-specific metrics [52]. For radiomics analysis, feature extraction includes first-order statistics, shape-based features, and texture features derived from gray-level co-occurrence matrices and run-length matrices [58] [54]. In deep learning approaches, feature extraction is automated through convolutional neural networks, which learn discriminative patterns directly from the imaging data without requiring hand-crafted feature engineering [55].
The integration of structural and diffusion features occurs at multiple possible levels: early fusion (combining raw images), intermediate fusion (merging extracted features), or late fusion (combining model outputs) [56]. Cross-modal attention mechanisms have emerged as particularly effective for intermediate fusion, dynamically weighting the contribution of each modality based on diagnostic relevance [56]. Validation follows rigorous standards, with nested cross-validation to prevent overfitting and external testing on completely independent datasets to assess generalizability [55].
Diagram Title: Multimodal MRI Integration Workflow
Research Reagents and Computational Tools
Essential Research Solutions
The implementation of multimodal MRI integration requires both specialized software tools and computational resources. For structural MRI analysis, several FDA-cleared volumetric quantification packages are available, including NeuroQuant, NeuroReader, and IcoMetrix, which provide automated segmentation of brain structures and comparison to normative databases [53]. These tools typically employ atlas-based parcellation approaches and have demonstrated high diagnostic performance in neurodegenerative diseases, with effect sizes comparable to research-grade software like FreeSurfer and FSL [53].
DTI processing relies on specialized toolboxes such as FSL's FDT (FMRIB's Diffusion Toolbox), MRtrix3, or Dipy, which implement tensor estimation, eddy current correction, and tractography algorithms [52]. For advanced microstructural modeling beyond the tensor approach, tools like NODDI (Neurite Orientation Dispersion and Density Imaging) require multi-shell diffusion data and provide more biologically specific parameters like neurite density and orientation dispersion index [52]. These advanced models come with increased acquisition time requirements and computational complexity, limiting their current clinical translation.
Deep learning frameworks for multimodal integration predominantly utilize Python-based ecosystems with TensorFlow or PyTorch backends. Specific architectures that have demonstrated success in neuroimaging include 3D U-Net variants for segmentation, Transformer models with cross-modal attention mechanisms for feature fusion, and graph neural networks for connectome-based analysis [55] [56]. Implementation typically requires GPU acceleration, with recommended specifications including NVIDIA RTX 3080 or higher with at least 10GB VRAM for processing 3D medical images [55].
Table 3: Essential Research Tools for Multimodal MRI Integration
| Tool Category | Specific Solutions | Primary Function | Compatibility |
|---|---|---|---|
| Volumetric Analysis | NeuroQuant, NeuroReader, FreeSurfer | Automated brain structure segmentation | Clinical & Research |
| DTI Processing | FSL FDT, MRtrix3, Dipy | Tensor estimation, tractography | Primarily Research |
| Multimodal Fusion | 3D Transformer- CNN hybrids, Graph Neural Networks | Cross-modal feature integration | Research |
| Visualization | MRICloud, TrackVis, BrainNet Viewer | Results visualization and interpretation | Research |
The integration of structural MRI with DTI and quantitative imaging parameters represents a significant advancement in neuroimaging, providing more comprehensive characterization of brain structure and integrity than any single modality alone. The experimental evidence consistently demonstrates superior diagnostic and prognostic performance across neurological disorders, with quantitative improvements in accuracy metrics ranging from 15-23% compared to single-modality approaches [58] [54] [55]. This performance advantage, coupled with the biological plausibility of combined macrostructural and microstructural assessment, positions multimodal integration as the emerging standard for advanced neuroimaging applications in both clinical and research settings.
Future developments in multimodal integration will likely focus on several key areas: (1) standardization of acquisition protocols and processing pipelines to improve reproducibility across centers [55]; (2) development of more sophisticated integration algorithms, particularly cross-modal attention mechanisms and graph-based fusion approaches [57] [56]; (3) incorporation of additional modalities including functional MRI, quantitative susceptibility mapping, and molecular imaging to create even more comprehensive brain signatures [55]; and (4) implementation of federated learning approaches to enable model training across institutions while preserving data privacy [55]. As these technical advances mature, the primary challenge will shift from methodological development to clinical translation, requiring robust validation in real-world settings and demonstration of cost-effectiveness for routine healthcare implementation.
For researchers and clinicians selecting imaging approaches, the evidence strongly supports multimodal integration for applications requiring high sensitivity to microstructural changes, early disease detection, or comprehensive characterization of complex neurological conditions. While single-modality approaches remain valuable for specific clinical questions and resource-limited settings, the progressive validation and standardization of integrated frameworks suggest they will increasingly define the future of quantitative neuroimaging.
The reliability of brain imaging data is a fundamental prerequisite for valid neuroscience research and clinical drug development. Magnetic Resonance Imaging (MRI), particularly structural T1-weighted and diffusion MRI (dMRI), serves as a cornerstone for analyzing brain structure and pathological changes, especially in neurodegenerative diseases and oncology [62] [63]. However, the derived diagnostic and research measurements can be significantly compromised by artifacts from multiple sources, including patient motion, physiological processes, and technical scanner issues [64] [65]. These artifacts introduce uncontrolled variability, confound experimental observations, and ultimately reduce the statistical power of studies [65].
Traditional reliance on manual quality control presents major limitations for modern large-scale studies. Visual inspection is inherently subjective, time-consuming, and impractical for datasets comprising hundreds or thousands of scans with multiple tissue contrasts and sub-millimeter resolution [63] [66]. This challenge has driven the development of automated quality assessment (AQA) methods that provide consistent, quantitative, and scalable evaluation of brain imaging data [64]. These automated tools are particularly vital in multi-center clinical trials—common in drug development—where consistency across different scanners and sites is essential for generating reliable, comparable results [63].
Key Artifacts in Brain Imaging and Detection Methodologies
Classification and Impact of Common Artifacts
Artifacts in brain imaging can be broadly categorized as physiological (originating from the patient) and technical (originating from equipment or environment). The table below summarizes the primary artifacts, their characteristics, and detection methodologies.
Table 1: Key Artifacts in Brain MRI and Their Automated Detection
| Artifact Category | Specific Artifact | Manifestation in MRI/dMRI | Primary Detection Methods |
|---|---|---|---|
| Physiological | Bulk Motion | Blurring, ghosting in 3D structural MRI; misalignment in dMRI volumes [64] [67] | Air background analysis [64]; 3D CNN classifiers [67] |
| Physiological | Cardiac Pulse | Rhythmical spike artifacts, often near mastoids/arteries [65] | ICA with ECG recording; average referencing [65] |
| Physiological | Eye Blink/Movement | High-amplitude deflections in frontal/temporal regions [65] | ICA; regression-based subtraction [65] |
| Physiological | Muscular (clenching, neck tension) | High-frequency noise overlapping EEG spectrum; affects mastoids [65] | ICA; artifact rejection; filtering [65] |
| Technical | Incomplete Spoiling / Eddy Currents | Signal inhomogeneity, distortions in dMRI [64] [67] | Air background analysis [64]; 3D Residual SE-CNN [67] |
| Technical | Low Signal-to-Noise Ratio (SNR) | Poor tissue contrast-to-noise, graininess [67] | 3D Residual SE-CNN [67] |
| Technical | Line Noise / EMI | 50/60 Hz interference and harmonics [65] | Notch filters; spectral analysis [65] |
| Technical | Gibbs Ringing & Gradient Distortions | Ringing artifacts at tissue boundaries; geometric distortions [67] | 3D Residual SE-CNN [67] |
Experimental Protocols for Artifact Detection
Automated artifact detection relies on sophisticated image analysis and machine learning protocols. Below are detailed methodologies for two key approaches cited in the literature.
Protocol 1: Multi-modality Semi-Automatic Segmentation with ITK-SNAP This protocol, used for segmenting structures like brain tumors from multiple MRI contrasts (e.g., T1-w, T2-w, FLAIR), employs a two-stage pipeline within ITK-SNAP [66].
Stage 1: Speed Image Generation via Random Forest Classification
- User Interaction: The expert loads all available imaging modalities and uses paintbrush or polygon tools to place examples (brushstrokes) of different tissue classes (e.g., tumor, healthy tissue, edema).
- Feature Extraction: For each labeled voxel, a feature vector is generated. Features include intensity from each modality, and optionally, intensities of neighboring voxels (for texture) and spatial coordinates.
- Classifier Training & Application: A Random Forest classifier is trained on the labeled feature vectors. The classifier is then applied to all voxels in the image domain to generate a posterior probability map for each class.
- Speed Function: The user defines which classes constitute the foreground (S) and background (Ω\S). The scalar speed image ( g(x) ) is computed as ( g(x) = P(x \in S) - P(x \in \Omega \backslash S) ).
Stage 2: Active Contour Segmentation
- Initialization: The user places one or more spherical seeds within the structure of interest.
- Contour Evolution: A parametric contour ( C ), initialized by the seeds, evolves over time ( t ) according to the level set equation:
∂C/∂t = [g(C) + ακC]NCwhere ( κC ) is contour curvature, ( NC ) is the unit normal, and ( α ) is a user-controlled smoothness parameter. The contour expands where ( g(x) ) is positive and contracts where it is negative. - Visualization & Iteration: The evolving contour is visualized in 2D and 3D in real-time, allowing the user to stop, adjust parameters, or reinitialize as needed [66].
Protocol 2: Automated Multiclass dMRI Artifact Detection using 3D CNNs This protocol describes a deep learning framework for classifying entire dMRI volumes by their dominant artifact type [67].
Step 1: Data Preparation and Slab Extraction
- Poor-quality dMRI volumes are identified and labeled with a primary artifact class (e.g., Motion, Low SNR, Out-of-FOV, Miscellaneous).
- Due to GPU memory constraints, each 3D dMRI volume is partitioned into smaller, mutually exclusive collectively exhaustive (MECE) 3D sub-volumes or "slabs."
Step 2: Slab-Level Classification with Residual SE-CNN
- A custom 3D Convolutional Neural Network (CNN) is designed, built upon residual blocks equipped with Squeeze-and-Excitation (SE) components.
- The SE block is a self-attention unit that models interdependencies between feature channels. It uses global average pooling and fully connected layers to learn channel-wise importance weights, which are then used to recalibrate the feature tensor, helping the network focus on the most relevant features for artifact identification.
- The network is trained to predict the artifact class for each individual 3D slab.
Step 3: Volume-Level Prediction via Voting
- The predicted labels for all slabs from a single dMRI volume are aggregated.
- The final artifact classification for the whole volume is determined by a majority vote among its constituent slabs, making the prediction robust to slab-level misclassifications [67].
Comparative Analysis of Automated Quality Assessment Tools
Performance Benchmarking of QC Tools
The performance of AQA tools is critical for their adoption in research and clinical pipelines. The following table synthesizes experimental performance data from validation studies.
Table 2: Performance Comparison of Automated Quality Assessment Tools
| Tool / Framework | Imaging Modality | Primary Function | Reported Performance | Reference Dataset |
|---|---|---|---|---|
| Proposed RUS Classifier | T1-weighted MRI | Accept/Reject Classification | 87.7% Balanced Accuracy [63] | Multi-site clinical dataset (N=2438) |
| MRIQC | T1-weighted MRI | Accept/Reject Classification | Kappa=0.30 (Agreement with visual QC) [63] | Multi-site clinical dataset (N=2438) |
| CAT12 | T1-weighted MRI | Accept/Reject Classification | Kappa=0.28 (Agreement with visual QC) [63] | Multi-site clinical dataset (N=2438) |
| 3D Residual SE-CNN | Diffusion MRI (dMRI) | Multiclass Artifact Identification | 96.61% - 97.52% Average Accuracy [67] | ABCD & HBN datasets (N>6,700) |
| Original AQA Method | 3D Structural MRI (T1/T2) | Accept/Reject Classification | >85% Sensitivity & Specificity [64] | ADNI (749 scans, 36 sites) |
Tool Functionality and Applicability
Different tools are designed with specific use cases, modalities, and technical approaches in mind.
Table 3: Functional Comparison of Quality Control and Segmentation Tools
| Feature | ITK-SNAP | MRIQC | 3D Residual SE-CNN | BrainVision Analyzer 2 |
|---|---|---|---|---|
| Primary Function | Interactive Segmentation | Automated Quality Control | Automated Artifact Classification | EEG Artifact Handling |
| Modality | 3D MRI, CT | Structural MRI | Diffusion MRI (dMRI) | EEG |
| Automation Level | Semi-Automatic | Fully Automatic | Fully Automatic | Semi-Automatic |
| Key Strength | Multi-modality fusion with user guidance [66] | Standardized feature extraction for large datasets [63] | High-accuracy multiclass artifact identification [67] | Comprehensive toolbox for physiological artifacts [65] |
Visualizing Workflows and System Architectures
Workflow for Multiclass dMRI Artifact Detection
The following diagram illustrates the two-step protocol for automated dMRI artifact classification, from slab extraction to the final volume-level prediction [67].
ITK-SNAP Semi-Automatic Segmentation Pipeline
The diagram below outlines the interactive semi-automatic segmentation workflow used in ITK-SNAP for leveraging multi-modality data [66].
Successful implementation of automated quality assessment relies on a suite of software tools, datasets, and computational resources.
Table 4: Key Reagents and Resources for Automated Quality Assessment Research
| Resource Name | Type | Primary Function / Application | Key Features / Notes |
|---|---|---|---|
| ITK-SNAP | Software Tool | 3D Medical Image Navigation and Semi-Automatic Segmentation [68] [66] | Open-source (GPL); supports multi-modality data via Random Forests; intuitive interface [66] |
| MRIQC | Automated Pipeline | Quality Control for Structural T1-weighted MRI [63] | Extracts quantitative quality metrics (e.g., from air background); enables batch processing [64] [63] |
| Adolescent Brain Cognitive Development (ABCD) | Dataset | Training/Validation Data for dMRI Artifact Detector [67] | Large-scale, publicly available dataset; contains labeled poor-quality dMRI volumes |
| 3D Residual SE-CNN | Deep Learning Model | Multiclass Artifact Detection in dMRI Volumes [67] | Employs squeeze-and-excitation blocks for channel attention; uses slab-level voting for robustness |
| Alzheimer's Disease Neuroimaging Initiative (ADNI) | Dataset | Benchmarking Structural MRI QC Algorithms [64] | Multi-site, multi-scanner dataset with variable image quality; provides reference standard ratings |
| BrainVision Analyzer 2 | Software Tool | EEG Artifact Handling and Preprocessing [65] | Offers tools like ICA and regression for removing physiological artifacts (blinks, muscle noise) |
Optimizing Reliability: Identifying and Mitigating Technical Error Sources
In vivo brain imaging techniques are increasingly "quantitative," providing measurements on a ratio scale intended to be objective and reproducible. In this context, recognizing and controlling for artifacts through rigorous quality assurance (QA) becomes fundamental for both research and clinical applications [69]. Physical test objects known as "phantoms" have emerged as indispensable tools for evaluating, calibrating, and optimizing medical imaging devices such as MRI and CT scanners. These specialized tools are physical models that mimic human tissues and organs, allowing technicians and radiologists to ensure their equipment produces accurate and consistent images [70]. The reliability of data extracted from quantitative imaging is crucial for longitudinal studies tracking neurodegenerative disease progression, multi-centre clinical trials, and drug development research where detecting subtle biological changes is paramount [69] [71]. Without consistent calibration and quality control using standardized phantoms, apparent changes in brain structure or function between scans could reflect scanner drift or performance variation rather than true biological phenomena.
Phantom Types and Their Applications
Imaging test phantoms come in various forms tailored to specific imaging modalities and clinical needs. They contain materials that simulate the physical properties of human tissues, such as density, elasticity, and electrical conductivity [70]. This simulation enables precise testing of imaging parameters, resolution, contrast, and spatial accuracy.
CT Phantoms for Multi-Energy Applications
Modern CT phantoms are designed for sophisticated applications, including multi-energy (spectral) CT imaging. The Spectral CT Phantom (QRM-10147), for instance, is a 100mm diameter cylinder containing 8 holes to house different solid rods and fillable tubes [72]. Its key features include:
- Tissue-equivalent materials: Contains inserts simulating ICRU Adipose, Muscle, Lung, and Liver tissues based on standardized reports [72]
- Quantification inserts: Includes four different solid Iodine rods (2, 5, 10, and 15 mg I/cm³) and four Ca-Hydroxyapatite rods (100, 200, 400, and 800 mg CaHA/cm³) for bone mineral quantification [72]
- Modular design: Can be used with extension rings (160mm or 320mm diameter) or combined with thorax and abdomen phantoms for more realistic calibration scenarios [72]
Another option for multi-energy CT QA is the PH-75A Phantom, constructed from "Aqua Slab" material that is equivalent to water across diagnostic energy levels (40-190 keV). It includes plug-in inserts containing iodine and other metals to assess Hounsfield Unit (HU) stability, image contrast, signal-to-noise ratio (SNR), and artifact presence across varying kVp settings [73].
MRI Phantoms for System Performance Evaluation
MRI phantoms are designed to evaluate critical performance parameters specific to magnetic resonance imaging. The American College of Radiology (ACR) MRI phantom is widely used for accreditation and quality assurance [74]. This hollow cylinder (148mm length, 190mm diameter) is filled with a solution containing 10 mM NiClâ‚‚ and 75 mM NaCl and includes internal structures for qualitative and quantitative analysis [74]. It enables assessment of:
- Geometric accuracy
- High-contrast spatial resolution
- Slice thickness and position accuracy
- Image intensity uniformity
- Percent signal ghosting
- Low-contrast object detectability
The PH-31 MRI Quality Assurance Phantom offers another approach, constructed from durable acrylic resin that maintains uniformity under high magnetic fields up to 3.0 Tesla. The set includes two phantom units and various contrast solutions with different concentrations [73].
Table 1: Comparison of Primary Phantom Types for Scanner Calibration
| Phantom Type | Primary Applications | Key Measured Parameters | Example Products |
|---|---|---|---|
| Spectral CT Phantom | Multi-energy CT calibration, material decomposition, quantification | Iodine/CaHA concentration accuracy, HU stability across energies, tissue equivalence | QRM Spectral CT Phantom II (QRM-10147), Kyoto Kagaku PH-75A [72] [73] |
| ACR MRI Phantom | MRI accreditation, routine quality assurance | Geometric accuracy, slice thickness, image uniformity, ghosting, low-contrast detectability | ACR MRI Phantom (standardized), PH-31 MRI Phantom [74] [73] |
| Research MRI Phantom | Advanced sequence validation, longitudinal study calibration | Signal-to-noise ratio, contrast-to-noise ratio, relaxation time stability | Custom fluid-filled phantoms, ADNI phantom [7] |
Experimental Protocols for Reliability Assessment
Well-designed experimental protocols are essential for meaningful reliability assessment using phantoms. These protocols vary based on the imaging modality and specific research questions.
Phantom Test Protocols for MRI Quality Assurance
The ACR phantom test protocol for MRI involves delicate positioning of the phantom at the center of the head coil, followed by acquisition of 11 axial images with a slice thickness of 5mm and an inter-slice gap of 5mm [74]. Key sequence parameters include:
- T1-weighted imaging: Spin echo sequence (TR/TE = 500/20 ms)
- T2-weighted imaging: Dual echo spin echo (TR/TE = 2000/20 ms for first echo, 2000/80 ms for second echo)
- In-plane resolution: 1 × 1 mm [74]
Following acquisition, quantitative analysis measures geometric accuracy, slice thickness accuracy, slice position accuracy, signal intensity uniformity, and percentage signal ghosting. Qualitative assessment evaluates high-contrast spatial resolution and low-contrast object detectability [74].
Test-Retest Study Designs for Reliability Assessment
For assessing the reliability of brain measurements in research contexts, specialized test-retest datasets have been developed. These typically employ carefully controlled scanning protocols:
- The ADNI (Alzheimer's Disease Neuroimaging Initiative) protocol is widely used for structural brain imaging, featuring accelerated sagittal 3D IR-SPGR with specific parameters: 27cm FOV, 256×256 matrix, 1.2mm slice thickness, TR=7.3ms, TE=3ms, TI=400ms, flip angle=11 degrees [7]
- Paired acquisition designs involve scanning participants twice within the same session with repositioning between scans, allowing separation of intra-session (repositioning, noise, segmentation errors) and inter-session (biological variation, scanner drift) variability [7]
- Long-term reliability assessments scan participants over extended intervals (e.g., 103-189 days) to evaluate stability of measurements over timeframes relevant to clinical trials [8]
Table 2: Quantitative Reliability Metrics from Brain Volume Test-Retest Studies
| Brain Structure | Coefficient of Variation (CV) | Intra-class Correlation (ICC) | Key Influencing Factors |
|---|---|---|---|
| Subcortical Volumes (e.g., caudate) | 1.6% (CV) [7] | 0.97-0.99 (cross-sectional), >0.97 (longitudinal pipeline) [71] | Head tilt, FreeSurfer version, processing pipeline |
| Cortical Volumes | Not reported | 0.97-0.99 (cross-sectional), >0.97 (longitudinal pipeline) [71] | Head tilt, FreeSurfer version |
| Cortical Thickness | Not reported | 0.82-0.87 (cross-sectional), >0.82 (longitudinal pipeline) [71] | Head tilt (most significant effect) |
| Lateral Ventricles | Shows significant inter-session variability (P<0.0001) [7] | Not reported | Biological factors (e.g., hydration) |
| fMRI Memory Encoding (MTL activity) | Not reported | ≤0.45 (poor to fair reliability) [75] | Stimulus type, brain region |
Quality Assessment Methodologies
Automated Quality Assessment for Structural MRI
Beyond phantom-based quality assurance, automated methods have been developed for assessing image quality in human structural MRI scans. These techniques typically analyze the background (air) region of the image to detect artifacts, as artifactual signal intensity often propagates into the background and corrupts the expected noise distribution [76]. The methodology involves:
- Background region segmentation: Establishing the scalp/air boundary using image gradient computation and atlas-based refinement to focus on regions above the cerebellum [76]
- Artifactual voxel detection (QI1): Applying intensity thresholding and morphological operations to identify clusters of voxels with artifactual signal, then calculating the proportion of artifactual voxels normalized by background size [76]
- Noise distribution analysis (QI2): Fitting a expected noise distribution model (e.g., Rician or non-central chi depending on coil elements) to the background intensity distribution and evaluating goodness-of-fit [76]
When validated against expert quality ratings, these automated quality indices can achieve high sensitivity and specificity (>85%) in differentiating low-quality from high-quality scans [76].
Factors Affecting Measurement Reliability
Several studies have systematically examined factors influencing the reliability of structural brain measurements:
- Head tilt has the most significant adverse effect on reliability, particularly for cortical thickness measurements (reducing mean right cortical thickness ICC to 0.74) [71]
- FreeSurfer version and processing stream: Updated FreeSurfer versions demonstrate increased reliability, with the longitudinal pipeline consistently outperforming the cross-sectional pipeline [71]
- Scanner and sequence changes: Interestingly, changes in MRI scanner (same model) or ADNI sequence (ADNI-2 vs. ADNI-3) have minimal effects on reliability compared to head position [71]
- Inter-scan interval: Both short-term (3 weeks) and long-term (1 year) intervals maintain high reliability for volume measurements when using appropriate processing streams [71]
The Researcher's Toolkit: Essential Materials and Reagents
Table 3: Key Research Reagent Solutions for Imaging Quality Assurance
| Item | Function | Example Specifications |
|---|---|---|
| ACR MRI Phantom | Standardized quality assurance for clinical MRI scanners | Hollow cylinder filled with 10mM NiClâ‚‚ + 75mM NaCl solution; includes internal structures for comprehensive quality assessment [74] |
| Spectral CT Phantom Inserts | Calibration of multi-energy CT quantification | Solid iodine rods (2, 5, 10, 15 mg I/cm³); CaHA rods (100, 200, 400, 800 mg CaHA/cm³); tissue-equivalent rods (adipose, muscle, lung, liver) [72] |
| NiCl Contrast Solutions | Variation of contrast and relaxation properties in MRI phantoms | Various concentrations (5-25 mmol) for tuning T1 and T2 relaxation times [73] |
| Fillable Rods/Tubes | Custom material testing in phantom setups | Ø20mm tubes for water, contrast media, or experimental materials [72] |
| Extension Rings | Simulation of different patient sizes in CT | Various diameters (160mm, 320mm) to simulate different anatomical regions and body habitus [72] |
| N,N-dimethyl-3-phenylpropan-1-amine | N,N-dimethyl-3-phenylpropan-1-amine | High-Purity Reagent | N,N-dimethyl-3-phenylpropan-1-amine for research. A key phenylpropanamine derivative for neuroscience & chemistry. For Research Use Only. Not for human consumption. |
| 3,3',4,4',5,5'-Hexachlorobiphenyl | 3,3',4,4',5,5'-Hexachlorobiphenyl (PCB 169)|High-Purity Reference Standard | High-purity 3,3',4,4',5,5'-Hexachlorobiphenyl (PCB 169), a coplanar PCB and potent AhR agonist. For Research Use Only. Not for human or veterinary use. |
Workflow for Comprehensive Quality Assurance
The following diagram illustrates a systematic workflow for implementing phantom-based quality assurance in a research or clinical setting:
Phantom protocols form the foundation of reliable quantitative brain imaging in both clinical and research settings. The comprehensive comparison presented in this guide demonstrates that different phantom types serve distinct but complementary roles in quality assurance programs. Current trends indicate development of more sophisticated, tissue-specific phantoms that can simulate complex biological structures, along with integration with digital and AI-driven analysis tools to enhance calibration precision and workflow efficiency [70].
For researchers designing brain imaging studies, particularly longitudinal clinical trials, the reliability data presented here provides crucial guidance for protocol optimization. Key recommendations include:
- Implementing the ACR phantom test regularly to monitor scanner performance [74]
- Using the longitudinal FreeSurfer processing stream for improved reliability of structural measurements [71]
- Controlling for head tilt during scanning to minimize variability in cortical thickness measurements [71]
- Selecting appropriate phantoms based on specific research goals, whether for routine quality assurance (ACR phantom) or specialized spectral CT calibration (Spectral CT Phantom) [72] [74]
As quantitative brain imaging continues to evolve, phantom technologies and reliability assessment methodologies will play an increasingly critical role in ensuring that reported findings reflect true biological phenomena rather than technical variability.
Subject motion remains one of the most significant technical obstacles in magnetic resonance imaging (MRI) of the human brain, with head tilt and movement during scanning inducing artifacts that compromise image quality and quantitative analysis [77]. These motion-induced artifacts present as blurring, ghosting, and signal alterations that systematically bias neuroanatomical measurements, potentially mimicking cortical atrophy or other pathological changes [78] [77]. The reliability of automated segmentation tools varies considerably in handling these artifacts, creating a critical need for systematic comparison across processing methodologies. This review objectively evaluates the performance of leading neuroimaging segmentation pipelines under varying motion conditions, providing experimental data to guide researchers in selecting appropriate analytical tools for motion-corrupted data, particularly within clinical trials and drug development contexts where accurate volumetric assessment is paramount.
Experimental Protocols for Motion Artifact Assessment
Head Motion Induction and Image Quality Rating
To quantitatively evaluate the impact of motion on segmentation reliability, researchers have developed standardized protocols for inducing and rating motion artifacts. One prominent methodology involves collecting T1-weighted structural MRI scans from participants under both rest and active head motion conditions [78]. In this paradigm, subjects are instructed via visual cues to perform specific head movements during image acquisition:
- Still Condition: Subjects remain motionless throughout scanning.
- 5-Nod Condition: Subjects nod their heads approximately 5 times during acquisition.
- 10-Nod Condition: Subjects nod their heads approximately 10 times during acquisition.
A "nod" is defined as tilting the head up along the sagittal plane (pitch rotation) and returning to the original position [79]. The resulting images are then evaluated by multiple radiologists who blind rate image quality into categorical classifications of clinically good, medium, or bad based on the severity of visible motion artifacts [78].
Segmentation Performance Evaluation
Performance comparison across segmentation methods typically employs a standardized evaluation framework:
- Ground Truth Establishment: High-quality, motion-free images segmented with established tools (e.g., FreeSurfer) serve as reference standards.
- Consistency Metric Calculation: Segmentation consistency across motion conditions is quantified using overlap metrics (Dice-Sørensen Coefficient) and volume similarity measures.
- Statistical Comparison: Statistical tests compare segmentation reliability between traditional and deep learning methods across image quality categories.
Figure 1: Experimental workflow for evaluating motion artifact impact on brain segmentation.
Quantitative Comparison of Segmentation Tools Under Motion Conditions
Test-Retest Reliability Across Motion Severity
Table 1: Segmentation consistency across image quality levels
| Segmentation Method | Good Quality Consistency | Medium Quality Consistency | Bad Quality Consistency | Processing Speed |
|---|---|---|---|---|
| FreeSurfer | Baseline | Significant decrease | Severe degradation | Hours (~7-15) |
| FastSurferCNN | Higher than FreeSurfer [78] | More consistent than FreeSurfer [78] | More reliable than FreeSurfer [78] | ~1 minute [78] |
| Kwyk | Comparable to FastSurferCNN [78] | Comparable to FastSurferCNN [78] | Comparable to FastSurferCNN [78] | Minutes [78] |
| ReSeg | Comparable to FastSurferCNN [78] | Comparable to FastSurferCNN [78] | Comparable to FastSurferCNN [78] | Minutes [78] |
| SynthSeg+ | High robustness [79] | Maintains performance [79] | Most robust to motion [79] | Fast [79] |
Deep learning-based methods demonstrate superior consistency across all image quality levels compared to traditional pipelines like FreeSurfer, while offering dramatically faster processing times [78]. Notably, SynthSeg+ shows particularly high robustness to all forms of motion in comparative studies [79].
Segmentation Accuracy Under Controlled Motion
Table 2: Dice similarity coefficient under simulated motion conditions
| Segmentation Tool | No Motion (DSC) | 5 Nods (DSC) | 10 Nods (DSC) | Change with Severe Motion |
|---|---|---|---|---|
| FreeSurfer | 0.89 | 0.79 | 0.68 | -23.6% |
| BrainSuite | 0.87 | 0.81 | 0.72 | -17.2% |
| ANTs | 0.86 | 0.80 | 0.71 | -17.4% |
| SAMSEG | 0.88 | 0.83 | 0.75 | -14.8% |
| FastSurfer | 0.90 | 0.85 | 0.78 | -13.3% |
| SynthSeg+ | 0.89 | 0.86 | 0.82 | -7.9% |
The Dice-Sørensen Coefficient (DSC) quantifies segmentation overlap accuracy, with SynthSeg+ demonstrating the smallest performance degradation under severe motion conditions (10 nods), highlighting its robustness for motion-corrupted data [79].
Motion Artifact Impact on Cortical Measurement
Systematic Bias in Neuroanatomical Measures
Head motion introduces systematic biases rather than random noise in neuroanatomical measurements. Studies demonstrate that motion artifacts cause reduced cortical thickness and gray matter volume estimates across multiple processing pipelines, with the effect magnitude varying by anatomical region [77] [80]. This bias mimics cortical atrophy patterns and represents a critical confound in longitudinal studies and clinical trials.
Even subtle motion below visual detection thresholds can significantly impact measurements. Research shows that higher motion levels, estimated via fMRI, correlate with decreased thickness and volume, while mean curvature increases [80]. This non-uniform effect across brain regions complicates motion correction strategies.
Population Differences in Motion Vulnerability
Table 3: Motion prevalence across clinical populations
| Population | Relative Motion Level | Impact on Structural Measures |
|---|---|---|
| Healthy Adults | Baseline | Minimal with cooperation |
| Children | Increased [81] [80] | Significant thickness underestimation |
| ADHD | Increased [81] [80] | Significant thickness underestimation |
| Autism Spectrum Disorder | Increased [80] | Significant thickness underestimation |
| Externalizing Disorders | Increased [81] | Significant thickness underestimation |
| Internalizing Disorders | Trend toward reduced motion [81] | Less impact on measures |
Motion artifacts disproportionately affect pediatric and neuropsychiatric populations, potentially confounding group differences in neuroanatomical studies [81] [80]. Studies controlling for motion find attenuated neuroanatomical effect sizes, suggesting previously reported differences may reflect motion artifacts rather than genuine biological differences.
Computational Approaches for Motion Resilience
Deep Learning Architectures for Motion-Robust Segmentation
Advanced deep learning models address motion artifacts through several innovative architectures:
- FastSurferCNN: Utilizes a synthetic axial-sagittal-coronal slicing approach with view-aggregation, processing adjacent slices to provide 3D context while working with 2D computational efficiency [78].
- Kwyk: Employs Bayesian fully convolutional networks trained on non-overlapping subvolumes with spike-and-slab dropout for uncertainty estimation in segmentation [78].
- ReSeg: Implements a two-stage pipeline with initial brain cropping followed by semantic segmentation, reducing computational requirements while maintaining accuracy [78].
- SynthSeg+: Leverages synthetic data training for exceptional robustness to motion artifacts and contrast variations without retraining [79].
Figure 2: Deep learning pipeline for motion-robust brain segmentation.
Motion Simulation for Data Augmentation
For training motion-resilient algorithms, researchers developed sophisticated motion simulation techniques applied to motion-free magnitude MRI data. The modified TorchIO framework incorporates motion parameters specific to acquisition protocols and phase encoding directions, generating realistic motion artifacts that closely match real motion-corrupted data in image quality metrics [79]. This approach enables the creation of large-scale augmented datasets for robust network training without requiring original k-space data.
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key resources for motion artifact research
| Resource | Type | Primary Function | Application Context |
|---|---|---|---|
| MR-ART Dataset [79] | Dataset | Provides matched motion-free and motion-corrupted (5/10 nods) structural MRI | Method validation and benchmarking |
| TorchIO [79] | Software Library | Medical image augmentation including motion simulation | Data augmentation for deep learning |
| FreeSurfer [78] | Software Suite | Automated cortical and subcortical segmentation | Traditional segmentation benchmark |
| FastSurfer [78] | Software Pipeline | Deep learning-based whole-brain segmentation | Rapid, motion-resilient processing |
| SLOMOCO [82] | Software Tool | Slice-oriented motion correction for fMRI | Intravolume motion correction |
| FIRMM [83] | Software Tool | Real-time head motion monitoring | Prospective motion tracking |
| HBN Biobank [81] [80] | Dataset | Large-scale pediatric dataset with motion metrics | Population-based motion studies |
| SIMPACE [82] | Method | Simulates motion-corrupted data from phantoms | Gold-standard motion evaluation |
| 2,6-dipyridin-2-ylpyridine | 2,6-dipyridin-2-ylpyridine | Terpyridine Ligand | RUO | High-purity 2,6-dipyridin-2-ylpyridine (Terpyridine), a key tridentate ligand for catalysis & materials science. For Research Use Only. Not for human or veterinary use. | Bench Chemicals |
Subject positioning, particularly head tilt and motion, significantly impacts structural MRI quality and subsequent automated analysis. Traditional segmentation pipelines like FreeSurfer show substantial degradation with increasing motion severity, while modern deep learning approaches (FastSurferCNN, Kwyk, ReSeg, and particularly SynthSeg+) demonstrate superior resilience to motion artifacts while offering order-of-magnitude faster processing. The systematic bias introduced by motion—notably reduced cortical thickness and gray matter volume estimates—disproportionately affects pediatric and neuropsychiatric populations, potentially confounding research findings. Incorporating motion-robust processing tools and accounting for motion effects in statistical models is essential for reliable brain imaging analysis in both basic research and clinical trial contexts. Future methodological development should focus on improving motion resilience without specialized acquisitions, making robust segmentation accessible across diverse research and clinical settings.
The Alzheimer's Disease Neuroimaging Initiative (ADNI) has established itself as a pivotal longitudinal, multi-center study designed to validate biomarkers for Alzheimer's disease clinical trials [84]. Within this framework, magnetic resonance imaging protocols have evolved significantly, with a notable shift from traditional non-accelerated sequences to accelerated acquisitions utilizing parallel imaging techniques. This transition represents a critical methodological advancement in the pursuit of reliable, efficient, and patient-friendly neuroimaging for neurodegenerative disease research. The essential trade-off involves balancing scan acquisition time against image quality and measurement precision, particularly for quantifying subtle brain changes over time. As clinical trials increasingly rely on sensitive morphological biomarkers like brain volume and atrophy rates, understanding the comparability between these acquisition protocols becomes paramount for both data interpretation and future study design.
Protocol Specifications: A Technical Comparison
The ADNI MRI protocol has undergone refinements across its successive phases (ADNI-1, ADNI-GO, ADNI-2, and ADNI-3). A fundamental distinction exists between the non-accelerated and accelerated T1-weighted volumetric sequences, which differ primarily in their use of parallel imaging.
Core Technical Differences:
- Non-Accelerated Scans: These represent the original standard, typically requiring approximately 9 minutes for a 3T 3D structural brain MRI at 1 mm resolution [85]. They do not employ parallel imaging techniques, potentially yielding higher signal-to-noise ratio (SNR) and different tissue contrast properties but at the cost of longer acquisition times.
- Accelerated Scans: These utilize parallel imaging techniques (e.g., GRAPPA or SENSE) to significantly reduce scan time. The accelerated protocol in ADNI-GO/2 shortens the acquisition to approximately 5 minutes on a 3T scanner [85]. This is achieved at the potential expense of altered noise distribution and potentially reduced SNR, though it benefits from decreased susceptibility to motion artefacts.
It is crucial to note that the three different scanner manufacturers (Philips, Siemens, and General Electric) used across ADNI sites implement different proprietary acceleration protocols, details of which are specified on the ADNI website [85].
Table 1: Key Technical Specifications of ADNI Protocols
| Parameter | Non-Accelerated Protocol | Accelerated Protocol |
|---|---|---|
| Approximate Scan Time | ~9 minutes [85] | ~5 minutes [85] |
| Acceleration Technique | None | Parallel Imaging (varies by manufacturer) |
| Primary Advantage | Potentially higher SNR, established benchmark | Reduced motion artefacts, better patient tolerance [85] |
| Primary Disadvantage | Longer acquisition, more motion artefacts [85] | Altered noise distribution, potentially lower SNR |
Quantitative Performance Comparison
Empirical evidence directly comparing these protocols is essential to validate the use of accelerated scans in research. A key study using data from 861 subjects at baseline from the ADNI dataset provides a rigorous, head-to-head comparison of brain volume and atrophy rate measures [85].
Volumetric and Atrophy Rate Measures
The study calculated whole-brain, ventricular, and hippocampal atrophy rates using the boundary shift integral (BSI), a sensitive biomarker for clinical trials [85]. The findings demonstrate no statistically significant differences in the key volumetric measurements between the two protocols.
Table 2: Comparison of Quantitative Measures Between Protocols [85]
| Measurement Type | Comparison Between Protocols | Statistical Significance |
|---|---|---|
| Whole-Brain Volume & Atrophy | No significant differences found | Not Significant |
| Ventricular Volume & Atrophy | No significant differences found | Not Significant |
| Hippocampal Volume & Atrophy | No significant differences found | Not Significant |
| Scan Quality (Motion Artefacts) | Twice as many non-accelerated scan pairs had motion artefacts | p ≤ 0.001 |
| Clinical Trial Sample Size | No difference in estimated requirements | Not Significant |
Impact on Data Quality and Subject Coverage
A critical finding is the significant difference in data quality related to participant motion. The study reported that twice as many non-accelerated scan pairs exhibited at least some motion artefacts compared with accelerated scan pairs (p ≤ 0.001) [85]. This has profound implications for data integrity and study power, as motion can render scans unusable for quantitative analysis.
Furthermore, the characteristics of subjects who produced motion-corrupted scans differed between protocols. Those with poor-quality accelerated scans had a higher mean vascular burden and age, whereas those with poor-quality non-accelerated scans had poorer Mini-Mental State Examination (MMSE) scores [85]. This suggests that the choice of protocol can influence which participant subgroups are adequately represented in the final analyzable dataset.
Experimental Methodologies in Protocol Comparison Studies
Core Experimental Workflow
The following diagram illustrates the standard methodology for comparing MRI sequence protocols, as employed in studies such as the one analyzing the ADNI dataset [85].
Detailed Methodological Breakdown
Subject Population and Data: The cited analysis used data from 861 subjects at baseline, 573 at 6 months, and 384 at 12 months from the ADNI-GO/2 phases, which included both accelerated and non-accelerated scans for each participant [85]. This paired design allows for robust within-subject comparisons.
Image Acquisition: In the ADNI protocol, non-accelerated scans were always acquired prior to accelerated scans during the same scanning session [85]. This standardized the physiological state of the subject across sequences. All scans underwent pre-processing corrections for gradient warping and intensity non-uniformity [85].
Quality Control (QC): A critical, multi-stage QC process was implemented:
- Site-level QC: Imaging sites were instructed to immediately assess scan quality and re-acquire if necessary.
- Central QC: The Mayo Clinic performed an initial QC assessing protocol adherence, medical abnormalities, and severe artefacts.
- Analysis-level QC: The research team (e.g., at the Dementia Research Centre) performed visual assessment for artefacts and, after processing, a blinded rater assessed registered scan pairs for quality differences that could affect BSI measures. Scans with significant motion or geometric distortions were excluded [85].
Quantitative Analysis:
- Volumetric Measures: Whole-brain, ventricular, and hippocampal volumes were calculated using automated template-based methods for region delineation [85] [86].
- Atrophy Rates: The boundary shift integral (BSI) was used to calculate longitudinal atrophy. The BSI measures volume change by tracking how much the surface of a brain structure has moved between baseline and follow-up scans using normalized voxel intensities of co-registered images [85]. This method is distinct from tensor-based morphometry (TBM), which estimates volume change from deformation fields.
Statistical Analysis: The study employed statistical comparisons of volumes and atrophy rates between protocols. It also estimated sample size requirements for a hypothetical clinical trial to assess the practical impact of protocol choice on study power [85].
Table 3: Key Analytical Tools and Resources for ADNI MRI Data
| Tool/Resource | Function in Analysis | Relevance to Protocol Studies |
|---|---|---|
| Boundary Shift Integral (BSI) | Measures longitudinal brain volume change from serial MRI [85]. | Primary outcome measure for comparing atrophy rates between protocols. |
| FreeSurfer | Automated software for cortical reconstruction and volumetric segmentation [86]. | Widely used in ADNI for cross-sectional volume estimation of brain structures. |
| Voxel-Based Morphometry (VBM) | A computational approach to detect regional differences in brain tissue composition [87]. | Used to compare tissue classification (GM, WM, CSF) between different protocols. |
| ADNI Data Archive (IDA) | Secure repository for all ADNI data (clinical, genetic, imaging) [88]. | Source for downloading both accelerated and non-accelerated images for comparison. |
| Visual Quality Control Protocols | Standardized procedures for excluding scans with motion or artefacts [85]. | Critical for ensuring that quantitative comparisons are not biased by scan quality. |
The body of evidence indicates that accelerated MRI protocols provide a viable and, in some aspects, superior alternative to non-accelerated sequences for structural brain imaging in Alzheimer's disease research. The primary empirical data demonstrates no significant differences in the accuracy of measuring key biomarkers like whole-brain, ventricular, and hippocampal volumes and atrophy rates [85]. This foundational equivalence, coupled with the halving of scan time and a significant reduction in motion-related artefacts, presents a compelling case for the adoption of accelerated protocols in future studies and clinical trials.
The implications for research and drug development are substantial. The reduced acquisition time improves patient comfort and compliance, which is particularly beneficial in more cognitively impaired populations. The higher yield of usable data from accelerated scans enhances the statistical power of longitudinal studies without increasing the sample size or scanner time. Therefore, for clinical trials utilizing ADNI-type biomarkers, accelerated scans offer an efficient and robust methodological choice, balancing patient burden with precise measurement of disease progression.
Quantitative brain morphometry relies on automated segmentation tools, with FreeSurfer being one of the most widely used software suites in neuroscience research. However, the continuous development of this tool introduces a critical methodological consideration: how do different versions compare in their volumetric outputs and statistical inferences? This guide objectively compares FreeSurfer versions within the broader context of brain imaging method reliability assessment, providing researchers and drug development professionals with experimental data and protocols to inform their analytical choices.
FreeSurfer Version Comparison: Quantitative Data
Volumetric Differences Across Versions
Table 1: Absolute volume differences between FreeSurfer versions in key subcortical structures (in cm³) based on the Chronic Effects of Neurotrauma Consortium study [89].
| Brain Region | FreeSurfer 5.3 Mean Volume | FreeSurfer 6.0 Mean Volume | Absolute Difference | Statistical Significance |
|---|---|---|---|---|
| Total Intracranial Volume | 1,558.2 | 1,574.1 | 15.9 | p < 0.001 |
| Total White Matter | 490.3 | 501.7 | 11.4 | p < 0.001 |
| Total Ventricular Volume | 28.4 | 30.1 | 1.7 | p < 0.001 |
| Left Hippocampus | 3.92 | 3.87 | 0.05 | p < 0.05 |
| Right Hippocampus | 3.98 | 3.94 | 0.04 | p < 0.05 |
| Left Amygdala | 1.61 | 1.58 | 0.03 | p < 0.05 |
| Right Amygdala | 1.65 | 1.62 | 0.03 | p < 0.05 |
The volumetric differences between versions 5.3 and 6.0 were statistically significant across all measured regions, with absolute volume differences ranging from 0.03 cm³ in amygdalae to 15.9 cm³ in total intracranial volume [89]. Despite these absolute differences, correlational analyses between regions remained similar between versions, suggesting that relative volume relationships are preserved [89].
Statistical Inference Variability Across Versions
Table 2: Differential detection of case-control differences across FreeSurfer versions in a type 1 diabetes study [90].
| FreeSurfer Version | Cortical Volume Differences Detected | Subcortical Volume Differences Detected | Statistical Significance Level |
|---|---|---|---|
| 5.3 (with manual correction) | Yes (whole cortex, frontal cortex) | Yes (multiple regions) | p < 0.05 |
| 5.3 (raw) | Yes | Yes | p < 0.05 |
| 5.3 HCP | No | Yes (lower magnitude) | p < 0.05 |
| 6.0 | No | Yes (lower magnitude) | p < 0.05 |
| 7.1 | No | No | Not Significant |
Alarmingly, different FreeSurfer versions applied to the same dataset yielded different statistical inferences regarding group differences [90]. Version 5.3 detected both cortical and subcortical differences between healthy controls and type 1 diabetes patients, while newer versions reported only subcortical differences of lower magnitude, and version 7.1 failed to find any statistically significant inter-group differences [90]. This variability appeared to stem from substantially higher within-group variability in the pathological condition in newer versions rather than differences in group averages [90].
Processing Efficiency Improvements
Table 3: Computational efficiency improvements across FreeSurfer versions.
| FreeSurfer Version | Processing Time per Subject | Memory Requirements | Key Technological Advances |
|---|---|---|---|
| 6.0 | ~8 hours (single CPU) | ~8GB | Standard pipeline [91] |
| 7.X | ~8 hours (single CPU) | ~8GB | Incremental improvements [92] |
| 8.0 | ~2 hours (single CPU) | ~24GB | SynthStrip, SynthSeg, SynthMorph [92] |
FreeSurfer version 8.0 represents a substantial advancement in processing efficiency, reducing computation time from approximately 8 hours to about 2 hours per subject on a single CPU [92]. This performance improvement comes from integrating deep learning algorithms like SynthStrip for skull stripping and SynthSeg for segmentation, though memory requirements have increased to 24GB [92].
Experimental Protocols for Version Comparison
Multi-Version Volumetric Comparison Protocol
The Chronic Effects of Neurotrauma Consortium (CENC) study established a robust protocol for comparing FreeSurfer versions [89]:
- Subject Population: 249 participants with neurotrauma history from a multicenter observational study
- Image Acquisition: T1-weighted structural MRI scans collected across multiple sites
- Processing Pipeline: Each scan processed through both FreeSurfer 5.3 and 6.0 using standard recon-all pipeline
- Regions of Interest: Total intracranial volume, total white matter volume, total ventricular volume, total gray matter volume, and bilateral thalamus, pallidum, putamen, caudate, amygdala, and hippocampus
- Statistical Analysis: General linear modeling and random forest methods to compare absolute volumes and predictive accuracy for age-related changes
This study found that while absolute volumes were not interchangeable between versions, correlational analyses yielded similar results [89].
Case-Control Statistical Inference Protocol
The type 1 diabetes study implemented a comprehensive version comparison protocol [90]:
- Subject Cohorts: 24 type 1 diabetes patients and 27 healthy controls
- MRI Acquisition: 3T Siemens Prisma system with MPRAGE sequence (1mm isotropic voxels)
- Version Comparison: FS 5.3 raw, FS 5.3 with manual correction, FS 5.3 HCP, FS 6.0, and FS 7.1
- Preprocessing Variations:
- Standard pipeline for FS 5.3, 6.0, and 7.1
- HCP pipeline with gradient distortion correction and custom brain extraction
- Quality Control:
- Meticulous manual correction for FS 5.3 MC
- Less stringent criteria (3-voxel threshold) for other versions
- Statistical Testing: Student's T-test for group comparisons of 9 predefined regions of interest
This protocol revealed that version choice significantly impacted statistical conclusions about group differences [90].
Figure 1: FreeSurfer version comparison workflow. The choice of FreeSurfer version introduces variability at multiple stages of the research pipeline, potentially affecting final research conclusions [90] [89].
Comparative Performance Against Alternative Solutions
FreeSurfer vs. Deep Learning-Based Alternatives
Table 4: FreeSurfer comparison with emerging deep learning segmentation tools.
| Software Tool | Underlying Technology | Processing Time | Dice Similarity Coefficient | Ethnic Population Optimization |
|---|---|---|---|---|
| FreeSurfer 6.0 | Surface-based segmentation | ~8 hours | 0.6-0.8 [91] | Primarily Caucasian [91] |
| Neuro I | 3D CNN deep learning | <10 minutes | 0.8-0.9 [91] | East Asian (trained on 776 Koreans) [91] |
| Neurophet AQUA | Deep learning | ~5 minutes | >0.8 [93] | Multi-ethnic [93] |
Deep learning-based alternatives consistently demonstrate superior processing efficiency compared to FreeSurfer, with processing times reduced from hours to minutes [91] [93]. Neuro I, trained specifically on East Asian brains, showed significantly higher Dice similarity coefficients compared to FreeSurfer 6.0 (0.8-0.9 vs. 0.6-0.8), suggesting potential population-specific optimization benefits [91].
Reliability Across Magnetic Field Strengths
A 2024 study evaluated the reliability of FreeSurfer and Neurophet AQUA across different magnetic field strengths [93]:
- Dataset: 101 patients (1.5T-3T pairs) and 112 patients (3T-3T pairs) from multiple hospitals and open-source databases
- Methodology: Comparison of mean volume difference and average volume difference percentage between field strengths
- Findings:
- FreeSurfer showed larger volume differences across field strengths (>10% average volume difference percentage)
- Neurophet AQUA demonstrated more stable performance across field strengths (<10% average volume difference percentage)
- Both tools showed satisfactory intraclass correlation coefficients (0.869-0.965)
The study concluded that while both methods were reliable, Neurophet AQUA showed smaller volume variability due to changes in magnetic field strength [93].
The Scientist's Toolkit: Essential Research Reagents
Table 5: Key software solutions for automated brain segmentation in research.
| Tool Name | Type | Primary Function | Key Features |
|---|---|---|---|
| FreeSurfer | Automated segmentation suite | Structural MRI analysis | Surface-based cortical segmentation, subcortical volumetry, cross-platform compatibility [94] [92] |
| Neurophet AQUA | Commercial deep learning software | Brain volume segmentation | FDA-approved, rapid processing (~5 minutes), stable across magnetic field strengths [93] |
| Neuro I | Deep learning segmentation | Clinical volumetry | FDA Korea-approved, optimized for East Asian brains, 109 ROIs based on DKT atlas [91] |
| MAPER | Multi-atlas propagation | Volumetric segmentation | Multiple atlas registration, enhanced registration accounting for brain morphology [94] |
| SynthStrip | Deep learning tool | Skull stripping | Robust brain extraction across image types and populations [95] [92] |
FreeSurfer version differences introduce significant variability in both absolute volumetric measurements and statistical inferences in research contexts. While absolute volumes are not interchangeable across versions [89], the general patterns of correlation and relationships appear more stable. The research community faces a critical challenge: newer versions incorporate valuable improvements but may alter fundamental findings from earlier studies [90]. Researchers must carefully consider version control, document FreeSurfer versions thoroughly in publications, and consider confirmatory analyses with complementary methods when reporting subtle effects. The emergence of deep learning alternatives offers improved processing efficiency and potentially better performance for specific populations [91] [93], though FreeSurfer remains the benchmark in the field. As quantitative neuroimaging advances, standardized protocols for version comparison and validation in common research scenarios should be prioritized in the software development cycle.
In the field of brain imaging, the reliability and sensitivity of magnetic resonance imaging (MRI) derived biomarkers are paramount for both research and clinical applications. The choice of data processing pipeline—cross-sectional or longitudinal—fundamentally influences the quality and interpretability of these biomarkers. Cross-sectional processing analyzes each imaging time point independently, while longitudinal processing explicitly leverages the temporal relationship between scans from the same subject. This guide provides an objective comparison of these two approaches, framing the discussion within the broader context of brain imaging method reliability assessment. For researchers, scientists, and drug development professionals, understanding this distinction is critical for designing robust studies, accurately monitoring disease progression, and evaluating treatment effects.
Theoretical Foundations and Key Concepts
The fundamental difference between cross-sectional and longitudinal processing streams lies in their use of temporal information. Cross-sectional analysis treats each MRI scan session as an independent data point, processing images through a pipeline without reference to other time points from the same individual. This approach is computationally simpler and requires only single-time-point data, but it ignores the within-subject correlation across time. In contrast, longitudinal processing specifically incorporates the temporal dimension, typically by creating a subject-specific template from all available time points first, which then serves as a reference for processing individual scans. This within-subject alignment significantly reduces random variations unrelated to true biological change [96] [97].
The neuroimaging community increasingly recognizes longitudinal designs as essential for distinguishing true aging effects from simple age-related differences observed in cross-sectional studies [98]. In clinical trials for neurodegenerative diseases, this distinction becomes particularly crucial, as longitudinal pipelines can detect subtle treatment effects with greater sensitivity by reducing measurement variability. The reliability of these imaging biomarkers directly impacts the statistical power required for clinical trials and observational studies, with more reliable measures enabling smaller sample sizes or shorter trial durations to demonstrate significant effects [96].
Comparative Performance Analysis
Quantitative Reliability Metrics
Table 1: Comparative Reliability of Cross-sectional and Longitudinal Processing Streams
| Metric | Cross-sectional Stream | Longitudinal Stream | Improvement | Assessment Context |
|---|---|---|---|---|
| Reproducibility Error | Higher (reference value = 100%) | ≈50% lower | ~50% reduction | Multi-center 3T MRI studies, volume segmentations [96] |
| Sample Size Requirement | Higher (reference value = 100%) | <50% for most structures | >50% reduction | Power analysis for equivalent statistical power [96] |
| Statistical Power | Standard | Superior | Significantly improved | Detection of disease progression and treatment effects [99] |
| Classification Power | Lower in vivo | Improved with longitudinal information | Enhanced by incorporating temporal data | Mouse model of tauopathy [99] |
| Sensitivity to Change | Moderate | High | Increased sensitivity | Monitoring disease progression in mouse models [99] |
Application-Specific Performance
In studies of neurological diseases, longitudinal processing demonstrates particular advantages. Research on multiple sclerosis (MS) patients utilizing longitudinal MRI revealed accelerated brain aging associated with brain atrophy and increased white matter lesion load, findings that were more robustly characterized through longitudinal tracking [100]. Similarly, in animal models of neurodegenerative diseases like the rTg4510 mouse model of tauopathy, longitudinal in vivo imaging enabled researchers to track progressive brain atrophy over time, capturing disease progression and treatment effects that might be missed in cross-sectional analyses [99].
Quantitative MRI (qMRI) biomarkers, which provide physical measurements of tissue properties rather than qualitative contrasts, particularly benefit from longitudinal designs. A recent study investigating the longitudinal reproducibility of qMRI biomarkers in the brain and spinal cord found high reproducibility (intraclass correlation coefficient ≃ 1) for metrics including T1, fractional anisotropy, and mean diffusivity when the same protocol and scanner were used over multiple years [101]. This high reproducibility is essential for designing longitudinal clinical studies tracking disease progression or treatment response.
Experimental Protocols and Methodologies
Longitudinal Processing Implementation
Table 2: Key Stages in Longitudinal Processing Pipelines
| Processing Stage | Technical Implementation | Purpose | Tools/Examples |
|---|---|---|---|
| Within-Subject Template Creation | Unbiased within-subject template created using robust, inverse consistent registration | Serves as a stable reference for all time points from the same subject | FreeSurfer longitudinal stream [100] |
| Initialization with Common Information | Processing steps (skull stripping, Talairach transforms, atlas registration) initialized from the within-subject template | Increases reliability and statistical power | FreeSurfer longitudinal stream [100] |
| Individual Time Point Processing | Each time point is processed with the subject-specific template as a reference | Maintains consistency across sessions while capturing individual changes | FreeSurfer, ANTs, SCT [100] [101] |
| Quality Control | Visual inspection and automated quality indices | Identifies and excludes data of insufficient quality | Manual editing and exclusion [100] |
Multi-Center Study Protocols
Implementing longitudinal pipelines in multi-center studies requires meticulous standardization. Key considerations include:
- Protocol Harmonization: Different sites may use different scanner manufacturers, hardware, and software versions, potentially affecting imaging outcome measures. The imaging protocol should be kept identical throughout the scanning period whenever possible [100] [97].
- Handling Scanner Upgrades: A plan to cope with unforeseen circumstances, such as scanner upgrades, should be established in advance to maintain data consistency [97].
- Phantom Measurements: Regular phantom scans can help monitor and correct for scanner-specific drifts in quantitative metrics [76].
- Centralized Quality Control: Implementing standardized quality control procedures for both intra-site and inter-site reliability is essential. This includes visual inspection and automated quality assessment to identify artifacts [97] [76].
The following diagram illustrates a recommended workflow for implementing a longitudinal multi-center neuroimaging study:
Quality Assessment Methods
Robust quality assessment is crucial for both processing streams. Automated quality control methods can detect artifacts by analyzing the background (air) region of MR images, identifying signal intensity abnormalities caused by motion, ghosting, blurring, and other sources of degradation [76]. These methods can derive quality indices (QI) that correlate well with expert quality ratings, providing an objective measure of scan usability.
For functional MRI studies, reliability can be assessed using voxel-wise intraclass correlation coefficients (ICC), analysis of scatter plots comparing contrast values, and calculating the ratio of overlapping activation volumes across sessions [102]. These methods help quantify the consistency of functional activation patterns over time.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Tools for Neuroimaging Pipelines
| Tool/Resource | Function | Application Context |
|---|---|---|
| FreeSurfer | Automated cortical reconstruction and volumetric segmentation | Cross-sectional and longitudinal structural MRI analysis [100] [96] |
| FSL | FMRIB Software Library for MRI data analysis | Diffusion imaging, lesion filling, general image processing [100] |
| ANTs | Advanced Normalization Tools for image registration | Symmetric registration for creating within-subject templates [101] |
| Spinal Cord Toolbox (SCT) | Dedicated spinal cord MRI analysis | Spinal cord cross-sectional area and quantitative metric analysis [101] |
| qMRLab | Quantitative MRI data analysis | Fitting qMRI models to derive quantitative parameter maps [101] |
| Custom Headcases | Motion minimization during scanning | Improving reproducibility in longitudinal qMRI studies [101] |
| Multi-Atlas Segmentation | Automated structural parcellation | Preclinical and clinical MRI volume analysis [99] |
| Nextflow | Pipeline management for reproducible workflows | Orchestrating complex analysis pipelines [101] |
The choice between cross-sectional and longitudinal processing pipelines has profound implications for the reliability and sensitivity of neuroimaging biomarkers. Longitudinal processing consistently demonstrates superior performance in terms of reproducibility, statistical power, and sensitivity to biological change. This advantage is particularly valuable in contexts where detecting subtle changes over time is critical, such as clinical trials for neurodegenerative diseases or studies of brain development and aging. However, longitudinal approaches require multiple time points and more complex processing workflows. For researchers and drug development professionals, investing in longitudinal designs and processing streams offers substantial returns in data quality and statistical efficiency, ultimately enhancing the validity and impact of neuroimaging research.
Validation Frameworks: Comparing Tools, Scanners, and Sequences
In scientific research, particularly in fields requiring precise measurements like neuroimaging and biomechanics, test-retest reliability is a fundamental property that quantifies the consistency and reproducibility of measurements. This concept is critically divided into two distinct temporal frameworks: intra-session reliability, which assesses consistency within a single testing session, and inter-session reliability, which evaluates consistency across multiple sessions separated by hours, days, or months. Understanding the distinction between these reliability types is crucial for researchers, scientists, and drug development professionals when designing studies, interpreting results, and assessing the utility of biomarkers for clinical applications.
The importance of reliability assessment is particularly acute in brain imaging research, where the quest for valid biomarkers of disease risk is heavily dependent on measurement reliability. Unreliable measures are inherently unsuitable for predicting clinical outcomes or studying individual differences. As noted in a comprehensive meta-analysis, "the ability to identify meaningful biomarkers is limited by measurement reliability; unreliable measures are unsuitable for predicting clinical outcomes" [103]. This review systematically compares intra-session and inter-session reliability across multiple measurement domains, with particular emphasis on brain imaging methodologies, to provide researchers with evidence-based guidance for experimental design and interpretation.
Quantitative Reliability Comparisons Across Modalities
Comparative Reliability Metrics Across Research Domains
Table 1: Comparison of Intra-session and Inter-session Reliability Across Measurement Domains
| Measurement Domain | Specific Measure | Intra-session ICC Range | Inter-session ICC Range | Key Findings |
|---|---|---|---|---|
| Brain Function (fMRI) | Task-fMRI activation | Not reported | 0.067-0.485 (meta-analysis) | Poor overall reliability for individual differences [103] |
| Brain Structure/Function | Functional connectome fingerprinting | Not reported | 0.85 (whole-brain identification accuracy) | High identifiability over 103-189 days [104] |
| Pressure Pain Threshold | Low back PPT | 0.85-0.99 | 0.85-0.99 | Excellent reliability both intra- and inter-session [105] |
| Postural Control | Biodex Balance System (MLSI) | 0.71-0.95 | 0.72-0.96 | Moderate to high reliability across sessions [106] |
| Reaction Time | Knee extension RT (PFPS patients) | 0.78-0.94 | 0.70-0.94 | Three-trial mode most reliable [107] |
| Sprint Mechanics | Treadmill sprint kinetics | >0.94 | >0.94 | Excellent reliability for kinetic parameters [108] |
| Electrical Pain Threshold | Cutaneous EPT | 0.76-0.93 | 0.08-0.36 | Excellent intra-session but poor inter-session reliability [109] |
Table 2: Statistical Measures for Assessing Test-Retest Reliability
| Statistical Measure | Formula | Interpretation | Application Context |
|---|---|---|---|
| Intraclass Correlation Coefficient (ICC) | ICC = σ²S/(σ²S + σ²e) | Quantifies relative reliability: 0.9-1.0 (very high), 0.7-0.89 (high), 0.5-0.69 (moderate), <0.5 (poor) [106] [107] | General purpose reliability assessment |
| Standard Error of Measurement (SEM) | SEM = √σ²e | Absolute reliability in original units | Useful for clinical interpretation |
| Within-Subject Coefficient of Variation (WSCV) | WSCV = σe/μ | Scaled relative measure (%) | Common in PET brain imaging [110] |
| Minimum Detectable Change (MDC) | MDC = 1.96 × √2 × SEM | Smallest real difference at 95% confidence | Clinical significance of changes |
| Repeatability Coefficient (RC) | RC = 1.96 × √2 × σe | 95% limits of agreement for test-retest differences | Alternative to MDC [110] |
Key Patterns in Reliability Data
Analysis across studies reveals consistent patterns in reliability assessments. Intra-session reliability generally exceeds inter-session reliability across most measurement domains, as the shorter time frame minimizes potential sources of variability such as biological changes, environmental fluctuations, and instrumentation drift. The magnitude of this reliability gap varies substantially by measurement type, with some measures like pressure pain thresholds showing minimal differences [105], while others like electrical pain thresholds demonstrate dramatic declines from excellent intra-session (ICC: 0.76-0.93) to poor inter-session (ICC: 0.08-0.36) reliability [109].
The complexity of the measured system appears to influence reliability, with simpler physiological measures (e.g., sprint kinetics, pressure pain thresholds) generally demonstrating higher reliability coefficients than complex functional brain measures (e.g., task-fMRI activation). This pattern highlights the challenge of deriving reliable biomarkers from complex brain systems where multiple confounding factors can introduce measurement variability across sessions [103].
Experimental Protocols and Methodologies
Brain Imaging Reliability Assessment
Functional Magnetic Resonance Imaging (fMRI) Protocols for test-retest reliability assessment typically involve acquiring brain scans from the same participants across multiple sessions. In the BNU test-retest dataset, 61 healthy adults underwent scanning in two sessions separated by 103-189 days using a 3T Siemens scanner [8]. The protocol included high-resolution structural images (T1-weighted MPRAGE) and resting-state functional MRI (rfMRI) scans. For rfMRI, participants were instructed to "relax without engaging in any specific task, and remain still with your eyes closed during the scan" [8]. The imaging parameters were slightly different between sessions, meaning reliability estimates reflect lower bounds of true reliability.
Functional Connectome Fingerprinting analysis involves extracting individual functional connectivity estimates from rfMRI data. Typically, preprocessing includes motion censoring (discarding volumes with displacement >0.5 mm), followed by computation of pairwise bivariate correlations among hundreds of cortical regions-of-interest [104]. The resulting connectivity profiles are compared between sessions using correlation coefficients, with within-subject similarity determining identification accuracy. This approach has demonstrated 85% accuracy for whole-brain connectivity profiles over intervals of several months [104].
Psychophysical and Biomechanical Protocols
Pressure Pain Threshold (PPT) Assessment in the lower back of asymptomatic individuals followed a standardized protocol. PPTs were assessed among 14 anatomical locations in the low back region over two sessions separated by one hour. For each session, three PPT assessments were performed on each location using a pressure algometer [105]. Reliability was assessed comparing different combinations of trials and sessions, revealing that either two or three consecutive measurements provided excellent reliability.
Postural Control Evaluation using the Biodex Balance System typically involves assessing single-leg-stance performance under varying difficulty levels (static and dynamic conditions with and without visual feedback). Participants stand on the platform with hands placed on iliac crests, maintaining their center of pressure in the smallest concentric ring on the monitor [106]. Each measurement lasts 20 seconds with three repetitions, and average scores are used for analysis. The platform stability levels can be adjusted, with more challenging conditions (eyes closed) often demonstrating higher reliability coefficients [106].
Decision Framework for Researchers
Practical Implications for Research Design
The choice between emphasizing intra-session or inter-session reliability in experimental design should be guided by the research question and intended application of the measurements:
For technical validation of instruments or establishing immediate consistency, intra-session reliability provides the most relevant information, as it minimizes biological and environmental sources of variability.
For biomarker development or measures intended to track changes over time, inter-session reliability is essential, as it reflects real-world stability against confounding temporal factors.
In brain imaging studies, the generally lower inter-session reliability of task-fMRI measures (ICCs: 0.067-0.485) suggests caution when using these for individual-differences research or clinical applications [103]. In contrast, functional connectome fingerprinting shows remarkable stability over months, with 85% identification accuracy [104].
Methodological Recommendations to Enhance Reliability
Based on the synthesized evidence, several strategies can enhance reliability in research measurements:
Optimize trial structure: Multiple studies found that using the average of three trials provides more reliable measures than single trials [105] [107]. However, for pressure pain thresholds, either two or three consecutive measurements provided excellent reliability [105].
Standardize testing conditions: Controlling for time of day, environmental factors, and (for women) menstrual cycle phase can reduce unwanted variability in inter-session assessments [109].
Account for task design characteristics: In fMRI, task design elements (blocked vs. event-related, task length) influence reliability, with longer tasks generally providing more stable estimates [103].
Consider population-specific factors: Reliability should be established within specific populations of interest, as it varies between healthy controls and clinical groups [106] [107] [111].
Essential Research Toolkit
Table 3: Key Research Reagent Solutions for Reliability Studies
| Tool/Category | Specific Examples | Primary Function | Considerations for Reliability Studies |
|---|---|---|---|
| Brain Imaging Systems | 3T Siemens Scanner (MAGENTOM Trio) [8] | Acquisition of structural and functional brain data | Consistent scanner parameters between sessions critical |
| Balance Assessment | Biodex Balance System (BBS) [106] [111] | Quantification of dynamic postural stability | Standardize difficulty levels and visual conditions |
| Pain Threshold Measurement | Pressure algometer [105] | Objective quantification of mechanical pain sensitivity | Multiple trials (2-3) recommended for reliability |
| Electrical Stimulation | Dantec Keypoint Focus System [109] | Selective stimulation of cutaneous and muscle afferents | Poor inter-session reliability for pain thresholds |
| Reaction Time Assessment | Deary-Liewald reaction time (DLRT) task [107] | Measurement of central processing speed | Custom knee extension package available for functional assessment |
| Statistical Analysis Packages | SPSS, R with metafor and agRee packages [103] [110] | Computation of reliability metrics (ICC, SEM, WSCV) | Multilevel models account for nested data structures |
The comprehensive comparison between intra-session and inter-session reliability reveals a complex landscape where measurement consistency varies substantially across domains, methodologies, and timeframes. While intra-session reliability generally exceeds inter-session reliability due to minimized temporal confounding factors, the clinical and research utility of measurements ultimately depends on their stability across meaningful time intervals. This distinction is particularly crucial in brain imaging research, where the pursuit of valid biomarkers requires careful attention to the methodological limitations of current approaches, especially the generally poor reliability of task-fMRI measures for studying individual differences.
Researchers should select reliability assessment strategies that align with their specific applications, with intra-session designs suiting technical validation studies and inter-session designs being essential for biomarker development and longitudinal research. Future methodological advances should focus on enhancing the inter-session reliability of brain imaging measures through optimized task designs, acquisition parameters, and analytical approaches to fulfill the promise of neuroscience in clinical applications and individual-differences research.
This guide provides an objective comparison of leading brain imaging software tools, evaluating their performance, reliability, and suitability for different research scenarios within the context of brain imaging method reliability assessment.
Automated brain imaging segmentation tools are indispensable in modern neuroimaging research and clinical studies. These software pipelines enable the quantitative assessment of brain structures from MRI data, providing critical biomarkers for neurodegenerative diseases, psychiatric conditions, and neurodevelopmental disorders. The reliability of these measurements is paramount, particularly in longitudinal studies and drug development trials where detecting subtle changes over time is essential. This comparison guide objectively evaluates three categories of solutions: the widely established traditional pipeline FreeSurfer, the deep learning-based FastSurfer, and emerging commercial tools, with a focus on their performance characteristics, reliability metrics, and suitability for different research scenarios.
FreeSurfer: Established Traditional Pipeline
FreeSurfer is a comprehensive, widely-adopted suite for cortical surface-based processing and subcortical volumetric segmentation of brain MRI data. Its methodology relies on a series of computationally intensive optimization steps including non-linear registration, probabilistic atlas-based segmentation, and intensity-based normalization. The pipeline incorporates Bayesian inference, spherical surface registration, and complex geometric models to reconstruct cortical surfaces and assign neuroanatomical labels. This multi-stage approach involves thousands of iterative optimization steps per volume, resulting in extensive processing times typically ranging from 5 to 20 hours per subject but providing highly detailed morphometric outputs [112].
FastSurfer: Deep Learning Alternative
FastSurfer is a deep learning-based pipeline designed to replicate FreeSurfer's anatomical segmentation while dramatically reducing computation time. Its core innovation is FastSurferCNN, an advanced neural network architecture employing competitive dense blocks and competitive skip pathways to induce local and global competition during segmentation. The network operates on coronal, axial, and sagittal 2D slice stacks with a final view aggregation step, effectively combining the advantages of 3D patches (local neighborhood) and 2D slices (global view). This approach is specifically tailored toward accurate recognition of both cortical and subcortical structures. For surface processing, FastSurfer introduces a novel spectral spherical embedding method that directly maps cortical labels from the image to the surface, replacing FreeSurfer's iterative spherical inflation with a one-shot parametrization using the eigenfunctions of the Laplace-Beltrami operator [37] [113] [112].
Commercial Solutions: Emerging Alternatives
Commercial neuroimaging tools represent a growing segment of the market, typically offering optimized algorithms with regulatory approval for clinical use. This category includes solutions like Neurophet AQUA, which employs deep learning architectures specifically designed for robust performance across varying MRI acquisition parameters. These tools often focus on specific clinical applications such as dementia, epilepsy, or multiple sclerosis, and frequently undergo extensive validation for regulatory approval. While implementation details are often proprietary, they generally emphasize clinical workflow integration, standardized reporting, and technical support [93].
Figure 1: Architectural comparison of neuroimaging pipelines showing fundamental methodological differences between traditional, deep learning-based, and commercial approaches.
Performance Comparison Data
Quantitative Performance Metrics
Table 1: Comprehensive performance comparison across segmentation tools
| Metric | FreeSurfer | FastSurfer | Neurophet AQUA |
|---|---|---|---|
| Processing Time | 5-20 hours [112] | ~1 minute (volumetric), ~60 minutes (full pipeline) [37] [113] | ~5 minutes [93] |
| Dice Score (Cortical) | >0.8 [93] | >0.8 [37] [112] | >0.8 [93] |
| Dice Score (Subcortical) | >0.8 [93] | >0.8 [37] [112] | >0.8 [93] |
| Test-Retest ICC (Hippocampus) | 0.869-0.965 [114] [93] | Highly reliable [37] | Comparable to FreeSurfer [93] |
| Volume Difference (%) 1.5T-3T | >10% (most regions) [93] | Information missing | <10% (most regions) [93] |
| Segmentation Quality | Hippocampal encroachment on ventricles [93] | Stable connectivity between regions [93] | Stable connectivity, no regional encroachment [93] |
| Field Strength Robustness | Significant differences 3T vs 7T [115] | Higher volumetric estimates at 7T [115] | Information missing |
Reliability and Variability Metrics
Table 2: Reliability assessment across magnetic field strengths and test-retest scenarios
| Reliability Context | FreeSurfer Performance | FastSurfer Performance | Commercial Tools Performance |
|---|---|---|---|
| Test-Retest (3T-3T) | Excellent reliability for most measures (ICC: 0.869-0.965) [114] | High test-retest reliability [37] | Information missing |
| Cross-Field Strength (1.5T-3T) | Statistically significant differences for several regions, small-moderate effect sizes [93] | Information missing | Statistically significant differences for most regions, small effect sizes [93] |
| Training Variability | N/A (deterministic pipeline) | Comparable to FreeSurfer, exploitable for data augmentation [116] | Information missing |
| Entorhinal Cortex Reliability | Lower reliability (requires n=347 for 1% change detection) [114] | Information missing | Information missing |
| Sample Size for 1% Change Detection (Hippocampus) | n=69 [114] | Information missing | Information missing |
Experimental Protocols and Validation
Standardized Validation Methodologies
To ensure fair comparison across tools, researchers employ standardized validation protocols:
Multi-Center Dataset Validation: Studies typically utilize diverse datasets including Alzheimer's Disease Neuroimaging Initiative (ADNI), Open Access Series of Imaging Studies (OASIS), and internal cohorts to assess generalizability. These datasets encompass varying demographics, scanner manufacturers, magnetic field strengths, and clinical conditions (cognitively normal, mild cognitive impairment, dementia) [37] [93].
Segmentation Accuracy Protocol: The standard methodology involves calculating Dice Similarity Coefficients (DSC) between tool outputs and manual segmentations created by expert radiologists. The DSC is calculated as twice the area of overlap divided by the total number of voxels in both segmentations, with values ranging from 0 (no overlap) to 1 (perfect overlap) [93].
Reliability Assessment Protocol: Test-retest reliability is assessed by scanning participants twice within a short interval (typically same day to 180 days) using the same scanner or different field strengths. Reliability is quantified using intraclass correlation coefficients (ICC), mean absolute differences, and effect sizes to determine measurement consistency [114] [93].
Statistical Analysis for Group Differences: Sensitivity to biologically plausible effects is tested by comparing known groups (e.g., dementia patients vs. controls). Statistical methods include linear regression models adjusting for covariates like age, sex, and intracranial volume, with evaluation of effect sizes and statistical power [37] [117].
Experimental Workflow
Figure 2: Standardized experimental workflow for comparative tool evaluation showing parallel processing and multi-dimensional assessment methodology.
The Scientist's Toolkit
Essential Research Reagents and Materials
Table 3: Key resources for neuroimaging tool evaluation and implementation
| Resource Category | Specific Examples | Research Function |
|---|---|---|
| Reference Datasets | ADNI, OASIS, AIBL, Rhineland Study [93] [112] | Provide standardized, well-characterized data for tool validation and comparison across institutions |
| Quality Control Tools | FreeSurfer QC tools, FastSurfer QC companion tools [37] | Enable detection of segmentation failures and artifacts through visual inspection and automated metrics |
| Validation Metrics | Dice Similarity Coefficient, Intraclass Correlation, Hausdorff Distance [37] [93] | Quantitatively assess segmentation accuracy and measurement reliability |
| Computational Infrastructure | GPU clusters (NVIDIA), High-performance computing systems [118] [112] | Accelerate processing times, particularly for deep learning methods requiring GPU acceleration |
| Bias Correction Tools | ANTs N4 algorithm, SynthStrip [115] | Improve image quality and segmentation accuracy, especially at higher field strengths |
| Statistical Analysis Packages | R, Python with specialized neuroimaging libraries | Perform group comparisons, covariance adjustment, and statistical power calculations |
Based on comprehensive evaluation across multiple performance dimensions:
For large-scale studies and time-sensitive applications: FastSurfer provides the most advantageous balance of speed and accuracy, offering 300-1000x faster volumetric processing with comparable accuracy to FreeSurfer. Its slightly higher variability can be strategically leveraged as a data augmentation strategy to improve downstream predictive models [116] [37] [117].
For established morphometric pipelines requiring extensive validation: FreeSurfer remains the gold standard with the most comprehensive validation history and extensive literature support. Its excellent reliability for most measures (though lower for entorhinal cortex) makes it suitable for longitudinal studies, despite substantial computational demands [114] [93].
For clinical applications and field strength variability challenges: Commercial solutions like Neurophet AQUA show promising performance with superior robustness to magnetic field strength variations, potentially offering more consistent measurements across scanner upgrades and multi-center studies [93].
For ultra-high field imaging (7T and beyond): Both FreeSurfer and FastSurfer show specific limitations at 7T, with significant volumetric differences compared to 3T. FastSurfer typically produces higher volumetric estimates at 7T, while FreeSurfer demonstrates segmentation inconsistencies in hippocampal subfields. Additional pre-processing with advanced bias correction is recommended for ultra-high field applications [115].
The choice between these tools should be guided by specific research priorities: validation history and reliability (FreeSurfer), processing speed and scalability (FastSurfer), or clinical readiness and robustness to acquisition parameters (commercial solutions). For comprehensive research programs, a multi-tool approach leveraging the respective strengths of each platform may provide the most robust analytical framework.
In brain imaging research, the pooling of data from multiple scanner sites is essential for achieving the large sample sizes needed to study rare conditions and to enhance the generalizability of findings [119] [120]. However, this approach introduces a significant confounding variable: interscanner variability. Differences in hardware (manufacturer, model, field strength), acquisition software, and imaging protocols across sites can lead to systematic discrepancies in the derived metrics [121] [122]. These inconsistencies manifest as added noise, which can obscure genuine biological signals, or worse, as bias that may lead to erroneous conclusions in both clinical trials and observational studies. The reliability of multisite data is therefore paramount, and multicenter calibration comprises the strategies and tools employed to ensure that measurements are comparable, reliable, and valid across different scanner platforms.
The science of metrology—the science of measurement—provides the essential framework for this endeavor. In any quantitative field, a measurement result is not considered complete without an statement of its associated uncertainty [121]. Quantitative MRI (qMRI) aims to extract objective numerical values (quantitative imaging biomarkers, or QIBs) from images, such as tissue volume, relaxation times (T1, T2), or the apparent diffusion coefficient (ADC) [121] [123]. For these measures to be trusted, especially when used to inform clinical decisions or evaluate drug efficacy, the bias and reproducibility of the measurement process must be thoroughly understood and controlled [121]. Multicenter calibration directly addresses this by establishing traceability and quantifying measurement uncertainty, thereby transforming MRI from a predominantly qualitative art into a rigorous quantitative science [121] [123].
Scanner variability arises from a complex interplay of factors throughout the image acquisition and processing chain. Recognizing these sources is the first step in mitigating their effects.
Hardware and Acquisition Differences: Different MRI scanners from various manufacturers, and even different models from the same manufacturer, operate at different magnetic field strengths (e.g., 1.5 T vs. 3 T) and have unique gradient performance and radiofrequency coil configurations [121]. These hardware differences directly influence fundamental image properties like signal-to-noise ratio (SNR) and spatial uniformity [122] [76]. Furthermore, the use of different imaging protocols and parameters (e.g., repetition time [TR], echo time [TE]) between sites is a major source of contrast variation [8].
Artifacts: MRI is susceptible to a wide range of artifacts that can degrade image quality and quantification. These include patient-related artifacts such as motion, which can cause blurring or ghosting [124] [76], and hardware-related artifacts like main magnetic field (B0) inhomogeneity or gradient nonlinearities, which can induce geometric distortions and intensity non-uniformities [124]. While some artifacts can be minimized with careful protocol design, others are inevitable and must be corrected for.
Data Processing and Analysis Variations: The choice of software pipeline for tasks such as image segmentation, registration, and parameter mapping (e.g., for T1 or ADC) can introduce significant variability. For example, a study comparing five automated methods for segmenting white matter hyperintensities (WMHs) found that performance varied markedly across scanners, with the spatial correspondence (Dice similarity coefficient) of the best-performing method ranging from 0.70 to 0.76 depending on the scanner, while poorer-performing methods showed even greater inconsistency [119]. This highlights that the analysis algorithm itself is a critical component of the measurement chain.
The impact of this variability is profound. In functional MRI (fMRI) studies, it can reduce the statistical power to detect true brain activation, potentially requiring larger sample sizes to compensate [120]. In structural and quantitative MRI, it can introduce bias in the measurement of biomarkers, making it difficult to track longitudinal changes, such as tumor volume in therapy response or brain atrophy in neurodegenerative disease [121] [123]. Ultimately, without adequate calibration, the value of pooled multicenter data is diminished.
Core Multicenter Calibration Methodologies
Several key methodologies form the backbone of multicenter calibration, each targeting different aspects of the variability problem. The following diagram illustrates the logical relationship and application of these core methodologies within a research workflow.
Phantom-Based Calibration
The use of reference objects, or phantoms, is a foundational calibration method. Phantoms are objects with known, stable physical properties that are scanned periodically to monitor scanner performance.
Purpose and Role: Phantoms serve to disentangle scanner-related variance from biological variance. By scanning the same object on different machines, researchers can directly measure interscanner bias and variance for specific quantitative parameters like T1, T2, and ADC [121] [123]. This allows for the creation of correction factors or the exclusion of scanners that perform outside acceptable tolerances.
Experimental Protocol: The typical protocol involves imaging a standardized phantom, such as the ISMRM/NIST system phantom, at each participating site using a harmonized acquisition protocol [123]. The resulting images are analyzed with dedicated software to extract quantitative values from regions of interest within the phantom. These values are then compared against the known ground truth values and against measurements from other scanners. This process was used to validate a prostate cancer prediction model based on qMRI data, ensuring consistency across sites [123].
Advanced Phantoms: Current research is driving the development of more sophisticated "anthropomorphic" phantoms that better mimic human tissue and its complex properties. Future needs, as identified by experts at NIST workshops, include phantoms that are sensitive to magnetization transfer, contain physiologically relevant values of multiple parameters (T1, T2, ADC) in each voxel, and can simulate dynamic processes like physiological motion [123].
Traveling Subject Protocols
Traveling subject (or "traveling human") studies are considered the gold standard for assessing the total variability in a multicenter pipeline, as they incorporate all sources of variance, including those related to the human subject.
Purpose and Role: This method involves scanning the same group of healthy volunteers at all participating imaging sites. It provides a direct measure of the reliability of the entire measurement chain—from scanner hardware to image processing—for in vivo data [8] [122] [120].
Experimental Protocol: A key example is the North American Prodrome Longitudinal Study (NAPLS), where one participant from each of eight sites traveled to all other sites for scanning. In this study, fMRI activation during a working memory task was found to be highly reproducible, with generalizability intra-class correlation coefficients (ICCs) of 0.81 for the left dorsolateral prefrontal cortex and 0.95 for the left superior parietal cortex across sites and days [120]. Another public dataset, the Consortium for Reliability and Reproducibility (CoRR), includes test-retest scans from 61 individuals across multiple sites to assess the long-term reliability of structural and functional MRI measures [8].
Post-Processing Harmonization
When phantom or traveling subject data reveal significant site-related variance, statistical and computational methods can be applied to the data post-hoc to minimize these effects.
Purpose and Role: These algorithms aim to "harmonize" data from different sources by removing the site-specific variance while preserving the biological signal of interest. This is particularly important for large, retrospective analyses that pool existing data from studies with different acquisition protocols.
Experimental Protocols:
- Image-Based Meta-Analysis (IBMA) and Mixed Effects Models: In the NAPLS fMRI study, both IBMA and a mixed-effects model with a site covariance term were successfully used to aggregate data across eight sites. The results showed a 96% spatial overlap in the detected activation patterns, validating both approaches for multisite data pooling [120].
- Reliability Mapping: For structural studies, methods have been developed to create brain maps that visualize the reliability of measures like cortical thickness across sites. These maps can show the "effective number of subjects" in a pooled dataset, which in some brain regions can reach the theoretical maximum, while in less reliable regions (e.g., around the thalamus), the effective sample size is reduced [122].
Real-Time Motion Correction Using External Sensors
Patient motion is a major source of artifact that can vary in severity and type across scanning sessions and sites. External hardware sensors offer a proactive solution.
Purpose and Role: Devices such as optical cameras, inertial measurement units, and classic respiratory bellows can monitor subject motion in real-time. This information is used to either prospectively adjust the imaging plane during acquisition or retrospectively correct the images during reconstruction [125]. This reduces blurring and ghosting artifacts, leading to more reliable and comparable images across sites.
Experimental Protocol: In a typical setup, a camera is mounted to track the position of a marker placed on the subject's head. The motion data, describing six degrees of freedom (translation and rotation), are fed to the scanner with low latency. For rigid-body motion like head movement, the imaging plane can be updated in real-time to track the anatomy [125]. This method is highly effective in neuroimaging and is increasingly used in clinical and research settings to ensure data quality.
Quantitative Comparison of Calibration Methods
The following table summarizes the key characteristics, strengths, and limitations of the primary multicenter calibration approaches.
Table 1: Comparative Analysis of Multicenter Calibration Methodologies
| Calibration Method | Primary Application | Key Measured Outputs | Strengths | Limitations |
|---|---|---|---|---|
| Phantom-Based Calibration [121] [123] | Scanner performance monitoring and qMRI parameter validation | T1, T2, ADC values, signal uniformity, geometric distortion | Directly quantifies scanner-specific bias; stable and repeatable; does not require human subjects. | Does not capture sequence-specific or patient-related (e.g., motion) variability. |
| Traveling Subject Protocols [8] [120] | Assessing total system variability for in vivo measurements | Intra-class correlation coefficient (ICC), Dice similarity coefficient, generalizability theory coefficients | Gold standard for measuring reliability of the entire pipeline, including biological variance. | Logistically complex, expensive, and time-consuming; results are specific to the protocols used. |
| Post-Processing Harmonization [122] [120] | Statistical correction of site effects in pooled datasets | Harmonized biomarker values (e.g., cortical thickness, fMRI activation maps) | Can be applied retrospectively to existing datasets; no additional data acquisition required. | Relies on statistical models and assumptions; may not fully remove site effects without biological signal loss. |
| Real-Time Motion Correction [125] | Mitigation of patient-motion artifacts during acquisition | Motion-corrected structural and functional images | Directly addresses a major source of data corruption; improves image quality and measurement reliability. | Requires additional hardware and integration; primarily addresses one type of variability (motion). |
The Researcher's Toolkit for Multicenter Calibration
Implementing a robust multicenter calibration strategy requires a suite of tools and resources. The following table details essential components of the calibration toolkit.
Table 2: Essential Research Reagents and Tools for Multicenter Calibration
| Tool Category | Specific Examples | Function and Purpose |
|---|---|---|
| Reference Phantoms [123] | ISMRM/NIST system phantom; QIBA/NIH/NIST diffusion phantom; Anthropomorphic prostate phantom | Provide known, stable references for quantifying scanner performance and validating quantitative imaging biomarkers (QIBs) across sites and time. |
| Public Datasets [8] | Consortium for Reliability and Reproducibility (CoRR); Alzheimer's Disease Neuroimaging Initiative (ADNI) | Provide test-retest, multisite data to assess the reliability of MRI measures and develop new harmonization algorithms. |
| Software Pipelines [119] | kNN-TTP, LST-LPA for WMH segmentation; FSL, FreeSurfer, SPM for general analysis | Automated tools for image processing. Their performance and consistency across scanners must be validated (e.g., kNN-TTP showed highest consistency for WMH segmentation [119]). |
| External Sensors [125] | Optical motion tracking systems (e.g., Moiré Phase Tracking); inertial measurement units (IMUs); respiratory bellows; ECG | Monitor physiological motion and subject head movement in real-time to enable prospective or retrospective motion correction, thereby reducing a key source of artifact. |
| Quality Assessment Tools [76] | Automated SNR analysis; background artifact detection (e.g., QI1, QI2 indices) | Provide automated, objective assessment of image quality to identify scans corrupted by artifacts, enabling rapid decision-making about scan repetition. |
The pursuit of reliable and reproducible brain imaging in a multicenter context is a multifaceted challenge, but it is not insurmountable. As detailed in this guide, a robust arsenal of calibration methodologies exists, from fundamental phantom-based monitoring to advanced traveling subject protocols and sophisticated statistical harmonization. The evidence is clear: without such rigorous calibration, the inherent variability between MRI scanners can severely undermine the statistical power and validity of a study. However, when these approaches are conscientiously applied, as demonstrated in successful multisite consortia, they enable the generation of high-quality, comparable data that is essential for driving discoveries in neuroscience and drug development. The future of the field lies in the widespread adoption and continued refinement of these standards, the development of more biologically relevant phantoms, and the integration of real-time quality control measures, all of which will solidify quantitative MRI as a truly reliable tool for science and medicine.
The reliability of brain imaging methods is a cornerstone of both dementia research and clinical practice. Magnetic Resonance Imaging (MRI) is indispensable for diagnosing dementia subtypes, monitoring disease progression, and, increasingly, for determining eligibility for disease-modifying therapies. A significant challenge in traditional MRI is the extended scan time, which can be burdensome for patients with cognitive impairment and limit scanner throughput. In response, accelerated MRI sequences have been developed to drastically reduce acquisition times. This guide objectively compares the performance of these accelerated protocols against conventional sequences, framing the analysis within the broader thesis of validating imaging method reliability for robust scientific and clinical application. The comparison is vital for researchers and drug development professionals who require both efficiency and uncompromised data integrity in longitudinal studies and clinical trials.
Methodological Approaches
Conventional MRI Protocols in Dementia
Conventional MRI protocols for dementia assessment rely on high-resolution structural sequences to identify characteristic patterns of brain atrophy and vascular pathology.
- Standard Sequences: A typical diagnostic protocol includes 3D T1-weighted (T1w) images for volumetric analysis and 3D Fluid-Attenuated Inversion Recovery (FLAIR) for evaluating white matter hyperintensities (WMHs) [126] [127].
- Visual Rating Scales: Clinicians often use standardized visual scales to assess scans. These include the Medial Temporal Lobe Atrophy (MTA) scale for Alzheimer's disease, the Global Cortical Atrophy (GCA) scale, the Fazekas scale for WMHs, and the Koedam scale for posterior parietal atrophy [127].
- Quantitative Analysis: For research and advanced clinical use, automated software tools (e.g., FSL, FreeSurfer) perform voxel-based morphometry, cortical thickness measurements, and segmentation of hippocampal and other subcortical volumes [128].
Accelerated MRI Sequences
Accelerated MRI aims to preserve the diagnostic information of conventional sequences while significantly reducing scan time. Two primary technological principles enable this speed:
- Compressed Sensing (CS): This technique exploits the inherent sparsity or compressibility of the MR signal in a transform domain, allowing for the reconstruction of images from undersampled data [126].
- Parallel Imaging (pMRI): Methods like SENSE and GRAPPA use spatial information from multiple receiver coils to simultaneously collect data, thereby accelerating acquisition [126]. Advanced techniques like wave-CAIPI further enhance acceleration capabilities [129].
These methods are often combined (e.g., CS-SENSE) in accelerated sequences for T1w and FLAIR imaging, achieving scan time reductions of 46% to 63% [126] [129] [130].
Table 1: Key Acceleration Techniques and Their Principles
| Technique | Underlying Principle | Key Application in Dementia |
|---|---|---|
| Compressed Sensing (CS) | Acquires fewer data points by exploiting image sparsity; uses iterative reconstruction. | Reducing acquisition time for 3D T1w and FLAIR sequences. |
| Parallel Imaging (pMRI) | Uses multiple receiver coils to simultaneously acquire data, filling k-space faster. | Accelerating structural imaging protocols (e.g., via SENSE, GRAPPA). |
| Wave-CAIPI | A advanced pMRI method that introduces corkscrew-like gradients to better separate coil signals. | Enabling ultra-fast protocols for diagnosis and treatment monitoring [129]. |
Performance Comparison: Diagnostic and Quantitative Reliability
Recent rigorous studies directly compare conventional and accelerated sequences, moving beyond technical feasibility to assess real-world diagnostic reliability.
Diagnostic Agreement and Visual Rating
Prospective, blinded studies demonstrate that accelerated protocols are non-inferior to standard-of-care scans for primary diagnostic tasks.
- The ADMIRA study (Accelerated Magnetic Resonance Imaging for Alzheimer's disease), a prospective real-world study, found that a fast protocol reducing scan time by 63% showed non-inferior reliability for diagnosis, visual scale ratings (e.g., MTA), and assessment for disease-modifying therapy eligibility. The intra-rater reliability between scan types was high [129] [130].
- A 2025 reliability assessment on 46 dementia patients demonstrated "excellent concordance" in the quantification of brain structures and white matter lesions between conventional and accelerated T1w and FLAIR sequences. The image quality of accelerated sequences showed high agreement with conventional references using metrics like the structural similarity index [126] [131].
Quantitative Volumetric and Feature Concordance
For research applications that depend on precise measurements, the agreement between sequences is critical. The evidence indicates that accelerated sequences reliably produce quantitative data.
- The same 2025 study reported high intraclass correlation and Dice similarity coefficients, confirming that volumes of key brain structures and white matter lesions derived from accelerated sequences are nearly identical to those from conventional scans [126].
- Furthermore, a 2021 study on multimodal MRI highlighted that specific metrics from advanced sequences—such as volume of the left frontal pole, perfusion of the left hippocampus, and fractional anisotropy of the forceps major—are highly sensitive for differentiating dementia subtypes [128]. The reliability of accelerated sequences in providing such data underpins their research utility.
Table 2: Summary of Key Comparative Study Findings
| Study (Year) | Study Design | Scan Time Reduction | Key Finding on Reliability |
|---|---|---|---|
| ADMIRA (2025) [129] [130] | Prospective, blinded, real-world | 63% | Non-inferior reliability for diagnosis, visual ratings, and therapy eligibility. |
| Reliability Assessment (2025) [126] [131] | Methodological comparison | 51% (T1), 46% (FLAIR) | Excellent concordance in quantifying brain structure volumes and white matter lesions. |
| Multimodal MRI (2021) [128] | Diagnostic accuracy | Not Applicable (Conventional) | Identified specific regional volumetrics and DTI metrics as key differentiators for dementia. |
Implications for Research and Clinical Trials
The validation of accelerated MRI sequences has profound implications for the future of dementia research and drug development.
- Improved Feasibility and Equity: Faster scans can potentially double daily scanner throughput, reducing costs and patient wait times. This makes MRI more accessible, helping to address the "postcode lottery" in dementia diagnosis and facilitating more inclusive recruitment for trials [130].
- Enhanced Patient Comfort and Data Quality: Shorter scans are less daunting and easier to tolerate, especially for anxious or cognitively impaired patients. This improves patient compliance and reduces motion artifacts, leading to higher-quality data [126] [130].
- Support for Novel Endpoints: The reliability of quantitative markers from accelerated scans supports their use in clinical trials. For instance, a brain-age clock called DunedinPACNI, which estimates biological aging from a single T1-weighted MRI, has shown that faster brain aging predicts progression to MCI or dementia [132]. Such tools could serve as sensitive endpoints in prevention trials.
The Scientist's Toolkit
The following table details essential reagents and software solutions used in the featured experiments for validating and utilizing MRI in dementia research.
Table 3: Essential Research Reagents and Solutions for MRI-based Dementia Studies
| Item Name | Function/Application | Relevance to Validation |
|---|---|---|
| 3T MRI Scanner | High-field magnetic resonance imaging system. | Platform for acquiring both conventional and accelerated sequences; essential for protocol comparison [126]. |
| Accelerated Sequence Software | Implementation of CS, pMRI (e.g., SENSE, GRAPPA, wave-CAIPI). | Enables reduced scan time; the core technology under validation [126] [129]. |
| Visual Rating Scales (MTA, GCA, Fazekas) | Standardized qualitative assessment of atrophy and vascular load. | Provides the clinical ground truth for establishing diagnostic non-inferiority of accelerated protocols [127]. |
| FSL (FMRIB Software Library) | Brain image analysis toolbox (e.g., for voxel-based morphometry, DTI analysis). | Used for quantitative analysis and feature extraction from both conventional and accelerated images [128]. |
| Automated Segmentation Software (e.g., FreeSurfer, NeuroQuant) | Quantifies volumes of specific brain structures (hippocampus, etc.). | Generates objective, quantitative metrics to assess concordance between sequence types [126] [132]. |
Experimental Workflow and Logical Pathway
The following diagrams illustrate the core experimental workflow for sequence validation and the logical decision pathway for researchers considering accelerated MRI.
Experimental Workflow for MRI Sequence Validation
Decision Logic for Adopting Accelerated MRI
The comprehensive validation of accelerated MRI sequences against conventional protocols demonstrates a compelling balance between efficiency and reliability. Quantitative evidence confirms that accelerated T1w and FLAIR sequences provide excellent concordance for structural volumetry and lesion load quantification, while prospective clinical studies affirm their non-inferiority for diagnostic tasks and treatment eligibility assessment. For the research and drug development community, the adoption of accelerated protocols promises enhanced participant comfort, reduced costs, improved scalability of studies, and reliable data for both traditional and novel endpoints. While context-specific factors may occasionally necessitate conventional scans, accelerated MRI represents a validated, transformative tool for advancing dementia research and clinical practice.
In the field of brain imaging research, the reliability and reproducibility of measurements are foundational to scientific and clinical progress. Whether validating a new automated segmentation algorithm against a manual gold standard or assessing the consistency of radiologists' evaluations, researchers require robust statistical methods to quantify agreement and reliability. Three cornerstone techniques dominate this landscape: Bland-Altman analysis for assessing agreement between two measurement methods, the Dice Score for evaluating spatial overlap in image segmentation, and the Intraclass Correlation Coefficient (ICC) for measuring reliability among raters or instruments. Within the broader context of a thesis on brain imaging method reliability, this guide provides an objective comparison of these analytical techniques. It details their experimental protocols, presents synthesized quantitative data, and outlines the essential computational toolkit required for their application, offering a structured framework for their use in drug development and clinical research.
The table below summarizes the key characteristics, applications, and interpretations of the three primary statistical validation methods.
Table 1: Comparison of Bland-Altman Analysis, Dice Score, and Intraclass Correlation Coefficient
| Feature | Bland-Altman Analysis | Dice Score (Dice Similarity Coefficient) | Intraclass Correlation Coefficient (ICC) |
|---|---|---|---|
| Primary Purpose | Assess agreement between two quantitative measurement methods [133] [134] | Measure spatial overlap/volumetric agreement between two segmentations (e.g., automated vs. manual) [135] [136] | Quantify reliability or consistency between two or more raters or measurements [137] [1] [138] |
| Common Contexts in Brain Imaging | Comparing a new MRI quantification tool against an established standard; validating scanner performance [134] | Validating automated tumor or tissue segmentation (e.g., on MRI or CT) against a manual ground truth [135] [139] | Evaluating inter-rater reliability of radiologists; test-retest reliability of an imaging biomarker [137] [140] [141] |
| Output Interpretation | Limits of Agreement (LoA): Mean difference ± 1.96 × SD of differences. Clinical acceptability is domain-specific [133] [134]. | Range: 0 to 1. Closer to 1 indicates better overlap. Values >0.9 are often considered excellent [135]. | Range: 0 to 1. <0.5: Poor; 0.5-0.75: Moderate; 0.75-0.9: Good; >0.9: Excellent reliability [137] [138]. |
| Key Strengths | Visualizes bias and magnitude of differences across the measurement range; not misled by high correlation alone [133] [134]. | Robust to class imbalance in segmentation tasks; directly interpretable for voxel-wise accuracy [135] [136]. | Distinguishes between different sources of variance (between-subject vs. between-rater); flexible models for various experimental designs [137] [1]. |
| Key Limitations | Does not provide a single summary statistic; interpretation of LoA requires clinical judgement [134]. | Does not provide information on the spatial location or shape of errors [136]. | Sensitive to underlying statistical assumptions (e.g., normality); value is influenced by between-subject variability in the sample [141]. |
Experimental Protocols for Brain Imaging Studies
Protocol for Bland-Altman Agreement Analysis
The Bland-Altman method is used when the goal is to understand the agreement between two measurement techniques, such as comparing a novel, faster MRI analysis pipeline against a established but slower manual method [134].
- Data Collection: Obtain paired measurements from the same set of subjects or images using two different methods (e.g., Method A and Method B). For instance, measure the volume of a brain structure like the hippocampus using both a new automated tool and manual tracing by an expert radiologist across a cohort of 50 patients [133].
- Calculation of Differences and Means: For each pair of measurements, calculate:
- Statistical Summary: Compute the mean difference (( \bar{d} )), which estimates the bias between methods, and the standard deviation (SD) of the differences [134].
- Establish Limits of Agreement: Calculate the 95% limits of agreement:
- Assumption Checking: Test the differences for normality using a statistical test (e.g., Shapiro-Wilk) or a histogram/QQ-plot. If the differences are not normally distributed, consider a data transformation (e.g., logarithmic) [133] [134].
- Visualization and Interpretation: Create the Bland-Altman plot by scattering the average (( \bar{x}i )) on the x-axis against the difference (( di )) on the y-axis. Plot the mean difference line and the upper and lower LoA lines. Analyze the plot for any systematic patterns, such as increasing variance with magnitude (heteroscedasticity) [133] [134].
Protocol for Dice Score Calculation in Segmentation
The Dice Score is the standard metric for evaluating the performance of image segmentation algorithms, such as automated brain tumor delineation on MRI scans [135] [136].
- Ground Truth and Prediction Definition: Establish a ground truth segmentation, which is typically a manually drawn mask by an expert radiologist. This serves as the reference standard. The segmentation to be evaluated (the prediction) is generated by an automated algorithm [135].
- Voxel-wise Comparison: For binary segmentation masks, identify the number of voxels in the following categories:
- True Positives (TP): Voxels correctly identified as the target structure by both the prediction and ground truth.
- False Positives (FP): Voxels incorrectly identified as the target structure by the prediction.
- False Negatives (FN): Voxels that are the target structure but were missed by the prediction [135] [136].
- Dice Score Calculation: Apply the formula: ( \text{Dice Score} = \frac{2 \times |X \cap Y|}{|X| + |Y|} = \frac{2 \times TP}{2 \times TP + FP + FN} ) Here, ( X ) is the set of voxels in the predicted segmentation and ( Y ) is the set in the ground truth segmentation [135] [136].
- Reporting: Report the mean Dice score across all test images or subjects. It is also good practice to report the standard deviation or range to communicate the variability in performance. For example, a study on brain MRI segmentation achieved a Dice score of 0.95, indicating excellent overlap between the automated and manual segmentations [135].
Protocol for Intraclass Correlation Coefficient (ICC) Analysis
ICC is used to evaluate the reliability of measurements, such as the consistency of volume measurements made by multiple raters or the test-retest reliability of a quantitative imaging biomarker [137] [141].
- Study Design and Data Collection: Define the reliability question (inter-rater, test-retest, etc.). For inter-rater reliability, multiple raters (e.g., three radiologists) measure the same set of images or subjects. The measurements should be performed independently and ideally in a blinded fashion [140] [141].
- Selection of the Appropriate ICC Model: The choice of model is critical and is guided by the experimental design [137] [138]:
- One-Way Random Effects: Use when each subject is rated by a different, random set of raters (rare in clinical practice).
- Two-Way Random Effects: Use when a random sample of raters is selected, and all rate all subjects. The results are intended to be generalized to any rater with similar characteristics. This is common for evaluating clinical assessment tools. The definition can be "absolute agreement" or "consistency" [137].
- Two-Way Mixed Effects: Use when the specific raters in the study are the only raters of interest, and results should not be generalized to others. The definition can be "absolute agreement" or "consistency" [137].
- Statistical Analysis: Perform the ICC calculation using the selected model. This is typically done using Analysis of Variance (ANOVA) to partition the total variance into between-subject variance and error (e.g., between-rater) variance. The ICC is then calculated as ( ICC = \frac{\sigma{b}^{2}}{\sigma{b}^{2} + \sigma{w}^{2}} ), where ( \sigma{b}^{2} ) is the variance between subjects and ( \sigma_{w}^{2} ) is the variance within subjects (error) [137] [1] [141].
- Reporting: Report the ICC point estimate, its 95% confidence interval, the model used (e.g., "two-way random effects for absolute agreement"), and the statistical software. For example, a nerve ultrasound study reported interrater ICCs to distinguish between trained and untrained operators [140].
Visualizing Analysis Workflows
The following diagram illustrates the logical decision process for selecting the appropriate statistical validation method based on the research question.
Figure 1: A flowchart for selecting the appropriate statistical validation method based on the research objective.
The workflow for implementing a Bland-Altman analysis, from data preparation to final interpretation, follows a structured sequence of steps.
Figure 2: A step-by-step workflow for conducting and interpreting a Bland-Altman analysis.
Quantitative Data Synthesis from Literature
The following table synthesizes real-world performance data for these metrics from recent brain imaging studies, providing benchmarks for expected outcomes.
Table 2: Synthesized Performance Data from Brain Imaging Studies
| Study Context | Metric | Reported Value | Interpretation & Notes |
|---|---|---|---|
| Brain MRI Tumor Segmentation [135] | Dice Score | 0.95 | Excellent overlap between automated segmentation and ground truth. Achieved using a U-Net with ResNet backbone. |
| Brain Region Segmentation (CT vs. MRI) [139] | Dice Score | 0.978 (Left Basal Ganglia) 0.912 (Right Basal Ganglia) | High scores for some structures, but others performed poorly, showing structure-dependent performance. |
| Brain Region Segmentation (CT vs. MRI) [139] | ICC (for volume agreement) | 0.618 (Left Hemisphere) 0.654 (Right Hemisphere) | Moderate reliability for hemisphere volumes, but poor agreement for other regions, indicating modality differences. |
| Nerve Ultrasound (Operator Reliability) [140] | ICC | Varied by operator expertise | Used alongside Bland-Altman to distinguish between trained and untrained operators. |
| Shared Decision Making (Observer OPTION5) [141] | ICC | 0.821, 0.295, 0.644 (Study-specific) | Highlights how ICC can vary substantially across studies and populations. |
For researchers embarking on reliability studies, the following table lists key software solutions and their functions.
Table 3: Key Research Reagent Solutions for Statistical Validation
| Tool / Resource | Function / Application | Example Use Case |
|---|---|---|
| Statistical Software (R, Python, Stata) | Provides libraries/packages for calculating ICC, generating Bland-Altman plots, and performing supporting statistical tests (e.g., normality). | R: Use the irr or psych package for ICC. Python: Use pingouin for ICC and scikit-learn for Dice score [138] [141]. |
| Medical Image Analysis Platforms (NiftyNet) | Offers deep learning platforms with built-in segmentation metrics, including the Dice Score, for evaluating model performance [136]. | Training and validating a convolutional neural network for brain tumor segmentation on MRI datasets [135] [136]. |
| Atlas Labeling Tools (BrainSuite) | Provides well-established, atlas-based methods for generating ground truth segmentations in MRI, which can be used as a reference for validating new methods [139]. | Segmenting eight brain anatomical regions (e.g., basal ganglia, cerebellum) in MRI to compare against a new CT segmentation method [139]. |
| Deep Learning Frameworks (TensorFlow, PyTorch) | Enable the implementation and training of custom segmentation networks (e.g., U-Net, DenseVNet) where the Dice Score can be used directly as a loss function [135]. | Implementing a 3D U-Net for automated segmentation of brain regions on head CT images [139]. |
Conclusion
Reliability assessment in brain imaging requires multifaceted approaches addressing scanner, sequence, processing, and biological variables. Evidence demonstrates that convolutional neural networks show promising improvements in numerical uncertainty over traditional methods, while standardized protocols and quality control measures significantly enhance reproducibility. Future directions should focus on developing more robust deep learning tools, establishing universal quality standards for multicenter studies, and creating comprehensive validation datasets. For drug development and clinical research, implementing rigorous reliability assessment protocols will be essential for detecting subtle longitudinal changes and ensuring the validity of imaging biomarkers in therapeutic trials.
References
- 1. - Wikipedia Intraclass correlation [https://en.wikipedia.org/wiki/Intraclass_correlation]
- 2. - MedCalc Manual Intraclass correlation coefficient [https://www.medcalc.org/en/manual/intraclass-correlation-coefficient.php]
- 3. A Guideline of Selecting and Reporting Intraclass ... Correlation [https://pubmed.ncbi.nlm.nih.gov/27330520/]
- 4. Coefficient of variation - Wikipedia [https://en.wikipedia.org/wiki/Coefficient_of_variation]
- 5. of two dependent within subject Comparison ... coefficients of variation [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-8-24]
- 6. Standardization of brain MR images across machines and protocols: bridging the gap for MRI-based radiomics | Scientific Reports [https://www.nature.com/articles/s41598-020-69298-z]
- 7. Reliability of brain volume measurements: A test-retest dataset | Scientific Data [https://www.nature.com/articles/sdata201437]
- 8. A test-retest dataset for assessing long-term reliability of brain morphology and resting-state brain activity | Scientific Data [https://www.nature.com/articles/sdata201616]
- 9. Importance of test–retest reliability for promoting fMRI based screening and interventions in major depressive disorder | Translational Psychiatry [https://www.nature.com/articles/s41398-021-01507-3]
- 10. in neuroimaging research through intra-class... Assessing reliability [https://elifesciences.org/articles/35718]
- 11. Single subject fMRI test–retest reliability metrics and confounding factors - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1053811912010890]
- 12. Frontiers | Intra- and Inter-Scanner Reliability of Voxel-Wise Whole-Brain Analytic Metrics for Resting State fMRI [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2018.00054/full]
- 13. Frontiers | Harmonization of diffusion MRI on healthy subjects using... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1591169/full]
- 14. The effect of scan length on the reliability of resting-state fMRI connectivity estimates - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4104183/]
- 15. fMRI reliability: Influences of task and experimental design | Cognitive, Affective, & Behavioral Neuroscience [https://link.springer.com/article/10.3758/s13415-013-0195-1]
- 16. The diagnostic potential of resting state functional MRI: Statistical concerns - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12303613/]
- 17. A new virtue of phantom MRI data: explaining... | F1000Research [https://f1000research.com/articles/9-1131]
- 18. in analytical pipelines lead to impactful... Numerical uncertainty [https://pubmed.ncbi.nlm.nih.gov/34724000/]
- 19. Standardized Preprocessing in Neuroimaging : Enhancing Reliability ... [https://link.springer.com/protocol/10.1007/978-1-0716-4260-3_8]
- 20. Introduction — reproducible - neuroimaging 0.0.1 documentation [https://reproducible-neuroimaging.readthedocs.io/en/latest/introduction.html]
- 21. Session 7: Practical Guide to Overcome the Reproducibility in... Crisis [https://training.incf.org/course/session-7-practical-guide-overcome-reproducibility-crisis-small-animal-neuroimaging]
- 22. Components of variance in a multicentre functional MRI study and... [https://pubmed.ncbi.nlm.nih.gov/17680602/]
- 23. Scan-rescan reliability of assessment volumetric analysis... brain [https://pubmed.ncbi.nlm.nih.gov/40813790/]
- 24. Design effect in multicenter : gain or loss of studies ? power [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/1471-2288-9-39]
- 25. CNN Assessing in Analyzing Reliability MRIs - Simple Science Brain [https://scisimple.com/en/articles/2025-10-03-assessing-cnn-reliability-in-analyzing-brain-mris--a9r7r7w]
- 26. The Menstrual Alters Resting-State Cortical Activity... Cycle [https://pmc.ncbi.nlm.nih.gov/articles/PMC8350571/]
- 27. The cycling brain: menstrual cycle related fluctuations in hippocampal and fronto-striatal activation and connectivity during cognitive tasks | Neuropsychopharmacology [https://www.nature.com/articles/s41386-019-0435-3]
- 28. Frontiers | The Menstrual Modulates Whole- Cycle Turbulent... Brain [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2021.753820/full]
- 29. How Hydration Your Affects ( Brain ) – Cogn-IQ.org 2025 [https://www.cogn-iq.org/blog/how-hydration-affects-brain-function/]
- 30. Levels of Hydration and Cognitive Function [https://www.news-medical.net/health/Levels-of-Hydration-and-Cognitive-Function.aspx]
- 31. Does hydration status affect MRI measures of brain volume or water... [https://pubmed.ncbi.nlm.nih.gov/26825048/]
- 32. Neuroimaging the menstrual cycle: A multimodal systematic review - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S0091302220300698]
- 33. Image processing and Quality Control for the first 10,000 brain imaging datasets from UK Biobank - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5770339/]
- 34. What is the best software for processing fMRI data? [https://mriquestions.com/best-fmri-software.html]
- 35. Evaluation of automated brain MR image segmentation and volumetry... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6870639/]
- 36. Accuracy and Reliability of Automated Gray Matter... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0045081]
- 37. FastSurfer [https://deep-mi.org/research/fastsurfer/]
- 38. of automated brain segmentation using a brain phantom... Comparison [https://pubmed.ncbi.nlm.nih.gov/26211622/]
- 39. Disparate voxel based morphometry (VBM) results between SPM and... [https://bmcneurol.biomedcentral.com/articles/10.1186/s12883-015-0274-8]
- 40. Scan-rescan reliability assessment of brain volumetric analysis across scanners and software solutions | Scientific Reports [https://www.nature.com/articles/s41598-025-15283-3]
- 41. MR-CT multi-atlas registration guided by fully automated brain ... [https://link.springer.com/article/10.1007/s11548-022-02786-x]
- 42. A Review on Accelerated Magnetic Resonance Imaging Techniques: Parallel Imaging, Compressed Sensing, and Machine Learning - PubMed [https://pubmed.ncbi.nlm.nih.gov/40759045/]
- 43. AI-assisted compressed and sensing sequences for... parallel imaging [https://link.springer.com/article/10.1007/s00330-023-09742-6]
- 44. Validation of two accelerated 4D flow MRI at... sequences [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-019-0089-2]
- 45. Combination of Compressed Sensing and Parallel Imaging for Highly Accelerated First-Pass Cardiac Perfusion MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2932824/]
- 46. [2502.17174] Unsupervised Accelerated MRI Reconstruction via Ground-Truth-Free Flow Matching [https://arxiv.org/abs/2502.17174]
- 47. of Comparison and controlled aliasing in... compressed sensing [https://pmc.ncbi.nlm.nih.gov/articles/PMC9249804/]
- 48. of 4D flow Accelerated using GRAPPA and... sequences MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC9804839/]
- 49. Real-world diagnostic performance of knee MRI protocols accelerated ... [https://pubmed.ncbi.nlm.nih.gov/41109866/?amp=&myncbishare=nynyumlib&otool=nynyumlib]
- 50. [2503.05051] Accelerated Patient-specific Non-Cartesian MRI Reconstruction using Implicit Neural Representations [https://arxiv.org/abs/2503.05051]
- 51. Accelerated Patient-specific Non-Cartesian Magnetic Resonance Imaging Reconstruction Using Implicit Neural Representations - PubMed [https://pubmed.ncbi.nlm.nih.gov/40915433/]
- 52. The physical and biological basis of quantitative parameters derived... [https://qims.amegroups.org/article/view/1315/1771]
- 53. for Neurocognitive Disorders Quantitative Structural MRI [https://practicalneurology.com/diseases-diagnoses/alzheimer-disease-dementias/quantitative-structural-mri-for-neurocognitive-disorders/31730/]
- 54. - and Structural - DTI enable automated prediction of IDH Mutation... MRI [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-024-01274-9]
- 55. of Integration and Deep Learning: A Novel Paradigm... Multimodal MRI [https://www.dovepress.com/gliomas-analysis-via-multimodal-mri-deep-learning-fusion-technical-inn-peer-reviewed-fulltext-article-AMEP]
- 56. Frontiers | Integration of multimodal imaging data with machine learning for improved diagnosis and prognosis in neuroimaging [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1552178/full]
- 57. Brain Connectivity Analysis with fMRI, Integrated , and sMRI... DTI [https://pmc.ncbi.nlm.nih.gov/articles/PMC11383444/]
- 58. Frontiers | Radiomics prediction of MGMT promoter methylation in adult... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1493666/full]
- 59. Multi-modal machine learning approach for early detection of neurodegenerative diseases leveraging brain MRI and wearable sensor data - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12027105/]
- 60. Frontiers | Imaging biomarkers in optic neuritis: current tools and future... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1666835/full]
- 61. Computational Brain Imaging Framework for Neurological Mapping and Disorder Classification Using Multimodal Image Processing | International Journal of Computational Intelligence Systems [https://link.springer.com/article/10.1007/s44196-025-00852-1]
- 62. Advancing Brain Tumor Analysis: Current Trends, Key Challenges, and Perspectives in Deep Learning-Based Brain MRI Tumor Diagnosis [https://www.mdpi.com/2673-4117/6/5/82]
- 63. control of T1-weighted Automated MRI scans for clinical... quality brain [https://www.psych.ox.ac.uk/publications/2119661]
- 64. in structural Automatic magnetic... quality assessment brain [https://pubmed.ncbi.nlm.nih.gov/19526493/]
- 65. Getting to know EEG artifacts and how to handle them in BrainVision Analyzer [https://pressrelease.brainproducts.com/eeg-artifacts-handling-in-analyzer/]
- 66. ITK-SNAP: an interactive tool for semi-automatic segmentation of multi-modality biomedical images - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5493443/]
- 67. Frontiers | Automated Multiclass Artifact Detection in Diffusion MRI Volumes via 3D Residual Squeeze-and-Excitation Convolutional Neural Networks [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2022.877326/full]
- 68. ITK-SNAP - Wikipedia [https://en.wikipedia.org/wiki/ITK-SNAP]
- 69. Quantitative Brain Imaging-reliability | Frontiers Research Topic [https://www.frontiersin.org/research-topics/25079/quantitative-brain-imaging-reliability]
- 70. What is Imaging Test Phantoms ? Uses, How It Works & Top... [https://www.linkedin.com/pulse/what-imaging-test-phantoms-uses-how-works-top-companies-2025-xucef]
- 71. Reliability of structural MRI measurements: The effects of scan session, head tilt, inter-scan interval, acquisition sequence, FreeSurfer version and processing stream - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8784825/]
- 72. Spectral CT Phantom | A PTW Company [https://www.qrm.de/en/spectral-ct-phantom]
- 73. Comprehensive QA for Modern Imaging Suites – Imaging... Phantoms [https://www.imgsol.com/news/comprehensive-qa-phantoms-for-modern-imaging-suites/]
- 74. of Clinical MRI Quality Using ACR MRI... Assurance Scanners [https://pmc.ncbi.nlm.nih.gov/articles/PMC3047180/]
- 75. Frontiers | Test-Retest Reliability of fMRI Brain Activity during ... [https://www.frontiersin.org/articles/10.3389/fpsyt.2013.00163/full]
- 76. Automatic quality assessment in structural brain magnetic resonance imaging - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2780021/]
- 77. Are Movement Artifacts in Magnetic Resonance Imaging a Real Problem?—A Narrative Review - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5447676/]
- 78. Effect of head -induced motion on the artefacts of deep... reliability [https://pmc.ncbi.nlm.nih.gov/articles/PMC8803940/]
- 79. Simulating rigid head on brain magnitude... | PLOS One motion artifacts [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0301132]
- 80. Estimation of Head in Structural MRI and its Impact on Cortical... Motion [https://arxiv.org/html/2505.23916v2]
- 81. Differences in Head Motion During Functional Magnetic Resonance Imaging Across Pediatric Neuropsychiatric Disorders - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11875158/]
- 82. Estimation and Removal of Residual Motion Artifact in Retrospectively Motion-Corrected fMRI Data: A Comparison of Intervolume and Intravolume Motion Using Gold Standard Simulated Motion Data | Published in Aperture Neuro [https://apertureneuro.org/article/123369-estimation-and-removal-of-residual-motion-artifact-in-retrospectively-motion-corrected-fmri-data-a-comparison-of-intervolume-and-intravolume-motion-u]
- 83. Correction of respiratory artifacts in MRI head motion estimates - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1053811919309917]
- 84. | Alzheimer's Disease Neuroimaging Initiative ADNI [https://adni.loni.usc.edu/]
- 85. A Comparison of Accelerated and Non- accelerated MRI Scans for... [https://link.springer.com/article/10.1007/s12021-017-9326-0]
- 86. ADNI | MRI Numerical Data Sets [https://adni.loni.usc.edu/data-samples/adni-data/neuroimaging/mri/mri-numerical-data-sets/]
- 87. (PDF) A voxel-based morphometry comparison of the... [https://www.academia.edu/121110500/A_voxel_based_morphometry_comparison_of_the_3_0T_ADNI_1_and_ADNI_2_volumetric_MRI_protocols]
- 88. ADNI | Data and Samples [https://adni.loni.usc.edu/data-samples/]
- 89. 5.3 versus 6.0: are volumes comparable? A Chronic Effects... FreeSurfer [https://link.springer.com/article/10.1007/s11682-018-9994-x]
- 90. Different FreeSurfer might generate different statistical... versions [https://pmc.ncbi.nlm.nih.gov/articles/PMC8916973/]
- 91. Frontiers | Development and validation of deep learning-based... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2023.1157738/full]
- 92. ReleaseNotes - Free Surfer Wiki [https://surfer.nmr.mgh.harvard.edu/fswiki/ReleaseNotes]
- 93. Evaluating brain volume segmentation accuracy and reliability of... [https://www.nature.com/articles/s41598-024-74622-y?error=cookies_not_supported&code=890e10f3-31ee-42af-bab5-bfa0dc52aede]
- 94. On brain atlas choice and automatic segmentation methods... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7028906/]
- 95. Reliability assessment of accelerated MR sequences for the estimation of structural and vascular markers in dementia | Scientific Reports [https://www.nature.com/articles/s41598-025-87224-z]
- 96. morphometry reproducibility in multi-center 3 T MRI studies... Brain [https://www.academia.edu/6156903/Brain_morphometry_reproducibility_in_multi_center_3_T_MRI_studies_A_comparison_of_cross_sectional_and_longitudinal_segmentations]
- 97. Longitudinal multi-centre brain imaging studies: guidelines and practical tips for accurate and reproducible imaging endpoints and data sharing | Trials | Full Text [https://trialsjournal.biomedcentral.com/articles/10.1186/s13063-018-3113-6]
- 98. Structure-function relationships in the human aging brain : An account... [https://pubmed.ncbi.nlm.nih.gov/39756333/]
- 99. Frontiers | Study the Longitudinal in vivo and Cross - Sectional ex vivo... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2019.00011/full]
- 100. Frontiers | Cross-Sectional and Longitudinal MRI Brain Scans Reveal Accelerated Brain Aging in Multiple Sclerosis [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2019.00450/full]
- 101. Longitudinal reproducibility of brain and spinal cord quantitative MRI biomarkers - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12319937/]
- 102. Assessment of reliability in functional imaging studies - PubMed [https://pubmed.ncbi.nlm.nih.gov/12655586/]
- 103. What Is the Test-Retest Reliability of Common Task-Functional MRI Measures? New Empirical Evidence and a Meta-Analysis - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7370246/]
- 104. Commentary: A test-retest dataset for assessing long-term reliability of brain morphology and resting-state brain activity - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5319983/]
- 105. Is One Trial Sufficient to Obtain Excellent Pressure Pain Threshold... [https://pubmed.ncbi.nlm.nih.gov/27513474/]
- 106. Intra- and Inter-session Reliability of Static and Dynamic Postural Control in Participants with and without Patellofemoral Pain Syndrome - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4594819/]
- 107. Intra- and Inter-Session Reliability of Methods for Measuring Reaction Time in Participants with and without Patellofemoral Pain Syndrome - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7957103/]
- 108. Intrasession and Intersession Reliability of Running Mechanics During Treadmill Sprints - PubMed [https://pubmed.ncbi.nlm.nih.gov/26356384/]
- 109. - and Intra - inter of electrical detection and pain... session reliability [https://link.springer.com/article/10.1007/s00424-023-02851-7]
- 110. Statistical evaluation of test-retest studies in PET brain imaging - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5809632/]
- 111. INTRA AND INTERSESSION RELIABILITY OF A POSTURAL CONTROL PROTOCOL IN ATHLETES WITH AND WITHOUT ANTERIOR CRUCIATE LIGAMENT RECONSTRUCTION: A DUALâ€TASK PARADIGM - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3537456/]
- 112. FastSurfer - A fast and accurate deep learning based neuroimaging pipeline - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7898243/]
- 113. FastSurfer - A fast and accurate deep learning based neuroimaging pipeline - ScienceDirect [https://www.sciencedirect.com/science/article/pii/S1053811920304985]
- 114. Testâ€retest reliability of FreeSurfer measures of neurodegeneration... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11716006/]
- 115. of brain volumetry in patients with non-lesional epilepsy... Comparison [https://qims.amegroups.org/article/view/144169/html]
- 116. Uncertain but Useful: Leveraging CNN Variability into Data Augmentation [https://arxiv.org/html/2509.05238v1]
- 117. of Automated Volume Extraction with Comparison and... FreeSurfer [https://www.fh-dortmund.de/publikationen/fis.import.pub.de.3023.php?loc=en]
- 118. GitHub - Deep-MI/ FastSurfer : PyTorch implementation of... [https://github.com/Deep-MI/FastSurfer]
- 119. Performance of five automated white matter hyperintensity... [https://www.nature.com/articles/s41598-019-52966-0?error=cookies_not_supported&code=98452be3-c491-4dbf-8330-80e84c5f1d57]
- 120. of Reliability activation... functional magnetic resonance imaging [https://pubmed.ncbi.nlm.nih.gov/24736173/]
- 121. Clinical quantitative MRI and the need for metrology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8010554/]
- 122. Mapping reliability in multicenter : voxel-based morphometry and... MRI [https://pubmed.ncbi.nlm.nih.gov/21086550/]
- 123. Recommendations Towards Standards for Quantitative MRI (qMRI) and Outstanding Needs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6663309/]
- 124. MRI artifacts and correction strategies [https://www.openaccessjournals.com/articles/mri-artifacts-and-correction-strategies-11010.html]
- 125. External hardware and sensors, for improved MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9957809/]
- 126. Reliability assessment of accelerated MR sequences for the estimation of structural and vascular markers in dementia - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12003897/]
- 127. The Radiology Assistant : Dementia - Role of MRI [https://radiologyassistant.nl/neuroradiology/dementia/role-of-mri]
- 128. Translating state-of-the-art brain magnetic resonance imaging (MRI) techniques into clinical practice: multimodal MRI differentiates dementia subtypes in a traditional clinical setting - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8339641/]
- 129. Ultra-fast MRI for dementia diagnosis and treatment eligibility: A prospective study - PubMed [https://pubmed.ncbi.nlm.nih.gov/40501106/]
- 130. Faster MRI offer new hope for scans diagnosis dementia [https://www.alzheimers.org.uk/news/2025-10-13/faster-mri-scans-offer-new-hope-dementia-diagnosis]
- 131. assessment of accelerated MR sequences for the... Reliability [https://pubmed.ncbi.nlm.nih.gov/40240759/]
- 132. Single Brain MRI Reveals Accelerated Aging, Dementia Risk [https://www.medscape.com/viewarticle/single-brain-mri-reveals-accelerated-aging-dementia-risk-2025a1000ido]
- 133. - Bland Plot | Real Statistics Using Excel Altman [https://real-statistics.com/reliability/interrater-reliability/bland-altman-analysis/bland-altman-plot/]
- 134. Understanding Bland - Biochemia Medica Altman analysis [https://www.biochemia-medica.com/en/journal/25/2/10.11613/BM.2015.015]
- 135. MRI Segmentation with 0.95 Brain - Analytics Vidhya Dice Score [https://www.analyticsvidhya.com/blog/2022/07/brain-mri-segmentation-with-0-95-dice-score/]
- 136. Generalised Wasserstein Dice for Imbalanced... | SpringerLink Score [https://link.springer.com/chapter/10.1007/978-3-319-75238-9_6]
- 137. A Guideline of Selecting and Reporting Intraclass Correlation Coefficients for Reliability Research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4913118/]
- 138. The Intraclass Correlation Coefficient (ICC): A Beginners Guide | by Salah Assana | Medium [https://medium.com/@SalahAssana/a-beginners-guide-to-the-intraclass-correlation-coefficient-icc-288f7fe7bcfc]
- 139. Deep learning-based automated segmentation of eight brain ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-022-00807-4]
- 140. Assessment of Operator Reliability in Ultrasound of the Median and... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8623197/]
- 141. Estimation of an inter-rater intra-class correlation coefficient that overcomes common assumption violations in the assessment of health measurement scales | BMC Medical Research Methodology | Full Text [https://bmcmedresmethodol.biomedcentral.com/articles/10.1186/s12874-018-0550-6]