AI-Driven Automated Perfusion Analysis in Acute Stroke: Revolutionizing Diagnosis, Treatment, and Clinical Research
This article provides a comprehensive analysis of the transformative role of Artificial Intelligence (AI) in automated perfusion analysis for acute ischemic stroke.
AI-Driven Automated Perfusion Analysis in Acute Stroke: Revolutionizing Diagnosis, Treatment, and Clinical Research
Abstract
This article provides a comprehensive analysis of the transformative role of Artificial Intelligence (AI) in automated perfusion analysis for acute ischemic stroke. Tailored for researchers, scientists, and drug development professionals, it explores the foundational principles of AI in stroke imaging, details the methodologies and clinical applications of leading software platforms, and addresses key challenges in optimization and integration. The scope extends to rigorous comparative validation of emerging AI tools against established standards, synthesizing evidence from recent multicenter studies and clinical trials. By examining the entire pipeline from image acquisition to outcome prediction, this review aims to inform the development of next-generation diagnostic tools and refine patient stratification for novel therapeutic interventions.
The Foundation of AI in Stroke Perfusion: Core Principles, Clinical Imperatives, and Workflow Integration
The management of acute ischemic stroke is governed by the fundamental principle that "time is brain," a concept which quantitatively establishes that 1.9 million neurons are lost each minute during untreated ischemia [1]. This paradigm underscores the irreversible nature of brain tissue damage as stroke progresses, creating a narrow therapeutic window for intervention. While this time-sensitive foundation has traditionally driven stroke systems of care, a significant evolution is underway—the augmentation of temporal urgency with advanced imaging precision [2].
The integration of artificial intelligence (AI) into acute stroke triage represents a transformative advancement, enabling both accelerated diagnostic pathways and sophisticated tissue viability assessment. AI-powered platforms now facilitate a paradigm that synergizes speed with imaging-based physiological evaluation, allowing for patient selection based on vascular and physiologic information rather than rigid time windows alone [2]. This application note details the protocols and analytical frameworks through which AI-driven automated perfusion analysis is reshaping acute stroke triage, providing researchers and drug development professionals with the methodological foundation for advancing this critical field.
Quantifying the Urgency: The Biological Imperative
The "Time is Brain" Equation
The original quantification of neural loss in acute ischemic stroke revealed the staggering pace of circuitry destruction, providing a biological rationale for emergent intervention. The foundational research calculated that during a typical large vessel supratentorial ischemic stroke:
Table 1: Quantified Neural Loss in Acute Ischemic Stroke [1]
| Neural Metric | Loss Per Hour | Loss Per Minute |
|---|---|---|
| Neurons | 120 million | 1.9 million |
| Synapses | 830 billion | 14 billion |
| Myelinated Fibers | 714 km (447 miles) | 12 km (7.5 miles) |
This neural loss occurs over an average stroke evolution duration of 10 hours, resulting in a typical final infarct volume of 54 mL [1]. When contextualized against normal brain aging, the ischemic brain ages 3.6 years each hour without treatment, emphasizing the profound impact of timely intervention [1].
Contemporary Stroke Burden and Access Disparities
The global burden of stroke continues to escalate, with recent epidemiological data revealing 11.9 million incident strokes annually worldwide [3]. This burden is disproportionately concentrated in low- and middle-income countries, which bear 87% of global stroke deaths and 89% of stroke-related disability-adjusted life years (DALYs) [3].
Geographic disparities in access to specialized stroke care present significant challenges to realizing the "time is brain" imperative. Recent spatial analyses demonstrate that approximately 20% of the U.S. adult population (49 million people) resides in census tracts beyond a 60-minute drive from advanced, endovascular-capable stroke care [4]. Critically, these underserved areas demonstrate significantly higher prevalence of stroke risk factors, including hypertension, diabetes, and coronary heart disease, creating a concerning mismatch between need and resource availability [4].
AI-Powered Perfusion Analysis: Technical Frameworks
Platform Architecture and Core Functions
AI-powered acute stroke triage platforms employ sophisticated computational architectures to automate the analysis of perfusion imaging. These systems function through multi-step analytical pipelines that transform raw imaging data into clinically actionable information.
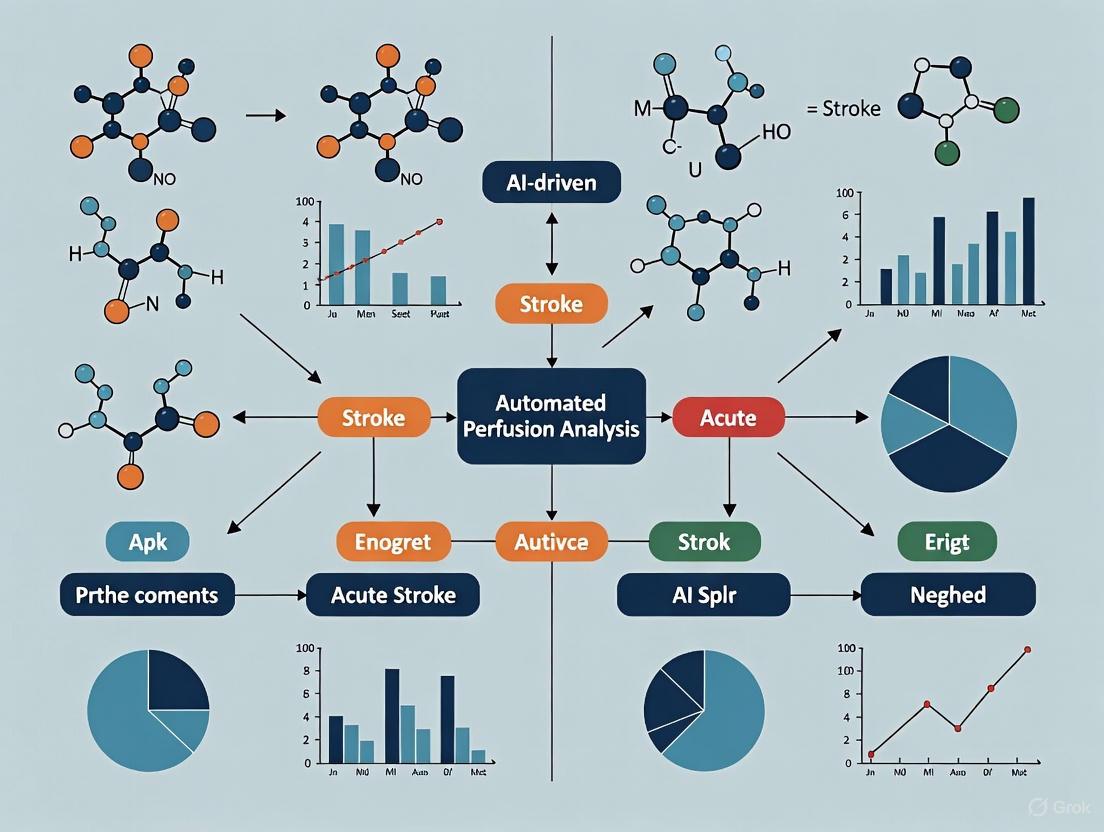
Figure 1: AI-Powered Perfusion Analysis Workflow
The workflow illustrates the transformation from raw imaging data to clinical decision support, emphasizing the automated processing steps that enable rapid triage. Platforms such as RAPID and JLK PWI implement variations of this pipeline, with specific methodological differences in algorithmic approaches to perfusion parameter calculation and threshold application [5].
Validation Framework for AI Perfusion Platforms
Rigorous validation of AI perfusion analysis tools requires standardized assessment protocols to establish diagnostic accuracy and clinical concordance. The following methodology, adapted from a recent multicenter comparative study, provides a template for platform evaluation:
Table 2: Core Validation Metrics for AI Perfusion Platforms [5]
| Validation Dimension | Quantitative Metrics | Statistical Methods | Acceptability Threshold |
|---|---|---|---|
| Volumetric Agreement | Ischemic core volume; Hypoperfused volume; Mismatch volume | Concordance correlation coefficient (CCC); Bland-Altman plots; Pearson correlation | Excellent agreement (CCC > 0.81) |
| Clinical Decision Concordance | EVT eligibility based on DAWN/DEFUSE-3 criteria | Cohen's kappa coefficient | Substantial agreement (κ = 0.61-0.80) |
| Technical Performance | Processing time; Success rate; Artifact resistance | Descriptive statistics; Failure rate analysis | >95% technical adequacy |
Experimental Protocol 1: Multicenter Platform Validation
Study Population: Recruit 250-300 patients with acute ischemic stroke who underwent perfusion imaging within 24 hours of symptom onset. Key inclusion criteria: clinical diagnosis of acute ischemic stroke, availability of quality perfusion imaging (PWI or CTP), and documented clinical outcomes.
Imaging Acquisition: Standardize imaging protocols across participating centers with documentation of scanner manufacturer, field strength, sequence parameters (TR/TE), and contrast administration protocols.
Parallel Analysis: Process all imaging studies through both reference (e.g., RAPID) and test (e.g., JLK PWI) platforms using standardized operating procedures.
Outcome Measures:
- Primary: Volumetric agreement for ischemic core and hypoperfused tissue
- Secondary: Concordance in endovascular therapy eligibility classification
- Exploratory: Correlation with 90-day functional outcomes (modified Rankin Scale)
Statistical Analysis Plan:
- Calculate concordance correlation coefficients (CCC) with 95% confidence intervals
- Generate Bland-Altman plots with limits of agreement
- Compute Cohen's kappa for categorical treatment decisions
- Perform subgroup analyses by stroke etiology, onset-to-imaging time, and imaging modality
This validation framework recently demonstrated excellent agreement between emerging and established platforms, with CCC values of 0.87 for ischemic core and 0.88 for hypoperfused volume, alongside substantial clinical decision concordance (κ = 0.76-0.90) [5].
Research Reagent Solutions: Essential Materials for AI Stroke Research
Table 3: Research Reagent Solutions for AI-Powered Stroke Investigation
| Category | Specific Solution | Function | Example Platforms |
|---|---|---|---|
| Imaging Analysis Software | Automated PWI/CTP processing | Quantifies perfusion parameters; delineates core/penumbra | RAPID, JLK PWI, Viz.ai, Aidoc |
| Clinical Decision Support | AI-powered triage platforms | Automates large vessel occlusion detection; facilitates care coordination | Viz.ai, RapidAI |
| Data Integration Tools | Interoperability frameworks | Enables PACS integration; supports DICOM standardization | Custom middleware solutions |
| Validation Datasets | Curated imaging libraries with reference standards | Provides ground truth for algorithm training/validation | Multicenter retrospective cohorts |
| Computational Infrastructure | High-performance computing resources | Supports deep learning model training/inference | Cloud-based GPU clusters |
The AI-powered acute stroke triage market reflects significant investment in these solutions, projected to grow from $1.72 billion in 2025 to $3.83 billion by 2029 at a compound annual growth rate of 22.2% [6]. Leading commercial platforms have demonstrated real-world impact, with implementation associated with reduced door-to-groine puncture times and improved coordination in hub-and-spoke networks [7].
Advanced Experimental Protocols
Protocol for Comparative Platform Assessment
Experimental Protocol 2: Methodological Framework for PWI Platform Comparison [5]
Image Preprocessing Standardization:
- Apply consistent motion correction algorithms to all dynamic susceptibility contrast-enhanced PWI data
- Implement automated brain extraction via skull stripping and vessel masking
- Normalize signal intensity curves across scanner platforms and magnetic field strengths
Perfusion Parameter Calculation:
- Employ automated arterial input function selection using standardized geometric criteria
- Apply block-circulant singular value decomposition for deconvolution operations
- Calculate quantitative maps for CBF, CBV, MTT, and Tmax using identical mathematical models across platforms
Tissue Classification Implementation:
- Apply consistent threshold for hypoperfused tissue definition (Tmax > 6 seconds)
- Implement platform-specific infarct core segmentation (ADC thresholding vs. deep learning approaches)
- Calculate mismatch ratio as (Hypoperfused Volume - Ischemic Core Volume) / Ischemic Core Volume
Validation Against Reference Standards:
- Compare volumetric outputs against manually segmented reference standards created by expert neuroradiologists
- Assess spatial overlap using Dice similarity coefficients in addition to volumetric correlations
- Evaluate clinical concordance using established trial criteria (DAWN, DEFUSE-3) as reference standard
This protocol recently demonstrated that emerging PWI analysis platforms can achieve excellent technical agreement (CCC = 0.87-0.88) and substantial clinical decision concordance (κ = 0.76-0.90) with established commercial systems [5].
Implementation Science Framework
Experimental Protocol 3: Health Systems Integration and Impact Assessment
Pre-Implementation Baseline Assessment:
- Establish baseline metrics for key stroke care time intervals (door-to-imaging, door-to-needle, door-to-puncture)
- Document existing workflow processes and identify potential bottlenecks
- Assess specialist availability and communication pathways between emergency departments, radiologists, and stroke neurologists
Staged Implementation Approach:
- Phase 1: Implement AI-powered automated detection with PACS integration
- Phase 2: Add automated notification systems to mobile devices and secure messaging platforms
- Phase 3: Integrate telemedicine capabilities for remote expert consultation
Outcome Measurement Framework:
- Primary effectiveness endpoints: time metrics for critical care pathway steps
- Secondary clinical endpoints: rates of intravenous thrombolysis and endovascular therapy, 90-day functional outcomes
- System efficiency endpoints: reduction in inter-facility transfer times, appropriate triage decisions
Economic Impact Assessment:
- Calculate operational costs associated with platform implementation and maintenance
- Measure resource utilization changes including length of stay and ICU days
- Assess cost-effectiveness through quality-adjusted life year (QALY) analysis
Real-world implementation of these systems has demonstrated meaningful improvements in workflow efficiency, with one study reporting significant reductions in inter-facility transfer times and hospital length of stay following AI coordination platform deployment [7].
The integration of AI-powered perfusion analysis into acute stroke triage represents a maturation of the "time is brain" paradigm, augmenting temporal urgency with precision imaging assessment. The experimental frameworks and validation methodologies detailed in these application notes provide researchers and drug development professionals with standardized approaches for advancing this rapidly evolving field. As the technology continues to develop, priorities include prospective multicenter validation, addressing algorithmic bias across diverse populations, and demonstrating cost-effectiveness across healthcare systems. Through rigorous implementation of these protocols, the stroke research community can further refine the synthesis of speed and precision that defines modern acute stroke care.
Perfusion is a fundamental biological function that refers to the delivery of oxygen and nutrients to tissue by means of blood flow at the capillary level [8]. Unlike bulk blood flow through major vessels, perfusion imaging captures hemodynamic processes at the microcirculatory level, providing critical insights into tissue viability and function [9]. In the context of acute ischemic stroke (AIS) and neuro-oncology, perfusion imaging has emerged as an indispensable tool for identifying salvageable brain tissue, guiding treatment decisions, and advancing therapeutic development.
The transition from raw imaging data to quantitative perfusion maps relies on sophisticated tracer kinetic models and computational algorithms. With the advent of artificial intelligence (AI), this process is being transformed through automated analysis, enhanced accuracy, and reduced processing times. This article explores the fundamental principles, protocols, and emerging AI applications that are shaping the future of perfusion imaging in clinical research and drug development.
Physical Principles and Technical Foundations
Core Hemodynamic Parameters
Perfusion imaging quantifies three primary hemodynamic parameters that characterize tissue vascularity and function, as defined in the table below.
Table 1: Key Perfusion Parameters and Their Significance
| Parameter | Abbreviation | Units | Physiological Significance |
|---|---|---|---|
| Cerebral Blood Flow | CBF | mL/100g/min | Rate of blood delivery to capillary beds [8] [9] |
| Cerebral Blood Volume | CBV | mL/100g | Volume of flowing blood in capillary network [10] [9] |
| Mean Transit Time | MTT | seconds | Average time for blood to pass through tissue vasculature [10] [8] |
These parameters are interrelated through the central volume principle: CBV = CBF × MTT [9]. This relationship forms the mathematical foundation for calculating perfusion maps from tracer kinetics data.
Tracer Kinetic Models
The conversion of pixel intensity changes to quantitative perfusion maps relies on tracer kinetic modeling. Two primary approaches dominate clinical practice:
- Compartmental Models: These models describe contrast agent distribution between intravascular and extravascular compartments. The Patlak model quantifies blood volume and capillary permeability, assuming unidirectional transfer from intravascular to extravascular space [11].
- Deconvolution Methods: These approaches use arterial and tissue time-concentration curves to calculate the impulse residue function, which characterizes the tissue response to an ideal arterial bolus [11]. Deconvolution is particularly valuable for calculating perfusion despite variable arterial input functions.
The mathematical foundation for these models is represented in the following workflow:
Modality-Specific Imaging Approaches
Computed Tomography Perfusion (CTP)
CT perfusion imaging follows the tracer kinetic model using iodinated contrast agents. During a CTP study, dynamic CT scanning captures the first pass of contrast through cerebral vasculature, generating time-attenuation curves for each voxel [9] [11]. The fundamental equation relating signal intensity to contrast concentration is:
ΔHU(t) ∝ C(t)
where ΔHU(t) is the change in Hounsfield Units over time and C(t) is the tissue concentration of contrast agent [11].
Table 2: Typical CTP Acquisition Protocol for Acute Stroke
| Parameter | Specification | Rationale |
|---|---|---|
| Scanner Type | Multidetector CT (≥16-slice) | Adequate temporal and spatial resolution [11] |
| Contrast Volume | 40-50 mL | Sufficient bolus for first-pass kinetics [9] |
| Injection Rate | 4-6 mL/sec | Compact bolus for accurate parameter estimation [9] [11] |
| Temporal Sampling | 1 image/second for 45-60 seconds | Capture complete first-pass kinetics [9] |
| Coverage | 80-160 mm (depending on detector array) | Include major vascular territories [9] |
| Tube Parameters | 80 kVp, 100-200 mAs | Balance radiation dose and image quality [9] |
Magnetic Resonance Perfusion Imaging
MR perfusion encompasses three distinct techniques with different contrast mechanisms and applications:
Dynamic Susceptibility Contrast (DSC) MRI: Based on T2* susceptibility effects during the first pass of gadolinium-based contrast agents. The signal intensity follows the relationship: S(t) = S₀ · exp(-ΔR2(t)), where ΔR2 is the change in transverse relaxation rate proportional to contrast concentration [10] [8]. DSC-MRI is particularly valuable for brain tumors and cerebrovascular diseases.
Dynamic Contrast-Enhanced (DCE) MRI: Utilizes T1-weighted sequences to track contrast extravasation into the extravascular extracellular space. The signal change is proportional to contrast concentration: R1 = R10 + r1·C, where R1 is the longitudinal relaxation rate, R10 is the pre-contrast relaxation rate, r1 is the longitudinal relaxivity, and C is contrast concentration [8].
Arterial Spin Labeling (ASL): A completely non-invasive technique that uses magnetically labeled arterial blood water as an endogenous diffusible tracer [8]. ASL provides quantitative CBF measurements without exogenous contrast administration but has lower signal-to-noise ratio compared to contrast-based methods.
Table 3: Comparison of MR Perfusion Techniques
| Feature | DSC-MRI | DCE-MRI | ASL |
|---|---|---|---|
| Contrast Mechanism | T2*/T2 weighting | T1 weighting | Endogenous blood labeling |
| Contrast Agent | Gadolinium-based | Gadolinium-based | None |
| Primary Parameters | rCBV, rCBF, MTT | Ktrans, ve, vp | CBF |
| Key Applications | Tumor grading, stroke | Oncology, permeability assessment | Pediatric imaging, longitudinal studies |
| Strengths | High sensitivity to microvasculature | Quantifies permeability | Non-invasive, absolute quantification |
| Limitations | Susceptibility to leakage effects | Complex modeling | Low signal-to-noise ratio |
Experimental Protocols and Methodologies
CT Perfusion Protocol for Acute Stroke
For acute ischemic stroke evaluation, CTP protocols prioritize rapid acquisition and processing to identify potentially salvageable tissue [9] [12]:
- Patient Preparation: Establish large-bore (18-gauge) intravenous access in antecubital vein.
- Baseline Imaging: Perform non-contrast head CT to exclude hemorrhage and establish anatomical reference.
- Scan Planning: Position CTP volume to include territories of anterior, middle, and posterior cerebral arteries.
- Contrast Administration: Inject 40 mL of non-ionic iodinated contrast (300-370 mgI/mL) at 4-5 mL/sec followed by saline flush.
- Image Acquisition: Initiate cine acquisition 5-7 seconds after injection start; acquire 4-8 slices every 1-2 seconds for 45-60 seconds.
- Post-Processing: Utilize deconvolution algorithms to generate CBF, CBV, and MTT maps with automated vessel identification.
MR Perfusion Protocol for Neuro-Oncology
Comprehensive brain tumor evaluation often combines DSC and DCE techniques to capture both vascularity and permeability characteristics [10] [13]:
- Patient Setup: Place 20-gauge or larger peripheral IV for power injector.
- Pre-Contrast Imaging: Acquire structural sequences including 3D T1-weighted GRE, T2-weighted, and FLAIR.
- DSC-MRI Acquisition:
- Use T2* weighted EPI sequence
- Inject 2/3 total contrast dose at 4-5 mL/sec 8-10 seconds after sequence start
- Apply flip angle of 30-35° to minimize T1 leakage effects
- Acquire 1.5-2 second temporal resolution for 60-90 seconds
- DCE-MRI Acquisition:
- Use 3D T1-weighted sequence
- Inject remaining 1/3 contrast dose at 2 mL/sec
- Acquire pre-contrast baseline with variable flip angles for T1 mapping
- Maintain 3-5 second temporal resolution during 5-10 minute acquisition
- Post-Contrast Imaging: Obtain high-resolution 3D T1-weighted images for anatomical reference.
The integration of these techniques is visualized in the following workflow:
AI-Driven Automation in Perfusion Analysis
Current AI Applications in Perfusion Imaging
Artificial intelligence is revolutionizing perfusion analysis through automated processing, enhanced accuracy, and novel approaches to data interpretation:
Fully Automated Processing: Commercial platforms like RAPID AI automatically coregister images, identify arterial input functions, generate parametric maps, and segment perfusion abnormalities based on validated thresholds (e.g., Tmax >6 seconds for critically hypoperfused tissue) [12]. These systems achieve sensitivity of 95.55% and specificity of 81.73% for detecting arterial occlusions in acute stroke [12].
Cross-Modality Prediction: Generative adversarial networks (GANs) can predict perfusion parameters directly from non-contrast CT images, potentially eliminating the need for dedicated perfusion studies. Recent studies demonstrate moderate performance (SSIM 0.79-0.83) in generating CBF and Tmax maps from NCHCT [14].
Workflow Integration: AI platforms like deepcOS integrate automated perfusion analysis directly into clinical workflows, providing processing in under three minutes with DEFUSE-3 criteria visualization for evidence-based treatment decisions [15].
Validation and Performance Metrics
AI algorithms for perfusion analysis require rigorous validation against ground truth measurements:
Table 4: Performance Metrics of AI-Based Perfusion Analysis Tools
| Metric | Current Performance | Validation Standard |
|---|---|---|
| Sensitivity for LVO Detection | 95.55% (CI: 93.50-97.10%) [12] | CTA-confirmed occlusion |
| Specificity for LVO Detection | 81.73% (CI: 75.61-86.86%) [12] | CTA-confirmed occlusion |
| Negative Predictive Value | 98.22% (CI: 97.39-98.79%) [12] | CTA as reference standard |
| SSIM for Synthetic CBF Maps | 0.79 (GAN-based prediction) [14] | Ground truth CTP |
| Processing Time | <3 minutes [15] | Manual processing (>10 minutes) |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of perfusion imaging protocols requires specific technical resources and analytical tools:
Table 5: Essential Research Resources for Perfusion Imaging Studies
| Resource | Specification | Research Application |
|---|---|---|
| CT Scanner | Multidetector (≥16 slices) with 0.5-1s rotation time | Adequate temporal resolution for tracer kinetics [11] |
| MRI System | 1.5T or 3T with high-performance gradients | DSC/DCE/ASL sequence implementation [10] [13] |
| Contrast Agent | Iodinated (370-400 mgI/mL) or Gadolinium-based | Optimal bolus characteristics for first-pass imaging [9] [11] |
| Power Injector | Dual-syringe with programmable rates | Precise bolus administration and saline flush [9] [13] |
| Post-Processing Software | RAPID, Olea, MITK, or custom algorithms | Parametric map generation and quantitative analysis [15] [12] |
| AI Platforms | deepcOS, mRay-VEOcore, custom neural networks | Automated analysis and cross-modality prediction [15] [14] |
Advanced Applications in Stroke Research and Drug Development
Perfusion imaging provides critical biomarkers for evaluating novel therapeutics in stroke and neuro-oncology:
Ischemic Penumbra Identification: CTP and MRP define the mismatch between critically hypoperfused tissue (Tmax >6 seconds) and the irreversibly injured core (CBF <30% normal or ADC reduction) [9] [12]. This mismatch identifies patients most likely to benefit from revascularization therapies beyond conventional time windows.
Treatment Response Assessment: In neuro-oncology, perfusion parameters (particularly rCBV) correlate with tumor grade, differentiate true progression from pseudo-progression, and provide early biomarkers of treatment efficacy [10] [8].
Clinical Trial Endpoints: Automated perfusion analysis enables standardized assessment of therapeutic efficacy across multiple centers, supporting drug development through quantitative imaging biomarkers [15] [12].
The integration of AI into the perfusion analysis pipeline creates new opportunities for research and drug development:
The management of acute ischemic stroke is a race against time, where every minute of delay results in the loss of nearly 1.9 million neurons [7]. Traditional neuroimaging modalities, while foundational to diagnosis, present significant limitations including processing delays, accessibility issues, and interpretive variability. The integration of Artificial Intelligence (AI), particularly deep learning, is fundamentally transforming this landscape by extracting nuanced, quantitative data from standard imaging studies that far surpasses human visual assessment capabilities [16].
This revolution is most evident in perfusion imaging analysis, where automated platforms now provide rapid, objective quantification of ischemic core, penumbra, and tissue-at-risk volumes. These AI-driven insights are crucial for extending treatment windows and personalizing therapeutic strategies, particularly for endovascular thrombectomy (EVT) [17]. This document provides detailed application notes and experimental protocols to guide researchers in implementing and validating these transformative technologies within acute stroke research programs.
Quantitative Performance Validation of Automated Perfusion Analysis Platforms
Table 1: Comparative Performance Metrics of RAPID and JLK PWI Platforms
| Performance Parameter | RAPID Platform | JLK PWI Platform | Validation Metrics |
|---|---|---|---|
| Ischemic Core Volume Agreement | Reference Standard | Excellent Agreement (CCC = 0.87) [17] | Concordance Correlation Coefficient (CCC), Pearson Correlation |
| Hypoperfused Volume Agreement | Reference Standard | Excellent Agreement (CCC = 0.88) [17] | Concordance Correlation Coefficient (CCC), Pearson Correlation |
| EVT Eligibility (DAWN Criteria) | Reference Classification | Very High Concordance (κ = 0.80 - 0.90) [17] | Cohen's Kappa |
| EVT Eligibility (DEFUSE-3 Criteria) | Reference Classification | Substantial Agreement (κ = 0.76) [17] | Cohen's Kappa |
| Primary Clinical Application | Triage for Thrompectomy | Reliable Alternative for MRI-based Perfusion [17] | Multicenter Retrospective Validation |
Key: CCC: Concordance Correlation Coefficient; EVT: Endovascular Therapy; κ: Kappa statistic for inter-rater reliability.
Experimental Protocol: Validation of an Automated PWI Analysis Pipeline
Study Population and Data Acquisition
- Patient Cohort: Recruit patients with acute ischemic stroke who underwent MR Perfusion-Weighted Imaging (PWI) within 24 hours of symptom onset. A typical cohort size is n=299, with a median NIHSS score of 11 [17].
- Inclusion Criteria: Confirmed acute ischemic stroke; availability of PWI and DWI sequences; known time of symptom onset.
- Exclusion Criteria: Significant motion artifacts; abnormal arterial input function; inadequate image quality [17].
- Imaging Parameters: Acquire Dynamic Susceptibility Contrast-enhanced PWI using a gradient-echo echo-planar imaging (GE-EPI) sequence. Standard parameters include [17]:
- Repetition Time (TR): 1,500–2,000 ms
- Echo Time (TE): 40–50 ms
- Field of View (FOV): 230 × 230 mm²
- Slice Thickness: 5 mm with no interslice gap
Automated Perfusion Processing Workflow
The following diagram illustrates the core computational pipeline for automated perfusion analysis.
Protocol Steps:
- Image Preprocessing: Export reconstructed images in DICOM format. Perform motion correction and apply brain extraction via skull stripping and vessel masking [17].
- Arterial Input Function (AIF) Selection: Automatically select the AIF and Venous Output Function (VOF), followed by conversion of the MR signal [17].
- Deconvolution and Map Calculation: Perform block-circulant singular value decomposition (SVD) to calculate quantitative perfusion maps, including [17]:
- Cerebral Blood Flow (CBF)
- Cerebral Blood Volume (CBV)
- Mean Transit Time (MTT)
- Time to maximum (Tmax)
- Ischemic Core and Mismatch Calculation:
- For RAPID: Ischemic core is estimated using ADC < 620 × 10⁻⁶ mm²/s [17].
- For JLK PWI: A deep learning-based algorithm segments the infarct core on b1000 DWI, which is then co-registered to the perfusion maps [17].
- The hypoperfused region is delineated using a threshold of Tmax > 6 seconds. The mismatch volume is computed as the difference between the hypoperfused volume and the ischemic core volume [17].
- Visual Inspection: Technically adequacy of all segmentations and resulting images must be confirmed by visual inspection before inclusion in the final analysis [17].
Statistical Analysis for Platform Validation
- Volumetric Agreement: Assess agreement for ischemic core, hypoperfused volume, and mismatch volume using Concordance Correlation Coefficients (CCC), Pearson correlation coefficients, and Bland-Altman plots [17].
- Clinical Decision Concordance: Evaluate agreement in EVT eligibility based on DAWN and DEFUSE-3 trial criteria using Cohen’s kappa (κ) [17].
- Interpretation of Agreement Statistics:
- CCC/Pearson: Values > 0.80 indicate excellent correlation.
- Kappa: < 0.20 (Poor); 0.21-0.40 (Fair); 0.41-0.60 (Moderate); 0.61-0.80 (Substantial); > 0.80 (Almost Perfect) [17].
Advanced AI Applications: Overcoming Specific Imaging Limitations
Generative AI for Cross-Modality Perfusion Prediction
A novel application of generative AI uses a modified pix2pix-turbo Generative Adversarial Network (GAN) to predict perfusion parameters like relative CBF (rCBF) and Tmax directly from non-contrast head CT (NCHCT) images [14]. This approach addresses the limitations of CT perfusion, including additional radiation exposure and processing delays.
Experimental Workflow for Generative AI Perfusion Mapping:
Performance Metrics: In a pilot study, GAN-generated Tmax maps achieved a Structural Similarity Index Measure (SSIM) of 0.827 and Fréchet Inception Distance (FID) of 62.21, demonstrating the feasibility of capturing key hemodynamic features from NCHCT [14].
Machine Learning for Stroke Sub-Type Identification in Resource-Limited Settings
In environments lacking advanced neuroimaging, ML frameworks can classify stroke type (ischemic vs. hemorrhagic) using clinical data alone.
Table 2: Performance of ML Framework for Stroke-Type Identification
| Metric | Performance | Context & Comparison |
|---|---|---|
| Weighted Accuracy | 82.42% | Trained on 2,190 patients with 79 clinical attributes [18] |
| Sensitivity | 82.19% | Ability to correctly identify true stroke types [18] |
| Specificity | 82.65% | Ability to correctly rule out non-existent stroke types [18] |
| F1-Score | 86.68% | Harmonic mean of precision and recall [18] |
| Prospective Validation | 16.42% improvement over Siriraj clinical score | Demonstrates real-world utility and generalizability [18] |
Key Methodology:
- Data Imputation: Employs Multiple Imputation by Chained Equations (MICE) to handle missing data robustly [18].
- Feature Reduction: Utilizes SHAP analysis to identify the 19 most significant clinical attributes, maintaining 82.20% accuracy with a reduced feature set [18].
- Bias Mitigation: Addresses class imbalance (70% Ischemic, 30% Hemorrhagic) by assigning equal weights to both classes during model training [18].
The Scientist's Toolkit: Essential Research Reagents & Software
Table 3: Key Research Reagents and Software Platforms for AI Stroke Research
| Item Name | Type | Primary Function in Research | Example Use Case |
|---|---|---|---|
| RAPID | Commercial AI Software | Automated processing of CTP and PWI to quantify ischemic core and penumbra [19]. | Triage for thrombectomy; core lab adjudication in clinical trials [17] [19]. |
| JLK PWI | Research AI Software | Automated PWI analysis pipeline for ischemic core estimation and hypoperfusion volume calculation [17]. | Comparative validation studies; MRI-based perfusion analysis [17]. |
| GAN (pix2pix-turbo) | Deep Learning Model | Generative network for cross-modality translation of NCHCT to synthetic perfusion maps [14]. | Exploring perfusion imaging in resource-limited settings; reducing radiation exposure [14]. |
| MICE Imputer | Statistical Algorithm | Handles missing data in clinical datasets for robust model training [18]. | Preprocessing of real-world, incomplete clinical stroke registries [18]. |
| SHAP Analysis | Explainable AI Tool | Identifies the most important clinical/model features driving predictions [18]. | Interpreting "black box" models; feature reduction for efficiency [18]. |
| DSC-PWI Sequence | MRI Protocol | Dynamic Susceptibility Contrast perfusion imaging for acquiring hemodynamic data [17]. | Generating ground truth perfusion maps for model training and validation [17]. |
Critical Analysis and Future Directions
While AI demonstrates remarkable performance, researchers must account for critical pitfalls. Dataset bias from single-institution data, temporal drift in clinical practices, and domain shifts across scanner vendors can severely limit model generalizability [20]. Furthermore, the explainability gap—the inability of many complex models to provide a rationale for their outputs—remains a significant barrier to clinical trust and adoption, especially in high-stakes decisions like thrombolysis eligibility [20].
Future research must prioritize:
- Multicenter Prospective Validation: Moving beyond retrospective studies to demonstrate real-world efficacy [7] [20].
- Explainable AI (XAI): Integrating attention maps and saliency features to align model outputs with clinical reasoning and build trust [20].
- Cross-Modality Fusion: Developing transformer-based networks and other advanced architectures to effectively integrate multimodal data (e.g., CT, MRI, clinical notes) for a more holistic patient assessment [16].
The integration of AI into acute stroke imaging is not about replacing clinicians but about providing powerful, objective tools that augment clinical decision-making. By standardizing assessments, compressing time-sensitive workflows, and revealing otherwise imperceptible diagnostic patterns, AI is fundamentally overcoming the long-standing limitations of traditional imaging and paving the way for more precise and accessible stroke care [7] [20].
Perfusion imaging has revolutionized treatment decisions in acute ischemic stroke (AIS), transitioning patient selection from a purely time-based paradigm to a more sophisticated tissue-based model. By quantifying the ischemic core (irreversibly injured tissue) and the hypoperfused penumbra (salvageable tissue), perfusion analysis enables clinicians to identify patients most likely to benefit from reperfusion therapies while avoiding harm in those with minimal potential for recovery. The integration of automated, artificial intelligence (AI)-driven perfusion analysis platforms has further standardized this assessment, facilitating rapid and evidence-based treatment decisions in time-sensitive scenarios. This application note delineates how perfusion analysis informs eligibility for intravenous thrombolysis (IVT) and endovascular thrombectomy (EVT), core pillars of acute stroke reperfusion therapy.
Clinical Application: Perfusion Analysis for Thrombolysis Decisions
Extending the Therapeutic Time Window
For patients presenting within the standard 4.5-hour time window, current guidelines do not mandate perfusion imaging for IVT eligibility. A recent retrospective analysis found that IVT was equally safe and effective in AIS patients without perfusion deficits on CT perfusion (CTP) as in those with perfusion deficits, suggesting limited clinical utility for routine CTP in early presenters [21]. However, perfusion imaging is crucial for patients presenting in extended or unknown time windows.
A 2025 systematic review and meta-analysis demonstrated that IVT in selected patients beyond 4.5 hours from last known well significantly improved excellent functional outcome (modified Rankin Scale [mRS] 0-1) at 90 days (RR=1.24; 95%CI:1.14–1.34) despite a higher rate of symptomatic intracerebral hemorrhage (sICH) (RR=2.75; 95%CI:1.49–5.05) [22]. This evidence supports the use of perfusion imaging to identify patients with favorable perfusion patterns who may benefit from late-window thrombolysis.
Predicting Hemorrhagic Transformation Risk
Beyond identifying salvageable tissue, perfusion parameters can help stratify the risk of hemorrhagic transformation (HT), a serious complication of IVT. Research has identified that the permeability surface area product (PS), a parameter reflecting blood-brain barrier disruption, is significantly elevated in patients who develop HT post-IVT [23].
A dynamic nomogram model integrating the National Institutes of Health Stroke Scale (NIHSS) score before IVT, atrial fibrillation (AF), and relative PS (rPS) achieved an area under the curve (AUC) of 0.899 (95% CI: 0.814–0.984) for predicting HT risk, providing a valuable tool for personalized risk assessment [23]. This allows clinicians to weigh the benefits of reperfusion against the risks of hemorrhage more accurately.
Table 1: Key Perfusion Parameters for Thrombolysis Decisions
| Parameter | Clinical Role | Interpretation | Evidence Source |
|---|---|---|---|
| Perfusion Deficit Presence | Identifies salvageable tissue (penumbra) in extended windows | Patients with targetable penumbra may benefit from IVT beyond 4.5 hours | Systematic Review/Meta-analysis [22] |
| Permeability Surface (PS) | Predicts hemorrhagic transformation risk | Higher values indicate blood-brain barrier disruption; elevated risk of post-thrombolysis hemorrhage | Retrospective Cohort [23] |
| Ischemic Core Volume | Estimates extent of irreversible injury | Larger core volumes may be associated with poorer outcomes and higher complication risks | Retrospective Analysis [21] |
Clinical Application: Perfusion Analysis for Thrombectomy Decisions
Standardizing EVT Eligibility with Automated Platforms
Perfusion imaging plays a critical role in patient selection for EVT, particularly in extended time windows (>6 hours from last known well). Automated software platforms utilize validated criteria from landmark trials (DAWN, DEFUSE-3) to standardize EVT eligibility assessment [5] [17]. These platforms automatically calculate key volumetric parameters, including ischemic core volume, hypoperfused volume (Tmax >6s), and mismatch ratio (penumbra/core), applying trial-specific thresholds to determine treatment candidacy.
A 2025 multicenter comparative validation study demonstrated that a novel AI-based perfusion-weighted imaging (PWI) software (JLK PWI) showed excellent agreement with the established RAPID platform for ischemic core volume (concordance correlation coefficient [CCC]=0.87) and hypoperfused volume (CCC=0.88) [5] [17]. The platforms showed very high concordance in EVT eligibility classification using DAWN criteria (κ=0.80–0.90) and substantial agreement using DEFUSE-3 criteria (κ=0.76) [5], supporting the use of automated platforms for reliable and reproducible EVT triage.
Expanding EVT to Large Core Infarctions
Historically, patients with large ischemic cores were excluded from EVT due to concerns about limited benefit and increased procedural risks. Recent trials have fundamentally changed this paradigm, showing that thrombectomy consistently improved functional outcomes in large core patients compared to medical management alone [24]. Perfusion imaging, particularly non-contrast CT Alberta Stroke Program Early CT Score (ASPECTS) and CTP core volume measurement, is essential for identifying appropriate candidates for large core thrombectomy.
While absolute functional independence rates (mRS 0-2) were lower than in trials enrolling patients with smaller cores, they still significantly favored thrombectomy, with no significant increase in rates of sICH [24]. This expansion of EVT eligibility underscores the critical role of precise perfusion imaging in identifying patients who may benefit from intervention despite extensive baseline infarction.
Table 2: Key Perfusion Parameters for Thrombectomy Decisions
| Parameter | Clinical Role | Interpretation | Evidence Source |
|---|---|---|---|
| Ischemic Core Volume | Quantifies irreversibly injured tissue | DEFUSE-3: <70 mL; DAWN: age/NIHSS-dependent thresholds | Comparative Validation [5] |
| Hypoperfused Volume (Tmax >6s) | Identifies total tissue at risk | Larger volumes indicate more extensive perfusion compromise | Comparative Validation [5] |
| Mismatch Ratio | Estimates penumbra relative to core | DEFUSE-3: Ratio ≥1.8; indicates sufficient salvageable tissue | Comparative Validation [5] |
| Mismatch Volume | Absolute volume of salvageable tissue | DEFUSE-3: Absolute penumbra volume ≥15 mL | Comparative Validation [5] |
Experimental Protocols for Perfusion Analysis
MRI Perfusion Analysis Protocol for EVT Triage
The following protocol is adapted from a 2025 multicenter validation study comparing perfusion software platforms [5] [17] [25].
Imaging Acquisition Parameters:
- Sequence: Dynamic susceptibility contrast-enhanced perfusion imaging using gradient-echo echo-planar imaging (GE-EPI)
- Scanner Field Strength: 3.0T (62.3%) or 1.5T (37.7%)
- Typical Parameters: Repetition time (TR)=1,500–2,000ms; Echo time (TE)=40–50ms; Field of view (FOV)=230×230mm²; Slice thickness=5mm with no interslice gap
- Coverage: Entire supratentorial brain with 17–25 slices
Image Processing and Analysis (JLK PWI Software):
- Preprocessing: Motion correction, brain extraction (skull stripping, vessel masking), MR signal conversion
- Perfusion Map Calculation: Automatic arterial input function (AIF) and venous output function selection, block-circulant single value deconvolution to generate quantitative maps (CBF, CBV, MTT, Tmax)
- Ischemic Core Delineation: Deep learning-based segmentation on b1000 DWI images using ADC < 620×10⁻⁶ mm²/s threshold
- Hypoperfused Tissue Definition: Tmax >6 seconds threshold
- Mismatch Calculation: Automated co-registration of diffusion and perfusion lesions with volumetric quantification
Validation Methods:
- Volumetric Agreement: Assessed using concordance correlation coefficients (CCC), Bland-Altman plots, and Pearson correlations
- Clinical Concordance: EVT eligibility classification based on DAWN and DEFUSE-3 criteria using Cohen's kappa
CTP Protocol for HT Risk Prediction Post-Thrombolysis
The following protocol is adapted from a 2025 study developing a nomogram for hemorrhagic transformation prediction [23].
CTP Acquisition Parameters:
- Scanner: 256-slice CT scanner
- Acquisition Parameters: 80kVp, 200mA, slice thickness=5mm, matrix=512×512mm, FOV=230mm×230mm
- Contrast Protocol: 40mL non-ionic contrast agent (Ioversol, 350mgI/mL) injected at 4mL/s followed by 30mL saline flush
- Scan Duration: 34 seconds with 20 cycles
Image Analysis Workflow:
- Processing: CTP images processed using CTP 4D software with anterior cerebral artery as input artery and superior sagittal sinus as outflow vein
- Parameter Calculation: Automated generation of CBV, CBF, MTT, TTP, Tmax, and PS maps
- ROI Placement: Regions of interest (10-15mm diameter) placed in ischemic lesion and mirrored to contralateral normal hemisphere
- Relative Parameter Calculation: rCBV, rCBF, rMTT, rTTP, rTmax, and rPS calculated as pathological-to-asymptomatic hemisphere ratios
- Model Development: Logistic regression analysis incorporating clinical (NIHSS, AF) and perfusion (rPS) parameters to create predictive nomogram
Visualization of Decision Pathways
The Scientist's Toolkit: Essential Research Reagents and Platforms
Table 3: Automated Perfusion Analysis Platforms for Stroke Research
| Platform/Software | Modality | Key Features | Research Applications |
|---|---|---|---|
| RAPID | CTP & PWI | FDA-cleared; DEFUSE-3/DAWN criteria automation; Ischemic core (ADC <620) & hypoperfusion (Tmax >6s) quantification | Reference standard for EVT trial eligibility assessment; Ischemic core volume estimation [5] [17] |
| JLK PWI | PWI | Deep learning-based infarct segmentation; Multi-step preprocessing pipeline; High concordance with RAPID (CCC=0.87-0.88) | Alternative for MRI-based perfusion analysis; EVT decision-making concordance studies [5] [17] [25] |
| mRay-VEOcore | CTP & PWI | Fully automated perfusion evaluation (<3 mins); DEFUSE-3 criteria visualization; Automated quality control | Rapid triage in extended time windows; CT/MRI perfusion studies with reduced radiation dose [15] |
| GE AW Workstation with CTP 4D | CTP | Vendor-specific processing; CBV, CBF, MTT, TTP, Tmax, PS mapping; ROI-based relative parameter calculation | Hemorrhagic transformation risk prediction; Permeability surface area product analysis [23] |
The integration of Artificial Intelligence (AI) into acute stroke care has created a transformative shift in diagnostic workflows, triage efficiency, and treatment decision-making. The U.S. Food and Drug Administration (FDA) has cleared a suite of AI-powered tools that automate the detection of intracranial hemorrhage (ICH), large vessel occlusion (LVO), and the quantification of early ischemic changes. These technologies, including platforms from industry leaders such as RapidAI, Brainomix, Aidoc, and Methinks AI, leverage non-contrast CT (NCCT), CT angiography (CTA), and perfusion imaging to provide real-time notifications to stroke teams. This application note details the regulatory-cleared landscape, providing researchers and drug development professionals with a structured overview of available tools, their validated performance metrics, and experimental protocols for their evaluation. This landscape is critical for framing research within the context of AI-driven automated perfusion analysis, ensuring that new methodologies are benchmarked against clinically adopted standards.
Acute ischemic stroke remains a leading cause of death and long-term disability worldwide, where rapid reperfusion is critical for salvaging brain tissue [14]. The advent of AI has addressed key bottlenecks in the stroke imaging workflow, which traditionally relied on expert human interpretation under significant time pressure. FDA-cleared AI tools now function as computer-aided triage (CADt) and notification systems, automatically analyzing images and prioritizing urgent cases, such as those with ICH or LVO, directly to clinicians' smartphones or worklists [26] [27].
The regulatory landscape for these tools has expanded rapidly. By mid-2025, the FDA had cleared approximately 873 AI algorithms for radiology, making medical imaging the single largest AI target among medical specialties [28]. These tools are predominantly based on convolutional neural networks (CNNs), which excel at pattern detection and classification tasks in medical images [28]. The clinical impact is measurable; for instance, the implementation of one AI platform (Viz.ai) has been associated with a 66-minute faster treatment time for stroke patients [28]. For research into AI-driven perfusion analysis, understanding this ecosystem of cleared devices is essential for contextualizing new developments against existing regulatory benchmarks and clinical practices.
FDA-Cleared AI Tools for Stroke: A Comparative Analysis
The following tables summarize key FDA-cleared AI tools for stroke triage and notification, their imaging modalities, primary functions, and reported performance metrics.
Table 1: AI Tools for Hemorrhage and Large Vessel Occlusion Detection
| AI Tool (Vendor) | FDA-Cleared Function | Imaging Modality | Key Performance Metrics |
|---|---|---|---|
| Brainomix 360 Triage ICH [26] | ICH Detection & Notification | Non-Contrast CT (NCCT) | Provides real-time alerts to clinician smartphones. |
| Methinks AI NCCT Stroke [29] | ICH & LVO Detection | Non-Contrast CT (NCCT) | Reduces false negatives by nearly 50% compared to existing NCCT triage tools; detects distal LVOs (e.g., MCA-M2). |
| Aidoc Stroke Package [27] | ICH & LVO Triage | NCCT and CTA | Reduces turnaround time for ICH by 36.6% (University of Rochester Medical Center study). |
| Rapid LVO [19] | LVO Detection | CT Angiography (CTA) | 97% Sensitivity, 96% Specificity for LVO detection. |
| Rapid NCCT Stroke [19] | Suspected LVO Detection | Non-Contrast CT (NCCT) | 55% increase in sensitivity for LVO; 18 minutes faster decision-making vs. no AI. |
| CINA-HEAD (Avicenna.AI) [30] | ICH Detection, LVO Identification, ASPECTS | NCCT and CTA | ICH Detection Accuracy: 94.6%; LVO Identification Accuracy: 86.4%. |
Table 2: AI Tools for Ischemic Core and Perfusion Analysis
| AI Tool (Vendor) | FDA-Cleared Function | Imaging Modality | Key Performance Metrics / Indications |
|---|---|---|---|
| Rapid Perfusion Imaging [19] | Ischemic Core & Penumbra Mismatch | CT Perfusion (CTP) | The only perfusion imaging solution cleared in the U.S. with a mechanical thrombectomy indication; used in pivotal trials (DAWN, DEFUSE 3). |
| Rapid ASPECTS [19] | Automated ASPECT Scoring | Non-Contrast CT (NCCT) | 10% improvement in reader accuracy; provides a standardized ASPECTS score in <2 minutes. |
| Rapid Hypodensity [19] | Quantification of Subacute Infarction | Non-Contrast CT (NCCT) | First and only solution to provide automated quantification of hypodense tissue. |
| mRay-VEOcore (mbits) [15] | Automated Perfusion Analysis (CE-Marked) | CT & MR Perfusion | Fully automated perfusion evaluation in under 3 minutes; visualizes DEFUSE-3 criteria. |
Detailed Experimental Protocols for AI Tool Validation
For research and development professionals, understanding the methodologies used to validate these AI tools is critical for designing comparative studies and evaluating new algorithms. The following protocols are synthesized from recent multicenter studies.
Protocol 1: Multi-step Stroke Imaging Performance Evaluation
This protocol is based on a multicenter diagnostic study evaluating an AI tool with multiple modules [30].
- 1. Study Design: Retrospective, multicenter cohort study.
- 2. Patient Population:
- Inclusion: Patients with NCCT and/or CTA scans acquired for suspicion of acute stroke.
- Exclusion: As defined by the study, typically including severe motion artifacts or inadequate image quality.
- Sample Size: 405 patients (373 NCCT, 331 CTA) from two university hospitals.
- 3. Ground Truth Definition:
- Expert evaluations from a panel of four neuroradiologists, who reviewed images independently or by consensus to establish the reference standard for ICH presence, LVO location, and ASPECTS scores.
- 4. AI Tool Analysis:
- The AI software (e.g., CINA-HEAD) processes the NCCT datasets to flag ICH and calculate ASPECTS.
- The AI processes the CTA datasets to identify LVO.
- 5. Outcome Measures & Statistical Analysis:
- Primary Outcomes: Diagnostic accuracy, sensitivity, specificity, with 95% confidence intervals for ICH detection and LVO identification.
- ASPECTS Analysis: Region-based accuracy and dichotomized ASPECTS classification (e.g., ≥6 vs. <6) accuracy.
- Statistical Tests: Calculation of intraclass correlation coefficients (ICC) for ASPECTS agreement.
Protocol 2: Comparative Validation of Automated Perfusion Analysis Platforms
This protocol is adapted from a study comparing a new perfusion software (JLK PWI) against the established RAPID platform [5]. It serves as a model for benchmarking new perfusion analysis tools.
- 1. Study Design: Retrospective, multicenter study.
- 2. Patient Population:
- Inclusion: Patients with acute ischemic stroke who underwent MR perfusion-weighted imaging (PWI) within 24 hours of symptom onset.
- Final Cohort: 299 patients after exclusions for abnormal arterial input function or severe motion artifacts.
- 3. Imaging and Analysis:
- Image Acquisition: PWI performed on 1.5T or 3.0T scanners from multiple vendors (GE, Philips, Siemens).
- Central Analysis: All datasets underwent standardized preprocessing and normalization in a central image laboratory to minimize inter-scanner variability.
- Software Comparison: Each patient's dataset was processed through two software platforms:
- Reference Platform: RAPID (using ADC < 620 × 10⁻⁶ mm²/s for infarct core).
- Test Platform: JLK PWI (using a deep learning-based algorithm on DWI for infarct core and Tmax >6s for hypoperfusion).
- 4. Outcome Measures:
- Volumetric Agreement: Concordance correlation coefficients (CCC) and Bland-Altman plots for ischemic core volume, hypoperfused volume, and mismatch volume.
- Clinical Decision Concordance: Cohen’s kappa (κ) coefficient to evaluate agreement in endovascular therapy (EVT) eligibility based on DAWN and DEFUSE-3 trial criteria.
- 5. Data Interpretation:
- Agreement magnitude classified as poor (0.0-0.2), fair (0.21-0.40), moderate (0.41-0.60), substantial (0.61-0.80), and excellent (0.81-1.0).
Workflow and Logical Diagrams
The following diagram illustrates the integrated workflow of AI tools in an acute stroke pathway, from image acquisition to treatment decision.
This workflow demonstrates how AI tools process different imaging modalities in parallel to provide a comprehensive set of inputs that inform the final treatment decision.
The Scientist's Toolkit: Research Reagent Solutions
For researchers designing experiments in the field of AI-driven stroke analysis, the following table outlines essential "research reagents" – the key software platforms and data components required for robust study design and validation.
Table 3: Essential Research Reagents for AI-Driven Stroke Perfusion Analysis
| Research Reagent | Function in Experimental Protocol | Example in Use |
|---|---|---|
| Reference Standard Software | Serves as the benchmark for comparing new AI algorithms. Provides validated volumetric and clinical decision outputs. | RAPID software, central to DAWN and DEFUSE-3 trials, is used as a reference in comparative studies [5] [19]. |
| Curated Multicenter Imaging Datasets | Provides a diverse, real-world dataset for training and validating AI models. Essential for assessing generalizability. | Retrospective collections of NCCT, CTA, and CTP from multiple hospitals and scanner vendors [5] [30]. |
| Expert-Adjudicated Ground Truth | Establishes the reference standard for performance evaluation, against which AI output is measured. | Consensus readings from panels of expert neuroradiologists for ICH, LVO, and infarct core [30]. |
| Clinical Trial Criteria Frameworks | Translates imaging outputs into clinically actionable eligibility criteria, enabling validation of clinical utility. | Automated application of DAWN and DEFUSE-3 criteria to software outputs to determine EVT eligibility [5]. |
| Automated Perfusion Mapping Algorithms | Generates quantitative maps (CBF, CBV, MTT, Tmax) from raw CTP or PWI data, forming the basis for tissue classification. | JLK PWI and RAPID perfusion pipelines that deconvolve time-concentration data to create maps [5]. |
| Image Preprocessing & Normalization Tools | Standardizes images from different scanners and protocols, reducing variability and improving AI reliability. | Tools for motion correction, brain extraction, and signal conversion used prior to perfusion analysis [5]. |
AI Perfusion Platforms in Action: Methodologies, Algorithms, and Clinical Workflow Applications
The integration of advanced computational techniques is revolutionizing acute ischemic stroke (AIS) research and clinical care. Automated perfusion analysis has become indispensable for extending the treatment window for endovascular therapy (EVT), with algorithms now capable of quantifying ischemic core and penumbra volumes to guide patient selection [31] [5]. This evolution encompasses three fundamental computational approaches: traditional deconvolution methods that form the mathematical foundation of perfusion parameter calculation, deep learning networks that enable rapid image analysis and feature detection, and emerging generative artificial intelligence that can synthesize functional information from structural scans. The synergy of these techniques is creating a new paradigm in stroke imaging, moving beyond simple automation to providing previously unattainable diagnostic insights.
Deconvolution techniques provide the mathematical backbone for calculating hemodynamic parameters from time-resolved perfusion studies. These algorithms reverse the blurring introduced by the vascular system's impulse response, essentially solving the inverse problem to determine the underlying tissue perfusion characteristics [31] [5]. Deep learning architectures, particularly convolutional neural networks (CNNs) and object detection models like YOLO (You Only Look Once), have demonstrated remarkable capabilities in automating the detection of pathological features such as large vessel occlusions (LVOs) and medium vessel occlusions (MeVOs) [32] [19]. Most recently, generative AI approaches have emerged that can predict perfusion maps directly from non-contrast images, potentially bypassing the need for specialized perfusion imaging altogether [33]. Together, these technologies are creating increasingly sophisticated tools for quantifying salvageable brain tissue and optimizing treatment decisions in time-critical scenarios.
Core Algorithmic Frameworks and Methodologies
Deconvolution Fundamentals and Implementation
Deconvolution techniques operate on the fundamental principle of reversing a system's impulse response from the observed data. In perfusion imaging, this impulse response is represented by the vascular transport function, which describes how a contrast bolus is modified as it passes through the cerebral vasculature. The mathematical foundation relies on modeling the observed tissue contrast concentration time curve, ( C{tissue}(t) ), as the convolution of the arterial input function (AIF), ( C{arterial}(t) ), with the tissue residue function, ( R(t) ), scaled by cerebral blood flow (CBF): ( C{tissue}(t) = CBF \cdot C{arterial}(t) \otimes R(t) ) [5]. Deconvolution solves for CBF and R(t) to derive critical perfusion parameters.
In clinical practice, several deconvolution algorithms are employed, each with distinct advantages and limitations. Block-circulant singular value decomposition (cSVD) is widely implemented in commercial software like RAPID and Viz CTP due to its robustness to delay and dispersion effects commonly encountered in pathology [5]. The cSVD approach incorporates temporal delay insensitivity by creating a block-circulant matrix structure, making it particularly suitable for acute stroke applications where arrival time delays are expected in ischemic territories. Osemplar algorithms offer an alternative approach based on model-free deconvolution, but may be more sensitive to noise in low-signal conditions. Advanced implementations now incorporate bayesian methods and tikhonov regularization to stabilize solutions in regions with severely reduced perfusion, though these approaches may increase computational complexity [5].
Figure 1: Deconvolution Workflow in CT Perfusion Analysis
Deep Learning Architectures for Stroke Imaging
Deep learning approaches have dramatically expanded the capabilities of automated perfusion analysis, particularly through convolutional neural networks (CNNs) and specialized object detection architectures. The YOLO (You Only Look Once) family of models has demonstrated exceptional performance in real-time detection of acute ischemic stroke in magnetic resonance imaging [32]. A comparative evaluation of state-of-the-art versions found YOLOv11 achieved the highest mean average precision at IoU 0.5 (mAP@50) of 98.5%, with balanced precision (95.4%) and recall (96.6%) across multiple classes including Normal, PD-Patient, Acute Ischemic Stroke, and Control categories [32]. YOLOv12 performed comparably (mAP@50 98.3%) with slightly slower inference speeds, while YOLO-NAS offered the fastest processing (154 FPS) but lower precision (76.3%) [32].
These architectures employ sophisticated feature extraction mechanisms tailored to medical imaging challenges. YOLOv11 incorporates Cross Stage Partial Self-Attention (C2PSA) for enhanced feature propagation, allowing the model to maintain contextual relationships across image regions [32]. YOLOv12 integrates attention mechanisms such as Area Attention and Flash Attention to improve detection of subtle ischemic changes while maintaining near real-time inference speeds critical for emergency settings [32]. YOLO-NAS utilizes Neural Architecture Search (NAS) and quantization-aware modules to optimize the trade-off between detection performance and computational efficiency, making it particularly suitable for deployment on edge devices in resource-limited environments [32]. Specialized variants like TE-YOLOv5 have been developed specifically for stroke lesion detection in diffusion-weighted imaging (DWI), integrating Technical Aggregate Pool (AP) and Reverse Attention (RA) modules to boost performance in feature extraction and edge tracing for ill-defined lesion boundaries [32].
Generative AI for Cross-Modality Prediction
Generative artificial intelligence represents the cutting edge of perfusion analysis research, with demonstrated capabilities to synthesize functional information from structural scans. A groundbreaking approach utilizes a modified pix2pix-turbo generative adversarial network (GAN) to translate co-registered non-contrast head CT (NCHCT) images into corresponding perfusion maps for parameters including relative cerebral blood flow (rCBF) and time-to-maximum (Tmax) [33]. This cross-modality learning bypasses the need for actual CT perfusion imaging, potentially reducing radiation exposure, decreasing processing times, and expanding access to perfusion data in settings where dedicated CTP is unavailable.
In the pilot implementation, the GAN architecture was trained using paired NCHCT-CTP data with training, validation, and testing splits of 80%:10%:10% [33]. Quantitative performance assessment demonstrated that generated Tmax maps achieved a structural similarity index measure (SSIM) of 0.827, peak signal-to-noise ratio (PSNR) of 16.99, and Fréchet inception distance (FID) of 62.21, while rCBF maps showed comparable metrics (SSIM 0.79, PSNR 16.38, FID 59.58) [33]. These results indicate the model successfully captures key cerebral hemodynamic features from non-contrast images alone. The approach is particularly valuable for patients with contraindications to contrast administration or when traditional CTP provides limited diagnostic information due to technical factors or artifact.
Experimental Protocols and Validation Frameworks
Protocol: Multi-Center Software Validation Study
Objective: To evaluate the performance and clinical concordance of automated perfusion analysis software against established reference standards in acute ischemic stroke.
Patient Population:
- Inclusion: Patients with acute ischemic stroke presenting within 24 hours of symptom onset, confirmed large vessel occlusion on CTA or MRA, complete perfusion imaging (CTP or PWI), and baseline clinical documentation [5].
- Exclusion: Non-diagnostic perfusion studies, significant motion artifacts, posterior circulation strokes, or incomplete clinical/imaging data [31].
Imaging Protocol:
- Acquisition: CT perfusion studies should cover the entire supratentorial brain with standardized parameters (80 kVp, 150-200 mAs, 5-mm slice thickness). For PWI, utilize dynamic susceptibility contrast-enhanced imaging with parameters: TR=1500-2000 ms, TE=40-50 ms, FOV=230×230 mm², 5-mm slice thickness with no gap [5].
- Contrast Administration: Iohexol (350 mgI/mL) or gadoterate meglumine (0.5 mmol/mL) at 5-6 mL/s followed by 40 mL saline flush using a power injector [5].
Software Analysis:
- Process all studies through both reference (e.g., RAPID) and test software (e.g., JLK PWI, Viz CTP) [31] [5].
- Ensure consistent pre-processing including motion correction, brain extraction, and arterial input function selection.
- Generate core perfusion parameter maps: CBF, CBV, MTT, Tmax with standardized thresholds (CBF <30% for core, Tmax >6s for hypoperfusion) [31].
Outcome Measures:
- Primary: Volumetric agreement for ischemic core and hypoperfused tissue using concordance correlation coefficients (CCC), Pearson correlation, and Bland-Altman analysis [5].
- Secondary: Treatment eligibility concordance based on DAWN/DEFUSE-3 criteria assessed via Cohen's kappa coefficient [31] [5].
- Statistical Analysis: Classify agreement as poor (0.0-0.2), fair (0.21-0.40), moderate (0.41-0.60), substantial (0.61-0.80), or excellent (0.81-1.0) per Landis and Koch criteria [5].
Protocol: Generative AI Model Development and Testing
Objective: To develop and validate a generative AI model for predicting perfusion parameters from non-contrast CT images.
Data Curation:
- Retrospectively identify patients with paired NCHCT, CTA, and CTP studies performed for acute stroke evaluation [33].
- Apply exclusion criteria: significant motion artifacts, prior large territory infarction, intracranial hemorrhage, or poor image quality.
- Allocate data into training (80%), validation (10%), and testing (10%) sets maintaining case distribution balance [33].
Model Architecture:
- Implement a modified pix2pix-turbo generative adversarial network with U-Net generator and PatchGAN discriminator [33].
- Input: Co-registered NCHCT image slices with standard brain windowing (80/40 HU).
- Output: Synthetic perfusion maps for rCBF and Tmax parameters.
Training Protocol:
- Pre-processing: Normalize image intensities, resample to isotropic resolution (1mm³), and augment data with random rotations (±5°), translations (±10 pixels), and intensity variations (±10%) [33].
- Loss Function: Combine adversarial loss, L1 distance, and perceptual loss with weighting factors 1:100:10 respectively.
- Optimization: Use Adam optimizer with initial learning rate 2×10⁻⁴, batch size 8, trained for 200 epochs with early stopping [33].
Validation Framework:
- Quantitative Metrics: Calculate structural similarity index (SSIM), peak signal-to-noise ratio (PSNR), and Fréchet inception distance (FID) against ground truth CTP maps [33].
- Clinical Validation: Assess concordance in identifying tissue-at-risk (Tmax >6s) and ischemic core (rCBF <30%) with board-certified neuroradiologist reads as reference standard.
- Statistical Analysis: Perform receiver operating characteristic analysis for detection of clinically significant perfusion deficits.
Performance Comparison and Clinical Validation
Quantitative Software Performance Metrics
Table 1: Performance Comparison of Automated Perfusion Analysis Platforms
| Software Platform | Ischemic Core Volume Concordance (CCC) | Hypoperfused Volume Concordance (CCC) | EVT Eligibility Agreement (κ) | Processing Time |
|---|---|---|---|---|
| RAPID (Reference) | 0.87 [5] | 0.88 [5] | 0.96 (DAWN) [31] | <5 minutes [19] |
| Viz CTP | 0.96 [31] | 0.93 [31] | 0.96 (DAWN) [31] | <5 minutes [31] |
| JLK PWI | 0.87 [5] | 0.88 [5] | 0.80-0.90 (DAWN) [5] | Not specified |
| Generative AI (NCHCT) | SSIM: 0.79-0.83 [33] | SSIM: 0.79-0.83 [33] | Under investigation | <2 minutes [33] |
Table 2: Deep Learning Model Performance for Acute Ischemic Stroke Detection
| Model Architecture | Precision (%) | Recall (%) | mAP@0.5 (%) | Inference Speed (FPS) |
|---|---|---|---|---|
| YOLOv11 | 95.4 [32] | 96.6 [32] | 98.5 [32] | 142 [32] |
| YOLOv12 | 95.2 [32] | 96.0 [32] | 98.3 [32] | 138 [32] |
| YOLO-NAS | 76.3 [32] | 87.5 [32] | 92.1 [32] | 154 [32] |
| TE-YOLOv5 | 81.5 [32] | 75.8 [32] | 80.7 [32] | Not specified |
Clinical validation studies demonstrate that automated software platforms show excellent agreement in critical decision-making parameters. In a direct comparison of 46 patients, RAPID and Viz CTP showed almost perfect agreement for EVT eligibility by DAWN criteria (κ=0.96) with no significant difference in final treatment decisions [31]. Similarly, a multicenter study of 299 patients found JLK PWI demonstrated excellent agreement with RAPID for both ischemic core (CCC=0.87) and hypoperfused volume (CCC=0.88) measurements [5]. These results confirm that well-validated automated platforms can be used interchangeably in clinical workflows without affecting treatment eligibility for the majority of patients.
The implementation of these AI-driven solutions has demonstrated tangible improvements in clinical workflows. Institutions utilizing the RAPID platform have reported an 18-minute faster time-to-decision, 51% increase in mechanical thrombectomy procedures post-implementation, and 35 minutes saved with direct-to-angio suite patient routing [19]. These workflow optimizations are clinically significant, as reduced time to treatment directly correlates with improved functional outcomes in acute ischemic stroke.
Integration Framework for Clinical Deployment
Figure 2: Integrated AI-Driven Stroke Imaging Workflow
Research Reagent Solutions and Computational Tools
Table 3: Essential Research Tools for Algorithm Development in Perfusion Analysis
| Tool Category | Specific Solutions | Primary Function | Application Context |
|---|---|---|---|
| Commercial Perfusion Software | RAPID (RAPID AI), Viz CTP (Viz.ai), JLK PWI (JLK Inc.) | Automated processing of CTP/PWI studies with core/penumbra quantification | Clinical trial patient selection, routine stroke care [31] [5] [19] |
| Deep Learning Frameworks | YOLO architectures (v11, v12, NAS), CNN models (ResNest, U-Net) | Real-time detection of ischemic changes, segmentation of pathology | Research prototyping, algorithm development [32] [33] |
| Generative AI Models | Modified pix2pix-turbo GAN, Diffusion Models | Cross-modality prediction of perfusion maps from non-contrast images | Resource-limited settings, contrast contraindication research [33] |
| Validation Datasets | REFINE SPECT Registry, Multi-center stroke imaging cohorts | Model training, benchmarking, and validation | Algorithm validation, performance comparison [5] [34] |
The deployment of these computational tools requires careful consideration of integration frameworks and validation protocols. Commercial platforms like RAPID and Viz CTP have established regulatory clearance and are integrated with hospital PACS systems, enabling seamless implementation into clinical workflows [19]. For research implementations, the use of standardized metrics (SSIM, PSNR, FID for generative models; CCC and kappa for clinical concordance) ensures comparable results across institutions [5] [33]. The emerging trend toward holistic AI analysis that incorporates extra-cerebral findings and clinical parameters demonstrates the evolution from purely imaging-based assessment to comprehensive patient evaluation [34].
Future developments in this field will likely focus on enhanced generalization across imaging protocols and scanners, refined detection of medium vessel occlusions, and more sophisticated integration of non-imaging clinical data. The demonstrated feasibility of generating perfusion information from non-contrast studies suggests a potential paradigm shift in stroke imaging workflows, particularly in resource-limited settings. As these algorithms continue to evolve, maintaining rigorous validation standards and clinical correlation will be essential to ensuring their safe and effective implementation in patient care.
The management of acute ischemic stroke has been revolutionized by the transition from a "time window" to a "tissue window" paradigm, guided by advanced neuroimaging. Artificial intelligence (AI) driven automated perfusion analysis platforms are central to this shift, enabling rapid, standardized identification of salvageable brain tissue (penumbra) and irreversibly injured tissue (core infarct). These tools provide critical, quantitative data for patient selection in endovascular thrombectomy (EVT), particularly in extended time windows up to 24 hours after symptom onset [35] [36]. This application note provides a detailed technical comparison of four prominent AI perfusion platforms—RAPID, JLK PWI, UGuard, and mRay-VEOcore—framed within the context of their capabilities for supporting rigorous clinical research and drug development.
Platform Technical Specifications and Workflows
Core Technical Capabilities
The following table summarizes the key technical specifications, imaging modalities, and primary outputs of the four platforms, highlighting their roles in acute stroke assessment.
Table 1: Core Technical Capabilities of Automated Perfusion Analysis Platforms
| Platform | Primary Imaging Modality | Core Analysis Outputs | Key Technical Features | Research Context |
|---|---|---|---|---|
| RAPID | CTP, MR-PWI | Ischemic core volume (rCBF<30%), Penumbra volume (Tmax>6s), Mismatch Ratio [19] [36] | Delay-insensitive deconvolution algorithm; automated AIF/VOF selection; integrated scan quality controls [19] [36] | Gold standard in DAWN/DEFUSE-3 trials; FDA-cleared; used in >75% of US Comprehensive Stroke Centers [19] |
| JLK PWI | MR-PWI, DWI | Ischemic core (Deep Learning on DWI), Hypoperfused volume (Tmax>6s), Mismatch volume [5] [37] | Deep learning-based infarct segmentation on b1000 DWI; automated pre-processing & perfusion parameter pipeline [5] | Demonstrates excellent concordance with RAPID for volumetric measures and EVT eligibility (κ=0.76-0.90) [5] [37] |
| UGuard | CTP | Ischemic Core Volume (rCBF<30%), Penumbra Volume (Tmax>6s) [38] | Machine learning algorithm; adaptive anisotropic filtering networks; deep convolutional model for artery/vein segmentation [38] | Strong agreement with RAPID (ICC ICV:0.92, PV:0.80); comparable predictive value for clinical outcome [38] |
| mRay-VEOcore | CTP, MR-PWI | Infarct core volume, Penumbra volume, Mismatch ratio, e-ASPECTS [39] [15] | Fully automated perfusion evaluation; includes quality control for patient motion/contrast issues; supports DEFUSE-3 criteria [39] | Enables rapid, evidence-based triage; integrated for real-time clinical collaboration via deepcOS platform [15] |
Platform Workflows
The following diagram illustrates the generalized operational workflow shared by automated perfusion analysis platforms, from image acquisition to treatment decision support.
Figure 1: Generalized AI Perfusion Analysis Workflow. This flowchart outlines the common steps from scan initiation to result dissemination, enabling rapid therapy decisions.
Experimental Validation and Performance Data
Comparative Validation Metrics
Validation against the reference standard, RAPID, is a common study design. The table below consolidates key quantitative performance metrics from recent comparative studies.
Table 2: Comparative Validation Metrics of Alternative Platforms vs. RAPID
| Performance Metric | JLK PWI (vs. RAPID) | UGuard (vs. RAPID) | mRay-VEOcore |
|---|---|---|---|
| Ischemic Core Agreement | CCC = 0.87 [5] [37] | ICC = 0.92 (95% CI: 0.89–0.94) [38] | Information Not Specified in Sources |
| Hypoperfused Volume Agreement | CCC = 0.88 [5] [37] | ICC = 0.80 (95% CI: 0.73–0.85) [38] | Information Not Specified in Sources |
| EVT Eligibility Concordance | DAWN Criteria: κ=0.80-0.90DEFUSE-3: κ=0.76 [5] [37] | Model with UGuard ICV/PV showed best predictive performance for favorable outcome [38] | Visualizes DEFUSE-3 inclusion criteria per ESO guidelines [39] |
| Sensitivity/Specificity | Information Not Specified in Sources | Specificity for outcome prediction higher than RAPID [38] | Fully automated evaluation in <3 minutes [39] |
Detailed Experimental Protocols
For researchers seeking to validate or utilize these platforms, understanding the underlying experimental methodology is crucial.
Protocol 1: Comparative Validation of Perfusion Software (Based on [5] [37])
- Study Design: Retrospective, multicenter cohort study.
- Population: 299 patients with acute ischemic stroke who underwent perfusion-weighted imaging (PWI) within 24 hours of symptom onset.
- Intervention: Each patient's imaging data was processed in parallel by the established RAPID software and the novel JLK PWI software.
- Primary Outcomes:
- Volumetric Agreement: Measured for ischemic core and hypoperfused volume using Concordance Correlation Coefficients (CCC) and Bland-Altman plots.
- Clinical Decision Concordance: Agreement on endovascular therapy (EVT) eligibility was assessed using Cohen's kappa (κ) statistic, based on the DAWN and DEFUSE-3 trial criteria.
- Statistical Analysis: CCC values >0.80 were considered "excellent." Kappa values were interpreted as: substantial (0.61–0.80) and almost perfect (0.81–1.00).
Protocol 2: Validating Automated ASPECTS Scoring (Based on [40] [41])
- Study Design: Retrospective, single-center blinded assessment.
- Population: 55 acute ischemic stroke patients with baseline non-contrast CT (NCCT) and follow-up MRI.
- Intervention: NCCT images were scored by the automated UGuard e-ASPECTS tool and by nine physicians of varying experience levels (residents, junior, senior).
- Reference Standard: The ASPECTS score on Diffusion-Weighted Imaging (DWI) from MRI, determined by expert consensus.
- Primary Outcomes:
- Diagnostic Accuracy: Sensitivity and specificity for identifying a large infarct core (ASPECTS < 6).
- Agreement with Ground Truth: Measured using Concordance Correlation Coefficient (CCC) and Bland-Altman plots.
- Processing Time: The time taken for assessment was recorded for both the device and human raters.
- Statistical Analysis: A non-inferiority test was used to compare the device's sensitivity and specificity to physician groups, with a margin of 0.1.
The Scientist's Toolkit: Research Reagent Solutions
For scientists designing studies in the field of AI-driven stroke imaging, the following table catalogs essential "research reagents" – the key software platforms and their functions within an experimental setup.
Table 3: Essential Research Reagents for AI-Driven Stroke Perfusion Studies
| Research Reagent | Function in Experimental Context | Key Characteristics for Study Design |
|---|---|---|
| RAPID | Reference Standard Platform | FDA-cleared; extensive historical trial data (DAWN, DEFUSE-3); considered the benchmark for validating new software or therapeutic interventions [19] [35] [36]. |
| JLK PWI | MRI-Specific Perfusion Analysis | Validated alternative for MR-based perfusion analysis; demonstrates high technical concordance with RAPID; suitable for studies prioritizing MRI's superior spatial resolution [5] [37]. |
| UGuard | CTP Analysis & Automated ASPECTS | Provides a validated alternative for CTP analysis with strong agreement on core/penumbra volumes; its integrated e-ASPECTS tool automates NCCT interpretation, reducing inter-rater variability [38] [40]. |
| mRay-VEOcore | Multi-Modality & Integrated Workflow | Enables rapid, standardized triage across both CT and MRI perfusion; its integration into clinical platforms (e.g., deepcOS) facilitates real-world evidence generation and workflow studies [39] [15]. |
| DAWN/DEFUSE-3 Criteria | Patient Stratification Algorithm | Standardized software-interpretable inclusion criteria for selecting late-window EVT candidates; essential for ensuring study population comparability to landmark trials [19] [5] [39]. |
The evolving landscape of AI-driven perfusion analysis offers researchers and clinicians multiple robust tools for quantifying tissue viability in acute stroke. RAPID remains the established benchmark, extensively validated in pivotal trials. However, the emergence of platforms like JLK PWI, UGuard, and mRay-VEOcore demonstrates that high technical and clinical concordance is achievable, fostering a competitive and innovative field. JLK PWI presents a strong alternative for MRI-centric protocols, UGuard shows compelling performance in CTP analysis and automated ASPECTS, and mRay-VEOcore offers flexibility across modalities with integrated workflow solutions. The choice of platform for clinical research or drug development should be guided by the imaging modality of choice, the need for integration into existing workflows, and the strength of validation evidence for the specific patient population of interest.
Application Notes
The integration of Artificial Intelligence (AI) into acute ischemic stroke care is advancing beyond the foundational assessment of ischemic core and penumbra. Modern AI-driven platforms now provide a multi-faceted imaging evaluation that encompasses large vessel occlusion (LVO) detection, automated ASPECTS scoring, and dynamic collateral assessment, offering a more comprehensive tool for patient stratification and treatment planning in both clinical and research settings [42] [19].
Table 1: Performance Metrics of Automated LVO Detection Platforms
| Platform / Tool | Reported Sensitivity | Reported Specificity | Key Functional Output | Impact on Workflow Time |
|---|---|---|---|---|
| Rapid LVO | 97% [19] | 96% [19] | Automated LVO notification & vessel density asymmetry [19] | 26% reduction in CTA-to-groin puncture time [19] |
| Viz.ai | N/A | N/A | AI-driven LVO detection with automated alerts & communication [43] | Significantly lesser CT scan to EVT time (SMD -0.71, p<0.001) [43] |
| Rapid CTA (Vessel Density) | N/A | N/A | Identifies area of occlusion & quantifies impacted vasculature [19] | 53% of MeVOs identified when combined with Rapid LVO [19] |
Table 2: Automated ASPECTS and Collateral Assessment Tools
| Tool | Primary Function | Key Performance / Utility | Modality |
|---|---|---|---|
| Rapid ASPECTS | Automated ASPECTS scoring | 10% improvement in reader accuracy; standardized score in <2 min [19] | NCCT |
| Rapid Hypodensity | Identifies & quantifies subacute infarction | First solution for automated quantification of hypodense tissue [19] | NCCT |
| Dynamic CTA (dCTA) Score | Qualitative collateral assessment from CTP source data | Superior prediction of infarct growth & final volume vs. single-phase CTA [44] | CT (CTA/CTP) |
| Rapid CTA (Vessel Density) | Automated collateral vessel assessment | Informs treatment and prognostic decisions via color-coded overlays [19] | CTA |
The implementation of these AI tools has demonstrated a significant, measurable impact on clinical workflows. A meta-analysis of the Viz.ai platform showed it was associated with a reduction in door-to-groin puncture time (SMD -0.50), CT-to-EVT start time (SMD -0.71), and door-in-door-out time (SMD -0.49) [43]. Similarly, the use of a direct-to-angiosuite pathway, facilitated by such technologies, has been reported to save a median of 35 minutes [19].
A critical advancement in collateral status evaluation is the shift from static single-phase CTA (sCTA) to dynamic CTA (dCTA) scoring using CT Perfusion (CTP) source images. One study found that the dCTA score frequently reclassified patients with "poor" collaterals on sCTA to "good" collaterals (n=23), while the reverse was rare (n=5) [44]. This dynamic assessment proved to be a more reliable predictor of tissue fate, showing a superior model fit (R² = 0.36 vs. 0.32) for core volume and a unique ability to significantly modify the association between core volume and time since stroke onset [44].
Experimental Protocols
Protocol 1: Validation of a Novel Perfusion Analysis Software
This protocol outlines a methodology for technically validating a new AI-based perfusion analysis platform against an established reference standard, as demonstrated in a comparative study of JLK PWI versus RAPID software [5].
- Objective: To evaluate the volumetric agreement and clinical decision concordance between a newly developed perfusion analysis software and an established platform.
- Patient Cohort: Retrospectively enroll patients with acute ischemic stroke who underwent perfusion-weighted imaging (PWI) within 24 hours of symptom onset. A typical cohort size is ~300 patients after exclusions for factors like motion artifacts or inadequate images [5].
- Image Acquisition: Perform MRI on 1.5T or 3.0T scanners. Use a dynamic susceptibility contrast-enhanced perfusion sequence with parameters: TR = 1,500–2,000 ms, TE = 40–50 ms, FOV = 230 × 230 mm², slice thickness of 5 mm with no gap [5].
- Software Analysis: Process all patient data through both the new and established software platforms. The analysis pipeline should include:
- Motion correction and brain extraction.
- Automated selection of arterial input function (AIF) and venous output function.
- Deconvolution and calculation of quantitative perfusion maps (CBF, CBV, MTT, Tmax).
- Infarct core estimation (e.g., via deep learning-based segmentation on DWI for JLK PWI, or ADC < 620 for RAPID) [5].
- Delineation of hypoperfused tissue (e.g., Tmax > 6s).
- Outcome Measures:
- Volumetric Agreement: Calculate concordance correlation coefficients (CCC) and generate Bland-Altman plots for ischemic core volume, hypoperfused volume, and mismatch volume [5].
- Clinical Concordance: Assess agreement in endovascular therapy (EVT) eligibility using Cohen’s kappa (κ), based on trial criteria such as DAWN (stratified by age and NIHSS) and DEFUSE-3 (mismatch ratio ≥1.8, core <70 mL, penumbra ≥15 mL) [5].
Protocol 2: Evaluating a Dynamic CTA Collateral Score
This protocol describes the development and validation of a qualitative dynamic CTA collateral score derived from CTP source images, providing a more robust prognostic tool than conventional single-phase CTA [44].
- Objective: To develop and validate a direct, qualitative dynamic CTA (dCTA) collateral score based on CTP source images without post-processing software.
- Imaging Protocol: Acquire a standardized imaging protocol within 8 hours of symptom onset, including non-contrast CT, single-phase CTA, and CTP with a z-axis coverage of at least 4 cm [44].
- Collateral Scoring:
- sCTA Score: Grade collaterals on a 4-point scale: 0 (absent), 1 (>0% but <50% filling), 2 (>50% but <100% filling), 3 (100% filling) [44].
- Novel dCTA Score: Grade collaterals on CTP source images using a 4-point subjective scale assessing collateral extension and speed of filling: 0 (poor extension, slow), 1 (poor extension, fast), 2 (good extension, slow), 3 (good extension, fast) [44].
- Image Analysis: Two blinded, experienced neuroradiologists should independently review images. CTP data should be post-processed to define the ischemic core (e.g., rCBF <40% & Tmax >2s) and hypoperfused tissue (Tmax >6s). Final infarct volume should be measured on follow-up NCCT at 24-72 hours [44].
- Statistical Analysis: Use linear regression to assess the association of sCTA and dCTA scores with CTP-derived volumes, infarct growth, and final infarct volume, adjusting for confounders like NIHSS and clot burden score. Test for interaction between collateral status and time since stroke onset [44].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential AI Software and Analysis Tools for Stroke Imaging Research
| Tool / Solution | Vendor / Developer | Primary Research Function | Key Differentiators / Technical Notes |
|---|---|---|---|
| RAPID | RapidAI [19] [5] | Integrated platform for CTP analysis, LVO detection, ASPECTS, and collateral assessment. | Gold standard in many trials; provides automated, quantified outputs for core, penumbra, and vessel status. |
| Viz.ai | Viz.ai [43] | AI-driven LVO detection platform with integrated communication tools for workflow optimization. | Focus on end-to-end workflow impact; facilitates real-time team coordination and transfer decisions. |
| JLK PWI | JLK Inc. [5] | Automated MRI perfusion analysis for infarct core and hypoperfusion volume estimation. | Employs a deep learning-based infarct segmentation algorithm on DWI; validated against RAPID. |
| mRay-VEOcore | mbits imaging [15] | Fully automated perfusion analysis for CT and MRI, visualizing DEFUSE-3 criteria. | Dual-modality support; includes quality control layers for motion/bolus issues; reduced radiation dose. |
| Olea Sphere | Olea Medical [44] | Software for post-processing CTP images, generating perfusion maps. | Utilizes a Bayesian deconvolution method for calculating perfusion parameters. |
Computed tomography perfusion (CTP) imaging is a cornerstone in the evaluation of acute ischemic stroke, vital for identifying candidates for mechanical thrombectomy in extended time windows [45]. However, inherent technical challenges such as high image noise, radiation dose considerations, and the limited availability of specialized perfusion scanners can restrict its utility [46] [47]. Consequently, a significant innovation frontier has emerged in the development of cross-modality artificial intelligence (AI) techniques that can generate critical perfusion information from routinely acquired non-contrast CT (NCCT) scans.
This Application Note details the protocols and validation metrics for a generative AI framework that synthesizes perfusion maps from NCCT. By leveraging the widespread availability of NCCT, this approach aims to make quantitative perfusion analysis accessible in diverse clinical settings, potentially accelerating treatment decisions and streamlining stroke research and drug development workflows.
Theoretical Foundation and Rationale
The scientific premise for deriving perfusion data from NCCT is rooted in the pathophysiological changes that occur in ischemic brain tissue. While NCCT is traditionally used to detect early ischemic signs like hypoattenuation and edema, these visible changes are the sequelae of underlying perfusion deficits [47] [48]. Generative AI models are trained to discern the subtle, sub-visual patterns in NCCT data that correlate with these hemodynamic disturbances.
A key theoretical insight underpinning this cross-modality approach is the profound influence of baseline image noise on the quality of derived perfusion maps. Research demonstrates that in both deconvolution- and non-deconvolution-based CTP systems, the noise in cerebral blood volume (CBV) maps is heavily dominated by the noise present in the pre-contrast baseline images [46]. This relationship is quantitatively expressed for non-deconvolution systems as:
σ²_CBV ≈ (κΔt/ρβ)² (Nσ² + N²σ_b²)
where σ²_b is the noise variance of the baseline image and carries a much greater weight than the noise of subsequent frames [46]. Therefore, methods that effectively enhance the NCCT data can directly and significantly improve the quality of perfusion-related outputs.
Furthermore, the ischemic core identified on NCCT as hypodense tissue largely reflects vasogenic edema, which develops 1-4 hours after stroke onset and indicates irreversibly damaged tissue [48]. Deep learning models can segment this hypodense core on NCCT with an accuracy non-inferior to expert neuroradiologists [48], providing a foundational element for more complex perfusion mapping.
Workflow and Algorithmic Framework
The process of generating perfusion maps from NCCT involves a sequential, multi-stage AI pipeline. The logical flow of data from input to final output is outlined below.
Workflow Diagram Explanation
The workflow begins with the acquisition of a standard NCCT scan. The image data first undergoes essential preprocessing, including motion correction, skull stripping, and intensity normalization, to standardize the input [5] [48]. A deep feature extraction module, typically a 3D Convolutional Neural Network (CNN), then analyzes the preprocessed volumes to identify complex, high-level patterns associated with perfusion abnormalities [48].
The extracted features feed into two parallel pathways:
- Ischemic Core Segmentation: This branch utilizes asymmetry analysis, comparing homologous regions in both brain hemispheres, to identify and segment the hypodense ischemic core [49] [48].
- Perfusion Map Synthesis: This branch employs a generative model, such as a Generative Adversarial Network (GAN), to synthesize pixel-wise maps of key perfusion parameters: Tmax, Cerebral Blood Flow (CBF), and Cerebral Blood Volume (CBV) [46].
The final output integrates the segmented core and synthesized perfusion maps to provide quantitative volumes and visualizations that support clinical decision-making, such as estimating the mismatch volume (penumbra) [45] [47].
Experimental Protocols and Validation
Model Training and Validation Protocol
Objective: To train and validate a generative AI model for synthesizing CTP maps from NCCT inputs. Dataset Curation:
- Source: Retrospective collection from multicenter clinical trials (e.g., DEFUSE 3) or large-scale hospital databases [48].
- Inclusion Criteria: Patients with acute ischemic stroke who underwent both NCCT and CTP (or MR-PWI) within a short time interval (e.g., <1 hour). CTP serves as the ground truth.
- Data Split: A minimum of 700 patients for training, 100 for validation, and 150 for testing is recommended [48].
- Ground Truth Definition: CTP maps processed by FDA-cleared software (e.g., RAPID) using validated thresholds: Core = relative CBF (rCBF) <30%; Penumbra = Tmax >6s [5] [45].
Training Procedure:
- Preprocessing: Apply spatial co-registration between NCCT and CTP maps. Normalize NCCT voxel intensities to a standard range (e.g., 0-100 Hounsfield Units).
- Architecture: Implement a 3D Conditional GAN (cGAN) or a U-Net-based architecture. The input is the NCCT volume, and the output is the synthetic CBF, CBV, and Tmax maps.
- Loss Function: Use a combined loss, e.g., L1 loss for voxel-wise accuracy and a perceptual loss to maintain structural consistency.
- Optimization: Train using the Adam optimizer with an initial learning rate of 1e-4, which is reduced upon plateau.
Performance Metrics: Table 1: Key Quantitative Metrics for Model Validation
| Metric | Formula/Description | Target Performance | ||||||
|---|---|---|---|---|---|---|---|---|
| Dice Similarity Coefficient (DSC) | ( DSC = \frac{2 | X \cap Y | }{ | X | + | Y | } ) where X and Y are segmented lesion volumes. | >0.45 vs. expert radiologists [48] |
| Surface Dice at 5mm | Measures overlap of lesion boundaries with a 5mm tolerance. | >0.46 [48] | ||||||
| Absolute Volume Difference (AVD) | ( AVD = | V{pred} - V{truth} | ) | <7.5 mL [48] | ||||
| Concordance Correlation Coefficient (CCC) | Measures agreement for continuous volumetric data (e.g., core volume). | >0.87 [5] |
Validation Against Clinical Endpoints
Objective: To ensure the synthetic perfusion maps yield clinically concordant treatment decisions. Protocol:
- Apply the trained model to an independent, held-out test set of NCCT scans from 200-300 patients [5].
- Use the synthetic maps to automatically calculate the ischemic core volume, hypoperfused volume (Tmax>6s), and mismatch volume [5].
- Determine endovascular thrombectomy (EVT) eligibility based on clinical trial criteria (DAWN and DEFUSE-3) [5] [45].
- Compare the EVT eligibility decisions derived from the AI-generated maps with those derived from the ground-truth CTP.
Success Criteria: Table 2: Clinical Decision Concordance Metrics
| Clinical Criteria | Definition | Target Agreement |
|---|---|---|
| DAWN Trial Criteria | Mismatch between clinical deficit (NIHSS) and core volume [45]. | Cohen's κ = 0.80 - 0.90 [5] |
| DEFUSE-3 Trial Criteria | Core <70 mL, mismatch ratio ≥1.8, and penumbra ≥15 mL [45]. | Cohen's κ ≥ 0.76 [5] |
| Ischemic Core Volume | Volume of tissue with rCBF <30%. | CCC > 0.87 [5] |
The Scientist's Toolkit
Table 3: Essential Research Reagents and Computational Solutions
| Item / Solution | Function / Explanation | Example Vendors / Platforms |
|---|---|---|
| Co-registered NCCT-CTP Datasets | Provides the essential paired data for training supervised generative AI models. Ground truth CTP should be processed with standardized software. | Internal hospital archives; Public trials data (e.g., DEFUSE 3) [48] |
| Automated Perfusion Analysis Software | Generates the ground truth perfusion maps and volumes from CTP source data using validated, consistent thresholds. | RAPID, JLK PWI [5] [45] |
| AI Model Development Platform | Offers the infrastructure for building, training, and validating complex 3D deep learning models. | TensorFlow, PyTorch |
| Integrated AI Deployment Platform | Enables seamless integration of validated models into clinical/research workflows without major IT disruption, facilitating real-world testing. | deepcOS [15] |
| Gaitboter Gait Analysis System | Provides multi-dimensional gait parameters that can be used with machine learning to assess stroke severity and motor outcomes, serving as a functional validation tool. | Institute of Computing Technology, Chinese Academy of Sciences [50] |
Generative AI for perfusion mapping from NCCT represents a paradigm shift in acute stroke imaging. By translating ubiquitous NCCT scans into quantitative, actionable perfusion data, this technology holds the potential to democratize advanced stroke care, enhance triage in resource-limited settings, and create consistent, automated biomarkers for clinical trials. The protocols outlined herein provide a foundational framework for researchers and industry professionals to rigorously develop, validate, and implement these innovative tools, ultimately contributing to improved outcomes for stroke patients worldwide.
The management of acute ischemic stroke (AIS) is a time-critical endeavor where rapid and accurate decision-making significantly influences patient outcomes. The integration of artificial intelligence (AI)-driven automated perfusion analysis into clinical pathways represents a transformative advancement, creating a seamless bridge from initial imaging to definitive intervention in the angio suite. This paradigm shift, embodied in direct-to-treatment protocols, leverages quantitative imaging biomarkers to expedite triage and treatment selection for patients with large vessel occlusion (LVO). The evolution of these integrated pathways is crucial for optimizing workflow efficiency, reducing door-to-recanalization times, and ultimately improving functional outcomes. This document details the application notes, experimental data, and procedural protocols that underpin the successful implementation of these advanced care pathways within the broader context of AI-driven acute stroke research.
Application Notes: AI and Workflow Integration
The Role of AI in Stroke Imaging Triage
Artificial intelligence tools have matured to provide comprehensive support across the stroke imaging cascade. Their integration is now recognized as a foundational element for certified stroke centers, as outlined by the American Heart Association (AHA) [51]. These tools offer a multi-faceted solution:
- Multi-Task Evaluation: Modern AI systems perform a sequential diagnostic cascade, including detection of intracerebral hemorrhage (ICH), identification of LVO, and automated calculation of Alberta Stroke Program Early CT Score (ASPECTS) [52]. This integrated performance is critical, as the accuracy of each step directly influences the next.
- Diagnostic Performance: In a study of 405 patients, an AI tool (CINA-HEAD) demonstrated an accuracy of 94.6% for ICH detection on non-contrast CT (NCCT) and 86.4% for LVO identification on CTA. The region-based ASPECTS analysis yielded an accuracy of 88.6% [52]. This high level of performance supports its use in rapid triage.
- Workflow Impact: A prospective evaluation within the Mayo Clinic Telestroke Network, while not showing statistically significant changes in primary outcomes, reported good user satisfaction and pointed towards potential reductions in time to treatment decisions for intravenous thrombolysis (IVT) [53].
Advanced CTP Analysis for Specificity in Infarct Detection
The reliability of CT perfusion (CTP) maps, particularly for small lacunar infarcts, has traditionally been a challenge due to variability in post-processing software. A 2025 study provides critical insights into the performance of different software packages [54].
Table 1: Specificity of CTP Software Packages in Patients with Negative Follow-Up DWI (n=58)
| Software and Settings | Median Ischemic Core Volume (mL) | Interquartile Range (IQR) | Specificity (True Negative) | Key Finding |
|---|---|---|---|---|
| Cercare Medical Neurosuite (CMN) | 0.0 | 0.0–0.0 mL | 57/58 (98.3%) | Zero infarct volume reported in 57/58 cases. |
| syngo.via (Setting A: CBV <1.2 mL/100mL) | 92.1 | Not Reported | 0/58 (0%) | Produced false-positive ischemic cores. |
| syngo.via (Setting B: Default + Filter) | Not Reported | Not Reported | 0/58 (0%) | Produced false-positive ischemic cores. |
| syngo.via (Setting C: rCBF <30%) | 21.3 | Not Reported | 0/58 (0%) | Still showed substantial overestimation (max 207.9 mL). |
This data underscores that advanced post-processing algorithms, such as the gamma distribution-based model used by CMN, can achieve high specificity in ruling out infarction. This is a vital characteristic for a CTP-based rule-out pathway, potentially reducing reliance on follow-up MRI and improving resource allocation [54].
Direct-to-Angiosuite and Hybrid Workflow Protocols
Bypassing the conventional emergency department (ED) workflow is a key strategy for time-saving. The Direct to Angiography Suite (DTAS) pathway, facilitated by hybrid CT-angio suites, has been shown to dramatically reduce time to treatment.
Table 2: Time Metric Comparison: Standard Workflow vs. Direct-to-Angiosuite (Simulation Study)
| Time Metric | Standard DTCT Workflow (min) | Direct DTAS Workflow (min) | P-value | Time Saved |
|---|---|---|---|---|
| Door-to-Puncture Time (Primary) | 39.83 (±4.36) | 22.17 (±2.4) | < 0.0001 | 17.66 minutes |
| Door-to-CT Start | 19.5 (±7.15) | 15.0 (±2.97) | 0.1848 | 4.5 minutes |
| CT-to-Puncture Time | 20.33 (±5.01) | 7.17 (±1.47) | 0.0009 | 13.16 minutes |
| CT-Complete to Puncture | 12.33 (±3.93) | 2.33 (±1.03) | 0.0011 | 10.00 minutes |
A prospective simulation study demonstrated that the DTAS workflow using a hybrid multidetector CT (MDCT)-angiography suite (Nexaris) significantly reduced the mean door-to-puncture time by over 17 minutes compared to the standard direct-to-ED-CT (DTCT) pathway [55] [56]. The most significant saving was in the "CT-to-Puncture" interval, which includes transfer and preparation time, highlighting the efficiency of a single-location workflow.
Early Specialist Involvement in the Treatment Pathway
Beyond technological and physical integration, human factor integration is equally critical. A retrospective study of 501 patients demonstrated that the early involvement of neuroendovascular interventionists from the point of patient arrival was associated with significantly improved outcomes [57].
- Outcome Improvement: The protocol group, with early specialist involvement, showed a higher frequency of favorable neurological outcomes (modified Rankin Scale 0-2) at discharge (44.4% vs. 31.9%; adjusted odds ratio: 2.92) [57].
- Time Savings: The protocol reduced door-to-needle time for IVT by 55.9 minutes and door-to-puncture time for EVT by 59.8 minutes [57]. This underscores the value of parallel processing and early decision-making by the treating physician.
Experimental Protocols and Methodologies
Protocol for Simulating and Timing Direct-to-Angiosuite Workflows
Objective: To quantitatively compare time metrics between standard (DTCT) and direct-to-angiosuite (DTAS) workflows for acute ischemic stroke thrombectomy [55] [56].
Materials:
- Medical mannequin simulating an AIS patient.
- Hybrid MDCT-angiography suite (e.g., Siemens Somatom Definition AS on rails with Artis Q biplane angiography).
- Standard ED CT scanner.
- Hospital electronic medical record (EMR) system for simulation.
Methodology:
- Study Design: A single-center, prospective, randomized, and blinded analysis. Twelve simulations are conducted (six per protocol).
- Scenario: All mock patients are LVO thrombectomy candidates (e.g., S-LAMS ≥4) with contraindications to thrombolysis.
- DTCT Workflow:
- EMS pre-notification and ED arrival.
- Triage, clinical assessment, and registration in the ED.
- Transfer to the ED CT scanner for NCCT and CTA.
- Image analysis and LVO confirmation by radiologist.
- Transfer from CT to the angiography suite.
- Preparation, sterilization, draping, and simulated groin puncture.
- DTAS Workflow:
- EMS pre-notification.
- Triage and clinical assessment in the ED.
- Direct transfer to the hybrid CT-angiography suite.
- NCCT and CTA performed on the rotational table in the angio suite.
- Image analysis and LVO confirmation.
- Table rotation to angiography position.
- Preparation and simulated groin puncture.
- Data Collection: Record all key timepoints (door, triage complete, CT start, CT complete, angio suite arrival, puncture). The primary endpoint is door-to-puncture time.
Protocol for Evaluating AI Perfusion Software Specificity
Objective: To assess the specificity of different automated CTP software packages in ruling out cerebral infarction, using follow-up DWI-MRI as the ground truth [54].
Materials:
- CTP datasets from patients with suspected AIS but negative follow-up DWI.
- CTP post-processing software (e.g., syngo.via VB60A, Cercare Medical Neurosuite v15.0).
- MRI scanners for DWI acquisition.
Methodology:
- Study Population: Consecutive patients with clinical suspicion of AIS, CTP acquisition prior to treatment, and follow-up MRI with DWI confirming no infarct. Exclude patients with severe motion artifacts, vessel occlusion on CTA, or chronic infarcts in the perfusion abnormality region.
- Imaging Acquisition: All CTP scans should be performed on the same scanner model with standardized parameters (e.g., kernel, contrast agent, injection rate).
- Image Post-Processing: Process all perfusion data using the software packages and settings under investigation.
- For syngo.via, include multiple settings: (A) CBV <1.2 mL/100mL, (B) default with smoothing filter, (C) rCBF <30%.
- The software should apply automated registration, segmentation, and motion correction.
- Ground Truth and Analysis: The reference standard is the absence of an acute infarct on follow-up DWI and FLAIR imaging.
- A false-positive CTP core is defined as a software-reported ischemic core volume >0 mL with no corresponding acute infarct on DWI.
- Two blinded neuroradiologists should independently review perfusion maps and MRI findings.
- Statistical Analysis: Report median and interquartile range (IQR) for core volumes. Calculate specificity as the proportion of true negatives (zero CTP core and zero DWI lesion) in the DWI-negative cohort.
Visualization of Integrated Pathways
The following diagrams illustrate the logical flow and key decision points in the advanced stroke pathways discussed.
Integrated AI Imaging Pathway
Direct-to-Angiosuite Workflow
Early Specialist Involvement Protocol
The Scientist's Toolkit: Research Reagents & Essential Materials
Table 3: Key Research Reagents and Technologies for Stroke Pathway Research
| Item / Technology | Function / Application in Research | Exemplary Product / Model |
|---|---|---|
| Hybrid MDCT-Angiography Suite | Enables DTAS workflow by combining diagnostic-quality CT imaging with interventional angiography in a single location, eliminating patient transfers. | Nexaris (Siemens Somatom Definition AS + Artis Q) [55] |
| Automated CTP Post-Processing Software | Provides quantitative maps of ischemic core and penumbra using advanced algorithms (e.g., delay-insensitive deconvolution, gamma model-based SVD). Critical for patient selection. | syngo.via CT Neuro Perfusion, Cercare Medical Neurosuite [54] |
| Multi-Task AI Imaging Software | Provides automated, sequential analysis of NCCT (for ICH), CTA (for LVO), and NCCT (for ASPECTS) to streamline the initial imaging triage process. | CINA-HEAD (Avicenna.AI) [52] |
| Medical Simulation Mannequin | Allows for realistic, prospective, and blinded timing studies of complex clinical workflows without risk to real patients. | Not specified (Generic medical mannequin) [55] |
| Flat-Panel CT (FPCT) | A technology available on modern angiographs for post-procedural imaging in the angio suite to detect complications (e.g., hemorrhage) and assess reperfusion. | Biplane Angiography System with FPCT capability [58] |
| Low-Field Portable MRI | A developing technology for neuroimaging in prehospital, hyperacute, or resource-limited settings to facilitate rapid stroke diagnosis. | Commercial systems in development [58] |
Optimizing AI Performance: Addressing Technical Challenges, Artifacts, and Workflow Bottlenecks
Computed Tomography Perfusion (CTP) is an indispensable tool in acute ischemic stroke research and drug development, enabling the quantification of the ischemic core and penumbra to identify patients who may benefit from reperfusion therapies. However, the reliability of automated, AI-driven perfusion analysis is fundamentally dependent on image quality and acquisition protocols. Technical pitfalls—specifically motion artifacts, suboptimal bolus timing, and contrast-related issues—can introduce significant variance, compromising data integrity and potentially skewing research outcomes. This document provides detailed application notes and experimental protocols to help researchers navigate these challenges, ensuring the high-quality data required for robust scientific inquiry and therapeutic development. The guidance is framed within the context of validating and utilizing AI-based perfusion analysis platforms, which are particularly sensitive to these input variables.
Motion Artifacts: Impact and Mitigation
The Challenge for Automated Analysis
Motion artifacts occur from patient movement during the CTP acquisition, which can last over 60 seconds. These artifacts distort time-attenuation curves, leading to inaccurate calculation of perfusion parameters such as Cerebral Blood Flow (CBF) and Time to Maximum (Tmax) [59]. For AI-driven software, which relies on precise voxel-wise data, motion can cause severe misclassification of the ischemic core and penumbra, resulting in false positives or negatives [45] [59].
Quantitative Impact on Research Data
A 2025 study assessed the specificity of two automated CTP software packages in patients with no confirmed stroke on follow-up MRI. The results, summarized in Table 1, highlight how software performance varies and can be adversely affected by data quality issues, including motion.
Table 1: Impact of Software and Artifacts on Ischemic Core Overestimation (n=58 patients with negative MRI)
| Software Package | Analysis Setting | Median False-Positive Core Volume (mL) | Specificity (Patients with 0mL Core) |
|---|---|---|---|
| Cercare Medical Neurosuite (CMN) | Model-based deconvolution | 0.0 | 98.3% (57/58) |
| syngo.via (Siemens) | A: CBV <1.2 mL/100mL | 92.1 | 0% |
| syngo.via (Siemens) | B: Default (A + smoothing filter) | Not Specified | 0% |
| syngo.via (Siemens) | C: rCBF <30% | 21.3 | Some patients (number not specified) |
The study noted that severe motion artifacts were grounds for exclusion, underscoring the necessity of mitigation protocols for reliable data [60].
Experimental Protocol: Mitigating Motion Artifacts
Aim: To establish a standardized pre-scanning procedure to minimize patient motion during CTP acquisition.
Materials:
- Immobilization devices: Head straps and foam padding.
- Radiographer checklist for patient preparation.
Method:
- Patient Preparation: Explain the critical importance of remaining still to the patient and any accompanying family members. Ensure the patient is as comfortable as possible before positioning.
- Head Immobilization: Securely place the patient's head in the head coil using a combination of foam padding and head straps. Avoid over-tightening for patient comfort.
- Comfort Measures: Provide a head support that allows the patient to relax their neck muscles. If possible, tilt the gantry to align with the orbitomeatal line, a more natural head position.
- Verification: The supervising radiologist or technician should confirm the stability of the setup before initiating the scan.
Integration with AI Workflow: As a critical quality control step, researchers should implement automated motion detection systems. Solutions like mRay-VEOcore incorporate quality control layers to flag studies with significant patient motion [15]. Any dataset flagged for motion should be scrutinized before inclusion in research analysis, as most post-processing software includes motion correction algorithms that may not fully restore data fidelity [5].
Bolus Timing: The Achilles' Heel of CTP Quantification
The Source of Variance
The arrival of the contrast bolus in the neurocranium is not uniform across patients. It is influenced by individual physiological factors such as cardiac output, which is often related to age and ejection fraction. CTA scans typically use bolus-tracking for optimal timing, but CTP scans are often initiated after a fixed delay (e.g., 5-10 seconds). This fixed delay can lead to bolus truncation, where the scan fails to capture the complete inflow and washout of the contrast agent, resulting in inaccurate perfusion maps [61] [45].
Quantitative Evidence of Timing Variance
A large retrospective study of 1,843 cases found substantial variances in contrast bolus arrival, which were strongly associated with patient factors [61]. A separate analysis of 2,624 perfusion scans confirmed these findings and further detailed the age-dependent nature of bolus arrival [62]. Key data is consolidated in Table 2.
Table 2: Factors Influencing Contrast Bolus Arrival Time
| Factor | Correlation with Bolus Peak Delay | Statistical Significance (p-value) | Source |
|---|---|---|---|
| Patient Age | Positive correlation (ρ = 0.334) | < 0.001 | [62] |
| Ejection Fraction | Negative correlation (r = -0.25) | < 0.001 | [61] |
| CTA Trigger Time | Positive correlation (r = 0.83) | < 0.001 | [61] |
| Bolus Peak Width | Positive correlation (r = 0.89) | < 0.001 | [61] |
The 2025 study concluded that using CTA timing information to adjust the CTP scan delay could significantly reduce the variance of the arterial input function (AIF) peak (p < 0.001) [61].
Experimental Protocol: Rule-Based Bolus Timing Optimization
Aim: To leverage timing data from a preceding CTA scan to determine a patient-specific delay for CTP initiation, thereby ensuring complete bolus coverage.
Materials:
- Integrated CTA/CTP stroke imaging protocol.
- DICOM header extraction tool or PACS with metadata viewing capability.
Method:
- Perform CTA with Bolus Tracking: Conduct the CTA scan as usual, using automated bolus tracking in the ascending aorta with a trigger threshold of 100 HU.
- Extract Timing Metadata: From the DICOM headers of the CTA scan, extract the
Contrast Bolus Start Timeand theAcquisition Timeof the first image. Calculate the patient's individual CTA Scan Delay. Scan Delay = (Acquisition Time of First CTA Image) - (Contrast Bolus Start Time) - Calculate Optimized CTP Delay: Apply a rule-based adjustment to determine the CTP start time. The study by Kasasbeh et al. suggests that the CTP delay can be derived from the CTA trigger time. A simplified approach is to set the CTP delay to be proportional to the observed CTA delay, ensuring the CTP scan starts sufficiently early to capture the bolus arrival in the brain.
- Implement and Acquire: Program the calculated, patient-specific delay into the CT scanner and initiate the CTP acquisition.
This protocol is summarized in the workflow below.
AI Research Implications: For researchers developing or validating AI perfusion models, consistent and complete bolus coverage is critical. Training models on data with truncated boluses will embed inaccuracies. Implementing this protocol ensures a higher quality, more consistent dataset for both model training and subsequent analysis in clinical trials.
Contrast Issues: Administration and Quality Control
Technical Pitfalls and Bolus Characteristics
Issues with contrast administration directly affect bolus geometry—its peak, width, and shape. Inadequate contrast concentration, slow flow rates, or suboptimal saline chaser volumes can lead to a diluted and dispersed bolus. This flattening of the time-attenuation curve reduces the contrast-to-noise ratio, making it difficult for AI algorithms to accurately calculate perfusion parameters [61] [45]. Furthermore, injecting via the left upper extremity can cause contrast reflux due to compression of the left brachiocephalic vein, stretching the bolus and degrading image quality [45].
Experimental Protocol: Standardized Contrast Administration
Aim: To achieve a compact, well-defined contrast bolus for consistent and reliable CTP data.
Materials:
- Power injector with dual-bore saline-chase injection pumps.
- High-concentration iodinated contrast agent (e.g., ≥350 mgI/mL).
- Large-bore (16-18G) intravenous catheter placed in the right antecubital vein.
Method:
- IV Access: Secure IV access in the right upper extremity to avoid potential venous compression [45].
- Contrast Injection: Use a power injector with the following parameters, which align with joint guidelines from ACR, ASNR, and SPR [45]:
- Volume: At least 40 mL (typical range 35-40 mL).
- Flow Rate: 5-6 mL/s for adults.
- Saline Chase: Immediately follow with a saline flush of at least 30-40 mL at the same flow rate to propel the entire contrast column into the central circulation [45].
- Quality Control: Monitor the arterial input function (AIF) and venous output function (VOF) curves generated by the post-processing software. A well-formed AIF curve should peak earlier and higher than the VOF curve. Automated QC software, like that in
mRay-VEOcore, can flag issues with bolus injection [15].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for High-Quality CTP Research
| Item | Specification / Function in Research |
|---|---|
| Power Injector | Dual-bore saline-chase capability. Ensures precise, reproducible contrast delivery, standardizing the bolus geometry across all subjects in a study. |
| Iodinated Contrast Agent | High concentration (≥350 mgI/mL). Provides the required attenuation change per unit time for robust signal-to-noise ratio in time-attenuation curves. |
| Large-Bore IV Catheter | 16-18G, placed in the right antecubital vein. Facilitates high flow rates and prevents bolus dispersion from venous compression. |
| Head Immobilization System | Foam padding and straps. Minimizes motion artifacts, a primary confounder in voxel-wise perfusion analysis. |
| AI-Powered QC Software | e.g., mRay-VEOcore, RAPID. Provides automated detection of technical failures (motion, bolus issues), ensuring only high-fidelity data is included in research analysis [15]. |
| DICOM Metadata Extraction Tool | Custom script or PACS feature. Enables the extraction of contrast timing data for implementing rule-based bolus timing protocols [61]. |
Integrated AI Research Workflow
The following diagram integrates the protocols for mitigating motion, optimizing timing, and standardizing contrast into a single, cohesive research workflow. This ensures that data input into AI analysis platforms is of the highest possible quality.
Technical pitfalls in CTP acquisition represent a significant source of error that can compromise the validity of acute stroke research, particularly with the increased reliance on automated AI analysis. By systematically addressing motion through immobilization protocols, personalizing bolus timing based on preceding CTA data, and standardizing contrast administration, researchers can significantly enhance data quality and reliability. The experimental protocols and materials detailed herein provide a actionable framework for generating robust, reproducible perfusion data, which is the foundation for meaningful scientific discovery and effective drug development in the field of acute ischemic stroke.
Computed tomography perfusion (CTP) plays a pivotal role in the evaluation of patients with suspected acute ischemic stroke, particularly for identifying candidates for mechanical thrombectomy within extended time windows [45]. The accurate interpretation of CTP is essential for optimal patient management, guiding decisions on reperfusion therapies by distinguishing the core infarct from the ischemic penumbra [45]. However, CTP performance varies significantly due to differences in patient characteristics, spatial/temporal resolution, and post-processing methods [60]. Artificial intelligence (AI) driven automated perfusion analysis has emerged as a valuable tool to support clinicians across the stroke workflow, improving inter-rater agreement and reducing interpretation time [52]. These systems provide a meaningful alternative to improve consistency in assessment, which is crucial given the moderate inter-rater agreement often observed in traditional evaluation methods influenced by factors such as reader experience and image quality [52]. This application note details protocols for implementing AI-based quality control flagging systems to automatically identify non-diagnostic perfusion studies, thereby enhancing the reliability of acute stroke research and drug development.
Performance Validation of AI in Stroke Imaging
Established Performance Metrics for AI Stroke Tools
Comprehensive validation studies demonstrate the reliable performance of AI-based imaging tools across the stroke diagnostic cascade. The evaluated AI tool (CINA-HEAD, Avicenna.AI) achieved 94.6% accuracy [95% CI: 91.8%-96.7%] for intracerebral hemorrhage (ICH) detection on non-contrast CT and 86.4% accuracy [95% CI: 82.2%-89.9%] for large vessel occlusion (LVO) identification on CTA [52]. In ASPECTS region-based analysis, the system yielded 88.6% accuracy [95% CI: 87.8%-89.3%], with the dichotomized ASPECTS classification (ASPECTS ≥6) achieving 80.4% accuracy [52]. This robust multi-stage evaluation supports the potential of AI systems for streamlining acute stroke triage and decision-making.
Comparative Performance of CTP Software Packages
Significant variability exists in the ability of different CTP software packages to reliably rule out small lacunar infarcts, which is crucial for minimizing false negatives in stroke detection [60]. The following table summarizes the specificity findings from a comparative study of two software packages in patients without evidence of stroke on follow-up diffusion-weighted imaging (DWI):
Table 1: Specificity Comparison of CTP Software Packages in Ruling Out Stroke
| Software Package | Specificity | Median Core Volume | Key Findings |
|---|---|---|---|
| Cercare Medical Neurosuite (CMN) | 98.3% (57/58 patients) | 0.0 mL (IQR 0.0-0.0 mL) | Highest specificity; minimal false positives |
| syngo.via Setting A (CBV <1.2 mL/100 mL) | Substantially lower | 92.1 mL | Significant false-positive ischemic cores |
| syngo.via Setting B (with smoothing filter) | Substantially lower | Not specified | Produced false-positive ischemic cores |
| syngo.via Setting C (rCBF <30%) | Substantially lower | 21.3 mL | Substantial overestimation (maximum 207.9 mL) |
This performance variability highlights the critical need for automated quality control systems that can flag non-diagnostic studies and identify software-related inaccuracies in perfusion analysis [60].
Experimental Protocols for AI Flagging System Validation
Ground Truth Establishment Protocol
Purpose: To establish reliable reference standards for training and validating AI-based quality control flagging systems.
Materials and Equipment:
- Non-contrast CT (NCCT) and computed tomography angiography (CTA) datasets from suspected stroke patients
- CTP datasets with corresponding follow-up DWI-MRI
- Expert neuroradiology panel (minimum 3 reviewers with 3-17 years of experience)
- AI processing tool (e.g., CINA-HEAD, Avicenna.AI)
Methodology:
- Retrospective Data Collection: Collect NCCT and/or CTA scans for suspicion of stroke consecutively over a defined period (e.g., 12 months) [52].
- Expert Consensus Evaluation: Three senior neuroradiologists jointly review each case simultaneously, agreeing on findings through discussion [52].
- Reference Standard Categorization:
- Evaluate presence of ICH on NCCT and categorize subtypes (IPH, IVH, SAH, SDH/EDH)
- Assess presence and location of LVO within proximal ICA, MCA-M1, or distal MCA-M2 segments on CTA
- Determine ASPECT score via visual assessment of early ischemic changes on NCCT images
- Use CTA to confirm infarct location when available [52]
- AI Processing: Process the same cases through the AI tool to flag ICH, LVO, and calculate ASPECTS [52].
- Discrepancy Resolution: An independent expert neuroradiologist reviews all cases to establish final ground truth, resolving discrepancies between consensus readings and AI outputs through majority agreement [52].
Quality Control Measures:
- Exclude cases with significant image artifacts, post-neurosurgery changes, or failed AI processing
- Ensure clinical history is accessible to evaluators when available
- Maintain blinding between different evaluation stages
CTP Specificity Assessment Protocol
Purpose: To evaluate the ability of CTP software to correctly exclude ischemia in patients without confirmed stroke.
Materials and Equipment:
- CTP datasets from patients with suspected acute ischemic stroke but negative follow-up DWI-MRI
- Multiple CTP post-processing software packages (e.g., syngo.via, Cercare Medical Neurosuite)
- MRI systems with DWI capability (1.5T or 3.0T)
- Standardized contrast injection protocols
Methodology:
- Patient Selection: Include consecutive patients with:
- Clinical suspicion of acute ischemic stroke
- CTP dataset acquired prior to treatment
- Follow-up MRI with DWI sequence confirming no infarct
- Mean delay of approximately 68 hours between CTP and MRI to minimize DWI-negative early scans [60]
- Exclusion Criteria: Apply the following exclusion criteria:
- Patients receiving intravenous thrombolysis between CTP and MRI
- Severe motion artifacts or poor scan quality on CTP or MRI
- Failed automated perfusion post-processing
- Evidence of chronic infarct on FLAIR/DWI in perfusion abnormality regions
- Vessel occlusion or stenosis on CT angiography [60]
- Image Acquisition: Perform all CTP scans on the same scanner model with standardized parameters:
- Kernel: T20F
- Contrast agent: Imeron 300
- Injection rate: 5 mL/s
- Acquisition start: 3 seconds after injection [60]
- Post-processing: Analyze all perfusion data using multiple fully automated software packages applying automated registration, segmentation, and motion correction [60].
- Outcome Measures:
- Define false-positive CTP core: automated CTP-identified ischemic core volume >0 mL with no corresponding acute infarct on follow-up DWI
- Define true negatives: no core on CTP and no lesion on DWI [60]
- Independent Review: Two neuroradiologists independently review each software's perfusion maps to verify presence/absence of core lesions and rule out matches with older tissue defects [60].
Implementation Workflow for Quality Control Flagging
The following diagram illustrates the integrated quality control workflow for AI-driven flagging of non-diagnostic perfusion studies:
AI Quality Control Workflow for CTP Studies
Flagging Criteria for Non-Diagnostic Studies
The following table details specific criteria for automated flagging of non-diagnostic perfusion studies:
Table 2: Automated Flagging Criteria for Non-Diagnostic Perfusion Studies
| Category | Specific Criteria | AI Assessment Method |
|---|---|---|
| Image Quality | Significant motion artifactsInadequate brain coverageSevere noise or artifacts | Image analysis algorithms detecting unnatural edge patterns, registration errors |
| Technical Adequacy | Poor contrast bolus (low peak, flat curve)Incorrect AIF/VOF selectionInsufficient temporal resolution | Analysis of time-attenuation curves; AIF should peak earlier and lower than VOF [45] |
| Perfusion Map Reliability | Mismatch volume calculations outside expected rangeInconsistent core-penumbra relationshipsASPECTS region analysis failures | Comparison to validated thresholds (e.g., Tmax >6s for hypoperfusion, rCBF <30% for core) [45] |
| Clinical Correlation | Discrepancy between clinical deficit and imaging findingsUnexpected perfusion patterns | Integration with clinical data and NCCT findings [45] |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials for AI Perfusion QC Validation
| Reagent/Material | Function/Application | Implementation Example |
|---|---|---|
| Percoll Density Gradients | Isolation of immune cells from brain tissue for flow cytometric analysis of post-ischemic neuroinflammation | Discontinuous (30/70%) Percoll gradients for leukocyte separation at interphase [63] |
| Collagenase/DNase Solutions | Tissue dissociation for viable immune cell yield in stroke immunology studies | Digestion buffers (DNase + collagenase I/II) for mechanical dissociation of brain tissue [63] |
| Flow Cytometry Antibody Panels | Immunophenotyping of immune cell subsets in stroke-induced neuroinflammation | Pre-determined antibody titrations specific for cell types; FC receptor blocking reagents to reduce false positives [63] |
| CTP Post-processing Software | Quantitative analysis of perfusion parameters for core-penumbra differentiation | Software employing delay-insensitive deconvolution models or gamma distribution-based residue functions [60] |
| Reference Standard Datasets | Ground truth establishment for AI training and validation | Retrospectively collected NCCT/CTA datasets with expert neuroradiologist consensus readings [52] |
Technical Integration and Color Mapping Specifications
The following diagram illustrates the logical relationships in AI-based perfusion analysis and flagging criteria:
AI Perfusion Analysis Logic and Color Compliance
Color Palette Implementation for Visualization
All diagrams and visualizations in this protocol adhere to the specified color palette to ensure sufficient contrast for interpretability while maintaining accessibility standards:
- Primary Action Nodes:
#4285F4(blue) for process steps with white text - Terminal/Decision Nodes:
#34A853(green) for start/pass states with white text;#EA4335(red) for fail/flags with white text - Informational Elements:
#FBBC05(yellow) for review steps with dark text - Background:
#F1F3F4(light gray) for overall background - Text and Borders:
#202124(near black) and#5F6368(dark gray) for optimal contrast
This implementation ensures sufficient color contrast ratios in accordance with WCAG 2.1 AA guidelines, requiring at least 4.5:1 for standard text and 3:1 for large text [64]. The selected palette provides clear visual differentiation between process states while maintaining accessibility for researchers with color vision deficiencies.
Computed tomography perfusion (CTP) is a critical tool for evaluating patients with suspected acute ischemic stroke (AIS), enabling rapid assessment of cerebral perfusion deficits and ischemic core volume [60]. However, its integration into AI-driven automated perfusion analysis for acute stroke research faces significant standardization challenges. The core dilemma lies in the substantial variation in CTP imaging protocols across different stroke centers and the fundamental differences in how vendor software packages process this data to estimate ischemic regions [65]. This variability directly impacts the consistency of scientific results and the validity of clinical guidelines derived from multicenter research [65]. For researchers, scientists, and drug development professionals, these inconsistencies present formidable hurdles in achieving reproducible, reliable results across studies and institutions, potentially compromising the development and validation of new therapeutic interventions.
Quantitative Evidence of Variability
Recent studies provide compelling quantitative evidence of the significant disparities in CTP analysis outputs between different software platforms and acquisition protocols.
Table 1: Specificity Comparison of CTP Software Packages in Excluding Stroke (n=58 patients with negative follow-up DWI-MRI) [60]
| Software Package | Specific Analysis Setting | Specificity | Median Reported Core Volume (mL) | Range of Reported Core Volumes (mL) |
|---|---|---|---|---|
| Cercare Medical Neurosuite (CMN) | Default Model-Based Algorithm | 98.3% (57/58 patients) | 0.0 | 0.0 - 4.7 |
| syngo.via (Siemens) | Setting A (CBV < 1.2 mL/100 mL) | Not Reported (False positives in all 58 patients) | 92.1 | Not Reported |
| syngo.via (Siemens) | Setting B (CBV < 1.2 mL/100 mL + Smoothing Filter) | Not Reported (False positives in all 58 patients) | 37.2 | Not Reported |
| syngo.via (Siemens) | Setting C (rCBF < 30%) | Not Reported (False positives in most patients) | 21.3 | Up to 207.9 |
Table 2: Inter-Vendor Variability in Ischemic Core Volume Estimation Against Phantom Ground Truth (30 mL Core) [65]
| Vendor Software | Software Version | Perfusion Algorithm | Median Error in Core Volume (mL) | Interquartile Range (mL) |
|---|---|---|---|---|
| Vendor A (IntelliSpace Portal) | 10.1 | Arrival-time-sensitive SVD | -2.5 | 6.5 |
| Vendor B (syngo.via) | VB40A-HF02 | Singular Value Decomposition (SVD) | -18.2 | 1.2 |
| Vendor C (Vitrea) | 7.14 | Bayesian | -8.0 | 1.4 |
| All Vendors (Pre-Standardization) | Not Applicable | Various | -8.2 | 14.6 |
| All Vendors (Post-Standardization) | Not Applicable | Logistic Model | -3.1 | 2.5 |
The data reveals that the choice of software alone can lead to dramatic differences in diagnosis. CMN demonstrated high specificity in correctly ruling out stroke, whereas syngo.via, depending on its internal settings, consistently overestimated the ischemic core, in some cases by over 200 mL [60]. Furthermore, when tested against a known ground truth using an anthropomorphic phantom, vendor software showed significant and variable median errors in estimating a 30 mL ischemic core, with Vendor B underestimating by over 18 mL on average [65]. This highlights that the variability is not just random but contains systematic biases specific to software algorithms.
Experimental Protocols for Validation and Harmonization
To address these standardization hurdles, researchers can employ the following detailed experimental protocols to validate and harmonize CTP data.
Protocol 1: Software-Specificity Validation for Lacunar Infarct Exclusion
This protocol is designed to evaluate the ability of different CTP software packages to reliably rule out small infarcts, thereby reducing dependence on follow-up MRI.
- Objective: To compare the specificity of automated CTP software packages in patients without confirmed acute infarction, using follow-up diffusion-weighted imaging (DWI) as the reference standard [60].
- Patient Population:
- Inclusion Criteria: Consecutive patients with clinical suspicion of AIS; availability of a CTP dataset prior to treatment; follow-up MRI with DWI sequence performed, confirming no infarct [60].
- Exclusion Criteria: Patients who received intravenous thrombolysis between CTP and MRI; severe motion artifacts or poor scan quality; failed automated perfusion post-processing; evidence of chronic infarct in the region of perfusion abnormality; vessel occlusion or stenosis on CT angiography [60].
- Imaging Acquisition:
- CTP Scans: Perform on a consistent scanner model to control for inter-scanner variability. Example parameters: Kernel H20f or T20F; contrast agent Imeron 300; injection rate of 5 mL/s; start of acquisition 3 seconds after injection [60].
- MRI (Reference Standard): Conduct follow-up MRI on systems of varying field strengths (e.g., 1.5T and 3.0T). Use a standard DWI protocol (b-values of 0 and 1,000 s/mm²) to minimize scanner-related variability. The mean delay from CTP to MRI should be approximately 68 hours to minimize false negatives from early scanning [60].
- Image Post-Processing & Analysis:
- Process all perfusion data using the software packages under investigation (e.g., syngo.via, Cercare Medical Neurosuite) with their default settings [60].
- For software with configurable parameters, test multiple common threshold settings. For example, with syngo.via:
- Setting A: Ischemic core defined as CBV < 1.2 mL/100 mL.
- Setting B: Apply an additional smoothing filter with the CBV < 1.2 mL/100 mL threshold.
- Setting C: Define ischemic core as a reduction in relative CBF (rCBF) to < 30% [60].
- Have at least two independent, blinded neuroradiologists review each software's perfusion maps to verify the presence or absence of a core lesion as defined by the software.
- Outcome Measures:
- Primary: Specificity, calculated as the proportion of patients with no infarct on DWI who were correctly identified as having zero infarct core volume by the CTP software [60].
- Secondary: Median and range of false-positive ischemic core volumes reported by the software.
Protocol 2: Multicenter Phantom-Based Harmonization
This protocol uses a standardized phantom to quantify and correct for inter-scanner and inter-software variability in a controlled environment.
- Objective: To evaluate the real-world variation in CTP imaging protocols across stroke centers and explore the potential of a standardized post-processing method to harmonize CTP images [65].
- Phantom Data Acquisition:
- Utilize an anthropomorphic digital phantom designed for realistic CTP simulation of acute ischemic stroke, incorporating a known ground truth infarct core (e.g., 30 mL) and penumbra (e.g., 55 mL) [65].
- Collect real-world CTP scan protocols (including tube voltage kVp, exposure mAs, and frame timing) from multiple participating stroke centers.
- Implement these center-specific acquisition parameters in the digital phantom to generate CTP data sets. Generate multiple noise realizations (e.g., n=10) for each scan protocol to account for the effect of stochastic noise [65].
- Perfusion Analysis:
- Analyze each phantom data set using the center-specific vendor software (e.g., Philips IntelliSpace Portal, Siemens syngoVIA, Vital Images Vitrea) with their default settings and thresholds (see Table 2). Allow arterial input functions to be determined automatically [65].
- Export the resulting perfusion parameter maps (Cerebral Blood Flow - CBF, Cerebral Blood Volume - CBV, Mean Transit Time - MTT, Time To Maximum - TMAX).
- Standardized Post-Processing:
- Apply a unified, standardized method to estimate ischemic regions from the vendor-generated perfusion maps. This could involve a multivariable, multivariate logistic model trained to predict the known ground truth from the perfusion map values [65].
- This model should be robust, generalizable, and require minimal training data to provide reliable predictions.
- Outcome Measures & Analysis:
- Primary: Median error and interquartile range of the infarct core volumes estimated by the vendor software compared to the phantom's ground truth.
- Secondary: Comparison of the error metrics before and after applying the standardized post-processing method to assess harmonization efficacy [65].
Visualization of Standardization Challenges and Workflows
The following diagrams, defined using the DOT language and adhering to the specified color palette and contrast rules, illustrate the core challenges and proposed solutions.
CTP Analysis Variability Landscape
AI-Driven Harmonization Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Software for CTP Standardization Research
| Item Name | Type | Function / Application in Research | Example / Specification |
|---|---|---|---|
| Anthropomorphic Digital Phantom | Validation Tool | Provides a ground truth for ischemic core and penumbra volumes, enabling quantitative evaluation of software accuracy and harmonization methods without patient variability [65]. | Phantom combining MR brain images with CT parameters, containing known 30 mL core and 55 mL penumbra. |
| Multi-Vendor Perfusion Software | Analysis Software | Represents the real-world clinical landscape. Used to quantify inter-software variability and test the robustness of harmonization algorithms across different platforms [60] [65]. | Siemens syngo.via, Philips IntelliSpace Portal, Vital Images Vitrea, Cercare Medical Neurosuite. |
| Standardized Logistic Model | Computational Algorithm | A harmonization tool applied to vendor-derived perfusion maps to reduce inter-software and inter-protocol variability, producing more consistent estimates of ischemic regions [65]. | Multivariable, multivariate model using CBF, CBV, TMAX/TTP maps as input. |
| CTP Acquisition Parameter Set | Experimental Variable | Allows for the systematic investigation of how specific scan settings (e.g., kVp, mAs) contribute to overall variability, informing future protocol guidelines [65]. | Defined sets of tube voltage (kVp), exposure (mAs), and frame timing. |
| AI-Based Stroke Imaging Tool | Integrated Solution | Provides a multi-task system for full workflow analysis (ICH detection, LVO identification, ASPECTS computation), serving as a benchmark for integrated AI performance [52]. | Tools like CINA-HEAD (Avicenna.AI) with reported ICH detection accuracy of 94.6%. |
The integration of artificial intelligence (AI) into acute stroke care is revolutionizing the paradigm of neuroimaging, enabling a significant reduction in radiation exposure without compromising diagnostic accuracy. For researchers and drug development professionals, understanding these dose optimization strategies is critical for designing safer clinical trials and developing next-generation imaging biomarkers. AI-driven automated perfusion analysis now allows for diagnostic-quality images to be obtained from CT protocols with substantially lower radiation doses and from entirely radiation-free portable MRI systems, thereby minimizing patient exposure while maintaining the precision required for therapeutic decision-making [66] [15]. This document details the application notes and experimental protocols for implementing these strategies in a research setting, providing a framework for validating low-dose imaging against established high-dose standards.
Establishing Diagnostic Reference Levels for Radiation Dose Optimization
A fundamental step in dose optimization is establishing Diagnostic Reference Levels (DRLs), which serve as benchmarks for radiation exposure in standard imaging protocols. A recent large-scale study analyzed dosimetry data from 1,790 patients to propose novel DRLs for an extended stroke CT protocol encompassing non-contrast CT (NCCT), multiphase CT angiography (MP-CTA), and CT perfusion (CTP) [67].
Table 1: Proposed Local Diagnostic Reference Levels (75th Percentile CTDIvol) for Extended Stroke CT Protocol [67]
| Sequence | Dual-Source CT (DSCT-1) (mGy) | Dual-Source CT (DSCT-2) (mGy) | Single-Source CT (SSCT) (mGy) |
|---|---|---|---|
| NCCT | 37.3 | 49.1 | 43.7 |
| Arterial CTA | 3.6 | 5.5 | 4.9 |
| Early Venous CTA | 1.2 | 2.5 | 2.2 |
| Late Venous CTA | 1.2 | 2.5 | 2.2 |
| CTP | 141.1 | 220.5 | 200.8 |
The data reveals that additive MP-CTA scans contribute only a minor increase in total radiation exposure, particularly when using modern dual-source scanners (DSCT) [67]. Furthermore, CTP represents the most significant source of radiation exposure within the protocol. The study demonstrated that targeted protocol adjustments, such as optimizing the tube current-time product, could achieve a 28.2% dose reduction in CTP without sacrificing diagnostic image quality, underscoring the potential for protocol-specific optimization [67].
Experimental Protocol: Validating Dose-Optimized CT Angiography
- Objective: To compare the diagnostic accuracy of a dose-optimized MP-CTA protocol against standard-dose MP-CTA for detecting Large Vessel Occlusion (LVO) and quantifying collateral scores.
- Imaging Protocol:
- Scanner: Third-generation dual-source CT (e.g., Siemens SOMATOM Force).
- Arterial CTA: Use a low tube voltage (70-80 kV) with automated exposure control (AEC) and iterative reconstruction (IR) enabled. Administer 50 mL of non-ionic iodinated contrast material (e.g., Imeron 400 mg I/mL) at 5 mL/s [67].
- MP-CTA: Acquire early and late venous phases with an 8-second delay between each, using identical low-dose head CT settings [67].
- Dosimetry Analysis: Extract the Volumetric CT Dose Index (CTDIvol) and Dose-Length Product (DLP) from radiation dose structured reports. The effective dose (ED) is calculated as ED = DLP × k, where k (head) = 0.0016 mSv/mGy·cm [67].
- Image Quality Assessment:
- Objective Quality: Calculate the Contrast-to-Noise Ratio (CNR) by placing regions of interest in the M1 segment of the middle cerebral artery and adjacent brain tissue.
- Subjective Quality: Employ a 4-point Likert scale (1 = non-diagnostic, 4 = excellent) for blinded image evaluation by two neuroradiologists, focusing on LVO detection and collateral score assessment [67].
- Statistical Analysis: Compare dose metrics using the Kruskal-Wallis test and image quality ratings using intraclass correlation coefficients (ICC).
AI-Driven Perfusion Analysis for Low-Dose and Radiation-Free Imaging
AI is pivotal for extracting consistent, quantitative data from low-dose CT and radiation-free MRI, ensuring diagnostic accuracy is maintained.
Validation of Automated MRI Perfusion Software
A recent multicenter study conducted a comparative validation of a new AI-based MR perfusion-weighted imaging (PWI) software (JLK PWI) against the established RAPID platform [5].
Table 2: Performance Metrics for JLK PWI vs. RAPID in a Multicenter Cohort (n=299) [5]
| Parameter | Concordance Correlation Coefficient (CCC) | Cohen's Kappa (κ) for EVT Eligibility |
|---|---|---|
| Ischemic Core Volume | 0.87 (Excellent) | - |
| Hypoperfused Volume (Tmax >6s) | 0.88 (Excellent) | - |
| DAWN Trial Criteria | - | 0.80 - 0.90 (Very High) |
| DEFUSE-3 Trial Criteria | - | 0.76 (Substantial) |
The study demonstrated excellent volumetric agreement for both ischemic core and hypoperfused tissue, confirming that the AI platform can reliably quantify key biomarkers from PWI data [5]. Furthermore, the very high concordance in EVT eligibility based on clinical trial criteria underscores the clinical translatability of such automated tools for treatment decisions in both research and clinical practice [5].
Portable Ultra-Low-Field MRI as a Radiation-Free Alternative
The Swoop portable ultra-low-field (pULF) MRI (0.064 T) represents a paradigm shift towards radiation-free neuroimaging. A pilot study evaluated its diagnostic value in acute stroke care [68].
- Methodology: Seventeen consecutive patients with suspected ischemic stroke underwent pULF-MRI in addition to standard high-field (HF) MRI. Scans were blindly assessed for lesion detection and a virtual treatment decision was made based on pULF-MRI [68].
- Results:
- pULF-MRI detected ischemic lesions in 8 out of 12 patients with confirmed infarcts on HF-MRI. The four missed infarcts were all smaller than 6 mm in diameter [68].
- In all cases, the virtual treatment decision based on pULF-MRI matched the actual clinical decision, proving its utility in guiding reperfusion therapy [68].
- Advantages and Limitations:
- Advantages: No ionizing radiation; portable and can be deployed at the point-of-care; lower cost; no requirement for extensive shielding [68].
- Limitations: Lower sensitivity for very small infarcts (<6 mm); longer acquisition times; current lack of vessel imaging and highly hemorrhage-sensitive sequences [68].
Experimental Protocol: Implementing AI-Based Perfusion Analysis
- Objective: To assess the agreement of a new AI perfusion software (e.g., mRay-VEOcore, JLK PWI) with a reference standard (e.g., RAPID) for core/penumbra volumetry in acute ischemic stroke.
- Patient Cohort: Retrospective or prospective inclusion of patients with anterior circulation LVO who underwent CTP or PWI within 24 hours of symptom onset. Exclude cases with severe motion artifacts or inadequate bolus injection [5].
- Image Analysis Workflow:
- Preprocessing: The AI software performs motion correction, brain extraction, and arterial input function selection.
- Map Generation: Calculation of quantitative perfusion maps (CBF, CBV, MTT, Tmax) via deconvolution.
- Tissue Segmentation: Ischemic core and hypoperfused tissue are segmented using validated thresholds (e.g., ADC < 620 × 10⁻⁶ mm²/s for MR core; Tmax >6s for penumbra) [5].
- Output: Volumetric data (mL) for core, penumbra, and mismatch ratio/volume.
- Statistical Analysis:
Integrated Workflow and Essential Research Toolkit
The following diagram and table summarize the key components for implementing a dose-optimized, AI-driven stroke imaging pipeline.
Diagram 1: Integrated workflow for dose-optimized, AI-driven stroke imaging analysis. The process begins with image acquisition using low-dose protocols or radiation-free alternatives, followed by automated AI analysis that includes quality control, and culminates in the generation of quantitative data for research and clinical decision-making.
Table 3: Research Reagent and Software Solutions for AI-Driven Perfusion Analysis
| Item | Function/Application | Example Vendor/Product |
|---|---|---|
| AI Perfusion Analysis Platform | Fully automated core/penumbra segmentation and mismatch visualization from CT or MRI data; applies clinical trial criteria (DEFUSE-3) for treatment selection. | RAPID (RAPID AI); JLK PWI (JLK Inc.); mRay-VEOcore (mbits imaging) [5] [15] |
| AI Integration Infrastructure | Platform enabling seamless integration and deployment of multiple validated AI solutions into clinical PACS workflows without additional IT burden. | deepcOS (deepc) [15] |
| Iodinated Contrast Agent | Non-ionic contrast medium for CT angiography and perfusion imaging. | Iomeprol (Imeron 400 mg I/mL) [67] |
| Portable ULF-MRI System | Radiation-free, point-of-care MRI system for neuroimaging in acute stroke; requires minimal infrastructure. | Swoop Portable MR Imaging System (Hyperfine, Inc.) [68] |
| Advanced CT Scanner | High-performance scanner enabling substantial dose reduction in multiphase CTA and CTP through technical features like dual-source detection. | SOMATOM Force/Drive (Siemens Healthineers) [67] |
The integration of Picture Archiving and Communication Systems (PACS) with Electronic Medical Records (EMR) represents a critical foundation for deploying artificial intelligence (AI) platforms in acute stroke research. Seamless interoperability enables the automated, high-speed data transfer essential for AI-driven perfusion analysis, which operates within narrow therapeutic windows where minutes directly impact patient outcomes. In acute ischemic stroke, advanced imaging like CT Perfusion (CTP) generates vast datasets that require rapid processing and integration with clinical data for effective decision-making regarding endovascular thrombectomy (EVT) [12] [30]. The 21st Century Cures Act and Trusted Exchange Framework and Common Agreement (TEFCA) have made interoperability an urgent necessity rather than a long-term goal, with compliance directly tied to both patient safety and financial stability [69]. Despite technological advances, significant interoperability gaps persist—only 43% of hospitals routinely engage in all four domains of interoperable exchange (send, receive, find, and integrate), creating substantial barriers for multi-center stroke research and AI validation [70]. This document establishes application notes and experimental protocols to bridge these gaps, specifically focusing on AI-driven automated perfusion analysis in acute stroke research.
Technical Specifications and Technical Data
Quantitative Performance of AI Perfusion Tools in Stroke Imaging
Table 1: Diagnostic Performance of AI Tools in Acute Stroke Imaging
| AI Function | Imaging Modality | Sensitivity (%) | Specificity (%) | Overall Accuracy (%) | Sample Size (Patients) |
|---|---|---|---|---|---|
| ICH Detection | Non-contrast CT | 95.55 [12] | 81.73 [12] | 94.6 [30] | 373 NCCT [30] |
| LVO Identification | CTA | 93.50-97.10 [12] | 75.61-86.86 [12] | 86.4 [30] | 331 CTA [30] |
| ASPECTS Scoring | CT | N/A | N/A | 88.6 (region-based) [30] | 405 [30] |
| Multi-step Stroke Evaluation | NCCT & CTA | N/A | N/A | 94.6 (ICH), 86.4 (LVO) [30] | 405 [30] |
Table 2: Hospital Interoperability Statistics Relevant for AI Platform Deployment
| Interoperability Metric | 2018 (%) | 2023 (%) | Change | Impact on AI Research |
|---|---|---|---|---|
| Hospitals engaged in all 4 interoperability domains | 46 [70] | 70 [70] | +52% | Enables multi-center data pooling |
| Hospitals routinely engaged in interoperability | 28 [70] | 43 [70] | +54% | Critical for algorithm validation |
| Hospitals with EMR integration of external data | ~60 (est.) [70] | 71 [70] | ~+18% | Reduces data siloing for AI training |
| Clinicians routinely using integrated data | N/A | 42 [70] | N/A | Indicates workflow integration challenges |
Interoperability Standards and Specifications
Successful integration of AI perfusion platforms requires adherence to established and emerging interoperability standards:
- HL7 FHIR (Fast Healthcare Interoperability Resources): Modern RESTful API standard for clinical data exchange, enabling seamless integration between PACS, EMR, and AI applications [69] [71]. FHIR resources essential for stroke research include Patient, ImagingStudy, Observation, and DiagnosticReport.
- DICOM (Digital Imaging and Communications in Medicine): The universal standard for medical imaging communication, ensuring consistent transfer of CT perfusion data and AI results [72]. Critical for maintaining image quality and metadata integrity.
- IHE (Integrating the Healthcare Enterprise) Profiles: Implementation frameworks that ensure consistent application of standards. For stroke imaging, the IHE INV (Image Navigator) profile supports unified access to images across multiple repositories [72].
- CDS Hooks: FHIR-based standard for embedding AI decision support directly into clinician workflows within the EMR [71].
Application Notes and Experimental Protocols
Protocol 1: System Integration and Data Flow Validation
Purpose: To establish and verify seamless data exchange between PACS, EMR, and AI perfusion analysis platforms for acute stroke imaging.
Materials:
- Hospital PACS with DICOM protocol support [72]
- EMR system with FHIR API capabilities [71]
- AI perfusion analysis software (e.g., RAPID, CINA-HEAD) [12] [30]
- DICOM tag editor and validation tool
- Network monitoring system
Methodology:
- Interface Configuration
Data Mapping and Transformation
Validation Procedure
- Execute test series of 50 historical stroke cases with known outcomes
- Verify completeness of data transfer at each integration point
- Measure time intervals from scan completion to AI result availability in EMR
- Validate accuracy of data transformation through independent expert review
Quality Control:
- Automated daily validation of first 5 stroke cases using known outcome data
- Continuous monitoring of data transfer success rates (>99% required)
- Monthly reconciliation of imaging and clinical data integrity
Protocol 2: AI Performance Validation in Clinical Workflow
Purpose: To evaluate the diagnostic performance and clinical impact of integrated AI perfusion analysis in acute stroke management.
Materials:
- Consecutive acute stroke patients presenting within 24 hours of symptom onset [12]
- Multi-phase CT imaging protocol: NCCT, CTA, CTP [12] [30]
- Reference standard: Independent interpretation by two neuroradiologists blinded to AI results [30]
- Integrated PACS-EMR-AI platform as validated in Protocol 1
Methodology:
- Patient Recruitment and Imaging
AI Processing and Integration
Reference Standard Establishment
Outcome Measures
Statistical Analysis:
- Calculate performance metrics with 95% confidence intervals
- Assess inter-rater reliability using intraclass correlation coefficients for continuous measures
- Perform multivariate analysis to identify factors affecting diagnostic performance
Visualizations and Workflows
Acute Stroke AI Integration Architecture
Acute Stroke AI Validation Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Components for AI Perfusion Platform Integration
| Component | Function | Example Solutions | Implementation Notes |
|---|---|---|---|
| Cloud PACS | Scalable image storage and retrieval enabling multi-center research | Enterprise Imaging Platform [72], Cloud PACS [73] | Provides unlimited scalability and robust disaster recovery; essential for pooling multi-center stroke data |
| FHIR Server | Clinical data exchange and API management | FHIR API [71], SMART on FHIR | Enables standardized integration between AI outputs and EMR systems; supports research data extraction |
| AI Perfusion Software | Automated processing of CTP data for core/penumbra quantification | RAPID [12], CINA-HEAD [30] | FDA-cleared tools provide validated metrics for research endpoints; ensure DICOM integration capability |
| DICOM Middleware | Protocol translation and workflow orchestration | Integration Engine [69], DICOM Router | Handles transformation between legacy systems and modern AI platforms; critical for heterogeneous environments |
| De-identification Tool | PHI removal for research data sets | De-identification Toolset [73] | Essential for creating research datasets compliant with HIPAA Safe Harbor methodology; removes 18 PHI identifiers |
| Validation Framework | Performance assessment and statistical analysis | Reference Standard [30], Ground Truth [30] | Structured methodology for establishing ground truth through expert consensus; critical for algorithm validation |
Seamless PACS-EMR integration for AI perfusion platforms represents a transformative capability for acute stroke research, enabling robust multi-center studies that can accelerate therapeutic development. The protocols and application notes described provide a framework for implementing and validating these integrated systems, with specific attention to the requirements of AI-driven perfusion analysis. As regulatory frameworks evolve with initiatives like the FDA's "Artificial Intelligence and Machine Learning Software as a Medical Device Action Plan" [74] [75], and interoperability standards mature through TEFCA implementation [69] [70], the research community must maintain focus on both technical integration and clinical validation. Future developments in generative AI for report generation and federated learning for multi-center research without data centralization will further enhance capabilities, provided that interoperability remains a foundational priority.
Validating AI Tools: Comparative Performance, Clinical Trial Evidence, and Predictive Accuracy
The application of Artificial Intelligence (AI) in acute ischemic stroke care represents a paradigm shift in neurovascular research and therapeutic development. AI-driven automated perfusion analysis has transitioned from a research concept to a critical tool for endovascular therapy (EVT) selection, particularly for patients presenting in extended time windows [76]. The established relationship between imaging biomarkers and clinical outcomes has made perfusion imaging analysis a cornerstone of modern stroke trials [17].
The RAPID platform has emerged as a de facto gold standard in this domain, with its algorithms extensively validated through landmark clinical trials including DEFUSE, SWIFT PRIME, EXTEND-IA, and DEFUSE 3 [77]. This validation has positioned RAPID as a benchmark against which novel AI platforms are measured. For researchers and pharmaceutical developers, understanding the comparative performance of emerging technologies against this established standard is crucial for evaluating their potential in both clinical trial and eventual clinical practice settings. This application note synthesizes recent comparative validation studies to guide protocol development and technology assessment in acute stroke research.
Comparative Performance Data of AI Platforms
Table 1: Diagnostic Performance of AI Platforms for Large Vessel Occlusion (LVO) Detection
| Platform | Sensitivity (%) | Specificity (%) | PPV (%) | Number of Cases | Reference Standard |
|---|---|---|---|---|---|
| RAPIDAI (Systematic Review) | 90.5 | 85.7 | - | 1,645 | Neuroradiologist Interpretation [78] |
| RAPIDAI (Manufacturer Claim) | 97 | 96 | 95 | - | Clinical Validation [19] |
| AIDoc (Single Center) | 78 | - | - | 49 | Vascular Neurologist + Neuroradiologist [78] |
| CINA-HEAD (Multicenter) | - | - | - | 331 | Expert Neuroradiologists [30] |
Table 2: Volumetric Agreement for Perfusion Parameter Estimation
| Platform Comparison | Ischemic Core (ICC) | Hypoperfused Volume (ICC) | EVT Decision Concordance (κ) | Sample Size |
|---|---|---|---|---|
| JLK PWI vs. RAPID (MRI) | 0.87 | 0.88 | 0.76-0.90 | 299 [17] |
| UGuard vs. RAPID (CTP) | 0.92 | 0.80 | - | 159 [38] |
Specialized Detection Capabilities
For medium vessel occlusions (MeVOs), which present particular detection challenges, a recent large-scale comparison demonstrated significant performance differences between platforms. In an analysis of 1,122 eligible cases, RapidAI detected 93% (109) of MeVOs using CT Perfusion alone, compared to 70% (82) by Viz.ai [77]. This 33% improvement in detection rate highlights substantial variability in algorithm performance for more subtle vascular occlusions.
Experimental Protocols for Validation Studies
Protocol 1: Volumetric Agreement and Clinical Concordance Study
Objective: To evaluate the technical and clinical agreement between a novel AI perfusion platform and an established reference standard (RAPID) for both volumetric measurements and endovascular therapy eligibility determination.
Imaging Acquisition Parameters:
- Modality: CT Perfusion or MR Perfusion
- CTP Scanner Requirements: 80-100 kV tube voltage, 400-500 mAs, 50-60 second acquisition time [38]
- CTP Contrast Protocol: 70 mL iodixanol injection at 5 mL/s [38]
- PWI Parameters: TR=1,500-2,000 ms, TE=40-50 ms, FOV=230 × 230 mm², slice thickness=5 mm [17]
Software Analysis Methodology:
- RAPID Settings: Version 7.0+, delay-insensitive block-circulant SVD deconvolution
- Ischemic Core Definition: rCBF < 30% (CTP) or ADC < 620 × 10⁻⁶ mm²/s (PWI) [17] [38]
- Hypoperfused Tissue Definition: Tmax > 6 seconds [17] [38]
- Co-registration: Automatic coregistration of diffusion and perfusion maps for mismatch computation [17]
Statistical Analysis Plan:
- Volumetric Agreement: Concordance correlation coefficients (CCC), Bland-Altman plots with limits of agreement, Pearson correlation coefficients [17]
- Clinical Decision Concordance: Cohen's kappa (κ) for EVT eligibility based on DAWN/DEFUSE-3 criteria [17]
- Predictive Performance: Receiver operating characteristic (ROC) analysis, area under curve (AUC) comparison using DeLong test [38]
- ICC Interpretation: Poor (<0.5), moderate (0.5-0.75), good (0.75-0.9), strong (>0.9) [38]
Protocol 2: Diagnostic Accuracy Study for LVO Detection
Objective: To determine the sensitivity, specificity, and accuracy of an AI platform for detecting large vessel occlusions compared to expert human interpretation.
Reference Standard Development:
- Expert Panel: Board-certified vascular neurologist and board-certified neuroradiologist
- Blinding: Independent reads without access to AI results
- Adjudication: Process for resolving discrepant interpretations [78]
Case Selection Criteria:
- Inclusion: Patients ≥18 years with acute LVO identified on imaging who underwent mechanical thrombectomy [78]
- Exclusion: Patients transferred after external vascular imaging, studies with motion artifacts or inadequate quality [78] [38]
- Sample Size Justification: Power calculation based on expected sensitivity/specificity
Statistical Methods:
- Diagnostic Performance: Sensitivity, specificity, PPV, NPV with 95% confidence intervals
- Comparison of Proportions: Z-test for population proportions [78]
- Handling of Indeterminate Results: Predefined protocol for non-diagnostic AI outputs
Workflow Visualization: AI Validation Pathway
AI Platform Validation Workflow
The Scientist's Toolkit: Essential Research Reagents & Solutions
Table 3: Research Reagent Solutions for AI Perfusion Platform Validation
| Category | Specific Product/Solution | Research Application | Key Features |
|---|---|---|---|
| Reference Standard Software | RAPID (iSchemaView) | Gold standard comparison for novel AI platforms | FDA-cleared; validated in landmark stroke trials; delay-insensitive algorithm [17] [38] |
| Validation Dataset | ISLES 2018 (Ischemic Stroke Lesion Segmentation) | Public benchmark for algorithm validation | Standardized reference segmentations; enables cross-study comparisons [79] |
| Deconvolution Algorithm | Block-Circulant SVD | Perfusion parameter calculation from CTP/PWI data | Delay-insensitive; reduces artifacts from collateral flow [17] [38] |
| Statistical Analysis Package | R Statistical Software (v4.1.3+) | Comprehensive statistical analysis for validation studies | ICC, Bland-Altman, ROC analysis with pROC package [38] |
| Image Preprocessing Framework | SPPINN (Spatio-temporal Perfusion Physics-Informed Neural Network) | Advanced CTP analysis robust to noise | Physics-informed learning; implicit neural representations [79] |
The benchmarking studies summarized in this application note demonstrate that several novel AI platforms, including JLK PWI and UGuard, show strong technical agreement with the established RAPID standard for volumetric perfusion analysis [17] [38]. This suggests that these platforms may be viable alternatives for research applications, potentially offering cost efficiencies or specialized capabilities.
However, significant performance variability exists in detection-focused tasks, particularly for more challenging vascular occlusions like MeVOs [77]. For pharmaceutical developers and clinical researchers, these findings highlight the importance of platform-specific validation when selecting AI tools for trial enrollment or biomarker assessment. The protocols provided herein offer a standardized framework for conducting such validations, ensuring that performance claims are assessed consistently across the research ecosystem.
As AI continues to evolve toward multi-step stroke imaging analysis [30], comprehensive benchmarking against gold standards remains essential for maintaining scientific rigor in both basic research and drug development contexts.
In the realm of AI-driven automated perfusion analysis for acute stroke research, the validation of new technologies against established reference standards is paramount for clinical translation. Quantitative volumetric agreement metrics serve as the statistical foundation for demonstrating reliability and validity in multicenter trials. This document outlines the core concepts of Intraclass Correlation Coefficient (ICC), Concordance Correlation Coefficient (CCC), and Bland-Altman analysis, providing structured protocols for their application in evaluating automated perfusion software. These metrics are essential for researchers and drug development professionals to objectively assess whether new AI tools meet the rigorous requirements for both regulatory approval and clinical adoption in time-sensitive stroke care pathways.
Core Volumetric Agreement Metrics
In the context of AI-driven perfusion analysis, three statistical methods form the cornerstone of volumetric agreement assessment between different software platforms or against reference standards.
Intraclass Correlation Coefficient (ICC) measures the reliability of measurements and the consistency between two or more quantitative measurements. It is particularly valuable for assessing inter-software and inter-rater reliability in multicenter trials where multiple observers and scanners may be involved. ICC values range from 0 to 1, with higher values indicating better reliability. In stroke perfusion analysis, ICC is commonly used to evaluate the consistency of ischemic core volume measurements between different software platforms [80] [81].
Concordance Correlation Coefficient (CCC) evaluates the agreement between two measures of the same variable by assessing how well pairs of observations fall along the 45-degree line of perfect concordance. CCC incorporates both precision (how far observations are from the fitted line) and accuracy (how far the line is from the 45-degree line). Recent studies evaluating automated perfusion software have reported CCC values of 0.87-0.88 for ischemic core and hypoperfused volume measurements between new platforms and established reference standards like RAPID [17] [5].
Bland-Altman Analysis provides a visual and quantitative assessment of the agreement between two measurement techniques by plotting the differences between the methods against their averages. This method establishes limits of agreement (mean difference ± 1.96 SD) within which 95% of the differences between measurement methods are expected to fall. Bland-Altman analysis is particularly useful for identifying systematic biases (through the mean difference) and proportional errors in perfusion volume measurements across the range of clinically relevant values [80] [81].
Table 1: Interpretation Guidelines for Agreement Metrics in Perfusion Analysis
| Metric | Value Range | Agreement Level | Clinical Interpretation in Stroke Imaging |
|---|---|---|---|
| ICC | 0.0-0.5 | Poor | Unacceptable for clinical decision-making |
| 0.5-0.75 | Moderate | Limited reliability for treatment decisions | |
| 0.75-0.9 | Good | Appropriate for supportive clinical use | |
| >0.9 | Excellent | Suitable for primary clinical decision-making | |
| CCC | 0.0-0.2 | Poor | Negligible agreement between platforms |
| 0.21-0.40 | Fair | Minimal clinical utility | |
| 0.41-0.60 | Moderate | May inform general trends | |
| 0.61-0.80 | Substantial | Appropriate for research applications | |
| 0.81-1.0 | Excellent | Suitable for clinical validation studies |
Experimental Protocols for Metric Evaluation
Multicenter Trial Design for Perfusion Software Validation
Objective: To evaluate the volumetric agreement between a novel AI-based perfusion analysis software and an established reference standard in acute ischemic stroke patients across multiple clinical centers.
Patient Population:
- Target enrollment: 150-300 patients with acute ischemic stroke presenting within 24 hours of symptom onset [17] [5]
- Inclusion criteria: Clinical suspicion of acute ischemic stroke, age ≥18 years, availability of perfusion imaging (CTP or PWI) prior to treatment
- Exclusion criteria: Severe motion artifacts, inadequate image quality, contraindications to contrast administration, pre-morbid modified Rankin Scale (mRS) score ≥2 [38]
Imaging Protocol:
- Multicenter acquisition using various CT and MRI scanners (e.g., Siemens, Philips, GE systems) [17] [5]
- Standardized perfusion parameters: CT perfusion (80-100 kV, slice thickness 5mm) or MR perfusion (TR=1,000-2,500 ms, TE=30-70 ms, slice thickness 5mm) [17] [5] [54]
- Follow-up diffusion-weighted imaging (DWI) MRI at 24-48 hours for infarct validation [54]
Software Comparison Methodology:
- Process all perfusion datasets through both reference (e.g., RAPID) and test software platforms
- Extract volumetric outputs for ischemic core (typically defined by rCBF <30% or ADC <620×10⁻⁶ mm²/s) and hypoperfused tissue (typically Tmax >6s) [17] [5] [38]
- Ensure blinded analysis where software operators are unaware of clinical information and paired software results
Statistical Analysis Protocol
Data Collection:
- Collect continuous volume measurements (in mL) for ischemic core, hypoperfused tissue, and mismatch ratio from both software platforms
- Record clinical decision outcomes (EVT eligibility based on DAWN/DEFUSE-3 criteria) for each platform [17] [31]
Agreement Assessment:
- Calculate ICC using two-way mixed-effects models for absolute agreement [80] [81]
- Compute CCC with precision and accuracy components [17] [5]
- Perform Bland-Altman analysis with calculation of mean difference (bias) and 95% limits of agreement [80] [81]
- Assess clinical decision concordance using Cohen's kappa for EVT eligibility [17] [5] [31]
Implementation Code:
Results from Recent Multicenter Trials
Recent validation studies for automated perfusion analysis software demonstrate the application of these agreement metrics in stroke research.
Table 2: Volumetric Agreement Results from Recent Perfusion Software Validation Studies
| Study/Software | Metric | Ischemic Core Volume | Hypoperfused Volume | Clinical Decision Concordance |
|---|---|---|---|---|
| JLK PWI vs RAPID [17] [5] | CCC | 0.87 (0.83-0.90) | 0.88 (0.84-0.91) | κ=0.80-0.90 (DAWN criteria) |
| ICC | 0.89 (0.86-0.92) | 0.91 (0.88-0.93) | κ=0.76 (DEFUSE-3 criteria) | |
| UGuard vs RAPID [38] | ICC | 0.92 (0.89-0.94) | 0.80 (0.73-0.85) | N/A |
| Bland-Altman Bias | -2.1 mL | +15.3 mL | N/A | |
| Viz CTP vs RAPID [31] | ICC | 0.96 (0.93-0.97) | 0.93 (0.90-0.96) | κ=0.96 (DAWN criteria) |
| Clinical Impact | N/A | N/A | 10.6% discordance in EVT eligibility |
Key Findings:
- Excellent technical agreement (ICC/CCC >0.8) is consistently demonstrated between established and novel perfusion platforms [17] [5] [38]
- High clinical decision concordance (κ>0.8) supports the use of new platforms for EVT eligibility determination [17] [31]
- Bland-Altman analysis reveals minimal systematic bias for ischemic core volumes (<5 mL) in most comparisons [38]
- Moderate agreement for penumbra volume estimation highlights the need for continued refinement in hypoperfusion assessment algorithms
The Scientist's Toolkit
Table 3: Essential Research Reagent Solutions for Perfusion Software Validation
| Tool/Category | Specific Examples | Research Function |
|---|---|---|
| Reference Standard Software | RAPID (iSchemaView) [17] [5] [31] | Established benchmark for perfusion analysis in clinical trials |
| Validation Platforms | JLK PWI [17] [5], Viz CTP [31], UGuard [38], syngo.via [54], Cercare Medical Neurosuite [54] | Test platforms for comparison against reference standards |
| Statistical Analysis Tools | R Statistical Software, IBM SPSS, Python SciPy | Implementation of ICC, CCC, Bland-Altman analyses |
| Imaging Data Sources | Multicenter patient cohorts (n=150-300) with CTP/PWI and follow-up DWI [17] [5] [38] | Ground truth for volumetric agreement assessment |
| Clinical Decision Frameworks | DAWN Trial Criteria, DEFUSE-3 Criteria [17] [5] [31] | Standardized endpoints for treatment eligibility concordance |
Workflow Visualization
Diagram 1: Multicenter Validation Workflow for Perfusion Analysis Software
The rigorous application of ICC, CCC, and Bland-Altman analysis in multicenter trials provides the statistical foundation for validating AI-driven perfusion analysis tools in acute stroke research. Recent studies demonstrate that novel software platforms can achieve excellent technical agreement (ICC/CCC >0.8) and substantial clinical decision concordance (κ>0.8) with established reference standards. These metrics collectively enable researchers and drug development professionals to comprehensively evaluate new technologies, ensuring they meet the stringent requirements for both regulatory approval and clinical implementation in time-sensitive stroke care. The standardized protocols outlined in this document provide a framework for conducting robust validation studies that advance the field of automated perfusion analysis while maintaining scientific rigor.
In the rapidly evolving field of acute ischemic stroke care, artificial intelligence (AI)-driven automated perfusion analysis software has become indispensable for extending treatment windows and personalizing therapy [5]. These platforms provide critical volumetric data on the ischemic core and hypoperfused tissue, enabling clinicians to identify patients who may benefit from endovascular thrombectomy (EVT) beyond the conventional time window based on the landmark DAWN and DEFUSE-3 trial criteria [5]. As new AI algorithms emerge, rigorous validation against established platforms is essential to ensure reliability in clinical decision-making. This application note examines the use of Cohen's kappa statistic to evaluate agreement in EVT eligibility classification between a newly developed perfusion software and an established reference platform, providing researchers with standardized methodologies for AI validation in acute stroke research.
Theoretical Framework: Kappa Statistics
Principles of Interrater Agreement
Cohen's kappa (κ) is a chance-corrected measure of agreement between two raters for categorical items [82]. Unlike simple percent agreement calculations, kappa accounts for the possibility of agreement occurring by chance, providing a more robust assessment of diagnostic concordance [83]. The kappa statistic is calculated as:
[κ = \frac{po - pe}{1 - p_e}]
where (po) represents the observed agreement proportion, and (pe) represents the expected agreement proportion due to chance alone [82]. Kappa values range from -1 (complete disagreement) to +1 (complete agreement), with values above 0 indicating agreement beyond chance.
Interpretation Guidelines
For healthcare research, kappa values are typically interpreted using standardized thresholds as shown in Table 1 [82].
Table 1: Interpretation of Kappa Statistic Values
| Kappa Value | Level of Agreement |
|---|---|
| < 0.00 | Poor |
| 0.00 - 0.20 | Slight |
| 0.21 - 0.40 | Fair |
| 0.41 - 0.60 | Moderate |
| 0.61 - 0.80 | Substantial |
| 0.81 - 1.00 | Almost Perfect |
Experimental Data and Results
A recent retrospective multicenter study directly compared a newly developed AI-based perfusion software (JLK PWI) against the established RAPID platform for MRI-based perfusion analysis in acute stroke [5]. The study included 299 patients with acute ischemic stroke who underwent perfusion-weighted imaging (PWI) within 24 hours of symptom onset [5]. Baseline characteristics of the study population are summarized in Table 2.
Table 2: Study Population Baseline Characteristics (N=299)
| Characteristic | Value |
|---|---|
| Mean Age (years) | 70.9 |
| Male Sex | 55.9% |
| Median NIHSS Score | 11 (IQR 5-17) |
| Median Time from LKW to PWI (hours) | 6.0 |
| Hypertension | 65.2% |
| Diabetes Mellitus | 31.4% |
| Atrial Fibrillation | 28.4% |
Volumetric and Clinical Decision Concordance
The study assessed both volumetric agreement for key perfusion parameters and clinical decision concordance for EVT eligibility based on DAWN and DEFUSE-3 criteria [5]. The results demonstrated excellent technical agreement between the platforms, with high concordance in clinical treatment decisions as detailed in Table 3.
Table 3: Agreement Between JLK PWI and RAPID Software
| Parameter | Metric | Value |
|---|---|---|
| Ischemic Core Volume | Concordance Correlation Coefficient (CCC) | 0.87 (p < 0.001) |
| Hypoperfused Volume | Concordance Correlation Coefficient (CCC) | 0.88 (p < 0.001) |
| EVT Eligibility (DAWN Criteria) | Cohen's Kappa (κ) | 0.80 - 0.90 |
| EVT Eligibility (DEFUSE-3 Criteria) | Cohen's Kappa (κ) | 0.76 |
The kappa values observed across all subgroups and criteria indicate substantial to almost perfect agreement in EVT eligibility classification between the two platforms [5]. This high level of clinical decision concordance supports the validity of the new software for routine clinical application.
Experimental Protocols
Patient Selection and Imaging Protocol
Inclusion Criteria:
- Clinical diagnosis of acute ischemic stroke
- PWI performed within 24 hours of symptom onset
- Availability of complete imaging data including DWI and PWI sequences
Exclusion Criteria:
- Abnormal arterial input function (n=6)
- Severe motion artifacts (n=2)
- Inadequate image quality (n=11)
Imaging Parameters: All perfusion MRI scans were performed on either 3.0T (62.3%) or 1.5T (37.7%) scanners from multiple vendors [5]. Dynamic susceptibility contrast-enhanced perfusion imaging was performed using a gradient-echo echo-planar imaging sequence with the following parameters:
- Repetition Time (TR): 1,000-2,500 ms
- Echo Time (TE): 30-70 ms
- Field of View (FOV): 210×210 mm² or 230×230 mm²
- Slice thickness: 5 mm with no interslice gap
Automated Perfusion Analysis Protocol
Software Specifications:
- Reference Platform: RAPID (RAPID AI, CA, USA)
- Test Platform: JLK PWI (JLK Inc., Republic of Korea)
Image Processing Workflow:
- Preprocessing: Motion correction, brain extraction via skull stripping, and vessel masking
- Signal Conversion: Conversion of MR signal intensity to concentration-time curves
- Input Function Selection: Automated identification of arterial input function and venous output function
- Deconvolution: Block-circulant singular value deconvolution
- Parameter Calculation: Generation of quantitative perfusion maps (CBF, CBV, MTT, Tmax)
- Lesion Segmentation:
- Ischemic core: Deep learning-based segmentation on b1000 DWI images
- Hypoperfused volume: Tmax > 6 seconds threshold
- Co-registration: Automated alignment of DWI lesions with perfusion maps for mismatch calculation
EVT Eligibility Assessment Protocol
DAWN Criteria Application:
- Stratify patients into predefined subgroups based on age and NIHSS score
- Apply corresponding infarct core volume thresholds for each subgroup
- Classify as EVT-eligible if meeting criteria for respective subgroup
DEFUSE-3 Criteria Application:
- Calculate mismatch ratio (ischemic volume to infarct core volume)
- Measure absolute infarct core volume
- Determine absolute volume of penumbra (Tmax >6s volume)
- Classify as EVT-eligible if meeting all criteria:
- Mismatch ratio ≥1.8
- Infarct core volume <70 mL
- Absolute penumbra volume ≥15 mL
Statistical Analysis Protocol
Volumetric Agreement Assessment:
- Calculate concordance correlation coefficients (CCC) for ischemic core, hypoperfused volume, and mismatch volume
- Generate Bland-Altman plots with limits of agreement
- Compute Pearson correlation coefficients
Clinical Decision Concordance Assessment:
- Create 2×2 contingency tables for EVT eligibility classification (yes/no) between platforms
- Calculate observed agreement proportion (pₒ)
- Calculate expected agreement proportion (pₑ) due to chance
- Compute Cohen's kappa statistic using standard formula
- Classify magnitude of agreement using established guidelines
Subgroup Analysis:
- Stratify analysis by anterior circulation large vessel occlusion
- Calculate subgroup-specific kappa statistics
- Compare point estimates and confidence intervals across subgroups
Visualizations
Kappa Statistical Analysis Workflow
EVT Eligibility Decision Pathway
The Scientist's Toolkit
Table 4: Essential Research Reagents and Solutions
| Item | Function/Application | Specifications |
|---|---|---|
| JLK PWI Software | Test platform for AI-driven perfusion analysis | Deep learning-based infarct segmentation; Tmax >6s for hypoperfusion [5] |
| RAPID Software | Reference platform for perfusion analysis | Commercial standard; ADC <620×10⁻⁶ mm²/s for core [5] |
| MRI Scanners | Image acquisition for DWI and PWI sequences | 1.5T and 3.0T systems; multi-vendor compatibility [5] |
| DSC-PWI Sequence | Dynamic susceptibility contrast perfusion imaging | Gradient-echo EPI; TR: 1,000-2,500ms; TE: 30-70ms [5] |
| Cohen's Kappa Calculator | Statistical analysis of classification agreement | Accounts for chance agreement; categorical data [83] [82] |
| DAWN Criteria Checklist | EVT eligibility assessment | Age/NIHSS stratified infarct core volume thresholds [5] |
| DEFUSE-3 Criteria Checklist | EVT eligibility assessment | Mismatch ratio ≥1.8, core <70mL, penumbra ≥15mL [5] |
The validation of AI-driven perfusion analysis platforms using kappa statistics provides a robust framework for assessing clinical decision concordance in acute stroke research. The demonstrated substantial to almost perfect agreement (κ = 0.76-0.90) between JLK PWI and the established RAPID platform supports the reliability of automated perfusion software for EVT eligibility determination based on DAWN and DEFUSE-3 criteria [5]. The experimental protocols outlined in this application note provide researchers with standardized methodologies for conducting rigorous validation studies of emerging AI technologies in stroke imaging, ultimately contributing to the advancement of precision medicine in acute stroke care.
The integration of Artificial Intelligence (AI) into acute stroke care is revolutionizing the prognostication of patient recovery. Accurately predicting functional outcomes following a stroke is critical for clinical decision-making, patient counseling, and the development of new therapeutics. The 90-day modified Rankin Scale (mRS) and the National Institutes of Health Stroke Scale (NIHSS) are gold standards for assessing long-term disability and short-term neurological deficit, respectively. Within the context of AI-driven automated perfusion analysis in acute stroke research, this document outlines the robust correlation between quantitative AI outputs and these clinical scores, and provides detailed protocols for validating these AI biomarkers in a research setting. The ability of AI to automatically extract imaging biomarkers from perfusion scans offers a powerful, objective tool for stratifying patient risk and predicting recovery trajectories, thereby enhancing both clinical trial efficiency and personalized medicine approaches.
Quantitative Correlation of AI Outputs with Clinical Scores
Research consistently demonstrates that specific imaging biomarkers quantified by AI software show strong, statistically significant associations with standard clinical outcome measures. The following tables summarize key quantitative findings from recent studies.
Table 1: Correlation of AI Biomarkers with 90-day modified Rankin Scale (mRS)
| AI Biomarker | Source | Correlation Metric | Value | Clinical Context |
|---|---|---|---|---|
| Final Infarct Volume (FIV) | Abraham et al. (2025) [84] | Concordance | 0.819 | Strong association with 90-day mRS outcome. |
| Random Forest Model | PMC10748594 (2023) [85] | Accuracy / AUC | 0.823 / 0.893 | Predicts 90-day mRS using clinical & registry data. |
| e-ASPECTS & Clinical Features | Frontiers in Neurology (2022) [86] | AUC (XGBoost Model) | 0.84 | Pre-interventional prediction of 90-day mRS. |
| CTPredict (Multimodal DL) | Scientific Reports (2025) [87] | Accuracy | 0.77 | Predicts 90-day mRS from 4D CTP & clinical data. |
Table 2: Correlation of AI Biomarkers with NIHSS Scores
| AI Biomarker | Source | Correlation Metric | Value | Clinical Context |
|---|---|---|---|---|
| Final Infarct Volume (FIV) | Abraham et al. (2025) [84] | Concordance | 0.722 | Association with 24-hour NIHSS score. |
| ChatGPT 4.0 Model | Springer (2025) [88] | Pearson Correlation (r) | 0.513 | Prediction of 7th-day NIHSS score. |
Experimental Protocols for Validation
To ensure the reliability and reproducibility of AI-powered biomarkers, rigorous experimental validation is required. The following protocols detail the methodology for establishing the correlation between AI outputs and clinical endpoints.
Protocol 1: Validating Automated FIV against 90-day mRS
This protocol is designed to confirm the prognostic value of automatically quantified Final Infarct Volume.
- Primary Objective: To determine the strength of association between AI-quantified FIV and the 90-day mRS score.
- Study Population:
- Cohort: Adult patients (≥18 years) with Acute Ischemic Stroke (AIS) who underwent mechanical thrombectomy.
- Inclusion Criteria: Availability of follow-up non-contrast CT (NCCT) or MRI within 12-96 hours post-treatment and a documented 90-day mRS assessment.
- Sample Size: A minimum of 800 patients is recommended for robust statistical power [84].
- Imaging and Analysis:
- Image Acquisition: Perform follow-up NCCT scans according to standardized clinical stroke protocols.
- AI Processing: Process the DICOM images through an automated AI software (e.g., Brainomix 360 Stroke) to generate the FIV measurement in milliliters (mL).
- Outcome Assessment: A certified neurologist or trained research nurse, blinded to the FIV results, should assess the 90-day mRS via a structured telephone or in-person interview.
- Statistical Analysis:
- Use ordinal regression models with the 90-day mRS as the dependent variable and FIV as the primary independent variable.
- Report the concordance statistic (C-statistic) to quantify the predictive power of FIV for the ordinal mRS.
- Perform multivariate analysis adjusting for confounders such as age, baseline NIHSS, and reperfusion status (mTICI score) [84].
Protocol 2: Predicting Short-Term NIHSS using Multimodal AI
This protocol outlines a method for predicting short-term neurological function (NIHSS) by integrating AI-derived imaging features with clinical data.
- Primary Objective: To develop and validate a machine learning model for predicting the 7-day NIHSS score.
- Data Collection:
- Clinical Variables: Demographics (age, sex), medical history (hypertension, diabetes, atrial fibrillation), baseline NIHSS, pre-stroke mRS, and details of reperfusion therapy (symptom-to-door, symptom-to-needle times) [88].
- Imaging Biomarkers:
- Acute Imaging: From baseline CTA/CTP, extract features using automated software (e.g., e-ASPECTS for ischemic core, e-CTA for collateral scores, and volumes of brain atrophy) [86].
- Follow-up Imaging: 24-hour post-treatment CT scan results, categorized for Hemorrhagic Transformation (HT) using ECASS II criteria [88].
- Model Development and Training:
- Data Preprocessing: Clean the dataset, handle missing values, and standardize continuous variables.
- Feature Selection: Apply a model-based approach (e.g., sequential backward feature selection) to identify the most predictive features from the combined clinical and imaging set [86].
- Algorithm Selection: Train and compare multiple ML algorithms, such as Extreme Gradient Boosting (XGBoost), Random Forest, and Support Vector Machines, using 10-fold cross-validation.
- Hyperparameter Tuning: Optimize model parameters using a grid search or Bayesian optimization framework [86].
- Model Evaluation:
- Assess the model's performance on a held-out test set using the Pearson correlation coefficient (r) between the predicted and actual 7-day NIHSS scores and the coefficient of determination (R²) [88].
Workflow and Signaling Pathways
The process of using AI for outcome prediction involves a structured workflow from data acquisition to clinical interpretation. Furthermore, the biological pathways linking AI-derived imaging findings to clinical outcomes can be conceptualized as a "signaling" cascade.
AI Outcome Prediction Workflow
Diagram 1: AI outcome prediction workflow.
Pathway from Imaging Biomarker to Clinical Outcome
Diagram 2: Biomarker to clinical outcome pathway.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Software for AI-Driven Stroke Outcome Research
| Item Name | Type | Function in Research | Example Vendor/Software |
|---|---|---|---|
| Automated Perfusion Analysis Software | Software | Quantifies core, penumbra, and mismatch volumes from CTP or PWI data; critical for EVT eligibility and outcome prediction. | RAPID, JLK PWI [17] [5] |
| AI-Powered NCCT Analysis Suite | Software | Automatically scores early ischemic changes (e-ASPECTS), estimates infarct core volume, and quantifies brain atrophy from non-contrast CT. | e-Stroke (Brainomix) [86] |
| Automated CTA Analysis Platform | Software | Identifies large vessel occlusion location and quantifies collateral circulation deficit volume. | e-CTA (Brainomix) [86] |
| Multimodal Deep Learning Framework | Software/Model | Integrates 4D imaging data (e.g., CTP) with clinical metadata to simultaneously predict lesion and functional outcomes. | CTPredict [87] |
| Validated Clinical Stroke Registry | Data Resource | Provides structured, high-quality data on demographics, treatments, complications, and outcomes for model training and validation. | Get With The Guidelines-Stroke, HGH Stroke Registry [85] [89] [90] |
| Model Interpretability Library | Software Library | Explains model predictions and identifies feature importance, building trust in AI outputs. | SHAP (SHapley Additive exPlanations) [86] |
Artificial Intelligence (AI)-driven automated perfusion analysis has emerged as a transformative technology in acute stroke research and drug development. These tools provide quantitative biomarkers essential for patient stratification in clinical trials and offer decision support in time-critical clinical settings. The real-world impact of these platforms is measured through three critical parameters: analytical sensitivity in detecting ischemic tissue, clinical specificity in identifying treatment-eligible patients, and operational efficacy in reducing time-to-treatment intervals. This assessment provides researchers and pharmaceutical developers with structured performance data and validated experimental protocols for evaluating AI perfusion technologies in stroke research and therapeutic development.
Performance Metrics of Validated AI Platforms
Diagnostic Accuracy of Integrated Stroke Evaluation Tools
Comprehensive AI tools that perform multiple analytical steps in the stroke imaging workflow have demonstrated high diagnostic accuracy in real-world settings. The table below summarizes the performance of an FDA-cleared and CE-marked AI-based device (CINA-HEAD) evaluated in a multicenter diagnostic study [30].
Table 1: Performance Metrics of a Multi-Step AI Stroke Imaging Tool
| Function | Imaging Modality | Accuracy (%) | Sensitivity (%) | Specificity (%) | Clinical Application |
|---|---|---|---|---|---|
| ICH Detection | NCCT | 94.6 [91.8-96.7] | - | - | Rule-out hemorrhagic stroke |
| LVO Identification | CTA | 86.4 [82.2-89.9] | - | - | Triage for thrombectomy |
| ASPECTS Region Analysis | NCCT | 88.6 [87.8-89.3] | - | - | Ischemic change quantification |
| ASPECTS Dichotomized (≥6) | NCCT | 80.4 | - | - | Thrombectomy eligibility |
This multi-step AI tool demonstrates particular strength in ICH detection with high accuracy (94.6%), ensuring safe rule-out of hemorrhage while maintaining robust LVO identification capabilities (86.4% accuracy)—a critical combination for rapid patient triage in time-sensitive stroke scenarios [30].
Comparative Performance of Perfusion Analysis Software
Automated perfusion analysis platforms provide critical quantitative biomarkers for infarct core and penumbra estimation. Recent comparative validations have evaluated new software against established reference standards.
Table 2: Agreement Metrics for Perfusion Software in Ischemic Stroke
| Software Comparison | Imaging Modality | Parameter | Concordance/ICC | Clinical Decision Concordance (κ) |
|---|---|---|---|---|
| JLK PWI vs. RAPID | MR PWI | Ischemic Core | CCC = 0.87 | DAWN Criteria: 0.80-0.90 |
| JLK PWI vs. RAPID | MR PWI | Hypoperfused Volume | CCC = 0.88 | DEFUSE-3 Criteria: 0.76 |
| UGuard vs. RAPID | CT Perfusion | Ischemic Core Volume | ICC = 0.92 [0.89-0.94] | - |
| UGuard vs. RAPID | CT Perfusion | Penumbra Volume | ICC = 0.80 [0.73-0.85] | - |
The JLK PWI software demonstrates excellent agreement with the established RAPID platform for both ischemic core (CCC=0.87) and hypoperfused volume (CCC=0.88) quantification [37] [17] [5]. This technical concordance translates to high clinical decision alignment, particularly for DAWN criteria (κ=0.80-0.90), supporting its use as a reliable alternative for MRI-based perfusion analysis in acute stroke care [17].
Similarly, UGuard software shows strong agreement with RAPID for ischemic core volume (ICC=0.92) and penumbra volume (ICC=0.80) measurement on CTP [38]. Predictive performance for favorable outcome was comparable between platforms (AUC 0.72 vs. 0.70, P=0.43), with UGuard measurements demonstrating higher specificity [38].
Predictive Performance for Functional Outcomes
Machine learning approaches integrating imaging biomarkers with clinical data have advanced outcome prediction for acute ischemic stroke.
Table 3: Machine Learning Models for Stroke Outcome Prediction
| Prediction Target | Model Type | Features | Performance (AUC) | Key Predictors |
|---|---|---|---|---|
| Short-term prognosis (mRS ≥3) in HTPR patients | Random Forest | Clinical + CYP2C19 genotype | 0.84 [0.71-0.97] | DBP, BUN, homocysteine, CRP, WBC, CYP2C19 PM |
| 90-day mRS >2 | Autoencoder + Clinical | DWI + Clinical features | 0.754 | Imaging biomarkers + clinical variables |
| Length of stay >8 days | Autoencoder + Clinical | DWI + Clinical features | 0.817 | Imaging biomarkers + clinical variables |
| Functional independence (3-month) | Deep Neural Network | Baseline clinical variables | 0.888 | Baseline severity + treatment variables |
The random forest model for predicting short-term prognosis in high on-treatment platelet reactivity (HTPR) patients demonstrated superior performance (AUC 0.84) compared to other machine learning models [91]. Explainable AI techniques identified key predictors including diastolic blood pressure, blood urea nitrogen, homocysteine, C-reactive protein, white blood cells, and CYP2C19 poor metabolizer status [91].
For operational outcomes, the integration of 2.5D DWI with clinical features using autoencoders achieved strong predictive performance for length of stay (AUC 0.817), highlighting the value of combining imaging biomarkers with clinical data for comprehensive outcome prediction [92].
Experimental Protocols for Validation Studies
Multicenter Software Validation Protocol
Study Design: Retrospective multicenter cohort study [17] [5]
Population:
- Inclusion: Acute ischemic stroke patients undergoing perfusion imaging within 24 hours of symptom onset
- Sample Size: 299 patients recommended for adequate statistical power
- Exclusion Criteria: Abnormal arterial input function, severe motion artifacts, inadequate image quality
Imaging Protocol:
- Modality: MR Perfusion-Weighted Imaging (PWI) with DWI sequence or CT Perfusion
- Scanner Parameters: Standardized across multiple vendors (GE, Philips, Siemens) at both 1.5T and 3.0T
- Acquisition: Dynamic susceptibility contrast-enhanced perfusion imaging using gradient-echo echo-planar imaging sequence
- Processing: Automated preprocessing including motion correction, brain extraction, and arterial input function selection
Analysis Workflow:
- Automated coregistration of diffusion and perfusion maps
- Ischemic core segmentation (ADC < 620 × 10⁻⁶ mm²/s for RAPID; deep learning algorithm for JLK PWI)
- Hypoperfused tissue delineation (Tmax >6s threshold)
- Mismatch volume calculation and ratio determination
Statistical Analysis:
- Volumetric agreement: Concordance correlation coefficients, Bland-Altman plots, Pearson correlations
- Clinical decision concordance: Cohen's kappa for EVT eligibility based on DAWN/DEFUSE-3 criteria
- Subgroup analyses: Anterior circulation LVO, late time windows, low NIHSS scores
Predictive Model Development Protocol
Data Collection:
- Cohort: Retrospective enrollment of 515 AIS patients with HTPR [91]
- Variables: 42 feature factors including basic characteristics, blood test indices, CYP2C19 genotype
- Outcome Definition: Poor functional outcome (mRS ≥3) at 3 months
- Data Splitting: Training (80%) and testing (20%) sets with stratification
Feature Preprocessing:
- Data cleaning: Outlier detection using interquartile range (IQR) method
- Missing data imputation: Mean-filling with sensitivity analysis using multiple imputation
- Categorical variable encoding: One-hot encoding for non-ordinal variables
- Data normalization: StandardScaler for continuous variables
- Class imbalance handling: Tomek Links, SMOTE, or random undersampling
Model Training & Evaluation:
- Algorithms: Logistic regression, support vector machine, decision tree, random forest, XGBoost, LightGBM
- Validation: 10-fold cross-validation with repeated hold-out validation
- Interpretability: SHAP values for global and local interpretability
- Performance Metrics: AUC, accuracy, precision, recall, F1-score
The Scientist's Toolkit: Essential Research Reagents
Table 4: Key Research Reagents for AI Stroke Perfusion Studies
| Reagent/Software | Manufacturer/Developer | Primary Function | Validation Status |
|---|---|---|---|
| RAPID | iSchemaView | Reference standard for CTP/MRP analysis | FDA-cleared, extensive validation in clinical trials |
| JLK PWI | JLK Inc., Seoul | Automated MR perfusion analysis | Multicenter validation vs. RAPID (n=299) |
| UGuard | Qianglianzhichuang Technology, Beijing | Automated CTP analysis with deep learning | Comparative validation vs. RAPID (n=159) |
| CINA-HEAD | Avicenna.AI | Multi-step stroke imaging (ICH, LVO, ASPECTS) | FDA-cleared, multicenter diagnostic study |
| Brainomix 360 | Brainomix | AI-based imaging biomarker extraction | 60+ peer-reviewed validations |
| CYP2C19 Genotyping Assay | Multiple | Pharmacogenetic stratification for antiplatelet response | Clinical grade, used in HTPR studies |
AI-driven automated perfusion analysis platforms demonstrate robust real-world performance with high sensitivity, specificity, and clinical concordance for acute stroke evaluation. The validated experimental protocols provide researchers with standardized methodologies for technology assessment, while the comprehensive reagent toolkit facilitates implementation. These advanced analytical capabilities support both clinical trial enrichment through precise patient stratification and therapeutic development through quantitative biomarker assessment. Future directions should focus on prospective multicenter validation, standardization across imaging platforms, and integration of multimodal data for personalized outcome prediction.
Conclusion
The integration of AI-driven automated perfusion analysis marks a paradigm shift in acute stroke care, offering unprecedented speed, accuracy, and standardization in the assessment of ischemic tissue. Evidence from rigorous validation studies demonstrates that emerging platforms like JLK PWI and UGuard show strong agreement with the established benchmark, RAPID, in quantifying ischemic core and penumbra, with direct implications for endovascular therapy selection. The field is rapidly advancing beyond traditional perfusion imaging, with generative AI models now capable of predicting perfusion parameters from non-contrast CT and multi-modal tools enhancing the detection of medium vessel occlusions. For biomedical researchers and drug developers, these technologies provide robust, quantitative biomarkers for patient stratification in clinical trials and the evaluation of novel neuroprotective agents. Future directions must focus on large-scale, prospective multicenter validations, the development of standardized reporting criteria, and the creation of interoperable platforms that can seamlessly integrate into diverse clinical and research ecosystems. The continued evolution of AI in perfusion analysis promises not only to refine individual patient care but also to accelerate the development of next-generation stroke therapeutics through enhanced phenotyping and outcome prediction.
References
- 1. Time is brain--quantified - PubMed [https://pubmed.ncbi.nlm.nih.gov/16339467/]
- 2. A Paradigm Shift in the Management of Acute Ischemic ... [https://pubmed.ncbi.nlm.nih.gov/32037629/]
- 3. World Stroke Organization: Global Stroke Fact Sheet 2025 [https://pmc.ncbi.nlm.nih.gov/articles/PMC11786524/]
- 4. Disparities in Timely Access to Certified Stroke Care ... [https://www.cdc.gov/pcd/issues/2025/24_0429.htm]
- 5. Comparative validation of automated perfusion analysis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620487/]
- 6. AI-Powered Acute Stroke Triage Research Report 2025 [https://www.globenewswire.com/news-release/2025/11/04/3180621/28124/en/AI-Powered-Acute-Stroke-Triage-Research-Report-2025-Market-to-Reach-3-83-Billion-by-2029-at-a-CAGR-of-22-2-Amid-Push-for-Faster-Smarter-Emergency-Care-Global-Long-term-Forecast-to-.html]
- 7. Artificial Intelligence in Stroke Care: A Narrative Review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12570115/]
- 8. Perfusion Magnetic Resonance Imaging - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC4170157/]
- 9. CT Perfusion Imaging [https://www.barrowneuro.org/for-physicians-researchers/education/grand-rounds-publications-media/barrow-quarterly/volume-17-no-3-2001/ct-perfusion-imaging/]
- 10. The basics of diffusion and perfusion imaging in brain tumors [https://pmc.ncbi.nlm.nih.gov/articles/PMC4599787/]
- 11. CT perfusion in oncology: how to do it - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2842179/]
- 12. Utility of automated CT perfusion software in acute ... [https://pubmed.ncbi.nlm.nih.gov/39375881/]
- 13. MR Brain Frameless Stereotactic W or WWO + Perfusion ... [https://www.ohsu.edu/school-of-medicine/diagnostic-radiology/mr-brain-frameless-stereotactic-w-or-wwo-perfusion-neuro]
- 14. Generative Artificial Intelligence to Automate Cerebral ... [https://link.springer.com/article/10.1007/s10278-025-01628-x]
- 15. deepc and mbits Partner to Accelerate Stroke Diagnosis ... [https://www.deepc.ai/news/deepc-and-mbits-partner-to-accelerate-stroke-diagnosis-with-ai-powered-perfusion-analysis]
- 16. Deep Learning in Ischemic Stroke Imaging Analysis [https://pmc.ncbi.nlm.nih.gov/articles/PMC9678444/]
- 17. Frontiers | Comparative validation of automated ... perfusion analysis [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1660870/full]
- 18. A novel machine learning framework for stroke type ... [https://www.nature.com/articles/s41598-025-16660-8]
- 19. RapidAI Stroke Imaging Solutions | Advanced AI for Ischemic Stroke [https://www.rapidai.com/neurovascular/ischemic-stroke]
- 20. Rethinking Clinical AI Applications in Stroke - Pitfalls ... [http://www.j-nn.org/journal/view.php?number=206]
- 21. Evaluating the Safety and Efficacy of Intravenous ... [https://pubmed.ncbi.nlm.nih.gov/41154133/]
- 22. Efficacy and Safety of Intravenous Thrombolysis in the ... [https://www.mdpi.com/2077-0383/14/15/5474]
- 23. A quantitative CT perfusion-derived online dynamic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12465048/]
- 24. Current perspectives on endovascular therapy for large ... [https://www.sciencedirect.com/science/article/pii/S187874792500100X]
- 25. Comparison of Automated MRI Perfusion Analysis Software [https://www.medrxiv.org/content/10.1101/2025.08.07.25333241]
- 26. Brainomix | Triage ICH [https://www.brainomix.com/stroke/triage-ich/]
- 27. Complete Stroke Package | AI Clearance for FDA of LVO Triage [https://www.aidoc.com/learn/blog/stroke-ai/]
- 28. in Radiology: AI Trends, 2025 Approvals & Adoption | IntuitionLabs FDA [https://intuitionlabs.ai/articles/ai-radiology-trends-2025]
- 29. 510(k) Clearance: Methinks FDA Enhances AI with... Stroke Triage [https://med-tech.world/news/fda-510k-methinks-ai-stroke-triage-ct/]
- 30. Performance of an artificial intelligence tool for multi-step ... [https://www.sciencedirect.com/science/article/pii/S2352047725000450]
- 31. Differences in Automated CT Perfusion Software - Viz.ai [https://www.viz.ai/publications/automated-ct-perfusion-software-differences]
- 32. Advanced real-time detection of acute ischemic stroke ... [https://www.nature.com/articles/s41598-025-18997-6]
- 33. Generative Artificial Intelligence to Automate Cerebral ... [https://pubmed.ncbi.nlm.nih.gov/40790003/]
- 34. Holistic AI analysis of hybrid cardiac perfusion images for ... [https://www.nature.com/articles/s41746-025-01526-0]
- 35. The Application of Software “Rapid Processing of Perfusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9688896/]
- 36. RAPID Automated CT Perfusion in Clinical Practice [https://practicalneurology.com/diseases-diagnoses/imaging-testing/rapid-automated-ct-perfusion-in-clinical-practice/31600/]
- 37. Comparative validation of automated perfusion analysis ... [https://pubmed.ncbi.nlm.nih.gov/41255820/]
- 38. Validation of a novel CT perfusion software compared to ... [https://www.nature.com/articles/s41598-025-96340-9]
- 39. AI image analysis: mRay-VEOcore [https://mbits.info/en/perfusionsanalyse/]
- 40. Performance of automated CT ASPECTS in comparison ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8485462/]
- 41. Performance of automated CT ASPECTS in comparison to ... [https://www.springermedizin.de/performance-of-automated-ct-aspects-in-comparison-to-physicians-/25792024]
- 42. A Narrative Review on Collateral Circulation Classification ... [https://www.sciencedirect.com/science/article/pii/S2590123025036369]
- 43. Automated Emergent Large Vessel Occlusion Detection Using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12596299/]
- 44. Collateral Status Evaluation Using CT Angiography and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12563574/]
- 45. A Practical Guide to CT Perfusion Interpretation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12571803/]
- 46. Leveraging non-contrast head CT to improve the image ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7754793/]
- 47. CT perfusion (CTP) [https://www.stroke-manual.com/ct-perfusion-ctp-stroke/]
- 48. Non-inferiority of deep learning ischemic stroke ... - Nature [https://www.nature.com/articles/s41598-023-42961-x]
- 49. Deep learning derived automated ASPECTS on non ... [https://pubmed.ncbi.nlm.nih.gov/35357053/]
- 50. Quantitative evaluation method of stroke association based ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2025.1544372/full]
- 51. AHA Foundational Requirements for Stroke Programs [https://www.aidoc.com/learn/blog/aha-guidelines-one-year-later/]
- 52. Performance of an artificial intelligence tool for multi-step ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12419105/]
- 53. Prospective Evaluation of Artificial Intelligence Imaging ... [https://www.sciencedirect.com/science/article/pii/S2542454825000426]
- 54. Assessing the accuracy of automated CT perfusion ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12615249/]
- 55. Direct to hybrid CT-angiosuite (Nexaris) reduces treatment ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12380727/]
- 56. Direct to hybrid CT-angiosuite (Nexaris) reduces treatment ... [https://pubmed.ncbi.nlm.nih.gov/40856694/]
- 57. Effect of early neuroendovascular team involvement in ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1568572/full]
- 58. Session Report - Stroke Imaging 2025 [https://eso-stroke.org/blog-session-stroke-imaging/]
- 59. “Code-Stroke” CT Perfusion; Challenges and Pitfalls [https://www.sciencedirect.com/science/article/abs/pii/S1076633219300066]
- 60. Assessing the accuracy of automated CT perfusion ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1613078/full]
- 61. Contrast bolus timing in CT-angiography and CT-perfusion [https://pmc.ncbi.nlm.nih.gov/articles/PMC12125062/]
- 62. Assessing bolus peak position in CT perfusion [https://www.sciencedirect.com/science/article/pii/S0720048X24003115]
- 63. Flow cytometry and stroke: from current methodology to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8820698/]
- 64. Understanding Success Criterion 1.4.3: Contrast (Minimum) [https://www.w3.org/WAI/WCAG21/Understanding/contrast-minimum.html]
- 65. Standardizing the estimation of ischemic regions can ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10853359/]
- 66. Editorial: Advancing precision medicine in acute stroke care [https://pmc.ncbi.nlm.nih.gov/articles/PMC12643980/]
- 67. Optimizing Radiation Dose and Image Quality in Stroke CT ... [https://www.mdpi.com/2075-4418/14/24/2866]
- 68. Portable ultra-low-field MRI in acute stroke care: A pilot study [https://pmc.ncbi.nlm.nih.gov/articles/PMC12170540/]
- 69. Healthcare organizations can't ignore interoperability in 2025 [https://healthcareintegrations.com/why-healthcare-organizations-cant-ignore-interoperability-in-2025/]
- 70. Interoperable Exchange of Patient Health Information Among ... [https://www.ncbi.nlm.nih.gov/books/NBK606033/]
- 71. Interoperability in Healthcare Explained [https://www.oracle.com/health/interoperability-healthcare/]
- 72. Why Your Hospital PACS Strategy Could Make or Break ... [https://sarcmediq.com/hospital-pacs/]
- 73. The Cloud and Imaging in Healthcare: 2025 Outlook [https://dcmsys.com/project/the-cloud-and-imaging-in-healthcare-2024-outlook/]
- 74. Artificial Intelligence in Software as a Medical Device [https://www.fda.gov/medical-devices/software-medical-device-samd/artificial-intelligence-software-medical-device]
- 75. AI Medical Devices: 2025 Status, Regulation & Challenges [https://intuitionlabs.ai/articles/ai-medical-devices-regulation-2025]
- 76. Artificial Intelligence in Stroke Care: A Narrative Review of ... [https://pubmed.ncbi.nlm.nih.gov/41170263/?utm_source=FeedFetcher&utm_medium=rss&utm_campaign=None&utm_content=0nK-FGmcPzruPpJferMpyd8mRld7hsB1ra05TRUDXN6&fc=None&ff=20251031131406&v=2.18.0.post22+67771e2]
- 77. New Study Finds RapidAI Significantly Outperforms Viz.ai ... [https://www.biospace.com/press-releases/new-study-finds-rapidai-significantly-outperforms-viz-ai-in-detecting-medium-vessel-occlusions-in-stroke-patients]
- 78. A retrospective analysis comparing AIDoc and RAPIDAI in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12164790/]
- 79. A novel approach to CT perfusion analysis in acute ... [https://www.sciencedirect.com/science/article/pii/S1361841523002311]
- 80. Quantitative Measures of Pure Ground-Glass Nodules from an ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12292494/]
- 81. Lung volume segmentation in fetal MRI: super-resolution ... [https://eurradiolexp.springeropen.com/articles/10.1186/s41747-025-00628-4]
- 82. Cohen's kappa [https://en.wikipedia.org/wiki/Cohen%27s_kappa]
- 83. Interrater reliability: the kappa statistic - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3900052/]
- 84. - AI Imaging Biomarkers Powered Recovery Outcomes in... Predict [https://medicaldialogues.in/neurology-neurosurgery/news/ai-powered-imaging-biomarkers-predict-recovery-outcomes-in-acute-ischemic-stroke-study-finds-146197]
- 85. - Predicting prognosis for patients with 90 : a machine... day stroke [https://pmc.ncbi.nlm.nih.gov/articles/PMC10748594/]
- 86. Interpretable Machine Learning Modeling for Ischemic ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2022.884693/full]
- 87. A multimodal multitask deep learning model for predicting ... [https://www.nature.com/articles/s41598-025-21945-z]
- 88. Short-term NIHSS score prediction using AI model with chat GPT... [https://link.springer.com/article/10.1007/s44337-025-00393-8]
- 89. Machine learning-based prediction of 90-day prognosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12064682/]
- 90. AI can identify stroke types using clinical notes, study shows [https://www.utsouthwestern.edu/newsroom/articles/year-2025/oct-ai-strokes.html]
- 91. Prediction of the short-term prognosis of acute ischaemic ... [https://www.nature.com/articles/s41598-025-20763-7]
- 92. AI post-intervention operational and functional outcomes ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-025-01864-1]