Deep Brain Stimulation Parameter Optimization: From Foundational Principles to AI-Driven Future
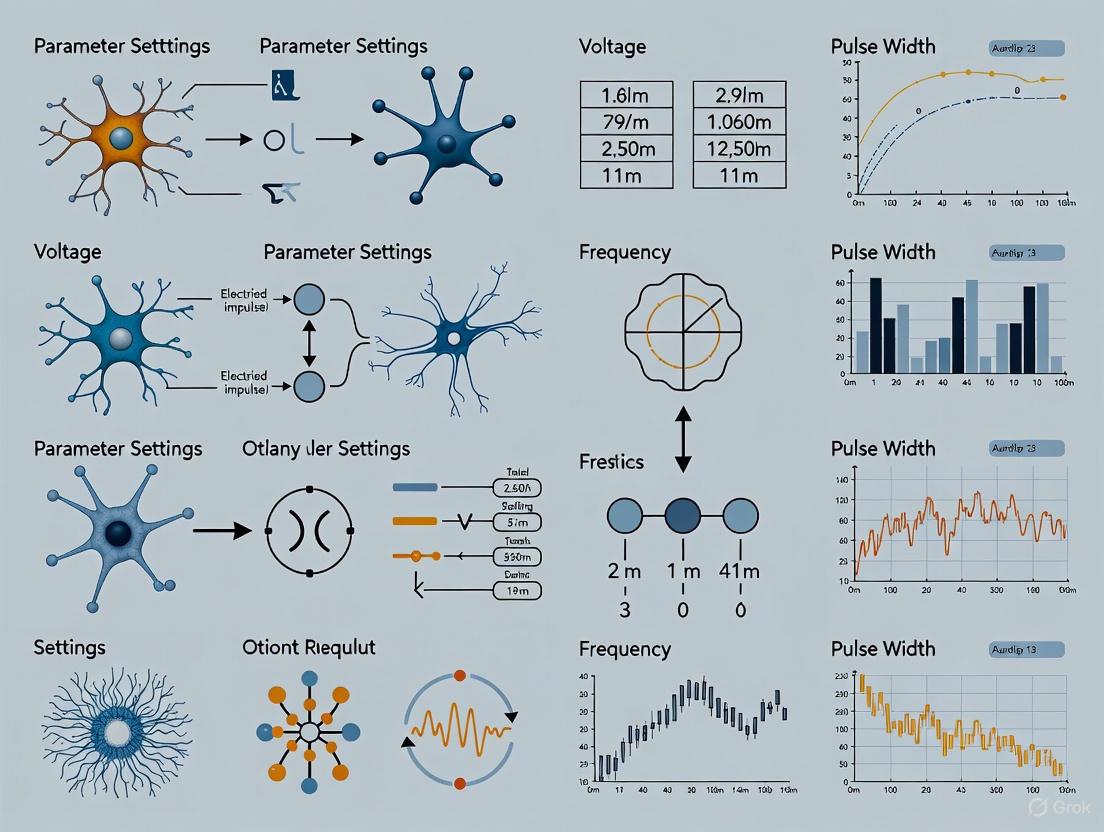
This article provides a comprehensive analysis of deep brain stimulation (DBS) parameter settings, addressing the critical needs of researchers and clinical scientists.
Deep Brain Stimulation Parameter Optimization: From Foundational Principles to AI-Driven Future
Abstract
This article provides a comprehensive analysis of deep brain stimulation (DBS) parameter settings, addressing the critical needs of researchers and clinical scientists. It explores the foundational principles of neural circuit engagement and ethical considerations in trial design. The content details cutting-edge methodological advances, including geometry-based algorithms, MRI-guided programming, and adaptive closed-loop systems. It further examines troubleshooting paradigms for suboptimal outcomes and comparative validation of novel approaches against standard care. By synthesizing evidence across neurological and psychiatric indications, this review aims to bridge computational innovation with clinically viable optimization strategies for personalized neuromodulation.
The Fundamentals of DBS: Targeting Circuit Dysfunction and Establishing Ethical Frameworks
The efficacy of neuromodulation therapies, such as deep brain stimulation (DBS), hinges on a multi-scale understanding of neural mechanisms. These mechanisms range from the modulation of single ion channels to the emergent dynamics of entire neural networks [1] [2]. In the context of DBS, precise parameter settings are critical for maximizing therapeutic benefit while minimizing side-effects. However, the optimization of these parameters remains a significant clinical challenge due to the vast possible combination of settings and the dynamic, patient-specific nature of neural tissue [3]. This document provides detailed application notes and experimental protocols, framed within DBS research, to guide the investigation of these neural mechanisms. It is intended for researchers, scientists, and drug development professionals seeking to bridge foundational neurobiology with clinical application, and includes structured data, methodologies, and visualization tools to support this work.
Core Neurobiological Mechanisms
Ion Channel Modulation in the Axon
The axon is a critical locus for neuromodulation, where G-protein coupled receptors (GPCRs) activate intracellular signaling cascades that directly modify ion channel properties [1]. This modulation profoundly impacts action potential (AP) initiation, propagation, and, ultimately, neurotransmitter release.
Key Modulatory Mechanisms include:
- Dopaminergic Modulation: Dopamine, acting through D3 receptors, hyperpolarizes the voltage-dependent steady-state inactivation of CaV3.2 channels in the axon initial segment (AIS). This reduces the availability of these calcium channels, which typically contribute to subthreshold depolarization and high-frequency AP bursts, thereby decreasing neuronal burstiness [1].
- Cholinergic Modulation: In contrast, acetylcholine hyperpolarizes the voltage-dependent activation of AIS-localized CaV3.2 channels. This increases basal calcium levels at the AIS, which in turn reduces calcium-sensitive KV7 potassium current. The net effect is a lower threshold for AP initiation [1].
- Serotonergic Modulation: Serotonin, via 5-HT1A receptors, can suppress HCN channels in the AIS through Gi/o-mediated inhibition of cyclic AMP. This leads to a hyperpolarization of the resting membrane potential and the AP threshold. Serotonin can also inhibit sodium channel current density, preferentially affecting NaV1.2 subtypes in the cortex [1].
The following table summarizes the effects of different neuromodulators on axonal ion channels:
Table 1: Neuromodulator Effects on Axonal Ion Channels
| Neuromodulator | Receptor | Primary Ion Channel Target | Biophysical Effect | Net Functional Outcome |
|---|---|---|---|---|
| Dopamine | D3 | CaV3.2 | Hyperpolarizes steady-state inactivation | Reduced burst firing [1] |
| Acetylcholine | Not Specified | CaV3.2 | Hyperpolarizes voltage-dependent activation | Lowered AP initiation threshold [1] |
| Serotonin | 5-HT1A | HCN | Suppresses channel function via ↓cAMP | Hyperpolarized RMP and AP threshold [1] |
| Serotonin | 5-HT1A | NaV1.2 | Reduces sodium current density | Reduced excitability [1] |
Network-Level Dynamics: Attractor Landscapes in Decision and Memory
Cognitive functions like decision-making (DM) and working memory (WM) are supported by the dynamics of attractor networks in areas such as the prefrontal and parietal cortices [4]. In this framework, stable patterns of neural activity (attractors) represent distinct decisions or memory items.
Circuit Architecture and Cognitive Function:
- Selective Inhibition: Recent evidence indicates that inhibitory neurons form functional subnetworks that are selective to specific stimuli, similar to excitatory populations. Circuits with this selective inhibition architecture exhibit stronger resting states, which improves the accuracy of DM by reducing spontaneous transitions between attractor states [4].
- Robustness-Flexibility Trade-off: While selective inhibition improves DM accuracy, it can result in weaker decision states, making WM representations more vulnerable to distracting stimuli. This highlights a fundamental trade-off between the robustness of WM and the flexibility/accuracy of DM [4].
- Temporal Gating via Non-Selective Input: Presenting a ramping, non-selective input during the delay period of a DM task can act as a temporal gating mechanism. This input stabilizes the active WM representation against distractors with a minimal increase in total thermodynamic cost compared to a constant non-selective input [4].
The diagram below illustrates the core concepts of the attractor network model for decision-making and working memory.
Network Architecture for Decision-Making
Application Notes: Quantifying Neuromodulation for DBS
Quantitative Assessment of DBS Parameter Efficacy
Optimizing DBS parameters is a central challenge in neuromodulation. The following table summarizes key quantitative findings from recent research on stimulation parameters for different targets, illustrating the effect of parameter selection on therapeutic outcomes.
Table 2: Quantitative Outcomes of Deep Brain Stimulation Parameters
| DBS Target | Stimulation Parameters | Key Efficacy Metric | Reported Outcome | Source |
|---|---|---|---|---|
| Anterior Thalamic Nuclei (ANT) for Epilepsy | iHFS: 145 Hz, 90 μs, 1 min on/5 min off (SANTE protocol) | Median Seizure Frequency Reduction | 33% reduction (IQR = 0-65) [5] | |
| Anterior Thalamic Nuclei (ANT) for Epilepsy | cLFS: 7 Hz, 200 μs, continuous | Median Seizure Frequency Reduction | 73% reduction (IQR = 30-79) [5] | |
| Subthalamic Nucleus (STN) for Parkinson's | Automated programming based on electrode location | Change in Clinical Outcome | Non-inferior to expert programming in blinded trial [3] | |
| General DBS Targets | Local Field Potential (LFP) beta power (13-35 Hz) | Correlation with Motor Impairment | Used as biomarker for adaptive and automated DBS [3] |
The Scientist's Toolkit: Essential Reagents and Materials
This section lists key tools and reagents for investigating neural mechanisms and developing neuromodulation therapies.
Table 3: Research Reagent Solutions for Neuromodulation Studies
| Item/Category | Function/Application | Specific Examples / Notes |
|---|---|---|
| Sharp Microelectrodes | Intracellular recording of membrane potential and AP dynamics in single neurons. | 3 M KCl-filled electrodes for recording spontaneous tonic spiking [6]. |
| CW-NIR Laser System | Non-invasive optical stimulation to modulate neuronal excitability and study thermal effects on ion channels. | Diode laser, 830 nm wavelength, 90 mW output power; used for sustained and activity-dependent stimulation [6]. |
| Programmable DBS Systems | Precisely control electrical stimulation parameters in clinical or pre-clinical research. | Systems with independent current control for high-resolution DBS [3]. |
| Local Field Potential (LFP) Recording | Capture aggregate neural population activity to identify biomarkers for disease state and stimulation efficacy. | Beta band (13-35 Hz) power in subthalamic nucleus correlates with Parkinsonian motor symptoms [3]. |
| Computational Modeling Software | Simulate neural dynamics from ion channels to network attractors; test algorithms for automated DBS. | Used for mean-field models of attractor networks and biophysical models of neuronal polarization [4] [2]. |
| Wearable Kinematic Sensors | Objective, continuous measurement of motor symptoms (tremor, bradykinesia) for outcome assessment. | Accelerometer-based wristwatches; used to automate DBS programming [3]. |
Experimental Protocols
Protocol: Intracellular Recording During Optical Neuromodulation
This protocol details the methodology for quantifying the effects of continuous-wave near-infrared (CW-NIR) laser illumination on single neuron dynamics [6].
1. Preparation and Setup
- Animal Model: Use the isolated central nervous system of Lymnaea stagnalis. Select the Right Parietal Ganglion (RPG) for its large, spontaneously active neurons.
- Solution: Prepare saline solution (in mM: 51.3 NaCl, 1.7 KCl, 1.5 MgCl₂·6H₂O, 4.1 CaCl₂·2H₂O, 5 HEPES, pH 7.8 with NaOH).
- Dissection: Isolate the neural system and remove the sheath above the ganglia using protease (Sigma type XIV) to facilitate electrode access.
2. Instrumentation and Calibration
- Recording: Use sharp electrodes filled with 3 M KCl. Acquire membrane potential recordings at 10 kHz using a DC amplifier and an A/D board.
- Temperature Calibration: Employ the open-pipette method. Calibrate the relationship between electrode resistance and temperature in the solution using a thermistor to estimate laser-induced temperature changes.
3. Stimulation Paradigms
- Sustained Stimulation: Deliver CW-NIR laser illumination (830 nm wavelength, ~90 mW, power density ~146 W/cm²) for periods exceeding 1 minute.
- Activity-Dependent (Closed-Loop) Stimulation: Use open-source RTXI software to trigger transient laser illumination (e.g., 500 ms duration) based on real-time detection of specific neural events, such as action potentials.
4. Data Analysis
- Spike Waveform Characterization: For each detected action potential, calculate the following metrics:
- Duration (at half-width)
- Amplitude (min to max voltage)
- Depolarization slope (1 ms around half-width point pre-peak)
- Repolarization slope (1 ms around half-width point post-peak)
- Statistical Comparison: Compare the distributions of these metrics during pre-stimulation, stimulation, and post-stimulation periods to quantify CW-NIR effects.
The workflow for this protocol is visualized below.
Optical Neuromodulation Experimental Workflow
Protocol: Two-Choice Operant Assay for Social vs. Nonsocial Reward
This behavioral protocol is used to investigate the neural circuits underlying reward-seeking behavior and can be adapted to study the effects of neuromodulation on decision-making [7].
1. Apparatus Assembly
- Chamber: Construct an acrylic chamber with two reward access zones on opposite sides.
- Choice Ports: Drill two 1-inch circular holes on one wall for nose-poke ports. Install infrared sensors to detect entries.
- Reward Ports:
- Sucrose Reward: Drill a 1-inch circle on an adjacent wall for a sucrose delivery port.
- Social Reward: On the opposite wall, cut a 2" x 2" square for social target access. Cover this with an automated gate (e.g., an aluminum sheet attached to a motorized camera slider or linear actuator controlled by an Arduino Uno).
2. Behavioral Training
- Habituation: Acclimate mice to the operant chamber.
- Shaping: Train mice to perform a nosepoke response to earn rewards.
- Sucrose Reward: Deliver a liquid sucrose solution.
- Social Reward: Open the social gate to provide temporary access to a conspecific mouse upon a correct nosepoke.
- Two-Choice Task: Present both reward options concurrently. The mouse's choice (nosepoke in the corresponding port) determines the reward delivered.
3. Combining with Neural Manipulations
- Neural Recording: Implant electrodes or optical fibers to record/manipulate activity in target brain regions (e.g., Medial Amygdala, Ventral Tegmental Area) during the task.
- Data Correlation: Analyze neural activity patterns during the choice phase, reward anticipation, and reward consumption for social versus nonsocial rewards.
Visualization of Neuromodulatory Pathways
The following diagram summarizes the GPCR-mediated signaling pathways that modulate ion channels in the axon initial segment, as described in Section 2.1.
GPCR Modulation of Axonal Ion Channels
Deep brain stimulation (DBS) has evolved from an empirical treatment to a network-level therapy grounded in circuit-based targeting. This approach recognizes that neurological and neuropsychiatric diseases arise from distributed network dysfunction rather than isolated pathology in single brain regions [8]. The fundamental principle of circuit-based targeting is that specific symptoms and disease manifestations map onto distinct, though often overlapping, neural circuits. By identifying and modulating critical nodes within these pathological networks, DBS can restore more normal neural dynamics and alleviate symptoms [8] [9]. This paradigm shift has been driven by growing understanding of brain network organization and the recognition that traditional single-target approaches may be insufficient for diseases with distributed circuitry.
The transition to circuit-based frameworks represents a significant advancement in neuromodulation, enabling more precise targeting of the neural substrates underlying specific pathological states. This approach requires integration of neuroimaging, electrophysiology, and clinical data to identify optimal stimulation targets for each patient's symptom profile. The following sections detail the specific circuit-pathology relationships, quantitative evidence, methodological protocols, and technical tools that form the foundation of modern circuit-based DBS.
Disease-Specific Circuit Pathologies and Target Relationships
Table 1: Circuit-Based Targets for Specific Pathologies and Symptoms
| Disease | Primary Symptoms/Circuits | Established DBS Targets | Emerging/Multi-Target Approaches |
|---|---|---|---|
| Parkinson's Disease | Akinesia, rigidity, tremor [9] | STN, GPi [9] | Dual-target (STN+GPi) for gait [8] |
| Dystonia | Abnormal postures, sustained muscle contractions [9] | GPi [9] | STN for cervical dystonia [9] |
| Essential Tremor | Action tremor [9] | Vim [9] | Posterior subthalamic area [9] |
| Obsessive-Compulsive Disorder | Compulsions, anxiety [8] | ALIC, VC/VS [10] [11] | BNST, STN, individualized targets [11] |
| Treatment-Resistant Depression | Anhedonia, depressed mood [8] [11] | SCC, SLF-MFB [11] | Individualized circuits based on biomarkers [11] [12] |
| Chronic Pain | Nociceptive, neuropathic pain [8] [12] | VC/VS, SCC [8] | Personalized cortico-striatal-thalamocortical targets [12] |
Table 2: Quantitative Outcomes for Circuit-Based DBS Approaches
| Disease | Intervention | Clinical Outcome Measure | Improvement | Evidence Level |
|---|---|---|---|---|
| Parkinson's Disease | STN-DBS | UPDRS-III motor score | 50.5% reduction [9] | Meta-analysis |
| Parkinson's Disease | GPi-DBS | UPDRS-III motor score | 29.8% reduction [9] | Meta-analysis |
| Dystonia | GPi-DBS | Burke-Fahn-Marsden Motor Score | 60.6% improvement [9] | Meta-analysis |
| Essential Tremor | Unilateral Vim-DBS | Tremor rating scales | 53-63% reduction [9] | Systematic review |
| Essential Tremor | Bilateral Vim-DBS | Tremor rating scales | 66-78% reduction [9] | Systematic review |
| Essential Tremor | PSA-DBS | Tremor rating scales | 64-89% reduction [9] | Clinical trial |
| OCD | ALIC-DBS with optimized targeting | Yale-Brown OCD Scale | Correlation with evoked potential amplitude [13] | Clinical study |
Experimental Protocols for Circuit-Based Target Engagement
Protocol: Intraoperative Evoked Potential Mapping for Target Optimization
Application: Refining DBS lead placement in the anterior limb of the internal capsule (ALIC) for obsessive-compulsive disorder [13].
Materials and Equipment:
- DBS macroelectrode (e.g., Medtronic 3387/3389, Abbott 6172)
- Electroencephalography system with forehead electrodes
- Neurophysiological recording system
- Stereotactic surgical frame
- Probabilistic tractography data from preoperative diffusion MRI
Procedure:
- After initial DBS lead placement using standard stereotactic coordinates, deliver monopolar stimulation through each electrode contact at 2Hz with predefined current amplitude.
- Record EEG evoked potentials (EPs) from forehead electrodes with sampling rate ≥1000Hz.
- Average EEG responses across 50-100 stimulation pulses to improve signal-to-noise ratio.
- Analyze EP waveforms for consistent oscillatory peaks at ~35ms, ~75ms, and ~120ms latencies.
- Calculate EP amplitude for each stimulation contact and correlate with tractography-defined target engagement.
- Verify that contacts producing highest EP amplitudes align with maximal white matter connectivity to ventromedial prefrontal cortex/orbitofrontal cortex.
- Finalize lead position to optimize EP characteristics before securing the electrode.
Validation: Treatment nonresponders exhibit less consistent EP waveforms across contacts, supporting the predictive validity of this biomarker [13].
Protocol: Personalized Biomarker Identification for Closed-Loop DBS
Application: Developing patient-specific biomarkers for adaptive DBS in chronic pain and neuropsychiatric disorders [12].
Materials and Equipment:
- Implantable DBS system with sensing capability (e.g., Medtronic Percept, Summit RC+S)
- Ambulatory symptom logging device (smartphone app or dedicated device)
- Signal processing software (MATLAB, Python with MNE, FieldTrip)
- Machine learning frameworks (scikit-learn, TensorFlow, PyTorch)
Procedure:
- Inpatient Brain Mapping Phase: Conduct intensive monitoring over 5-10 days with simultaneous intracranial EEG recording and patient-reported symptom metrics.
- Feature Extraction: Calculate spectral power features (beta, gamma, theta bands) from local field potentials across multiple brain regions.
- Biomarker Discovery: Apply machine learning algorithms (e.g., support vector machines, random forests) to identify neural features that correlate with symptom severity states.
- Model Validation: Use cross-validation to test generalizability of biomarker-symptom relationships across different time periods and conditions.
- Algorithm Development: Program closed-loop DBS system to respond to identified biomarker thresholds with appropriate stimulation parameter adjustments.
- Ambulatory Validation: Test biomarker performance in home environment with continuous neural recording and ecological momentary assessments.
- Iterative Refinement: Adjust biomarker detection parameters based on real-world performance and side effect profiles.
Implementation: For chronic pain, this approach has successfully identified personalized biomarkers in cortico-striatal-thalamocortical pathways that predict pain states and enable effective closed-loop stimulation [12].
Protocol: Geometry-Based DBS Programming Optimization
Application: Data-efficient optimization of DBS parameters for Parkinson's disease using anatomical imaging [14].
Materials and Equipment:
- Preoperative and postoperative MRI scans (T1-weighted, T2-weighted)
- Lead reconstruction software (Lead-DBS)
- Electric field simulation platform (OSS-DBS)
- Clinical evaluation records of initial stimulation testing
Procedure:
- Image Processing: Coregister preoperative and postoperative MRI scans using SPM or ANTs algorithms in Lead-DBS toolbox.
- Electrode Reconstruction: Manually reconstruct DBS electrode trajectory and contact positions in normalized space.
- Target Definition: Identify motor subregion of STN using DISTAL atlas or manual segmentation.
- Contact Selection: Calculate geometry score for each contact based on:
- Euclidean distance to motor STN centroid
- Rotation angle between contact and centroid relative to electrode axis
- Rank and combine these metrics to identify optimal contacts
- Current Selection: Simulate Volume of Tissue Activated (VTA) for candidate contacts using OSS-DBS with varying current amplitudes.
- Optimization: Select stimulation parameters that maximize VTA overlap with target structure while minimizing leakage to adjacent regions.
- Clinical Integration: Optionally incorporate existing clinical review data to fine-tune selection and avoid contacts associated with side effects.
Validation: This approach demonstrates significantly better target coverage (p < 5e-13) and reduced electric field leakage (p < 2e-10) compared to expert manual programming [14].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Circuit-Based DBS Investigations
| Tool/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| DBS Platforms with Sensing | Medtronic Percept PC, Abbott Infinity, Summit RC+S [15] [12] | Chronic neural recording & adaptive stimulation | Simultaneous stimulation and local field potential recording |
| Computational Modeling | Lead-DBS, OSS-DBS, StimVision [14] | Electrode reconstruction & VTA modeling | Predicting stimulation field spread and target engagement |
| Neuroimaging | Diffusion MRI tractography, fMRI, 3T/1.5T MRI [13] [14] | Target identification & connectivity analysis | Visualizing structural and functional connectivity of targets |
| Electrophysiology Analysis | Local field potential biomarkers, beta power, evoked potentials [13] [15] | Biomarker discovery & closed-loop control | Providing feedback signals for adaptive stimulation |
| Machine Learning Frameworks | Support vector machines, random forests, deep learning [12] | Personalized biomarker identification | Identifying patient-specific neural signatures of symptoms |
| Clinical Assessment Tools | Ecological momentary assessments, UPDRS, Y-BOCS [15] [12] | Symptom monitoring & outcome measurement | Quantifying treatment efficacy in real-world settings |
Emerging Frontiers in Circuit-Based Targeting
Multi-Target Stimulation Approaches
Network-level dysfunctions in neurological and psychiatric disorders often require simultaneous modulation of multiple nodes within affected circuits. Multi-target DBS represents an advanced approach where two or more distinct anatomical structures are stimulated concurrently to address complex symptom profiles [8]. This strategy is particularly relevant for conditions like Parkinson's disease with treatment-resistant symptoms such as gait impairment and speech difficulties, where single-target stimulation may be insufficient. Clinical studies have explored combinations such as GPi+Vim for mixed tremor syndromes, with one study demonstrating 90.6% tremor reduction with dual-target stimulation compared to 21.8% with GPi stimulation alone [8].
The implementation of multi-target approaches requires careful consideration of the risk-benefit ratio, as implanting additional electrodes increases surgical complexity. However, technological advances including directional electrodes, current steering, and multi-independent current control systems are making multi-target strategies more feasible [8]. Future developments in system-on-chip micro-stimulators and closed-loop control systems capable of coordinating stimulation across multiple targets will further enhance the clinical utility of this approach.
Adaptive Closed-Loop DBS Systems
Adaptive DBS represents a paradigm shift from continuous, open-loop stimulation to dynamic, feedback-controlled therapy. These systems automatically adjust stimulation parameters based on detected neural biomarkers, creating a personalized neuromodulation approach that responds to the patient's fluctuating symptoms and brain states [15]. Commercial aDBS systems now available for Parkinson's disease utilize subthalamic beta power as a control signal, with stimulation amplitude dynamically adjusted between predefined upper and lower limits based on real-time biomarker levels [15].
Clinical implementation of aDBS requires a structured programming approach addressing three key challenges: (1) biomarker selection and validation, (2) threshold definition, and (3) stimulation limit optimization [15]. Programming protocols must account for individual variations in biomarker expression and modulation, with specific strategies needed for cases with absent or double beta peaks. Ecological momentary assessment data from recent studies indicates that aDBS can significantly improve overall well-being (p=0.007) and general movement (p=0.058) compared to continuous DBS, with six of eight patients choosing to remain on adaptive therapy long-term [15].
Personalized Target Identification Methodologies
The future of circuit-based targeting lies in fully personalized approaches that identify optimal stimulation sites based on individual brain network architecture and symptom expression. The PRESIDIO trial for depression exemplifies this approach, using individualized targeting based on functional neuroimaging and intracranial EEG mapping to identify patient-specific nodes within the depression network [11]. Similarly, recent work in chronic pain has demonstrated that individualized targets within cortico-striatal-thalamocortical pathways can be identified through intensive brain mapping and subsequently used for effective closed-loop stimulation [12].
These personalized methodologies typically involve extended inpatient monitoring with simultaneous symptom tracking and neural recording across multiple candidate regions. Machine learning algorithms then identify the neural features and locations that most strongly correlate with symptom expression in each individual. This patient-specific circuit mapping enables precise targeting of stimulation to modulate the pathological networks most relevant to each person's clinical presentation, potentially improving outcomes in heterogeneous disorders where one-size-fits-all approaches have shown limited success.
Deep Brain Stimulation (DBS) represents a cornerstone therapy for managing symptoms of neurological disorders such as Parkinson's disease (PD) and epilepsy. While the surgical implantation of electrodes is critical, the therapeutic efficacy of DBS is predominantly governed by the precise configuration of its core stimulation parameters: frequency, pulse width, amplitude, and spatial configuration. The optimization of these parameters is a complex process that must be tailored to both the anatomical target and the individual patient's clinical presentation. Current research is moving beyond standardized settings to explore a wider parameter space, including non-conventional combinations and adaptive systems that respond to neural biomarkers. This document synthesizes recent clinical evidence and provides detailed protocols to guide researchers in the systematic investigation of DBS parameter settings.
Quantitative Data Synthesis of Stimulation Parameters
Table 1: Clinical Outcomes of Alternative DBS Frequencies Across Disorders
| Disorder & Target | Stimulation Frequency | Pulse Width | Key Clinical Outcome | Citation |
|---|---|---|---|---|
| Epilepsy (ANT) | 145 Hz (iHFS) | 90 μs | 33% median seizure reduction [5] [16] | |
| Epilepsy (ANT) | 7 Hz (cLFS) | 200 μs | 73% median seizure reduction [5] [16] | |
| PD (STN) - Gait | 130 Hz (Conventional) | 60 μs | Reference for gait comparison [17] | |
| PD (STN) - Gait | 80 Hz (Low Frequency) | 60 μs | Improved gait speed in cognitive dual-task [17] | |
| PD (STN) - Gait | 130 Hz | 30 μs (Short Pulse Width) | Improved single and double support phases [17] | |
| PD (STN) - Cognition | ~130 Hz | Not Specified | Decreased decision thresholds (less response caution) [18] | |
| PD (STN) - Cognition | 4 Hz | Not Specified | Increased decision thresholds (more response caution) [18] | |
| PD (Dual-Target) | 125 Hz | Not Specified | Best reduction of bradykinesia [19] | |
| PD (Dual-Target) | 50 Hz | Not Specified | Effective at reducing bradykinesia [19] |
Table 2: Amplitude Modulation in Adaptive DBS for Parkinson's Disease
| Programming Aspect | Continuous DBS (cDBS) | Adaptive DBS (aDBS) | Citation |
|---|---|---|---|
| Amplitude Characteristics | Fixed amplitude (mean 2.04 mA) | Dynamic range (mean lower limit: 1.71 mA; mean upper limit: 2.28 mA) [15] | |
| Clinical Outcome (Group Level) | Baseline | Improved overall well-being (p=0.007); trend for enhanced general movement (p=0.058) [15] | |
| Patient Preference | N/A | 6 out of 8 patients chose to remain on aDBS long-term [15] |
Experimental Protocols for Parameter Investigation
Protocol: Randomized Crossover Trial for ANT-DBS in Epilepsy
This protocol outlines a methodology for comparing radically different parameter sets for anterior thalamic nucleus (ANT) deep brain stimulation in drug-resistant epilepsy [5] [16].
- Objective: To prospectively compare the efficacy and safety of continuous low-frequency stimulation (cLFS) against intermittent high-frequency stimulation (iHFS) for ANT-DBS.
- Patient Population: Individuals with focal drug-resistant epilepsy. A sample size of 16 patients was used in the referenced study.
- Stimulation Arms:
- iHFS Arm: Parameters modeled on the SANTE trial (145 Hz, 90 μs pulse width, cycling 1 minute on/5 minutes off).
- cLFS Arm: Alternative parameters (7 Hz, 200 μs pulse width, continuous stimulation).
- Study Design:
- Randomization: Patients are randomly assigned to one of the two stimulation parameter sets.
- Initial Phase: Patients remain on the first assigned settings for a 3-month period.
- Crossover: Unless the patient is seizure-free, they are switched to the alternative parameter set for a second 3-month period.
- Final Assessment: At the end of the second 3-month period, trial completion is marked. Patients then choose to remain on their current settings or revert to the previous one.
- Primary Outcome Measure: Median percentage reduction in seizure frequency from baseline.
- Key Statistical Considerations: Use non-parametric tests like the Wilcoxon signed-rank test for paired comparisons of seizure frequency reduction. A p-value of <0.05 is typically considered statistically significant.
Protocol: At-Home Assessment of Adaptive DBS in Parkinson's Disease
This protocol describes a framework for evaluating adaptive DBS (aDBS) using ecological momentary assessments (EMA) in a home-setting [15].
- Objective: To compare the effects of chronic aDBS versus conventional continuous DBS (cDBS) on patient-reported symptoms in Parkinson's disease.
- Patient Population: PD patients implanted with a sensing-capable DBS system. The referenced study included 8 patients.
- Stimulation Modes:
- Continuous DBS (cDBS): Conventional, fixed-amplitude stimulation.
- Adaptive DBS (aDBS): Dual-threshold aDBS system where stimulation amplitude is dynamically adjusted based on real-time subthalamic beta power.
- Programming of aDBS:
- Signal Quality Check: Verify the presence of a robust beta peak in the local field potential (LFP), preferably in the OFF-medication state.
- Threshold Definition: Set the upper and lower LFP thresholds to the 75th and 25th percentiles of daytime beta power, respectively. These thresholds exhibit strong inter-individual variance and require review over several days.
- Amplitude Limit Setting: Define the upper and lower stimulation amplitude limits. The lower limit should be evaluated in the OFF-medication state to prevent undertreatment.
- Optimization Visits: Refine LFP thresholds and amplitude limits based on patient reports and data logs to address under-stimulation, over-stimulation, or maladaptation.
- Outcome Measurement - Ecological Momentary Assessment (EMA):
- Patients receive repeated electronic questionnaires on a smartphone or device during their daily lives.
- Questions assess overall well-being, general movement, dyskinesia severity, and tremor on Likert-like scales.
- The study aimed for multiple assessments per day over two-week periods for each stimulation mode.
- Analysis: Compare mean scores for each EMA item between the cDBS and aDBS conditions using linear mixed-effects models to account for repeated measures.
Protocol: LFP-Guided Contact Selection for STN-DBS in Parkinson's Disease
This protocol utilizes local field potentials (LFP) to predict the optimal stimulation contact, potentially streamlining the clinical programming process [20].
- Objective: To validate LFP recordings for predicting the clinically chosen optimal monopolar stimulation contact.
- Patient Population: PD patients with implanted DBS systems capable of chronic LFP recording. The method was validated across 121 STN hemispheres.
- LFP Data Acquisition:
- Record bipolar LFP surveys (e.g., BrainSense Survey) from all possible electrode contact pairs.
- Perform recordings in the OFF-medication state (overnight suspension of dopaminergic drugs) to enhance beta-band visibility.
- Feature Extraction:
- For each bipolar recording channel, calculate the power spectral density.
- Identify the patient-specific beta peak frequency (typically 13-35 Hz).
- Extract features from the beta band. The "Max" feature (maximum beta power relative to the 1/f background) is most feasible for in-clinic use.
- Prediction Algorithm ("Decision Tree" Method):
- Rank Channels: Rank all bipolar recording channels based on the amplitude of the selected beta feature ("Max").
- Selection Tree: The top-ranked bipolar channel indicates that the contact situated between the two recording contacts is a candidate for the optimal stimulation contact.
- Elimination Tree: If the beta feature is flat across channels, the algorithm can also eliminate contacts with low predictive value.
- Validation: The predicted top two contact-levels achieved an accuracy of 86.5% compared to the clinician's choice based on monopolar review.
Workflow and Signaling Pathway Visualizations
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for DBS Parameter Research
| Item | Function in Research | Example/Notes |
|---|---|---|
| Sensing Neurostimulator | Enables recording of local field potentials (LFPs) and adaptive stimulation. | Medtronic Percept PC, Boston Scientific Vercise Genus [15] [20]. |
| Local Field Potential (LFP) Biomarkers | Serves as a physiological feedback signal for symptom state and target engagement. | Subthalamic beta power (13-35 Hz) for Parkinson's bradykinesia/rigidity [15] [20]. |
| Ecological Momentary Assessment (EMA) | Captures real-world, patient-reported outcomes in daily life. | Smartphone-based questionnaires on well-being, movement, and side-effects [15]. |
| Computational Decision Models | Quantifies latent cognitive processes affected by stimulation parameters. | Diffusion decision modeling to analyze decision thresholds in cognitive tasks [18]. |
| LFP-Guided Prediction Algorithms | Automates and objectifies the initial selection of optimal stimulation contacts. | "Decision tree" method using beta power features to rank contacts [20]. |
| Biophysical Models | Tests hypotheses and predicts outcomes of novel stimulation paradigms in silico. | Used to explore low-frequency dual-target DBS with intrahemispheric pulse delays [19]. |
Within deep brain stimulation (DBS) research, the optimization of stimulation parameters represents a rapidly advancing frontier. This progress, however, occurs within a complex ethical framework governing clinical trials, particularly concerning two pillars: the equitable selection of patient participants and the scientifically necessary yet ethically challenging use of sham-controlled procedures. These considerations are not mere regulatory hurdles but foundational to conducting research that is both scientifically valid and morally defensible. This application note examines these intertwined ethical dimensions, providing structured data and protocols to guide researchers in navigating this critical aspect of DBS parameter settings research.
Ethical Framework for Sham-Controlled Trials
Justifications and Controversies of Sham Procedures
Sham-controlled trials are a subject of intense ethical debate, characterized by a balance of compelling justifications and significant concerns. The core ethical arguments are summarized in the table below.
Table 1: Ethical Arguments For and Against Sham Procedures in Clinical Trials
| Supporting Arguments | Opposing Arguments |
|---|---|
| ↑ Scientific Validity: Enables blinding to prevent performance and ascertainment bias; isolates specific treatment effects from placebo effects. [21] [22] | Risk-Harm Balance: Exposes participants to risks without prospect of direct therapeutic benefit, violating the principle of non-maleficence. [23] [21] |
| Societal Benefit: Generates reliable knowledge about true efficacy, protecting future patients from ineffective treatments. [21] | Clinical Misconception: Blurs the line between clinical care and research; clinicians may engage in deliberate deception. [23] |
| Informed Consent: Legitimized by prior authorization and full disclosure that a sham procedure may be administered. [23] | Necessity Questioned: A sham control is not always necessary; comparison to an established effective treatment may be sufficient. [21] |
The placebo effect is a particularly critical factor in trials with subjective patient-reported outcomes like pain or quality of life. This effect is a complex psychobiological phenomenon influenced by patient preconceptions, expectations, and the therapeutic context itself. [22] For instance, the act of undergoing an invasive procedure, regardless of its actual therapeutic component, can generate significant symptom relief. Without a sham control, this effect can be misattributed to the intervention under investigation, leading to false positive conclusions and the adoption of ineffective treatments. [22]
Distinction from Clinical Practice
A key ethical concept is that the morality of a sham procedure in a research context is fundamentally different from its use in clinical practice. Performing a fake procedure on a patient in a clinical setting would be considered fraudulent. In contrast, within a clinical trial, it is a methodologically necessary research intervention. [23] This distinction hinges on the prior informed consent of the research subject, which transforms the act from a deceptive fraud into a legitimate, consented element of an experiment. [23] Researcher integrity is maintained by recognizing that their primary role has shifted from clinician to scientist, with a balanced commitment to rigorous science, the advancement of care, and subject protection. [23]
Ethical Patient Selection for DBS Trials
Ethical patient selection requires a multi-faceted approach that balances scientific needs with patient safety and justice.
Table 2: Key Considerations for Ethical Patient Selection in DBS Trials
| Consideration | Ethical Principle | Application in DBS Parameter Trials |
|---|---|---|
| Medical Refractoriness | Beneficence / Non-maleficence | Select patients with symptoms refractory to conventional pharmacological therapy who thus have a potential for net benefit. [24] [9] |
| Realistic Potential for Benefit | Justice | Preference for patients with established DBS indications (e.g., Parkinson's disease, essential tremor) when testing new parameters or programming methods. [3] [15] |
| Ability to Provide Informed Consent | Autonomy | Ensure patients have the cognitive capacity and are free from coercion; assess understanding of risks, including the possibility of sham assignment. [23] [21] |
| Appropriate Disease Stage | Scientific Validity | Selection depends on the research question: advanced stages for refractory symptoms vs. earlier stages for disease-modification studies. [9] |
| Absence of Absolute Contraindications | Non-maleficence | Exclude patients with significant comorbidities, high surgical risk, or contraindications to implanted hardware. [24] |
The following diagram illustrates the key ethical relationships and decision points in designing a DBS trial:
Experimental Protocols
Protocol for a Sham-Controlled DBS Parameter Trial
This protocol outlines a methodology for a double-blind, sham-controlled RCT investigating a novel adaptive DBS algorithm versus standard continuous DBS.
1. Ethics and Regulatory Preparation
- Submit the full protocol, including justification for the sham control and the complete informed consent document, to an independent Research Ethics Committee (REC) or Institutional Review Board (IRB). [23] [21]
- Obtain regulatory agency approval as required by national law.
2. Patient Selection and Screening
- Inclusion Criteria: (a) Diagnosis of idiopathic Parkinson's disease; (b) Documented motor fluctuations despite optimized medication; (c) Successful bilateral STN-DBS implantation at least 3 months prior; (d) Age 18-75; (e) Capacity to provide informed consent.
- Exclusion Criteria: (a) Significant cognitive impairment (MMSE <26); (b) Major active psychiatric comorbidity; (c) Contraindications to MRI; (d) Other serious medical illness limiting life expectancy or study participation.
3. Randomization and Blinding
- Use a central web-based randomization system to assign participants to either
Active aDBSorSham cDBSgroup. [22] - The sham intervention involves programming the DBS device to the patient's established effective cDBS parameters. The novel aDBS algorithm is installed on the device but is functionally disabled, with the device interface displaying simulated "adaptive" activity.
- Both the patient and the outcome assessors are blinded to the group assignment. The programming clinician is unblinded but does not participate in outcome assessments.
4. Informed Consent Process
- The consent form must explicitly state: "You will be randomly assigned to one of two groups. One group will receive the new adaptive stimulation, and the other will continue with your standard stimulation. Efforts will be made to make these two treatments indistinguishable to you and the evaluating doctor." [23]
- Clearly detail all foreseeable risks, including those related to the surgical implantation (already past) and those related to the stimulation paradigms and study visits.
- Emphasize the right to withdraw at any time without penalty to their clinical care.
5. Intervention and Follow-up
- The intervention period is 8 weeks.
- Participants have their devices programmed according to their randomization.
- Schedule follow-up assessments at 2, 4, and 8 weeks.
6. Outcome Assessment
- Primary Outcome: Change in blinded video-rated UPDRS-III motor score in the OFF-medication state from baseline to 8 weeks.
- Secondary Outcomes: Patient-reported quality of life (PDQ-39); daily motor symptom diary; device-specific data loggers for energy use.
7. Data Monitoring
- An independent Data and Safety Monitoring Board (DSMB) reviews unblinded interim data for patient safety and trial integrity.
Protocol for Computational DBS Parameter Optimization
This protocol describes a patient-specific, imaging-based method for optimizing DBS settings, which can reduce the burden of empirical programming and serves as a non-invasive research tool. [14] [25]
1. MRI Data Acquisition and Preprocessing
- Acquire pre-operative T1-weighted and T2-weighted MRI scans.
- Acquire a post-operative CT scan to visualize the implanted electrode.
- Co-register the pre- and post-operative images using rigid body transformation in a toolbox like Lead-DBS. [14] [25]
2. Electrode Localization and Target Identification
- Manually or automatically reconstruct the position of the DBS lead(s) within the native brain space. [25]
- Normalize the patient's brain images to a standard template (e.g., MNI space).
- Identify the target structure (e.g., the motor subregion of the STN) using an integrated atlas (e.g., DISTAL Atlas). [14]
3. Volume of Tissue Activated (VTA) Modeling
- Create a patient-specific computational model of the electric field using software such as OSS-DBS. [14] [25] This model incorporates the electrode location, tissue dielectric properties, and stimulation parameters (contact, amplitude, pulse width).
- Simulate the VTA for different stimulation configurations.
4. Optimization of Stimulation Parameters
- The optimal contact is selected based on a geometry score that ranks contacts by their Euclidean distance to the centroid of the target structure and, for directional leads, their angular orientation. [14]
- The stimulation amplitude is iteratively adjusted in the model until the simulated VTA achieves maximal overlap with the target structure and minimal leakage into adjacent regions associated with side-effects. [14] [25]
5. Clinical Validation
- The model-suggested parameters are applied to the patient's device.
- Clinical efficacy and side-effect thresholds are assessed through standard clinical examination and patient feedback in a supervised clinical setting.
The workflow for this computational protocol is as follows:
The Scientist's Toolkit
Table 3: Essential Research Reagents and Tools for DBS Trials
| Item / Tool | Function in Research | Example / Note |
|---|---|---|
| Lead-DBS Toolbox | Open-source software for pre/post-op image processing, lead localization, and VTA modeling. [14] [25] | Core platform for computational DBS research; enables atlas-based targeting and data aggregation across centers. |
| OSS-DBS | Open-source simulator for calculating the VTA based on patient-specific imaging and stimulation parameters. [14] [25] | Used to predict neural activation and optimize settings in silico before clinical testing. |
| Directional DBS Leads | Electrodes with segmented contacts allowing current steering. | A key technological advance; enables more precise targeting, reducing side-effects and informing parameter optimization algorithms. [3] |
| Local Field Potential (LFP) Sensing | Capability of implanted pulse generators to record neural signals. | Enables biomarker discovery (e.g., beta oscillations in PD) and is the foundation for adaptive DBS. [3] [15] |
| Adaptive DBS (aDBS) Systems | Next-generation devices that adjust stimulation in response to neural feedback. | Used in trials to test closed-loop therapy against conventional open-loop stimulation; requires specialized programming protocols. [15] |
| Wearable Sensors | Accelerometers, gyroscopes, etc., to objectively quantify motor symptoms. | Provide continuous, real-world outcome measures for assessing DBS efficacy, supplementing clinical rating scales. [3] |
Multidisciplinary Team Requirements for Safe DBS Research and Implementation
Deep brain stimulation (DBS) represents a significant advancement in the treatment of neurological and psychiatric disorders, yet its successful implementation hinges on a comprehensive multidisciplinary team (MDT) approach. The complexity of DBS interventions, which integrate advanced neurosurgical techniques with personalized neuromodulation, demands collaboration across diverse specialties to ensure patient safety, optimize clinical outcomes, and maintain ethical integrity throughout the research and clinical care continuum. This framework delineates the core composition, responsibilities, and protocols essential for MDTs engaged in DBS research and implementation, with particular emphasis on the context of investigating DBS parameter settings.
Core Multidisciplinary Team Composition
The effective functioning of a DBS program relies on a well-defined MDT with complementary expertise. The core team should include, but not be limited to, the following members and their primary responsibilities:
Table 1: Core Multidisciplinary Team Members and Responsibilities
| Team Member | Essential Roles and Responsibilities |
|---|---|
| Functional Neurosurgeon | Performs stereotactic lead implantation; manages surgical risks and intraoperative complications; collaborates on target selection. |
| Movement Disorder Neurologist / Psychiatrist | Leads patient selection and diagnostic confirmation; manages medical therapy; directs postoperative DBS programming and parameter optimization. |
| Neuropsychologist | Conducts pre- and post-operative cognitive and psychological assessments; evaluates decision-making capacity. |
| DBS Nurse Coordinator | Serves as the central point of contact for patients and families; coordinates care across the MDT; provides patient education. |
| Bioethicist | Guides ethical review of protocols, especially for vulnerable populations; ensures adherence to principles of respect, beneficence, and justice [11]. |
| Social Worker | Assesses psychosocial support systems and caregiver burden; connects patients with community resources [26]. |
| Neuroradiologist | Performs pre-operative structural and functional imaging for targeting; conducts post-operative imaging to verify lead placement. |
This team composition is fundamental to conducting a thorough risk-benefit analysis, establishing appropriate goals, and providing comprehensive patient education [26]. For research involving vulnerable populations, such as those with neuropsychiatric disorders or profound cognitive impairments, the inclusion of a bioethicist and meticulous attention to informed consent processes are particularly critical [11] [27].
Pre-Implementation Phase: Protocols for Patient Selection and Assessment
Patient Selection Criteria
A rigorous, protocol-driven patient selection process is the cornerstone of successful DBS outcomes. The interdisciplinary evaluation aims to identify candidates for whom the potential benefits of surgery significantly outweigh the associated risks [26]. General inclusion and exclusion criteria are summarized below.
Table 2: General DBS Candidate Selection Criteria Framework
| Domain | Typical Considerations |
|---|---|
| Diagnosis | Idiopathic Parkinson's disease, medically refractory epilepsy, essential tremor, dystonia, or investigationally, OCD, MDD, or PTSD [11] [28]. |
| Disease Severity & Chronicity | Advanced disease with significant impairment despite optimal medical therapy. For PD, criteria may include significant motor fluctuations or troublesome dyskinesias [26]. |
| Treatment Refractoriness | Inadequate response or intolerance to multiple standard-of-care treatments (e.g., pharmacotherapy, psychotherapy) [29] [28]. |
| Levodopa Responsiveness (for PD) | Generally, a significant positive response to levodopa predicts better DBS outcomes for certain symptoms, though DBS can be effective for medication-resistant tremor [26]. |
| Psychological & Cognitive Status | Absence of untreated major psychiatric comorbidity or significant cognitive impairment that would impede cooperation or consent. |
| Social Support | Availability of a reliable care partner to assist with post-operative care and follow-up [26]. |
| Realistic Expectations | Patient and family understanding of the procedure's goals, potential benefits, risks, and limitations [26]. |
Comprehensive Pre-operative Assessment Protocol
The pre-operative assessment is a multi-session process involving all MDT members.
- Neurological/Psychiatric Evaluation: A comprehensive review of diagnosis, symptom profile, medication history, and confirmation of treatment refractoriness.
- Levodopa Challenge Test (for PD): Administration of a supra-threshold dose of levodopa after a 12-hour medication-free period. A >30% improvement in the Unified Parkinson's Disease Rating Scale (UPDRS) motor score is often used as a benchmark, though its predictive value for long-term outcomes is variable [26].
- Neuropsychological Assessment: A detailed battery evaluating executive function, memory, attention, and mood to establish a cognitive baseline and identify contraindications.
- High-Resolution Neuroimaging: Pre-operative MRI (and sometimes CT) for surgical planning and target identification (e.g., STN, GPi, fornix, NBM) [27] [30].
- Psychosocial and Ethical Review: Assessment of social support structures, caregiver burden, and patient capacity for informed consent, particularly crucial in research contexts for disorders like schizophrenia or severe Alzheimer's disease [11] [27] [29].
Figure 1: Pre-operative Patient Assessment Workflow
Implementation Phase: Surgical and Initial Programming Protocols
Surgical Procedure and Lead Verification
The surgical protocol involves stereotactic implantation of DBS leads into the pre-defined target. Key steps include:
- Frame-Based or Frameless Stereotaxy: Using a stereotactic head frame or fiducial markers for coordinate determination.
- Intraoperative Microelectrode Recording (MER): Used in some centers to physiologically confirm the target location by recording characteristic neuronal activity.
- Intraoperative Clinical Testing: Application of temporary stimulation to assess therapeutic benefits and screen for adverse effects (e.g., motor contractions, paresthesia).
- Post-operative Imaging: A post-operative CT or MRI is coregistered with the pre-operative plan to anatomically verify lead placement prior to initiating chronic stimulation [30].
Initial DBS Programming Protocol
DBS programming is a systematic, iterative process to identify optimal stimulation parameters. Programming is typically initiated 2-4 weeks post-surgery to allow the resolution of microlesion effects and tissue edema [30].
Table 3: DBS Programming Parameters and Considerations
| Parameter | Function | Typical Ranges (Disease-Dependent) |
|---|---|---|
| Amplitude | Controls the intensity of stimulation (field size). | Voltage (V) or current (mA); titrated from low to high. |
| Pulse Width | Duration of each electrical pulse. | 60-120 microseconds (μs). |
| Frequency | Rate of pulse delivery. | High-frequency (e.g., 130-180 Hz) for PD; lower frequencies may be used for gait [31]. |
| Electrode Configuration | Selection of active cathode(s) and anode(s). | Monopolar or bipolar review; directional steering with segmented leads. |
A standard initial programming methodology, such as a monopolar review, is employed [30]:
- System Integrity Check: Verify lead impedance to rule out short or open circuits.
- Monopolar Review: Each electrode contact is tested sequentially as the cathode (negative) with the neurostimulator case as the anode (positive).
- Threshold Determination: For each contact, the amplitude is gradually increased to determine:
- Therapeutic Window: The range between the amplitude that first produces a clinical benefit and the amplitude that first elicits a persistent adverse effect.
- Contact Selection: The contact with the widest therapeutic window is typically selected for chronic stimulation.
Post-Implementation Phase: Long-Term Management and Research-Specific Protocols
Long-Term Clinical Management
The MDT's role continues long after surgery. The neurologist/psychiatrist manages stimulation parameters and medications, the neurosurgeon addresses any hardware-related issues, and the neuropsychologist and social worker monitor and support the patient's psychological and social well-being. Long-term follow-up is essential to manage disease progression and adjust therapy accordingly.
Research-Specific Protocols for Parameter Optimization
Research into DBS parameter settings employs advanced protocols to move beyond empiric programming. Key experimental methodologies include:
Table 4: Research Reagent Solutions for DBS Parameter Investigation
| Research Tool / Reagent | Function in DBS Research |
|---|---|
| Bidirectional Neural Implants (e.g., RC+S) | Allows simultaneous delivery of stimulation and chronic recording of local field potentials (LFPs) to identify symptom-linked neural biomarkers [31]. |
| Inertial Measurement Units (IMUs) | Provides objective, high-fidelity kinematic data (e.g., stride velocity, arm swing) for quantitative assessment of motor symptoms [31]. |
| Bayesian Optimization Models | Data-driven models that efficiently navigate the vast parameter space to predict personalized optimal DBS settings with limited trials [31]. |
| Standardized Behavioral Tasks | Used to evoke and measure specific symptoms (e.g., fear conditioning/extinction in PTSD) and correlate them with neural activity [28]. |
An example experimental workflow for gait optimization in Parkinson's disease is detailed below, integrating several of these tools [31].
Figure 2: Research Protocol for Gait Optimization
Detailed Experimental Protocol for Gait Optimization [31]:
- Baseline Data Acquisition: Patients equipped with IMUs and a bidirectional implant perform overground walking. Baseline local field potentials (LFPs) from targets like the globus pallidus and motor cortex are recorded synchronously with full-body kinematics.
- Systematic Parameter Variation: DBS parameters (amplitude, frequency, pulse width) are varied within a safe range across multiple sessions. A wide spectrum is tested (e.g., 60 Hz to higher frequencies).
- Multi-Metric Outcome Assessment: A composite Walking Performance Index (WPI) is calculated from key gait metrics: stride velocity, arm swing amplitude, and variability in step length and step time.
- Data Modeling and Analysis: A machine learning model (e.g., Gaussian Process Regressor) is trained on the collected data to predict the WPI based on DBS settings. Neural data is analyzed to identify spectral biomarkers (e.g., reduced pallidal beta power) correlated with improved gait.
- Validation: The model-predicted optimal settings are tested in the patient to confirm improvement in the WPI and the associated normalization of neural biomarkers.
The safe and effective research and implementation of Deep Brain Stimulation is fundamentally dependent on a robust, well-integrated multidisciplinary team. This framework has outlined the essential composition of the MDT, detailed the critical protocols spanning pre-operative assessment to long-term management, and provided examples of advanced research methodologies for parameter optimization. Adherence to this structured, collaborative approach ensures that DBS advances not only as a powerful therapeutic tool but also as a rigorously investigated and ethically conducted field of scientific inquiry.
Advanced Programming Methodologies: From Computational Modeling to Adaptive Systems
Deep Brain Stimulation (DBS) is an established treatment for advanced Parkinson's disease (PD), but achieving optimal therapy requires meticulous programming of stimulation parameters—a process that remains largely manual, time-consuming, and dependent on clinician expertise [3]. Modern approaches seeking to overcome these limitations have increasingly turned toward data-intensive machine learning methods, which can sometimes function as "black boxes" with limited explainability in clinical settings [14] [25].
Geometry-based optimization represents a promising alternative by leveraging patient-specific anatomical data and electrode location to guide programming. This approach utilizes the spatial relationship between the implanted lead and target structures to recommend optimal stimulation contacts and parameters, offering a more interpretable and clinically integrable solution [14]. This Application Note details the protocols and methodologies for implementing geometry-based DBS optimization, providing researchers with a framework for enhancing programming precision and efficiency.
Core Principles and Quantitative Evidence
Geometry-based optimization operates on the principle that the physical position of DBS electrode contacts relative to the anatomical target structure is a primary determinant of therapeutic efficacy. The method uses preoperative magnetic resonance imaging (MRI) and postoperative lead localization to calculate a geometry score for each contact, prioritizing those closest to the target centroid and optimally oriented toward it [14] [25].
Key Performance Data
Recent clinical evidence demonstrates the effectiveness of this approach. A retrospective study of 174 implanted electrodes from 87 PD patients yielded the following results compared to expert manual programming [14] [25]:
Table 1: Performance of Geometry-Based Optimization vs. Expert Programming
| Performance Metric | Statistical Significance (p-value) | Effect Size (Hedges' g) |
|---|---|---|
| Target Structure Coverage | p < 5 x 10⁻¹³ | g > 0.94 |
| Electric Field Leakage Minimization | p < 2 x 10⁻¹⁰ | g > 0.46 |
| Predicted Motor Outcome | p = 0.09 - 1.0 | g = 0.05 - 0.08 |
These findings indicate that algorithmically selected contacts can achieve superior anatomical precision and potentially equivalent clinical outcomes to manual selections, without the need for protracted iterative testing [14] [25].
The Impact of Electrode Geometry on Stimulation
Beyond lead placement, the physical design of the electrode itself influences stimulation efficiency. Computational modeling reveals that sharper, smaller electrodes enhance stimulation efficiency, while bipolar configurations with separation distances of less than 1 mm can provide higher efficiency and focality compared to traditional monopolar configurations [32]. Furthermore, designs that increase electrode perimeter, such as serpentine variations, create greater variation in current density, which enhances the activating function—a key determinant of neural excitation—and improves stimulation efficiency [33].
Experimental Protocols
Core Optimization Workflow
The following diagram illustrates the end-to-end pipeline for geometry-based DBS optimization, from data acquisition to parameter suggestion.
Figure 1: Geometry-Based DBS Optimization Workflow. The pipeline integrates imaging data and computational modeling to suggest optimal stimulation parameters. STN: Subthalamic Nucleus; VTA: Volume of Tissue Activated.
Protocol 1: Image Processing and Lead Reconstruction
Objective: To accurately localize the implanted DBS lead and identify the target structure within the patient's native brain space.
Materials:
- Preoperative T1-weighted and T2-weighted MRI scans (3D volumes recommended)
- Postoperative CT or MRI scan for electrode visualization
- Lead-DBS software toolbox (https://www.lead-dbs.org/)
- Standard computational environment (MATLAB or Python)
Methodology:
- Image Co-registration: Co-register pre- and postoperative images using the SPM algorithm within Lead-DBS to account for potential brain shift [14] [25].
- Spatial Normalization: Normalize images into standard space (e.g., MNI ICBM 2009b NLIN asymmetric space) using the ANTs algorithm (Advanced Normalization Tools) with SyN nonlinear transformation [14].
- Brain Shift Correction: Apply subcortical brainshift correction algorithms to improve anatomical accuracy in the region of the implanted lead [14].
- Electrode Reconstruction: Manually reconstruct the DBS electrode trajectory and contact positions. For research purposes, this can be performed using the "Manual Reconstruction" module in Lead-DBS. The final reconstruction should be validated by an expert neurologist [14] [25].
- Target Identification: Segment the target structure, typically the motor subregion of the Subthalamic Nucleus (STN), using appropriate atlas definitions (e.g., DISTAL Atlas) within Lead-DBS [14] [34].
- Native Space Conversion: Convert all reconstructions and segmentations back to the patient's native pre-operative space for all subsequent calculations to preserve individual anatomical specificity [14] [34].
Protocol 2: Geometry-Based Contact Selection
Objective: To computationally identify the electrode contact with the most favorable geometric positioning relative to the target.
Materials:
- Native space lead reconstruction data
- Native space target segmentation (motor STN centroid coordinates)
- Custom Python scripts for geometric calculations
Methodology:
- Centroid Calculation: Compute the center of mass (centroid) of the segmented motor STN.
- Distance Metric: For each electrode contact, calculate the Euclidean distance to the motor STN centroid.
- Angular Metric (for directional contacts): For directional contacts, calculate the rotation angle between the contact's center and the STN centroid, relative to the electrode axis.
- Ranking and Scoring: Independently rank all contacts from lowest to highest for both distance and angle. Sum the ranks for each contact to generate a final geometry score (
s_geometry,C). A lower score indicates a more optimal position [14] [25]. - Contact Selection: Select the contact with the lowest aggregate geometry score as the candidate for stimulation.
Protocol 3: VTA-Based Current Optimization
Objective: To determine the stimulation amplitude that optimally covers the target structure while minimizing leakage to adjacent regions.
Materials:
- OSS-DBS simulation software (https://oss-dbs.github.io/)
- Selected optimal contact from Protocol 2
- Tissue conductivity parameters (default: 0.2 S/m for gray matter)
Methodology:
- VTA Simulation: Use OSS-DBS to simulate the Volume of Tissue Activated (VTA) for the selected contact across a range of stimulation currents (e.g., 0.5 mA to 4.0 mA in 0.5 mA steps) [14].
- Overlap Analysis: For each simulated VTA, calculate the percentage overlap with the target structure (motor STN) and with adjacent non-target regions.
- Current Selection: Identify the stimulation current that achieves one of the following:
- Maximal Target Coverage: The current that yields the highest overlap with the target structure.
- Efficiency Optimization: The lowest current that achieves a predefined target coverage threshold (e.g., >80%), thereby maximizing battery life.
- Side-effect Avoidance: Ensure the selected current does not produce a VTA that significantly overlaps with known side-effect zones (e.g., the corticospinal tract) [34].
Advanced Protocol: Integration of Clinical Review Data
Objective: To refine the geometry-based model by incorporating initial clinical testing observations.
Methodology:
- Clinical Data Collection: During the initial programming session, test predefined contact groups (e.g., 4 groups per hemisphere) at incremental current levels. Record therapeutic efficacy (e.g., rigidity reduction) and side-effect thresholds for each configuration [14].
- Scoring: Generate a clinical review score (
s_clinical,C) based on the recorded therapeutic and side-effect observations for each contact group. - Data Fusion: Combine the geometry score (
s_geometry,C) and the clinical review score (s_clinical,C) into a weighted composite score to determine the final optimal contact [14].
The Scientist's Toolkit
Table 2: Essential Reagents and Software for Geometry-Based DBS Optimization
| Item | Function/Description | Example/Source |
|---|---|---|
| Lead-DBS Toolbox | Open-source software for image co-registration, normalization, and DBS electrode reconstruction. Essential for processing MRI/CT data. | https://www.lead-dbs.org/ [14] |
| OSS-DBS | Open-source simulation tool for calculating the Volume of Tissue Activated (VTA). Used for predicting neural activation. | https://oss-dbs.github.io/ [14] |
| Clinical Evaluation Data | Structured records of patient's response to intraoperative or initial clinical test stimulation. Used for model fine-tuning. | e.g., Rigidity, akinesia, tremor scores [14] |
| Pre-op & Post-op MRI | High-resolution anatomical images. Pre-op MRI defines anatomy; post-op MRI/CT verifies lead location. | 3T MRI recommended [14] [25] |
| Normative Brain Atlas | Digital atlas providing standardized definitions of subcortical structures like the STN and its functional subregions. | e.g., DISTAL Atlas, CIT168 [34] |
Validation and Refinement Workflow
After implementing the core optimization protocol, validation is a critical final step. The following diagram outlines the process for correlating model predictions with clinical and electrophysiological outcomes.
Figure 2: Model Validation and Refinement Loop. Predictions are validated against electrophysiological and clinical measures to iteratively improve model accuracy. VTA: Volume of Tissue Activated; DF: Driving Force.
Validation Methodologies:
- Cortical Evoked Potentials (cEPs): Use short-latency cEPs as a direct measure of pathway activation (e.g., hyperdirect pathway or corticospinal tract activation) to validate model predictions. The Driving Force (DF) model in native space has been shown to be the most accurate for quantitatively predicting experimental subcortical pathway activations [34].
- Local Field Potentials (LFPs): Record LFPs from the implanted DBS lead to identify biomarkers of effective stimulation (e.g., reduced beta power) and correlate these with VTA models [31].
- Wearable Sensors: Use inertial measurement units (IMUs) to quantify motor outcomes (e.g., stride length, tremor power) objectively, providing a continuous measure for correlating with simulated VTAs [35] [31].
Geometry-based optimization represents a significant advancement in DBS programming, moving from a purely empirical trial-and-error process to a principled, data-driven approach. By leveraging routinely collected MRI data and established computational tools, this method provides a patient-specific, interpretable, and efficient path to optimal stimulation settings. The protocols outlined herein provide a foundation for researchers to implement, validate, and refine these techniques, ultimately contributing to more standardized, effective, and accessible DBS therapies. Future developments will likely focus on tighter integration with real-time electrophysiological biomarkers and closed-loop adaptive systems, further personalizing treatment for neurological disorders.
MRI and Lead-DBS Integration for Patient-Specific VTA Modeling
Deep Brain Stimulation (DBS) is an established therapy for movement disorders such as Parkinson's disease (PD) and essential tremor, yet optimizing stimulation parameters for individual patients remains challenging [14]. The integration of magnetic resonance imaging (MRI) with computational modeling through the Lead-DBS toolbox represents a transformative approach for personalizing DBS therapies. This methodology enables researchers and clinicians to visualize electrode placement and predict the Volume of Tissue Activated (VTA) by electrical stimulation, creating patient-specific models that can enhance therapeutic outcomes while minimizing side effects [14]. The following application notes and protocols detail the implementation of this technology for research applications, framed within a broader thesis on advancing DBS parameter optimization through computational modeling.
Background and Significance
Traditional DBS programming relies on empirical, clinical observations during iterative parameter adjustments, a process that is time-intensive and often requires multiple clinical visits [14]. Patient-specific VTA modeling addresses this limitation by leveraging anatomical data to predict neural activation patterns, potentially streamlining the optimization process. Recent advances have demonstrated that algorithmic approaches to contact selection and current amplitude setting can outperform manual expert selections in covering target structures while minimizing electric field leakage to adjacent regions [14]. Furthermore, the integration of clinical review data with computational models enables fine-tuning of stimulation parameters to avoid adverse effects while maintaining therapeutic efficacy.
Core Methodologies for VTA Computation
VTA Computation Methods
Computational models for predicting DBS effects employ various methodologies to calculate the VTA, each with distinct advantages and limitations [36]. The table below summarizes the primary approaches:
Table 1: Comparison of VTA Computation Methodologies
| Method | Description | Applications | Considerations |
|---|---|---|---|
| Axon Model Method | Simulates effects of extracellular potentials on mammalian motor axons; traditional standard [36] | Gold standard validation; fundamental research | Computationally intensive; requires significant technical expertise |
| Activating Function (AF) Methods | Calculates second spatial derivative of extracellular voltage along axons [36] | Rapid VTA estimation; clinical applications | Sensitivity to axon orientation relative to stimulation source |
| Electric Field Norm Method | Uses norm of electric field for VTA estimation [36] | Monopolar stimulation with cylindrical leads; clinical tools like Lead-DBS | Limited validation for complex electrode configurations |
Technical Considerations for VTA Modeling
The computational efficiency of VTA modeling must be balanced against biological accuracy. The axon model method, while considered a standard, is computationally demanding and requires specialized expertise [36]. Alternative approaches based on the activating function provide faster computation while maintaining reasonable accuracy:
- AF-Tan: Calculates activating function at each grid point in the tangential direction [36]
- AF-3D: Computes activating function in the maximally activating direction at each grid point, free from axon orientation bias [36]
- AF-Max: Determines maximum activating function along the entire length of a tangential fiber, accounting for virtual cathode effects [36]
For monopolar stimulation, all methods produce highly similar volumes, while for bipolar configurations, only the AF-Max method reliably reproduces VTAs generated by direct axon modeling [36].
Experimental Protocols
MRI Data Acquisition and Processing Protocol
Table 2: MRI Acquisition Parameters for DBS Modeling
| Parameter | Pre-operative | Post-operative |
|---|---|---|
| Magnetic Field Strength | 3T | 1.5T |
| Image Type | T1-weighted, T2-weighted | CT or MRI |
| Spatial Resolution | ≤1mm isotropic | ≤1mm isotropic |
| Coregistration | ANTs method with SyN nonlinear transform [14] | SPM method [14] |
| Special Processing | - | Subcortical brainshift correction [14] |
Step-by-Step Protocol:
- Pre-operative Imaging: Acquire high-resolution T1-weighted and T2-weighted MRI scans at 3T field strength [14]
- Post-operative Verification: Obtain post-implantation CT or MRI scans to visualize electrode placement
- Data Import: Transfer images in NIfTI format to Lead-DBS toolbox [14]
- Spatial Normalization: Coregister pre-operative and post-operative images using ANTs method with SyN nonlinear transformation and mutual information metric [14]
- Brainshift Correction: Apply specialized algorithms to correct for post-operative anatomical shifts [14]
- Electrode Reconstruction: Manually reconstruct electrode trajectories and contact locations within Lead-DBS interface [14]
- Atlas Co-registration: Normalize patient anatomy to standard stereotactic space (e.g., MNI space) for target identification [14]
VTA Simulation and Optimization Protocol
Materials:
- Processed Lead-DBS reconstruction data
- OSS-DBS software for finite element method (FEM) modeling [14]
- Computational resources for electric field simulations
Procedure:
FEM Model Setup:
- Create individual FEM meshes of DBS lead designs embedded in brain tissue models [36]
- Incorporate tissue conductivity parameters appropriate for gray matter, white matter, and encapsulation layers
Electric Field Calculation:
Contact Selection:
Current Amplitude Optimization:
Diagram Title: MRI-Lead-DBS VTA Modeling Workflow
Integration of Clinical Data for Parameter Refinement
For enhanced personalization, clinical evaluations can be incorporated into the optimization pipeline:
Clinical Testing:
Data Integration:
- Combine clinical scores with geometry-based rankings [14]
- Weight clinical outcomes appropriately in final parameter selection
- Prioritize contacts with optimal therapeutic window (separation between efficacy and side effects)
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for MRI-Guided DBS Research
| Resource | Type | Function | Example Sources |
|---|---|---|---|
| Lead-DBS | Software Toolbox | Electrode reconstruction, atlas co-registration, VTA visualization [14] | www.lead-dbs.org |
| OSS-DBS | Computational Tool | Finite element method modeling, electric field calculation [14] | Butenko et al. 2020 |
| Clinical DBS Systems | Hardware | MR-conditional DBS implants for post-operative imaging [37] [38] | Abbott, Boston Scientific, Medtronic |
| Pattern Fill Module | Visualization Tool | Enhanced chart accessibility for scientific publications [39] | Highcharts Pattern Fill |
| Probabilistic Sweet Spots | Analytical Method | Statistical mapping of stimulation efficacy across patient cohorts [40] | Custom MATLAB/Python implementation |
Advanced Applications and Novel Research Directions
Personalized Parameter Optimization
Recent approaches have leveraged machine learning techniques to predict optimal DBS parameters:
- Geometry-Based Optimization: Uses spatial relationships between electrode contacts and target structures to suggest optimal settings [14]
- Bayesian Optimization: Employs Gaussian Process Regressors to efficiently explore parameter space with limited trials [31]
- Neurophysiology-Guided Programming: Integrates local field potential recordings to identify neural biomarkers of effective stimulation [31]
Gait-Specific DBS Programming
For addressing complex symptoms such as gait disturbances in Parkinson's disease:
Walking Performance Index (WPI) Development:
Neural Biomarker Identification:
Diagram Title: DBS Neural Mechanisms and Outcomes
Data Analysis and Interpretation Framework
Quantitative Assessment of VTA Optimization
To evaluate the efficacy of patient-specific VTA modeling:
Target Coverage Metrics:
Side Effect Avoidance:
Statistical Approaches for Probabilistic Sweet Spots
Different statistical methods yield variations in probabilistic stimulation mapping:
- Traditional Parametric Tests: t-tests with false discovery rate (FDR) correction [40]
- Nonparametric Alternatives: Wilcoxon tests with nonparametric permutations [40]
- Bayesian Methods: Bayesian t-tests for probabilistic interpretation [40]
- Linear Mixed Models: Account for repeated measures across patients [40]
The integration of MRI with Lead-DBS for patient-specific VTA modeling represents a significant advancement in DBS research and clinical practice. This approach enables data-driven parameter optimization based on individual anatomy and electrode placement, potentially reducing the time and effort required for programming while improving therapeutic outcomes. The protocols and methodologies outlined herein provide a framework for implementing this technology in research settings, with applications ranging from basic investigation of stimulation mechanisms to personalized therapeutic optimization. As the field progresses, the incorporation of additional data modalities—including neurophysiological recordings, functional imaging, and clinical assessments—will further enhance the precision and efficacy of DBS therapies.
Adaptive Deep Brain Stimulation (aDBS) represents a paradigm shift in neuromodulation therapy for Parkinson's disease (PD). Unlike traditional open-loop DBS that delivers constant stimulation, aDBS systems automatically adjust therapeutic stimulation in response to fluctuating brain signals [41]. Medtronic's BrainSense technology, embedded in the Percept PC neurostimulator, is the first commercially available closed-loop DBS system capable of sensing local field potentials (LFPs) while simultaneously delivering therapeutic stimulation [42] [43]. This bidirectional interface enables personalized therapy that responds to the brain's changing needs throughout the day, addressing a fundamental limitation of conventional DBS systems.
Technical Principles & Physiological Basis
Core Operating Principles
The BrainSense platform operates on a closed-loop feedback mechanism comprising three fundamental processes:
- Neural Signal Acquisition: The implanted DBS lead captures local field potentials (LFPs) from surrounding neural tissue, even while delivering therapeutic stimulation [43].
- Biomarker Detection & Classification: Proprietary algorithms analyze LFPs in real-time, identifying specific spectral signatures correlated with PD symptom severity.
- Therapeutic Modulation: Stimulation parameters automatically adjust based on the detected biomarker state to optimize symptom control.
The system specifically targets elevated beta-band oscillations (13-30 Hz), which research has established as a reliable biomarker correlating with motor symptom severity, particularly rigidity and bradykinesia [41]. When beta power exceeds a predetermined threshold, the system increases stimulation intensity; when beta power normalizes, stimulation decreases accordingly.
Quantitative Performance Metrics
Table 1: BrainSense aDBS Clinical Performance Data
| Parameter | Traditional DBS | Adaptive DBS | Clinical Significance |
|---|---|---|---|
| Motor Symptom Control | Baseline reference | Superior improvement [43] | Better management of rigidity, bradykinesia, tremor |
| Stimulation Energy Usage | Constant delivery | Reduced overall energy [41] | Potential battery conservation |
| Therapy Personalization | Fixed parameters | Continuous adaptation | Responds to symptom fluctuations |
| Patient Preference | Not applicable | 75% preference for aDBS [42] | Higher satisfaction with adaptive approach |
Research Protocols & Methodologies
ADAPT-PD Clinical Trial Framework
The pivotal ADAPT-PD study established the clinical validation framework for BrainSense aDBS [42] [41]. The methodological approach included:
Study Design: A non-randomized clinical trial investigating long-term personalized aDBS in Parkinson's disease, with results published in JAMA Neurology [42].
Primary Endpoints:
- Clinical effectiveness measured by Unified Parkinson's Disease Rating Scale (UPDRS) Part III motor scores
- Incidence and severity of stimulation-related adverse effects
- Patient preference between conventional and adaptive DBS
Participant Criteria: Parkinson's disease patients with responsive beta-band oscillations, typically with advanced disease experiencing motor fluctuations inadequately controlled by medication.
Implementation Protocol:
- Baseline Assessment: Characterize individual beta oscillation patterns through LFP recording
- Threshold Determination: Establish patient-specific beta power thresholds for stimulation adjustment
- Dual-Threshold Operation: Program upper threshold for stimulation increase and lower threshold for stimulation decrease
- Safety Monitoring: Document stimulation-related side effects during initial programming phase
Experimental Workflow for aDBS Implementation
Signaling Pathways & Neural Mechanisms
Research Reagent Solutions & Technical Toolkit
Table 2: Essential Research Materials for aDBS Investigation
| Component | Specification | Research Application |
|---|---|---|
| Implantable Neurostimulator | Medtronic Percept PC with BrainSense [43] | Core platform for bidirectional neural interfacing |
| DBS Leads | Directional or omnidirectional electrodes (Medtronic 3389, B33 series, Abbott 6172) [14] | Neural signal recording and stimulation delivery |
| Lead Localization Software | Lead-DBS toolbox [14] | Electrode reconstruction and anatomical localization |
| Computational Modeling | OSS-DBS software [14] | Volume of Tissue Activated (VTA) simulations |
| Biomarker Analysis Tools | Custom MATLAB/Python scripts for LFP analysis | Beta oscillation detection and quantification |
| Clinical Assessment Scales | UPDRS Part III, patient symptom diaries | Objective and subjective outcome measures |
| Motion Sensors | Wearable inertial sensors [35] | Quantitative gait parameter measurement |
Advanced Programming & Optimization Protocols
Geometry-Based Contact Selection Algorithm
Recent research has established computational methods for optimizing DBS parameters using routinely collected MRI data [14]. The protocol involves:
Input Data Requirements:
- Pre-operative and post-operative MRI (3T & 1.5T respectively)
- Lead reconstruction data in Lead-DBS format
- Clinical review records of contact performance
Algorithmic Optimization Process:
- Contact Geometry Scoring: Calculate Euclidean distance and rotation angle between each contact and motor STN centroid
- Volume of Tissue Activated (VTA) Modeling: Simulate electrical field spread using OSS-DBS software
- Target Coverage Optimization: Maximize VTA overlap with dorsolateral STN motor subregion
- Adverse Effect Minimization: Reduce electric field leakage to adjacent structures
Performance Validation: In retrospective analysis of 174 electrode implants, algorithm-selected parameters demonstrated significantly better target structure coverage (Wilcoxon p < 5e-13, Hedges' g > 0.94) and reduced side-effect profiles compared to expert manual programming [14].
Multi-Target Stimulation for Gait Impairment
For addressing complex symptoms like freezing of gait (FoG), advanced protocols combining standard subthalamic nucleus (STN) stimulation with substantia nigra pars reticulata (SNr) stimulation have shown promise [35].
Stimulation Conditions:
- Mono-site STN stimulation at 119 Hz
- Dual-site STN+SNr stimulation with SNr frequencies of 119 Hz, 71 Hz, or 30 Hz
- Total electrical energy delivered (TEED) maintained constant across conditions
Assessment Methodology:
- Wearable inertial sensors for kinematic gait analysis
- Spatial parameters: stride length, swing time variability
- Temporal parameters: gait cycle timing, freezing episode duration
- Clinical scales: FoG questionnaire, UPDRS gait subscores
Outcome Correlation: Changes in stride length and swing time demonstrated high correlation coefficients (>0.8) with clinical FoG improvement, establishing digital biomarkers for protocol optimization [35].
Data Analysis & Interpretation Framework
Quantitative LFP Signal Processing
Table 3: BrainSignal Analytical Parameters
| Parameter | Normal Range | Pathological State | Therapeutic Response |
|---|---|---|---|
| Beta Power (13-30 Hz) | Low amplitude | Elevated oscillations | Reduction with effective stimulation |
| Beta Burst Duration | Short, transient | Prolonged episodes | Normalization of burst dynamics |
| Spectral Peak Frequency | Variable individual patterns | Consistent peak in low-beta | Stability or slight frequency shift |
| Medication Modulation | Levodopa-responsive | Reduced responsivity | aDBS complements medication effects |
Clinical-Physiological Correlation Protocol
The integration of neural signals with clinical assessments follows a standardized methodology:
- Simultaneous Recording: BrainSense LFP capture during clinical examination
- Symptom-Event Marking: Patient-triggered markers for symptom occurrence
- Signal Averaging: Time-locked analysis of LFP patterns around clinical events
- Stimulation Efficacy Quantification: Correlation between beta suppression and motor improvement
- Longitudinal Tracking: Monitoring of neural and clinical progression over time
This systematic approach enables researchers to establish patient-specific neural signatures of symptom states and validate the physiological basis for aDBS therapy adjustments.
Incorporating Clinical Review Data into Algorithmic Parameter Selection
Deep Brain Stimulation (DBS) is a well-established neurosurgical treatment for movement disorders like Parkinson's disease (PD), with a growing range of investigated indications [44]. A critical challenge in DBS therapy is the post-operative optimisation of stimulation parameters—specifically electrode contact selection and current amplitude—which has traditionally relied on clinician expertise and iterative in-clinic testing. This process is time-consuming, costly, and burdensome for patients [14]. Modern approaches have explored data-intensive machine learning methods to solve this problem, but these often function as "black boxes," lack interpretability, and require data not routinely collected in standard clinical workflows, limiting their clinical adoption [45] [14]. This application note details a novel, patient-specific, and interpretable pipeline for DBS parameter optimisation. This method integrates routine magnetic resonance imaging (MRI) data with existing clinical review records to provide a geometry-based, explainable, and effective solution that fits seamlessly into existing clinical practice [45] [46].
Key Methodologies and Experimental Protocols
The core methodology is an automated, cross-platform pipeline that leverages individual patient anatomy and optional clinical evaluations to recommend optimal stimulation parameters [14].
Patient Data and MRI Processing
Data Acquisition: The protocol utilizes retrospective data from patients who have undergone bilateral DBS implantation, such as a cohort of 87 PD patients (174 implantation instances) [45] [14]. Essential data includes:
- Pre-operative 3T MRI: For detailed anatomical visualization.
- Post-operative 1.5T MRI: For precise electrode localization.
- Clinical Review Records: Documentation from initial post-operative stimulation sessions, which typically include assessments of different contact groups at incremental current levels (e.g., 0.5 mA to 4.0 mA in 0.5 mA steps). Assessments focus on therapeutic efficacy (improvement in rigidity, akinesia, tremor) and thresholds for adverse effects [14].
Data Processing with Lead-DBS: The pre- and post-operative MRI images (in Nifti format) are processed using the well-established Lead-DBS toolbox [14]. The processing pipeline includes:
- Co-registration and Normalisation: Images are co-registered to standard atlas space using methods like SPM and ANTs with SyN nonlinear transformation [14].
- Brainshift Correction: Subcortical brainshift is corrected using established algorithms [14].
- Electrode Reconstruction: The DBS lead trajectory and contacts are reconstructed, preferably manually, and validated by an expert neurologist [14]. All subsequent volume and coordinate processing is performed after conversion back to the patient's native space for subject-specific accuracy [14].
Optimisation Algorithm Workflow
The optimisation occurs in two primary stages: contact selection and current selection.
Contact Selection
The goal is to identify the electrode contact with the most favorable spatial position relative to the target structure, such as the motor subregion of the subthalamic nucleus (STN) [14].
- Geometry-Based Score: For each contact, two geometric features are calculated relative to the centroid of the motor STN:
- The Euclidean distance to the centroid.
- The rotation angle between the contact and the centroid (particularly relevant for directional leads). These two metrics are independently ranked across all available contacts, and the ranks are summed to produce a final geometry-based score for each contact. The contact with the most favorable (lowest) score is selected [14].
- Clinical Review-Based Score (Optional): When clinical review data is available, it is incorporated. The data, which often evaluates contact groups rather than individual contacts, is used to rank the groups based on therapeutic effect (e.g., rigidity reduction) and the absence of adverse effects. This ranking is integrated with the geometry-based score to refine contact selection [14].
Current Selection
After the optimal contact is selected, the current amplitude is determined by modeling the Volume of Tissue Activated (VTA) [14] [46].
- VTA Simulation: The OSS-DBS tool is used to simulate the electric field spread from the selected contact [14]. This simulation is fast and adjustable.
- Target Coverage and Side-Effect Avoidance: The algorithm calculates the current amplitude that maximizes the overlap between the VTA and the target motor STN while simultaneously minimizing the electric field "leakage" into adjacent regions where stimulation might cause side effects [45] [46]. The tool allows for interactive user adjustment of the current settings for further fine-tuning.
Experimental Validation Protocol
To validate the algorithm's performance, a retrospective comparison against expert-chosen clinical settings is conducted [45] [14] [46].
- Metrics for Comparison: The effectiveness of the algorithmically selected parameters is evaluated using two primary computational metrics:
- Target Structure Coverage: The degree of overlap between the VTA and the motor STN.
- Electric Field Leakage: The extent of the electric field spreading into neighboring non-target regions.
- Statistical Analysis: The performance is statistically compared using Wilcoxon signed-rank tests (with Bonferroni correction) to assess significance, and effect sizes are calculated using Hedges' g [14]. A retrospective analysis of a patient subset can also be performed to predict clinical motor outcomes compared to the expert settings [14].
The following diagram illustrates the complete workflow from data input to parameter output.
Key Data and Performance Results
Validation on a substantial patient cohort demonstrates the algorithm's superior performance in silico compared to expert manual programming.
Table 1: Algorithm Performance vs. Expert Settings on Computational Metrics [45] [14] [46]
| Performance Metric | Expert Settings | Algorithm Settings | Statistical Significance (p-value) | Effect Size (Hedges' g) |
|---|---|---|---|---|
| Target Structure Coverage | Baseline | Superior | < 5e-13 | > 0.94 |
| Electric Field Leakage | Baseline | Reduced | < 2e-10 | > 0.46 |
Table 2: Retrospective Analysis of Clinical Motor Outcomes [14]
| Analysis Subset | Comparison Group | Predicted Motor Outcome | Statistical Significance (p-value) | Effect Size (Hedges' g) |
|---|---|---|---|---|
| Limited patient cohort (n=50) | Expert settings | Comparable improvement | 0.09 - 1.0 | 0.05 - 0.08 |
The data indicates that the algorithm's parameter settings are significantly more effective than expert settings at covering the intended target structure while minimizing unwanted field leakage into adjacent areas. Furthermore, a retrospective analysis predicts that this improved targeting could translate to comparable clinical motor outcomes, a finding that warrants prospective validation [14].
Implementation and Integrated Workflow
For researchers aiming to implement this methodology, the following workflow and toolkit are essential. The pipeline is packaged as a standalone, cross-platform GUI-based tool, ensuring ease of use and integration [14].
The Scientist's Toolkit: Essential Research Reagents and Software
Table 3: Key Materials and Software for Protocol Implementation [45] [44] [14]
| Item Name | Type/Model Example | Primary Function in Protocol |
|---|---|---|
| MRI Scanner | 3T (pre-op), 1.5T (post-op) | High-resolution anatomical imaging and post-implant localization. |
| DBS Electrodes | Medtronic 3389, Abbott 6172 | Implanted device for electrical stimulation. |
| Lead-DBS Toolbox | Open-source software (Horn & Kühn, 2015) | Coregistration, normalization, brainshift correction, and electrode reconstruction. |
| OSS-DBS | Open-source software (Butenko et al., 2020) | Fast, adjustable simulation of the Volume of Tissue Activated (VTA). |
| Python Environment | Custom pipeline with SciPy, Pingouin | Execution of the optimisation algorithm and statistical analysis. |
The interplay between the core components of the DBS optimisation toolkit and the data they process is visualized below.
This application note outlines a robust and interpretable protocol for integrating clinical review data with patient-specific imaging to algorithmically determine optimal DBS parameters. The method addresses a critical bottleneck in clinical DBS workflows by providing a solution that is both computationally superior to manual expert settings and readily applicable using routinely collected data [45] [14]. By leveraging established, open-source tools like Lead-DBS and OSS-DBS, the pipeline ensures high accessibility and reproducibility for the research community. The promising retrospective results, demonstrating enhanced target coverage and reduced side-effect potential, provide a strong rationale for prospective clinical trials to validate its efficacy in improving patient outcomes. This approach represents a significant step toward more efficient, personalized, and data-driven neuromodulation therapies.
The optimization of Deep Brain Stimulation (DBS) parameters represents a critical challenge in translational neuroscience, balancing the need for computational precision with the practical demands of clinical workflows. Traditional DBS programming relies on empirical, iterative adjustments that are time-intensive, costly, and burdensome for patients, often requiring multiple clinical visits over several months [14]. Modern approaches have increasingly turned to computational models and machine learning to predict optimal stimulation parameters, but these often introduce significant computational overhead and lack explainability, limiting their clinical adoption [14].
The fundamental challenge lies in integrating increasingly sophisticated computational methods into clinical practice without overwhelming existing workflows. This application note addresses this challenge by presenting and validating a geometry-based optimization pipeline that leverages routinely collected clinical data to suggest optimal electrode contact and current settings, demonstrating how computational sophistication can be balanced with clinical practicality [14].
Quantitative Performance Analysis
The performance of the proposed geometry-based optimization method was evaluated against expert clinical settings using a substantial dataset of 174 implanted electrode reconstructions from 87 Parkinson's disease patients. The results demonstrate significant improvements in both target coverage and avoidance of side effects.
Table 1: Performance Comparison of Geometry-Based Optimization vs. Expert Settings
| Performance Metric | Statistical Significance | Effect Size (Hedges' g) | Clinical Implication |
|---|---|---|---|
| Target Structure Coverage | Wilcoxon p < 5e-13 [14] | g > 0.94 [14] | Superior coverage of the motor subregion of the STN |
| Electric Field Leakage Minimization | Wilcoxon p < 2e-10 [14] | g > 0.46 [14] | Reduced stimulation of adjacent regions to minimize side effects |
| Predicted Motor Outcomes | p = 0.09-1 (not significant) [14] | g = 0.05-0.08 [14] | Comparable clinical efficacy to expert programming |
A retrospective analysis of a limited subset (n=50) further predicted that the algorithmically selected parameters would yield motor outcomes comparable to those achieved by expert clinicians, suggesting that the technical improvements in stimulation targeting translate to maintained clinical efficacy [14].
Experimental Protocols
MRI Data Processing and Lead Reconstruction
This protocol details the processing of pre- and post-operative MRI data to reconstruct the implanted electrode position, a foundational step for the optimization pipeline.
Primary Objectives: To co-register pre-operative and post-operative MRI datasets, correct for post-operative brainshift, and precisely reconstruct the position of the implanted DBS electrode in standard atlas space [14].
Materials and Equipment:
- Pre-operative 3T MRI (T1-weighted, susceptibility-weighted imaging recommended)
- Post-operative 1.5T or 3T MRI (CT can be substituted for superior electrode visualization)
- Lead-DBS toolbox (https://www.lead-dbs.org/)
- Statistical Parametric Mapping (SPM) software
- Advanced Normalization Tools (ANTs)
Step-by-Step Procedure:
- Data Import: Import pre-operative and post-operative NIfTI format images into the Lead-DBS environment [14].
- Co-registration: Co-register pre-operative and post-operative images using the SPM method to account for spatial discrepancies [14].
- Normalization: Normalize the co-registered images into standard stereotactic space (e.g., MNI or ICBM 152) using the ANTs method with a SyN nonlinear transform and mutual information metric [14].
- Brainshift Correction: Apply a subcortical brainshift correction algorithm to compensate for post-operative anatomical displacement [14].
- Electrode Reconstruction: Manually reconstruct the trajectory and contacts of the implanted electrode. The reconstruction must be validated by an expert neurologist or neurosurgeon [14].
- Coordinate Conversion: Convert all normalization and reconstruction data back to native patient space for subsequent patient-specific optimization calculations [14].
Geometry-Based Contact Selection Protocol
This protocol outlines the computational method for selecting the optimal DBS electrode contact based on its spatial relationship to the target structure.
Primary Objectives: To algorithmically identify the electrode contact(s) with the most anatomically favorable position relative to the centroid of the motor subregion of the Subthalamic Nucleus (STN) [14].
Materials and Equipment:
- Lead reconstruction data (from Protocol 3.1)
- Segmented STN motor subregion (from normalized atlas data)
- Python-based optimization tool [14]
Step-by-Step Procedure:
- Centroid Identification: Calculate the center of mass (centroid) of the motor subregion of the STN in the patient's native space [14].
- Spatial Feature Calculation: For each electrode contact, calculate two geometric features:
- The Euclidean distance between the contact and the STN motor subregion centroid.
- The rotation angle between the contact and the centroid, relative to the electrode axis (particularly relevant for directional contacts) [14].
- Feature Ranking: Independently rank each contact from lowest to highest for both the Euclidean distance and rotation angle metrics. Since these metrics have different units and scales, ranking normalizes their contribution [14].
- Composite Score Calculation: Sum the individual ranks for distance and angle to generate a composite geometry-based score for each contact (
geometry,C) [14]. - Contact Selection: Propose the contact with the most favorable (lowest) composite geometry score as the candidate for stimulation.
VTA-Based Current Optimization Protocol
This protocol describes the process of determining the optimal stimulation current amplitude based on modeling the Volume of Tissue Activated (VTA).
Primary Objectives: To simulate the electrical field generated by DBS and select a stimulation current that maximizes coverage of the target structure while minimizing leakage into adjacent regions [14].
Materials and Equipment:
- Lead reconstruction data (from Protocol 3.1)
- Selected electrode contact (from Protocol 3.2)
- OSS-DBS software for fast VTA calculation [14]
- (Optional) Clinical review data from initial post-operative testing
Step-by-Step Procedure:
- VTA Simulation: Using OSS-DBS, simulate the Volume of Tissue Activated for the selected electrode contact across a range of clinically relevant current amplitudes (e.g., 0.5 mA to 4.0 mA in 0.5 mA steps) [14].
- Overlap Calculation: For each simulated VTA, calculate the percentage overlap with the target structure (motor STN). Concurrently, calculate the volume of the VTA that extends into non-target, potentially problematic adjacent regions [14].
- Optimal Current Selection: Identify the current amplitude that provides the best trade-off between high target coverage and low non-target leakage. This can be presented as a single recommendation or as a range for the clinician.
- Optional Clinical Integration: If clinical review data is available (e.g., therapeutic and side-effect thresholds for different contacts and currents), this information can be used to further constrain and fine-tune the current selection, particularly to avoid amplitudes that previously induced adverse effects [14].
Workflow Visualization
The following diagram illustrates the integrated workflow, from data input to the generation of stimulation parameters, highlighting the seamless integration of computational steps with clinical data and validation.
The Scientist's Toolkit: Research Reagent Solutions
This section catalogues the essential software tools and data types that constitute the core "research reagents" for developing and implementing integrated DBS optimization workflows.
Table 2: Essential Tools and Data for DBS Optimization Research
| Tool / Data Type | Primary Function | Role in Workflow Integration | Key Features |
|---|---|---|---|
| Lead-DBS Toolbox [14] | Atlas co-registration, normalization, and electrode reconstruction | Foundational data processing platform that converts raw imaging data into a spatially precise lead model. | Integration of SPM & ANTs, brainshift correction, support for multiple atlases, open-source. |
| OSS-DBS [14] | Fast calculation of the Volume of Tissue Activated (VTA) | Enables patient-specific simulation of stimulation fields to predict clinical effect and side-effects. | Adjustable parameters, fast computation, compatible with Lead-DBS output. |
| Pre/Post-op MRI [14] | Anatomical reference and lead localization | Provides the essential anatomical dataset for target identification and reconstructing electrode position. | Pre-op (3T) for planning, Post-op (1.5T/3T) or CT for verification. |
| Clinical Review Data [14] | Documented therapeutic & adverse effect thresholds | Optional data for fine-tuning and validating computational suggestions against empirical clinical observations. | Contact group testing, rigidity/akinesia/tremor scores, side-effect thresholds. |
| Python-based GUI Tool [14] | Pipeline integration and user interface | Packages the entire workflow into a clinically usable application, bridging the gap between computation and practice. | Cross-platform, interactive optimization, input of clinical data. |
| Computational Models [47] [48] | Predicting neural activation from electric fields | Provides the biophysical basis for VTA estimation; requires validation/calibration for accuracy. | Accounts for electrode geometry, tissue properties; open-source frameworks available. |
The integration of a geometry-based DBS optimization pipeline demonstrates a viable path for balancing computational sophistication with clinical practicality. By building upon established tools like Lead-DBS and OSS-DBS, and utilizing only routinely collected MRI and clinical data, the method achieves significant improvements in stimulation targeting without introducing prohibitive complexity or data requirements into the clinical workflow [14]. The provided protocols and toolkit offer researchers a framework for developing and validating similar integrated solutions, ultimately accelerating the translation of computational advances into enhanced patient care.
Overcoming Clinical Challenges: Strategies for Suboptimal Response and Side Effects
Within the broader research context of deep brain stimulation (DBS) parameter optimization, managing stimulation-induced side effects represents a critical translational challenge. As DBS therapies expand to new neurological and neuropsychiatric indications, the occurrence of side effects such as dysarthria, gait impairment, and stimulation-induced ataxia remains a significant barrier to optimal therapeutic outcomes [49]. The etiology of these effects is often linked to the spread of current to neighboring fiber tracts, modulating local and distal neural networks beyond the intended target [49]. This application note provides a structured framework for troubleshooting these adverse events, integrating evidence-based programming strategies, surgical considerations, and emerging computational approaches to maintain tremor suppression while minimizing side effects—a core objective in DBS parameter settings research.
Pathophysiology of Common Stimulation-Induced Side Effects
Neural Circuits and Associated Adverse Effects
Stimulation-induced side effects typically arise from unintended modulation of neural structures adjacent to the DBS target. Table 1 summarizes the primary side effects, their neuroanatomical correlates, and frequency across DBS targets.
Table 1: Common Stimulation-Induced Side Effects and Their Neural Correlates
| Side Effect | Primary Neuroanatomical Correlate | Common DBS Targets Where Observed | Reported Prevalence |
|---|---|---|---|
| Dysarthria | Corticospinal/corticobulbar tracts, dentato-rubro-thalamic tract (DRTT) | VIM, PSA, cZI | 9-75% [49] |
| Gait Impairment | Cerebellar pathways, basal ganglia-cortical circuits | STN, VIM | Part of "ET-plus" syndrome [49] |
| Stimulation-induced Ataxia | Cerebellar receiving areas, DRTT | VIM, PSA | Commonly encountered [49] |
| Dysphagia | Corticobulbar pathways | Thalamic region | Less common but reported [49] |
The mechanistic understanding of these side effects has been advanced through connectomic DBS modeling, which aims to identify specific brain network connections modulated during stimulation [50]. However, researchers should note substantial variability in pathway activation predictions across different structural connectomes, raising concerns about the general reliability of connectomic DBS studies without anatomical validation [50].
Visualization of Side Effect Pathways
The following diagram illustrates the primary neural pathways implicated in common stimulation-induced side effects and their relationship to DBS targets:
Pathway Diagram Title: Neural Pathways of DBS Side Effects
This visualization highlights the anatomical proximity between common DBS targets and critical fiber tracts whose unintended activation leads to therapeutic limitations. Research indicates that dysarthria may occur through current spread to the corticospinal/corticobulbar tracts and to the DRTT, reflecting either an aggravation of pre-existing cerebellar deficits and/or involvement of upper motor neuron fibers [49].
Structured Troubleshooting Protocol
Comprehensive Algorithm for Side Effect Management
The following workflow provides a systematic approach to identifying and mitigating stimulation-induced side effects in DBS patients:
Flowchart Title: DBS Side Effect Troubleshooting Algorithm
Programming Parameter Modifications: Evidence-Based Strategies
Table 2 summarizes programming adjustments for managing stimulation-induced side effects while maintaining therapeutic efficacy:
Table 2: Programming Strategies for Stimulation-Induced Side Effects
| Strategy | Protocol Implementation | Evidence Level | Considerations for Researchers |
|---|---|---|---|
| Amplitude Reduction | Decrease amplitude in 0.1-0.2 mA increments until side effects subside; reassess tremor control | Clinical consensus [49] | May result in suboptimal tremor control; requires balance in shared decision-making |
| Contact Selection Change | Switch to more ventral contacts; use dorsal contacts associated with higher dysarthria risk [49] | Observational studies [49] | Dysarthria more common with dorsal contacts, usually above intercommissural line |
| Bipolar Configuration | Set optimal tremor control contact as cathode; adjacent contact as anode; start at 1.0 mA, increase gradually | Case series [49] | Reduces current spread to adjacent structures; may require higher amplitudes |
| Interleaved Stimulation | Use different settings on adjacent contacts with alternating timing | Emerging evidence | Allows targeting of different neural populations; hardware-dependent |
| Current Directionality | Use directional leads to steer current away from internal capsule or cerebellar pathways | Emerging evidence [49] | Modifies volume of tissue activated; requires specialized leads and programming |
| Frequency Reduction | Consider lower frequencies (60-100 Hz) for side effect management | Limited evidence | May help with gait issues; potentially less effective for tremor |
| Double Monopolar Configuration | Simultaneously target multiple regions (e.g., Vim and PSA) with current fractionation | Case reports [49] | Utilizes current fractionation in commercially available devices |
Research indicates that in approximately one-third of patients, dysarthria will only appear with chronic stimulation, underscoring the importance of long-term monitoring even with well-placed electrodes [49]. The bilateral nature of DBS implantation significantly influences side effect risk, with dysarthria occurring more frequently in those undergoing bilateral DBS [49].
Research Reagent Solutions and Methodological Tools
Table 3 catalogs key research tools for investigating and optimizing DBS parameters to minimize side effects:
Table 3: Research Reagent Solutions for DBS Side Effect Investigation
| Tool/Category | Specific Examples | Research Application | Technical Notes |
|---|---|---|---|
| Connectomic Atlases | Horn normative connectome, Yeh population-averaged tract-to-region pathway atlas, Petersen histology-based pathway atlas (STN focused), Majtanik histology-based pathway atlas (ANT focused) [50] | Predicting pathway activation from DBS; modeling network effects of stimulation | Variability in predictions across different connectomes; histological atlases more anatomically realistic but regionally limited |
| DBS Simulation Platforms | Lead-DBS, OSS-DBS, StimVision [50] [14] | Volume of Tissue Activated (VTA) modeling; electric field calculations | Enables patient-specific optimization based on individual anatomy |
| Beta Peak Detection Algorithms | Algebraic dynamic peak amplitude thresholding approaches [51] | Identifying optimal contacts based on beta oscillatory activity (13-30 Hz) in PD | Algorithms matched expert consensus in performance; may reduce subjective bias in contact selection |
| Clinical Assessment Tools | UPDRS III gait sub-score (item 29) [52] | Quantifying gait impairment in PD DBS studies | Standardized outcome measures essential for comparative effectiveness research |
| Directional DBS Leads | Commercially available directional leads from multiple manufacturers | Current steering to avoid side effects while maintaining efficacy | Allows shaping of electrical field to avoid stimulation of adjacent fiber tracts |
Experimental Protocols for Side Effect Investigation
Geometry-Based Optimization Protocol
Based on recent research, the following protocol enables geometry-based optimization of DBS electrode contact and current selection using routinely collected MRI data:
Materials:
- Pre-operative and post-operative MRI images (Nifti format)
- Lead reconstruction data (Lead-DBS format)
- Clinical evaluation records (if available)
- Processing tools: Lead-DBS toolbox, OSS-DBS for VTA calculations
Methodology:
- MRI Data Processing: Import pre-operative (3T) and post-operative (1.5T) MRI images into Lead-DBS toolbox for atlas co-registration using SPM method, normalization using ANTs method with SyN nonlinear transform, subcortical brainshift correction, and manual electrode reconstruction [14].
- Contact Selection: Calculate spatial relationship of contacts to target structure centroid using two geometric features: (i) Euclidean distance to motor STN centroid, and (ii) rotation angle between contact and centroid relative to electrode axis for directional contacts. Rank these metrics from lowest to highest across contacts and sum ranks to yield geometry-based score for each contact [14].
- Current Selection: Model Volume of Tissue Activated (VTA) using OSS-DBS to estimate overlap with target structure. Optimize current settings to maximize coverage of target structure while minimizing electric field leakage to neighboring regions [14].
- Clinical Integration (Optional): Incorporate clinical review data using weighted scores for therapeutic effects (rigidity, akinesia, tremor improvement) and adverse effects. Combine geometry-based scores with clinical evaluation for final contact selection [14].
Validation: In a retrospective analysis of 174 implanted electrode reconstructions from 87 Parkinson's disease patients, this geometry-based approach demonstrated significantly better coverage of the target structure (Wilcoxon p < 5e-13, Hedges' g > 0.94) and reduced electric field leakage to neighboring regions (p < 2e-10, g > 0.46) compared to expert parameter settings [14].
Beta Peak Detection Algorithm Protocol
For researchers investigating data-driven DBS programming strategies in Parkinson's disease, the following protocol standardizes beta peak detection from local field potentials:
Materials:
- Local field potential recordings from implanted DBS electrodes
- Power spectral density (PSD) plots
- Computational resources for algorithm implementation
Methodology:
- Data Acquisition: Record local field potentials using a novel monopolar referencing strategy across distinct contacts along each DBS electrode implanted in the subthalamic nucleus [51].
- Spectral Analysis: Generate power spectral densities from LFP data, focusing on beta frequency range (13-30 Hz).
- Algorithm Application: Implement beta peak detection algorithms, prioritizing those with algebraic dynamic peak amplitude thresholding approaches. Algorithms sharing this underlying approach have demonstrated highest accuracy matching expert consensus [51].
- Validation: Compare algorithm-derived beta peaks with expert consensus using two-sample Kolmogorov-Smirnov tests. The most accurate algorithms in recent studies matched expert consensus and reliably predicted clinical stimulation parameters during follow-up visits [51].
Technical Notes: Algorithm performance varies by subject-specific PSD characteristics. In validation studies, certain participants contributed more challenging PSDs (e.g., Participant 5: 62% PSDs where <4 algorithms matched consensus peak), highlighting the need for robust algorithm selection and potential multi-algorithm approaches [51].
Discussion and Research Implications
The structured troubleshooting framework presented here integrates anatomical, computational, and clinical considerations for managing DBS side effects—a critical aspect of DBS parameter settings research. Evidence suggests that algorithmic approaches to contact selection and parameter optimization can outperform manual expert settings in simulation studies [14], though prospective clinical validation remains essential.
Future research directions should prioritize the validation of connectomic models against clinical outcomes, with attention to substantial variability in pathway activation predictions across different structural connectomes [50]. Additionally, the development of standardized beta peak detection algorithms offers promise for reducing subjective bias in DBS programming [51], potentially leading to more consistent therapeutic outcomes across diverse patient populations.
The integration of these computational approaches with clinical expertise represents the most promising path forward for minimizing stimulation-induced side effects while maintaining the therapeutic benefits of DBS across neurological disorders.
In deep brain stimulation (DBS) for Parkinson's disease, "threshold contraction" refers to the phenomenon where the therapeutic window for stimulation narrows over time, creating discrepancies between intraoperatively determined stimulation parameters and those required for chronic therapeutic efficacy. This presents a significant challenge in achieving long-term optimal patient outcomes. The pyramidal tract side effect (PTSE) threshold—the stimulation amplitude at which unwanted motor side effects like muscle contractions occur—often differs between intraoperative testing and chronic programming sessions [53]. Addressing this discrepancy is crucial for extending the therapeutic window and improving the durability of DBS outcomes. This application note examines the underlying mechanisms of threshold contraction and provides detailed protocols for researchers investigating this phenomenon within the context of advanced DBS parameter optimization.
Quantitative Data Comparison
Table 1: Comparative Analysis of Intraoperative vs. Chronic Programming Thresholds
| Metric | Intraoperative Values | Chronic Programming Values | Difference & Significance |
|---|---|---|---|
| PTSE Threshold | Mean: 4.3 mA (SD: 1.2 mA, Range: 2.0–8.0 mA) [53] | Mean: 3.7 mA (SD: 0.8 mA, Range: 2.0–6.5 mA) [53] | Linear regression: Statistically significant predictor (p < 0.001) [53] |
| Therapeutic Window | Established during awake surgery or via EMG under GA [53] | Often requires reprogramming; may be narrower [3] | Contributes to programming burden; necessitates repeated clinical visits [3] |
| Programming Time | N/A (Part of surgical procedure) | >12 hours labor per patient conventionally [3] | Automated programming aims to reduce this burden [3] |
| Key Measurement | EMG-based activation threshold (amplitude doubling baseline) [53] | Clinical observation of side effects (dysarthria, facial spasm, gaze deviation, limb contraction) [53] | Different biomarkers and measurement techniques contribute to observed differences |
Table 2: Automated Programming Biomarkers and Algorithm Performance
| Biomarker Class | Specific Modality | Research Context | Advantage for Chronic Programming |
|---|---|---|---|
| Wearable/Kinematic | Accelerometer-based watches, motion sensors [3] | Reduced programming time to achieve comparable motor outcome [3] | Objective, continuous measurement of tremor, rigidity, bradykinesia [3] |
| Neurophysiological | Local Field Potentials (LFP), Beta band activity [3] | LFP-guided programming shows feasibility in pilot studies [3] | Potential for closed-loop adjustment; correlates with motor impairment [3] |
| Image-Guided | Volume of Tissue Activated (VTA), Lead-DBS reconstruction [14] | Algorithmically selected contacts outperform manual selections in target coverage [14] | Patient-specific, based on individual anatomy; explainable recommendations [14] |
| Search Algorithms | Bayesian optimization, reinforcement learning [3] | Can efficiently search millions of possible parameter combinations [3] | Addresses complexity of next-generation DBS devices with multiple contacts [3] |
Experimental Protocols
Protocol 1: Intraoperative EMG-based PTSE Threshold Determination under General Anesthesia
This protocol details the methodology for predicting chronic PTSE thresholds during DBS lead implantation under general anesthesia (GA), enabling real-time surgical guidance without patient feedback [53].
Materials: Total intravenous anesthesia (TIVA) with propofol and remifentanil; Bispectral index (BIS) monitor; needle EMG setup; stereotactic surgical system; macroelectrode for stimulation.
Procedure:
- Anesthesia Management: Induce GA using TIVA. Maintain BIS between 40–60. Administer muscle relaxants only for intubation; allow effects to wear off prior to monitoring [53].
- EMG Setup: Place needle EMG electrodes into the deltoid and forearm extensor muscle groups contralateral to the implanted hemisphere [53].
- Macrostimulation: Perform monopolar macrostimulation through the macro contact of the DBS electrode at the site with optimal microelectrode recording signals.
- Stimulation Paradigm: Begin stimulation at parameters of 0.5 mA, 60 µs pulse width, and 130 Hz frequency. Gradually increase intensity in 0.5 mA increments [53].
- Threshold Definition: Define the EMG-based PTSE threshold as the stimulation amplitude at which the EMG signal amplitude doubles or exceeds the baseline level. Visually monitor for concurrent facial asymmetry, eye deviation, or pupillary changes [53].
- Surgical Decision: Use the established threshold to guide final lead placement. If the threshold is ≤ 2.5 mA, consider exploring revision tracts to achieve a safer lateral margin from the pyramidal tract [53].
Protocol 2: Image-Based and Clinical-Review Integrated DBS Parameter Optimization
This protocol describes a computational approach for optimizing chronic DBS settings using routinely collected MRI data and existing clinical review information, improving upon manual programming [14].
Materials: Pre-operative and post-operative MRI (Nifti format); Lead-DBS toolbox; OSS-DBS simulator; cross-platform GUI optimization tool [14].
Procedure:
- MRI Data Processing:
- Import pre-operative (3T) and post-operative (1.5T) MRI into Lead-DBS toolbox.
- Perform atlas co-registration, normalization, subcortical brainshift correction, and manual electrode reconstruction, validated by an expert [14].
- Contact Selection (Geometry-Based):
- Calculate the Euclidean distance from each electrode contact to the centroid of the motor subregion of the STN.
- For directional contacts, compute the rotation angle between the contact and the centroid relative to the electrode axis.
- Rank contacts based on these geometric features and sum the ranks to generate a geometry-based score for contact selection [14].
- Current Selection (VTA-Based):
- Use OSS-DBS to simulate the Volume of Tissue Activated (VTA) for candidate contacts.
- Calculate the overlap between the VTA and the target structure (motor STN). The optimal current maximizes this overlap while minimizing electric field leakage to adjacent regions [14].
- Integration of Clinical Review (Optional):
- Incorporate existing clinical evaluations of contact groups (if available) from initial programming sessions.
- Combine subjective clinical scores for rigidity, akinesia, and tremor with geometry-based scores for final contact and current selection [14].
Signaling Pathways and Workflows
Diagram 1: Threshold Contraction Experimental Workflow
Diagram 2: Computational DBS Parameter Optimization
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials
| Item | Function/Application in Research |
|---|---|
| Lead-DBS Toolbox | Open-source software for processing MRI data, electrode reconstruction, and atlas co-registration; foundational for image-based analysis [14]. |
| OSS-DBS Simulator | Computational tool for fast, adjustable calculations of the Volume of Tissue Activated (VTA) by DBS; enables electric field modeling [14]. |
| EMG System with Needle Electrodes | For recording muscle activity in response to intraoperative stimulation; critical for quantifying PTSE thresholds under GA [53]. |
| Total Intravenous Anesthesia (TIVA) | Propofol and remifentanil protocol maintaining BIS 40-60; enables neurophysiological monitoring under GA by minimizing interference [53]. |
| Validated Wearable Sensors | Accelerometer-based devices (e.g., wristwatches) for objective, continuous quantification of motor symptoms (tremor, bradykinesia) during programming [3]. |
| Directional DBS Leads | Advanced electrodes with segmented contacts allowing current steering; increase programming complexity but potentially improve therapeutic window [3]. |
Parameter Adjustment for Disease Progression and Symptom Fluctuation
Deep Brain Stimulation (DBS) parameter adjustment represents a significant challenge in the long-term management of progressive neurological disorders such as Parkinson's disease (PD). Conventional continuous DBS (cDBS) delivers fixed stimulation parameters that may become suboptimal as disease progression alters neural circuitry and symptom dynamics. Furthermore, symptom fluctuations occurring throughout the day require adaptive approaches that fixed parameters cannot address. This application note synthesizes current research findings and provides detailed protocols for implementing advanced parameter adjustment strategies. These approaches leverage neural biomarkers, computational modeling, and closed-loop technologies to maintain therapeutic efficacy against progressing pathology and fluctuating symptoms, representing a paradigm shift from static to dynamic neuromodulation therapies.
Quantitative Data Synthesis
Efficacy Outcomes of Adaptive Versus Conventional DBS
Table 1: Comparative Outcomes of Adaptive and Conventional DBS from Clinical Studies
| Study Metric | Adaptive DBS (aDBS) | Conventional DBS (cDBS) | Statistical Significance | Citation |
|---|---|---|---|---|
| Overall well-being (EMA score) | 6.73 ± 1.33 | 5.92 ± 1.01 | p = 0.007 | [54] |
| General movement (EMA score) | 6.2 ± 1.44 | 5.47 ± 1.22 | p = 0.058 (trend) | [54] |
| Favorable clinical status (ON time) | 87 ± 16% | 81.5 ± 25% | Not significant | [54] |
| Patient preference to remain on aDBS | 6/8 patients | 2/8 patients | N/A | [54] |
| LFP-guided contact prediction accuracy | 75.0-86.5% | N/A | Superior to existing algorithms | [20] |
| Image-guided programming UPDRS-III improvement | Significant improvement | Baseline | P < 0.05 sustained at 3 months | [55] |
Technical Parameters and Biomarkers in Advanced DBS Approaches
Table 2: Technical Specifications and Neural Biomarkers for DBS Parameter Adjustment
| Parameter/Biomarker | Description | Application in Parameter Adjustment | Citation |
|---|---|---|---|
| Subthalamic beta power | 13-35 Hz oscillatory activity correlated with bradykinesia/rigidity | Primary control signal for adaptive DBS; thresholds set at 25th-75th percentiles of daytime power | [54] |
| Evoked Resonant Neural Activity (ERNA) | Stereotyped local oscillations following DBS pulses (3-4 ms latency) | Paired-pulse facilitation varies by target (GPi vs. STN); potential biomarker for circuit engagement | [56] |
| Walking Performance Index (WPI) | Composite metric (stride velocity, arm swing, step variability) | Objective gait assessment for data-driven DBS parameter optimization | [31] |
| Volume of Tissue Activated (VTA) | Computational model of electrical field propagation | Image-guided programming to maximize STN coverage while minimizing leakage | [14] [55] |
| Geometry score | Spatial relationship between contacts and motor STN centroid | Contact selection based on Euclidean distance and rotation angle | [14] |
| Current steering | Horizontal/vertical shaping of stimulation field | Image-guided optimization to target dorsolateral STN | [55] |
Experimental Protocols
Protocol 1: Implementation of Chronic Adaptive DBS Based on Subthalamic Beta Power
Objective: To implement and optimize a commercially available dual-threshold adaptive DBS system for Parkinson's disease patients with residual motor fluctuations despite conventional DBS.
Background: Adaptive DBS dynamically adjusts stimulation amplitude based on neurophysiological feedback from subthalamic beta power, which correlates with bradykinesia and rigidity severity. This protocol enables stimulation intensity to automatically tailor to fluctuating symptom severity and medication state [54].
Materials:
- Implanted DBS system with sensing capability (e.g., Percept PC, Medtronic)
- Programming interface with BrainSense technology
- Ecological Momentary Assessment (EMA) platform for home symptom tracking
Procedure:
- Preparation Phase:
- Conduct initial assessment with patients in OFF medication state (≥12 hours overnight withdrawal) to enhance beta peak detection.
- Perform "BrainSense Streaming" to visualize local field potentials (LFP) and identify characteristic beta peaks (13-35 Hz).
- Select sensing contacts based on signal-to-noise ratio and clinical efficacy of test stimulation.
Initial Parameter Setup:
- Program upper and lower stimulation limits based on therapeutic windows established during conventional DBS.
- Set LFP thresholds to 25th and 75th percentiles of daytime beta power using continuous Timeline data acquisition over several days.
- Maintain pulse width (typically 60 μs) and frequency (typically 130 Hz) stable from conventional settings.
Optimization Phase:
- Schedule follow-up visits to ensure stimulation amplitude appropriately tracks beta power changes.
- Address common challenges:
- For stimulation stuck at limits: Adjust LFP thresholds to ensure dynamic adaptation.
- For persistent symptoms despite adaptation: Refine amplitude limits (e.g., raise lower limit if OFF symptoms persist).
- For over-stimulation effects: Reduce upper amplitude limit or adjust LFP thresholds.
- Continue optimization over approximately 8 programming visits (range 4-13) until satisfactory configuration achieved.
Outcome Assessment:
- Deploy ecological momentary assessments (EMA) during 2-week periods of both cDBS and aDBS.
- Evaluate overall well-being, general movement, dyskinesia severity, and tremor using structured questionnaires.
- Analyze time in therapeutic state (ON or ON with non-troublesome dyskinesia) [54].
Protocol 2: Data-Driven Optimization of DBS for Gait Enhancement
Objective: To identify personalized DBS parameters that improve gait in Parkinson's disease using a data-driven modeling approach with neurophysiological insights.
Background: Gait disturbances in PD often respond variably to DBS. This protocol uses a composite Walking Performance Index (WPI) and Gaussian Process regression to model the relationship between DBS parameters and gait outcomes, enabling identification of optimal settings [31].
Materials:
- Bidirectional neural stimulator (e.g., Summit RC+S, Medtronic)
- Full-body inertial measurement unit (IMU) sensors for gait kinematics
- Electrocorticography (ECoG) paddles over motor cortical areas
- Computational resources for Gaussian Process Regressor modeling
Procedure:
- Experimental Setup:
- Implant quadripolar DBS leads targeting the globus pallidus (GP) and subdural ECoG paddles over motor cortex.
- Connect cortical paddles and GP DBS leads to bidirectional Summit RC+S neural stimulators.
- Ensure system capability for simultaneous stimulation and high-resolution local field potential recording.
Gait Assessment Protocol:
- Conduct overground walking tests along a 6-meter loop.
- Record continuous neural data and gait kinematics during walking.
- Collect approximately 200 steps per parameter setting, excluding turns.
- Use full-body IMU sensors to capture stride velocity, arm swing amplitude, and variability in step length and step time.
Parameter Testing Sequence:
- Test clinically optimized settings as baseline.
- Systematically vary stimulation parameters:
- Amplitude: Test clinical amplitude, 25-30% reduction, and upper limits (typically 2.8-5.5 mA)
- Frequency: Test clinical frequency (typically 130 Hz), 60 Hz, and higher frequencies
- Pulse width: Maintain at clinical setting (typically 60 μs) or adjust if necessary
- Maintain charge-balanced stimulation throughout.
Data Analysis and Modeling:
- Calculate Walking Performance Index (WPI) by normalizing and equally weighting four gait parameters.
- Apply Gaussian Process Regressor to predict WPI based on DBS parameters.
- Identify neural correlates of improved walking by analyzing pallidal beta power during key gait phases.
- Determine optimal personalized DBS settings based on model predictions [31].
Protocol 3: LFP-Guided Contact Selection for Optimal Stimulation
Objective: To implement local field potential (LFP) guided algorithms for predicting optimal stimulation contacts, reducing programming time and patient burden associated with traditional monopolar review.
Background: Beta-band power (13-35 Hz) in subthalamic LFPs correlates with akinetic-rigid symptoms and can guide contact selection. This protocol validates two prediction algorithms that translate bipolar LFP recordings to monopolar stimulation recommendations [20].
Materials:
- DBS system with LFP recording capability (e.g., BrainSense technology)
- Programming software with LFP visualization tools
- Computational resources for implementing prediction algorithms
Procedure:
- LFP Data Acquisition:
- Conduct BrainSense Survey measurements after overnight withdrawal of dopaminergic medications.
- Record bipolar LFP from all possible contact pairs on the DBS lead.
- Ensure proper artifact rejection and signal quality assessment.
Feature Extraction:
- Calculate beta-band power features from LFP recordings:
- "Max": Maximum beta power in patient-specific range
- "AUC": Area under the curve of beta power spectrum
- "Maxflat" and "AUCflat": Flattened spectrum variants to reduce 1/f background influence
- Identify clear beta activity (based on "AUC_flat" threshold) in recording channels.
- Calculate beta-band power features from LFP recordings:
Contact Prediction:
- Apply "decision tree" method for in-clinic use:
- Rank channels based on beta power features
- Apply selection rules based on spatial relationships between recording pairs and contacts
- Combine with elimination tree to exclude contacts with poor signals
- Alternatively, implement "pattern based" method for offline validation:
- Match LFP patterns to known spatial configurations associated with optimal contacts
- Compare predictions with existing DETEC algorithm as benchmark.
- Apply "decision tree" method for in-clinic use:
Validation:
- Evaluate predictive accuracy for top two contact-levels against clinical choices from monopolar review.
- Assess performance across different centers and patient populations.
- Validate against chronic contact choices at 6-12 months post-implantation [20].
Visualization of Workflows
Adaptive DBS Programming Logic
Data-Driven Gait Optimization
LFP-Guided Contact Selection
The Scientist's Toolkit
Table 3: Essential Research Reagents and Materials for DBS Parameter Research
| Tool/Technology | Specifications | Research Application | Citation |
|---|---|---|---|
| Bidirectional Neural Stimulators (Summit RC+S, Medtronic) | Simultaneous stimulation and recording capability; 100 kHz sampling rate; chronic LFP streaming | Closed-loop DBS investigation; neural biomarker discovery during naturalistic behaviors | [31] |
| Directional DBS Leads (Medtronic, Abbott, Boston Scientific) | 8+ contacts; independent current control; segmented design | Current steering to optimize stimulation field shape; avoid side effects | [55] |
| Inertial Measurement Units (IMUs) | Full-body sensor suits; 3D accelerometry/gyroscopy; wireless data transmission | Objective gait assessment; quantification of motor symptoms outside lab | [31] |
| Image-Guided Programming Software (Stimview XT, Lead-DBS) | Pre/post-op MRI/CT fusion; VTA modeling; 3D visualization of anatomy | Patient-specific programming based on individual anatomy | [14] [55] |
| Local Field Potential Analysis Tools (BrainSense, custom MATLAB) | Beta power quantification; artifact rejection; spectral analysis | Neural biomarker identification for therapy guidance | [54] [20] |
| Computational Modeling Platforms (OSS-DBS, Gaussian Process Regressor) | Electric field simulation; Bayesian optimization; personalized prediction | Data-driven parameter selection; efficient exploration of parameter space | [31] [14] |
The evolution of DBS parameter adjustment strategies from fixed, continuous stimulation to adaptive, data-driven approaches represents a fundamental advancement in neuromodulation therapy. The integration of neural biomarkers, particularly subthalamic beta power for adaptive DBS and ERNA for circuit engagement assessment, provides objective guidance for parameter optimization that can respond to both disease progression and symptom fluctuation. Implementation of these advanced protocols requires specialized equipment including bidirectional neural interfaces, directional leads, and computational modeling resources, but offers the potential for substantially improved therapeutic outcomes. Future research directions should focus on validating these approaches in larger cohorts, developing integrated clinical platforms, and expanding the biomarker repertoire to address non-motor symptoms and other neurological disorders.
Directional Stimulation and Interleaving Programming to Maximize Therapeutic Window
Deep Brain Stimulation (DBS) has established itself as a fundamental therapy for movement disorders such as Parkinson's disease (PD) and essential tremor (ET) [30] [57]. The efficacy of this therapy is critically dependent on post-operative programming, the process of tailoring stimulation parameters to maximize symptom control while minimizing side effects for each individual patient [58]. The therapeutic window (TW)—defined as the range between the stimulation amplitude that produces clinical benefit and the amplitude that induces adverse effects—serves as a crucial metric for optimizing DBS efficacy [59] [60]. Recent technological advances, including directional leads and interleaving programming, provide clinicians with unprecedented control over the shape and delivery of the electrical field, offering powerful strategies to widen the therapeutic window [57]. These advanced programming techniques are particularly valuable for managing complex symptoms and compensating for suboptimally placed leads, thereby improving patient outcomes and satisfaction [58]. This application note details the practical implementation of these techniques within the context of ongoing DBS parameter research.
Quantitative Clinical Data and Adoption Trends
The integration of directional stimulation into clinical practice has been systematically evaluated in long-term studies. A 36-month retrospective review of 74 patients (56 with PD, 18 with ET) implanted with a directional DBS system provides clear evidence of its sustained clinical utility [59] [60].
Table 1: Adoption of Directional Stimulation in Clinical Practice Over 36 Months
| Time Point | PD Patients with Directional Stimulation | ET Patients with Directional Stimulation | Primary Reasons for Use |
|---|---|---|---|
| 3 Months | 22/56 (39%) | 13/18 (72%) | Better symptom control, reduced side effects [60] |
| 12 Months | 19/48 (40%) | 8/12 (67%) | Better symptom control, reduced side effects [60] |
| 24 Months | 12/31 (39%) | 5/8 (63%) | Better symptom control, reduced side effects [60] |
| 36 Months | 6/9 (67%) | 1/2 (50%) | Better symptom control, reduced side effects [60] |
The data indicates that directional stimulation is employed for a substantial proportion of patients, with higher initial adoption in ET, likely due to the less complex, monosymptomatic nature of the disorder compared to PD [59]. Over time, however, the use in PD increased as clinicians gained experience and sought solutions for complex symptoms [59].
Table 2: Clinical Outcomes and Stimulation Parameters for Advanced Programming
| Programming Technique | Clinical Application & Rationale | Reported Outcomes & Parameters |
|---|---|---|
| Directional DBS | Used to improve efficacy or reduce side effects by steering current away from anatomical structures that cause adverse effects [59] [60]. | A wider therapeutic window was demonstrated in 90% of cases in a large prospective trial [60]. Single-segment activation is recommended for maximal directionality [59]. |
| Interleaving/IL–IL Programming | A dual-frequency interleaving paradigm used to address both axial and appendicular symptoms in PD or to improve symptom control in ET [59] [60]. | Used in a subset of patients as an advanced programming strategy alongside directional stimulation [59]. The two interleaved programs can have different amplitudes, pulse widths, and active contacts [57]. |
| Low-Frequency Stimulation (LFS) | An alternative parameter set for ANT-DBS in epilepsy and explored for axial symptoms in PD [5] [57]. | In epilepsy, continuous LFS (7 Hz, 200 μs) showed superior seizure reduction (73%) vs. intermittent HFS (33%) [5]. In PD, LFS may improve gait and freezing [57]. |
Experimental Protocols for Clinical Programming
Protocol for Monopolar Review and Directional Steering
This foundational protocol is used to identify the optimal contact and configuration during initial programming sessions [30] [58].
Workflow Overview:
Detailed Methodology:
- Initiation and Baseline: Programming is typically initiated 2-4 weeks post-surgery to allow microlesion effects to subside and tissue impedance to stabilize [30]. Confirm the DBS lead location via post-operative imaging (e.g., CT co-registered with preoperative MRI) and check impedances for all contacts to ensure electrical integrity of the system [30].
- Parameter Initialization: Begin with standardized parameters: a pulse width of 60 μs and a frequency between 130-185 Hz [58]. The initial testing mode should be constant-current, which ensures a consistent current delivery regardless of impedance fluctuations, unlike constant-voltage [30].
- Ring Electrode Screening: In a monopolar configuration (contact as cathode, implantable pulse generator case as anode), test each ring contact separately [58]. Systematically increase the amplitude (e.g., in 0.1-0.5 mA steps) until a persistent therapeutic effect (e.g., reduction in rigidity or tremor) is observed. Continue increasing the amplitude to determine the threshold for stimulation-induced adverse effects [30] [58]. The therapeutic window is the difference between these two thresholds.
- Directional Segment Screening: Once the most effective ring contact is identified, proceed to test its individual directional segments [58]. Employ Single-Segment Activation (SSA) to maximize the axial asymmetry of the electrical field and achieve the greatest steering capability [59]. For each segment, repeat the amplitude titration to establish new thresholds for therapeutic and adverse effects.
- Final Configuration Selection: The final chronic stimulation configuration should be the contact or segment that provides the best clinical benefit with the widest therapeutic window, indicating a robust and tolerable setting [58].
Protocol for Interleaving Stimulation (IL-IL)
Interleaving stimulation uses two distinct programs delivered through the same DBS lead in an alternating, time-multiplexed fashion, allowing for the independent targeting of different neural pathways or symptoms [59] [57].
Workflow Overview:
Detailed Methodology:
- Patient Indication: Interleaving is considered when a patient presents with multiple symptom clusters (e.g., persistent appendicular tremor and axial gait symptoms) that cannot be adequately managed with a single stimulation program [59] [60].
- Program Definition: Design two separate programs (P1 and P2). These programs can have different active contacts (including directional segments), amplitudes, and pulse widths [57]. Crucially, they can also be set to different frequencies, though the device will deliver them in an interleaved manner such that the total output frequency is the sum of the two (with a maximum system output of 250 Hz) [57].
- Example: P1 could use a standard high-frequency (130 Hz) contact configuration optimized for tremor and rigidity, while P2 uses a ventral contact with a lower frequency (e.g., 60-80 Hz) to target axial symptoms [57].
- Titration and Clinical Testing: Activate the interleaving mode. The amplitudes for P1 and P2 must be titrated independently, as their thresholds for benefits and side effects will differ. A thorough clinical assessment of all target symptoms is necessary to find the optimal balance between the two programs [59].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Platforms for DBS Research and Programming
| Research Tool / Platform | Type | Primary Function in Research |
|---|---|---|
| Abbott Infinity DBS System | Commercial DBS System | Provides directional leads (6172) and a platform for clinical research on current steering and remote programming [59] [61]. |
| Lead-DBS Toolbox | Open-Source Software | Used for electrode reconstruction, atlas co-registration, and visualization of lead placement relative to anatomical targets in research analyses [14]. |
| OSS-DBS | Open-Source Software | Enables fast computation of the Volume of Tissue Activated (VTA) based on stimulation parameters and patient-specific anatomy, crucial for modeling stimulation effects [14]. |
| NeuroSphere Virtual Clinic | Remote Care Platform | Enables remote programming and adjustment of DBS parameters, facilitating decentralized clinical trials and improving patient access to care [61]. |
| Directional Lead (6172) | Hardware | A key research tool for investigating the effects of shaped electric fields on clinical outcomes and the therapeutic window [59]. |
| fMRI with DBS Cycling | Imaging & Paradigm | A research paradigm involving cycling DBS ON/OFF during fMRI acquisition to identify neural activation patterns associated with optimal stimulation [62]. |
Directional stimulation and interleaving programming represent significant advancements in DBS technology, moving beyond the limitations of conventional omnidirectional stimulation. Quantitative clinical data confirms that these techniques are widely adopted in practice to actively manage and widen the therapeutic window, primarily by enhancing symptom control and reducing side effects [59] [60]. The structured experimental protocols provided here offer a framework for researchers and clinicians to systematically implement and evaluate these advanced programming strategies. As DBS technology continues to evolve with increasingly complex lead designs, the role of these sophisticated programming techniques will become ever more critical. Future research directions include the development of automated, biomarker-driven programming algorithms and the deeper integration of patient-specific anatomical and functional imaging data to further refine and personalize therapy [14] [3].
Within deep brain stimulation (DBS) parameter settings research, a critical yet often underexplored factor influencing trial outcomes is the systematic management of patient expectations. For individuals with severe, treatment-refractory conditions, DBS represents a final therapeutic frontier, often leading to disproportionately high hopes that can jeopardize post-operative psychosocial adjustment and perceived success, even with optimized stimulation parameters [63] [64]. This application note synthesizes current evidence to provide detailed protocols for integrating expectation management into a comprehensive rehabilitation model, ensuring that technological advancements in parameter setting are complemented by robust psychological and educational support frameworks.
Quantitative Data on Expectations and Outcomes
Table 1: Impact of Patient Expectations on DBS Outcomes - Key Study Findings
| Study Focus | Study Design & Population | Key Findings on Expectations |
|---|---|---|
| Role of Expectations (Systematic Review) [64] | Systematic Review of 10 studies (n=272 PD patients) | - Patients' pre-operative expectations significantly contribute to treatment efficacy and post-operative satisfaction.- Unrealistic expectations are linked to poorer psychosocial adjustment post-DBS, regardless of objective motor improvement.- Experimental induction of positive expectations (placebo) can improve motor function, while negative expectations (nocebo) can worsen it. |
| Patient & Caregiver Qualitative Perspectives [63] | Prospective qualitative study (6 TRD patients, 5 caregivers) | - Decision for DBS is driven by treatment exhaustion and intolerability of life with depression, creating a "nothing to lose" mentality.- Life with active DBS is described as a "roller coaster," with unsustained mood improvements.- Participants expressed surprise at the lengthy, iterative process of parameter optimization. |
| Gait Improvement with Novel Parameters [17] | Multicenter, randomized, double-blind, crossover (n=14 PD patients) | - Preliminary results show specific motor improvements (e.g., single support time) are linked to particular parameter settings (short pulse width).- Highlights that benefits are parameter-specific and not a universal "cure," a key point for expectation setting. |
Experimental Protocols for Expectation Research and Management
Protocol for Assessing Pre-operative Patient Expectations
Objective: To quantitatively and qualitatively evaluate patient and caregiver expectations prior to DBS surgery, establishing a baseline for targeted education and post-operative support.
Methodology:
- Recruitment: Consecutive sampling of DBS candidates and their primary caregivers during pre-surgical screening.
- Data Collection:
- Semi-structured Interviews: Conduct separate, audio-recorded interviews with patients and caregivers. Key themes should cover:
- Understanding of DBS and its risks/benefits.
- Expectations for life after DBS (e.g., daily functioning, social roles, mood/motor symptoms).
- Awareness of the programming process and timeline.
- Sources of information that shaped their expectations [63].
- Standardized Questionnaires: Administer tools to quantify expectations. While the search results do not specify a single tool, studies in the field use ad-hoc or adapted questionnaires focusing on anticipated changes in symptoms, quality of life, and social functioning [64].
- Semi-structured Interviews: Conduct separate, audio-recorded interviews with patients and caregivers. Key themes should cover:
- Data Analysis:
- Qualitative: Employ iterative thematic analysis on interview transcripts to identify dominant themes, such as desperation, hope, and knowledge gaps [63].
- Quantitative: Analyze questionnaire data to score the level of expectations and identify patients with unrealistic or inflated hopes.
Protocol for a Randomized Controlled Trial on Expectation Management
Objective: To evaluate the efficacy of a structured educational intervention (vs. standard care) on aligning patient expectations with realistic outcomes and improving post-operative psychosocial adjustment.
Methodology:
- Design: Prospective, randomized, single-blind, controlled trial.
- Participants: Patients eligible for DBS for a neuropsychiatric or movement disorder.
- Intervention:
- Control Group: Receives standard informed consent and pre-operative education.
- Intervention Group: Receives a multi-component expectation management protocol including:
- Structured Counseling: A dedicated session focusing on DBS as one component of comprehensive rehabilitation, the iterative nature of programming, and the "burden of normality" [64] [10].
- Research Engagement Agreement: An IRB-approved document separate from the consent form, detailing mutual responsibilities, communication protocols, and the potential for incomplete symptom relief [10].
- Pamphlet of Resources: A guide to local, state, and federal agencies and support systems for psychosocial rehabilitation [10].
- Caregiver Involvement: Active inclusion of caregivers in all educational steps [63] [10].
- Outcome Measures: Assessed pre-operatively and at 3, 6, and 12 months post-operatively.
- Primary: Discrepancy between pre-operative expectations and post-operative reality (using a Likert-scale questionnaire).
- Secondary: Psychosocial adjustment scale, patient satisfaction score, depression/anxiety inventory, and quality of life measure [64].
Visualization of the Comprehensive DBS Rehabilitation Workflow
The following diagram illustrates the integrated workflow for managing patient expectations within the DBS and comprehensive rehabilitation pathway.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents and Tools for DBS Parameter and Expectation Research
| Item/Tool | Function/Application in Research |
|---|---|
| Lead-DBS Toolbox [25] | An open-source software for the reconstruction of DBS electrode localizations from post-operative medical imaging, crucial for correlating electrode position with clinical outcomes and modeling stimulation volumes. |
| OSS-DBS [25] | An open-source tool for simulating the Volume of Tissue Activated (VTA) based on specific DBS parameters and patient anatomy. Used to optimize stimulation settings and understand the physiological basis of effects. |
| Semi-Structured Interview Guides [63] | Qualitative research instruments designed to explore patient and caregiver perspectives, beliefs, and experiences in-depth. Essential for capturing nuanced data on expectations and subjective outcomes. |
| Expectation Quantification Questionnaires [64] | Standardized or ad-hoc instruments (e.g., Likert-scale surveys) used to quantitatively measure the level and nature of patient expectations before and after DBS intervention. |
| Computational Modeling Pipelines [25] | Custom or commercial pipelines (e.g., using Python, MATLAB) that integrate imaging, VTA simulations, and clinical scores to develop patient-specific, interpretable parameter settings. |
| Viz Palette Tool [65] | An online accessibility tool that allows researchers to test color palettes for data visualizations and figures to ensure they are interpretable by individuals with color vision deficiencies. |
Evaluating Efficacy and Outcomes: Metrics, Comparative Studies, and Research Gaps
Deep brain stimulation (DBS) therapeutic efficacy is highly dependent on accurate lead placement and optimized clinical programming [66]. The latter relies on clinicians' experience to search among available stimulation parameters and can be limited by the time constraints of clinical practice [66]. Recent innovations in device technology have expanded the number of possible electrode configurations and parameter sets available to clinicians, amplifying this challenge [66]. This document outlines application notes and protocols for validating novel computational algorithms against expert clinical programming, providing a standardized framework for researchers and drug development professionals working in neuromodulation.
The DBS Illumina 3D algorithm represents an inverse programming approach that automates selection of optimized stimulation parameters for overlapping the stimulation field model (SFM) with a desired anatomical or functional target [66]. This algorithm utilizes patient-specific imaging data paired with postoperative reconstruction of lead trajectory to search the available stimulation space and identify optimized stimulation parameters [66].
Key Algorithm Characteristics:
- Input: Preoperative neuroimaging data, postoperative lead trajectory reconstruction, clinician-defined benefit and avoidance regions
- Optimization Method: Inverse programming to maximize benefit-region coverage while minimizing stimulation of avoidance regions
- Output: Suggested electrode configurations and stimulation amplitudes
- Integration: Seamlessly integrated with clinician programmer software [66]
Quantitative Performance Data
Comparative Performance Metrics
Table 1: Algorithm vs. Clinical Programming Performance in Treatment-Resistant Depression
| Metric | Clinician Programming | Algorithm Programming | Statistical Significance |
|---|---|---|---|
| Target Coverage | Baseline reference | Similar or greater | Not significant |
| Stimulation Spillage Outside Target | Higher | Significantly smaller | P = 0.002 |
| Therapeutic Efficacy | Clinical standard | Equivalent or improved | Not reported |
| Programming Time | Multiple clinical visits | Rapid assistance | Not quantified |
fMRI-Based Prediction Performance
Table 2: Machine Learning Prediction of Optimal DBS Parameters in Parkinson's Disease
| Validation Cohort | Sample Size | Prediction Accuracy | Key Imaging Features |
|---|---|---|---|
| Training Set | 39 patients (35 STN-DBS, 4 GPi-DBS) | 88% | BOLD changes in motor circuit |
| Test Set 1 (A priori optimized) | 9 patients | Comparable accuracy | Preferential engagement of motor circuit |
| Test Set 2 (Stimulation-naïve) | 9 patients | Comparable accuracy | Ipsilateral thalamus, motor cortex responses |
Experimental Protocols
Patient-Specific Imaging Protocol
Objective: To acquire necessary neuroimaging data for algorithm input and validation.
Materials:
- 3T MRI scanner with appropriate DBS safety protocols
- T1-weighted anatomical imaging sequence (MPRAGE; 1mm isotropic)
- Diffusion weighted imaging data with multiple phase encoding directions
- Post-implantation CT scan for lead localization
Methodology:
- Acquire preoperative T1-weighted structural images
- Obtain diffusion weighted imaging data (92 diffusion-sensitizing gradient directions, b=2000 and b=1000)
- Perform stereotactic implantation of DBS leads
- Acquire post-implantation CT scan (0.67mm slice thickness)
- Co-register postoperative CT to preoperative structural scans
- Automatically extract trajectory and orientation of each DBS lead
- Verify lead placement by visual inspection [66]
fMRI Acquisition for Parameter Validation
Objective: To identify brain activity patterns associated with clinical benefits and predict optimal DBS parameters.
Materials:
- MRI-compatible DBS system with established safety profile
- 3T MRI scanner meeting DBS safety guidelines
- Paradigm for DBS-ON/OFF cycling (30s cycles, repeated 6 times)
Methodology:
- Establish safety protocols for fMRI in DBS patients
- Perform unilateral DBS stimulation at clinically defined optimal and non-optimal contacts or voltages
- Acquire fMRI data during DBS-ON/OFF cycling paradigm
- Preprocess fMRI data using established pipeline (motion and slice timing correction)
- Extract BOLD signal from 16 motor and non-motor regions-of-interest
- Normalize absolute t-values by mean positive t-values in areas presumed involved in non-optimal stimulation [62]
Algorithm Training and Validation Protocol
Objective: To train and validate machine learning models for predicting optimal DBS parameters.
Materials:
- Normalized BOLD changes from fMRI data
- Binary labeling of stimulation settings (optimal vs. non-optimal)
- Machine learning framework for classification
Methodology:
- Use normalized BOLD changes from clinically optimized patients as features
- Assign binary labels (optimal vs. non-optimal) to each stimulation setting
- Train machine learning model to classify stimulation settings based on fMRI patterns
- Validate model on unseen fMRI datasets acquired with different active contacts or voltages
- Assess model's ability to determine whether DBS setting was optimal or non-optimal according to corresponding fMRI pattern [62]
Visualization Framework
Algorithm Workflow Diagram
fMRI Validation Protocol
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for DBS Algorithm Validation Research
| Research Reagent | Function | Specifications |
|---|---|---|
| Directional DBS Leads | Enable precise current steering | 8 contacts in 1-3-3-1 electrode configuration |
| Multi-channel IPG | Deliver complex stimulation patterns | 16-contact rechargeable pulse generator |
| 3T MRI Scanner | High-resolution neuroimaging | DBS safety protocols, diffusion sequences |
| Neural Navigator Software | Visualization and programming interface | Integration with optimization algorithms |
| Finite Element Modeling | Stimulation field modeling | COMSOL Multiphysics with multi-resolute mesh |
| Diffusion Tensor Imaging | Tractography-guided targeting | 92 diffusion-sensitizing gradient directions |
| Lead Localization Module | Postoperative trajectory reconstruction | Automatic extraction with visual verification |
| fMRI Analysis Pipeline | BOLD signal processing | Motion correction, slice timing correction |
The validation framework presented establishes that algorithmic approaches to DBS programming can achieve equivalent or superior target engagement compared to expert clinical programming while significantly reducing stimulation outside target regions. The integration of patient-specific neuroimaging with computational optimization represents a paradigm shift in DBS therapy development, offering the potential to reduce programming time and improve therapeutic outcomes across neurological and psychiatric indications. Future research should focus on multi-center validation and expansion to additional DBS indications where programming challenges are particularly pronounced.
Motor Symptom Scales vs. Functional and Quality of Life Outcomes (DBS-QoL)
The optimization of Deep Brain Stimulation (DBS) for Parkinson's disease (PD) relies on the quantitative assessment of treatment efficacy. While motor symptom improvement is a primary target, the ultimate goal of therapy is to enhance the patient's day-to-day functioning and Quality of Life (QoL). This document provides application notes and experimental protocols for the standardized evaluation of DBS outcomes, correlating established motor symptom scales with functional and QoL measures. This work is situated within a broader thesis on DBS parameter settings, aiming to provide researchers and clinicians with a robust framework for a comprehensive, multi-dimensional assessment of therapeutic success. The following sections detail the key metrics, present quantitative comparisons, and outline standardized protocols for their application in clinical research.
Key Outcome Measures and Quantitative Comparisons
The following tables summarize the core assessment tools and comparative data on the efficacy of different surgical interventions for PD.
Table 1: Core Assessment Scales for DBS Outcome Measurement
| Scale Acronym | Full Name | Domain Measured | Score Range & Interpretation | Key References |
|---|---|---|---|---|
| UPDRS-III | Unified Parkinson's Disease Rating Scale, Part III | Motor Examination | 0-132 (MDS-UPDRS); Lower scores indicate better motor function. | [67] [68] |
| MDS-UPDRS-III | Movement Disorder Society-Revision of UPDRS, Part III | Motor Examination | 0-132; Lower scores indicate better motor function. | [68] [61] |
| PDQ-39 | 39-Item Parkinson's Disease Questionnaire | Health-Related Quality of Life | 0-100; Lower scores indicate better QoL. | [67] [61] |
| PDQ-8 | 8-Item Parkinson's Disease Questionnaire | Health-Related Quality of Life | 0-100; Lower scores indicate better QoL. | [68] |
| PGI-C | Patient Global Impression of Change | Patient-Rated Improvement | 7-point scale (1="Very much improved" to 7="Very much worse"). | [61] |
| SIP | Sickness Impact Profile | Health-Related Quality of Life | 0-100; Lower scores indicate better functioning. | [67] |
Table 2: Comparative Efficacy of DBS Targets and MRgFUS on Motor and QoL Outcomes (Network Meta-Analysis) [67]
| Intervention | UPDRS-III Off-Phase (SMD vs. MT) | UPDRS-III On-Phase (SMD vs. MT) | QoL (SMD vs. MT) | SUCRA Ranking (UPDRS Off) | SUCRA Ranking (UPDRS On) | SUCRA Ranking (QoL) |
|---|---|---|---|---|---|---|
| STN_DBS | -0.94 (CI: -1.40 to -0.48) | -0.83 (CI: -1.13 to -0.53) | -0.75 (CI: -1.46 to -0.05) | 69.1% (3rd) | 69.6% (2nd) | 67.3% (2nd) |
| GPi_DBS | Not Significant | -0.80 (CI: -1.20 to -0.40) | -0.58 (CI: -0.96 to -0.21) | Not Top 3 | 66.9% (3rd) | 77.2% (1st) |
| STN_FUS | Not Reported | -1.83 (CI: -2.97 to -0.68) | Not Significant | 79.6% (1st) | 95.7% (1st) | 56.9% (3rd) |
| Medication (MT) | Reference | Reference | Reference | - | - | - |
Abbreviations: SMD, Standardized Mean Difference (negative values favor intervention); CI, Confidence Interval; MT, Medication Therapy; SUCRA, Surface Under the Cumulative Ranking (higher % indicates better relative performance).
Table 3: Remote vs. In-Clinic DBS Optimization Timelines (Randomized Controlled Trial) [61]
| Optimization Group | Time to 1-Point PGI-C Improvement (Days) | Key Protocol Features |
|---|---|---|
| In-Clinic (IC) Only (n=48) | 54.2 (SD 3.7) | Standard of care; parameter adjustments during clinic visits. |
| Remote Internet-Based (RIBA) (n=48) | 39.1 (SD 3.3) | Adjustments via secure mobile application; decentralized data collection. |
Experimental Protocols for DBS Outcome Assessment
Protocol for Longitudinal Assessment of DBS and QoL Outcomes
Application: To systematically evaluate the long-term impact of DBS parameter adjustments on both motor symptoms and quality of life in PD patients.
Workflow Diagram:
Procedure:
- Baseline Assessment: Conduct a comprehensive pre-operative evaluation. Collect demographic data, disease duration, and baseline scores using the MDS-UPDRS-III (in defined OFF and ON medication states) and the PDQ-39 QoL questionnaire [67] [61].
- Intervention & Randomization: Following DBS implantation and initial parameter configuration, randomize patients into study groups (e.g., in-clinic optimization vs. remote internet-based adjustment) [61].
- Longitudinal Data Collection:
- Motor Symptoms: Administer the MDS-UPDRS-III at scheduled follow-ups (e.g., 1, 3, and 5 years). Assessments should be performed in the stim-ON condition, with consistent medication states (e.g., ON) to isolate the effect of DBS [68].
- Quality of Life: Administer the PDQ-39 or PDQ-8 at the same intervals [67] [68].
- Patient Global Impression: Collect Patient Global Impression of Change (PGI-C) scores to capture patient-perceived benefits [61].
- Data Analysis: Perform statistical analysis (e.g., linear mixed-effects models) to track changes in motor and QoL scores over time. Calculate correlation coefficients (e.g., Pearson's r) between the change in UPDRS-III scores and the change in PDQ-39 summary index scores from baseline to evaluate the relationship between motor improvement and QoL enhancement.
Protocol for Automated DBS Programming Using Biomarkers
Application: To employ objective biomarkers and search algorithms for the automated or guided optimization of DBS parameters, reducing reliance on subjective clinical ratings.
Workflow Diagram:
Procedure:
- Selection of Biomarker:
- Wearable Sensors: Fit patients with inertial measurement units (IMUs) on limbs. Use validated algorithms to quantify tremor amplitude, bradykinesia scores, and rigidity from the sensor data [69].
- Local Field Potentials (LFP): Utilize the implanted DBS system to record resting beta power (13-35 Hz) from the target nucleus (e.g., STN). The contact with the highest beta power may indicate the optimal trajectory for stimulation [69].
- Configuration of Search Algorithm:
- Implement a search algorithm (e.g., Bayesian optimization) to efficiently navigate the parameter space (contacts, amplitude, pulse width). The algorithm's objective function is to maximize the biomarker-derived benefit score [69].
- Iterative Optimization Loop:
- The algorithm selects a new DBS parameter set and applies it.
- The biomarker (e.g., beta power suppression or tremor power from wearables) is recorded and quantified as an outcome score.
- This score is fed back to the algorithm, which selects the next parameter set to test.
- Termpoint and Validation: The loop continues until a predefined stopping criterion is met (e.g., no significant improvement after several iterations). The final parameter set should be validated with a standard clinical motor examination (MDS-UPDRS-III) and patient-reported outcomes to ensure therapeutic benefit and absence of side-effects.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Tools for DBS-QoL Research
| Item | Function/Application in Research | Specific Examples/Notes |
|---|---|---|
| Clinical DBS System | Provides therapeutic stimulation and, in modern systems, sensing capabilities. | Systems with sensing-enabled implants (e.g., for LFP recording) and compatible programmers are essential for biomarker studies [69]. |
| Validated Motor Scale | Gold-standard quantitative assessment of motor symptoms. | MDS-UPDRS-III is the revised standard; requires trained, certified raters for reliable administration [67] [68]. |
| QoL Questionnaire | Captures patient-perceived health status and functional impact. | PDQ-39 (comprehensive) or PDQ-8 (abbreviated); self-administered or via interview [67] [61]. |
| Wearable Motion Sensors | Objective, continuous measurement of motor symptoms (tremor, bradykinesia). | Accelerometers and gyroscopes embedded in wrist-worn devices or full-body suits [69] [61]. |
| Neurophysiology Signal Processor | For acquiring and analyzing biomarker signals from the implanted device. | Software for visualizing and quantifying LFP (e.g., beta power) and evoked potentials (e.g., DLEP/ERNA) [69]. |
| Telemedicine Platform | Enables remote DBS programming and decentralized data collection in clinical trials. | Secure applications that allow clinicians to adjust stimulation parameters and collect PROs from patients' homes [61]. |
| Data Analysis Software | For statistical analysis and modeling of longitudinal clinical and biomarker data. | Platforms like R, Python, or Stata capable of running linear mixed-effects models and network meta-analyses [67]. |
Deep brain stimulation (DBS) represents a well-established neurosurgical intervention for movement disorders with a rapidly expanding spectrum of clinical applications [44]. The growing number of DBS publications reflects increasing investigation across neurological and psychiatric conditions, though randomized trials remain outnumbered by case reports in emerging applications [44]. Understanding differential treatment responses between primary and secondary dystonia provides crucial insights for optimizing stimulation parameters and developing personalized therapy approaches. This document establishes application notes and experimental protocols for comparative DBS effectiveness research, framed within the broader context of deep brain stimulation parameter optimization.
Pathophysiological Distinctions and Clinical Implications
Fundamental pathophysiological differences between primary and secondary dystonia underlie their varied responses to DBS therapy. While both disorders manifest similar clinical symptoms, their underlying mechanisms differ significantly [70].
Primary dystonia is characterized by reduced inhibition at multiple levels of the motor system, increased plasticity, and emerging evidence suggests cerebellar involvement [70]. Electrophysiological studies demonstrate abnormally enhanced cortical plasticity and reduced cerebellar-dependent conditioning in these patients.
Secondary dystonia results from identifiable lesions in basal ganglia or thalamic regions yet exhibits normal cortical plasticity responses and absent functional cerebellar involvement [70]. The preserved cerebellar function and normal response to plasticity protocols distinguish secondary from primary dystonia pathophysiologically.
These mechanistic differences explain the variable therapeutic outcomes observed clinically and underscore the necessity for disorder-specific parameter optimization strategies in DBS programming.
Comparative Data Synthesis
Table 1: Electrophysiological Profile Comparison Between Primary and Secondary Dystonia
| Electrophysiological Parameter | Primary Dystonia | Secondary Hemidystonia | Measurement Technique |
|---|---|---|---|
| Short-interval Intracortical Inhibition | Reduced | Reduced on affected side only | Transcranial Magnetic Stimulation (TMS) |
| Cortical Plasticity | Significantly increased | Normal response | Paired Associative Stimulation |
| Cerebellar Function | Reduced conditioning | Normal conditioning | Eye Blink Classical Conditioning |
| Resting Motor Threshold | Normal | Normal | Transcranial Magnetic Stimulation |
| Cortical Silent Period | Normal | Normal | Transcranial Magnetic Stimulation |
Table 2: DBS Clinical Trial Phases for New Indications
| Research Phase | Primary Objectives | Methodological Approach | Sample Considerations |
|---|---|---|---|
| Preclinical | Target identification; Safety and feasibility assessment; Therapeutic window estimation | Animal models; Literature review; Retrospective human studies; LFP recordings [44] | Translational models; Focus on core symptoms rather than multifaceted disorders [44] |
| Phase 1 | Evaluate target safety; Determine therapeutic stimulation parameters; Identify side effects | First-in-human implantation; Therapeutic window mapping; Adverse effect monitoring [44] | Small patient groups; Careful trajectory planning to avoid ventricles and vasculature [44] |
| Phase 2 | Further safety evaluation; Preliminary effectiveness testing | Controlled stimulation parameters; Standardized outcome measures; Biomarker identification [44] | Small to medium patient groups; Initial comparative effectiveness assessment |
| Phase 3 | Confirm effectiveness; Monitor long-term effects; Compare to existing treatments | Randomized controlled designs; Blinded assessment; Multi-center collaboration [44] | Medium to large patient groups; Extended follow-up periods |
| Phase 4 | Post-approval surveillance; Refine best use parameters | Longitudinal observational studies; Registry data analysis; Real-world outcomes [44] | Broader patient populations; Diverse clinical settings |
Experimental Protocols for DBS Research
Electrophysiological Characterization Protocol
Objective: Systematically evaluate neurophysiological differences between primary and secondary dystonia patients using transcranial magnetic stimulation and conditioning paradigms.
Materials:
- Transcranial magnetic stimulation apparatus with figure-eight coil
- Electromyography recording equipment
- Eye blink classical conditioning setup
- Standardized patient positioning system
Methodology:
- Participant Preparation: Secure informed consent; Position participants comfortably in reclining chair; Apply surface electrodes to first dorsal interosseous muscle bilaterally.
- Motor Threshold Determination: Establish resting motor threshold (RMT) for each hemisphere defined as minimum stimulus intensity required to elicit motor evoked potentials >50μV in 5 of 10 consecutive trials.
- Intracortical Inhibition Assessment: Deliver paired-pulse TMS protocols with interstimulus intervals of 2-5ms using conditioning stimulus intensity of 80% RMT and test stimulus intensity of 120% RMT.
- Cortical Plasticity Evaluation: Implement paired associative stimulation protocol with 90 paired electrical median nerve stimuli and TMS pulses at 25ms interstimulus interval delivered at 0.1Hz.
- Cerebellar Function Testing: Administer eye blink classical conditioning paradigm with tone conditioned stimulus followed by corneal air puff unconditioned stimulus at 500ms interval.
- Data Analysis: Compare all parameters between patient groups and healthy controls using appropriate statistical methods with correction for multiple comparisons.
Expected Outcomes: Primary dystonia patients demonstrate reduced intracortical inhibition, enhanced cortical plasticity, and impaired cerebellar conditioning compared to secondary dystonia patients and healthy controls [70].
Computational Modeling and Electrode Characterization Protocol
Objective: Develop validated computational models of neural activation for DBS parameter optimization through comprehensive electrode characterization.
Materials:
- Microelectrodes for implantation
- Impedance spectroscopy equipment
- High-resolution microscopy capabilities
- Computational modeling software (open-source platforms recommended)
- Histological preparation and analysis tools
Methodology:
- Pre-implantation Electrode Characterization:
- Perform detailed geometrical characterization of electrodes using microscopy techniques
- Conduct in vitro impedance spectroscopy across frequency ranges
- Create precise computational models of electrode geometry
In Vivo Validation:
- Implant characterized electrodes according to standardized surgical protocols
- Measure in vivo impedance spectra post-implantation
- Adjust computational models based on empirical impedance data
Tissue Activation Modeling:
- Incorporate characterized electrode geometry into volume of tissue activated (VTA) models
- Account for tissue distribution and dielectric properties
- Validate model predictions against physiological measurements
Parameter Optimization:
- Test multiple stimulation parameter sets in silico
- Predict neural activation patterns for each parameter combination
- Identify optimal stimulation settings for experimental validation
Validation Metrics: Compare model-predicted activation volumes with empirically observed therapeutic outcomes; Quantify accuracy improvements relative to unvalidated models [47].
Analytical Workflows and Data Visualization
DBScope Analytical Workflow for Chronic Sensing Data
The DBScope toolbox provides a comprehensive analytical framework for visualizing and interpreting sensing data from advanced DBS neurostimulators [71]. This open-source computational toolbox enables both clinical application and research investigation through user interface and programmatic access.
DBS Research Pathway for New Indications
The development of DBS applications for new clinical indications requires systematic progression through established research phases with decision points based on accumulating evidence [44].
Research Reagent Solutions
Table 3: Essential Research Tools for DBS Investigation
| Tool/Technology | Primary Function | Application Examples | Key Features |
|---|---|---|---|
| DBScope Toolbox | Visualization and analysis of chronic sensing data [71] | Clinical session review; Longitudinal analysis; Biomarker identification | User interface and programmatic access; ECG cleaning tool; Multiple sensing mode support |
| Transcranial Magnetic Stimulation | Assessment of cortical excitability and plasticity [70] | Differential diagnosis; Pathophysiological mechanism investigation; Treatment monitoring | Non-invasive cortical measurement; Multiple protocol options (SICI, CSP, PAS) |
| Computational Modeling Framework | Prediction of neural activation patterns [47] | Electrode characterization; Stimulation parameter optimization; Tissue activation prediction | Open-source platform; Impedance spectroscopy integration; Geometrical accuracy |
| Local Field Potential Recording | Chronic sensing of neural signals during stimulation [44] | Biomarker discovery; Therapy response monitoring; Adaptive stimulation development | Real-time signal acquisition; Stimulation artifact management; Ambulatory monitoring capability |
| Eye Blink Classical Conditioning | Cerebellar function assessment [70] | Differential pathophysiology evaluation; Cerebellar network involvement determination | Simple paradigm; Reliable cerebellar-dependent measure; Quantitative output metrics |
Application Note
This application note addresses a critical methodological gap in neuromodulation research, specifically the under-investigation of functional outcomes in Deep Brain Stimulation (DBS) for neurodevelopmental disorders (NDDs). While DBS parameter optimization has advanced significantly in movement disorders, comparable frameworks for measuring functional improvements in NDD populations remain underdeveloped. We synthesize current evidence, provide structured experimental protocols, and identify essential research tools to standardize the assessment of functional outcomes—defined as real-world adaptive skills, quality of life, and independence metrics—in populations with co-occurring NDDs and severe mood disorders. This framework aims to equip researchers with methodologies to bridge the translational gap between neurological targeting and meaningful clinical benefits.
Quantitative Evidence Synthesis: Current Landscape of NDD and DBS Outcomes
Table 1: Documented Associations Between NDDs and Clinical Outcomes
| Number of Co-occurring NDDs | Prevalence in Clinical Sample | Key Associated Clinical Factors | Impact on Treatment |
|---|---|---|---|
| None | 67% | Baseline reference group | Standard treatment protocols |
| One | 18% | Increased symptom duration, persistent irritability | Moderate protocol adjustment |
| Two | 7% | Higher rates of disruptive behavioral disorders | Significant multidisciplinary input required |
| Three or More | 7% (3: 5%, 4+: 2%) | Lower baseline functioning (CGAS score) | High probability of polypharmacy |
Source: Adapted from a multicenter observational study (n=305) [72].
Table 2: DBS Outcome Measurement Modalities Across Disorders
| Disorder Category | Common Outcome Biomarkers | Functional Outcome Assessment Gaps | Translational Potential for NDDs |
|---|---|---|---|
| Movement Disorders (PD) | Wearable sensors (tremor, bradykinesia), Local Field Potentials (beta power), fMRI motor circuit activation [3] [62] | Minimal – biomarkers closely linked to functional motor improvement | Limited – NDD functional outcomes are multidimensional (social, cognitive) |
| Treatment-Resistant Depression | Clinical rating scales (e.g., HAM-D), self-report mood inventories [73] | Moderate – mood improvement does not automatically equate to functional recovery | Moderate – requires coupling with measures of social/occupational function |
| Neurodevelopmental Disorders | Primarily behavioral observation, caregiver report, cognitive testing [72] | Critical – lack of objective, brain-based biomarkers predicting functional improvement | High – urgent need for validated biomarkers tied to real-world functioning |
Proposed Experimental Protocols for Functional Outcome Research
Protocol: Integrating Functional Measures into DBS Trials for NDDs
Objective: To evaluate the efficacy of DBS parameter settings on functional outcomes in individuals with NDDs and co-occurring severe mood disorders.
Background: Evidence suggests treatments for mood disorders demonstrate comparable effectiveness regardless of NDD co-occurrence [72]. However, individuals with NDDs present with more complex clinical profiles, including persistent irritability, disruptive behaviors, and lower global functioning, necessitating modified outcome assessments.
Materials:
- Patient Cohort: Adolescents or adults with diagnosed NDDs (e.g., ASD, ADHD, intellectual disability) and a co-occurring severe mood disorder eligible for DBS.
- DBS System: A sensing-enabled DBS system (e.g., Medtronic Percept PC) capable of recording Local Field Potentials (LFPs) [3].
- Assessment Tools:
- Children's Global Assessment Scale (CGAS) or WHODAS 2.0 for functional impairment.
- Standardized mood scales (e.g., HAM-D for depression).
- NDD-specific functional battery: Direct assessment of adaptive behavior skills (e.g., Vineland-3), social responsiveness, and goal-directed task performance.
Procedure:
- Pre-operative Baseline (T0): Conduct comprehensive clinical phenotyping, including the number and type of co-occurring NDDs. Administer full assessment battery.
- DBS Implantation & Lead Reconstruction: Implant DBS electrodes in the target of interest (e.g., VC/VS, SCC). Reconstruct lead locations using postoperative imaging integrated with tools like Lead-DBS [14].
- Initial Programming & Parameter Titration:
- Utilize a geometry-based optimization approach to simulate the Volume of Tissue Activated (VTA) and suggest initial contacts and current amplitudes [14].
- Titrate amplitude while monitoring for acute adverse effects and collecting LFP data.
- Outcome Evaluation Phase (T1, T2...Tn):
- At each follow-up, concurrently collect:
- Clinical Data: Mood scores, adverse effects log.
- Neurophysiological Data: LFP biomarkers (e.g., beta power in movement disorders; potential candidates like theta/alpha for NDDs under investigation) [3].
- Functional Data: CGAS/WHODAS, NDD-specific functional battery.
- Correlate stimulation parameters (contact, amplitude, pulse width) and LFP biomarkers with changes in functional outcome scores.
- At each follow-up, concurrently collect:
- Data Analysis:
- Employ machine learning models (e.g., support vector machines, multilayer perceptrons) to identify patterns of brain response (e.g., via fMRI) or LFP features that predict optimal functional outcomes [62].
- The primary outcome is the effect size of change in functional measures (e.g., CGAS), not just symptom reduction.
Workflow: From DBS Programming to Functional Outcome Assessment
Diagram 1: Functional outcome assessment workflow.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Key Resources for DBS and Functional Outcome Research
| Category | Item/Solution | Primary Function in Research | Example Use Case |
|---|---|---|---|
| Neuroimaging & Analysis | Lead-DBS Toolbox | Reconstructs DBS electrode placement from MRI/CT data; enables VTA modeling [14] | Coregistration of lead location with individual anatomy and normative atlases. |
| OSS-DBS | Open-source simulator for calculating the Volume of Tissue Activated (VTA) [14] | Predicting neural pathway activation for different stimulation parameters. | |
| Physiological Sensing | Sensing-enabled DBS Implant (e.g., Percept PC) | Records chronic Local Field Potentials (LFPs) from the stimulation target [3] | Capturing neural biomarkers (e.g., beta oscillations) correlated with clinical state. |
| Wearable Sensors | Accelerometers, Gyroscopes (wrist-worn) | Provides objective, continuous measurement of motor activity and behavior [3] | Quantifying tremor or akinesia in PD; potential for measuring agitation/restlessness in NDDs. |
| Clinical Assessment | Children's Global Assessment Scale (CGAS) | Numeric scale (1-100) measuring general functional impairment in children [72] | Primary functional outcome metric in adolescent populations with NDDs. |
| WHODAS 2.0 | Standardized assessment of health and disability across domains [72] | Measuring functional outcomes in adult DBS trials. | |
| Computational Modeling | Machine Learning Models (SVM, MLP) | Identifies complex patterns in neuroimaging or physiological data to predict optimal settings [62] | Using fMRI activation maps to classify a DBS parameter set as optimal or non-optimal. |
Proposed Neural Signaling Pathway Linking DBS to Functional Change
Diagram 2: Proposed pathway from DBS to functional gains.
This pathway hypothesizes that effective DBS normalizes circuit dysfunction, which manifests in measurable neurophysiological changes. These changes subsequently facilitate improved cognitive and emotional processes, which are the foundational components of real-world functional improvement. Research must now focus on validating these links within NDD populations.
Deep Brain Stimulation (DBS) represents a transformative therapy for neurological and neuropsychiatric disorders, yet establishing optimal stimulation parameters remains a significant challenge in the field. The evidence hierarchy provides a structured framework for evaluating the quality of medical research, with systematic reviews and well-designed clinical trials occupying its apex. Despite their critical importance, these high-level evidence sources are frequently underrepresented in the DBS parameter settings literature, leading to potential gaps in clinical guidance. This underrepresentation is particularly problematic given the intricate dose-response relationships and highly individualized nature of neuromodulation therapies. The reliance on lower levels of evidence can perpetuate clinical uncertainty and variability in patient outcomes. This article examines the position of clinical trials and systematic reviews within the evidence pyramid, analyzes their current representation in DBS parameter research, and provides detailed protocols to strengthen the evidence base for DBS therapy optimization.
The Evidence Pyramid in Medical Research
Hierarchical Organization of Evidence
The evidence hierarchy, often visualized as a pyramid, systematically categorizes medical research based on its methodological rigor and potential for bias. This structured approach enables clinicians and researchers to quickly identify the most reliable forms of evidence for informing clinical decisions.
Table 1: Levels of the Evidence Hierarchy
| Evidence Level | Study Type | Key Characteristics | Strength |
|---|---|---|---|
| Highest | Systematic Reviews & Meta-Analyses | Comprehensively identifies, appraises, and synthesizes all relevant studies | Minimizes bias through exhaustive, systematic methodology |
| Randomized Controlled Trials (RCTs) | Participants randomly allocated to intervention or control groups | Reduces selection bias; establishes causality | |
| Intermediate | Cohort Studies | Follows groups with/without exposure over time | Establishes temporal sequence; good for prognosis |
| Case-Control Studies | Compares cases with condition to controls without | Efficient for rare diseases; assesses associations | |
| Foundational | Case Reports/Series | Detailed reports on individual patients or small groups | Identifies rare events; generates hypotheses |
| Laboratory Research | Basic science and animal studies | Elucidates mechanisms; preliminary investigation |
The foundation of the pyramid consists of laboratory studies and case reports, which generate initial hypotheses but have limited generalizability. Ascending the pyramid, observational studies like cohort and case-control designs provide stronger evidence for associations but remain susceptible to confounding. At the apex, systematic reviews and meta-analyses represent the most comprehensive evidence synthesis, while randomized controlled trials (RCTs) provide the most reliable data for evaluating therapeutic efficacy [74].
Evolution of Evidence Pyramid Models
The conceptual model of the evidence hierarchy has evolved significantly, with recent iterations like the "5S" model proposed by Haynes providing more practical guidance for evidence retrieval in clinical practice [74]. This model organizes resources from base to apex as: Studies (original investigations), Syntheses (systematic reviews), Synopses (structured abstracts of studies and syntheses), Summaries (integrated evidence-based guidelines), and Systems (clinical decision support systems that automatically link individual patient characteristics to relevant evidence). This refined model acknowledges that not all evidence syntheses are equivalent and provides a more nuanced approach to evidence-based clinical decision-making [74].
Underrepresentation in DBS Parameter Settings Research
Current Gaps in High-Quality Evidence
The field of DBS parameter optimization faces significant challenges in generating high-quality evidence, creating a reliance on lower levels in the evidence hierarchy. Several factors contribute to this underrepresentation:
Methodological Complexity: DBS trials involve substantial methodological challenges, including ethical constraints against sham surgeries, difficulties with blinding, and the individualized nature of therapy response [11] [75]. These complexities often limit the feasibility of large-scale RCTs.
Technical Limitations: Traditional DBS programming relies on time-consuming empirical approaches where clinicians systematically test parameters while assessing symptom response [76]. The recent development of advanced DBS systems with thousands of possible parameter combinations further complicates systematic evaluation [76].
Limited Diversity in Trial Populations: Historical data shows significant underrepresentation of minority groups in clinical trials, with Black and Hispanic populations frequently accounting for less than 10% of participants despite potentially higher disease burdens for certain conditions [77]. This limited diversity reduces the generalizability of trial findings across real-world populations.
Quantitative Evidence Assessment
Table 2: Evidence Distribution in DBS Research (2025)
| Evidence Type | Number of Identified Studies | Key Focus Areas | Notable Gaps |
|---|---|---|---|
| Systematic Reviews | Limited (e.g., 1 comprehensive methodology guide [78]) | Methodological approaches for DBS trials | Lack of reviews specifically on parameter optimization |
| Randomized Trials | Active but limited (e.g., 33+ listed for neuropsychiatric indications [11]) | Efficacy of DBS for new indications; limited parameter comparisons | Few trials comparing programming strategies |
| Observational Studies | Numerous (e.g., multiple cohorts for PD [76] [15]) | Contact selection; biomarker validation | Heterogeneous methodologies limit comparability |
| Case Series/Reports | Extensive documentation | Novel programming approaches; adverse events | Limited generalizability |
Recent analyses of clinicaltrials.gov searches conducted in February 2025 identified 33 active clinical trials testing DBS for neuropsychiatric indications, demonstrating significant research activity [11] [75]. However, the majority focus on establishing efficacy for new disease indications rather than systematically comparing parameter optimization strategies. This distribution reveals a critical gap in high-quality evidence specifically addressing DBS programming approaches.
Protocols for Enhancing Evidence Quality
Systematic Review Protocol for DBS Parameter Evidence
Systematic reviews provide a methodological framework for comprehensively synthesizing existing evidence. The following protocol outlines a rigorous approach for reviewing DBS parameter settings literature:
Step 1: Formulating the Research Question Utilize the PICO framework (Population, Intervention, Comparison, Outcome) to structure a clinically relevant question [78] [74]:
- Population: Patients with specific DBS indications (e.g., Parkinson's disease, OCD, depression)
- Intervention: Specific DBS parameter settings (e.g., amplitude, frequency, pulse width, contact selection)
- Comparison: Alternative parameter settings or standard care
- Outcome: Standardized efficacy measures (e.g., UPDRS for PD, YBOCS for OCD) and adverse effects
Step 2: Comprehensive Literature Search Execute a systematic search across multiple databases including PubMed/MEDLINE, Embase, Cochrane Central, and clinical trial registries [78] [79]. Incorporate gray literature to mitigate publication bias. Utilize Boolean operators and database-specific subject headings (e.g., MeSH terms) to maximize sensitivity and specificity.
Step 3: Study Selection and Data Extraction Employ dual independent reviewers for study selection and data extraction to minimize bias [79]. Utilize systematic review software such as Covidence or Rayyan to manage the screening process. Develop standardized data extraction forms to capture:
- Study characteristics (design, duration, funding)
- Participant demographics (ensuring diversity reporting)
- Intervention details (DBS parameters, programming methods)
- Outcome measures and adverse events
Step 4: Quality Assessment and Synthesis Evaluate methodological quality using appropriate tools (e.g., Cochrane Risk of Bias Tool, Newcastle-Ottawa Scale) [78]. For quantitative synthesis, employ meta-analytical techniques if studies are sufficiently homogeneous. For heterogeneous studies, utilize narrative synthesis approaches following established guidelines such as Synthesis Without Meta-Analysis (SWiM) [78].
Clinical Trial Protocol for DBS Parameter Optimization
Well-designed clinical trials are essential for generating high-quality evidence regarding DBS parameter efficacy. The following protocol addresses common limitations in current DBS research:
Trial Design Considerations
- Adaptive Designs: Utilize response-adaptive randomization to efficiently allocate participants to more promising parameter sets based on interim analyses [76]
- Crossover Designs: Implement carefully controlled within-participant crossover designs to enhance statistical power while managing ethical concerns regarding sham periods [75]
- Blinding Procedures: Develop rigorous blinding protocols for both participants and outcome assessors, utilizing active sham stimulation where feasible
Participant Diversity and Inclusion Actively recruit diverse participant populations that reflect the real-world epidemiology of the condition being treated. Develop inclusive recruitment strategies that address historical barriers to trial participation in underrepresented communities [77]. Report demographic characteristics comprehensively in publications to enhance generalizability.
Outcome Measurement Standardization Implement standardized, validated outcome measures specific to the condition being treated. Incorporate both clinician-rated and patient-reported outcomes to capture the full therapeutic impact. For Parkinson's disease trials, utilize ecological momentary assessments (EMA) to capture real-world symptom fluctuations [15].
Ethical Framework and Participant Safety Adhere to the foundational principles of the Belmont Report: Respect for Persons, Beneficence, and Justice [11] [75]. Establish explicit criteria for prematurely exiting a sham condition due to clinical decompensation. Implement comprehensive safety monitoring protocols with independent data safety monitoring boards for larger trials.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for DBS Evidence Generation
| Tool Category | Specific Tools | Application in DBS Research | Key Features |
|---|---|---|---|
| Systematic Review Software | Covidence, Rayyan | Streamlining study selection and data extraction | Dual independent review; discrepancy resolution |
| Reference Management | EndNote, Zotero, Mendeley | Organizing literature sources | Duplicate detection; citation formatting |
| Statistical Analysis | R, RevMan, Python | Meta-analysis; quantitative synthesis | Forest plots; heterogeneity assessment; publication bias tests |
| Clinical Trial Platforms | ClinicalTrials.gov registry | Protocol registration; results reporting | Meets FDA reporting requirements; enhances transparency |
| Data Collection Tools | Electronic data capture systems | Standardized outcome assessment | REDCap; Medrio; Castor EDC |
| Neuroimaging Analysis | Lead-DBS, FSL, SPM | Electrode localization; target verification | Normalization to standard space; connectivity analysis |
| Electrophysiology Analysis | FieldTrip, EEGLAB, MNE | Local field potential analysis; biomarker identification | Spectral analysis; coherence measures; machine learning |
Advanced Methodologies: Machine Learning and Biomarker-Driven Approaches
Electrophysiological Biomarkers for Parameter Optimization
Recent advances in electrophysiological biomarker research offer promising approaches for evidence-based DBS parameter selection. Machine learning algorithms can integrate multiple neural features to predict optimal stimulation parameters:
Feature Selection and Model Development
- STN Power Features: Subthalamic power across multiple frequency bands (theta, alpha, beta, gamma, HFO) provides predictive information for therapeutic windows [76]
- STN-Cortex Coherence: Functional connectivity between stimulation target and cortical regions enhances prediction accuracy [76]
- Multimodal Integration: Combining electrophysiological features with anatomical information (distance to sweet spots) further improves model performance [76]
Validation Framework Implement rigorous cross-validation approaches such as leave-one-electrode-out (LOEO) validation to assess model generalizability [76]. External validation in independent cohorts is essential before clinical implementation.
Adaptive DBS Programming Protocols
The emergence of adaptive DBS systems requires new evidence-generation frameworks for parameter optimization:
Biomarker Selection and Threshold Definition
- Beta Peak Identification: Conduct signal tests in OFF medication state to ensure reliable biomarker detection [15]
- Threshold Optimization: Set long-term evolution (LTE) thresholds based on percentiles of daytime beta power, with individual adjustment based on symptom response [15]
- Stimulation Limit Determination: Establish minimum and maximum amplitude limits through systematic testing in both ON and OFF medication states [15]
Three-Step Programming Approach
- Preparation Phase: Select sensing contacts and respective beta peaks, repeating signal tests OFF medication if necessary
- Initial Setup: Define initial LFP thresholds and stimulation limits based on individual biomarker characteristics
- Optimization Phase: Adjust parameters based on therapeutic response and adverse effect profile [15]
Addressing the underrepresentation of high-quality evidence in DBS parameter research requires concerted effort across multiple domains. By implementing rigorous systematic review methodologies, enhancing clinical trial design through adaptive approaches and diverse recruitment, and leveraging advanced computational techniques like machine learning, the field can strengthen its evidence base significantly. The development of standardized protocols for evidence generation and synthesis will ultimately accelerate the translation of research findings into optimized clinical care, ensuring that DBS therapy achieves its full potential for improving patient outcomes across diverse populations. As the field advances, maintaining commitment to the highest standards of evidence-based practice will be essential for navigating the complex landscape of neuromodulation therapeutics.
Conclusion
The optimization of DBS parameters is rapidly evolving from empirical, symptom-led programming toward a precision medicine paradigm grounded in individual neuroanatomy and real-time neural circuit dynamics. Key takeaways include the demonstrated efficacy of geometry-based computational models, the transformative potential of adaptive closed-loop systems, and the critical need for validated functional outcome measures beyond traditional symptom scales. Future directions must prioritize the integration of artificial intelligence for predictive parameter adjustment, the expansion of telemedicine-capable remote programming, and targeted research to address significant evidence gaps, particularly for non-motor symptoms and neurodevelopmental disorders. For biomedical researchers, the convergence of sensing-enabled neurostimulators, computational modeling, and large-scale neural datasets presents an unprecedented opportunity to develop next-generation, patient-specific DBS therapies that dynamically adapt to the evolving needs of the nervous system.
References
- 1. Modulation of Ion Channels in the Axon: Mechanisms and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6533529/]
- 2. Neuron matters: neuromodulation with electromagnetic ... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-022-01094-4]
- 3. Are we ready for automated deep brain stimulation ... [https://www.sciencedirect.com/science/article/abs/pii/S1353802025000884]
- 4. Neural mechanisms balancing accuracy and flexibility in ... [https://www.nature.com/articles/s41540-025-00520-2]
- 5. Optimizing stimulation parameters for anterior thalamic nuclei ... [https://pubmed.ncbi.nlm.nih.gov/40423665/]
- 6. Modulation of neuronal dynamics by sustained and activity ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11100521/]
- 7. Protocol for the quantitative assessment of social and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12056402/]
- 8. Multitarget Neurostimulation of the Deep Brain - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC12453607/]
- 9. A framework for translational therapy development in deep ... [https://www.nature.com/articles/s41531-024-00829-5]
- 10. Best practices for clinical trials of deep brain stimulation ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1572972/full]
- 11. Best practices for clinical trials of deep brain stimulation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12041084/]
- 12. Personalized, closed-loop deep brain stimulation for ... [https://www.medrxiv.org/content/10.1101/2025.08.11.25333010v1]
- 13. Electrophysiological Biomarkers Reflect Target ... [https://www.sciencedirect.com/science/article/pii/S2667174325001636]
- 14. Patient-specific and interpretable deep brain stimulation ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1661987/full]
- 15. Chronic adaptive deep brain stimulation for Parkinson's ... [https://www.nature.com/articles/s41531-025-01124-7]
- 16. Optimizing stimulation parameters for anterior thalamic ... [https://www.medrxiv.org/content/10.1101/2025.01.22.25320034v1]
- 17. New deep brain stimulation settings to improve gait in ... [https://www.sciencedirect.com/science/article/pii/S0966636225006526]
- 18. Theta-frequency subthalamic nucleus stimulation ... [https://www.sciencedirect.com/science/article/pii/S1935861X25002098]
- 19. Low-Frequency Dual Target Deep Brain Stimulation May ... [https://scholars.duke.edu/individual/pub1671360]
- 20. Online prediction of optimal deep brain stimulation contacts ... [https://www.nature.com/articles/s41531-025-01092-y]
- 21. Reconsidering the ethics of sham interventions in an era ... [https://www.sciencedirect.com/science/article/abs/pii/S0039606014007867]
- 22. Evaluating the importance of sham-controlled trials in ... [https://eurointervention.pcronline.com/article/evaluating-the-importance-of-sham-controlled-trials-in-the-investigation-of-medical-devices-in-interventional-cardiology]
- 23. Sham procedures and the ethics of clinical trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC1079669/]
- 24. Deep brain stimulation: current challenges and future directions [https://pmc.ncbi.nlm.nih.gov/articles/PMC6397644/]
- 25. Patient-specific and interpretable deep brain stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12586115/]
- 26. Patient, target, device, and program selection for DBS in ... [https://www.nature.com/articles/s41531-025-01015-x]
- 27. Efficacy and Safety of Bilateral Deep Brain Stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12004396/]
- 28. Deep brain stimulation (DBS) shown to be safe in treating ... [https://sunnybrook.ca/media/item.asp?i=2533]
- 29. Ethical considerations of deep brain stimulation for treatment ... [https://bmcpsychiatry.biomedcentral.com/articles/10.1186/s12888-025-07128-0]
- 30. DBS Programming: An Evolving Approach for Patients with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5632902/]
- 31. Modeling and optimizing deep brain stimulation to ... [https://www.nature.com/articles/s41531-025-00990-5]
- 32. Computational analysis of electrode structure and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11208352/]
- 33. Analysis of high-perimeter planar electrodes for efficient ... [https://www.frontiersin.org/journals/neuroengineering/articles/10.3389/neuro.16.015.2009/full]
- 34. Evaluation of DBS computational modeling methodologies ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12083610/]
- 35. kinematic gait parameters inform optimization of stimulation ... [https://pubmed.ncbi.nlm.nih.gov/40926219/]
- 36. Evaluation of methodologies for computing the deep brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7187771/]
- 37. MRI Support DBS Lead-Only Systems [https://www.neuromodulation.abbott/us/en/healthcare-professionals/mri-support/mri-dbs-lead-only.html]
- 38. ImageReady™ MR-Conditional Deep Brain Stimulation ... [https://www.bostonscientific.com/imageready/en-US/dbs-system.html]
- 39. Patterns and contrast [https://highcharts.com/docs/accessibility/patterns-and-contrast]
- 40. Influence of statistical approaches on Probabilistic Sweet ... [https://www.sciencedirect.com/science/article/pii/S2213158225000907]
- 41. Adaptive DBS: A New Era in Parkinson's Disease Treatment [https://www.apdaparkinson.org/article/adaptive-deep-brain-stimulation-dbs/]
- 42. Medtronic BrainSense™ Adaptive Deep Brain Stimulation ... [https://news.medtronic.com/2025-10-09-Medtronic-BrainSense-TM-Adaptive-Deep-Brain-Stimulation-named-a-2025-TIME-Best-Inventions]
- 43. BrainSense™ Technology [https://www.medtronic.com/en-us/healthcare-professionals/products/neurological/deep-brain-stimulation/dbs-technologies/brainsense-technology.html]
- 44. Methodological Considerations for Setting Up Deep Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8836606/]
- 45. Patient-specific and interpretable deep brain stimulation ... [https://pubmed.ncbi.nlm.nih.gov/41200513/]
- 46. Patient-Specific and Interpretable Deep Brain Stimulation ... [https://www.medrxiv.org/content/10.1101/2025.07.17.25331690v1]
- 47. Improving computational models of deep brain stimulation ... [https://www.sciencedirect.com/science/article/pii/S0165027024002656]
- 48. Computational modeling of deep brain stimulation - PubMed [https://pubmed.ncbi.nlm.nih.gov/24112884/]
- 49. Management of essential tremor deep brain stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10918853/]
- 50. Comparison of structural connectomes for modeling deep ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12090019/]
- 51. Comparison of beta peak detection algorithms for data- ... [https://www.nature.com/articles/s41531-024-00762-7]
- 52. Comparison of the Efficacy of Deep Brain Stimulation in ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2021.749722/full]
- 53. Prediction of pyramidal tract side effect threshold by intra- ... [https://www.frontiersin.org/journals/surgery/articles/10.3389/fsurg.2024.1465840/full]
- 54. Chronic adaptive deep brain stimulation for Parkinson's ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12397205/]
- 55. Image-guided optimization of current steering in STN-DBS ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1618480/full]
- 56. Paired Deep Brain Stimuli Elicit Short‐Term Facilitation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224288/]
- 57. Update on Current Technologies for Deep Brain ... [https://www.e-jmd.org/journal/view.php?doi=10.14802/jmd.20052]
- 58. Deep Brain Stimulation Programming for Movement ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2019.00410/full]
- 59. Long-Term Clinical Experience with Directional ... Deep Brain [https://pmc.ncbi.nlm.nih.gov/articles/PMC9338213/]
- 60. Long-Term Clinical Experience with Directional Deep Brain ... [https://link.springer.com/article/10.1007/s40120-022-00381-5]
- 61. Accelerated symptom improvement in Parkinson's disease ... [https://www.nature.com/articles/s43856-025-00744-7]
- 62. Predicting optimal deep brain stimulation parameters for ... [https://www.nature.com/articles/s41467-021-23311-9]
- 63. “Nothing to Lose, Absolutely Everything to Gain”: Patient ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2021.755276/full]
- 64. Role of expectations in clinical outcomes after deep brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10576668/]
- 65. Best Color Palettes for Scientific Figures and Data ... [https://www.simplifiedsciencepublishing.com/resources/best-color-palettes-for-scientific-figures-and-data-visualizations]
- 66. Automated optimization of deep brain stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11090244/]
- 67. Ameliorating motor performance and quality of life in ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1449973/full]
- 68. Long-Term Motor and Cognitive Outcome of Deep Brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12549006/]
- 69. Are we ready for automated deep brain stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12599573/]
- 70. Secondary and primary dystonia: pathophysiological ... [https://pubmed.ncbi.nlm.nih.gov/23771342/]
- 71. DBScope as a versatile computational toolbox for the ... [https://www.nature.com/articles/s41531-024-00740-z]
- 72. Effects of Neurodevelopmental Disorders on the Clinical ... [https://pubmed.ncbi.nlm.nih.gov/39432201]
- 73. Dosing of Electrical Parameters in Deep Brain Stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6050377/]
- 74. Evidence-Based Medicine and Good Clinical Practice in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562602/]
- 75. Best practices for clinical trials of deep brain stimulation ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1572972/abstract]
- 76. Electrophysiological signatures predict the therapeutic ... [https://www.nature.com/articles/s41746-025-02089-w]
- 77. Diversity in Clinical Trials: A Scientific Imperative for 2025 [https://www.wcgclinical.com/insights/diversity-in-clinical-trials-a-scientific-imperative-for-2025/]
- 78. A comprehensive guide to conduct a systematic review and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12366998/]
- 79. Systematic Reviews: Step 7: Extract Data from Included Studies [https://guides.lib.unc.edu/systematic-reviews/extract-data]