Precision Neuromodulation: Optimizing TMS Protocols with Neuroimaging and AI for Clinical Translation
This article synthesizes the latest advancements in transcranial magnetic stimulation (TMS) protocol optimization, a critical endeavor for enhancing the efficacy and reliability of this non-invasive neuromodulation therapy.
Precision Neuromodulation: Optimizing TMS Protocols with Neuroimaging and AI for Clinical Translation
Abstract
This article synthesizes the latest advancements in transcranial magnetic stimulation (TMS) protocol optimization, a critical endeavor for enhancing the efficacy and reliability of this non-invasive neuromodulation therapy. Aimed at researchers, scientists, and drug development professionals, we explore the foundational neurobiology of TMS, the critical shift from standardized to personalized targeting methodologies, and the integration of multimodal neuroimaging and artificial intelligence (AI) for precision engagement. The content further addresses current methodological challenges and troubleshooting strategies, evaluates validation through electrophysiological and clinical outcomes, and discusses the future trajectory of TMS towards closed-loop, biomarker-driven systems for neuropsychiatric and neurological disorders.
The Neurobiological Basis of TMS: From Circuit Dysfunction to Targeted Intervention
Core Pathophysiology of Reward and Control Circuits in Neuropsychiatric Disorders
Pathophysiology of Reward and Control Circuits
Dysfunction in the brain's reward and cognitive control circuits is a transdiagnostic feature observed across numerous neuropsychiatric disorders. The core pathophysiology involves disrupted communication between key nodes within the limbic cortico-striatal-thalamic circuit [1].
Key Neural Circuitry and Disruption
Table 1: Core Components of the Reward and Control Circuitry
| Brain Region | Primary Function in Reward/Control | Manifestation of Dysfunction |
|---|---|---|
| Ventral Striatum (VS) / Nucleus Accumbens (NAc) | Incentive salience ("wanting"), reward prediction error coding, goal-directed behavior [2] [1]. | Blunted response to reward anticipation; impaired reward learning; anhedonia [3] [1]. |
| Ventral Tegmental Area (VTA) | Source of dopaminergic projections to VS, PFC, and amygdala; critical for reward signaling [1]. | Dysregulated dopamine release, affecting downstream targets and reward perception [1]. |
| Ventromedial Prefrontal Cortex (vmPFC) / Orbitofrontal Cortex (OFC) | Value representation, outcome evaluation, and decision-making [2]. | Impaired value computation and flexible decision-making [2]. |
| Dorsolateral Prefrontal Cortex (DLPFC) | Cognitive control, goal maintenance, and effort allocation [3]. | Reduced activation during cognitive control tasks; inflexible control allocation [3]. |
The interplay between these regions is critical for adaptive behavior. The mesolimbic dopamine pathway, originating in the VTA and projecting to the VS, is central for reward motivation and learning [1]. This pathway is gated and modulated by prefrontal regions, including the DLPFC and vmPFC/OFC [3] [2]. In Major Depressive Disorder (MDD), for example, adolescents show diminished activation in the left DLPFC and bilateral VLPFC during cues requiring high cognitive control, alongside weaker functional connectivity between these regions when rewards are involved [3]. This suggests a core deficit in integrating motivational and control signals.
Theoretical Frameworks for Circuit Dysfunction
The Expected Value of Control (EVC) theory provides a computational framework for understanding these deficits. It posits that cognitive control is allocated based on a cost-benefit analysis, where the brain weighs anticipated rewards against the effort cost of exerting control [3]. In depression, reduced sensitivity to anticipated rewards and an overestimation of effort costs lead to a diminished EVC, resulting in suboptimal allocation of cognitive control and impaired task performance [3]. This is supported by Hierarchical Drift Diffusion Modeling (HDDM) findings showing that depressed adolescents have a reduced starting bias toward rewarding responses and broader decision thresholds in reward contexts [3].
Application to Transcranial Magnetic Stimulation Protocol Optimization
The pathophysiological insights guide target selection and parameter refinement for Transcranial Magnetic Stimulation (TMS) protocols. While the search results primarily detail Transcranial Direct Current Stimulation (tDCS), the principles of targeting and parameter optimization are analogous and highly informative for TMS research.
Rationale for Target Engagement
TMS protocols can be optimized to modulate specific nodes of the dysregulated reward and control network:
- Stimulating Control Hubs: The DLPFC is a primary TMS target for disorders like MDD. The rationale is that facilitating DLPFC activity can enhance top-down cognitive control over negative emotional processing and improve the allocation of effort towards rewarded behaviors, thereby increasing the perceived EVC [3].
- Modulating Reward Valuation: While deeper structures like the VS are not directly accessible with standard TMS, the vmPFC/OFC can be targeted with specific coil geometries or through connectivity-guided protocols. Modulating this region may help normalize value representation and decision-making processes that are deficient in addiction and depression [2].
Table 2: Key TMS Protocol Parameters and Optimization Considerations
| Parameter | Considerations for Protocol Optimization | Evidence from Neuromodulation Research |
|---|---|---|
| Target | DLPFC (dorsolateral prefrontal cortex) is the most common target. Connectivity-based neuronavigation to specific network nodes (e.g., fronto-striatal circuit) may enhance efficacy [3]. | tDCS studies show that electrode montage (placement) substantially influences outcomes, underscoring the importance of precise targeting [4]. |
| Stimulus Intensity | Typically defined as a percentage of the individual's resting motor threshold (RMT). | In tDCS, intensity effects are non-linear; increasing intensity does not always enhance efficacy and can sometimes reverse effects [4]. This suggests careful titration of TMS intensity is crucial. |
| Pulse Pattern | Standard high-frequency (e.g., 10 Hz) vs. patterned protocols (e.g., Theta Burst Stimulation). | Patterned protocols may induce more robust neuroplastic changes. tDCS research shows "online" stimulation (during task performance) can be more effective than "offline" due to "activity-selectivity" [4]. |
| Number of Sessions | Multi-session protocols are standard for clinical effects. | Systematic reviews of tDCS suggest that interventions with ten or more sessions show more consistent cognitive improvements [5]. |
| Timing | The relationship between stimulation and task performance. | Evidence for "online" tDCS being more effective suggests that applying TMS during the performance of a reward or cognitive control task may optimize target engagement [4]. |
Experimental Protocols for Investigating TMS Effects
The following protocols are adapted from methodologies used to study circuit function and neuromodulation.
Protocol 1: Probing Reward-Modulated Cognitive Control with fMRI-navigated TMS
This protocol investigates how TMS over the DLPFC influences behavioral and neural correlates of reward-based decision-making.
- Participants: Recruit patient cohorts (e.g., MDD) and matched healthy controls.
- Task: AX-CPT (Continuous Performance Test) under reward and non-reward conditions [3].
- Cues: Letters "A" or "B" appear as cues.
- Probes: Letters "X" or "Y" appear as probes.
- Condition: The target trial is an "A" cue followed by an "X" probe (AX trial), requiring a specific response. Other combinations (AY, BX, BY) are non-targets.
- Reward Manipulation: In reward blocks, correct and fast responses on a subset of trials (e.g., AX trials) receive monetary or social reward feedback. No rewards are given in neutral blocks.
- Measures:
- Behavioral: Response time (RT) and error rates for AY and BX trials, which require proactive and reactive control [3].
- Computational: Hierarchical Drift Diffusion Modeling (HDDM) to decompose decisions into drift rate, decision threshold, and starting bias [3].
- Neural: Pre- and post-TMS fMRI to assess changes in activation within the reward network (VS, vmPFC) and connectivity between DLPFC and VS.
- TMS Protocol:
- Neuronavigation: Use individual fMRI data to identify the DLPFC target based on functional connectivity with the VS.
- Stimulation: Apply 10 Hz TMS (or intermittent Theta Burst Stimulation) to the left DLPFC. A control group receives sham TMS.
- Timing: "Online" stimulation is applied during the performance of the AX-CPT task.
- Dosage: A multi-session protocol (e.g., 10-15 sessions) is recommended for investigating therapeutic potential [5].
Protocol 2: Optimizing Target Engagement via Behavioral Synchronization
This protocol tests the principle of "activity-selectivity"—that stimulation is most effective when the target network is actively engaged [4].
- Task: A probabilistic reward learning task where participants learn to choose stimuli associated with different reward probabilities.
- Design: A within-subject, crossover design.
- Stimulation Timing:
- Condition A (Online TMS): TMS pulses are applied concurrently with the presentation of the reward-predicting cue or during the reward outcome phase.
- Condition B (Offline TMS): TMS is applied as a priming session before the task begins.
- Outcomes: The primary outcome is the learning rate, measured by the increase in choices for the high-probability reward stimulus. Secondary outcomes include model-based parameters from reinforcement learning models and VS activation measured with concurrent TMS-fMRI.
Signaling Pathways and Experimental Workflows
Simplified Reward Circuit Diagram
Experimental Protocol Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for Research on Reward Circuits and Neuromodulation
| Item / Reagent | Function / Application in Research |
|---|---|
| AX-CPT Task | A well-established behavioral paradigm to dissociate proactive and reactive cognitive control and test its modulation by reward contingencies [3]. |
| Hierarchical Drift Diffusion Model (HDDM) | A computational modeling tool to decompose behavioral task performance (e.g., AX-CPT) into distinct cognitive processes such as evidence accumulation rate (drift rate) and response caution (decision threshold), providing deeper insight into the mechanisms of impairment [3]. |
| fNIRS / fMRI | Functional neuroimaging techniques (functional Near-Infrared Spectroscopy and functional Magnetic Resonance Imaging) to measure hemodynamic responses and map neural activity within the reward and control circuits during task performance [3]. |
| Probabilistic Reward Learning Task | A family of tasks (e.g., two-armed bandit) used to assess reward learning and valuation. Critical for probing the function of the VS and vmPFC/OFC and their modulation by TMS [2]. |
| Neuromodulation Platform (TMS/tDCS) | Devices for non-invasive brain stimulation. TMS uses magnetic pulses to induce neuronal depolarization, while tDCS uses weak electrical currents to modulate cortical excitability. Both are used to test causal relationships between brain circuits and behavior [4] [5]. |
| Computational Models (Reinforcement Learning, EVC) | Mathematical models that formalize theories of how the brain learns from rewards (Reinforcement Learning) or allocates control (Expected Value of Control). These models generate quantitative predictions and fit behavioral/neural data [3]. |
| Hdac-IN-31 | Hdac-IN-31, MF:C25H24N4O2, MW:412.5 g/mol |
| Pefloxacin-d3 | Pefloxacin-d3, MF:C17H20FN3O3, MW:336.38 g/mol |
Understanding the dopaminergic, serotonergic, and glutamatergic pathways is fundamental to advancing neuromodulation therapies, particularly transcranial magnetic stimulation (TMS). These neurotransmitter systems regulate core brain functions—motor control, motivation, emotional affect, and cognition—and are frequently dysregulated in neurological and psychiatric disorders [6]. The efficacy of TMS is critically dependent on its ability to target and modulate these specific neurochemical pathways [7] [8]. This document provides a structured overview of these key systems, quantitative receptor data, and detailed experimental protocols to support research aimed at optimizing TMS parameters for precise engagement of these neurotransmitter pathways.
The following table summarizes the core functions, primary brain pathways, and associated disorders for the three key neurotransmitter systems.
Table 1: Core Characteristics of Key Neurotransmitter Systems
| System | Primary Functions | Key Brain Pathways | Associated Disorders |
|---|---|---|---|
| Dopaminergic | Motor control, reward, motivation, cognition [9] | Nigrostriatal, Mesolimbic, Mesocortical [10] | Parkinson's disease, Depression, ADHD, Addiction [7] [11] [10] |
| Serotonergic | Mood regulation, sleep, appetite, pain perception [9] | Projections from Dorsal Raphe Nucleus to Cortex, Amygdala, Hippocampus [9] | Depression, Anxiety, Chronic Pain [7] [9] |
| Glutamatergic | Major excitatory neurotransmission, synaptic plasticity, learning & memory [12] | Corticostriatal, Thalamocortical, Hippocampal circuits [7] | Depression, Chronic Pain, Neurodegenerative disorders [7] [9] [12] |
Data from positron emission tomography (PET) studies in healthy individuals provide a normative atlas of receptor density across the human cortex, which is crucial for informing TMS target engagement [6]. The values below represent relative, z-scored density across the cortex for various receptors and transporters.
Table 2: Relative Cortical Receptor and Transporter Density (z-scored) from PET Imaging [6]
| Receptor / Transporter | Mean Density (z-score) | Standard Deviation | Primary Neurotransmitter System |
|---|---|---|---|
| D1 receptor | 0.01 | 1.01 | Dopaminergic |
| D2 receptor | 0.02 | 0.99 | Dopaminergic |
| DAT | -0.03 | 0.98 | Dopaminergic |
| 5-HTâ‚A receptor | -0.01 | 1.02 | Serotonergic |
| 5-HTâ‚B receptor | 0.04 | 0.97 | Serotonergic |
| 5-HTâ‚‚A receptor | 0.05 | 1.03 | Serotonergic |
| SERT | -0.05 | 1.01 | Serotonergic |
| mGluR5 | 0.03 | 0.99 | Glutamatergic |
| NET | 0.00 | 1.00 | Norepinephrine (for comparison) |
Experimental Protocols for TMS Modulation Studies
Protocol 1: Investigating TMS-Induced Dopaminergic Changes in Rodent Models
Application: This protocol is designed to study the effects of high-frequency rTMS on the nigrostriatal and mesolimbic dopaminergic pathways in a rodent model of depression [10].
Workflow Diagram:
Detailed Methodology:
- Animal Model Preparation: Use adult male or female Sprague-Dawley rats. Induce a depression-like phenotype using the Chronic Unpredictable Mild Stress (CUMS) paradigm for 4-6 weeks. This involves exposing animals to varying, mild stressors daily (e.g., cage tilt, damp bedding, period of food/water deprivation) [10].
- Behavioral Baseline Assessment: Prior to TMS, assess depression-like behaviors using a test battery:
- Sucrose Preference Test (SPT): Measures anhedonia.
- Forced Swim Test (FST): Measures behavioral despair.
- Open Field Test (OFT): Assesses general locomotor activity and anxiety.
- Elevated Plus Maze (EPM): Further assesses anxiety-like behavior [10].
- rTMS Stimulation Protocol:
- Apparatus: A rodent-specific TMS coil with a compatible stimulator.
- Parameters: Apply 10 Hz rTMS. A typical protocol involves daily sessions for 15 days, with each session consisting of multiple trains (e.g., 50-100 trains), each train lasting 4-10 seconds with an inter-train interval of 26-60 seconds [10].
- Targeting: The coil is positioned over the skull to target the prefrontal cortex. A sham stimulation group (coil placed at an angle or using a sham coil) must be included for control.
- Post-Stimulation Assessment: Re-run the behavioral test battery (SPT, FST, OFT, EPM) 24 hours after the final TMS session.
- Tissue Preparation and Analysis:
- Brain Extraction: Euthanize animals and perfuse transcardially with phosphate-buffered saline (PBS) followed by 4% paraformaldehyde (PFA). Extract and post-fix brains.
- Immunofluorescence: Section brain regions of interest (e.g., dorsal striatum, prefrontal cortex). Incubate sections with primary antibodies against Tyrosine Hydroxylase (TH) and Dopamine D2 Receptors (D2R), followed by appropriate fluorescently-conjugated secondary antibodies [10].
- Imaging & Quantification: Use a confocal or fluorescence microscope to acquire images. Quantify fluorescence intensity or the number of labeled cells in defined regions using image analysis software (e.g., ImageJ).
Protocol 2: Human TMS Target Engagement with Neuroimaging
Application: This protocol outlines a method for personalized TMS target engagement of the dorsolateral prefrontal cortex (DLPFC) based on individual functional neuroimaging and structural connectivity, primarily aiming to modulate the serotonergic and glutamatergic systems implicated in depression [8] [13].
Workflow Diagram:
Detailed Methodology:
- Participant Screening and MRI Acquisition: Recruit eligible patients (e.g., with Major Depressive Disorder). Acquire high-resolution T1-weighted structural MRI, resting-state functional MRI (fMRI), and diffusion-weighted imaging (DWI) data [8] [13].
- Target Identification:
- Functional Targeting: Process resting-state fMRI data to identify the specific area within the left DLPFC that is most anti-correlated with the subgenual anterior cingulate cortex (sgACC), a key node in depressive pathology [13].
- Structural Connectivity: Process DWI data using tractography to map the structural connectivity of the target region, particularly focusing on pathways like the cingulum bundle [8].
- Neuronavigation Setup: Import the structural MRI and the identified target coordinates into a frameless stereotactic neuronavigation system. Co-register the patient's head to their MRI scan prior to the first TMS session.
- TMS Stimulation Protocol:
- Apparatus: A navigated TMS system with a figure-of-eight coil.
- Protocol Selection: Apply intermittent Theta Burst Stimulation (iTBS) or 10 Hz rTMS.
- iTBS Parameters: 3-pulse 50 Hz bursts repeated at 5 Hz (theta frequency). A common protocol is 2-second trains repeated every 10 seconds for a total of 600 pulses per session [7] [14].
- Targeting: Use the neuronavigation system to ensure precise and consistent coil placement over the personalized DLPFC target throughout the treatment course. The coil angle is often adjusted to induce a posterior-anterior current flow in the cortex [8].
- Outcome Monitoring: Assess clinical symptoms using standardized scales like the 17-item Hamilton Depression Rating Scale (HDRS-17) or Beck Depression Inventory (BDI-II) at baseline, weekly during treatment, and at follow-ups [14].
- Neurophysiological Verification (Optional): Use concurrent TMS with electroencephalography (TMS-EEG) to record and analyze TMS-evoked potentials (TEPs), providing a direct measure of cortical reactivity and target engagement at the neurophysiological level [8].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Reagents and Materials for Neurotransmitter & TMS Research
| Item | Function / Application | Example / Note |
|---|---|---|
| Selective Antibodies | Immunohistochemical labeling of specific proteins in tissue. | Anti-Tyrosine Hydroxylase (TH) for dopaminergic neurons; Anti-Dopamine D2 Receptor (D2R); Anti-5-HTâ‚A/5-HTâ‚‚A receptors [10]. |
| Radiolabeled PET Tracers | In vivo quantification of receptor/transporter density in humans. | [¹¹C]SCH23390 (D1 receptor); [¹¹C]raclopride (D2 receptor); [¹¹C]DASB (SERT); [¹¹C]ABP688 (mGluR5) [6]. |
| TMS-Compatible Neuromavigator | Precises positioning of TMS coil over individualized brain target. | Systems that integrate real-time MRI and/or fMRI data with optical tracking of the patient's head and TMS coil [8] [13]. |
| High-Density TMS-EEG System | Direct measurement of TMS-induced cortical potentials and oscillations. | A 64+ channel EEG system with hardware and software designed to suppress TMS-induced artifacts, allowing clean recording of TMS-evoked potentials [8]. |
| d-cycloserine & Lisdexamfetamine | Pharmacological augmentation of TMS to enhance neuroplasticity. | Used in accelerated protocols (e.g., ONE-D) to potentially potentiate NMDA receptor-dependent plasticity and enhance catecholamine release [14]. |
| Asperglaucin B | Asperglaucin B, MF:C19H26O3, MW:302.4 g/mol | Chemical Reagent |
| Galectin-3-IN-2 | Galectin-3-IN-2, MF:C24H30FN3O10S, MW:571.6 g/mol | Chemical Reagent |
Signaling Pathway Integration in TMS
The therapeutic effects of TMS are mediated through the modulation of complex, interconnected signaling pathways. The following diagram synthesizes the key neurochemical interactions influenced by TMS, particularly in the context of depression and chronic pain comorbidity [7] [9].
Pathway Diagram:
As illustrated, TMS acts on a network level. For example, high-frequency stimulation of the dorsolateral prefrontal cortex can lead to dopamine release in the striatum [7], modulate serotonin from the dorsal raphe nucleus [9], and induce long-term potentiation (LTP)-like plasticity through glutamatergic NMDA receptor activation [7]. This simultaneous modulation of multiple neurotransmitter systems underpins the broad therapeutic potential of TMS for complex neuropsychiatric disorders.
Transcranial magnetic stimulation (TMS) has emerged as a powerful non-invasive tool for modulating brain networks and inducing neuroplastic changes. By generating focused magnetic fields that induce electrical currents in targeted cortical regions, TMS can transiently or lastingly alter neural excitability and connectivity. The therapeutic potential of TMS is increasingly being realized across various neurological and psychiatric disorders, particularly through repetitive TMS (rTMS) protocols that can produce neuroplastic effects outlasting the stimulation period. This review synthesizes current theoretical frameworks explaining how TMS induces neuroplasticity and modulates brain networks, with particular emphasis on protocol optimization for research and clinical applications. Understanding these mechanisms is crucial for developing targeted, effective neuromodulation therapies, especially for conditions characterized by network dysconnectivity, where functional integration between brain regions is profoundly disturbed [15].
Theoretical Foundations of TMS-Induced Neuroplasticity
Basic Mechanisms of TMS Action
TMS operates on the principle of electromagnetic induction, where a brief, high-intensity current passed through a coil placed on the scalp generates a time-varying magnetic field perpendicular to the coil. This magnetic field, typically reaching 1-3 cm into the cortex, induces a secondary electrical current in the underlying brain tissue that can depolarize neurons and generate action potentials. The neurophysiological effects of TMS depend critically on stimulation parameters, particularly frequency. Low-frequency rTMS (≤1 Hz) generally suppresses cortical excitability, while high-frequency rTMS (≥5 Hz) tends to facilitate it. The pattern of stimulation also significantly influences outcomes, as evidenced by theta-burst stimulation (TBS), which delivers high-frequency pulses in short bursts to mimic natural theta rhythms and can produce rapid, powerful, and lasting plasticity [16] [17].
The after-effects of rTMS are believed to be mediated by neuroplastic mechanisms similar to long-term potentiation (LTP) and long-term depression (LTD). These involve complex molecular cascades including NMDA receptor activation, calcium influx, and subsequent changes in gene expression and protein synthesis that ultimately modify synaptic strength. Research using NMDA receptor blockers has provided causal evidence for the role of these receptors in rTMS after-effects, demonstrating that the plasticity-inducing effects can be pharmacologically disrupted [18] [19].
Network-Level Effects of TMS
While early TMS research focused predominantly on local effects at the stimulation site, contemporary frameworks emphasize that TMS modulates distributed brain networks. The effects of TMS are not confined to the targeted region but propagate to anatomically and functionally connected remote areas through established neural pathways. This network modulation is particularly relevant for therapeutic applications, as many neurological and psychiatric disorders involve distributed network disturbances rather than isolated regional dysfunction [15] [20].
Concurrent TMS-fMRI studies have robustly demonstrated that stimulating one node of a network can modulate activity throughout the entire network. For instance, TMS over the dorsolateral prefrontal cortex (DLPFC) - a common target for depression treatment - acutely modulates connectivity within critical brain circuits including the cognitive control network and default mode network. These network-level changes correlate with clinical improvement, suggesting they represent a key mechanism of therapeutic action [21]. The state of the targeted network at the time of stimulation significantly influences TMS effects, supporting the concept of "state-dependency" where current brain activity patterns shape response to neuromodulation [20].
Key Neuroplasticity Mechanisms
Synaptic Plasticity and Homeostatic Metaplasticity
The after-effects of rTMS are primarily mediated through activity-dependent synaptic plasticity. The induced electrical fields can alter the timing of pre- and postsynaptic spikes, potentially engaging spike-timing-dependent plasticity (STDP) mechanisms that strengthen or weaken synaptic connections based on temporal correlations. Repeated TMS sessions are thought to cumulatively modify synaptic weights in targeted circuits, leading to lasting reorganization of functional networks [18].
Homeostatic metaplasticity mechanisms ensure that neural activity operates within dynamic physiological ranges. The brain's response to TMS is influenced by its recent history of activity, with prior neural activity levels potentially shifting the threshold for subsequent plasticity induction. This homeostatic regulation may explain some of the variability in TMS responses across individuals and sessions, and highlights the importance of considering stimulation history in protocol design [18].
Oscillatory Entrainment and Phase-Dependent Effects
TMS can entrain neural oscillations by synchronizing the firing patterns of neuronal populations. This is particularly evident with patterned protocols like TBS, but also occurs with conventional rTMS. The phase of ongoing oscillations represents a brain state that influences neuronal excitability and responsiveness to stimulation. Emerging evidence suggests that synchronizing TMS pulses to specific phases of endogenous rhythms (e.g., alpha oscillations) can enhance efficacy and reduce interindividual variability in response [21] [19].
Combined TMS-EEG studies have demonstrated that the phase of oscillatory activity at the time of stimulation significantly influences TMS effects. For instance, delivering TMS pulses at the peak phase of beta oscillations in the motor cortex produces facilitatory after-effects, while stimulation at the trough phase may be inhibitory. This phase-dependency offers promising avenues for optimizing stimulation timing to maximize target engagement [19].
Neurotransmitter Systems
TMS-induced plasticity involves multiple neurotransmitter systems, including glutamate (for excitatory transmission), GABA (for inhibitory transmission), and monoamines (for neuromodulation). Different TMS protocols appear to engage distinct neurotransmitter systems - for example, short-interval intracortical inhibition (SICI) is thought to reflect GABAA receptor-mediated inhibition, while intracortical facilitation (ICF) involves glutamatergic NMDA receptors. Short-latency afferent inhibition (SAI) provides a marker of cholinergic function, and has been shown to be modulated by specific TMS protocols [19].
The differential engagement of neurotransmitter systems by various TMS parameters provides a neurochemical basis for protocol optimization. Understanding these neurochemical effects is particularly important for developing TMS as a therapeutic tool, as different neuropsychiatric conditions involve distinct neurotransmitter imbalances.
Table 1: Neuroplasticity Mechanisms in TMS
| Mechanism | Key Processes | Relevant TMS Protocols | Experimental Evidence |
|---|---|---|---|
| Synaptic Plasticity | LTP/LTD-like effects; NMDA receptor activation; calcium-dependent signaling | rPPS; iTBS; cTBS | NMDA receptor blockade abolishes facilitatory after-effects [19] |
| Oscillatory Entrainment | Phase-dependent effects; neural synchronization; cross-frequency coupling | EEG-synchronized TMS; tACS-TMS combinations | Enhanced efficacy with phase-locked stimulation [21] |
| Neurotransmitter Modulation | GABAergic inhibition; glutamatergic excitation; cholinergic modulation | LF-rTMS (GABA); HF-rTMS (glutamate); SAI protocols (ACh) | SICI (GABAA) and LICI (GABAB) changes post-TMS [19] |
| Network Reorganization | Functional connectivity changes; network topology shifts; pathway strengthening | DLPFC stimulation for depression; M1 stimulation for motor disorders | fMRI demonstrated DMN, CCN modulation [21] [20] |
Measuring and Quantifying TMS Effects
Neurophysiological Measures
Motor evoked potentials (MEPs) recorded via electromyography represent the gold standard for quantifying TMS effects on corticospinal excitability. Beyond MEP amplitude, various paired-pulse TMS paradigms permit assessment of specific inhibitory and facilitatory circuits within the motor cortex. These include short-interval intracortical inhibition (SICI), intracortical facilitation (ICF), short-latency afferent inhibition (SAI), and long-interval intracortical inhibition (LICI), each probing distinct neuropharmacological mechanisms [15] [19].
TMS combined with electroencephalography (TMS-EEG) provides a direct measure of cortical reactivity and connectivity beyond the motor system. TMS-EEG can capture TMS-evoked potentials (TEPs) and oscillatory responses across the cortex, offering insights into local and network-level excitability and connectivity. This approach is particularly valuable for assessing TMS effects in non-motor regions targeted for therapeutic applications [15].
Functional Connectivity and Network Analysis
Resting-state functional connectivity analyses, derived from either fMRI or EEG, enable quantification of TMS-induced changes in network organization. Studies have demonstrated that rTMS can modify functional connectivity patterns in distributed networks, with these changes often correlating with clinical improvements. For example, in mal de debarquement syndrome, rTMS-induced symptom changes were correlated with connectivity changes in the alpha band over parietal and occipital cortices [15].
Independent component analysis (ICA) of fMRI data has revealed that TMS over the primary motor cortex modulates not only the targeted motor network but also non-motor networks including those involved in bodily self-consciousness, such as the insular and rolandic operculum systems. These widespread effects highlight the network-level actions of TMS and underscore that stimulation at any node influences distributed brain systems [20].
Table 2: Quantitative Measures of TMS-Induced Neuroplasticity
| Measure | Methodology | Neural Correlate | Application in Protocol Optimization |
|---|---|---|---|
| Motor Evoked Potentials (MEP) | EMG recording from target muscle | Corticospinal excitability | Determining stimulation intensity; measuring facilitatory/inhibitory effects |
| Paired-Pulse Paradigms (SICI, LICI, ICF, SAI) | Condition-test pulse sequences | Intracortical inhibition/facilitation; cholinergic function | Probing specific neurotransmitter systems; target engagement verification |
| TMS-Evoked Potentials (TEPs) | EEG response to TMS pulses | Cortical reactivity and connectivity | Assessing direct cortical responses in non-motor regions |
| Resting-State Functional Connectivity | fMRI or EEG correlation analysis | Network integration and segregation | Evaluating network-level treatment effects; identifying novel targets |
| Oscillatory Power and Synchronization | Spectral analysis of EEG | Local and network oscillations | State-dependent stimulation; entrainment effects |
| Behavioral Measures | Task performance | Cognitive/motor function | Linking neurophysiological effects to functional outcomes |
Experimental Protocols and Applications
Standard rTMS Protocols for Research
Depression Protocol (DLPFC Stimulation)
- Target: Left dorsolateral prefrontal cortex (DLPFC)
- Localization: EEG 10-20 system (F3) or neuronavigation based on individual anatomy
- Parameters: 10 Hz frequency, 120% resting motor threshold, 4-second train duration, 26-second intertrain interval, 3000 pulses per session
- Session Schedule: Daily sessions for 4-6 weeks
- Mechanistic Basis: Modulates cognitive control network and default mode network connectivity; normalizes prefrontal-limbic interactions [21]
Motor Cortex Plasticity Protocol
- Target: Primary motor cortex (M1) hand area
- Localization: Motor hotspot identified via single-pulse TMS
- Parameters:
- Facilitatory: 10 Hz at 80-90% RMT or iTBS (2-second trains, 8-second intervals)
- Inhibitory: 1 Hz at 100-110% RMT or cTBS (continuous theta burst)
- Outcome Measures: MEP amplitude, SICI, ICF, SAI
- Applications: Studying basic plasticity mechanisms; developing protocols for motor recovery [19]
State-Dependent and Personalized Protocols
Emerging approaches aim to optimize TMS efficacy by personalizing stimulation parameters based on individual brain anatomy, connectivity, and dynamic state:
EEG-Guided Phase-Locked TMS
- Principle: Deliver TMS pulses at specific phases of endogenous oscillations
- Implementation: Real-time EEG analysis with trigger generation for TMS
- Evidence: Enhanced and more consistent plasticity effects when stimulating at peak of sensorimotor beta oscillations [21] [19]
fMRI-Neuronavigated Targeting
- Principle: Target stimulation based on individual functional connectivity profiles
- Implementation: Identify stimulation targets based on rs-fMRI connectivity maps
- Evidence: Improved clinical outcomes in depression when targeting DLPFC regions with strongest negative connectivity to subgenual cingulate [21]
Combined TMS-tACS Protocols
- Principle: Modulate oscillatory activity with tACS while inducing plasticity with TMS
- Implementation: Simultaneous application of tACS and TMS with precise phase relationship
- Evidence: rPPS synchronized to peak phase of β-tACS enhanced and stabilized facilitatory after-effects in M1 [19]
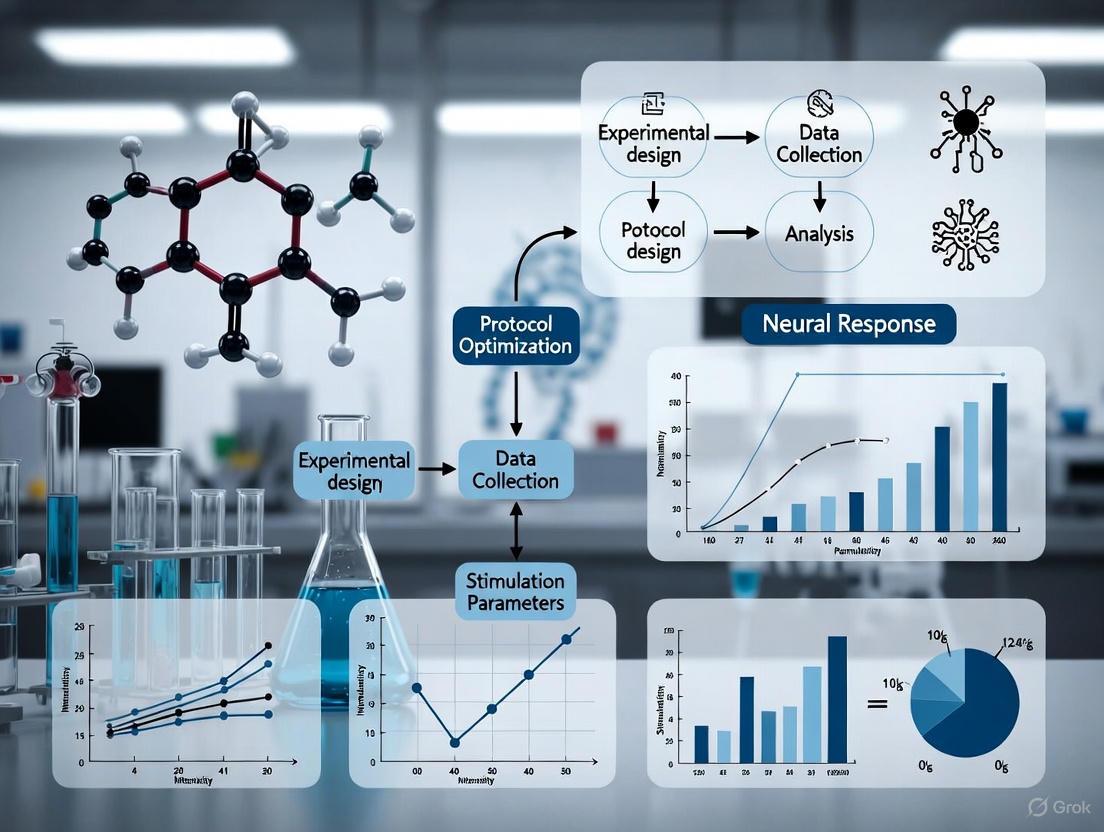
TMS Protocol Development Workflow: This diagram illustrates the iterative process for developing and optimizing TMS protocols, highlighting key decision points and individualization factors.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for TMS Neuroplasticity Studies
| Tool/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| TMS Devices | DuoMAG MP-Quad TMS; MagVenture; Brainsway | Delivering precise magnetic stimulation | Output characteristics; coil types; cooling systems |
| Neurophysiological Monitoring | EMG systems; EEG with TMS-compatible amplifiers; fMRI | Measuring TMS effects | Compatibility with TMS; artifact handling; temporal resolution |
| Neuronavigation | MRI-based systems (BrainSight; Localite); 3D camera systems | Precision targeting | Accuracy; registration methods; real-time tracking |
| Pharmacological Agents | NMDA receptor antagonists; GABAA agonists; cholinergic drugs | Probing plasticity mechanisms | Dosage; timing; safety with TMS |
| Behavioral Tasks | Cognitive batteries; motor learning paradigms; mood scales | Linking plasticity to function | Sensitivity to change; reliability; clinical relevance |
| Computational Tools | Electric field modeling; network analysis; signal processing | Predicting and analyzing effects | Realism of models; computational demands |
| TRPA1 Antagonist 1 | TRPA1 Antagonist 1 is a potent, selective channel blocker for pain and inflammation research. For Research Use Only. Not for human or veterinary diagnostic or therapeutic use. | Bench Chemicals | |
| Cletoquine-d4-1 | Cletoquine-d4-1, MF:C16H22ClN3O, MW:311.84 g/mol | Chemical Reagent | Bench Chemicals |
The theoretical frameworks explaining TMS-induced neuroplasticity have evolved from simplistic excitation/inhibition models toward sophisticated network-level perspectives that account for state-dependent, oscillatory, and neurotransmitter-mediated mechanisms. The future of TMS protocol optimization lies in personalized approaches that integrate individual structural and functional neuroimaging, real-time state assessment, and closed-loop systems that adapt stimulation parameters based on ongoing brain activity. As research continues to elucidate the complex relationships between TMS parameters and neuroplastic outcomes, we move closer to realizing the full potential of this powerful neuromodulation technique for both basic neuroscience and therapeutic applications.
Further validation of biomarker-driven approaches and refinement of state-dependent stimulation protocols will be essential for enhancing the precision and efficacy of TMS interventions. The integration of TMS with other neuromodulation techniques, such as tACS, represents a promising frontier for inducing more specific and powerful neuroplastic changes. As these approaches mature, they will undoubtedly expand the therapeutic reach of TMS across a broader range of neurological and psychiatric conditions characterized by network dysfunction.
Transcranial Magnetic Stimulation (TMS) has emerged as a promising therapeutic tool for various neurological and psychiatric disorders. The efficacy of TMS is critically dependent on the precise selection of stimulation targets, which requires a deep understanding of the functional roles and neurocircuitry of specific brain regions. This protocol optimization research focuses on four key cortical targets: the dorsolateral prefrontal cortex (DLPFC), pre-supplementary motor area (pre-SMA), insula, and subgenual anterior cingulate cortex (sgACC). These regions form critical nodes in networks governing cognitive control, emotional regulation, and decision-making processes. Understanding their distinct functions and interconnections enables more precise TMS targeting, potentially enhancing treatment outcomes for conditions including depression, addiction, and attention-deficit/hyperactivity disorder (ADHD). This article provides a comprehensive framework for researchers and clinicians, integrating current neuroanatomical, functional, and methodological insights to refine TMS protocols.
The following table summarizes the core functional roles and associated networks of the four target regions.
Table 1: Functional Profiles of Key TMS Targets
| Brain Region | Primary Functional Roles | Associated Networks/Pathways | Behavioral/Cognitive Correlates |
|---|---|---|---|
| Dorsolateral Prefrontal Cortex (DLPFC) | Executive control, working memory, adaptive coding of task-relevant information [22], conflict-induced behavioral adaptation [23]. | Multiple-Demand (MD) Network; top-down modulation of sensory and association cortices [22]. | Cognitive control, planning, behavioral flexibility. |
| Pre-Supplementary Motor Area (Pre-SMA) | Cognitive motor control, response selection, conflict monitoring [23]. | Cingulo-Opercular Network [24]. | Action planning, error detection, sequence learning. |
| Anterior Insula (aINS) | Interoceptive awareness, salience processing, risk assessment, integrating bodily states into subjective feeling [25] [26]. | Salience Network; functional connectivity with amygdala-striatal reward circuit (vAI) and prefrontal control system (dAI) [25]. | Risk-taking tendency [26], emotional experience, urge generation. |
| Subgenual Anterior Cingulate Cortex (sgACC) | Emotional processing, reward learning, autonomic regulation. | Default Mode and Affective Networks; target for antidepressant TMS via connectivity with DLPFC [24]. | Negative affect, mood regulation, visceral responses to emotion. |
Functional Connectivity and Circuit-Based Targeting
Effective TMS protocols are increasingly based on functional connectivity profiles. The distinct sub-regions of our targets interact with specific circuits to mediate behavior.
Insula Subdivisions and Their Networks
The insula is not a unitary structure. A tripartite subdivision reveals specialized functions and connectivity patterns crucial for somatic marker hypothesis and interoceptive processing [25]:
- Posterior Insula (PI): Primarily connected to the visceral-sensorimotor system, receiving and integrating interoceptive signals.
- Ventral Anterior Insula (vAI): Predominantly connected to the amygdala-striatal system, modulating reward-seeking and emotional processes.
- Dorsal Anterior Insula (dAI): Predominantly connected to prefrontal regions, modulating self-control and higher-order cognitive processes [25].
Quantitatively, cognitive performance is positively correlated with functional connectivity (FC) between the dAI and the ventrolateral PFC, and negatively correlated with FC between the vAI and reward-related regions like the orbitofrontal cortex and sgACC [25].
DLPFC in Top-Down Facilitation
Causal evidence from concurrent TMS-fMRI studies demonstrates that the DLPFC is necessary for enhancing the coding of task-relevant information across the frontoparietal network. Disruption of the right DLPFC with TMS specifically decreases the representation of attended stimulus features, with no statistically detectable effect on irrelevant information [22]. This supports a primary role for the DLPFC in facilitatory mechanisms rather than direct inhibition.
Cross-Dataset Validation for Target Identification
Robust target identification, particularly for disorders like ADHD, can be achieved by combining meta-analysis with cross-dataset validation of functional connectivity. This approach has identified consistent brain surface targets, including the DLPFC, right inferior frontal gyrus, and pre-SMA/SMA, by analyzing resting-state fMRI data from independent cohorts [27]. This method enhances the generalizability and reliability of identified TMS locations.
Experimental Protocols for Target Validation
Protocol 1: Functional Connectivity Mapping for Target Engagement
This protocol details how to identify a patient-specific DLPFC target based on its anti-correlation with the sgACC, a common clinical approach.
- Objective: To derive an individualized TMS target for Major Depressive Disorder (MDD) treatment by mapping the DLPFC region with strongest negative functional connectivity to the sgACC.
- Materials: MRI scanner, T1-weighted structural imaging protocol, resting-state fMRI (rs-fMRI) protocol, data processing software (e.g., SPM, FSL, or DPABI).
- Procedure:
- Data Acquisition: Acquire high-resolution T1-weighted structural images and a 10-minute rs-fMRI scan (eyes open, fixating on a cross) for each participant.
- Preprocessing: Process rs-fMRI data using a standard pipeline, including slice-timing correction, realignment, normalization to MNI space, and smoothing with a 6mm Gaussian kernel. Regress out nuisance signals (white matter, cerebrospinal fluid, motion parameters).
- Seed-Based FC Analysis:
- Define a spherical seed region of interest (ROI) for the sgACC (e.g., MNI coordinates: ±x, y, z).
- Extract the average BOLD time series from the sgACC seed.
- Calculate the Pearson's correlation coefficient between this seed time series and the time series of every other voxel in the brain.
- Convert correlation coefficients to z-scores using Fisher's transformation to create a subject-level FC map.
- Target Identification: Identify the voxel or cluster within the dorsolateral prefrontal cortex mask that shows the highest negative correlation (strongest anti-correlation) with the sgACC seed. This peak coordinate defines the patient-specific TMS target.
Protocol 2: Concurrent TMS-fMRI for Causal Mechanism Investigation
This protocol leverages multimodal integration to test the causal influence of a stimulated site on network function and information processing.
- Objective: To assess the causal effect of DLPFC stimulation on the coding of task-relevant information in distal brain regions using concurrent TMS-fMRI.
- Materials: MRI-compatible TMS system, head coil with integrated TMS unit, task-based fMRI paradigm, multivariate pattern analysis (MVPA) software.
- Procedure:
- Localization: Neurologically coregister the TMS coil position to the individual's structural MRI. Define the DLPFC target using the 10-20 EEG system (e.g., F3/F4) or an fMRI-guided neuronavigation system.
- Stimulation Paradigm: Employ a within-subjects design with Active (e.g., 110% motor threshold) and Control (e.g., 40% motor threshold) TMS intensities. During fMRI, deliver a short TMS train (e.g., 3 pulses at 13 Hz) on each trial of a cognitive task (e.g., a feature-selection task where participants attend to one stimulus dimension and ignore another) [22].
- Imaging & Analysis:
- Acquire whole-brain fMRI data during the task under both TMS conditions.
- Use Multivariate Pattern Analysis (MVPA) to quantify the strength of task-relevant and task-irrelevant information coding in regions of interest (e.g., frontoparietal network, visual cortices).
- Statistically compare the information coding strength between Active and Control TMS conditions across the brain.
Protocol 3: Behavioral Assay for Insula-Mediated Risk-Taking
This protocol details a behavioral task suitable for probing the function of the anterior insula, which can serve as a biomarker for target engagement.
- Objective: To quantify individual differences in risk-taking tendency relevant to insula function using the Analgesic Decision-making Task (ADT) [26].
- Materials: Paper-and-pencil or computerized version of the ADT, questionnaires for prior pain experience and imagined pain relief.
- Procedure:
- Task Administration: Present participants with 22 figurative scenarios across three sub-tasks: Analgesic Effect (ANE), Adverse Effect (ADE), and Time-course Effect (TE). In each scenario, participants choose between a "riskless" (conservative) and a "riskier" (more potent but less certain/slower/riskier) analgesic treatment.
- Behavioral Quantification: Calculate a Risk Preference Index (RPI) for each participant as the total frequency of choosing the riskier option across all scenarios (RPI = Nriskier / 22). Calculate sub-scores (RPIANE, RPI_ADE, RPITE) for each task domain.
- Correlation with Neural Measures: In a research context, the RPI can be correlated with structural (e.g., grey matter volume) and functional (e.g., degree centrality) signatures of the anterior insula to validate its behavioral relevance [26].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Reagents and Materials for TMS Protocol Research
| Item Name | Function/Application | Specific Examples/Notes |
|---|---|---|
| MRI-Compatible TMS System | Allows for precise, neuronavigated stimulation and concurrent causal investigation of network effects. | Systems from MagVenture, Magstim, or Neurosoft with specialized MR coils. Critical for Protocol 2. |
| Neuromavigation System | Precisely coregisters the TMS coil with the subject's neuroanatomy for accurate target engagement. | Brainsight, Localite, or Visor2 systems that use infrared tracking. |
| Functional Connectivity Toolboxes | Software for preprocessing and analyzing resting-state and task-based fMRI data. | CONN, DPABI, FSL, SPM12. Used for seed-based correlation analysis in Protocol 1. |
| Analgesic Decision-Making Task (ADT) | A behavioral probe for quantifying risk-taking tendency, linked to anterior insula function. | Paper-and-pencil or computerized version [26]. Used as a behavioral assay in Protocol 3. |
| Multivariate Pattern Analysis (MVPA) Toolbox | Decodes information content from distributed patterns of brain activity in fMRI data. | The Princeton MVPA Toolbox, PyMVPA, or custom scripts in Python/MATLAB. Essential for analyzing data in Protocol 2. |
| High-Definition TMS Cap | Improves the precision and focality of TMS stimulation without neuronavigation. | 4x1 ring configuration caps for HD-TMS from companies like Soterix Medical. |
| Pyrimethanil-13C,15N2 | Pyrimethanil-13C,15N2, MF:C12H13N3, MW:202.23 g/mol | Chemical Reagent |
| FTase Inhibitor III | FTase Inhibitor III – Farnesyltransferase Inhibitor | FTase Inhibitor III is a cell-permeable inhibitor that blocks Ras protein processing. For Research Use Only. Not for human use. |
Signaling Pathways and Logical Workflows
The following diagrams, generated with Graphviz DOT language, illustrate the key functional relationships and experimental workflows described in this article.
Functional Networks of Insula Subregions
DLPFC Causal Facilitation Mechanism
TMS Target Identification Workflow
Advanced TMS Methodologies: From Standardized Protocols to Personalized Targeting
Transcranial magnetic stimulation (TMS) has emerged as a cornerstone non-invasive neuromodulation technique in clinical neuroscience and psychiatry. Within its arsenal, several distinct protocols have been developed and refined, each with unique mechanisms and therapeutic applications. This analysis focuses on three predominant TMS modalities: conventional repetitive TMS (rTMS), the patterned protocol Theta Burst Stimulation (TBS), and Deep TMS. The optimization of these protocols is critical for enhancing treatment efficacy, efficiency, and accessibility across various neuropsychiatric conditions, particularly treatment-resistant depression (TRD). The evolution from standardized, one-size-fits-all rTMS protocols toward personalized, biomarker-guided approaches represents the forefront of TMS research and development [28] [29].
Comparative Efficacy and Safety Profiles
Quantitative data from recent meta-analyses and clinical trials provide a foundation for comparing the clinical outcomes of different TMS protocols. The tables below summarize key efficacy and safety parameters across multiple neurological and psychiatric indications.
Table 1: Comparative Efficacy of TMS Protocols in Treatment-Resistant Depression
| Protocol | Stimulation Parameters | Session Duration | Remission Rates | Key Comparative Findings |
|---|---|---|---|---|
| 10 Hz rTMS | 10 Hz, 3000 pulses/session | ~37.5 minutes [30] | 20-30% [29] | Similar efficacy to TBS; robust evidence base [31] |
| Standard iTBS | 50 Hz bursts, 600 pulses/session | ~3-10 minutes [31] [29] | 20-30% [29] | Non-inferior to 10 Hz rTMS for TRD [31] |
| Accelerated iTBS (SNT/PAiT) | 50 Hz bursts, 1800 pulses/session, 10 sessions/day for 5 days | ~10 minutes/session [29] | Up to ~79% [29] | High remission in studies; requires further validation [29] |
| Deep TMS | H-coil, 18-20 Hz | ~20 minutes | Not specified in results | Investigational for TRD [28] |
Table 2: Protocol Performance Across Other Neurological Conditions
| Condition | Most Effective Protocol | Key Outcome | Supporting Evidence |
|---|---|---|---|
| Post-Stroke Motor Recovery | ≥10 Hz rTMS (mild/severe, convalescent phase); iTBS (acute/subacute phase) [32] | Best for upper limb function & daily living [32] | Network Meta-Analysis of 95 RCTs [32] |
| Parkinson's Disease Depression | rTMS (DLPFC-targeted) | Improves depressive symptoms [7] | Mechanism: Prefrontal-striatal dopamine pathway modulation [7] |
| Late-Life Depression | Bilateral or High-Frequency rTMS [33] | Remission rates: 20-63% [33] | Scoping Review (16 studies) [33] |
| PD Anxiety | cTBS (DLPFC-targeted) | Potential anxiolytic effects [7] | Indirect amygdala/hippocampal regulation [7] |
Table 3: Safety and Tolerability Profile
| Adverse Event | rTMS vs. TBS (Odds Ratio) | Statistical Significance | Notes |
|---|---|---|---|
| Headache | OR = 1.00 [31] | Not significant (CI: 0.72-1.40) | Most common, typically transient and self-limiting [29] [33] |
| Nausea | OR = 1.42 [31] | Not significant (CI: 0.79-2.54) | |
| Fatigue | OR = 0.87 [31] | Not significant (CI: 0.46-1.64) | |
| Scalp Discomfort | Not quantitatively compared | Common to all protocols | Well-tolerated; rarely leads to discontinuation [29] [33] |
Detailed Experimental Protocols
Standard 10 Hz rTMS for TRD
- Objective: To alleviate depressive symptoms in patients with Major Depressive Disorder (MDD) or Treatment-Resistant Depression (TRD).
- Methodology:
- Rationale: High-frequency stimulation increases cortical excitability in the left DLPFC, a key node in the affective network [7] [17].
Accelerated iTBS (PAiT/SNT Protocol)
- Objective: To induce rapid remission in TRD through intensive, personalized stimulation.
- Methodology:
- Personalized Targeting: Target the left DLPFC subregion with strongest functional MRI (fMRI) anticorrelation to the subgenual Anterior Cingulate Cortex (sgACC) using resting-state fMRI [28] [29].
- Parameters: iTBS pattern, 1800 pulses per session, intensity at 90% of resting motor threshold [29].
- Accelerated Course: 10 sessions per day, with a 50-minute inter-session interval, over 5 days (50 sessions total) [29].
- Rationale: Functional connectivity-guided targeting may more effectively modulate dysfunctional mood circuits, while the accelerated, spaced schedule enhances synaptic strengthening via long-term potentiation-like mechanisms [7] [29].
Post-Stroke Motor Rehabilitation Protocol
- Objective: To improve upper limb motor function and activities of daily living (ADL) post-stroke.
- Methodology:
- Paradigm Selection: Choose protocol based on stroke phase [32]:
- Acute/Subacute Phase (<3 months): iTBS to affected motor cortex or 1 Hz rTMS to unaffected hemisphere.
- Convalescent Phase (>3 months): ≥10 Hz rTMS to affected motor cortex.
- Parameters: Follow established safety guidelines for frequency and pulse count [32].
- Course: Typically 10-20 sessions integrated with physical/occupational therapy.
- Paradigm Selection: Choose protocol based on stroke phase [32]:
- Rationale: Aims to rebalance interhemispheric competition by increasing excitability of the affected hemisphere or decreasing inhibition from the unaffected hemisphere [32].
Signaling Pathways and Neurophysiological Mechanisms
The therapeutic effects of TMS protocols are mediated through the induction of complex neuroplastic changes. The diagram below illustrates the primary signaling pathways and neural mechanisms involved.
Diagram 1: Neuroplasticity pathways activated by TMS.
Experimental Workflow for Protocol Comparison
A standardized methodology is essential for the direct comparison of TMS protocols in a research setting. The following workflow outlines a rigorous experimental design for evaluating efficacy in TRD.
Diagram 2: Workflow for comparative TMS trials.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key Materials and Equipment for TMS Research
| Item | Function/Application | Examples/Notes |
|---|---|---|
| TMS Device with TBS Capability | Core stimulation delivery | Must support conventional rTMS and TBS patterns (iTBS, cTBS) [31] [29]. |
| Neuronavigation System | Precision targeting via individual anatomy/connectivity | Integrates structural MRI (sMRI) or functional MRI (fMRI) for personalized coil placement [28] [29]. |
| MRI-Compatible EEG Cap | Concurrent TMS-EEG for mechanism investigation | Assesses immediate electrophysiological effects and cortical excitability [28]. |
| Structural MRI (sMRI) | Anatomical guidance & target identification | Used for targeting BA9/BA46 border [28]. |
| Resting-State fMRI | Functional connectivity mapping for target personalization | Identifies DLPFC subregion with optimal anticorrelation to sgACC [28] [29]. |
| Clinical Rating Scales | Primary outcome measurement for depression trials | HDRS, MADRS; essential for standardized efficacy assessment [28] [29]. |
| Motor Threshold Kit | Individualized stimulation intensity calibration | EMG system for measuring motor evoked potentials (MEPs) [33]. |
| Remdesivir-d4 | Remdesivir-d4, MF:C27H35N6O8P, MW:606.6 g/mol | Chemical Reagent |
| Top1 inhibitor 1 | Top1 inhibitor 1, MF:C24H22N6O2, MW:426.5 g/mol | Chemical Reagent |
The comparative analysis of rTMS, TBS, and Deep TMS reveals a nuanced landscape where no single protocol is universally superior. While standard 10 Hz rTMS and iTBS demonstrate comparable efficacy for TRD, their selection hinges on clinical context, with iTBS offering significant time efficiency [31]. The emergence of accelerated, connectivity-guided iTBS protocols promises enhanced remission rates, though these findings require validation in larger, independent trials [29]. Future research must prioritize the optimization of stimulation parameters, the development of reproducible personalized targeting methods, and the clarification of long-term outcomes and cost-effectiveness to solidify the role of each protocol in the next generation of neuromodulation therapies.
A Generalized Workflow for fMRI-Guided, Electric-Field-Optimized TMS Targeting
Transcranial Magnetic Stimulation (TMS) represents a cornerstone of non-invasive neuromodulation, yet its clinical efficacy has been limited by historical standardization in targeting approaches. The conventional reliance on scalp-based measurement systems, such as the Beam F3 method, fails to account for profound inter-individual variability in brain anatomy and functional network organization [34] [35]. This "one target for all" paradigm results in poorly defined TMS-induced electric field (E-field) intensity and uncertain engagement of the intended neurocircuitry, particularly for cortical targets beyond the primary motor cortex [8]. Consequently, the optimization of TMS protocols now demands a precision medicine framework that integrates individual functional neuroanatomy with computational modeling of induced electric fields.
The convergence of functional magnetic resonance imaging (fMRI) and electric field (E-field) modeling technologies has enabled a new generation of personalized TMS targeting. fMRI provides a non-invasive window into the intrinsic functional architecture of an individual's brain, allowing for the identification of patient-specific network nodes implicated in disease pathophysiology [34] [36]. When combined with computational approaches that simulate the TMS-induced E-field distribution, clinicians and researchers can now optimize coil placement and orientation to maximize the electric field strength in the target region while minimizing off-target stimulation [37]. This integrated methodology is particularly crucial for engaging deeply embedded structures, such as the subgenual cingulate cortex (SGC), through their functional connections with superficial cortical areas like the dorsolateral prefrontal cortex (DLPFC) [38] [39].
This protocol outlines a generalized workflow for integrating resting-state fMRI with electric field modeling to optimize TMS targeting, a approach with demonstrated efficacy in neuropsychiatric disorders. Naturalistic clinical data reveals that fMRI-guided targeting significantly improves outcomes in treatment-resistant depression, with response rates increasing from 62.2% with standard targeting to 77.5% with fMRI guidance (Number Needed to Treat = 6.5) [35]. Furthermore, studies quantifying E-field distributions confirm that functional targeting combined with coil orientation optimization produces significantly higher field intensity in the target region compared to anatomical approaches [37]. The following sections provide a comprehensive technical framework for implementing this precision targeting approach in both research and clinical settings.
The generalized workflow for fMRI-guided, E-field-optimized TMS comprises five integrated stages: (1) Neuroimaging Acquisition, (2) Target Identification, (3) Electric Field Modeling, (4) Neuronavigation, and (5) Treatment Delivery. This systematic approach transforms raw imaging data into a personalized stimulation protocol that maximizes target engagement while accounting for individual neuroanatomical variations.
Table 1: Key Stages in fMRI-Guided E-Field-Optimized TMS Workflow
| Stage | Primary Inputs | Core Processes | Key Outputs |
|---|---|---|---|
| 1. Neuroimaging Acquisition | Participant anatomy | T1-weighted MRI, resting-state fMRI, DTI (optional) | Anatomical volumes, BOLD time series, fiber tracts |
| 2. Target Identification | Processed fMRI data | Seed-based connectivity analysis (e.g., SGC as seed) | Personalized DLPFC target based on maximal anti-correlation with SGC |
| 3. Electric Field Modeling | T1 MRI, target coordinates | Finite Element Method (FEM) simulation, coil placement optimization | E-field magnitude and distribution, optimal coil orientation |
| 4. Neuronavigation | Target coordinates, T1 MRI, participant registration | MRI-to-head co-registration, real-time tracking | Real-time coil positioning guidance |
| 5. Treatment Delivery | Optimized protocol | iTBS/rTMS application, clinical monitoring | Applied stimulation, clinical outcomes, adverse event documentation |
Figure 1. Generalized Workflow for Precision TMS. This integrated pipeline transforms multi-modal neuroimaging data into an optimized, personalized TMS protocol. The process begins with data acquisition, progresses through computational target identification and electric field optimization, and culminates in precisely navigated treatment delivery with outcome assessment.
Quantitative Data and Comparative Efficacy
The implementation of fMRI-guided, E-field-optimized TMS protocols has yielded substantial improvements in both targeting precision and clinical outcomes. Quantitative analyses demonstrate the superiority of this integrated approach over conventional methods across multiple domains, from electric field characteristics to real-world clinical response rates.
Table 2: Electric Field Characteristics Across Targeting Methods in DLPFC Stimulation
| Targeting Method | E-Field Magnitude (V/m) in Functional Target | E-Field Magnitude (V/m) in Anatomical Target | Spatial Dispersion | Optimal Coil Orientation |
|---|---|---|---|---|
| Functional Targeting | 102.5 ± 18.3 | 78.4 ± 15.7 | Greater | Parallel to LOI (P < 0.001) |
| Anatomical Targeting | 85.7 ± 16.2 | 95.1 ± 19.5 | Lesser | Less critical |
| Statistical Significance | P < 0.001 | P < 0.01 | P < 0.05 | Directionally specific |
Electric field modeling reveals critical differences between targeting approaches. When the coil is positioned over the functionally defined target, the E-field magnitude is significantly higher in the functional target compared to adjacent anatomical regions [37]. This effect exhibits directional specificity, with parallel alignment to the local cortical orientation producing maximal field intensity (P < 0.001), while perpendicular orientation maintains functional stability with reduced anatomical interference [37]. These findings establish coil orientation optimization as a critical strategy for enhancing TMS precision.
Table 3: Clinical Outcomes of fMRI-Guided Versus Standard TMS for Depression
| Outcome Measure | fMRI-Guided aTMS (n=115) | Beam F3 Targeting (n=80) | Statistical Significance | Effect Size |
|---|---|---|---|---|
| Response Rate | 77.5% | 62.2% | P = 0.035 | OR = 2.30 |
| Remission Rate | 51.8% (overall sample) | 51.8% (overall sample) | Not reported | N/A |
| Number Needed to Treat | 6.5 | - | - | - |
| Patients with >5 Medication Failures | Lower response | Lower response | P = 0.038 (predictor) | - |
Naturalistic clinical data from 195 patients with treatment-resistant depression demonstrates the significant advantage of fMRI-guided accelerated TMS (aTMS) over standard scalp-based targeting [35]. After propensity score matching to control for baseline characteristics, the fMRI-guided group showed significantly higher response rates (77.5% vs. 62.2%, P = 0.035), with an odds ratio of 2.30 [35]. Multivariate logistic regression identified fMRI guidance as the only independent predictor of treatment response, highlighting its critical role in optimizing outcomes [35].
Experimental Protocols
Neuroimaging Data Acquisition and Preprocessing
Purpose: To acquire high-quality structural and functional MRI data for personalized target identification and E-field modeling.
Materials and Equipment:
- 3T MRI scanner with minimum 45 mT/m gradient strength
- 32-channel or higher head coil
- T1-weighted MPRAGE sequence (1mm isotropic resolution)
- T2*-weighted BOLD fMRI (3.5×3.5×4mm or higher resolution, TR=2000ms, 20+ minutes resting-state)
- Diffusion MRI (optional; 2mm isotropic, 64+ directions, b=1000 s/mm²)
Procedure:
- Structural Acquisition: Obtain T1-weighted anatomical images using a sagittal 3D MPRAGE sequence (FOV=256mm, matrix=256×256, slice thickness=1mm, no gap).
- Functional Acquisition: Acquire resting-state fMRI data with participants instructed to keep their eyes open, fixate on a crosshair, and remain awake. Implement real-time prospective motion correction.
- Data Preprocessing:
- Spatial Alignment: Coregister functional and structural images using SPM12 or FSL.
- Atlas Registration: Normalize images to standard MNI space using nonlinear transformation.
- Motion Censoring: Apply ART-based scrubbing with framewise displacement threshold of 0.5mm.
- Nuisance Regression: Implement global signal regression and bandpass temporal filtering (0.009-0.08 Hz).
- Spatial Smoothing: Apply 6mm FWHM Gaussian kernel.
Quality Control:
- Verify minimal head motion (<2mm translation, <2° rotation)
- Confirm adequate signal-to-noise ratio in prefrontal regions
- Ensure successful normalization to template space
Connectivity-Based Target Identification
Purpose: To identify the personalized DLPFC target exhibiting strongest anti-correlation with the subgenual cingulate cortex (SGC).
Materials and Software:
- Preprocessed fMRI data
- CONN toolbox or similar connectivity analysis package
- SGC seed region mask (default mask in CONN)
- Custom scripts for peak identification
Procedure:
- Seed Definition: Extract the BOLD time series from the SGC seed region (MNI coordinates: x=±4, y=26, z=-10).
- Voxel-wise Connectivity: Compute Pearson correlation coefficients between the SGC time series and all gray matter voxels in the prefrontal cortex.
- Connectivity Map Generation: Convert correlation coefficients to z-scores using Fisher transformation.
- Target Identification: Identify the voxel or cluster within the left DLPFC showing the strongest negative correlation (anti-correlation) with the SGC.
- Target Refinement: Apply manual review considering cluster size, anticipated tolerability, and accessibility with TMS coil placement.
Validation:
- Verify target location within Brodmann areas 9/46
- Confirm statistically significant anti-correlation (P < 0.05, FDR-corrected)
- Document target coordinates in both MNI and native space
Electric Field Modeling and Coil Optimization
Purpose: To simulate TMS-induced electric fields and optimize coil placement and orientation for maximal target engagement.
Materials and Software:
- T1-weighted anatomical in native space
- Target coordinates in native space
- SimNIBS software package (v4.0+)
- Figure-8 coil model (e.g., MagVenture MC-B70)
Procedure:
- Head Model Generation:
- Segment T1 image into five tissue types: skin, skull, CSF, gray matter, white matter
- Generate tetrahedral head mesh with approximately 3 million elements
Coil Placement:
- Position coil center over target coordinate
- Orient coil handle posteriorly at 45° from midline as starting position
Electric Field Simulation:
- Apply 100% stimulator output as input parameter
- Solve Maxwell's equations using finite element method
- Calculate E-field magnitude (Eₙᵣₘₛ) and normal component (E⊥)
Coil Optimization:
- Systematically vary coil orientation in 15° increments
- Identify orientation producing maximal E-field magnitude in target
- Calculate E-field ratio between target and adjacent regions
Validation:
- Confirm maximal E-field magnitude at target coordinates
- Verify acceptable E-field distribution (≤150 V/m in non-target regions)
- Document optimal coil orientation and expected target engagement
Neuronavigation and Treatment Delivery
Purpose: To precisely deliver TMS stimulation to the personalized target using real-time neuronavigation.
Materials and Equipment:
- Neuronavigation system (e.g., Localite TMS Navigator)
- Tracking markers and stereotactic camera
- TMS stimulator with figure-8 coil
- Optimized stimulation parameters
Procedure:
- System Calibration:
- Calibrate tracking system according to manufacturer specifications
- Register subject's head to MRI coordinates using facial landmarks
- Verify registration accuracy (<3mm error)
Coil Positioning:
- Position coil over target using neuronavigation guidance
- Orient coil according to E-field optimization results
- Maintain consistent coil contact and angle throughout session
Stimulation Protocol:
- Apply intermittent theta-burst stimulation (iTBS) protocol: 3-pulse 50Hz bursts repeated at 5Hz, 2s trains, 8s inter-train interval, 600 pulses/session
- Deliver multiple daily sessions (8-10 sessions/day) over 5 days for accelerated protocol
- Stimulation intensity: 90-120% resting motor threshold
Quality Assurance:
- Monitor head motion throughout session
- Recalibrate if movement exceeds 3mm
- Document actual stimulation site for each session
Safety Monitoring:
- Document adverse events (headache, fatigue, anxiety)
- Screen for seizure risk factors
- Implement contingency protocols for treatment-emergent anxiety
The Scientist's Toolkit
Table 4: Essential Research Reagents and Solutions for fMRI-Guided TMS
| Category | Item/Reagent | Specifications | Primary Function |
|---|---|---|---|
| Imaging Equipment | 3T MRI Scanner | Minimum 45 mT/m gradient, 32-channel head coil | High-resolution structural and functional data acquisition |
| Analysis Software | CONN Toolbox | v20+ with SPM12 integration | Resting-state functional connectivity analysis |
| Electric Field Modeling | SimNIBS | v4.0+ with headreco pipeline | Personalized E-field simulation and coil optimization |
| Neuronavigation | Localite TMS Navigator | Infrared tracking, MRI integration | Real-time coil positioning and target engagement verification |
| Stimulation Equipment | Figure-8 Coil | 70-75mm diameter, liquid-cooled | Focal TMS stimulation with precise field containment |
| Clinical Assessment | CGI-I Scale | 7-point clinician-rated instrument | Primary outcome measurement for treatment response |
| Computational Resources | High-Performance Workstation | 64GB RAM, GPU acceleration | Processing of neuroimaging data and E-field simulations |
| Dienogest-d6 | Dienogest-d6, MF:C20H25NO2, MW:317.5 g/mol | Chemical Reagent | Bench Chemicals |
| L-Glutamine-15N2,d5 | L-Glutamine-15N2,d5, MF:C5H10N2O3, MW:153.16 g/mol | Chemical Reagent | Bench Chemicals |
Figure 2. Mechanism of Action for Depression Treatment. This schematic illustrates the neurobiological rationale for targeting the DLPFC-SGC circuit in depression treatment. The model emphasizes how aberrant network connectivity manifests as depressive symptoms and how targeted stimulation induces network-level modulation that produces clinical improvement.
The integration of fMRI-guided targeting with electric field optimization represents a paradigm shift in transcranial magnetic stimulation, moving beyond standardized approaches toward truly personalized neuromodulation. The generalized workflow presented here provides a comprehensive framework for implementing this precision medicine approach, with robust empirical support demonstrating significantly enhanced clinical outcomes [35] and superior target engagement [37]. This methodology transforms TMS from a region-based to a circuit-based treatment, directly addressing the network-level pathophysiology underlying neuropsychiatric disorders.
Future developments in this field will likely focus on real-time closed-loop optimization, combining fMRI guidance with electrophysiological biomarkers to dynamically adjust stimulation parameters based on instantaneous brain state [36]. Additionally, the integration of artificial intelligence and machine learning approaches promises to further enhance target identification and outcome prediction [36]. As these technologies mature, fMRI-guided E-field-optimized TMS will establish a new standard for precision in neuromodulation, offering enhanced therapeutic efficacy for treatment-resistant conditions through circuit-specific engagement tailored to the individual's unique functional neuroanatomy.
The Rise of Multi-Locus TMS (mTMS) for Electronic Targeting and Network Modulation
Multi-locus transcranial magnetic stimulation (mTMS) represents a groundbreaking advancement in non-invasive brain stimulation technology that enables electronic targeting of cortical structures without physical coil movement. Unlike conventional TMS systems limited to single-site stimulation through mechanical manipulation, mTMS employs a transducer consisting of multiple overlapping coils whose individual electric fields can be superposed to create a precisely controlled resultant field [40]. This technological innovation allows researchers to stimulate distinct cortical targets with sub-millisecond interstimulus intervals, facilitating the investigation of causal interactions in functional brain networks and enabling more personalized therapeutic interventions for neurological disorders [41].
The fundamental operating principle of mTMS relies on the precise control of relative currents in multiple coils arranged in a spatially specific configuration. By adjusting the amplitude and timing of currents through each coil, the location, orientation, and characteristics of the induced electric field (E-field) maximum can be electronically manipulated within a defined cortical region [40]. This capability for rapid electronic targeting represents a paradigm shift from traditional TMS approaches, overcoming the limitations of mechanical coil movement and enabling novel experimental and therapeutic protocols previously impossible with conventional technology [42].
Technical Specifications and Performance Characteristics
mTMS System Components and Capabilities
The core mTMS system comprises several integrated components: a multi-coil transducer array, specialized power electronics with independent control channels, a field-programmable gate array (FPGA) for precise temporal control, and targeting software incorporating electric field optimization algorithms [40] [43]. Modern mTMS systems typically feature 5-6 independently controlled coil channels, each driven by its own H-bridge circuit and pulse capacitor, enabling true parallel control of stimulation parameters across all coils [40] [42].
Table 1: Technical Specifications of Representative mTMS Systems
| Parameter | 5-Coil mTMS System | Clinical mTMS Device | Preclinical 2-Coil Array |
|---|---|---|---|
| Number of Coils | 5 (oval, figure-of-eight, four-leaf-clover) | 5 | 2 |
| Targeting Area | ~30 mm diameter cortical region [40] | Similar to 5-coil system [42] | Smaller, predefined regions |
| Interstimulus Intervals | Sub-millisecond capability [40] | Millisecond-range [42] | Protocol-dependent |
| Control Electronics | Independent H-bridge circuits [40] | Enhanced safety features [42] | MRI-compatible [43] |
| Key Applications | Motor mapping, network interactions [40] | Clinical diagnostics, therapeutic protocols [42] | Simultaneous fMRI studies [43] |
Targeting Precision and Electric Field Control
mTMS technology enables precise spatial control of the stimulation focus, with the capability to electronically shift the E-field maximum within a cortical region approximately 30 mm in diameter [40]. This electronic targeting approach achieves millimeter-level precision in redirecting the stimulation focus, significantly surpassing the practical limitations of mechanical coil positioning systems [41]. The system allows smooth 360-degree rotation of the electric field orientation, which is particularly valuable for investigating the direction-dependent responses of cortical neurons [41] [42].
Table 2: Performance Characteristics of mTMS Electronic Targeting
| Performance Metric | Capability | Experimental Validation |
|---|---|---|
| Spatial Resolution | Millimeter-level precision in E-field control [40] | Motor mapping with distinct cortical locations [42] |
| Temporal Resolution | Sub-millisecond interstimulus intervals [40] [43] | Successive stimuli to distinct areas with millisecond intervals [43] |
| Orientation Control | 360-degree electric field rotation [41] | MEP amplitude variation with field direction [42] |
| Simultaneous Targets | Multiple nodes within coil array coverage [41] | Network stimulation paradigms [41] |
| Target Transition Speed | Instantaneous electronic switching [40] | Rapid mapping protocols without mechanical movement [40] |
Experimental Protocols for mTMS Applications
Automated Motor Cortex Mapping
Objective: To systematically map cortical motor representations while maintaining fixed transducer placement through electronic targeting.
Materials and Setup:
- mTMS system with 5-coil transducer array
- Electromyography (EMG) recording system for target muscle (e.g., first dorsal interosseous)
- Neuronavigation system co-registered with subject's structural MRI
- Subject comfortably seated with arm and hand properly supported
Procedure:
- System Calibration: Verify proper operation of all coil channels and calibrate current levels for each coil.
- Hotspot Identification: Locate the optimal scalp position for eliciting motor evoked potentials (MEPs) in the target muscle using conventional search procedures.
- Grid Definition: Define a rectangular or circular grid (e.g., 5×5 points with 3-5 mm spacing) centered on the motor hotspot using neuronavigation software.
- Stimulation Protocol: For each grid point:
- Calculate coil currents required to position E-field maximum at target location [40]
- Deliver 5-10 stimuli at 0.25 Hz with suprathreshold intensity (e.g., 110-120% of resting motor threshold)
- Record MEP amplitudes from target muscle
- Data Analysis:
- Calculate mean MEP amplitude for each grid point
- Construct motor representation maps using interpolation algorithms
- Determine center of gravity and map volume
Applications: Pre-surgical mapping, tracking neuroplastic changes, quantifying cortical reorganization in neurological disorders [42].
Closed-Loop Optimization of Stimulation Parameters
Objective: To automatically identify optimal stimulation locations and parameters based on real-time physiological feedback.
Materials and Setup:
- mTMS system with targeting control software API
- EEG/EMG acquisition system for feedback signals
- Real-time signal processing platform (e.g., Simulink, LabVIEW)
- Custom optimization algorithm implementation
Procedure:
- Feedback Signal Selection: Choose appropriate physiological signal (EMG for motor cortex, EEG for cognitive areas, fMRI for deeper structures).
- Parameter Space Definition: Define the cortical region of interest and parameter ranges (location, orientation, intensity).
- Optimization Algorithm: Implement Bayesian optimization or similar efficient global optimization method.
- Closed-Loop Operation:
- Deliver stimulus with specific parameters
- Measure response amplitude from feedback signal
- Update parameter estimates based on response
- Select next stimulation parameters to maximize information gain
- Convergence Criteria: Continue until optimal response is identified or parameter estimates stabilize.
Applications: Personalized therapy target identification, maximizing therapeutic response in depression, optimizing rehabilitation protocols [41].
Network Stimulation with Spatiotemporal Patterns
Objective: To investigate causal interactions in functional brain networks by stimulating multiple nodes with precise temporal sequences.
Materials and Setup:
- mTMS system capable of simultaneous multi-locus stimulation
- EEG/fMRI for monitoring network responses
- Neuronavigation system with individual tractography data
- Custom pulse sequence programming interface
Procedure:
- Network Identification: Identify target network nodes based on functional/structural connectivity (e.g., default mode network, frontoparietal network).
- Pulse Sequence Design: Program spatiotemporal stimulation patterns with precise interstimulus intervals (1-100 ms).
- Stimulation Protocol:
- Deliver patterned stimulation to multiple network nodes
- Vary timing and order of node activation
- Include control conditions (sham, reversed sequences)
- Response Assessment: Measure network-level responses using:
- TMS-evoked potentials (TEPs) with EEG
- BOLD signal changes with simultaneous fMRI
- Behavioral performance on relevant tasks
- Connectivity Analysis: Calculate changes in functional connectivity between stimulated nodes and network endpoints.
Applications: Investigating network dynamics, developing network-based therapies for psychiatric disorders, establishing causal connectivity maps [41].
Essential Research Toolkit for mTMS Experiments
Table 3: Essential Research Reagents and Equipment for mTMS Studies
| Item | Specification | Research Function |
|---|---|---|
| Multi-Coil Transducer | 5-coil array with overlapping E-fields [40] | Enables electronic field steering without mechanical movement |
| FPGA Control System | Field-programmable gate array with parallel output channels [40] | Provides precise temporal control of coil currents with sub-millisecond resolution |
| Neuronavigation System | MRI-based tracking with subject-specific head models | Ensures accurate targeting of anatomical structures |
| Electric Field Modeling | Real-time E-field calculation algorithms [40] | Optimizes coil currents for desired field characteristics at target location |
| EMG Recording System | Bipolar surface electrodes with high-input impedance amplifiers | Quantifies motor evoked potentials for motor mapping studies |
| EEG Acquisition System | High-density (64+ channels) with TMS-compatible hardware | Measures TMS-evoked potentials for network responses |
| Safety Monitoring | Temperature sensors, state-tracking mechanisms [42] | Ensures patient safety during extended stimulation protocols |
| AS-99 free base | AS-99 free base, MF:C27H30F3N5O3S2, MW:593.7 g/mol | Chemical Reagent |
| Perindoprilat-d4 | Perindoprilat-d4, MF:C17H28N2O5, MW:344.4 g/mol | Chemical Reagent |
mTMS Integration with Neuroimaging and Tractography
The combination of mTMS with advanced neuroimaging represents a powerful approach for understanding and manipulating brain networks. Integrating real-time tractography with mTMS targeting allows researchers to visualize the structural connections of the stimulated area during experiments, ensuring engagement of specific neural pathways [8]. This integration is particularly valuable for targeting specific white matter pathways or network nodes based on individual connectivity patterns.
Procedure for Tractography-Guided mTMS:
- Acquisition of Diffusion MRI: Obtain high-resolution diffusion-weighted images with sufficient gradient directions for fiber tracking.
- Tractography Reconstruction: Reconstruct target white matter pathways (e.g., cortico-striatal pathways for reward processing, frontoparietal connections for cognitive control).
- Target Identification: Identify cortical regions with strong connections to target networks.
- Field Orientation Optimization: Align the induced electric field with the principal direction of the targeted white matter fibers.
- Validation: Verify target engagement through simultaneous EEG/fMRI or behavioral measures.
This integrated approach addresses a fundamental challenge in neuromodulation: the precise targeting of specific brain circuits based on individual neuroanatomy. The pre-supplementary motor area (pre-SMA) and supplementary motor area (SMA) exemplify why this precision matters—though adjacent, these areas possess distinct structural connectomes and functional profiles [8]. The pre-SMA connects strongly with prefrontal and anterior cingulate cortices, while the SMA shows stronger connectivity with parietal and posterior cingulate regions [8]. mTMS combined with tractography enables selective targeting of these distinct circuits.
Clinical Translation and Safety Protocols
The translation of mTMS technology to clinical environments requires rigorous safety protocols and regulatory compliance. Recent developments have focused on creating mTMS systems suitable for hospital use, incorporating redundant safety mechanisms and state-tracking features that continuously monitor system operation [42]. These advancements represent critical steps toward establishing multicoil TMS as an accessible clinical tool for investigating and treating brain disorders.
Key Safety Considerations:
- Temperature Monitoring: Implementation of distributed temperature sensors throughout the coil array to prevent excessive heating during repetitive stimulation protocols [42].
- State-Tracking Mechanism: Robust monitoring of system operational status through distributed safety checks and heartbeat messages, with automatic disarming following any detected malfunction [42].
- Patient Protection: Mechanical design incorporating two means of patient protection against coil breakage or malfunction.
- Emergency Shutdown: Rapid discharge systems and fast shutdown protocols for immediate termination of stimulation when required.
The deployment of mTMS systems in clinical settings such as the Hertie Institute for Clinical Brain Research in Tübingen, Germany, demonstrates the feasibility of implementing this technology for patient care and clinical research [42]. This infrastructure enables the development of novel diagnostic and therapeutic paradigms leveraging the unique capabilities of electronic targeting for modulating dysfunctional brain networks in neurological and psychiatric disorders.
Leveraging Resting-state fMRI and DTI Tractography for Individualized Target Identification
Transcranial Magnetic Stimulation (TMS) is a non-invasive neuromodulation technique that has demonstrated significant clinical potential for various neuropsychiatric disorders. However, conventional TMS targeting methods, which often rely on standardized anatomical landmarks or the "5-cm rule," fail to account for substantial individual differences in brain structure and functional connectivity. This limitation results in considerable variability in treatment response and suboptimal clinical efficacy [36] [44]. The integration of resting-state functional magnetic resonance imaging (rs-fMRI) and diffusion tensor imaging (DTI) tractography represents a paradigm shift toward precision neuromodulation. These advanced neuroimaging techniques enable the identification of personalized stimulation targets based on individual brain network architecture, potentially revolutionizing TMS protocol optimization [36] [45].
Rs-fMRI captures spontaneous low-frequency fluctuations in the blood oxygen level-dependent (BOLD) signal, revealing intrinsic functional brain networks without requiring task performance. DTI, in contrast, maps the microstructural organization and anatomical pathways of white matter tracts by measuring the directional diffusion of water molecules. The synergistic integration of these modalities provides a comprehensive framework for understanding the relationship between brain structure and function, allowing researchers to identify individualized targets based on both functional connectivity patterns and structural wiring diagrams [45] [8]. This approach is particularly valuable for TMS optimization, as it enables targeting of specific cortical nodes embedded within pathological brain circuits, potentially enhancing treatment outcomes through personalized electric field engagement [36] [8].
Quantitative Evidence for Personalized Targeting
Variability in Targeting Methods
Empirical studies have quantified significant variability in personalized TMS targeting, highlighting the importance of methodological optimization. The following table summarizes key findings on the reliability of different targeting approaches:
Table 1: Variability and Reliability of Personalized TMS Targeting Methods
| Targeting Approach | Single-Run Variability (Euclidean Distance) | Multi-Run Variability (Euclidean Distance) | Single-Run Repeatability | Multi-Run Repeatability | Impact on Electric Field |
|---|---|---|---|---|---|
| fMRI-Based Personalization | 8.75 - 31.48 mm | 1.44 - 13.5 mm (p<0.0001) | 0.12% - 5.1% | 4.2% - 78.6% (p<0.0001) | Significant (p<0.0001) |
| fMRI-Navigated TMS | N/A | N/A | N/A | N/A | Improved consistency with multiple runs |
| Standard 5-cm Rule | High inter-individual variability | N/A | Low | N/A | Variable engagement of DLPFC |
The data clearly demonstrate that targeting methods based on a single rs-fMRI scan introduce substantial variability in target localization (8.75-31.48 mm), which significantly impacts the resulting cortical electric field distribution. Conversely, averaging data across multiple rs-fMRI scans significantly reduces this variability (1.44-13.5 mm) and improves repeatability (4.2-78.6%), producing more consistent electric fields at the targeted cortical area [46].
Clinical Efficacy of Personalized Targeting
Emerging evidence suggests that personalized TMS targeting based on functional connectivity metrics significantly enhances clinical outcomes, particularly in treatment-resistant depression:
Table 2: Clinical Efficacy of Personalized TMS Targeting
| Targeting Method | Clinical Population | Key Connectivity Biomarker | Clinical Outcome | Protocol Details |
|---|---|---|---|---|
| Stanford Neuromodulation Therapy (SNT) | Treatment-resistant depression | DLPFC subregion most anticorrelated with subgenual anterior cingulate cortex (sgACC) | ~80% remission rate | Accelerated iTBS over 5 days |
| Conventional TMS | Treatment-resistant depression | Standard 5-cm rule or EEG-guided motor hotspot | ~30-50% response rates | Standard 4-6 week protocol |
| Connectivity-Guided rTMS | Depression | DLPFC functional connectivity with sgACC | Enhanced response rates | Individualized targeting |
| Parkinson's Disease rTMS | Parkinson's disease with depression | Prefrontal-striatal dopamine pathway | Improved depressive symptoms | Individualized parameters |
The remarkable efficacy of Stanford Neuromodulation Therapy (approximately 80% remission rates in treatment-resistant depression) highlights the transformative potential of precision targeting. This protocol synergistically combines personalized targeting using rs-fMRI to identify the DLPFC subregion most anticorrelated with the sgACC with an accelerated stimulation schedule [36].
Experimental Protocols and Methodologies
Data Acquisition Protocols
MRI Acquisition Parameters:
Resting-state fMRI: Acquire T2*-weighted echoplanar imaging (EPI) sequences with the following parameters: TR/TE = 2000/30 ms, flip angle = 90°, voxel size = 3×3×3 mm³, 40-50 axial slices, 300-400 volumes (10-13 minutes). Participants should remain awake with eyes closed during scanning to minimize introduced variability [46].
Diffusion Tensor Imaging: Acquire diffusion-weighted images using a spin-echo EPI sequence with the following parameters: TR/TE = 8000-12000/80-100 ms, voxel size = 2×2×2 mm³, 60-80 axial slices, 64+ diffusion directions with b-value = 1000 s/mm², plus 7-10 b0 images. Multi-shell acquisition (e.g., b=1000, 2000 s/mm²) is recommended for improved fiber tracking in crossing regions [45] [48].
High-resolution T1-weighted Structural Imaging: Acquire 3D MPRAGE or SPGR sequences with the following parameters: TR/TE = 2300/2-3 ms, TI = 900 ms, flip angle = 9°, voxel size = 1×1×1 mm³, 176-192 sagittal slices. This structural data serves as a reference for spatial normalization and electric field modeling [8].
Quality Control and Optimization:
Perform multiple rs-fMRI runs (minimum 2-3 sessions with 2 runs each) to enhance reliability of functional connectivity estimates [46].
Monitor participant head motion during fMRI acquisition using real-time motion tracking. Implement prospective motion correction if available.
For DTI, ensure adequate signal-to-noise ratio (SNR > 20) and minimal eddy current distortion by using parallel imaging and incorporating reversed phase-encoding directions for distortion correction.
Data Preprocessing Pipeline
Rs-fMRI Preprocessing Steps:
Slice Timing Correction: Correct for acquisition time differences between slices using temporal interpolation.
Realignment: Estimate and correct for head motion using rigid-body transformation. Exclude participants with excessive motion (>3mm translation or >3° rotation).
Coregistration: Align functional images to individual T1-weighted structural scan.
Normalization: Spatially normalize images to standard Montreal Neurological Institute (MNI) space using high-dimensional warping algorithms.
Spatial Smoothing: Apply Gaussian kernel with 6-8mm full-width at half maximum to improve signal-to-noise ratio.
Temporal Filtering: Apply band-pass filter (0.008-0.09 Hz) to retain low-frequency fluctuations relevant to resting-state networks.
Nuissance Regression: Remove confounding signals including: (1) 6 motion parameters and their derivatives, (2) mean cerebrospinal fluid signal, (3) mean white matter signal, and (4) global signal if desired.
DTI Preprocessing Steps:
Eddy Current Correction: Correct for distortions and head motion using rigid-body affine registration to b0 images.
EPI Distortion Correction: Address susceptibility-induced distortions using field maps or reverse phase-encoding methods.
Skull Stripping: Remove non-brain tissue using brain extraction algorithms.
Tensor Calculation: Fit diffusion tensor model at each voxel to derive fractional anisotropy (FA) and mean diffusivity (MD) maps.
Tractography: Reconstruct white matter pathways using deterministic or probabilistic algorithms with appropriate seeding strategies.
Target Identification Methodologies
Functional Connectivity Mapping:
Seed-Based Connectivity Analysis:
- Place spherical seed regions (6-8mm radius) in key network nodes (e.g., sgACC for depression treatment targeting)
- Extract mean BOLD time series from seed region
- Compute Pearson's correlation coefficients between seed time series and all other brain voxels
- Convert correlation coefficients to z-scores using Fisher's transformation
- Identify DLPFC voxels showing strongest negative correlation with sgACC for depression treatment targeting [36]
Independent Component Analysis (ICA):
- Perform temporal concatenation group ICA using validated algorithms (e.g., MELODIC)
- Identify relevant intrinsic connectivity networks (e.g., default mode, executive control, salience networks)
- Back-reconstruct individual-level network maps
- Determine peak coordinates within targeted networks for stimulation
Parcellation-Based Connectivity:
- Apply brain atlases (e.g., Brainnetome, Schaefer parcellations) to define regions of interest
- Compute region-to-region connectivity matrices using Pearson correlation or partial correlation
- Identify connections that deviate from healthy norms or correlate with symptom severity
- Target regions showing maximal connectivity abnormalities
Structural Connectivity Mapping:
Tractography-Guided Targeting:
- Perform whole-brain tractography using deterministic or probabilistic algorithms
- Identify specific white matter pathways relevant to target disorder (e.g., hyperdirect pathway for OCD, medial forebrain bundle for depression)
- Determine cortical termination zones of these pathways as potential stimulation targets [8]
Multimodal Integration:
- Overlay functional connectivity maps with structural connectivity data
- Identify cortical regions that are both functionally aberrant and structurally connected to pathological networks
- Use structural connectivity to inform likely network effects of stimulating a given target
Figure 1: Workflow for Multimodal TMS Target Identification. This diagram illustrates the comprehensive pipeline from data acquisition through target identification, highlighting the integration of functional and structural connectivity information.
Electric Field Modeling and Target Engagement
Finite Element Method (FEM) Modeling:
Head Model Construction:
- Segment T1-weighted images into six tissue types: scalp, skull, cerebrospinal fluid, gray matter, white matter, and air cavities
- Assign tissue-specific electrical conductivity values based on literature
- Generate tetrahedral mesh with appropriate density (1-2mm resolution)
Electric Field Simulation:
- Incorporate TMS coil configuration (figure-8, H-coil, etc.) and positioning
- Solve Maxwell's equations using FEM approaches
- Calculate electric field magnitude and direction throughout the brain
- Optimize coil placement and orientation to maximize field strength at target while minimizing off-target stimulation [8]
Target Engagement Validation:
- Combine TMS with simultaneous EEG to measure evoked potentials and assess direct brain response to stimulation
- Use neuroimaging biomarkers (fMRI connectivity changes, perfusion alterations) to verify target engagement
- Implement closed-loop approaches that adjust stimulation parameters based on real-time neurophysiological feedback [36]
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Multimodal TMS Target Identification
| Resource Category | Specific Tools/Platforms | Primary Function | Application Notes |
|---|---|---|---|
| Neuroimaging Analysis | FSL, SPM, AFNI, FreeSurfer, CATO | fMRI/DTI preprocessing, normalization, segmentation | CATO provides specialized connectivity analysis; FSL's FDT for diffusion data |
| Connectivity Modeling | CONN, DPABI, Brainstorm, GAT | Functional connectivity analysis, graph theory metrics | CONN offers comprehensive pipeline for ROI-to-ROI and voxel-wise connectivity |
| Tractography Software | MRtrix, DSI Studio, TrackVis | White matter fiber tracking, structural connectomes | MRtrix3 enables advanced CSD-based tractography for crossing fibers |
| Electric Field Modeling | SimNIBS, ROAST, COMETS | TMS electric field simulation, dosimetry | SimNIBS provides user-friendly interface for individualized field modeling |
| TMS Navigation | Localite, BrainSight, Visor2 | Neuronavigation for precise coil placement | Integrates individual MRI data with real-time head tracking |
| Multimodal Integration | IBrainGNN, custom MATLAB/Python scripts | Deep learning fusion of fMRI/DTI/sMRI | Graph neural networks for cross-modal pattern recognition |
| Normative Modeling | PCNtoolkit, NeuroPM-box | Individual deviation mapping from healthy norms | Enables single-subject abnormality detection for personalized targeting |
Implementation Framework and Clinical Translation
Quality Assurance and Validation
Test-Retest Reliability Assessment:
- Conduct multiple rs-fMRI scans within the same session (2-3 runs) and across different sessions (1-2 weeks apart) to establish reliability of connectivity measures
- Calculate intraclass correlation coefficients (ICC) for key connectivity values, targeting ICC > 0.8 for clinical applications
- Establish minimum scan duration requirements for reliable connectivity estimates (typically 10+ minutes total acquisition time) [46]
Target Verification Methods:
- Anatomical validation: Ensure targets fall within cytoarchitectonically defined regions using probabilistic atlases
- Functional validation: Verify that stimulated targets produce expected changes in network connectivity during concurrent TMS-fMRI
- Clinical validation: Corrogate target location accuracy with symptom improvement in clinical trials
Integration with TMS Treatment Protocols
Practical Implementation Workflow:
Baseline Assessment: Acquire multimodal MRI (rs-fMRI, DTI, T1-weighted) prior to TMS initiation
Target Identification: Process imaging data to derive individualized target coordinates using validated pipelines
Electric Field Optimization: Simulate electric field distribution for various coil placements and orientations
Neuronavigation Setup: Register individual MRI data to real-time head tracking system for precise coil placement
Treatment Delivery: Administer TMS with continuous monitoring of coil position relative to target
Adaptive Optimization: Periodically reassess functional connectivity and adjust target if needed based on treatment response
Figure 2: Mechanism of Action for Connectivity-Guided TMS. This diagram illustrates how TMS targeted to specific DLPFC subregions identified through functional and structural connectivity analysis modulates pathological networks in depression.
The integration of resting-state fMRI and DTI tractography represents a significant advancement in personalized neuromodulation, enabling individualized TMS target identification based on unique brain network architecture. The protocols and methodologies outlined in this application note provide researchers and clinicians with a comprehensive framework for implementing these precision approaches. Key considerations for successful implementation include acquiring multiple rs-fMRI runs to enhance reliability, employing robust preprocessing pipelines to minimize artifacts, and utilizing multimodal integration strategies that leverage both functional and structural connectivity information. As the field progresses, future developments in real-time tractography visualization, closed-loop stimulation systems, and AI-driven target optimization promise to further enhance the precision and efficacy of personalized TMS protocols [36] [8] [46].
Overcoming Variability: Strategies for Reliable Target Engagement and Parameter Optimization
Addressing Inter-Subject Anatomical and Functional Variability with Neuronavigation
Transcranial Magnetic Stimulation (TMS) has emerged as a cornerstone non-invasive neuromodulation technique for treating various psychiatric and neurological disorders. A critical challenge in TMS applications is the significant inter-subject anatomical and functional variability in human brain architecture. Traditional TMS targeting methods that rely on standardized scalp measurements (e.g., the "5-6 cm rule" or Beam F3 method) fail to account for this individual neuroanatomical diversity, potentially compromising treatment efficacy [51] [44].
Neuronavigation systems address this variability by co-registering the patient's head to their structural magnetic resonance imaging (MRI) scans, providing real-time feedback on coil positioning relative to individualized neuroanatomical targets [51]. This technology enables researchers and clinicians to account for individual differences in cortical morphology, gyral patterns, and functional neurocircuitry, thereby delivering more precise and reproducible stimulation [44]. The integration of neuronavigation represents a paradigm shift from standardized to personalized targeting approaches in TMS research and clinical application.
Quantitative Comparison of Targeting Methodologies
Accuracy and Precision Metrics
Recent research provides compelling quantitative evidence supporting the superiority of neuronavigation over traditional cap-based targeting methods. A comprehensive study comparing these approaches across 42 participants and 10,224 measurements revealed statistically significant differences in targeting accuracy [51].
Table 1: Comparison of Targeting Accuracy Between Cap-Based and Neuronavigation Methods
| Parameter | Cap-Based Targeting | Neuronavigation Targeting | P-value |
|---|---|---|---|
| Distance Deviation | 10.66 mm (SEM = 0.19 mm) | 0.3 mm (SEM = 0.03 mm) | < 0.0001 |
| Roll/Pitch Angle Deviation | 7.79° (SEM = 1.07°) | 0.34° (SEM = 0.01°) | < 0.0001 |
| Yaw Angle Deviation | 5.99° (SEM = 0.12°) | 0.22° (SEM = 0.004°) | < 0.0001 |
| Inter-operator Differences | Significant (p < 0.05) | Not Significant | - |
Electric Field Modeling Consequences
The positional inaccuracies associated with cap-based targeting translate directly into suboptimal stimulation at the cortical level. Electric field (E-field) modeling demonstrates that coil placement errors result in significantly reduced E-field magnitudes at the intended prefrontal cortical target [51].
- Cap-based targeting resulted in E-field equivalents of 110.7% motor threshold (range = 58.3–127.4%) despite application of 120% MT stimulation
- Neuronavigated targeting delivered consistent E-field equivalents of 119.9% MT (range = 115–123.3%) with 120% MT stimulation [51]
- The variability in cap-based targeting was substantial, with some individuals receiving only 48.6% of the intended on-target E-field [51]
These findings underscore the critical relationship between targeting accuracy and delivered stimulation dose, highlighting neuronavigation's role in ensuring consistent and biologically relevant dosing in TMS research.
Technical Foundations of Neuronavigation Systems
Core System Components
Modern neuronavigation systems integrate several hardware and software components to achieve precise tracking and targeting capabilities:
Optical Tracking Systems (OTS): Utilize infrared cameras to track reflective markers attached to the patient's head and TMS coil, providing sub-millimeter accuracy [52] [53]. OTS currently represents the gold standard in surgical stereotactic navigation due to its proven accuracy and reliability [52].
Dynamic Reference Frame (DRF): A patient-specific tracker with calibrated reflective fiducial markers that maintains registration between the patient's head and pre-operative MRI data [52]. Custom-made DRFs can be 3D-printed using biocompatible and sterilizable materials for optimal patient-specific fit [52].
Registration Software: Algorithms that co-register the patient's physical space with imaging data based on anatomical landmarks (e.g., ear and nose structures) or surface matching [51] [53].
Augmented Reality (AR) Interfaces: Emerging head-mounted display (HMD) technologies, such as the VOSTARS platform, integrate virtual navigation information directly with the surgeon's view of the surgical field, reducing cognitive load and focus shifting [52]. These systems have demonstrated targeting accuracy comparable to commercial navigation systems (median accuracy of 2 mm) [52].
Integration with Neuroimaging Modalities
Neuronavigation systems can incorporate various imaging modalities to enhance targeting precision:
- Structural MRI: Provides high-resolution anatomical reference for target identification and trajectory planning [51] [53].
- Functional MRI (fMRI): Enables targeting based on functional neurocircuitry, such as the cortical location most anticorrelated with subgenual anterior cingulate cortex in depression treatment [51] [53].
- Diffusion Tensor Imaging (DTI): Allows visualization and avoidance of critical white matter pathways during surgical planning [53].
- Functional Ultrasound (fUS): An emerging preclinical modality that enables automatic vascular-based neuronavigation by leveraging unique cerebral vascular fingerprints [54].
Research Reagent Solutions and Experimental Materials
Table 2: Essential Research Materials for Neuronavigation Studies
| Category | Specific Examples | Research Function |
|---|---|---|
| Neuronavigation Systems | Brainsight, Localite, VOSTARS, StealthStation | Core platform for co-registration, tracking, and visualization of TMS coil position relative to neuroanatomy [51] [52] |
| Tracking Modalities | Optical Tracking Systems (OTS), Electromagnetic Tracking Systems (EMTS) | Real-time spatial localization of subject anatomy and TMS coil; OTS offers superior accuracy while EMTS doesn't require line-of-sight [52] |
| Imaging Contrast Agents | Gadolinium-based contrast (MRI), Microbubbles (fUS) | Enhance vascular and soft tissue visualization for improved registration accuracy; microbubbles enable ultrasound localization microscopy [54] |
| Fiducial Markers | Reflective spheres, Electromagnetic sensors | Serve as reference points for co-registration between physical space and imaging data [51] [52] |
| Computational Modeling Software | SimNIBS, ROAST, ANSYS | Electric field modeling to estimate cortical stimulation strength and distribution based on individual anatomy [51] |
Experimental Protocols for Neuronavigation Research
Protocol 1: Neuronavigated TMS for DLPFC Targeting
This protocol outlines the methodology for precise dorsolateral prefrontal cortex (DLPFC) targeting using neuronavigation, as validated in recent accelerated TMS studies [51].
Preparatory Phase:
- MRI Acquisition: Obtain high-resolution T1-weighted structural MRI scans using standardized parameters (e.g., TR = 2300 ms, TE = 2.26 ms) [51]. For functional targeting, acquire resting-state fMRI to identify personalized functional networks.
- Target Identification: Import structural MRI into neuronavigation software. Define the DLPFC target using either:
- System Calibration: Calibrate the optical tracking system and TMS coil tracker according to manufacturer specifications. Verify calibration accuracy using phantom targets.
Experimental Phase:
- Subject Registration: Affix head tracker with reflective fiducial markers. Perform co-registration using anatomical landmarks (nasion, pre-auricular points) or surface matching.
- Accuracy Verification: Validate registration accuracy by targeting known anatomical landmarks (e.g., motor cortex hotspot) and confirming correspondence with expected neuroanatomy.
- Stimulation Procedure: Position TMS coil using real-time neuronavigational feedback to maintain target accuracy within predetermined thresholds (e.g., <2 mm distance, <2° angle deviation) throughout stimulation session.
- Quality Control: Document actual coil position and orientation for each session, enabling post-hoc analysis of targeting consistency and E-field modeling.
Protocol 2: Multi-Session Accelerated TMS with Consistency Control
This protocol adapts neuronavigation for intensive accelerated TMS paradigms involving multiple daily sessions, where maintenance of targeting consistency is particularly challenging [51] [55].
Session Workflow:
- Baseline Registration: Perform comprehensive registration at the beginning of each treatment day using identical fiducial marker placement.
- Inter-session Verification: Before each subsequent session, verify registration accuracy and adjust if deviation exceeds predetermined threshold (e.g., >1 mm).
- Intra-session Monitoring: Continuously monitor coil position throughout stimulation delivery, providing real-time feedback to operators when adjustments are needed.
- Data Documentation: Record all positional data (XYZ coordinates, angles) for each session to enable analysis of targeting drift over time.
Validation Measures:
- Operator Consistency: Assess inter-operator differences in targeting accuracy [51]
- E-field Modeling: Compute electric field distributions based on actual coil positions to quantify biological dose delivery [51]
- Clinical Correlations: Relate targeting accuracy metrics to clinical outcomes in therapeutic applications
Protocol 3: Vascular-Based Neuronavigation for Preclinical Research
This protocol describes an automated vascular-based neuronavigation approach for preclinical functional ultrasound (fUS) studies, applicable to TMS target validation in animal models [54].
Imaging Preparation:
- Reference Atlas Alignment: Pre-align a 3D Doppler reference volume with the Allen Mouse Brain Common Coordinate Framework or other appropriate stereotaxic atlas.
- Vascular Imaging: Acquire whole-brain 3D Power Doppler volumes using ultrafast ultrasound imaging (e.g., 100 μm × 100 μm in-plane resolution).
- Automated Registration: Implement the Brain Positioning System (BPS) algorithm for automatic alignment of live Doppler images with the reference atlas based on cerebral vascular fingerprints.
Experimental Application:
- Target Identification: Select anatomical or functional targets based on the reference atlas.
- Automated Positioning: Utilize motorized probe positioning system to automatically align ultrasound probe with predetermined targets.
- Validation: Verify positioning accuracy using super-resolution ultrasound localization microscopy (achieving 44-96 μm accuracy) [54].
- Functional Mapping: Conduct fUS imaging during TMS or other neuromodulatory interventions to map functional activation patterns within precisely targeted regions.
Workflow Visualization
Implementation Challenges and Technical Considerations
Addressing System Limitations
While neuronavigation significantly enhances targeting precision, researchers must account for several technical limitations:
- Brain Shift Phenomenon: Surgical procedures or cerebrospinal fluid leakage can cause displacement of brain structures relative to pre-operative imaging, requiring intraoperative updates or real-time imaging correction [53].
- Registration Errors: Inaccuracies in co-registration between imaging data and physical space can introduce systematic errors. Implementation of rescue reference points on the patient's skull enables intraoperative correction [53].
- Technical Expertise Requirements: Effective operation requires specialized training in both system operation and neuroanatomical interpretation [51] [53].
Economic and Practical Considerations
The implementation of neuronavigation in research settings involves important practical considerations:
- Equipment Costs: Commercial neuronavigation systems represent substantial investments (approximately $60,000), though emerging technologies may reduce this barrier over time [51] [53].
- Time Requirements: Preoperative imaging, image processing, and registration procedures add to protocol duration, though this is offset by enhanced experimental precision [51] [53].
- Operator Variability: Interestingly, while cap-based targeting shows significant inter-operator differences, neuronavigation demonstrates consistent accuracy across operators with appropriate training [51].
Future Directions and Emerging Technologies
The field of neuronavigation continues to evolve with several promising technological developments:
- Augmented Reality Integration: Head-mounted displays specifically designed for surgical navigation, such as the VOSTARS platform, provide ergonomic advantages by preserving the operator's egocentric view while overlaying navigation information [52].
- Functional Ultrasound Navigation: Vascular-based neuronavigation using ultrafast Doppler imaging enables automatic structure identification in preclinical research with remarkable accuracy (44-96 μm positioning error) [54].
- Real-Time Field Modeling: Integration of real-time E-field computation based on actual coil position and individual head models could provide immediate feedback on delivered stimulation dose [51].
- Multi-Modal Data Fusion: Advanced integration of structural, functional, and vascular imaging data creates comprehensive personalized brain maps for ultra-precise targeting [44] [54].
Neuronavigation technology represents a critical advancement for addressing the fundamental challenge of inter-subject anatomical and functional variability in TMS research. The quantitative evidence demonstrates substantial improvements in targeting accuracy, consistency, and biological dose delivery compared to traditional methods. As neuromodulation research increasingly focuses on personalized targeting approaches, neuronavigation provides the methodological foundation for achieving the precision necessary to elucidate mechanism-of-action and optimize therapeutic efficacy. The continued refinement of these technologies, coupled with standardized implementation protocols as outlined in this document, will further enhance the reproducibility and translational impact of TMS research across diverse populations and neuropsychiatric conditions.
Determining Optimal Stimulation Intensity and Number of Pulses for Reliable Output
The efficacy of Transcranial Magnetic Stimulation (TMS) as a non-invasive neuromodulation technique is critically dependent on the precise optimization of its stimulation parameters. Among these, stimulation intensity and total pulse number represent two of the most fundamental variables governing the reliability and magnitude of neurophysiological and clinical outcomes [44]. The establishment of robust, reproducible protocols is essential for both basic neuroscience research and clinical applications, particularly in the treatment of neuropsychiatric disorders such as major depressive disorder (MDD) and treatment-resistant depression (TRD) [55] [29]. This document synthesizes current evidence and provides detailed methodologies for determining these key parameters, framed within the broader context of TMS protocol optimization research.
Meta-regression analyses and clinical trials have elucidated clear dose-response relationships for TMS. The tables below summarize key quantitative findings related to pulse number and stimulation intensity for reliable output.
Table 1: Impact of Total Pulse Number on Clinical Outcomes in Accelerated rTMS/TBS for Depression
| Protocol Type | Total Sessions | Pulses per Session | Total Pulses | Key Findings on Efficacy |
|---|---|---|---|---|
| Standard 10 Hz rTMS [29] | 30 | 3,000 | 90,000 | Benchmark remission rate ~25% in TRD |
| Accelerated iTBS (PAiT) [29] | 50 (over 5 days) | 1,800 | 90,000 | High remission rates (up to ~79% in some studies) |
| Accelerated HF-rTMS/iTBS [55] | >20 | Variable | Higher total pulses | Associated with enhanced antidepressant effects |
Table 2: Key Parameter Interactions for Optimized Output
| Parameter | Optimal Range/Consideration | Impact on Output Reliability |
|---|---|---|
| Inter-Session Interval (ISI) [55] [29] | ≥50 minutes | Allows for neural recovery and synaptic strengthening, enhancing effect durability. |
| Stimulation Target [36] [8] | Personalized DLPFC (anti-correlated with sgACC) | Superior to standardized targeting (e.g., Beam-F3 method), leading to higher remission rates. |
| Stimulation Intensity [56] | Often set relative to individual's resting motor threshold (rMT) | Critical for balancing efficacy with safety; ensures adequate cortical engagement. |
Experimental Protocols
Protocol 1: Determining Motor Threshold for Intensity Calibration
Objective: To establish the resting Motor Threshold (rMT) for a subject, which serves as a reference for setting stimulation intensity in subsequent experiments or treatments.
Materials: TMS apparatus with a figure-of-eight coil, electromyography (EMG) system, surface electrodes.
Methodology:
- Subject Preparation: Seat the subject comfortably. Place surface EMG electrodes on the contralateral First Dorsal Interosseous (FDI) muscle in a belly-tendon montage. Ensure skin is cleaned to reduce impedance.
- Coil Positioning: Use neuromavigation or the manual "hotspot" method to position the TMS coil over the primary motor cortex (M1) hand area, tangentially to the scalp with the handle pointing posteriorly. The optimal site is the location where TMS pulses elicit the largest MEPs in the FDI muscle.
- Threshold Determination: Apply single-pulse TMS at a low intensity (e.g., 30% of maximum stimulator output). Gradually increase the intensity in 1-5% increments.
- Resting Motor Threshold (rMT): Define rMT as the minimum stimulus intensity required to elicit MEPs of >50 µV peak-to-peak amplitude in at least 5 out of 10 consecutive trials while the target muscle is at rest [56].
- Intensity Setting: For experimental or treatment protocols (e.g., rTMS to DLPFC), set the stimulation intensity as a percentage of the determined rMT (e.g., 80%-120% of rMT), based on the specific protocol's requirements and safety guidelines.
Protocol 2: Evaluating the Dose-Response Relationship of Pulse Number
Objective: To systematically investigate the effects of total pulse number on the reliability of motor evoked potentials (MEPs) or clinical outcomes.
Materials: Navigated TMS system, EMG equipment, robot-assisted coil holder (optional for stability), clinical rating scales (e.g., HAM-D for depression).
Methodology:
- Study Design: A test-retest, within-subjects design is recommended to control for inter-individual variability.
- Stimulation Parameters: Fix the stimulation intensity at 120% of rMT. The coil location and orientation over M1 must be kept constant, ideally using a robot-assisted holder [56].
- Pulse Delivery: On separate days, in a randomized order, deliver different total numbers of pulses (e.g., 500, 1000, 1500, 2000) using the same pulse pattern (e.g., single-pulse at 0.25 Hz).
- Outcome Measurement:
- Neurophysiological: Record MEP amplitude and latency for each pulse. Calculate the intra-individual coefficient of variation (CoV) for each pulse-number condition.
- Clinical: In clinical trials, correlate total pulse number with pre-post changes in clinical scores (e.g., HAM-D). Meta-regression analysis can be applied across multiple studies to establish dose-response curves [55].
- Data Analysis: Compare the CoV across different pulse-number conditions. Lower CoV indicates higher reliability. A positive, saturating relationship between total pulse number and clinical improvement is often observed [55].
Protocol 3: Personalized Accelerated iTBS Protocol for Depression
Objective: To administer a high-dose, accelerated iTBS protocol with personalized targeting for treatment-resistant depression.
Materials: MRI scanner, neuromavigation system, TMS device capable of iTBS, fMRI processing software.
Methodology:
- Personalized Target Identification:
- Acquire a high-resolution structural MRI and a resting-state fMRI scan for the patient.
- Identify the left dorsolateral prefrontal cortex (DLPFC) subregion that demonstrates the strongest negative functional connectivity (anti-correlation) with the subgenual anterior cingulate cortex (sgACC) [36] [29].
- This individualized coordinate is imported into the neuromavigation system as the stimulation target.
- Stimulation Parameters:
- Protocol: Intermittent TBS (iTBS).
- Pattern: Triplets of 50 Hz pulses, repeated at 5 Hz.
- Session Structure: 10 sessions per day.
- Intersession Interval: 50 minutes.
- Treatment Course: 5 consecutive days (50 total sessions).
- Total Pulses: 1800 pulses/session × 50 sessions = 90,000 pulses [29].
- Coil Placement: Use the neuromavigation system to precisely target the personalized DLPFC coordinate for every session.
- Outcome Assessment: Administer clinical depression scales (e.g., MADRS, HAM-D) at baseline, after the 5-day treatment, and at multiple follow-up time points (e.g., 4, 12, 26 weeks) to assess acute and long-term efficacy [29].
Signaling Pathways and Workflows
The following diagram illustrates the logical workflow and key parameter interactions for optimizing TMS protocols, from target identification to outcome assessment.
Diagram 1: TMS protocol optimization workflow for reliable output. The process integrates personalized neuroimaging, parameter calibration, and precise administration, highlighting the role of pulse number, pattern, and timing.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for TMS Optimization Research
| Item | Function in Research |
|---|---|
| Neuromavigation System | Core technology for precise, individualized coil placement over the intended cortical target (e.g., DLPFC) using the subject's own MRI, drastically improving target engagement [36] [8]. |
| Robot-Assisted Coil Holder | Maintains stable coil position and orientation relative to the head throughout the stimulation session, critical for reducing variability in the induced electric field and improving test-retest reliability [56]. |
| EMG System with Surface Electrodes | The primary tool for quantifying TMS output reliability at the motor cortex by recording Motor Evoked Potentials (MEPs), used for determining motor threshold and measuring corticospinal excitability [56]. |
| Pulse Parameter Sets (TBS, HF-rTMS) | Different pulse patterns (e.g., Theta Burst Stimulation, high-frequency rTMS) are the "reagents" that differentially modulate cortical excitability and plasticity, enabling the study of different dose-response relationships [17] [29]. |
| Functional & Structural MRI | Used to identify personalized stimulation targets based on individual functional connectivity (e.g., DLPFC-sgACC anti-correlation) and to understand the structural circuitry engaged by stimulation [36] [8]. |
| TMS-EEG Integration Platform | Allows direct measurement of cortical responses to TMS (TMS-Evoked Potentials), providing a biomarker of cortical excitability and connectivity beyond the motor system, crucial for probing network-level effects [8]. |
The Role of AI and Machine Learning in Predicting Treatment Response and Optimizing Parameters
Transcranial Magnetic Stimulation (TMS) is a non-invasive neuromodulation technique based on electromagnetic induction that modulates cortical excitability to treat neuropsychiatric disorders [36] [57]. Conventional TMS targeting methods often rely on anatomical landmarks and do not adequately account for individual differences in brain structure and functional networks, leading to considerable variability in treatment responses [36]. Artificial intelligence (AI) and machine learning (ML) are now revolutionizing TMS by enabling precise targeting, predicting treatment outcomes, and optimizing stimulation parameters through the analysis of large-scale multimodal datasets [36] [58] [59]. This document provides detailed application notes and experimental protocols for researchers investigating AI-driven TMS optimization, framed within the broader context of transcranial magnetic stimulation protocol optimization research.
AI and ML Predictive Modeling Performance
Machine learning models have demonstrated significant potential in predicting individual patient responses to TMS treatment across various disorders and data modalities. The table below summarizes quantitative performance data from recent studies.
Table 1: Performance Metrics of ML Models in Predicting TMS Treatment Response
| Study Focus | Data Modality | Sample Size | ML Algorithm(s) | Key Performance Metrics | Top Predictive Features |
|---|---|---|---|---|---|
| Treatment-Resistant Depression [58] | Electronic Medical Records (32 clinical/demographic features) | 232 patients | Supervised ML with nested cross-validation | Response AUC: 0.689 (0.638-0.740); Remission AUC: 0.745 (0.692-0.797) | Comorbid anxiety, obesity, benzodiazepine/antipsychotic use, chronicity of TRD, iTBS protocol, number of sessions |
| Comorbid PTSD & MDD [59] | Resting-state EEG (8-channel) | 29 patients | Lasso Regression, Support Vector Machine | MDD Response AUC: 0.83; PTSD Response AUC: 0.71; Pre/post TMS classification accuracy: 73.8-78.6% | EEG coherence in alpha, beta, theta, and delta bands |
| Smoking Cessation [60] | Resting-state & task-based fMRI | 42 participants | Machine Learning Algorithms | Significant reduction in cigarettes smoked (p<0.05); Increased cessation rates | Salience network connectivity, particularly during smoking cue exposure |
Experimental Protocols and Methodologies
Predictive Modeling Using Electronic Health Records
Objective: To develop and validate ML models for predicting rTMS treatment response and remission in patients with treatment-resistant depression (TRD) using routinely collected clinical data [58].
Patient Selection Criteria:
- Primary diagnosis of Major Depressive Disorder (MDD)
- Age ≥ 18 years
- Failure to respond to at least two antidepressant pharmacotherapy trials
- Completion of at least 15 rTMS sessions
- Baseline PHQ-9 score > 4
Feature Extraction:
- Collect 32 EMR-derived features including demographics, clinical characteristics, and treatment parameters
- Key variables: age, gender, BMI category, psychiatric comorbidities, medication use, depression chronicity, TMS protocol parameters
- Outcome measures: PHQ-9 scores pre- and post-treatment defining response (>50% reduction) and remission (PHQ-9 < 5)
ML Pipeline:
- Implement nested cross-validation to prevent overfitting
- Train multiple algorithms (e.g., random forest, SVM, gradient boosting)
- Calculate Shapley values for feature importance interpretation
- Assess model calibration and clinical utility using decision curve analysis
Neuroimaging-Based Biomarker Discovery
Objective: To identify neural biomarkers of TMS response using functional MRI and machine learning [60].
fMRI Acquisition Parameters:
- Acquire both resting-state and task-based fMRI (smoking cue reactivity for addiction studies)
- Scanning parameters: TR/TE = 800/30ms, flip angle = 52°, voxel size = 2×2×2mm
- Task paradigm: block design with alternating neutral and salient cue presentations
Data Preprocessing Pipeline:
- Standard preprocessing: slice-time correction, motion realignment, normalization to MNI space
- Nuisance regression (white matter, CSF signals)
- Functional connectivity analysis: seed-based or independent component analysis (ICA)
- Extract connectivity matrices for major networks: salience network, default mode network, central executive network
Machine Learning Framework:
- Use connectivity features as input to classifiers
- Implement feature selection to reduce dimensionality
- Train models to predict continuous outcomes (symptom reduction) and categorical outcomes (responder/non-responder)
- Validate models using held-out test sets or cross-validation
EEG-Based Response Prediction
Objective: To predict clinical response to TMS using resting-state EEG coherence patterns [59].
EEG Data Collection:
- Equipment: 8-channel EEG system
- Protocol: 5-minute resting-state recording eyes closed
- Settings: sampling rate 500 Hz, impedance < 5 kΩ
- Timing: pre-TMS and post-TMS treatment series
Feature Extraction:
- Calculate coherence values between all electrode pairs
- Analyze in standard frequency bands: delta (1-4 Hz), theta (4-8 Hz), alpha (8-13 Hz), beta (13-30 Hz)
- Generate symmetric coherence matrices for each frequency band
Machine Learning Analysis:
- Apply Lasso regression for feature selection and prediction
- Implement Support Vector Machine (SVM) classifiers
- Train models to: (1) predict clinical response from baseline EEG, (2) classify pre- vs post-TMS treatment state
- Assess accuracy, sensitivity, specificity using ROC analysis
Research Reagent Solutions
Table 2: Essential Materials and Analytical Tools for AI-Driven TMS Research
| Category | Specific Tools/Platforms | Primary Function | Application Notes |
|---|---|---|---|
| TMS Equipment | Magventure MagPro with B70 coil; BrainsWay H1-coil system | TMS stimulation delivery | B70 coil for cortical stimulation; H1-coil for deeper targets [58] |
| Neuroimaging Systems | 3T fMRI scanners; 8-channel EEG systems | Brain activity and connectivity assessment | fMRI for spatial localization; EEG for temporal dynamics [59] [60] |
| Computational Modeling | Finite Element Modeling (FEM) software; DTI tractography | Electric field simulation; Structural connectivity | Individualized electric field simulations for targeting [36] |
| Machine Learning Frameworks | Scikit-learn, TensorFlow, PyTorch | Predictive model development | Including SVM, random forests, deep learning architectures [36] [58] |
| Clinical Assessment Tools | PHQ-9, PTSD checklists, craving scales | Treatment outcome quantification | Self-report measures for symptom tracking [58] [59] |
Integrated Workflow for AI-Driven TMS Personalization
The following diagram illustrates the comprehensive workflow for AI-guided personalized TMS treatment, integrating multimodal data acquisition, computational modeling, and closed-loop optimization.
AI-Driven TMS Personalization Workflow: This diagram outlines the integrated pipeline for precision neuromodulation, from initial patient assessment through treatment delivery and outcome evaluation.
Signaling Pathways and Network Mechanisms
The therapeutic effects of TMS are mediated through modulation of specific brain networks. AI approaches have identified key networks that predict treatment response across disorders.
TMS Network Modulation Pathways: This diagram illustrates the key neural networks and neurobiological mechanisms through which TMS exerts its therapeutic effects, particularly highlighting the salience network identified as a crucial predictor of treatment response.
The integration of AI and machine learning with TMS represents a paradigm shift in neuromodulation, moving from standardized protocols toward truly personalized treatment approaches. The application notes and protocols detailed herein provide researchers with methodologies to advance this field through rigorous data collection, appropriate analytical techniques, and comprehensive validation frameworks. As these technologies mature, they hold the promise of significantly improving outcomes for patients with various neuropsychiatric disorders by enabling data-driven personalization of TMS therapy.
Real-Time Tractography-Assisted Navigation and Electric Field Modeling for Precision
Application Notes
The integration of real-time tractography-assisted neuronavigation with electric field (E-field) modeling represents a paradigm shift in transcranial magnetic stimulation (TMS), moving from standardized scalp-based targeting toward fully personalized, network-informed stimulation. This approach addresses the core challenge in TMS: the substantial inter-individual variability in brain anatomy and connectivity that leads to inconsistent treatment outcomes. By visualizing structural connections during stimulation and precisely modeling the resulting E-field, clinicians and researchers can now target specific brain networks with unprecedented accuracy, paving the way for more effective and reliable neuromodulation protocols.
Core Technological Foundations
The precision TMS framework rests on two complementary technological pillars:
1.1.1 Real-Time Tractography-Assisted Neuronavigation Conventional neuronavigation systems display TMS coil position relative to structural MRI but cannot visualize the white matter networks through which TMS effects propagate. Real-time tractography solves this limitation by enabling on-the-fly visualization of structural connections during stimulation. A modular framework integrates offline diffusion MRI analysis with online probabilistic tractography using the parallel transport approach. This system combines open-source software Trekker for tractography with InVesalius for neuronavigation, allowing interactive parameter tuning and real-time visualization of thousands of streamlines through an innovative uncertainty visualization method [61].
Feasibility studies demonstrate this approach's capacity to capture substantial portions of target area connectivity within seconds, often surpassing offline method coverage. Considerable inter-subject variability highlights its importance—in visual cortex (V1) stimulation, approximately 15,000 streamlines were observed in one subject while another showed no streamlines for the same target, underscoring how individual connectome differences dramatically affect stimulation outcomes [61].
1.1.2 Electric Field Modeling for Personalized Dosing Traditional TMS dosing relies on percentage of maximum stimulator output (%MSO) or motor threshold (MT) titrated for the motor cortex, even when stimulating non-motor regions. E-field modeling reveals substantial inter-individual variability in stimulation intensity and spread at fixed %MSO intensities, primarily arising from differences in scalp-to-cortex distance and cortical gyrification [62] [63].
Computational E-field modeling employs subject-specific, anatomically accurate head models derived from structural MRI to quantify the delivered "E-field dose" in terms of strength, focality, and spatial distribution. The methodology encompasses TMS physics, modeling assumptions, coil modeling, and numerical techniques for solving the E-field distribution. The induced E-field consists of primary components from the coil's changing magnetic field and secondary components from charge accumulation at tissue interfaces with varying conductivities [63]. Advanced numerical methods like the Hybridizable Discontinuous Galerkin Finite Element Method (HDG-FEM) now enable highly accurate E-field calculation, particularly for thin-layer head structures like meninges and cerebrospinal fluid where conventional methods struggle [64].
Quantitative Data and Efficacy Metrics
Table 1: Tractography Performance Metrics Across Different TMS Targets
| TMS Target | Streamline Count Range | Overlap with Offline Tractography | Key Connectivity Pathways |
|---|---|---|---|
| Broca's Area | 8,000-12,000 | ~75% coverage after 20,000 streamlines | Frontal aslant tract, arcuate fasciculus, uncinate fasciculus |
| Primary Motor Cortex | 10,000-15,000 | ~80% coverage after 25,000 streamlines | Corticospinal tract, corpus callosum |
| Visual Cortex (V1) | 0-15,000 (subject-dependent) | ~70% coverage after 30,000 streamlines | Optic radiation, corpus callosum |
| Dorsolateral Prefrontal Cortex | 9,000-14,000 | ~72% coverage after 22,000 streamlines | Frontal-striatal-thalamic circuit, cingulum bundle |
Table 2: E-Field Modeling Impact on Clinical Outcomes in Depression Studies
| Study Parameter | Standard 5-cm Rule Targeting | MRI-Guided Targeting | E-Field Model Guided |
|---|---|---|---|
| DLPFC E-field Strength | Lowest | Intermediate | Highest and most consistent |
| Inter-subject Variability | Highest | Intermediate | Lowest |
| Correlation with Depression Reduction | Weak (r ~0.3) | Moderate (r ~0.5) | Strong (r ~0.7-0.8) |
| Treatment Response Rate | 20-30% | 30-40% | 45-55% |
Table 3: Computational Methods for E-Field Modeling in TMS
| Numerical Method | Accuracy in Thin Layers | Computational Efficiency | Anisotropy Handling | Implementation Complexity |
|---|---|---|---|---|
| CG-FEM | Moderate | Moderate | Good | Moderate |
| BEM | High | High (with fast multipole) | Poor | High |
| HDG-FEM | Highest | High with hybrid orders | Excellent | High |
Clinical Validation and Therapeutic Impact
The therapeutic potential of precision TMS is most evident in depression treatment. E-field modeling studies reveal that conventional 5-cm rule targeting produces the lowest dorsolateral prefrontal cortex (DLPFC) E-field compared to F3 and MRI-guided targeting, partially explaining negative clinical trial results using this method in adolescents [63]. Higher induced E-field strength in the left DLPFC correlates with greater depression rating scale reductions in both adolescent and adult populations [63].
Network-targeted TMS using functional connectivity between the DLPFC and subgenual anterior cingulate cortex (sgACC) represents another precision approach. Precision network modeling reveals that homotopic scalp positions (F3 vs. F4) target different networks within and across individuals, with right F4 generally favoring a right-lateralized control network [65]. TMS coil positions over the DLPFC zone anticorrelated with the sgACC most frequently target reward circuitry connected to the ventral striatum but miss this network in some individuals, highlighting the need for personalized targeting [65].
Accelerated protocols like the Stanford Neuromodulation Therapy (SNT) protocol combine personalized targeting with intensive stimulation schedules (10 sessions daily over 5 days), achieving remarkable ~80% remission rates in treatment-resistant depression [29] [36]. Meta-regression analyses confirm that both higher pulse numbers and greater total sessions (particularly >20 sessions) with longer inter-session intervals (≥50 minutes) enhance antidepressant effects in accelerated protocols [55].
Experimental Protocols
Protocol 1: Real-Time Tractography-Assisted TMS Neuronavigation
2.1.1 Objective To implement and validate a real-time tractography-assisted TMS neuronavigation system for targeting specific structural connectivity pathways during transcranial magnetic stimulation.
2.1.2 Materials and Equipment
- MRI scanner with multi-shell high-angular resolution diffusion imaging (HARDI) capability
- TMS system with compatible neuronavigation
- Structural T1-weighted MRI sequence
- Diffusion MRI protocol (multi-shell, ≥64 directions)
- Trekker open-source tractography software [61]
- InVesalius neuronavigation platform [61]
- High-performance computing workstation (≥64GB RAM, GPU acceleration)
2.1.3 Preprocessing and Offline Analysis
- Acquire high-resolution structural T1-weighted MRI and multi-shell diffusion-weighted images using appropriate parameters for tractography.
- Perform diffusion data preprocessing: denoising, eddy-current correction, motion correction, and tensor estimation using FSL or similar pipelines.
- Reconstruct whole-brain fiber orientation distributions using spherical deconvolution approaches.
- Identify target region of interest (ROI) for TMS stimulation based on clinical or research objectives.
- Generate seed masks for tractography in target regions using automated or manual segmentation approaches.
2.1.4 Real-Time Tractography Setup
- Integrate Trekker tractography engine with InVesalius neuronavigation system through modular application programming interface.
- Configure real-time tracking of TMS coil position and orientation relative to subject's head.
- Set probabilistic tractography parameters: 0.5-1.0 mm step size, 30-45° maximum curvature, 0.1 minimum fractional anisotropy.
- Implement uncertainty visualization method using ROC-based transfer functions for real-time display [61].
- Establish quantitative output metrics: streamline count, connection probability, and pathway coverage.
2.1.5 Intraoperative Procedure
- Coregister subject with neuronavigation system using facial landmarks.
- Position TMS coil over target ROI based on structural MRI.
- Activate real-time tractography with 5,000-10,000 streamlines initially.
- Adjust coil position and orientation to optimize connectivity with desired network.
- Tune tractography parameters interactively based on initial results.
- Monitor streamline count and overlap metrics until stabilization (typically 15,000-30,000 streamlines).
- Administer TMS stimulation while maintaining optimal coil positioning.
- Document final tractography parameters, streamline counts, and coverage metrics.
2.1.6 Validation and Quality Control
- Compare real-time tractograms with offline gold standard (100 million streamlines)
- Calculate Dice coefficient or Jaccard index for spatial overlap
- Verify anatomical plausibility of reconstructed pathways
- Assess test-retest reliability through repeated measurements
Real-Time Tractography TMS Workflow
Protocol 2: Subject-Specific E-Field Modeling for TMS Dosing
2.2.1 Objective To create subject-specific E-field models for precise TMS dosing and coil placement optimization to maximize target engagement while minimizing off-target stimulation.
2.2.2 Materials and Equipment
- High-resolution T1-weighted and T2-weighted structural MRI
- Optional: Diffusion-weighted imaging for anisotropy modeling
- Finite element method (FEM) or boundary element method (BEM) software (SimNIBS, ROAST, or custom HDG-FEM)
- Validated TMS coil model with ≥3000 distributed current dipoles [63]
- High-performance computing resources for numerical simulation
- Neuronavigation system for coil tracking
2.2.3 Head Model Generation
- Acquire high-resolution (≤1 mm isotropic) T1-weighted and T2-weighted structural MRI.
- Segment head tissues into five compartments: scalp, skull, cerebrospinal fluid (CSF), gray matter, and white matter.
- Assign electrical conductivity values: scalp 0.43 S/m, skull 0.0063 S/m, CSF 1.79 S/m, gray matter 0.33 S/m, white matter 0.14 S/m (isotropic) or tensor from DTI.
- Generate finite element mesh with adaptive refinement for thin tissues (meninges, skull).
- Implement mesh quality control: prevent intersections, ensure adequate element count (>5 million).
2.2.4 Coil Modeling and Positioning
- Select appropriate coil model from validated database of 25 coil types [63].
- Model coil winding with rectangular cross-sections and discrete turns or >3000 distributed current dipoles.
- Position coil model relative to head model using neuronavigation data.
- Define coil current waveform parameters matching clinical TMS system.
2.2.5 E-Field Calculation
- Solve governing equation using numerical method (HDG-FEM recommended for thin layers):
∇⋅(σ(-∇φ-∂A/∂t)) = 0
where σ is conductivity, φ is electric potential, A is magnetic vector potential [63].
- For anisotropic models, incorporate conductivity tensors derived from diffusion MRI.
- Calculate E-field magnitude and direction throughout brain volume.
- Extract summary metrics: maximum, mean, percentile values in target regions.
2.2.6 Optimization and Targeting
- Identify target region based on clinical application (e.g., DLPFC subregion anticorrelated with sgACC for depression).
- Simulate E-field distribution for multiple coil positions and orientations.
- Select optimal configuration maximizing E-field in target while minimizing off-target exposure.
- Export optimal coil parameters to neuronavigation system.
- Validate model predictions with motor threshold measurements when possible.
E-Field Modeling for TMS Dosing
Protocol 3: Precision Network-Targeted TMS for Depression
2.3.1 Objective To implement precision network-targeted TMS for major depressive disorder using functional connectivity-guided targeting combined with accelerated stimulation protocols.
2.3.2 Materials and Equipment
- 3T MRI scanner with resting-state fMRI capability
- TMS system with theta-burst stimulation capability
- Neuronavigation system with functional connectivity targeting software
- Resting-state fMRI processing pipeline (FSL, AFNI, SPM, or CONN)
- Clinical assessment tools for depression (MADRS, HAMD, IDS)
2.3.3 Individualized Target Identification
- Acquire resting-state fMRI: 10-minute eyes-open rest, 2-3 mm isotropic resolution, 300+ volumes.
- Preprocess fMRI data: slice-time correction, motion correction, normalization, smoothing (6mm FWHM).
- Extract subgenual anterior cingulate cortex (sgACC) seed region timecourse.
- Calculate whole-brain functional connectivity with sgACC seed.
- Identify left DLPFC voxels showing strongest negative correlation (anticorrelation) with sgACC.
- Generate target coordinate for TMS stimulation within this anticorrelated DLPFC subregion.
2.3.4 Accelerated Stimulation Protocol
- Implement Stanford Neuromodulation Therapy-inspired protocol:
- 10 sessions daily for 5 consecutive days (50 total sessions)
- 50-minute inter-session intervals
- 1800 pulses per session (90,000 total pulses)
- Intermittent theta-burst stimulation pattern: 3-pulse 50Hz bursts every 200ms
- Alternative: twice-daily high-frequency protocol (10Hz, 3000 pulses/session).
2.3.5 Neuronavigation and Monitoring
- Coregister individualized target with subject's anatomy.
- Navigate TMS coil to target using real-time tracking.
- Maintain consistent coil positioning and angulation across sessions.
- Monitor adverse effects and tolerability throughout treatment.
- Assess clinical response at days 0, 5, 14, 28, and 84.
2.3.6 Outcome Assessment and Optimization
- Primary outcome: remission rate (MADRS ≤ 10 or HAMD-17 ≤ 7).
- Secondary outcomes: response rate (≥50% reduction), depression scale scores.
- Compare outcomes with historical controls using standard targeting.
- Optimize protocol based on individual response patterns.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Resources for Precision TMS Research
| Resource Category | Specific Tools/Solutions | Primary Function | Key Features |
|---|---|---|---|
| Tractography Software | Trekker [61], MRtrix3, FSL XTRACT | White matter pathway reconstruction | Real-time capability, probabilistic methods, ROI-based analysis |
| Neuronavigation Platforms | InVesalius [61], Localite, BrainSight | Coil tracking and target visualization | fMRI integration, real-time tracking, target memory |
| E-Field Modeling Software | SimNIBS [63], ROAST, HDG-FEM [64] | Electric field simulation | FEM/BEM computation, coil modeling, anisotropy support |
| Functional Connectivity Tools | CONN, FSL Nets, DPABI | Resting-state fMRI analysis | Network identification, sgACC-DLPFC anticorrelation mapping |
| Diffusion MRI Processors | FSL FDT, DIPY, DSI Studio | Diffusion data preprocessing | Eddy current correction, tensor estimation, ODF reconstruction |
| Head Model Generators | FreeSurfer, SPM12, FSL BET | Tissue segmentation and mesh creation | Multi-compartment models, conductivity assignment |
| Clinical Outcome Tools | MADRS, HAMD-17, IDS-C | Treatment efficacy assessment | Standardized scales, sensitivity to change, reliability |
Measuring Success: Validating Protocol Efficacy through Neurophysiology and Clinical Outcomes
Transcranial Magnetic Stimulation combined with Electroencephalography (TMS-EEG) represents a transformative approach in clinical neurophysiology for assessing cortical engagement and brain network dynamics. This framework enables the direct measurement of cortical reactivity and connectivity with millisecond temporal precision, providing robust biomarkers for proof-of-mechanism studies in drug development and neuromodulation research [66] [67]. The integration of TMS-evoked potentials (TEPs), motor evoked potentials (MEPs), and functional connectivity measures offers a multi-dimensional assessment of brain states, excitability, and network resilience. For researchers investigating pharmacological interventions or optimization of stimulation protocols, these biomarkers provide sensitive, quantifiable readouts of target engagement and treatment effects [66] [68]. This document outlines standardized application notes and experimental protocols to reliably capture and interpret these biomarkers within translational research settings.
Quantitative Biomarkers of Cortical Engagement
The following tables summarize key quantitative biomarkers derived from TMS-EEG and TMS-EMG paradigms, their physiological significance, and representative drug effects.
Table 1: Core TMS-EMG and TMS-EEG Biomarkers of Cortical Excitability
| Biomarker | Description | Physiological Significance | Measurement Parameters |
|---|---|---|---|
| Motor Evoked Potential (MEP) | Muscle response from motor cortex TMS [67] | Corticospinal excitability index [66] | Peak-to-peak amplitude (μV) [66] |
| Short-Intracortical Inhibition (SICI) | Paired-pulse inhibition at 2-5 ms intervals [67] | GABAA receptor-mediated inhibition [67] | Ratio of conditioned/unconditioned MEP [66] |
| Long-Intracortical Inhibition (LICI) | Paired-pulse inhibition at 50-200 ms intervals [67] | GABAB receptor-mediated inhibition [66] | Ratio of conditioned/unconditioned MEP [66] |
| TMS-Evoked Potential (TEP) | EEG response to cortical TMS perturbation [67] | Cortical reactivity and effective connectivity [67] | Component amplitude (N45, N100) & latency [66] |
Table 2: Pharmacodynamic Effects on TMS Biomarkers (Adapted from a Placebo-Controlled Cross-Over Study) [66]
| Pharmacological Agent | Mechanism of Action | Effect on MEP Amplitude (Estimated Difference vs. Placebo) | Effect on LICI (50-ms ISI) | Key TEP Findings |
|---|---|---|---|---|
| Levetiracetam (2000 mg) | SV2A modulator | −378.4 μV (95% CI: −644.3, −112.5; P < .01) | Enhanced (−60.3%; P < .001) | ↑ N45 amplitude; ↓ N100 amplitude [66] |
| Valproic Acid (1000 mg) | GABA enhancer / Na+ channel blocker | −268.8 μV (95% CI: −532.9, −4.6; P = .047) | Not significant | Not reported in source |
| Lorazepam (2 mg) | GABAA positive allosteric modulator | −330.7 μV (95% CI: −595.6, −65.8; P = .02) | Enhanced (−68.2%; P < .001) | Not reported in source |
Experimental Protocols
Protocol 1: Pharmaco-TMS-EEG for Proof-of-Mechanism Studies
This protocol is designed to characterize the pharmacodynamic effects of central nervous system (CNS) active compounds on cortical excitability and connectivity in humans [66].
1. Study Design:
- Implement a randomized, double-blind, placebo-controlled, cross-over design.
- Utilize a Williams design to balance first-order carry-over effects.
- Include at least 16 subjects to achieve sufficient statistical power.
2. Subject Selection:
- Recruit healthy male subjects (18-45 years) to control for hormonal fluctuations.
- Exclude subjects with contraindications to TMS, abnormal sleeping patterns, illicit drug use, or resting motor threshold (rMT) >83% of maximum stimulator output (MSO) [66].
3. Dosing and Timing:
- Administer single oral doses within the therapeutic range.
- Perform TMS-EMG-EEG measurements at baseline (pre-dose) and at 1.5, 7, and 24 hours post-dose to capture pharmacokinetic and pharmacodynamic profiles [66].
4. TMS-EEG Data Acquisition:
- Use a MagPro R30 stimulator with a MCF-B65 butterfly coil or equivalent.
- Employ neuronavigation to ensure consistent coil positioning across sessions. Real-time electric-field modeling is crucial for precision and reproducibility [69].
- Determine the resting motor threshold (rMT) for the dominant abductor digiti minimi muscle.
- Apply 50 single pulses at 120% rMT.
- Apply 50 paired pulses at various interstimulus intervals (ISIs: 2, 5, 50, 100, 150, 200, 250, 300 ms) in randomized order. Use 80% rMT for conditioning pulses at short ISIs (2, 5 ms) [66].
- Maintain an inter-trial interval of ≥3 seconds to avoid carry-over effects.
- Implement auditory masking with noise specifically designed to mask the coil click (e.g., using TMS-Adaptable Auditory Control software) to minimize confounding auditory evoked potentials [69].
5. Data Analysis:
- MEP Analysis: Calculate peak-to-peak amplitudes for single pulses. Analyze paired-pulse data as the ratio of conditioned to unconditioned MEP amplitude.
- TEP Analysis: Preprocess EEG data to remove artifacts. Calculate average TEPs and identify key components (e.g., N45, N100). Use cluster-based permutation analysis for robust statistical comparison of TEP waveforms [66].
- Statistical Modeling: Employ mixed-model ANCOVA to analyze treatment effects on MEP amplitudes and inhibition/facilitation ratios, adjusting for baseline values and subject effects [66].
Protocol 2: State-Dependent and Closed-Loop TMS-EEG
This protocol leverages real-time EEG to synchronize TMS pulses with specific brain states, probing dynamic brain network properties and reducing measurement variability [67].
1. System Setup:
- Integrate a TMS-compatible EEG system with real-time processing capabilities.
- Use a neuronavigation system co-registered with the participant's structural MRI (or fMRI data) for precise and repeatable targeting [67] [69].
2. Real-Time EEG Feature Extraction:
- Program the system to compute specific features from the ongoing EEG signal. Common features include:
- Instantaneous Phase: Of oscillations in a pre-defined frequency band (e.g., alpha: 8-12 Hz).
- Power: In a specific frequency band.
- Connectivity: A simple measure of functional connectivity between two regions.
3. Closed-Loop Stimulation Triggering:
- Define a trigger threshold for the selected EEG feature.
- Example 1 (Phase-Locked): Configure the system to automatically deliver a TMS pulse when the instantaneous phase of the posterior alpha rhythm crosses a specific value (e.g., 0° for the peak) [67].
- Example 2 (Power-Dependent): Trigger TMS when the power in the frontal theta band falls below a certain threshold.
4. Data Collection:
- For each experimental condition (e.g., different phase bins or power states), deliver a sufficient number of pulses (typically >100) to obtain a reliable average TEP.
- Include a resting-state, open-loop TMS-EEG session as a control.
5. Data Analysis:
- Sort and average TEPs based on the pre-trigger EEG feature (e.g., phase bin).
- Compare early TEP components (0-50 ms) and TMS-induced oscillatory power across different brain states to quantify state-dependent cortical reactivity [67].
Diagram 1: Closed-loop TMS-EEG workflow.
The Scientist's Toolkit: Essential Research Reagents & Equipment
Table 3: Essential Materials and Equipment for TMS-EEG Studies
| Item | Function/Application | Key Specifications |
|---|---|---|
| Navigated TMS System [69] | Precise coil placement and E-field modeling for reproducible stimulation. | Integrated optical tracking, electric-field neuronavigation, compatibility with structural/fMRI data. |
| TMS-Compatible EEG System [67] | Recording TMS-evoked potentials with minimal artifact. | High sampling rate (≥5 kHz), actively discharging electrodes, specialized amplifiers. |
| Auditory Masking System [69] | Eliminates confounding auditory evoked potentials from coil click. | Customized noise-masking generator (e.g., TAAC software), insert earphones. |
| Pharmacological Agents [66] | Positive controls for validating biomarker sensitivity (e.g., GABAergic modulation). | Levetiracetam (2000 mg), Lorazepam (2 mg), Valproic Acid (1000 mg). |
| Real-Time TEP Visualization Tool [69] | Online feedback for optimizing coil placement and stimulation parameters. | rt-TEP tool or equivalent custom software. |
Signaling Pathways and Neurophysiological Basis
The biomarkers discussed are grounded in specific neurochemical pathways and circuit mechanisms. Pharmacological studies have been instrumental in elucidating these relationships.
- GABAergic Inhibition: The enhancement of LICI by lorazepam and levetiracetam strongly implicates GABAA and GABAB receptor-mediated inhibition in this biomarker [66]. LICI is considered a marker of GABAB receptor activity, while SICI is linked to GABAA receptor function [67].
- Glutamatergic Excitation: Early TEP components (e.g., P30, N45) are thought to reflect glutamatergic, NMDA receptor-mediated excitatory postsynaptic potentials. The modulation of the N45 component by levetiracetam suggests an interaction with synaptic release mechanisms, consistent with its binding to synaptic vesicle glycoprotein 2A (SV2A) [66].
- Cortical Inhibition and the N100: The N100 TEP component is a robust, long-latency negative deflection. Its reduction by GABAergic drugs like levetiracetam indicates it is a marker of widespread, long-range cortical inhibition, potentially involving GABAB receptor-mediated mechanisms [66] [68].
Diagram 2: Proposed neurophysiological pathways for TMS biomarkers.
Within transcranial magnetic stimulation (TMS) research, protocol optimization represents a critical pathway for enhancing treatment efficacy and efficiency. The emergence of targeted beamFMM protocols, which utilize advanced targeting and parameter refinement, promises to overcome limitations of standard approaches. This application note synthesizes evidence from randomized controlled trials (RCTs) and network meta-analyses to evaluate the comparative efficacy of these protocol classes, providing detailed methodologies and data to guide research and development.
Quantitative Efficacy Comparison of TMS Protocols
Table 1: Comparative Efficacy of Different TMS Protocols Across Conditions
| Condition | Protocol Type | Specific Protocol | Key Efficacy Findings | Evidence Certainty |
|---|---|---|---|---|
| Fibromyalgia [70] | Standard HF-rTMS | HF-rTMS over M1 | SMD: -0.58 (-1.00 to -0.17) for pain reduction | Moderate |
| Targeted Inhibitory | LF-rTMS over right DLPFC | SMD: -1.20 (-1.82 to -0.58) for pain reduction; effects maintained short-term | High | |
| Major Depressive Disorder [71] | Standard Protocol | Standard bilateral rTMS | Clinically significant benefits over medication | Moderate |
| Optimized Protocol | Priming TMS | Greater response rates vs. continuous TBS; lower attrition vs. sham | Moderate | |
| Accelerated Protocol | Accelerated iTBS (SNT) | Superior to sham; more effective than intranasal esketamine in one study | High | |
| Early Stroke Motor Recovery [72] | Standard Protocol | Unilateral HF-rTMS | Effective for upper extremity function | Moderate |
| Targeted Protocol | Bilateral HF/LF-rTMS (BL-rTMS) | Best for upper extremity function (SUCRA: 92.8%) and ADL (SUCRA: 100%) | High | |
| Substance Use Disorders [73] | Standard Protocol | Multiple rTMS sessions to left DLPFC | Medium to large effect sizes (Hedge's g > 0.5) for reducing craving/use | Moderate |
Abbreviations: SMD: Standardized Mean Difference; SUCRA: Surface Under the Cumulative Ranking Curve; HF: High Frequency; LF: Low Frequency; rTMS: repetitive TMS; TBS: Theta Burst Stimulation; DLPFC: Dorsolateral Prefrontal Cortex; M1: Primary Motor Cortex; SNT: Stanford Neuromodulation Therapy; ADL: Activities of Daily Living.
Detailed Experimental Protocols
Targeted Low-Frequency Protocol for Fibromyalgia Pain
This protocol, derived from network meta-analysis findings, applies inhibitory stimulation to the right dorsolateral prefrontal cortex (DLPFC) for chronic pain conditions [70].
- Patient Population: Adults with fibromyalgia diagnosed according to established criteria (e.g., ACR 2016). Participants should have stable medication regimens.
- Stimulation Parameters:
- Frequency: Low-frequency (1 Hz)
- Target: Right DLPFC (localized via EEG 10-20 system at position F4)
- Intensity: 90% of resting motor threshold (RMT)
- Pulses per Session: 1200 pulses
- Session Duration: 20 minutes
- Treatment Course: Daily sessions for 5 consecutive days, with assessment of short-term maintenance at 4-week follow-up.
- Equipment Setup:
- TMS device with a cooled figure-8 coil.
- Neuronavigation system is recommended for precise, consistent targeting.
- Outcome Measures:
- Primary: Pain intensity measured by Visual Analog Scale (VAS) or Numerical Pain Rating Scale (NPRS) at baseline, post-intervention, and 1-month follow-up.
- Secondary: Fibromyalgia Impact Questionnaire (FIQ), fatigue scales, and sleep quality diaries.
- Blinding: Use a sham coil with acoustic masking for the control group.
Bilateral rTMS (BL-rTMS) Protocol for Motor Recovery in Early Stroke
This protocol outlines the application of combined high- and low-frequency rTMS to both hemispheres, identified as the most effective approach for improving motor function and activities of daily living (ADL) in early stroke patients [72].
- Patient Population: Patients within 3 months of a first-ever ischemic or hemorrhagic stroke, with unilateral motor deficits.
- Stimulation Parameters:
- Hemisphere 1 (Lesioned): High-frequency (10 Hz) stimulation over the primary motor cortex (M1) hand area.
- Hemisphere 2 (Non-lesioned): Low-frequency (1 Hz) stimulation over the contralateral M1 hand area.
- Intensity: 90% of RMT for the HF-rTMS; 110% of RMT for the LF-rTMS.
- Pulses: 1000 pulses per hemisphere per session.
- Treatment Course: 5 sessions per week for 3 weeks. Assess outcomes at end of treatment and at 3-month follow-up.
- Equipment Setup:
- TMS device with a figure-8 coil.
- EMG system for monitoring motor evoked potentials (MEPs) and ensuring accurate motor hotspot localization.
- Outcome Measures:
- Primary: Fugl-Meyer Assessment for Upper Extremity (FMA-UE).
- Secondary: Action Research Arm Test (ARAT), Barthel Index (BI) for ADL, and National Institutes of Health Stroke Scale (NIHSS).
- Safety Monitoring: Continuous observation for adverse events, particularly seizures. Document any incidences of headache or neck pain.
Pragmatic Trial Design for Comparative Effectiveness Research
This framework is essential for evaluating TMS protocols in real-world settings, thereby enhancing the generalizability of findings [74].
- Study Design: Pragmatic randomized controlled trial (RCT), which emphasizes effectiveness in routine practice over efficacy in ideal conditions.
- Key Design Features:
- Participant Recruitment: Conducted within ongoing clinical practice settings with broad, inclusive eligibility criteria to reflect the typical patient population [74].
- Intervention Flexibility: Allow clinicians to make minor, clinically justified adjustments to the TMS protocol (e.g., slight intensity adjustments) to accommodate individual patient tolerability, mirroring real-world application [74].
- Comparator: Active control (e.g., validated sham TMS) or standard of care TMS protocol.
- Outcome Measures: Select clinically relevant endpoints that matter to patients and clinicians, such as return-to-work rates, quality of life measures, or reduction in analgesic use, in addition to standard symptom scales. Data should be collected during routine clinical appointments to minimize patient burden [74].
- Follow-up: Include long-term follow-up periods (e.g., 6 and 12 months) to assess the durability of treatment effects, which is critical for clinical decision-making [74].
Logical Workflow for Protocol Selection and Evaluation
Figure 1: A systematic workflow for selecting and evaluating TMS protocols in research and clinical practice, emphasizing iterative optimization based on patient outcomes and emerging evidence.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for TMS Research
| Item Name | Specification / Model Example | Primary Function in Research |
|---|---|---|
| Figure-8 Coil | Cooled, solid-core design | Standard focal stimulation for cortical targets like M1 and DLPFC. |
| H-Coil (Deep TMS) | H1 or H7 helmet coil | Deeper and broader field stimulation; FDA-cleared for certain MDD and smoking cessation protocols [73]. |
| Neuronavigation System | Brainsight, Localite | Integrates with individual MRI to provide real-time, precise coil positioning over target anatomy. |
| Sham Coil | Placebo coil with acoustic masking | Mimics sound and scalp sensation of active TMS for blinding in controlled trials. |
| Resting Motor Threshold (RMT) Kit | EMG system, surface electrodes | Determines individual stimulus intensity by measuring minimal intensity to elicit MEP in target muscle. |
| Theta Burst Stimulation (TBS) Software | cTBS, iTBS protocols | Enables patterned stimulation protocols (e.g., 3-minute iTBS) that mimic endogenous rhythms [71] [73]. |
| Electroencephalography (EEG) | Synchronized TMS-EEG cap | Measures neurophysiological effects of stimulation and can be used for personalized protocol timing [71]. |
| Clinical Outcome Scales | HDRS (depression), NPRS (pain), FMA (motor) | Validated tools for quantifying treatment efficacy across different disorders. |
The evidence from recent RCTs and meta-analyses strongly indicates that targeted TMS protocols, which incorporate precise neuroanatomical targeting, optimized parameter selection, and sometimes accelerated dosing, consistently demonstrate superior efficacy compared to standard protocols. The continued refinement of these protocols through rigorous comparative effectiveness research, including pragmatic trial designs, is paramount for advancing the field of neuromodulation and delivering improved patient outcomes.
Transcranial Magnetic Stimulation (TMS) has emerged as a pivotal non-invasive neuromodulation technique for various psychiatric and neurological disorders. However, its clinical application is hampered by significant interindividual variability in treatment response, largely attributable to non-optimized, universal stimulation protocols [75]. The principle of protocol optimization—systematically tailoring stimulation parameters, target engagement, and treatment personalization—is fundamental to advancing TMS from a generically applied intervention to a precision medicine tool. This application note examines protocol optimization strategies across three distinct clinical domains: depression, substance use disorders (SUDs), and post-stroke cognitive impairment (PSCI). By synthesizing current evidence and methodologies, we provide a framework for researchers and drug development professionals to enhance TMS efficacy through rigorous optimization approaches, ultimately improving therapeutic outcomes and accelerating the development of next-generation neuromodulation therapies.
Depression: Optimizing Community-Based and Clinical Management Pathways
Major Depressive Disorder (MDD) represents one of the most established indications for TMS therapy, yet optimization extends beyond stimulation parameters to encompass broader treatment pathways and community engagement strategies.
Community-Based Intervention Optimization Using Factorial Design
A novel approach to optimizing community-based depression care employs the Multiphase Optimization Strategy (MOST) framework, utilizing a 2 × 3 factorial randomized controlled trial design to identify active intervention components [76]. This methodology systematically evaluates individual intervention elements to determine their specific contributions to overall efficacy, thereby streamlining interventions for maximum efficiency and scalability.
Table 1: Components of the Gain-Life Intervention for Depression Help-Seeking
| Component | Description | Targeted Barrier |
|---|---|---|
| Depression Information | Psychoeducation about depression symptoms and nature | Poor mental health literacy |
| Service Awareness | Information about available treatment services | Lack of knowledge about resources |
| Stigma Reduction | Dispelling myths and facts about depression | Internalized and social stigma |
| Life Transformation Story | Personal recovery narrative from someone with lived experience | Negative attitudes toward treatment |
The optimization trial conducted in Nepal focuses on improving help-seeking behavior—a critical barrier in low- and middle-income countries where 77% of individuals with mental health conditions receive no treatment [76]. The primary outcome measure is the percentage of people seeking care from a healthcare provider within one month of receiving intervention components, with secondary outcomes including treatment adherence and reduction in depression symptom severity.
Clinical Management Optimization Through Implementation Strategies
Comparative effectiveness research examines implementation strategies for optimizing depression treatment within integrated care settings. A randomized controlled trial comparing system-level strategies (enhanced usual care focusing on staff and behavioral health provider activation) versus multi-level strategies (adding primary care provider behavioral support and patient activation tools) found that system-level strategies alone demonstrated significant pre-post improvement in patient optimization (30.4% to 44.9%, p=0.001), while multi-level strategies showed no additional benefit [77].
Table 2: Depression Treatment Optimization Outcomes in Integrated Care Settings
| Strategy Component | Optimization Outcome | Statistical Significance |
|---|---|---|
| System-Level Strategy (EUC) | Increased patient optimization from 30.4% to 44.9% | p = 0.001 |
| Multi-Level Strategy (Intervention) | Increased patient optimization from 30.0% to 39.1% | p = 0.10 (non-significant) |
| Comparison Between Strategies | No significant advantage for multi-level approach | OR = 0.78; 95% CI: 0.50-1.22, p = 0.27 |
This finding challenges conventional implementation wisdom that more intensive, multi-level strategies are inherently superior, suggesting instead that foundational system-level enhancements may provide the most efficient path to treatment optimization in mature integrated care settings [77].
Diagram 1: MOST Framework for Intervention Optimization
Substance Use Disorders: Endpoint and Measurement Optimization
The therapeutic development landscape for Substance Use Disorders is undergoing a paradigm shift from abstinence-based endpoints toward reduced-use outcomes that better reflect the chronic nature of addiction and patient-centered recovery trajectories.
Endpoint Optimization in Clinical Trials
The National Institute on Drug Abuse (NIDA) and FDA have recognized the clinical value of reduced substance use as a meaningful endpoint in clinical trials, moving beyond the traditional high bar of complete abstinence [78]. This optimization acknowledges that reduction in use provides substantial public health benefits, including decreased overdoses, reduced infectious disease transmission, and lower healthcare utilization.
Evidence supporting this optimized endpoint includes:
- Cocaine Use Disorder: Achieving ≥75% cocaine-negative urine screens associates with significant improvements in psychosocial functioning and addiction severity measures [78].
- Cannabis Use Disorder: Reductions short of abstinence (50% reduction in use days, 75% reduction in amount used) correlate with meaningful improvements in sleep quality and cannabis use disorder symptoms [78].
- Stimulant Use Disorders: Reduced use associates with improvement in depression severity, craving, and multiple domains of functioning in analyses across 13 clinical trials [78].
This endpoint optimization potentially expands therapeutic interventions, reduces stigma associated with return to use, and may increase treatment engagement by offering more achievable initial goals [78].
Management Protocol Optimization in Inpatient Settings
A scoping review of substance use management on psychiatric units identified seven recurring intervention domains for protocol optimization, with structured screening demonstrating up to two-fold improvement in detection rates and brief interventions reducing 30-day readmissions by up to 18% [79]. These optimized protocols emphasize patient-centered approaches over purely punitive security measures, which show inconsistent effects on contraband entry or aggression.
Table 3: Substance Use Management Strategies in Psychiatric Inpatient Settings
| Intervention Domain | Key Components | Reported Outcomes |
|---|---|---|
| Systematic Screening | Urine toxicology, standardized questionnaires | Up to 2-fold improvement in detection rates |
| Brief Interventions | SBIRT, BIMI | Increased post-discharge engagement, 18% reduction in 30-day readmissions |
| Policy/Protocol Development | Clear patient-centered policies, consistent response protocols | Improved staff consistency, reduced arbitrary enforcement |
| Harm Reduction Strategies | Nicotine replacement, take-home naloxone | Reduced acute harms, bridging to community care |
| Staff Training & Culture Change | De-stigmatizing education, trauma-informed care | Improved therapeutic alliance, earlier intervention |
Post-Stroke Cognitive Impairment: Therapeutic Protocol Optimization
Post-stroke cognitive impairment affects 30-70% of stroke survivors, with approximately 30% experiencing persistent deficits years after onset [80]. Optimization of cognitive rehabilitation protocols is therefore crucial for improving functional outcomes and quality of life.
Comparative Efficacy of Digital Interventions
A network meta-analysis of 27 randomized controlled trials evaluated digital interventions for PSCI, revealing domain-specific efficacy patterns that can guide intervention selection and optimization [81].
Table 4: Digital Interventions for Post-Stroke Cognitive Impairment
| Intervention | MoCA Performance (Executive Focus) | MMSE Performance (Global Cognition) | Domain-Specific Strengths |
|---|---|---|---|
| Computer-Assisted Cognitive Therapy (CACT) | MD=3.03, 95% CI: 1.69-4.38; SUCRA=91.53% | Moderate efficacy | Executive function, memory, processing speed |
| Robot-Assisted Therapy (RAT) | Lower efficacy | MD=5.99, 95% CI: 3.20-8.79; SUCRA=99.44% | Basic cognitive activities, engagement |
| Virtual Reality (VR) | Moderate efficacy | No significant improvement | Visuospatial and executive functions, ecological validity |
| Conventional Cognitive Training (CCT) | No significant improvement | No significant improvement | Traditional approach, limited efficacy |
The analysis demonstrates that optimal intervention selection depends on the targeted cognitive domain, with CACT showing superiority for executive functions measured by MoCA, while RAT demonstrates the highest efficacy for global cognition measured by MMSE [81]. This evidence supports a personalized, domain-specific approach to PSCI rehabilitation protocol optimization.
Brain Stimulation Optimization for Cognitive Recovery
Beyond digital interventions, brain stimulation approaches show significant promise for PSCI. Systematic review evidence indicates that transcranial direct current stimulation (tDCS) produces substantial cognitive benefits (MD 4.56, 95% CI: 3.19-5.93 on MoCA), with early initiation (within 3 months post-stroke) proving most effective [80]. Pharmacological interventions also demonstrate robust effects (MD 4.00, 95% CI: 3.48-4.52), while acupuncture shows potential albeit with considerable variability (MD 2.65, 95% CI: 1.07-4.23) [80].
Diagram 2: PSCI Intervention Selection Algorithm
TMS Protocol Optimization: Targeting and Engagement Strategies
The efficacy of TMS is critically dependent on anatomical precision of brain target engagement and understanding of the neurophysiological response of stimulated circuits [82]. Current optimization strategies focus on overcoming the limitations of standardized "one target for all" approaches.
Personalized Targeting Techniques
Precise targeting is essential because adjacent cortical areas may have completely different connectivity patterns. For example, the pre-supplementary motor area (pre-SMA) and supplementary motor area (SMA)—both within Brodmann's area 6—demonstrate distinct structural connectomes and electrophysiological signatures [82]. Optimization approaches include:
- Real-Time Tractography: Visualization of structural connections during stimulation to ensure reliability of target engagement [82].
- TMS-EEG Integration: Combined with high-density EEG to characterize the neurophysiological signature of the stimulated area [82].
- Electric Field Modeling: Computational approaches to optimize coil placement and electric field distribution [83].
- Multi-Locus TMS (mTMS): Simultaneous targeting of multiple brain networks with navigated systems [82].
Parameter Optimization Framework
TMS parameter optimization encompasses multiple modifiable elements that collectively influence treatment efficacy:
- Stimulation Pattern Selection: Choice between single-pulse, paired-pulse, repetitive TMS (rTMS), theta burst stimulation (TBS), quadripulse stimulation (QPS), and paired-associative stimulation (PAS) [75].
- Frequency and Intensity Titration: Individualized dosing based on neurophysiological biomarkers rather than fixed parameters [75].
- Coil Selection and Orientation: Impact on electric field distribution and cortical activation [75].
- Target Localization: From gross anatomical landmarks to personalized network engagement based on individual functional connectivity [83].
The development of automated optimization algorithms, such as the Targeted Functional Network Stimulation (TANS) approach, represents a significant advancement by systematically personalizing coil placement to maximize engagement of specific functional networks [83].
The Scientist's Toolkit: Research Reagent Solutions
Table 5: Essential Resources for Neuromodulation Protocol Optimization Research
| Resource Category | Specific Tools/Measures | Research Application |
|---|---|---|
| Optimization Frameworks | Multiphase Optimization Strategy (MOST), Factorial Design | Efficient intervention development and component testing |
| Clinical Outcome Measures | PHQ-9, MoCA, MMSE, Urine Drug Screens, Help-Seeking Behavior | Standardized assessment of intervention efficacy |
| Neurophysiological Tools | TMS-EEG, hd-EEG, Motor Evoked Potentials (MEP) | Target engagement verification and mechanism investigation |
| Neuroimaging Platforms | dMRI Tractography, fMRI, Real-Time Navigation | Personalized targeting and connectivity analysis |
| Digital Intervention Systems | CACT, VR, RAT Platforms | Domain-specific cognitive rehabilitation |
| Stimulation Protocols | rTMS, TBS, QPS, PAS Protocols | Investigation of different neuromodulation approaches |
| Implementation Metrics | RE-AIM Framework, Fidelity Measures | Translation and scalability assessment |
Protocol optimization across depression, substance use disorders, and post-stroke cognitive impairment demonstrates the critical importance of moving beyond universal intervention approaches toward personalized strategies that account for individual differences in neurobiology, clinical characteristics, and treatment goals. The evolving paradigm emphasizes: (1) component-level intervention testing to identify active ingredients; (2) endpoint selection that reflects meaningful clinical improvement rather than idealized outcomes; (3) domain-specific rehabilitation matching; and (4) precision targeting of brain circuits based on individual neurobiology. For researchers and drug development professionals, these optimization frameworks provide methodological roadmaps for developing more effective, efficient, and personalized neuromodulation protocols that maximize therapeutic outcomes while accelerating the translation of neuroscience discoveries into clinical practice. Future directions should focus on integrating multimodal data streams to develop predictive optimization models and establishing standardized frameworks for validating target engagement across different disorder-specific circuits.
This application note provides a structured framework for defining and measuring success in transcranial magnetic stimulation (TMS) research, specifically linking clinical remission benchmarks with functional connectivity changes. As the field moves toward personalized neuromodulation, establishing clear, quantitative correlations between behavioral outcomes and neurophysiological changes is paramount for protocol optimization [17] [84]. This document outlines standardized metrics, experimental methodologies, and analytical tools to advance reproducible research in TMS for neurological and psychiatric disorders.
The foundational premise is that effective TMS protocols produce measurable and predictable changes in both clinical symptoms and brain network dynamics. Recent evidence indicates that TMS-induced changes in functional connectivity, particularly following protocols like intermittent theta-burst stimulation (iTBS), can systematically predict treatment outcomes [84]. This note synthesizes current findings to offer actionable protocols for researchers aiming to validate and optimize TMS parameters.
Quantitative Benchmarks for Clinical Remission
Clinical remission is defined by a sustained reduction in symptom-specific scales to within a predefined normative range. The benchmarks vary significantly by disorder, and the chosen scale must be validated for the target population. The following table consolidates key clinical remission benchmarks for conditions commonly treated with TMS.
Table 1: Clinical Remission Benchmarks in TMS Research
| Disorder | Primary Assessment Scale | Remission Benchmark Definition | Corresponding Functional Connectivity Target |
|---|---|---|---|
| Major Depressive Disorder | Hamilton Depression Rating Scale (HAMD) | Score ≤ 7 [84] | Increased connectivity between left dorsolateral prefrontal cortex (dlPFC) and subgenual Anterior Cingulate Cortex (sgACC) [84] |
| Motor Recovery Post-Stroke | Fugl-Meyer Assessment (Upper Extremity) | Score increase ≥ 4.5-6.2 points [85] | Restoration of inter-hemispheric balance; increased connectivity within the ipsilesional motor network [85] |
| Chronic Pain | Visual Analog Scale (VAS) | Score reduction ≥ 50% from baseline [86] | Modulation of connectivity between dlPFC and descending pain modulatory pathways [86] |
| Alzheimer's Disease | Alzheimer's Disease Assessment Scale-Cognitive (ADAS-Cog) | Score change not uniformly defined; stabilization or improvement is key. | Improvement in short-latency afferent inhibition, a TMS-EEG metric of central cholinergic transmission [86] |
Defining Functional Connectivity Changes
Functional connectivity (FC) refers to the temporal correlation of neural activity signals between different brain regions. TMS is understood to induce plastic changes that alter these functional networks. The benchmarks below define the magnitude and direction of FC changes that are indicative of successful intervention.
Table 2: Benchmarks for Functional Connectivity Changes via rs-fMRI
| FC Metric | Measurement Method | Benchmark for Successful Change | Associated Clinical Outcome |
|---|---|---|---|
| dlPFC-sgACC Connectivity | Resting-state fMRI (rs-fMRI) | Significant increase in correlation strength post-iTBS [84] | Rapid remission of depression symptoms [84] |
| Inter-Hemispheric Motor Cortex Connectivity | rs-fMRI or TMS with Electromyography | Reduction of excessive inhibition from contralesional to ipsilesional hemisphere [86] [85] | Improvement in hand function and motor recovery post-stroke [85] |
| Cortical Excitability (Inhibition) | TMS Short-Interval Intracortical Inhibition (SICI) | Normalization of reduced SICI, indicating restored GABAergic function [86] | Diagnostic utility and potential symptom improvement in ALS and movement disorders [86] |
| Cortical Excitability (Facilitation) | TMS Intracortical Facilitation (ICF) | Normalization of altered ICF [86] | Diagnostic aid in neurodegenerative and psychiatric diseases [86] |
| Effective Connectivity | TMS-Electroencephalography (TMS-EEG) | Alterations in TMS-evoked potential (TEP) amplitude and complexity [86] | Measure of neuroplastic changes and network-level effects of TMS [86] |
Experimental Protocols for Correlation Analysis
Protocol 1: Pre-Post iTBS for Depression with rs-fMRI
This protocol is designed to characterize the plasticity-induced changes in functional connectivity following an accelerated iTBS intervention.
- Aim: To quantify changes in whole-brain functional connectivity following neuronavigated iTBS to the left dlPFC and correlate these changes with clinical remission.
- Patient Population: Adults with Major Depressive Disorder or Persistent Depressive Disorder [84].
- Intervention Protocol:
- Stimulation Target: Left dlPFC.
- Protocol: Intermittent TBS (iTBS).
- Parameters: 70% of Resting Motor Threshold (RMT); 2400 pulses per day delivered in forty 10-second trains (2s stimulation, 8s inter-train interval) [84].
- Treatment Duration: 3 consecutive days.
- Clinical Outcome Measures: Administered at baseline and post-intervention (e.g., day after last session). HAMD is the primary metric for defining clinical remission (benchmark: score ≤7) [84].
- Neurophysiological Outcome Measures:
- rs-fMRI Acquisition: Collected within 1-4 days before the first intervention and on the day after the last intervention.
- Analysis: Construct correlation matrices from cleaned rs-fMRI data. Electric-field (E-field) models of the TMS pulse are conducted and used to predict pre-post changes in rs-fMRI connectivity, particularly between the dlPFC and sgACC [84].
- Key Correlation Analysis: Perform regression analysis to test if the E-field model-predicted connectivity changes significantly correlate with the actual change in HAMD scores.
Protocol 2: TMS for Motor Recovery Post-Stroke
This protocol outlines a method for assessing the efficacy of different iTBS dosing strategies on motor recovery.
- Aim: To determine the most effective iTBS modality for improving hand function in chronic stroke survivors by assessing motor function and cortical connectivity/excitability.
- Patient Population: Adults >21 years old, >6 months post-first stroke with confirmed hand muscle weakness [85].
- Intervention Protocol (Crossover Design):
- All participants undergo three iTBS modalities in a randomized order:
- Focal conventional iTBS (FiTBS600): 600 pulses over a single spot on the ipsilesional motor cortex.
- Focal high-dose iTBS (FiTBS2400): 2400 pulses (4 bouts of 600 pulses) over a single spot.
- Diffuse high-dose iTBS (DiTBS2400): 2400 pulses distributed over 4 spots (600 pulses/spot) on the ipsilesional motor cortex [85].
- All participants undergo three iTBS modalities in a randomized order:
- Clinical Outcome Measures: Fugl-Meyer Assessment (Upper Extremity) is a key metric. An increase of 4.5-6.2 points is considered clinically significant [85].
- Neurophysiological Outcome Measures:
- Resting Motor Threshold (RMT): Measured from the affected hand muscle at baseline and follow-up to assess changes in cortical excitability [85].
- Neuroimaging: Optional rs-fMRI to assess changes in motor network connectivity.
- Key Correlation Analysis: Compare the efficacy of the three iTBS modalities. Correlate the integrity of transcallosal motor fibers (via diffusion MRI) with motor improvement to understand patient-specific response factors [85].
Visualizing the Research Workflow
The following diagram illustrates the integrated workflow for correlating clinical and functional connectivity outcomes in a TMS study.
Integrated TMS Research Workflow
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and tools required for executing the protocols described in this note.
Table 3: Essential Research Materials and Tools
| Item Name | Function/Application | Specification Notes |
|---|---|---|
| TMS Stimulator & Coil | Delivers precise magnetic pulses for neuromodulation. | Magventure MagPro X100 with a B65 figure-8 coil is cited for iTBS studies [84]. Neuronavigation compatibility is critical. |
| MRI-Compatible TMS Equipment | Allows for concurrent TMS-fMRI or anatomical targeting. | Required for neuronavigation and electric-field modeling. Specific components for safe use within the MRI environment are needed [84]. |
| Neuronavigation System | Co-registers subject anatomy with TMS coil for precise, individualized targeting. | Uses individual structural MRI scans to ensure accurate and reproducible stimulation of targets like the dlPFC [84]. |
| Electromyography (EMG) System | Records motor evoked potentials (MEPs) for measuring cortical excitability. | Used to determine Resting Motor Threshold (RMT) by recording from target muscles (e.g., abductor pollicis brevis) [86] [84]. |
| Electroencephalography (EEG) System | Records direct cortical responses to TMS pulses. | TMS-EEG combines are used to measure cortical excitability, effective connectivity, and response complexity without bias from spinal/peripheral circuits [86]. |
| Electric Field (E-Field) Modeling Software | Computes the simulated distribution of electrical energy from TMS in individual brains. | Used to model the TMS-induced electric field and predict changes in functional connectivity, helping to optimize targeting [84]. |
| Structured Clinical Interview (SCID-V) | Standardizes patient diagnosis to ensure a homogeneous research cohort. | Used for confirming primary diagnosis of Major Depressive Disorder and ruling out specific exclusions [84]. |
Conclusion
The optimization of TMS protocols is undergoing a paradigm shift from a one-size-fits-all approach to a precision medicine framework. The integration of individualized neuroimaging, electric-field modeling, and AI is paramount for achieving reliable target engagement and improving clinical outcomes across diverse neuropsychiatric conditions. Future directions must focus on the development of closed-loop TMS systems that use real-time neurophysiological feedback to dynamically adjust stimulation parameters, the validation of robust biomarkers for patient stratification, and the conduct of large-scale trials to establish standardized, yet personalized, protocols. These advances will solidify TMS as a versatile, data-driven tool for modulating brain networks and accelerating drug development and therapeutic discovery.
References
- 1. Reward circuitry dysfunction in psychiatric and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3464940/]
- 2. Mechanisms of reward circuit dysfunction in psychiatric illness [https://pmc.ncbi.nlm.nih.gov/articles/PMC4035048/]
- 3. Behavioral and neural dysfunctions in reward-related ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12527516/]
- 4. Optimising transcranial direct current stimulation application ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12460327/]
- 5. Optimization of Transcranial Direct Current Stimulation ... [https://brieflands.com/journals/mejrh/articles/163727]
- 6. Mapping neurotransmitter systems to the structural and ... [https://www.nature.com/articles/s41593-022-01186-3]
- 7. Advances in transcranial magnetic stimulation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12417940/]
- 8. Optimization of TMS target engagement: current state and ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1517228/full]
- 9. Neurochemical crossroads: exploring the neurotransmitter ... [https://www.frontiersin.org/journals/molecular-neuroscience/articles/10.3389/fnmol.2025.1675814/full]
- 10. High-frequency transcranial magnetic stimulation ... [https://www.sciencedirect.com/science/article/pii/S0006899325005797]
- 11. Neurotransmitter transporters and their impact on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1760736/]
- 12. Understanding Neurotransmitters Is Key to New Drug R&D [https://www.pharmacytimes.com/view/2007-07-6645]
- 13. Transcranial Magnetic Stimulation (TMS) in 2025 [https://mindbraintms.com/transcranial-magnetic-stimulation-tms-for-depression/]
- 14. Real-world effectiveness of a single-day regimen for ... [https://www.sciencedirect.com/science/article/pii/S3050529125001163]
- 15. Lasting Modulation Effects of rTMS on Neural Activity and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5638649/]
- 16. Comparative efficacy of different modalities of transcranial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12352168/]
- 17. Status and trends in transcranial magnetic stimulation ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1593987/full]
- 18. Neuroplastic effects of transcranial alternating current ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1548478/full]
- 19. Neural mechanisms underlying the after-effects of ... [https://www.nature.com/articles/s41598-025-92444-4]
- 20. Modulating Brain Networks With Transcranial Magnetic ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2020.00031/full]
- 21. TMS-induced modulation of brain networks and its ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/39763561/]
- 22. Concurrent neuroimaging and neurostimulation reveals a ... [https://www.nature.com/articles/s42003-021-02109-x]
- 23. Distinct Roles for the Anterior Cingulate and Dorsolateral ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5939207/]
- 24. Cingulo-Opercular Connectivity Enhances the ... [https://pubmed.ncbi.nlm.nih.gov/41201398/]
- 25. How distinct functional insular subdivisions mediate ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9977390/]
- 26. Functional and Structural Signatures of the Anterior Insula ... [https://www.nature.com/articles/srep37816]
- 27. Potential locations for non-invasive brain stimulation in ... [https://www.nature.com/articles/s41398-025-03303-9]
- 28. Effectiveness of personalized repetitive transcranial ... [https://www.sciencedirect.com/science/article/abs/pii/S0165032725005890]
- 29. Comparison of 5-Day Multidaily Neuronavigated Theta- ... [https://www.researchprotocols.org/2025/1/e70121]
- 30. Comparison of clinical outcomes with two Transcranial ... [https://www.sciencedirect.com/science/article/pii/S1935861X20303065]
- 31. A meta-analysis comparing the effectiveness and safety of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11841443/]
- 32. Comparative Efficacy of Different Repetitive Transcranial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9240662/]
- 33. Efficacy and Safety of Transcranial Magnetic Stimulation for ... [https://www.mdpi.com/2077-0383/14/10/3609]
- 34. MRI-Guided TMS for Depression: A New Approach to ... [https://www.cognitivefxusa.com/blog/mri-guided-tms-for-depression-a-new-approach-to-personalized-treatment]
- 35. Naturalistic Outcomes with fMRI-Guided and Non- ... [https://www.medrxiv.org/content/10.1101/2025.09.03.25334813v1.full-text]
- 36. Precision TMS through the integration of neuroimaging and ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1682852/full]
- 37. Electric field variations across DLPFC targeting methods in ... [https://pubmed.ncbi.nlm.nih.gov/40701134/]
- 38. TMS-induced modulation of brain networks and its ... [https://pubmed.ncbi.nlm.nih.gov/41109521/]
- 39. TMS-induced modulation of brain networks and its ... [https://www.sciencedirect.com/science/article/pii/S1935861X25003596]
- 40. - Multi system for... locus transcranial magnetic stimulation [https://pmc.ncbi.nlm.nih.gov/articles/PMC8807400/]
- 41. Modulating brain networks in space and time: Multi-locus ... [https://www.sciencedirect.com/science/article/abs/pii/S1388245723008040]
- 42. Design, construction, and deployment of a multi-locus ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12085834/]
- 43. Electronics and methods for multi - locus ... transcranial magnetic [https://aaltodoc.aalto.fi/items/89195792-339a-42f4-9ca0-9281c6541f31]
- 44. Clinical development and guiding theory of transcranial ... [https://pubmed.ncbi.nlm.nih.gov/41182327/]
- 45. Fusing DTI and FMRI Data: A Survey of Methods and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4012015/]
- 46. Variability and repeatability of personalized rTMS targeting ... [https://www.sciencedirect.com/science/article/pii/S1053811925003490]
- 47. Advances in transcranial magnetic stimulation for ... [https://pubmed.ncbi.nlm.nih.gov/40933148/]
- 48. Integrated brain connectivity analysis with fMRI, DTI, and ... [https://www.sciencedirect.com/science/article/pii/S1361841525001173]
- 49. Evaluating Individualâ€Level Information in Neural Mass ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12620565/]
- 50. Personalized biomarkers of multiscale functional ... [https://www.nature.com/articles/s41467-025-65042-1]
- 51. Neuronavigation maximizes accuracy and precision in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10026380/]
- 52. Neuronavigation accuracy of the VOSTARS wearable AR ... [https://www.nature.com/articles/s41598-025-14555-2]
- 53. Neuronavigation - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/neuronavigation]
- 54. A functional ultrasound brain GPS for automatic vascular- ... [https://www.nature.com/articles/s41598-021-94764-7]
- 55. Meta-Regression Insights for Optimizing Accelerated ... [https://www.sciencedirect.com/science/article/abs/pii/S002239562500651X]
- 56. The influence of pulse shape and current direction of TMS ... [https://www.sciencedirect.com/science/article/pii/S0006899325002744]
- 57. Precision TMS through the integration of neuroimaging and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12515893/]
- 58. Predictive modeling of response to repetitive transcranial ... [https://www.nature.com/articles/s41398-025-03380-w]
- 59. Use of machine learning in predicting clinical response to ... [https://pubmed.ncbi.nlm.nih.gov/30978624/]
- 60. MUSC study could help lead to personalized TMS for ... [https://web.musc.edu/about/news-center/2025/09/19/musc-study-could-help-lead-to-personalized-tms-for-smokers-who-want-to-quit]
- 61. Real-Time Tractography-Assisted Neuronavigation for ... [https://pubmed.ncbi.nlm.nih.gov/39737576/]
- 62. Electric Field Modeling in Personalizing Transcranial ... [https://www.sciencedirect.com/science/article/abs/pii/S0006322323017523]
- 63. Electric field modeling in personalizing TMS interventions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10922371/]
- 64. Highly accurate calculation of electric field for transcranial ... [https://www.nature.com/articles/s41598-024-76867-z]
- 65. Precision Network Modeling of Transcranial Magnetic ... [https://pubmed.ncbi.nlm.nih.gov/40772472/]
- 66. Transcranial magnetic stimulation as biomarker of excitability ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9303426/]
- 67. State-Dependent Transcranial Magnetic Stimulation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12293497/]
- 68. Predictive and mechanistic biomarkers of treatment response to... [https://pubmed.ncbi.nlm.nih.gov/40925485/]
- 69. Nexstim - TMS - EEG [https://www.nexstim.com/research/tms-eeg]
- 70. Comparative Effectiveness of Noninvasive Brain ... [https://pubmed.ncbi.nlm.nih.gov/40091857/]
- 71. Optimization Strategies of Transcranial Magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10837582/]
- 72. a systematic review and network meta-analysis [https://pubmed.ncbi.nlm.nih.gov/39910020/]
- 73. A systematic review and meta-analysis of neuromodulation ... [https://www.nature.com/articles/s41386-023-01776-0]
- 74. Pragmatic trials of pain therapies: a systematic review of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8675058/]
- 75. Clinical development and guiding theory of transcranial ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12584837/]
- 76. study protocol for a randomized factorial trial [https://pmc.ncbi.nlm.nih.gov/articles/PMC12358067/]
- 77. Comparing implementation strategies for optimizing ... [https://www.medrxiv.org/content/10.1101/2025.01.14.25320533v1.full-text]
- 78. Advancing reduction of drug use as an endpoint in addiction ... [https://nida.nih.gov/about-nida/noras-blog/2025/03/advancing-reduction-drug-use-endpoint-in-addiction-treatment-trials]
- 79. Managing substance abuse on psychiatric units: a scoping ... [https://www.frontiersin.org/journals/psychiatry/articles/10.3389/fpsyt.2025.1653093/full]
- 80. Novel therapies for post-stroke cognitive impairment [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2025.1569329/full]
- 81. Digital Interventions for Cognitive Dysfunction in Patients With ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12288705/]
- 82. Optimization of TMS target engagement: current state and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11814169/]
- 83. Automated optimization of TMS coil placement for ... [https://www.sciencedirect.com/science/article/pii/S0896627322007449]
- 84. Neuromodulatory transcranial magnetic stimulation (TMS) ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11323191/]
- 85. for Stroke · Info for Participants... Transcranial Magnetic Stimulation [https://www.withpower.com/trial/phase-transcranial-magnetic-stimulation-tms-2025-5066b]
- 86. diagnostic utility of Clinical in... transcranial magnetic stimulation [https://pubmed.ncbi.nlm.nih.gov/37068329/]