Synthetic Control Arms vs. Traditional Designs: The Future of Neuroscience Clinical Trials
This article provides a comprehensive analysis for researchers and drug development professionals on the paradigm shift from traditional randomized control trials (RCTs) to synthetic control arms (SCAs) in neuroscience.
Synthetic Control Arms vs. Traditional Designs: The Future of Neuroscience Clinical Trials
Abstract
This article provides a comprehensive analysis for researchers and drug development professionals on the paradigm shift from traditional randomized control trials (RCTs) to synthetic control arms (SCAs) in neuroscience. It explores the foundational principles of SCAs, detailing their construction from real-world data and historical trial datasets. The content covers practical methodological applications across neurodegenerative, psychiatric, and rare neurological diseases, supported by case studies. It further addresses critical troubleshooting strategies for mitigating bias and optimizing data quality, and presents a rigorous validation framework comparing the efficacy, ethical, and economic outcomes of SCAs against traditional designs. The synthesis offers actionable insights for designing more efficient, patient-centric, and successful neuroscience trials.
Synthetic Control Arms 101: Redefining Clinical Trial Foundations in Neuroscience
In clinical trials, a control arm is the group of participants that does not receive the investigational therapy being studied, serving as a comparison benchmark to evaluate whether the new treatment is safe and effective [1] [2]. These control groups provide critical context, helping researchers determine if observed outcomes result from the experimental intervention or other factors such as natural disease progression or placebo effects [3]. The fundamental principle of controlled trials enables discrimination of patient outcomes caused by the investigational treatment from those arising from other confounding variables [3].
Traditional Randomized Controlled Trials (RCTs) remain the gold standard for clinical research, where participants are randomly assigned to either treatment or control arms, balancing both known and unknown confounding factors to ensure valid conclusions [4] [3]. However, evolving methodological approaches have introduced innovative alternatives like synthetic control arms (SCAs) that leverage external data sources to optimize trial efficiency and accelerate drug development, particularly valuable in rare diseases or complex conditions where recruitment challenges exist [4] [5].
Defining Traditional Control Arms
Traditional control arms constitute groups of participants within the same clinical trial who receive a reference treatment rather than the investigational therapy. These concurrent controls enable direct comparison under identical study conditions and timeframes [3]. Several standardized control arm methodologies have been established in clinical research, each with specific applications and implementation considerations.
Types of Traditional Control Arms
Placebo Concurrent Control: Placebos are inert substances or interventions designed to simulate medical therapy without specificity for the condition being treated [3]. They must share identical appearance, frequency, and formulation as the active drug to maintain blinding. Placebo controls help discriminate outcomes due to the investigational intervention from outcomes attributable to other factors and are used to demonstrate superiority or equivalence [3]. Ethical considerations restrict their use to situations where no effective treatment exists and no permanent harm (death or irreversible morbidity) would result from delaying available active treatment for the trial duration [3].
Active Treatment Concurrent Control: This design compares a new drug to an established standard therapy or evaluates a combination of new and standard therapies versus standard therapy alone [3]. The active comparator should preferably represent the current standard of care. This approach can demonstrate equivalence, non-inferiority, or superiority and is considered most ethical when approved treatments exist for the disease under study [3]. The Declaration of Helsinki mandates using standard treatments as controls when available [3].
No Treatment Concurrent Control: In this design, no intervention is administered to the control arm, requiring objective study endpoints to minimize observer bias [3]. The inability to blind participants and researchers to treatment assignment represents a significant limitation, as knowledge of who is receiving no treatment may influence outcome assessment and reporting [3].
Dose-Comparison Concurrent Control: Different doses or regimens of the same treatment serve as active and control arms in this design, establishing relationships between dosage and efficacy/safety profiles [3]. This approach may include active and placebo groups alongside different dose groups but can prove inefficient if the drug's therapeutic range is unknown before trial initiation [3].
Methodological Variations in Controlled Trials
Several specialized trial designs incorporate control arms in unique configurations to address specific research scenarios:
Add-on Design: All patients receive standard treatment, with the experimental therapy or placebo added to this background therapy [3]. This design measures incremental benefit beyond established treatments but may require large sample sizes if the additional improvement is modest [3].
Early Escape Design: Patients meeting predefined negative efficacy criteria are immediately withdrawn from the study to minimize exposure to ineffective treatments [3]. The time to withdrawal serves as the primary outcome variable, though this approach may sacrifice statistical power and primarily evaluates short-term efficacy [3].
Double-Dummy Technique: When comparator interventions differ in nature (e.g., oral versus injectable), both groups receive both a active and placebo formulation to maintain blinding [3]. For example, one group receives active drug A with placebo matching drug B, while the other receives active drug B with placebo matching drug A [3].
Table 1: Traditional Control Arm Types and Characteristics
| Control Arm Type | Key Features | Primary Applications | Ethical Considerations |
|---|---|---|---|
| Placebo Control | Inert substance matching investigational treatment; maintains blinding | Superiority trials; conditions with no established treatment | Only justified when withholding treatment causes no permanent harm |
| Active Treatment Control | Established standard of care as comparator | Equivalence, non-inferiority, or superiority trials | Preferred when effective treatments exist; aligns with Declaration of Helsinki |
| No Treatment Control | No intervention administered; requires objective endpoints | Conditions where placebo effect is minimal | Challenging for blinding; may raise ethical concerns if effective treatment exists |
| Dose-Comparison Control | Different doses or regimens of same intervention | Dose-response relationship establishment | All participants receive active treatment, just at different levels |
Defining Synthetic Control Arms
Synthetic control arms (SCAs) represent an innovative methodology that utilizes external data sources to construct comparator groups, reducing or potentially eliminating the need for concurrent placebo or standard-of-care control arms within the same trial [4] [5]. Also known as external control arms, SCAs are generated using statistical methods applied to one or more external data sources, such as results from separate clinical trials or real-world data (RWD) [5]. The FDA defines external controls as any control group not part of the same randomized study as the group receiving the investigational therapy [5].
SCAs are particularly valuable when traditional RCTs with concurrent control arms present ethical concerns, practical difficulties, or feasibility challenges [5]. By leveraging existing data, SCAs can provide supportive evidence that contextualizes treatment effects and safety profiles in situations where this information would not otherwise be available, especially in single-arm trials [5]. Regulatory agencies including the FDA and EMA have increasingly accepted RWD-based SCAs, recognizing their value in modern clinical development, particularly for rare diseases and serious conditions with unmet medical needs [4] [6].
SCAs are constructed using patient-level data from patients not involved in the investigational clinical trial, with these external patients "matched" to the experimental participants using statistical methods to achieve balanced baseline characteristics [5]:
Historical Clinical Trial Data: Data from previous clinical trials provides highly standardized, quality-controlled information, though it may not fully represent the broader patient population due to recruitment biases [5].
Real-World Data (RWD): RWD originates from routine clinical practice through electronic health records, insurance claims, patient registries, and other healthcare sources [4] [5]. While offering higher volume and greater diversity, RWD often requires more processing to standardize formats and address missing data elements [5].
Combined Data Approaches: Mixed SCAs integrate both clinical trial and real-world data sources to maximize population matching and statistical power, as demonstrated in a 2025 DLBCL lymphoma study that combined data from the LNH09-7B trial and the REALYSA real-world observational cohort [7].
Methodological Framework for Synthetic Control Arms
Constructing valid SCAs requires rigorous statistical methodologies to minimize bias and ensure comparable groups [5] [6]:
Propensity Score Matching (PSM): This statistical technique estimates the probability of a patient receiving the investigational treatment based on observed baseline characteristics, creating balanced groups by matching trial participants with similar individuals from external data sources [5] [7].
Inverse Probability of Treatment Weighting (IPTW): Using propensity scores, IPTW assigns weights to patients in the external control group to create a synthetic population that resembles the baseline characteristics of the trial participants [7]. Stabilized IPTW (sIPTW) variants help minimize variance in the weighted population [7].
Covariate Balance Assessment: After applying matching or weighting methods, researchers assess balance using standardized mean differences (SMD) for each covariate included in the propensity score model, with SMD <0.1 generally indicating adequate balance [7].
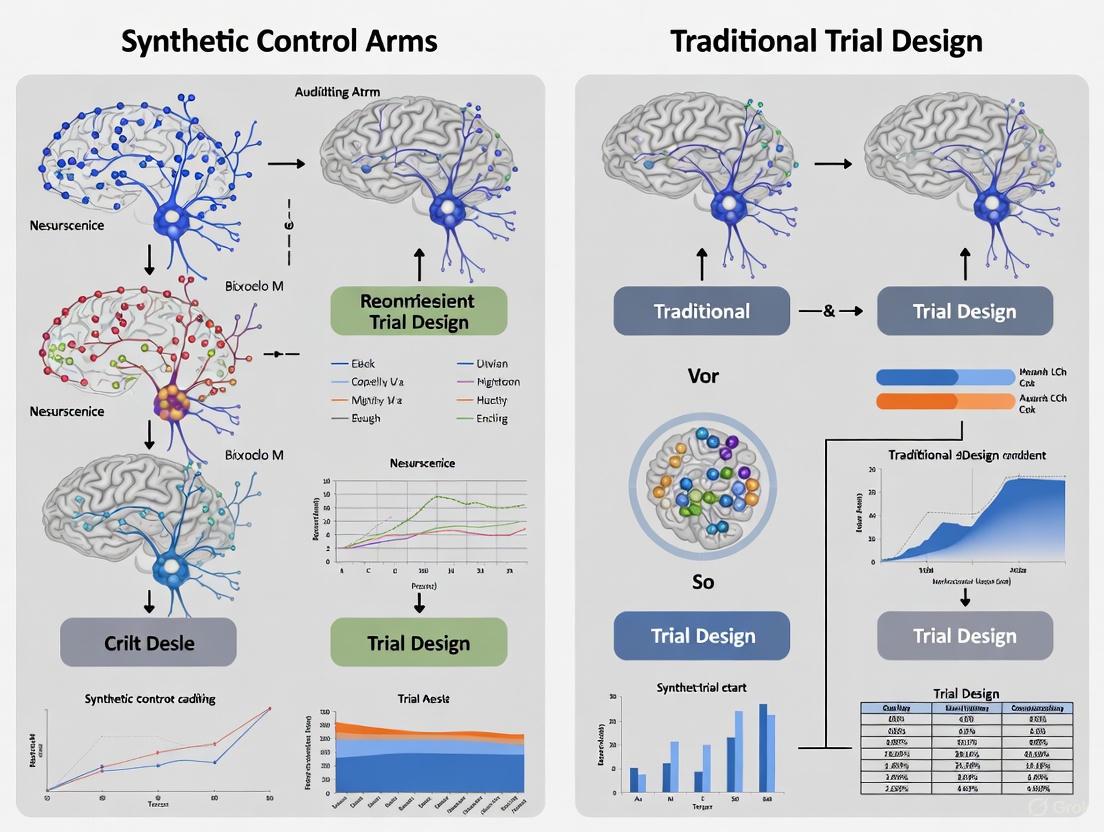
The following diagram illustrates the comprehensive workflow for constructing and validating synthetic control arms:
Comparative Analysis: Synthetic vs. Traditional Control Arms
Advantages and Limitations
Table 2: Comprehensive Comparison of Synthetic vs. Traditional Control Arms
| Characteristic | Traditional Control Arms | Synthetic Control Arms |
|---|---|---|
| Ethical Considerations | Ethical concerns when assigning patients to placebo in life-threatening conditions with no clear standard of care [4] | Reduces ethical concerns by ensuring all trial participants receive active treatment [4] |
| Recruitment & Timelines | Recruiting control-arm patients can be difficult, leading to extended timelines, especially in rare diseases [4] [5] | Accelerates development by reducing need to recruit control patients; shortens trial durations [4] |
| Cost Implications | Higher costs associated with recruiting, randomizing, and following control-arm patients [5] | More cost-effective by avoiding expenses related to control patient recruitment and trial conduct [5] |
| Generalizability | May lack diversity and representativeness due to strict inclusion criteria [4] | Enhances generalizability through diverse real-world populations from multiple geographies [4] |
| Data Quality | Highly standardized data collection with consistent quality [5] | Variable quality depending on source; missing data and standardization challenges [5] |
| Bias Control | Randomization balances both known and unknown confounding factors [3] | Potential for selection bias if external data unrepresentative; only addresses measured confounders [5] |
| Regulatory Acceptance | Established regulatory pathway with clear expectations [3] | Growing acceptance but requires robust justification and validation [5] [6] |
| Methodological Flexibility | Limited flexibility once trial begins | Can incorporate multiple data sources and adapt to new information [5] |
Application Contexts and Appropriateness
The decision between synthetic and traditional control arms depends heavily on specific research contexts and constraints:
Rare Diseases and Precision Medicine: SCAs offer particular value in rare diseases where recruiting sufficient control patients presents significant challenges [4] [6]. Similarly, in precision medicine with genetically defined subpopulations, SCAs can provide historical comparators when concurrent randomization proves impractical [6].
Oncology Applications: SCAs have gained traction in oncology, where rapid treatment advances may render concurrent controls ethically problematic when superior alternatives emerge during trial conduct [5] [6]. Regulatory approvals have been granted for several oncology treatments based partially on synthetic control evidence [6].
Neuroscience Research Context: For neuroscience applications, particularly in neurodegenerative diseases with progressive courses and limited treatments, SCAs may address ethical concerns about placebo assignment while providing meaningful comparative data [4] [6]. However, careful attention to outcome measurement standardization is essential, as many neurological endpoints involve functional assessments potentially influenced by observer bias [3].
Experimental Evidence and Validation Studies
Case Study: DLBCL Lymphoma Research (2025)
A November 2025 study demonstrated the application of mixed synthetic control arms for elderly patients (≥80 years) with newly diagnosed diffuse large B-cell lymphoma (DLBCL), a population typically underrepresented in clinical trials [7]. The research aimed to validate SCAs by reconstructing the control arm of the SENIOR randomized trial using external data sources.
Methodology:
- Data Sources: Combined real-world data from the REALYSA observational cohort (n=127) with historical clinical trial data from the LNH09-7B trial (n=149) to create a mixed SCA [7].
- Patient Matching: Used stabilized Inverse Probability of Treatment Weighting (sIPTW) based on propensity scores to balance baseline characteristics including sex, age, disease stage, performance status, and international prognostic index score [7].
- Endpoint: Overall survival (OS) censored at 24 months to address follow-up duration disparities [7].
- Missing Data Handling: Employed multiple imputation with 15 imputations per patient for covariates with substantial missing values in the real-world cohort [7].
Results: The synthetic control arm demonstrated comparable performance to the internal control arm of the SENIOR trial. After weighting, all covariates showed good balance with standardized mean differences <0.1. The hazard ratio for overall survival comparing the mixed SCA to the SENIOR experimental arm was 0.743 (95% CI: 0.494-1.118, p=0.1654), not statistically different from the original SENIOR results [7]. Sensitivity analyses using only real-world data and different missing data management approaches yielded consistent findings, supporting methodological robustness [7].
Regulatory Precedents and Historical Applications
Several regulatory decisions have established precedents for synthetic control arm acceptance:
Cerliponase Alfa Approval: The FDA approved cerliponase alfa for a specific form of Batten disease based on a synthetic control study comparing 22 patients from a single-arm trial against an external control group of 42 untreated patients [6].
Alectinib Label Expansion: Across 20 European countries, alectinib (a non-small cell lung cancer treatment) received expanded labeling based on a synthetic control study using external data from 67 patients [6].
Palbociclib Indication Expansion: The kinase inhibitor palbociclib gained an expanded indication for men with HR+, HER2-advanced or metastatic breast cancer based on external control data [6].
Implementation Considerations and Research Toolkit
Essential Methodological Components
Successfully implementing synthetic control arms requires careful attention to several methodological components:
Propensity Score Estimation: The foundation of valid SCA construction, involving logistic regression with carefully selected covariates that potentially influence both treatment assignment and outcomes [7]. Key covariates typically include demographic factors, disease characteristics, prognostic indicators, and prior treatment history [7].
Balance Diagnostics: After applying weighting or matching methods, researchers must quantitatively assess covariate balance between the investigational arm and the synthetic control using standardized mean differences, with values <0.1 generally indicating adequate balance [7].
Sensitivity Analyses: Comprehensive sensitivity analyses testing different statistical approaches, inclusion criteria, and missing data handling methods are essential to demonstrate result robustness [6] [7].
Regulatory and Protocol Considerations
Engaging regulatory agencies early when considering synthetic control arms is strongly recommended by the FDA, EMA, and MHRA [5]. Regulatory submissions should include:
- Justification for the proposed study design and reasons why traditional randomization is impractical or unethical [5]
- Detailed description of all data sources accessed with rationale for source selection and exclusion [5]
- Proposed statistical analysis plan with methodologies for addressing potential biases [5]
- Comprehensive data management plan and submission strategy for agency review [5]
Table 3: Research Reagent Solutions for Control Arm Implementation
| Research Component | Purpose/Function | Implementation Considerations |
|---|---|---|
| High-Quality RWD Sources | Provides real-world patient data for SCA construction | Verify data quality, completeness, and relevance to target population; assess longitudinal follow-up [4] [5] |
| Propensity Score Methods | Statistical balancing of baseline characteristics | Select appropriate covariates; choose between matching, weighting, or stratification approaches [5] [7] |
| Multiple Imputation Techniques | Handles missing data in real-world sources | Determine appropriate imputation models; assess impact of missing data patterns [7] |
| Sensitivity Analysis Framework | Tests robustness of findings to methodological choices | Plan varied analytical approaches; assess impact of different assumptions [6] [7] |
| Regulatory Engagement Strategy | Facilitates agency feedback and acceptance | Prepare comprehensive briefing documents; schedule early meetings [5] |
Synthetic control arms represent a significant methodological advancement in clinical trial design, offering a viable alternative to traditional concurrent control arms in specific circumstances. While traditional RCTs with internal control arms remain the gold standard for establishing efficacy due to randomization's unique ability to balance both known and unknown confounders [3], SCAs provide a valuable approach when ethical, practical, or feasibility concerns limit traditional trial conduct [4] [5].
The growing regulatory acceptance of synthetic control methodologies reflects their potential to address challenging research scenarios, particularly in rare diseases, precision medicine applications, and situations where established standards of care make randomization ethically problematic [6] [7]. As real-world data sources continue to expand in quality and comprehensiveness, and statistical methodologies for leveraging these data become increasingly sophisticated, the appropriate application of synthetic control arms will likely continue to expand, offering promising opportunities to accelerate therapeutic development while maintaining scientific rigor.
The pursuit of novel therapeutics for complex neurological disorders is increasingly hampered by the methodological and ethical constraints of traditional randomized controlled trials (RCTs). Challenges such as patient recruitment, ethical concerns with placebo arms, and extensive heterogeneity in rare diseases are particularly acute in neuroscience. This review objectively compares the performance of an innovative alternative—synthetic control arms (SCAs)—against traditional trial designs. We synthesize current experimental data and regulatory guidance to demonstrate that SCAs, which use external data sources to construct virtual control groups, offer a viable path for accelerating drug development while maintaining scientific rigor in neurological research.
Neuroscience drug development faces a perfect storm of methodological challenges. Rare diseases with small patient populations, such as spinal cord injury (SCI), make recruiting for traditional RCTs difficult and sometimes impractical [8]. Furthermore, the ethical dilemma of assigning patients to placebo or substandard care in life-threatening or severely debilitating conditions creates significant barriers to trial participation and completion [5] [9]. The extensive heterogeneity in the clinical presentation and recovery trajectories of many neurological disorders further complicates the creation of well-matched control groups through randomization alone [8]. These limitations collectively underscore why traditional trials are reaching their practical and ethical limits in neuroscience, necessitating a paradigm shift toward more innovative designs.
Head-to-Head: Synthetic Control Arms vs. Traditional Randomized Trials
The following analysis compares the core characteristics, performance metrics, and applicability of synthetic control arms against traditional randomized trial designs.
Table 1: Comparative Analysis of Trial Designs
| Feature | Traditional Randomized Controlled Trial (RCT) | Synthetic Control Arm (SCA) |
|---|---|---|
| Core Methodology | Prospective randomization of patients to investigational or concurrent control arm [10]. | External data (historical trials, RWD) analyzed to create a virtual control group matched to the investigational arm [10] [5]. |
| Control Group Source | Patients recruited and treated concurrently within the same study [11]. | Real-world data (RWD), historical clinical trial data, registry data [10] [5] [4]. |
| Typical Trial Duration | Longer, due to the need to recruit and follow a full control cohort [9]. | Shorter, attributed to faster recruitment as all trial patients receive the investigational treatment [9] [4]. |
| Ethical Concerns | Higher; patients may be assigned to a placebo or inferior standard of care, which can deter participation [5] [6]. | Lower; all enrolled patients receive the investigational therapy, removing the placebo dilemma [9] [4]. |
| Patient Recruitment | Challenging, especially for rare diseases; ~50% of patients may not receive the active drug [9]. | Easier; as all patients receive the active drug, participation is more attractive [5] [9]. |
| Primary Regulatory Challenge | Maintaining clinical equipoise and managing high costs/delays [6]. | Demonstrating control arm comparability and mitigating unknown confounding and bias [10] [5]. |
| Ideal Application | Common diseases with established standards of care and large available populations. | Rare diseases, severe conditions with unmet medical need, and orphan diseases [10] [5] [8]. |
Table 2: Quantitative Performance Metrics from Experimental Data
| Performance Metric | Traditional RCT (Typical Range) | Synthetic Control Arm (Evidence from Research) |
|---|---|---|
| Cohort Size Requirement | Requires full control cohort (often 1:1 ratio) [6]. | No or significantly fewer concurrent control patients needed; one Phase II case reduced trial size using SCA-informed sizing [10]. |
| Data Quality & Standardization | High, due to controlled, prospective, and protocol-driven data collection [5]. | Variable; high if built from historical clinical trial data, but can be lower with RWD due to missing data or formatting issues [10] [5]. |
| Risk of Bias | Low risk of selection and confounding bias due to randomization. | Risk of unknown confounding and selection bias is a key concern, mitigated via statistical methods [10] [5]. |
| Predictive Accuracy (Case Study) | N/A (Baseline) | In a spinal cord injury model, a convolutional neural network predicting recovery achieved a median RMSE of 0.55 for motor scores, showing no significant difference from randomized controls in simulation [8]. |
| Regulatory Precedence | Established gold standard for decades. | Growing acceptance; FDA and EMA have approved drugs using SCA data, particularly in oncology and rare diseases [10] [6]. |
Experimental Protocols: How Synthetic Control Arms Are Built and Validated
The construction of a regulatory-grade synthetic control arm is a multi-stage process that relies on robust data and rigorous methodology.
Core Methodology and Workflow
The process begins with the acquisition and curation of high-quality external data, followed by patient matching and statistical analysis to create a virtual cohort for comparison.
Detailed Protocol: Building a Machine Learning-Driven SCA for Spinal Cord Injury
A 2025 study on spinal cord injury (SCI) provides a template for a data-driven SCA protocol [8].
- Objective: To generate synthetic controls from personalized predictions of neurological recovery for use in single-arm trials for acute traumatic SCI.
- Data Sources:
- Primary Cohort: Data from 4,196 patients from the European Multicenter Study about Spinal Cord Injury (EMSCI).
- External Validation: Data from 587 patients from the historical Sygen trial.
- Input Data: International Standards for Neurological Classification of SCI (ISNCSCI) assessments, including segmental motor scores (MS), light touch scores (LTS), pinprick scores (PPS), AIS grade, and neurological level of injury (NLI). Patient age, sex, and time of assessment were also included.
- Model Benchmarking: Six prediction architectures were trained and compared:
- Regularized linear regression
- Random forest
- Extreme gradient-boosted trees (XGBoost)
- Convolutional Neural Network (CNN)
- Sequence-to-sequence transformers
- Graph Neural Networks (GNN)
- Performance Evaluation: Model performance was quantified using the root mean squared error (RMSE) between true and predicted segmental motor scores below the initial neurological level of injury (RMSEbl.NLI).
- Validation: The best-performing model was applied in a simulation framework to model the randomization process and in a case study re-evaluating the completed NISCI trial as a single-arm trial post hoc.
The Scientist's Toolkit: Research Reagent Solutions for SCA Implementation
| Tool / Resource | Function & Application | Example / Key Feature |
|---|---|---|
| High-Quality RWD Sources | Provide the raw, real-world data from clinical practice used to build the control population. | IRIS Registry (Ophthalmology), AUA AQUA Registry (Urology); Verana Health curates data from over 90 million de-identified patients [4]. |
| Historical Clinical Trial Data | Provides a source of high-quality, standardized control data with less missing information. | Data from previous RCTs in the same disease area, such as the Sygen trial for spinal cord injury [10] [8]. |
| Propensity Score Matching | A statistical method to balance baseline characteristics between the investigational arm and the external control pool, reducing selection bias. | Creates an "apples-to-apples" comparison by matching patients on key prognostic factors [5]. |
| Machine Learning Models | Advanced algorithms to predict patient outcomes and create more precise, individualized counterfactuals. | Convolutional Neural Networks (CNNs) for predicting sequential motor score recovery [8]. |
| Sensitivity Analysis Frameworks | Assess the robustness of the trial's conclusions by testing how they hold up under different assumptions about unmeasured confounding. | "Tipping point" analyses to determine how much unmeasured confounding would be needed to alter the study's primary finding [10]. |
Signaling Pathways in Trial Design: A Conceptual Workflow
The decision to employ a synthetic control arm is not arbitrary. It follows a logical pathway based on specific trial constraints and scientific requirements. The following diagram outlines the key decision points and methodological branches in modern clinical trial design.
Discussion and Future Directions
Synthetic control arms represent a significant evolution in clinical trial methodology, particularly suited to the pressing challenges of neuroscience research. While traditional RCTs remain the gold standard where feasible, the evidence indicates that SCAs are a scientifically valid and ethically superior alternative in contexts of high unmet medical need, rarity, and heterogeneity [10] [8]. Regulatory bodies like the FDA and EMA are increasingly receptive to this approach, especially when supported by high-quality data and robust statistical methods that address potential confounding [5] [6].
The future of SCAs lies not only in full replacement of control arms but also in hybrid designs, where a small randomized control arm is supplemented with synthetic control patients [10]. This hybrid model can bolster confidence in the results by allowing a direct comparison between randomized controls and external data patients. As machine learning models for outcome prediction become more sophisticated and real-world data sources continue to grow in quality and scope, the adoption of synthetic control arms is poised to accelerate, helping to bring effective neurological therapies to patients faster and more efficiently.
Synthetic control arms (SCAs) are transforming clinical trial design by using existing data to create virtual control groups, offering a powerful alternative to traditional randomized control arms. In neuroscience research, where patient recruitment is challenging and placebo groups can raise ethical concerns, SCAs provide a pathway to more efficient and robust comparative studies. The foundation of any effective SCA lies in the strategic use of two primary data sources: clinical trial repositories and real-world evidence (RWE).
This guide objectively compares the performance characteristics of these data sources and the platforms that provide them, supported by current experimental data and methodological insights.
Composing a Synthetic Control Arm: Source Data and Workflow
Constructing a SCA is a multi-stage process that relies on robust data and rigorous statistical methods to ensure the virtual control group is comparable to the interventional arm. The following diagram illustrates the key stages, from raw data sourcing to the final analysis-ready SCA.
Synthetic Control Arm Construction Workflow
The validity of a SCA hinges on the quality and appropriateness of its underlying data. The two principal sources—historical clinical trial data and real-world data (RWD)—offer complementary strengths and weaknesses.
Table 1: Comparison of Primary Data Sources for Synthetic Control Arms
| Characteristic | Historical Clinical Trial Data | Real-World Data (RWD) |
|---|---|---|
| Data Standardization & Quality | Highly standardized; consistent collection; generally low missing data [5] | Variable formats and quality; requires extensive processing; potential for missing data [5] |
| Patient Population Representativeness | Can suffer from recruitment bias; may under-represent elderly, certain ethnic, or socio-economic groups [5] | Broader representation of real-world demographics and clinical practice [12] |
| Data Volume & Diversity | Lower volume; limited to specific trial protocols and populations [5] | Higher volume; captures diverse treatment patterns and comorbidities [13] |
| Primary Strengths | High internal validity due to controlled collection; familiar to regulators [5] | High external validity/generalizability; large sample sizes [13] [12] |
| Key Limitations | May not reflect current standard of care or broader patient populations [5] | Potential for unmeasured confounding; data curation is resource-intensive [5] [14] |
Market analysis indicates that RWD is the dominant data source for SCAs, holding a 53.5% market share in 2024 due to its volume and real-world applicability. However, the hybrid approach (RWD + Historical Trial Data) is expected to be the fastest-growing segment, as it can mitigate the limitations of using either source alone [14].
Key Platform Vendors and Technology Solutions
Specialized technology platforms are essential for curating, managing, and analyzing the complex data required for SCAs. The table below summarizes leading providers of real-world evidence and clinical data solutions.
Table 2: Key RWE and Clinical Data Platform Vendors
| Provider | Core Technology & Data Focus | Reported Applications & Differentiators |
|---|---|---|
| IQVIA | Large-scale, multi-source RWE analytics; one of the largest global longitudinal datasets [15] [16] | Supports regulatory and payer evidence needs; uses AI/ML for outcome prediction [16] [17] |
| Flatiron Health | Oncology-focused RWE platform; data from a network of oncology clinics and EHRs [15] [16] | High-quality, structured oncology data; demonstrated use in FDA-accepted SCAs (e.g., in NSCLC) [14] [16] |
| Aetion | Transparent and validated real-world analytics platform with a focus on regulatory-grade evidence [16] | Emphasizes reproducibility and audit trails; used by regulators like FDA and EMA for policy simulations [16] |
| Optum Life Sciences | Integrated healthcare data from claims, EHRs, and provider networks; strong payer perspective [15] [16] | Expertise in health economics and U.S. payer insights; robust data for cost and utilization analyses [16] |
| TriNetX | Global health research network providing access to EHR data from healthcare organizations [15] | Platform facilitates cohort discovery and feasibility analysis for clinical trials [15] |
The adoption of AI/ML analytics platforms is a key technological trend, as they are crucial for analyzing vast datasets to create well-matched synthetic control groups. This technology segment held the largest share (37.5%) of the SCA market in 2024 [14].
Experimental Protocol for SCA Validation: A Case Study in DLBCL
A 2025 study on diffuse large B-cell lymphoma (DLBCL) in elderly patients provides a robust, real-world example of SCA construction and validation, offering a template for neuroscience applications [7].
Objective
To build and validate a mixed SCA from real-world and clinical trial data for patients aged ≥80 years with newly diagnosed DLBCL, and to assess if it could replicate the results of the SENIOR randomized controlled trial (RCT) [7].
- Real-World Data (RWD): Patient-level data from the REALYSA observational cohort [7].
- Historical Clinical Trial Data: Data from the LNH09-7B clinical trial [7].
- Validation Data: Data from the SENIOR RCT (used as the benchmark for comparison) [7].
Methodology
- Patient Matching: Patients from the SCA sources (REALYSA and LNH09-7B) were matched to the SENIOR trial arms based on key covariates, including sex, age, disease stage, performance status, and other prognostic factors [7].
- Statistical Harmonization - sIPTW: A stabilized Inverse Probability of Treatment Weighting (sIPTW) approach was used to balance the covariates between the SCA and the SENior trial arms. This technique weights patients based on their propensity scores to create a balanced synthetic cohort [7].
- Endpoint Analysis: The primary endpoint was Overall Survival (OS), censored at 24 months. The hazard ratio (HR) between the SCA and the SENIOR experimental arm was calculated [7].
Results and Validation
The SCA successfully replicated the results of the original RCT. The analysis showed no statistically significant difference in overall survival between the SCA and the SENIOR experimental arm, with a Hazard Ratio of 0.743 [0.494-1.118] (p = 0.1654). This confidence interval overlapped with that of the original SENIOR trial, confirming the SCA's ability to mimic the internal control arm [7].
The Scientist's Toolkit: Essential Reagents for SCA Research
Building a regulatory-grade SCA requires a suite of methodological and technological "reagents."
Table 3: Essential Research Reagents for SCA Development
| Tool / Solution | Function in SCA Research |
|---|---|
| Propensity Score Matching (PSM) | A statistical method to reduce selection bias by matching each patient in the treatment arm with one or more patients from external data sources with similar observed characteristics [5] [12]. |
| Stabilized Inverse Probability of Treatment Weighting (sIPTW) | A weighting technique used to balance covariate distributions between the treatment and synthetic control arm, improving the validity of comparative outcomes [7]. |
| AI/ML Analytics Platforms | Technology used to analyze large, complex datasets (RWD, clinical trials), identify patterns, and create precise synthetic control groups through advanced algorithms [14]. |
| Multiple Imputation Methods | A statistical approach for handling missing data, which is common in RWD. It creates multiple plausible values for missing data to avoid bias and retain statistical power [7]. |
| Real-World Evidence (RWE) Platforms | Integrated software solutions (e.g., from IQVIA, Flatiron, Aetion) that provide curated data, analytics tools, and workflows specifically designed for generating regulatory-grade evidence [15] [16]. |
For neuroscience researchers, the strategic selection and combination of data sources is paramount for constructing valid synthetic control arms. While historical clinical trial data offers precision and standardization, real-world evidence provides essential generalizability and volume.
The emerging best practice is a hybrid approach, leveraging the strengths of both to create robust, efficient, and ethically advantageous alternatives to traditional control groups. Supported by advanced AI/ML platforms and rigorous statistical methodologies like sIPTW, SCAs are poised to accelerate drug development in neuroscience and beyond, offering a viable path to generate robust evidence even for the most challenging patient populations.
The use of external controls in clinical drug development represents a paradigm shift in how evidence of therapeutic efficacy is established, particularly in fields like neuroscience research where traditional randomized controlled trials (RCTs) face significant ethical and practical challenges. External control arms (ECAs), including synthetic control arms (SCAs), utilize existing data from external sources—such as historical clinical trial data, real-world evidence (RWE), or natural history studies—to construct comparator groups when randomizing patients to a control intervention may be unethical or unfeasible. This approach has gained substantial traction in orphan drug development and oncology trials, and is increasingly being applied to complex neurological disorders such as Alzheimer's disease, amyotrophic lateral sclerosis (ALS), and rare genetic neurological conditions.
The regulatory landscape governing these innovative trial designs is evolving rapidly, with the U.S. Food and Drug Administration (FDA) and European Medicines Agency (EMA) demonstrating both convergence and divergence in their approaches. While both agencies recognize the potential of external controls to accelerate development of promising therapies, particularly for serious conditions with unmet medical needs, they maintain distinct regulatory philosophies, evidence standards, and implementation frameworks. The International Council for Harmonisation (ICH) guidelines provide a foundational framework for trial quality and design, but specific regulatory expectations for external controls continue to develop through case-by-case applications and emerging guidance documents. Understanding these nuanced differences is critical for researchers, scientists, and drug development professionals seeking to implement synthetic control arms successfully within global development programs.
FDA and EMA: Structural Foundations and Regulatory Philosophies
Organizational Structure and Governance
The FDA and EMA differ fundamentally in their organizational structures, which directly influences their approach to evaluating innovative trial designs like external controls.
The FDA operates as a centralized federal authority within the U.S. Department of Health and Human Services, functioning as a unified regulatory body with direct decision-making power. The Center for Drug Evaluation and Research (CDER) and Center for Biologics Evaluation and Research (CBER) employ full-time review teams who conduct comprehensive assessments of new drug applications [18] [19]. This centralized model enables relatively streamlined decision-making processes and consistent internal communication. The FDA maintains direct authority to approve, reject, or request additional information independently, with decisions applying immediately to the entire United States market upon approval [19].
In contrast, the EMA functions as a coordinating network rather than a centralized decision-making authority. Based in Amsterdam, the EMA coordinates the scientific evaluation of medicines through a complex network of national competent authorities across EU Member States [20]. For the centralized procedure, EMA's scientific committees—primarily the Committee for Medicinal Products for Human Use (CHMP)—conduct evaluations by appointing Rapporteurs from national agencies who lead the assessment. The CHMP issues scientific opinions that are then forwarded to the European Commission, which holds the legal authority to grant actual marketing authorization [19]. This decentralized model incorporates broader European perspectives but requires more complex coordination across diverse healthcare systems and regulatory traditions.
Review Timelines and Procedural Frameworks
These structural differences manifest in varying review timelines and procedural approaches that impact development planning for sponsors utilizing external controls:
Table: Comparative Review Timelines and Procedures
| Aspect | FDA (United States) | EMA (European Union) |
|---|---|---|
| Standard Review Timeline | 10 months for New Drug Applications (NDAs) and Biologics License Applications (BLAs) [19] | 210-day active assessment (approximately 7 months), plus clock-stop periods and European Commission decision-making, typically totaling 12-15 months [18] [19] |
| Priority/Accelerated Review | 6 months for priority review of applications addressing serious conditions [18] [19] | 150 days for accelerated assessment of medicines of major public health interest [19] |
| Decision-Making Authority | FDA has direct approval authority [19] | EMA provides recommendations to European Commission, which grants marketing authorization [20] |
| Expedited Pathway Options | Fast Track, Breakthrough Therapy, Accelerated Approval, Priority Review [19] | Accelerated Assessment, Conditional Approval [19] |
ICH Guidelines: Quality Foundations for Innovative Trial Designs
The International Council for Harmonisation (ICH) provides critical foundational guidelines that establish quality standards for clinical development programs, including those utilizing external controls. While not specifically addressing external controls, several ICH guidelines create the framework within which these innovative designs must operate.
The ICH E8(R1) guideline on "General Considerations for Clinical Studies" emphasizes the importance of quality by design principles throughout clinical development [21]. This guideline encourages sponsors to identify factors critical to quality (CTQ) during trial planning, including those related to data collection, patient population definitions, and endpoint selection—all particularly relevant when constructing external control arms. The guideline promotes a risk-based approach to clinical trial design and conduct, recognizing that innovative designs may require tailored methodologies to ensure reliability and interpretability of results [21].
ICH E9 on "Statistical Principles for Clinical Trials" provides the statistical foundation for evaluating trial designs, including discussions on trial design choices, bias reduction, and handling of missing data [21]. The addendum ICH E9(R1) specifically addresses estimands and sensitivity analysis, providing a structured framework for aligning trial objectives with design elements and statistical analyses. This is especially pertinent to external control arms, where precise definition of the target estimand and thoughtful handling of potential confounding are critical to regulatory acceptance [21].
ICH E6(R2) on "Good Clinical Practice" establishes standards for clinical trial conduct, data integrity, and participant protection. For external controls utilizing real-world data, compliance with GCP principles—particularly regarding data accuracy, reliability, and robust audit trails—is essential for regulatory acceptability [21].
The FDA and EMA have demonstrated commitment to harmonizing their approaches to quality by design, as evidenced by their joint pilot program for parallel assessment of quality-by-design applications [22]. This collaboration has resulted in strong alignment on implementation of ICH Q8, Q9, and Q10 guidelines, fostering greater consistency in regulatory expectations for innovative approaches, including potentially those involving external controls [22].
Regulatory Approaches to External Controls: Comparative Analysis
Evidentiary Standards and Acceptance Criteria
The FDA and EMA maintain notably different approaches to evidentiary standards for drug approval, which directly impacts their acceptance of external controls in supporting efficacy determinations.
The FDA's statutory requirement for "substantial evidence of effectiveness" has traditionally been interpreted as requiring at least two adequate and well-controlled investigations [20]. However, the agency has demonstrated significant flexibility in implementing this standard, particularly for serious conditions with unmet needs. FDA guidance acknowledges that substantial evidence may be demonstrated with one adequate and well-controlled study along with confirmatory evidence [20]. This flexibility creates regulatory space for external controls to potentially serve as confirmatory evidence when derived from appropriate sources and subjected to rigorous methodological controls.
The EMA generally expects multiple sources of evidence supporting efficacy but may place greater emphasis on consistency across studies and generalizability to European populations [19]. The agency has issued specific reflection papers on topics relevant to external controls, including "Single-arm Trials as Pivotal Evidence for the Authorisation of Medicines in the EU" and "Guideline on Clinical Trials in Small Populations" [20]. These documents indicate openness to innovative designs while emphasizing methodological rigor and comprehensive bias assessment.
Table: Comparative Evidentiary Standards for External Controls
| Consideration | FDA Approach | EMA Approach |
|---|---|---|
| Basis for Efficacy Determination | Substantial evidence from adequate and well-controlled studies, potentially including one pivotal trial with confirmatory evidence [20] | Multiple sources of evidence supporting benefit-risk assessment, with emphasis on consistency and generalizability [19] |
| Explicit Guidance on External Controls | Limited specific guidance, but accepted within expedited programs and rare disease development [20] | Reflection paper on single-arm trials as pivotal evidence [20] |
| Key Methodological Concerns | Control for confounding, data quality, relevance of historical data, statistical approaches to address bias [20] | Comparability of external data to target population, reliability of data sources, appropriateness of statistical methods [20] |
| Natural History Study Utilization | Specific draft guidance on natural history studies for drug development [20] | Considered within framework for registry-based studies and real-world evidence [20] |
Expedited Pathways and Rare Disease Applications
Both agencies have developed specialized pathways that frequently accommodate external controls, particularly for rare diseases and serious conditions where traditional RCTs may be impractical or unethical.
The FDA's expedited programs include Fast Track, Breakthrough Therapy, Accelerated Approval, and Priority Review designations [19]. The Accelerated Approval pathway is particularly relevant for external controls, as it allows approval based on effects on surrogate or intermediate endpoints reasonably likely to predict clinical benefit, with required post-approval confirmatory studies [19]. This pathway has frequently accommodated innovative trial designs, including those utilizing external controls, especially in oncology and rare neurological disorders.
The EMA's expedited mechanisms include Conditional Approval and Accelerated Assessment [19]. The Conditional Approval pathway allows authorization based on less comprehensive data than normally required when addressing unmet medical needs, with obligations to complete ongoing or new studies post-approval [19]. The Accelerated Assessment reduces the standard review timeline from 210 to 150 days for medicines of major public health interest representing therapeutic innovation [19].
For orphan drug development, both agencies offer special designations with varying criteria. The FDA grants orphan designation for products treating conditions affecting fewer than 200,000 individuals in the United States, while EMA's threshold is not more than 5 in 10,000 individuals in the EU [20]. The EMA additionally requires that the product either addresses a condition with no available treatment or provides "significant benefit" over existing therapies [20]. These orphan drug pathways frequently accommodate external controls due to the challenges of conducting traditional RCTs in small patient populations.
Practical Application: Implementing External Controls in Neuroscience Research
Methodological Framework and Protocol Development
Successfully implementing external controls in neuroscience research requires meticulous attention to methodological details and comprehensive protocol development. The following workflow outlines key considerations when designing studies incorporating synthetic control arms:
Defining the Target Estimand: The ICH E9(R1) estimand framework provides a structured approach to precisely define the treatment effect of interest, accounting for intercurrent events (e.g., treatment discontinuation, use of rescue medication) and how they will be handled in the analysis [21]. For neuroscience applications, this includes careful consideration of disease progression patterns, standard care variations, and concomitant medications.
Data Source Identification and Assessment: Potential data sources for external controls in neuroscience include historical clinical trials, disease registries, natural history studies, and real-world data from electronic health records. Each source must be evaluated for completeness, accuracy, and relevance to the target population. Key considerations include diagnostic criteria consistency, endpoint measurement standardization, and follow-up duration compatibility [20].
Statistical Analysis Plan Development: The statistical analysis plan must pre-specify methods for addressing confounding and bias, which are inherent challenges when using external controls. Propensity score methods, matching techniques, and sensitivity analyses should be detailed to demonstrate robustness of results across various assumptions and methodological approaches [20].
Researchers implementing external controls in neuroscience should be familiar with key methodological resources and regulatory documents:
Table: Essential Resources for External Control Implementation
| Resource Category | Specific Examples | Application in Neuroscience Research |
|---|---|---|
| Regulatory Guidelines | FDA: "Rare Diseases: Natural History Studies for Drug Development"; EMA: "Guideline on Registry-Based Studies" [20] | Informs development of natural history studies for neurodegenerative diseases; guides utilization of patient registries for external controls |
| Statistical Methodologies | Propensity score matching, weighting, stratification; Bayesian dynamic borrowing; Sensitivity analyses [20] | Addresses confounding in ALS trials; incorporates historical data with precision in rare epilepsy studies |
| Data Standards | CDISC standards (required for FDA submissions) [21] | Ensures regulatory compliance in data structure for Alzheimer's disease trials |
| Quality Frameworks | ICH E8(R1) quality by design principles; ICH E6(R2) Good Clinical Practice [21] | Guides critical-to-quality factor identification in Parkinson's disease trials; ensures data integrity standards for real-world data sources |
Comparative Regulatory Analysis: FDA vs. EMA on External Controls
Strategic Considerations for Global Development Programs
Researchers pursuing global development programs incorporating external controls must navigate nuanced differences in FDA and EMA expectations:
Clinical Trial Design Preferences: The EMA generally expects comparison against relevant existing treatments when available, while the FDA has traditionally been more accepting of placebo-controlled trials even when active treatments exist [19]. This difference has implications for external control construction, as EMA may expect the external control to reflect current standard of care rather than historical placebo responses.
Pediatric Development Requirements: The EU's Pediatric Investigation Plan (PIP) requirement mandates earlier pediatric development planning compared to FDA's Pediatric Research Equity Act (PREA) [19]. This front-loaded requirement may create opportunities for incorporating external controls in pediatric neuroscience studies, where randomized trials are particularly challenging.
Risk Management Planning: The EMA requires a Risk Management Plan (RMP) for all new marketing authorization applications, typically more comprehensive than standard FDA risk management documentation [19]. For products approved based on studies with external controls, the RMP may require more extensive post-authorization safety studies and monitoring commitments.
Emerging Trends and Future Evolution
Both agencies are actively evolving their approaches to external controls, with several emerging trends particularly relevant to neuroscience research:
Real-World Evidence Integration: Both FDA and EMA have initiatives to advance the use of real-world evidence in regulatory decision-making [20]. The FDA's Real-World Evidence Program and EMA's Data Quality Framework represent significant steps toward establishing standardized approaches for utilizing real-world data in external controls [20].
Advanced Statistical Methodologies: Regulatory acceptance of more complex statistical approaches, including Bayesian methods that dynamically borrow information from external controls, is increasing particularly in orphan drug development [20]. These methodologies are especially promising for neuroscience applications with progressive diseases where historical natural history data may provide informative baselines.
International Harmonization Efforts: Despite differences in specific implementation, both agencies participate in international harmonization initiatives through the ICH and collaborative bilateral programs [22] [20]. The FDA-EMA parallel assessment pilot for quality-by-design applications demonstrates a commitment to regulatory convergence that may extend to innovative trial designs like external controls [22].
The regulatory evolution of FDA and EMA approaches to external controls reflects a broader transformation in drug development paradigms, particularly impactful in complex fields like neuroscience research. While both agencies maintain distinct regulatory philosophies and procedural frameworks, they share a common commitment to facilitating efficient development of innovative therapies for serious conditions with unmet medical needs. The ICH guidelines provide a foundational framework for quality and statistical rigor that supports appropriate implementation of external controls.
Successful navigation of this evolving landscape requires researchers to engage early with both agencies, develop robust methodological approaches addressing potential confounding and bias, and maintain flexibility to accommodate region-specific regulatory expectations. As regulatory science continues to advance, external controls—particularly synthetic control arms—are poised to play an increasingly important role in accelerating the development of transformative neuroscience therapies while maintaining the evidentiary standards necessary to protect patient welfare and ensure therapeutic benefit.
Building Better Trials: Methodologies and Real-World Applications in Neurology and Psychiatry
In the evolving landscape of neuroscience clinical research, the demand for robust and ethical study designs is paramount. The growing use of synthetic control arms (SCAs) presents a compelling alternative to traditional randomized controlled trials (RCTs), especially when assigning patients to a placebo or standard-of-care group is unethical, impractical, or leads to high dropout rates [5] [23]. The core validity of an SCA hinges on a single critical process: statistically matching patients receiving an investigational therapy to comparable patients from external data sources, such as historical clinical trials or real-world data (RWD) [24] [5]. This matching is primarily accomplished through propensity score (PS) methods, which distill multiple patient covariates into a single probability of having received the treatment. The accuracy of this "statistical engine room" directly determines the reliability of the entire trial. This guide provides an objective comparison of the methods used to estimate propensity scores, from traditional logistic regression to modern machine learning (ML) algorithms, equipping researchers with the data needed to build more valid and powerful synthetic control arms.
Synthetic vs. Traditional Controls: A Paradigm Shift
Synthetic control arms are a type of external control where a control group is constructed using statistical methods on patient-level data from one or more external sources, rather than being recruited concurrently [5]. The table below contrasts this innovative approach with traditional trial designs.
Table 1: Comparison of Synthetic Control Arms and Traditional Randomized Trials
| Aspect | Traditional Randomized Controlled Trial (RCT) | Trial with a Synthetic Control Arm (SCA) |
|---|---|---|
| Control Group | Concurrently recruited patients randomized to control/placebo. | Constructed from external data (historical trials, RWD) [5]. |
| Key Advantage | Gold standard for minimizing bias through randomization. | Addresses ethical/recruitment challenges; can be faster and more cost-effective [5] [23]. |
| Key Limitation | Can be unethical, impractical, or slow to recruit; high dropout risk [23]. | Validity is entirely dependent on the quality and comparability of external data and the matching process [5]. |
| Ideal Use Case | Most scenarios where feasible and ethical. | Rare diseases, serious conditions with known outcomes, when concurrent randomization is infeasible [24] [5]. |
The Propensity Score Engine: Estimation Methods
The propensity score is the probability of a patient being in the treatment group given their observed baseline characteristics [25]. Accurate estimation is critical. Below, we compare the dominant methods.
Traditional Workhorse: Logistic Regression
For decades, logistic regression (LR) has been the default model for estimating propensity scores, used in up to 98% of medical articles applying PS methods [26]. It models the log-odds of treatment assignment as a linear combination of covariates. Its main strengths are interpretability and simplicity. However, its performance relies on the researcher correctly specifying the model, including all relevant interactions and non-linear terms—assumptions that are often violated in complex real-world data [25].
Modern Challengers: Machine Learning Algorithms
Machine learning models offer a powerful alternative by automatically detecting complex relationships and interactions without relying on pre-specified model forms [25] [27]. The following visualization outlines the core workflow for using these models in patient matching.
The most prominent ML algorithms for this task include:
- Random Forests (RF): An ensemble method that builds many decision trees on bootstrapped samples and averages the results. It is particularly strong at handling non-additive relationships and is less prone to overfitting than a single tree [25] [28].
- Boosted CART (e.g., Gradient Boosting): Another ensemble method that builds trees sequentially, with each new tree focusing on the errors of the previous ones. It is known for high prediction accuracy and has been shown to perform well in PS weighting [25] [27].
- Other Models: Bagged CART, Neural Networks, and Naive Bayes classifiers have also been explored, with varying performance depending on the data structure and application [25] [28].
Comparative Performance Data
The theoretical advantages of ML models are validated by extensive simulation studies and empirical comparisons. The following tables summarize key performance metrics from the literature.
Table 2: Comparative Performance of PS Models in Simulation Studies
| Estimation Method | Key Strengths | Key Weaknesses / Considerations | Performance in Complex Scenarios (Non-linearity & Non-additivity) |
|---|---|---|---|
| Logistic Regression (LR) | Interpretable, simple, widely accepted. | Prone to model misspecification bias [25]. | Subpar performance; high bias and poor CI coverage [25]. |
| Random Forests (RF) | Handles complex interactions well; robust. | Less interpretable ("black box"); requires tuning [28]. | Excellent performance, often top-ranked, especially for PS weighting [28]. |
| Boosted CART | High prediction accuracy; handles non-linearity. | Computationally intensive; sensitive to tuning [25]. | Substantially better bias reduction and consistent coverage vs. LR [25]. |
| Neural Networks | Very flexible function approximator. | "Black box"; requires large sample sizes and significant tuning. | Excellent performance, similar to Random Forests [28]. |
Table 3: Empirical Results from a Real-World Data Analysis (Lee et al., 2019 [28])
| Metric | Logistic Regression | Random Forests | Boosted CART | Neural Networks |
|---|---|---|---|---|
| Absolute Standardized Average Mean (ASAM)* | Baseline | Best Overall Balance | Good Balance | Excellent Balance |
| Bias of Causal Effect Estimator | Moderate | Lowest | Low | Low |
| Recommendation | Reliable for simple, main-effects models. | Top performer, especially for PS weighting. | Strong alternative, requires careful tuning. | Strong alternative, requires large data. |
Note: A lower ASAM indicates better covariate balance between matched groups. A threshold of <10% is commonly used [28].
A 2025 study on educational data further underscores that results can be mixed; while ML models like Random Forest and Gradient Boosted Machines often show superior prediction accuracy, they do not always guarantee perfect covariate balance and may even worsen balance for specific variables like race/ethnicity [26]. This highlights the non-negotiable need for rigorous post-matching diagnostics regardless of the method used.
Experimental Protocols and Methodologies
To ensure reproducibility, this section details the core methodologies used in the cited comparative studies.
- Data Generation: Simulate multiple datasets (e.g., n=500, 1000, 2000) with a binary exposure, continuous outcome, and ten covariates. Covariates are generated with pre-specified correlations.
- Scenario Design: Create several scenarios systematically varying the degree of non-linearity (e.g., quadratic terms) and non-additivity (interaction terms) in the true propensity score model.
- Propensity Score Estimation: Estimate propensity scores for each simulated dataset using all methods under comparison (e.g., LR, CART, RF, Boosted CART).
- Application of PS: Apply the propensity scores using a consistent method (e.g., weighting for the average treatment effect on the treated).
- Performance Evaluation: For each method and scenario, calculate performance metrics:
- Covariate Balance: Using metrics like Absolute Standardized Average Mean (ASAM).
- Bias: Percent absolute bias of the estimated treatment effect versus the known true effect.
- Coverage: Whether the 95% confidence interval for the effect contains the true value.
- Data Source: Use a well-defined observational dataset (e.g., birth records, educational longitudinal data).
- Define Treatment/Outcome: Clearly specify the treatment (e.g., labor induction, STEM major) and outcome (e.g., caesarean section, graduation outcome).
- Model Fitting: Fit the propensity score using different algorithms on the same set of pre-treatment covariates.
- Matching/Weighting: Use a consistent matching algorithm (e.g., 1:1 nearest-neighbor with caliper) or weighting scheme based on the estimated scores.
- Balance Assessment: Compute balance metrics (e.g., SMD, ASAM) for the matched/weighted sample.
- Effect Estimation & Comparison: Estimate the treatment effect and compare the results and the quality of balance achieved by the different PS estimation methods.
The Scientist's Toolkit for Patient Matching
Successfully implementing a patient matching strategy requires a suite of methodological and computational tools. The following table details the essential "research reagents" for this task.
Table 4: Essential Toolkit for Propensity Score-Based Patient Matching
| Tool / Solution | Function / Purpose | Examples & Notes |
|---|---|---|
| Statistical Software | Provides the environment for data manipulation, model fitting, and analysis. | R (with MatchIt, twang, randomForest packages) [25] [27] or Python (with scikit-learn, causalinference libraries). |
| Propensity Score Models | The core algorithms that estimate the probability of treatment assignment. | Logistic Regression, Random Forests, Gradient Boosting Machines [25] [27] [28]. |
| Matching Algorithms | The procedures that use PS to create comparable treatment and control groups. | Nearest-neighbor (with/without caliper), Optimal matching, Full matching [27]. The choice impacts bias and sample size. |
| Balance Diagnostics | Metrics and plots to verify that matching successfully balanced covariates. | Absolute Standardized Mean Differences (ASAM/SMD) (target <0.1) [28], Visualizations (e.g., Love plots, distribution plots) [27]. |
| High-Quality Data | The foundational input for constructing a valid synthetic control arm. | Curated RWD, historical clinical trial data. Must be relevant, complete, and representative of the trial population [24] [5]. |
The final workflow, incorporating both model selection and critical validation checks, can be summarized as follows.
The construction of synthetic control arms represents a significant advancement in clinical trial methodology, particularly for neuroscience where patient heterogeneity and ethical concerns are prominent. The statistical engine powering these designs—propensity score-based patient matching—has itself evolved. While logistic regression remains a reliable and interpretable tool for simpler scenarios, empirical evidence consistently demonstrates that machine learning algorithms, particularly Random Forests and Boosted CART, provide superior performance in the presence of the complex, non-linear relationships often found in real-world patient data [25] [28]. For researchers aiming to build the most robust and valid synthetic controls, adopting a multi-model strategy, rigorously validating covariate balance, and transparently reporting methodology are no longer best practices—they are necessities for gaining the confidence of regulators and the scientific community.
The evaluation of novel therapies for Alzheimer's disease (AD) faces a critical challenge: the growing ethical and practical difficulty of enrolling participants into concurrent placebo control groups, especially as effective treatments become available. This reluctance can stall the development of potentially groundbreaking therapies. Synthetic control arms (SCAs) have emerged as an innovative statistical methodology that can potentially overcome this barrier. This case study examines the proof-of-concept implementation of SCAs in Alzheimer's research, using data from the I-CONECT trial, and provides a comparative analysis with traditional randomized controlled trial (RCT) designs [29] [5].
SCAs are constructed from external data sources—such as historical clinical trial data or real-world data (RWD)—using statistical methods to create a control group that is comparable to the intervention group in a current study. This approach is particularly relevant in neuroscience research, where patient recruitment is often a major bottleneck, and the use of placebos can raise significant ethical concerns [5] [6].
Proof-of-Concept: The I-CONECT Trial and NACC-UDS Dataset
Experimental Aims and Design
A 2025 proof-of-concept study directly tested the feasibility and reliability of synthetic control methods in Alzheimer's disease research. The researchers utilized the I-CONECT trial, which investigates the impact of conversational interaction on cognitive function, as a platform for their analysis. The primary aim was to determine if a high-quality control group could be synthesized from existing data to replace or augment a concurrent control arm without compromising the validity of the efficacy estimates [29].
The study employed two distinct statistical methods for creating the synthetic controls:
- Case Mapping: This method involves identifying individual historical patients from an external database who closely match each participant in the current intervention group.
- Case Modeling: This approach uses statistical models to create a composite control profile based on the characteristics of the intervention group as a whole [29].
Data Source and Patient Matching
The external data was sourced from the National Alzheimer's Coordinating Center Uniform Data Set (NACC-UDS), a large, standardized database compiling clinical and neuropathological data from numerous US Alzheimer's Disease Centers. This registry provided an ideal pool for identifying historical cases with similar demographic, biological, and social characteristics to the participants in the I-CONECT trial. The quality of the SCA hinges on the robustness of this data source and the sophistication of the algorithms used to match or model the patients [29].
Table 1: Key Components of the SCA Workflow in the I-CONECT Proof-of-Concept Study
| Component | Description | Role in SCA Creation |
|---|---|---|
| Intervention Group | Participants from the I-CONECT trial receiving the conversational interaction intervention. | Served as the target for matching; the group to which the synthetic control would be compared. |
| External Data Source (NACC-UDS) | A large, curated registry of patient data from numerous Alzheimer's Disease Centers. | Provided the raw historical data from which potential control patients were selected or modeled. |
| Similarity Algorithms | Statistical methods (e.g., for case mapping and modeling) used to assess and match patient characteristics. | Critical for ensuring the synthetic control group is comparable to the intervention group in key baseline covariates. |
| Primary Outcome | Cognitive function measures. | The endpoint used to compare the treatment effect between the intervention group and the synthetic control. |
Results and Validation
The study demonstrated that synthetic control methods are both feasible and reliable for Alzheimer's disease studies. The key finding was the close alignment of treatment effect estimates between the original randomized trial and the analyses using synthetic controls [29].
- In parallel-group designs, the treatment effect size (β) for the primary cognitive outcome was 1.67 in the original trial. The SCA analyses produced nearly identical estimates, ranging from 1.40 to 1.65 [29].
- For n-of-1 designs, which focus on individual patient responses, the two SCA methods showed a high level of agreement in identifying treatment responders, with a Kappa statistic between 0.75 and 0.82 [29].
This validation confirmed that a well-constructed SCA could replicate the results of a traditional RCT in this context, providing a viable alternative when a concurrent control arm is not feasible.
Comparative Analysis: SCAs vs. Traditional RCT Designs
The implementation of SCAs presents a paradigm shift in clinical trial design. The following table contrasts the two approaches across several critical dimensions.
Table 2: Comparison of Synthetic Control Arm vs. Traditional Randomized Controlled Trial Designs
| Feature | Traditional RCT (Placebo/Standard-of-Care) | Synthetic Control Arm (SCA) |
|---|---|---|
| Control Group Source | Concurrently recruited patients, randomized to control. | Historical data from previous trials, registries, or real-world sources [5] [23]. |
| Patient Recruitment | Can be slow and challenging; requires recruiting enough patients for all arms. | Faster for the intervention arm; no need to recruit for the control arm [5] [30]. |
| Ethical Concerns | Higher; patients may be reluctant to participate due to chance of placebo assignment. | Lower; all trial participants receive the investigational therapy [5] [6]. |
| Cost & Duration | Typically higher costs and longer duration due to larger scale and longer recruitment. | Potentially reduced costs and shorter timelines by eliminating control arm operations [5] [30]. |
| Risk of Bias | Gold standard; randomization minimizes confounding and selection bias. | Susceptible to selection bias and unmeasured confounding if matching is imperfect [5] [6]. |
| Generalizability | Can be limited by strict inclusion/exclusion criteria. | May better reflect real-world populations if using broad RWD sources [30]. |
| Regulatory Acceptance | Well-established and widely accepted. | Growing acceptance but requires robust justification and validation [5] [6]. |
| Ideal Use Case | Common diseases, where recruitment is feasible; high-stakes regulatory submissions. | Rare diseases, oncology, settings where recruitment is impractical or unethical [5] [30] [6]. |
Experimental Protocols and Methodological Framework
Implementing a valid SCA requires a rigorous, pre-specified methodology. The following workflow outlines the key steps, drawing from the I-CONECT study and other successful implementations [29] [7].
Diagram 1: SCA Implementation Workflow.This chart outlines the sequential steps for creating and validating a synthetic control arm, from data sourcing to regulatory submission.
Data Source Selection and Justification
The first step is identifying high-quality, relevant external data. As showcased in the I-CONECT study, ideal sources are often large, prospectively collected datasets with detailed patient-level information [29]. Common sources include:
- Historical Clinical Trial Data: Highly standardized and quality-controlled, but may have narrow inclusion criteria [5].
- Disease Registries & Natural History Studies: e.g., NACC-UDS for Alzheimer's, CRC-SCA for spinocerebellar ataxia [29] [31]. These are crucial for understanding disease progression.
- Real-World Data (RWD): From electronic health records (EHRs) or claims databases. Higher volume but requires significant processing to standardize and handle missing data [5] [7].
Data Processing and Harmonization
Data from different sources must be harmonized to ensure comparability. This involves:
- Mapping Variables: Ensuring outcome definitions (e.g., cognitive scores), lab values, and demographic data are consistent between the trial and external data [6].
- Managing Missing Data: Using methods like multiple imputation to account for missing covariates, as was done in the DLBCL study where 15 imputations per patient were used [7].
- Temporal Alignment: Accounting for changes in standard of care over time to avoid comparing against outdated practices [5].
Patient Matching and Covariate Balancing
This is the statistical core of SCA creation. The goal is to create a synthetic control group with baseline characteristics that are balanced with the intervention group. The predominant method is Propensity Score Matching or related techniques [7] [6].
- Propensity Score (PS): The probability of a patient being in the intervention group, given their observed covariates. It is typically estimated using logistic regression [7].
- Weighting Procedure: The stabilized Inverse Probability of Treatment Weighting (sIPTW) uses the propensity scores to weight patients in the external data pool, creating a balanced synthetic cohort [7].
- Balance Checking: After weighting, researchers check the balance of all covariates included in the PS model using metrics like Standardized Mean Differences (SMD). A well-balanced model is a prerequisite for valid outcome comparison [7].
Outcome Analysis and Sensitivity Analysis
Once balance is achieved, the outcome of interest (e.g., cognitive score, overall survival) is compared between the intervention group and the weighted SCA. To assess robustness, extensive sensitivity analyses are mandatory. These test how the results change under different assumptions, such as using different matching algorithms or methods for handling missing data [7] [6]. The DLBCL study, for instance, confirmed that their results were consistent across different missing data management methods [7].
The Scientist's Toolkit: Essential Reagents for SCA Implementation
Building a robust SCA requires a suite of statistical, computational, and data resources. The following table details the key "research reagents" and their functions in the experimental protocol.
Table 3: Key Research Reagent Solutions for SCA Implementation
| Tool Category | Specific Example(s) | Function in SCA Workflow |
|---|---|---|
| High-Quality Data Sources | National Alzheimer's Coordinating Center Uniform Data Set (NACC-UDS) [29]; Clinical trial data from LNH09-7B; Real-world data from REALYSA cohort [7]. | Provides the foundational historical or real-world patient data from which the control arm is constructed. |
| Statistical Software Packages | R (with packages for propensity scoring, e.g., MatchIt, twang); Python (with scikit-learn, pymc3). |
Enables the execution of complex statistical procedures like propensity score estimation, weighting, and outcome modeling. |
| Propensity Score Methods | Logistic Regression for PS estimation; Stabilized Inverse Probability of Treatment Weighting (sIPTW) [7]. | The core statistical method for balancing covariates between the intervention group and the external control pool to reduce selection bias. |
| Sensitivity Analysis Frameworks | Multiple imputation for missing data [7]; Varying PS model specifications; E-value analysis. | Tests the robustness of the primary findings to different methodological assumptions, strengthening validity for regulatory review. |
| AI & Harmonization Tools | AI for imaging protocol matching [23]; TWIN-GPT for data imputation [32]. | Addresses data heterogeneity, especially in imaging or unstructured data, by harmonizing variables and imputing missing values. |
| Regulatory Guidance Documents | FDA Guidance on "Considerations for the Use of Real-World Data and Real-World Evidence" (2023) [5]; EMA guidelines on external controls. | Provides the framework for acceptable SCA design, data standards, and analysis plans to ensure regulatory acceptance. |
The proof-of-concept implementation of synthetic control arms in Alzheimer's disease research marks a significant advancement in clinical trial methodology. The successful replication of I-CONECT trial results using NACC-UDS data demonstrates that SCAs are a feasible and reliable alternative when traditional control arms are impractical or unethical [29]. This approach, validated in other therapeutic areas like diffuse large B-cell lymphoma and idiopathic pulmonary fibrosis, offers a path to more efficient, patient-centric, and cost-effective clinical research [7] [33].
While SCAs do not replace the gold standard of RCTs and introduce unique challenges regarding data quality and potential bias, their role in the neuroscientist's toolkit is undeniable. As regulatory frameworks mature and data sources become more standardized, the integration of SCAs is poised to accelerate drug development, particularly for complex neurodegenerative diseases like Alzheimer's, ultimately bringing new treatments to patients faster.
Clinical trials for rare neurological diseases face a unique set of challenges that render traditional randomized controlled trial (RCT) designs often impractical or unethical. With an estimated 500 million people worldwide affected by rare diseases—approximately half of whom are children—and fewer than 5% of the 7,000 known rare diseases having approved treatments, the need for innovative trial methodologies is acute [34] [35]. These trials confront limitations including extremely small, geographically dispersed patient populations, heterogeneous disease presentation and progression, and ethical concerns about placebo use in conditions with rapid deterioration [36] [37]. The rise of precision medicine has further complicated patient recruitment by defining increasingly specific disease subtypes [38]. Synthetic control arms (SCAs) have emerged as a promising alternative that can accelerate therapeutic development while maintaining scientific rigor, particularly for rare neurological conditions where conventional randomized trials face significant obstacles [5] [37].
Understanding Synthetic Control Arms
Definition and Composition
A synthetic control arm (SCA) is a type of external control group generated using statistical methods applied to one or more external data sources, rather than recruiting concurrent control patients [5]. SCAs are constructed from patient-level data obtained from individuals not enrolled in the investigational clinical trial, with patients "matched" using statistical or analytical methods to achieve balanced baseline characteristics such as demographics and disease composition [5]. These methodologies enable a direct comparison between the SCA and the investigational arm receiving the experimental therapy.
SCAs can be distinguished from simpler external control arms by their sophisticated construction. While external control arms typically use data "as is" from previous trials or treated patients, synthetic controls are generated using advanced statistical models that combine various sources, including previous clinical trials and real-world observational data, to create a control group that closely matches the intervention group [38].
The construction of robust SCAs relies on multiple data sources, each with distinct advantages and limitations:
- Historical Clinical Trial Data: Generally features high standardization and quality but may represent limited patient populations due to recruitment biases [5].
- Real-World Data (RWD): Includes electronic health records, patient registries, and insurance claims data, offering higher volume but often with worse standardization and more missing data points [5].
- Natural History Studies: Prospective or retrospective observational studies that document disease progression without intervention, providing essential baseline data for comparison [37].
Table: Comparison Data Sources for Synthetic Control Arms
| Data Source | Advantages | Limitations | Common Applications |
|---|---|---|---|
| Historical Clinical Trials | High data quality; Standardized collection; Regulatory familiarity | Limited representation; Recruitment biases; May not reflect current standards | Rare diseases with previous trial data; Established assessment tools |
| Real-World Data (RWD) | Larger patient numbers; Reflects clinical practice; Includes diverse populations | Variable quality; Missing data; Requires significant processing | Ultra-rare diseases; Conditions with established care pathways |
| Natural History Studies | Comprehensive disease understanding; Captures longitudinal progression | Time-consuming to conduct; Resource intensive; Potential selection bias | Neurodegenerative diseases; Progressive disorders with documented trajectories |
Experimental Validation and Methodologies
Proof of Concept in Spinal Cord Injury
A 2025 study provides compelling experimental validation for SCAs in rare neurological disorders, specifically focusing on acute traumatic spinal cord injury (SCI)—a condition with fewer than 250 cases per million inhabitants per year [8]. The research established a comprehensive benchmark of data-driven prediction architectures for neurological recovery after SCI, comparing six different modeling approaches:
- Regularized linear regression
- Random forest
- Extreme gradient-boosted trees
- Convolutional neural networks (CNN)
- Sequence-to-sequence transformers
- Graph neural networks (GNN)
The primary dataset included 4,196 patients from the European Multicenter Study about Spinal Cord Injury (EMSCI) and 587 patients from the Sygen trial for external validation [8]. The research focused on predicting all segmental motor scores from the International Standards for Neurological Classification of SCI (ISNCSCI) examination, providing a more nuanced perspective on recovery compared to aggregate metrics.
Experimental Protocol and Workflow
The experimental methodology followed a rigorous multi-stage process:
Data Collection and Preprocessing:
- ISNCSCI assessments comprising segmental motor scores, light touch scores, and pinprick scores
- Inclusion of patient age at injury, sex, and assessment time points as covariates
- Exclusion of patients showing deterioration (≥2 point motor score decrease) to filter complications
- Handling of missing values through standardized imputation approaches
Model Training and Validation:
- Implementation of six architectures with appropriate hyperparameter tuning
- Performance quantification using root mean squared error below neurological level of injury (RMSEbl.NLI)
- External validation using held-out Sygen trial dataset
- Uncertainty quantification through input perturbation based on ISNCSCI assessment variances
Trial Simulation Framework:
- Comparison of synthetic and randomized controls in absence of investigative treatment
- Quantification of natural recovery differences between groups due to stochastic effects
- Application to NISCI trial data as case study for single-arm trial reassessment
The researchers identified a convolutional neural network as the best-performing architecture, achieving a median RMSEbl.NLI of 0.55—demonstrating high predictive accuracy for neurological recovery [8].
DLBCL Validation Study Methodology
A 2025 study on diffuse large B-cell lymphoma (DLBCL) in patients over 80 years demonstrated a robust methodology for SCA construction, employing:
Data Integration:
- Combination of clinical trial data (LNH09-7B) and real-world data (REALYSA cohort)
- Application to SENIOR trial data for validation
Statistical Balancing:
- Propensity score estimation using logistic regression with multiple covariates
- Stabilized inverse probability of treatment weighting (sIPTW) approach
- Exclusion of patients with extreme propensity scores (<0.1 or >0.9) to avoid positivity violations
Missing Data Management:
- Multiple imputation method with 15 imputations per patient
- Calculation of propensity scores for each imputed dataset
- Use of median propensity score for weighting procedures
The study successfully demonstrated that the mixed SCA could mimic the control arm of an RCT, with overall survival hazard ratios of 0.743 [0.494-1.118] (p = 0.1654) showing no statistical difference from the actual trial results [39].
Comparative Performance Analysis
Quantitative Comparison of Trial Designs
Table: Performance Comparison of Trial Designs in Rare Neurological Diseases
| Performance Metric | Traditional RCT | Single-Arm Trial | Synthetic Control Arm |
|---|---|---|---|
| Patient Recruitment | 36-48 months [37] | 18-24 months | 18-24 months [38] |
| Trial Duration | 5-7 years | 3-4 years | 3-4 years [38] |
| Control Group Costs | High (site monitoring, drug supply, assessments) | None | Moderate (data acquisition, statistical analysis) |
| Statistical Power | High with sufficient recruitment | Limited without historical comparison | Moderate to high with adequate data sources |
| Regulatory Acceptance | Established gold standard | Requires justification and context | Growing acceptance with validation [6] |
| Ethical Concerns | Placebo use problematic in serious diseases | All patients receive active treatment | Eliminates placebo concerns [5] |
Model Performance Benchmarks
The spinal cord injury study provides direct comparative data on SCA prediction models [8]:
Table: Prediction Model Performance for Neurological Recovery
| Model Architecture | RMSEbl.NLI | Key Advantages | Implementation Complexity |
|---|---|---|---|
| Regularized Linear Regression | 0.68 [8] | High interpretability; Computational efficiency | Low |
| Random Forest | 0.63 [8] | Handles non-linear relationships; Robust to outliers | Medium |
| XGBoost | 0.61 [8] | High accuracy; Feature importance scoring | Medium |
| Convolutional Neural Network (CNN) | 0.55 [8] | Captures sequential dependencies; State-of-the-art performance | High |
| Sequence-to-Sequence Transformer | 0.57 [8] | Models complex temporal patterns; Attention mechanisms | High |
| Graph Neural Network (GNN) | 0.59 [8] | Explicitly models anatomical relationships; Incorporates domain knowledge | High |
Regulatory Considerations and Implementation Framework
Regulatory Landscape
Regulatory agencies including the FDA, EMA, and MHRA have demonstrated growing acceptance of SCAs while emphasizing the need for rigorous methodology [5] [6]. Key regulatory considerations include:
FDA Perspective:
- Acceptance of external controls where justified, assessed case-by-case [5]
- Emphasis on early SCA design consideration during protocol development
- Requirement for comprehensive documentation of all accessed data sources
EMA Position:
- Recognition of SCAs as valuable tools when conventional trials present challenges [5]
- Encouragement of SCA use in specific cases but discouragement when randomized trials can be conducted ethically within reasonable timeframes [38]
Common Regulatory Requirements:
- Early engagement with regulatory agencies during protocol development [5]
- Robust justification for SCA use with appropriate data sources and statistical analyses [37]
- Comprehensive documentation of data sources, matching methodologies, and potential limitations [6]
- Demonstration of minimized bias through appropriate statistical methods [5]
Implementation Framework
Successful implementation of SCAs in rare neurological disease trials requires a structured approach:
Early Planning Phase:
- Initiate natural history data collection early, preferably using prospective designs [37]
- Design SCA during protocol development with finalization before trial initiation [5]
- Engage biostatistics expertise for propensity matching, sensitivity analyses, and missing data strategies [37]
Data Source Selection:
- Combine multiple data sources including historical literature, RWD, and clinical trial data [5]
- Ensure data quality through rigorous assessment of completeness, accuracy, and relevance
- Document all accessed data sources with justifications for inclusion/exclusion [5]
Methodological Considerations:
- Select statistical matching methods (e.g., propensity score matching) acceptable to regulatory authorities [5]
- Address potential selection bias through sensitivity analyses [6]
- Consider changes in standard of care over time that may render historical data less relevant [5]
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table: Essential Research Reagents and Methodological Solutions for SCA Implementation
| Tool Category | Specific Solution | Function | Application Example |
|---|---|---|---|
| Data Collection Platforms | Electronic Health Records (EHRs) | Source of real-world patient data and outcomes | REALYSA cohort for DLBCL [39] |
| Patient Registries | Disease-specific longitudinal databases | Natural history documentation; Patient recruitment | EMSCI for spinal cord injury [8] |
| Statistical Software | R, Python with specialized packages | Propensity score estimation; Weighting procedures | Stabilized IPTW for DLBCL analysis [39] |
| Machine Learning Frameworks | TensorFlow, PyTorch, XGBoost | Advanced prediction model implementation | CNN for motor score prediction [8] |
| Data Harmonization Tools | OMOP Common Data Model | Standardization of disparate data sources | Integration of clinical trial and RWD [39] |
| Imputation Methods | Multiple Imputation by Chained Equations (MICE) | Handling missing data in real-world datasets | "Across" method for REALYSA data [39] |
Synthetic control arms represent a transformative methodological innovation for clinical trials in rare neurological diseases, effectively addressing the fundamental challenge of small patient populations while maintaining scientific rigor. The experimental validation in conditions like spinal cord injury demonstrates that properly constructed SCAs can replicate the results of randomized controls while accelerating therapeutic development and addressing ethical concerns associated with placebo groups [8].
The successful implementation of SCAs requires meticulous attention to data quality, appropriate statistical methodologies, and early regulatory engagement. As evidenced by the growing regulatory acceptance and successful applications across multiple disease areas, SCAs are transitioning from novel approaches to established methodologies in the clinical development toolkit [37]. For researchers and drug development professionals working in rare neurological diseases, SCAs offer a viable path to generate robust evidence while acknowledging the practical and ethical constraints of traditional trial designs in these challenging populations.
The continued evolution of SCA methodologies—particularly through advances in machine learning and expanded real-world data resources—promises to further enhance their utility and application across the spectrum of rare neurological disorders, potentially accelerating the development of effective treatments for conditions that currently lack therapeutic options.
The following table provides a high-level comparison of traditional randomized control trial (RCT) designs against emerging synthetic control arm (SCA) methodologies, highlighting their integration with biomarker-driven enrichment strategies.
| Feature | Traditional RCT Designs | Synthetic Control Arm (SCA) Designs |
|---|---|---|
| Core Principle | Prospective, concurrent randomization of patients into investigational and control groups [10] | Use of external/historical data to create a virtual control group for comparison [10] [38] |
| Patient Recruitment | Requires large numbers, leading to longer timelines and higher costs; challenging for rare diseases [38] [40] | Reduces number of patients needed to recruit for control arm, accelerating timelines [10] [13] |
| Control Group Data Source | Prospectively enrolled patients concurrently with investigational arm [10] | Previously completed clinical trials, real-world data (RWD), registry data [10] [40] |
| Ethical Considerations | Using placebos or no-treatment arms can be unethical in severe diseases with unmet need [38] [40] | Mitigates ethical concerns of withholding potential treatment by using existing data [38] |
| Integration with Biomarkers | Biomarker-based enrichment strategies can limit already challenging recruitment [41] [38] | Facilitates use of complex biomarkers by leveraging large, pre-existing datasets for patient matching [41] [40] |
| Primary Regulatory Stance | Long-established gold standard [38] | Considered innovative; accepted on a case-by-case basis, especially for rare diseases and unmet need [10] [38] |
| Key Risk | Recruitment failure and high costs [38] | Unknown confounding and data quality issues [10] |
Foundational Methodologies and Experimental Protocols
Biomarker-Driven Patient Enrichment Designs
Patient enrichment strategies are critical in precision medicine, as they improve trial efficiency by targeting biomarker-defined populations most likely to respond to treatment [41].
- Two-Stage Enrichment with Multiple Biomarkers: A novel framework accommodates two or more continuous biomarkers, moving beyond the limitation of single-biomarker approaches [41]. In the first stage, data from a broad population is used to estimate optimal biomarker thresholds that define the target population. In the second stage, the trial proceeds, enriching for patients who meet these criteria. This method utilizes two treatment effect metrics: the Average Treatment Effect (ATE) and the Standardized ATE [41].
- Protocol for Threshold Estimation: The stage-one sample size is a critical determinant in the accuracy of the multiple biomarker thresholds. A simulation-based study can be used to assess this impact, using a hypothetical trial in early-stage Alzheimer's patients as an illustration [41].
- Data Analysis Workflow: The process involves collecting biomarker and outcome data from a preliminary cohort, using statistical models (which can account for the correlation between treatment effect and biomarkers) to determine the combination of thresholds that optimizes the treatment effect, and then applying these thresholds as inclusion criteria in the subsequent definitive trial [41].
Synthetic Control Arm Construction Workflows
Creating a robust SCA requires a rigorous methodology to ensure the virtual control group is a valid comparator for the prospectively enrolled investigational arm.
- Digital Twinning Protocol: Advanced approaches involve creating a "digital twin" for each treated patient from external data sources [40]. This is a multi-modal process that matches on key baseline characteristics, including clinical variables (e.g., demographics, disease severity) and quantitative data from imaging or other biomarkers, which are known to be linked to disease progression [40].
- Data Curation and Validation: The foundation is a large, well-curated dataset of the target patient population. Data must be benchmarked against established clinical endpoints and known disease trajectories to confirm quality and relevance [40]. This involves intensive curation to remove low-quality or incomplete data and benchmarking datasets from different sources for consistency [40].
- Statistical Matching and Analysis: Proprietary AI-based quantitative tools are used to handle variability in data sources (e.g., different imaging techniques) [40]. After filtering by trial inclusion criteria, statistical techniques are employed to create a tightly matched synthetic control pool. One method involves generating thousands of randomly sampled control groups from this pool and using the best-matched cohorts to assess comparative efficacy [40].
The following diagram illustrates the core workflow for constructing and validating a synthetic control arm.
The following table details key reagents, data sources, and computational tools essential for implementing advanced enrichment and synthetic control methodologies.
| Item/Resource | Type | Primary Function/Application |
|---|---|---|
| Induced Pluripotent Stem Cells (iPSCs) | Biological Reagent | Patient-derived cells used to generate brain organoids for disease modeling and in vitro drug screening [42]. |
| Brain Organoids | Experimental Model | 3D, self-organizing in vitro models that recapitulate aspects of human brain development and disease pathology [42]. |
| Regional Patterning Factors | Biochemical Reagents | Small molecules and growth factors (e.g., morphogens) used to direct organoid differentiation into specific brain regions (cortex, midbrain, striatum) [42]. |
| Quantitative Imaging AI Tools | Computational Tool | Proprietary software to analyze medical images (e.g., MRI, CT) and extract biomarker data for patient matching in SCAs [40]. |
| Curated Real-World Data (RWD) Platforms | Data Resource | Validated, longitudinal datasets from clinical trials and electronic health records used to build robust synthetic controls [40] [13]. |
| Microfluidic Co-culture Devices | Labware/Platform | Enables precise control of the cellular microenvironment and promotes vascular network formation in advanced organoid models [42]. |
Applications in Neuroscience Research
The convergence of biomarker enrichment, synthetic controls, and advanced neural models is particularly transformative for neuroscience, where traditional trials face significant hurdles.
Target Discovery and Validation with Brain Organoids
Brain organoids have emerged as a powerful platform for target and biomarker discovery. Compared to traditional 2D cell models and animal models, 3D brain organoids more accurately recapitulate the human brain's cellular diversity and spatial architecture [42]. They are generated from induced pluripotent stem cells (iPSCs) derived from patients, providing an unparalleled platform for modeling human diseases and advancing personalized medicine [42].
- Protocol for Assembloid Generation: To study interactions between brain regions, scientists use an "assembloid" technique. This involves assembling organoids from different brain regions (e.g., cortical-striatal, cortical-thalamic) to simulate complex neurodevelopmental processes and long-range axonal connections [42].
- Functional Analysis: Emerging techniques like whole-cell patch-clamp recording, calcium imaging, and optogenetics are employed to document the morphological and functional dynamics of brain organoids, providing a foundation for validating therapeutic targets [42].
- Vascularization Advances: A key limitation of traditional organoids is the lack of vasculature. New protocols involve fusing brain organoids with induced vascular organoids to create models with a functional blood-brain barrier (BBB) structure, enhancing their physiological relevance [42].
Clinical Trial Applications in Neurodegenerative Disease
The application of SCAs in neurological conditions is advancing, particularly in areas with high unmet need and difficult recruitment.
- Case Study: Idiopathic Pulmonary Fibrosis (IPF): While not a neurological condition, a pioneering application of SCAs in IPF provides a methodological blueprint for brain disorders. In a study of an inhaled pirfenidone therapy (AP01), a treatment-naïve synthetic placebo arm was created using real-world patients matched on clinical and radiological markers. From a large dataset, over 10,000 randomly sampled control groups were generated, and the top 1,000 best-matched cohorts were used to assess the comparative efficacy of the investigational therapy, providing an ethical and rigorous alternative to a traditional placebo arm [40].
- Potential in Alzheimer's Disease: Research is exploring novel two-stage enrichment designs capable of handling multiple continuous biomarkers, using a hypothetical clinical trial involving early-stage Alzheimer's patients as an illustration [41]. This approach aims to fully utilize information from all relevant biomarkers to improve target population identification.
Quantitative Outcomes and Performance Data
Trial Efficiency and Operational Metrics
The adoption of synthetic control arms and enrichment strategies is primarily driven by their potential to significantly improve the operational efficiency of clinical development.
| Performance Metric | Traditional RCT | Synthetic Control Arm (SCA) / Enrichment | Data Source / Context |
|---|---|---|---|
| Patient Recruitment | Large numbers required; can be slow and costly [38] | Reduces number of control patients needed; accelerates timelines [10] [13] | Industry expert analysis [10] [13] |
| Development Cost | High, due to large size and long duration [40] | Reduces trial cost and duration [40] | Analysis of SCA use cases [40] |
| Phase II Trial Sizing | Sized based on traditional treatment effect estimates | Potential for reduced size using more precise effect estimates from SCA-informed designs [10] | Use case where SCA analysis informed Phase II trial sizing [10] |
| Overall Drug Development Success Rate | ~7.9% (across all diseases), ~5.3% (oncology) [43] | Aims to improve probability of success via better target population identification [41] | Industry-wide statistics [43] |
Biomarker and Model Performance Characteristics
The technical performance of biomarkers and models underpins the validity of these advanced trial designs.
| Characteristic | Exemplary Performance / Feature | Context |
|---|---|---|
| Multiple Biomarker Enrichment | Framework accommodates 2+ continuous biomarkers; uses ATE and Standardized ATE [41] | Novel statistical methodology [41] |
| MRI Resolution (Anatomical) | 0.2mm in-plane; 1mm slice thickness (11.7T Iseult machine) [44] | Technological advance in a key neuroscience tool [44] |
| Organoid Batch Generation | Hundreds of high-quality organoids per batch with minimal stress pathway activation (Hi-Q method) [42] | Protocol advancement for improved scalability and reproducibility [42] |
| Data Quality for SCA | Leverages "observed data from historical clinical trials" noted for high quality [10] | Foundational requirement for building reliable synthetic controls [10] |
The following diagram maps the logical decision process for selecting a trial design, integrating considerations of biomarkers, patient population, and regulatory strategy.
Regulatory and Industry Outlook
The regulatory landscape for these innovative designs is evolving, with a clear focus on maintaining scientific rigor while enabling efficiency.
- Regulatory Acceptance: Regulatory bodies like the FDA and EMA have issued guidance on using external control arms. Their use is becoming more accepted, particularly in clinical trials for rare cancers and severe diseases where traditional control arms are difficult or unethical to implement [40]. The FDA shows significant interest in hybrid designs that combine a small, randomized control arm with a synthetic control for supplementation and validation [10].
- Industry Adoption Trajectory: SCAs are expected to become a more established clinical trial approach within the next five years, with progress anticipated in both regulatory and non-regulatory (e.g., internal decision-making, Phase II dose-finding) spaces [10]. The overall CRO market supporting such innovations is projected to surpass $100 billion by 2028 [43].
- Neuroethical Considerations: As neuroscience tools advance, the field must grapple with neuroethical questions surrounding neural enhancement, data privacy, and the potential misuse of brain data. Ensuring that patients are informed of the risks associated with technologies like digital twins is critical for maintaining trust [44].
Navigating Pitfalls: A Practical Guide to Optimizing Synthetic Control Arms
In the rigorous world of clinical research and neuroscience drug development, selection bias and confounding bias represent two fundamental threats to the validity of study conclusions. Selection bias arises when the individuals selected for a study are not representative of the target population, compromising external validity and generalizability. This occurs when there are systematic differences between participants and non-participants, or between treatment groups in characteristics that influence outcomes. In contrast, confounding bias occurs when an observed association between an exposure and outcome is distorted by a third variable (confounder) that is associated with both the exposure and the outcome, thereby compromising internal validity and the ability to establish causation [45] [46].
The distinction between these biases is scientifically crucial: confounding bias provides an alternative explanation for an association, while selection bias questions whether the results are representative of the population of interest [45]. Even if confounding bias is completely controlled, a study may still suffer from selection bias that renders its results non-generalizable [45]. With the emergence of novel trial designs like synthetic control arms (SCAs) in neuroscience research, understanding and mitigating these biases becomes increasingly important for researchers, scientists, and drug development professionals.
Synthetic Control Arms vs. Traditional Trial Designs: A Comparative Framework
Traditional Randomized Controlled Trials (RCTs)
Randomized Controlled Trials (RCTs) remain the gold standard for evaluating experimental interventions, primarily because randomization theoretically eliminates both selection and confounding biases by ensuring that exposure groups are comparable across all known and unknown variables [6] [47]. In traditional RCTs, patients are randomly allocated to either an experimental intervention arm or a control arm (placebo or standard-of-care). This process, when properly implemented, ensures that the only systematic difference between groups is the intervention itself, allowing differences in outcomes to be attributed to the treatment effect [47].
However, traditional RCTs face significant challenges, including patient recruitment and retention difficulties, particularly when patients are less willing to participate in placebo-controlled trials [6]. In rapidly evolving fields like oncology and neuroscience, the standard of care may change during the trial, challenging the ethical principle of "clinical equipoise" that justifies randomizing patients to control groups [6]. For rare diseases or increasingly stratified disease classifications based on genetic makeup, recruiting sufficient patients becomes exceptionally challenging, leading to insufficient statistical power [6].
Synthetic Control Arms (SCAs)
Synthetic Control Arms (SCAs) represent an innovative methodology that uses external control data to evaluate the comparative effectiveness of an intervention [6] [23]. Instead of randomizing patients to a concurrent control group, SCAs are constructed from existing data sources—including historical clinical trial data, real-world data (RWD), and patient registries—using statistical methods to create a comparator group that closely matches the intervention group on key characteristics [6] [23] [5].
The synthetic control method employs a data-driven algorithm to identify an optimal weighted control unit based on pre-intervention data from available control units [48]. This approach is particularly valuable when conducting traditional RCTs with placebo or standard-of-care arms presents ethical or practical challenges, such as in rare diseases or life-threatening conditions where withholding potential treatment may be problematic [5]. Regulatory agencies including the FDA and EMA have recognized these applications and have approved treatments based on evidence incorporating synthetic control methodologies [6] [23].
Quantitative Comparison of Bias Susceptibility
Table 1: Bias Susceptibility Across Trial Designs
| Bias Type | Traditional RCT | Single-Arm Trial | Synthetic Control Arm |
|---|---|---|---|
| Selection Bias | Low (when properly randomized) | High (no control group for comparison) | Moderate to High (depends on data source representativeness) |
| Confounding Bias | Low (randomization balances known/unknown confounders) | High (no comparable control group) | Moderate (statistical methods control for measured confounders only) |
| Time-related Bias | Low (concurrent controls) | High (historical comparison) | Moderate to High (depends on data currency) |
| Allocation Bias | Low (with proper randomization) | Not applicable | Moderate (depends on matching quality) |
| Performance Bias | Low (with blinding) | High (no blinding) | High (knows treatment assignment) |
| Attrition Bias | Moderate (differential loss to follow-up) | Moderate (loss to follow-up) | Variable (depends on data completeness) |
Table 2: Advantages and Limitations of Synthetic Control Arms
| Aspect | Advantages | Limitations |
|---|---|---|
| Ethical Considerations | Reduces ethical concerns of placebo assignment; patients more willing to participate [5] | Cannot completely replace RCTs when direct randomization is ethically acceptable |
| Recruitment & Retention | Improves recruitment; reduces drop-out rates from control assignment [23] [5] | Dependent on quality and accessibility of historical data sources |
| Time & Cost Efficiency | Potentially more cost-effective and time-efficient; avoids costs of recruiting control patients [5] | Requires significant expertise in statistical methods and data management |
| Statistical Power | Enables studies in rare diseases where patient numbers are limited [6] [23] | Vulnerable to unmeasured confounding; can only adjust for known measured variables |
| Regulatory Acceptance | Growing acceptance by FDA, EMA, and other regulatory agencies [6] [23] [5] | Requires robust justification and validation of methodology; early regulatory engagement critical |
| Generalizability | May better represent real-world populations if using diverse RWD sources [5] | May not capture population diversity if historical data lacks representativeness |
Experimental Protocols for Bias Assessment and Mitigation
Protocol for Evaluating Synthetic Control Validity
Purpose: To systematically assess the suitability of external data sources for constructing a valid synthetic control arm in neuroscience research.
Procedure:
- Data Source Evaluation: Document all accessed data sources and provide justification for inclusion/exclusion. Prefer data from recent RCTs or high-quality prospective cohorts with similar design and implementation processes [6].
- Population Similarity Assessment: Compare baseline characteristics (age, disease severity, biomarkers, treatment history, geographic distribution) between synthetic control and intervention populations. Use standardized difference measures with threshold <0.1 indicating good balance [6].
- Outcome Harmonization: Ensure outcome definitions and measurement methods are identical between synthetic control and intervention groups. For neuroscience applications, confirm imaging protocols, biomarker assays, and cognitive assessment methods are comparable [6] [23].
- Pre-Intervention Trend Alignment: Validate that the synthetic control matches the intervention group's outcome trajectory during the pre-intervention period using statistical tests for trend equivalence [48].
- Covariate Balance Optimization: Apply statistical matching methods (propensity scores, weighting) to create comparable groups based on comprehensive baseline characteristics [6] [5].
- Sensitivity Analysis: Conduct multiple analyses under different assumptions about unmeasured confounding to test result robustness [6].
Protocol for Mitigating Selection Bias in Participant Recruitment
Purpose: To minimize systematic differences between study participants and the target population in neuroscience trials.
Procedure:
- Define Study Population: Establish clear, pre-specified scientific and practical inclusion/exclusion criteria based on disease characteristics, demographics, and clinical features [45].
- Multiple Recruitment Sources: Utilize diverse recruitment strategies (clinical sites, registries, community-based recruitment) to minimize selection bias from single-source recruitment [46].
- Comparison of Participants vs. Non-Participants: Collect limited baseline data on non-participants when possible to assess differences from participants on key characteristics [45].
- Standardized Recruitment Protocols: Implement uniform recruitment materials and procedures across all sites to minimize site-specific selection biases [46].
- Analysis of Missing Data Patterns: Document reasons for non-participation and missing data, assessing potential systematic differences [45].
Protocol for Controlling Confounding Bias
Purpose: To identify and adjust for confounding variables that may distort the association between intervention and outcomes.
Procedure:
- Confounder Identification: Use directed acyclic graphs (DAGs) to map hypothesized causal relationships and identify potential confounders based on subject matter knowledge [45] [47].
- Comprehensive Data Collection: systematically measure and document all identified potential confounders at baseline, including demographic, clinical, environmental, and genetic factors relevant to neuroscience outcomes [45].
- Statistical Adjustment: Implement appropriate adjustment methods including regression analysis, propensity score matching, stratification, or inverse probability weighting based on the data structure and research question [45] [46].
- Residual Confounding Assessment: Quantify the potential impact of unmeasured confounding using sensitivity analyses [6].
- Effect Modification Evaluation: Test for and appropriately account for effect modification through stratification or interaction terms [46].
Visualization of Bias Assessment Workflow
Bias Assessment Workflow: This diagram illustrates the systematic process for evaluating and mitigating biases in studies using synthetic control arms, from initial data assessment to final analytical decisions.
Table 3: Research Reagent Solutions for Bias Mitigation
| Tool/Resource | Function in Bias Mitigation | Application Context |
|---|---|---|
| Propensity Score Methods | Statistical technique to balance measured covariates between treatment and control groups by creating a probability of treatment assignment based on observed characteristics [6] [5] | Creating comparable synthetic control arms from observational data; adjusting for confounding in non-randomized studies |
| Real-World Data (RWD) Platforms | Provide access to longitudinal patient data from electronic health records, claims databases, and patient registries for constructing external control arms [23] [5] | Sourcing data for synthetic control arms; understanding natural history of disease for comparator groups |
| Data Harmonization Tools | Standardize variable definitions, measurement scales, and data collection methods across different sources to improve comparability [23] | Integrating multiple data sources for synthetic controls; ensuring outcome measurement consistency |
| Sensitivity Analysis Packages | Statistical software tools that quantify how results might change under different assumptions about unmeasured confounding or selection mechanisms [6] | Testing robustness of study conclusions to potential biases; quantifying uncertainty in observational studies |
| Directed Acyclic Graph (DAG) Software | Visual tools to map hypothesized causal relationships and identify potential confounders that require adjustment [45] [47] | Planning stage of studies to identify minimal sufficient adjustment sets; communicating causal assumptions |
| Dynamic Borrowing Methods | Statistical approaches that selectively incorporate historical data based on its similarity to concurrent controls, down-weighting dissimilar data [49] | Hybrid trial designs combining limited concurrent controls with synthetic controls; platform trials with historical controls |
The strategic mitigation of selection and confounding bias represents a critical challenge in modern neuroscience research and drug development. While traditional RCTs remain methodologically strongest for minimizing these biases, practical and ethical considerations increasingly necessitate alternative approaches like synthetic control arms. The key to valid scientific inference lies not in dogmatic adherence to any single methodology, but in thoughtful application of rigorous bias assessment protocols, transparent reporting of limitations, and appropriate use of statistical tools to quantify and control for systematic errors. As regulatory agencies increasingly accept well-justified synthetic control methodologies, researchers must maintain rigorous standards for evaluating data source quality, population comparability, and outcome harmonization to ensure that accelerated development pathways do not come at the cost of scientific validity and patient safety.
The use of real-world data (RWD) is transforming clinical research, particularly in the challenging field of neuroscience. Derived from electronic health records, insurance claims, and other routine healthcare sources, RWD offers unprecedented opportunities to understand disease progression and treatment effects in diverse patient populations [5]. However, the fitness for use of this data in formal research contexts, especially for constructing synthetic control arms (SCAs), depends entirely on addressing fundamental data quality challenges [50].
SCAs represent an innovative approach that uses historical clinical trial data or RWD to create external control groups, instead of recruiting patients into concurrent control arms within randomized controlled trials (RCTs) [5]. In neuroscience, where traditional RCTs face unique challenges including disease heterogeneity, high placebo effects, and ethical concerns when using placebos in serious conditions, SCAs offer a promising alternative [51] [52]. The quality and standardization of RWD becomes the critical factor determining whether SCAs can reliably support regulatory decisions and advance treatment development for neurological and psychiatric disorders.
The Data Quality Framework: Essential Dimensions for RWD
Data quality is a multidimensional concept with specific implications for RWD in clinical research. The following six dimensions provide a comprehensive framework for evaluating RWD fitness for use in SCAs [50]:
Table 1: Essential Data Quality Dimensions for RWD in Neuroscience Research
| Dimension | Definition | Impact on SCA Validity | Neuroscience-Specific Challenges |
|---|---|---|---|
| Completeness | Extent to which expected data is present | Missing values reduce statistical power and introduce bias | Cognitive assessments often incomplete in routine care; disease progression markers inconsistently recorded |
| Accuracy | Degree to which data correctly represents real-world scenario | Inaccurate data misrepresents treatment effects | Misdiagnosis common in early neurodegenerative diseases; symptom subjectivity in psychiatry |
| Consistency | Absence of variation between data representations | Inconsistencies create noise that obscures true signals | Multiple rating scales for same condition across institutions; medication dosing variations |
| Validity | Conformance to expected syntax and format | Invalid data points cannot be aggregated or analyzed | Non-standard neurological exam documentation; unstructured imaging reports |
| Uniqueness | No duplicate records for the same entity | Duplicates artificially inflate sample size and distort outcomes | Multiple care transitions (inpatient->outpatient->rehab) creating duplicate entries |
| Timeliness | Availability within expected timeframe | Outdated data doesn't reflect current standards of care | Rapidly evolving treatment landscape in multiple sclerosis; dementia staging delays |
The interconnected nature of these dimensions means that deficiencies in one area often compound issues in others. For instance, incomplete medical histories (completeness) for Parkinson's patients make it difficult to accurately stage disease progression (accuracy), which in turn affects the ability to match SCA patients to those in the experimental intervention arm [5] [50].
Comparative Analysis: SCA Versus Traditional Trial Designs
The fundamental differences between synthetic control arms and traditional randomized designs create distinct data quality requirements and challenges:
Table 2: SCA vs. Traditional RCT Designs in Neuroscience
| Design Characteristic | Traditional RCT | Synthetic Control Arm |
|---|---|---|
| Control Group Source | Concurrently randomized patients | Historical data/RWD from previous studies or clinical practice |
| Data Collection Methods | Protocol-defined, systematic assessments | Heterogeneous, care-dependent documentation |
| Completeness Assurance | Protocol mandates complete data collection | Variable completeness requiring statistical imputation |
| Accuracy Validation | Source data verification against original records | Dependent on original data entry quality in EHRs |
| Patient Matching Approach | Randomization balances known/unknown factors | Statistical matching (e.g., propensity scores) on available variables |
| Regulatory Evidence Level | Established gold standard for efficacy | Contextual support; case-by-case acceptance [5] |
| Implementation Timeline | Longer (recruitment of both arms) | Shorter (only experimental arm recruitment) |
| Ethical Considerations | 50% chance of placebo assignment in typical 1:1 randomization [9] | All participants receive experimental intervention |
The selection bias risk represents a paramount concern for SCAs. As the FDA emphasizes, bias can occur if outcome data from the historical sources is already known and inconsistent with prior experience, or if standard-of-care treatments have evolved since the RWD was collected [5]. This is particularly relevant in neuroscience, where treatment paradigms for conditions like Alzheimer's disease and multiple sclerosis have undergone significant changes in recent years.
The Neuroscience Context: Special Considerations
Neurological and psychiatric disorders present unique challenges for RWD quality:
- Diagnostic Precision: The shift from syndromic to biological definitions in neuroscience, exemplified by the Research Domain Criteria (RDoC) framework, creates mismatches with clinically documented diagnoses in RWD sources [51].
- Disease Heterogeneity: Conditions like depression encompass substantial biological variability, with 126 possible symptom combinations for major depressive episode diagnosis, complicating patient matching for SCAs [51].
- Progression Metrics: The subjective nature of many neurological symptoms and their documentation in clinical practice affects data consistency across sources [51].
Methodologies: Ensuring RWD Quality for SCAs
Experimental Protocols for RWD Quality Assessment
Establishing robust quality assessment protocols is essential before RWD can be utilized in SCAs. The following methodologies provide a structured approach:
Protocol 1: Completeness and Accuracy Validation
- Source Verification: Select a random sample of patient records (typically 5-10%) from the RWD source for verification against original medical records [50].
- Cross-System Reconciliation: Compare key variables (diagnoses, medications, procedures) across available data sources (EHR, claims, registry) for the same patients to identify discrepancies.
- Clinical Validation: Engage subject matter experts to review a subset of records for clinical plausibility, focusing on diagnosis-treatment concordance and temporal sequencing of events.
- Completeness Calculation: For each critical variable, calculate completeness percentage as (number of non-missing records / total records) × 100, with thresholds set based on planned analyses [50].
Protocol 2: Temporal Consistency Analysis
- Standards Evolution Mapping: Document changes in clinical practice guidelines, coding systems (ICD-9 to ICD-10), and assessment tools during the RWD collection period.
- Practice Pattern Analysis: Assess whether medication prescribing patterns, diagnostic approaches, and referral pathways remained consistent throughout the data collection period.
- Outcome Stability Testing: Evaluate whether key outcomes (e.g., hospitalization rates, mortality) show abrupt shifts unrelated to known interventions or policy changes.
The following workflow illustrates the comprehensive process for transforming raw RWD into a quality-validated dataset suitable for SCA construction:
Advanced Statistical Methods for Quality Assurance
Several statistical approaches have emerged specifically for addressing RWD quality challenges in SCAs:
Propensity Score Matching: This method creates comparable groups by estimating each patient's probability of being in the treatment group given their baseline characteristics, then matching treated patients with untreated patients from the RWD source having similar probabilities [5].
High-Dimensional Propensity Score (hdPS): An extension that systematically screens large numbers of covariates (including diagnoses, procedures, and medications) to automatically identify and adjust for potential confounders not specified a priori.
Negative Control Outcomes: This approach uses outcomes not expected to be affected by the treatment to detect residual confounding in the RWD, providing a quantitative assessment of unmeasured bias.
The Scientist's Toolkit: Research Reagent Solutions
Implementing robust RWD quality assurance requires specific methodological tools and approaches:
Table 3: Essential Research Reagent Solutions for RWD Quality
| Tool Category | Specific Solutions | Function in RWD Quality Assurance |
|---|---|---|
| Data Quality Profiling Tools | Automated completeness assessment scripts; Value distribution analyzers | Systematically identifies missingness patterns and anomalous values across large datasets |
| Terminology Mapping Systems | OHDSI/OMOP CDM vocabulary; UMLS terminology services | Standardizes heterogeneous coding systems (ICD, CPT, local codes) to common data model |
| Temporal Integrity Checkers | Sequence validity analyzers; Clinical timeline reconstructors | Verifies logical temporal sequences (diagnosis before treatment, lab test before procedure) |
| Linkage Quality Tools | Deterministic and probabilistic matching algorithms; Linkage validation suites | Ensures accurate patient-level data integration across disparate source systems |
| Plausibility Assessment Frameworks | Clinical rule engines; Outlier detection algorithms | Applies domain knowledge to identify clinically implausible values or combinations |
| Bias Quantification Packages | Propensity score modelers; E-value calculators | Quantifies potential confounding and selection biases in observational data [53] |
Regulatory Considerations and Future Directions
Regulatory agencies including the FDA, EMA, and MHRA have shown increasing openness to SCAs but emphasize rigorous attention to data quality [5]. The early engagement with regulatory authorities is strongly recommended to ensure the proposed data sources, quality control methods, and statistical approaches will be acceptable [5].
The FAIR Guiding Principles (Findable, Accessible, Interoperable, and Reusable) provide a framework for enhancing the utility of RWD for research purposes [54]. Implementing these principles specifically for neuroscience RWD involves:
- Findability: Creating comprehensive metadata describing the context, limitations, and provenance of neurological RWD sources.
- Accessibility: Establishing secure, compliant mechanisms for researchers to access diverse RWD sources while protecting patient privacy.
- Interoperability: Implementing common data models specifically adapted for neurological concepts and assessments.
- Reusability: Documenting data quality assessments and preprocessing steps to enable appropriate reuse across multiple research questions.
Emerging technologies, particularly large language models (LLMs), show promise for improving RWD quality by extracting structured information from unstructured clinical notes (e.g., neurologist documentation, imaging reports) and standardizing terminology [52]. As these technologies mature, they may help address fundamental data quality challenges that currently limit the utility of RWD for constructing SCAs in neuroscience.
The transformation of raw real-world data into quality-validated evidence for synthetic control arms represents both a tremendous opportunity and a substantial methodological challenge in neuroscience research. By systematically addressing the six core dimensions of data quality—completeness, accuracy, consistency, validity, uniqueness, and timeliness—researchers can unlock the potential of SCAs to accelerate therapeutic development while maintaining scientific rigor.
The successful implementation of SCAs in neuroscience requires close collaboration among clinical experts, data scientists, and regulatory specialists to ensure that the resulting evidence is both biologically meaningful and methodologically sound. As the field advances, continued attention to RWD quality will be essential for realizing the promise of more efficient, ethical, and generalizable clinical trials for neurological and psychiatric disorders.
In modern neuroscience research, particularly in areas like developmental neurotoxicity (DNT) and clinical trials for neurological disorders, two methodological frontiers are converging: advanced protocol harmonization and innovative trial designs using synthetic controls. Protocol harmonization addresses the critical challenge of standardizing data collection across multiple studies to enable meaningful analysis of combined datasets [55]. Meanwhile, synthetic control methods offer a transformative approach for comparing outcomes against constructed control groups derived from historical data rather than concurrent randomized participants [56] [57]. This guide examines how these approaches interrelate, their relative performance, and practical implementation strategies for research teams.
Core Concepts and Definitions
Protocol Harmonization
Protocol harmonization involves standardizing data collection methods, measures, and variables across different studies or cohorts to enable combined analysis. In collaborative research designs like the Environmental influences on Child Health Outcomes (ECHO) program, which pools data from over 57,000 children across 69 cohorts, harmonization uses a Common Data Model (CDM) and derived analytical variables to facilitate timely analyses and reduce errors [55]. The process requires methodical approaches to handle both extant (existing) and new data collection.
Synthetic Control Arms
Synthetic control methods represent an advanced causal inference technique that creates weighted combinations of control units to construct a "synthetic" control group that closely resembles the treated unit before an intervention [56]. In clinical research, this approach uses real-world data (RWD) and historical trial data to create external control arms, potentially replacing expensive non-treatment arms in traditional trials [13] [58]. These methods are particularly valuable when contamination between treatment and control groups is a concern or when treatment is expensive to administer at large scale [56].
Methodological Comparison: Experimental Protocols and Data Requirements
Protocol Harmonization Workflow and Implementation
The following diagram illustrates the comprehensive workflow for implementing protocol harmonization in multi-cohort research studies:
Implementation Methodology: The ECHO program's harmonization approach demonstrates a structured process for standardizing data across cohorts. The protocol distinguishes between "essential" elements (must collect) and "recommended" elements (collect if possible) for new data collection [55]. For each essential data element, the protocol allows cohorts to use preferred or acceptable measures, with understanding that data may require harmonization. The Cohort Measurement Identification Tool (CMIT) enables systematic assessment of each cohort's current measures and planned protocols, facilitating decisions about which legacy measures to incorporate as preferred, acceptable, or alternative measures [55].
Synthetic Control Method Implementation
The following diagram outlines the key steps in creating and validating synthetic control arms for clinical research:
Implementation Methodology: Synthetic control methods require carefully constructed experiments with four key steps: (1) identifying relevant treatment units and a donor pool of similar control units; (2) performing the intervention on the target unit only; (3) training the method on the pre-intervention period to create optimal weights for the synthetic control group; and (4) interpreting results by observing pre-intervention fit and post-intervention divergence [57]. The mathematical foundation expresses the synthetic control estimate (Ŷ) as a weighted combination of units in the donor pool, with the causal effect (τ̂) representing the difference between the synthetic control estimate and the observed outcome [57].
Performance Comparison: Quantitative Analysis of Research Outcomes
Table 1: Comparative Performance Metrics Across Methodological Approaches
| Performance Metric | Traditional Randomized Trials | Protocol Harmonization | Synthetic Control Arms |
|---|---|---|---|
| Patient Recruitment | 40% of trial costs [58] | Enables pooling of >57,000 participants across 69 cohorts [55] | Reduces need for concurrent control participants [13] |
| Implementation Timeline | 10+ years for drug development [58] | Dedicated time needed for harmonization but enables rapid subsequent analyses [55] | 50% reduction in trial durations reported [58] |
| Cost Efficiency | $2.6 billion per drug [58] | High initial investment but cost-effective for large-scale collaboration | 20% reduction in recruitment costs [58] |
| Statistical Power | Limited by individual study sample sizes | Addresses rare outcomes through combined cohorts [55] | Enables inference with single treated unit [56] |
| Risk of Bias | Gold standard when properly randomized | Potential for heterogeneity across cohorts [55] | Requires careful validation of pre-treatment fit [57] |
| Regulatory Acceptance | Well-established pathway | Case-by-case evaluation of harmonized data [59] | Assessed case-by-case with emphasis on validation [58] |
Table 2: Applications in Neuroscience and Neurotoxicology Research
| Research Context | Traditional Trials | Protocol Harmonization Benefits | Synthetic Control Applications |
|---|---|---|---|
| Developmental Neurotoxicity (DNT) | Standard guideline studies [59] | Harmonizes neurobehavioral, pathological, and morphometric data [59] | Historical control data for rare endpoints |
| Neurological Disorders | Randomized placebo-controlled | Combines data from multiple clinical sites | External control arms for progressive diseases |
| Rare Neurological Diseases | Challenging due to small populations | Increases power through combined cohorts | Digital twins for virtual comparisons [58] |
| Neurodevelopmental Outcomes | Controlled experimental conditions | Standardizes cognitive, motor, and behavioral assessment [55] | Leverages real-world data for comparison |
Integrated Applications in Neuroscience Research
Case Example: Developmental Neurotoxicity Assessment
In DNT studies, regulatory guidelines generate neurobehavioral, neuropathological, and morphometric data evaluated by agencies globally [59]. Protocol harmonization addresses inconsistencies in how the same study data may be interpreted across different jurisdictions. Meanwhile, synthetic control approaches could enhance these assessments by providing better historical controls for rare endpoints. The workshop proceedings from Society of Toxicology and Neurobehavioral Teratology Society meetings emphasized practical guidance for data interpretation and reporting of DNT datasets, highlighting the need for harmonized scientific approaches within different regulatory frameworks [59].
Advanced Applications: Digital Twins and AI Integration
Artificial intelligence is enabling more sophisticated applications of both harmonization and synthetic controls through digital twins - virtual patient representations that integrate real-world data with AI models to simulate disease progression and treatment responses [58]. In one case example, Sanofi's use of digital twins in an asthma trial allowed refinement of dosing strategies and eliminated the need for additional Phase 2 cohorts, saving millions and reducing trial duration by six months [58]. These approaches are particularly valuable in rare disease neuroscience research where patient populations are small and recruitment is challenging.
Table 3: Essential Methodological Tools for Implementation
| Tool Category | Specific Tools/Platforms | Function | Applicability |
|---|---|---|---|
| Data Harmonization Systems | ECHO Data Transform [55] | Converts existing and new data to Common Data Model | Multi-cohort research |
| Statistical Analysis Packages | R Synth library [57] | Implements synthetic control method with weighted combinations | Causal inference studies |
| Clinical Trial Platforms | Saama AI platform [58] | Improves data quality by over 40% with real-time insights | Industry-sponsored trials |
| Patient Recruitment AI | Deep 6 AI (Tempus) [58] | Leverages NLP to identify suitable candidates; 34% reduction in screening times | Clinical trial recruitment |
| Data Collection Systems | REDCap Central [55] | Secured web-based system for direct data entry | Multi-site studies |
| Predictive Modeling | Lantern Pharma RADR [58] | Analyzes clinical data points to predict patient responses | Precision medicine applications |
Protocol harmonization and synthetic control methods represent complementary approaches advancing neuroscience research. Harmonization enables more powerful combined analyses across existing studies, while synthetic controls offer ethical and efficient alternatives to traditional control arms. The most successful research programs will strategically implement both approaches: using harmonization to maximize value from existing data investments while employing synthetic controls to optimize future trial designs. As regulatory acceptance grows for these methodologies [58], their integration into standard research practice will accelerate, particularly for challenging areas like neurodevelopmental disorders and rare neurological diseases where traditional trial designs face significant practical and ethical constraints.
Synthetic Control Arms (SCAs) are revolutionizing clinical development by using external data to replace or augment traditional control groups in randomized controlled trials (RCTs). This approach presents a paradigm shift for neuroscience research, where patient recruitment challenges and ethical concerns around placebo use can significantly impede progress. The successful implementation of SCAs, however, is critically dependent on early and continuous regulatory engagement. This guide examines the integral role of regulatory strategy in SCA design, providing neuroscientists and drug development professionals with a structured framework for navigating the complex landscape of regulatory requirements, methodological considerations, and practical implementation challenges.
Synthetic control arms (SCAs) represent an innovative approach increasingly adopted in clinical trials, constituting a type of external control arm study [5]. Regulatory bodies like the FDA define external controls as any control group not part of the same randomized study as the group receiving the investigational therapy [5]. SCAs are generated using statistical methods applied to one or more data sources—typically real-world data (RWD) or historical clinical trial results—with the data imputed to make it comparable to the intervention population within the clinical trial [5].
The application of SCAs is particularly valuable when conducting traditional RCTs with placebo or standard-of-care arms presents ethical, practical, or feasibility challenges [5]. While RCTs remain the gold standard for evaluating medical treatments, maintaining a concurrent control arm can sometimes be unethical, impractical, or infeasible, potentially increasing patient burden and threatening trial completion [5] [6]. In such scenarios, SCAs provide supportive evidence that contextualizes the treatment effect and safety profile [5].
For neuroscience research, where diagnostic complexity, disease heterogeneity, and high placebo responses often complicate trial design, SCAs offer promising alternatives. They can reduce the number of patients required in traditional control arms, particularly active-comparator or standard-of-care arms, thereby decreasing study costs, accelerating results, and enhancing clinical trial participation attractiveness [60]. The growing adoption of SCAs reflects their potential to address persistent challenges in neurological drug development while maintaining scientific rigor and regulatory standards.
SCA Versus Traditional Trial Designs: A Comparative Analysis
Fundamental Design Differences
Traditional randomized controlled trials (RCTs) represent the established benchmark for evaluating experimental interventions, with patients typically randomized to either an experimental intervention arm or a control arm receiving placebo or standard-of-care [6]. This approach, while methodologically robust, presents significant challenges including patient recruitment difficulties, high costs, and ethical concerns when patients potentially forego effective treatment [6] [23].
In contrast, SCAs utilize external control data derived from sources such as previous clinical trials, electronic health records (EHRs), payer claims, product and disease registries, and patient-reported outcomes [5] [60]. The SCA methodology applies statistical techniques to create comparable control groups that can replace or augment traditional control arms, potentially accelerating trial timelines and reducing costs while maintaining scientific validity [60].
Table 1: Comparative Analysis of Trial Design Attributes
| Attribute | Traditional RCT | Synthetic Control Arm |
|---|---|---|
| Control Group Source | Concurrently randomized patients | Historical clinical trial data, real-world evidence, disease registries |
| Patient Recruitment | Requires full cohort recruitment | Reduced recruitment for control arm |
| Ethical Considerations | Patients may receive placebo | All participants receive investigational treatment |
| Time Requirements | Longer duration for full enrollment | Potentially accelerated timelines |
| Cost Implications | Higher per-patient costs | Significant cost savings possible |
| Regulatory Acceptance | Established gold standard | Growing acceptance with validation |
Quantitative Advantages of SCAs
The return on investment for SCAs can be substantial, particularly in specialized fields like neuroscience. Analysis indicates that oncology trials using SCAs can achieve 20% to 50% reduction in control cohorts, generating approximately $10 million to $20 million in savings per trial [60]. Beyond direct financial benefits, this approach allows approximately 300 patients who would traditionally be enrolled in comparator arms to instead receive innovative treatments in a typical 600-patient Phase 3 trial [60].
For neuroscience applications, where patient recruitment often proves challenging and standard of care may be well-established, SCAs present particularly compelling advantages. They can reduce dropout rates by eliminating the possibility of placebo assignment, thus addressing a critical obstacle in neurological trials where patients may seek alternative treatments if their condition deteriorates [5]. Additionally, SCAs may reduce the burden of disease assessments, as sponsors may require less frequent monitoring to determine disease progression [5].
Limitations and Considerations
Despite their advantages, SCAs present unique limitations that researchers must carefully consider. The validity and applicability of SCAs are intrinsically limited by the quality and quantity of data fed into their algorithms [5]. Selection bias represents a particular concern if outcomes of clinical trials used as SCA data sources are already known but inconsistent with prior experience [5].
SCAs may not fully capture the diversity of patient populations or reflect changes in the standard of care over time, potentially limiting the generalizability of trial results [5]. This challenge is especially relevant in neuroscience, where diagnostic criteria and treatment paradigms evolve rapidly. Researchers must also consider that despite growing acceptance, regulatory agencies may still approach trials with SCAs cautiously, requiring robust justification and validation of the methodology [5].
The Regulatory Landscape for Synthetic Control Arms
Evolving Regulatory Positions
Regulatory agencies globally have demonstrated increasing openness to SCAs while emphasizing the need for rigorous methodological standards. The FDA has accepted the use of external controls, where justified, to support regulatory decisions, stating in its latest guidance that external controls should be considered on a case-by-case basis [5]. Similarly, the European Medicines Agency (EMA) recognizes that SCAs can be a valuable tool when conventional trials present challenges, particularly in rare diseases or life-threatening conditions [5].
This regulatory evolution is evidenced by several approved applications. The FDA approved cerliponase alfa for a specific form of Batten disease based on an SCA study comparing 22 patients in a single-arm trial versus an external control group of 42 untreated patients [6]. Similarly, alectinib, a non-small cell lung cancer treatment, received expanded labeling across 20 European countries based on an SCA study using external data from 67 patients [6]. These precedents demonstrate regulatory willingness to accept well-designed SCA applications while underscoring the importance of methodological rigor.
Regulatory Engagement Framework
Early and continuous regulatory engagement represents a critical success factor for SCA-based trials. The FDA, EMA, and MHRA all recommend early engagement to ensure agencies can provide feedback on proposed approaches [5]. Researchers should present regulators with comprehensive justifications for why an SCA design is appropriate, detailed descriptions of data sources with selection rationales, proposed statistical analyses, and comprehensive data management plans [5].
Table 2: Key Regulatory Considerations for SCA Submissions
| Regulatory Element | Documentation Requirements | Agency Emphasis |
|---|---|---|
| Study Justification | Rationale for SCA use, ethical considerations, feasibility assessment | Clear explanation why RCT is impractical or unethical |
| Data Source Selection | Comprehensive description of all accessed data sources, justification for inclusions/exclusions | Transparency in data provenance and quality assessment |
| Methodological Approach | Detailed statistical analysis plan, matching methodology, handling of missing data | Robustness of methods to minimize bias and confounding |
| Validation Strategy | Sensitivity analyses, comparison with historical controls where available | Assessment of result robustness across different assumptions |
| Patient Matching | Propensity scoring methods, covariate balance assessment, handling of temporal changes | Demonstration of comparability between treatment and control groups |
Regulators extensively emphasize the need to reduce bias in SCAs, highlighting the importance of early SCA design consideration during clinical trial protocol development to inform factors such as eligibility criteria and covariates [5]. The FDA specifically recommends that sponsors document and describe all accessed data sources in associated study protocols and provide information on why data sources are excluded [5]. This transparency enables regulators to assess potential biases and data quality issues that might affect trial validity.
Experimental Protocols for SCA Implementation
SCA Development Workflow
Implementing a robust SCA requires a methodical, multi-stage approach. The following workflow outlines the key stages in developing a regulatory-compliant SCA:
Data Source Evaluation and Selection
The foundation of any valid SCA lies in appropriate data source selection. SCAs are constructed using patient-level data obtained from patients not involved in the investigational clinical trial, with patients "matched" using statistical methods to achieve balanced baseline features [5]. Data primarily arises from large datasets of historical clinical trials and real-world data (RWD), each presenting distinct advantages and challenges [5].
Clinical trial data is generally lower volume but highly standardized with good quality, though it may not represent the broader patient population due to recruitment biases [5]. Conversely, RWD offers higher volume but often comes from multiple sources with worse standardization, requiring more extensive processing [5]. RWD is also more likely to contain missing data, necessitating careful consideration of whether specific patient data remains usable or how to impute minor missing data [5].
Researchers should design the SCA early in protocol development and implement it once the clinical trial protocol is finalized, initiating recruitment to enable patient matching while avoiding biases from manipulating the clinical trial protocol to match available SCA data [5]. This sequential approach ensures the SCA complements rather than dictates trial design, maintaining scientific integrity while leveraging external data sources.
Statistical Matching Methodologies
Once appropriate data sources are identified and processed, data matching of synthetic control individuals with investigational participants can proceed. Multiple statistical methods exist for this matching, with propensity scoring methods being particularly prominent [5]. There is significant regulatory interest in these methodologies, and selecting approaches acceptable to regulatory authorities is paramount [5].
The matching process aims to create balanced cohorts where the distribution of measured baseline covariates is similar between the treatment group and the synthetic control group. This balance is crucial for generating unbiased treatment effect estimates. Successful implementation requires:
- Comprehensive identification of potential confounding variables
- Appropriate handling of missing data through multiple imputation or other validated techniques
- Assessment of covariate balance using standardized differences or statistical tests
- Iterative refinement of matching algorithms to achieve optimal balance
Regulatory agencies do not recommend a particular analytical method for externally controlled trials, acknowledging that no single statistical approach suits all trials involving external control arms [5]. This flexibility necessitates thoughtful method selection and robust justification tailored to specific trial characteristics and research questions.
Successful SCA implementation requires specialized methodological expertise and access to comprehensive data resources. The following table outlines essential components for researchers developing SCAs for neuroscience applications:
Table 3: Research Reagent Solutions for SCA Implementation
| Tool Category | Specific Applications | Implementation Considerations |
|---|---|---|
| Real-World Data Platforms | Electronic health records, disease registries, claims data | Data quality assessment, interoperability standards, privacy compliance |
| Statistical Software | Propensity score matching, Bayesian methods, machine learning | Regulatory acceptance, validation requirements, documentation capabilities |
| Data Standards | CDISC, OMOP, FHIR | Interoperability, regulatory familiarity, mapping requirements |
| Validation Frameworks | Sensitivity analyses, quantitative bias analysis, bootstrap validation | Comprehensive assessment of robustness to assumptions and missing data |
| Regulatory Documentation | eCTD format, analysis data sets, patient profiles | Alignment with agency expectations, transparency, reproducibility |
Beyond technical resources, successful SCA implementation requires specialized expertise in statistical methods, regulatory science, and clinical neurology. Early consultation with statisticians experienced in causal inference methods and regulatory professionals familiar with SCA submissions can prevent methodological missteps and facilitate smoother regulatory review [5] [6]. Additionally, engagement with clinical neurologists ensures that SCA designs reflect contemporary practice patterns and clinically meaningful endpoints.
Regulatory Strategy: Building Confidence in SCA Designs
Proactive Regulatory Engagement
Early regulatory engagement represents perhaps the most critical element in successful SCA implementation. Sponsors should present regulators with comprehensive rationales for why the proposed study design is appropriate, detailed descriptions of data sources with selection justifications, proposed statistical analyses, and detailed data management plans [5]. This proactive approach allows agencies to provide feedback on proposed approaches before significant resources are committed.
Regulatory discussions should explicitly address potential biases and methodological limitations, presenting comprehensive strategies to mitigate these concerns. The FDA emphasizes the need for early consideration of SCA design during clinical trial protocol development to inform factors such as eligibility criteria and covariates [5]. Researchers should also carefully document all data sources accessed and provide clear rationales for source exclusion, enabling regulators to assess potential selection biases [5].
Validation and Sensitivity Analyses
Comprehensive validation strategies are essential for establishing SCA credibility with regulatory agencies. Researchers should conduct extensive sensitivity analyses to assess result robustness across different methodological assumptions and potential sources of bias [6]. These analyses might include:
- Varying propensity score matching algorithms and caliper widths
- Assessing impact of unmeasured confounding through quantitative bias analysis
- Testing different approaches for handling missing data
- Comparing results across multiple external data sources when available
The SCHOLAR-1 and MAMMOTH trials in oncology provide exemplary models for such validation approaches, demonstrating how comprehensive sensitivity analyses can build regulatory confidence in SCA methodologies [23]. Similar rigorous validation should be standard practice in neuroscience applications, where disease progression trajectories and treatment responses may be particularly variable.
Synthetic control arms represent a transformative methodology for neuroscience clinical trials, offering potential solutions to persistent challenges in patient recruitment, ethical concerns, and escalating development costs. Their successful implementation, however, depends critically on rigorous methodology, comprehensive validation, and—most importantly—early and continuous regulatory engagement. By adopting a strategic approach to SCA design that prioritizes regulatory collaboration from the earliest stages of protocol development, neuroscientists and drug development professionals can harness the potential of this innovative methodology while maintaining the scientific rigor necessary for regulatory approval and, ultimately, improving patient care.
Head-to-Head: Validating Efficacy and Comparing Synthetic vs. Traditional Controls
Synthetic Control Arms (SCAs) represent a paradigm shift in clinical trial design, leveraging historical and real-world data to create virtual control groups. In neuroscience research, where patient recruitment is challenging and ethical concerns around placebos are pronounced, SCAs offer a compelling alternative to traditional Randomized Controlled Trials (RCTs). The data demonstrates that SCAs can significantly accelerate development timelines, reduce prohibitive costs, and improve patient recruitment and retention, thereby speeding the delivery of novel therapies to patients with neurological conditions.
Quantitative Comparison: SCA vs. Traditional Trial Designs
The advantages of Synthetic Control Arms can be quantified across key operational metrics, offering substantial improvements over the traditional clinical trial model.
Table 1: Quantitative Advantages of Synthetic Control Arms
| Performance Metric | Traditional Randomized Controlled Trial (RCT) | Synthetic Control Arm (SCA) | Quantitative Advantage & Source |
|---|---|---|---|
| Patient Recruitment | Accounts for ~40% of total trial costs; challenging for rare diseases [58] [61]. | Reduces number of patients needed for control arm by up to 2/3 in some cases; enhances recruitment by eliminating placebo dilemma [62] [30]. | Faster enrollment & 200% faster enrollment reported with data-driven designs [58]. |
| Overall Trial Duration | Can take over 10 years from start to completion [58] [61]. | Can shorten overall trial durations by up to 50% [58]. | Accelerated development timeline by ~50%. |
| Overall Drug Development Cost | Averages over $2.6 billion per approved drug [58] [61]. | AI-driven designs (including SCAs) can cut recruitment costs by 20% and significantly reduce operational costs [58] [30]. | Significant cost reduction, primarily from reduced recruitment and operational burdens. |
| Trial Screening Time | Lengthy screening processes contribute to long timelines. | AI and RWD can reduce screening times by 34% [58]. | 34% reduction in screening time. |
| Ethical Patient Impact | Patients in control arm may receive placebo or outdated standard of care, leading to dropout rates over 30% in some long-term neurology trials. | Allows more patients to receive the investigational treatment; addresses ethical concerns of placebo use in severe diseases [62] [38] [10]. | Improves patient access to experimental therapy and trial retention. |
Experimental Protocols: Methodologies for Constructing and Validating SCAs
The construction of a regulator-grade Synthetic Control Arm is a rigorous process that relies on sophisticated statistical methods and high-quality data. The following workflow outlines the core protocol.
SCA Construction and Validation Workflow
Phase 1: Data Foundation
Protocol 1.1: Data Source Selection and Aggregation The integrity of an SCA depends on the quality and relevance of the underlying data.
- Data Sources: SCAs are constructed from two primary sources:
- Historical Clinical Trial Data: Considered the "gold standard" for building SCAs due to its high quality, standardized collection procedures, and detailed capture of covariates and endpoints [62] [10]. For example, platforms may leverage databases from over 36,000 historical clinical trials [62].
- Real-World Data (RWD): Sourced from electronic health records (EHRs), patient registries, and claims databases [39] [30]. RWD provides large sample sizes and reflects diverse treatment settings but requires extensive curation to handle missing or non-standardized data [13].
- Data Integration: In many studies, a mixed approach is used, combining both clinical trial and RWD to maximize data availability and robustness [39].
Protocol 1.2: Data Processing and Curation Raw data must be transformed into an analysis-ready format.
- Standardization and Harmonization: Data from disparate sources are mapped to a common data model. This includes standardizing medical terminologies, units of measurement, and time scales [62] [61].
- De-identification: Patient-level data is anonymized to protect privacy [61].
- Management of Missing Data: Advanced statistical techniques, such as multiple imputation, are employed to handle missing covariate data. For example, one study used 15 imputations per patient to generate complete datasets for analysis [39].
Phase 2: Statistical Analysis and Validation
Protocol 2.1: Patient Matching and Covariate Balancing This critical step ensures the SCA is comparable to the experimental arm at baseline.
- Propensity Score (PS) Estimation: A logistic regression model is typically used to estimate the probability (propensity) of a patient being in the experimental group versus the external control group, based on key baseline characteristics [39].
- Weighting Procedures: The Stabilized Inverse Probability of Treatment Weighting (sIPTW) method uses the propensity scores to weight patients in the SCA, creating a balanced pseudo-population where the distribution of covariates mimics that of the experimental arm [39].
- Assessment of Balance: After weighting, Standardized Mean Differences (SMD) are calculated for each covariate. An SMD of <0.1 for all key prognostic factors indicates successful balance between the groups [39].
Protocol 2.2: Outcome Analysis and Sensitivity Testing
- Primary Endpoint Comparison: Once balance is achieved, outcomes (e.g., Overall Survival, disease progression scores) are compared between the experimental arm and the weighted SCA using standard statistical methods like Cox regression for time-to-event data [39].
- Sensitivity Analyses ("Tipping Point Analyses"): These are essential to assess the robustness of the findings. Analyses test how strong an unmeasured confounder would need to be to overturn the study's conclusion, providing regulators with confidence in the results [10].
- Hybrid Design Validation: In a hybrid design, a small randomized control arm is retained. The outcomes of this internal control group are compared to the SCA. If the outcomes are similar, it provides strong evidence that the SCA is a valid counterfactual, mitigating concerns about unmeasured confounding [10].
The Scientist's Toolkit: Research Reagent Solutions for SCA Construction
The following table details the essential "research reagents"—the data, methodologies, and computational tools—required to implement SCAs in neuroscience research.
Table 2: Essential Research Reagents for SCA Development
| Tool Category | Specific Tool / Methodology | Function & Application in Neuroscience |
|---|---|---|
| Data Assets | Historical Clinical Trial Databases (e.g., Medidata Enterprise Data Store) | Provides high-quality, structured data from previous trials in indications like Alzheimer's, Parkinson's, or Spinal Cord Injury, serving as the foundation for the SCA [62] [61]. |
| Real-World Data (RWD) from Neurological Registries & EHRs | Supplements trial data with longitudinal, real-world patient journeys; crucial for rare diseases or long-term outcomes [39] [8] [30]. | |
| Statistical Reagents | Propensity Score (PS) Modeling | A statistical tool (e.g., via logistic regression) to estimate the probability of group assignment, used to control for selection bias by matching or weighting [39]. |
| Stabilized Inverse Probability of Treatment Weighting (sIPTW) | A weighting technique that uses propensity scores to create a balanced synthetic cohort, minimizing differences in baseline characteristics between trial and control patients [39]. | |
| Computational & AI Reagents | Machine Learning Architectures (e.g., CNN, Transformers) | Advanced models to predict granular, patient-level outcomes for controls. For example, a Convolutional Neural Network (CNN) was used to predict segmental motor scores in spinal cord injury research with high precision (RMSE <0.55) [8]. |
| Multiple Imputation Techniques | A statistical method for handling missing data by generating multiple plausible values for missing points, ensuring the analysis dataset is robust and complete [39]. | |
| Regulatory & Validation Reagents | Hybrid Control Arm Design | A study design that combines a small prospective randomized control arm with a larger SCA, used to validate the SCA against a gold-standard and increase regulatory acceptance [10]. |
| Tipping Point Analysis | A sensitivity analysis that quantifies the robustness of the trial conclusion to potential unmeasured confounding, a key requirement for regulatory submissions [10]. |
Case Study in Neuroscience: Validating SCAs in Spinal Cord Injury
A 2025 benchmark study provides a compelling proof-of-concept for using SCAs in a neurological context. The study aimed to build synthetic controls from personalized predictions of neurological recovery after Spinal Cord Injury (SCI)—a rare and heterogeneous condition where RCTs are exceptionally challenging [8].
- Experimental Protocol: Researchers used data from the European Multicenter Study about SCI (EMSCI). They benchmarked six machine learning architectures, including regularized linear regression, random forests, and deep learning models (CNNs, Transformers), to predict sequences of segmental motor scores—a granular endpoint in SCI trials [8].
- Key Findings: A Convolutional Neural Network (CNN) was identified as the best-performing model, achieving a median root mean squared error (RMSE) below the neurological level of injury of 0.55, demonstrating high predictive accuracy for individual patient recovery [8].
- Trial Simulation: The researchers simulated a clinical trial randomization process. The results demonstrated that synthetic controls generated by these models were a viable alternative, reducing intercohort heterogeneity and showing no significant differences compared to randomized controls [8]. This validates that SCAs can maximize the number of patients receiving an investigative treatment in rare neurological disorders without compromising scientific rigor.
Synthetic control arms (SCAs) represent an innovative approach in clinical trial design, using existing data to create virtual control groups. In neuroscience research, where patient recruitment is challenging and placebo arms can be ethically problematic, SCAs offer apparent advantages. However, their adoption requires careful consideration of significant ethical and practical trade-offs. This guide objectively compares the performance of SCA-based trials against traditional randomized designs, examining limitations through current experimental data and regulatory experiences, with a specific focus on implications for neuroscience drug development.
How Synthetic Control Arms Work: Methodologies and Mechanisms
SCAs are constructed using statistical methods to create control groups from historical data sources rather than concurrently randomized patients. Two primary methodological approaches dominate current applications:
Real-World Data (RWD) and Clinical Trial Archives: SCAs are typically built from mixed data sources, including historical clinical trial data and real-world evidence from disease registries and electronic health records [7] [5]. The data quality is crucial, with clinical trial data generally being more standardized but potentially less representative, while RWD offers larger volumes but requires more processing due to formatting inconsistencies and missing data points [5].
Propensity Score Balancing: The most common statistical method involves using propensity scores (PS) to balance covariates between the investigational arm and the synthetic control group. Researchers typically employ approaches like stabilized Inverse Probability of Treatment Weighting (sIPTW) based on propensity scores to achieve balance across known prognostic factors [7]. This method weights patients in both groups to create a balanced distribution of baseline characteristics, simulating the balance that would be achieved through randomization.
Hybrid Control Arms: A more recent development combines small randomized control groups with externally sourced patients to create augmented control arms. This hybrid approach allows researchers to validate the SCA against a concurrent control subset, increasing confidence in the comparison [10].
Experimental Workflow for SCA Implementation
The standard workflow for implementing synthetic control arms in clinical research follows a multi-stage process of data collection, balancing, and validation, as detailed below:
Comparative Performance: SCA vs. Traditional Trial Designs
The practical implementation of SCAs reveals significant trade-offs when compared to traditional randomized controlled trials (RCTs). The following table summarizes key comparative metrics based on current evidence:
| Performance Metric | Traditional RCTs | Synthetic Control Arms | Experimental Evidence |
|---|---|---|---|
| Statistical Power | Higher (direct randomization) | Potentially reduced | DLBCL trial: 30% power for HR=0.743 vs. 249 patients in RCT [63] |
| Recruitment Efficiency | Slower (requires full recruitment) | Faster (smaller active arm) | Ovarian cancer case: Reduced Phase II trial size [10] |
| Data Quality Control | Standardized protocols | Variable quality sources | RWD has "worse standardization" than clinical trial data [5] |
| Bias Control | Controls known and unknown confounders | Only known, measured confounders | "Unknown confounding" remains a key concern [10] |
| Endpoint Reliability | Consistent across all endpoints | Better for objective endpoints (OS) | Protocol-dependent endpoints (PFS) more vulnerable to bias [63] |
| Regulatory Acceptance | Established gold standard | Case-by-case assessment | FDA CRL for SCA in spinocerebellar ataxia [64] |
Quantitative Performance Data from Recent Studies
DLBCL Trial Simulation: A recent study testing SCAs in diffuse large B-cell lymphoma demonstrated the power limitations of this approach. When researchers replaced the internal control arm of the SENIOR trial with an SCA, the resulting hazard ratio of 0.743 (95% CI 0.494-1.118) had only 30% statistical power to detect a true effect, based on the included patient numbers [63].
Trial Efficiency Gains: Despite power limitations, SCAs can improve trial efficiency in specific contexts. One use case demonstrated that an SCA in ovarian cancer helped reduce the size of a subsequent Phase II trial by providing a more precise treatment effect estimate during early development [10].
Real-World Data Performance: In a study combining real-world data with historical clinical trial patients, researchers created a mixed SCA for elderly DLBCL patients. After balancing using sIPTW, all covariates were well balanced, and overall survival between the mixed SCA and the experimental arm showed no statistical difference (HR 0.743 [0.494-1.118], p = 0.1654) [7].
Ethical Considerations in SCA Implementation
The adoption of SCAs presents distinctive ethical considerations that differ from traditional trial designs. The table below compares these ethical dimensions:
| Ethical Dimension | Traditional RCTs | Synthetic Control Arms | Practical Implications |
|---|---|---|---|
| Placebo Use | Some patients receive placebo | All participants receive active treatment | Eliminates ethical concerns about placebo use in serious conditions [38] |
| Patient Burden | High (strict protocols, frequent visits) | Reduced for some participants | "Reduces the burden of disease assessments" for patients [5] |
| Recruitment Ethics | Challenging for rare diseases | Improved access to trials | Particularly beneficial for rare diseases where recruitment is difficult [10] |
| Data Privacy | Controlled research environment | Complex privacy considerations | Synthetic data may reduce "risk of revealing sensitive patient information" [65] |
| Representativeness | Narrow eligibility criteria | Broader real-world populations | RWD may better represent "ethnic, socio-economic, or age groups" [5] |
| Transparency | Established reporting standards | Evolving disclosure requirements | Requires "preplanned use of an SCA" to avoid post-hoc bias [63] |
Regulatory Assessment and Validation Challenges
Recent regulatory experiences highlight the practical limitations of SCAs in drug development:
FDA Rejection of SCA-Based Application: In November 2025, the FDA issued a Complete Response Letter for Biohaven's VYGLXIA for spinocerebellar ataxia, despite statistically significant results from a real-world evidence study using an external control arm. The FDA cited "potential bias, design flaws, lack of pre-specification and unmeasured confounding factors" as limitations, noting that "a large and robust treatment effect would be needed to overcome the biases of an externally controlled trial" [64].
Prospective Planning Requirements: Regulatory agencies emphasize that SCA methodologies must be pre-specified before knowing single-arm trial results to avoid bias. The statistical analysis plan should include matching variables and prognostic covariates for adjusted efficacy analyses [63].
Endpoint Selection Limitations: Endpoints based on protocolized assessments, such as progression-free survival (PFS), are more vulnerable to bias in SCA studies compared to objective endpoints like overall survival (OS) or acute event-based endpoints such as time-to-next-treatment [63].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Implementing rigorous SCA methodologies requires specific analytical tools and approaches. The following table details key solutions for addressing common challenges:
| Research Tool | Function | Application Context |
|---|---|---|
| Stabilized Inverse Probability of Treatment Weighting (sIPTW) | Balances baseline covariates between treatment and synthetic control groups | Used in DLBCL study to balance age, disease stage, ECOG performance status [7] |
| Multiple Imputation Methods | Handles missing data in real-world data sources | "Across" method with 15 imputations per patient used for REALYSA data with high missingness [7] |
| Propensity Score Estimation | Estimates probability of treatment assignment based on covariates | Logistic regression with clinical factors creates scores for weighting [7] |
| Tipping Point Analyses | Quantifies robustness of results to potential unmeasured confounding | Assesses how much unmeasured confounding would nullify the treatment effect [10] |
| Standardized Mean Differences (SMD) | Measures covariate balance after weighting | Post-weighting assessment to ensure adequate balance (SMD <0.1) [7] |
| Hybrid Control Designs | Combines small randomized controls with external data | Allows validation of SCA against concurrent controls; favored by FDA [10] |
| Synthetic Data Generators | Creates artificial instances from empirical data distribution | CTGAN and Survival CTGAN algorithms generate synthetic control arms [65] |
Synthetic control arms present a promising but nuanced alternative to traditional randomized designs in neuroscience research and drug development. While they offer ethical advantages in reducing placebo use and practical benefits in accelerating recruitment, particularly for rare diseases, their limitations are substantial. Statistical power constraints, vulnerability to unmeasured confounding, and regulatory scrutiny require careful methodological planning and transparent validation. The recent FDA rejection of an SCA-based application in spinocerebellar ataxia underscores that robust treatment effects and rigorous prospective designs are essential for regulatory acceptance. As methodological standards evolve, hybrid approaches that combine small randomized controls with synthetic augmentation may offer the most promising path forward, balancing ethical considerations with scientific rigor in neuroscience therapeutic development.
The table below summarizes the core performance metrics of synthetic control arms (SCAs) against traditional trial designs, highlighting key efficiency gains and methodological considerations.
| Performance Metric | Traditional Randomized Controlled Trial (RCT) | Synthetic Control Arm (SCA) | Supporting Data/Evidence |
|---|---|---|---|
| Patient Recruitment | Accounts for ~40% of trial costs; major bottleneck [58]. | Reduces need for control-group participants; overcomes recruitment challenges in rare diseases [10] [66]. | |
| Screening Time | Baseline (No specific reduction) | Can reduce screening time by 34% [58]. | AI-powered tools demonstrated a 34% reduction [58]. |
| Trial Duration | Often exceeds 10 years [58]. | Shortens trial timelines significantly [66]. | Sanofi's use of digital twins (a related AI model) reduced a trial duration by 6 months [58]. |
| Cost Implications | Can exceed $2.6 billion per drug [58]. | Reduces costs by limiting patient enrollment and operational burdens [10] [66]. | Using AI for analysis early in development helped size a Phase II trial, saving time and money [10]. |
| Primary Methodological Risk | Placebo use in severe diseases poses ethical dilemmas [58]. | Risk of "unknown confounding" causing biased treatment effect [10]. | |
| Key Mitigation Strategy | Randomization balances known and unknown prognostic factors. | Use of high-quality historical data and "tipping point" sensitivity analyses [10]. | |
| Regulatory Acceptance | Established gold standard [66]. | Considered innovative; accepted on a case-by-case basis, especially in rare diseases and unmet need [10]. | Successes reported with both FDA and EMA [10]. |
Experimental Protocols for Validation
A rigorous, multi-stage validation framework is essential for establishing the credibility of Synthetic Control Arms. This process extends from initial analytical checks to demonstrating real-world clinical value [67].
Stage 1: Establishing Analytical Validity
This first stage answers the question: Does the model and the data it generates produce reliable and accurate results under controlled conditions? [67]
- Objective: To ensure the generative model creating the synthetic patient data is technically sound and that the SCA's outcomes are precise and reproducible before clinical application.
- Protocol:
- Data Generation and Comparison: Generate multiple synthetic datasets from the same source historical data. The statistical properties and distributions of these datasets should be consistent with each other and with the original data.
- Method Comparison Analysis: Employ statistical methods like Passing-Bablok regression or Deming regression to compare the outcomes (e.g., a key biomarker level) of the synthetic control arm against a reference, such as a small, prospectively collected control dataset or a high-quality historical trial dataset [67].
- Agreement Assessment: Use Bland-Altman plots to visualize the bias and the limits of agreement between the SCA outcomes and the reference standard, identifying any systematic over- or under-estimation [67].
- Lot-to-Lot Consistency: Assess the consistency of results across different synthetic data generation runs ("lots") to ensure model stability [67].
Stage 2: Demonstrating Clinical Validity
This stage answers the question: Does the measured outcome from the SCA correctly classify the disease state or treatment effect in the intended patient population? [67]
- Objective: To validate that the SCA can replicate known clinical outcomes and show discriminatory performance equivalent to a real control arm.
- Protocol:
- Retrospective Validation Study: Design a study where both an investigational treatment and a standard-of-care control group are simulated from historical data. The SCA methodology must correctly identify the known, inferior performance of the control.
- ROC/AUC Analysis: Use Receiver Operating Characteristic (ROC) curves and Area Under the Curve (AUC) analysis to measure the SCA's ability to discriminate between treatment responders and non-responders. DeLong's test can be used to compare the statistical significance of differences between AUCs [67].
- Statistical Testing for Agreement: For categorical outcomes, use McNemar's test for paired nominal data to check for disagreements between the SCA and a reference. Use Cohen's κ to measure inter-rater agreement beyond chance [67].
- Covariate Adjustment: Apply logistic regression to adjust for clinical covariates and ensure the treatment effect is not confounded by imbalances in baseline patient characteristics [67].
Stage 3: Assessing Clinical Utility
This final stage answers the question: Does using the SCA in a trial actually lead to better drug development decisions and improved patient outcomes? [67]
- Objective: To demonstrate that the integration of an SCA provides tangible benefits in efficiency, ethics, and decision-making.
- Protocol:
- Pragmatic or Hybrid Trial Design: Implement a hybrid trial design, which combines a small, prospective randomized control arm with a larger SCA to supplement the control group [10].
- Outcome-Focused Endpoints: Measure endpoints that reflect real-world impact, such as:
- Economic Analysis: Conduct a budget-impact model or cost-per-QALY analysis to quantify the value for health systems, demonstrating reduced costs per successful drug developed [67].
Workflow and Signaling Pathways
SCA Validation Framework
The following diagram illustrates the integrated, multi-stage validation workflow for Synthetic Control Arms, from data preparation to regulatory and clinical application.
Sensitivity Analysis Protocol
This diagram outlines the specific workflow for conducting sensitivity analyses, which are critical for assessing the robustness of Synthetic Control Arm results and addressing regulator concerns about bias.
The Scientist's Toolkit: Research Reagent Solutions
The table below details key methodological components required for implementing and validating synthetic control arms in clinical research.
| Tool / Solution | Function in SCA Research |
|---|---|
| Generative AI Models [66] | Creates statistically accurate, privacy-preserving synthetic patient datasets from historical sources to form the core of the SCA. |
| High-Quality Historical Data [10] | Serves as the foundational input; high-quality data from previous clinical trials reduces the risk of unknown confounding. |
| Bayesian Statistical Models [58] | Provides a probabilistic framework for incorporating prior knowledge and dynamically adapting trial parameters using incoming data. |
| Hybrid Trial Design [10] | A study design that combines a small, prospective randomized control arm with a larger SCA, used to validate the SCA and mitigate bias. |
| Tipping Point Analysis [10] | A specific sensitivity analysis that determines how much unmeasured confounding would be required to nullify the observed treatment effect. |
| Staged Validation Framework [67] | A structured roadmap that guides developers from analytical bench validation through clinical utility assessment, de-risking development. |
Clinical trials are the cornerstone of medical advancement, yet they present significant challenges in neuroscience due to the heterogeneity of neurological and psychiatric disorders. Traditional randomized controlled trials (RCTs) remain the gold standard for evaluating new medical treatments, where patients are randomly assigned to either an investigational treatment or a control group (placebo or standard-of-care) [5]. However, synthetic control arms (SCAs) represent an innovative approach that uses external control groups constructed from historical clinical trial data or real-world data (RWD) through statistical methods [5] [9]. These approaches are particularly relevant in neuroscience, where patient heterogeneity, diagnostic complexity, and ethical concerns about placebo use create unique challenges for clinical development [51] [52].
The adoption of innovative trial designs has grown substantially since 2011, with neuroscience and rare diseases representing therapeutic areas where these methodologies have shown significant promise [52]. This analysis examines comparative performance between traditional and synthetic control approaches through specific regulatory case studies, providing researchers with evidence-based frameworks for trial design selection in neuroscience research.
Comparative Performance Analysis: Quantitative Outcomes
The following tables summarize key performance metrics and regulatory outcomes for traditional versus synthetic control trial designs, with particular emphasis on neuroscience applications.
Table 1: Key Performance Metrics Comparison Between Traditional RCTs and SCAs
| Performance Metric | Traditional RCTs | Synthetic Control Arms | Data Source/Context |
|---|---|---|---|
| Patient Recruitment | 80% of trials fail to meet initial enrollment goals/timelines [68] | Faster recruitment; all participants receive active drug [9] [10] | Industry-wide analysis [68] |
| Typical Recruitment Challenge | Delays cost ~$8 million daily in lost revenue [68] | Significant reduction in number of patients needed [9] | Financial impact assessment [68] |
| Ethical Considerations | 50% of participants receive placebo/standard care [9] | All participants receive investigational treatment [9] | Patient allocation perspective |
| Data Source Quality | Highly standardized, prospective collection [5] | Depends on source: historical trial data (high) vs. RWD (variable) [5] [10] | Regulatory assessment framework [5] |
| Primary Regulatory Acceptance | Gold standard; universally accepted [5] | Case-by-case assessment, especially rare diseases/severe conditions [5] [10] | FDA/EMA guidance [5] [10] |
| Implementation Cost | High (patient recruitment, site management) [68] | More cost-effective; avoids control arm costs [5] | Industry cost analysis [5] [68] |
Table 2: Regulatory Success Cases for Synthetic Control Arms
| Therapeutic Area | Drug/Intervention | Regulatory Outcome | Basis for Decision | Data Source |
|---|---|---|---|---|
| Batten Disease | Cerliponase alfa | FDA approval [6] | Single-arm trial (22 patients) vs. external control (42 patients) [6] | Historical control data [6] |
| Non-Small Cell Lung Cancer | Alectinib | Label expansion across 20 European countries [6] | External dataset of 67 patients [6] | Historical cohort data [6] |
| Advanced Breast Cancer | Palbociclib | Expanded indication for men [6] | External control data [6] | Real-world evidence [6] |
| Rare Diseases | Multiple (unspecified) | Regulatory acceptance | Hybrid design with small randomized control supplemented by external data [10] | Mixed: prospective + external [10] |
Methodological Approaches and Experimental Protocols
Traditional Randomized Controlled Trial Design
Workflow Overview: Traditional RCTs follow a structured, linear pathway where all data collection occurs prospectively within the study framework.
Key Methodological Components:
- Randomization: Participants are randomly assigned to investigational or control groups to minimize selection bias and ensure group comparability [5]
- Blinding: Double-blind designs where neither participants nor investigators know treatment assignments prevent assessment bias [5]
- Prospective Data Collection: All efficacy and safety data collected according to pre-specified protocol during trial execution [5]
- Control Group Management: Placebo or standard-of-care administration with identical monitoring to investigational arm [5]
Statistical Analysis Approach: Primary analysis typically follows intention-to-treat principle using pre-specified statistical tests to compare primary endpoints between groups at predetermined significance levels [5].
Synthetic Control Arm Methodology
Workflow Overview: SCAs integrate external data sources with statistical matching to create comparable control groups, reducing prospective randomization needs.
Key Methodological Components:
Data Source Evaluation: SCAs are constructed using patient-level data from one or more sources, including historical clinical trials, real-world data (electronic health records, insurance claims), or patient registries [5] [13]. Clinical trial data is generally lower volume but highly standardized, while RWD is higher volume but requires more processing [5].
Patient Matching Methods: Patients are "matched" using statistical methods to achieve balanced baseline features such as demographics and disease composition [5]. Propensity score matching is commonly used to create comparable groups by balancing prognostic factors between the investigational arm and external control patients [6].
Bias Mitigation Approaches: Unknown confounding is addressed through tipping point analyses that test assumptions about potential confounders, and hybrid designs that combine small randomized control arms with external data supplementation [10]. The FDA has shown significant interest in this hybrid approach as it enables direct comparison between prospective randomized controls and external control patients [10].
Statistical Analysis Approach: Comparative analysis using matched groups with sensitivity analyses to test robustness of findings to potential unmeasured confounding [10] [6].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Table 3: Essential Resources for Implementing Synthetic Control Arms
| Tool/Category | Specific Examples | Function/Purpose | Implementation Considerations |
|---|---|---|---|
| Data Sources | Historical clinical trial data; Real-world data (EHR, claims); Patient registries [5] [13] | Provides control group population; Replaces prospective randomization [5] | Data quality assessment; Relevance to current population; Temporal changes in standard-of-care [5] [6] |
| Statistical Software | Propensity score modeling; Bayesian methods; Machine learning algorithms [5] [52] | Patient matching; Bias reduction; Treatment effect estimation [5] [10] | Regulatory acceptability; Transparency; Validation requirements [5] [6] |
| Data Standards | CDISC; OMOP Common Data Model; FHIR standards [69] | Data harmonization; Interoperability between sources [69] | Mapping complexity; Semantic consistency; Terminology standards [69] |
| Regulatory Frameworks | FDA RWE Program; EMA qualification advice; ICH E10/E6 guidelines [5] [6] | Defines acceptability criteria; Study design requirements [5] [6] | Early engagement recommended; Case-by-case assessment; Evolving guidance [5] [10] |
| Quality Assessment Tools | Bias risk assessment; Data completeness evaluation; Sensitivity analysis frameworks [10] [6] | Study validity evaluation; Confidence in results [10] [6] | Pre-specified analysis plans; Tipping point analyses; Hybrid design options [10] |
Regulatory Landscape and Submission Strategies
Evolving Regulatory Perspectives
Regulatory agencies recognize that maintaining concurrent control arms is sometimes unethical, impractical, or infeasible, particularly in serious diseases with unmet medical needs [5]. The FDA has accepted the use of external controls where justified, stating in its latest guidance that external controls should be considered on a case-by-case basis [5]. Similarly, the European Medicines Agency (EMA) acknowledges that SCAs can be valuable when conventional trials present challenges [5].
The regulatory approach to SCAs remains appropriately cautious, with emphasis on early engagement with agencies to ensure acceptability of proposed approaches [5]. Regulators extensively emphasize the need to reduce bias in SCAs and recommend early consideration of SCA design during clinical trial protocol development [5]. The FDA, EMA, and MHRA do not recommend a particular analytical method, acknowledging that no single statistical approach will be suitable for all trials involving external control arms [5].
Successful Regulatory Submission Strategies
Early and Strategic Engagement: Successful regulatory submissions typically involve early engagement with regulatory agencies during the protocol development phase [5] [69]. Sponsors should present reasons why the proposed design is appropriate, detail data sources with justifications for their selection, outline statistical analyses, and explain data management plans [5].
Comprehensive Documentation: Regulatory success requires thorough documentation of all data sources accessed, including justification for exclusions, and description of analytical methods used for patient matching [5] [6]. This documentation should demonstrate rigorous attention to potential biases and confounding factors [6].
Fit-for-Purpose Application: SCAs have demonstrated greatest regulatory acceptance in rare diseases and severe conditions with inadequate standard-of-care [10]. The hybrid design approach—combining small randomized controls with supplemental external data—has garnered significant FDA interest as it enables direct comparison between prospective randomized controls and external control patients [10].
Synthetic control arms represent a promising alternative to traditional RCT designs in specific scenarios where randomization is unethical, impractical, or infeasible. While traditional RCTs remain the gold standard for establishing efficacy, SCAs offer distinct advantages in patient recruitment, ethical considerations, and development efficiency [5] [9]. The growing regulatory acceptance of SCAs, particularly in neuroscience and rare diseases, reflects an evolving evidence paradigm that strategically incorporates real-world and historical data [52] [10].
Future adoption of SCAs will likely expand beyond current applications in rare diseases to include earlier phase trials and decision-making contexts without direct regulatory implications [10]. As one industry expert noted, significant potential exists for using SCAs in non-regulatory applications to improve development efficiency and decision-making [10]. Advancements in data quality, standardization, and analytical methods will further enhance the validity and applicability of SCAs across therapeutic areas [13] [52].
For researchers considering SCA implementation, success depends on early regulatory engagement, rigorous attention to bias mitigation, and strategic application in appropriate clinical contexts. When these conditions are met, SCAs offer a powerful tool for advancing therapeutic development while addressing ethical concerns and practical challenges associated with traditional controlled trials.
Conclusion
The integration of synthetic control arms represents a fundamental evolution in neuroscience clinical research, offering a powerful tool to address the profound challenges of patient recruitment, ethical concerns, and soaring costs associated with traditional trials. While not a universal replacement for RCTs, SCAs provide a scientifically rigorous and regulatory-accepted alternative, particularly valuable in rare diseases, rapidly evolving therapeutic areas, and when placebo use is problematic. Future success hinges on collaborative efforts to build high-quality, accessible data repositories, advance robust statistical methodologies for causal inference, and foster ongoing dialogue with regulatory bodies. By strategically adopting and refining SCA approaches, the neuroscience community can significantly accelerate the delivery of novel therapies to patients in need.
References
- 1. Control arm - NCATS Toolkit - NIH [https://toolkit.ncats.nih.gov/glossary/control-arm/]
- 2. Control Arm [https://friendsofcancerresearch.org/glossary-term/control-arm/]
- 3. Clinical Trial Designs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6434767/]
- 4. How External Control Arms and Real-World Data Are ... [https://veranahealth.com/how-external-control-arms-and-real-world-data-are-driving-clinical-trial-innovation/]
- 5. The Pros And Cons Of Synthetic Control Arms In Clinical ... [https://www.clinicalleader.com/doc/the-pros-and-cons-of-synthetic-control-arms-in-clinical-trials-0001]
- 6. Synthetic and External Controls in Clinical Trials [https://pmc.ncbi.nlm.nih.gov/articles/PMC7218288/]
- 7. Synthetic control arm from mixed clinical trials and real-world ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12583804/]
- 8. Exploring synthetic controls in rare diseases with a proof of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12551237/]
- 9. The Promise and Limitations of Synthetic Control Arms [https://cglife.com/blog/synthetic-control-arms-promise-limitations/]
- 10. Synthetic control arms: full impact yet to be realised [https://www.clinicaltrialsarena.com/interviews/synthetic-control-arms-full-impact-yet-to-be-realised/]
- 11. Overview of clinical study designs - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11009715/]
- 12. The Role of Synthetic Control Arms in Modern Clinical Trials [https://www.linkedin.com/pulse/role-synthetic-control-arms-modern-clinical-trials-overview-beelke-nd8we]
- 13. 2025 Trends: Leveraging Real-World Data for Synthetic ... [https://www.appliedclinicaltrialsonline.com/view/2025-trends-leveraging-real-world-data-synthetic-control-arms]
- 14. Synthetic Control Arms Market Size, Report by 2034 [https://www.precedenceresearch.com/synthetic-control-arms-market]
- 15. 36 Top RWE Platforms in 2025 [https://www.mahalo.health/insights/top-real-world-evidence-rwe-platforms]
- 16. Best RWE Companies for Patient Insights in 2025 [https://www.mamahealth.com/resources/best-rwe-companies-patient-insights]
- 17. RWE as the Top Trend in 2025 [https://www.iqvia.com/blogs/2025/01/rwe-as-the-top-trend-in-2025]
- 18. FDA vs EMA: Key Regulatory Differences in 2025 [https://pharmuni.com/2024/08/12/from-fda-to-ema-navigating-global-regulatory-requirements/]
- 19. FDA vs EMA: Key Regulatory Differences for ... [https://lsacademy.com/en/fda-vs-ema-key-regulatory-differences-for-pharmaceuticals/]
- 20. FDA and EMA Resources, Policies, and Programs ... - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK609376/]
- 21. A Basic Introduction to Clinical Data Management ... [https://acdmglobal.org/a-basic-introduction-to-clinical-data-management-regulations/]
- 22. Quality by design | European Medicines Agency (EMA) [https://www.ema.europa.eu/en/human-regulatory-overview/research-development/quality-design]
- 23. How can synthetic control arms transform clinical trials? We ... [https://quibim.com/news/synthetic-control-arm-in-clinical-studies/]
- 24. Synthetic control methods for n‐of‐1 and parallel‐group ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12230867/]
- 25. Improving propensity score weighting using machine learning - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC2807890/]
- 26. Abstract: The Machine in Propensity Scores: Comparison of Machine-Learning Models and Logistic Regression in Propensity Score Matching (Society for Social Work and Research 29th Annual Conference) [https://sswr.confex.com/sswr/2025/webprogram/Paper58593.html]
- 27. Propensity Score Matching in R — 2025 Edition [https://dev.to/vamshi_e_eebe5a6287a27142/propensity-score-matching-in-r-2025-edition-3c5c]
- 28. A comparison of machine learning algorithms and covariate balance measures for propensity score matching and weighting - PubMed [https://pubmed.ncbi.nlm.nih.gov/31090108/]
- 29. Synthetic control methods for n-of-1 and parallel-group trials in ... [https://pubmed.ncbi.nlm.nih.gov/40621876/]
- 30. Synthetic Control Arms: Overcoming Barriers in Clinical Trials [https://www.indegene.com/what-we-think/blogs/leveraging-rwd-for-synthetic-control-arms]
- 31. Development and Validation of SCACOMS, a Composite ... [https://link.springer.com/article/10.1007/s12311-024-01697-8]
- 32. AI and innovation in clinical trials | npj Digital Medicine [https://www.nature.com/articles/s41746-025-02048-5]
- 33. Benefits of synthetic control arms reinforced by buloxibutid ... [https://www.clinicaltrialsarena.com/analyst-comment/ers-2025-synthetic-control-arms-buloxibutid/]
- 34. News [https://www.oxfordharrington.org/events-news/news/oxford-harrington-rare-disease-centre-announces-2025-scholars-advancing-promising-treatments]
- 35. Oxford-Harrington Rare Disease Centre Announces 2025 ... [https://www.prnewswire.com/news-releases/oxford-harrington-rare-disease-centre-announces-2025-scholars-advancing-promising-treatments-302621835.html]
- 36. Study design challenges and strategies in clinical trials for ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2023.1098454/full]
- 37. Smarter Trial Designs for Rare Neurological Disease Trials [https://tfscro.com/resources/rare-neurological-disease-trials-smarter-design-with-natural-history-external-controls-and-real-world-evidence/]
- 38. Will synthetic control arms revolutionize clinical trials? [https://servier.com/en/newsroom/synthetic-control-arms-revolutionize-clinical-trials/]
- 39. Synthetic control arm from mixed clinical trials and real ... [https://www.nature.com/articles/s41408-025-01374-x]
- 40. When placebos aren't an option: synthetic control arms in ... [https://www.drugdiscoverynews.com/when-placebos-aren-t-an-option-synthetic-control-arms-in-rare-and-severe-diseases-16496]
- 41. Using multiple biomarkers for patient enrichment in two- ... [https://pubmed.ncbi.nlm.nih.gov/40784648/]
- 42. Brain organoids: a new paradigm for studying human ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1699814/full]
- 43. 2025 Biotech Economics: CROs, Advanced Therapies & ... [https://www.precisionformedicine.com/blog/2025-biotech-economics-cros-advanced-therapies-trends-in-funding]
- 44. Top 5 Trends in Neuroscience You Need to Know in 2025 [https://www.qmenta.com/blog/top-5-trends-in-neuroscience-you-need-to-know-in-2025]
- 45. Distinguishing selection bias and confounding bias in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4043938/]
- 46. Biases and Confounding [https://www.healthknowledge.org.uk/public-health-textbook/research-methods/1a-epidemiology/biases]
- 47. How causal perspectives can inform neuroscience data ... [https://arxiv.org/html/2503.10710v3]
- 48. Synthetic Control Methods for the Evaluation of Single-Unit ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634614/]
- 49. HOW TO GET CONTROL? CONCURRENT VS ... [https://www.berryconsultants.com/resource/how-to-get-control--concurrent-vs-contemporary-vs-historical-vs-synthetic-controls]
- 50. The 6 Data Quality Dimensions with Examples [https://www.collibra.com/blog/the-6-dimensions-of-data-quality]
- 51. Clinical Trial Design - Neuroscience Trials of the Future - NCBI [https://www.ncbi.nlm.nih.gov/books/NBK396104/]
- 52. Insights into the adoption of innovative clinical trials across ... [https://www.nature.com/articles/s41598-025-18488-8]
- 53. Rethinking the pros and cons of randomized controlled trials ... [https://bmcproc.biomedcentral.com/articles/10.1186/s12919-023-00285-8]
- 54. FAIR Principles [https://www.go-fair.org/fair-principles/]
- 55. Approaches to protocol standardization and data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11245389/]
- 56. Understanding Synthetic Control Methods [https://towardsdatascience.com/understanding-synthetic-control-methods-dd9a291885a1/]
- 57. Causal inference using synthetic controls [https://medium.com/data-science-at-microsoft/causal-inference-using-synthetic-controls-d96a890c83a7]
- 58. The Pivotal Role of AI in Clinical Trials: From Digital Twins ... [https://www.biopharmatrend.com/artificial-intelligence/the-pivotal-role-of-ai-in-clinical-trials-from-digital-twins-to-synthetic-control-arms-176/]
- 59. Recommendations for harmonization of data collection and ... [https://www.sciencedirect.com/science/article/abs/pii/S0892036217301022]
- 60. Transforming Clinical Trials with Real-World Evidence [https://www.bcg.com/publications/2021/synthetic-control-arms-changing-clinical-trials]
- 61. AI in Clinical Trials: Synthetic Control Arms & Faster Enrollment [https://www.promptwire.co/articles/ai-in-clinical-trials-synthetic-control-arms-faster-enrollment]
- 62. Synthetic Control Arm® in Clinical Trials | Medidata AI [https://www.medidata.com/en/clinical-trial-products/medidata-ai/real-world-data/synthetic-control-arm/]
- 63. Opportunities and risks associated with external ... [https://www.nature.com/articles/s41408-025-01426-2]
- 64. FDA Issues Complete Response Letter for Biohaven's ... [https://ir.biohaven.com/news-releases/news-release-details/fda-issues-complete-response-letter-biohavens-vyglxia]
- 65. Synthetic data as external control arms in scarce single-arm ... [https://journals.plos.org/digitalhealth/article?id=10.1371/journal.pdig.0000581]
- 66. Rethinking clinical trials with synthetic data [https://www.aindo.com/blog/synthetic-clinical-trials/]
- 67. POC Diagnostic Validation Framework - dicentra [https://dicentra.com/blog/medical-device/integrated-framework-for-point-of-care-diagnostic-validation]
- 68. Factors Affecting Success of New Drug Clinical Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10173933/]
- 69. Why Early-Stage Regulatory Planning is Essential for ... [https://synergbiopharma.com/early-stage-regulatory-planning-is-essential-for-success/]