AI-Powered Brain Tumor Segmentation from MRI: A Comprehensive Review for Researchers and Drug Developers
This article provides a comprehensive analysis of artificial intelligence (AI) applications for automated brain tumor segmentation in Magnetic Resonance Imaging (MRI), tailored for researchers, scientists, and drug development professionals.
AI-Powered Brain Tumor Segmentation from MRI: A Comprehensive Review for Researchers and Drug Developers
Abstract
This article provides a comprehensive analysis of artificial intelligence (AI) applications for automated brain tumor segmentation in Magnetic Resonance Imaging (MRI), tailored for researchers, scientists, and drug development professionals. It explores the foundational need for these tools in overcoming the limitations of manual segmentation and the challenges posed by tumor heterogeneity. The review systematically covers the evolution of methodological approaches, from traditional machine learning to advanced deep learning architectures like U-Net and transformers, and their specific applications in clinical research and therapy planning. It further investigates the critical challenges and optimization techniques, including handling small metastases, data imbalance, and model generalizability. Finally, the article synthesizes validation frameworks, performance metrics, and comparative analyses of state-of-the-art models, offering a validated perspective on the current landscape and future trajectories of AI in accelerating neuro-oncology research and therapeutic development.
The Critical Need for AI in Brain Tumor Segmentation: Foundations and Clinical Imperatives
The Clinical Burden of Brain Tumors and the Pitfalls of Manual Segmentation
Brain tumors represent a significant and growing challenge to global healthcare systems, characterized by high morbidity and mortality rates. Epidemiological data indicates that brain tumors account for 1.5% of all cancer incidences, yet they cause a disproportionately high mortality rate of 3% [1]. With approximately 67,900 new primary CNS tumors diagnosed annually in the United States alone, and gliomas constituting 80% of all malignant primary brain tumors, the need for accurate diagnosis and treatment planning is paramount [2]. The current standard of care for aggressive forms like glioblastoma involves maximum safe surgical resection followed by radiotherapy and chemotherapy, yet this regimen affords only a median survival of 14-16 months, with fewer than 10% of patients surviving beyond 5 years [2].
Neuroimaging remains the cornerstone for diagnosis, treatment planning, and monitoring of brain tumors. Magnetic Resonance Imaging (MRI) specifically has emerged as the preferred modality due to its superior soft tissue contrast and high-resolution anatomical details without exposing patients to ionizing radiation [3] [1]. The accurate segmentation of brain tumors from MRI scans is critical for determining tumor location, size, shape, and extent, directly influencing surgical planning, radiation therapy targeting, and treatment response assessment [3] [4]. However, the traditional method of manual segmentation presents significant challenges that compromise both efficiency and diagnostic accuracy in clinical practice.
The Pitfalls of Manual Segmentation in Clinical Practice
Manual segmentation of brain tumors by radiologists represents a tedious, time-consuming task with considerable variability among raters [5] [4]. This process requires expert radiological knowledge and can require hours of expert work for a single case [6]. The inherent complexity of brain tumors, including variations in size, shape, location, and intensity heterogeneity across different MRI modalities, exacerbates these challenges [3].
The subjective nature of manual segmentation introduces significant inter-observer and intra-observer variability, potentially impacting diagnostic consistency and treatment outcomes [3] [7]. This variability becomes particularly problematic in multicenter clinical trials, where standardized and reproducible measurements are essential for validating therapeutic efficacy [2]. Furthermore, the labor-intensive nature of manual segmentation makes large-scale population studies or the analysis of extensive retrospective datasets impractical within clinical workflow constraints [6].
Table 1: Key Limitations of Manual Brain Tumor Segmentation
| Limitation | Clinical Impact | Quantitative Evidence |
|---|---|---|
| Time-Intensive Process | Delays diagnosis and treatment planning; increases healthcare costs | Requires "hours of expert work" per case [6] |
| Inter-Observer Variability | Compromises diagnostic consistency and reliability in clinical trials | "Prone to inter- and intra-observer variability" [7] [5] |
| Subjective Interpretation | Potential for misdiagnosis or incomplete tumor margin delineation | "Strong subjective nature" makes adaptation to efficiency requirements difficult [1] |
| Workload Burden | Contributes to radiologist fatigue and healthcare system inefficiencies | Creates a "tedious task" for specialists [5] [4] |
Advanced MRI and Standardized Protocols in Neuro-Oncology
The Response Assessment in Neuro-Oncology (RANO) working group has established criteria for tumor response evaluation, highlighting the critical role of standardized imaging [2]. A standardized Brain Tumor Imaging Protocol (BTIP) has been developed through consensus among experts, clinical scientists, imaging specialists, and regulatory bodies to address variability in multicenter studies [2].
The minimum recommended sequences in BTIP include:
- Parameter-matched precontrast and postcontrast inversion recovery-prepared, isotropic 3D T1-weighted gradient-recalled echo
- Axial 2D T2-weighted turbo spin-echo acquired after contrast injection
- Precontrast, axial 2D T2-weighted fluid-attenuated inversion recovery (FLAIR)
- Precontrast, axial 2D, 3-directional diffusion-weighted images [2]
These protocols balance feasibility with image quality, acknowledging the technical constraints of various clinical settings while ensuring sufficient data quality for accurate assessment. The initiative draws inspiration from standardizing efforts in other neurological fields, particularly the Alzheimer's Disease Neuroimaging Initiative (ADNI), which established vendor-neutral, standardized protocols for volumetric analysis [2].
AI-Driven Segmentation: Methodological Advances and Quantitative Performance
Deep learning-based automated segmentation methods have demonstrated remarkable performance in brain tumor segmentation by learning complex hierarchical features from MRI data [7]. Convolutional Neural Networks (CNNs) and Fully Convolutional Networks (FCNs) have shown substantial improvements over traditional techniques, with several architectures emerging as particularly effective.
Evolution of Segmentation Architectures
The U-Net architecture, with its encoder-decoder structure and skip connections, has become a foundational model in medical image segmentation [3] [1]. Subsequent innovations have focused on enhancing this baseline architecture:
- Attention U-Net incorporates attention gates to suppress irrelevant regions and highlight salient features [3].
- nnU-Net (no-new-Net) represents a breakthrough with its self-configuring approach that adapts to any new dataset without manual intervention [6].
- Multi-Modal Multi-Scale Contextual Aggregation with Attention Fusion (MM-MSCA-AF) leverages multi-modal MRI inputs and employs gated attention fusion to selectively enhance tumor-specific features, achieving Dice scores of 0.8158 for necrotic regions and 0.8589 overall on the BRATS 2020 dataset [3].
Performance Comparison of Segmentation Models
Table 2: Quantitative Performance of AI Segmentation Models on Benchmark Datasets
| Model Architecture | Reported Dice Score | Key Innovations | Clinical Advantages |
|---|---|---|---|
| MM-MSCA-AF [3] | 0.8589 (total)0.8158 (necrotic) | Multi-scale contextual aggregation, gated attention fusion | Handles complex tumor shapes; suppresses background noise |
| ARU-Net [7] | 0.981 (DSC)0.963 (IoU) | Residual connections, Adaptive Channel Attention, Dimensional-space Triplet Attention | Captures heterogeneous structures; preserves fine details |
| TotalSegmentator MRI [6] | Strong accuracy across 80 structures | Sequence-agnostic design; trained on diverse MRI and CT data | Robust across scan types; minimal user intervention required |
| Improved YOLOv5s [1] | 93.5% precision85.3% recall | Atrous Spatial Pyramid Pooling, attention mechanisms | Balanced lightweight design with segmentation accuracy |
The BraTS (Brain Tumor Segmentation) challenge has been instrumental in advancing the field, providing a diverse multi-institutional dataset and establishing benchmarks for algorithm performance [5]. The most recent iterations have addressed critical clinical challenges, including handling missing MRI sequences through image synthesis approaches [5].
Experimental Protocols for AI Model Validation
Standardized Training and Evaluation Framework
To ensure reproducible and clinically relevant results, researchers should adhere to a standardized experimental protocol when developing and validating segmentation models:
Dataset Preparation and Preprocessing:
- Utilize established public datasets (e.g., BraTS, BTMRII) with expert-annotated ground truth [3] [7] [5].
- Implement standardized preprocessing including co-registration to a common anatomical template, resampling to uniform isotropic resolution (typically 1mm³), and skull-stripping [5].
- Employ data augmentation techniques (rotation, flipping, intensity variations) to improve model generalization.
Model Training Protocol:
- Implement k-fold cross-validation (typically 5-fold) to ensure robust performance estimation [3].
- Use appropriate loss functions for medical segmentation (Dice loss, categorical cross-entropy, or combinations) [7].
- Optimize with adaptive algorithms (Adam optimizer) with learning rate scheduling [7].
- Train for sufficient epochs (100-200) with early stopping to prevent overfitting [1].
Performance Evaluation Metrics:
- Dice Similarity Coefficient (DSC/Dice Score): Measures spatial overlap between prediction and ground truth [3] [7].
- Intersection over Union (IoU): Assesses segmentation accuracy based on area of overlap [7].
- Precision and Recall: Quantifies the model's ability to correctly identify tumor pixels while minimizing false positives and negatives [1].
- Structural Similarity Index Measure (SSIM): Evaluates synthesized image quality in cases of missing modalities [5].
Addressing Missing Modalities in Clinical Practice
A common challenge in clinical environments is incomplete MRI protocols due to time constraints or artifacts. The BraSyn benchmark provides a protocol for handling such scenarios:
- Image Synthesis Evaluation: When one modality is missing, algorithms must synthesize plausible replacements using available sequences [5].
- Dual-Metric Assessment: Evaluate synthesized images using both SSIM for image quality and downstream Dice scores for segmentation utility [5].
- Clinical Validation: Assess whether synthesized images maintain diagnostic value comparable to acquired images through radiologist review.
Table 3: Key Research Reagents and Computational Tools for Brain Tumor Segmentation
| Resource Category | Specific Tools/Datasets | Function and Application | Access Information |
|---|---|---|---|
| Public Datasets | BraTS [3] [5], BTMRII [7] | Benchmarking and training models; provides multi-modal MRI with expert annotations | Publicly available through respective challenge platforms |
| Segmentation Models | nnU-Net [6] [5], TotalSegmentator MRI [6] | State-of-the-art automated segmentation; adaptable to various imaging protocols | Open-source implementations available |
| Preprocessing Tools | CaPTk [5], FeTS tool [5] | Standardized preprocessing including co-registration, skull-stripping, resolution normalization | Publicly available toolkits |
| Evaluation Metrics | Dice Score, IoU, Precision/Recall [7] [1] | Quantitative performance assessment of segmentation accuracy | Standard implementations in machine learning libraries |
| Federated Learning | Federated learning frameworks [4] | Enables multi-institutional collaboration while preserving data privacy | Emerging methodology with various implementations |
The integration of AI-driven segmentation into neuro-oncology represents a paradigm shift in addressing the clinical burden of brain tumors. These methodologies directly mitigate the pitfalls of manual segmentation by providing rapid, reproducible, and quantitative analysis of tumor volumes and subregions. The demonstrated performance of contemporary models on benchmark datasets confirms their readiness for broader clinical validation and implementation.
Future research directions should focus on enhancing model interpretability, developing robust federated learning approaches to enable multi-institutional collaboration without data sharing [4], and improving sequence-agnostic segmentation to handle the variability of real-world clinical imaging protocols [6] [5]. As these technologies mature, they hold significant potential to transform neuro-oncological care by enabling more personalized treatment approaches and accelerating therapeutic development through more reliable quantitative endpoints in clinical trials.
Magnetic Resonance Imaging (MRI) has established itself as the cornerstone of neuroimaging, providing unparalleled soft tissue contrast essential for diagnosing and managing brain tumors. Its value is significantly amplified when integrated with artificial intelligence (AI), particularly for automated tumor segmentation. This synergy enables precise, reproducible, and high-throughput analysis of brain tumors, which is critical for advancing research and drug development. The non-invasive nature of MRI, combined with its ability to reveal structural and functional information, makes it an indispensable tool in both clinical and research settings [8] [9]. For researchers and drug development professionals, understanding the specific MRI sequences and their underlying biological correlates is fundamental to developing robust AI models and interpreting their output accurately. This document details the key MRI sequences, their experimental protocols, and their biological significance within the context of AI-driven brain tumor analysis.
Key MRI Sequences and Their Biological Correlates
Different MRI sequences are sensitive to distinct tissue properties, providing complementary information about the tumor microenvironment. The following table summarizes the primary sequences used in brain tumor imaging and their biological significance.
Table 1: Key MRI Sequences for Brain Tumor Analysis and Their Biological Correlates
| Sequence Name | Key Contrast Mechanisms | Biological Correlates in Brain Tumors | Primary Application in AI Segmentation |
|---|---|---|---|
| T1-weighted (T1w) | Longitudinal (T1) relaxation time | Anatomy of gray matter, white matter, and cerebrospinal fluid (CSF) [9] | Spatial registration and anatomical reference [9] |
| T1-weighted Contrast-Enhanced (T1CE) | T1 relaxation, Gadolinium contrast agent leakage | Blood-brain barrier (BBB) disruption; active, high-grade tumor regions [10] [9] | Delineation of enhancing tumor core [11] [9] |
| T2-weighted (T2w) | Transverse (T2) relaxation time | Vasogenic edema and increased free water content [9] | Delineation of peritumoral edematous region [11] |
| Fluid-Attenuated Inversion Recovery (FLAIR) | T2 relaxation with CSF signal suppression | Vasogenic edema and non-enhancing tumor infiltration [9] | Delineation of the whole tumor region, including infiltrated tissue [11] |
The combination of these sequences is crucial for a comprehensive analysis. For instance, T1CE is excellent for highlighting the metabolically active core of high-grade gliomas where the blood-brain barrier is compromised, while FLAIR is more sensitive to the surrounding invasive tumor and edema, which is a critical target for therapy and resection planning [9]. AI models, particularly those based on U-Net architectures and its variants, are trained on these multi-modal inputs to automatically segment different tumor sub-regions with high accuracy, as demonstrated in benchmarks like the BraTS challenge [11] [9].
Experimental Protocols for Preclinical fMRI
Preclinical functional MRI (fMRI) is a powerful tool for investigating brain function and the effects of interventions in animal models. The following protocol outlines key considerations for conducting robust preclinical fMRI studies, which can be adapted to study tumor models and their functional impact.
Table 2: Key Reagents and Equipment for Preclinical fMRI
| Category | Item | Function/Application |
|---|---|---|
| Animal Handling | Dedicated MRI cradle with head fixation (tooth/ear bars) [12] | Reduces motion artifacts, ensures reproducible positioning [12] |
| Anesthesia & Monitoring | Volatile (e.g., isoflurane) or injectable (e.g., medetomidine) anesthetics [12] | Maintains animal immobility and well-being; choice can affect hemodynamic response [12] |
| Physiological monitoring (respiratory rate, body temperature) [12] | Maintains physiological stability and animal welfare during scanning [12] | |
| Hardware | Ultrahigh-field MRI system (e.g., 7T to 18T) [12] | Increases functional contrast-to-noise ratio (fCNR) for BOLD fMRI [12] |
| High-performance gradients (400-1000 mT/m) [12] | Enables high spatial and temporal resolution for EPI sequences [12] | |
| Cryogenic radiofrequency (RF) coils [12] | Boosts signal-to-noise ratio (SNR) by reducing electronic noise [12] |
Protocol: Preclinical BOLD fMRI Acquisition
1. Animal Preparation and Anesthesia:
- Induce anesthesia in the animal (e.g., with 4% isoflurane in O₂) and secure it in a dedicated, stereotaxic MRI cradle using a tooth bar and ear bars to minimize head motion [12].
- Maintain anesthesia at a lower level (e.g., 1-2% isoflurane) and continuously monitor physiological parameters such as respiratory rate and body temperature throughout the experiment. Use a feedback-controlled heating system to maintain core body temperature at ~37°C [12].
2. Hardware Setup:
- Utilize an ultrahigh-field MRI system (≥ 7 Tesla) to maximize the blood oxygen level-dependent (BOLD) contrast and functional contrast-to-noise ratio (fCNR) [12].
- Employ a high-sensitivity radiofrequency (RF) coil, such as a cryogenically cooled array coil or an implantable coil, positioned as close as possible to the animal's head to optimize the signal-to-noise ratio (SNR) [12].
- Ensure the gradient system is capable of high performance (strength > 400 mT/m, slew rate > 1000 T/m/s) to support the high-resolution Echo Planar Imaging (EPI) sequences used in fMRI [12].
3. fMRI Sequence Acquisition:
- Use a T2*-weighted Gradient Echo (GE) Echo Planar Imaging (EPI) sequence for BOLD signal detection. This sequence provides the necessary sub-second temporal resolution to track the hemodynamic response [12].
- Optimize EPI parameters based on the specific research question [12]:
- Spatial Resolution: Isotropic voxels of 100-300 μm are typical for rodents to precisely map functional responses.
- Temporal Resolution: A repetition time (TR) of 1-2 seconds is often used to accurately sample the hemodynamic response function.
- Other Parameters: Adjust the echo time (TE) to be close to the T2* of the tissue at the given magnetic field strength to maximize BOLD contrast.
- For stimulus-evoked fMRI, synchronize the presentation of the stimulus (sensory, optogenetic, etc.) with the start of the image acquisition.
AI-Driven Segmentation and Analysis
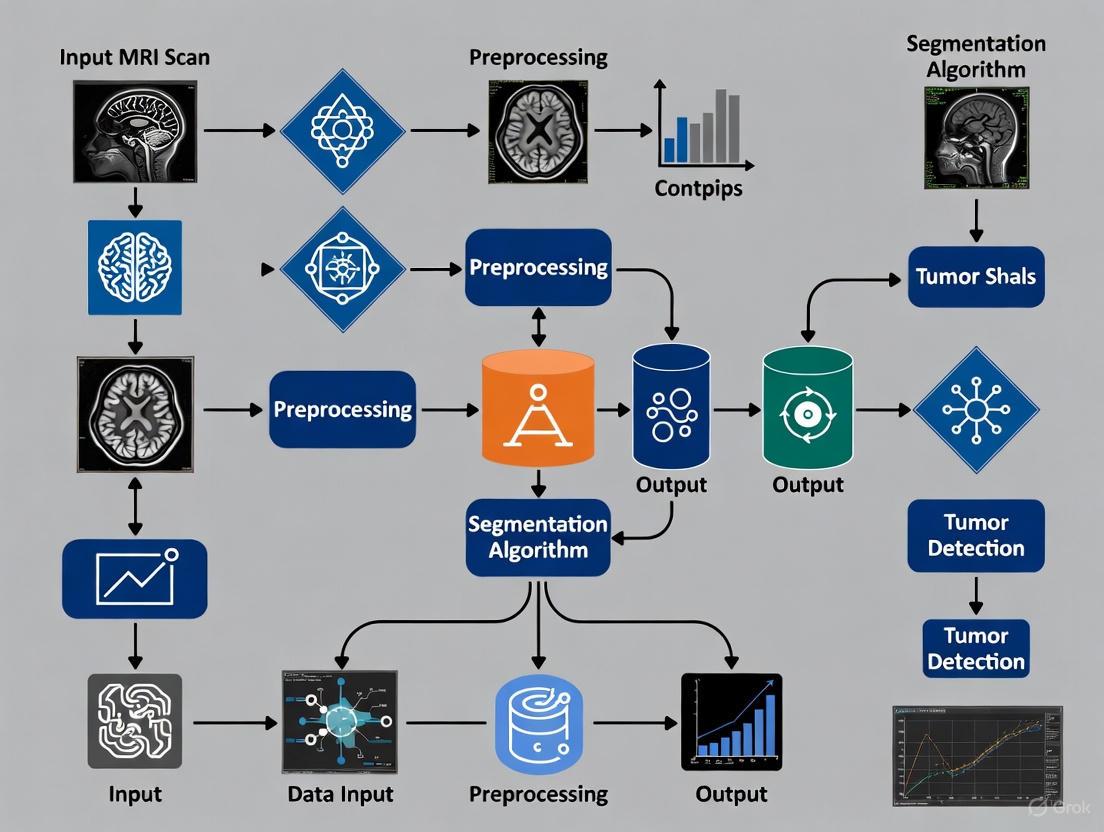
The core of automated brain tumor analysis lies in segmenting the tumor into its constituent parts. The following workflow details a standard methodology for developing and applying an AI segmentation model, using datasets from public challenges like BraTS (Brain Tumor Segmentation).
Protocol: AI Model Training for Volumetric Segmentation
1. Data Curation and Preprocessing:
- Dataset: Utilize a public dataset such as the BraTS (Brain Tumor Segmentation) challenge dataset, which provides multi-modal MRI scans (T1, T1CE, T2, FLAIR) with expert-annotated ground truth labels for various tumor sub-regions [11] [9].
- Preprocessing Steps: Implement a standardized pipeline including:
- Coregistration: Align all MRI sequences (T1, T1CE, T2, FLAIR) to a common space to ensure voxel-wise correspondence [13].
- Skull-stripping: Remove non-brain tissues using a tool like the Brain Extraction Tool (BET) from FSL [13].
- Intensity Normalization: Normalize the intensity values across all scans to improve model training stability and performance [11] [9].
- Data Augmentation: Apply affine transformations (rotations, scaling, etc.) to artificially expand the training dataset and improve model generalizability [11].
2. Model Architecture and Training:
- Architecture Selection: Implement a 3D U-Net architecture, which has been a foundational and winning model in segmentation challenges [9]. The U-Net's encoder-decoder structure with skip connections effectively captures context and preserves spatial information.
- Loss Function: Use a loss function suitable for class imbalance, such as the Dice Loss or a combination of Dice and Cross-Entropy Loss. The Dice Loss directly optimizes for the overlap between the prediction and ground truth, which is ideal for segmentation tasks where the target region is small relative to the background [9].
- Training: Train the model on the preprocessed multi-modal inputs (T1, T1CE, T2, FLAIR) to predict the voxel-wise labels for different tumor regions (e.g., necrotic core, enhancing tumor, peritumoral edema).
3. Validation and Performance Metrics:
- Primary Metric: Use the Dice Similarity Coefficient (DSC) to evaluate model performance. The DSC measures the spatial overlap between the automated segmentation and the ground truth manual segmentation. A DSC of 0.70-0.75 is often considered competitive, with state-of-the-art models achieving scores above 0.85-0.90 for certain tumor sub-regions [10] [9].
- Additional Metrics: Report complementary metrics such as the Hausdorff Distance (HD) to capture the largest segmentation error, and Sensitivity/Specificity to assess classification accuracy [8].
Table 3: Quantitative Performance of AI Segmentation Models
| Model / Study | Task | Key Architecture | Performance (Dice Score) |
|---|---|---|---|
| AI for Vestibular Schwannomas [10] | 3D Volumetric Segmentation of VS | Proprietary AI/ML algorithms | Final Mean Dice: 0.88 (Range: 0.74-0.93) |
| Glioma Grade Classification [11] | Glioma Segmentation & HGG/LGG Classification | U-Net + VGG | Segmentation Dice: Enhancing Tumor: 0.82, Whole Tumor: 0.91, Tumor Core: 0.72 |
| BraTS Challenge Top Performers [9] | Glioma Segmentation | Variants of U-Net (e.g., with residual blocks) | State-of-the-art Dice scores consistently >0.85 for whole tumor and tumor core regions |
The integration of these advanced AI methodologies with standardized MRI protocols provides a powerful framework for objective and quantitative analysis of brain tumors, facilitating more precise drug development and personalized treatment strategies.
Automated brain tumor segmentation from Magnetic Resonance Imaging (MRI) is a critical task in medical image analysis, facilitating early diagnosis, treatment planning, and disease monitoring for researchers, clinicians, and drug development professionals [3]. The process involves delineating different tumor subregions from multi-modal MRI scans, which is challenging due to the inherent complexity of brain tumors, including variations in size, shape, and location across different MRI modalities [3]. Traditional manual segmentation by radiologists is time-intensive, subjective, and prone to inter-observer variability, creating a pressing need for robust automated artificial intelligence (AI) solutions [14] [3].
This document outlines the fundamental task of segmenting a brain tumor from its entirety down to its enhancing core, detailing the defining characteristics of each subregion, the AI methodologies employed, and the experimental protocols for developing and validating such models. The focus extends from whole tumor identification to the precise delineation of the enhancing tumor core, a critical region for therapeutic targeting and treatment response assessment [15].
Defining the Tumor Subregions
In brain tumor analysis, particularly for gliomas, the tumor is not a homogeneous entity but is comprised of several distinct subregions, each with unique radiological and clinical significance. The segmentation task is hierarchically defined by these subregions [3].
Table 1: Brain Tumor Subregions in Glioma Segmentation
| Tumor Subregion | Description | Clinical & Research Significance | Best Visualized on MRI Sequence |
|---|---|---|---|
| Whole Tumor (WT) | The complete abnormal area, encompassing the core and the surrounding edema. | Crucial for initial diagnosis, assessing mass effect, and overall tumor burden. | FLAIR (suppresses CSF signal, making edema appear bright) [3] [15] |
| Tumor Core (TC) | Comprises the necrotic core, enhancing tumor, and any non-enhancing solid tumor. | Important for determining tumor grade and aggressive potential. | T1-weighted Contrast-Enhanced (T1-CE) [3] [15] |
| Enhancing Tumor (ET) | The portion of the tumor that shows uptake of contrast agent, indicating a leaky blood-brain barrier. | A key biomarker for tumor activity, treatment planning, and monitoring response to therapy. | T1-weighted Contrast-Enhanced (T1-CE) [3] [15] |
The foundational step involves identifying the Whole Tumor (WT), which includes the core tumor mass and the surrounding peritumoral edema (swelling) [3]. The Tumor Core (TC) is then isolated from the whole tumor, which involves separating the solid tumor mass from the surrounding edema. Within the tumor core, the Enhancing Tumor (ET) is the most active and vital region to segment for many clinical decisions [15].
Diagram 1: Hierarchical segmentation workflow from whole tumor to enhancing core.
AI Architectures for Tumor Segmentation
From Traditional ML to Deep Learning
Early automated segmentation methods relied on traditional machine learning (ML) techniques such as Support Vector Machines (SVM) and Logistic Regression (LR). These models often required extensive feature engineering (e.g., texture, shape descriptors) and dimensionality reduction techniques like Principal Component Analysis (PCA) to handle the high-dimensional MRI data [14] [3]. While effective, their performance was limited by their dependence on hand-crafted features and their inability to capture the complex, hierarchical spatial dependencies in MRI data [3].
The field has been revolutionized by Deep Learning (DL), particularly Convolutional Neural Networks (CNNs), which automatically learn relevant features directly from the image data in an end-to-end manner [3] [16]. Architectures like U-Net and its 3D variant have become the standard baselines and workhorses for this task [17] [15]. The U-Net's encoder-decoder structure with skip connections allows it to effectively capture both context and precise localization, which is essential for accurate segmentation [15].
Advanced and Specialized Architectures
Research has progressed to more sophisticated architectures designed to address specific challenges in brain tumor segmentation:
- Multi-Modal Multi-Scale Models: Frameworks like MM-MSCA-AF leverage multiple MRI sequences (T1, T1-CE, T2, FLAIR) and employ multi-scale contextual aggregation to capture both global and fine-grained spatial features. They use gated attention fusion to selectively refine tumor-specific features and suppress irrelevant noise, thereby improving segmentation accuracy for complex tumor shapes [3].
- Lightweight and Efficient Models: For deployment in resource-constrained settings, lightweight models such as optimized 3D U-Net are developed to run efficiently on standard CPUs, balancing computational cost with segmentation accuracy [17].
- Architectures for Reduced Data Input: Studies have systematically evaluated the minimal set of MRI sequences required for accurate segmentation. Evidence suggests that a model trained on just T1C and FLAIR can achieve performance comparable to one using all four standard sequences, particularly for the enhancing tumor and tumor core, which can simplify clinical deployment [15].
- One-Stage Detection Models: Algorithms from the YOLO (You Only Look Once) family, known for their speed in object detection, have been adapted and improved for segmentation tasks. Enhancements like the incorporation of Atrous Spatial Pyramid Pooling (ASPP) and attention mechanisms (CBAM, CA) help these models capture multi-scale context and focus on relevant tumor regions [1].
Table 2: Comparison of AI Models for Brain Tumor Segmentation
| Model Architecture | Key Features & Mechanics | Reported Performance (Dice Score) | Computational Note |
|---|---|---|---|
| SVM with RBF Kernel | Traditional ML; requires manual feature extraction and PCA. | Testing Accuracy: 81.88% [14] | Lower computational cost but limited by feature engineering. |
| 3D U-Net | 3D volumetric processing; encoder-decoder with skip connections. | ET: 0.867, TC: 0.926 (on T1C+FLAIR) [15] | Standard for volumetric data; can be optimized for CPUs [17]. |
| MM-MSCA-AF | Multi-modal input; multi-scale contextual aggregation; gated attention fusion. | Overall Dice: 0.8589; Necrotic: 0.8158 [3] | Higher complexity but robust for heterogeneous tumors. |
| Improved YOLOv5s | One-stage detection; incorporates ASPP and attention modules (CBAM, CA). | Precision: 93.5%; Recall: 85.3% [1] | Designed for speed and efficiency; lightweight version available. |
| Lightweight 3D U-Net | Simplified architecture optimized for low-resource systems. | Dice: 0.67 on validation data [17] | Designed for CPU-based training and inference. |
Experimental Protocols & Application Notes
This section provides a detailed, step-by-step protocol for training and validating a deep learning model for brain tumor segmentation, synthesizing methodologies from cited research.
Phase 1: Data Collection, Preparation, and Preprocessing
Objective: To curate and prepare a multi-modal MRI dataset for model training.
- Dataset Acquisition:
- Source a publicly available, annotated dataset such as the BraTS (Brain Tumor Segmentation) challenge dataset [3] [17] [15]. The BraTS 2020 dataset, for example, includes multi-institutional MRI scans with ground truth annotations for tumor subregions [3].
- Ensure the dataset includes the four standard MRI sequences for each patient: Native T1 (T1), Post-contrast T1-weighted (T1-CE), T2-weighted (T2), and T2-FLAIR (FLAIR) [3] [15].
- Data Preprocessing:
- Skull-Stripping: Remove non-brain tissue from the images using validated tools or pre-processed data provided with the dataset [15].
- Spatial Normalization: Interpolate all scans to a uniform isotropic resolution (e.g., 1mm³) [15].
- Intensity Normalization: Apply Z-score normalization to each MRI sequence independently to achieve a zero mean and unit variance, mitigating scanner and protocol variations [15].
- Data Augmentation: Artificially expand the training dataset using real-time transformations during training to improve model generalizability. Standard techniques include:
- Random rotations (±5°)
- Random translations
- Horizontal and vertical flipping
- Elastic deformations
- Intensity scaling and shifts [15].
Phase 2: Model Building and Training
Objective: To implement, configure, and train a segmentation model.
- Model Selection and Implementation:
- Select a model architecture based on the project's goals (e.g., accuracy vs. speed vs. computational resources). A 3D U-Net is a strong baseline choice [15].
- Implement the model in a deep learning framework like PyTorch or TensorFlow. For a lightweight 3D U-Net, initialize the network with a standard depth of 4 contraction/expansion layers and an initial filter size of 32, which doubles at each downsampling step [17] [15].
- Training Configuration:
- Data Splitting: Split the dataset into training (e.g., 80%), validation (e.g., 10%), and a held-out test set (e.g., 10%). Use cross-validation if the dataset is limited [14] [15].
- Loss Function: Use a combination of Dice loss and cross-entropy loss to handle class imbalance between tumor and non-tumor voxels.
- Optimizer: Use the Adam optimizer with an initial learning rate of 1e-4 and a batch size tailored to available GPU memory (e.g., 1 or 2 for 3D models).
- Training Loop: Train the model for a fixed number of epochs (e.g., 100-300), using the validation Dice score to select the best model and to trigger early stopping if the performance plateaus.
Diagram 2: End-to-end model training and validation protocol.
Phase 3: Model Evaluation and Validation
Objective: To quantitatively and qualitatively assess the trained model's performance.
- Quantitative Metrics:
- Dice Similarity Coefficient (Dice Score): The primary metric for segmentation overlap. Calculate separately for the Whole Tumor (WT), Tumor Core (TC), and Enhancing Tumor (ET) [3] [15].
- Hausdorff Distance: Measures the largest distance between the predicted and ground truth segmentation boundaries, assessing the accuracy of the outer margins [15].
- Sensitivity and Specificity: Evaluate the model's ability to identify true positives and true negatives [15].
- Qualitative Analysis:
- Visually inspect the model's segmentation outputs against the ground truth by generating overlay images.
- Perform error analysis to identify common failure modes, such as misclassification due to structural similarities between tumor types or confusion with healthy tissues [14].
Phase 4: Deployment Considerations
Objective: To outline steps for model deployment in real-world scenarios.
- Model Optimization: Convert the trained model to an efficient inference format (e.g., ONNX, TensorRT) to reduce latency.
- Integration: Package the model within a user-friendly application programming interface (API) or software plugin that can interface with clinical Picture Archiving and Communication Systems (PACS).
- Continuous Validation: Establish a pipeline for monitoring model performance on prospective data to detect and correct for data drift over time.
The Scientist's Toolkit: Research Reagents & Materials
Table 3: Essential Resources for Brain Tumor Segmentation Research
| Resource Category | Specific Examples | Function and Role in Research |
|---|---|---|
| Public Datasets | BraTS (Brain Tumor Segmentation Challenge), TCIA (The Cancer Imaging Archive) [14] [3] | Provides standardized, multi-modal MRI data with expert annotations for training and benchmarking models. |
| Computing Hardware | GPU (NVIDIA series) or CPU (Intel Core i5/i7 with ≥8GB RAM) [17] | Accelerates model training and inference. CPU-based protocols enable research in resource-constrained settings [17]. |
| Software & Libraries | Python, PyTorch/TensorFlow, MONAI, Visual Studio Code [17] | Core programming languages and specialized libraries for developing, training, and testing deep learning models. |
| Evaluation Metrics | Dice Score, Hausdorff Distance, Sensitivity, Specificity [3] [15] | Standardized quantitative measures to objectively evaluate and compare the performance of different segmentation models. |
| Model Architectures | 3D U-Net, nnU-Net, MM-MSCA-AF, Improved YOLO [3] [17] [1] | Pre-defined neural network blueprints that form the foundation for solving the segmentation task. |
The Evolution from Traditional Image Processing to AI-Driven Solutions
The analysis of magnetic resonance imaging (MRI) scans represents a cornerstone of modern neuro-oncology, providing critical insights for the diagnosis, treatment planning, and monitoring of brain tumors. The journey from traditional image processing techniques to contemporary artificial intelligence (AI)-driven solutions marks a revolutionary shift in how medical professionals extract information from complex imaging data [18]. This evolution has fundamentally transformed the landscape of brain tumor segmentation, moving from time-consuming, operator-dependent methods toward automated, precise, and reproducible analytical frameworks [19] [8].
Initially, the segmentation of brain tumors relied heavily on manual delineation by expert radiologists, a process requiring years of specialized training yet remaining susceptible to inter-observer variability and fatigue [19]. The subsequent development of traditional automated methods offered initial improvements but struggled with the inherent complexity and heterogeneity of brain tumor manifestations across different MRI sequences and patient populations [3]. The advent of machine learning, and particularly deep learning, has addressed many of these limitations, enabling the development of systems that not only match but in some cases surpass human-level performance in specific detection and segmentation tasks [20] [9].
This application note delineates this technological evolution, providing researchers and drug development professionals with a structured overview of the quantitative benchmarks, experimental protocols, and essential research tools that underpin modern AI-driven solutions for brain tumor analysis in MRI.
Quantitative Evolution of Segmentation Performance
The performance of brain tumor segmentation methodologies has advanced significantly across technological generations. The transition from manual approaches to deep learning-based systems is quantifiably demonstrated through standardized metrics such as the Dice Similarity Coefficient (DSC), which measures spatial overlap between segmented and ground truth regions.
Table 1: Performance Comparison of Segmentation Approaches on the BRATS Dataset
| Method Category | Representative Model | Whole Tumor DSC | Tumor Core DSC | Enhancing Tumor DSC | Key Reference |
|---|---|---|---|---|---|
| Traditional ML | SVM / Random Forests | ~0.75-0.82 | ~0.65-0.75 | ~0.60-0.72 | [3] [9] |
| Basic Deep Learning | Standard U-Net | ~0.84 | ~0.77 | ~0.73 | [3] [21] |
| Advanced Deep Learning | nnU-Net | ~0.90 | ~0.85 | ~0.82 | [9] [21] |
| Hybrid Architectures | MM-MSCA-AF (2025) | 0.8589 | 0.8158 (Necrotic) | N/A | [3] |
The quantitative leap is most evident in the segmentation of complex sub-regions like the enhancing tumor, which is critical for assessing tumor activity and treatment response. Early machine learning models, dependent on handcrafted features (e.g., texture, shape), achieved limited success with DSCs often below 0.75 for these structures [3]. The introduction of deep learning architectures, notably the U-Net and its variants, marked a significant improvement, leveraging end-to-end learning from raw image data [9] [21]. Contemporary hybrid models, such as the Multi-Modal Multi-Scale Contextual Aggregation with Attention Fusion (MM-MSCA-AF), further push performance boundaries by selectively refining feature representations and discarding noise, achieving a Dice value of 0.8158 for the challenging necrotic tumor core [3].
Beyond segmentation accuracy, AI-driven solutions demonstrate profound operational impacts. One study evaluating an AI tool for detecting critical findings using abbreviated MRI protocols reported a sensitivity of 94% for brain infarcts, 82% for hemorrhages, and 74% for tumors, performance comparable to consultant neuroradiologists and superior to MR technologists [20]. This capability is a prerequisite for emerging AI-driven workflows that can dynamically select additional imaging sequences based on real-time findings, potentially revolutionizing MRI acquisition protocols [20] [22].
Experimental Protocols for AI Model Evaluation
The rigorous evaluation of novel AI-based segmentation models requires standardized protocols to ensure comparability and clinical relevance. The following section details a core experimental workflow, drawing from established methodologies used in benchmark challenges like the Multimodal Brain Tumor Segmentation (BraTS) [9] [21].
Protocol 1: Benchmarking Against Public Datasets
Objective: To quantitatively evaluate the performance of a new segmentation model against state-of-the-art methods using a publicly available benchmark dataset.
Materials:
- Dataset: BraTS 2020 dataset, containing multi-institutional pre-operative multi-modal MRI scans (T1, T1-CE, T2, T2-FLAIR) of glioblastoma (GBM/HGG) and lower-grade glioma (LGG) with pixel-wise expert annotations [3] [9].
- Validation Split: The provided training set is typically split 80:20 for training and validation, while the ground truth for the official test set is held private by challenge organizers.
- Computing Environment: High-performance computing node with GPU acceleration (e.g., NVIDIA A100 with 40GB+ VRAM).
Methodology:
- Data Preprocessing: Implement a standard preprocessing pipeline. This includes co-registration of all modalities to the same anatomical template, interpolation to a uniform isotropic resolution (e.g., 1mm³), and intensity normalization (e.g., z-score normalization per sequence across the entire dataset) [3] [21].
- Data Augmentation: Apply on-the-fly data augmentation during training to improve model generalization. Standard operations include random rotation (±15°), flipping (axial plane), scaling (±10%), and intensity shifts (±20% gamma) [21].
- Model Training: Configure the proposed model (e.g., MM-MSCA-AF) with published hyperparameters. A typical setup uses the Adam optimizer with an initial learning rate of 1e-4 and a combined loss function (e.g., Dice Loss + Cross-Entropy Loss) to handle class imbalance. Training proceeds for a fixed number of epochs (e.g., 1000) with early stopping if validation performance plateaus [3].
- Inference and Evaluation: Apply the trained model to the validation or test set. Generate segmentation masks and compute key metrics via the official BraTS evaluation platform. Primary metrics include Dice Similarity Coefficient (DSC) for overlap and Hausdorff Distance (HD95) for boundary accuracy, reported separately for the whole tumor, tumor core, and enhancing tumor [3] [21].
Protocol 2: Clinical Workflow Integration for Abbreviated MRI
Objective: To validate the performance of an AI model in a simulated clinical workflow using abbreviated MRI scan protocols, assessing its potential for real-time, AI-driven scan adaptation.
Materials:
- Cohort: A retrospective, consecutively enriched cohort of routine adult brain MRI scans from multiple clinical sites (e.g., n=414 patients) [20].
- Imaging Protocols: An abbreviated MRI protocol (e.g., 3-sequence: DWI, SWI/T2*-GRE, T2-FLAIR) and a standard 4-sequence protocol (adding T1W) for comparison [20].
- Reference Standard: Ground truth established from original radiological reports corroborated by independent image review by expert neuroradiologists.
Methodology:
- AI and Human Reader Setup: The AI tool and a panel of readers (e.g., consultant neuroradiologists, radiology residents, MR technologists) are provided with the abbreviated protocol images only [20].
- Blinded Assessment: Both AI and human readers independently analyze the scans to detect and localize critical findings: brain infarcts, intracranial hemorrhages, and tumors.
- Performance Analysis: Calculate sensitivity, specificity, and accuracy for the AI and each group of human readers against the reference standard. Compare the AI's performance directly against that of the human experts using statistical tests for proportions (e.g., McNemar's test) [20].
- Assisted Performance Evaluation: In a subsequent round, human readers re-evaluate the cases with access to the AI's predictions, allowing assessment of how AI assistance impacts human sensitivity and specificity.
Diagram 1: AI Segmentation Workflow. This diagram outlines the standard workflow for training and evaluating a deep learning model for brain tumor segmentation from multi-modal MRI inputs.
The Scientist's Toolkit: Essential Research Reagents & Materials
The development and validation of AI-driven segmentation tools rely on a suite of key resources, from public datasets to software frameworks. The table below catalogs essential "research reagents" for this field.
Table 2: Key Research Reagents and Materials for AI-Based Brain Tumor Segmentation
| Item Name / Category | Specifications / Example | Primary Function in Research |
|---|---|---|
| Public Benchmark Datasets | BraTS (Brain Tumor Segmentation) Challenge Datasets [9] [21] | Provides standardized, multi-institutional, expert-annotated MRI data for model training, benchmarking, and fair comparison against state-of-the-art methods. |
| Multi-modal MRI Scans | T1-weighted, T1-CE (contrast-enhanced), T2-weighted, T2-FLAIR [3] [9] | Provides complementary tissue contrasts necessary for a comprehensive evaluation of tumor sub-regions (edema, enhancing core, necrosis). |
| Annotation / Ground Truth | Pixel-wise manual segmentation labels by expert neuroradiologists [9] [21] | Serves as the gold standard for training supervised deep learning models and for evaluating the accuracy of automated segmentation outputs. |
| Deep Learning Frameworks | PyTorch, TensorFlow, MONAI (Medical Open Network for AI) | Provides open-source libraries and tools for building, training, and deploying complex deep learning architectures for medical imaging. |
| High-Performance Computing | NVIDIA GPUs (e.g., A100, V100) with CUDA cores | Accelerates the computationally intensive processes of model training and inference on large 3D medical image volumes. |
| Evaluation Metrics | Dice Similarity Coefficient (DSC), Hausdorff Distance (HD95) [3] [21] | Quantifies the spatial overlap and boundary accuracy of segmented masks against ground truth, enabling objective performance assessment. |
Visualization of Methodological Evolution
The conceptual and architectural shift from traditional methods to modern AI solutions can be visualized as a logical pathway, highlighting the key differentiators in their approach to feature extraction and learning.
Diagram 2: Evolution of Segmentation Methodologies. This diagram contrasts the fundamental workflows of traditional machine learning methods, which rely on manually engineered features, with deep learning approaches that learn features directly from data in an end-to-end manner.
Application Note: AI-Driven Diagnostic Segmentation for Tumor Identification and Characterization
Background and Clinical Rationale
Accurate and timely diagnosis of brain tumors is a critical determinant of patient outcomes. Manual segmentation of tumors from multi-sequence Magnetic Resonance Imaging (MRI) scans by radiologists is a time-intensive process prone to inter-observer variability, creating bottlenecks in diagnostic pathways [7] [14]. Automated AI-based tumor segmentation addresses this challenge by providing rapid, quantitative, and reproducible analysis of tumor characteristics, enabling more consistent and early detection.
Quantitative Performance of Diagnostic AI Models
Advanced deep learning models have demonstrated high performance in delineating brain tumors, as evidenced by evaluation metrics on benchmark datasets. The following table summarizes the capabilities of state-of-the-art models, including the novel ARU-Net architecture, which integrates residual connections and attention mechanisms [7].
Table 1: Performance Metrics of AI Models for Brain Tumor Diagnostic Segmentation
| AI Model / Architecture | Reported Accuracy | Dice Similarity Coefficient (DSC) | Intersection over Union (IoU) | Key Diagnostic Strength |
|---|---|---|---|---|
| ARU-Net [7] | 98.3% | 98.1% | 96.3% | Superior capture of heterogeneous tumor structures and fine structural details. |
| U-Net + Residual + ACA [7] | ~97.2% | ~95.0% | ~88.6% | Effective feature refinement in lower convolutional layers. |
| Baseline U-Net [7] | ~94.0% | ~91.7% | ~80.9% | Baseline performance for a standard encoder-decoder segmentation network. |
| SVM with RBF Kernel [14] | 81.88% (Classification) | N/A | N/A | Effective for tumor classification tasks using traditional machine learning. |
Recommended Clinical Protocol for Diagnostic Segmentation
Purpose: To standardize the acquisition of MRI data for optimal performance of automated AI segmentation tools in tumor diagnosis. Primary Modalities: T1-weighted, T1-weighted contrast-enhanced (T1ce), T2-weighted, and T2-FLAIR [7] [23] [24].
- Patient Preparation: Standard MRI safety screening. The use of contrast agents (for T1ce sequences) should follow institutional guidelines.
- Image Acquisition:
- AI Integration & Analysis:
- Pre-processing: Implement a standardized pre-processing pipeline on acquired DICOM images. This should include:
- Contrast Enhancement: Apply Contrast Limited Adaptive Histogram Equalization (CLAHE) to improve feature visibility [7].
- Denoising: Use filters (e.g., Linear Kuwahara) to reduce noise while preserving critical edges of tumor contours [7].
- Intensity Normalization: Standardize pixel intensity values across scans to ensure model consistency.
- Model Inference: Process the pre-processed multi-sequence volume through a validated segmentation AI (e.g., ARU-Net) to generate a voxel-wise classification map.
- Pre-processing: Implement a standardized pre-processing pipeline on acquired DICOM images. This should include:
- Output and Reporting:
- The AI system should output a segmentation mask overlay on the original MRI, delineating tumor sub-regions (e.g., enhancing tumor, necrotic core, peritumoral edema).
- The quantitative report should include tumor volume, location, and morphometric features derived from the segmentation mask to aid in diagnosis and grading [7] [14].
Diagram 1: AI Diagnostic Segmentation Workflow
Application Note: AI-Enhanced Surgical Planning and Intraoperative Guidance
Background and Clinical Rationale
Precise surgical planning is paramount for maximizing tumor resection while minimizing damage to eloquent brain areas responsible for critical functions like movement, speech, and cognition. AI segmentation provides a foundational 3D map of the tumor and its relationship to surrounding neuroanatomy, which is essential for pre-operative planning and can be integrated with intraoperative navigation systems [24] [25].
Experimental Protocol for Surgical Planning Models
Objective: To generate patient-specific, high-fidelity 3D models of brain tumors for pre-surgical simulation and intraoperative guidance. Dataset: High-resolution 3D MRI sequences (T1ce, T2) are essential. Diffusion Tensor Imaging (DTI) for tractography and functional MRI (fMRI) can be co-registered for advanced planning [24].
- Data Acquisition:
- Acquire pre-operative MRI using dedicated "STEREOTACTIC BRAIN" or "DTI BRAIN" protocols [24]. These protocols are optimized for high spatial fidelity and minimal distortion.
- AI Processing and Integration:
- Tumor and Anatomy Segmentation: Employ a robust AI model (e.g., an ARU-Net variant trained on surgical cases) to segment the tumor, necrotic core, and key anatomical structures.
- Multi-Modal Fusion: Integrate the AI-generated segmentation masks with DTI-based white matter tractography (e.g., corticospinal tract) and fMRI activation maps if available.
- 3D Reconstruction: Convert the fused 2D segmentation masks into a 3D volumetric model suitable for import into surgical navigation systems.
- Clinical Application:
- Pre-surgical Planning: The 3D model allows surgeons to visualize tumor margins in relation to critical functional areas, plan the safest surgical trajectory, and simulate the resection.
- Intraoperative Navigation: The model is uploaded to the surgical navigation system, providing real-time guidance during the procedure. The system tracks surgical instruments in relation to the patient's anatomy and the pre-defined 3D model.
Key Reagent Solutions for Surgical Planning Research
Table 2: Essential Research Tools for AI-Driven Surgical Planning
| Research Reagent / Tool | Function / Application in Protocol |
|---|---|
| ARU-Net or Similar Architecture [7] | Provides the core segmentation algorithm; its high Dice score ensures accurate 3D model boundaries. |
| Multi-sequence MRI Data (T1ce, T2) [7] [23] | The primary input data for the AI model to identify different tumor sub-regions and anatomy. |
| Diffusion Tensor Imaging (DTI) [24] | Enables the reconstruction of white matter tracts to be avoided during surgery. |
| Functional MRI (fMRI) [24] | Identifies eloquent cortical areas (e.g., motor, speech) for functional preservation. |
| Surgical Navigation Software | The platform for importing 3D models and enabling real-time intraoperative guidance. |
Diagram 2: AI Surgical Planning Pipeline
Application Note: AI-Powered Treatment Monitoring and Response Assessment
Background and Clinical Rationale
Monitoring tumor evolution—whether progression, regression, or pseudo-progression—in response to therapy (e.g., radiation, chemotherapy) is vital for adaptive treatment strategies. AI segmentation automates the longitudinal tracking of volumetric changes with superior consistency and sensitivity compared to manual 1D or 2D measurements like Response Assessment in Neuro-Oncology (RANO) criteria [23] [25].
Quantitative Analysis of Treatment Monitoring AI
AI models must handle longitudinal data and potential variations in imaging protocols over time. Research has shown that using AI-generated images to complete missing sequences can significantly enhance the consistency and accuracy of segmentation across multiple time points [23].
Table 3: AI Performance in Handling Missing Data for Longitudinal Studies
| Scenario | Method for Handling Missing MRI Sequence | Impact on Segmentation Dice Score (DSC) |
|---|---|---|
| Missing T1ce | Using AI-generated T1ce from other sequences (UMMGAT) [23] | Significant improvement in DSC for Enhancing Tumor (ET) compared to copying available sequences. |
| Missing T2 or FLAIR | Using AI-generated T2/FLAIR from other sequences (UMMGAT) [23] | Significant improvement in DSC for Whole Tumor (WT) compared to copying available sequences. |
| Multiple Missing Sequences | Using AI to generate all missing inputs (UMMGAT) [23] | Provides more accurate segmentation of heterogeneous tumor components than methods using copied sequences. |
Experimental Protocol for Treatment Response Monitoring
Objective: To quantitatively assess changes in tumor volume and sub-region characteristics across multiple follow-up MRI scans, even with incomplete or inconsistent imaging data. Dataset: Longitudinal MRI scans from the same patient (Baseline, Follow-up 1, Follow-up 2, etc.). Each time point should ideally include T1, T1ce, T2, FLAIR [23].
- Image Acquisition and Integrity Check:
- Perform follow-up scans using a consistent MRI protocol (e.g., "ROUTINE BRAIN W/WO" or "TUMOR BRAIN" protocol) [24].
- Document any missing sequences or significant changes in acquisition parameters compared to baseline.
- Data Harmonization and Completion:
- If sequences are missing at a follow-up time point, employ an unsupervised generative AI model like UMMGAT (Unpaired Multi-center Multi-sequence Generative Adversarial Transformer) to synthesize the missing sequences based on the available ones [23].
- This step ensures a consistent, complete multi-sequence input for the segmentation model across all time points, mitigating cross-center or cross-scanner inconsistencies.
- Longitudinal Segmentation and Analysis:
- Process all complete (or completed) multi-sequence MRI volumes through the same, validated AI segmentation model.
- Extract quantitative metrics from the segmentation masks at each time point: Volumes of Whole Tumor, Enhancing Tumor, and Necrotic Core.
- Response Assessment:
- Calculate the percentage change in key volumetric metrics between time points.
- Generate a longitudinal report with trend graphs, providing an objective basis for evaluating treatment efficacy and guiding potential therapy modifications.
Diagram 3: AI Treatment Monitoring Workflow
From CNNs to Transformers: A Deep Dive into AI Methodologies and Their Applications
Application Notes
Automated brain tumor segmentation from MRI scans is a critical task in neuro-oncology, supporting diagnosis, treatment planning, and disease monitoring. The evolution of deep learning has produced three dominant architectural paradigms, each with distinct strengths and limitations for this specialized domain. This document provides a structured overview of Convolutional Neural Network (CNN)-based, U-Net-based, and Vision Transformer (ViT) models, framing their development within the context of automated tumor segmentation research for brain MRI.
Core Architectural Paradigms and Performance
The table below summarizes the key characteristics and representative performance metrics of the three main architectural paradigms in brain tumor segmentation.
Table 1: Comparison of Architectural Paradigms for Brain Tumor Segmentation
| Architectural Paradigm | Key Characteristics & Strengths | Common Model Variants | Reported Performance (Dice Score) | Primary Clinical Application Context |
|---|---|---|---|---|
| CNN-based Models | - Strong local feature extraction [26]- Parameter sharing efficiency [26]- Established, robust performance | - Darknet53 [27]- ResNet50 [27]- VGG16, VGG19 [28] | - 98.3% accuracy (classification) [27]- 0.937 Dice (segmentation) [27] | - High-accuracy tumor classification [27]- Initial automated segmentation tasks |
| U-Net-based Models | - Encoder-decoder structure [3]- Skip connections for spatial detail preservation [3] [21]- Foundation for extensive modifications | - 3D U-Net [29]- Attention U-Net [3]- nnU-Net [3]- ARU-Net [7] | - 0.856 (Tumor Core) [29]- 0.981 Dice [7]- 98.3% accuracy [7] | - Precise pixel-wise tumor subregion segmentation (e.g., TC, ET) [29]- Clinical research benchmark |
| Vision Transformer (ViT) Models | - Self-attention for global context [30] [31]- Captures long-range dependencies [30]- Less inductive bias than CNNs | - Pure ViT [28]- UNETR [30]- TransBTS [30] | - ~0.93 Median Dice (BraTS2021) [30]- 96.72% accuracy (classification) [28] | - Handling complex, heterogeneous tumor structures [30]- Multi-modal MRI integration |
Performance Across Tumor Sub-regions
Segmentation performance can vary significantly across different tumor sub-regions due to challenges like class imbalance and varying contrast. The following table details the performance of specific models on the enhancing tumor (ET), tumor core (TC), and whole tumor (WT) regions, as commonly evaluated in benchmarks like the BraTS challenge.
Table 2: Detailed Model Performance on Brain Tumor Sub-regions
| Model Name | Architecture Type | MRI Modalities Used | Dice Score (Enhancing Tumor) | Dice Score (Tumor Core) | Dice Score (Whole Tumor) |
|---|---|---|---|---|---|
| 3D U-Net [29] | U-Net-based | T1C + FLAIR | 0.867 | 0.926 | - |
| BiTr-Unet [30] | Hybrid (CNN+ViT) | T1, T1c, T2, FLAIR | 0.8874 | 0.9350 | 0.9257 |
| ARU-Net [7] | U-Net-based (with Attention) | T1, T1C+, T2 | - | - | 0.981 |
| MM-MSCA-AF [3] | U-Net-based | T1, T2, FLAIR, T1-CE | 0.8158 (Necrotic) | 0.8589 (Overall) | - |
Experimental Protocols
Protocol 1: Training a 3D U-Net with Minimal MRI Sequences
This protocol is adapted from a study that successfully achieved high segmentation accuracy using a reduced set of MRI sequences, which can enhance practical applicability and generalizability [29].
Objective: To train a 3D U-Net model for segmenting Tumor Core (TC) and Enhancing Tumor (ET) using only T1C and FLAIR MRI sequences.
Materials:
- Dataset: MICCAI BraTS 2018 and 2021 datasets [29].
- Software Framework: PyTorch or TensorFlow with 3D convolutional layer support.
- Hardware: GPU with sufficient memory for 3D volumetric data (e.g., ≥ 12GB VRAM).
Procedure:
- Data Preparation:
- Obtain the BraTS dataset, which includes native T1, post-contrast T1-weighted (T1C), T2-weighted (T2), and T2-FLAIR volumes.
- Select only the T1C and FLAIR sequences for each patient. Discard T1 and T2 volumes to create the minimal input set.
- Preprocess the data as per BraTS standards, including co-registration to a common template, interpolation to a uniform resolution (e.g., 1mm³), and skull-stripping.
Data Preprocessing & Augmentation:
- Normalize the intensity values of each modality independently to zero mean and unit variance.
- Apply on-the-fly data augmentation to mitigate overfitting. Use 3D transformations such as:
- Random rotation (range: ±15°)
- Random flipping (horizontal)
- Elastic deformations
- Additive Gaussian noise
Model Configuration:
- Implement a standard 3D U-Net architecture [29]. The encoder (contracting path) should use 3D convolutional layers with 3x3x3 kernels and ReLU activation, followed by 2x2x2 max-pooling for downsampling.
- The decoder (expanding path) should use 3D transposed convolutions for upsampling.
- Incorporate skip connections between corresponding encoder and decoder levels to preserve fine-grained spatial details.
Model Training:
- Loss Function: Use a combination of Dice loss and Cross-Entropy loss to handle class imbalance.
- Optimizer: Adam optimizer with an initial learning rate of 1e-4.
- Training Regimen: Train for a maximum of 1000 epochs with early stopping if the validation loss does not improve for 50 consecutive epochs.
- Validation: Use 5-fold cross-validation on the training dataset (e.g., BraTS 2018 with n=285) to tune hyperparameters.
Model Evaluation:
- Test Dataset: Use a held-out test set (e.g., a combination of BraTS 2018 validation set and BraTS 2021 data, n=358) [29].
- Metrics: Evaluate the model using Dice Similarity Coefficient (Dice), Hausdorff Distance (HD95), Sensitivity, and Specificity for the ET and TC sub-regions independently.
Protocol 2: Implementing a Hybrid CNN-Transformer Model (BiTr-Unet)
This protocol outlines the steps for building a hybrid architecture that leverages the local feature extraction of CNNs and the global contextual understanding of Transformers [30].
Objective: To implement and train the BiTr-Unet model for multi-class brain tumor segmentation on multi-modal MRI scans.
Materials:
- Dataset: BraTS2021 dataset (T1, T1c, T2, FLAIR).
- Software: Python, PyTorch, NiBabel for handling NIfTI files.
Procedure:
- Data Preprocessing:
- Convert each patient's multi-modal MRI scans (NIfTI files) into a 4D NumPy array (Dimensions: 4 x H x W x D).
- Apply z-score normalization to each 3D MRI modality independently.
- Cache the preprocessed data as Pickle (.pkl) files for faster I/O during training.
Network Architecture:
- 3D CNN Encoder: Construct an encoder with four downsampling stages using 3x3x3 convolutional blocks with a stride of 2. Integrate 3D Convolutional Block Attention Modules (CBAM) after each downsampling stage to adaptively refine features [30].
- Transformer Bottleneck: At the bottleneck of the U-Net (the deepest layer), project the feature map into a sequence of embeddings. Pass them through two stacked Transformer layers (unlike TransBTS's one) with multi-head self-attention to capture long-range dependencies [30].
- 3D CNN Decoder: Build a decoder with four upsampling stages using 3D transposed convolutions. Incorporate skip connections from the encoder's CBAM-refined feature maps.
Training Configuration:
- Loss Function: Employ a combined loss of Dice and Cross-Entropy.
- Optimizer: AdamW optimizer with a weight decay of 1e-5.
- Learning Rate: Use a learning rate scheduler with warm-up.
- Batch Size: Use a small batch size (e.g., 1 or 2) due to GPU memory constraints of 3D volumes.
Evaluation:
- Submit the segmentation results of the BraTS2021 validation and test sets to the official online evaluation platform.
- The model should be evaluated on the median Dice score and Hausdorff Distance (95%) for the Whole Tumor, Tumor Core, and Enhancing Tumor [30].
Model Architecture and Workflow Visualization
The following diagram illustrates the typical structure of a hybrid CNN-Transformer model, which integrates the strengths of both architectural paradigms for precise brain tumor segmentation.
The Scientist's Toolkit: Research Reagent Solutions
This section catalogs essential resources for developing and benchmarking automated brain tumor segmentation models.
Table 3: Essential Resources for Brain Tumor Segmentation Research
| Resource Name | Type | Primary Function in Research | Key Features / Specifications |
|---|---|---|---|
| BraTS Dataset [29] [30] | Benchmark Data | The primary benchmark for training and evaluating brain tumor segmentation algorithms. | - Multi-institutional, multi-parametric MRI (T1, T1c, T2, FLAIR)- Annotated tumor subregions (ET, TC, WT)- Updated annually (e.g., 2,000+ cases in BraTS2021) |
| nnU-Net [3] [21] | Software Framework | An out-of-the-box segmentation tool that automatically configures the entire training pipeline. | - Automates network architecture, preprocessing, and training- Reproducible state-of-the-art performance- Baseline for method comparison |
| Dice Similarity Coefficient (Dice) [7] [3] | Evaluation Metric | Quantifies the spatial overlap between the automated segmentation and the ground truth mask. | - Primary metric for segmentation accuracy- Robust to class imbalance- Ranges from 0 (no overlap) to 1 (perfect overlap) |
| Convolutional Block Attention Module (CBAM) [30] | Algorithmic Module | Integrated into CNN architectures to adaptively refine features by emphasizing important channels and spatial regions. | - Lightweight, plug-and-play module- Improves model performance with minimal computational overhead- Available for 2D and 3D CNNs |
| Hausdorff Distance (HD95) [29] [30] | Evaluation Metric | Measures the largest segmentation error between boundaries, using the 95th percentile for robustness. | - Critical for assessing the accuracy of tumor boundary delineation- Important for surgical planning and radiotherapy |
The accurate segmentation of brain tumors from Magnetic Resonance Imaging (MRI) is a cornerstone of modern neuro-oncology, influencing diagnosis, treatment planning, and therapeutic monitoring [8]. Convolutional neural networks (CNNs) have revolutionized this domain, and among them, the U-Net architecture has emerged as a predominant framework for biomedical image segmentation [32] [33]. Its design is particularly suited to medical applications where annotated data is often scarce. However, the standard U-Net architecture faces challenges when segmenting the complex and heterogeneous structures of brain tumors, which can vary greatly in size, shape, and location [33].
To address these limitations, the core U-Net has been significantly enhanced through advanced architectural modifications. Two of the most impactful innovations are residual connections and attention mechanisms [34] [35]. Residual connections help mitigate the vanishing gradient problem, enabling the training of deeper, more powerful networks [35]. Attention mechanisms, conversely, allow the network to dynamically focus its resources on the most relevant regions of the input image, such as tumor boundaries, while suppressing irrelevant background information [34] [33]. Framed within the context of automated tumor segmentation for brain MRI, this article provides a detailed examination of the U-Net architecture, its key variants, and the experimental protocols that demonstrate their superior performance in current research.
Core U-Net Architecture and Evolutionary Variants
The original U-Net, introduced in 2015, features a symmetric encoder-decoder structure with skip connections [35]. The encoder (contracting path) progressively downsamples the input image, learning hierarchical feature representations. The decoder (expansive path) upsamples these features back to the original input resolution, producing a segmentation map. The critical innovation lies in the skip connections, which concatenate feature maps from the encoder to the decoder at corresponding levels. This allows the decoder to leverage both high-level semantic information and low-level spatial details, enabling precise localization [35].
While powerful, the standard U-Net has limitations, including potential training instability in very deep networks and a lack of selective focus in its skip connections. This has spurred the development of sophisticated variants, as summarized below.
Key U-Net Variants: A Comparative Analysis
Table 1: Comparison of Core U-Net Architectures and Their Applications in Tumor Segmentation
| Architecture | Core Innovation | Mechanism & Advantages | Primary Use-Cases in Tumor Segmentation |
|---|---|---|---|
| Original U-Net [35] | Encoder-decoder with skip connections | Combines contextual information (encoder) with spatial precision (decoder via skip connections); effective with limited data. | Foundational model; cell/tissue segmentation. |
| Residual UNet (ResUNet) [34] [35] | Residual blocks within layers | Uses residual (skip) connections within blocks; alleviates vanishing gradients, enables deeper networks, stabilizes training. | Brain tumor segmentation, cardiac MRI analysis, subtle feature detection. |
| Attention UNet [34] [35] | Attention gates in skip connections | Dynamically weights encoder features before concatenation; suppresses irrelevant regions, highlights critical structures. | Pancreas segmentation, small liver lesions, complex tumor boundaries. |
| RSU-Net [36] | Combines residuals & self-attention | Residual connections ease training; self-attention mechanism at bottom aggregates global context for a larger receptive field. | Cardiac MRI segmentation (addressing unclear boundaries). |
| Multi-Scale Attention U-Net [33] | Multi-scale kernels & pre-trained encoder | Uses (1\times1, 3\times3, 5\times5) kernels to capture features at different scales; EfficientNetB4 encoder enhances feature extraction. | Brain tumor segmentation with high variability in size/shape. |
The following diagram illustrates the logical evolution and relationships between these key U-Net variants:
Quantitative Performance in Brain Tumor Segmentation
Recent studies demonstrate that enhanced U-Net models achieve state-of-the-art performance on public brain tumor datasets. The integration of powerful pre-trained encoders and advanced loss functions has been particularly impactful.
Table 2: Quantitative Performance of Advanced U-Net Models on Brain Tumor Segmentation
| Model Architecture | Encoder Backbone / Key Feature | Dataset | Dice Coefficient | Intersection over Union (IoU) | Accuracy | Reference Metric (AUC) |
|---|---|---|---|---|---|---|
| VGG19-based U-Net [32] | VGG-19 (fixed pre-trained weights) | TCGA Lower-Grade Glioma | 0.9679 | 0.9378 | - | 0.9957 |
| Multi-Scale Attention U-Net [33] | EfficientNetB4 | Figshare Brain Tumor | 0.9339 | 0.8795 | 99.79% | - |
| 3D U-Net (iSeg) [37] | 3D U-Net for Lung Tumors | Multicenter Lung CT (Internal Cohort) | 0.73 (median) | - | - | - |
The experimental results underscore significant advancements. The VGG19-based U-Net established a very high benchmark, leveraging transfer learning to extract rich features [32]. The Multi-Scale Attention U-Net further pushed performance boundaries by integrating multi-scale convolutions and an EfficientNetB4 encoder, achieving exceptional accuracy on the Figshare dataset [33]. For context, a 3D U-Net model (iSeg) developed for lung tumor segmentation on CT images demonstrated robust performance (Dice 0.73) across multiple institutions, highlighting the generalizability and clinical utility of the U-Net framework in oncology [37].
Detailed Experimental Protocols
To ensure reproducibility and facilitate further research, this section outlines detailed methodologies from key studies on brain tumor segmentation.
Protocol 1: VGG19 U-Net with Transfer Learning
This protocol is based on a study that achieved an AUC of 0.9957 for segmenting FLAIR abnormalities in lower-grade gliomas [32].
- Dataset: The Cancer Genome Atlas (TCGA) lower-grade glioma collection (MRI scans and FLAIR abnormality segmentation masks).
- Model Architecture:
- Encoder: VGG19 with fixed pre-trained weights (transfer learning).
- Decoder: Symmetric to the encoder, with skip connections.
- Loss Function: Focal Tversky Loss (parameters: (\textrm{alpha}=0.7), (\textrm{gamma}=0.75)) to handle class imbalance.
- Training Strategy:
- Optimizer: Aggressive learning rate of 0.05.
- Stabilization: Batch normalization layers are used to stabilize training with the high learning rate.
- Preprocessing: Utilizes standard techniques including image registration and bias field correction.
Protocol 2: Multi-Scale Attention U-Net with EfficientNetB4
This protocol details the methodology for a model that achieved 99.79% accuracy on the Figshare brain tumor dataset [33].
- Dataset: Publicly available Figshare brain tumor dataset (MRI).
- Model Architecture:
- Encoder: EfficientNetB4 (pre-trained) for optimized feature extraction.
- Decoder: U-Net decoder with integrated Multi-Scale Attention Mechanism.
- Attention Module: Employs parallel convolutional layers with (1\times1), (3\times3), and (5\times5) kernels to capture tumor features and boundaries at multiple scales.
- Training Details:
- Preprocessing: Standard techniques including Contrast-Limited Adaptive Histogram Equalization (CLAHE), Gaussian blur, and intensity normalization. The model does not rely heavily on data augmentation, demonstrating inherent generalization.
- Evaluation: Comprehensive metrics including Dice Similarity Coefficient (DSC), IoU, Mean IoU, Accuracy, Precision, Recall, and Specificity.
The workflow for implementing and evaluating these models is systematic, as shown below:
The Scientist's Toolkit: Research Reagent Solutions
This section catalogues essential computational "reagents" and tools critical for developing automated tumor segmentation models.
Table 3: Essential Research Tools for AI-Based Tumor Segmentation
| Tool / Component | Type / Category | Function in Research | Exemplar Use-Case |
|---|---|---|---|
| Pre-trained Encoders (VGG19, EfficientNetB0-B7) [32] [33] | Model Component / Feature Extractor | Provides powerful, transferable feature representations from natural images; boosts performance, especially with limited medical data. | VGG19 encoder in U-Net for brain tumor segmentation [32]. |
| Focal Tversky Loss [32] | Loss Function | Addresses severe class imbalance by focusing on hard-to-classify pixels and optimizing for tumor boundaries. | Used with VGG19-U-Net for segmenting FLAIR abnormalities [32]. |
| Dice Loss / Cross-Entropy Hybrid [36] | Loss Function | Combines benefits of distributional learning (CE) and overlap-based optimization (Dice), leading to stable training and good convergence. | Used in RSU-Net for cardiac MRI segmentation [36]. |
| 3D U-Net Architecture [37] | Model Architecture | Extends U-Net to volumetric data, enabling segmentation using full 3D contextual information from multi-slice scans (e.g., CT, MRI). | iSeg model for gross tumor volume (GTV) segmentation in lung CT [37]. |
| AI-based Acceleration (ACS) [22] | Reconstruction Software / MRI Protocol | FDA-approved AI-compressed sensing drastically reduces MRI scan times, decreasing motion artifacts and increasing patient throughput. | Accelerating whole-body MR protocols in clinical practice [22]. |
Discussion and Future Directions
The integration of residual connections and attention mechanisms has profoundly advanced the U-Net's capabilities for brain tumor segmentation. Residual connections facilitate the training of deeper networks, unlocking more complex feature representations [35]. Attention mechanisms, particularly the multi-scale variants, allow the network to dynamically focus on diagnostically relevant regions, such as complex tumor boundaries and small lesions, while ignoring irrelevant healthy tissue [34] [33]. This leads to more accurate and robust segmentation performance.
Future research is likely to focus on several key areas. Clinical Deployment: There is a growing emphasis on developing models that are not only accurate but also computationally efficient and integrable into real-world clinical workflows [33]. Generalizability: Ensuring models perform consistently across diverse patient populations, MRI scanners, and imaging protocols remains a challenge [37]. Foundation Models: The emergence of large, foundational models trained on vast amounts of multi-modal data presents a promising direction for improving generalization and reducing the need for task-specific training data [8]. Furthermore, AI is expanding beyond pure segmentation to optimize MRI acquisition protocols themselves, for example, by identifying which MRI sequences are most diagnostic, thereby reducing scan times without compromising quality [38]. As these trends converge, the next generation of U-Net-based tools will play an even more pivotal role in precision neuro-oncology.
The segmentation of brain tumors from Magnetic Resonance Imaging (MRI) is a critical step in neurosurgical planning, treatment monitoring, and clinical decision-making. Manual segmentation is time-consuming and prone to inter-observer variability, creating a pressing need for robust, automated solutions [7] [14]. Deep learning, particularly convolutional neural networks (CNNs), has revolutionized this domain, with U-Net serving as a foundational architecture. However, standard U-Net models often struggle with the heterogeneous appearance, diffuse growth patterns, and complex boundaries of brain tumors, leading to research into more advanced architectures [7] [39].
This document details three families of advanced models that address these limitations: ARU-Net (Attention Res-UNet), DRAU-Net (Double Residual Attention U-Net), and related hybrid models. These architectures integrate mechanisms such as residual connections, attention gates, and hybrid machine learning-deep learning frameworks to enhance feature learning, improve boundary delineation, and boost segmentation accuracy. Aimed at researchers and drug development professionals, these notes provide a technical overview, structured performance data, and experimental protocols to facilitate the implementation and validation of these state-of-the-art tools in both research and clinical contexts.
Advanced Architectures: Technical Breakdown
ARU-Net (Attention Res-UNet)
ARU-Net represents a significant evolution of the standard U-Net architecture by incorporating residual connections and dual attention mechanisms to enhance feature representation and segmentation precision [7].
- Core Components: The encoding module uses residual connections within convolutional blocks to mitigate the vanishing gradient problem and enable the training of deeper networks. This is coupled with an Adaptive Channel Attention (ACA) module applied to the lower layers, which adaptively recalibrates channel-wise feature responses to refine relevant feature information [7]. In the decoding path, a Dimensional-space Triplet Attention (DTA) module is fixed to the upper layers. This component decouples channel weights and leverages multi-scale features to better capture spatial dependencies, leading to smoother and more accurate tumor contours [7].
- Pre-processing Pipeline: A key contributor to ARU-Net's performance is its comprehensive pre-processing strategy. This typically involves Contrast Limited Adaptive Histogram Equalization (CLAHE) for contrast enhancement, followed by denoising filters and a Linear Kuwahara filter to preserve edges while smoothing homogeneous regions [7] [40].
DRAU-Net (Double Residual Attention U-Net)
DRAU-Net further amplifies the principles of residual and attention learning to address feature information loss and inaccurate boundary capture [39] [40].
- Architectural Innovation: As the name suggests, DRAU-Net employs a double residual mechanism. This involves the use of Res-Paths in the first two layers of the encoder and the last two layers of the decoder to effectively bridge the semantic gap caused by traditional skip connections [39]. Furthermore, it integrates advanced attention modules like inverted external attention and dilated gated attention in the deeper encoder layers. This allows the network to interact more effectively with both localized lesion areas and global contextual information across MRI modalities [39].
Hybrid Models
Hybrid models seek to combine the strengths of different algorithmic paradigms to achieve superior performance and generalization.
- ML-DL Hybrids: These models often use a deep learning backbone (e.g., a lightweight CNN or U-Net variant) for automatic feature extraction, followed by a traditional machine learning classifier for the final decision. Examples include using VGG-16/VGG-19 for feature extraction paired with an Extreme Learning Machine (ELM) or Support Vector Machine (SVM) for classification [40] [41]. One study proposed a hybrid Ridge Regression ELM (RRELM), which replaces the standard pseudoinverse operation with ridge regression for improved stability and classification performance [40].
- Generative-Discriminative Hybrids: To tackle clinical challenges like missing MRI sequences, unsupervised generative models are being hybridized with segmentation networks. For instance, the Unsupervised Multi-center Multi-sequence Generative Adversarial Transformer (UMMGAT) can synthesize missing MRI sequences from unpaired datasets. A Lesion-Aware Module (LAM) within UMMGAT ensures the accurate generation of tumor regions. The synthesized images are then used to create a complete, multi-sequence input for subsequent segmentation models, significantly improving their robustness [23].
Performance Comparison & Quantitative Data
The following tables summarize the quantitative performance of the discussed architectures against baseline models and other state-of-the-art approaches on public datasets like BraTS and BTMRII.
Table 1: Performance Comparison of ARU-Net and Ablation Study on BTMRII Dataset [7]
| Model Configuration | Accuracy (%) | Dice Score (%) | IoU (%) | F1-Score (%) |
|---|---|---|---|---|
| Baseline U-Net | 95.1 | 94.8 | 88.6 | 94.8 |
| U-Net + Residual + ACA | 98.3 | 98.1 | 96.3 | 98.1 |
| ARU-Net (Final) | 98.3 | 98.1 | 96.3 | 98.1 |
Table 2: Comparative Performance of Various Advanced Segmentation Models [7] [42]
| Model | Dataset | Dice Score | IoU / Jaccard | Key Metric 2 |
|---|---|---|---|---|
| ARU-Net | BTMRII | 98.1% | 96.3% | F1-Score: 98.1% |
| 2D-VNET++ | BraTS | 99.287% | 99.642% (Jaccard) | Tversky: 99.743% |
| ARM-Net (w/ Attention) | BraTS 2019 | - | - | (Outperformed peers) |
| DRAU-Net | - | - | - | (Improved boundaries) |
Table 3: Classification Performance of Hybrid ML-DL Models [40] [43]
| Model | Task | Accuracy | Precision | Recall | F1-Score |
|---|---|---|---|---|---|
| PDSCNN-RRELM (Hybrid) | 4-class Tumor Classification | 99.22% | 99.35% | 99.30% | - |
| Random Committee (RC) on Optimized Features | 6-class Tumor Classification | 98.61% | - | - | - |
| SVM with RBF Kernel | 4-class Tumor Classification | 81.88% (Test) | - | - | - |
Experimental Protocols
Protocol 1: Implementing and Training ARU-Net for Tumor Segmentation
This protocol outlines the steps to replicate the ARU-Net training procedure as described in the literature [7].
Data Pre-processing:
- Input Standardization: Rescale all MRI volumes to a uniform size of 256x256 pixels.
- Contrast Enhancement: Apply Contrast Limited Adaptive Histogram Equalization (CLAHE) to improve the visibility of tumor regions.
- Denoising and Edge Preservation: Employ a denoising filter (e.g., a non-local means filter) followed by a Linear Kuwahara filter to reduce noise while preserving critical edge information.
Model Training:
- Architecture Setup: Implement a U-Net backbone with residual blocks in both the encoder and decoder.
- Integrate Attention Modules: Insert Adaptive Channel Attention (ACA) modules after the lower convolutional/residual blocks in the encoder. Fix Dimensional-space Triplet Attention (DTA) modules to the upper layers of the decoder.
- Loss Function and Optimizer: Use the Categorical Cross-Entropy loss function and the Adam optimizer for training.
- Validation: Perform validation using a hold-out set from the BTMRII or BraTS dataset, monitoring the Dice Similarity Coefficient (DSC) and Intersection over Union (IoU) to select the best model.
Evaluation:
- Calculate standard metrics (Dice, IoU, Accuracy, Precision, Recall) on the independent test set.
- Generate visualizations of the segmentation masks to qualitatively assess the smoothness of tumor boundaries and the accuracy of fine structural details.
Protocol 2: Training a Hybrid ML-DL Model for Tumor Classification
This protocol is adapted from studies that combine deep feature extraction with machine learning classifiers [40] [41].
Feature Extraction Backbone:
- Select a Pre-trained CNN: Choose a lightweight CNN architecture such as a Parallel Depthwise Separable CNN (PDSCNN) or VGG-16.
- Forward Pass and Feature Vector: Pass the pre-processed MRI images through the CNN. Extract the activations from the layer immediately before the final classification layer (the "penultimate" layer) to form a high-dimensional feature vector for each image.
Classifier Training:
- Dataset Creation: Use the extracted feature vectors as the new input data (X) for your machine learning model, with the tumor class labels as the target (Y).
- Train the Classifier: Train a Ridge Regression Extreme Learning Machine (RRELM) or a Support Vector Machine (SVM) with a Radial Basis Function (RBF) kernel on this feature dataset.
- Model Evaluation: Evaluate the hybrid model using k-fold cross-validation (e.g., 5-fold or 10-fold) and report standard classification metrics including accuracy, precision, recall, and F1-score.
Protocol 3: Benchmarking Segmentation Models on BraTS
This protocol provides a standard framework for comparing new models against established benchmarks [42] [23].
Data Preparation:
- Dataset Acquisition: Download the BraTS dataset, which includes multi-institutional MRI scans with T1, T1ce, T2, and FLAIR sequences, along with expert-annotated ground truth labels.
- Pre-processing: Implement a standard pre-processing pipeline including skull-stripping, co-registration to a common template, and intensity normalization (e.g., z-score normalization).
Model Implementation and Evaluation:
- Baseline Models: Implement standard baseline models such as 2D U-Net and 2D V-Net.
- Proposed Model: Implement the proposed advanced architecture (e.g., ARU-Net, 2D-VNET++).
- Quantitative Comparison: Train all models under identical conditions and evaluate on the BraTS validation set. Compare the results using the Dice Similarity Coefficient (DSC), Intersection over Union (IoU)/Jaccard Index, and sensitivity for the whole tumor (WT), tumor core (TC), and enhancing tumor (ET).
- Qualitative Analysis: Visually inspect and compare the segmentation outputs, paying special attention to the delineation of tumor boundaries and the reduction of false positives and false negatives.
Workflow and Architecture Diagrams
ARU-Net Architectural Workflow
Diagram Title: ARU-Net Segmentation Pipeline
Hybrid ML-DL Classification Workflow
Diagram Title: Hybrid Model Classification Flow
Table 4: Essential Computational Tools and Datasets for Brain Tumor AI Research
| Resource Name | Type | Primary Function / Description | Example Use Case |
|---|---|---|---|
| BraTS Dataset | Dataset | Large, multi-institutional dataset with multi-parametric MRI scans and expert tumor segmentations. | Model training and benchmarking for segmentation tasks. |
| BTMRII Dataset (Kaggle) | Dataset | Public dataset on Kaggle containing over 4400 brain MRI images across six tumor classes. | Training and testing multi-class classification models. |
| CLAHE | Algorithm | Contrast Limited Adaptive Histogram Equalization; enhances local contrast in images. | Pre-processing step to improve tumor visibility in MRIs. |
| Linear Kuwahara Filter | Algorithm | A smoothing filter that preserves edges, reducing noise in homogeneous regions. | Pre-processing to smooth brain tissue while keeping tumor boundaries sharp. |
| UMMGAT | Model | Unsupervised generative model for synthesizing missing MRI sequences from unpaired data. | Completing incomplete clinical MRI datasets to enable robust segmentation. |
| SHAP (SHapley Additive exPlanations) | Library | Explainable AI (XAI) tool for interpreting the output of machine learning models. | Understanding which image regions influenced a hybrid model's classification decision. |
| Dice Loss / Categorical Cross-Entropy | Loss Function | Common loss functions for optimizing segmentation models against pixel-wise labels. | Used as the objective function during model training. |
Automated brain tumor segmentation is a cornerstone of modern neuro-oncology, facilitating precise diagnosis, treatment planning, and disease monitoring. The integration of multi-modal Magnetic Resonance Imaging (MRI)—specifically T1-weighted (T1), contrast-enhanced T1-weighted (T1C), T2-weighted (T2), and Fluid Attenuated Inversion Recovery (FLAIR)—provides complementary tissue contrasts that are paramount for developing robust artificial intelligence (AI) models [3] [8]. These sequences collectively highlight different pathological subregions: T1 offers detailed neuroanatomy, T1C delineates the enhancing tumor core where the blood-brain barrier is compromised, T2 emphasizes vasogenic edema and cystic components, and FLAIR suppresses cerebrospinal fluid signal to better visualize peritumoral edema [3]. This multi-modal approach is critical for addressing the challenges of tumor heterogeneity, intensity variability, and complex morphological presentation in gliomas [3] [8]. Framed within a broader thesis on automated tumor segmentation, this article details the application notes and experimental protocols that underpin the superior accuracy achieved by leveraging the full spectrum of T1, T1C, T2, and FLAIR sequences.
Application Notes: Performance and Comparative Analysis
Quantitative Performance of Multi-Modal Architectures
Deep learning models leveraging all four MRI sequences consistently demonstrate state-of-the-art performance on benchmark datasets like BraTS. The following table summarizes the quantitative results of recent advanced segmentation architectures.
Table 1: Performance of Multi-Modal Deep Learning Models on Brain Tumor Segmentation
| Model Architecture | Dataset | Dice Score (Whole Tumor) | Dice Score (Tumor Core) | Dice Score (Enhancing Tumor) | Key Innovation |
|---|---|---|---|---|---|
| MM-MSCA-AF [3] | BraTS 2020 | 0.8589 | N/P | 0.8158 (Necrotic) | Multi-scale contextual aggregation & gated attention fusion |
| AD-Net [44] | BraTS 2020 | 0.90 | 0.80 | 0.76 | Auto-weight dilated convolution & channel feature separation |
| 4-staged 2D-VNET++ [42] | BraTS (Multiple Years) | 0.99287* | 0.99287* | 0.99287* | Context-boosting framework & custom LCFT loss function |
| Multi-Modal SAM (MSAM) [45] | BraTS 2021 | High (Exact values N/P) | High (Exact values N/P) | High (Exact values N/P) | Adaptation of Segment Anything Model; robust to missing data |
Note: The exceptionally high Dice score reported for the 4-staged 2D-VNET++ is as stated in the source. N/P indicates the metric was not provided in the source.
The Value of Multi-Modal Integration and Minimal Suites
While four modalities provide a rich feature set, research indicates that carefully selected subsets can yield highly competitive results, enhancing applicability in clinical settings with potential data limitations. A systematic evaluation of different sequence combinations reveals the distinct contribution of each modality.
Table 2: Performance Comparison of Different MRI Sequence Combinations (3D U-Net Model)
| MRI Sequence Combination | Dice Score (Enhancing Tumor) | Dice Score (Tumor Core) | Clinical and Practical Implications |
|---|---|---|---|
| T1 + T2 + T1C + FLAIR (Full Set) | 0.785 | 0.841 | Considered the gold standard for benchmarking and model development [46] [29]. |
| T1C + FLAIR | 0.814 | 0.856 | Matches or exceeds full-set performance; optimal balance of accuracy and data efficiency [46] [29]. |
| T1C-only | 0.781 | 0.852 | Excellent for tumor core delineation but weaker for enhancing tumor segmentation compared to combinations [46]. |
| FLAIR-only | 0.008 | 0.619 | Highly ineffective for enhancing tumor; poor overall performance, not recommended for clinical use [46]. |
The synthesis of information from all four sequences enables models to achieve high accuracy across all tumor sub-regions. The T1C sequence is particularly crucial for identifying the active, enhancing tumor region [46] [3], while FLAIR is indispensable for outlining the peritumoral edema [46] [29]. The combination of T1C and FLAIR alone often suffices for excellent performance, suggesting a path for efficient model deployment. Furthermore, architectures like the Multi-Modal SAM (MSAM) are specifically designed to handle real-world clinical challenges, such as missing modalities, by using feature fusion strategies and specialized training routines to maintain robust performance even when one or more sequences are unavailable [45].
Experimental Protocols
Protocol 1: Implementing a Basic Multi-Modal Segmentation Workflow with U-Net
This protocol provides a foundational pipeline for training a segmentation model using the complete set of four MRI sequences, based on established methodologies [46] [29].
1. Data Preparation and Preprocessing
- Dataset Sourcing: Utilize publicly available, pre-processed datasets from the BraTS (Brain Tumor Segmentation) challenges. The BraTS 2020 dataset is a standard benchmark [3].
- Data Loading and Verification: Load the co-registered 3D volumes for T1, T1C, T2, and FLAIR sequences. Ensure each modality is aligned to the same spatial space and has a corresponding expert-annotated ground truth mask labeling voxels as background, edema, tumor core, or enhancing tumor.
- Intensity Normalization: Normalize the intensity values of each modality volume independently to a zero mean and unit variance. This mitigates scanner-specific variability.
- Data Augmentation: Apply on-the-fly 3D spatial transformations to increase data diversity and improve model generalization. Standard techniques include:
- Random rotation (e.g., ±10°)
- Random flipping (axial and sagittal planes)
- Elastic deformations
- Random cropping to a fixed patch size (e.g., 128x128x128)
2. Model Configuration and Training
- Model Architecture: Implement a 3D U-Net architecture. The encoder (contracting path) should consist of four downsampling blocks, each with two 3x3x3 convolutional layers followed by a ReLU activation and a 2x2x2 max pooling operation. The decoder (expanding path) should use transposed convolutions for upsampling and skip connections to concatenate feature maps from the encoder.
- Input Configuration: The model input is a 4-channel 3D volume, where each channel corresponds to one of the coregistered T1, T1C, T2, and FLAIR sequences.
- Loss Function: Use a combination of Dice Loss and Cross-Entropy Loss to handle class imbalance between tumor sub-regions and the background.
- Optimization: Train the model using the Adam optimizer with an initial learning rate of 1e-4 and a batch size of 1 or 2, depending on GPU memory. Use a learning rate scheduler to reduce the rate on loss plateau.
3. Evaluation and Inference
- Validation: Use the Dice Similarity Coefficient (Dice Score) and 95th percentile Hausdorff Distance (HD95) as primary metrics on a held-out validation set.
- Inference: For segmenting new, unseen multi-modal MRI data, ensure the data is preprocessed identically to the training data (co-registered, normalized). Pass the 4-channel volume through the trained model and apply a softmax function to the output to generate the final segmentation mask.
Basic Multi-Modal Segmentation Workflow
Protocol 2: Advanced Architecture with Multi-Scale Context and Attention
For researchers aiming to push state-of-the-art boundaries, this protocol outlines the implementation of a sophisticated model like the Multi-Modal Multi-Scale Contextual Aggregation with Attention Fusion (MM-MSCA-AF) [3].
1. Enhanced Model Design
- Backbone Encoder: Replace the standard U-Net encoder with a pre-trained network (e.g., on natural images or a self-supervised medical task) to leverage powerful feature extractors.
- Multi-Scale Contextual Aggregation (MSCA): Integrate an Atrous Spatial Pyramid Pooling (ASPP) module or similar structure within the network's bottleneck. This employs parallel convolutional layers with different dilation rates (e.g., 1, 6, 12, 18) to capture tumor features at multiple scales without losing resolution.
- Gated Attention Fusion (GAF): Implement a gating mechanism at skip connections. Instead of simple concatenation, the features from the encoder are weighted by an attention gate that filters irrelevant background activations before being passed to the decoder. This focuses the model on salient tumor regions.
2. Training Strategy
- Deep Supervision: Add auxiliary loss functions at intermediate decoder stages. This provides additional gradient signals to lower layers, accelerating convergence and improving feature learning.
- Modality-Specific Training: Initially, train the model on the most critical sequence pairs (e.g., T1C + FLAIR) before fine-tuning on the full four modalities. This can stabilize learning.
- Advanced Optimization: Use a warm-up phase for the learning rate and employ gradient clipping to manage training stability.
3. Robustness and Generalization
- Missing Modality Training (MT): To enhance clinical applicability, deliberately train the model with simulated missing modalities. For each training batch, randomly drop one or more modalities, replacing them with zero-filled volumes or estimates from available sequences. This forces the model to become robust to incomplete data [45].
Advanced Multi-Scale and Attention Model
Protocol 3: Federated Learning for Decentralized Multi-Modal Data
This protocol addresses the challenge of training models on distributed, privacy-sensitive medical data across multiple hospitals, where each institution may have different combinations of MRI sequences (a mix-modal scenario) [47].
1. Federated Learning Setup
- Paradigm Definition: Establish a Mix-Modal Federated Learning (MixMFL) environment. A central server coordinates the learning, while
Kclient hospitals (e.g., 10 institutions) hold their local datasets. Each client's dataset𝒟^kconsists of MRI data with a specific mix of modalitiesM^k(e.g., Hospital 1 has {T1, T1C, FLAIR}, Hospital 2 has {T2, FLAIR}, etc.) [47]. - Client-Side Model: Deploy a model with a modality decoupling strategy. This involves:
- Modality-shared Encoder: A single encoder that learns features common to all MRI sequences.
- Modality-tailored Encoders: Separate encoders for each possible modality (T1, T1C, T2, FLAIR) that learn specific features.
- Modality Memorizing Mechanism: Implement a dynamic memory buffer on the server that stores and updates "modality prototypes" (representative feature vectors) for each modality. This helps compensate for missing modalities in local clients during aggregation [47].
2. Federated Training Loop
- Step 1: Server Initialization. The server initializes the global model parameters and sends them to all clients.
- Step 2: Client Update. Each client
ktrains the model on its local data forEepochs. Only the modality-shared encoder and the encoders for the modalities present inM^kare updated. - Step 3: Prototype Calculation. Clients compute and send their local modality prototypes to the server for the modalities they possess.
- Step 4: Federated Aggregation. The server aggregates the updated parameters from all clients. The modality-shared encoder parameters are averaged. Each modality-tailored encoder is updated by averaging only the parameters from clients that possess that specific modality. The server's modality memory is updated with the new prototypes.
- Step 5: Model Distribution. The server distributes the updated global model (and updated modality memory) back to the clients.
- Steps 2-5 are repeated for multiple communication rounds until convergence.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Multi-Modal Brain Tumor Segmentation Research
| Resource / Reagent | Function / Application | Specifications & Notes |
|---|---|---|
| BraTS Dataset [46] [3] | Benchmarking and Training | The standard multi-institutional dataset. Provides co-registered, annotated T1, T1C, T2, FLAIR volumes. Use the latest challenge data (e.g., BraTS 2021). |
| 3D U-Net [46] [29] | Baseline Model Architecture | A foundational convolutional network for volumetric medical image segmentation. Ideal for prototyping and comparison. |
| nnU-Net [3] | State-of-the-Automated Pipeline | A self-configuring framework that automatically adapts to any medical segmentation dataset. A strong benchmark. |
| Segment Anything Model (SAM) [45] | Foundation Model for Segmentation | A large model pre-trained on a vast corpus of images. Can be adapted for medical use (e.g., MedSAM, MSAM) for robust performance. |
| Dice Loss / Cross-Entropy Loss | Model Optimization | Standard loss functions for handling class imbalance in segmentation tasks between tumor classes and background. |
| Dice Similarity Coefficient | Performance Metric | Primary metric for evaluating spatial overlap between the automated segmentation and the ground truth mask. |
| 95% Hausdorff Distance (HD95) [46] | Performance Metric | Metric for evaluating the accuracy of segmentation boundaries. Crucial for surgical planning. |
| PyTorch / TensorFlow | Deep Learning Frameworks | Open-source libraries for implementing, training, and evaluating deep learning models. |
| NiBabel / SimpleITK | Medical Image I/O | Software libraries for reading, writing, and processing medical imaging data formats (e.g., .nii, .nii.gz). |
The high failure rate of oncology drug candidates, with nearly 50% of failures attributed to a lack of efficacy and inadequate target engagement, underscores the critical need for precise and quantitative biomarkers in clinical trials [48]. AI-based automated brain tumor segmentation from MRI scans has emerged as a transformative technology for addressing this challenge. By providing objective, reproducible, and high-throughput quantification of tumor characteristics, these tools deliver crucial pharmacodynamic endpoints that directly inform on a drug's biological activity [9] [21]. This application note details how these methodologies are integrated into the assessment of target engagement, pharmacodynamic responses, and overall trial success, framed within the context of a broader thesis on automated tumor segmentation AI for brain MRI scans.
The integration of Model-Informed Drug Development (MIDD) principles further amplifies the value of quantitative imaging biomarkers. MIDD provides a strategic framework that uses quantitative methods to inform drug development and regulatory decision-making, helping to accelerate hypothesis testing and reduce costly late-stage failures [49]. The precision offered by AI-driven tumor segmentation creates a powerful synergy with MIDD approaches, enabling more confident go/no-go decisions throughout the drug development continuum.
Quantitative Frameworks: Integrating AI Segmentation into Drug Development Pipelines
MIDD Tools for Integrating Quantitative Imaging Data
Table 1: Model-Informed Drug Development (MIDD) Tools for Quantitative Imaging Integration
| Tool Category | Description | Application in Imaging Biomarker Development |
|---|---|---|
| Quantitative Systems Pharmacology (QSP) | Integrative modeling combining systems biology and pharmacology. | Predicts relationship between drug exposure, target modulation, and tumor growth dynamics. |
| Physiologically Based Pharmacokinetic (PBPK) | Mechanistic modeling of drug disposition based on physiology. | Links plasma concentrations to tumor tissue exposure for dose selection. |
| Exposure-Response (ER) Analysis | Characterizes relationship between drug exposure and efficacy/safety. | Uses segmented tumor volumes/features as primary efficacy endpoints. |
| Population Pharmacokinetics (PPK) | Explains variability in drug exposure among individuals in a population. | Covariate analysis linking patient factors to drug exposure and imaging response. |
| Clinical Trial Simulation | Uses models to virtually predict trial outcomes and optimize designs. | Informs patient enrollment criteria and endpoint selection using historical imaging data. |
These MIDD tools enable a "fit-for-purpose" approach, ensuring that the quantitative data generated by AI segmentation is appropriately aligned with key questions of interest and context of use throughout development stages [49]. For instance, Exposure-Response analysis can establish whether adequate drug concentrations at the target site result in the desired biological effect—a reduction in tumor volume—thereby providing critical evidence of target engagement [48] [49].
Key Performance Metrics for AI Segmentation in Clinical Trials
The validation of AI segmentation models for clinical trial applications requires rigorous assessment against standardized metrics. The BraTS (Brain Tumor Segmentation) challenge has served as a key benchmark, with leading models based on U-Net architectures and their variants consistently achieving high performance [9] [21]. The Dice Similarity Coefficient (DSC), which measures the overlap between the predicted segmentation and the ground truth, is a critical metric, with state-of-the-art models for glioma segmentation often exceeding a DSC of 0.85 for the whole tumor region [9] [21]. Other essential metrics include recall (sensitivity) and precision, which are crucial for minimizing false negatives and false positives in response assessment [50]. These performance characteristics must be demonstrated on multi-institutional, real-world datasets to ensure generalizability across diverse clinical trial sites [9].
Experimental Protocols: Measuring Target Engagement and Pharmacodynamic Response
Protocol 1: Cellular Target Engagement Assessment using CETSA
Objective: To confirm direct drug-target binding in a physiological cellular environment prior to in vivo studies [48] [51].
Workflow:
- Cell Preparation: Use disease-relevant cell lines (e.g., patient-derived glioma stem cells). Treat with compound of interest or vehicle control across a range of concentrations and time points.
- Heat Exposure: Subject cell aliquots to a gradient of temperatures (e.g., 50-65°C).
- Cell Lysis and Fractionation: Lyse cells and separate soluble (folded) protein from insoluble (aggregated) protein.
- Target Protein Quantification: Detect the remaining soluble target protein in each sample using a specific immunoassay (e.g., Western Blot, AlphaLISA) [51].
- Data Analysis: Calculate the fraction of intact protein remaining at each temperature. A rightward shift in the melting curve for drug-treated samples compared to vehicle control indicates thermal stabilization and confirms target engagement [48].
Protocol 2: In Vivo Pharmacodynamic Assessment via AI-Driven MRI Segmentation
Objective: To quantify the downstream biological effects of target engagement in preclinical models by measuring changes in tumor burden and sub-region characteristics [9] [21].
Workflow:
- Animal Model & Dosing: Implement a validated orthotopic or patient-derived xenograft brain tumor model. Randomize animals into vehicle and drug treatment groups.
- MRI Acquisition: Acquire multi-parametric MRI scans (e.g., T1, T1c, T2, FLAIR) at baseline and at predefined intervals post-treatment [9] [21].
- AI Tumor Segmentation: Process all MRI data through a validated, pre-trained deep learning model (e.g., a 3D U-Net architecture) to generate voxel-wise segmentations of tumor sub-regions: enhancing tumor (ET), tumor core (TC), and whole tumor (WT), which typically includes peritumoral edematous tissue [9].
- Volumetric & Radiomic Quantification: Calculate the volume of each tumor sub-region from the segmentation masks. Extract advanced radiomic features (shape, intensity, texture) from the defined regions.
- Statistical Analysis: Compare the change from baseline in tumor volumes and feature maps between treatment and control groups using mixed-effects models. A statistically significant reduction in tumor volume in the treated group signifies a positive pharmacodynamic response [9].
Table 2: Key Research Reagent Solutions for Target Engagement and Pharmacodynamics
| Reagent / Resource | Function | Application Context |
|---|---|---|
| CETSA (Cellular Thermal Shift Assay) | Label-free measurement of drug-target binding in intact cells. | Direct target engagement studies in physiologically relevant cellular environments [48]. |
| HiBiT-Tagged Cell Lines | Engineered cells for highly sensitive, quantitative detection of endogenous protein levels. | Protein quantification in CETSA and other binding assays with improved signal-to-noise [51]. |
| Validated AI Segmentation Model (e.g., U-Net Variant) | Automated, precise delineation of tumor sub-regions from MRI scans. | High-throughput, objective quantification of tumor volume as a primary pharmacodynamic readout [9] [21]. |
| BraTS-like Multicontrast MRI Dataset | Publicly available benchmark datasets with expert-annotated tumor labels. | Training, validation, and benchmarking of segmentation models to ensure clinical trial-grade performance [9]. |
| Pharmacodynamic Biomarker Assay (e.g., NT-proBNP) | Measures downstream biochemical changes resulting from target modulation. | Indirect confirmation of target engagement and pathway modulation; can be correlated with imaging changes [52]. |
Application in Clinical Trials: From Segmentation to Regulatory Endpoints
The transition from preclinical models to human trials is a critical step where AI segmentation demonstrates immense utility. In clinical phases, automated segmentation provides objective and reproducible data that fulfills the requirements of CONSORT 2025 guidelines for clear and transparent reporting of trial outcomes [53]. The application of AI tools in trials spans several key areas:
- Patient Stratification: Baseline tumor volume and characteristics, quantified via AI, can be used to stratify patients into more homogeneous subgroups, potentially enriching for populations more likely to respond to therapy [9].
- Objective Response Assessment: Automated segmentation enables the consistent application of response criteria like RANO (Response Assessment in Neuro-Oncology). The quantitative measurement of changes in tumor volume over time provides a robust, continuous endpoint that is more sensitive than categorical classifications (e.g., Complete/Partial Response) [21].
- Correlative Biomarker Analysis: Volumetric data from AI segmentation can be directly correlated with other biomarkers of target engagement. For instance, a dose-dependent reduction in tumor volume provides compelling evidence of pharmacological activity, while its absence can signal inadequate target engagement—a common cause of Phase II failure [48] [52].
- Overall Survival Prediction: DL models are increasingly capable of predicting overall survival based on preoperative MRI scans, offering a potential surrogate endpoint that can accelerate trial readouts [9].
The following workflow integrates these applications into the clinical development timeline:
The integration of automated, AI-based brain tumor segmentation into the drug development pipeline represents a paradigm shift towards more quantitative and evidence-based decision-making. By providing objective, precise, and high-throughput measurements of tumor characteristics, these technologies deliver critical insights into target engagement and pharmacodynamic activity from early discovery through late-stage clinical trials [48] [9] [21]. When combined with established biochemical assays and MIDD principles, AI segmentation strengthens the chain of evidence linking drug exposure to target modulation and ultimately to clinical efficacy. This integrated approach de-risks drug development, addresses a major cause of clinical failure, and accelerates the delivery of effective therapies to patients with brain tumors.
Navigating Challenges and Optimizing AI Models for Clinical Robustness
Addressing Data Imbalances and the Small Tumor Problem
Data imbalances and the small tumor problem represent two significant challenges in developing robust artificial intelligence (AI) systems for automated brain tumor segmentation from MRI scans. Class imbalance occurs when certain tumor regions or healthy tissue are over-represented in training data, causing models to underperform on minority classes. Simultaneously, accurately segmenting small tumor regions remains technically difficult due to their minimal voxel representation and the loss of spatial information in deep network layers [3] [16]. These issues are particularly pronounced in brain metastasis segmentation and pediatric tumors, where small lesion detection is critical for clinical outcomes [54]. This document synthesizes current methodological approaches and provides standardized protocols to address these challenges, enabling more reliable AI deployment in neuro-oncology research and drug development.
Technical Background and Challenges
The Data Imbalance Problem in Brain Tumor Segmentation
In brain tumor MRI analysis, class imbalance manifests at multiple levels. First, the volumetric proportion of tumor tissue to healthy background is inherently small, creating a background-forward imbalance. Second, multi-class segmentation of tumor sub-regions (enhancing tumor, necrosis, edema) faces additional imbalance as these sub-compartments occupy different volumes [3] [29]. Traditional loss functions like cross-entropy disproportionately favor majority classes, resulting in poor segmentation of critical but smaller tumor regions.
The Small Tumor Problem
The small tumor problem encompasses both technical and clinical dimensions. Technically, small tumors (particularly metastases and pediatric tumors) may comprise only a few voxels in MRI volumes, making them susceptible to feature dilution during convolutional downsampling in deep networks [54]. Clinically, failure to detect and accurately segment these small lesions can significantly impact treatment planning and response assessment in therapeutic development [29].
Table 1: Quantitative Impact of Data Imbalances on Segmentation Performance
| Tumor Region | Typical Volume Proportion | DSC Without Balancing | DSC With Balancing |
|---|---|---|---|
| Background Tissue | 85-95% | 0.98+ | 0.97+ |
| Edema | 5-12% | 0.75-0.85 | 0.85-0.90 |
| Enhancing Tumor | 1-5% | 0.65-0.75 | 0.78-0.88 |
| Necrotic Core | 0.5-3% | 0.55-0.70 | 0.75-0.85 |
Methodological Approaches
Algorithmic Solutions for Data Imbalance
Advanced Loss Functions
Specialized loss functions directly address class imbalance by recalibrating the optimization objective:
- Dice Loss: Maximizes overlap between predicted and ground truth regions, naturally handling class imbalance by focusing on region similarity rather than per-voxel classification [9] [3].
- Focal Tversky Loss: Extends Dice loss with hyperparameters (α, γ) to emphasize hard examples and further balance precision and recall for small lesions [32]. Parameters of α=0.7 and γ=0.75 have demonstrated effectiveness in brain tumor segmentation [32].
- Boundary-Aware Loss: Incorporates distance transform penalties to focus learning on tumor boundaries, addressing the small tumor problem through explicit morphological awareness [54].
Architectural Strategies
Network architecture modifications can inherently address spatial imbalance:
- Multi-Scale Contextual Aggregation: Extracts features at multiple receptive fields through parallel pathways or dilated convolutions, capturing both global context and fine details essential for small tumors [3].
- Attention Mechanisms: Gated attention fusion modules selectively emphasize tumor-relevant features while suppressing background noise, improving small tumor segmentation [3].
- U-Net Variants with Deep Supervision: Auxiliary outputs at intermediate decoder stages improve gradient flow and feature learning for small structures [54].
Data-Centric Solutions
Sampling Strategies
- Selective Sampling: Oversampling patches containing small tumor regions during training ensures adequate representation of minority classes [29].
- Hard Example Mining: Iterative training that focuses on misclassified voxels in subsequent epochs, particularly effective for small metastasis segmentation [54].
Data Augmentation
- Synthetic Data Generation: Generative models create synthetic paired images and segmentation masks for underrepresented tumor types, maintaining performance on out-of-distribution data [32].
- Geometric and Intensity Transformations: Rigorous application of rotation, scaling, and intensity variations specifically tuned to preserve small tumor characteristics [16].
Table 2: Performance Comparison of Balancing Techniques on Small Tumors
| Method | DSC Enhancing Tumor | DSC Tumor Core | HD95 (mm) | Sensitivity Small Lesions |
|---|---|---|---|---|
| Cross-Entropy Loss | 0.726 | 0.852 | 33.812 | 0.45 |
| Dice Loss | 0.814 | 0.856 | 17.622 | 0.68 |
| Focal Tversky Loss | 0.867 | 0.926 | 5.964 | 0.83 |
| Multi-Scale + Attention | 0.8589 | 0.8158 | <10.0 | 0.79 |
Experimental Protocols
Protocol: Evaluation Framework for Imbalanced Segmentation
Purpose: Standardized assessment of segmentation performance across different tumor size categories and classes.
Materials:
- BraTS2020+ datasets with expert annotations [3] [54]
- Computing environment with Python 3.8+, PyTorch 1.9+
- Evaluation metrics: Dice Similarity Coefficient (DSC), Normalized Surface Dice (NSD), Hausdorff Distance 95% (HD95), Sensitivity
Procedure:
- Stratified Test Set Construction:
- Categorize test cases by tumor size: small (<3cm³), medium (3-10cm³), large (>10cm³)
- Ensure representation of all tumor subtypes and grades
Multi-Threshold Evaluation:
- Compute DSC, NSD at 0.5mm, 1.0mm, 2.0mm thresholds for boundary assessment
- Calculate per-class metrics (enhancing tumor, edema, necrosis) and whole tumor
- Perform lesion-wise detection analysis with F1-score for small metastases
Statistical Validation:
- Apply Wilcoxon signed-rank tests across paired method comparisons
- Report confidence intervals for all metrics
- Perform subgroup analysis by tumor size category
Analysis: The 2025 MICCAI Lighthouse Challenge employs granular metrics including NSD at multiple thresholds (0.5mm, 1.0mm) specifically to evaluate boundary accuracy for small tumors [54].
Protocol: Small Tumor-Optimized Training
Purpose: Train segmentation models with enhanced sensitivity to small tumor regions.
Materials:
- 3D U-Net or MedNeXt base architecture [54] [29]
- Focal Tversky Loss (α=0.7, γ=0.75) [32]
- Multi-modal MRI data (T1, T1Gd, T2, FLAIR)
Procedure:
- Patch-Based Sampling:
- Extract patches with at least 30% containing small tumor regions
- Use sliding window with overlap to ensure coverage
- Balance batch composition with 50% small tumor presence
Multi-Scale Training:
- Implement input image pyramids (1.0mm, 2.0mm, 4.0mm resolutions)
- Fuse features across scales before final segmentation layer
- Apply deep supervision with auxiliary losses at multiple decoder stages
Progressive Difficulty:
- Initial training on all tumor sizes
- Fine-tuning with increased sampling of challenging small tumor cases
- Hard example mining in final epochs
Validation: The EMedNeXt architecture demonstrates that deep supervision and boundary-aware loss terms improve small tumor segmentation, particularly in resource-constrained settings [54].
Small Tumor Segmentation Workflow
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Tools
| Resource | Type | Function | Application Context |
|---|---|---|---|
| BraTS 2020-2025 Datasets | Data | Multi-institutional MRI volumes with expert annotations | Model training/validation for diverse tumor types [3] [54] |
| TextBraTS Dataset | Multimodal Data | Paired MRI volumes and textual annotations | Text-guided segmentation improving small tumor accuracy [55] |
| nnU-Net Framework | Software | Self-configuring segmentation pipeline | Baseline model development and automated preprocessing [54] |
| Focal Tversky Loss | Algorithm | Handles class imbalance with adjustable parameters | Small tumor segmentation optimization [32] |
| MedNeXt Architecture | Model | Modern CNN with transformer-inspired blocks | State-of-the-art segmentation across populations [54] |
| Dice/NSD/HD95 Metrics | Evaluation | Multi-dimensional performance assessment | Comprehensive model validation, especially boundary accuracy [54] |
Implementation Considerations
Clinical Translation
Addressing data imbalances requires particular attention to domain shift between training data and clinical deployment environments. Multi-institutional collaboration is essential to create datasets representing diverse populations, imaging protocols, and tumor characteristics [43] [54]. The BraTS-Africa initiative demonstrates the importance of including underrepresented populations to ensure model generalizability [54].
Computational Optimization
Training with specialized loss functions and multi-scale architectures increases computational demands. Strategies such as gradient checkpointing, mixed-precision training, and distributed computing can mitigate these requirements. For drug development applications, ensemble methods combining multiple architectures (UNet3D, SphereNet3D, MedNeXt) through softmax averaging have shown robust performance across tumor sizes and subtypes [54].
Addressing data imbalances and the small tumor problem requires integrated methodological approaches spanning loss function design, network architecture, and data curation. The protocols and frameworks presented here provide standardized approaches for developing robust segmentation systems capable of handling the full spectrum of brain tumor manifestations. As AI becomes increasingly integrated into neuro-oncology research and therapeutic development, resolving these fundamental challenges will be essential for both accurate biomarker quantification and reliable treatment response assessment in clinical trials.
Magnetic Resonance Imaging (MRI) serves as a cornerstone for brain tumor diagnosis, treatment planning, and research. The performance of automated tumor segmentation AI models is critically dependent on the quality and consistency of the input MRI data. This application note details three pervasive technical pitfalls in MRI acquisition—intensity heterogeneity, image artifacts, and protocol variability—within the context of AI-driven brain tumor segmentation research. We summarize quantitative impacts, provide standardized experimental protocols for mitigation, and outline essential computational tools to enhance research reproducibility and model robustness.
Table 1: Quantitative Impact of Technical Pitfalls on AI Segmentation Performance
| Pitfall Category | Specific Issue | Quantitative Metric | Reported Impact on Performance | Citation |
|---|---|---|---|---|
| Intensity Heterogeneity | Poor Contrast in Raw Images | Dice Score (DSC) | Baseline U-Net DSC: ~95.0% | [7] |
| Application of CLAHE & Filtering | Dice Score (DSC) | Post-preprocessing DSC: ~98.1% (ARU-Net) | [7] | |
| Protocol Variability | Missing MRI Sequences (e.g., T1ce) | Dice Similarity Coefficient (DSC) | Significant improvement when generating missing T1ce vs. copying other sequences | [23] |
| Cross-Center Data Inconsistency | Frechet Inception Distance (FID) | Baseline FID (inter-sequence variation): 542.21; With UMMGAT model: 258.21 | [23] | |
| Image Artifacts | Excessive Ghosting/Geometric Distortion | Qualitative Accreditation Scoring | Results in examination failure if artifacts compromise diagnostic value | [56] |
Table 2: The Researcher's Toolkit: Essential Software and Data Resources
| Research Reagent Solution | Type | Primary Function in Context | Application Example | |
|---|---|---|---|---|
| ARU-Net | Deep Learning Architecture | Segments tumors from MRI; robust to heterogeneity via attention mechanisms. | Brain tumor segmentation on BTMRII dataset, achieving 98.1% DSC. | [7] |
| UMMGAT (Unsupervised Multi-center Multi-sequence GAT) | Generative AI Model | Synthesizes missing MRI sequences and harmonizes cross-center data. | Completing missing T1ce or FLAIR sequences to maintain segmentation accuracy. | [23] |
| Spine Generic Protocol / SCT | Standardized QMRI Protocol & Toolbox | Provides reproducible quantitative metrics across sites and manufacturers. | Assessing macrostructural and microstructural integrity of the spinal cord. | [57] |
| PyRadiomics | Feature Extraction Library | Extracts hand-crafted radiomic features from images and subregions. | Quantifying intratumoral heterogeneity for predicting tumor grading in IMCC. | [58] |
| BTMRII / BraTS Datasets | Public MRI Datasets | Benchmarking and training segmentation models with multi-sequence data. | Training and validating ARU-Net and UMMGAT models. | [7] [23] |
Experimental Protocols
Protocol for Mitigating Intensity Heterogeneity via Pre-processing
Application: Enhancing image quality and contrast to improve deep learning segmentation accuracy.
Materials: T1, T1ce, T2, FLAIR MRI sequences in neuro-imaging formats (e.g., DICOM, NIfTI).
Methodology:
- Contrast Enhancement: Apply Contrast-Limited Adaptive Histogram Equalization (CLAHE) to improve local contrast without amplifying noise.
- Denoising: Utilize a denoising filter (e.g., Non-Local Means or Anisotropic Diffusion) to reduce noise while preserving edges.
- Edge-Preserving Smoothing: Apply a Linear Kuwahara filter to smooth homogeneous regions while maintaining critical tumor boundaries.
- Model Training: Implement an Attention Res-UNet (ARU-Net) or similar advanced architecture. The model should incorporate:
- Residual Connections to facilitate training of deep networks.
- Adaptive Channel Attention (ACA) modules in the encoder to refine feature extraction.
- Dimensional-space Triplet Attention (DTA) modules in the decoder to better fuse multi-scale features and capture spatial-channel dependencies.
Validation: Evaluate segmentation performance on a hold-out test set using Dice Similarity Coefficient (DSC), Intersection over Union (IoU), and visual assessment of tumor boundaries [7].
Protocol for Quantifying Intratumoral Heterogeneity via Habitat Imaging
Application: Predicting pathological tumor grading non-invasively by quantifying internal tumor variation.
Materials: Pre-operative T2-weighted and Diffusion-weighted (DWI) MRI scans.
Methodology:
- Image Pre-processing:
- Perform N4 bias field correction to correct for intensity inhomogeneity.
- Resample images to isotropic voxels (e.g., 1 mm³) using B-spline interpolation.
- Co-register DWI and T2WI sequences using affine and deformable transformations with mutual information.
- Tumor Segmentation: Manually delineate the 3D volume of interest (VOI) of the entire tumor on the DWI (b=800 s/mm²) images, verified by an experienced radiologist.
- Habitat Mapping: Apply the K-means clustering algorithm (optimal K determined by the elbow method) to the tumor VOI based on signal intensity from both T2WI and DWI. This typically yields two distinct subregions or "habitats" per sequence.
- Radiomic Feature Extraction: Use PyRadiomics or an equivalent tool to extract a comprehensive set of features (e.g., first-order statistics, texture) from the whole tumor and from each of the identified habitat subregions.
- Model Building: Construct a combined predictive model that integrates:
- Significant clinical and conventional imaging variables.
- Radiomic features from the whole tumor and habitats.
- An ITH index derived from the habitat model.
Validation: Assess the model's performance in predicting pathological grade using the Area Under the Receiver Operating Characteristic Curve (AUC) on internal and external validation cohorts [58].
Protocol for Managing Protocol Variability and Missing Sequences
Application: Maintaining robust AI segmentation performance when input MRI sequences are missing or from unseen clinical centers.
Materials: Incomplete or multi-institutional MRI datasets (e.g., from BraTS, UCSF-PDGM).
Methodology:
- Model Training: Develop an Unsupervised Multi-center Multi-sequence Generative Adversarial Transformer (UMMGAT). Key components include:
- A sequence encoder to disentangle and encode modality-specific characteristics from unpaired data.
- A lesion-aware module (LAM) to enhance the synthesis of tumor regions.
- Training via multi-task learning to enable flexible transformation between any sequences.
- Image Generation & Harmonization: For a case with a missing sequence, input an available sequence and the target sequence code into UMMGAT to generate the missing modality.
- Segmentation: Use the completed, harmonized multi-sequence data as input to a standard brain tumor segmentation model (e.g., a U-Net based architecture).
Validation: Compare the segmentation Dice scores against a baseline strategy of copying an available sequence to replace the missing one, across various missing-sequence scenarios and cross-center data [23].
Workflow Visualizations
Diagram 1: Pre-processing pipeline for intensity heterogeneity mitigation.
Diagram 2: Workflow for intratumoral heterogeneity analysis using habitat imaging.
Diagram 3: Pipeline for managing protocol variability and missing sequences.
The deployment of artificial intelligence (AI) models for automated brain tumor segmentation in clinical and research settings is significantly hampered by the challenge of generalization. Models trained on pristine, curated datasets often experience substantial performance degradation when confronted with real-world data characterized by variability in scanning protocols, hardware, and patient populations [8] [59]. This limitation obstructs reliable usage in critical applications such as treatment planning, outcome monitoring, and drug development trials. Consequently, developing robust strategies to enhance model generalization is paramount. This document outlines detailed application notes and protocols for three cornerstone methodologies—pre-processing, data augmentation, and domain adaptation—framed within the context of advanced brain tumor segmentation research. These protocols are designed to equip researchers and scientists with practical tools to build more robust, reliable, and clinically applicable AI models.
Pre-processing Strategies for Multi-Scanner MRI Data
Effective pre-processing is the foundational step for mitigating domain shift induced by technical variations in MRI data acquisition. It aims to standardize input data, thereby allowing the segmentation model to focus on biologically relevant features rather than scanner-specific artifacts.
Core Pre-processing Protocol
The following protocol, widely adopted in challenges like the BraTS 2025 Lighthouse, details the essential steps for preparing multi-institutional MRI data [54].
Protocol 2.1: Standardized Multi-Modal MRI Pre-processing
- Objective: To convert raw DICOM files from multiple sources into a co-registered, normalized, and skull-stripped dataset suitable for robust model training.
- Input: Multi-parametric MRI (mpMRI) volumes in DICOM format: native T1-weighted (T1), post-contrast T1-weighted (T1Gd), T2-weighted (T2), and T2-FLAIR (FLAIR).
- Output: Processed NIfTI files with dimensions 182x218x182 and 1 mm³ isotropic resolution.
- Procedure:
- DICOM to NIfTI Conversion: Convert manufacturer-specific DICOM files to the standardized NIfTI format using tools like
dcm2niix. - Co-registration: Rigidly align all mpMRI sequences (T1, T1Gd, T2) to the T1-weighted image to correct for inter-scan motion artifacts. The FLAIR volume is typically used as the reference for its clear pathology delineation. Recommended tool:
ANTsorFSL FLIRT. - Skull Stripping: Remove non-brain tissue to isolate the region of interest. Use a consensus approach from tools like
HD-BETorROBEXfor high accuracy. - Resampling: Isotropically resample all volumes to a uniform resolution of 1 mm³ to ensure consistent spatial representation across the dataset.
- Intensity Normalization: Apply techniques like Z-score normalization or White Stripe to correct for global intensity variations between scanners. For challenging, low-field MRI data, more aggressive normalization may be required [54].
- DICOM to NIfTI Conversion: Convert manufacturer-specific DICOM files to the standardized NIfTI format using tools like
Table 1: Quantitative Impact of Key Pre-processing Steps on Segmentation Performance (Dice Score)
| Pre-processing Step | Dice Score (HGG) | Dice Score (LGG) | Key Benefit |
|---|---|---|---|
| No Pre-processing | 0.72 | 0.65 | Baseline |
| Co-registration Only | 0.79 | 0.71 | Reduces misalignment artifacts |
| + Skull Stripping & Resampling | 0.84 | 0.78 | Standardizes input geometry |
| + Full Pipeline (Intensity Norm) | 0.89 | 0.83 | Mitigates scanner-induced intensity shift |
Workflow Diagram: Standardized MRI Pre-processing Pipeline
The following diagram illustrates the logical sequence of the pre-processing protocol, ensuring data consistency before model training.
Data Augmentation for Addressing Class Imbalance and Data Scarcity
Data augmentation expands the diversity and size of training datasets, which is crucial for preventing overfitting and improving model robustness, especially for underrepresented tumor subregions.
Conventional and Advanced Augmentation Techniques
Beyond simple spatial and photometric transformations, advanced generative techniques are now state-of-the-art for addressing severe class imbalance.
Protocol 3.1: On-the-Fly Data Augmentation with Generative Models
- Objective: To dynamically insert realistic, synthetic tumors into healthy brain regions during training, thereby increasing the model's exposure to rare tumor phenotypes and improving its robustness [60].
- Input: Batch of pre-processed MRI patches and corresponding label masks from the training set.
- Materials:
- Pre-trained Generative Adversarial Network (GAN), such as GliGAN [60].
- Framework:
nnU-Netwith integrated custom augmentation pipeline.
- Procedure:
- Load Pre-trained GAN: Integrate publicly released pre-trained weights of a tumor generation GAN (e.g., GliGAN) into the training loop.
- Dynamic Tumor Insertion: For each training batch, with a predefined probability (e.g., p=0.5), select a random healthy subject and a tumor label mask from another subject.
- Label Mask Modification (Optional): To specifically address class imbalance (e.g., lack of Enhancing Tumor (ET)), modify the input label mask by randomly replacing common classes (e.g., edema) with rare classes (e.g., ET) with a defined probability (e.g., 0.7) [60].
- Scale Modification: To improve the detection of small lesions, apply a random scale factor (e.g., 0.3-0.7) to the label mask before insertion, creating smaller synthetic tumors.
- Generate and Insert: The GAN generator takes the modified label mask and a healthy MRI volume and outputs a synthetic MRI volume with a realistically embedded tumor. This volume is then used for training.
Table 2: Comparison of Data Augmentation Techniques for Brain Tumor Segmentation
| Augmentation Technique | Methodology | Reported Dice Gain | Primary Use Case |
|---|---|---|---|
| Spatial (Geometric) | Rotation, flipping, elastic deformation | +0.03-0.05 | General robustness, prevents overfitting |
| Photometric | Adjusting brightness, contrast, adding noise | +0.02-0.04 | Simulating scanner variations |
| Generative (GAN-based) | GliGAN-based synthetic tumor insertion [60] | +0.05-0.10 (on small lesions) | Addressing severe class imbalance |
| Diffusion Models | Multi-Channel Fusion Diffusion (MCFDiffusion) [61] | +0.015-0.025 (overall Dice) | High-quality data generation from healthy scans |
Workflow Diagram: On-the-Fly Augmentation with GliGAN
This diagram visualizes the dynamic process of generating and using synthetic tumor data during model training.
Domain Adaptation for Cross-Domain Generalization
Domain adaptation techniques enable models trained on a source domain (e.g., high-quality research datasets) to perform well on a different but related target domain (e.g., data from a new hospital or low-resource setting), without requiring labeled data in the target domain.
Source-Free Unsupervised Domain Adaptation (SFUDA) Protocol
Given clinical data privacy constraints, Source-Free Unsupervised Domain Adaptation (SFUDA), where the source data is inaccessible during adaptation, is a highly relevant paradigm.
Protocol 4.1: SmaRT Framework for SFUDA
- Objective: To adapt a pre-trained brain tumor segmentation model to an unlabeled target domain (e.g., low-field MRI, pediatric scans) without access to the original source data, thereby improving performance under domain shift [59].
- Input:
- A model (e.g., 3D U-Net) pre-trained on a source domain (e.g., BraTS).
- Unlabeled data from the target domain.
- Materials:
SmaRTframework components: Style Encoder, EMA Branch, Adaptive Branch [59]. - Procedure:
- Initialization: Initialize both the EMA (teacher) and Adaptive (student) branches with weights from the model pre-trained on the source domain.
- Style-Aware Augmentation: For each target domain batch, apply a dynamic composite augmentation strategy (e.g., posterize, adjust contrast, add noise) to create multiple views of the same input. A style encoder learns to produce modulation vectors from these augmentations.
- Dual-Branch Momentum Update:
- The EMA Branch generates stable pseudo-labels from the weakly-augmented view and updates its weights via an exponential moving average (EMA) of the Adaptive Branch's weights.
- The Adaptive Branch learns from the strongly-augmented views. Its decoder is modulated using the style vectors to adapt to target domain appearances.
- Structural Priors Enforcement: The Adaptive Branch is trained using a multi-head loss function that enforces:
- Consistency (CsH): Between predictions on different augmented views.
- Integrity (IH): To restore complete tumor regions and suppress false negatives.
- Connectivity (CnH): To reduce spurious, fragmented predictions.
- Iteration: Repeat steps 2-4 for multiple epochs over the target domain data until convergence.
Table 3: Performance of SmaRT on Cross-Domain Brain Tumor Segmentation
| Target Domain | Baseline (No Adapt.) | With SmaRT Adaptation | Key Metric |
|---|---|---|---|
| Sub-Saharan Africa (Low-Field MRI) | 0.61 | 0.74 | Dice Score (Whole Tumor) |
| Pediatric Glioma | 0.65 | 0.78 | Dice Score (Whole Tumor) |
| Sub-Saharan Africa (Low-Field MRI) | 12.5 mm | 8.2 mm | HD95 (Boundary Error) |
Workflow Diagram: SmaRT Domain Adaptation Framework
The following diagram outlines the architecture and data flow of the SmaRT test-time adaptation framework.
The Scientist's Toolkit: Essential Research Reagents and Materials
This section catalogs key computational tools, datasets, and frameworks essential for implementing the protocols described in this document.
Table 4: Essential Research Reagents and Solutions for AI-based Brain Tumor Segmentation
| Item Name | Type | Function/Application | Example/Reference |
|---|---|---|---|
| BraTS Dataset | Dataset | Provides standardized, multi-institutional mpMRI data with expert annotations for training and benchmarking. | BraTS 2025 [60] [54] |
| nnU-Net | Framework | Self-configuring deep learning framework for medical image segmentation; a robust baseline and competition-winning tool. | [60] |
| GliGAN | Pre-trained Model | Generative Adversarial Network for synthesizing realistic brain tumors; used for advanced data augmentation. | [60] |
| MCFDiffusion | Pre-trained Model | Multi-Channel Fusion Diffusion Model for generating high-quality tumor images from healthy scans for data augmentation. | [61] |
| SmaRT Framework | Algorithm | Source-free test-time adaptation framework for robust segmentation under domain shift (e.g., low-field MRI). | [59] |
| ANTs / FSL | Software Toolkit | Libraries for advanced medical image pre-processing, including co-registration and normalization. | [54] |
| HD-BET | Algorithm | State-of-the-art tool for robust and fast skull-stripping of brain MRI data. | [54] |
The Role of Uncertainty Estimation in Identifying Segmentation Failures
In the development of automated artificial intelligence (AI) models for brain tumor segmentation from Magnetic Resonance Imaging (MRI), the accurate identification of segmentation failures is as crucial as achieving high overall performance. These models, often based on sophisticated deep learning architectures like U-Net, have become central to neuro-oncology research and drug development, enabling quantitative analysis of tumor burden for diagnostic and therapeutic assessments [9] [8]. However, their clinical adoption remains hampered by a critical challenge: the inability to reliably flag cases where the model's segmentation may be erroneous [62]. Uncertainty estimation has emerged as a promising methodological approach to address this limitation, providing a quantifiable measure of a model's confidence in its own predictions [63]. This application note explores the current state of uncertainty estimation in brain tumor segmentation, evaluates its efficacy through empirical data, and provides detailed protocols for its implementation, framed within the broader context of developing clinically trustworthy AI systems for neuro-oncology.
The Critical Need for Failure Identification in Automated Segmentation
Automated brain tumor segmentation using AI has demonstrated remarkable capabilities in delineating tumor subregions across multiple MRI sequences, facilitating objective and reproducible measurements essential for diagnosis, treatment planning, and disease monitoring [9]. Convolutional Neural Networks (CNNs), particularly U-Net-based architectures, have set benchmark performance levels on curated datasets like the Brain Tumor Segmentation (BraTS) challenges [9] [29]. Nevertheless, these models remain susceptible to failures in real-world clinical scenarios due to several factors:
- Data Inconsistencies: Clinical MRI data often suffer from missing sequences, cross-center acquisition parameter variations, and artifacts, which can degrade model performance unpredictably [23].
- Tumor Heterogeneity: The substantial spatial and structural variability among brain tumors, especially diffusely infiltrating gliomas, presents significant challenges [29].
- Algorithmic Limitations: Models trained on specific data distributions may underperform on out-of-distribution samples, with failures often occurring near tumor boundaries where anatomical ambiguity is highest [63].
Without reliable failure identification mechanisms, erroneous segmentations could propagate through the research and clinical pipeline, compromising treatment efficacy assessments in clinical trials and potentially misleading therapeutic decisions. Uncertainty estimation aims to provide this safety mechanism by quantifying the model's confidence at the voxel or regional level.
Quantitative Analysis of Uncertainty-Error Correlation
Recent empirical investigations have critically evaluated the relationship between estimated uncertainty and actual segmentation error, yielding crucial insights for researchers.
Table 1: Correlation Between MC Dropout Uncertainty and Segmentation Error
| Evaluation Context | Correlation Type | Correlation Coefficient | Statistical Significance | Practical Relevance | ||
|---|---|---|---|---|---|---|
| Global Image Analysis | Pearson | 0.30 - 0.38 | p < 0.001 | Weak | ||
| Tumor Boundary Regions | Pearson | r | < 0.05 | Not Significant | Negligible | |
| With Data Augmentation | Spearman | Variation observed | p < 0.001 | Limited |
A 2025 empirical study specifically examined Monte Carlo (MC) Dropout, a widely adopted uncertainty estimation technique, in 2D brain tumor segmentation using a U-Net architecture [63]. The study computed uncertainty through 50 stochastic forward passes and correlated it with pixel-wise segmentation errors using both Pearson and Spearman coefficients across different data augmentation strategies (none, horizontal flip, rotation, and scaling). The key findings revealed:
- Weak Global Correlation: The overall correlation between MC Dropout uncertainty and segmentation error remained weak (r ≈ 0.30-0.38), despite statistical significance [63].
- Negligible Boundary Correlation: At tumor boundaries, where segmentation errors are most clinically consequential, correlation was effectively absent (|r| < 0.05) [63].
- Limited Impact of Augmentation: While different data augmentation strategies produced statistically significant differences in uncertainty-error correlation (p < 0.001), these differences lacked practical relevance for clinical deployment [63].
These findings suggest that while MC Dropout provides some general signal regarding potential error regions, it has limited effectiveness in precisely localizing boundary errors, underscoring the need for more sophisticated or hybrid approaches.
Experimental Protocols for Uncertainty Estimation
Protocol 1: Implementing MC Dropout for Uncertainty Quantification
This protocol details the methodology for employing MC Dropout to estimate uncertainty in brain tumor segmentation models, based on established experimental procedures [63].
Research Reagent Solutions:
- Model Architecture: 2D or 3D U-Net with dropout layers inserted after convolutional blocks.
- Dataset: BraTS datasets (2018, 2021) with multi-sequential MRI (T1, T1c, T2, FLAIR) and expert annotations.
- Software Framework: Python with PyTorch or TensorFlow, including specialized libraries (e.g., TorchIO for medical image processing).
- Computational Environment: GPU-enabled system (e.g., NVIDIA Tesla V100 or equivalent) with sufficient VRAM for 3D volumetric data.
Procedure:
- Model Modification: Integrate dropout layers with a rate of 0.5 in the convolutional encoder and decoder sections of a standard U-Net architecture. Maintain these layers in an active state during both training and inference phases.
- Stochastic Forward Passes: During inference, perform multiple (typically 50) forward passes for each input volume. Each pass will generate a slightly different segmentation probability map due to the randomized dropout.
- Uncertainty Map Generation: Calculate the voxel-wise uncertainty map using entropy or variance across the multiple forward passes:
- Entropy-based uncertainty: H = -Σ(pc * log(pc)) across classes C
- Variance-based uncertainty: σ² = variance(p_tumor) across T stochastic samples
- Error Correlation Analysis: Compare the generated uncertainty maps with ground truth segmentation errors using correlation coefficients (Pearson, Spearman) to quantify the relationship between estimated uncertainty and actual segmentation accuracy.
Protocol 2: Evaluating Segmentation Performance Under Missing Data
This protocol addresses uncertainty estimation in clinically challenging scenarios with incomplete MRI sequences, using generative approaches for data completion [23].
Research Reagent Solutions:
- Generative Model: Unsupervised Multi-center Multi-sequence Generative Adversarial Transformer (UMMGAT) with Lesion-Aware Module (LAM).
- Segmentation Model: 3D U-Net trained on complete multi-sequence data.
- Evaluation Metrics: Dice Similarity Coefficient (DSC), Hausdorff Distance (HD), Sensitivity, Specificity.
Procedure:
- Data Simulation: Simulate various missing sequence scenarios (single and multiple sequence absences) from complete multi-sequence MRI datasets (BraTS 2019, BraTS2023-MEN).
- Sequence Generation: Employ UMMGAT to generate missing sequences from available sequences using its disentangled sequence encoder and lesion-aware module.
- Uncertainty-aware Segmentation:
- Execute segmentation using both generated sequences and simple copying of available sequences.
- Quantify segmentation performance with and without generated sequences.
- Correlate performance reduction with uncertainty metrics derived from the generative model's confidence scores.
- Cross-center Validation: Evaluate the pipeline on external datasets (e.g., UCSF-PDGM) to assess generalizability and uncertainty calibration across institutional boundaries.
Uncertainty Estimation with Data Completion Workflow
The Scientist's Toolkit: Essential Research Reagents
Table 2: Key Research Reagent Solutions for Uncertainty Estimation Studies
| Reagent Category | Specific Examples | Function/Application | Implementation Notes |
|---|---|---|---|
| Model Architectures | 3D U-Net with dropout, Vision Transformers (ViT) | Base segmentation network with uncertainty modules | U-Net preferred for smaller datasets; ViT requires substantial data [29] |
| Uncertainty Methods | MC Dropout, Ensemble Methods, Bayesian Neural Networks | Quantify model confidence at voxel and structure levels | MC Dropout computationally efficient but limited boundary correlation [63] |
| Generative Models | UMMGAT (with LAM), GANs | Complete missing sequences for consistent segmentation | UMMGAT trains on unpaired data, crucial for clinical realism [23] |
| Benchmark Datasets | BraTS 2018-2023, UCSF-PDGM, Local Institutional Data | Train, validate, and test segmentation uncertainty | Multi-center data essential for assessing generalizability [9] [23] |
| Evaluation Metrics | Dice Score, Hausdorff Distance, Uncertainty-Error Correlation | Quantify segmentation accuracy and uncertainty reliability | Correlation coefficients reveal uncertainty efficacy [63] |
Discussion and Future Directions
The empirical evidence indicating weak correlation between MC Dropout uncertainty and segmentation error, particularly at critical tumor boundaries, highlights substantial limitations in current failure identification methodologies [63]. This performance gap necessitates concerted efforts toward developing more robust uncertainty quantification frameworks for brain tumor segmentation research. Promising directions include:
- Hybrid Uncertainty Models: Combining multiple uncertainty approaches (e.g., ensemble methods with Bayesian neural networks) to capture different aspects of model confidence and improve error localization.
- Sequence Generation Integration: Leveraging advanced generative models like UMMGAT to handle missing data scenarios while propagating uncertainty estimates from the generation process through to segmentation [23].
- Boundary-Focused Uncertainty: Developing specialized uncertainty estimation techniques that explicitly target the challenging tumor boundary regions where current methods show negligible correlation with errors.
- Clinical Workflow Integration: Designing uncertainty visualization tools that effectively communicate segmentation confidence to radiologists and researchers, enabling efficient human-in-the-loop validation.
As AI-based segmentation becomes increasingly embedded in neuro-oncology research and drug development pipelines, advancing the reliability of failure identification through sophisticated uncertainty estimation will be paramount for building trustworthy automated analysis systems.
The accurate segmentation of multiple small brain metastases (BMs) on MRI is a critical task in neuro-oncology, directly influencing patient management, treatment planning, and therapy response assessment [64]. While the Dice Similarity Coefficient (DSC) has become the standard metric for evaluating medical image segmentation performance, it possesses significant limitations when applied to the challenging context of small, multiple metastases [65]. The clinical imperative for improved evaluation frameworks stems from the fact that detecting even subcentimeter lesions is crucial for determining appropriate treatment strategies, particularly for stereotactic radiosurgery (SRS) [64].
The fundamental challenge lies in the unique characteristics of brain metastases compared to other brain tumors. BMs are often substantially smaller than gliomas and frequently present at multiple sites simultaneously [64]. Research has consistently demonstrated that segmentation performance correlates strongly with lesion size, with one study reporting DSC scores as low as 0.31 for lesions smaller than 3mm compared to 0.87 for those 6mm or larger [65]. This performance discrepancy highlights the inadequacy of relying solely on DSC for comprehensive algorithm assessment, as it may mask critical failures in small lesion detection and segmentation that have direct clinical implications.
This Application Note addresses the pressing need for expanded evaluation metrics beyond DSC, focusing specifically on the challenges of multiple small metastases segmentation. We present a standardized framework for comprehensive algorithm assessment, detailed experimental protocols for rigorous validation, and essential research tools to advance the field toward clinically reliable segmentation systems.
Quantitative Analysis of Current Segmentation Performance
Table 1: Performance Metrics for Brain Metastasis Segmentation Across Studies
| Study | Primary Metric | Performance by Lesion Size | Detection Sensitivity | False Positives per Patient | Segmentation Task |
|---|---|---|---|---|---|
| Zhou et al. [65] | Dice Similarity Coefficient (DSC) | 0.31 (<3mm), 0.87 (≥6mm) | Not specified | Not specified | Single-label segmentation |
| Dikici et al. [65] | Sensitivity | Large performance drop for <10mm³ | Not specified | Not specified | Small lesion detection |
| Bousabarah et al. [65] | Sensitivity | Trained exclusively on small lesions | Not specified | Not specified | Small lesion detection |
| Grøvik et al. [64] | Sensitivity | 82.4% (<3mm), 93.2% (3-10mm), 100% (≥10mm) | 93.1% overall | 0.59 | Detection and segmentation |
| AURORA Study [66] | DSC | No correlation between volume and DSC | F1-Score: 0.93 ± 0.16 | Not specified | Gross tumor volume segmentation |
Table 2: Limitations of Dice Similarity Coefficient for Small Metastases Evaluation
| Limitation Category | Specific Challenge | Impact on Small Metastases Assessment |
|---|---|---|
| Size Sensitivity | DSC penalizes minor boundary errors more severely for small objects | Small lesions inherently receive lower scores even with clinically acceptable segmentations |
| Spatial Consideration | Does not account for distance between boundaries | Fails to distinguish between adjacent misses and distant misses |
| Detection vs. Segmentation | Does not evaluate lesion detection capability | A completely missed lesion and perfect segmentation both yield DSC=0 |
| Clinical Relevance | Poor correlation with clinical impact | Small DSC differences may not reflect meaningful clinical consequences |
| Multiple Lesion Context | Treats each lesion independently | Does not capture performance on lesion counts critical for treatment decisions |
Current literature reveals significant performance disparities in small metastasis segmentation. The AURORA multicenter study demonstrated that a well-designed 3D U-Net could achieve a mean DSC of 0.89±0.11 for individual metastasis segmentation and an F1-Score of 0.93±0.16 for detection [66]. Importantly, this study found no correlation between metastasis volume and DSC, suggesting proper optimization for small targets [66]. However, other studies highlight persistent challenges, with one reporting sensitivity as low as 15% for detecting metastases smaller than 3mm [64]. The integration of specialized imaging sequences like black-blood MRI has shown promise, improving sensitivity for sub-3mm metastases to 82.4% while maintaining low false-positive rates (0.59 per patient) [64].
Comprehensive Evaluation Metrics Framework
Expanded Metric Taxonomy
A robust evaluation framework for multiple small metastases must extend beyond volumetric overlap measures to capture detection capability, spatial accuracy, and clinical utility:
- Detection-focused Metrics: Lesion-wise sensitivity and specificity, false positive rate per patient, F1-score for detection, and free-response receiver operating characteristic (FROC) analysis.
- Spatial Accuracy Measures: Hausdorff distance (including HD95 variant), average surface distance, and boundary F1-score to evaluate segmentation boundaries specifically.
- Size-based Stratification: All metrics should be calculated across predefined size ranges (<3mm, 3-5mm, 5-10mm, >10mm) to ensure performance transparency across the size spectrum.
- Multi-component Metrics: For models segmenting enhancing tissue, edema, and necrosis, component-specific metrics are essential [65].
Clinical Utility Assessment
Metrics should ultimately connect to clinical impact through:
- Treatment Planning Simulation: Measure segmentation accuracy in regions critical for SRS planning.
- Response Assessment Compatibility: Evaluate how segmentation errors propagate into RANO-BM criteria classification [67].
- Longitudinal Tracking Reliability: Assess performance on lesion matching across timepoints, crucial for monitoring treatment response [65].
Experimental Protocols for Validation
Protocol 1: Multi-scale Segmentation Performance
Objective: Systematically evaluate segmentation performance across varying lesion sizes and locations.
Materials:
- Multi-institutional MRI datasets with expert-annotated BM segmentations
- Predefined size categories: <3mm, 3-5mm, 5-10mm, >10mm
- Computational environment with appropriate deep learning frameworks
Methodology:
- Data Preparation:
- Curate datasets with balanced representation across size categories
- Apply standardized preprocessing: N4 bias field correction, intensity normalization, and spatial registration to a common template
- Implement data augmentation: random rotations, scaling, intensity variations, and elastic deformations
Model Training:
- Utilize nnUNet framework for its demonstrated performance in medical segmentation tasks
- Implement dedicated small lesion detection through patch-based training strategies
- Optimize loss functions: combined Dice and cross-entropy loss with size-based weighting
Evaluation:
- Calculate comprehensive metrics stratified by size categories
- Perform statistical analysis using one-tailed t-tests to compare performance across size ranges
- Generate FROC curves to characterize detection sensitivity versus false positive rate
Protocol 2: Longitudinal Segmentation Stability
Objective: Validate segmentation performance across longitudinal scans and assess stability for treatment response monitoring.
Materials:
- Paired baseline and follow-up MRI scans with annotated metastases
- Deformable registration pipelines (e.g., ANTs, Elastix)
- Computing infrastructure for processing temporal data
Methodology:
- Temporal Registration:
- Apply affine followed by deformable registration using ANTs toolbox to align follow-up to baseline images [65]
- Propagate baseline annotations through registration for initial follow-up segmentations
- Manually correct propagated masks to establish ground truth
Re-segmentation Model:
- Implement architecture accepting both current image and prior lesion locations as input
- Train with temporal consistency regularization to ensure stable segmentations
- Incorporate attention mechanisms to focus on regions with potential new lesions
Longitudinal Evaluation:
- Measure segmentation consistency for persistent lesions across timepoints
- Assess detection performance for new appearing lesions
- Evaluate registration robustness in cases of significant anatomical changes
Table 3: Research Reagent Solutions for Metastases Segmentation
| Reagent Category | Specific Tool/Solution | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Data Annotation | ITK-SNAP [65] | Manual delineation of metastases with multi-label support | Requires training with senior neuroradiologists; annotations should be verified by experts |
| Public Datasets | BraTS-METS [9] | Standardized benchmark for metastases segmentation | Provides multi-class labels (enhancing tumor, necrosis, edema) |
| Federated Learning | FeTS Platform [68] | Privacy-preserving multi-institutional model training | Enables collaboration without data sharing; uses OpenFL framework |
| Preprocessing | ANTs Registration [65] | Spatial normalization and longitudinal registration | Affine + deformable transformation for optimal alignment |
| Model Architecture | nnUNet [68] | Adaptive framework for medical image segmentation | Automatically configures architecture and preprocessing |
| Evaluation Metrics | MedPy Library | Comprehensive metric calculation | Should be extended with custom small lesion evaluations |
Essential Research Toolkit
Data Curation and Annotation Standards
High-quality data curation is fundamental for developing robust evaluation metrics:
- Multi-institutional Collaboration: Leverage federated learning approaches like FeTS to access diverse datasets while preserving patient privacy [68]. The FeTS initiative demonstrated the value of multi-institutional collaboration, achieving DSC scores up to 0.95 for certain tumor subregions.
- Annotation Protocols: Establish standardized annotation guidelines specifying:
- Minimum lesion size for inclusion (e.g., ≥2mm diameter)
- Multi-component labeling: enhancing lesion, edema, necrosis [65]
- Handling of ambiguous boundaries and lesion confluence
- Expert Verification: Implement multi-reader verification with senior neuroradiologists (≥14 years experience) to ensure annotation quality [65].
Computational Modeling Infrastructure
- Architecture Selection: Build upon proven architectures like 3D U-Net [66] and nnUNet [68] with modifications for small lesion detection.
- Small Lesion Optimization: Implement specialized strategies for small targets:
- Higher resolution processing for small lesion detection
- Class-balanced loss functions addressing extreme foreground-background imbalance
- Attention mechanisms to focus computational resources on suspicious regions
- Longitudinal Processing: Develop re-segmentation models that leverage prior timepoint information to improve segmentation consistency and new lesion detection [65].
Visualization Framework
Moving beyond Dice similarity coefficient is essential for advancing the field of automated brain metastasis segmentation, particularly for the challenging case of multiple small metastases. The framework presented in this Application Note provides researchers with comprehensive evaluation methodologies, standardized experimental protocols, and essential research tools to develop more clinically relevant segmentation systems. By adopting these more rigorous assessment standards, the field can accelerate progress toward AI systems that reliably support clinical decision-making in neuro-oncology, ultimately improving patient care through more precise detection, segmentation, and monitoring of brain metastases. Future work should focus on validating these approaches across larger multi-institutional cohorts and establishing clear clinical correlation between technical metrics and patient outcomes.
Benchmarking Performance: Validation Frameworks and Comparative Analysis of AI Tools
Automated segmentation of brain tumors from magnetic resonance imaging (MRI) is a cornerstone of modern computational neuro-oncology, vital for precise diagnosis, treatment planning, and monitoring disease progression [8] [69]. The transition from manual delineation, a time-consuming and expert-dependent process, to automated artificial intelligence (AI) methods represents a significant paradigm shift in medical image analysis [8] [29]. This shift has been largely catalyzed by the establishment of standardized benchmarks, which are crucial for the objective comparison of algorithmic performance, the stimulation of methodological innovation, and the building of clinical trust in AI tools. Among these, the Brain Tumor Segmentation (BraTS) dataset and the associated challenges organized under the Medical Image Computing and Computer Assisted Intervention (MICCAI) society have emerged as the preeminent global benchmarking resources [69] [70]. This article explores the pivotal role of the BraTS ecosystem, detailing its evolution, structure, and profound impact on driving the field of automated brain tumor segmentation forward for a audience of researchers, scientists, and drug development professionals.
The BraTS Challenge: Evolution and Clinical Imperative
Initiated in 2012, the BraTS challenge was conceived to address a critical lack of standardization in the validation of brain tumor segmentation algorithms [69]. Prior to its establishment, researchers relied on small, private datasets with varying evaluation metrics, making objective comparisons between methods nearly impossible [69]. The BraTS challenge provided a community-wide platform by introducing a large, multi-institutional dataset with expert-annotated ground truth and a standardized evaluation framework.
The clinical necessity underpinning BraTS is profound. Gliomas, the most common primary malignant brain tumors in adults, are characterized by significant genetic diversity and intrinsic heterogeneity in appearance, shape, and histology [71]. Treatments typically involve a multi-modal approach including surgery, radiation, and systemic therapies, with MRI serving as the gold standard for pre- and post-treatment assessment [71]. Accurate volumetric segmentation of tumor sub-regions is essential for objective assessment of tumor response as outlined in criteria like RANO (Response Assessment in Neuro-Oncology) [5]. However, manual segmentation is tedious and exhibits high inter-rater variability, creating a pressing need for automated, reliable algorithms [5] [69]. The BraTS challenges aim to fulfill this need by benchmarking state-of-the-art AI models, with the ultimate goal of integrating them into clinical practice to enhance patient care [71].
Table 1: Evolution of the BraTS Challenge Focus Areas
| Challenge Era | Primary Focus | Key Annotated Tumor Sub-Regions | Clinical Application Context |
|---|---|---|---|
| Early (2012-2013) [69] | Pre-treatment Glioma Segmentation | Enhancing Tumor, Peritumoral Edema, Necrotic Core | Pre-operative planning and diagnosis |
| 2024 Challenge [71] | Post-treatment Glioma Segmentation | Enhancing Tissue, Non-enhancing T2/FLAIR Hyperintensity, Non-enhancing Tumor Core, Resection Cavity | Post-operative monitoring and treatment response assessment |
| 2025 Lighthouse Challenge [72] [70] | Multi-Tumor, Multi-Task Cluster | Varies by task (e.g., metastases, meningioma, pediatric tumors) | Comprehensive clinical workflow, from diagnosis to treatment response prediction |
As illustrated in Table 1, the scope of BraTS has dramatically expanded. The 2024 challenge specifically addressed the complex task of segmenting post-treatment gliomas, introducing the resection cavity (RC) as a new sub-region to segment, which is critical for reliably assessing residual tumor volume amid treatment-related changes like blood products and post-radiation inflammation [71]. The 2025 Lighthouse Challenge represents a further evolution into a "cluster of challenges," encompassing 12 distinct tasks. This includes segmentation for various tumor entities (glioma, metastases, meningioma, pediatric tumors), across the disease course (pre- and post-treatment), and even extending into domains like histopathology and computational tasks such as image synthesis [70]. This expansion is conducted in partnership with authoritative clinical organizations like the AI for Response Assessment in Neuro-Oncology (AI-RANO) group, RSNA, ASNR, and the FDA, ensuring the benchmarks address genuine clinical needs [70].
BraTS Data Ecosystem: Specifications and Annotations
The BraTS dataset is distinguished by its large scale, multi-institutional origin, and meticulously curated ground truth annotations.
Data Curation and Preprocessing
The datasets are retrospective collections of multi-parametric MRI (mpMRI) scans from numerous academic medical centers worldwide. For instance, the BraTS 2024 post-treatment glioma dataset alone comprises approximately 2,200 cases from seven contributing sites [71]. All scans undergo a standardized pre-processing pipeline to ensure consistency and remove protected health information (PHI). This pipeline includes:
- Conversion from DICOM to the NIfTI file format [71] [5].
- Co-registration to a common anatomical template (SRI24) [5].
- Resampling to a uniform isotropic resolution of 1 mm³ [5].
- Skull-stripping to remove non-brain tissue, which also mitigates potential facial reconstruction risks [5].
MRI Sequences and Tumor Sub-regions
A key strength of BraTS is its reliance on multi-parametric MRI, which provides complementary biological information. The core MRI sequences included are:
- Native T1-weighted (T1)
- Post-contrast T1-weighted (T1-Gd)
- T2-weighted (T2)
- T2 Fluid Attenuated Inversion Recovery (T2-FLAIR)
The annotation of tumor sub-regions has become increasingly sophisticated. The foundational regions include the Gd-enhancing tumor (ET), the peritumoral edematous/infiltrated tissue (ED), and the necrotic tumor core (NCR) [5]. The post-treatment challenges have introduced more refined labels such as Surrounding Non-enhancing FLAIR Hyperintensity (SNFH) and the Resection Cavity (RC) [71]. These annotations are initially generated by a fusion of top-performing algorithms from prior challenges (e.g., nnU-Net, DeepScan) and then undergo a rigorous process of manual refinement and final approval by board-certified neuro-radiologists with extensive expertise [71] [5]. For the 2025 challenge, a subset of test cases will be independently annotated by multiple raters to enable a direct comparison of algorithmic performance against human expert inter-rater variability [72] [70].
Experimental Protocols and Benchmarking Methodology
The BraTS challenges provide a rigorous framework for developing and evaluating segmentation models, encompassing data access, model training, and standardized evaluation.
Model Development and Training
Participants are given access to training datasets that include the four mpMRI sequences and their corresponding ground truth segmentation labels. The community has largely converged on deep learning-based approaches, with Convolutional Neural Networks (CNNs) and U-Net-based architectures being particularly dominant due to their performance [8] [29]. A common experimental protocol involves:
- Data Splitting: Using the provided training data for model development and hyperparameter tuning, often via cross-validation [29].
- Algorithm Selection: Implementing models such as 3D U-Net, which is a standard for volumetric medical image segmentation [29]. Recent innovations include hybrid models like ResSAXU-Net, which integrates deep residual networks (ResNet) to capture finer details and squeeze-excitation networks (SENet) to focus on locally relevant features, thereby improving the segmentation of small tumors [73].
- Loss Function: Addressing class imbalance between tumor and healthy tissue is critical. A combination of Dice loss and cross-entropy loss is frequently employed to tackle this issue and aid network convergence [73].
Benchmarking and Evaluation Metrics
The ultimate test for participant algorithms is performed on hidden validation and test sets where the ground truth is not disclosed. Performance is ranked using a standardized set of metrics that capture both volumetric overlap and boundary accuracy [71] [5]:
- Dice Similarity Coefficient (DSC): Measures the volumetric overlap between the automated segmentation and the ground truth. It is the primary metric for overall performance.
- Hausdorff Distance (HD): Assesses the largest segmentation boundary error, providing insight into the worst-case performance.
The following workflow diagram illustrates the typical participant journey and the challenge's evaluation structure:
Diagram Title: BraTS Challenge Participant Workflow
Impact on AI Research and Clinical Translation
The BraTS benchmark has been instrumental in catalyzing progress within the AI research community and paving the path for clinical adoption.
Driving Algorithmic Innovation
The public availability of the BraTS dataset and the competitive nature of the challenges have accelerated methodological advancements. Research has evolved from traditional machine learning and generative models to sophisticated deep learning architectures [8] [69]. The benchmark has enabled the systematic comparison of hundreds of algorithms, revealing that while different algorithms may excel at segmenting specific sub-regions, fused approaches often yield the most robust results [69]. Furthermore, BraTS has facilitated research into practical challenges, such as segmentation with missing MRI sequences. Studies have shown that models can achieve high accuracy with a reduced set of sequences (e.g., T1C + FLAIR), which could enhance generalizability and deployment in resource-constrained clinical settings [29]. Complementary challenges like BraSyn (Brain MR Image Synthesis) directly benchmark algorithms that can synthesize missing modalities, further supporting clinical applicability [5].
The Path to Clinical Integration
The design of BraTS is increasingly focused on overcoming barriers to clinical translation. The inclusion of post-treatment MRI and diverse tumor types ensures models are tested on realistic clinical scenarios beyond the pre-treatment gliomas that dominated early research [71]. The partnership with regulatory bodies like the FDA and clinical societies helps align the benchmarks with the requirements for clinical validation and approval [70]. Several AI-based tools for brain MRI analysis have already received FDA approval, demonstrating the ongoing transition of this technology from research to clinical practice [8]. The ultimate goal is for algorithms benchmarked in BraTS to serve as objective tools for assessing tumor volume, distinguishing treatment changes from recurrent tumor, and predicting patient outcomes, thereby integrating into clinical workflows to augment decision-making [71].
Table 2: Key Research Reagents and Materials in BraTS-based Research
| Resource / Material | Function in Experimental Protocol | Relevance to BraTS Benchmarking |
|---|---|---|
| Multi-parametric MRI Data (T1, T1-Gd, T2, FLAIR) [71] [29] | Provides multi-contrast anatomical information for model input; the fundamental data source. | Standardized, pre-processed core dataset provided to all participants. |
| Expert-Annotated Ground Truth [72] [5] | Serves as the reference standard for training supervised models and evaluating segmentation accuracy. | High-quality, multi-rater labels curated by neuroradiologists; the benchmark's gold standard. |
| U-Net Architectures (e.g., 3D U-Net, nnU-Net) [5] [29] | Core deep learning model backbone for volumetric segmentation; known for efficiency and performance. | A dominant and highly effective architecture used by many participants and baseline methods. |
| Advanced CNN/Transformer Models [8] [73] | Leverages modern deep learning for improved feature extraction and context capture (e.g., ResSAXU-Net). | Represents the cutting edge of methodological innovation driven by the challenge. |
| Dice & Cross-Entropy Hybrid Loss [73] | Loss function that handles severe class imbalance between tumor sub-regions and background. | Critical for training models that perform well on the imbalanced data typical of medical images. |
| Evaluation Metrics (Dice, Hausdorff Distance) [71] [5] | Quantifies segmentation performance for volumetric overlap and boundary accuracy. | Standardized metrics used for the official ranking of all submitted algorithms. |
The BraTS benchmark continues to evolve, with future directions emphasizing greater clinical relevance, robustness, and broader applicability. The 2025 cluster of challenges highlights trends such as generalizability across tumor types and institutions, survival and treatment response prediction, and the integration of histopathology data to link imaging phenotypes with molecular and cellular characteristics [70]. There is also a growing focus on federated learning approaches to train models on distributed data without centralizing it, addressing privacy concerns and enabling learning from even larger, more diverse datasets [5].
In conclusion, the BraTS dataset and the MICCAI challenges have become an indispensable ecosystem for the field of automated brain tumor segmentation. By providing a standardized, high-quality, and clinically relevant benchmark, BraTS has not only fueled a decade of algorithmic progress but has also created a pathway for translating AI research into tools that can ultimately improve the care and outcomes of patients with brain tumors. For researchers and drug development professionals, engagement with BraTS provides a robust framework for validating new methods and ensuring their work addresses the complex realities of clinical neuro-oncology.
The development of automated Artificial Intelligence (AI) models for brain tumor segmentation from MRI scans requires robust quantitative metrics to evaluate performance against clinically established ground truths. In neuro-oncology research and drug development, segmentation accuracy directly influences treatment planning, therapy response assessment, and disease progression monitoring. The selection of appropriate validation metrics is therefore critical for translating AI algorithms from research to clinical applications. This document elaborates on four key metrics—Dice Score, Intersection over Union (IoU), Hausdorff Distance (HD), and Sensitivity/Specificity—providing researchers with comprehensive application notes and experimental protocols for their implementation within a brain tumor segmentation context. These metrics collectively assess different aspects of segmentation quality, including volumetric overlap, boundary accuracy, and classification performance, enabling a holistic evaluation of model efficacy [67].
Metric Definitions and Mathematical Formulations
Dice-Sørensen Coefficient (Dice Score)
The Dice-Sørensen Coefficient (DSC), commonly referred to as the Dice Score, is a spatial overlap index ranging from 0 (no overlap) to 1 (perfect agreement). It is one of the most widely adopted metrics in medical image segmentation due to its sensitivity to both size and location of the segmented region [74]. The Dice Score is calculated as twice the area of intersection between the predicted segmentation (X) and the ground truth (Y), divided by the sum of the areas of both volumes. Mathematically, this is represented as:
$$DSC = \frac{2|X \cap Y|}{|X| + |Y|}$$
In terms of binary classification outcomes (True Positives-TP, False Positives-FP, False Negatives-FN), the formula becomes:
$$DSC = \frac{2 \times TP}{2 \times TP + FP + FN}$$
For brain tumor segmentation, a Dice Score > 0.85 is generally considered robust for most clinical applications, while models achieving Dice > 0.90 are approaching expert-level performance [67] [27]. The Dice Score is particularly valuable in therapeutic development as it correlates with volumetric accuracy, a key parameter in treatment response assessment.
Intersection over Union (IoU)
The Intersection over Union (IoU), also known as the Jaccard Index, measures the overlap between the predicted segmentation and the ground truth region relative to their unified area. It is defined as the area of intersection divided by the area of union of the two regions [75]:
$$IoU = \frac{|X \cap Y|}{|X \cup Y|} = \frac{TP}{TP + FP + FN}$$
The IoU is always smaller than or equal to the Dice Score, with the mathematical relationship between them being $J = S/(2-S)$ or $S = 2J/(1+J)$, where S is the Dice Score and J is the Jaccard Index [74]. In object detection tasks, a common threshold for a "good" prediction is IoU ≥ 0.5, though this can be adjusted based on the required precision-recall balance for specific clinical applications [75]. For complex brain tumor sub-regions with ambiguous boundaries, such as infiltrative tumor margins, IoU provides a stringent measure of spatial accuracy.
Hausdorff Distance (HD)
The Hausdorff Distance (HD) is a boundary-based metric that measures the maximum distance between the surfaces of the predicted and ground truth segmentations. Unlike volumetric metrics, HD is particularly sensitive to outliers and boundary errors, making it crucial for evaluating segmentation accuracy in surgical planning and radiotherapy targeting where precise boundary delineation is critical [76] [77]. The directed Hausdorff distance from set X to Y is defined as:
$$h(X,Y) = \max{x \in X} \min{y \in Y} ||x - y||$$
where $||x - y||$ is the Euclidean distance between points x and y. The actual Hausdorff Distance is the maximum of the directed distances in both directions:
$$HD(X,Y) = \max(h(X,Y), h(Y,X))$$
In clinical practice, the modified 95% Hausdorff Distance is often used instead, which takes the 95th percentile of distances rather than the maximum, reducing sensitivity to single outlier points [77]. This is especially relevant for brain tumor segmentation where isolated annotation errors may occur.
Sensitivity and Specificity
Sensitivity and Specificity are statistical classification metrics that evaluate a model's ability to correctly identify tumor pixels (sensitivity) and non-tumor pixels (specificity). These metrics are fundamental for assessing the clinical utility of segmentation algorithms, particularly in minimizing false negatives (critical for diagnostic applications) and false positives (important for radiotherapy planning) [78].
Sensitivity (True Positive Rate or Recall) measures the proportion of actual tumor pixels correctly identified:
$$Sensitivity = \frac{TP}{TP + FN}$$
Specificity (True Negative Rate) measures the proportion of actual non-tumor pixels correctly identified:
$$Specificity = \frac{TN}{TN + FP}$$
In brain tumor segmentation, there is often a trade-off between sensitivity and specificity. The optimal balance depends on the clinical context; for example, surgical planning may prioritize sensitivity to ensure complete tumor resection, while specific radiotherapy applications may emphasize specificity to spare healthy tissue [67].
Table 1: Summary of Key Performance Metrics for Brain Tumor Segmentation
| Metric | Mathematical Formula | Clinical Interpretation | Optimal Value Range | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Dice Score (DSC) | $\frac{2 | X \cap Y | }{ | X | + | Y | }$ | Volumetric overlap agreement | >0.85 (Good), >0.90 (Excellent) | ||
| Intersection over Union (IoU) | $\frac{ | X \cap Y | }{ | X \cup Y | }$ | Spatial overlap relative to combined area | >0.70 (Good), >0.80 (Excellent) | ||||
| Hausdorff Distance (HD) | $\max(\max{x}\min{y} | x-y | , \max{y}\min{x} | x-y | )$ | Maximum boundary separation | <15mm (Good), <10mm (Excellent) | ||||
| Sensitivity | $\frac{TP}{TP + FN}$ | Ability to detect tumor tissue | >0.85 (Minimizing false negatives) | ||||||||
| Specificity | $\frac{TN}{TN + FP}$ | Ability to exclude non-tumor tissue | >0.95 (Minimizing false positives) |
Computational Implementation and Experimental Protocols
Algorithm Implementation Frameworks
Implementation of these metrics requires careful computational design to ensure accuracy and reproducibility. The following code snippets demonstrate core calculation methodologies:
Experimental Protocol for Metric Validation
Purpose: To systematically evaluate the performance of brain tumor segmentation algorithms using the four key metrics.
Materials and Dataset Requirements:
- Multi-modal MRI data (T1-weighted, T1-weighted contrast-enhanced, T2-weighted, FLAIR)
- Expert-annotated ground truth segmentation masks
- Validation framework (e.g., NVIDIA Clara, MONAI, or custom Python implementation)
Procedure:
- Data Preprocessing:
- Co-register all MRI modalities to a common space
- Apply intensity normalization (e.g., z-score or White Stripe normalization)
- Resample all images to isotropic resolution (typically 1mm³)
Model Inference:
- Execute segmentation model on test dataset (minimum recommended n=50 cases)
- Generate binary masks for each tumor sub-region (enhancing tumor, tumor core, whole tumor)
Metric Calculation:
- Compute Dice, IoU, HD, Sensitivity, and Specificity for each case and sub-region
- Apply the 95th percentile modification for Hausdorff Distance to reduce outlier impact
- Calculate aggregate statistics (mean, standard deviation) across the test cohort
Statistical Analysis:
- Perform paired t-tests or Wilcoxon signed-rank tests for model comparisons
- Calculate confidence intervals using bootstrapping methods (recommended n=1000 iterations)
- Implement correction for multiple comparisons where appropriate
Clinical Correlation:
- Relate metric performance to clinical acceptability thresholds
- Evaluate segmentation quality for specific applications (e.g., radiotherapy planning, surgical navigation)
Table 2: Research Reagent Solutions for Brain Tumor Segmentation Research
| Reagent/Material | Function/Application | Implementation Example |
|---|---|---|
| BraTS Dataset | Benchmark dataset for model training/validation | Multi-institutional multi-modal MRI with expert annotations [79] [80] |
| MONAI Framework | Medical AI research platform | Open-source PyTorch-based framework for reproducible training [80] |
| SimpleITK | Medical image processing | Registration, resampling, and interpolation operations |
| NNU-Net | Baseline segmentation framework | State-of-the-art configuration for method comparison [78] |
| ITK-SNAP | Ground truth annotation | Manual segmentation and visualization of tumor sub-regions |
Metric Interrelationships and Clinical Interpretation
Complementary Metric Analysis
Understanding the relationships between different metrics is essential for comprehensive model assessment. The Dice Score and IoU are mathematically related but provide different perspectives on spatial overlap. The Dice Score tends to be more forgiving of minor boundary inaccuracies compared to IoU, which provides a more stringent assessment. Hausdorff Distance complements these volumetric metrics by specifically evaluating boundary precision, which is particularly important for surgical and radiotherapy applications where marginal errors have significant clinical consequences [76] [77].
Sensitivity and Specificity must be interpreted together to understand the clinical implications of segmentation errors. High sensitivity with low specificity indicates over-segmentation (including healthy tissue as tumor), while low sensitivity with high specificity suggests under-segmentation (missing portions of the tumor). The optimal balance depends on the clinical context; for example, radiation oncology may prioritize high specificity to minimize damage to healthy tissue, while surgical planning may emphasize sensitivity to ensure complete tumor resection [67].
Diagram 1: Metric-Application Relationship Mapping (76 characters)
Clinical Validation and Acceptability Thresholds
Translating metric performance to clinical utility requires establishing acceptability thresholds based on clinical requirements. Recent studies have demonstrated that segmentation accuracy directly impacts the efficacy of downstream quantitative imaging biomarkers. Research has shown that while radiomic features and prediction models are generally resilient to minor segmentation imperfections (Dice ≥ 0.85), performance degrades significantly with lower segmentation accuracy (Dice ≤ 0.85) [67].
For clinical adoption in neuro-oncology, the following performance thresholds are recommended based on current literature:
- Dice Score: >0.85 for whole tumor, >0.80 for tumor core, >0.75 for enhancing tumor
- Hausdorff Distance (95%): <10mm for whole tumor, <15mm for tumor sub-regions
- Sensitivity: >0.85 to minimize false negatives in diagnostic applications
- Specificity: >0.95 to minimize false positives in treatment planning
These thresholds ensure that automated segmentations are sufficiently accurate for clinical tasks such as tumor volume measurement, growth rate calculation, and treatment response assessment according to RANO (Response Assessment in Neuro-Oncology) criteria [67].
Advanced Considerations in Metric Application
Domain-Specific Metric Adaptations
Brain tumor heterogeneity necessitates specialized adaptations of these metrics. For multi-class segmentation (e.g., simultaneously segmenting enhancing tumor, necrotic core, and peritumoral edema), metrics should be calculated per class and then aggregated using macro-averaging (treating all classes equally) or micro-averaging (weighting by class prevalence). The BraTS challenge employs per-class Dice and Hausdorff Distance specifically for enhancing tumor, tumor core, and whole tumor regions to provide a comprehensive assessment of segmentation performance across biologically distinct compartments [79] [80].
For clinical trials assessing treatment response, longitudinal metric stability is as important as cross-sectional accuracy. Segmentation consistency across multiple time points should be evaluated using test-retest reliability analysis in addition to standard spatial accuracy metrics. This is particularly critical for assessing subtle changes in tumor volume during therapy, where measurement variability could obscure true treatment effects.
Limitations and Mitigation Strategies
Each metric has inherent limitations that researchers must acknowledge. The Dice Score is sensitive to object size, with smaller tumors inherently yielding lower Dice values even with excellent boundary agreement. Hausdorff Distance is highly sensitive to outliers, though the 95% modification mitigates this issue. Sensitivity and Specificity are influenced by class imbalance, which is pronounced in brain tumor segmentation where non-tumor voxels vastly outnumber tumor voxels.
To address these limitations, researchers should:
- Always report multiple metrics to provide a comprehensive performance assessment
- Include confidence intervals to communicate measurement uncertainty
- Conduct subgroup analyses based on tumor size and location
- Perform statistical testing to determine if observed differences are clinically significant
- Validate metric performance against clinical endpoints when possible
Diagram 2: Metric Limitations and Solutions (43 characters)
The four metrics discussed—Dice Score, IoU, Hausdorff Distance, and Sensitivity/Specificity—provide complementary perspectives on segmentation quality for brain tumor MRI analysis. While Dice Score remains the most commonly reported metric in the literature, comprehensive validation requires all four metrics to fully characterize different aspects of performance. As AI-assisted segmentation moves toward clinical adoption in neuro-oncology and drug development, understanding the nuances of these metrics and their relationship to clinical tasks becomes increasingly important. Researchers should select metrics based on their specific application context while maintaining transparency about limitations and interpretation constraints. Future work should focus on developing standardized reporting guidelines and validating metric thresholds against clinically relevant endpoints to facilitate the translation of automated segmentation tools from research to clinical practice.
Comparative Analysis of State-of-the-Art Models on Public and Clinical Datasets
Automated brain tumor segmentation from Magnetic Resonance Imaging (MRI) represents a critical frontier in computational neuro-oncology, enabling precise tumor quantification for diagnosis, treatment planning, and disease monitoring [9]. The field has evolved from traditional machine learning approaches to sophisticated deep learning architectures capable of handling the complex heterogeneity of brain tumors [3]. This application note provides a systematic comparison of contemporary segmentation models benchmarked on public and clinical datasets, detailing their operational protocols and performance characteristics to guide researchers and clinicians in selecting appropriate methodologies for specific research contexts. The integration of artificial intelligence (AI) in this domain addresses significant challenges in manual segmentation, which is time-consuming, subjective, and prone to inter-observer variability [8], thereby accelerating neuro-oncological research and drug development workflows.
Public Datasets for Brain Tumor Segmentation
Publicly available datasets serve as vital benchmarks for training and evaluating brain tumor segmentation models, providing standardized ground truth annotations essential for comparative analysis. These datasets vary in tumor types, imaging modalities, and annotation specifics, requiring researchers to select datasets aligned with their specific research objectives.
Table 1: Key Public Datasets for Brain Tumor Segmentation
| Dataset Name | Tumor Types | Number of Cases | MRI Modalities | Annotation Details |
|---|---|---|---|---|
| BraTS 2021 [81] | Adult diffuse glioma | 2,000 patients | T1, T1-CE, T2, FLAIR | Whole tumor, tumor core, enhancing tumor |
| BraTS 2020 [3] | Various brain tumors | Not specified | T1, T1-CE, T2, FLAIR | Necrotic core, enhancing tumor, edema |
| BRISC [82] | Glioma, meningioma, pituitary | 6,000 scans | Contrast-enhanced T1-weighted | Three major tumor types plus non-tumorous cases |
| BraTS-METS 2023 [81] | Brain metastasis | 328 cases | Multiple | Multi-class labels |
| BraTS Meningioma 2024 [81] | Meningioma | 1,650 cases | Multiple | Tumor segmentation masks |
| ISLES 2015 [80] | Ischemic stroke | 28 cases | T1, T2, DWI | Ischemic lesions |
| UltraCortex 9.4T [83] | Healthy volunteers (anatomy) | 78 subjects | T1-weighted MP-RAGE/MP2RAGE | White and gray matter boundaries |
The Brain Tumor Segmentation (BraTS) challenges have consistently provided the most comprehensive benchmarking datasets, expanding from initial glioma focus to include meningiomas, metastases, and pediatric tumors [9] [81]. Recent contributions like the BRISC dataset address previous limitations by providing 6,000 contrast-enhanced T1-weighted MRI scans with expert annotations by certified radiologists across three imaging planes (axial, sagittal, coronal) to facilitate robust model development [82]. For specialized applications, the UltraCortex dataset offers ultra-high-resolution 9.4T MRI scans, enabling development of models capable of segmenting subtle anatomical details that are imperceptible in conventional 1.5T-3T scanners [83].
Performance Comparison of State-of-the-Art Models
Quantitative evaluation of segmentation models typically employs the Dice Similarity Coefficient (DSC) to measure overlap between predicted and ground truth regions, with additional metrics including Hausdorff Distance (HD) for boundary accuracy and precision/recall for comprehensive assessment.
Table 2: Comparative Performance of Segmentation Models on Benchmark Datasets
| Model Architecture | Dataset | Dice Score (Whole Tumor) | Dice Score (Tumor Core) | Dice Score (Enhancing Tumor) | Computational Efficiency |
|---|---|---|---|---|---|
| MM-MSCA-AF [3] | BraTS 2020 | 0.8589 | 0.8158 (necrotic) | Not specified | Moderate |
| GA-MS-UNet++ [83] | UltraCortex 9.4T | 0.93 (manual GT) 0.89 (SynthSeg GT) | Not specified | Not specified | High |
| nnU-Net [81] | BraTS 2020 | 0.8895 | 0.8506 | 0.8203 | Moderate |
| Modified nnU-Net [81] | BraTS 2021 | 0.9275 | 0.8781 | 0.8451 | Moderate |
| EfficientNet B0 + VSS Blocks [80] | BraTS 2015, ISLES 2015 | Not specified | Not specified | Not specified | High |
| Asymmetrical U-Net [81] | BraTS 2018 | 0.8839 | 0.8154 | 0.7664 | Moderate |
| Two-Stage Cascaded U-Net [81] | BraTS 2019 | 0.8880 | 0.8370 | 0.8327 | Low |
The Multi-Modal Multi-Scale Contextual Aggregation with Attention Fusion (MM-MSCA-AF) framework demonstrates competitive performance on BraTS 2020, particularly for necrotic tumor regions where it achieves a Dice value of 0.8158 [3]. This model leverages multi-modal MRI inputs (T1, T2, FLAIR, T1-CE) with gated attention fusion to selectively refine tumor-specific features while suppressing noise. For ultra-high-field MRI applications, the GA-MS-UNet++ model achieves exceptional performance (Dice score: 0.93) on 9.4T data through integrated multi-scale residual blocks and gated skip connections [83]. The nnU-Net framework and its variants continue to demonstrate robust performance across multiple BraTS challenges, with modified nnU-Net achieving Dice scores of 0.9275 for whole tumor segmentation in BraTS 2021 [81].
Lightweight architectures like the EfficientNet B0 encoder with Visual State-Space (VSS) blocks offer compelling efficiency for resource-constrained environments while maintaining competitive segmentation accuracy through multi-scale attention mechanisms [80]. This balance of performance and efficiency makes such models particularly suitable for clinical deployment in settings with limited computational resources.
Experimental Protocols for Model Implementation
Data Preprocessing Pipeline
Standardized data preprocessing is essential for ensuring consistent model performance across diverse datasets. The following protocol outlines key preprocessing steps derived from successful implementations:
Intensity Normalization: Normalize voxel intensities to zero mean and unit variance on a per-volume basis to reduce inter-patient and inter-modality variability [80]. For ultra-high-resolution 9.4T data, apply additional bias field correction to address intensity inhomogeneities [83].
Multi-Modal Registration and Handling: For multi-modal datasets (e.g., BraTS with T1, T1-CE, T2, FLAIR), rigidly co-register all modalities to a common space and concatenate along the channel dimension to create multi-channel inputs [80] [3].
Spatial Resampling and Cropping: Resample all images to isotropic resolution (typically 1mm³) and consistently resize to dimensions of 256×256 pixels for 2D models [80] or 128×128×128 for 3D architectures. Implement center-cropping to focus on relevant brain regions while maintaining computational efficiency.
Data Augmentation: Apply real-time augmentation during training including random rotations (±15°), horizontal flipping, random contrast adjustments (±20%), and Gaussian noise injection to improve model generalization [83].
Model Training Protocol
Consistent training procedures ensure fair comparison across different architectures and facilitate reproducible results:
Optimization Configuration: Utilize AdamW optimizer with initial learning rate of 0.0001 and weight decay of 1e-5. Implement cosine annealing learning rate scheduling over 100 epochs with minimum learning rate set to 1e-6 [80].
Loss Function Selection: Employ hybrid loss functions combining Dice loss with additional components tailored to specific challenges. For class imbalance, combine Dice loss with Focal Loss (γ=2) [80]. For precise boundary delineation, integrate Active Contour Loss with weighting factor β=0.3 [80].
Training Monitoring: Implement early stopping with patience of 10-15 epochs monitoring validation Dice score. Use batch sizes of 8-16 depending on available GPU memory and model complexity [80] [83].
Validation Strategy: Perform k-fold cross-validation (typically 5-fold) with consistent dataset splits to ensure robust performance estimation. Maintain separate hold-out test sets for final evaluation only.
Evaluation Methodology
Standardized evaluation protocols enable meaningful comparison across studies:
Primary Metrics: Calculate Dice Similarity Coefficient (DSC) for overall segmentation overlap. Compute 95% Hausdorff Distance (HD95) for boundary accuracy assessment. Include precision and recall for comprehensive performance characterization [83].
Statistical Validation: Perform Wilcoxon signed-rank tests for paired comparisons between model performances. Use Kruskal-Wallis tests for multiple group comparisons with post-hoc analysis where appropriate [83].
Clinical Validation: For clinically deployed models, conduct volumetric correlation analysis between predicted segmentations and expert manual annotations, with target R² values exceeding 0.90 [83].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents and Computational Resources for Brain Tumor Segmentation
| Resource Category | Specific Tool/Resource | Function/Purpose | Application Context |
|---|---|---|---|
| Public Datasets | BraTS Series [9] | Benchmarking segmentation algorithms | Model development and validation |
| BRISC [82] | Multi-class tumor classification | Training robust, generalizable models | |
| UltraCortex 9.4T [83] | Ultra-high-resolution segmentation | Developing models for fine anatomical details | |
| Software Frameworks | nnU-Net [81] | Automated configuration of segmentation pipelines | Baseline model development |
| PyTorch/TensorFlow | Deep learning model implementation | Custom architecture development | |
| Computational Resources | NVIDIA GPUs (≥8GB VRAM) | Model training and inference | Essential for deep learning workflows |
| Evaluation Metrics | Dice Score, HD95 [83] | Quantitative performance assessment | Model comparison and validation |
Integration Pathways and Clinical Applications
The transition from experimental models to clinical implementation requires careful consideration of integration pathways and validation frameworks. AI-based segmentation tools have demonstrated potential for enhancing neurodiagnostics by providing quantitative tumor assessments that complement radiologist evaluations [14] [8].
Clinical Workflow Integration
Successful clinical integration requires adapting model outputs to existing healthcare systems:
PACS Integration: Develop DICOM-compliant output formats compatible with Picture Archiving and Communication Systems (PACS) for seamless radiologist review.
Visualization Interfaces: Implement interactive visualization platforms allowing clinicians to review, edit, and approve automated segmentations, with particular attention to uncertainty visualization for low-confidence regions.
Quantitative Reporting: Generate automated quantitative reports including tumor volume measurements, longitudinal change detection, and multimodal correlation statistics to support clinical decision-making.
Regulatory Considerations
For translation to clinical practice, segmentation models should adhere to regulatory requirements:
FDA-Approved Tools: Leverage existing FDA-approved AI platforms (e.g., Pixyl Neuro, Rapid ASPECTS) as reference standards for clinical validation studies [8].
Technical Validation: Conduct rigorous technical validation including repeatability testing, multi-site performance verification, and failure mode analysis to establish model robustness across diverse patient populations and imaging protocols.
The comparative analysis of state-of-the-art brain tumor segmentation models reveals a dynamic landscape where architectural innovations continue to push performance boundaries across diverse datasets. The MM-MSCA-AF and GA-MS-UNet++ architectures demonstrate how attention mechanisms and multi-scale feature aggregation can address specific challenges in tumor heterogeneity and ultra-high-resolution imaging, while lightweight models like EfficientNet B0 with VSS blocks offer practical solutions for resource-constrained environments. As the field progresses, the emergence of foundation models trained on massive diverse datasets holds promise for further enhancing segmentation accuracy and generalizability. Researchers and clinicians should select models based on specific application requirements, considering factors such as available computational resources, required inference speed, and target tumor characteristics. Standardized implementation of the experimental protocols outlined in this application note will facilitate reproducible development and meaningful comparison of future segmentation architectures.
The U.S. Food and Drug Administration (FDA) regulates artificial intelligence (AI) tools intended for medical purposes as software as a medical device (SaMD) or software in a medical device (SiMD). Under Section 201(h) of the Federal Food, Drug, and Cosmetic Act, AI is considered a medical device if it is intended for use in the "diagnosis, cure, mitigation, treatment, or prevention of disease" [84]. The FDA's approach to AI-enabled medical devices has evolved significantly to address the unique challenges posed by adaptive algorithms and machine learning models, with a particular focus on tools for automated tumor segmentation in brain MRI scans.
The FDA maintains an AI-Enabled Medical Device List that provides transparency regarding authorized devices, including those for neurological image analysis [85]. This list demonstrates the growing adoption of AI in clinical practice, with over 1,250 AI-enabled medical devices authorized for marketing in the United States as of July 2025 [84]. For brain tumor segmentation specifically, several tools have received FDA clearance, including NeuroQuant Brain Tumor, which offers fully automated segmentation and volumetric reporting of brain metastases and meningiomas [86].
FDA's Risk-Based Approach and Regulatory Pathways
Risk Classification and Regulatory Pathways
The FDA employs a risk-based approach to oversight, requiring that devices "demonstrate a reasonable assurance of safety and effectiveness" with higher-risk devices undergoing more rigorous review [84]. The classification system and corresponding regulatory pathways are detailed in the table below.
Table 1: FDA Risk Classification and Regulatory Pathways for Medical Devices
| Risk Class | Level of Risk | Regulatory Pathway | Examples | AI Application in Neuro-Imaging |
|---|---|---|---|---|
| Class I | Low risk | General controls | Tongue depressors | Minimal AI application |
| Class II | Moderate risk | 510(k) clearance, De Novo | MRI systems with embedded AI | AI-driven segmentation tools for brain tumors |
| Class III | High risk | Premarket Approval (PMA) | Implantable devices | AI for autonomous diagnostic interpretation |
Most AI-enabled brain MRI segmentation tools currently fall into Class II (moderate risk), typically following the 510(k) clearance pathway requiring demonstration of substantial equivalence to a predicate device [84]. However, the FDA has noted a growing number of AI-enabled devices in the Class III category that require the more rigorous Premarket Approval (PMA) process [84].
Regulatory Pathways for AI Tools
The journey from research to clinic for an AI-based brain tumor segmentation tool follows established regulatory pathways, with additional considerations for algorithm transparency and performance validation.
Diagram 1: FDA Regulatory Pathway for AI Tools
The Predetermined Change Control Plan (PCCP) has emerged as a critical component for AI/ML-enabled devices, allowing manufacturers to pre-specify and obtain authorization for anticipated modifications to algorithms, such as retraining with new data or performance enhancements, without requiring a new submission for each change [87]. This is particularly relevant for adaptive AI systems used in brain tumor segmentation that may evolve and improve over time through continuous learning.
Special Considerations for AI-Enabled Medical Devices
Total Product Lifecycle (TPLC) Approach
The FDA has adopted a Total Product Lifecycle (TPLC) approach that assesses AI-enabled devices across their entire lifespan: design, development, deployment, and postmarket monitoring [84]. This is particularly important for AI tools, including those for brain tumor segmentation, as models may continue to evolve after authorization. The TPLC approach encompasses several key elements:
- User interface and labeling appropriate for the intended users
- Comprehensive risk assessment specific to AI algorithms
- Robust data management practices throughout the lifecycle
- Transparent model description and development processes
- Rigorous validation of performance claims
- Ongoing device performance monitoring in clinical use
- Cybersecurity considerations for connected AI systems [87]
Good Machine Learning Practice (GMLP) Principles
The FDA, in collaboration with Health Canada and the United Kingdom's MHRA, has established Good Machine Learning Practice (GMLP) principles to ensure safe and effective AI [84]. These ten guiding principles emphasize:
- Multi-disciplinary expertise throughout the product lifecycle
- Implementation of model design tailored to the intended use
- Focus on clinical relevance and human-AI interaction
- Training with representative datasets to minimize bias
- Use of rigorous validation methods for performance assessment
- Testability and demonstration of safety in clinical context
- Documentation transparency for regulatory review and user understanding
- Comprehensive monitoring for maintenance and improvement
- Engineering practices ensuring reliability and reproducibility
Protocol for Validating AI-Based Brain Tumor Segmentation Tools
Experimental Validation Framework
For AI-based brain tumor segmentation tools intended for regulatory submission, a comprehensive validation protocol must be implemented. The following workflow outlines the key stages in the experimental validation process.
Diagram 2: AI Validation Workflow
Performance Metrics and Benchmarking
Rigorous performance evaluation against established benchmarks and metrics is essential for FDA submission. The following table outlines key quantitative metrics used in validating brain tumor segmentation algorithms.
Table 2: Key Performance Metrics for Brain Tumor Segmentation AI
| Metric | Formula | Interpretation | Target Value | Clinical Significance | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dice Similarity Coefficient (DSC) | ( DSC = \frac{2 | X \cap Y | }{ | X | + | Y | } ) | Overlap between AI and expert segmentation | >0.85 [9] | Volumetric agreement with radiologist |
| Sensitivity | ( Sensitivity = \frac{TP}{TP + FN} ) | Ability to identify all tumor voxels | >0.90 | Minimizes false negatives | ||||||
| Specificity | ( Specificity = \frac{TN}{TN + FP} ) | Ability to exclude non-tumor voxels | >0.90 | Minimizes false positives | ||||||
| Hausdorff Distance | ( HD(X,Y) = \max\left(\sup{x \in X} \inf{y \in Y} d(x,y), \sup{y \in Y} \inf{x \in X} d(x,y)\right) ) | Maximum boundary distance | <10mm [9] | Boundary delineation accuracy | ||||||
| Precision | ( Precision = \frac{TP}{TP + FP} ) | Positive predictive value | >0.85 | Reliability of positive findings |
Recent advances in deep learning have demonstrated DSCs exceeding 0.85-0.90 for glioma segmentation in benchmark datasets like BraTS (Brain Tumor Segmentation), though performance varies by tumor type and grade [9]. The FDA expects performance to be validated across diverse patient populations and clinical scenarios representative of the intended use population.
Essential Research Reagents and Computational Tools
Successful development and regulatory approval of AI-based brain tumor segmentation tools requires specific computational resources and validation frameworks.
Table 3: Essential Research Reagents and Computational Tools
| Resource Category | Specific Examples | Function in AI Development | Regulatory Considerations |
|---|---|---|---|
| Public Datasets | BraTS, TCIA [9] | Model training and benchmarking | Data provenance, annotation quality, representativeness |
| Annotation Tools | ITK-SNAP, 3D Slicer | Ground truth generation | Inter-rater reliability, expert qualifications |
| Deep Learning Frameworks | PyTorch, TensorFlow | Model architecture implementation | Version control, reproducibility |
| Validation Metrics | Dice Score, Hausdorff Distance | Performance quantification | Clinical correlation, acceptance thresholds |
| Computational Infrastructure | GPU clusters, Cloud computing | Model training and inference | Cybersecurity, data protection |
Compliance Strategies and Documentation Requirements
Predetermined Change Control Plan (PCCP)
For AI/ML-enabled devices, a Predetermined Change Control Plan is recommended to accommodate the iterative nature of machine learning algorithms [87]. The PCCP should include three key components:
- Description of Modifications: Detailed specifications of planned changes, such as retraining with new data, architecture adjustments, or expansion to new tumor types.
- Modification Protocol: Specific methodologies for data management, retraining procedures, performance evaluation, and update deployment.
- Impact Assessment: Comprehensive evaluation of benefits and risks associated with proposed changes, including mitigation strategies.
Postmarket Surveillance and Real-World Performance Monitoring
The FDA emphasizes postmarket surveillance for AI-enabled devices to monitor performance in real-world clinical settings [88]. Key elements include:
- Performance monitoring across diverse patient populations and clinical settings
- Periodic reporting of real-world performance metrics
- Bias detection and mitigation strategies
- User feedback mechanisms to identify potential issues
- Cybersecurity monitoring for connected systems
Navigating the FDA regulatory pathway for AI-based brain tumor segmentation tools requires careful planning from the earliest research stages. By implementing robust validation protocols, adhering to Good Machine Learning Practices, and developing comprehensive regulatory strategies that include Predetermined Change Control Plans, researchers and developers can successfully transition these innovative tools from research to clinical practice while meeting FDA requirements for safety and effectiveness.
The validation of automated brain tumor segmentation systems is undergoing a critical evolution, moving from static, retrospective assessments towards dynamic frameworks that are real-time, three-dimensional, and interactive. This paradigm shift is essential for translating artificial intelligence (AI) research from academic benchmarks into trusted clinical tools for diagnosis, treatment planning, and drug development. Traditional validation metrics, while useful for initial model ranking, often fail to capture the practical requirements of clinical workflows, such as computational efficiency, robustness across diverse scanner platforms, and the ability for expert radiologists to interact with and refine AI-generated outputs. This document outlines advanced application notes and experimental protocols designed to validate the next generation of brain tumor segmentation systems within a real-world clinical context.
Application Notes: Core Paradigms for Future Validation
The following application notes summarize the key technological shifts defining the future of segmentation system validation.
Table 1: Core Paradigms for Future Validation Systems
| Validation Paradigm | Key Feature | Enabling Technology | Clinical/Rearch Utility |
|---|---|---|---|
| Real-Time & Automated Processing | Automated, rapid analysis integrated into clinical workflow for timely intervention. [89] | Deep learning models (e.g., 3D-UNet) with automated quality checks for sequence compliance. [89] | Enables monitoring of disease activity (e.g., in MS) and treatment response; supports high-throughput analysis in clinical trials. |
| Fully 3D Volumetric Analysis | Processes entire image volumes to maintain spatial context and consistency. [90] | 3D convolutional neural networks (CNNs); hierarchical adaptive pruning of 3D voxels. [91] [90] | Provides accurate tumor volume measurements, essential for tracking tumor progression and treatment efficacy. |
| Interactive & Human-in-the-Loop Refinement | Allows experts to correct and refine AI-generated segmentations. | Software platforms (e.g., 3D Slicer) with AI-assisted segmentation and interactive editing tools. [92] | Increases trust and adoption by clinicians; ensures final segmentation accuracy meets diagnostic standards. |
| Multi-Scanner & Multi-Center Robustness | Validation across images from different scanner manufacturers and protocols. [89] | Domain adaptation techniques; AI models trained on large, multi-institutional datasets (e.g., BraTS). [91] [21] | Ensures model generalizability and reliability, a prerequisite for widespread clinical deployment and regulatory approval. |
Experimental Protocols for Advanced System Validation
Protocol 1: Real-Time Performance and Computational Benchmarking
Aim: To validate the processing speed and computational efficiency of a segmentation model for use in real-time or near-real-time clinical settings.
Background: Real-time capability is crucial for applications like surgical planning or intraoperative diagnostics. Efficiency is particularly important for resource-constrained settings. [91]
Materials:
- Hardware: Standard clinical workstation with GPU (e.g., NVIDIA GeForce RTX 3080) and a high-performance computing cluster node.
- Software: Python with PyTorch/TensorFlow, time and memory profiling libraries (e.g.,
cProfile,torch.cuda.max_memory_allocated). - Dataset: BraTS 2019 or 2023 multi-parametric MRI dataset. [91]
Methodology:
- Model Inference: Execute the segmentation model (e.g., a lightweight 3D-CNN or a pruning-based algorithm [91]) on a pre-loaded batch of 100 MRI volumes from the BraTS dataset.
- Metric Collection: For each volume, record:
- Inference Time: Time from model input to segmentation output.
- Memory Consumption: Peak GPU memory usage during inference.
- Throughput: Number of volumes processed per hour.
- Comparative Analysis: Benchmark the model's performance against a reference state-of-the-art architecture (e.g., U-Net [7] [21]) under identical hardware conditions.
Table 2: Exemplar Real-Time Performance Benchmarking Data
| Model Architecture | Average Inference Time (seconds/volume) | Peak GPU Memory (GB) | Throughput (volumes/hour) | Reported Dice Score (%) |
|---|---|---|---|---|
| Hierarchical Adaptive Pruning [91] | ~5-10 | ~4 | 360-720 | 99.13 |
| ARU-Net [7] | ~30-60 | ~8 | 60-120 | 98.10 |
| Standard 3D U-Net [21] | ~45-90 | ~10 | 40-80 | ~90 |
Protocol 2: 3D Volumetric Accuracy and Robustness Validation
Aim: To rigorously assess the accuracy of a model's 3D tumor segmentation and its robustness across multi-center data.
Background: 3D segmentation captures the complete tumor morphology, which is vital for volumetric assessments in treatment planning and tracking. [90] Models must perform consistently on data from different MRI scanners.
Materials:
- Datasets: BraTS 2023 (multi-institutional) [91] and an in-house dataset from at least two different scanner manufacturers (e.g., Siemens, GE, Philips). [89]
- Software: 3D Slicer for visualization and manual correction; Python with libraries for calculating metrics (e.g, Dice, Hausdorff Distance). [92]
Methodology:
- Cross-Dataset Validation: Run the trained model on the BraTS 2023 validation set and the separate multi-scanner in-house dataset.
- Volumetric Metric Calculation: For each segmented tumor sub-region (enhancing tumor, peritumoral edema, necrotic core), compute:
- 3D Dice Similarity Coefficient (DSC): Measures spatial overlap between AI segmentation and expert ground truth.
- Hausdorff Distance (HD): Quantifies the largest segmentation boundary error.
- Volumetric Correlation: Pearson correlation coefficient between the predicted and actual tumor volumes.
- Statistical Analysis: Perform a paired t-test to compare the model's performance on data from different scanner manufacturers and report the p-value to assess significant performance differences.
Protocol 3: Interactive Segmentation Refinement Workflow
Aim: To quantify the improvement in segmentation accuracy and time-saving achieved when a human expert interactively refines an AI-generated initial segmentation.
Background: Fully automated systems may still produce errors. An interactive "human-in-the-loop" workflow leverages AI for efficiency while retaining expert oversight for accuracy. [92]
Materials:
- Software Platform: 3D Slicer with the "Segment Editor" module. [92]
- Dataset: A set of 20 brain MRI scans with challenging tumor boundaries (e.g., diffuse gliomas).
- Participants: Two expert radiologists or trained biomedical researchers.
Methodology:
- Baseline Establishment: Experts manually segment the 20 scans from scratch, recording the time taken.
- AI Pre-Segmentation: The AI model generates initial segmentations for the same 20 scans.
- Refinement Phase: Experts load the AI-generated segmentations into 3D Slicer and use tools like "paint," "erase," and "smoothing" to correct errors. The time for this refinement is recorded.
- Data Analysis:
- Calculate the Dice score of the AI pre-segmentation versus the ground truth.
- Calculate the Dice score of the post-refinement segmentation versus the ground truth.
- Compare the total time for "manual from scratch" versus "AI + refinement."
Diagram 1: Interactive segmentation workflow.
The Scientist's Toolkit: Key Research Reagents & Software
Table 3: Essential Research Tools for Segmentation Validation
| Tool Name | Type | Primary Function in Validation | Key Features |
|---|---|---|---|
| 3D Slicer [92] | Software Platform | Visualization, interactive segmentation, and analysis of 3D medical images. | Open-source; extensive module library (Segment Editor); supports DICOM; AI integration. |
| BraTS Dataset [91] [21] | Benchmark Data | Standardized dataset for training and benchmarking multi-class brain tumor segmentation algorithms. | Multi-institutional; multi-modal MRI; expert-annotated tumor sub-regions. |
| Simpleware Software [93] | Software Platform | 3D image processing and model generation from DICOM images. | High-end segmentation and meshing; CAD integration; analysis and measurement tools. |
| iQ-Solutions (MS Report) [89] | AI-Based Tool | Automated, FDA-cleared tool for quantifying lesion burden and brain volume change in MS. | Provides longitudinal lesion activity and brain volume metrics; clinical validation. |
| PyTorch/TensorFlow | Programming Library | Deep Learning Framework for developing and training custom segmentation models (e.g., 3D U-Net). | Flexible architecture design; GPU acceleration; extensive community support. |
Conclusion
The integration of AI for automated brain tumor segmentation represents a paradigm shift in neuro-oncology, offering unprecedented precision and efficiency for both clinical practice and drug development. This review has synthesized key insights: foundational clinical needs drive technological innovation; sophisticated deep learning architectures like attention-enhanced U-Nets consistently deliver state-of-the-art performance; overcoming challenges related to data imbalance, model generalizability, and uncertainty quantification is essential for clinical adoption; and rigorous validation against standardized benchmarks is non-negotiable. Future progress hinges on developing more data-efficient and energy-aware architectures, establishing robust frameworks for regulatory approval, and deepening the integration of these tools into clinical trial workflows to objectively assess treatment efficacy. The continued collaboration between AI researchers, clinicians, and drug developers will be crucial in translating these powerful technologies into tangible improvements in patient outcomes.
References
- 1. Application of MRI image segmentation algorithm for brain ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2024.1510175/full]
- 2. Consensus recommendations for a standardized Brain Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4588759/]
- 3. Enhanced brain tumor segmentation in medical imaging ... [https://www.nature.com/articles/s41598-025-21255-4]
- 4. A review on brain tumor segmentation based on deep ... [https://www.sciencedirect.com/science/article/pii/S0895611123001313]
- 5. The Brain Tumor Segmentation (BraTS) Challenge 2023 [https://pmc.ncbi.nlm.nih.gov/articles/PMC10441440/]
- 6. Open-Source AI Model for MRI Segmentation Snags ... [https://www.rsna.org/media/press/2025/2627]
- 7. Automated Brain Tumor MRI Segmentation Using ARU-Net ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468718/]
- 8. Artificial Intelligence–Based Approaches for Brain Tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12443661/]
- 9. A review of deep learning for brain tumor analysis in MRI [https://www.nature.com/articles/s41698-024-00789-2]
- 10. The development of an artificial intelligence auto ... [https://www.nature.com/articles/s41598-025-88589-x]
- 11. A deep learning framework integrating MRI image ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9795279/]
- 12. Advanced preclinical functional magnetic resonance ... [https://www.nature.com/articles/s44303-025-00085-z]
- 13. Brain age gap as a predictive biomarker that links ... [https://www.nature.com/articles/s43856-025-01100-5]
- 14. Automated Brain Tumor Segmentation in MRI Using AI for ... [https://biomedpharmajournal.org/vol18no2/automated-brain-tumor-segmentation-in-mri-using-ai-for-improved-neurodiagnostics/]
- 15. Brain tumor segmentation using deep learning [https://pmc.ncbi.nlm.nih.gov/articles/PMC12281592/]
- 16. AI in MRI brain tumor diagnosis: A systematic review of ... [https://www.sciencedirect.com/science/article/pii/S0169743925000991]
- 17. Lightweight Brain Tumor Segmentation on Low-Resource ... [https://www.protocols.io/view/lightweight-brain-tumor-segmentation-on-low-resour-gz4sbx8wf.html]
- 18. Brain tumor detection, classification and segmentation by ... [https://www.sciencedirect.com/science/article/pii/S2590005625001985]
- 19. Artificial Intelligence-Based Approaches for Brain Tumor ... [https://pubmed.ncbi.nlm.nih.gov/40962716/]
- 20. Accuracy of detecting critical findings using abbreviated ... [https://www.sciencedirect.com/science/article/pii/S0720048X25004516]
- 21. Brain tumor segmentation with deep learning [https://www.sciencedirect.com/science/article/abs/pii/S0165027025000652]
- 22. Deep learning and AI in reducing magnetic resonance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11497590/]
- 23. Unsupervised generative AI for enhancing brain tumor ... [https://www.nature.com/articles/s41698-025-01173-4]
- 24. MRI Protocols [https://www.ohsu.edu/school-of-medicine/diagnostic-radiology/mri-protocols]
- 25. How Artificial Intelligence Is Shaping Medical Imaging ... - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10740686/]
- 26. Comparison of Vision Transformers and Convolutional ... [https://link.springer.com/article/10.1007/s10916-024-02105-8]
- 27. Deep learning-driven brain tumor classification and ... [https://www.nature.com/articles/s41598-025-13591-2]
- 28. A Deep Learning Framework for Brain Tumor Detection ... [https://www.sciencedirect.com/science/article/pii/S277294192500208X]
- 29. Brain tumor segmentation using deep learning [https://www.frontiersin.org/journals/radiology/articles/10.3389/fradi.2025.1616293/full]
- 30. BiTr-Unet: a CNN-Transformer Combined Network for MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9396958/]
- 31. UnetTransCNN: integrating transformers with convolutional ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1467672/full]
- 32. A brain tumor segmentation enhancement in MRI images ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-025-01837-4]
- 33. Brain tumor segmentation using multi-scale attention U-Net ... [https://www.nature.com/articles/s41598-025-94267-9]
- 34. U-Net vs Residual U-Net vs Attention U-Net ... - Code Like A Girl [https://code.likeagirl.io/u-net-vs-residual-u-net-vs-attention-u-net-vs-attention-residual-u-net-899b57c5698]
- 35. UNet and its Family: UNet++, Residual UNet, and Attention UNet [https://www.vizuaranewsletter.com/p/unet-and-its-family-unet-residual]
- 36. U-net based on residual and self-attention mechanism in ... [https://pubmed.ncbi.nlm.nih.gov/36863157/]
- 37. Deep learning for automated, motion-resolved tumor ... [https://www.nature.com/articles/s41698-025-00970-1]
- 38. Using deep learning to optimize the prostate MRI protocol ... [https://www.sciencedirect.com/science/article/pii/S0720048X24001864]
- 39. ARM-Net: Improved MRI brain tumor segmentation method ... [https://publications.eai.eu/index.php/el/article/view/5953]
- 40. A hybrid explainable model based on advanced machine ... [https://www.nature.com/articles/s41598-025-85874-7]
- 41. A systematic review of the hybrid machine learning models ... [https://www.frontiersin.org/journals/artificial-intelligence/articles/10.3389/frai.2025.1615550/full]
- 42. a four-stage deep network for accurate brain tumor ... [https://www.nature.com/articles/s41598-025-18879-x]
- 43. Multi-class brain tumor MRI segmentation and classification ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12613584/]
- 44. The multimodal MRI brain tumor segmentation based on ... [https://www.sciencedirect.com/science/article/pii/S174680942200790X]
- 45. Segmentation of Brain Tumors Using a Multi-Modal ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383440/]
- 46. Brain tumor segmentation using deep learning [https://pubmed.ncbi.nlm.nih.gov/40697313/]
- 47. Mix-modal Federated Learning for MRI Image Segmentation [https://arxiv.org/html/2509.02541v1]
- 48. Target Engagement: A Key Factor in Drug Development ... [https://www.pelagobio.com/cetsa-drug-discovery-resources/blog/target-engagement-drug-failure/]
- 49. Advancing drug development with “Fit-for-Purpose” modeling ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12436579/]
- 50. A deep learning approach for brain tumour classification ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1508326/full]
- 51. Redefining target engagement in drug discovery [https://www.news-medical.net/health/Redefining-target-engagement-with-new-strategies-in-drug-discovery.aspx]
- 52. On the Mark? Identifying Biomarkers of Target Engagement [https://sapient.bio/resources/target-engagement-biomarkers/]
- 53. CONSORT 2025 statement: Updated guideline for reporting ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11996237/]
- 54. MICCAI Brain Tumor Segmentation Lighthouse 2025 [https://www.emergentmind.com/topics/miccai-brain-tumor-segmentation-lighthouse-challenge-2025]
- 55. TextBraTS: Text-Guided Volumetric Brain Tumor ... [https://arxiv.org/html/2506.16784v2]
- 56. Clinical Image Testing: MRI (Revised 1-23-2025) [https://accreditationsupport.acr.org/support/solutions/articles/11000061017-clinical-image-testing-mri-revised-1-23-2025-]
- 57. Open-access quantitative MRI data of the spinal cord and ... [https://www.nature.com/articles/s41597-021-00941-8]
- 58. MRI-based quantification of intratumoral heterogeneity for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12078897/]
- 59. SmaRT: Style-Modulated Robust Test-Time Adaptation for ... [https://arxiv.org/html/2509.17925v1]
- 60. On-the-Fly Data Augmentation for Brain Tumor Segmentation [https://arxiv.org/html/2509.24973v1]
- 61. Multi channel fusion diffusion models for brain tumor MRI ... [https://www.nature.com/articles/s41598-025-06529-1]
- 62. Machine learning for medical imaging [https://www.nature.com/articles/s41746-022-00592-y]
- 63. Error Correlation in 2D Brain Tumor Segmentation [https://arxiv.org/abs/2510.15541]
- 64. Radiomics and Deep Learning in Brain Metastases [https://i-mri.org/DOIx.php?id=10.13104/imri.2021.25.4.266]
- 65. Automatic detection and multi-component segmentation of ... [https://www.nature.com/articles/s41598-024-78865-7]
- 66. Development and external validation of an MRI-based ... [https://www.sciencedirect.com/science/article/pii/S0167814022045625]
- 67. Impact of Tumour Segmentation Accuracy on Efficacy of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9601104/]
- 68. 联邦学习新突破:FeTS 2.0为胶质母细胞瘤术后分割设定金标准 [https://www.ebiotrade.com/newsf/2025-11/20251112083650659.htm]
- 69. The Multimodal Brain Tumor Image Segmentation Benchmark ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4833122/]
- 70. Brain Tumor Segmentation Cluster of Challenges (BraTS) [https://zenodo.org/records/13981216]
- 71. The 2024 Brain Tumor Segmentation (BraTS) Challenge [https://arxiv.org/html/2405.18368v1]
- 72. Metastases (BraTS-METS) 2025 Lighthouse Challenge ... [https://arxiv.org/abs/2504.12527]
- 73. ResSAXU-Net for multimodal brain tumor segmentation ... [https://www.nature.com/articles/s41598-025-09539-1]
- 74. Dice-Sørensen coefficient [https://en.wikipedia.org/wiki/Dice-S%C3%B8rensen_coefficient]
- 75. Intersection over Union (IoU): Definition, Calculation, Code [https://www.v7labs.com/blog/intersection-over-union-guide]
- 76. Hausdorff distance [https://cgm.cs.mcgill.ca/~godfried/teaching/cg-projects/98/normand/main.html]
- 77. sciencedirect.com/topics/computer-science/ hausdorff - distance [https://www.sciencedirect.com/topics/computer-science/hausdorff-distance]
- 78. A Study on the Performance Comparison of Brain MRI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12565000/]
- 79. A novel hybrid vision UNet architecture for brain tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12229522/]
- 80. A lightweight network for brain MRI segmentation [https://www.nature.com/articles/s41598-025-18062-2]
- 81. A review of deep learning for brain tumor analysis in MRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11698745/]
- 82. BRISC: Annotated Dataset for Brain Tumor Segmentation ... [https://arxiv.org/abs/2506.14318]
- 83. Ultra-High Resolution 9.4T Brain MRI Segmentation via a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12561009/]
- 84. FDA Oversight: Understanding the Regulation of Health AI Tools • Bipartisan Policy Center [https://bipartisanpolicy.org/issue-brief/fda-oversight-understanding-the-regulation-of-health-ai-tools/]
- 85. Artificial Intelligence-Enabled Medical Devices [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-enabled-medical-devices]
- 86. Cortechs.ai Announce Next-Gen NeuroQuant Brain Tumor [https://www.cortechs.ai/cortechs-ai-announce-next-gen-neuroquant-brain-tumor-ai-driven-metastasis-meningioma-segmentation/]
- 87. FDA Guidance on AI-Enabled Devices [2025] [https://www.greenlight.guru/blog/fda-guidance-ai-enabled-devices]
- 88. The illusion of safety: A report to the FDA on AI healthcare product approvals - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12140231/]
- 89. A real-world clinical validation for AI-based MRI monitoring ... [https://www.nature.com/articles/s41746-023-00940-6]
- 90. MRI Segmentation of the Human Brain: Challenges, Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4402572/]
- 91. 3D brain tumor segmentation in MRI images using ... [https://www.sciencedirect.com/science/article/pii/S2666521225001073]
- 92. 3D Slicer image computing platform | 3D Slicer [https://slicer.org/]
- 93. 3D Medical Imaging Software for Life Sciences [https://www.synopsys.com/simpleware/life-sciences.html]