Digital Twin Models for Predicting Neurological Disease Progression: From Foundations to Clinical Applications
This article provides a comprehensive examination of digital twin (DT) technology for predicting neurological disease progression, tailored for researchers, scientists, and drug development professionals.
Digital Twin Models for Predicting Neurological Disease Progression: From Foundations to Clinical Applications
Abstract
This article provides a comprehensive examination of digital twin (DT) technology for predicting neurological disease progression, tailored for researchers, scientists, and drug development professionals. It explores the foundational concepts defining DTs in neuroscience, contrasting them with digital models and shadows. The manuscript details cutting-edge methodological approaches, including AI and mechanistic model integration, and their specific applications in conditions like Alzheimer's disease, Parkinson's disease, and brain tumors, highlighting use cases in clinical trial optimization and personalized treatment planning. It critically addresses troubleshooting and optimization challenges, such as data integration, model validation, and computational scalability. Finally, the article assesses validation frameworks, regulatory acceptance, and performance metrics, offering a comparative analysis with traditional methods. The goal is to serve as a foundational resource for advancing the development and clinical translation of neurological digital twins.
Defining the Neurological Digital Twin: Core Concepts and Current Landscape
What is a Digital Twin? Distinguishing from Digital Models and Shadows
In the realm of modern technological research, the concepts of digital twins, digital models, and digital shadows represent a spectrum of virtual representations of physical entities. For researchers in neurology and drug development, precise distinctions between these terms are critical. A digital twin is more than a simple model; it is a dynamic, virtual representation that is interconnected with its physical counterpart through a continuous, bidirectional flow of data [1] [2]. This allows the digital twin not only to mirror the current state of a physical system but also to simulate future states, predict outcomes, and even influence the physical system itself [3]. This capability is particularly transformative for predicting neurological disease progression, offering a pathway to personalized, predictive medicine by creating a virtual replica of a patient's brain or autonomic nervous system [4] [5].
Core Definitions and Distinctions
Digital Model
A digital model is a static digital representation of a physical object, system, or process, such as a 3D computer-aided design (CAD) file or a mathematical algorithm [1] [6]. Its key characteristic is the absence of any automated data exchange with the physical entity it represents [3]. Any updates to the model based on changes in the physical world must be performed manually. In neuroscience, a digital model could be a static 3D reconstruction of a patient's brain from an MRI scan, used for surgical planning but not updating automatically [4].
Digital Shadow
A digital shadow represents a significant evolution from a digital model. It is a virtual representation that automatically receives and updates its state based on real-time data from its physical counterpart through sensors or IoT devices [1] [6]. However, this data flow is strictly one-way; the physical process influences the digital shadow, but the shadow cannot directly cause changes in the physical world [3]. For example, a digital shadow of a neuro-intensive care unit could monitor real-time intracranial pressure and EEG data from multiple patients, providing a live dashboard for clinicians to observe trends.
Digital Twin
A digital twin establishes a bidirectional, real-time connection between the physical and digital entities [1]. The physical entity provides operational data to the digital twin, and the twin, in turn, can send back commands, simulations, or insights to influence and optimize the physical entity [3]. This closed-loop, interactive relationship is the defining feature of a true digital twin. In neurological research, a digital twin of a patient's brain could use continuous data from wearables and clinical assessments to simulate the progression of a disease like Parkinson's and test the potential efficacy of different drug regimens in silico before recommending a specific therapy [5] [2].
Comparative Analysis
The table below summarizes the key differences:
| Feature | Digital Model | Digital Shadow | Digital Twin |
|---|---|---|---|
| Data Connection | None [3] | One-way (from physical to digital) [1] [3] | Two-way, bidirectional [1] [3] |
| Real-Time Updates | No [3] | Yes [3] | Yes [3] |
| Influence on Physical System | No [3] | No (monitoring only) [3] | Yes (can control/optimize) [3] |
| Primary Use Case | Design, prototyping, visualization [1] | Monitoring, reporting, predictive maintenance [1] [3] | Optimization, autonomous control, predictive analytics [1] [3] |
| Neurology Example | Static 3D brain model from MRI | Live dashboard of patient vitals from wearables | Simulating drug response & adapting therapy in real-time [5] |
Data Flow Relationships Among Digital Concepts
The Digital Twin in Neurological Disease Research
The Conceptual Framework
In neurological research, a digital twin is a dynamic, virtual replica of a patient's brain or specific neural systems [4] [5]. It is built and maintained using multimodal data and is designed to simulate, predict, and optimize health outcomes in the physical patient. The core value lies in its ability to perform "in-silico" experiments—testing countless hypotheses and treatment strategies on the virtual twin to identify the most promising ones for real-world application, thereby accelerating research and personalizing therapy [7].
Key Application Areas
- Personalized Disease Modeling: Creating patient-specific computational models of brain network dynamics to understand how pathologies like tumors or neurodegenerative diseases disrupt normal function [4]. These models can incorporate individual neuroimaging, genetic, and clinical data to simulate disease trajectories.
- Treatment Optimization and Virtual Clinical Trials: A digital twin can simulate a patient's response to various medications (e.g., pro-amatine or pyridostigmine for POTS) or neuromodulation strategies, guiding personalized dosing and reducing trial-and-error [5]. Furthermore, aggregating thousands of digital twins enables the design of in-silico clinical trials, drastically reducing the time and cost of bringing new neurological drugs to market [2].
- Symptom Prediction and Prevention: For conditions like Postural Tachycardia Syndrome (POTS), a digital twin can continuously monitor physiological signals (e.g., heart rate, respiration, end-tidal CO2) [5]. By identifying precursors to symptomatic events like cerebral hypoperfusion, the system can alert the patient or clinician to intervene preemptively, potentially preventing symptoms before they occur [5].
Experimental Protocols for Neurological Digital Twins
Protocol: Building a Digital Twin for a Neuro-Oncology Study
This protocol outlines the methodology for creating a patient-specific digital twin to model brain tumor growth and predict the impact of surgical interventions [4].
1. Hypothesis and Objective Definition:
- Define the clinical/research question (e.g., "How will resection of tumor X impact the functional connectivity of network Y?").
- Establish the primary outcome measures (e.g., prediction of post-surgical cognitive deficit).
2. Multimodal Data Acquisition and Ingestion:
- Structural MRI: Provides high-resolution anatomical data for constructing the base model [4].
- Functional MRI (fMRI): Measures blood-oxygen-level-dependent (BOLD) signals to map brain activity and functional connectivity between regions [4].
- Diffusion MRI (dMRI): Traces the movement of water molecules to map the white matter structural connectome—the "wiring" of the brain [4].
- Clinical and Neuropsychological Data: Includes patient-reported outcomes, quality of life assessments, and standardized cognitive test scores [4].
- Genomic Data: Tumor genomics or patient genetic markers when relevant.
3. Data Harmonization and Fusion:
- Spatial co-registration of all neuroimaging data into a common coordinate system.
- Data cleaning and normalization to account for variability in acquisition protocols.
- Multimodal fusion techniques to integrate structural, functional, and clinical data into a unified model [4].
4. Model Building and Personalization:
- Use a platform like The Virtual Brain (TVB) to create a personalized mathematical model of brain dynamics [4].
- The structural connectome from dMRI serves as the scaffold upon which neural mass models simulate population-level neuronal activity.
- Model parameters are iteratively adjusted so that the simulated fMRI activity patterns closely match the empirical fMRI data from the individual patient.
5. Simulation and Intervention Testing:
- Run the personalized model to establish a baseline simulation.
- Introduce a virtual intervention, such as "lesioning" the model by removing nodes and connections corresponding to the planned tumor resection.
- Run the post-intervention simulation to predict new patterns of network dynamics and functional outcomes.
6. Validation and Clinical Translation:
- Compare the model's predictions with the patient's actual post-surgical outcome.
- Use this feedback to refine and validate the model's accuracy for future use.
Digital Twin Model Creation Workflow
Protocol: Implementing a Digital Twin for Autonomic Disorder Management (POTS)
This protocol describes the framework for a continuous, adaptive digital twin for Postural Tachycardia Syndrome, focusing on real-time symptom prediction and intervention [5].
1. System Architecture and Component Setup:
- Monitoring Subsystem: Deploy wearable devices (e.g., chest patch for ECG, continuous blood pressure monitor, accelerometer) to stream heart rate, heart rate variability, and activity data. Optionally, include a capnometer for end-tidal CO2 monitoring [5].
- Modeling Subsystem: Implement a cloud-based analytics platform that integrates mechanistic models (e.g., of cardiovascular response to orthostatic stress) with AI/machine learning models trained on population and individual data.
- Simulation Subsystem: Develop a module capable of running short-term forecasts of physiological state based on current data trends.
- Interface Subsystem: Create a clinician dashboard integrated with Electronic Health Records (EHR) and a patient-facing mobile application for alerts and feedback.
2. Continuous Data Ingestion and Preprocessing:
- Establish secure, real-time data pipelines from wearables, EHR, and patient-reported outcome apps to the cloud platform.
- Implement data cleaning and filtering algorithms to handle artifacts and noise from sensor data.
- Perform data fusion to create a unified, time-synchronized view of the patient's state.
3. AI-Driven State Prediction and Alert Generation:
- The AI model continuously analyzes the incoming data stream. For instance, it detects patterns of inappropriate hyperventilation (a precursor to cerebral hypoperfusion and dizziness in POTS) [5].
- Upon detecting a pre-symptomatic pattern, the system triggers an alert hierarchy:
- Stage 1: A subconscious haptic vibration from the patient's wearable or smartphone, prompting them to slow their breathing without conscious effort.
- Stage 2: If the pattern persists, an auditory or visual alert through the mobile app with explicit instructions.
- Stage 3: An escalation alert sent to the clinician's dashboard for further investigation.
4. Intervention Simulation and Personalization:
- The clinician uses the dashboard to simulate the effect of lifestyle changes (e.g., a new exercise regimen) or medication adjustments on the digital twin before prescribing them to the patient [5].
- The digital twin's model is continuously updated based on the patient's response to actual interventions, creating a learning, adaptive system.
The Scientist's Toolkit: Key Research Reagents and Technologies
| Item | Function & Application in Neurological Digital Twins |
|---|---|
| The Virtual Brain (TVB) | An open-source neuroinformatics platform for constructing and simulating personalized brain network models based on individual connectome data [4]. |
| Multi-modal MRI Data | Structural MRI: For anatomy. fMRI: For functional connectivity. dMRI: For structural white matter connectivity. Forms the core imaging data for model building [4]. |
| Wearable Biometric Sensors | Devices (e.g., ECG patches, actigraphs) to collect continuous, real-time physiological and activity data for dynamic model updating, especially in outpatient settings [5]. |
| AI/ML Modeling Platforms (Python-based) | Platforms like TensorFlow or PyTorch, and ecosystem libraries, are used to develop AI-driven predictive models that learn from continuous patient data streams [5]. |
| Data Harmonization Tools | Software and pipelines (e.g., from the FMRIB Software Library - FSL) for co-registering and standardizing diverse neuroimaging data into a consistent format for analysis [4]. |
| IoT/Data Streaming Protocols | Communication protocols like MQTT and AMQP enable reliable, real-time transmission of sensor data from the physical patient to the cloud-based digital twin [8]. |
Technical and Ethical Considerations
Implementing digital twins in neurological research presents significant challenges. The data volume generated from continuous monitoring is immense, requiring robust infrastructure for storage, processing, and compression [5]. Model transparency is another hurdle; while AI models are powerful, their "black-box" nature can be a barrier to clinical trust and adoption. Efforts to develop explainable AI (XAI) are crucial [5]. Furthermore, data privacy and security are paramount when handling sensitive patient health information in real-time, necessitating stringent protocols and potentially decentralized data architectures like blockchain [5].
Ethically, the use of digital twins raises questions regarding patient consent for continuous data use, algorithmic bias, and the potential for a "responsibility gap" if autonomous actions taken by the system lead to adverse outcomes. A collaborative, interdisciplinary approach involving clinicians, data scientists, and ethicists is essential to navigate these challenges responsibly [4] [2].
The National Academies of Sciences, Engineering, and Medicine (NASEM) has established a rigorous definition for digital twins in healthcare that sets a crucial standard for research and clinical application. According to NASEM, a digital twin is "a set of virtual information constructs that mimics the structure, context, and behavior of a natural, engineered, or social system (or system-of-systems), is dynamically updated with data from its physical twin, has a predictive capability, and informs decisions that realize value" [9]. This definition emphasizes the bidirectional interaction between physical and virtual systems as central to the digital twin concept, distinguishing true digital twins from simpler digital models or shadows [10].
For researchers investigating neurological disease progression, the NASEM framework provides a structured approach for developing sophisticated computational models that can personalize treatments, dynamically adapt to patient changes, and generate accurate predictions of disease trajectories. The framework's emphasis on verification, validation, and uncertainty quantification (VVUQ) establishes critical standards for model reliability that are particularly important in the context of complex neurological disorders where treatment decisions have significant consequences [9].
Core Components of the NASEM Framework
Personalization: Creating Patient-Specific Computational Representations
Personalization requires developing virtual representations that reflect the unique characteristics of individual patients, moving beyond generalized population models. This involves integrating multi-scale data including genomics, clinical parameters, imaging findings, and lifestyle factors to create comprehensive patient profiles [11] [10].
In neurological applications, effective personalization has been demonstrated in multiple domains. For Alzheimer's disease research, conditional restricted Boltzmann machine (CRBM) models have been trained on harmonized datasets from 6,736 unique subjects, incorporating demographics, genetics, clinical severity measures, cognitive assessments, and laboratory measurements to create individualized predictions [12]. In Parkinson's disease management, digital twin-based healthcare systems have achieved 97.95% prediction accuracy for earlier identification from remote locations by incorporating patient-specific motor and non-motor symptoms [11]. For brain tumor management, hybrid approaches combining Semi-Supervised Support Vector Machine (S3VM) and improved AlexNet CNN have achieved feature recognition accuracy of 92.52% with impressive segmentation metrics by personalizing to individual tumor characteristics [11].
Table 1: Quantitative Outcomes of Personalized Digital Twin Approaches in Neurological Research
| Condition | Model Type | Personalization Data Sources | Achieved Accuracy | Clinical Application |
|---|---|---|---|---|
| Alzheimer's Disease | Conditional Restricted Boltzmann Machine (CRBM) | Demographics, genetics, clinical severity, cognitive measures, lab values | Partial correlation 0.30-0.46 with actual outcomes [12] | Prognostic covariate adjustment in clinical trials |
| Parkinson's Disease | Digital Twin Healthcare System | Motor symptoms, non-motor symptoms, remote monitoring data | 97.95% prediction accuracy [11] | Early disease identification and progression tracking |
| Brain Tumors | S3VM with AlexNet CNN | Imaging features, tumor characteristics, clinical parameters | 92.52% feature recognition accuracy [11] | Radiotherapy planning and treatment response prediction |
| Multiple Sclerosis | Physics-based Progression Model | Imaging, clinical assessments, biomarker data | Identified progression 5-6 years before clinical onset [11] | Disease progression forecasting and intervention timing |
Dynamic Updating: The Bidirectional Data Flow
Dynamic updating establishes a continuous feedback loop between the physical patient and their digital counterpart, enabling the model to evolve alongside the patient's changing health status. This bidirectional flow of information represents a fundamental distinction between true digital twins and static computational models [9] [10].
The implementation of dynamic updating in neurological disorders faces unique challenges, as updating a human system typically necessitates a "human-in-the-loop" approach rather than fully automated updates [9]. Successful implementations have overcome these challenges through various technological strategies. The Cardio Twin architecture demonstrates this capability in another domain with real-time electrocardiogram (ECG) monitoring achieving 85.77% classification accuracy and 95.53% precision through continuous data assimilation [11]. For respiratory monitoring, systems using ESP32 Wi-Fi Channel State Information sensors have achieved 92.3% accuracy in breathing rate estimation, while ML techniques demonstrated classification accuracies of 89.2% for binary-class and 83.7% for multi-class respiratory pattern recognition [11]. In diabetes management, the Exercise Decision Support System (exDSS) for type 1 diabetes provides personalized recommendations during exercise, increasing time in target glucose range from 80.2% to 92.3% through continuous monitoring and model adjustment [11].
Table 2: Dynamic Updating Methodologies and Performance Across Medical Domains
| Update Mechanism | Data Sources | Update Frequency | Performance Metrics | Relevance to Neurology |
|---|---|---|---|---|
| Wearable Sensor Networks | Movement patterns, vital signs, sleep metrics | Continuous real-time | 92.3% accuracy in breathing pattern classification [11] | Motor symptom tracking in Parkinson's, seizure detection in epilepsy |
| Periodic Clinical Assessment | Cognitive testing, imaging, laboratory values | Days to months | Correlation of 0.30-0.39 with 96-week cognitive changes [12] | Disease progression modeling in Alzheimer's and MS |
| Patient-Reported Outcomes | Symptom diaries, medication adherence, quality of life | Daily to weekly | 15% reduction in residual variance in clinical trials [12] | Tracking subjective symptoms in migraine, multiple sclerosis |
| Automated Imaging Analysis | MRI, CT, PET scans | Weeks to months | 16.7% radiation dose reduction while maintaining equivalent outcomes [11] | Tumor response assessment in neuro-oncology |
Predictive Power: Forecasting Disease Trajectories and Treatment Responses
Predictive capability represents the third essential component of the NASEM framework, enabling digital twins to forecast future health states and intervention outcomes under various scenarios. This predictive power transforms digital twins from descriptive tools to proactive decision-support systems [9].
In neurological applications, predictive digital twins have demonstrated significant potential across multiple domains. For Alzheimer's disease trials, AI-generated digital twins have reduced total residual variance by 9-15% while maintaining statistical power, potentially reducing control arm sample size requirements by 17-26% in future trials [12]. In neurodegenerative disease management, physics-based models integrating the Fisher-Kolmogorov equation with anisotropic diffusion have successfully simulated the spread of misfolded proteins across the brain, capturing both spatial and temporal aspects of disease progression [11]. For personalized radiotherapy planning in high-grade gliomas, digital twin approaches have demonstrated either increased tumor control or significant reductions in radiation dose (16.7%) while maintaining equivalent outcomes through accurate prediction of treatment response [11].
Application Notes: Implementing the NASEM Framework in Neurological Research
Protocol 1: Creating NASEM-Compliant Digital Twins for Alzheimer's Disease Clinical Trials
Background and Purpose: This protocol outlines the methodology for developing prognostic digital twins for Alzheimer's disease clinical trials, based on validated approaches that have received regulatory acceptance [12]. The digital twins serve as prognostic covariates to reduce statistical variance and improve trial power.
Materials and Equipment:
- Historical clinical trial datasets (minimum n=5,000 recommended)
- Target trial baseline characteristics including cognitive assessments, demographic data, and biomarker profiles
- Conditional Restricted Boltzmann Machine (CRBM) or equivalent deep learning architecture
- High-performance computing infrastructure with GPU acceleration
- Data harmonization pipelines for multi-source data integration
Procedure:
- Data Harmonization and Preprocessing
- Collect and harmonize data from historical clinical trials and observational studies
- Perform quality control including assessment of missing data patterns and variable distributions
- Create unified data schema encompassing demographics, genetics, clinical severity, cognitive measures, and functional assessments
Model Training and Validation
- Train CRBM model on historical integrated dataset using leave-one-trial-out cross-validation
- Validate model on independent clinical trial datasets not used in training
- Assess partial correlation between digital twin predictions and actual outcomes across multiple cognitive assessment scales
Prognostic Covariate Adjustment in Target Trial
- Generate digital twins for all participants in the target trial using baseline data
- Incorporate digital twin predictions as covariates in mixed-effects models for repeated measures
- Calculate variance reduction and sample size optimization achieved through covariate adjustment
Quality Control and Validation:
- Establish benchmarking against traditional statistical methods
- Verify consistency of correlation coefficients across validation datasets (target range: 0.30-0.46)
- Ensure computational reproducibility through containerized implementation
Expected Outcomes: Implementation of this protocol typically achieves 9-15% reduction in total residual variance, enabling sample size reductions of 9-15% overall and 17-26% in control arms while maintaining statistical power [12].
Protocol 2: Dynamic Digital Twins for Progressive Neurological Conditions
Background and Purpose: This protocol describes the development of dynamically updated digital twins for progressive neurological conditions such as Parkinson's disease and multiple sclerosis, enabling continuous adaptation to disease progression and treatment response.
Materials and Equipment:
- Multi-modal data streams (clinical assessments, wearable sensor data, imaging, patient-reported outcomes)
- Cloud-based data assimilation infrastructure
- Ensemble modeling framework combining mechanistic and machine learning approaches
- Real-time data processing pipelines with automated quality checks
Procedure:
- Initial Model Personalization
- Develop baseline model using comprehensive initial assessment data
- Incorporate individual neuroanatomy, functional connectivity, and clinical phenotype
- Establish individual-specific parameters for disease progression models
Dynamic Updating Implementation
- Implement automated data ingestion from continuous monitoring sources
- Establish model updating triggers based on data arrival and significance thresholds
- Deploy ensemble filtering techniques for state and parameter estimation
Predictive Forecasting and Intervention Planning
- Generate short-term and long-term forecasts of disease progression
- Simulate intervention effects under multiple scenarios
- Update interventional recommendations based on model predictions and confidence intervals
Quality Control and Validation:
- Implement rigorous VVUQ (verification, validation, and uncertainty quantification) processes
- Establish benchmarking against static models using historical datasets
- Deploy real-time monitoring of model performance metrics with alerting systems
Expected Outcomes: Successful implementation has demonstrated prediction accuracy of 97.95% for Parkinson's disease identification and enabled detection of progressive brain tissue loss 5-6 years before clinical symptom onset in multiple sclerosis [11].
Table 3: Essential Research Reagents and Computational Resources for Neurological Digital Twins
| Category | Specific Resources | Function/Application | Implementation Notes |
|---|---|---|---|
| Data Acquisition | Wearable sensors (actigraphy, physiological monitors) | Continuous real-world data collection for dynamic updating | Select devices with validated accuracy for target population [11] |
| Standardized cognitive assessment batteries | Longitudinal cognitive profiling for personalization and validation | Ensure cultural and linguistic appropriateness for diverse populations | |
| Multimodal neuroimaging protocols (MRI, PET, fMRI) | Structural and functional characterization for model initialization | Implement standardized acquisition protocols across sites | |
| Computational Infrastructure | High-performance computing clusters with GPU acceleration | Training of complex models (CRBM, deep neural networks) | Cloud-based solutions facilitate collaboration and scalability [12] |
| Federated learning frameworks | Multi-institutional collaboration while preserving data privacy | Essential for rare disease research with distributed patient populations | |
| Containerized deployment platforms (Docker, Singularity) | Reproducible model implementation and validation | Critical for regulatory submission and peer verification | |
| Modeling Approaches | Conditional Restricted Boltzmann Machines (CRBM) | Generation of prognostic digital twins for clinical trials | Particularly effective for Alzheimer's disease applications [12] |
| Physics-based progression models (Fisher-Kolmogorov equations) | Simulation of neurodegenerative protein spread | Captures spatiotemporal aspects of disease progression [11] | |
| Hybrid mechanistic-machine learning frameworks | Combining domain knowledge with data-driven insights | Balances interpretability with predictive power |
Technical Considerations and Implementation Challenges
Verification, Validation, and Uncertainty Quantification (VVUQ)
The NASEM framework emphasizes VVUQ as a critical standard for ensuring digital twin reliability [9]. However, current implementations show significant gaps in this area, with only two studies in a recent comprehensive review mentioning VVUQ processes [9]. For neurological applications, rigorous VVUQ should include:
- Verification: Ensuring the computational model correctly implements the intended mathematical framework
- Validation: Assessing how accurately the model represents real-world neurological processes
- Uncertainty Quantification: Characterizing and communicating uncertainties in model predictions
Implementation of comprehensive VVUQ requires specialized expertise in computational neuroscience, statistics, and domain-specific clinical knowledge. Establishing standardized VVUQ protocols for neurological digital twins remains an urgent research priority.
Computational and Infrastructure Requirements
The development of NASEM-compliant digital twins demands substantial computational resources. Successful implementations have leveraged:
- High-performance computing environments with parallel processing capabilities
- Secure data storage infrastructure for multimodal neurological data
- Automated pipelines for data preprocessing, quality control, and model updating
- Visualization platforms for interpreting complex model outputs for clinical decision support
Computational efficiency considerations are particularly important for real-time clinical applications, where model predictions must be available within clinically relevant timeframes.
The NASEM framework provides a rigorous foundation for developing digital twins that meet the complex challenges of neurological disease research. By emphasizing personalization, dynamic updating, and predictive power, the framework addresses critical needs in understanding and treating conditions such as Alzheimer's disease, Parkinson's disease, multiple sclerosis, and brain tumors.
Current research demonstrates the substantial potential of this approach, with documented improvements in prediction accuracy, clinical trial efficiency, and personalized treatment planning. However, full implementation across the NASEM criteria remains challenging, with only approximately 12% of current studies meeting all requirements [9]. Continued advancement in data integration, computational methods, and validation frameworks will be essential for realizing the full potential of digital twins in neurological research and clinical care.
The digital twin (DT) concept has undergone a significant transformation from its industrial origins to its current status as a cutting-edge tool in neurological research and clinical practice. First introduced by Grieves in 2002 as a "conceptual ideal" for product lifecycle management and later coined by NASA in 2010 for aerospace applications, the framework originally consisted of three core elements: a physical system, its virtual representation, and bidirectional information flow linking them [9] [11] [13]. This technology has since transcended its engineering roots, emerging as a transformative force in healthcare that enables highly personalized medicine through patient-specific models that simulate disease progression and treatment response [11].
In neurological applications, digital twins represent a paradigm shift from population-based medicine to truly individualized patient care. By creating virtual replicas of patient brains, researchers and clinicians can now run simulations to predict disease trajectories, optimize therapeutic interventions, and understand individual brain dynamics without risking patient safety [14]. This review examines the historical trajectory of digital twin technology and its current applications in neurology, providing detailed protocols and analytical frameworks for researchers working at the intersection of computational modeling and neurological disease progression.
From Industry to Clinic: The Healthcare Transformation
The transition of digital twins from industrial to medical applications represents one of the most significant technological migrations in recent scientific history. In clinical applications, DTs facilitate personalized medicine by enabling the construction of patient-specific models that integrate data from electronic health records (EHR), imaging modalities, and Internet of Things (IoT) devices to account for individual physiological and historical nuances [11]. This fundamental shift required adapting industrial concepts to the complexity and variability of human physiology, particularly the challenges of modeling the most complex biological system—the human brain.
According to a comprehensive scoping review of Human Digital Twins (HDTs) in healthcare, the National Academies of Sciences, Engineering, and Medicine (NASEM) has established a precise definition requiring that a digital twin must be personalized, dynamically updated, and have predictive capabilities to inform clinical decision-making [9]. This definition provides a crucial framework for distinguishing true digital twins from related concepts such as digital models (no automatic data exchange) and digital shadows (one-way data flow only) [9].
Table 1: Digital Twin Classification in Healthcare Based on NASEM Criteria
| Model Type | Prevalence in Healthcare Literature | Key Characteristics | Neurological Examples |
|---|---|---|---|
| True Digital Twin | 12.08% (18 of 149 studies) | Personalized, dynamically updated, enables decision support | Virtual Brain Twins for epilepsy surgery planning |
| Digital Shadow | 9.40% (14 studies) | One-way data flow from physical to virtual | Brain activity monitoring systems |
| Digital Model | 37.58% (56 studies) | Personalized but not dynamically updated | Static computational brain models |
| Virtual Patient Cohorts | 10.07% (15 studies) | Generated populations for in-silico trials | Synthetic populations for Alzheimer's trial optimization |
The table above illustrates that only a minority of models labeled as "digital twins" in healthcare literature actually meet the full NASEM criteria, highlighting the importance of precise terminology and methodological rigor in this emerging field [9].
Neurological Applications: Current Landscape
Digital twin technology has demonstrated remarkable potential across various neurological conditions, enabling unprecedented insights into disease progression and treatment planning. The applications span from neurodegenerative disorders to epilepsy and brain tumors, each with distinct methodological approaches and clinical implications.
Virtual Brain Twins (VBTs)
Virtual Brain Twins represent one of the most advanced implementations of digital twin technology in neuroscience. A VBT combines a person's structural brain data (from MRI or diffusion imaging) with functional data measuring brain activity (such as EEG, MEG, or fMRI) to build a computational model of their brain's network [14]. This network model simulates how different brain regions are connected and communicate through neural pathways, creating a personalized digital replica that can be used to test "what-if" scenarios in a safe, virtual environment before applying treatments or interventions to the patient [14].
The creation of a VBT involves three key steps: (1) Structural mapping where brain scans are processed to identify regions (nodes) and the white-matter connections between them (the connectome); (2) Model integration where each node is assigned a mathematical model representing the average activity of large groups of neurons, while the connectome defines how signals travel between regions; and (3) Personalization through data where functional brain recordings fine-tune the model using statistical inference, adapting it to the individual's physiology and condition [14].
Specific Neurological Applications
Table 2: Digital Twin Applications in Neurology
| Condition | Digital Twin Application | Reported Efficacy/Performance |
|---|---|---|
| Epilepsy | Virtual Epileptic Patient model identifies seizure origins and evaluates tailored surgical strategies | Enables precise intervention planning for drug-resistant cases [14] |
| Alzheimer's Disease | Physics-based models integrate Fisher-Kolmogorov equation with anisotropic diffusion to simulate misfolded protein spread | Captures spatial and temporal aspects of neurodegenerative disease progression [11] |
| Multiple Sclerosis | Modeling how lesions disrupt brain connectivity | Informs rehabilitation and therapy planning; reveals tissue loss begins 5-6 years before clinical onset [11] [14] |
| Parkinson's Disease | DT-based Healthcare Systems for remote monitoring and prediction | Achieves 97.95% prediction accuracy for earlier identification [11] |
| Brain Tumors | Hybrid approaches combining Semi-Supervised Support Vector Machine and improved AlexNet CNN | 92.52% feature recognition accuracy; personalized radiotherapy planning enables 16.7% radiation dose reduction while maintaining outcomes [11] |
Experimental Protocols and Methodologies
Protocol 1: Generating AI-Based Digital Twins for Alzheimer's Clinical Trials
This protocol outlines the methodology for creating and implementing AI-generated digital twins to enhance clinical trial efficiency in Alzheimer's disease research, based on the approach used in the AWARE trial analysis [12].
Materials and Data Requirements:
- Historical Training Data: Harmonized dataset combining control arms from 29 clinical trials (≥7,000 participants) and observational studies (1,728 participants) from sources like CODR-AD and ADNI [12]
- Baseline Variables: Demographics, genetics, clinical severity scores, component-level cognitive and functional measures, laboratory measurements [12]
- Target Trial Data: Baseline patient characteristics from the clinical trial being enhanced (e.g., AWARE trial with 453 MCI/mild AD patients) [12]
Methodological Steps:
Model Training:
- Train a Conditional Restricted Boltzmann Machine (CRBM) on the historical dataset after data harmonization
- CRBM is an unsupervised machine learning model with probabilistic neural networks
- Pre-train and validate the model prior to application to the target trial
Digital Twin Generation:
- Input baseline data from each trial participant into the trained CRBM
- Generate individualized predictions of each participant's clinical outcomes if they had received placebo
- Output includes comprehensive, longitudinal computationally generated clinical records
Statistical Integration:
- Incorporate DT predictions as prognostic covariates in statistical models using PROCOVA (prognostic covariate adjustment) or PROCOVA-Mixed-Effects Model for Repeated Measures (MMRM)
- Analyze treatment effects while accounting for expected placebo progression
- Assess variance reduction and potential sample size savings
Validation and Quality Control:
- Evaluate partial correlation coefficients between DTs and actual change scores from baseline (expected range: 0.30-0.46 based on validation studies) [12]
- Calculate total residual variance reduction (typically ~9% to 15% with DTs) [12]
- Determine potential sample size reductions while maintaining statistical power (total sample: ~9-15%; control arm: 17-26%) [12]
Protocol 2: Virtual Brain Twin Development for Surgical Planning
This protocol details the creation of personalized Virtual Brain Twins for neurological conditions requiring surgical intervention, such as drug-resistant epilepsy [14].
Data Acquisition and Preprocessing:
- Structural Imaging: Acquire high-resolution T1-weighted MRI and diffusion-weighted imaging (DWI) for connectome reconstruction
- Functional Data: Collect resting-state fMRI, task-based fMRI, EEG, and/or MEG data
- Clinical Phenotyping: Document seizure semiology, frequency, medication history, and prior interventions
Computational Modeling Pipeline:
Structural Connectome Reconstruction:
- Process structural MRI using FreeSurfer or similar pipeline for cortical parcellation
- Reconstruct white matter pathways from DWI using tractography (e.g., probabilistic tractography in FSL or MRtrix)
- Create adjacency matrix representing connection strengths between brain regions
Neural Mass Model Implementation:
- Implement a system of differential equations representing average neuronal population activity
- Parameters include synaptic gains, time constants, and propagation speeds
- Use The Virtual Brain (TVB) platform or custom MATLAB/Python code
Model Personalization and Fitting:
- Adjust model parameters to minimize difference between simulated and empirical functional data
- Apply Bayesian inference or similar optimization approaches
- Validate model by comparing simulated activity with held-out empirical data
Intervention Simulation:
- Simulate surgical resections by removing corresponding nodes/connections
- Test neuromodulation parameters (e.g., DBS, responsive neurostimulation)
- Predict post-intervention network dynamics and clinical outcomes
Validation Framework:
- Compare predicted seizure propagation pathways with intracranial EEG findings
- Assess accuracy of predicted clinical outcomes following intervention
- Evaluate model robustness through sensitivity analysis and uncertainty quantification
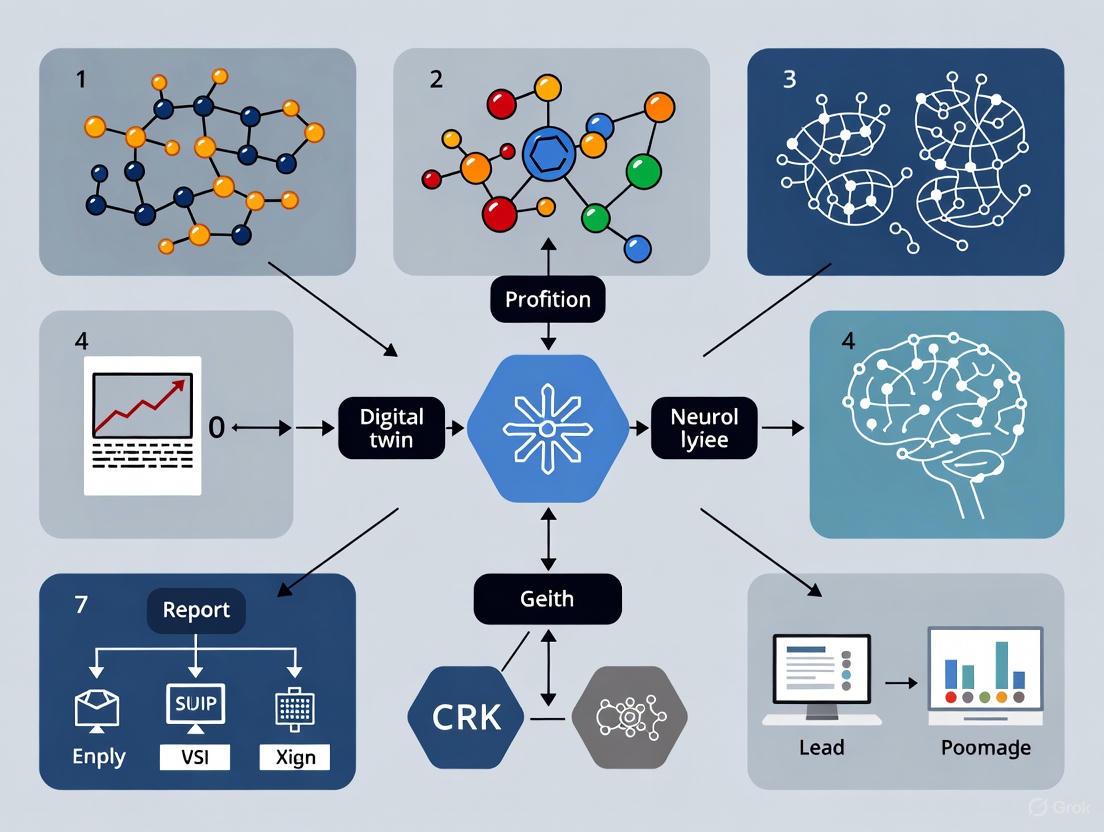
Visualization: Digital Twin Workflow in Neurological Research
Figure 1: Digital Twin Framework for Neurological Applications. This workflow diagram illustrates the bidirectional data flow between physical patient systems and their virtual counterparts, highlighting continuous data integration, computational modeling, and clinical application pathways.
Table 3: Essential Research Resources for Neurological Digital Twin Development
| Resource Category | Specific Tools/Platforms | Function/Purpose |
|---|---|---|
| Data Acquisition | MRI, diffusion MRI, EEG, MEG, fMRI | Capture structural and functional brain data for model personalization [14] |
| Computational Modeling | The Virtual Brain (TVB), Finite Element Analysis, Neural Mass Models | Implement mathematical representations of brain dynamics and physiology [14] |
| AI/ML Frameworks | Conditional Restricted Boltzmann Machines (CRBM), Deep Generative Models | Generate predictive digital twins and simulate disease progression [12] |
| Data Harmonization | CODR-AD, ADNI, Disease-specific Registries | Provide historical training data from clinical trials and observational studies [12] |
| Validation Frameworks | Verification, Validation, Uncertainty Quantification (VVUQ) | Ensure model reliability and predictive accuracy [9] |
| Clinical Integration | PROCOVA, PROCOVA-MMRM Statistical Methods | Incorporate digital twin predictions into clinical trial analysis [12] |
The migration of digital twin technology from industrial applications to neurological research represents a remarkable example of cross-disciplinary innovation. The historical trajectory demonstrates how core engineering concepts have been adapted to address the profound complexity of human brain function and neurological disease. Current applications in epilepsy, Alzheimer's disease, multiple sclerosis, Parkinson's disease, and brain tumors show consistent patterns of success in prediction accuracy, treatment optimization, and clinical decision support [11] [14].
Future development must address several critical challenges, including the need for more comprehensive validation frameworks, improved data integration across multiple scales, and solutions to computational scalability constraints. Furthermore, as noted in the scoping review by [9], only 12.08% of current healthcare digital twin implementations fully meet the NASEM criteria, indicating substantial room for methodological refinement. The continued evolution of this technology promises to accelerate the transition from reactive to predictive and preventive neurology, ultimately enabling truly personalized therapeutic strategies based on individual brain dynamics and disease trajectories.
Application Note: Digital Twin Modeling of Neurological Systems
Core Concept and Rationale
Digital twins (DTs) represent a transformative approach in neurological research and drug development, creating dynamic, virtual replicas of patient-specific physiological systems. These computational models integrate multi-scale data—from molecular pathways to whole-organ systems—to predict disease progression and treatment responses in silico. The fundamental value proposition lies in their ability to reduce clinical trial sample sizes by 9-15% while maintaining statistical power, and specifically decreasing control arm requirements by 17-26% through generating artificial intelligence-powered prognostic covariates [12]. This technology has received positive qualification opinions from regulatory agencies including the European Medicines Agency and U.S. Food and Drug Administration for clinical trial applications [12].
For neurological disorders specifically, digital twins address critical challenges including disease heterogeneity, high variability in clinical outcomes, and the limited generalizability of traditional randomized controlled trials. By creating patient-specific computational models that forecast individual placebo outcomes based on baseline characteristics, researchers can reduce statistical uncertainty and improve trial efficiency without compromising validity [12] [15]. The adaptive nature of digital twins—continuously updating with real-time data—distinguishes them from conventional simulations, enabling truly personalized predictive modeling in neurological care [5].
Quantitative Validation in Neurological Disorders
Table 1: Digital Twin Performance Metrics in Alzheimer's Disease Clinical Trials
| Performance Metric | AWARE Trial Results (Week 96) | Independent Trial Validation Range | Impact on Trial Efficiency |
|---|---|---|---|
| Partial Correlation with Cognitive Change | 0.30-0.39 | 0.30-0.46 | Improved prognostic accuracy |
| Residual Variance Reduction | 9-15% | N/A | Enhanced statistical power |
| Total Sample Size Reduction | 9-15% | N/A | Reduced recruitment burden |
| Control Arm Size Reduction | 17-26% | N/A | Ethical improvement |
| Primary Assessment Scales | CDR-SB, ADAS-Cog 14, MMSE, FAQ | Consistent across multiple trials | Multiple endpoint validation |
Data derived from application of digital twin methodology to the AWARE Phase 2 clinical trial (NCT02880956) in Alzheimer's Disease [12]
Protocol: Implementing Digital Twin Framework for Neurological Disease Modeling
Data Acquisition and Integration Protocol
Multi-Modal Data Sourcing
The foundational step in digital twin creation involves comprehensive data aggregation from diverse sources. Implement a structured acquisition protocol covering these data streams:
Clinical and Demographic Data: Extract from electronic health records including age, education, medical history, medication history, and family history. For Alzheimer's applications, ensure capture of baseline MMSE (22.2 ±4.6 typical in training cohorts), CDR-SB (2.7 ±2.2), and ADAS-Cog 14 scores [12].
Genetic and Molecular Profiling: Collect APOE ε4 genotype status, amyloid status (where available), and other relevant biomarker data. Historical training datasets typically contain 20-30% complete genetic information [12].
Wearable and Continuous Monitoring: Implement devices for real-time physiological tracking including heart rate, blood pressure, end-tidal CO₂, electroencephalogram, and cerebral blood flow measurements. Sample at minimum 1Hz frequency for autonomic function assessment [5].
Patient-Reported Outcomes: Standardize collection of symptom logs, activity levels, sleep patterns, stress measurements, and medication adherence using validated instruments.
Environmental Context: Document relevant environmental factors such as weather conditions, altitude, and temperature that may influence autonomic nervous system function [5].
Data Harmonization Procedure
- Execute ETL (Extract, Transform, Load) Pipeline to integrate heterogeneous data from clinical trials, observational studies, and real-world evidence sources.
- Apply syntactic normalization to standardize variable names, units, and formats across datasets.
- Implement semantic harmonization to resolve coding system differences (e.g., ICD-9 vs ICD-10, various cognitive assessment versions).
- Handle missing data using multiple imputation techniques validated for neurological datasets.
Model Training and Validation Protocol
Algorithm Selection and Configuration
For neurological applications, the Conditional Restricted Boltzmann Machine (CRBM) has demonstrated robust performance in generating digital twins:
Training Protocol:
- Pre-training Phase: Initialize CRBM model on harmonized historical dataset (6,736 unique subjects from CODR-AD and ADNI databases) [12].
- Feature Engineering: Incorporate 66+ harmonized variables spanning demographics, genetics, clinical severity, cognitive measures, and laboratory values.
- Transfer Learning: Fine-tune pre-trained weights on target trial population (e.g., 453 subjects for AWARE Alzheimer's trial).
- Hyperparameter Optimization: Conduct systematic search over learning rate (0.01-0.001), hidden units (50-500), and regularization parameters.
Validation Framework
Implement rigorous multi-level validation to ensure model reliability:
- Internal Validation: Cross-validation within training dataset using 80/20 split with 100 iterations.
- External Validation: Application to three independent clinical trials with correlation benchmarks of 0.30-0.46 against actual clinical outcomes [12].
- Prospective Validation: Blind prediction of ongoing trial outcomes before unblinding.
Experimental Workflow for Therapeutic Testing
In Silico Clinical Trial Implementation
Table 2: Research Reagent Solutions for Digital Twin Experiments
| Reagent/Category | Specification/Platform | Primary Function | Example Sources |
|---|---|---|---|
| Data Integration | CODR-AD, ADNI Databases | Historical training data with control arms | CPAD Consortium [12] |
| Modeling Framework | CRBM, Simply, Open Digital Twin Project | Core AI algorithms for twin generation | Open-source Python platforms [5] |
| Simulation Environment | PyTwin, TumorTwin-derived platforms | Running virtual treatment scenarios | Academic/industry collaborations [5] |
| Validation Tools | SHAP, PROCOVA-MMRM | Model interpretability and statistical adjustment | Regulatory guidance [12] [15] |
| Clinical Endpoints | CDR-SB, ADAS-Cog 14, MMSE, FAQ | Standardized outcome measures for validation | NIH/consortium standards [12] |
Protocol Execution Steps
Baseline Digital Twin Generation:
- Input comprehensive baseline data for each participant
- Generate individualized placebo progression forecasts using validated CRBM
- Establish pre-treatment prognostic scores for covariance adjustment
Virtual Cohort Simulation:
- Create synthetic control arms mirroring real participant characteristics
- Simulate virtual treatment groups by applying investigational drug effects
- Run 10,000+ in silico trial iterations with parameter variations
Integrated Analysis:
- Implement PROCOVA-Mixed Effects Model for Repeated Measures (PROCOVA-MMRM)
- Adjust for digital twin prognostics as covariates in primary analysis
- Calculate variance reduction and power improvements
Application Note: Pathway-Specific Targeting in Neurological Digital Twins
Multi-Scale Physiological Targeting
Digital twin technology enables unprecedented resolution in modeling neurological systems across multiple biological scales. The most effective implementations target specific physiological subsystems with appropriate modeling techniques:
Cellular Pathway Modeling: Approach signaling pathways not as fixed circuits but as plastic, proto-cognitive systems capable of memory and adaptation. This perspective enables modeling of phenomena like pharmacodynamic tolerance and sensitization at the molecular level [16]. Digital twins can simulate how repeated drug exposures alter pathway responsiveness over time, addressing significant challenges in chronic neurological disease management.
Autonomic Nervous System Implementation: For disorders like Postural Tachycardia Syndrome (POTS), digital twins create virtual replicas of autonomic cardiovascular control. These models integrate real-time data from wearables with mechanistic knowledge of cerebral blood flow regulation, orthostatic tachycardia mechanisms, and neurotransmitter dynamics [5]. The twins can predict cerebral hypoperfusion events by detecting precursor signals like inappropriate hyperventilation before symptom onset.
Whole-Brain System Integration: At the highest level, digital twins model brain-body physiology through hierarchical control loops spanning local, reflex, and central regulation levels [17]. This enables researchers to simulate how investigational therapies might affect the integrated system rather than isolated components.
Protocol Implementation for Autonomic Disorders
The following specialized protocol extends the general digital twin framework for autonomic nervous system applications:
Specialized Data Acquisition:
- Implement continuous non-invasive cardiac monitoring (heart rate, HRV)
- Measure end-tidal CO₂ as surrogate for cerebral blood flow regulation
- Record transcranial Doppler measurements when available
- Track symptom triggers and environmental context
Autonomic-Specific Modeling:
- Mechanistic Component: Implement known physiology of baroreflex function, respiratory-cardiovascular coupling, and cerebral autoregulation
- AI Component: Train machine learning algorithms on autonomic testing results (deep breathing, Valsalva, head-up tilt)
- Integration Layer: Fuse mechanistic and AI approaches through weighted consensus forecasting
Intervention Simulation:
- Test medication responses (e.g., pro-amatine, pyridostigmine) in silico before clinical use
- Simulate lifestyle interventions (exercise protocols, dietary modifications)
- Predict orthostatic tolerance under various environmental conditions
This specialized approach demonstrates how digital twin technology can be adapted to the unique challenges of specific neurological disease classes, from neurodegenerative conditions to autonomic disorders.
The convergence of systems medicine, the digital revolution, and social networking is catalyzing a profound shift in neurological care, embodied by the P4 medicine framework—Predictive, Preventive, Personalized, and Participatory. This approach represents a fundamental transformation from reactive to proactive medicine, examining patients through the lens of their interconnected biological parts and the dynamic functioning of their systems [18]. In neurological disciplines, disease emerges from the perturbation of informational networks that extend from the genome to molecules, cells, organs, the individual, and ultimately social networks [18]. The P4 approach leverages multidimensional data and machine-learning algorithms to develop interventions and monitor population health status with focus on wellbeing and healthy ageing, making it particularly relevant to neurological disorders [19].
Digital twin technology serves as the foundational engine for implementing P4 neurology in clinical practice and research. A digital twin is a dynamic, virtual replica of a patient's physiological system—in this context, the brain and nervous system—that continuously updates with real-time data to mirror the life cycle of its physical counterpart [5] [4]. This technology enables researchers and clinicians to move beyond traditional static models to interactive, adaptive systems that simulate brain dynamics in relation to pathology, therapeutic interventions, or external stimuli [4]. The integrative and adaptive nature of digital twins distinguishes them from conventional simulations; whereas simulations are typically isolated and designed for specific scenarios, digital twins are dynamic, continuously evolving models that reflect and respond to changes in the real-world system they represent [5].
The application of P4 medicine through digital twins is particularly suited to neurology due to the brain's complex network dynamics and the multifactorial nature of neurological diseases. Neurological conditions such as Postural Tachycardia Syndrome (POTS), Alzheimer's disease, brain tumors, and epilepsy exhibit complex pathophysiology that involves structural, functional, and network-level disturbances [5] [20] [4]. Digital twins offer a computational framework to model these interactions, providing a window into disease mechanisms and potential therapeutic avenues that align with the core principles of P4 medicine.
Digital Twin Technology: Enabling P4 Neurology
System Architecture and Core Components
The architecture of a neurological digital twin consists of several integrated subsystems that work in concert to create a comprehensive virtual representation. These components include: (1) Monitoring modules for continuous data acquisition from multiple sources; (2) Modeling engines that incorporate both mechanistic and artificial intelligence models of neural function; (3) Simulation platforms for running experiments and treatment scenarios; and (4) Patient-Physician interaction interfaces that facilitate communication between the patient, digital twin, and clinician [5].
This infrastructure enables the digital twin to serve as both a diagnostic and therapeutic tool. For instance, in managing Postural Tachycardia Syndrome (POTS), a digital twin can continuously monitor physiological signals such as heart rate, blood pressure, respiratory rate, and metabolic state. When the system detects inappropriate hyperventilation—a precursor to cerebral hypoperfusion and dizziness—it can alert the patient to slow their breathing through subconscious vibration signals, auditory cues, or by escalating the alert to the patient's physician for further investigation [5]. This closed-loop feedback system exemplifies the predictive and preventive dimensions of P4 medicine in clinical practice.
Data Integration and Personalization
The construction and maintenance of a high-fidelity digital twin requires continuous collection of patient data from diverse sources. Wearable devices provide real-time monitoring of vital signs like heart rate, blood pressure, end-tidal CO2, electroencephalogram patterns, and cerebral blood flow [5]. Electronic health records contribute historical data, including previous diagnoses, medical history, laboratory results, and medication records. Patient-reported outcomes capture self-reported data on symptoms, activity levels, sleep patterns, stress levels, and medication adherence. Additionally, environmental factors such as weather conditions that might influence neurological symptoms are integrated into the model [5].
Advanced neuroimaging forms a crucial data source for neurological digital twins. Magnetic resonance imaging (MRI) data, composed of 3D volumetric pixels (voxels), provides structural information about the brain [4]. Functional MRI (fMRI) measures blood flow related to neural activity, enabling simulation of brain functions and detection of patterns associated with specific cognitive tasks or disorders. Diffusion MRI (dMRI) traces water molecule movements in brain tissue, offering insights into structural connectivity between brain regions [4]. These multimodal data streams are fused to create a personalized, mathematical, dynamic brain model based on established biological principles, enabling simulation of how brain regions interact and respond to various stimuli, diseases, or potential neurosurgical interventions [4].
Table 1: Data Sources for Neurological Digital Twins
| Data Category | Specific Data Types | Application in Digital Twins |
|---|---|---|
| Clinical Data | Electronic health records, medical history, laboratory results, medication records | Establishing baseline health status and historical trends |
| Physiological Monitoring | Heart rate, blood pressure, respiratory rate, end-tidal CO2, cerebral blood flow | Real-time system status monitoring and anomaly detection |
| Neuroimaging | Structural MRI, functional MRI (fMRI), diffusion MRI (dMRI) | Mapping brain structure, function, and connectivity |
| Genetic & Molecular | Genome sequencing, proteomic data, biomarker profiles | Understanding individual susceptibility and molecular mechanisms |
| Patient-Reported Outcomes | Symptoms, activity levels, sleep patterns, medication adherence | Capturing subjective experience and quality of life metrics |
| Environmental Factors | Weather conditions, air quality, allergens | Contextualizing symptom triggers and exacerbating factors |
Application Notes: Implementing P4 Neurology
Predictive Applications: Modeling Disease Trajectories
The predictive power of P4 neurology leverages AI-driven digital twins to forecast individual patient disease progression and treatment responses. These models analyze vast amounts of research, clinical trials, and patient data to build evolving models that predict how a patient's condition might progress [5]. This capability empowers clinical teams to test hypotheses and develop new treatment plans more rapidly, potentially accelerating advances in both research and care [5].
In neuro-oncology, digital twins enable the modeling of tumor dynamics and their impact on brain function. By integrating neuroimaging data with genomic analyses and clinical outcomes, digital twins can simulate tumor effects on surrounding brain tissue and predict the efficacy of proposed treatments [4]. For example, platforms like The Virtual Brain (TVB) software integrate manifold data to construct personalized, mathematical, dynamic brain models based on established biological principles to simulate human-specific cognitive functions at the cellular and cortical level [4]. These simulations can elucidate topographical differences in neural activity responses, helping predict how brain tumors affect not only physical structures but also functional integrity.
Preventive Applications: Early Intervention Strategies
Prevention in P4 neurology operates through continuous monitoring and early detection of physiological deviations that precede clinical symptoms. Digital twins facilitate this by providing a platform for real-time physiological modeling and adaptive intervention simulations [5]. For instance, in managing autonomic disorders like POTS, digital twins can detect subtle warning signs—such as changes in heart rate or blood pressure variability—that precede acute episodes, thereby enabling preemptive interventions that reduce complications, hospitalizations, and improve outcomes [5].
The preventive capacity of digital twins also extends to lifestyle interventions. Because digital twins are continuously updated with real-time patient data, they can provide immediate feedback on how lifestyle changes affect a patient's health [5]. If a patient with a neurological condition begins an exercise program, the digital twin could monitor vital signs like heart rate, blood pressure, and respiratory pattern in real time, allowing adjustments to the plan as needed [5]. This dynamic feedback loop represents a significant advancement over traditional static lifestyle recommendations.
Personalized Applications: Precision Therapeutics
Personalization in P4 neurology represents the move from population-based treatment protocols to individually tailored interventions. Digital twins enable this by simulating patient-specific responses to medications and other therapies. For example, POTS patients often respond differently to medications like pro-amatine or pyridostigmine due to their unique autonomic profiles [5]. A digital twin can guide personalized dosing, reducing trial-and-error and minimizing side effects [5].
In the drug development pipeline, digital twins create highly detailed and dynamic virtual models of patients that enable researchers to simulate and predict how new drugs interact with different biological systems [15]. This approach is particularly valuable for neurological conditions where blood-brain barrier penetration, target engagement, and neuropharmacokinetics present unique challenges. During clinical trial simulation, digital twins can generate virtual cohorts that resemble real-world populations to model various dosing regimens, treatment plans, and patient selection factors, thereby improving trial design and success probability [15].
Participatory Applications: Engaging Patients as Partners
The participatory dimension of P4 neurology acknowledges patients as active partners in their health management rather than passive recipients of care. Digital twins facilitate this participation through intuitive interfaces that allow patients to visualize their health status, understand the potential outcomes of different choices, and actively contribute to their care decisions [18]. Patient-driven social networks will demand access to data and better treatments, further reinforcing this participatory model [18].
Digital twin platforms can enhance patient engagement by providing educational simulations that help patients understand their conditions and treatment rationales. For example, a patient with epilepsy might interact with a digital twin that visualizes how their seizure activity propagates through brain networks and how a proposed medication or neurostimulation approach would modulate this activity. This demystification of neurological disease empowers patients to actively participate in therapeutic decisions and adhere to treatment plans.
Table 2: P4 Applications in Neurological Conditions
| Neurological Condition | Predictive Application | Preventive Application | Personalized Application | Participatory Application |
|---|---|---|---|---|
| Postural Tachycardia Syndrome (POTS) | Forecast cerebral hypoperfusion episodes from respiratory patterns [5] | Preemptive breathing alerts to prevent dizziness [5] | Tailored medication dosing based on autonomic profile [5] | Patient interaction with digital twin for lifestyle adjustments [5] |
| Alzheimer's Disease & Related Dementias | Model disease progression using multifactorial risk algorithms [20] | Early detection through biomarker monitoring and lifestyle intervention [21] [20] | Customized drug combinations targeting multiple pathways [20] | Brain Care Score tools for patient-driven risk reduction [21] |
| Brain Tumors | Simulate tumor growth and functional impact on brain networks [4] | Optimization of surgical approaches to preserve function [4] | Individualized resection plans based on functional mapping [4] | Visualized surgical outcomes for informed consent [4] |
| Epilepsy | Identify seizure precursors from neurophysiological patterns | Adjust neuromodulation parameters preemptively | Tailored antiepileptic drug regimens | Patient-reported seizure diaries integrated with digital twin |
Experimental Protocols for Digital Twin Implementation
Protocol 1: Constructing a Base Digital Twin Framework
Objective: To create a foundational digital twin architecture for neurological applications that integrates multimodal data sources and supports basic simulation capabilities.
Materials and Equipment:
- High-performance computing infrastructure with GPU acceleration
- Data integration platform (e.g., Open Digital Twin Project, PyTwin, Simply) [5]
- Secure data storage solution compliant with healthcare regulations
- Wearable sensors for physiological monitoring (heart rate, blood pressure, activity)
- Neuroimaging capabilities (MRI, fMRI, dMRI)
- Laboratory information system access for genomic and biomarker data
Methodology:
- Data Acquisition and Harmonization: Collect multimodal patient data including structural neuroimaging (T1-weighted MRI), functional connectivity (resting-state fMRI), white matter tractography (dMRI), genetic profiling (APOE status for dementia risk), clinical history, and baseline cognitive assessments. Implement data harmonization protocols to manage variability across different imaging platforms and ensure consistency [4].
Model Initialization: Utilize established computational frameworks like The Virtual Brain (TVB) to construct an initial base model [4]. Parameterize the model using the collected patient data to create a personalized brain network model. This involves mapping individual connectivity matrices derived from dMRI data and adjusting neural mass model parameters to fit individual fMRI dynamics.
Model Validation and Refinement: Implement a validation pipeline where the digital twin's predictions are compared against actual patient outcomes. Use discrepancy measures to iteratively refine model parameters through machine learning approaches. Employ techniques such as SHapley Additive exPlanations (SHAP) to enhance model transparency and interpretability [15].
Interface Development: Create clinician and patient-facing interfaces that display the digital twin's status, simulations, and recommendations in an intuitive format. Ensure these interfaces integrate with existing electronic health record systems for seamless clinical workflow integration [5].
Quality Control Considerations:
- Implement rigorous data quality checks at each acquisition stage
- Establish protocols for handling missing or noisy data
- Conduct regular model performance assessments against holdout datasets
- Maintain audit trails of all model modifications and updates
Protocol 2: Clinical Trial Enhancement with Digital Twins
Objective: To employ digital twins as virtual control arms in neurological clinical trials, reducing recruitment needs while maintaining statistical power.
Materials and Equipment:
- Historical clinical trial data for model training
- AI-based digital twin platform capable of generating synthetic control arms
- Randomization and trial management system
- Statistical analysis software adapted for digital twin integration
Methodology:
- Digital Twin Development: Create digital twins for trial participants by training models on comprehensive historical control datasets derived from previous clinical trials, disease registries, and real-world evidence studies [15]. For each real participant enrolled in the experimental arm, generate a matched digital twin that simulates their expected disease progression under standard care.
Trial Design Implementation: Implement an adaptive trial design where the digital twins serve as a virtual control cohort. In this approach, each real participant receiving the experimental treatment is paired with a digital twin whose progression is projected under standard care, offering comparator data without exposing additional patients to a placebo [15].
Treatment Effect Estimation: Calculate treatment effects by comparing outcomes between the experimentally-treated patients and their digitally-modeled counterparts under control conditions. Employ Bayesian statistical methods that incorporate the uncertainty in digital twin predictions into the treatment effect estimates [22].
Validation and Calibration: Continuously validate digital twin predictions against any actual control patients enrolled in the trial (if applicable). Calibrate models based on any discrepancies to improve accuracy throughout the trial period.
Statistical Considerations:
- Conduct power analyses that account for the precision added by digital twins
- Implement bias detection algorithms to identify systematic prediction errors
- Pre-specified statistical analysis plans that define how digital twin data will be incorporated
- Sensitivity analyses to assess robustness of findings to model assumptions
The following diagram illustrates the fundamental workflow for creating and utilizing a digital twin in neurological research and care:
Protocol 3: Personalized Therapeutic Optimization for Neurological Disorders
Objective: To utilize digital twins for simulating individual patient responses to neurological therapies and optimizing treatment parameters.
Materials and Equipment:
- Validated digital twin platform with therapeutic simulation capabilities
- Drug databases with pharmacokinetic and pharmacodynamic parameters
- Neuromodulation equipment interfaces (for DBS, TMS, etc.)
- High-fidelity physiological monitoring systems
Methodology:
- Baseline Characterization: Conduct comprehensive phenotyping of the patient's neurological status using quantitative assessments, including cognitive testing, motor evaluation, autonomic function tests, and quality of life measures. Integrate these data with the patient's digital twin.
Intervention Simulation: Simulate the effects of potential therapeutic interventions on the digital twin. For pharmacological approaches, this involves modeling drug pharmacokinetics and pharmacodynamics based on the patient's metabolic profile and blood-brain barrier characteristics. For neuromodulation approaches, simulate the electrical field distributions and their effects on neural circuitry.
Response Prediction: Use the digital twin to forecast acute and long-term responses to each potential intervention, including both therapeutic effects and adverse events. For example, in Parkinson's disease, simulate how different deep brain stimulation parameters would affect network dynamics across the basal ganglia-thalamocortical circuit.
Optimization and Personalization: Employ optimization algorithms to identify intervention parameters that maximize predicted therapeutic benefit while minimizing adverse effects. This may include dose titration schedules for medications or parameter settings for neuromodulation devices.
Closed-Loop Refinement: Implement a closed-loop system where the digital twin is continuously updated with real-world patient response data, allowing for dynamic refinement of therapeutic recommendations over time.
Clinical Validation:
- Compare digital twin predictions with actual patient responses
- Conduct n-of-1 trials to validate personalized recommendations
- Assess clinical outcomes compared to standard care approaches
- Evaluate patient engagement and satisfaction with personalized recommendations
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Research Reagents and Computational Tools for Neurological Digital Twins
| Tool Category | Specific Examples | Function/Application | Key Characteristics |
|---|---|---|---|
| Computational Platforms | The Virtual Brain (TVB) [4] | Whole-brain simulation platform | Personalized brain network models, biologically realistic neural mass models |
| Open Digital Twin Project, PyTwin, Simply [5] | General digital twin development | Python-based, open-source, modular architecture for physical systems | |
| Data Acquisition Tools | Multimodal MRI (fMRI, dMRI) [4] | Brain structure and function mapping | Voxel-based data on brain structure, functional connectivity, and structural connectivity |
| Wearable physiological monitors [5] | Continuous vital sign monitoring | Real-time heart rate, blood pressure, respiratory rate, activity levels | |
| AI/Modeling Frameworks | Deep generative models [15] | Synthetic patient cohort generation | Replicate underlying structure of real-world populations for clinical trials |
| SHapley Additive exPlanations (SHAP) [15] | Model interpretability and transparency | Explains output of complex machine learning models | |
| Therapeutic Simulation | TumorTwin software [5] | Cancer care applications | Integrates medical imaging with mathematical modeling to tailor interventions |
| Pharmacokinetic/pharmacodynamic models [15] | Drug response prediction | Simulates medication absorption, distribution, metabolism, and effect |
The integration of P4 medicine principles with digital twin technology represents a paradigm shift in neurology, transitioning the field from reactive disease management to proactive health optimization. This approach leverages predictive modeling to forecast disease trajectories, preventive strategies to intercept pathological processes, personalized interventions tailored to individual biology and circumstances, and participatory engagement that empowers patients as active partners in their care.
Digital twins serve as the computational engine that makes P4 neurology practicable, providing dynamic virtual representations of patients that continuously update with real-world data. These models enable simulation of disease processes, prediction of therapeutic responses, and optimization of interventions before their implementation in actual patients. The implementation frameworks and experimental protocols outlined in this article provide researchers and clinicians with practical roadmaps for deploying these advanced approaches across various neurological conditions.
As digital twin technology continues to evolve alongside advances in neuroimaging, biosensing, and artificial intelligence, its capacity to transform neurological care will expand accordingly. Future developments will likely include more sophisticated multi-scale models that span from molecular to systems levels, enhanced real-time integration with wearable and implantable devices, and more intuitive interfaces for both clinicians and patients. Through these advancements, P4 medicine powered by digital twins promises to deliver more precise, proactive, and patient-centered neurological care.
Building and Applying Neurological Digital Twins: AI, Data, and Clinical Workflows
The emergence of the digital twin paradigm represents a transformative approach in neurological disease research. A digital twin is a "computational model that describes the evolution of an individual's health over time," creating a virtual representation of a patient that can simulate disease progression and treatment response in silico [12]. The fidelity of these models depends entirely on the quality, breadth, and temporal resolution of the input data. This necessitates sophisticated data acquisition strategies that integrate multidimensional biomarkers across complementary modalities [23] [24]. For complex neurological disorders such as Alzheimer's disease (AD) and Parkinson's disease (PD), which exhibit considerable heterogeneity in progression patterns and treatment response, digital twins offer the potential to personalize disease management and accelerate therapeutic development [12] [7].
The development of accurate digital twins requires the integration of four critical data domains: multi-omics profiles for molecular-level insights, neuroimaging for structural and functional assessment, wearable sensor data for continuous real-world monitoring, and EHR for comprehensive clinical contextualization. Each domain captures distinct aspects of the disease phenotype, and their integration creates a more holistic representation of the pathological processes [25] [24]. This application note provides detailed protocols and frameworks for acquiring and integrating these diverse data types to build robust digital twin models for neurological disease progression research.
Data Acquisition Protocols
Multi-Omics Profiling
Multi-omics data integration provides unprecedented insights into the molecular mechanisms underlying neurological diseases, capturing interactions across genomic, transcriptomic, proteomic, and metabolomic layers [24]. The integration of these disparate data types is essential for constructing comprehensive digital twin models.
Table 1: Multi-Omics Data Types and Their Relevance to Neurological Digital Twins
| Data Type | Key Biomarkers | Relevance to Digital Twins | Acquisition Methods |
|---|---|---|---|
| Genomics | APOE ε4 genotype, disease-risk SNPs | Baseline risk stratification, progression forecasting | Whole-genome sequencing, targeted SNP arrays |
| Transcriptomics | Gene expression patterns, miRNA signatures | Monitoring disease activity states, treatment response | RNA-seq, single-cell RNA-seq |
| Proteomics | Aβ42, p-Tau, NfL, GFAP | Dynamic tracking of central pathological processes | Mass spectrometry, immunoassays |
| Metabolomics | Lipid profiles, energy metabolites | Functional readout of physiological state, treatment effects | LC-MS, NMR spectroscopy |
Protocol 1.1: Cerebrospinal Fluid (CSF) and Blood Plasma Proteomic Profiling for Alzheimer's Disease Digital Twins
Purpose: To acquire quantitative protein biomarker data for input into AD digital twin models, enabling tracking of amyloid pathology, tau pathology, and neuronal injury.
Materials:
- Paired CSF and blood plasma samples
- Proteomic sample preparation kit
- Mass spectrometer (e.g., LC-MS/MS system)
- Multiplex immunoassay platform for validation
- Low-protein-binding tubes and pipettes
Procedure:
- Sample Collection: Collect CSF via lumbar puncture (10-15 mL) and blood (20 mL) in appropriate containers. Process plasma within 2 hours of collection by centrifugation at 2,000 × g for 10 minutes.
- Sample Preparation: Concentrate CSF using 10kDa molecular weight cut-off filters. Digest proteins with trypsin (1:50 enzyme-to-substrate ratio) overnight at 37°C.
- Data Acquisition: Analyze digested peptides using LC-MS/MS with a 120-minute gradient. Use data-independent acquisition (DIA) for comprehensive proteome coverage.
- Quality Control: Include pooled quality control samples after every 10 injections to monitor instrument performance. Assess coefficient of variation (<15% for high-abundance proteins).
- Data Processing: Process raw files using Spectronaut or similar software. Normalize data using global intensity normalization.
- Biomarker Validation: Confirm key AD biomarkers (Aβ42, p-Tau181, NfL) using validated ELISA or SIMOA assays.
Computational Integration: Processed proteomic data should be structured in a matrix format with samples as rows and protein intensities as columns, annotated with clinical metadata for integration with other data modalities in the digital twin framework.
Neuroimaging Data Acquisition
Neuroimaging provides critical structural and functional information for digital twin models, with magnetic resonance imaging (MRI) serving as a cornerstone for tracking brain changes in neurological disorders [26] [27].
Protocol 2.1: Accelerated MRI Acquisition with Super-Resolution Reconstruction for High-Throughput Digital Twin Applications
Purpose: To reduce MRI acquisition time while maintaining diagnostic quality for hippocampal volumetry and other structural measurements in digital twin models.
Materials:
- 3T MRI scanner with parallel imaging capabilities
- Standard head coil (e.g., 32-channel)
- Computing workstation with GPU acceleration
- Pix2Pix network implementation (TensorFlow or PyTorch)
Procedure:
- Protocol Setup: Implement a compressed sensing accelerated 3D T1-weighted sequence (e.g., MPRAGE) with acceleration factor R=4, reducing acquisition time from approximately 6 minutes to 3.5 minutes.
- Image Acquisition: Acquire both high-resolution (256 × 256 matrix, 1mm isotropic) and low-resolution (64 × 64 matrix, 4mm isotropic) images for training purposes.
- Network Training:
- Preprocess training images with zero-filling to create square matrices (256 × 256)
- Downsample high-resolution images using bicubic interpolation to create low-resolution inputs
- Train Pix2Pix network with U-Net generator and PatchGAN discriminator
- Use L1 loss with weight λ = 1×10³ and adversarial loss
- Train for minimum 200 epochs with batch size 1
- Super-Resolution Generation: Apply trained model to low-resolution acquisitions to generate super-resolution images (256 × 256) for analysis.
- Quality Assessment: Evaluate generated images using PSNR (>27 dB target) and MS-SSIM (>0.96 target) metrics [26].
- Volumetric Analysis: Process both original and generated super-resolution images through BAAD software or similar automated hippocampal volumetry pipeline.
Computational Integration: The super-resolution imaging pipeline enables more frequent assessment of structural changes in digital twin models by reducing acquisition time constraints, providing temporal data on brain atrophy rates for progression forecasting.
Diagram 1: Super-Resolution MRI Pipeline for Digital Twin Structural Data Acquisition
Wearable Sensor Data Acquisition
Wearable devices enable continuous, real-world monitoring of motor function, daily activities, and physiological parameters, providing high-temporal-resolution data that captures disease progression and fluctuation in natural environments [28].
Table 2: Wearable Sensor Modalities for Neurological Digital Twins
| Sensor Type | Parameters Measured | Clinical Relevance | Device Examples |
|---|---|---|---|
| Inertial Measurement Units (IMUs) | Gait speed, stride length, tremor frequency, joint range of motion | Motor symptom progression, treatment response | ErgoLAB system, Opal sensors |
| Force Sensors | Muscle strength, grip strength | Disease progression in NMDs, stroke recovery | Digital dynamometers |
| Electrophysiological Sensors | EEG, ECG, EMG | Seizure detection, autonomic dysfunction, muscle activity | Head-mounted eye trackers, smart watches |
| Soft Strain Sensors | Muscle deformation, swallowing function | Bulbar function in ALS, PD | Novel research prototypes |
Protocol 3.1: Continuous Motor Function Monitoring for Parkinson's Disease Digital Twins
Purpose: To acquire quantitative, continuous data on motor symptoms in real-world settings for PD digital twin calibration and validation.
Materials:
- Opal APDM sensors or similar IMU-based system
- Smartphone application for patient-reported outcomes
- Cloud data infrastructure for continuous data upload
- Algorithm processing pipeline for feature extraction
Procedure:
- Sensor Configuration: Deploy six IMU sensors (wrists, ankles, trunk, sternum) with sampling rate ≥128 Hz. Ensure sensors contain tri-axial accelerometers, gyroscopes, and magnetometers.
- Data Collection Protocol:
- Continuous monitoring: 12 hours per day for 7 days to capture diurnal variations
- Structured tasks: 30-second resting tremor assessment, 10-meter walk test, timed up-and-go test
- Patient-reported symptoms: Through smartphone app 3x daily (morning, afternoon, evening)
- Feature Extraction:
- Gait parameters: stride length, cadence, swing time variability, turning velocity
- Tremor metrics: amplitude, frequency, duration during rest and action
- Bradykinesia: movement speed, amplitude decrement during repetitive tasks
- Data Quality Control:
- Implement sensor wear detection algorithm to identify non-wear periods
- Apply signal quality indices to identify motion artifacts
- Use automated outlier detection to flag physiologically implausible values
- Data Aggregation: Calculate daily summaries (mean, variability) for each motor feature, maintaining temporal alignment with medication logs.
Computational Integration: Motor features should be timestamped and structured in a time-series database aligned with other data streams. These data provide the high-frequency behavioral measurements needed to calibrate the motor component of PD digital twins and detect subtle progression between clinical visits.
Electronic Health Records (EHR) Data Extraction
EHR systems contain rich longitudinal clinical data that provide essential context for digital twin models, but extracting research-quality data requires careful methodology to address inconsistencies and missing data [29] [30].
Protocol 4.1: Structured EHR Data Extraction for Neurological Digital Twin Cohorts
Purpose: To extract and structure EHR data for digital twin development while addressing common challenges in clinical data quality and completeness.
Materials:
- EHR database access (e.g., Epic, Cerner, or custom system)
- OMOP Common Data Model infrastructure
- Secure data warehouse environment
- ETL (Extract, Transform, Load) pipelines
Procedure:
- Cohort Definition:
- Identify eligible patients using structured diagnosis codes (ICD-10), medication records, and clinical notes
- Apply inclusion/exclusion criteria systematically across all data domains
- Document cohort selection process with flow diagram
Data Domain Extraction:
- Demographics: age, sex, race, education level
- Diagnoses: all neurological and relevant comorbid conditions
- Medications: drug name, dose, frequency, duration with start/stop dates
- Laboratory results: all values with timestamps and reference ranges
- Procedures: neurosurgical interventions, neuromodulation therapies
- Clinical assessments: MMSE, CDR-SB, UPDRS when available
Temporal Alignment:
- Establish index date (e.g., diagnosis date, treatment initiation)
- Align all clinical events relative to index date
- Resolve conflicting timestamps through manual review of sample records
Data Quality Assessment:
- Implement METRIC framework (Measure process, Timeliness, Representativeness, Informativeness, Consistency)
- Calculate completeness metrics for key variables (>80% target for critical variables)
- Assess plausibility of clinical values through range checks and cross-validation
Feature Engineering:
- Create derived variables (e.g., disease duration, treatment exposure duration)
- Calculate comorbidity indices (Charlson, Elixhauser)
- Implement imputation strategies for missing data with appropriate documentation
Computational Integration: Extracted EHR data should be structured according to OMOP CDM standards to facilitate integration across sites. Clinical variables serve as anchoring points for digital twin calibration and provide ground truth for model validation.
Integration Framework and Computational Tools
The integration of multi-modal data requires sophisticated computational frameworks that can handle heterogeneous data types while maintaining temporal relationships essential for dynamic disease progression modeling.
Diagram 2: Multi-Modal Data Integration Framework for Neurological Digital Twins
Computational Protocol 5.1: Conditional Restricted Boltzmann Machine (CRBM) for Digital Twin Generation
Purpose: To integrate multi-modal patient data and generate personalized digital twins for neurological disease progression forecasting.
Materials:
- Harmonized multi-modal dataset (multi-omics, imaging, wearables, EHR)
- High-performance computing cluster with GPU acceleration
- CRBM implementation (Python/PyTorch)
- Historical cohort data for training (e.g., ADNI, CPAD)
Procedure:
- Data Harmonization:
- Align all data modalities to common temporal grid
- Normalize continuous variables to z-scores
- Encode categorical variables using one-hot encoding
- Handle missing data using multivariate imputation
Model Architecture:
- Implement CRBM with two-layer structure (visible and hidden units)
- Configure visible layer to accommodate mixed data types (Gaussian for continuous, binary for categorical)
- Initialize hidden layer with 500-1000 units depending on data complexity
- Include conditioning layer for baseline patient characteristics
Model Training:
- Pre-train model on historical dataset (e.g., 6,736 subjects from CODR-AD and ADNI) [12]
- Use contrastive divergence with 1-step Gibbs sampling (CD-1)
- Train for minimum 100 epochs with learning rate 0.01
- Apply early stopping with patience of 10 epochs
Digital Twin Generation:
- Input baseline patient data into conditioned visible layer
- Generate probabilistic predictions of disease progression under placebo conditions
- Run multiple simulations to capture prediction uncertainty
Model Validation:
- Assess correlation between predicted and actual outcomes in held-out test set
- Evaluate clinical utility through sample size reduction estimates in simulated trials
- Validate across diverse patient subgroups to assess generalizability
Implementation Considerations: The CRBM approach qualified by EMA as PROCOVA methodology can reduce sample size requirements by 9-15% in Alzheimer's trials while maintaining statistical power [12]. This makes it particularly valuable for accelerating therapeutic development in neurological disorders.
Research Reagent Solutions
Table 3: Essential Research Tools for Neurological Digital Twin Development
| Tool Category | Specific Solutions | Application in Digital Twins | Key Features |
|---|---|---|---|
| Data Acquisition Platforms | ErgoLAB multi-channel wearable system | Continuous motor function monitoring | Synchronous acquisition of facial, neck, and respiratory muscle parameters |
| Biosensor Technologies | Electrochemical CRISPR-based biosensors | Ultra-sensitive biomarker detection | Femtomolar detection of Aβ, Tau in blood, saliva, tears |
| Neuroimaging Software | BAAD (Brain Anatomical Analysis with Diffeomorphic deformation) | Hippocampal volumetry for AD progression | Machine learning-enhanced voxel-based morphometry |
| Multi-Omics Integration | Variational Autoencoders (VAEs) | Integration of genomic, transcriptomic, proteomic data | Handles high-dimensionality, missing data, identifies latent factors |
| Digital Twin Generation | Conditional Restricted Boltzmann Machine (CRBM) | Patient-specific progression forecasting | Generates placebo predictions from baseline characteristics |
| EHR Data Management | OMOP Common Data Model | Standardized clinical data structure | Enables multicenter data integration and federated learning |
The development of accurate digital twins for neurological disease progression requires methodical acquisition and integration of multi-modal data streams. The protocols presented here provide a framework for generating high-quality data across omics, imaging, wearable sensors, and EHR domains. When integrated using advanced computational approaches like CRBMs, these data enable the creation of dynamic patient-specific models that can forecast disease progression and simulate intervention outcomes. As these technologies mature, they hold the potential to transform neurological disease research from population-level generalizations to truly personalized predictions, ultimately accelerating therapeutic development and improving patient outcomes.
Digital twins—dynamic, virtual replicas of physical systems—are emerging as a transformative tool in neurological disease research, enabling personalized prediction of disease progression and evaluation of therapeutic interventions [12] [5]. The construction of effective digital twins relies heavily on sophisticated computational architectures that can learn from complex, multimodal clinical data. Two distinct yet complementary approaches have shown significant promise: Conditional Restricted Boltzmann Machines (CRBMs) and Foundation Models. CRBMs are probabilistic graphical models that generate multivariate patient trajectories by learning the joint probability distribution of clinical variables over time [31]. In contrast, Foundation Models are large-scale neural networks trained on vast datasets that can be adapted to diverse downstream tasks through transfer learning [32] [33]. This application note examines both architectural paradigms within the context of neurological digital twin development, providing technical specifications, performance comparisons, and detailed experimental protocols for researchers and drug development professionals.
Table 1: Core Architectural Comparison Between CRBMs and Foundation Models
| Feature | Conditional Restricted Boltzmann Machine (CRBM) | Foundation Model |
|---|---|---|
| Primary Architecture | Undirected probabilistic graphical model with visible and latent units [31] | Transformer, diffusion, or other deep learning architectures [32] [34] |
| Training Data Scale | Thousands of patient records (e.g., 1,909-6,736 patients) [12] [31] | Massive datasets (e.g., 45GB+ text, millions of images) [34] |
| Training Approach | Self-supervised, maximum likelihood with adversarial training [31] | Self-supervised learning on broad data [32] [33] |
| Output Capability | Simulates evolution of multiple clinical variables simultaneously [31] | Generates predictions, content, or classifications across modalities [32] |
| Key Advantage | Probabilistic forecasting of entire patient profiles | Exceptional generalization and adaptation to new tasks |
Technical Specifications and Performance Metrics
Conditional Restricted Boltzmann Machines (CRBMs)
CRBMs are particularly suited for modeling the progression of multifactorial neurological conditions such as Alzheimer's Disease (AD) and Mild Cognitive Impairment (MCI). Their architecture effectively captures the stochastic nature of disease progression by learning conditional probability distributions between time points [31]. A CRBM defines its probability density through an energy function that incorporates connections between visible variables (clinical measurements) and latent variables (learned representations), with parameters learned through contrastive divergence or adversarial training approaches [35] [31].
In practical application, CRBMs have demonstrated robust performance in forecasting AD progression. When trained on the Coalition Against Major Diseases (CAMD) Online Data Repository for AD, containing 18-month trajectories of 44 clinical variables from 1,909 patients, CRBMs successfully simulated the evolution of individual components of cognitive exams, laboratory tests, and their correlations [31]. The model achieved prediction accuracy for changes in total ADAS-Cog scores comparable to specifically trained supervised models, while additionally capturing the correlation structure across all sub-components.
Table 2: CRBM Performance in Neurological Digital Twin Applications
| Application Context | Dataset | Key Performance Metrics | Outcome |
|---|---|---|---|
| Alzheimer's Disease Progression Forecasting [31] | 1,909 patients with MCI/AD from CODR-AD; 44 variables over 18 months | Accuracy in predicting change in ADAS-Cog score vs. supervised models; Statistical fidelity of synthetic data | Matched specialized supervised models; Synthetic data indistinguishable from real data by logistic regression |
| Clinical Trial Efficiency (AWARE Trial) [12] | Harmonized dataset of 6,736 unique subjects from historical trials + ADNI | Partial correlation between DT predictions and actual outcomes (0.30-0.46); Residual variance reduction | 9-15% reduction in total sample size; 17-26% reduction in control arm size |
Foundation Models
Foundation Models represent a paradigm shift in AI applications for healthcare, characterized by their massive scale, broad training data, and exceptional adaptability [32] [33]. These models typically employ transformer architectures with self-attention mechanisms that enable them to capture complex patterns across diverse data types. In neuroscience specifically, foundation models have been trained on extensive neural activity data to predict neuronal responses to novel stimuli with remarkable generalization capabilities [36].
A recent breakthrough application in neuroscience involved training a foundation model on neural activity from visual cortices of multiple mice, achieving accurate prediction of neuronal responses to both natural videos and novel stimulus types like coherent motion and noise patterns [36]. The model generalized effectively to new subjects with minimal retraining and successfully predicted anatomical cell types, dendritic features, and neuronal connectivity, demonstrating its utility as a foundational tool for neural circuit analysis.
Application Notes for Neurological Digital Twins
Digital Twin Framework for Alzheimer's Disease Clinical Trials
The integration of CRBM-generated digital twins into clinical trial design represents a significant advancement for neurological drug development. The following workflow outlines the implementation process:
This workflow demonstrates how CRBMs trained on historical clinical data (6,736 subjects from 29 trials plus ADNI data) generate digital twins that serve as prognostic covariates in the PROCOVA statistical framework [12]. When applied to the AWARE Phase 2 clinical trial for Alzheimer's Disease, this approach demonstrated significant efficiency improvements, reducing total sample size requirements by 9-15% and control arm size by 17-26% while maintaining statistical power [12].
Foundation Models for Neural Activity Prediction
Foundation models for neural simulation employ sophisticated modular architectures to accurately predict brain activity across diverse conditions:
This modular foundation model architecture for neural activity prediction incorporates specialized components for processing visual perspectives and behavioral modulation, feeding into a core network that combines 3D convolutional layers with recurrent LSTM components [36]. When trained on approximately 135,000 neurons across multiple visual cortex areas, this architecture achieved a 25-46% increase in predictive accuracy compared to previous models and demonstrated remarkable generalization to novel stimulus domains including coherent motion and noise patterns [36].
Experimental Protocols
Protocol: CRBM for Alzheimer's Disease Progression Forecasting
Objective: Train a Conditional Restricted Boltzmann Machine to generate digital twins for forecasting Alzheimer's Disease progression and simulating clinical trials.
Materials and Data Sources:
- Patient data from CODR-AD and ADNI databases (6,736 subjects recommended) [12]
- Clinical variables: CDR-SB, ADAS-Cog components, MMSE, FAQ, demographics, genetic factors [31]
- Computational resources: Standard GPU workstation sufficient for CRBM training
Procedure:
Data Harmonization and Preprocessing
- Combine data from multiple historical clinical trials and observational studies
- Select 44+ clinical variables covering cognitive assessments, functional measures, and biomarkers
- Structure data into 3-month intervals across 18-month trajectories
- Split data into training (80%), validation (5%), and test sets (20%) using 5-fold cross-validation [31]
CRBM Model Configuration
Digital Twin Generation
- Initialize with baseline patient data
- Iteratively sample future time points using conditional distribution P(x(t))|x(t-1))
- Generate multiple trajectories to capture prognostic uncertainty
Clinical Trial Simulation
- Integrate digital twins as prognostic covariates in PROCOVA-MMRM analysis model [12]
- Calculate sample size requirements with and without digital twin adjustment
- Validate against actual clinical trial outcomes (e.g., AWARE trial)
Validation Metrics:
- Partial correlation between predicted and actual outcomes (target: 0.30-0.46) [12]
- Residual variance reduction (target: 9-15%) [12]
- Statistical indistinguishability of synthetic vs. real data (logistic regression test) [31]
Protocol: Foundation Model for Neural Activity Prediction
Objective: Develop and adapt a foundation model to predict neural activity across multiple subjects and stimulus domains.
Materials and Data Sources:
- Neural recording data from visual cortices (135,000+ neurons recommended) [36]
- Stimulus sets: Natural videos, moving dots, Gabor patches, noise patterns
- Behavioral data: Locomotion, pupil dilation, eye tracking
- Computational resources: Extensive GPU cluster for foundation model training
Procedure:
Large-Scale Data Collection
- Record neural responses to natural videos from multiple visual areas (V1, LM, RL, AL, AM, PM)
- Collect complementary behavioral data (locomotion, pupil diameter)
- Aggregate data across 8+ subjects for foundation cohort
Foundation Model Training
- Implement four-module architecture: perspective, modulation, core, readout [36]
- Core architecture: 3D convolutional layers + LSTM recurrent components
- Train using Poisson negative-log likelihood loss function
- Freeze core parameters after foundation training
Model Adaptation to New Subjects
- Transfer frozen foundation core to new subjects
- Fit only perspective, modulation, and readout components with limited new data (4-76 minutes)
- Compare against individual models trained end-to-end without foundation
Generalization Testing
- Evaluate predictive accuracy on novel stimulus domains
- Test capacity to predict anatomical features and connectivity
- Measure cross-subject and cross-area performance consistency
Validation Metrics:
- Normalized correlation coefficient (CCnorm) between predicted and recorded neural activity
- Data efficiency: Training time required to achieve CCnorm > 0.65
- Generalization accuracy across stimulus domains and anatomical predictions
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Digital Twin Implementation in Neurological Research
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Data Repositories | CODR-AD (Coalition Against Major Diseases) [31], ADNI (Alzheimer's Disease Neuroimaging Initiative) [12] | Source of harmonized clinical trial data and neuroimaging data for model training |
| Model Architectures | Conditional Restricted Boltzmann Machine (CRBM) [31], Transformer-based Foundation Models [36] | Core algorithmic frameworks for generating digital twins and predicting neural activity |
| Software Platforms | Simply, Open Digital Twin Project, PyTwin [5] | Open-source Python platforms for implementing digital twin workflows |
| Validation Frameworks | PROCOVA (Prognostic Covariate Adjustment) [12], 5-fold cross-validation [31] | Statistical methods for validating digital twin predictions in clinical trial contexts |
| Computational Resources | GPU clusters (NVIDIA A100 for large models) [34], Standard GPU workstations (for CRBMs) | Hardware infrastructure for model training and inference |
Conditional Restricted Boltzmann Machines and Foundation Models offer distinct yet complementary architectural approaches for developing digital twins in neurological disease research. CRBMs provide a robust, probabilistic framework for forecasting multi-dimensional disease progression and optimizing clinical trials, with demonstrated efficacy in Alzheimer's Disease applications [12] [31]. Foundation Models deliver exceptional generalization capabilities and cross-modal adaptability, showing particular promise in neural activity prediction and analysis [36]. The choice between these architectures depends on specific research objectives: CRBMs are ideally suited for clinical trial optimization with limited data, while Foundation Models excel in scenarios requiring broad generalization across subjects and conditions. As digital twin methodologies continue to evolve, both architectures will play crucial roles in advancing personalized neurology and accelerating therapeutic development.
The complexity of neurological diseases, with their multifaceted pathogenesis spanning molecular, cellular, and systemic levels, presents a formidable challenge for traditional modeling approaches [37]. Digital twins—dynamic virtual representations of physical systems updated with real-world data—are emerging as a transformative paradigm in biomedical research, enabling patient-specific simulation, prediction, and treatment optimization [38] [11]. The development of effective digital twins for neurology hinges on the strategic integration of two complementary modeling philosophies: mechanistic (physics-based) models derived from established biological principles and data-driven (AI) models that extract complex patterns from high-dimensional biomedical data [39] [40]. This integration is particularly critical for neurodegenerative diseases like Alzheimer's and Parkinson's, where disease progression involves nonlinear interactions across multiple biological scales that are difficult to capture with any single approach [41] [37]. By combining first-principles understanding with data-driven insights, researchers can create more accurate, predictive, and clinically actionable digital twin frameworks for neurological disease management.
Table: Fundamental Characteristics of Modeling Approaches for Neurological Digital Twins
| Feature | Mechanistic/Physics-Based Models | Data-Driven/AI Models | Hybrid Models |
|---|---|---|---|
| Theoretical Basis | Established physical laws and biological principles (e.g., Fisher-Kolmogorov equation) [11] | Patterns learned from data via neural networks (CNNs, RNNs, GNNs) [41] | Integrates both physical laws and data patterns [42] |
| Data Requirements | Can operate with limited data based on first principles [39] | Require large, high-quality datasets for training [41] | Flexible, benefits from both physics and data availability [42] |
| Interpretability | High; model structure reflects known biology [40] | Low; often "black box" with limited inherent explainability [41] | Variable; depends on integration strategy, can be designed for explainability [42] |
| Strengths | Reliable extrapolation, strong theoretical foundation [40] | Excellence at pattern recognition in complex data [41] | Balanced performance, leveraging strengths of both parent approaches [39] [42] |
| Clinical Application Example | Simulating protein misfolding spread in neurodegeneration [11] | Classifying disease subtypes from neuroimaging [41] | Personalizing radiotherapy planning for brain tumors [11] |
Foundational Technologies and Modeling Approaches
Mechanistic Modeling Foundations
Mechanistic modeling for neurological digital twins employs mathematical formalisms grounded in the biophysics of disease processes. A prominent application involves using the Fisher-Kolmogorov equation to simulate the anisotropic diffusion and spread of misfolded proteins (e.g., tau, α-synuclein) across brain networks, capturing both spatial and temporal aspects of neurodegenerative progression [11]. These physics-based models integrate neuroimaging data to create patient-specific simulations of pathology spread, providing a window into disease trajectory based on known biological principles. At the organ level, finite element analysis and computational fluid dynamics principles are adapted to model whole-organ brain mechanics and cerebrospinal fluid dynamics, though these approaches often face computational constraints when applied to real-time clinical decision support [40].
Data-Driven Modeling Architectures
Artificial intelligence, particularly deep learning, provides a powerful toolkit for analyzing the complex, high-dimensional data characteristic of neurological disorders [41]. Several neural network architectures have demonstrated particular utility:
- Convolutional Neural Networks (CNNs) excel at processing structural and functional neuroimaging data (MRI, PET) for tasks such as lesion segmentation, brain atrophy analysis, and disease classification [41].
- Graph Neural Networks (GNNs) are ideally suited for modeling brain connectomes, protein-protein interaction networks, and drug-target interactions, capturing the relational information inherent in biological systems [41].
- Recurrent Neural Networks (RNNs), particularly Long Short-Term Memory (LSTM) networks, analyze temporal sequences such as electrophysiological signals (EEG) for seizure prediction or tracking symptom progression [41].
- Transformers with attention mechanisms increasingly handle complex data integration tasks, weighing the importance of different data elements and capturing long-range dependencies in multimodal data streams [41].
Hybrid Integration Strategies
Hybrid modeling combines mechanistic and data-driven approaches to overcome their individual limitations while leveraging their respective strengths [39] [42]. Four predominant hybrid strategies show particular promise for neurological digital twins:
- Physics-Informed Neural Networks (PINNs): Embed physical laws (e.g., conservation laws, diffusion equations) directly into the loss function of neural networks, constraining solutions to be physically plausible while learning from data [39].
- Residual Modeling: Uses mechanistic models as a baseline and employs data-driven approaches to learn the discrepancy or residual between physics-based predictions and actual clinical observations [42].
- Surrogate Modeling: Trains data-driven models to emulate computationally intensive physics-based simulations, dramatically accelerating parameter exploration and uncertainty quantification while preserving key physical behaviors [39] [40].
- Sequential Hybridization: Uses mechanistic models to generate synthetic training data or feature representations that subsequently inform data-driven models, effectively augmenting limited clinical datasets with physics-based exemplars [41].
Application Notes: Protocol for Alzheimer's Disease Digital Twin Development
Experimental Workflow for Multimodal Data Integration
The development of a comprehensive digital twin for Alzheimer's disease requires the integration of multimodal data across biological scales. The following workflow outlines the key procedural stages for constructing and validating such a system.
Protocol 1: Multimodal Biomarker Acquisition and Processing
Objective: To standardize the collection and processing of multimodal biomarker data for initializing Alzheimer's disease digital twins.
Materials: Table: Key Research Reagents and Materials for Biomarker Analysis
| Reagent/Material | Specifications | Primary Function |
|---|---|---|
| EDTA Plasma Tubes | 10-16 mL draw volume | Stabilization of blood samples for plasma proteomics [43] |
| CSF Collection Kit | Sterile polypropylene tubes | Collection of cerebrospinal fluid via lumbar puncture [44] |
| AMYLOID PET Tracers | [^18F]-florbetapir, [^18F]-flutemetamol | In vivo detection of amyloid-beta plaques [44] |
| TAU PET Tracers | [^18F]-flortaucipir | Visualization of neurofibrillary tau tangles [44] |
| SomaScan Platform | ~7,000 protein assays | High-throughput plasma proteomic profiling [43] |
| Olink Platform | Proximity extension assay | Validation of key protein biomarkers [43] |
Procedural Steps:
Participant Characterization:
- Recruit participants across disease spectrum (cognitively normal, mild cognitive impairment, Alzheimer's dementia)
- Obtain informed consent following institutional review board protocols
- Collect comprehensive clinical data including medical history, cognitive scores (MMSE, MoCA), and APOE genotyping
Biofluid Collection and Processing:
- Perform lumbar puncture for CSF collection following standardized protocols [44]
- Collect blood samples in EDTA tubes, process within 2 hours to isolate plasma
- Aliquot and store biofluids at -80°C until batch analysis
- Analyze CSF and plasma for core Alzheimer's biomarkers (Aβ42/Aβ40 ratio, p-tau181, p-tau217, total-tau) using validated immunoassays or mass spectrometry [44]
Neuroimaging Acquisition:
- Acquire high-resolution 3T MRI (T1-weighted, FLAIR, resting-state fMRI)
- Perform amyloid PET imaging using FDA-approved tracers ([^18F]-florbetapir)
- Conduct tau PET imaging where available ([^18F]-flortaucipir)
- Process images through standardized pipelines for segmentation, normalization, and feature extraction
Proteomic Profiling:
- Subject plasma samples to large-scale proteomic analysis using SomaScan or Olink platforms
- Generate normalized protein expression values through standardized preprocessing pipelines
- Perform quality control to exclude samples with technical artifacts or hemolysis
Protocol 2: Hybrid Model Implementation for Disease Progression Forecasting
Objective: To implement a hybrid physics-AI framework for simulating Alzheimer's disease progression in patient-specific digital twins.
Materials:
- High-performance computing infrastructure (GPU clusters recommended)
- The Virtual Brain platform for brain network modeling [37]
- Python-based deep learning frameworks (PyTorch, TensorFlow)
- Longitudinal multimodal dataset from Alzheimer's Disease Neuroimaging Initiative (ADNI) or similar cohort
Procedural Steps:
Mechanistic Model Configuration:
- Implement patient-specific brain network models using The Virtual Brain framework
- Incorporate structural connectivity matrices derived from diffusion tensor imaging
- Parameterize neural mass models to represent key neurotransmitter systems (cholinergic, glutamatergic) affected in Alzheimer's
- Configure the Fisher-Kolmogorov equation to simulate tau protein propagation along structural connectome pathways [11]
Data-Driven Component Development:
- Train Graph Neural Networks on population-level data to learn mapping between baseline biomarkers and future disease progression
- Implement Convolutional Neural Networks for automated extraction of progression-relevant features from longitudinal MRI scans
- Develop transformer-based models to integrate temporal patterns from clinical assessments, cognitive scores, and biomarker measurements
Hybrid Model Integration:
- Employ a residual learning approach where mechanistic models provide baseline predictions and AI components learn the discrepancy from observed clinical trajectories [42]
- Implement physics-informed neural networks that embed biological constraints (e.g., blood-brain barrier transport equations) into deep learning architectures
- Create surrogate models that emulate computationally intensive mechanistic simulations for rapid scenario testing
Model Validation and Refinement:
- Validate digital twin predictions against held-out longitudinal data from clinical cohorts
- Assess model accuracy for predicting clinical conversion (e.g., from MCI to dementia) over 3-5 year horizons
- Quantify concordance between simulated biomarker changes and actual patient measurements
- Refine model parameters through iterative comparison with validation datasets
Performance Benchmarks and Clinical Applications
Quantitative Performance of Neurological Digital Twin Components
Table: Performance Metrics of Digital Twin Components in Neurological Applications
| Application Domain | Model Type | Key Performance Metrics | Clinical Utility |
|---|---|---|---|
| Parkinson's Disease Prediction | AI-Driven (Remote Monitoring) | 97.95% prediction accuracy for early identification [11] | Enables earlier intervention through remote symptom monitoring |
| Brain Tumor Radiotherapy | Hybrid (Personalized Planning) | 16.7% radiation dose reduction while maintaining equivalent outcomes [11] | Minimizes cognitive side effects while maintaining tumor control |
| Seizure Focus Localization | Deep Learning (DeepSIF) | 96% spatial specificity, 3.80 ± 5.74 mm spatial discreteness [41] | Improves surgical targeting for drug-resistant epilepsy |
| Cardiac Arrhythmia Treatment | Digital Twin (Virtual Drug Testing) | 13.2% reduction in recurrence rates (40.9% vs. 54.1%) [11] | Guides optimal antiarrhythmic drug selection through virtual testing |
| Multiple Sclerosis Progression | Physics-Based Modeling | Detects tissue loss 5-6 years before clinical symptom onset [11] | Enables earlier therapeutic intervention in preclinical stage |
Implementation Framework for Clinical Translation
The pathway from research prototypes to clinically deployed digital twins requires addressing multiple implementation challenges:
Data Integration and Standardization:
- Establish standardized data pipelines for harmonizing multimodal inputs across imaging, omics, and clinical assessments
- Implement FHIR-based interfaces for electronic health record integration
- Develop data quality control frameworks to ensure input data fidelity
Computational Scalability:
- Deploy cloud-native architectures to handle computational demands of population-scale digital twin simulations
- Implement model compression techniques for real-time inference at point of care
- Develop federated learning approaches to train models across institutions without sharing sensitive patient data
Clinical Validation and Regulatory Compliance:
- Design prospective clinical trials to validate digital twin predictions against patient outcomes
- Establish protocols for model explainability to build clinical trust and facilitate regulatory approval
- Implement continuous learning frameworks that adapt to new evidence while maintaining performance stability
The strategic integration of mechanistic and AI-driven approaches represents the most promising path toward clinically actionable digital twins for neurological diseases. Physics-based models provide the biological plausibility and theoretical foundation, while data-driven methods extract complex patterns from high-dimensional patient data that may elude first-principles modeling [39] [40]. The hybrid frameworks outlined in these application notes enable researchers to leverage the complementary strengths of both paradigms, creating digital twins that are both biologically grounded and adaptively personalized. As validation studies continue to demonstrate clinical utility—from personalized radiotherapy planning to predicting neurodegenerative disease progression—these integrated approaches are poised to transform the precision and predictive power of neurological disease management [11]. The ongoing challenge lies not in choosing between physics-based or data-driven approaches, but in developing the sophisticated integration frameworks that harness the full potential of both methodologies for advancing patient care.
Application Notes: Current State and Quantitative Findings
Disease progression modeling (DPM) and digital twin technology are transforming research and drug development for Alzheimer's disease (AD) and Parkinson's disease (PD). These computational approaches mathematically describe disease trajectories, enabling personalized prediction, trial optimization, and individualized therapeutic strategy development.
Alzheimer's Disease Applications
Table 1: Quantitative Outcomes of Digital Twin Applications in Alzheimer's Disease Trials
| Application Domain | Key Metric | Reported Outcome | Data Source |
|---|---|---|---|
| Clinical Trial Efficiency | Sample Size Reduction | 9% to 15% total reduction; 17% to 26% control arm reduction | AWARE Phase 2 Trial Analysis [12] |
| Prognostic Accuracy | Partial Correlation (DT vs. Actual Score) | 0.30 to 0.39 at Week 96 | AWARE Trial Validation [12] |
| Variance Reduction | Total Residual Variance | ~9% to 15% reduction with DT covariate adjustment | PROCOVA-MRM Analysis [12] |
| Model Training | Training Cohort Size | 6,736 unique subjects | Harmonized CODR-AD & ADNI Data [12] |
| Diagnostic Uncertainty | Probabilistic Staging | Validated on 582 amyloid-positive individuals | Neuroimaging Study [45] |
Probabilistic DPM in Alzheimer's disease quantifies diagnostic uncertainty for individual disease severity assessment. These models explicitly describe the transition of biomarkers from normal to pathological stages, showing particular utility in staging and predicting outcomes in pre-dementia stages [45]. The incorporation of AI-generated digital twins as prognostic covariates in statistical models (e.g., PROCOVA-Mixed-Effects Model for Repeated Measures) follows qualified regulatory pathways from both the FDA and EMA [12].
Parkinson's Disease Applications
Table 2: Parkinson's Disease Progression Modeling Approaches and Biomarker Findings
| Model Type | Key Biomarker | Pattern Observed | Clinical Correlation |
|---|---|---|---|
| Linear Model | DAT Binding (SPECT/PET) | Near-linear reduction in early stages | Approximates early motor symptom progression [46] |
| Exponential Model | FDOPA Uptake | Early rapid loss, followed by plateau | Corresponds to rapid putamen decline in 1-4 years post-diagnosis [46] |
| Sigmoidal Model | Alpha-synuclein (Hypothetical) | Slow initiation, acceleration, plateau | Aligns with prion-like spread theory; not yet validated [46] |
| Amyloid Co-pathology | CSF Aβ42 | 30.6% positivity in PD ≥73y vs 10.0% in younger PD | Associated with greater risk of future cognitive decline [47] |
PD progression models face the challenge of misalignment between biomarker trajectories and clinical symptomatology. Neuroimaging biomarkers like dopamine transporter (DAT) binding often change before clinical symptoms manifest, and compensatory mechanisms such as motor reserve can mask underlying degeneration [46]. This disconnect necessitates models that can account for both pathological progression and its clinical expression.
Digital Twin Framework for Neurological Disorders
Digital twins represent a transformative advancement over traditional simulations through their adaptive, integrative nature. A DT is defined as a dynamic, virtual replica of a patient's physiological system that continuously updates with real-time data [5]. The core value proposition in neurodegenerative diseases includes:
- Personalized Predictive Modeling: Forecast individual disease trajectories based on patient-specific data [5]
- Clinical Trial Optimization: Generate synthetic control arms and reduce placebo group sizes [12] [48]
- Treatment Simulation: Test interventions in silico before real-world application [5]
- Continuous Learning: Adapt and improve predictions as new data becomes available [5]
Experimental Protocols
Protocol 1: Developing an AI-Generated Digital Twin for AD Clinical Trials
Objective: Create and validate AI-generated digital twins to improve efficiency in Alzheimer's disease clinical trials by reducing sample size requirements while maintaining statistical power.
Workflow Overview:
Materials and Reagents:
Table 3: Research Reagent Solutions for Digital Twin Development
| Item | Specification | Function | Example Source |
|---|---|---|---|
| Historical AD Data | Control arms from 29 clinical trials; >7,000 participants | Model training foundation | C-Path Online Data Repository for Alzheimer's Disease (CODR-AD) [12] |
| Observational Cohort Data | 1,728 participants across AD spectrum | Complement clinical trial data | Alzheimer's Disease Neuroimaging Initiative (ADNI) [12] |
| CRBM Model | Conditional Restricted Boltzmann Machine | Generate digital twins from baseline data | Unsupervised machine learning framework [12] |
| Clinical Endpoints | CDR-SB, ADAS-Cog14, MMSE, FAQ | Validation against standard outcomes | AWARE Trial measures [12] |
| PROCOVA-MRM Method | Prognostic covariate adjustment | Statistical analysis with DT covariates | EMA-qualified methodology [12] |
Procedure:
Data Harmonization:
- Integrate data from CODR-AD and ADNI databases
- Harmonize 66 variables including demographics, genetics, clinical severity scores, component cognitive measures, and laboratory results
- Create unified dataset of 6,736 unique subjects spanning mild cognitive impairment (MCI) to AD dementia [12]
Model Training:
- Train Conditional Restricted Boltzmann Machine (CRBM) on harmonized historical dataset
- Configure model to accept baseline patient characteristics and generate prognostic forecasts
- Validate model on independent clinical trial datasets (correlation range: 0.30-0.46 between predictions and actual outcomes) [12]
Digital Twin Generation:
- Input baseline data from new trial participants (e.g., AWARE trial: 453 patients with MCI or mild AD)
- Generate individualized predictions of each participant's clinical outcomes if they had received placebo
- Output trajectories for key cognitive and functional assessments over trial duration (e.g., 96 weeks) [12]
Clinical Trial Integration:
- Incorporate digital twins as prognostic covariates in statistical analysis models (PROCOVA-MMRM)
- Maintain randomization and blinding while reducing variance
- Calculate sample size reductions achievable while maintaining statistical power [12]
Validation:
- Calculate partial correlation coefficients between digital twin predictions and actual change scores from baseline
- Measure reduction in total residual variance after digital twin adjustment
- Compute potential sample size reductions for future trials [12]
Protocol 2: Modeling Parkinson's Disease Progression Using Neuroimaging Biomarkers
Objective: Characterize the trajectory of Parkinson's disease progression using longitudinal neuroimaging biomarkers to inform clinical trial design and patient stratification.
Workflow Overview:
Materials and Reagents:
Table 4: Essential Materials for PD Neuroimaging Progression Modeling
| Item | Specification | Function | Application Context |
|---|---|---|---|
| DAT SPECT | Dopamine Transporter Imaging | Quantify presynaptic dopaminergic integrity | Linear decline modeling in early PD [46] |
| FDOPA PET | [18F]fluoro-L-dopa PET | Measure aromatic amino acid decarboxylase activity | Exponential progression pattern detection [46] |
| CSF Biomarkers | Aβ42, tau, alpha-synuclein | Assess co-pathologies and disease mechanisms | Detecting amyloid co-pathology in PD without dementia [47] |
| Clinical Rating Scales | MDS-UPDRS Part III | Quantify motor symptom severity | Correlating biomarker changes with clinical progression [46] |
| Computational Models | Linear, Exponential, Sigmoidal functions | Mathematical modeling of disease trajectories | Testing hypotheses about progression patterns [46] |
Procedure:
Cohort Selection and Stratification:
- Recruit PD patients across disease stages (de novo to advanced)
- Stratify by age at diagnosis, symptom laterality, and clinical subtypes
- Include PD without dementia cohorts for amyloid co-pathology studies (e.g., n=89) [47]
Multi-modal Data Acquisition:
- Conduct baseline neuroimaging (DAT SPECT, FDOPA PET)
- Collect CSF samples for Aβ42, tau, and alpha-synuclein analysis
- Perform comprehensive clinical assessments (MDS-UPDRS, cognitive batteries)
- Establish longitudinal follow-up protocol (e.g., annual assessments) [46]
Biomarker Trajectory Modeling:
- Plot longitudinal biomarker data against time since diagnosis
- Fit multiple mathematical models to biomarker data:
- Linear model: Constant rate of decline
- Exponential model: Early rapid decline followed by plateau
- Sigmoidal model: Slow initiation, acceleration, then plateau
- Compare model fit using appropriate statistical measures (AIC, BIC) [46]
Model Selection and Validation:
- Assess which model best fits the empirical data for each biomarker
- Validate models using hold-out samples or cross-validation
- Account for floor and ceiling effects in biomarker measurements [46]
Clinical Correlation and Application:
- Correlate biomarker trajectories with clinical progression rates
- Identify tipping points or "functional cliffs" where clinical decline accelerates
- Apply models to optimize clinical trial design (enrichment, duration, endpoint selection) [46]
Implementation Framework
The Clinical Trials Transformation Initiative (CTTI) provides key recommendations for implementing disease progression modeling in medical product development:
- Begin Early: Introduce DPM early in the medical product development lifecycle to build confidence for later stages [49] [50]
- Assess Data Resources: Ensure necessary data sources are available, relevant, and reliable for model development [49]
- Validate Continuously: Continually assess model performance and ensure qualification for the intended application [49]
- Leverage Technology: Utilize new computational methods, including AI and digital twin technology, to advance model capabilities [49] [50]
These protocols provide a foundation for implementing disease progression modeling and digital twin frameworks in neurodegenerative disease research, offering researchers standardized approaches to advance personalized medicine and clinical trial efficiency.
Clinical trials in neurological diseases, particularly Alzheimer's disease (AD), face significant challenges including high screen failure rates, substantial costs, and extensive durations [12] [51]. A major driver of these inefficiencies is the high variability in clinical outcomes among participants at similar disease stages, necessitating large sample sizes to achieve statistical power [12]. Prognostic Covariate Adjustment (PROCOVA) represents a transformative methodology that addresses these challenges by integrating artificial intelligence (AI)-generated digital twins into clinical trial design and analysis [12] [52]. This approach leverages machine learning models trained on rich historical datasets to create digital twins—personalized predictions of each participant's expected disease progression under the control condition using only their baseline data [12] [53]. By incorporating these prognostic scores as covariates in statistical analyses, PROCOVA reduces variance in treatment effect estimation, enabling substantial sample size reductions while maintaining statistical power [12] [52] [53]. The methodology has received regulatory qualification from both the European Medicines Agency (EMA) and acceptance from the U.S. Food and Drug Administration (FDA), establishing it as a validated approach for enhancing trial efficiency in neurological drug development programs [12] [52].
Quantitative Efficacy Assessment
Documented Efficiency Gains in Neurological Trials
Implementation of PROCOVA with digital twins has demonstrated significant improvements in clinical trial efficiency across multiple neurological indications. The table below summarizes key quantitative findings from recent studies and trial reanalyses.
Table 1: Documented Efficiency Gains from PROCOVA Implementation in Neurological Trials
| Trial/Study | Therapeutic Area | Variance Reduction | Sample Size Reduction | Control Arm Reduction | Key Endpoints |
|---|---|---|---|---|---|
| AWARE Trial [12] | Alzheimer's Disease | 9-15% | 9-15% (total) | 17-26% | CDR-SB, ADAS-Cog 14, MMSE, FAQ |
| PROCOVA-MMRM AD Analysis [53] | Alzheimer's Disease | Significant improvement in precision | Substantial reduction feasible | Not specified | Longitudinal cognitive and functional measures |
| PROCOVA-MMRM ALS Analysis [53] | Amyotrophic Lateral Sclerosis | Significant improvement in precision | Substantial reduction feasible | Not specified | ALSFRS-R progression |
| Digital Twin Framework [52] | Alzheimer's Disease | Reduced variance across all outcomes | 280 patients in Phase 3 scenario | Not specified | Multiple clinical endpoints |
Correlation and Validation Metrics
The predictive accuracy of digital twins generated for PROCOVA has been rigorously validated across multiple trials. In the AWARE trial analysis, positive partial correlation coefficients between digital twins and actual change scores ranged from 0.30 to 0.39 at Week 96 for key cognitive assessments [12]. Validation across three independent trials demonstrated consistent correlations ranging from 0.30 to 0.46, confirming the robustness of the prognostic scores [12]. These correlations directly translate to the variance reductions and sample size efficiencies documented in Table 1.
Experimental Protocols
Digital Twin Generation and PROCOVA Workflow
Table 2: Research Reagent Solutions for PROCOVA Implementation
| Resource Category | Specific Resource | Function in PROCOVA Workflow |
|---|---|---|
| Historical Data | CODR-AD Database [12] | Provides harmonized control arm data from 29 clinical trials (>7,000 participants) for model training |
| Observational Data | ADNI Database [12] | Supplies longitudinal data from observational studies (1,728 participants) across AD spectrum |
| AI Model Architecture | Conditional Restricted Boltzmann Machine (CRBM) [12] | Generates digital twin predictions using probabilistic neural networks |
| Advanced AI Architecture | Neural Boltzmann Machine (NBM) [53] | Enables flexible prognostic scoring at arbitrary timepoints for longitudinal analyses |
| Statistical Methodology | PROCOVA-MMRM [53] | Extends PROCOVA for longitudinal continuous endpoints using time-matched prognostic scores |
| Validation Framework | Monte Carlo Simulation [51] | Provides statistical validation through 10,000 iterations for robustness assessment |
Protocol 1: Digital Twin Generation and Validation
Data Harmonization: Integrate and harmonize historical clinical trial data and observational study data. The AWARE trial implementation utilized a combined dataset of 6,736 unique subjects from CODR-AD and ADNI databases [12].
Model Training: Train conditional restricted Boltzmann machine (CRBM) or neural Boltzmann machine (NBM) models on the harmonized historical dataset. CRBMs utilize probabilistic neural networks to capture complex, non-linear relationships in longitudinal disease progression data [12].
Baseline Input Processing: For each trial participant, input comprehensive baseline variables into the trained model. These typically include demographics, genetic markers (e.g., APOE ε4 status), clinical severity scores (e.g., MMSE, CDR-SB), cognitive measures, and functional assessments [12].
Digital Twin Generation: Generate individualized predictions of each participant's expected outcome trajectories under control conditions across all planned trial timepoints.
Model Validation: Validate prognostic accuracy through correlation analysis between predicted and actual outcomes in historical datasets or control arms. Target partial correlation coefficients of ≥0.30 with actual change scores [12].
PROCOVA-MMRM Implementation Protocol
Protocol 2: Statistical Analysis with PROCOVA-MMRM
Prognostic Score Incorporation: Include time-matched prognostic scores from digital twins as covariates in Mixed Models for Repeated Measures (MMRM) analysis [53].
Model Specification: Implement the PROCOVA-MMRM model with the following structure:
- Fixed effects for treatment group, time, treatment-by-time interaction
- Prognostic score as a continuous covariate
- Appropriate covariance structure for within-subject measurements
Treatment Effect Estimation: Calculate the treatment effect estimate at the final timepoint, which benefits from reduced variance due to the prognostic covariate adjustment.
Inference Testing: Conduct hypothesis testing using the adjusted model, which demonstrates enhanced statistical power compared to unadjusted MMRM.
Sensitivity Analysis: Perform robustness checks to confirm the stability of results under different model specifications and missing data assumptions.
Workflow Visualization
Digital Twin Generation and Application
PROCOVA-MMRM Analytical Framework
Application Note 1: AI-Generated Digital Twins for Glioblastoma (GBM) Therapeutic Planning
Background and Rationale
Glioblastoma (GBM) is the most aggressive glial tumor of the central nervous system, with a median survival of only 15 months despite standard treatment [54]. The inherent heterogeneity of GBM necessitates patient-tailored treatment approaches to significantly prolong survival. Digital twin (DT) technology offers a transformative approach by creating dynamic, virtual replicas of individual patients' tumors and physiological systems. These computational models simulate disease progression and predict therapeutic responses, enabling personalized intervention strategies before clinical implementation [48]. AI-generated digital twins leverage baseline clinical data to create individualized predictions of clinical outcomes, potentially reducing required sample sizes in clinical trials by 9-15% while maintaining statistical power [12].
Quantitative Data on GBM Surgical Strategies and Outcomes
Table 1: Neurosurgical Strategies for Glioblastoma Resection and Associated Outcomes
| Neurosurgical Strategy | Extent of Resection | Impact on Overall Survival | Clinical Applications |
|---|---|---|---|
| Supramaximal Resection (SMR) | Complete resection of contrast-enhancing tumor + partial resection of T2/FLAIR-hyperintense zone | Improved OS and PFS (Class III evidence) [54] | Non-eloquent area tumors |
| Gross Total Resection (GTR) | Complete resection of contrast-enhancing tumor (100%) | Best outcomes with 100% resection; significant differences even in 90-100% range [54] | Primary strategy for resectable tumors |
| Near Total Resection (NTR) | ≥95% of contrast-enhancing tumor | Better outcomes with ≥95% resection or <1 cm³ residual tumor [54] | Tumors near eloquent areas |
| Subtotal Resection (STR) | <95% of contrast-enhancing tumor | Clinical benefit threshold: ~80% resection or <5 cm³ residual tumor [54] | Large GBMs infiltrating crucial brain centers |
| Biopsy | Diagnostic procedure without resection | No therapeutic benefit; for diagnosis guidance [54] | Poor general health, inoperable GBM |
Table 2: Technical Advancements in GBM Surgical Planning
| Technology | Application | Impact on Surgical Outcomes |
|---|---|---|
| Intraoperative Neuronavigation | Surgical guidance using pre-operative imaging | Improved extent of resection and OS [54] |
| Fluorescence-Guided Surgery | 5-aminolevulinic acid (5-ALA) for tumor visualization | Improved extent of resection and PFS in RCTs [54] |
| Intraoperative MR Imaging | Real-time visualization during resection | Significantly enhanced extent of resection and OS [54] |
| Intraoperative Mass Spectrometry | DESI mass spectrometry for tumor cell detection | Real-time feedback on tumor margins [54] |
Experimental Protocol: Developing GBM Digital Twins for Treatment Simulation
Protocol Title: Development and Validation of GBM Digital Twins for Personalized Therapeutic Planning
Objective: To create patient-specific digital twins of glioblastoma that accurately predict tumor progression and response to various treatment modalities.
Materials and Reagents:
- Multi-parametric MRI data (T1, T2, FLAIR, contrast-enhanced, functional MRI, magnetic resonance spectroscopy)
- Histopathological samples from biopsy or resection
- Genomic and molecular profiling data (including DNA methylation, mutation status)
- Radiomics feature extraction software
- AI modeling platform (Python-based with TensorFlow/PyTorch)
- High-performance computing infrastructure
Methodology:
Step 1: Comprehensive Data Integration
- Collect multi-modal patient data including:
- Structural and functional imaging (MRI, PET)
- Histopathological characterization
- Genomic sequencing (MGMT promoter methylation, IDH1/2 mutation, 1p/19q co-deletion)
- Clinical parameters (age, Karnofsky Performance Status, neurological symptoms)
- Perform data harmonization and feature extraction
- Create standardized data repository with quality control measures
Step 2: AI Model Training and Digital Twin Generation
- Implement conditional restricted Boltzmann machine (CRBM) or similar deep learning architecture
- Train model on historical GBM datasets (minimum 1000+ patient records recommended)
- Validate model prediction accuracy against known clinical outcomes
- Generate patient-specific digital twin with individualized growth parameters
Step 3: Therapeutic Intervention Simulation
- Simulate standard therapies (temozolomide, radiotherapy) on digital twin
- Model combination therapies and novel agents based on molecular targets
- Predict response patterns and potential resistance mechanisms
- Optimize dosing schedules and treatment sequences
Step 4: Validation and Clinical Translation
- Compare predicted outcomes with actual patient responses
- Refine model parameters based on validation results
- Implement adaptive learning for continuous model improvement
- Integrate with clinical decision support systems
Quality Control:
- Regular calibration against phantom datasets
- Cross-validation with independent patient cohorts
- Audit trails for model predictions and updates
Application Note 2: Digital Autonomic Twins for Postural Tachycardia Syndrome (POTS)
Background and Rationale
Autonomic disorders, particularly Postural Tachycardia Syndrome (POTS), affect approximately 3 million Americans and present significant diagnostic and therapeutic challenges due to their complex pathophysiology and limited access to specialized care [55]. POTS is characterized by orthostatic intolerance associated with symptomatic cerebral hypoperfusion and orthostatic tachycardia [5]. Digital autonomic twins offer a transformative approach by creating dynamic, virtual replicas of a patient's autonomic system, enabling personalized understanding, prediction, and management of these conditions [55]. This technology integrates mechanistic and AI-based modeling with continuous physiological, clinical, genetic, and patient-reported data to enhance individualized diagnosis, disease monitoring, and treatment optimization.
Quantitative Data on Autonomic Digital Twin Components
Table 3: Digital Twin Framework Components for Autonomic Disorders
| System Component | Data Sources | Function in Digital Twin |
|---|---|---|
| Monitoring Subsystem | Wearable devices (heart rate, BP, ET-CO₂, EEG, CBF) [55] | Continuous real-time data acquisition for model updating |
| Modeling Subsystem | Electronic health records, genetic profiles, patient-reported outcomes [55] | Mechanistic and AI models of autonomic function |
| Simulation Subsystem | Environmental factors, medication history, lifestyle data [55] | Running simulations of disease and treatment scenarios |
| Interaction Subsystem | Clinician inputs, patient feedback, telehealth platforms [55] | Facilitating communication between patient, digital twin and clinician |
Table 4: Therapeutic Applications of Autonomic Digital Twins
| Application Domain | Digital Twin Function | Expected Clinical Impact |
|---|---|---|
| Medication Response | Simulate patient-specific responses to drugs like pro-amatine or pyridostigmine [55] | Reduced trial-and-error, minimized side effects |
| Lifestyle Interventions | Monitor vital signs in real-time during exercise programs [55] | Personalized activity regimens based on tolerance |
| Symptom Prevention | Detect hyperventilation as precursor to cerebral hypoperfusion [5] | Preemptive interventions to prevent dizziness |
| Dietary Management | Monitor biometrics in relation to salt intake and hydration [55] | Optimized nutritional recommendations for POTS |
Experimental Protocol: Implementing Digital Autonomic Twins for POTS Management
Protocol Title: Development and Implementation of Digital Autonomic Twins for Postural Tachycardia Syndrome
Objective: To create and validate patient-specific digital autonomic twins that predict individual responses to therapies and enable personalized treatment optimization for POTS patients.
Materials and Reagents:
- Multi-parameter wearable sensors (continuous HR, BP, respiratory rate, SpO₂, EEG)
- Mobile health platform for patient-reported outcomes
- Environmental sensors (ambient temperature, humidity, atmospheric pressure)
- AI modeling platforms (Simply, Open Digital Twin Project, PyTwin)
- Blockchain technology for secure health data management
- Cloud computing infrastructure for real-time analytics
Methodology:
Step 1: Comprehensive Autonomic Phenotyping
- Perform baseline autonomic testing (HUTT, Valsalva, deep breathing)
- Collect continuous physiological data via wearable sensors (7-14 day baseline)
- Obtain genetic profiling (particularly relevant polymorphisms)
- Document comprehensive medication history and response patterns
- Assess environmental and lifestyle factors affecting symptoms
Step 2: Digital Twin Model Development
- Implement hybrid modeling approach combining:
- Mechanistic models of cardiovascular physiology
- AI-based predictive algorithms (machine learning, deep learning)
- Train models on historical POTS patient data (minimum 200+ patients recommended)
- Validate model predictions against known clinical outcomes
- Establish individual patient digital twin with personalized parameters
Step 3: Therapeutic Intervention Simulation
- Simulate medication responses based on individual pharmacokinetic/pharmacodynamic profiles
- Model autonomic responses to lifestyle interventions (exercise, dietary changes)
- Predict symptom triggers and preemptive management strategies
- Test combination therapies and timing of interventions
Step 4: Clinical Implementation and Validation
- Integrate digital twin with clinical decision support systems
- Compare predicted vs. actual patient responses in real-world setting
- Implement continuous learning from patient outcomes
- Refine model parameters based on clinical validation
Step 5: Cerebral Hypoperfusion Prevention Protocol
- Implement real-time monitoring of respiratory patterns and ET-CO₂
- Establish alert system for hyperventilation precursors
- Develop staged intervention protocol (vibration signals → auditory cues → clinician notification)
- Validate cerebral blood flow responses via continuous monitoring
Quality Assurance:
- Regular calibration of all monitoring equipment
- Data integrity checks through blockchain verification
- Model performance audits every 3 months
- Patient privacy protection through encryption and access controls
Cerebral Hypoperfusion Prevention Pathway
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 5: Key Research Reagent Solutions for Digital Twin Development
| Reagent/Platform | Type | Function | Application Context |
|---|---|---|---|
| Conditional Restricted Boltzmann Machine (CRBM) | AI Algorithm | Generates digital twins from baseline data using probabilistic neural networks [12] | GBM and neurological disorder prediction models |
| Simply Platform | Python-based Digital Twin Platform | Creates dynamic, data-driven predictive models for physical systems [55] | Autonomic disorder digital twin development |
| Open Digital Twin Project | Open-source Platform | Digital twin development with focus on interoperability and standardization [55] | Multi-scale physiological modeling |
| PyTwin | Python-based Framework | AI-driven digital twin modeling and simulation [55] | Real-time autonomic response prediction |
| 5-Aminolevulinic Acid (5-ALA) | Fluorescent Agent | Fluorescence-guided surgery for tumor margin identification [54] | GBM surgical resection enhancement |
| Desorption Electrospray Ionization (DESI) | Mass Spectrometry Technique | Intraoperative tumor cell detection with real-time feedback [54] | GBM margin assessment during surgery |
| TumorTwin Software | Cancer Digital Twin Platform | Patient-specific cancer modeling and treatment simulation [55] | GBM treatment optimization |
| Multi-parameter Wearable Sensors | Monitoring Devices | Continuous physiological data acquisition (HR, BP, ET-CO₂, CBF) [55] | Autonomic function assessment |
Digital twin technology represents a paradigm shift in personalized treatment planning for complex neurological conditions such as glioblastoma and autonomic disorders. By creating dynamic, virtual replicas of individual patients' physiological systems and disease processes, clinicians and researchers can simulate interventions, predict outcomes, and optimize therapeutic strategies before implementation in actual patients. The protocols and frameworks outlined in this application note provide actionable methodologies for implementing these advanced technologies in both research and clinical settings, potentially significantly improving outcomes for patients with these challenging conditions.
Overcoming Implementation Hurdles: Data, Validation, and Ethical Challenges
The development of digital twin models for predicting neurological disease progression represents a paradigm shift in personalized neurology. These dynamic, virtual replicas of a patient's physiological system rely on the continuous integration of high-volume, multi-modal data to simulate disease trajectories and personalize interventions [5]. The fidelity of a digital twin is directly contingent on the quality, volume, and cohesiveness of the data from its constituent sources. This document outlines the principal challenges and provides detailed application notes and protocols for managing data within a neurological digital twin research framework, supporting the broader thesis that robust data engineering is a critical enabler for predictive accuracy in these models.
Core Data Challenges in Neurological Digital Twins
The construction of a digital twin for a complex, multi-factorial condition like Postural Tachycardia Syndrome (POTS), Alzheimer's Disease (AD), or Parkinson's Disease (PD) involves navigating a landscape of significant data-related hurdles [5] [12].
Data Volume and Veracity
Digital twins are built and maintained by continuously collecting patient data from a variety of sources, leading to vast amounts of information. This includes real-time data from wearables (e.g., heart rate, blood pressure), Electronic Health Records (EHRs), patient-reported outcomes, and environmental factors [5]. While some data, such as genetic information, must be stored indefinitely, the high frequency of real-time physiologic data necessitates strategies for compression or filtering to manage storage and computational load effectively [5].
Data Integration and Silos
Data is often scattered across different systems and sources in isolated, underutilized silos, such as departmental databases and legacy systems [56]. In healthcare, providers often manage separate patient databases across departments, making it difficult to provide seamless care and collaborate on research [56]. This fragmentation creates several challenges:
- Manual processes that slow down data usage and analysis.
- Hidden insights that remain locked away due to disconnected sources.
- Redundant efforts as teams work on overlapping datasets [56].
A primary technical challenge is data format inconsistency. Data exists in structured (e.g., databases), semi-structured (e.g., XML, JSON), and unstructured (e.g., clinical notes, images) forms. Incompatible formats and unique, incompatible schemas require extensive transformation and standardization to enable compatibility and establish meaningful relationships between data elements [56].
Privacy and Regulatory Compliance
Integrating sensitive patient data, especially in real-time, requires stringent data privacy and security protocols [5]. Regulations such as the Health Insurance Portability and Accountability Act (HIPAA) and the General Data Protection Regulation (GDPR) impose strict requirements on how sensitive data is collected, stored, and shared. The complexity of data use is amplified when working with multiple jurisdictions, each with its own compliance standards, creating significant barriers to global collaboration [56].
Protocols for Data Integration and Management
Protocol: A Standardized Data Integration Workflow
This protocol outlines a systematic process for combining data from disparate sources into a research-ready format suitable for digital twin modeling.
Objective: To establish a reproducible Extract, Transform, Load (ETL) workflow that ensures data quality and interoperability. Materials: Source data (EHRs, wearable outputs, patient surveys), data harmonization platform (e.g., Python-based libraries, commercial ETL tools), secure data repository (e.g., data lake or warehouse).
Procedure:
- Need Identification & Source Mapping: Define the specific parameters for the data required (e.g., date ranges, variables). Identify all relevant data sources and the specific data elements to be extracted from each [57].
- Data Extraction: Extract data from the identified sources in their native formats. Automation through scripts or tools is recommended for high-frequency data sources [57].
- Data Transformation and Cleaning (Harmonization): This is the most critical and effort-intensive step.
- Standardization: Normalize nomenclature and units of measurement across all datasets.
- Cleaning: Remove duplicate records and correct inaccurate or erroneous data (e.g., implausible physiological values).
- Structuring: Convert unstructured or semi-structured data into a consistent, analysis-ready format.
- Note: Automate as much of this cleansing process as possible to enable a self-service environment and minimize manual error [57].
- Loading and Validation: Load the transformed and cleaned data into a centralized, secure repository (e.g., a data lake or warehouse). Perform validation checks to ensure data integrity and completeness [57].
- Continuous Updating: Establish a pipeline for periodic or real-time data refreshes from source systems, repeating the ETL process as needed [56].
Protocol: Leveraging Privacy-Enhancing Technologies (PETs)
This protocol describes the use of PETs to enable secure data collaboration and analysis without sharing raw, sensitive patient data, thus addressing key privacy and regulatory hurdles.
Objective: To perform advanced analytics or train predictive models on combined datasets from multiple parties while preserving data privacy. Materials: Sensitive datasets from disparate sources (e.g., different clinical trial sites), software libraries supporting PETs (e.g., for Homomorphic Encryption or Secure Multi-Party Computation).
Procedure:
- Technology Selection: Choose an appropriate PET based on the project's needs [56]:
- Federated Learning: For model training on decentralized datasets. A "traveling algorithm" is sent to each data source, and the model learns locally without data leaving the original site. The improved model is then aggregated.
- Homomorphic Encryption: For performing computations on encrypted data without needing to decrypt it, ensuring data security at rest, in transit, and in use.
- Secure Multi-Party Computation (MPC): Allows multiple parties to perform joint computations on their individual inputs without revealing the underlying data to each other.
- Model Configuration: Configure the analytical or machine learning model to operate within the chosen PET framework.
- Execution and Aggregation: Execute the analysis. In the case of federated learning, aggregate the model updates from each participating site to create a globally improved model.
- Insight Generation: Derive final insights or predictions from the PET-processed results. The raw data remains private and is never exposed to other parties [56].
Quantitative Performance of Data-Driven Models in Neurology
The following tables summarize the performance of machine learning models, which form the computational core of many digital twins, in predicting neurological disease progression. These metrics underscore the potential value of well-integrated data.
Table 1: Performance of EML-based Prediction Models for Neurological Diseases Over Time [58]
| Disease | Area Under the Curve (AUC) at 0 Months Pre-Diagnosis | AUC at 12 Months Pre-Diagnosis | AUC at 24 Months Pre-Diagnosis | AUC at 60 Months Pre-Diagnosis |
|---|---|---|---|---|
| Alzheimer's Disease | 0.794 | 0.742 | 0.709 | 0.645 |
| Amyotrophic Lateral Sclerosis | 0.883 | 0.710 | 0.658 | 0.620 |
| Multiple Sclerosis | 0.922 | 0.877 | 0.849 | 0.781 |
| Parkinson's Disease | 0.809 | 0.738 | 0.700 | 0.651 |
Note: AUC (Area Under the Receiver Operating Characteristic Curve) measures model performance, where 1.0 is a perfect prediction and 0.5 is no better than random chance. Data derived from a retrospective study using Cleveland Clinic EMR data and the eXtreme Gradient Boosting algorithm [58].
Table 2: Clinical Trial Efficiency Gains from AI-Generated Digital Twins in Alzheimer's Disease [12]
| Metric | Improvement with Digital Twin Covariate Adjustment |
|---|---|
| Partial Correlation with Actual Outcomes | 0.30 to 0.39 |
| Reduction in Total Residual Variance | ~9% to 15% |
| Potential Reduction in Total Sample Size | ~9% to 15% |
| Potential Reduction in Control Arm Size | 17% to 26% |
Note: Data based on an analysis of the AWARE Phase 2 clinical trial for Alzheimer's disease, using a conditional restricted Boltzmann machine (CRBM) model trained on historical data [12].
Visualization of Data Workflows
The following diagram illustrates the integrated and adaptive data flow that powers a digital twin for a neurological disorder, from data acquisition to clinical feedback.
The Scientist's Toolkit: Research Reagents & Essential Materials
Table 3: Essential Tools and Technologies for Digital Twin Development
| Item | Category | Function |
|---|---|---|
| eXtreme Gradient Boosting (XGBoost) | Machine Learning Algorithm | Creates powerful predictive models from structured EMR data (e.g., for risk stratification of neurological disease) [58]. |
| Conditional Restricted Boltzmann Machine (CRBM) | Generative AI Model | An unsupervised neural network used to generate AI-based digital twins that predict an individual's placebo progression in clinical trials [12]. |
| Python-based Platforms (e.g., SimPly, Open Digital Twin Project) | Modeling Software | Open-source environments for building and simulating digital twin models of physical (or physiological) systems [5]. |
| Federated Learning | Privacy-Enhancing Technology (PET) | Enables model training on decentralized datasets without moving or sharing raw data, preserving privacy [56]. |
| Homomorphic Encryption | Privacy-Enhancing Technology (PET) | Allows computation on encrypted data, ensuring sensitive information remains secure during analysis [56]. |
| Wearable Biosensors | Data Acquisition | Continuously capture real-time physiological data (e.g., heart rate, blood pressure, activity) from the physical twin [5]. |
The adoption of Artificial Intelligence (AI)-generated digital twins (DTs) represents a paradigm shift in neurological disease research and therapeutic development. These virtual patient models—computational representations that simulate disease progression in response to individual patient baseline characteristics—are demonstrating significant potential to enhance clinical trial efficiency and predictive accuracy [12] [15]. However, as these models grow more complex, ensuring their transparency and interpretability has become a critical requirement for regulatory acceptance, clinical adoption, and ethical implementation [59]. The "black box" problem, where AI systems provide accurate predictions without explainable reasoning, poses particular challenges in medical contexts where understanding the basis for predictions is essential for trust and safety [60].
In neurological research, where DTs are increasingly deployed to forecast disease progression in conditions like Alzheimer's disease (AD) and multiple sclerosis (MS), interpretability transcends technical preference to become a clinical necessity [11] [59]. Researchers, clinicians, and regulatory bodies must understand which factors drive individual progression predictions to validate model behavior, identify potential biases, and build confidence in DT-guided decisions. This Application Note establishes protocols and frameworks for implementing transparent, interpretable AI approaches in neurological DT research, enabling the field to advance beyond black box limitations while maintaining predictive performance.
Interpretable AI Techniques for Digital Twin Development
Comparative Framework: Interpretable vs. Post-Hoc Explanation Methods
Two primary approaches exist for making AI models understandable: intrinsically interpretable models that are transparent by design, and post-hoc explanation methods that apply interpretability techniques to complex models after training [59]. The choice between these approaches involves balancing predictive accuracy, explanatory fidelity, and implementation complexity.
Table 1: Comparison of Interpretable AI Approaches for Neurological Digital Twins
| Approach Type | Example Techniques | Best-Suited Applications | Advantages | Limitations |
|---|---|---|---|---|
| Intrinsically Interpretable Models | Logistic regression, Decision trees, Generalized additive models | Preliminary analysis, Regulatory submissions, High-stakes clinical decisions | Transparent reasoning process, Theoretical guarantees, Regulatory familiarity | Potentially lower complex pattern recognition, Limited capacity for high-dimensional data |
| Post-Hoc Explanation Methods | SHAP (SHapley Additive exPlanations), LIME (Local Interpretable Model-agnostic Explanations), Attention mechanisms | Complex deep learning architectures, Multimodal data integration, Pattern recognition in neuroimaging | High predictive performance, Flexibility in model architecture, Ability to handle diverse data types | Potential explanation inaccuracies, Computational overhead, Complex validation requirements |
| Hybrid Approaches | Explainable boosting machines, Transparent neural networks with attention | Balanced performance and interpretability needs, Clinical decision support systems | Competitive performance with enhanced explainability, Better validation potential | Implementation complexity, Emerging validation frameworks |
As demonstrated in a multiple sclerosis case study, post-hoc methods like SHAP can produce feature importance profiles aligned with those of interpretable models, supporting their use when greater model complexity is required within a DT architecture [59]. This alignment validation is crucial for establishing trust in explanation methods.
Technical Implementation of Explainability Methods
For neurological DT applications, specific technical implementations have demonstrated particular utility:
SHAP (SHapley Additive exPlanations): This game theory-based approach quantifies the contribution of each input feature to individual predictions, making it valuable for understanding which patient characteristics most influence progression forecasts [15] [59]. In practice, SHAP values can reveal whether a DT's prediction of rapid cognitive decline is driven primarily by specific baseline cognitive scores, genetic markers, or imaging characteristics.
Attention Mechanisms: Integrated directly into neural network architectures, attention mechanisms highlight which parts of input data (e.g., specific brain regions in MRI scans) the model "pays attention to" when making predictions [27]. For example, in Alzheimer's progression prediction, attention weights can visualize whether the model focuses on hippocampal atrophy patterns or cortical thinning.
Model-Specific Interpretability Techniques: For traditional statistical models used in prognostic covariate adjustment (PROCOVA), standard significance testing, coefficient examination, and confidence intervals provide inherent interpretability [12]. These methods align well with current regulatory expectations for clinical trial applications.
Performance Metrics: Quantitative Validation of Interpretable Models
Establishing interpretability requires both qualitative assessment and quantitative validation. The following performance metrics demonstrate that interpretable models can maintain competitive predictive accuracy while providing explanatory capabilities.
Table 2: Performance Benchmarks for Interpretable AI in Neurological Applications
| Application Domain | Model Architecture | Interpretability Approach | Key Performance Metrics | Clinical/Research Utility |
|---|---|---|---|---|
| Alzheimer's Disease Progression Prediction [12] | Conditional Restricted Boltzmann Machine (CRBM) | PROCOVA statistical framework | 9-15% reduction in residual variance; 17-26% reduction in control arm sample size | Increased clinical trial efficiency while maintaining statistical power |
| Multiple Sclerosis Disability Progression [59] | Logistic Regression vs. Neural Networks | Intrinsic interpretability vs. SHAP explanations | Comparable AUC scores; Alignment of feature importance profiles | Reliable progression forecasting with validated explanatory insights |
| Neurological Disorder Classification from MRI [27] | STGCN-ViT (Spatial-Temporal Graph Convolutional Network + Vision Transformer) | Attention mechanisms and feature visualization | 93.56-94.52% accuracy; 94.41-95.03% precision | Early detection of Alzheimer's and Parkinson's disease with localized explanatory insights |
| Parkinson's Disease Management [11] | Digital Twin Healthcare System | Transparent feature weighting | 97.95% prediction accuracy for early identification | Remote disease monitoring with explainable deterioration alerts |
The quantitative evidence confirms that interpretable approaches need not sacrifice predictive power. In the case of Alzheimer's clinical trials, the PROCOVA framework with DTs demonstrated both statistical efficiency gains (9-15% sample size reduction) and inherent interpretability through clearly defined covariate relationships [12].
Experimental Protocol: Implementing Interpretable Digital Twins for Alzheimer's Clinical Trials
This section provides a detailed methodological protocol for developing and validating transparent DT models for neurological disease progression prediction, based on established implementations in Alzheimer's research [12].
Phase 1: Data Harmonization and Preprocessing
Objective: Create a unified, analysis-ready dataset from diverse neurological data sources.
Steps:
- Data Collection: Aggregate data from historical clinical trials and observational studies, ensuring appropriate ethical approvals and data use agreements. The Alzheimer's Disease Neuroimaging Initiative (ADNI) and Critical Path for Alzheimer's Disease (CPAD) consortium data provide exemplary starting points [12].
- Variable Harmonization: Map common data elements across sources, including:
- Demographics (age, sex, education)
- Genetic markers (APOE ε4 status)
- Cognitive scores (MMSE, CDR-SB, ADAS-Cog)
- Functional assessments (FAQ)
- Neuroimaging biomarkers
- Quality Control: Implement rigorous outlier detection, missing data handling (multiple imputation recommended), and distribution normalization.
Deliverable: Harmonized dataset with standardized variables, ready for model training.
Phase 2: Model Training with Interpretability Constraints
Objective: Develop a predictive model for disease progression with built-in interpretability features.
Steps:
- Architecture Selection: Choose model architecture based on interpretability requirements:
- High Interpretability Need: Generalized additive models or regularized linear models
- Balance Needs: Gradient boosting machines with SHAP explainability
- Complex Pattern Recognition: Neural networks with attention mechanisms
- Model Training: Implement appropriate training paradigm:
- For CRBM models as used in Alzheimer's applications: Train on historical control data to predict placebo-group progression patterns [12]
- Incorporate regularization techniques to enhance model generalizability
- Implement cross-validation to prevent overfitting
- Interpretability Integration:
- For attention-based models: Record and visualize attention patterns across patient subgroups
- For tree-based models: Calculate feature importance metrics
- For all models: Establish protocol for generating individual prediction explanations
Deliverable: Trained model with associated interpretability infrastructure.
Phase 3: Validation and Explanation Fidelity Assessment
Objective: Rigorously validate both predictive accuracy and explanation quality.
Steps:
- Predictive Performance Validation:
- Assess correlation between predicted and actual outcomes in holdout datasets
- Evaluate calibration (alignment between predicted probabilities and observed frequencies)
- Validate across patient subgroups to identify potential biases
- Explanation Fidelity Assessment:
- Conduct domain expert review of feature importance rankings
- Perform sensitivity analysis to test explanation stability
- Implement "right for the right reasons" validation where possible
- Clinical Validation:
- Compare model explanations with established clinical knowledge
- Assess actionable insights generated from model explanations
Deliverable: Comprehensive validation report covering both predictive performance and explanation quality.
Visualization Framework: Model Interpretability Workflow
The following diagram illustrates the integrated workflow for developing and validating interpretable digital twin models for neurological disease progression prediction.
Successful implementation of interpretable AI for neurological digital twins requires specific computational tools, software libraries, and data resources. The following table details essential components for establishing this research capability.
Table 3: Research Reagent Solutions for Interpretable Digital Twin Development
| Tool Category | Specific Tools/Libraries | Primary Function | Implementation Notes |
|---|---|---|---|
| Explainable AI Libraries | SHAP, LIME, Captum, InterpretML | Model explanation and interpretability | SHAP provides theoretical guarantees; LIME offers local approximations; Choose based on model type |
| Machine Learning Frameworks | PyTorch, TensorFlow, Scikit-learn | Model development and training | Scikit-learn for interpretable models; PyTorch/TensorFlow for neural networks with attention mechanisms |
| Neurological Data Resources | ADNI, CPAD CODR-AD, OASIS | Training data and validation cohorts | Ensure data use agreements; Implement harmonization protocols [12] [27] |
| Visualization Tools | Matplotlib, Seaborn, Plotly, Graphviz | Explanation visualization and reporting | Critical for communicating model behavior to diverse stakeholders |
| Clinical Data Standards | CDISC, OMOP Common Data Model | Data harmonization and interoperability | Essential for multi-site studies and regulatory submissions |
| Validation Frameworks | Algorithmic fairness tools, Sensitivity analysis packages | Model validation and bias detection | Implement before clinical deployment to identify potential limitations |
The movement beyond black box AI in neurological digital twin research represents both an ethical imperative and practical necessity. As demonstrated through the protocols and examples in this Application Note, interpretable AI approaches can deliver both predictive accuracy and explanatory transparency when properly implemented [12] [59]. The rigorous validation frameworks, coupled with advanced explanation techniques like SHAP and attention mechanisms, enable researchers to build trust in DT predictions while maintaining the complex pattern recognition capabilities required for accurate disease progression forecasting.
For the field to advance, standardized interpretability assessment protocols must become integral to DT development and validation workflows. By adopting the methodologies outlined herein, researchers can accelerate the translation of digital twin technologies from research tools to clinically valuable assets that enhance therapeutic development for neurological disorders. The future of neurological digital twins lies not merely in accurate predictions, but in predictions that clinicians and researchers can understand, trust, and act upon to improve patient outcomes.
Computational and Scalability Constraints for Real-Time Clinical Use
The integration of digital twin technology in clinical neurology represents a paradigm shift towards personalized, predictive medicine. A human digital twin (HDT) is defined by the National Academies of Sciences, Engineering, and Medicine (NASEM) as a set of virtual information constructs that mimics the structure, context, and behavior of a patient, is dynamically updated with data from its physical counterpart, possesses predictive capability, and informs clinical decisions [9]. However, the operationalization of HDTs for real-time clinical use faces significant computational and scalability constraints that must be addressed through optimized architectures, efficient algorithms, and specialized hardware infrastructure. This document outlines these challenges and provides detailed protocols for implementing neurologically-focused HDT systems capable of functioning within clinical time constraints.
Performance Benchmarks and Computational Demands
Current Performance Metrics in Neurological Digital Twin Systems
Table 1: Performance benchmarks of neurological AI and digital twin systems
| Model/System | Clinical Task | Accuracy | AUC | Computational Resources | Inference Time |
|---|---|---|---|---|---|
| Neuro AI Ensemble [61] | ED admission prediction | N/A | 0.88 | Gemini 1.5-pro LLM + XGBoost + Logistic Regression | Not specified |
| STGCN-ViT [27] | Early ND detection from MRI | 94.52% | 0.9524 | EfficientNet-B0 + STGCN + Vision Transformer | Not specified |
| Integrated AD Model [62] | CN to AD progression | 85% | N/A | Ensemble Transfer Learning + ViT-GAN + 3D CNN | Not specified |
| Cardiac DT Platform [15] | VT ablation planning | N/A | N/A | AI-guided platform | 60% shorter procedure time |
Analysis of Computational Requirements
The implementation of HDTs for real-time clinical use demands substantial computational resources across multiple dimensions:
Model Complexity: Neurological HDTs typically employ ensemble architectures combining multiple specialized models. For instance, the Neuro AI ensemble framework leverages three distinct model types: large language models (Gemini 1.5-pro), tree-based models (XGBoost), and statistical models (logistic regression) [61]. This diversity enhances predictive performance but significantly increases computational overhead.
Data Volume and Velocity: HDTs require processing high-frequency, multimodal data streams including neuroimaging (MRI, CT, PET), electrophysiological signals, clinical assessments, and omics data. The integrated AD progression model processes longitudinal MRI data with generative components that simulate disease progression over multi-year horizons [62].
Memory Constraints: The STGCN-ViT model for neurological disorder detection exemplifies memory-intensive architectures, combining convolutional networks for spatial feature extraction with graph convolutional networks for temporal dynamics and vision transformers for attention mechanisms [27]. This multi-component approach requires substantial GPU memory for both training and inference.
Implementation Protocols for Real-Time Clinical Deployment
Protocol 1: Ensemble Framework for Emergency Department Decision Support
Table 2: Experimental protocol for ED neurological decision support system
| Protocol Component | Specification | Purpose | Implementation Notes |
|---|---|---|---|
| Data Collection | 1368 consecutive ED patients with neurological consultations [61] | Training and validation | Structured and unstructured EHR data, neurological exams, radiological findings, laboratory results |
| LLM Configuration | Gemini 1.5-pro-002 on Google Cloud Vertex AI [61] | Process unstructured clinical data | Temperature=1, top_p=1, n=1; five runs per query with mean scoring |
| RAG Implementation | all-miniLM-L6-v2 embeddings + Faiss library [61] | Retrieve clinically similar cases | Five most relevant historical cases based on cosine similarity |
| Machine Learning Models | XGBoost (learning rate=0.1, max depth=3, 50 estimators) + Logistic Regression (L2 regularization, C=1.0) [61] | Structured data analysis | Handles missing values natively without imputation |
| Ensemble Framework | Weighted combination (≈0.33 each) of LLM, XGBoost, and Logistic Regression [61] | Optimize predictive performance | Weights optimized on validation split by grid-searching probability simplex |
Protocol 2: Multi-Modal Neurological Disorder Detection Pipeline
Table 3: Experimental protocol for ML-based neurological disorder detection
| Protocol Component | Specification | Purpose | Implementation Notes |
|---|---|---|---|
| Dataset | OASIS and Harvard Medical School datasets [27] | Model training and validation | Includes Alzheimer's disease, Parkinson's disease, and brain tumor cases |
| Spatial Feature Extraction | EfficientNet-B0 [27] | Process high-resolution images | Pre-trained on natural images, adapted for neuroimaging |
| Temporal Modeling | Spatial-Temporal Graph Convolutional Network (STGCN) [27] | Capture disease progression dynamics | Models anatomical changes across brain regions over time |
| Attention Mechanism | Vision Transformer (ViT) [27] | Focus on clinically relevant regions | Self-attention mechanisms identify subtle pathological patterns |
| Performance Validation | Comparison against standard and transformer-based models [27] | Benchmark accuracy and efficiency | Achieved 94.52% accuracy, 95.03% precision, AUC 0.9524 |
Scalability Analysis and Optimization Strategies
Infrastructure Requirements for Clinical Deployment
Table 4: Computational resource requirements for neurological digital twins
| System Component | Hardware Requirements | Software Dependencies | Scalability Considerations |
|---|---|---|---|
| LLM Processing | GPU clusters (e.g., NVIDIA A100/H100) with high VRAM [61] | TensorFlow/PyTorch, Hugging Face Transformers | Batch processing of multiple patients; model quantization for efficiency |
| Medical Imaging Analysis | High-memory GPUs for 3D volumetric data processing [27] [62] | MONAI, ITK, SimpleITK, NiBabel | Distributed inference across multiple GPUs; progressive loading of large scans |
| Ensemble Model Integration | Multi-core CPUs with parallel processing capability [61] | Scikit-learn, XGBoost, MLflow | Asynchronous execution of component models; caching of intermediate results |
| Real-Time Data Integration | High-throughput data pipelines with streaming capability [15] [9] | Apache Kafka, Spark Streaming, FHIR interfaces | Load balancing across multiple instances; priority queuing for critical cases |
Optimization Techniques for Clinical Time Constraints
Model Compression: For real-time inference, implement quantization (FP16/INT8) of neural network weights, particularly for vision transformers and 3D CNNs used in neuroimaging analysis [27] [62]. This can reduce memory footprint by 50-75% with minimal accuracy loss.
Hierarchical Processing: Adopt a multi-tier analysis approach where lightweight models perform initial screening, reserving computationally intensive ensemble methods for complex cases [61]. This optimizes resource allocation in time-sensitive clinical environments.
Federated Learning: To address data scalability while preserving privacy, implement federated learning approaches where model training occurs across institutions without sharing sensitive patient data [63]. This is particularly relevant for neurological disorders where datasets are often limited and distributed.
Edge-Cloud Hybrid Architecture: Deploy lightweight models on edge devices for immediate preliminary analysis, with cloud-based comprehensive ensemble processing for complex decision support [15]. This balances responsiveness with analytical depth.
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential research reagents and computational tools for neurological digital twin development
| Tool/Reagent | Function | Application Context | Implementation Example |
|---|---|---|---|
| Google Vertex AI | Cloud-based ML platform with managed infrastructure [61] | Hosting and deployment of LLM components | Gemini 1.5-pro for unstructured clinical text processing |
| Faiss Library | Efficient similarity search and clustering of dense vectors [61] | Retrieval-augmented generation for clinical cases | Identifying similar historical cases for context-aware predictions |
| EfficientNet-B0 | Convolutional neural network with optimized accuracy/efficiency trade-off [27] | Spatial feature extraction from neuroimaging | Base network for STGCN-ViT hybrid model |
| Vision Transformer (ViT) | Transformer architecture adapted for image recognition [27] | Attention-based analysis of neuroimaging data | Identifying subtle pathological patterns in early disease stages |
| 3D Convolutional Neural Networks | Volumetric processing of medical imaging data [62] | Analysis of longitudinal structural brain changes | Alzheimer's disease progression prediction from MRI sequences |
| XGBoost | Gradient boosting framework with optimized performance [61] | Structured clinical data analysis | Handling missing laboratory values without imputation |
| Grad-CAM | Gradient-weighted Class Activation Mapping [62] | Model interpretability and ROI identification | Visualizing critical brain regions contributing to predictions |
The implementation of digital twin technology for real-time clinical use in neurology requires careful balancing of computational complexity and scalability constraints. The protocols and frameworks presented herein demonstrate that through optimized ensemble architectures, strategic resource allocation, and specialized infrastructure, it is feasible to deploy predictive neurological digital twins within clinical time constraints. Future work should focus on standardization of deployment pipelines, development of specialized neuromorphic computing solutions, and creation of optimized model compression techniques specifically for clinical neurological applications. As these technologies mature, they hold the potential to transform neurological care from reactive to precisely predictive, enabling earlier interventions and personalized treatment strategies for patients with progressive neurological disorders.
Application Note: Enhancing Clinical Trial Design with Digital Twins
Quantitative Evidence of Efficacy in Neurological Research
Digital twins (DTs) demonstrate significant potential to improve the efficiency and predictive power of clinical trials for neurological diseases. The following table summarizes key performance metrics from recent implementations.
Table 1: Performance Metrics of Digital Twins in Neurological Disease Research
| Trial / Application Area | Key Metric | Performance Result | Impact |
|---|---|---|---|
| AD Phase 2 Trial (AWARE) [12] | Partial Correlation (DT vs. Actual Score) | 0.30 to 0.39 at Week 96 | High prognostic accuracy for disease progression |
| AD Phase 2 Trial (AWARE) [12] | Residual Variance Reduction | ~9% to 15% | Increased statistical power for detecting treatment effects |
| AD Phase 2 Trial (AWARE) [12] | Sample Size Reduction (Total) | ~9% to 15% | Maintained power with fewer participants |
| AD Phase 2 Trial (AWARE) [12] | Sample Size Reduction (Control Arm) | 17% to 26% | Reduced placebo group enrollment needs |
| Neurodegenerative Disease Prediction [11] | General Prediction Accuracy | 97% | Enabled earlier identification and intervention |
| Parkinson's Disease Management [11] | Remote Prediction Accuracy | 97.95% | Facilitated monitoring from remote locations |
Experimental Protocol: Integrating Digital Twins as Prognostic Covariates
Protocol Title: Utilizing AI-Generated Digital Twins as Prognostic Covariates in a Randomized Clinical Trial for Alzheimer's Disease.
Objective: To reduce sample size requirements and increase statistical power in a Phase 2 clinical trial by incorporating digital twin predictions as covariate adjustments in the statistical analysis.
Materials:
- Historical Training Data: Harmonized dataset from 6,736 unique subjects, combining control arms from 29 clinical trials (e.g., CODR-AD) and observational studies (e.g., ADNI) [12].
- Baseline Trial Data: Data from the ongoing trial (e.g., the AWARE trial with 453 MCI/mild AD subjects) including demographics, genetics, clinical severity scores, and cognitive measures [12].
- AI Model: A pre-trained and validated Conditional Restricted Boltzmann Machine (CRBM) [12].
- Computing Infrastructure: High-performance computing environment capable of running deep generative models.
Procedure:
- Model Input Preparation: For each participant in the new trial, compile baseline data matching the input variables used during the CRBM's training. This includes age, education, baseline cognitive scores (e.g., MMSE, CDR-SB, ADAS-Cog), genetic markers (e.g., APOE ε4), and amyloid status [12].
- Digital Twin Generation: Input the compiled baseline data into the validated CRBM. The model will output a DT for each participant, which is an individualized, longitudinal prediction of their clinical outcome trajectories (e.g., CDR-SB change from baseline) under the placebo condition [12] [48].
- Integration into Statistical Analysis: Integrate the DT predictions as a covariate in the primary statistical model (e.g., a PROCOVA-Mixed-Effects Model for Repeated Measures - PROCOVA-MMRM). The model will compare the observed outcomes in the active treatment group against the DT-predicted placebo trajectory, adjusting for the prognostic information contained in the DT [12].
- Outcome Assessment: Evaluate the treatment effect by testing the null hypothesis that the adjusted mean difference between the active treatment group and their digital twins' predictions is zero. Assess the reduction in residual variance and the consequent effective increase in statistical power.
Visualization of Workflow:
Application Note: Mitigating Algorithmic Bias in Digital Twin Development
Documented Evidence of AI Bias in Healthcare
The performance and fairness of digital twins are contingent on the data and algorithms used to create them. The following table catalogs real-world instances of algorithmic bias with direct relevance to neurological DT development.
Table 2: Documented Cases of Algorithmic Bias in Healthcare AI
| Study / Source | AI Application | Bias Identified | Disadvantaged Group(s) |
|---|---|---|---|
| Obermeyer et al. (Science) [64] | Resource Allocation Algorithm | Used healthcare cost as a proxy for need, underestimating illness severity. | Black Patients |
| London School of Economics (LSE) [64] | LLM for Case Note Summarization | Systematically downplays health needs; uses less severe language. | Women |
| Massachusetts Institute of Technology (MIT) [64] | Medical Imaging Analysis (X-rays) | Uses "demographic shortcuts," leading to diagnostic inaccuracies. | Women, Black Patients |
| University of Florida [64] | Machine Learning for Diagnostics | Varied accuracy in diagnosing bacterial vaginosis. | Asian & Hispanic Women |
Experimental Protocol: Fairness Auditing for a Digital Twin Model
Protocol Title: Pre-Deployment Fairness Audit of a Digital Twin Generation Model for Predicting Multiple Sclerosis Progression.
Objective: To identify and quantify potential performance disparities of a digital twin model across predefined demographic subgroups before its use in a research setting.
Materials:
- Test Dataset: A held-out dataset with known demographic attributes (e.g., self-reported race, gender, age), not used in model training. This dataset should be enriched for demographic diversity to ensure sufficient power for subgroup analysis [65] [66].
- AI Model: The trained model intended for generating digital twins (e.g., a CRBM or foundation model) [12] [7].
- Performance Metrics: Standard metrics relevant to the prediction task (e.g., Mean Absolute Error, R-squared for continuous outcomes; AUC for classification).
- Fairness Metrics: Selected fairness criteria, such as:
- Statistical Analysis Software: Capable of conducting subgroup analysis and statistical tests for difference (e.g., t-tests, chi-square).
Procedure:
- Subgroup Definition: Define the demographic subgroups for auditing based on the test dataset's attributes (e.g., Group 1: White, Group 2: Black, Group 3: Female, Group 4: Male, etc.).
- Model Prediction: Run the digital twin generation model on the entire test dataset to obtain predictions for each subject.
- Performance Disaggregation: Calculate the chosen performance metrics (e.g., MAE between predicted and actual outcomes) separately for each demographic subgroup.
- Bias Detection Analysis:
- Quantitative Comparison: Compare the disaggregated performance metrics across subgroups. A significant difference (e.g., p < 0.05) in MAE between groups indicates a performance disparity.
- Fairness Assessment: Evaluate whether the model meets the predefined fairness criteria. For instance, check if the false positive rate for disease progression prediction is significantly higher in one racial group versus another.
- Reporting: Document all findings in a fairness audit report. If significant bias is detected, mitigation strategies (e.g., data augmentation, reweighting, algorithmic debiasing) must be implemented before model deployment [65] [66].
Visualization of Bias Mitigation Workflow:
Application Note: Navigating the Data Privacy and Regulatory Environment
Evolving Regulatory Frameworks for Health Data
Digital twin research involves processing sensitive health data, necessitating strict adherence to a complex regulatory landscape. The following table summarizes key regulations.
Table 3: Key Data Privacy Regulations Impacting Digital Twin Research
| Regulation / Law | Jurisdiction / Authority | Key Provisions & Relevance to Digital Twin Research | Status (as of 2025) |
|---|---|---|---|
| Health Insurance Portability and Accountability Act (HIPAA) [67] [68] [69] | U.S. (HHS) | Safeguards electronically Protected Health Information (ePHI). Mandates access controls, encryption, and breach notification. | Enforced; Security Rule update proposed in 2025 [67] [68]. |
| Health Breach Notification Rule (HBNR) [68] | U.S. (FTC) | Requires vendors of health apps and wearable tech (not covered by HIPAA) to notify users of data breaches. | Enforced, amended July 2024 [68]. |
| General Data Protection Regulation (GDPR) [66] [69] | European Union | Requires explicit consent for data processing, emphasizes data minimization, and grants individuals rights over their data. A global benchmark. | Enforced. |
| My Health My Data Act (MHMDA) [68] | Washington State, U.S. | Protects "consumer health data" broadly defined, including data derived from wearables. Requires opt-in consent. | Effective March 2024 [68]. |
| California Privacy Rights Act (CPRA) [68] | California, U.S. | Classifies health data from wearables as "sensitive personal information," granting consumers opt-out rights. | Enforced. |
Protocol for Data Governance in Digital Twin Research
Protocol Title: Data Anonymization and Secure Processing Protocol for Multi-Source Neurological Data.
Objective: To establish a standardized procedure for collecting, harmonizing, and anonymizing patient data for digital twin model training and application while ensuring compliance with global privacy regulations.
Materials:
- Source Data: De-identified data from clinical trials (e.g., CODR-AD), observational studies (e.g., ADNI), and potentially real-world data sources [12] [69].
- Data Processing Software: Statistical software (e.g., R, Python) with secure data environments.
- Secure Computing Infrastructure: A dedicated, access-controlled server with encryption for data at rest and in transit, aligned with proposed HIPAA Security Rule updates [68].
Procedure:
- Data Use Agreement & Legal Basis: Establish a legal basis for data processing. For historical data, this relies on the original study's informed consent and ethics approvals. For new data collection, obtain explicit, informed consent that covers the use of data for creating and validating AI models [48] [69].
- Data Harmonization: Transform variables from different source datasets into a common format and standard terminology (e.g., harmonizing different cognitive test scores) to create an integrated training dataset [12].
- De-identification & Anonymization:
- HIPAA Safe Harbor Method: Remove all 18 specified identifiers, including names, geographic subdivisions smaller than a state, all elements of dates (except year), and phone numbers [69].
- Assess Re-identification Risk: Perform a statistical risk assessment to ensure the remaining data cannot be used to identify an individual.
- Secure Model Training: Execute the AI model training (e.g., CRBM) within the secure, access-controlled computing environment. No raw, identifiable data shall be moved to less secure systems.
- Model Output Validation: When applying the model to a new clinical trial, use only baseline data from trial participants as input. The output (the digital twin) is a synthetic data point representing a predicted outcome, not the actual patient data, which helps maintain privacy [48].
Visualization of Data Governance Logic:
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Resources for Digital Twin Research in Neurological Diseases
| Item | Function / Description | Example Sources / Notes |
|---|---|---|
| Conditional Restricted Boltzmann Machine (CRBM) | An unsupervised machine learning model using probabilistic neural networks to generate digital twins from baseline data. Core prognostic algorithm. | Used in AWARE trial for Alzheimer's disease [12]. |
| Harmonized Historical Datasets | Large-scale, integrated datasets from control arms of clinical trials and observational studies used to train the prognostic AI model. | C-PATH CODR-AD, Alzheimer's Disease Neuroimaging Initiative (ADNI) [12]. |
| PROCOVA-MMRM Analysis | Statistical methodology (Prognostic Covariate Adjustment with Mixed-Model for Repeated Measures) that integrates digital twin predictions to reduce variance. | Method qualified by EMA; improves trial power [12]. |
| SHAP (SHapley Additive exPlanations) | A game-theoretic approach to explain the output of any machine learning model, providing interpretability for the digital twin's predictions. | Critical for model transparency and regulatory acceptance [48]. |
| Fairness Audit Toolkit | A set of software libraries and protocols for measuring and evaluating algorithmic bias across demographic subgroups in model performance. | Includes metrics like disparate impact, equal performance [66] [64]. |
The adoption of Verification, Validation, and Uncertainty Quantification (VVUQ) represents a critical paradigm shift in the development and application of digital twin technology for neurological disease progression research. VVUQ provides a systematic framework for establishing the credibility of computational models by ensuring they are technically correct (verification), accurately represent real-world biology (validation), and transparently account for inherent variabilities (uncertainty quantification) [70] [71]. For computational models aiming to predict the progression of complex neurological disorders such as Alzheimer's disease (AD) and multiple sclerosis (MS), implementing rigorous VVUQ is not merely a best practice but a fundamental necessity for clinical translation [12] [72].
The "validation gap" in this context refers to the significant challenge of demonstrating that a digital twin model, often trained on heterogeneous and multi-scale data, provides accurate and clinically meaningful predictions for individual patients. This gap is particularly pronounced in neurological diseases characterized by slow progression, high patient-to-patient variability, and the lack of perfect biomarkers. Closing this gap requires the implementation of standardized VVUQ protocols that are specifically adapted to the complexities of neurodegenerative disease modeling [37] [72].
Foundational VVUQ Concepts and Terminology
A precise understanding of VVUQ components is essential for its correct implementation. The following table defines the core concepts as formalized by leading standards organizations like ASME [70].
Table 1: Core Components of VVUQ
| Component | Definition | Key Question | Primary Focus |
|---|---|---|---|
| Verification | The process of determining that a computational model accurately represents the underlying mathematical model and its solution. | "Are we solving the equations correctly?" | Numerical accuracy, code correctness, solution convergence [70] [71]. |
| Validation | The process of determining the degree to which a model is an accurate representation of the real world from the perspective of the intended uses of the model. | "Are we solving the correct equations?" | Model fidelity to physical/biological reality [70] [71]. |
| Uncertainty Quantification (UQ) | The science of quantifying, characterizing, tracing, and managing uncertainties in computational and real-world systems. | "How reliable are the predictions given the uncertainties?" | Probabilistic output, confidence intervals, sensitivity analysis [70] [71]. |
Uncertainty in modeling is further classified into two primary types: Aleatoric uncertainty, which is inherent variability in the system (e.g., the stochastic nature of disease progression) and is irreducible, and Epistemic uncertainty, which stems from a lack of knowledge (e.g., imperfectly known model parameters) and can be reduced with more data [71]. A robust VVUQ process for digital twins must address both.
VVUQ Application in Neurological Digital Twins: A Case Study on Alzheimer's Disease
AI-generated digital twins are emerging as powerful tools for enhancing clinical trial efficiency in Alzheimer's disease. These digital twins are computational forecasts of an individual patient's placebo-condition disease trajectory, generated from their baseline data [12].
Application Protocol: Digital Twins as Prognostic Covariates
Objective: To reduce sample size and increase statistical power in a Phase 2 clinical trial (AWARE, NCT02880956) for Alzheimer's disease by using AI-generated digital twins as prognostic covariates in the statistical analysis model [12].
Methods Summary:
- Model Training: A Conditional Restricted Boltzmann Machine (CRBM), an unsupervised machine learning model, was trained on a harmonized historical dataset of 6,736 unique subjects from the C-Path Online Data Repository for Alzheimer's Disease (CODR-AD) and the Alzheimer's Disease Neuroimaging Initiative (ADNI) database [12].
- Digital Twin Generation: The trained model used baseline data from participants in the AWARE trial (n=453) to generate individualized digital twins—predictions of their cognitive score changes (e.g., on CDR-SB, ADAS-Cog14) over 96 weeks had they received a placebo [12].
- Analysis: The digital twin prediction was included as a covariate in a statistical model (PROCOVA-Mixed-Effects Model for Repeated Measures) to analyze the actual trial outcomes, adjusting for the prognostic forecast [12].
VVUQ Implementation and Results: The validation of this approach involved quantifying the correlation between the digital twin predictions and the actual observed outcomes in the trial. The results demonstrated the methodology's value for closing the validation gap in a regulatory context.
Table 2: VVUQ Outcomes for Alzheimer's Disease Digital Twins [12]
| VVUQ Metric | Result | Impact on Clinical Trial Efficiency |
|---|---|---|
| Validation Metric: Partial correlation between DT and actual cognitive score change | 0.30 to 0.39 (at Week 96) | Confirms model predictive accuracy and real-world biological relevance. |
| Uncertainty Quantification: Residual variance reduction | ~9% to 15% | Quantifies improvement in model precision. |
| Overall Impact: Potential sample size reduction | ~9% to 15% (total); 17% to 26% (control arm) | Directly demonstrates increased efficiency while maintaining statistical power. |
This methodology, which received a positive qualification opinion from the European Medicines Agency (EMA), highlights how a rigorous VVUQ process can facilitate the adoption of advanced computational models in drug development [12].
Experimental Protocol: Bayesian Framework with Uncertainty Quantification
For the research and development of predictive models themselves, implementing UQ is critical. The following protocol outlines a method for predicting Alzheimer's disease progression with inherent uncertainty quantification.
Objective: To predict future Alzheimer's Disease Assessment Scale (ADAS-13) and Clinical Dementia Rating – Sum of Boxes (CDR-SB) scores for individual patients while providing confidence intervals for each prediction [73] [74].
Materials & Methods:
- Data: Alzheimer's Disease Neuroimaging Initiative (ADNI) dataset, including baseline and Year 1 data for demographics, cognitive test scores, and MRI biomarkers [74].
- Model Architecture: A Bayesian Encoder-Decoder Gated Recurrent Unit (BEND-GRU) network. The Bayesian framework incorporates Monte Carlo Dropout during inference to quantify uncertainty by approximating the posterior distribution of the predictions [74].
- Training: The model is trained to map sequences of baseline and Year 1 data to cognitive scores at Year 2 and Year 3.
- Interpretability: The Integrated Gradients method is applied to identify which input features (e.g., MMSE scores, delayed recall, ventricle volume) most strongly influenced the predictions [74].
VVUQ Outcomes: The model demonstrated strong predictive performance for ADAS-13 (Year 3: MAE 3.60, R² 0.80) and CDR-SB (Year 3: MAE 0.95, R² 0.72) [74]. Crucially, it provided a confidence interval around each prediction, allowing clinicians to assess the reliability of the forecast for a specific patient. Feature attribution revealed that MMSE scores and delayed recall totals were among the strongest predictors, offering transparency and helping to validate the model's reasoning against clinical knowledge [74].
The Scientist's Toolkit: Essential Research Reagent Solutions
Successful implementation of VVUQ for neurological digital twins relies on a suite of data, computational tools, and methodological standards.
Table 3: Key Research Reagent Solutions for Digital Twin VVUQ
| Reagent / Resource | Function in VVUQ Process | Example in Context |
|---|---|---|
| Standardized Terminology (ASME VVUQ 1-2022) | Provides a common language for VVUQ activities, ensuring clear communication and understanding among researchers and regulators. | Using precise definitions for "verification" and "validation" as per the ASME standard [70]. |
| Risk-Based VVUQ Framework (ASME V&V 40) | Guides the level of VVUQ effort based on the model's intended use and the associated decision risk. | Applying a higher level of validation rigor to a digital twin intended for regulatory submission versus one used for early research [70]. |
| High-Quality Historical Datasets (e.g., ADNI, CODR-AD) | Serves as the foundational data for model training and provides a source for external validation. | Training a generative model on ADNI and CODR-AD data to create digital twins for a new clinical trial [12]. |
| Uncertainty Quantification Software Tools (e.g., SmartUQ) | Facilitates the design of experiments, model calibration, and propagation of input uncertainties to quantify output confidence. | Performing sensitivity analysis to determine which input parameters (e.g., specific cognitive scores) contribute most to uncertainty in progression forecasts [71]. |
| Bayesian Neural Networks | A model architecture that natively quantifies predictive uncertainty by learning probability distributions over its weights. | Using a BEND-GRU to predict cognitive scores with a confidence interval, incorporating both model and data noise [74]. |
Integrated VVUQ Workflow for Neurological Digital Twins
The following diagram synthesizes the core concepts, protocols, and tools into a logical workflow for implementing VVUQ in the development of digital twins for neurological disease progression.
Diagram 1: Integrated VVUQ Workflow for Neurological Digital Twins. This workflow outlines the sequential and interconnected processes of Verification, Validation, and Uncertainty Quantification, supported by a foundational toolkit of resources, to ultimately assess the overall credibility of a digital twin model for predicting neurological disease progression.
Application Notes: Digital Twins in Neurological Disease
Core Concept and Clinical Rationale
Digital twins (DTs) represent a transformative approach in clinical research and practice, creating dynamic, virtual replicas of individual patients or physiological systems. These computational models leverage artificial intelligence (AI) to integrate multi-source data, enabling predictive simulations of disease progression and treatment response [5] [75]. The translation of this technology from research models to bedside decision support is particularly valuable in neurological disorders, where disease heterogeneity, complex pathophysiology, and limited access to specialized care present significant challenges [12] [5].
Quantitative Evidence from Clinical Studies
Recent clinical trials demonstrate the tangible impact of digital twin technology in improving research efficiency and patient outcomes.
Table 1: Efficacy of Digital Twins in Clinical Trials
| Therapeutic Area | Trial Design | Key Efficacy Outcomes | Trial Efficiency Outcomes | Citation |
|---|---|---|---|---|
| Alzheimer's Disease | Phase 2 trial (AWARE); DTs as prognostic covariates | Partial correlation between DTs and cognitive score change: 0.30-0.39 | Residual variance reduced by 9-15%; sample size reduced by 9-15%; control arm reduced by 17-26% | [12] |
| Type 1 Diabetes | 6-month RCT (N=72); DT-guided insulin optimization | Time-in-range improved from 72% to 77% (p<0.01); HbA1c reduced from 6.8% to 6.6% | 41% of participants achieved clinically meaningful improvement (>5% TIR) | [76] |
| Postural Tachycardia Syndrome (POTS) | Conceptual framework for autonomic disorders | Proposed for real-time prediction of cerebral hypoperfusion and personalized drug dosing | Aims to enable preemptive intervention and reduce trial-and-error prescribing | [5] |
Implementation Workflows for Neurological Applications
The implementation of digital twins for neurological conditions involves a structured, iterative process. The following workflow outlines the key stages from model creation to clinical decision support.
Diagram 1: Digital Twin Clinical Translation Workflow (77 characters)
Experimental Protocols
Protocol 1: Generating Prognostic Digital Twins for Alzheimer's Disease Trials
This protocol details the methodology used in the AWARE trial to create and validate digital twins for prognostic covariate adjustment in Alzheimer's disease clinical trials [12].
Objectives
- To generate patient-specific digital twins predicting individual disease progression under placebo conditions.
- To incorporate digital twin predictions as covariates in statistical models to reduce variance and required sample size.
- To validate the digital twin methodology against independent clinical trial datasets.
Materials and Reagents
Table 2: Research Reagent Solutions for Digital Twin Generation
| Item | Function/Description | Example Sources/Platforms |
|---|---|---|
| Conditional Restricted Boltzmann Machine (CRBM) | Unsupervised machine learning model with probabilistic neural networks for DT generation | Custom development based on [12] |
| Harmonized Historical Training Data | Integrated datasets from control arms of clinical trials and observational studies for model training | C-Path Online Data Repository for Alzheimer's Disease (CODR-AD), Alzheimer's Disease Neuroimaging Initiative (ADNI) [12] |
| Baseline Patient Data | Input variables from trial participants for DT instantiation | Demographics, genetics, clinical severity scores, cognitive measures, laboratory values [12] |
| Clinical Endpoint Data | Outcome measures for model validation and analysis | CDR-SB, ADAS-Cog 14, MMSE, FAQ [12] |
| Computational Environment | Hardware and software infrastructure for model training and simulation | Python-based platforms (Simply, Open Digital Twin Project, PyTwin) [5] |
Step-by-Step Procedure
Data Harmonization and Preprocessing
- Curate and harmonize historical data from multiple sources (e.g., 29 clinical trials from CODR-AD and ADNI observational studies, totaling 6,736 unique subjects) [12].
- Process 66+ background and longitudinal variables, including demographics, genetics, clinical severity, cognitive/functional measures, and laboratory data.
- Implement quality control checks for data completeness and consistency.
Model Training
- Train the Conditional Restricted Boltzmann Machine (CRBM) on the harmonized historical dataset.
- Validate the model by assessing its predictive accuracy against held-out validation datasets from three independent trials, targeting partial correlation coefficients of 0.30-0.46 with actual outcomes [12].
Digital Twin Generation for Trial Participants
- Input baseline data from each participant in the target clinical trial (e.g., AWARE trial: 453 subjects with MCI or mild AD) into the trained CRBM.
- Generate a digital twin for each participant, producing an individualized forecast of their clinical outcomes over the trial duration (e.g., 96 weeks) under the placebo condition [12].
Statistical Analysis and Validation
- Incorporate the digital twin predictions as prognostic covariates in the primary statistical analysis model (e.g., PROCOVA-Mixed-Effects Model for Repeated Measures) [12].
- Calculate the partial correlation between the digital twin prediction and the observed clinical change score.
- Assess the reduction in residual variance of the treatment effect estimate.
- Calculate potential sample size reductions while maintaining statistical power.
Protocol 2: Co-Adaptation Using Digital Twins for Chronic Disease Management
This protocol, adapted from a successful trial in type 1 diabetes, provides a framework for using digital twins to enable personalized, adaptive treatment for chronic neurological conditions [76].
Objectives
- To create a feedback loop between the patient and their digital twin for optimizing therapeutic parameters.
- To enable patients and clinicians to test interventions in silico before real-world implementation.
- To demonstrate improvement in clinically relevant outcomes through digital twin-guided co-adaptation.
Materials and Reagents
- Continuous physiological monitors (e.g., wearable sensors for heart rate, blood pressure, cerebral blood flow) [5].
- Cloud-based digital twin ecosystem for data integration and simulation.
- Patient-facing application interface for interaction with the digital twin and receipt of recommendations.
- Clinical dashboards integrated with Electronic Health Records for clinician oversight [5].
Step-by-Step Procedure
System Initialization and Mapping
- Transmit baseline and continuous monitoring data from the patient to a cloud application.
- Map the patient to their corresponding digital twin within the simulation environment [76].
Automated Parameter Optimization
- The system automatically optimizes therapy control parameters (e.g., medication dosages, lifestyle suggestions) at predefined intervals (e.g., bi-weekly) based on the digital twin's simulation of outcomes [76].
- The optimized parameters are presented as recommendations to the clinician and/or patient via the application interface.
Interactive Patient Co-Adaptation
- Patients and clinicians can actively use the application to run "what-if" scenarios, replaying past data through the digital twin to visualize potential outcomes of different management choices [76].
- This interactive simulation helps users understand the impact of potential changes before implementing them.
Outcome Assessment and Model Refinement
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Neurological Digital Twins
| Tool Category | Specific Examples | Research Function |
|---|---|---|
| Computational Modeling Platforms | Conditional Restricted Boltzmann Machine (CRBM) [12]; Simply, Open Digital Twin Project, PyTwin [5]; TumorTwin [5] | Core engines for creating and running the digital twin simulations; CRBM was pivotal for prognostic DT generation in Alzheimer's trials. |
| Data Integration & Harmonization Tools | C-Path Online Data Repository for Alzheimer's Disease (CODR-AD) [12]; Alzheimer's Disease Neuroimaging Initiative (ADNI) [12] | Provide large-scale, harmonized historical datasets (demographics, omics, clinical outcomes) essential for training robust and generalizable AI models. |
| Real-Time Data Acquisition | Wearable devices (heart rate, blood pressure, end-tidal CO2, EEG) [5]; Patient-Reported Outcome (PRO) platforms | Capture continuous, real-world physiological and symptom data to initialize and dynamically update the digital twin, enabling true personalization. |
| Analytical & Validation Frameworks | PROCOVA-Mixed-Effects Model for Repeated Measures (PROCOVA-MMRM) [12]; SHapley Additive exPlanations (SHAP) [15] | Statistical methods for integrating DTs into trial analysis (PROCOVA) and tools for interpreting AI model outputs, ensuring regulatory acceptance and clinical transparency. |
System Architecture for Clinical Deployment
The effective deployment of digital twins at the bedside requires a robust and secure technical architecture that facilitates real-time data flow and clinician interaction.
Diagram 2: Digital Twin System Architecture (43 characters)
Evaluating Performance and Impact: Validation Frameworks and Comparative Efficacy
Within the advancing field of neurological disease research, digital twin technology is emerging as a transformative tool for creating dynamic, virtual representations of individual patients. These models leverage real-time data integration and generative artificial intelligence (AI) to forecast disease trajectories and simulate interventions. Accurate benchmarking of predictive models is paramount for validating their clinical utility in preventive and personalized medicine [75]. This document establishes standardized application notes and protocols for evaluating the predictive accuracy of digital twin technologies, with a specific focus on trajectories in Alzheimer's disease, other neurodegenerative conditions, and neurological sequelae of cancer [77] [78]. The protocols are designed for researchers, scientists, and drug development professionals, providing a framework for rigorous, comparable validation of forecasting models.
Quantitative Benchmarking of Forecasting Performance
A critical step in model validation is the systematic comparison of performance against established benchmarks across diverse neurological conditions. The following table summarizes key accuracy metrics from recent peer-reviewed studies for models forecasting disease progression.
Table 1: Benchmarking Predictive Accuracy Across Neurological Conditions and Models
| Disease Context | Forecasting Model | Prediction Task | Key Accuracy Metric | Performance Value | Data Source |
|---|---|---|---|---|---|
| Alzheimer's Disease [79] [78] | DT-GPT (LLM-based) | MMSE Score (24-month) | Scaled Mean Absolute Error (MAE) | 0.553 | ADNI Dataset (n=1,140) |
| Alzheimer's Disease [79] [78] | DT-GPT (LLM-based) | CDR-SB Score (24-month) | Scaled Mean Absolute Error (MAE) | 0.485 | ADNI Dataset (n=1,140) |
| Alzheimer's Disease [79] [78] | Transformer | MMSE Score (Longitudinal) | Scaled Mean Absolute Error (MAE) | 0.553 | ADNI Dataset |
| Alzheimer's Disease [78] | Deep Learning (Multimodal) | Cognitive Impairment Classification | Accuracy | 85-95%* | Homogeneous Cohorts |
| Alzheimer's Disease [78] | Deep Learning (Multimodal) | Cognitive Impairment Classification | Real-World Accuracy (Estimated) | 70-80% | Diverse Clinical Settings |
| Pediatric Cancer (Neurological Sequelae) [77] | Digital Twin (Black Box) | Neurological Complications | Predictive/Prognostic Pattern Generation | Qualitative | EHR & Expanded Networks |
Note: The 85-95% accuracy reported for deep learning models in Alzheimer's disease often derives from small, homogeneous cohorts. Critical analysis suggests real-world performance in diverse clinical settings may be 10-15% lower, emphasizing the need for external validation [78]. MAE values are scaled; lower values indicate better performance. CDR-SB: Clinical Dementia Rating - Sum of Boxes; MMSE: Mini-Mental State Examination.
Experimental Protocols for Model Benchmarking
To ensure reproducibility and robust validation, the following detailed protocols outline the procedure for benchmarking studies, from data preparation to performance evaluation.
Protocol 1: Benchmarking Long-Term Cognitive Trajectory Forecasting
Application Note: This protocol is designed for benchmarking models that predict the progression of cognitive scores in neurodegenerative diseases like Alzheimer's over multi-year horizons. It is adapted from studies using the Alzheimer's Disease Neuroimaging Initiative (ADNI) dataset [79].
Materials & Data Requirements:
- Datasets: Longitudinal cohort data (e.g., ADNI) containing baseline and follow-up cognitive scores (MMSE, CDR-SB, ADAS-Cog).
- Data Preprocessing: Standardization of variables, handling of missing data via appropriate imputation, and splitting into training/validation/test sets by patient, not by time points.
Experimental Workflow:
Procedure:
- Data Preprocessing & Splitting: Execute the steps in the "Data Preparation" module above. For the test set, ensure all future time points for a patient are hidden from the model during training.
- Model Training & Fine-Tuning: Train the candidate model (e.g., DT-GPT, Transformer, RNN) on the training set. For LLM-based models, this involves fine-tuning on the structured clinical data. Optimize hyperparameters using the validation set.
- Generate Multi-Year Forecasts: Using only baseline data from the held-out test set patients, run the trained model to generate forecasts for cognitive scores at pre-defined future intervals (e.g., 6, 12, 18, 24 months).
- Quantitative Accuracy Benchmarking: Calculate the Scaled Mean Absolute Error (MAE) between the forecasted and actual values for each cognitive score and time point. Compare the results against state-of-the-art models (e.g., results from Table 1). Additionally, assess whether the model maintains the distribution and cross-correlations of the clinical variables, which is crucial for clinical plausibility [79].
Protocol 2: Validating Digital Twin Predictive Accuracy for Neurological Sequelae
Application Note: This protocol outlines a procedure for validating digital twin predictions of neurological complications, such as those arising from pediatric cancer or its treatment. It leverages real-world data (RWD) from sources like Electronic Health Records (EHRs) [77] [75].
Materials & Data Requirements:
- Data Sources: EHRs, specialized clinician inputs, and potentially data from expanded clinical networks or wearable sensors [77].
- Model Types: Define the digital twin category: Grey Box (relies on existing clinical knowledge), Surrogate Box (incorporates data from expanded networks), or Black Box (uses deep learning to generate novel predictors without prior physician knowledge) [77].
Experimental Workflow:
Procedure:
- Digital Twin Model Initialization: Create the digital twin by integrating multimodal patient data. Select the appropriate model type (Grey, Surrogate, or Black Box) based on the available data and research question [77].
- Generate Patient-Specific Predictors: Run the model to generate risk predictions for neurological complications. For Black Box models, the focus is on isolating novel, data-driven predictors that are not part of standard clinical knowledge.
- Clinical Validation & Consensus: This is a critical step. Compare the model's predictions and identified predictors against the assessment of expert clinicians. The goal is not to replace clinical judgement but to complement it. Evaluate the model's ability to consolidate a spectrum of clinician opinions and reduce the margin of error in prognostication [77]. The success of this validation is measured by the model's contribution to scientific diagnostic and prognostic understanding.
The Scientist's Toolkit: Research Reagent Solutions
The development and benchmarking of digital twins for disease forecasting rely on a suite of computational and data resources. The following table details essential "research reagents" for this field.
Table 2: Essential Research Reagents for Digital Twin Forecasting
| Tool / Resource | Type | Primary Function in Research | Relevance to Benchmarking |
|---|---|---|---|
| DT-GPT Model [79] | Generative AI Model | Forecasts multi-variable clinical trajectories from EHR data. | Serves as a state-of-the-art benchmark for forecasting tasks; enables zero-shot prediction. |
| ADNI Dataset [79] [78] | Longitudinal Clinical Data | Provides structured, longitudinal data for Alzheimer's disease progression. | Standardized public dataset for benchmarking long-term cognitive trajectory forecasts. |
| Electronic Health Records (EHR) [77] [75] | Real-World Data (RWD) | Serves as primary data source for building and validating patient-specific digital twins. | Critical for validating predictions of complications (e.g., neurological sequelae of cancer). |
| ClinicalTrials.gov / TrialBench [80] | Clinical Trial Data Repository | Provides data on trial protocols, outcomes, and failure reasons. | Used to build models for predicting trial outcomes, adverse events, and patient dropout. |
| Transformer Neural Networks [81] [79] | Deep Learning Architecture | Models complex temporal and spatial dynamics in multi-source data. | Core architecture for many state-of-the-art forecasting models; baseline for performance comparison. |
| Multi-Source Data Fusion [81] [78] | Methodology | Integrates disparate data types (e.g., clinical, social media sentiment). | Framework for testing if added data modalities (e.g., digital biomarkers) improve forecast accuracy. |
| Scaled Mean Absolute Error (MAE) [79] | Quantitative Metric | Aggregates forecast error across variables of different scales. | A primary metric for objectively comparing model performance on clinical trajectory forecasting. |
The rigorous benchmarking of predictive accuracy, as outlined in these protocols and case studies, is the cornerstone of translating digital twin technology from a theoretical concept to a clinically actionable tool. By adhering to standardized evaluation frameworks that utilize robust quantitative metrics like Scaled MAE, diverse and representative datasets, and clear validation workflows, researchers can consistently validate the performance of disease trajectory forecasting models. This disciplined approach ensures that digital twin models for neurological disease progression meet the high standards required for application in precision medicine, drug development, and ultimately, improving patient outcomes.
The integration of digital twin technology into neurological disease research represents a paradigm shift in how we approach diagnosis, prognosis, and therapeutic development. Digital twins—dynamic virtual replicas of physical entities—enable researchers to simulate disease progression, test interventions, and personalize treatment strategies in silico before clinical application [82] [11]. For neurodegenerative disorders like Alzheimer's disease (AD) and multiple sclerosis (MS), where heterogeneity dominates clinical presentation and progression, these models offer unprecedented opportunities to address complexity [83] [84]. However, the translational potential of digital twins hinges on rigorous clinical validation frameworks that transcend traditional statistical correlation to demonstrate tangible impacts on patient outcomes. This protocol outlines comprehensive validation metrics and methodologies essential for establishing digital twins as clinically credible tools in neurological research and drug development.
Quantitative Clinical Validation Metrics for Digital Twin Technologies
The clinical validation of digital twin technologies requires a multi-faceted approach encompassing discrimination accuracy, prognostic precision, and real-world clinical utility. The table below summarizes key quantitative metrics derived from recent validation studies across neurological applications.
Table 1: Clinical Validation Metrics for Digital Twin Technologies in Neurology
| Application Domain | Validation Metric | Reported Performance | Clinical Outcome Correlation |
|---|---|---|---|
| Mild Cognitive Impairment (MCI) to Alzheimer's Dementia Prediction | Area Under ROC Curve (AUC-ROC) | 0.91 (IQR 0.87-0.93) [85] | Accurate identification of patients at highest risk for progression to dementia |
| 3-Year Cognitive Decline Forecast | Mean Absolute Error (MAE) for CDR-SB | 1.32 (IQR 1.30-1.33) [85] | Precise forecasting of clinical disability measured by CDR-Sum of Boxes |
| 3-Year Cognitive Decline Forecast | Mean Absolute Error (MAE) for MMSE | 1.51 (IQR 1.50-1.52) [85] | Accurate prediction of cognitive decline measured by Mini-Mental State Examination |
| Multiple Sclerosis MRI Monitoring | Case-Level Sensitivity | 93.3% vs. 58.3% for standard radiology [86] | Enhanced detection of disease activity necessitating treatment escalation |
| Multiple Sclerosis MRI Monitoring | Specificity | Minimal loss compared to standard reporting [86] | Maintenance of diagnostic accuracy while improving sensitivity |
| Brain Volume Loss Quantification | Percentage Brain Volume Change (PBVC) | -0.32% vs. -0.36% (core lab reference) [86] | Equivalent measurement of neurodegeneration biomarker |
| Plasma p-Tau 217 for Amyloid Pathology | Clinical Sensitivity/Specificity | >90% (with 2-cutoff approach) [87] | Accurate detection of underlying Alzheimer's pathology |
These metrics demonstrate a progression from traditional statistical correlation to clinically meaningful endpoints. For digital twins in neurology, discrimination accuracy (e.g., AUC-ROC) establishes diagnostic capability, while forecasting precision (e.g., MAE) validates predictive utility in tracking disease trajectory [85]. Most importantly, comparative metrics against current clinical standards (e.g., radiology reports) demonstrate real-world value in enhancing diagnostic sensitivity or matching gold-standard measurements [86].
Experimental Protocols for Clinical Validation
Protocol 1: Validation of Disease Progression Prediction Models
Purpose: To validate digital twin models for predicting conversion from mild cognitive impairment (MCI) to Alzheimer's dementia and forecasting cognitive decline.
Materials and Methods:
- Study Population: Recruit 200+ participants encompassing MCI and Alzheimer's dementia patients, with 80% allocation to training sets and 20% to validation sets [85]
- Predictor Variables: Collect age, sex, APOE-ε4 carrier status, and comprehensive neuropsychological test results (e.g., MMSE, CDR-SB) [85]
- Model Development: Implement machine learning algorithms (support vector machine, gradient boosting, random forest) with nested stratified cross-validation [85]
- Outcome Measures:
- MCI-to-dementia conversion within 3-year prediction window
- Longitudinal cognitive scores (CDR-SB, MMSE) at annual intervals
- Validation Framework:
- Perform 100 iterations of random train-test splits
- Calculate median AUC-ROC for classification tasks
- Compute median mean absolute error (mMAE) for regression tasks
- Compare against baseline models using Mann-Whitney-Wilcoxon tests [85]
Analysis and Interpretation: The Florey Fusion Model exemplifies this protocol, achieving AUC-ROC of 0.91 for MCI-to-AD prediction and MAE of 1.32 for 3-year CDR-SB forecast [85]. Clinical validation requires comparison against the ~10% annual conversion rate benchmark observed in clinical populations [85].
Protocol 2: Real-World Clinical Validation for MRI Monitoring in Multiple Sclerosis
Purpose: To validate AI-based digital twin tools for detecting disease activity and brain volume loss in multiple sclerosis against clinical standards.
Materials and Methods:
- Study Population: 400+ scan pairs from 300+ MS patients with longitudinal MRI data [86]
- Image Acquisition: 3D-T1 and 3D-FLAIR sequences with slice thickness ≤3mm across multiple scanner platforms [86]
- Reference Standards:
- Qualitative radiology reports generated in clinical practice
- Quantitative measurements from core imaging laboratory
- Consensus ground truth for lesion activity
- AI Tool Implementation:
- Automated quality checks for sequence compliance
- Deep learning segmentation (3D-UNet architecture) for lesions and brain structures
- Lesion-inpainting (LG-Net) to ameliorate segmentation bias
- Longitudinal brain volume change (DeepBVC algorithm) [86]
- Outcome Measures:
- Case-level sensitivity/specificity for new/enlarging lesions
- Percentage brain volume change (PBVC) correlation with core lab
- Inter-rater reliability between AI tool and radiology reports
Analysis and Interpretation: Validation demonstrates superior sensitivity of AI tools (93.3%) over standard radiology reports (58.3%) for detecting disease activity, with equivalent brain volume measurement to core labs (mean PBVC -0.32% vs. -0.36%) [86]. This establishes clinical utility in enhancing routine practice.
Protocol 3: Analytical and Clinical Validation of Plasma Biomarkers
Purpose: To establish clinical-grade validation of plasma biomarkers for integration into digital twin models of neurodegenerative disease.
Materials and Methods:
- Technology Platform: Single Molecule Array (Simoa) digital immunoassay on HD-X instrument [87]
- Study Population: 800+ symptomatic individuals from multiple independent cohorts [87]
- Reference Standards: Amyloid PET or cerebrospinal fluid biomarkers as ground truth [87]
- Assay Protocol:
- 3-step sandwich immunoassay with anti-p-Tau 217 capture beads
- Biotinylated detector antibody (anti-tau HT43)
- Streptavidin-ß-galactosidase conjugation
- Resorufin ß-D-galactopyranoside substrate solution
- Digital detection via microwell array [87]
- Validation Framework:
- Analytical validation: sensitivity, precision, reproducibility
- Clinical validation: sensitivity/specificity against reference standards
- Implementation of two-cutoff approach for diagnostic gray zone [87]
Analysis and Interpretation: The Simoa p-Tau 217 assay demonstrates >90% clinical sensitivity, specificity, and accuracy, meeting recommended performance thresholds for diagnostic use [87]. The two-cutoff approach maximizes predictive values while acknowledging biological variability.
Visualizing Clinical Validation Workflows
Figure 1: Clinical Validation Workflow for Neurological Digital Twins. This framework outlines the comprehensive validation pathway from study design through to clinical deployment decision-making.
Research Reagent Solutions for Validation Studies
Table 2: Essential Research Reagents and Platforms for Digital Twin Validation
| Reagent/Platform | Specifications | Research Application |
|---|---|---|
| Simoa HD-X Analyzer | Fully automated digital immunoassay platform [87] | Ultrasensitive plasma biomarker quantification (p-Tau 217, Aβ42/40, GFAP, NfL) |
| LucentAD p-Tau 217 Assay | Analytical sensitivity: <0.01 pg/mL; Two-cutoff approach [87] | Detection of amyloid pathology in Alzheimer's disease |
| EuroPOND EBM Toolbox | Open-source event-based modeling software [83] | Disease staging and sequence analysis in neurodegenerative disorders |
| iQ-Solutions (MS Report) | AI algorithms based on 3D-UNet deep neural networks [86] | Automated MRI lesion segmentation and brain volume quantification |
| HARVEY CFD Solver | Computational fluid dynamics solver for hemodynamics [88] | Physics-based simulation of cardiovascular and cerebrovascular systems |
| 3D-UNet Architecture | Deep learning network for medical image segmentation [86] | Volumetric analysis of brain structures and pathological lesions |
The clinical validation of digital twin technologies for neurological diseases requires a multidimensional approach that progresses from traditional statistical correlation to demonstrated impact on patient outcomes. Through standardized validation protocols encompassing discrimination accuracy, forecasting precision, and real-world clinical utility, researchers can establish these models as credible tools for both fundamental research and clinical application. The integration of high-sensitivity biomarker assays, advanced AI analytics, and comprehensive validation frameworks will accelerate the translation of digital twin technologies from research concepts to clinically valuable tools that enhance patient care and therapeutic development. As these technologies mature, ongoing validation against evolving clinical standards will remain essential to maintaining their relevance and utility in the rapidly advancing field of neurological medicine.
The development of novel therapeutics for neurological diseases faces significant challenges, including high clinical trial failure rates and substantial costs. A critical factor in this process is the determination of sample size, which directly impacts a study's statistical power, cost, duration, and ethical considerations [89] [90]. Insufficient sample sizes produce underpowered studies that may fail to detect genuine treatment effects (Type II errors), while excessively large samples expose unnecessary participants to potential risks and consume limited resources [91]. This application note explores quantitative frameworks for optimizing sample size and enhancing statistical power through the integration of digital twin technology and advanced analytical approaches within neurological disease research.
Digital twins—virtual representations of physiological processes—are emerging as transformative tools for clinical trial design [75]. By creating patient-specific computational models that simulate disease progression and treatment response, researchers can generate more precise estimates of expected treatment effects and outcome variability [92]. These refined parameters directly influence sample size calculations, potentially enabling substantial sample size reductions while maintaining or even enhancing statistical power. For neurological conditions such as Alzheimer's disease, where patient recruitment is challenging and disease heterogeneity complicates trial design, digital twin approaches offer promising pathways to more efficient and informative clinical studies [92] [75].
Quantitative Foundations: Sample Size, Power, and Effect Size
Core Statistical Relationships
The interrelationship between sample size, statistical power, effect size, and significance level forms the foundation of clinical trial design [89] [90]. Statistical power, defined as the probability of correctly rejecting a false null hypothesis (1 - β), is directly influenced by several key factors [93]. The following formulae illustrate these relationships for common trial designs:
Sample size calculation for two independent proportions [89]:
Where P = (P1 + P2)/2, Zα/2 and Zβ are normal deviates for Type I and Type II error, and P1, P2 are outcome proportions.
Sample size calculation for two means [89]:
Where σ is the pooled standard deviation, and d is the difference between group means.
Key Parameter Definitions and Impact on Sample Size
Table 1: Factors Influencing Sample Size in Clinical Trials
| Factor | Definition | Impact on Sample Size | Digital Twin Enhancement Potential |
|---|---|---|---|
| Effect Size (ES) | Magnitude of the treatment effect | Larger ES reduces sample size | Personalized models provide more precise ES estimation |
| Statistical Power (1-β) | Probability of detecting true effect | Higher power increases sample size | Enables maintained power with smaller samples via reduced variability |
| Significance Level (α) | Probability of Type I error | Lower α increases sample size | Optimized α selection through simulation |
| Variance (σ²) | Variability in outcome measures | Higher variance increases sample size | Reduced through patient stratification and precise phenotyping |
| Attrition Rate | Participant dropout | Higher attrition increases initial recruitment needs | Improved retention through participant targeting |
The traditional alpha level (α) of 0.05 represents a 5% risk of Type I error (false positives), while the conventional power (1-β) of 80% or 0.8 indicates a 20% chance of Type II error (false negatives) [89] [91]. Increasing the significance level (e.g., from α=0.05 to α=0.10) can boost power but simultaneously raises false positive risk [93]. Digital twin simulations facilitate optimal balancing of these parameters by modeling outcomes under various scenarios before trial initiation [92] [75].
Table 2: Sample Size Requirements for Different Effect Sizes in Neurological Trials
| Trial Design | Effect Size | Power | Alpha | Control Group Event Rate | Required Sample Size Per Group |
|---|---|---|---|---|---|
| Cognitive Decline Prevention | Cohen's d = 0.4 | 80% | 0.05 | N/A | 100 |
| Cognitive Decline Prevention | Cohen's d = 0.6 | 80% | 0.05 | N/A | 45 |
| Alzheimer's Diagnostic (CSF+) | OR = 3.5 | 80% | 0.05 | 30% | 82 |
| Alzheimer's Diagnostic (CSF+) | OR = 5.0 | 80% | 0.05 | 30% | 46 |
| Disease Progression (Conversion) | HR = 0.6 | 80% | 0.05 | 40% (2-year) | 127 total events |
Digital Twin Methodology for Neurological Clinical Trials
Digital Twin Architecture and Workflow
Digital twins in neurological research are virtual representations of brain structure and function that integrate multiscale biological data to simulate disease progression and treatment response [37] [75]. The DADD (Digital Alzheimer's Disease Diagnosis) model exemplifies this approach, creating personalized computational models that infer neurodegeneration patterns from non-invasive electroencephalography (EEG) recordings [92]. These models incorporate well-documented Alzheimer's disease mechanisms, including synaptic degradation, connectivity alterations, and protein misfolding, to generate patient-specific biomarkers that predict clinical trajectories.
Digital Twin Workflow for Clinical Trial Optimization
Protocol: Implementing Digital Twins for Sample Size Optimization
Objective: Reduce sample size requirements while maintaining statistical power through digital twin-generated biomarkers and patient stratification in neurological clinical trials.
Materials:
- High-density EEG system (64+ channels)
- Computational modeling framework (The Virtual Brain, DADD model)
- Multimodal data integration platform
- Statistical analysis software (R, Python with appropriate packages)
Procedure:
Participant Recruitment and Data Acquisition
- Recruit participants meeting eligibility criteria (e.g., subjective cognitive decline, mild cognitive impairment)
- Acquire multimodal baseline data: resting-state EEG, task-based EEG/ERPs, structural MRI, clinical neuropsychological assessments, and optional molecular biomarkers (CSF, blood) [92]
Digital Twin Personalization
- Implement the DADD model architecture to create patient-specific computational twins
- Parameterize models using individual neurophysiological data (ERP amplitudes, functional connectivity metrics)
- Calibrate model parameters to match individual patient characteristics and baseline disease state [92]
Treatment Response Simulation
- Simulate disease progression under control and active treatment conditions
- Run multiple iterations to account for biological variability and uncertainty
- Generate personalized trajectories of cognitive decline and biomarker progression [75]
Effect Size and Variance Estimation
- Calculate treatment effect sizes from simulated outcomes across the cohort
- Estimate outcome variability within and between simulated patient subgroups
- Compare digital twin-derived parameters with conventional estimation approaches
Sample Size Calculation
- Input digital twin-derived effect sizes and variance estimates into standard sample size formulae
- Calculate sample requirements for various power (80-90%) and significance (0.05-0.01) levels
- Compare results with traditional sample size estimation approaches
Patient Stratification Optimization
- Identify digital biomarkers that predict differential treatment response
- Develop enrichment strategies to select patients most likely to benefit from intervention
- Recalculate sample size requirements for enriched populations
Validation: Compare predicted treatment effects from digital twins with actual clinical trial outcomes in independent cohorts to assess predictive accuracy.
Experimental Validation and Case Studies
Alzheimer's Disease Diagnostic and Prognostic Accuracy
The DADD digital twin model has demonstrated remarkable accuracy in early Alzheimer's disease identification and prognosis prediction [92]. In a study of 124 participants with varying cognitive status, the model achieved 88% accuracy in identifying cerebrospinal fluid (CSF) biomarker-positive individuals, significantly outperforming standard EEG biomarkers (58% accuracy). Furthermore, the model predicted clinical conversion to cognitive decline with 87% accuracy (versus 54% for standard EEG) [92]. These results highlight the potential of digital twin approaches to enhance endpoint precision in clinical trials, thereby reducing sample size requirements.
Sample Size Reduction Through Variance Minimization
Digital twin technology reduces outcome variability through multiple mechanisms:
Precise Phenotyping: Computational models integrate multimodal data to create refined disease subtypes, reducing heterogeneity within treatment groups [37] [75]
Endpoint Optimization: Model-derived biomarkers show stronger treatment signals than conventional clinical endpoints, increasing effect size estimates [92]
Patient Enrichment: Predictive models identify patients most likely to respond to specific interventions, creating more homogeneous study populations [75]
In the DADD model implementation, the enhanced classification accuracy (from 58% to 88%) corresponds to substantially increased effect sizes (Cohen's d increasing from approximately 0.4 to 1.2), which could enable sample size reductions of up to 70% while maintaining equivalent statistical power [92].
Impact of Digital Twins on Sample Size and Power Parameters
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Digital Twin-Enhanced Clinical Trials
| Resource Category | Specific Solution | Function/Application | Key Features |
|---|---|---|---|
| Data Acquisition | High-density EEG Systems (64+ channels) | Recording neural electrical activity | High temporal resolution, compatibility with ERP paradigms |
| Computational Modeling | The Virtual Brain Platform | Whole-brain network modeling | Multiscale integration, personalization capabilities |
| Biomarker Analysis | DADD Model Implementation | Alzheimer's-specific digital twin framework | EEG-to-biomarker translation, CSF prediction |
| Statistical Analysis | R Statistical Environment with power/simulation packages | Sample size calculation and power analysis | Comprehensive statistical modeling, bootstrap methods |
| Data Integration | Multi-omics Analysis Platforms | Integration of genomic, proteomic, metabolic data | Systems biology approach, network analysis |
| Clinical Assessment | Standardized Neuropsychological Batteries | Cognitive endpoint measurement | Validated instruments, disease-specific sensitivity |
Practical Implementation Protocol
Power Enhancement Through Adaptive Digital Twin Frameworks
Objective: Enhance statistical power through continuous learning and model refinement during clinical trial execution.
Procedure:
Initial Power Analysis
- Conduct conventional power analysis based on existing literature and preliminary data
- Supplement with digital twin-derived effect size and variability estimates
- Establish target sample size with appropriate inflation for anticipated attrition
Interim Analysis and Model Refinement
- Perform blinded interim analyses using digital twin predictions
- Refine model parameters based on accumulating trial data
- Re-estimate sample size requirements using group sequential methods
Adaptive Enrichment
- Apply digital twin classifiers to identify patient subgroups with enhanced treatment responses
- Optionally modify enrollment criteria to enrich for responsive populations
- Recalculate statistical power for enriched cohort
Endpoint Validation
- Compare digital twin-derived biomarkers with conventional clinical endpoints
- Assess correlation between model predictions and observed outcomes
- Validate surrogate endpoint candidates against clinical progression
Statistical Considerations: Implement appropriate alpha-spending functions to control Type I error inflation in adaptive designs. Utilize simulation-based power calculations to account for complex adaptive features.
Digital twin technology represents a paradigm shift in clinical trial design for neurological diseases. By creating patient-specific computational models that simulate disease progression and treatment response, researchers can generate more precise estimates of effect sizes and outcome variability—the two key parameters driving sample size requirements [92] [75]. The documented ability of digital twin approaches to accurately predict pathological status and clinical progression in Alzheimer's disease demonstrates their potential to substantially enhance trial efficiency [92].
Implementation of digital twin frameworks requires specialized expertise in computational modeling, neuroimaging, and clinical neurology. However, the potential benefits—including sample size reductions of 30-70%, enhanced statistical power, more efficient resource utilization, and accelerated therapeutic development—justify the necessary investment [92] [75]. As these technologies mature and validation evidence accumulates, digital twin-enhanced trial designs are poised to become standard practice in neurological drug development, particularly for complex, heterogeneous conditions where traditional approaches have struggled to demonstrate efficacy.
The regulatory acceptance of digital twin methodologies is evolving rapidly, with the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) establishing frameworks to evaluate these innovative tools in biomedical research and drug development. Digital twins—dynamic, virtual representations of physical objects or processes—are demonstrating significant potential to transform clinical trials for neurological diseases and other conditions by creating synthetic control arms, enhancing trial efficiency, and enabling more personalized treatment approaches. Recent initiatives, including a collaborative $6 million research program funded by the NSF, NIH, and FDA, underscore the growing institutional support for developing digital twins for therapeutic and clinical use [94]. Both regulatory bodies have signaled openness to these technologies, with the FDA releasing discussion papers on AI/ML in drug development and the EMA publishing a detailed workplan for data and AI in medicines regulation through 2028 [95] [96]. For researchers focusing on neurological disease progression, understanding the emerging qualification pathways and evidentiary standards for these computational models is critical for successful regulatory adoption.
Current Regulatory Positions and Qualification Frameworks
FDA Position and Qualification Pathway
The FDA has adopted a flexible, case-specific model for evaluating digital twin methodologies, emphasizing early engagement and collaborative development of evidentiary standards [97]. The agency's approach is exemplified by its seven-step risk-based framework for using AI in clinical trials, which provides sponsors with a structured pathway for implementation [98]:
- Step 1: Define the Question of Interest – Clearly articulate the trial's primary safety and efficacy objectives.
- Step 2: Define the Context of Use (COU) – Precisely specify the digital twin's role, such as generating prognostic covariates from baseline data to increase statistical power without altering trial conduct, endpoints, or eligibility [98].
- Step 3: Assess the AI Model Risk – Evaluate both statistical risks (e.g., Type I error inflation) and operational risks (e.g., data leakage). Methods like PROCOVA demonstrate that adding prognostic covariates to an ANCOVA analysis does not inflate Type I error rate while boosting power [98].
- Step 4: Develop a Plan to Establish Credibility – Pre-specify and lock the model architecture, hyperparameters, inputs, and outputs before trial commencement, ensuring determinism and reproducibility [98].
- Step 5: Execute the Plan – Generate prognostic covariates using the locked model through an automated, pre-specified pipeline with comprehensive quality checks and version control [98].
- Step 6: Document the Results – Compile a credibility assessment report including system logs, quality control artifacts, and audit trails showing data transformation from baseline inputs to prognostic covariates [98].
- Step 7: Determine Adequacy for COU – Validate that model application is adequate for its intended use at both population and individual levels, investigating and documenting any anomalies [98].
The FDA has demonstrated particular interest in digital twins as "catalyzers of biomedical innovation" and encourages sponsors to discuss proposed uses of digital twins as external control arms during the Investigational New Drug (IND) application stage [94] [96].
EMA Position and Qualification Pathway
The EMA has established a more structured, risk-tiered approach to digital twin regulation, integrating oversight into its broader framework for AI in medicines regulation [97]. Key aspects include:
- Risk-Based Classification: The EMA focuses on 'high patient risk' applications affecting safety and 'high regulatory impact' cases with substantial influence on regulatory decision-making [97].
- Prohibited Incremental Learning: Unlike the FDA's approach with locked models, the EMA explicitly prohibits incremental learning during clinical trials to ensure evidence integrity [97].
- Comprehensive Technical Requirements: The mandate includes traceable documentation of data acquisition and transformation, explicit assessment of data representativeness, and strategies to address class imbalances and potential discrimination [97].
- Preference for Interpretable Models: The EMA shows a clear preference for interpretable models but accepts black-box models when justified by superior performance, requiring explainability metrics and thorough documentation [97].
- Structured Engagement Pathways: The agency provides clear consultation pathways through its Innovation Task Force for experimental technology, Scientific Advice Working Party, and qualification procedures for novel methodologies [97].
The EMA's "AI Action Plan" includes a specific commitment to conduct technical deep dives into digital twin technology, emphasizing the value of real-world evidence in clinical decision-making, which aligns well with the construction of digital twins [95] [96].
Table 1: Comparative Analysis of FDA and EMA Digital Twin Regulatory Approaches
| Aspect | FDA Approach | EMA Approach |
|---|---|---|
| Overall Philosophy | Flexible, case-specific model [97] | Structured, risk-tiered approach [97] |
| Key Guidance Documents | AI/ML in Drug Development Discussion Papers [96] | AI Workplan to 2028, Reflection Paper on AI [95] [97] |
| Model Locking Requirements | Requires pre-specified, locked models before trial commencement [98] | Prohibits incremental learning during trials [97] |
| Preference in Modeling | Focus on statistical performance and error control [98] | Preference for interpretable models with explainability requirements [97] |
| Engagement Mechanism | Type C meetings, IND application discussions [98] [96] | Innovation Task Force, Scientific Advice Working Party [97] |
| Evidentiary Standards | Seven-step AI framework emphasizing reproducibility [98] | Comprehensive technical requirements focusing on data representativeness [97] |
Experimental Protocols for Digital Twin Qualification
Protocol for Establishing Analytical Validation
Objective: To verify that the digital twin computational model accurately represents the underlying mathematical framework and computational processes for neurological disease progression.
Materials and Reagents:
- High-performance computing cluster with containerization platform (Docker/Singularity)
- Version control system (Git)
- Continuous integration/continuous deployment (CI/CD) pipeline
- Numerical simulation software (MATLAB, Python with NumPy/SciPy)
- Reference neurological datasets with known ground truth (e.g., ADNI, PPMI)
Procedure:
- Code Verification: Implement unit tests for all model components to verify individual functions produce expected outputs for predefined inputs [99].
- Numerical Convergence Analysis: Perform mesh refinement studies for finite element models of brain structures to ensure solution stability [99].
- Software Quality Engineering: Establish comprehensive documentation, version control, and change management procedures following ISO 62304 standards for medical device software [99].
- Determinism Testing: Execute the digital twin pipeline multiple times with identical inputs to verify bitwise identical outputs, ensuring reproducibility [98].
- Boundary Condition Testing: Validate model behavior at operational extremes relevant to neurological applications (e.g., extreme biomarker values, edge case disease states) [99].
- Documentation: Generate a verification report tracing all requirements to test cases and results for regulatory submission [98].
Protocol for Clinical Validation in Neurological Disease Applications
Objective: To demonstrate that digital twin predictions accurately reflect real-world neurological disease progression and treatment responses.
Materials and Reagents:
- Curated historical clinical trial data for neurological conditions (e.g., Alzheimer's, Parkinson's, Multiple Sclerosis)
- Real-world evidence datasets from healthcare systems with diverse patient populations
- Statistical analysis software (R, Python pandas/statsmodels)
- Data harmonization tools (OMOP CDM, FHIR standards)
Procedure:
- Cohort Identification: Identify relevant patient cohorts from historical clinical trials and real-world data sources matching the target population for the neurological indication [15].
- Digital Twin Generation: Create digital twins for all patients in the validation cohort using only baseline characteristics, mirroring the intended clinical application [15] [96].
- Prognostic Accuracy Assessment: Compare digital twin-predicted disease progression trajectories against actual observed outcomes using concordance statistics, calibration curves, and mean squared error metrics [15].
- Treatment Effect Estimation: For interventional applications, compare digital twin-predicted treatment effects against observed treatment effects from randomized controlled trials [15].
- Subgroup Analysis: Assess predictive performance across relevant demographic and clinical subgroups to identify potential performance disparities [97].
- Uncertainty Quantification: Implement Bayesian methods or conformal prediction to establish confidence intervals for digital twin predictions [99].
- Documentation: Compile a validation report including performance metrics, subgroup analyses, and uncertainty quantification for regulatory submission [98].
Table 2: Research Reagent Solutions for Digital Twin Implementation
| Reagent/Category | Specific Examples | Function in Digital Twin Research |
|---|---|---|
| Data Resources | ADNI, PPMI, UK Biobank, OMOP CDM datasets | Provide real-world and clinical trial data for model training and validation [15] [100] |
| Computational Frameworks | TensorFlow, PyTorch, STAN, FEniCS | Enable development of AI and mechanistic models for disease progression [2] [99] |
| Simulation Platforms | OpenSim, Living Heart Project, NEURON | Provide validated multi-scale physiological models for component integration [2] [101] |
| Containerization Tools | Docker, Singularity, Kubernetes | Ensure computational reproducibility and environment consistency [98] [99] |
| Version Control Systems | Git, DVC, MLflow | Maintain model lineage, hyperparameters, and data versioning [98] |
| Uncertainty Quantification | PyMC3, TensorFlow Probability, UQLab | Enable Bayesian inference and uncertainty propagation [99] |
Application to Neurological Disease Progression Research
Specific Considerations for Neurological Applications
Digital twin applications in neurological disease progression research present unique opportunities and challenges. The complex pathophysiology of conditions like Alzheimer's disease, Parkinson's disease, and multiple sclerosis requires sophisticated multi-scale modeling approaches [100]. Successful regulatory qualification in this domain requires:
- Multi-Modal Data Integration: Incorporating diverse data types including neuroimaging (MRI, PET, fMRI), electrophysiology (EEG), genomics, proteomics, clinical assessments, and digital biomarkers from wearables [2] [101].
- Temporal Dynamics Modeling: Capturing the often non-linear progression patterns characteristic of neurodegenerative diseases through appropriate mathematical frameworks (e.g., differential equations, stochastic processes) [99].
- Blood-Brain Barrier Considerations: Accounting for drug penetration challenges specific to neurological therapies when simulating treatment effects [100].
- Functional Outcome Measures: Focusing on clinically relevant endpoints such as cognitive scores, motor function, and activities of daily living rather than purely biological parameters [15].
Recent studies have demonstrated the potential for digital twins to enhance randomized clinical trials for neurological conditions by improving ethical standards, enabling early detection of adverse events, and streamlining trial design through synthetic control arms [15]. The European Medicines Regulatory Network's focus on establishing shared understanding of methodologies including digital twin data positions this approach as increasingly relevant for neurological drug development [95].
Regulatory Strategy for Neurological Disease Applications
Developing a successful regulatory strategy for digital twin methodologies in neurological disease progression research requires addressing several key elements:
- Early Regulatory Engagement: Seek scientific advice from both FDA and EMA during the exploratory research phase to align on evidentiary requirements specific to neurological endpoints [97] [96].
- Model Transparency: Implement explainable AI techniques and mechanistic modeling approaches to enhance interpretability of predictions, particularly important for the complex pathophysiology of neurological disorders [99] [101].
- Prospective Validation: Design prospective observational studies specifically for validating digital twin predictions against natural history data for the target neurological condition [15].
- Computational Bill of Materials: Maintain a comprehensive "comp-BOM" documenting all data, software, and model components to facilitate regulatory review [98].
- Risk Management Approach: Implement a risk-based strategy focusing initial applications on lower-risk contexts such as trial enrichment before progressing to primary efficacy endpoints [97].
The regulatory landscape for digital twin methodologies is rapidly evolving, with both the FDA and EMA establishing frameworks to evaluate these innovative approaches. For researchers focused on neurological disease progression, successful regulatory qualification requires rigorous analytical and clinical validation, comprehensive uncertainty quantification, and early, continuous engagement with regulatory agencies. The differing philosophical approaches between the FDA's flexible model and EMA's structured framework necessitate tailored strategies for each jurisdiction. By implementing the protocols and considerations outlined in this document, researchers can position their digital twin methodologies for successful regulatory acceptance, potentially accelerating the development of effective treatments for complex neurological conditions.
The research and development of therapies for neurological diseases are at a pivotal juncture. Traditional clinical trial methodologies, while considered the gold standard for generating evidence, face significant challenges in the context of complex, progressive neurological disorders such as Alzheimer's disease, Parkinson's disease, and brain tumors. These challenges include extensive durations, high costs, recruitment difficulties, and ethical concerns in including control groups [15]. Digital Twin (DT) technology emerges as a transformative paradigm, offering a patient-specific, dynamic computational framework to simulate disease progression and treatment responses in silico [4] [11]. This analysis provides a comparative examination of digital twin approaches against traditional statistical and trial designs, detailing their application within neurological disease research and drug development.
Core Conceptual Comparison
Digital twins represent a fundamental shift from group-level, population-averaged statistical inferences to patient-specific, dynamic simulations. The table below summarizes the core conceptual differences between the two paradigms.
Table 1: Fundamental Paradigms of Traditional Trials vs. Digital Twins
| Aspect | Traditional Trial Designs | Digital Twin Approaches |
|---|---|---|
| Foundational Unit | Patient cohort or population [15] | Individual patient virtual replica [5] [102] |
| Temporal Resolution | Discrete timepoints (e.g., baseline, follow-up) [15] | Continuous, real-time updating via data streams [5] [11] |
| Control Mechanism | Concurrent randomized control group [15] | Synthetic control from individual's own predicted trajectory [15] [103] |
| Primary Objective | Establish average treatment effect for a population [15] | Predict individualized treatment effect and optimize therapy [4] [5] |
| Key Limitation | Limited generalizability to underrepresented subgroups [15] | Dependent on quality and representativeness of training data [15] |
Quantitative Performance and Outcome Comparison
Empirical evidence from initial applications demonstrates the potential of DT technology to enhance the efficiency and predictive power of clinical research. The following table compiles key quantitative findings from recent studies and trials.
Table 2: Quantitative Comparison of Trial Outcomes and Efficiency
| Metric | Traditional Trial Performance | Digital Twin Enhancement |
|---|---|---|
| Sample Size | Large cohorts required for statistical power [15] | Up to 15% overall reduction; control arm reduced by 20-33% [103] |
| Trial Power | Fixed at design stage; can be compromised by attrition | Up to 13% power boost demonstrated in retrospective analysis [103] |
| Procedural Outcomes | Standard catheter ablation for VT [15] | 60% shorter procedure time, 15% absolute increase in acute success [15] |
| Disease Prediction | Clinical symptom-based diagnosis [11] | 97.95% accuracy for Parkinson's, 92.52% feature recognition for brain tumors [11] |
| Chronic Disease Management | Standard care for Type 2 Diabetes [15] | 0.48% HbA1c reduction, improved mental distress scores [15] |
Application Notes and Experimental Protocols
Protocol 1: Generating a Digital Twin for a Neurological Disease Clinical Trial
This protocol outlines the methodology for creating and deploying AI-generated digital twins to enhance randomized controlled trials (RCTs) for neurological diseases, based on established frameworks [15] [103].
1. Objective: To create patient-specific digital twins for use as synthetic controls or for treatment response prediction, thereby increasing trial power and reducing required sample size.
2. Materials and Data Requirements:
- Data Sources: Historical longitudinal clinical trial data, disease registries, real-world evidence studies [103].
- Baseline Patient Data: Comprehensive baseline clinical information, including neuroimaging (MRI, fMRI, dMRI), genetic profiles, cerebrospinal fluid biomarkers, neuropsychological scores, and quality of life assessments [4] [103].
- Computational Infrastructure: High-performance computing resources capable of running deep learning models and simulations.
3. Workflow Diagram:
4. Step-wise Procedure:
- Step 1: Data Collection and Curation. Aggregate and harmonize high-quality, longitudinal historical data from completed clinical trials and observational studies relevant to the neurological condition of interest (e.g., Alzheimer's, Parkinson's). This data must include baseline covariates and longitudinal outcomes [15] [103].
- Step 2: Model Training. Train a deep learning model, often a Deep Neural Network (DNN) architecture, on the curated historical data. This model, termed a Digital Twin Generator (DTG), learns the probabilistic relationship between a patient's baseline state and their future disease trajectory across all relevant clinical endpoints (e.g., CDR-SB, ADAS-Cog for Alzheimer's) [103].
- Step 3: Digital Twin Generation. For each new patient enrolled in the clinical trial, input their baseline data into the trained DTG. The model generates a "digital twin" – a probabilistic forecast of the patient's future clinical trajectory in the absence of the experimental treatment [15] [103].
- Step 4: Trial Integration and Analysis.
- Synthetic Control Arm: In a single-arm trial, the ensemble of digital twins serves as the control group. The outcomes of the actual treated patients are compared against the predicted outcomes of their digital twins [15] [103].
- Augmented RCT: In a randomized trial, each patient in the control arm is paired with their digital twin. The analysis incorporates the twin's predicted trajectory to reduce variance and increase statistical power, allowing for sample size reduction [103].
- Step 5: Validation. Continuously validate the model's predictions against real-world control data from the ongoing trial, using techniques like SHapley Additive exPlanations (SHAP) for model interpretability [15].
Protocol 2: Building a Personalized Digital Twin of a Brain Tumor
This protocol describes the creation of a mechanistic digital twin for a brain tumor patient to simulate tumor dynamics and personalize treatment planning, based on neuroscience-specific applications like The Virtual Brain (TVB) platform [4] [11].
1. Objective: To develop a personalized computational model of a patient's brain and tumor to simulate the impact of the tumor on brain network dynamics and predict the outcomes of various therapeutic interventions.
2. Materials and Data Requirements:
- Imaging Data: Multi-modal MRI scans, including structural T1-weighted, functional MRI (fMRI), and diffusion MRI (dMRI) for structural connectivity [4].
- Clinical Data: Genomic analyses of tumor biopsy, neuropsychological assessment scores, and clinical outcomes data [4].
- Software Platform: A computational neuroscience platform such as The Virtual Brain (TVB) [4].
3. Workflow Diagram:
4. Step-wise Procedure:
- Step 1: Multi-modal Data Acquisition and Processing. Acquire high-resolution structural, functional, and diffusion MRI. Process the data to extract key features: from structural MRI, create a personalized brain mesh; from dMRI, reconstruct the structural connectome (white matter tracts); from fMRI, derive patterns of functional connectivity [4].
- Step 2: Model Personalization. Integrate the processed data into a computational platform like TVB. This involves mapping the individual's structural connectome to define the network architecture of the brain model. Model parameters are tuned so that the simulated neural activity matches the patient's empirical fMRI data [4].
- Step 3: Tumor Modeling. Incorporate the tumor's location, volume, and biological aggressiveness (inferred from imaging and genomics) into the personalized brain model. This can use physics-based equations (e.g., Fisher-Kolmogorov for simulating spread) to model how the tumor impacts and disrupts surrounding neural tissue and network dynamics [4] [11].
- Step 4: In-Silico Intervention and Simulation.
- Surgical Planning: Simulate the functional consequences of different surgical resection volumes on network dynamics to balance tumor removal with cognitive preservation [4].
- Radiotherapy Planning: Use the model to optimize radiation fields. Studies have shown this can increase tumor control or allow dose reductions of up to 16.7% while maintaining equivalent outcomes [11].
- Pharmacological Impact: Simulate the effect of drugs on brain network dynamics or tumor growth kinetics.
- Step 5: Clinical Validation and Iteration. Compare model predictions with actual post-intervention patient outcomes (e.g., post-surgical fMRI, tumor recurrence patterns). Use this feedback to iteratively refine and improve the accuracy of the digital twin for the specific patient [4].
The Scientist's Toolkit: Research Reagent Solutions
The development and application of digital twins in neurological research rely on a suite of computational tools, data sources, and software platforms.
Table 3: Essential Research Tools for Neurological Digital Twins
| Tool / Resource | Type | Primary Function in DT Research | Example Use Case |
|---|---|---|---|
| The Virtual Brain (TVB) | Software Platform | Whole-brain simulation platform for constructing personalized brain network models [4]. | Modeling the impact of a brain tumor or stroke on large-scale brain dynamics [4]. |
| Digital Twin Generator (DTG) | AI Model | A deep learning model trained on historical data to forecast individual patient disease trajectories [103]. | Creating synthetic control arms for Alzheimer's disease clinical trials [103]. |
| Multi-modal MRI Data | Data Input | Provides structural, functional, and connectivity information for model personalization [4]. | Deriving the structural connectome and informing model parameters for a brain DT [4]. |
| Longitudinal Clinical Data | Data Input | Provides ground-truth data on disease progression for model training and validation [15] [103]. | Training a DTG to predict scores on the CDR-SB in Alzheimer's disease [103]. |
| Wearable & Sensor Data | Data Input | Enables real-time, continuous updating of the digital twin with physiological data [5] [11]. | Monitoring heart rate, activity, and sleep in a POTS or Parkinson's DT [5] [11]. |
| SHAP (SHapley Additive exPlanations) | Analysis Library | Provides interpretability for AI models by quantifying the contribution of each input feature to the output [15]. | Understanding which baseline variables most influenced a DT's predicted prognosis [15]. |
Digital twin technology represents a profound methodological shift from traditional statistical and trial designs, moving from population-level inference to dynamic, patient-specific simulation and forecasting. In neurological disease research, this paradigm offers a powerful tool to overcome long-standing challenges related to heterogeneity, recruitment, and the high failure rate of therapeutic trials. While challenges in data integration, model validation, and computational scalability remain, the protocols and evidence outlined herein demonstrate the tangible potential of DTs to create more efficient, powerful, and personalized pathways for developing effective neurological treatments. The integration of digital twins into research protocols signifies a move towards a future where in-silico testing becomes a standard, indispensable component of the therapeutic development pipeline.
Assessing Generalizability and Limitations Across Diverse Patient Populations
Digital twin technology represents a transformative approach in neurological disease research, creating dynamic, virtual models of individual patients to predict disease progression and optimize therapeutic interventions [104] [2]. However, the promise of personalized medicine through digital twins is contingent on their generalizability across diverse patient populations [105]. Significant challenges persist in ensuring these models perform equitably across different ancestral backgrounds, socioeconomic statuses, and geographic locations [100] [106]. This application note systematically assesses the current limitations and validation strategies for digital twin models in neurological applications, providing researchers with structured frameworks to evaluate and enhance model generalizability during development and deployment phases.
Current Limitations in Population Generalizability
Quantitative Assessment of Performance Disparities
Table 1: Documented Performance Disparities in Neurological Digital Twin Models
| Model Domain | Performance in Majority Populations | Performance in Minority Populations | Performance Gap | Primary Contributing Factors |
|---|---|---|---|---|
| Alzheimer's Disease Prediction [107] | 97% accuracy, 96% F1 score (White participants) | Faster progression rates, higher variability (Black/African American participants) | Quantitative metrics not fully reported for subgroups | Underrepresentation in training data, heterogeneous risk factors |
| Genetic Risk Prediction (Standard PRS) [106] | Effective prediction in European ancestry | Poor generalization to minority populations | Significant decrease in AUC and R² values | Population structure bias in GWAS, overfitting to European genomes |
| Cross-Ancestry Genetic Prediction [108] | Maintained performance in European populations | Substantially improved prediction in non-European populations | Reduced performance disparity through specialized methods | Incorporation of diverse base genomes, Bayesian integration methods |
| Multimodal Deep Learning [104] | 85-95% claimed accuracy in homogeneous cohorts | 10-15% lower real-world performance in diverse settings | 10-15% performance reduction | Small, homogeneous training cohorts, limited external validation |
Root Causes of Generalizability Limitations
The observed disparities in digital twin performance across populations stem from interconnected technical and methodological challenges. Algorithmic bias represents a fundamental issue, where models trained predominantly on European ancestry populations capture population-specific correlations rather than biologically causal mechanisms [106]. This problem is exacerbated by inadequate representation in training data - most genomic studies and clinical trials significantly underrepresent minority populations despite their often higher disease burdens [107] [106].
The complexity of neurological diseases introduces additional challenges, as conditions like Alzheimer's disease involve multifaceted interactions among genetic, environmental, and social determinants that vary substantially across populations [105]. Data integration limitations further complicate model generalizability, as digital twins require harmonization of multimodal data sources (genomic, imaging, clinical, behavioral) that may have different quality and availability across healthcare settings [104] [102]. Finally, validation frameworks often prioritize internal validation over external testing in diverse real-world settings, creating an overoptimistic assessment of generalizability [104].
Experimental Protocols for Generalizability Assessment
Protocol 1: Multi-Ancestral Validation Framework for Alzheimer's Disease Digital Twins
This protocol provides a standardized methodology for evaluating the cross-population performance of digital twin models for Alzheimer's disease and related disorders.
Materials and Research Reagents
- National Alzheimer's Coordinating Center (NACC) Uniform Dataset: Contains longitudinal clinical, cognitive, and demographic data from multiple Alzheimer's disease research centers [107].
- Alzheimer's Disease Sequencing Project (ADSP) Data: Genomic sequencing data from diverse populations, accessible through dbGaP (accession numbers vary) [108].
- Multi-ancestral Genotype Data: Genome-wide association study (GWAS) summary statistics from European, African, East Asian, and admixed populations [106] [108].
- Computational Resources: High-performance computing environment with minimum 64GB RAM, 8-core processor, and 1TB storage for large-scale genomic analysis.
Procedure
- Cohort Stratification: Partition the study population into distinct subsets by genetically determined ancestry, race, and sex using standardized classification criteria [107].
- Model Training: Implement a multi-head deep learning architecture with early-fusion convolutional neural networks to process heterogeneous data modalities (time-series clinical data, cross-sectional assessments, MRI imaging data) [107].
- Feature Importance Analysis: Apply Shapley Additive Explanation (SHAP) algorithms to identify population-specific predictors of disease progression [107].
- Cross-Population Validation: Employ leave-one-population-out cross-validation, iteratively holding out each ancestral group as a test set while training on remaining populations [106].
- Performance Quantification: Calculate accuracy, F1 score, root mean square error, and area under the receiver operating characteristic curve separately for each population subgroup [107].
- Bias Assessment: Compare feature importance rankings and model calibration metrics across population subgroups to identify potential algorithmic biases [106].
Diagram 1: Multi-ancestral validation workflow
Protocol 2: Disentangled Representation Learning for Cross-Population Generalization
This protocol addresses the fundamental challenge of separating ancestry-specific effects from disease-relevant biological signals in digital twin models.
Materials and Research Reagents
- DisPred Framework: Deep learning-based disentangling autoencoder architecture for genomic data [106].
- Diverse Genomic Datasets: Integration of genomic data from multiple ancestral groups with associated phenotypic data [106] [108].
- High-Performance Computing Cluster: Specialized hardware with GPU acceleration for deep learning model training.
- Phenotype Validation Data: Clinical diagnostic information, cognitive assessment scores, and biomarker data (e.g., CSF Aβ42 levels, tau pathology) [108].
Procedure
- Data Preprocessing: Process genotype dosage data (values 0-2) from diverse populations, applying standard quality control and normalization procedures [106].
- Disentangled Autoencoder Implementation: Construct a deep learning autoencoder that separates latent representations into ancestry-specific (za) and phenotype-specific (zd) components using contrastive loss functions [106].
- Latent Space Optimization: Train the autoencoder to minimize reconstruction loss while enforcing similarity constraints in the latent space based on ancestry and disease status labels [106].
- Phenotype Prediction Model: Train a linear classifier on the disentangled phenotype-specific representations to predict disease status while minimizing ancestry-related confounding [106].
- Ensemble Model Construction: Combine predictions from the disentangled representation model with standard approaches to enhance overall performance [106].
- Cross-Ancestry Validation: Evaluate the model on held-out populations to assess generalizability compared to standard polygenic risk scores and conventional machine learning approaches [106] [108].
Diagram 2: Disentangled representation architecture
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Research Reagents and Computational Tools
| Research Reagent/Tool | Type | Primary Function | Application in Generalizability Research |
|---|---|---|---|
| DisPred Framework [106] | Deep Learning Architecture | Disentangles ancestry from phenotype-specific genetic representations | Creates more equitable models across populations by reducing ancestry-related confounding |
| Cross-ancestry PRS Models [108] | Bayesian Polygenic Risk Score | Integrates diverse GWAS datasets for improved risk prediction | Enhances genetic risk prediction accuracy in non-European populations for neurological disorders |
| β-Variational Autoencoders [109] | Generative Machine Learning Model | Creates digital twins that forecast clinical trajectories | Generates synthetic patient data for validating models across diverse clinical scenarios |
| National Alzheimer's Coordinating Center (NACC) Dataset [107] | Clinical/Imaging Data Repository | Provides multimodal, longitudinal data from multiple research centers | Enables validation of digital twins across diverse patient demographics and clinical presentations |
| SHAP (SHapley Additive Explanations) [107] | Model Interpretation Algorithm | Quantifies feature importance for model predictions | Identifies population-specific predictive features and potential algorithmic biases |
| Multi-head Convolutional Neural Networks [107] | Deep Learning Architecture | Processes heterogeneous data types with different dimensions and time steps | Enables integration of multimodal data (clinical, imaging, genetic) for comprehensive digital twins |
Ensuring the generalizability of digital twin models across diverse populations remains a critical challenge in neurological disease research. The protocols and frameworks presented in this application note provide methodological approaches to identify, quantify, and mitigate performance disparities across population subgroups. By implementing rigorous multi-ancestral validation, employing disentangled representation learning, and utilizing appropriate research reagents, researchers can enhance the equity and translational potential of digital twin technologies. Future work must prioritize the development of standardized benchmarking datasets representing global diversity and establish regulatory frameworks for evaluating algorithmic fairness in digital health technologies.
Conclusion
Digital twin technology represents a paradigm shift in modeling neurological disease progression, offering a powerful pathway to personalized, predictive medicine. Synthesizing the key intents, the foundational definition establishes a rigorous standard for what constitutes a true DT, moving beyond simple digital models. Methodological advances in AI and data integration are already demonstrating tangible benefits, from boosting clinical trial efficiency to enabling patient-specific treatment simulations. However, the journey from concept to clinic is fraught with challenges, including the critical need for robust validation, transparent models, and ethical frameworks. Looking forward, the successful integration of digital twins into mainstream neurology and drug development hinges on collaborative efforts to address these hurdles, standardize VVUQ processes, and generate compelling evidence of improved patient outcomes. The future of neurological care will increasingly be co-managed by clinicians and their patients' high-fidelity digital counterparts.
References
- 1. Exploring the concepts of digital twin, digital shadow, and ... [https://oxfordinsights.com/insights/exploring-the-concepts-of-digital-twin-digital-shadow-and-digital-model/]
- 2. Digital twins for health: a scoping review - Nature [https://www.nature.com/articles/s41746-024-01073-0]
- 3. Digital twin vs digital shadow vs digital model: key differences [https://www.flexcon.it/news-events/digital-twin-vs-digital-shadow-vs-digital-model/]
- 4. The digital twin in neuroscience: from theory to tailored therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC11457707/]
- 5. Digital twin framework for postural tachycardia syndrome ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1678955/full]
- 6. Difference Between Digital Twin, Digital Model, and ... [https://www.wizata.com/knowledge-base/difference-between-digital-twin-digital-model-and-digital-shadow]
- 7. AI models of the brain could serve as 'digital twins' in research [https://med.stanford.edu/news/all-news/2025/04/digital-twin.html]
- 8. Master Digital Twin Creation: Practical Guide for Beginners [https://www.simio.com/master-digital-twin-creation-practical-guide-for-beginners/]
- 9. A scoping review of human digital twins in healthcare ... [https://www.nature.com/articles/s41746-025-01910-w]
- 10. Digital twins for health: a scoping review - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC10960047/]
- 11. Digital twins in healthcare: a comprehensive review and ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1633539/full]
- 12. Using AI‐generated digital twins to boost clinical trial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12639399/]
- 13. Digital twins: Recent advances and future directions in ... [https://www.sciencedirect.com/science/article/pii/S2667305325000420]
- 14. Personalised Virtual Brain Twins: the Future of ... [https://www.ebrains.eu/news-and-events/personalised-virtual-brain-twins]
- 15. Enhancing randomized clinical trials with digital twins - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12494699/]
- 16. Cellular signaling pathways as plastic, proto-cognitive systems [https://pmc.ncbi.nlm.nih.gov/articles/PMC10201306/]
- 17. Review Brain-body physiology: Local, reflex, and central ... [https://www.sciencedirect.com/science/article/pii/S0092867424009796]
- 18. (Predictive, Personalized, Preventive, & Participatory)... P 4 Medicine [https://www.csescienceeditor.org/article/p4-medicine-predictive-personalized-preventive-participatory-catalyzing-a-revolution-from-reactive-to-proactive-medicine/]
- 19. of Application (Predictive, Preventive, Personalized, Participatory)... P 4 [https://pubmed.ncbi.nlm.nih.gov/35226650/]
- 20. 2025 NIH Alzheimer's Disease and Related Dementias ... [https://www.nia.nih.gov/about/2025-nih-dementia-research-progress-report]
- 21. Mass General Brigham Researchers Make Their 2025 ... [https://www.massgeneralbrigham.org/en/about/newsroom/articles/2025-predictions-about-neurology]
- 22. The Power of Digital Twins in Predicting Outcomes for ... [https://www.appliedclinicaltrialsonline.com/view/power-digital-twins-predicting-outcomes-clinical-trials]
- 23. Next-Generation Biosensor Technologies for Alzheimer's ... [https://www.sciencedirect.com/science/article/abs/pii/S1568163725003009]
- 24. Integrating Multi-Omics Data: Methods and Applications in ... [https://www.sciencedirect.com/science/article/pii/S2215017X25000657]
- 25. A technical review of multi-omics data integration methods [https://pubmed.ncbi.nlm.nih.gov/40748323/]
- 26. Reducing the acquisition time for magnetic resonance ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1507722/full]
- 27. Optimizing the early diagnosis of neurological disorders ... [https://www.nature.com/articles/s41598-025-05888-z]
- 28. Wearable devices in neurological disorders - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12432666/]
- 29. Advancements in Electronic Medical Records for Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC12071135/]
- 30. Challenges and Recommendations for Electronic Health ... [https://www.jmir.org/2025/1/e73987]
- 31. Machine learning for comprehensive forecasting of ... [https://www.nature.com/articles/s41598-019-49656-2]
- 32. What Are Foundation Models? [https://www.ibm.com/think/topics/foundation-models]
- 33. Foundation model [https://en.wikipedia.org/wiki/Foundation_model]
- 34. What are Foundation Models? - Generative AI [https://aws.amazon.com/what-is/foundation-models/]
- 35. Conditional Restricted Boltzmann Machines for Structured ... [https://arxiv.org/abs/1202.3748]
- 36. Foundation model of neural activity predicts response to ... [https://www.nature.com/articles/s41586-025-08829-y]
- 37. A Multiscale Integrated Approach to the Study of ... [https://www.mdpi.com/3042-8807/1/1/2]
- 38. A Technological Review of Digital Twins and Artificial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12294331/]
- 39. A Tale of Two Approaches: Physics-Based vs. Data-Driven ... [https://jpt.spe.org/a-tale-of-two-approaches-physics-based-vs-data-driven-models]
- 40. Physics-Based Versus Data-Driven Models [https://www.monolithai.com/blog/physics-based-models-vs-data-driven-models]
- 41. Harnessing artificial intelligence for brain disease: advances ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12336123/]
- 42. Combining physics-based and data-driven modeling for ... [https://www.sciencedirect.com/science/article/pii/S0306261925005835]
- 43. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 44. Biomarkers for Managing Neurodegenerative Diseases - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11048498/]
- 45. Probabilistic disease to characterize... progression modeling [https://pubmed.ncbi.nlm.nih.gov/29079521/]
- 46. Balancing practicality and complexity in neuroimaging models of... [https://www.nature.com/articles/s41531-025-01125-6?error=cookies_not_supported&code=1172a733-2af6-4331-8112-fadb493511ce]
- 47. Older Adults with Parkinson's Disease Have Increased ... [https://www.aging-us.com/news-room/older-adults-with-parkinsons-disease-have-increased-brain-amyloid-without-dementia]
- 48. Enhancing randomized clinical trials with digital twins [https://www.nature.com/articles/s41540-025-00592-0]
- 49. CTTI Recommendations: Disease Progression Modeling [https://ctti-clinicaltrials.org/about/ctti-projects/disease-progression-modeling/ctti-recommendations-disease-progression-modeling/]
- 50. What Is Disease Progression Modeling And When Is The ... [https://www.clinicalleader.com/doc/what-is-disease-progression-modeling-and-when-is-the-right-time-to-use-it-0001]
- 51. Multi-objective optimization formulation for Alzheimer's ... [https://www.sciencedirect.com/science/article/pii/S1532046425001844]
- 52. The Best 15 Minutes You'll Spend on Clinical Trials Today [https://www.unlearn.ai/blog/the-best-15-minutes-youll-spend-on-clinical-trials-today]
- 53. Enhancing Longitudinal Clinical Trial Efficiency with Digital ... [https://arxiv.org/html/2404.17576v1]
- 54. Personalized Treatment of Glioblastoma: Current State and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10296009/]
- 55. Digital twin framework for postural tachycardia syndrome ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549292/]
- 56. Integrating Disparate Data Sources: Challenges and ... [https://dualitytech.com/blog/integrating-disparate-data-sources/]
- 57. How to Integrate Data from Multiple Sources [https://www.oracle.com/analytics/integrating-data-multiple-data-sources/]
- 58. Explainable machine learning for predicting conversion to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11057348/]
- 59. Interpretable vs. Post-Hoc Explained Models for Digital ... [https://www.sciencedirect.com/science/article/pii/S1877050925034039]
- 60. What the Future Holds for Clinical Trials as AI and Digital ... [https://www.appliedclinicaltrialsonline.com/view/future-clinical-trials-ai-digital-twins-embedded]
- 61. AI Based Clinical Decision-Making Tool for Neurologists in the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12429661/]
- 62. An integrated predictive model for Alzheimer's disease ... [https://www.nature.com/articles/s41598-025-13478-2]
- 63. Revolutionizing Neurology: The Role of Artificial Intelligence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11224934/]
- 64. AI Bias in Healthcare: What Every C-Suite Needs to Know ... [https://www.baytechconsulting.com/blog/ai-bias-healthcare-risk-2025]
- 65. Algorithmic bias in public health AI: a silent threat to equity in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325396/]
- 66. AI-driven healthcare: A review on ensuring fairness and ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000864]
- 67. New HIPAA Regulations in 2025 [https://www.hipaajournal.com/new-hipaa-regulations/]
- 68. Updates to U.S. Health-Data Privacy and Wearable Tech [https://www.coblentzlaw.com/news/updates-to-u-s-health-data-privacy-and-wearable-tech/]
- 69. Data privacy in healthcare: Global challenges and solutions [https://pmc.ncbi.nlm.nih.gov/articles/PMC12138216/]
- 70. Verification, Validation and Uncertainty Quantification ... [https://www.asme.org/codes-standards/publications-information/verification-validation-uncertainty]
- 71. Verification, Validation, & Uncertainty Quantification (VVUQ) [https://smartuq.com/resources/uncertainty-quantification/]
- 72. Toward precision medicine using a “digital twin” approach [https://www.nature.com/articles/s41598-023-43618-5]
- 73. An interpretable Bayesian framework for Alzheimer's ... [https://pubmed.ncbi.nlm.nih.gov/41106661/]
- 74. An interpretable Bayesian framework for Alzheimer's ... [https://www.sciencedirect.com/science/article/abs/pii/S0306452225010139]
- 75. Digital twins as global learning health and disease models for ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-025-01435-7]
- 76. a randomised clinical trial using digital twin technology [https://www.nature.com/articles/s41746-025-01679-y]
- 77. Digital Twin Technology: The Future of Predicting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8807511/]
- 78. Digital Twin Cognition: AI-Biomarker Integration in ... [https://www.mdpi.com/2313-7673/10/10/640]
- 79. Large language models forecast patient health trajectories ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12488890/]
- 80. TrialBench: Multi-Modal AI-Ready Datasets for Clinical ... [https://www.nature.com/articles/s41597-025-05680-8]
- 81. A Deep Learning Approach for Enhancing Pandemic ... [https://www.sciencedirect.com/science/article/pii/S1755436525000532]
- 82. Digital twin for personalized medicine development - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC12369496/]
- 83. Independent validation and outlier analysis of EuroPOND ... [https://alzres.biomedcentral.com/articles/10.1186/s13195-025-01788-6]
- 84. Identification of clinical disease trajectories in ... [https://www.nature.com/articles/s41591-024-02843-9]
- 85. Development and validation of a model to predict ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288498/]
- 86. A real-world clinical validation for AI-based MRI monitoring ... [https://www.nature.com/articles/s41746-023-00940-6]
- 87. Analytical and clinical validation of a high accuracy fully ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1568971/full]
- 88. Digital twins for noninvasively measuring predictive ... [https://www.nature.com/articles/s41746-025-01920-8]
- 89. Sample size, power and effect size revisited - PMC - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC7745163/]
- 90. Impact of Sample Size and Its Estimation in Medical ... [https://www.sciencedirect.com/science/article/pii/S2773065425001397]
- 91. Sample size estimation and power analysis for clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3409926/]
- 92. Digital twins and non-invasive recordings enable early ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125947/]
- 93. Does increasing significance level increase power? [https://www.statsig.com/perspectives/increasing-significance-level-power]
- 94. NSF, NIH and FDA support research in digital twin ... [https://www.nsf.gov/news/nsf-nih-fda-support-research-digital-twin-technology]
- 95. Leveraging the power of data for public and animal health [https://www.ema.europa.eu/en/news/leveraging-power-data-public-animal-health]
- 96. A New Regulatory Road in Clinical Trials: Digital Twins [https://www.appliedclinicaltrialsonline.com/view/new-regulatory-road-clinical-trials-digital-twins]
- 97. The future of AI regulation in drug development: a comparative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12598624/]
- 98. How Unlearn Boosts Trial Power Using the FDA's AI ... [https://www.unlearn.ai/blog/how-unlearn-boosts-trial-power-using-the-fdas-ai-framework]
- 99. Survey and perspective on verification, validation, and ... [https://www.nature.com/articles/s41746-025-01447-y]
- 100. Digital twins as global learning health and disease models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11806862/]
- 101. The Virtual You | Department of Medicine News [https://med.stanford.edu/medicine/news/current-news/standard-news/medical-digital-twins.html]
- 102. Digital Twins for Personalized Medicine Require ... [https://www.jmir.org/2025/1/e72411]
- 103. Utility of Digital Twin AI-Generated Models to Improve ... [https://www.neurologylive.com/view/utility-digital-twin-ai-generated-models-improve-patient-selection-alzheimer-trials]
- 104. Digital Twin Cognition: AI-Biomarker Integration in Biomimetic Neuropsychology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561581/]
- 105. Challenges and opportunities for digital twins in precision ... [https://www.nature.com/articles/s41746-024-01402-3]
- 106. Improving genetic risk prediction across diverse population ... [https://www.nature.com/articles/s42003-023-05352-6]
- 107. Prediction and clustering of Alzheimer's disease by race ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11535522/]
- 108. Cross-Ancestry Polygenic Risk Scores Enhance ... [https://www.medrxiv.org/content/10.1101/2025.10.03.25337285v1]
- 109. A Digital Twins Machine Learning Model for Forecasting Disease Progression in Stroke Patients [https://www.mdpi.com/2076-3417/11/12/5576]