Brain-Computer Interfaces in 2025: From Foundational Principles to Clinical Applications and Future Trends
This article provides a comprehensive overview of the current state of Brain-Computer Interface (BCI) technology, tailored for researchers, scientists, and drug development professionals.
Brain-Computer Interfaces in 2025: From Foundational Principles to Clinical Applications and Future Trends
Abstract
This article provides a comprehensive overview of the current state of Brain-Computer Interface (BCI) technology, tailored for researchers, scientists, and drug development professionals. It explores the foundational principles of BCI systems, from non-invasive EEG to invasive and semi-invasive cortical implants. The scope covers the methodological pipeline—including signal acquisition, preprocessing, feature extraction, and classification—and details transformative medical applications in rehabilitation, communication, and neuroprosthetics. The review also addresses critical challenges in signal optimization, system reliability, and clinical translation, while offering a comparative analysis of leading technologies and validation frameworks essential for transitioning from laboratory research to real-world, plug-and-play clinical and biomedical applications.
Core Principles and the Modern BCI Landscape: Signals, Systems, and Key Players
A Brain-Computer Interface (BCI) is a system that establishes a direct communication pathway between the brain's electrical activity and an external device, such as a computer or robotic limb [1]. This technology bypasses conventional neuromuscular pathways, translating neural signals into digital commands [2]. A closed-loop BCI system is characterized by its real-time operation, which includes not only decoding neural signals to control an external device but also providing feedback to the user, creating a continuous cycle of interaction between the brain and the machine [3]. This feedback is crucial for the user to adjust their mental commands and for the system to adapt its decoding algorithms, enabling precise control for applications in rehabilitation, communication, and assistive technology [3] [2]. This document details the core principles, current applications, and experimental protocols central to BCI control applications research.
Core Components and Signaling Pathway of a Closed-Loop BCI
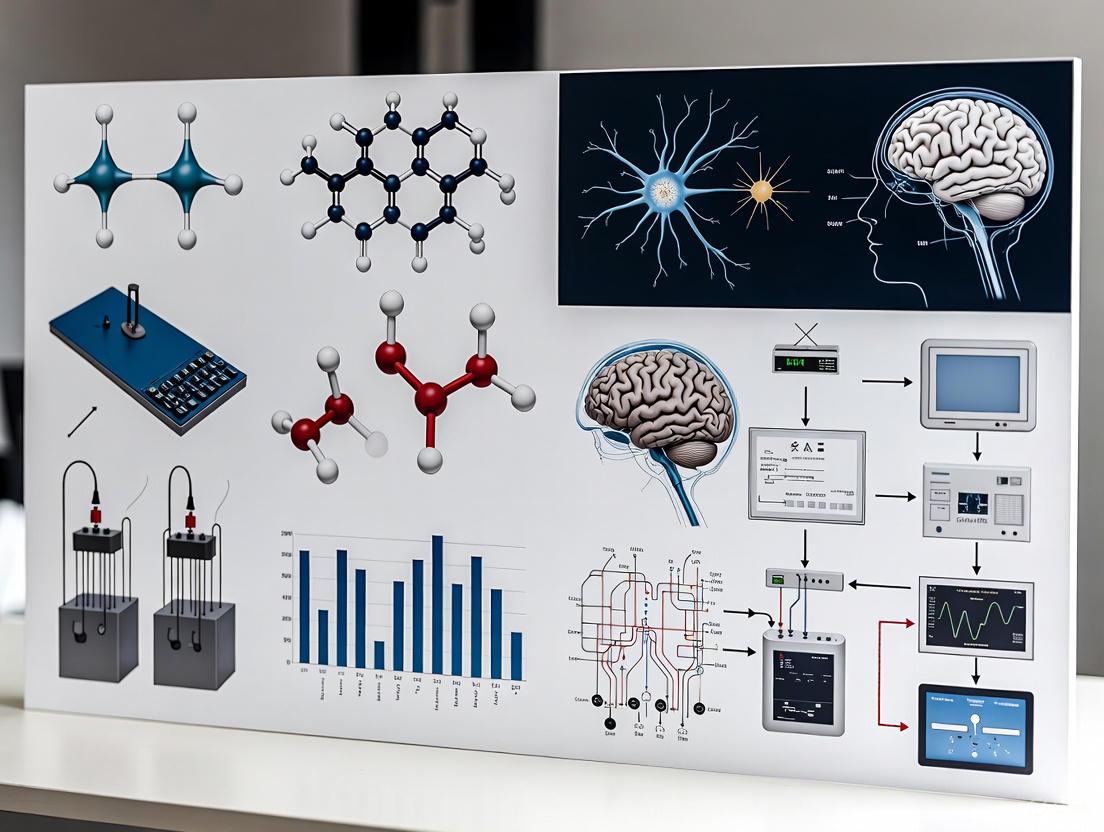
The operation of a closed-loop BCI can be conceptualized as a sequential signaling pathway. The diagram below illustrates the core workflow and the logical relationships between each component.
Closed-Loop BCI Workflow
Figure 1: The closed-loop BCI workflow. This diagram outlines the fundamental pathway from neural signal acquisition to device control and sensory feedback, which completes the loop for user adaptation.
A closed-loop BCI system functions through four standard, sequential components [3]:
- Signal Acquisition: The measurement of brain signals using various modalities. Invasive techniques, such as microelectrode arrays (e.g., Neuralink, Blackrock Neurotech), are implanted directly into the brain tissue to record the activity of individual neurons with high fidelity [2] [1]. Partially invasive techniques, like electrocorticography (ECoG), place electrodes on the surface of the brain, while endovascular approaches (e.g., Synchron's Stentrode) place electrodes within blood vessels [2] [4]. Non-invasive techniques, such as electroencephalography (EEG), record electrical activity from the scalp [3] [1].
- Signal Processing and Feature Translation: The acquired neural signals are typically noisy and must be processed. This stage involves filtering artifacts and extracting informative features (e.g., power in specific frequency bands, firing rates of neurons) [3]. Subsequently, machine learning (ML) and artificial intelligence (AI) algorithms, such as convolutional neural networks (CNNs) and support vector machines (SVMs), translate these features into commands that represent the user's intent [3].
- Device Output: The translated commands are executed to control an external device. This could be a computer cursor, a robotic arm, a speech synthesizer, or a wheelchair [2] [1].
- Sensory Feedback: The result of the device's action is relayed back to the user in real-time, typically through visual or auditory channels. This feedback is perceived by the user's brain, allowing them to assess the outcome and subconsciously adjust their neural activity for the next command, thereby closing the loop [3] [2].
Applications and Quantitative Performance Metrics
BCI technologies are being developed for a range of medical applications, particularly for individuals with severe neurological impairments. The table below summarizes key application areas and associated performance metrics from recent research and clinical trials.
Table 1: Key BCI Applications and Performance Metrics (2020-2025)
| Application Area | Specific Task / Paradigm | Key Performance Metrics (Reported Values) | Selected Companies/Institutions |
|---|---|---|---|
| Communication & Control | Text spelling via Steady-State Visual Evoked Potential (SSVEP) [5] | Information Transfer Rate (ITR): ~5.42 bits/sec [5] | Various research labs |
| Text spelling for locked-in syndrome [6] [4] | Typing speed, Accuracy, System longevity (>9 years) [6] [4] | Blackrock Neurotech, Johns Hopkins | |
| Motor Restoration & Rehabilitation | Control of robotic arm for self-feeding [1] | Task completion rate, Accuracy of movement trajectory | University of Pittsburgh |
| Combined BCI with Functional Electrical Stimulation (FES) for stroke rehab [7] | Restoration of movement, Improvement in clinical motor function scales | Various research labs | |
| Speech Decoding | Decoding speech from motor cortex activity [2] | Word decoding accuracy (~99%), Latency (<0.25 seconds) [2] | Neuralink, Paradromics |
The addressable market for these medical BCIs is significant. In the United States alone, an estimated 5.4 million people live with paralysis, and the global market for invasive BCIs is projected to be substantial, driven by these unmet clinical needs [2].
Experimental Protocols for BCI Research
Protocol: SSVEP-based BCI Speller
This protocol is adapted from the design of the BETA database, a large-scale benchmark for SSVEP-BCI applications [5].
- Objective: To design and validate a high-speed BCI speller for communication, using non-invasive EEG to record steady-state visual evoked potentials.
- Materials:
- EEG system with 64 channels.
- Visual stimulation monitor (e.g., 27-inch LED, 60Hz refresh rate).
- Software for sampled sinusoidal stimulation.
- Stimulus Design:
- Create a virtual keyboard with 40 targets (letters, numbers, symbols) arranged in a QWERTY layout.
- Implement a sampled sinusoidal stimulation method, with target frequencies ranging from 8 to 15.8 Hz.
- Ensure sufficient color contrast and spacing between targets to minimize visual interference.
- Procedure:
- Participant Preparation: Recruit participants with normal or corrected-to-normal vision. Apply EEG cap according to standard 10-20 system.
- Task: Instruct participants to focus on a cued target character on the screen. Each character will flicker at its specific frequency.
- Data Acquisition: Record EEG data across four blocks of trials. Each trial involves a cue period followed by a stimulation period.
- Signal Processing: Use frequency recognition methods like Canonical Correlation Analysis (CCA) to identify the target frequency the user is attending to.
- Validation: Calculate performance metrics, including classification accuracy and Information Transfer Rate (ITR), to validate the system.
Protocol: Implantable BCI for Communication in Locked-in Syndrome
This protocol summarizes the methodology from ongoing clinical trials, such as the CortiCom Study [6].
- Objective: To assess the safety and efficacy of a fully-implanted BCI system for restoring communication capabilities in patients with chronic locked-in syndrome.
- Materials:
- Implantable electrode array (e.g., ECoG grid or microelectrode array).
- Implantable wireless transmitter or transcutaneous pedestal.
- Decoding computer with specialized software.
- Participant Inclusion/Exclusion Criteria:
- Inclusion: Adults (age 22-70) with locked-in syndrome caused by brainstem stroke, trauma, or ALS; ability to communicate reliably only with caregiver assistance; cleared for brain surgery [6].
- Exclusion: Pre-existing visual impairment; presence of other diseases or implants that would contraindicate surgery or participation [6].
- Procedure:
- Surgical Implantation: A neurosurgeon implants electrodes onto the surface of the brain (ECoG) or into the cortical tissue (microelectrodes). The device is connected to a transmitter implanted in the chest.
- Post-operative Recovery: Allow for healing from surgery as per standard clinical protocols.
- Calibration & Training: Participants train with the BCI for up to 4 hours per day, several days per week, for a minimum of 6 months to one year. The system is calibrated to decode the user's neural signals associated with intent (e.g., moving a cursor, selecting a letter).
- Testing & Data Collection: Participants perform standardized communication tasks (e.g., typing, triggering an alert). Safety, accuracy, and communication speed data are collected.
- Data Analysis: Evaluate the system's performance based on typing speed, accuracy, and the incidence of adverse events.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagents and Materials for BCI Experiments
| Item | Function / Application in BCI Research |
|---|---|
| High-Density EEG System | Non-invasive recording of brain signals from the scalp; used in SSVEP, P300, and motor imagery paradigms [5]. |
| Microelectrode Arrays (Utah Array) | Invasive neural interfaces for recording and stimulating the activity of individual neurons or small neural populations; provide high signal fidelity [2] [1]. |
| Endovascular Stentrode | A minimally invasive electrode array delivered via blood vessels; records cortical signals without open-brain surgery [2] [4]. |
| Electrocorticography (ECoG) Grid | A partially invasive array of electrodes placed on the surface of the brain; offers a balance between signal resolution and invasiveness [1]. |
| Canonical Correlation Analysis (CCA) | A statistical method used for frequency recognition in SSVEP-based BCI systems [5]. |
| Deep Learning Algorithms (CNNs, RNNs) | Machine learning models for decoding complex neural signals, such as those for speech or kinematic parameters, from high-dimensional neural data [3]. |
| Robotic Arm / Assistive Device | An external actuator controlled by the BCI output to provide physical interaction with the environment for users with paralysis [1]. |
| Fmoc-Cys(tert-butoxycarnylpropyl)-OH | Fmoc-Cys(tert-butoxycarnylpropyl)-OH [102971-73-3] |
| 4-Hydroxy-2-oxoglutaric acid | 2-Hydroxy-4-oxopentanedioic Acid | High Purity |
BCI System Integration and Feedback Pathway
The integration of AI-driven decoding with the feedback loop is a critical advancement in modern BCI systems. The following diagram details the integration of the AI decoder within the broader system context and the specific data flows involved in the feedback pathway, which is essential for user adaptation and system performance.
Figure 2: AI-driven closed-loop BCI integration. This diagram emphasizes the central role of the AI/ML decoder in processing extracted neural features to predict user intent, which is then executed to generate sensory feedback, completing the adaptive loop.
The integration of Artificial Intelligence (AI) and Machine Learning (ML) is paramount for enhancing the performance of closed-loop BCIs [3]. Techniques such as Convolutional Neural Networks (CNNs) and Support Vector Machines (SVMs) improve real-time classification of neural signals for cognitive state monitoring and device control [3]. Transfer Learning (TL) is being explored to address the challenge of high variability in brain signals between users, which otherwise requires lengthy calibration sessions for each new subject [3]. The feedback loop is critical for the user to correct their mental commands, and for the AI model itself to adapt over time, creating a more robust and personalized system [3] [2].
Brain-computer interface (BCI) technology facilitates direct communication between the human brain and external devices, offering transformative potential for both clinical applications and human augmentation [8]. The core of BCI systems lies in their ability to record and interpret neural activity through various neuroimaging modalities, each with distinct characteristics, advantages, and limitations. These modalities span a spectrum from non-invasive techniques that measure brain activity externally to invasive methods that require surgical implantation of recording electrodes [9] [8].
The selection of an appropriate neuroimaging modality is paramount for BCI control applications, as it directly impacts signal quality, spatial and temporal resolution, practical implementation, and ultimately, the feasibility and performance of the BCI system [8] [10]. Non-invasive techniques like electroencephalography (EEG) and functional near-infrared spectroscopy (fNIRS) offer safer, more accessible options, though often at the cost of signal resolution. In contrast, invasive methods such as electrocorticography (ECoG) and intracortical microelectrode arrays (MEAs) provide high-fidelity neural signals but carry surgical risks and are subject to long-term biocompatibility challenges [9] [8] [11].
This article provides a comparative analysis of these key neuroimaging modalities within the context of BCI control applications. It presents structured quantitative comparisons, detailed experimental protocols, and visual frameworks to guide researchers and scientists in selecting and implementing the most appropriate modality for their specific BCI research and development objectives.
Comparative Analysis of Neuroimaging Modalities
The performance characteristics of neuroimaging modalities used in BCI research vary significantly across key parameters. The following table provides a systematic comparison of non-invasive and invasive modalities to inform research design decisions.
Table 1: Comparative Analysis of Neuroimaging Modalities for BCI Applications
| Modality | Spatial Resolution | Temporal Resolution | Invasiveness | Key BCI Applications | Primary Limitations |
|---|---|---|---|---|---|
| EEG [8] [10] | Low (Centimeters) | High (Milliseconds) | Non-invasive | Communication systems, motor imagery, epilepsy monitoring, sleep studies | Low spatial resolution, susceptible to noise and artifacts |
| fNIRS [8] [10] | Medium (1-2 cm) | Low (Seconds) | Non-invasive | Cognitive state monitoring, neurofeedback, emotional recognition | Low temporal resolution, measures hemodynamic response (indirect) |
| MEG [8] [12] | High (Millimeters) | High (Milliseconds) | Non-invasive | Mapping neural networks, clinical brain mapping | Expensive, non-portable, limited access |
| fMRI [8] [12] | High (Millimeters) | Low (Seconds) | Non-invasive | Localizing brain function, neurofeedback | Expensive, non-portable, measures indirect hemodynamic response |
| ECoG [9] [8] | High (Millimeters) | High (Milliseconds) | Semi-invasive (Subdural) | Refractory epilepsy mapping, motor decoding for prosthetics | Requires craniotomy, limited cortical coverage |
| Intracortical MEA [9] [8] | Very High (Microns) | Very High (Milliseconds) | Invasive (Intracortical) | High-dimensional prosthetic control, decoding movement kinematics | Highest surgical risk, potential for tissue reaction over time |
The choice of modality often involves a trade-off between key parameters. Invasive BCIs, such as those using intracortical microelectrode arrays, provide the highest spatial and temporal resolution, capturing signals from individual neurons or small neuronal populations [9]. This enables complex control tasks, such as dexterous manipulation of robotic arms [9] [13]. Conversely, non-invasive BCIs like EEG trade off signal resolution for safety and accessibility, making them suitable for a wider user base and applications where high precision is less critical [11]. Emerging research aims to bridge this gap; for instance, a 2025 study demonstrated real-time control of a robotic hand at the individual finger level using a deep-learning-based EEG decoder, showcasing the potential for more naturalistic control with non-invasive systems [13].
Experimental Protocols for BCI Modalities
Protocol: Non-invasive BCI for Robotic Hand Control via EEG
This protocol details the methodology for achieving real-time robotic hand control at the individual finger level using an EEG-based BCI, as demonstrated by recent research [13].
- Objective: To establish a closed-loop BCI system that translates finger movement execution (ME) and motor imagery (MI) into real-time control of a robotic hand.
- Primary Modality: Non-invasive Electroencephalography (EEG).
- Experimental Setup:
- Participants: Able-bodied individuals with prior BCI experience.
- EEG Acquisition: High-density EEG system is used to record scalp potentials.
- Robotic Interface: A robotic hand prosthesis is synchronized with the BCI output.
- Visual Cueing: A computer screen provides task instructions and visual feedback.
- Procedure:
- Offline Session (Model Training):
- Participants perform cued ME and MI of individual fingers (e.g., thumb, index, pinky).
- EEG data is recorded to train a subject-specific deep learning decoder (e.g., EEGNet).
- Online Session (Real-Time Control):
- The trained model decodes EEG signals in real-time.
- Decoded outputs are converted into commands to actuate the corresponding robotic finger.
- Participants receive simultaneous visual (on-screen) and physical (robotic hand movement) feedback.
- Model Fine-Tuning:
- To mitigate inter-session variability, the base model is fine-tuned using data from the first half of each online session, which is then applied to the second half to enhance performance.
- Offline Session (Model Training):
- Data Analysis:
- Performance Metrics: Majority voting accuracy, precision, and recall for each finger class are calculated.
- Statistical Testing: A repeated-measures ANOVA is used to assess performance improvements across sessions.
Protocol: Invasive BCI for Dexterous Control via Intracortical Arrays
This protocol outlines the use of invasive microelectrode arrays for high-precision BCI control, fundamental to applications requiring dexterous manipulation [9].
- Objective: To decode movement intentions from motor cortex activity for multi-dimensional control of external devices.
- Primary Modality: Invasive Intracortical Microelectrode Arrays (MEA).
- Experimental Setup:
- Participants: Typically individuals with tetraplegia in clinical trials, or animal models (e.g., non-human primates) in foundational research.
- Implantation: A microelectrode array (e.g., 96-channel) is surgically implanted into the primary motor cortex (M1) or posterior parietal cortex.
- Signal Acquisition: A neural signal processor records action potentials (spikes) and local field potentials (LFPs).
- Procedure:
- Neural Recording: Participants are instructed to observe, imagine, or attempt to perform specific arm and hand movements.
- Decoder Calibration: Recorded neural signals are correlated with kinematic parameters (e.g., velocity, position, gripping force) to calibrate a real-time decoding algorithm (e.g., Kalman filter, Bayesian decoder).
- Closed-Loop Control: The participant uses the decoded motor commands to control a computer cursor or robotic prosthetic arm in real-time, with visual feedback guiding the task.
- Data Analysis:
- Kinematic Decoding: The accuracy of the decoder is evaluated by comparing the decoded trajectory to the intended or actual movement trajectory.
- Task Performance: Success rates in completing functional tasks (e.g., reach-and-grasp) are measured.
Signaling Pathways and System Workflows
The following diagrams illustrate the core logical frameworks and information pathways in BCI systems, from signal acquisition to closed-loop control.
BCI Modality Comparison Framework
This diagram outlines the hierarchical relationship between signal invasiveness and resolution, which is a fundamental concept for comparing neuroimaging modalities.
Generalized BCI System Workflow
This workflow depicts the standard signal processing pipeline common to most BCI systems, regardless of the specific acquisition modality.
The Scientist's Toolkit: Research Reagent Solutions
Successful BCI experimentation relies on a suite of specialized hardware, software, and analytical tools. The following table catalogs essential components for building and testing BCI systems.
Table 2: Essential Research Tools for BCI Development
| Tool Category | Specific Examples | Function in BCI Research |
|---|---|---|
| Signal Acquisition Hardware | EEG caps, ECoG grids/strips, Intracortical Microelectrode Arrays (e.g., Utah Array), fNIRS optodes, MEG scanner, fMRI scanner [8] [10] | Captures raw neural or hemodynamic signals from the brain with varying degrees of spatial and temporal resolution. |
| Data Processing Platforms | BrainAMP, NIRScout, OpenBCI, custom microcontroller units [10] | Amplifies, digitizes, and sometimes preprocesses the acquired neural signals. |
| Signal Processing & ML Libraries | EEGLab, BCILAB, Scikit-learn, TensorFlow, PyTorch [14] [13] | Provides algorithms for preprocessing (e.g., ICA, wavelet transforms), feature extraction, and classification/decoding of brain signals. |
| Decoding Algorithms | Population Vector Algorithm, Kalman Filter, Bayesian Decoder, Convolutional Neural Networks (e.g., EEGNet) [9] [13] | Translates processed neural features into predicted user intent or kinematic parameters for device control. |
| External Actuators | Robotic arms (e.g., prosthetic limbs), computer cursors, spelling applications, virtual reality environments [9] [8] [13] | Serves as the end-effector controlled by the BCI, providing functional output and feedback to the user. |
| Integrated Dual-Modality Systems | Custom fNIRS-EEG helmets with 3D-printed or thermoplastic mounts [10] | Enables simultaneous acquisition of electrophysiological (EEG) and hemodynamic (fNIRS) data for a more comprehensive brain activity picture. |
| Methyl prednisolone-16alpha-carboxylate | Methyl prednisolone-16alpha-carboxylate | RUO | Methyl prednisolone-16alpha-carboxylate: A key metabolite for steroid metabolism and immunoassay research. For Research Use Only. Not for human or veterinary use. |
| 2-Bromo-3,5-dimethoxytoluene | 2-Bromo-3,5-dimethoxytoluene, CAS:13321-73-8, MF:C9H11BrO2, MW:231.09 g/mol | Chemical Reagent |
A brain-computer interface (BCI) is a system that measures central nervous system activity and converts it into artificial output to change the ongoing interactions between the brain and its external or internal environment [2]. In plainer terms, a BCI translates thought into action. This document details the standard BCI signal processing pipeline, a closed-loop system comprising four sequential stages: Signal Acquisition, Preprocessing, Decoding (Feature Extraction and Translation), and Output Generation. The content herein is framed within a broader thesis on BCI control applications, providing application notes and detailed experimental protocols for researchers and scientists.
The BCI Signal Processing Pipeline: A Stage-by-Stage Analysis
The BCI closed-loop system enables direct communication between a person and a computer, allowing users to operate external devices through their brain activity [15]. The system's backbone is its sequential design: acquire, decode, execute, and provide feedback [2]. Figure 1 illustrates the complete workflow of this pipeline, from signal acquisition to the final output and feedback loop.
Figure 1. The BCI Closed-Loop Processing Pipeline. This diagram outlines the standard stages of a BCI system, from capturing brain signals to generating a device output and providing feedback to the user. The feedback loop is critical for users to adjust their mental strategy.
Stage 1: Signal Acquisition
The first stage involves measuring neural activity from the brain. Methods vary in their invasiveness and spatial resolution, as detailed in Table 1.
Table 1: Neural Signal Acquisition Modalities in BCI Research
| Method | Invasiveness | Key Players/Examples | Key Characteristics & Applications |
|---|---|---|---|
| Electroencephalography (EEG) | Non-invasive | Kernel Flow [16] | Measures electrical activity via scalp electrodes; portable but susceptible to noise; used for Motor Imagery, SSVEP, and P300 paradigms [17]. |
| Electrocorticography (ECoG) | Minimally Invasive | Precision Neuroscience (Layer 7) [2] | Electrodes placed on the cortical surface; higher signal resolution than EEG; suitable for speech decoding and communication restoration. |
| Microelectrode Arrays | Invasive | Neuralink, Paradromics, Blackrock Neurotech [2] [16] | Micro-electrodes penetrate cortical tissue to record from individual neurons; provides the highest signal fidelity; targets severe paralysis and communication restoration. |
| Endovascular Stent Electrodes | Minimally Invasive | Synchron (Stentrode) [2] [18] | Electrodes delivered via blood vessels; balances signal quality and surgical risk; enables digital device control for paralyzed users. |
Stage 2: Preprocessing
Raw neural signals are inherently noisy. Preprocessing aims to enhance the signal-to-noise ratio (SNR) by removing artifacts and isolating relevant components. A recent 2025 study systematically evaluated preprocessing techniques for EEG-based BCIs, highlighting the performance impact of different pipelines [19].
Table 2: Efficacy of Common Preprocessing Techniques in EEG-based BCIs [19]
| Preprocessing Technique | Function | Contribution to Performance & Suitability for Online BCI |
|---|---|---|
| Baseline Correction | Removes DC offset and slow drifts | Consistently provided the most beneficial preprocessing effects; recommended for online implementation. |
| Bandpass Filtering | Isolates specific frequency bands (e.g., Mu 8-13 Hz, Beta 13-30 Hz) | Consistently provided the most beneficial preprocessing effects; recommended for online implementation. |
| Surface Laplacian | Spatial filter that improves locality and reduces volume conduction | Enhanced effectiveness when used with spatial-information algorithms; recommended for online implementation. |
| Independent Component Analysis (ICA) | Separates statistically independent sources (e.g., removes eye blinks, muscle artifacts) | Useful for artifact removal; can be computationally intensive for real-time use. |
Stage 3: Decoding
The decoding stage translates preprocessed signals into meaningful commands. It consists of two substages: feature extraction and feature translation/classification.
Feature Extraction
This process identifies and quantifies informative features from the preprocessed neural data. The choice of feature is often tied to the BCI paradigm.
Table 3: Feature Extraction Methods for Key BCI Paradigms
| BCI Paradigm | Description | Relevant Features & Extraction Methods |
|---|---|---|
| Motor Imagery (MI) | User imagines a movement without executing it [20]. | Event-Related Desynchronization/Synchronization (ERD/ERS) in Mu/Beta rhythms; Common Spatial Patterns (CSP); Wavelet Transform [20]. |
| P300 | Response to a rare, target stimulus amidst frequent stimuli. | Positive deflection in EEG signal around 300ms post-stimulus; temporal filtering and averaging [17]. |
| Steady-State Visual Evoked Potential (SSVEP) | Response to a visual stimulus flickering at a fixed frequency. | Oscillatory activity at the stimulus frequency and its harmonics; Power Spectral Density (PSD) analysis [17]. |
Feature Translation and Classification
This final decoding step uses machine learning (ML) and deep learning (DL) algorithms to map the extracted features to a specific output command. Table 4 compares the performance of various classifiers on a Motor Imagery task, highlighting the superiority of a hybrid deep learning model.
Table 4: Classifier Performance on Motor Imagery EEG Data [20]
| Classifier Type | Specific Model | Reported Accuracy | Key Notes |
|---|---|---|---|
| Traditional ML | Random Forest (RF) | 91.00% | Achieved the highest accuracy among traditional classifiers tested. |
| Traditional ML | Support Vector Classifier (SVC) | (Reported, value not given) | A commonly used, robust classifier for BCI. |
| Traditional ML | k-Nearest Neighbors (KNN) | (Reported, value not given) | Performance can be sensitive to feature scaling. |
| Deep Learning | Convolutional Neural Network (CNN) | 88.18% | Excels at extracting spatial features from EEG. |
| Deep Learning | Long Short-Term Memory (LSTM) | 16.13% | Poor performance alone on this specific task. |
| Deep Learning | Hybrid CNN-LSTM | 96.06% | Proposed model; combines spatial (CNN) and temporal (LSTM) feature extraction. |
Stage 4: Output Generation and Feedback
The classified intent is converted into a command for an external device. Examples include moving a robotic arm, controlling a wheelchair, typing text, or generating synthetic speech [2]. A key advancement in 2025 was Synchron's BCI integration with Apple's BCI Human Interface Device profile, allowing users to control Apple devices natively with their thoughts [18]. The resulting device action is fed back to the user visually or audibly, closing the loop and enabling the user to refine their mental commands for improved control.
Experimental Protocol: Decoding Inner Speech from Motor Cortical Activity
Background and Objective
Restoring communication is a primary goal of invasive BCI research. While decoding attempted speech has been successful, it can be fatiguing for users. This protocol, based on a recent 2025 Stanford study, details a methodology for decoding inner speech (imagined speech without movement) from signals in the motor cortex, a step toward more fluent and comfortable communication BCIs [21].
Figure 2 visualizes the experimental workflow for this inner speech decoding study.
Figure 2. Experimental Workflow for Inner Speech Decoding. This protocol involves implanting microelectrode arrays in the motor cortex of participants with severe speech impairments to record neural activity during both attempted and inner speech.
Detailed Methodology
Participants and Surgical Preparation
- Participants: Recruit individuals with severe speech and motor impairments (e.g., from ALS, brainstem stroke, or spinal cord injury). The Stanford study included four such participants [21].
- Implantation: Under regulatory and ethical approval, implant microelectrode arrays (e.g., the Utah array, smaller than a pea) onto the surface of the brain in regions of the motor cortex critical for speech articulation [21].
Data Collection and Experimental Paradigm
- Stimuli Presentation: Participants are presented with visual or auditory cues of words or sentences they are to produce.
- Task Conditions:
- Attempted Speech: The participant attempts to physically speak the cued words, even if no sound is produced.
- Inner Speech: The participant silently imagines speaking the cued words, focusing on the sounds and feeling of speech without any physical attempt [21].
- Neural Recording: The implanted arrays record high-resolution neural activity during both conditions over multiple trials to build a robust dataset.
Signal Processing and Decoding
- Preprocessing: Apply bandpass filtering and other preprocessing techniques (see Table 2) to raw neural data to improve SNR.
- Feature Extraction: Identify and isolate repeatable patterns of neural activity associated with phonemes—the smallest units of speech [21].
- Machine Learning Model Training: Use machine learning (e.g., neural networks) to train a decoder. The model is trained to recognize the neural patterns associated with each phoneme and learn how to stitch them together into coherent words and sentences. The study noted that inner speech patterns were a "similar, but smaller, version of the activity patterns evoked by attempted speech" [21].
Output Generation and Privacy Mitigation
- Output: The trained decoder translates real-time neural signals into text or synthetic speech output.
- Privacy Control: To prevent accidental decoding of unintended inner thoughts, the protocol can implement a "password-protection" system. The BCI only decodes speech if the user first imagines a specific, rare passphrase (e.g., "as above, so below"), effectively acting as a mental 'enter' key [21].
Research Reagent Solutions
Table 5: Essential Materials and Reagents for an Invasive Speech BCI Study
| Item | Function & Application in Protocol |
|---|---|
| Microelectrode Arrays (e.g., Utah Array) | High-density arrays for recording neural activity from populations of neurons in the cortical speech areas. The core data acquisition hardware [21]. |
| Neural Signal Amplifier & Digitizer | Conditions and converts analog microvolt-level brain signals into digital data for processing. |
| Sterile Surgical Equipment & Implant Tools | For the sterile implantation of the microelectrode arrays according to standard neurosurgical practice. |
| ML-Compatible Computing Cluster | High-performance computer with GPU acceleration for training the complex phoneme and language decoding models. |
| Stimulus Presentation Software (e.g., Psychopy) | To accurately present visual/auditory cues to the participant and synchronize them with neural data recording. |
| BCI Software Platform (e.g., BCI2000, OpenViBE) | An integrated software environment for real-time data acquisition, stimulus presentation, signal processing, and decoder operation. |
The BCI signal processing pipeline provides the foundational framework for transforming neural activity into actionable commands. As of 2025, advances in electrode technology, sophisticated preprocessing pipelines, and powerful AI-driven decoding models are pushing BCIs from laboratory demonstrations toward real-world clinical applications. The experimental protocol on inner speech decoding exemplifies the field's trajectory, tackling complex challenges like decoding internal states while proactively addressing ethical concerns such as neural privacy. Future work will focus on improving the robustness, speed, and accessibility of these systems, ultimately aiming to restore fundamental abilities like communication and mobility.
Application Notes: Core Technologies and Methodologies
The commercial brain-computer interface (BCI) landscape in 2025 is defined by pioneering companies translating laboratory research into clinical-grade neurotechnology. These systems are designed to transform thought into action for patients with severe paralysis and communication deficits, employing diverse technological pathways from fully implantable intracortical arrays to endovascular electrodes [2]. The following application notes detail the core methodologies and experimental protocols from four key industry innovators.
Neuralink
- Core Technology & Mechanism: Neuralink's "Link" is a coin-sized, fully implantable device containing ultra-high-bandwidth micro-electrodes threaded into the cortical surface by a specialized robotic surgeon [2]. The system is designed for wireless operation, sealed within the skull, and aims to record from more individual neurons than prior devices to achieve high-fidelity control of digital interfaces [2] [22].
- Primary Application & Trial Status: The first product, "Telepathy," aims to enable individuals with paralysis to control computers or other digital devices through thought alone [22]. An early feasibility human trial began in January 2024. As of mid-2025, five individuals with severe paralysis have received the implant and are using it to control digital and physical devices with their thoughts [2]. A second product, "Blindsight," aimed at restoring limited vision, has received FDA breakthrough device designation [22].
Synchron
- Core Technology & Mechanism: Synchron's "Stentrode" is an endovascular BCI delivered via a catheter through the jugular vein and lodged in the superior sagittal sinus, a blood vessel draining the motor cortex [2]. This approach avoids open brain surgery by recording brain signals through the vessel wall, representing a minimally invasive alternative to craniotomy [23] [2].
- Primary Application & Trial Status: The Stentrode is designed to allow patients with paralysis to control digital devices for tasks like texting and emailing [24]. A four-patient trial demonstrated the ability to control a computer via thought, with no serious adverse events or vessel blockages reported after 12 months [2]. The company is advancing towards a pivotal clinical trial and has established partnerships with mainstream technology ecosystems [2].
Blackrock Neurotech
- Core Technology & Mechanism: Blackrock's approach is built upon the "Utah Array" (NeuroPort Electrode), a bed-of-nails style intracortical electrode that has been the cornerstone of many academic BCI studies for over two decades [25] [2]. The company provides a complete BCI ecosystem, including implantable electrodes, hardware, and software [25]. They are developing next-generation technologies like "Neuralace," a flexible lattice for less invasive cortical coverage [2].
- Primary Application & Trial Status: Blackrock's technology enables control of prosthetics, computer functions, and communication for people with paralysis [25] [26]. Their first device for clinical use, the "MoveAgain" BCI system, received an FDA Breakthrough Designation in 2021 [25]. The technology has been validated over 19+ years of human studies and is currently being used in expanding in-home trials where paralyzed users live with the BCI daily [2] [26].
Paradromics
- Core Technology & Mechanism: The "Connexus BCI" is a fully implantable, high-data-rate platform using a modular array of 421 micro-electrodes, each thinner than a human hair, to capture activity from individual neurons [27] [28]. The device features an integrated wireless transmitter implanted in the chest and is engineered for long-term stability and high bandwidth, reportedly achieving over 200 bits per second in pre-clinical models [27] [28].
- Primary Application & Trial Status: The primary initial application is the restoration of speech and computer control for people with severe motor impairments, such as those caused by ALS, stroke, or spinal cord injury [27] [29]. The company received FDA Investigational Device Exemption (IDE) approval in late 2025 for its "Connect-One" Early Feasibility Study, with the first-in-human recording successfully completed at the University of Michigan [27] [28] [29]. The clinical study is slated to begin in late 2025 across three US sites [29].
Table 1: Quantitative Comparison of Key BCI Platform Specifications (2025)
| Company | Implant Type | Channel Count/Data Rate | Surgical Approach | Clinical Trial Stage |
|---|---|---|---|---|
| Neuralink | Intracortical microelectrode array | High (specifics not detailed) | Robotic-assisted craniotomy [2] | Early Feasibility Study (5 participants as of mid-2025) [2] |
| Synchron | Endovascular stent electrode | Not specified in detail | Minimally-invasive endovascular [23] [2] | Completed 4-patient trial; advancing to pivotal trial [2] |
| Blackrock Neurotech | Utah Array (intracortical) | Versatile system configurations [25] | Craniotomy [2] | MoveAgain FDA Breakthrough Designation (2021); in-home trials [25] [2] |
| Paradromics | Intracortical microelectrode array | 421 electrodes; >200 bits/sec [27] | Craniotomy (familiar to neurosurgeons) [27] [2] | FDA IDE approved; Connect-One Study starting late 2025 [27] |
Table 2: Primary Clinical Applications and Demonstrated Capabilities
| Company | Target Patient Population | Demonstrated/Planned Functional Outputs |
|---|---|---|
| Neuralink | Severe paralysis [2] [22] | Control of digital and physical devices [2] |
| Synchron | Paralysis with limited mobility [24] | Computer control, texting, emailing, online access [2] [24] |
| Blackrock Neurotech | Paralysis, neurological disorders [25] | Prosthetic limb control, typing (up to 90 char/min), email, digital art, word decoding (62 words/min) [25] [26] |
| Paradromics | Severe motor impairment (ALS, stroke, SCI) with speech loss [27] [29] | Restoration of speech via text/synthesized speech, computer control [27] [28] |
Experimental Protocols
General BCI Workflow and Signal Processing Pathway
The following diagram illustrates the core, universal signal processing pathway shared by modern implantable BCI systems.
Protocol 1: Surgical Implantation and Acute Recording
This protocol outlines the common procedures for the surgical implantation of intracortical BCIs, such as those from Paradromics and Blackrock Neurotech, and the subsequent acute neural recording validation [27] [28] [29].
- Objective: To surgically implant a BCI device and verify its functionality by recording neural signals in an acute setting.
- Materials:
- Procedure:
- Patient Preparation and Sterile Draping: Position the patient and prepare the surgical site according to standard neurosurgical protocols.
- Craniotomy: Perform a craniotomy to expose the dura mater over the target brain region (e.g., motor cortex for movement, speech cortex for communication) [2].
- Device Implantation:
- Closure and Signal Verification: Secure the device and partially close the surgical site. Connect the implant to the neural signal processor to verify the presence of multi-unit or single-unit neural activity.
- Acute Recording (if applicable): In an intraoperative setting, such as during epilepsy surgery, present the patient with motor or cognitive tasks (e.g., attempting to move a hand, imagine speaking) to confirm that task-modulated neural signals are being recorded [28].
- Conclusion: The device may be explanted (in an acute study) or fully secured for long-term implantation based on the study protocol [28].
Protocol 2: Chronic In-Home BCI Use for Communication
This protocol describes the methodology for deploying a BCI system for long-term, at-home use to restore communication, representative of the trials conducted by Blackrock Neurotech and planned by Paradromics [2] [26].
- Objective: To evaluate the safety and efficacy of a chronically implanted BCI in enabling computer control and communication for a paralyzed individual in their home environment.
- Materials:
- Chronically Implanted BCI System: e.g., Blackrock's MoveAgain system or Paradromics' Connexus BCI with its chest-mounted receiver [25] [27].
- External Decoder/Computer System: A computer equipped with the BCI software suite for real-time decoding of neural signals into control commands [25] [27].
- Calibration Software: Custom software for daily decoder calibration.
- Data Logging System: To record neural data, performance metrics, and user outcomes.
- Procedure:
- System Setup and Calibration: Each day, the participant dons the external headstage or connects wirelessly to the implant. A calibration routine is run where the participant is instructed to attempt specific motor imagery (e.g., moving a cursor left/right, attempting to speak) while the system records the corresponding neural patterns [25] [26].
- Decoder Training: Machine learning models are trained on the calibration data to create a personalized decoder that maps neural activity to intended outputs [2].
- Task Performance (Closed-Loop Control): The participant uses the trained decoder to perform functional tasks in a closed-loop setting. This includes:
- Data Collection and Outcome Measures:
- Long-Term Follow-up: Data is collected over months to years to assess system stability, performance improvement, and long-term safety [2] [26].
Protocol-Specific Visual Workflow
The following diagram details the specific workflow for chronic in-home BCI deployment and data collection as outlined in Protocol 2.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Components for BCI Research & Development
| Item / Component | Function / Rationale | Exemplar Product / Note |
|---|---|---|
| Implantable Electrode Array | The primary transducer for recording neural electrical activity; design dictates signal fidelity and longevity. | Utah Array (Blackrock) [25] [2], Stentrode (Synchron) [2], Connexus Micro-Electrodes (Paradromics) [27]. |
| Neural Signal Processor | Hardware for amplifying, filtering, and digitizing microvolt-level neural signals from electrodes. | Blackrock's headstage and acquisition hardware [25]. A critical component of the complete BCI ecosystem. |
| Biocompatible Materials | Ensures long-term safety and stability of the implant by minimizing immune response and tissue damage. | Use of titanium, platinum-iridium, and flexible, biocompatible polymers [27] [2]. |
| Decoding Software Suite | Machine learning algorithms to translate raw neural data into predicted user intent (e.g., movement, speech). | Advanced AI software for decoding intended speech or movement [27] [2]. |
| Surgical Tooling | Enables precise and repeatable implantation of the BCI device. | Robotic surgeon (Neuralink) [2] or standard neurosurgical tools for craniotomy. |
| (1,4-Dimethylpiperazin-2-yl)methanol | (1,4-Dimethylpiperazin-2-yl)methanol, CAS:14675-44-6, MF:C7H16N2O, MW:144.21 g/mol | Chemical Reagent |
| Diethylene glycol monostearate | Diethylene glycol monostearate, CAS:106-11-6, MF:C22H44O4, MW:372.6 g/mol | Chemical Reagent |
Brain-Computer Interface (BCI) technology, establishing a direct communication pathway between the human brain and external devices, is poised to fundamentally transform human-machine interaction [30] [31]. This field, progressing from foundational assistive applications to potential cognitive and sensory enhancement, represents a critical frontier in neurotechnology research and development. This document provides a detailed analysis of the projected market landscape from 2025 to 2040, examines the evolving policy and regulatory environment, and offers standardized experimental protocols for key BCI control applications. It is structured to serve researchers, scientists, and drug development professionals by synthesizing quantitative market data, delineating clear methodological frameworks, and cataloging essential research tools, thereby supporting advanced research within a broader thesis on BCI control applications.
Global Market Landscape and Growth Projections
The global BCI market is on a trajectory of significant expansion, driven by technological advancements, increasing investment, and the broadening of applications beyond healthcare into consumer and industrial sectors [30] [32]. Market analyses consistently project a robust Compound Annual Growth Rate (CAGR), with variations in absolute figures reflecting different methodological scopes and regional focuses. The following tables summarize key quantitative projections and market segmentations to facilitate comparative analysis.
Table 1: Global BCI Market Size Projections (2024-2040)
| Base Year (Value) | Projection Year (Value) | Compound Annual Growth Rate (CAGR) | Source / Region Focus |
|---|---|---|---|
| USD 2.09 Billion (2024) [33] | USD 8.73 Billion (2033) [33] | 15.13% [33] | Global Projection |
| USD 3.21 Billion (2025) [32] | USD 12.87 Billion (2034) [32] | 16.7% [32] | Global Projection |
| Not Specified | USD 70-200 Billion (2030-2040) [34] | Not Specified | McKinsey Global Forecast |
| ~RMB 1 Billion (2023) [34] | >RMB 120 Billion (2040) [34] | ~26% [34] | China Domestic Market |
Table 2: BCI Market Segmentation by Type, Application, and Region (2024-2025)
| Segmentation Category | Leading Segment | High-Growth Segment | Key Regional Leader | Fastest-Growing Region |
|---|---|---|---|---|
| Product Type | Non-Invasive BCIs (Largest share in 2024) [32] [33] | Invasive BCIs (Significant growth predicted) [32] | North America (Advanced infrastructure & key players) [32] [33] | Asia-Pacific (Projected fastest growth) [32] |
| Application | Healthcare (58.6% share in 2022) [32] | Smart Home Control (CAGR of 19.4%) [32] |
The market's momentum is fueled by several key drivers. The growing prevalence of neurodegenerative disorders (e.g., ALS, Parkinson's, spinal cord injuries) creates a pressing need for assistive and rehabilitative technologies [30] [32]. Concurrently, technological advancements in artificial intelligence (AI), machine learning (ML) for signal decoding, and miniaturization of wireless systems are enhancing BCI performance and usability [30] [31]. Increased funding from both government entities and private venture capital is further accelerating R&D and commercialization, with notable investments in companies like Neuralink, Synchron, and Precision Neuroscience [30] [31] [32].
Policy and Regulatory Initiatives
The regulatory landscape for BCI is complex and evolving, aiming to balance innovation with safety, efficacy, and ethical considerations. In the United States, the Food and Drug Administration (FDA) plays a pivotal role, exemplified by its "Breakthrough Device" program which accelerates the development and review of devices for life-threatening or irreversibly debilitating conditions [32]. Recent FDA approvals for limited commercial use of devices from companies like Precision Neuroscience mark significant regulatory milestones [32].
Globally, policy initiatives are increasingly recognizing BCI as a strategic technology. The European Union has its own regulatory frameworks for medical devices and data privacy that impact BCI development and deployment [30]. Notably, China's 14th Five-Year Plan (2021-2025) explicitly identified BCI as a key technology for the first time, emphasizing brain-machine fusion as a national priority and spurring regional support and industrial alliances [34]. This policy direction is catalyzing the growth of the domestic BCI ecosystem, involving major tech firms and research institutions.
Beyond medical device regulation, data privacy and security present a formidable regulatory challenge. The collection and interpretation of neural data raise profound questions about brain privacy and ownership [30] [32]. Cybersecurity threats to BCI devices, which could potentially allow malicious actors to manipulate a user's actions, are a critical concern that regulatory frameworks must address [32]. Furthermore, the potential for cognitive enhancement introduces complex ethical issues related to cognitive liberty, equity, and what it means to be human, necessitating ongoing dialogue among scientists, ethicists, and policymakers [30].
Experimental Protocols for BCI Control Applications
This section outlines standardized protocols for common BCI control paradigms, providing a reproducible methodology for research in this domain.
Protocol: P300-Based Spelling and Smart Home Control Application
1. Objective: To establish a non-invasive BCI system enabling users to communicate via a virtual keyboard and control basic smart home devices using the P300 event-related potential.
2. Materials and Reagents:
- EEG Acquisition System: A high-density EEG system (e.g., 32-channel or 64-channel) with active or passive electrodes.
- Electrolyte Gel: Conductive electrolyte gel to ensure impedance below 10 kΩ.
- Stimulus Presentation Software: Software capable of rendering a visual P300 speller matrix (e.g., 6x6 grid of characters and icons) and delivering precise timing markers.
- Signal Processing Unit: A computer with installed BCI software (e.g., BCI2000, OpenVibe) for real-time signal processing.
- Smart Home Interface: A custom API or middleware (e.g., based on IoT protocols like MQTT) to translate BCI commands into actions for devices like lights, TVs, or blinds.
3. Methodology: 1. Subject Preparation: Position the subject 60-80 cm from the visual stimulus monitor. Apply the EEG cap according to the 10-20 international system. Fill electrodes with conductive gel, focusing on sites Pz, Cz, and Oz, and ensure impedance is optimized. 2. System Calibration: Initiate a calibration run. Instruct the subject to focus on a pre-determined sequence of characters as they are highlighted. Record at least 10-15 repetitions of each target character to train a classifier (e.g., Linear Discriminant Analysis or Support Vector Machine). 3. Real-Time Operation: In the operational phase, the rows and columns of the speller matrix are randomly intensified. The system acquires EEG signals, extracts features (typically time-domain averaging or wavelet transforms), and applies the trained classifier to detect the P300 potential, thereby identifying the character or icon the user is focusing on. 4. Smart Home Integration: Map specific commands (e.g., "LIGHT ON," "TV OFF") to icons within the speller matrix. Upon selection, the BCI software triggers the corresponding command via the smart home interface.
4. Data Analysis: * Accuracy: Calculate the character selection accuracy as (Number of Correct Selections / Total Number of Selections) * 100. * Information Transfer Rate (ITR): Compute ITR in bits per minute to quantify communication bandwidth, accounting for both accuracy and speed.
Protocol: Motor Imagery (MI) for Neuroprosthetic Control
1. Objective: To implement a non-invasive BCI that decodes hand motor imagery (MI) patterns to control a robotic or prosthetic limb.
2. Materials and Reagents:
- EEG System: A multi-channel EEG system with a focus on sensors over the sensorimotor cortex (e.g., C3, Cz, C4).
- Visual Feedback Display: A monitor to provide real-time feedback on the MI task and prosthetic device state.
- Prosthetic Arm/Output Device: A robotic arm or a virtual representation that can be controlled via digital commands.
- Signal Processing Software: Software capable of processing sensorimotor rhythms (e.g., Mu/Beta rhythms) and running classification algorithms in real-time.
3. Methodology: 1. Subject Preparation & Screening: Apply the EEG cap as in Protocol 4.1. Screen the subject for their ability to generate distinct sensorimotor rhythm patterns during kinesthetic motor imagery (e.g., imagining squeezing a ball with the right hand). 2. Classifier Training: Conduct a training session. Present visual cues (e.g., arrows) instructing the subject to imagine either "Right-Hand Movement" or "Rest." Record EEG data for multiple trials (e.g., 80-100 trials per class). Use this data to train a spatial filter (e.g., Common Spatial Patterns) and a classifier to distinguish between the two mental states. 3. Closed-Loop Control with Feedback: In the closed-loop phase, the subject is presented with a goal (e.g., "grasp the object"). The system processes the EEG signals in real-time, applies the trained model, and translates the decoded intent into a proportional or discrete command for the prosthetic device. Visual feedback of the moving prosthetic is provided to the user to facilitate learning and improve control.
4. Data Analysis: * Offline Accuracy: Assess the classifier's performance using cross-validation on the calibration data. * Online Performance: Evaluate the success rate in completing specific tasks (e.g., reaching and grasping an object) within a time limit. * Electrophysiological Changes: Analyze event-related desynchronization (ERD) in the Mu/Beta bands over the contralateral sensorimotor cortex during MI.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials and their functions for BCI research, particularly for the protocols described above.
Table 3: Essential Research Reagents and Materials for BCI Experiments
| Item Name | Function / Application in BCI Research |
|---|---|
| Electroencephalography (EEG) System with Ag/AgCl Electrodes | The primary hardware for non-invasive recording of electrical activity from the scalp. Used for acquiring P300, Motor Imagery, and other evoked or spontaneous potentials [30]. |
| Conductive Electrolyte Gel | Improves electrical conductivity between the scalp and EEG electrodes, crucial for reducing impedance and obtaining high-quality, low-noise neural signals. |
| Electrocorticography (ECoG) Grid/Strip | A semi-invasive neural interface placed on the surface of the cortex. Offers higher spatial resolution and signal fidelity than EEG for more precise control applications [30]. |
| Intracortical Microelectrode Array (e.g., Utah Array) | Invasive neural interface implanted into the cortex to record single-neuron or multi-unit activity. Provides the highest signal resolution for complex prosthetic control [30]. |
| Signal Processing & BCI Software Platform (e.g., BCI2000, OpenVibe) | Software environment for designing experiments, acquiring data, implementing real-time signal processing pipelines (filtering, feature extraction, classification), and providing feedback. |
| Stimulus Presentation Software (e.g., Psychtoolbox, Presentation) | Software for rendering and controlling visual, auditory, or somatosensory stimuli with millisecond precision, ensuring accurate synchronization with neural data acquisition. |
| Classifiers (LDA, SVM, Deep Learning Models) | Algorithms that translate extracted neural features into device control commands. LDA and SVM are common for P300 and MI; deep learning is emerging for more complex decoding [32]. |
| Methyl-1,2-cyclopentene oxide | Methyl-1,2-cyclopentene oxide, CAS:16240-42-9, MF:C6H10O, MW:98.14 g/mol |
| N-(6-FORMYLPYRIDIN-2-YL)PIVALAMIDE | N-(6-FORMYLPYRIDIN-2-YL)PIVALAMIDE, CAS:372948-82-8, MF:C11H14N2O2, MW:206.24 g/mol |
BCI Experimental Workflow and Signaling Pathway
The following diagram illustrates the logical flow and core components of a standard BCI experiment, from signal acquisition to closed-loop feedback.
Diagram 1: BCI System Workflow. The process is a closed loop, beginning with Neural Signal Generation (e.g., from a user performing motor imagery), which is captured by Signal Acquisition Hardware. The raw data undergoes Preprocessing and Feature Extraction before a Classification/Decoding algorithm translates the neural patterns into a Device Command. The resulting User Feedback completes the loop, allowing the user to adapt their brain activity, a process known as neurofeedback or closed-loop learning.
From Signal to Action: BCI Methodologies and Their Transformative Medical Applications
In Brain-Computer Interface (BCI) research, the efficacy of control applications is fundamentally constrained by the signal-to-noise ratio (SNR) of neural recordings. Electroencephalography (EEG), a predominant non-invasive BCI modality, is particularly susceptible to contaminating artifacts of both physiological and non-physiological origin. These artifacts can obscure critical neural patterns, thereby degrading BCI performance and reliability. Consequently, advanced signal processing techniques for artifact removal are indispensable for enhancing the fidelity of neural signals. This application note provides a detailed examination of three cornerstone methodologies—Independent Component Analysis (ICA), Wavelet Transform (WT), and Canonical Correlation Analysis (CCA)—framed within the context of BCI control applications. We elucidate the underlying principles, present structured experimental protocols, and offer a comparative analysis to guide researchers and scientists in selecting and implementing optimal artifact removal strategies for their specific BCI paradigms.
Theoretical Foundations of Artifact Removal Techniques
Independent Component Analysis (ICA)
ICA is a blind source separation (BSS) technique that decomposes a multivariate signal into additive, statistically independent sub-components. The core assumption is that the recorded multi-channel EEG signal is a linear mixture of independent sources originating from the brain and various artifactual sources (e.g., ocular movements, muscle activity, cardiac rhythms). The model is formalized as X = AS, where X is the observed data matrix, A is the unknown mixing matrix, and S contains the underlying independent sources. The objective of ICA is to find a de-mixing matrix W such that Y = WX provides an estimate of the original source signals S [35] [14].
A critical step in ICA-based artifact removal is the identification and rejection of artifactual components. This often relies on measuring the non-Gaussianity of the components, frequently approximated using negentropy (J(y) = H(yGauss) - H(y)), where H is the differential entropy. Components with high negentropy are typically considered non-Gaussian and are candidates for being neural signals, though certain artifacts like eye blinks also exhibit high non-Gaussianity, necessitating careful inspection [35]. While powerful, ICA requires manual or semi-automated component classification, can be computationally intensive, and its performance is sensitive to the amount of available data [14].
Wavelet Transform (WT)
Wavelet Transform provides a multi-resolution analysis of a signal by decomposing it into basis functions (wavelets) that are localized in both time and frequency. This is a significant advantage over Fourier-based methods for processing non-stationary signals like EEG. The Discrete Wavelet Transform (DWT) is commonly used, employing a series of high-pass and low-pass filters to break down a signal into approximation (low-frequency) and detail (high-frequency) coefficients at different scales [36] [14].
Denoising in the wavelet domain typically involves thresholding the detail coefficients associated with noise. A common hybrid approach combines DWT with scalar quantization (DWTSQ) to both denoise and compress EEG signals, improving transmission efficiency in wireless BCI systems [36]. Advanced variants, such as denoising in the fractional wavelet domain using adaptive models, have been developed to better preserve the non-stationary and quasi-stationary components of the EEG while effectively removing noise [37]. The choice of the mother wavelet and the thresholding function (e.g., soft, hard) are critical parameters that influence the denoising performance.
Canonical Correlation Analysis (CCA)
While CCA is widely known as a feature extraction method for Steady-State Visual Evoked Potentials (SSVEPs), it also serves as a robust tool for artifact removal. CCA is a multivariate statistical method that finds linear combinations of two sets of variables that maximize the correlation between them. In the context of artifact removal, CCA can separate neural activity from artifacts by maximizing the correlation between the EEG signal and reference signals, thereby isolating artifact components [14].
Its utility is further demonstrated in hybrid spatial filtering methods. For instance, the CCA of Task-Related Components (CCAoTRC) method applies a spatial filter derived from Task-Related Component Analysis (TRCA) to enhance the SNR of the data before employing CCA for frequency recognition. This hybrid approach has been shown to be particularly effective for data recorded outside electromagnetic shields, making it suitable for real-world BCI applications [38].
Application Notes and Comparative Analysis
The selection of an appropriate artifact removal technique is highly dependent on the specific BCI paradigm, the nature of the artifacts, and the required signal integrity for downstream decoding tasks.
Table 1: Comparative Analysis of Artifact Removal Techniques in BCI Applications
| Technique | Primary Mechanism | Best-Suited BCI Paradigms | Key Advantages | Key Limitations |
|---|---|---|---|---|
| ICA | Blind source separation into independent components. | P300, Motor Imagery, general pre-processing. | Effective separation of neural and artifactual sources; does not require reference signals [39]. | Manual component classification is often needed; computationally intensive; performance depends on data quantity [14]. |
| Wavelet Transform | Multi-resolution time-frequency analysis and thresholding. | Epileptic spike detection, P300, data compression for transmission [36] [37]. | Preserves temporal localization of transients; suitable for non-stationary signals; allows for signal compression. | Selection of wavelet basis and threshold is critical and can be complex; may distort signal if not optimized [14]. |
| Canonical Correlation Analysis (CCA) | Maximizes correlation with reference signals or between signal subsets. | SSVEP frequency recognition, artifact removal in noisy environments [38] [14]. | High efficiency and robustness; can be combined with individual calibration data to improve performance [40]. | Standard CCA may be sensitive to noise; reference signals may not capture all individual variations. |
| Hybrid Methods (e.g., CCAoTRC, H-TRCCA) | Combines spatial filtering (e.g., TRCA) with CCA. | SSVEP, especially with limited training data or low SNR [38] [41]. | Leverages strengths of multiple methods; superior performance and robustness with limited calibration data [41]. | Increased algorithmic complexity; may require calibration data. |
Table 2: Impact of Artifact Removal on BCI Performance Metrics
| Study Focus | Technique Used | Key Performance Outcome | Implication for BCI Control |
|---|---|---|---|
| Robustness of ICA Artifact Removal [39] | Automated ICA Classifier | Little influence on average BCI performance with state-of-the-art methods; strong individual variation when using slow motor-related features. | Highlights the need for personalized processing pipelines, especially in motor rehabilitation BCIs. |
| SSVEP Recognition with Limited Data [41] | Hybrid H-TRCCA (CCA+TRCA) | Achieved 91.44% accuracy and 188.36 bits/min ITR using only two training trials. | Enables faster setup and higher usability for SSVEP-based communication and control systems. |
| Denoising for Signal Transmission [36] | DWT based Scalar Quantization | Improved SNR and classification accuracy for transmitted EEG signals. | Critical for the development of robust wireless and wearable BCI systems. |
| SSVEP in Noisy, Real-World Conditions [38] | CCAoTRC (CCA with TRC spatial filter) | Increased Wide-band SNR by 0.66 dB; achieved 70.94% accuracy in non-shielded environments. | Facilitates the deployment of practical BCIs outside controlled laboratory settings. |
The following workflow diagram illustrates a recommended, multi-stage approach for artifact removal in a BCI system, integrating the discussed techniques.
Experimental Protocols
Protocol 1: ICA for Ocular and Muscle Artifact Removal
This protocol is designed for the removal of common physiological artifacts, such as those from eye blinks (EOG) and muscle activity (EMG), from continuous EEG data.
1. Preprocessing:
- Data Import: Load raw EEG data (e.g., .set, .edf, or .xls format).
- Filtering: Apply a bandpass filter (e.g., 1-40 Hz) to remove DC offset and high-frequency noise.
- Re-referencing: Re-reference the data to the average of all electrodes or a specific reference (e.g., mastoids).
2. ICA Decomposition:
- Execute ICA decomposition using an algorithm such as Infomax or FastICA. The input is the preprocessed, multi-channel EEG data matrix.
- Critical parameters include the stopping convergence value (e.g., 1e-7) and maximum number of iterations (e.g., 1000).
3. Component Classification:
- Visualize independent components (ICs) by their topography, time course, and frequency spectrum.
- Identify artifactual components:
- Ocular Artifacts: Characterized by strong frontal scalp maps and large, low-frequency deflections in the time series.
- Muscle Artifacts: Exhibit high-frequency "spiky" activity in the time series and a broadband frequency spectrum.
- Utilize automated classifiers (e.g., ICLabel, EEGLAB plug-ins) or manual expert labeling to flag components for rejection [39].
4. Signal Reconstruction:
- Project the data back to the sensor space, excluding the artifactual components. This involves multiplying the de-mixing matrix Wâ»Â¹ by the source matrix S with the artifact components set to zero.
Protocol 2: Wavelet-Based Denoising for P300 Enhancement
This protocol focuses on enhancing the SNR of event-related potentials like the P300, which is crucial for P300 spellers.
1. Signal Preparation:
- Epoching: Segment the continuous EEG into epochs time-locked to the stimulus onset (e.g., -100 ms to 800 ms).
- Baseline Correction: Remove the mean baseline (-100 ms to 0 ms) from each epoch.
2. Wavelet Decomposition:
- Select a mother wavelet (e.g., Daubechies 4 'db4' is often suitable for EEG).
- Decompose each single-trial epoch into multiple levels (e.g., 5-8 levels) using DWT, producing one set of approximation coefficients and multiple sets of detail coefficients.
3. Thresholding and Denoising:
- Apply a thresholding rule (e.g., adaptive thresholding based on negentropy as in [35] or Stein's Unbiased Risk Estimate (SURE)) to the detail coefficients at each level.
- Use a thresholding function (soft or hard) to suppress coefficients below the threshold, which are presumed to be noise.
4. Signal Reconstruction:
- Reconstruct the denoised single-trial P300 epoch from the thresholded wavelet coefficients using the inverse DWT.
- Average the denoised single-trials to obtain a clean ERP waveform with an enhanced P300 component.
Protocol 3: Hybrid CCA-TRCA for SSVEP Recognition
This protocol outlines a hybrid method for robust SSVEP target identification, which inherently handles artifacts through optimized spatial filtering.
1. Data Preparation and Preprocessing:
- Training Data: Collect calibration data where the user focuses on known, flickering targets.
- Epoching: Segment EEG data into trials corresponding to each stimulation event.
- Filter Bank Decomposition (Optional): Decompose the EEG signals into sub-band components (e.g., covering harmonics) to leverage filter bank analysis [40].
2. Spatial Filter Construction:
- TRCA Filter: Compute a spatial filter W_TRCA that maximizes the inter-trial covariance of the training data for each stimulus frequency, enhancing task-related components [41].
- CCA Reference Templates: Generate reference signals Y for each stimulus frequency
fas sine-cosine pairs at the fundamental and harmonic frequencies: Y = [sin(2Ï€ft), cos(2Ï€ft), ..., sin(2Ï€Nhft), cos(2Ï€Nhft)]áµ€.
3. Target Identification during Testing:
- For a test epoch X, calculate the correlation coefficients between the spatially filtered test data and the reference signals for all possible frequencies.
- Candidate Selection: Use a clustering algorithm (e.g., k-means++) on the correlation coefficients to identify candidate stimuli with the highest average correlations [41].
- Decision Making: For each candidate stimulus, sum the correlation values from CCA-based filters and combine them with the correlation coefficient from the TRCA-based filter. The target frequency is identified as the one with the highest combined correlation value.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for BCI Artifact Removal Research
| Resource Category | Specific Tool / Software / Dataset | Function in Research |
|---|---|---|
| Software & Libraries | EEGLAB (with ICLabel, PREP pipeline) | Provides a complete interactive environment for ICA, including decomposition, visualization, and automated component labeling [39]. |
| BCILAB, MNE-Python | Offers comprehensive toolboxes for BCI research, including implementations of CCA, TRCA, and wavelet analysis. | |
| MATLAB Signal Processing Toolbox, PyWavelets | Supplies built-in functions for performing Discrete Wavelet Transform and various thresholding techniques. | |
| Benchmark Datasets | BCI Competition Datasets (e.g., 2003, P300) | Standardized data for developing and benchmarking denoising algorithms, such as for P300 enhancement [35]. |
| Benchmark Dataset (Wang et al., 2016) | Contains SSVEP data from 35 subjects, essential for validating SSVEP frequency recognition methods like H-TRCCA [41]. | |
| BETA Dataset (Liu et al., 2020) | Comprises SSVEP data from 70 subjects recorded in a non-laboratory environment, ideal for testing robustness and real-world applicability [38] [41]. | |
| Hardware & Acquisition | High-density EEG Systems (64+ channels) | Provides sufficient spatial information for effective source separation using ICA and spatial filtering techniques. |
| Wearable, Wireless EEG Headsets | Target systems for which efficient denoising and compression algorithms (e.g., DWTSQ) are developed [36]. | |
| 2-Ethyl-6-nitroquinolin-4-amine | 2-Ethyl-6-nitroquinolin-4-amine, CAS:1388727-03-4, MF:C11H11N3O2, MW:217.22 g/mol | Chemical Reagent |
| (4-Bromo-3-methylphenyl)thiourea | (4-Bromo-3-methylphenyl)thiourea |
The evolution of Brain-Computer Interfaces (BCIs) represents one of the most significant advancements at the intersection of neuroscience and artificial intelligence. At the core of this technology lies the challenge of accurately interpreting neural activity to enable direct communication between the brain and external devices. This process critically depends on sophisticated computational pipelines for feature extraction and intent decoding – the translation of raw, often noisy, brain signals into actionable commands. The performance of modern BCIs hinges on deploying advanced machine learning (ML) and deep learning (DL) algorithms that can navigate the complexities of neural data. These methodologies are foundational to developing clinical-grade neurotechnology for conditions such as amyotrophic lateral sclerosis (ALS), spinal cord injuries, and stroke, offering a pathway to restore communication and mobility for severely paralyzed individuals [2] [42].
Theoretical Foundations of Neural Signal Processing
The BCI pipeline systematically converts brain signals into device control, comprising stages of signal acquisition, preprocessing, feature extraction, decoding, and output with feedback.
The BCI Signal Processing Pipeline
A standardized BCI pipeline involves sequential stages: signal acquisition (collecting raw neural data), pre-processing (filtering and artifact removal), feature extraction (identifying discriminative patterns), decoding/classification (translating features into intent), and output with feedback (executing commands and providing user feedback) [2]. This closed-loop architecture is the backbone of current BCI research, enabling users to adapt their mental strategies based on system performance.
Signal Acquisition Paradigms
Brain signals can be captured through various modalities, each with distinct trade-offs between invasiveness and spatial-temporal resolution. Electroencephalography (EEG), a non-invasive technique, measures electrical potentials from the scalp and is widely used due to its portability and high temporal resolution [43] [17]. In contrast, intracortical microelectrode arrays (e.g., the Utah array or Neuralink's chip) are implanted directly into the brain tissue, providing high-fidelity signals from individual neurons but requiring neurosurgery [2]. Endovascular BCIs (e.g., Synchron's Stentrode) offer a middle ground, recording cortical signals from within blood vessels with minimal invasiveness [2]. The choice of acquisition modality directly influences the subsequent design of feature extraction and decoding algorithms.
Mathematical Representation of Neural Signals
Multichannel neural signals are formally represented as a matrix \(\mathscr{X} \in {R}^{C \times T}\), where \(C\) denotes the number of channels (electrodes) and \(T\) represents the temporal dimension [43]. Each element \(x_{c,t}\) corresponds to the electrical potential measured at channel \(c\) at time point \(t\). The observed signal is a composite of neural activity and noise, modeled as:
where \(s_s(t)\) represents the \(s^{th}\) source signal, \(a_{c,s}\) is its mixing coefficient at channel \(c\), and \(η_{c,t}\) represents measurement noise [43]. This formulation underpins the development of advanced signal processing techniques for source separation and noise reduction.
Machine Learning and Deep Learning Architectures for BCIs
Traditional Machine Learning Approaches
Before the rise of deep learning, BCI systems predominantly relied on classical machine learning techniques coupled with hand-crafted features. Common Spatial Patterns (CSP) and its extension, Filter Bank CSP (FBCSP), have been dominant feature extraction methods for motor imagery tasks, designed to maximize the variance between two classes of neural signals [43]. These spatial features were typically classified using algorithms such as Linear Discriminant Analysis (LDA) and Support Vector Machines (SVM), which achieved accuracies of 65-80% for binary classification problems but often plateaued due to the high-dimensional, non-stationary nature of EEG signals [43].
Deep Learning Architectures
Deep learning has revolutionized neural signal processing by enabling end-to-end learning from raw or minimally processed data, automatically discovering optimal feature representations.
Convolutional Neural Networks (CNNs): These architectures excel at extracting spatially invariant features, mimicking the brain's hierarchical processing. For EEG classification, models like EEGNet, ShallowNet, and DeepCovNet use convolutional layers to learn spatial filters that discriminate between different mental states [42]. CNNs have demonstrated comparable or superior performance to traditional methods without requiring hand-crafted features [43].
Recurrent Neural Networks (RNNs): Long Short-Term Memory (LSTM) networks, a variant of RNNs, are particularly effective at modeling the temporal dynamics and oscillatory patterns characteristic of neural signals [43] [42]. Their ability to learn long-range dependencies makes them suitable for capturing the evolving nature of brain activity during motor imagery or speech processes.
Hybrid Architectures: Combining CNNs and RNNs creates models that leverage both spatial and temporal information. A CNN-LSTM hybrid uses convolutional layers for spatial feature extraction from multi-channel EEG inputs, followed by LSTM layers to model temporal sequences, significantly outperforming individual CNN or LSTM models [43].
Attention-Enhanced Networks: The integration of attention mechanisms represents a recent advancement, allowing models to selectively weight different spatial locations and temporal segments based on their relevance. This biomimetic approach mirrors the brain's own selective processing strategies. One study demonstrated that a hierarchical attention-enhanced convolutional-recurrent framework achieved a state-of-the-art accuracy of 97.25% on a four-class motor imagery dataset, highlighting the transformative potential of attention for capturing task-relevant neural signatures [43].
Table 1: Performance Comparison of Select Deep Learning Architectures for Motor Imagery Classification
| Architecture | Key Features | Reported Accuracy | Application Context |
|---|---|---|---|
| Attention-enhanced CNN-RNN [43] | Spatial feature extraction, temporal modeling, and adaptive feature weighting | 97.25% (4-class MI) | Motor Imagery Classification |
| CNN-LSTM Hybrid [43] | Spatiotemporal feature learning | Superior to individual CNN/LSTM | Motor Imagery Classification |
| EEGNet [42] | Compact CNN for EEG-based BCIs | Comparable to traditional methods | General BCI Paradigms |
Application Notes and Experimental Protocols
This section provides detailed methodologies for implementing and validating feature extraction and intent decoding algorithms in specific BCI applications.
Protocol 1: Decoding Inner Speech from Motor Cortex Signals
This protocol details the methodology based on the Stanford University study that successfully decoded inner speech (imagined speech) from intracortical signals in participants with severe paralysis [44] [21].
Background and Objective
Objective: To decode inner speech from neural activity in the motor cortex and develop safeguards against the unintentional decoding of private thoughts. Rationale: Inner speech BCIs could offer a more natural and less physically effortful communication channel for people with paralysis compared to systems requiring attempted speech [21].
Experimental Workflow
The experimental process for decoding inner speech involves participant preparation, data acquisition, model training, and real-time decoding with privacy safeguards.
Materials and Reagents
Table 2: Research Reagent Solutions for Invasive Speech BCI Research
| Item | Specification / Function |
|---|---|
| Microelectrode Arrays [44] [21] | Intracortical arrays (e.g., Utah Array), smaller than a pea, implanted on the brain surface to record single-unit and multi-unit activity. |
| Neural Signal Amplifier | High-channel-count amplifier for acquiring raw neural data from implanted arrays. |
| Data Acquisition System | System with high sampling rate (>30 kHz) to capture neural signals and timestamps for stimulus presentation. |
| Custom Decoding Software | Machine learning software (e.g., based on RNNs or LSTMs) to map neural features to phonemes or words. |
| Privacy Lock Software | Algorithm to distinguish attempted from inner speech or detect a specific unlock phrase [44]. |
Data Analysis and Interpretation
The Stanford study reported error rates between 14% and 33% for a 50-word vocabulary during real-time sentence decoding [44]. A key finding was that attempted and inner speech evoked similar neural patterns in the motor cortex, but attempted speech generated stronger signals, providing a neural basis for distinguishing intended communication [44] [21]. The privacy safeguard models successfully prevented unintentional decoding, with a keyword recognition rate exceeding 98% [44].
Protocol 2: AI-Enhanced Non-Invasive BCI for Robotic Control
This protocol outlines the UCLA study that integrated an AI co-pilot with a non-invasive EEG-based BCI to improve the control of a robotic arm [45].
Background and Objective
Objective: To develop a non-invasive BCI system that uses an AI co-pilot to infer user intent and significantly improve task performance. Rationale: To overcome the performance limitations of non-invasive BCIs without the risks associated with surgical implantation [45].
Experimental Workflow
The system combines decoded EEG signals with a computer vision-based AI that interprets the user's intent and the task environment context.
Materials and Reagents
Table 3: Research Reagent Solutions for AI-Enhanced Non-Invasive BCI
| Item | Specification / Function |
|---|---|
| High-Density EEG System [45] | Wearable cap with multiple electrodes (e.g., 64-channel) for recording scalp potentials. |
| Custom Decoder Algorithms [45] | Algorithms (e.g., based on CNNs) to decode movement intentions from noisy EEG signals. |
| AI Co-Pilot System [45] | Camera-based AI platform that observes the environment and infers user goals (e.g., block positioning). |
| Robotic Arm System | A multi-degree-of-freedom robotic arm for executing physical tasks. |
| Stimulus Presentation Setup | Screen for cursor tasks or physical workspace for object manipulation. |
Data Analysis and Interpretation
The study quantified performance by the time taken to complete tasks. All participants completed the cursor-target and block-moving tasks significantly faster with AI assistance [45]. Notably, the paralyzed participant completed the robotic arm task in approximately 6.5 minutes with AI, whereas they were unable to finish the task without it, demonstrating a profound functional improvement [45].
Protocol 3: High-Accuracy Motor Imagery Classification with Attention Models
This protocol is based on the research that achieved state-of-the-art results on EEG motor imagery classification using a hierarchical attention-enhanced deep learning model [43].
Background and Objective
Objective: To design and validate a novel deep learning architecture that synergistically integrates spatial, temporal, and attention mechanisms for high-accuracy motor imagery classification. Rationale: Motor imagery is a major non-invasive BCI paradigm, but its clinical deployment is limited by decoding accuracy and robustness. Overcoming the low signal-to-noise ratio of EEG requires advanced models that can focus on task-relevant neural patterns [43].
Model Architecture and Workflow
The proposed framework is a tripartite architecture that processes EEG signals through parallel pathways for spatial, temporal, and joint spatiotemporal feature learning, followed by an attention-based fusion and classification head.
Materials and Reagents
Table 4: Research Reagent Solutions for Advanced Motor Imagery BCI
| Item | Specification / Function |
|---|---|
| EEG Recording System [43] | Research-grade EEG system with sufficient channels (e.g., >32) and sampling rate (>250 Hz). |
| Public MI Dataset [43] | Curated dataset (e.g., BCI Competition datasets) for benchmarking, containing multiple trials of MI tasks. |
| Deep Learning Framework | Software environment like TensorFlow or PyTorch for implementing and training complex models. |
| High-Performance Computing Unit | GPU cluster for efficient training of deep learning models, which can be computationally intensive. |
Data Analysis and Interpretation
The study reported a classification accuracy of 97.25% on a custom four-class motor imagery dataset comprising 4,320 trials from 15 participants [43]. Ablation studies confirmed the critical role of the attention mechanism in boosting performance by enabling the model to focus on the most salient spatiotemporal features of the EEG signal, effectively mitigating the low signal-to-noise ratio challenge [43].
The integration of sophisticated machine learning and deep learning algorithms has dramatically advanced the capabilities of BCIs in feature extraction and intent decoding. From enabling communication via inner speech to providing precise control of external devices through non-invasive systems, these technologies are pushing the boundaries of restorative neurotechnology. The experimental protocols detailed herein provide a framework for replicating and building upon these cutting-edge results. As the field progresses, key challenges remain, including improving the generalizability of models across subjects and sessions, enhancing the long-term stability of implanted systems, and developing robust ethical frameworks for neural data privacy. The convergence of higher-fidelity neural interfaces, more powerful AI algorithms, and a deeper understanding of brain function promises to usher in a new era of BCI applications that will fundamentally transform the lives of individuals with neurological impairments.
Application Notes: BCI for Communication Restoration
Clinical Context and User Profiles
Brain-Computer Interfaces (BCIs) offer a direct communication pathway for individuals with severe paralysis resulting from conditions such as locked-in syndrome (LIS), amyotrophic lateral sclerosis (ALS), and spinal cord injury (SCI) [46]. These systems are particularly vital for populations who have lost all voluntary muscle control, including eye movement, a state known as complete LIS, and for whom traditional augmentative and alternative communication (AAC) devices are no longer viable [46]. The primary aim is to restore the ability to communicate with family and caregivers, a factor critically linked to the subjective well-being of affected individuals [46].
Performance Data of Representative Communication BCIs
Table 1: Performance of Select BCI Systems for Communication Restoration
| Neural Signal / Platform | User Population | Key Performance Metrics | Notable Advantages |
|---|---|---|---|
| Intracortical Local Field Potentials (LFPs) [47] | ALS and LIS due to brain stem stroke | Spelling rates of 3.07 and 6.88 correct characters/minute over 76 and 138 days respectively [47] | Long-term stability without recalibration; suitable for everyday use [47] |
| P300 Evoked Potentials [46] | LIS individuals | Used for spelling and choice-based communication applications [46] | Adaptable to visual, auditory, and vibrotactile modalities [46] |
| Endovascular Stentrode (Synchron) [2] | Patients with paralysis | Enabled text-based communication; no serious adverse events at 12 months in a four-patient trial [2] | Minimally invasive implantation via blood vessels [2] |
| Motor/Speech Imagery Decoding [46] | LIS individuals | Demonstrated decoding of attempted speech and movements from neural signals [46] | Leverages intuitive neural correlates of speech and movement attempts [46] |
Experimental Protocol: P300 Speller BCI for Communication
This protocol outlines the methodology for establishing a P300-based spelling system, a common paradigm for communication BCIs [46].
Objective: To enable a user with LIS to communicate by selecting characters on a virtual keyboard using P300 event-related potentials.
Materials and Setup:
- Signal Acquisition: A non-invasive EEG system with at least 16 electrodes, positioned according to the international 10-20 system, focused over central and parietal areas.
- Stimulus Presentation: A computer screen displaying a 6x6 matrix of alphanumeric characters and commands.
- Software: BCI2000 or OpenVibe platforms for stimulus presentation, signal processing, and classifier training.
Procedure:
- Preparation and Calibration:
- Position the user comfortably in front of the screen. Explain the task and ensure the EEG cap has good impedance.
- In the calibration phase, rows and columns of the character matrix are highlighted in a random sequence. The user is instructed to mentally count the number of times a target character flashes.
- Record EEG data for 15-20 trials per character to gather training data for the classifier.
Signal Processing and Classification:
- Preprocessing: Apply a band-pass filter (e.g., 0.1-20 Hz) to the raw EEG and segment epochs from 0 to 600 ms post-stimulus.
- Feature Extraction: Down-sample the epochs and normalize the data.
- Classification: Train a linear discriminant analysis (LDA) or support vector machine (SVM) classifier to distinguish between target (P300 present) and non-target (P300 absent) stimuli.
Online Operation:
- The system flashes rows and columns. The classifier analyzes the EEG in real-time after each flash.
- The character at the intersection of the row and column that elicits the strongest P300 response is selected as the output.
- Provide clear feedback to the user by displaying the selected character.
Considerations: Session length should be managed to avoid cognitive fatigue. The interface appearance and flashing parameters may be adjusted for optimal user comfort and performance [48].
Diagram 1: BCI Communication Workflow
Application Notes: BCI for Mobility Restoration
Clinical Context and Technological Approaches
BCIs for mobility restoration aim to bypass damaged neural pathways to control external devices or directly activate muscles. Applications include controlling robotic arms, motorized wheelchairs, and, most notably, enabling the restoration of limb and facial movements through functional electrical stimulation (FES) [46]. This BCI-FES approach creates an "electronic neural bypass," using decoded brain signals to trigger FES systems that activate paralyzed muscles, thereby restoring functional movement [46].
Performance Data of Representative Mobility BCIs
Table 2: Performance of Select BCI Systems for Mobility Restoration
| System / Approach | Application | Key Performance Metrics | Notable Advantages |
|---|---|---|---|
| BCI-FES Hybrid System [46] | Restoration of limb and facial movements | Successful applications shown in stroke and spinal cord injury; proposed for LIS [46] | Enriches communication with body language; can restore simple to complex movements [46] |
| High-Channel-Count Implants (e.g., Paradromics) [2] | Restoring speech and device control | Connexus BCI uses 421 electrodes; first-in-human recording performed in 2025 [2] | Ultra-fast data transmission for complex control [2] |
| Ultra-High-Bandwidth Implant (Neuralink) [2] | Control of digital and physical devices | As of 2025, five individuals with severe paralysis are using the device [2] | Records from a large number of neurons [2] |
| Motor Imagery / Attempt Decoding [46] | Continuous control of devices (e.g., wheelchair) | Decoding of motor attempts from neural signals for real-time control [46] | Leverages intuitive neural correlates of movement [46] |
Experimental Protocol: BCI-FES for Hand Grasp Restoration
This protocol describes a methodology for combining a BCI with FES to restore a basic hand grasp function in an individual with tetraplegia.
Objective: To enable the user to open and close their hand by decoding movement attempts from motor cortex signals to trigger FES of forearm muscles.
Materials and Setup:
- Signal Acquisition: An implantable BCI system (e.g., using intracortical arrays or ECoG) for high-fidelity signal recording from the hand area of the motor cortex. Alternatively, a high-density EEG system can be used non-invasively.
- FES System: A functional electrical stimulator with surface electrodes placed on the forearm over the finger and wrist extensor and flexor muscles.
- Software: Custom software for real-time signal processing and a calibrated model to map neural features to FES commands.
Procedure:
- System Calibration:
- The user is asked to attempt a hand grasp movement repeatedly while neural activity is recorded.
- Simultaneously, the FES system is manually triggered to produce the desired grasp movement. This provides labeled data for the decoder.
- Features (e.g., power in specific frequency bands from motor cortex signals) are extracted and used to train a decoder (e.g., linear regression) that predicts the user's movement intent.
Closed-Loop Operation:
- The trained decoder runs in real-time. When the user attempts a hand grasp, the decoder identifies the specific neural pattern.
- Upon successful detection, the BCI system sends a command to the FES device.
- The FES device delivers a patterned electrical stimulation to the forearm muscles, resulting in a functional hand grasp.
Feedback and Adaptation:
- The user receives visual and proprioceptive feedback from their own moving hand, facilitating neuroplasticity and improved control.
- The decoder may be recalibrated periodically to adapt to changes in the user's neural signals or to improve performance.
Considerations: Muscle fatigue must be managed with appropriate rest periods. Electrode placement for FES is critical and requires expertise.
Diagram 2: BCI-FES Mobility Workflow
The Scientist's Toolkit: Research Reagents & Materials
Table 3: Essential Research Materials for BCI Experimentation
| Item | Function / Application in BCI Research |
|---|---|
| Electroencephalography (EEG) Systems [46] [49] | Non-invasive recording of electrical brain activity from the scalp; foundational for most non-invasive BCI paradigms. |
| Electrocorticography (ECoG) Grids/Strips [49] | Invasive recording of electrical activity directly from the cortical surface; provides higher spatial resolution and signal quality than EEG. |
| Intracortical Microelectrode Arrays (e.g., Utah Array) [47] [2] | Implanted arrays that record action potentials and local field potentials from populations of neurons; used for high-precision decoding. |
| Functional Electrical Stimulation (FES) System [46] | Delivers electrical currents to peripheral nerves or muscles to elicit contractions; used in hybrid BCI-FES systems to restore movement. |
| P300 Speller Paradigm Software [46] | Standardized software for presenting visual oddball stimuli and classifying P300 evoked potentials for communication BCIs. |
| Signal Processing & Machine Learning Toolboxes (e.g., BCI Toolbox in Python) [50] | Software suites for preprocessing neural data, extracting features, and training decoding models (e.g., for Bayesian causal inference). |
| Eye-Tracking Systems [46] | Often used in hybrid interfaces to provide an additional input modality or to validate BCI performance against a reliable control signal. |
| 3-(4-Hydroxy-phenoxy)-benzaldehyde | 3-(4-Hydroxy-phenoxy)-benzaldehyde|CAS 82186-80-9 |
| O-(3-quinolyl)methylhydroxylamine | O-(3-Quinolyl)methylhydroxylamine|Research Chemical |
Brain-computer interfaces represent a transformative technology in neurorehabilitation by establishing direct communication pathways between the brain and external devices. These systems operate through a closed-loop architecture that acquires neural signals, decodes intended actions, and executes commands through assistive or restorative devices while providing real-time feedback to users [2]. In clinical applications for stroke and neurological disorders, BCIs primarily function through three established paradigms: motor imagery-based BCIs, movement-attempt-based BCIs, and sensorimotor-rhythm-based BCIs [51]. The selection of appropriate BCI paradigms depends on multiple factors including the patient's residual neural pathways, clinical goals, and available technology infrastructure.
Current research demonstrates that BCI technology holds significant promise for improving motor rehabilitation in stroke patients, with clinical studies showing immediate improvements in motor functions [51]. The technology has evolved from purely assistive applications to include restorative functions that promote neuroplasticity through intensive, engaged rehabilitation protocols. The global BCI market reflects this growing importance, with projections estimating growth from USD 2.41 billion in 2025 to USD 12.11 billion by 2035, representing a compound annual growth rate of 15.8% [52]. This growth is largely driven by healthcare applications, particularly in addressing neurological conditions such as stroke, epilepsy, and Parkinson's disease.
BCI Control Paradigms: Technical Specifications and Applications
Comparative Analysis of BCI Approaches
Table 1: Technical comparison of primary BCI control paradigms for neurorehabilitation
| Parameter | Motor Imagery-Based BCI | Movement-Attempt-Based BCI | Sensorimotor-Rhythm-Based BCI |
|---|---|---|---|
| Neural Basis | Mental rehearsal of movement without physical execution | Effort or desire to move regardless of physical capability | Modulation of oscillatory patterns in sensorimotor cortex |
| Signal Features | Event-related desynchronization/synchronization (ERD/ERS) in mu/beta rhythms | Movement-related cortical potentials (MRCPs) | Beta rebound (ERS) following movement imagination |
| Typical Accuracy | 60-80% with feedback [51] | Higher than MI-BCI for motor skills [51] | Varies based on induction strategies |
| Clinical Advantages | Safe for patients with minimal movement capacity; activates motor circuits | Reinforces motor command generation; more intuitive for some patients | Can utilize haptic or visual stimuli to enhance performance |
| Patient Population | Severe to moderate motor impairment | Moderate to mild impairment where movement attempt is possible | Wide range, including lower limb applications |
| Feedback Modalities | Visual (avatars), robotic movement, functional electrical stimulation | Robotic devices, exoskeletons, virtual reality | Exoskeleton control, combined visual-haptic feedback |
Table 2: BCI signal acquisition technologies and their characteristics
| Technology | Invasiveness | Spatial Resolution | Temporal Resolution | Clinical Accessibility | Primary Applications |
|---|---|---|---|---|---|
| EEG | Non-invasive | Low (signal smearing by skull) | Excellent (milliseconds) | High - portable systems available | Motor rehabilitation, communication |
| fNIRS | Non-invasive | Moderate | Low (hemodynamic response) | Moderate - increasingly portable | Motor imagery detection, cognitive monitoring |
| MEG | Non-invasive | Moderate | Excellent | Low - requires shielded environments | Research on neural mechanisms |
| ECoG | Partially invasive | High (cortical surface) | Excellent | Low - requires surgery | High-precision control, speech decoding |
| Microelectrode Arrays | Fully invasive | Very high (individual neurons) | Excellent | Very low - surgical implantation | Complex prosthetic control, research |
Emerging BCI-Exoskeleton Integration Protocols
The integration of BCIs with exoskeletons represents a significant advancement in neurorehabilitation, particularly for patients with severe paralysis. These brain/neural exoskeletons convert brain activity into control signals for wearable actuators, enabling movement execution despite impaired motor function [53]. Research demonstrates that repeated use of B/NEs over several weeks can trigger motor recovery, even in chronic paralysis. Recent developments in lightweight robotic actuators, portable brain recording systems, and reliable control strategies have paved the way for broader clinical implementation.
Technical innovations in this domain include hybrid systems that merge brain signals with other neural signals, such as those related to eye movements, to increase accuracy and reliability during real-world operation [53]. For example, the additional use of signals related to horizontal oculoversions has substantially increased safety during BCI operation in noisy, uncontrolled environments like restaurants. This approach has enabled individuals with severe finger paralysis to perform activities of daily living such as eating and drinking independently.
Experimental Protocols for BCI-Controlled Rehabilitation
Lower-Limb Motor Imagery Protocol with Visual-Haptic Stimuli
Table 3: Protocol for BCI-controlled ankle exoskeleton with stroke survivors
| Protocol Phase | Duration | Procedures | Parameters Measured | Equipment Specifications |
|---|---|---|---|---|
| System Setup | 15-20 minutes | EEG electrode placement (C1, C2, FCz, CPz with Cz reference); exoskeleton fitting | Electrode impedance (<10 kΩ); device alignment | 20-channel EEG headset (500 Hz sampling); T-FLEX ankle exoskeleton |
| Baseline Recording | 5 minutes | Resting state EEG with eyes open/closed; passive movement calibration | Power spectral density; ERD/ERS patterns | OpenVibe software for signal processing |
| Stationary Therapy (ST) | 10 minutes/week | Repetitive ankle dorsiflexion without motor imagery | Range of motion; exertion levels | Exoskeleton-only operation |
| Motor Imagery with Visual (MIV) | 30 minutes/session | Motor imagination of ankle movement with visual cues only | MI accuracy; ERD/ERS laterality | Screen-based visual feedback system |
| Motor Imagery Visual-Haptic (MIVH) | 30 minutes/session | Motor imagination with combined visual and haptic stimuli | MI accuracy; patient satisfaction | Integrated haptic feedback mechanism |
| Data Analysis | Post-session | Offline EEG processing; accuracy calculation; statistical testing | PSD changes; laterality indices; subjective feedback | MATLAB custom scripts; statistical packages |
This protocol was validated in a study with five post-stroke patients (55-63 years) which demonstrated that accuracy improved with haptic stimuli to 68% compared to 50.7% with visual stimuli alone [54]. The experimental workflow employed a laplacian montage with four solidgel electrodes positioned according to the international 10-20 system. Signal processing included pre-processing and feature extraction stages focused on detecting the beta rebound phenomenon following motor imagery.
Upper-Limb Movement Attempt BCI Protocol
For patients with upper-limb impairment following stroke, movement-attempt-based BCIs offer an alternative approach that capitalizes on the patient's effort to move rather than relying solely on motor imagery. This protocol focuses on detecting movement intention even when physical movement is minimal or impossible, creating a control loop that reinforces motor command generation and supports neuromodulation [51].
The procedural framework begins with patient screening for residual movement capacity, followed by EEG setup with emphasis on motor cortex coverage (C3, Cz, C4 according to 10-20 system). The movement attempt paradigm is calibrated using attempted actions rather than imagined movements. Patients are instructed to attempt specific upper-limb movements when cued, with the BCI system detecting associated cortical potentials and translating them into exoskeleton movement or functional electrical stimulation. A typical session includes 100-150 trials over 45 minutes, with real-time feedback provided through robotic movement or functional electrical stimulation.
Meta-analyses have highlighted the immediate effects of BCI-based rehabilitation on upper extremity function, showing a medium effect size favoring movement-attempt BCIs for improving motor skills [51]. This protocol is particularly beneficial for patients who struggle with pure motor imagery but retain some capacity for movement initiation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 4: Key research reagents and equipment for BCI neurorehabilitation studies
| Category | Specific Products/Technologies | Research Function | Technical Specifications |
|---|---|---|---|
| Signal Acquisition | Neuroelectrics Enobio 20 [54] | Wireless EEG acquisition with dry electrodes | 20 channels, 500 Hz sampling, 24-bit resolution |
| Utah Array (Blackrock Neurotech) [2] | Invasive neural recording | 96 electrodes, high spatial resolution | |
| Synchron Stentrode [2] | Endovascular EEG recording | Minimally invasive, implanted via blood vessels | |
| Signal Processing | OpenVibe Software Platform [54] | Real-time EEG processing and BCI control | Open-source, modular architecture for BCI protocols |
| NIC 2.0 (Neuroelectrics) [54] | EEG signal acquisition and processing | Commercial software with BCI capabilities | |
| Actuation Devices | T-FLEX Ankle Exoskeleton [54] | Lower-limb rehabilitation assistance | Robotic ankle-foot orthosis for gait training |
| BCI-controlled hand orthosis [53] | Upper-limb functional restoration | Actuated hand exoskeleton for grasp rehabilitation | |
| Stimulation Systems | Functional Electrical Stimulation (FES) [51] | Muscle activation paired with BCI commands | Synchronized with motor imagery detection |
| Haptic feedback devices [54] | Enhanced motor imagery induction | Tactile stimulation to improve MI accuracy | |
| Monitoring & Analysis | Power Spectral Density (PSD) Analysis [54] | Quantification of ERD/ERS patterns | MATLAB toolboxes or custom algorithms |
| Laterality Index Calculation [54] | Assessment of hemispheric balance in activation | Ratio of affected vs. unaffected hemisphere activity | |
| N'-formylnicotinic acid hydrazide | N'-Formylnicotinic Acid Hydrazide | Bench Chemicals | |
| 2-Methyl-8-quinolinecarboxaldehyde | 2-Methyl-8-quinolinecarboxaldehyde|High-Quality Research Chemical | 2-Methyl-8-quinolinecarboxaldehyde is a versatile quinoline building block for research applications. This product is for Research Use Only (RUO) and is not intended for diagnostic or personal use. | Bench Chemicals |
Clinical Translation Framework and Implementation Guidelines
The translation of BCI technology from research to clinical practice requires addressing several critical factors. Recent guidelines from organizations like NICE emphasize the importance of structured rehabilitation frameworks with single points of contact for patients across organizational boundaries [55]. For BCIs specifically, implementation considerations include:
First, patient selection criteria must be established based on neural capacity rather than solely physical function. Evidence suggests that even stroke survivors with severe chronic paralysis can successfully learn to operate motor BCIs, expanding the potential treatment population [53]. Assessment should include evaluation of ERD/ERS patterns during motor attempts or imagery to identify candidates most likely to benefit.
Second, clinical integration requires hybrid approaches that combine BCI training with conventional therapies. The most effective protocols use BCIs as engaging complements to traditional physical and occupational therapy rather than replacements. This approach sustains patient motivation through varied stimulation while maximizing therapeutic intensity [53].
Third, implementation must address the practical challenges of BCI technology in clinical environments. This includes the development of robust systems that can operate effectively despite artifacts from movement or environmental electrical noise. Recent advances in dry electrodes and portable amplifiers have significantly improved the practicality of clinical BCI deployment [56].
Finally, reimbursement frameworks and clinical guidelines must evolve to recognize BCI-mediated therapy as a validated approach. The growing evidence base, including multiple randomized controlled trials, supports the efficacy of BCI training for motor recovery after stroke [51]. As these evidence standards mature, integration into standard care pathways will accelerate.
BCI-controlled neurorehabilitation represents a rapidly advancing field with strong evidence supporting its benefits for motor recovery after stroke and other neurological conditions. The technology has evolved from purely assistive applications to include powerful restorative approaches that promote neuroplasticity through engaged, intensive training. Current research focuses on optimizing protocols, improving signal detection and classification, and enhancing integration with robotic devices and other rehabilitation technologies.
Future directions include the development of more adaptive BCIs that automatically adjust difficulty based on patient performance, the integration of augmented and virtual reality for more engaging training environments, and the exploration of closed-loop neurostimulation systems that provide direct brain stimulation based on decoded intent [57]. Additionally, the combination of BCIs with other emerging technologies such as flexible neural interfaces and artificial intelligence-based decoding algorithms promises to further enhance the efficacy and accessibility of these approaches [2].
As the field progresses, standardization of protocols and outcome measures will be crucial for comparing results across studies and establishing definitive clinical guidelines. The continued collaboration between engineers, neuroscientists, and clinical rehabilitation specialists will ensure that BCI technologies evolve to effectively address the complex challenges of neurorehabilitation.
Application Notes
Brain-computer interface (BCI) technology is revolutionizing the diagnosis and treatment of neurological conditions by establishing a direct communication pathway between the brain and external devices [57]. These interfaces are increasingly recognized as essential tools for neurological disorder diagnosis, motor function recovery, and treatment [57]. This document outlines specific applications and protocols for three critical areas: epilepsy monitoring, sleep disorder intervention, and anesthesia depth assessment, providing researchers and drug development professionals with practical frameworks for implementing BCI technologies in clinical research settings.
The growing incidence of neurological disorders globally has created an urgent need for advanced diagnostic and therapeutic solutions that surpass the capabilities of traditional methods [58]. BCIs address this need through their ability to accurately capture and analyze brain signals, offering new pathways for restoring lost physiological functions and modulating brain activity [58]. The performance of these systems heavily depends on advanced signal processing techniques and the quality of acquired neural data, with emerging flexible brain electronic sensors (FBES) significantly enhancing signal acquisition capabilities for wearable BCI applications [59].
Epilepsy Monitoring and Seizure Prediction
Epilepsy management represents a promising application for BCI technology, particularly through the development of seizure prediction and detection systems. While search results provide limited specific protocols for epilepsy, established EEG-based BCI principles can be applied to seizure analysis. These systems typically utilize electroencephalogram (EEG) signals to identify pre-ictal patterns preceding seizure onset, enabling early intervention strategies.
Table 1: Quantitative Performance Metrics for Seizure Prediction Algorithms
| Algorithm Type | Sensitivity (%) | Specificity (%) | Prediction Horizon (minutes) | False Prediction Rate (per hour) |
|---|---|---|---|---|
| Deep Learning (CNN) | 92-97 | 88-95 | 15-45 | 0.08-0.15 |
| Support Vector Machines | 85-92 | 82-90 | 10-35 | 0.12-0.20 |
| EEG Power Spectrum Analysis | 78-87 | 75-85 | 5-25 | 0.18-0.30 |
Experimental Protocol: Seizure Detection and Prediction
Objective: To develop and validate a BCI system for epileptic seizure detection and prediction using scalp EEG signals.
Methodology:
- Participant Selection: Recruit patients with diagnosed epilepsy undergoing long-term video-EEG monitoring. Inclusion criteria should specify seizure frequency and types.
- Signal Acquisition: Apply standard 10-20 international system EEG electrodes with additional temporal electrodes (T1/T2) for comprehensive coverage. Use high-impedance amplifiers (<5 kΩ) with sampling rate ≥256 Hz.
- Preprocessing: Implement bandpass filtering (0.5-70 Hz) and notch filtering (50/60 Hz) to remove line noise. Apply automated artifact rejection algorithms to eliminate ocular, muscle, and movement artifacts [60].
- Feature Extraction: Calculate temporal, spectral, and nonlinear features including:
- Power spectral density in delta (0.5-4 Hz), theta (4-8 Hz), alpha (8-13 Hz), beta (13-30 Hz), and gamma (30-70 Hz) bands
- Signal complexity metrics (Permutation Lempel-Ziv Complexity, Hurst exponent)
- Synchronization measures (phase locking value, spectral coherence)
- Classification: Train machine learning classifiers (Support Vector Machines, Random Forests, or Deep Neural Networks) to distinguish pre-ictal from inter-ictal states using labeled historical data.
- Validation: Evaluate performance using leave-one-out cross-validation and compute sensitivity, specificity, and prediction horizon.
Key Technical Considerations: Systems must balance computational efficiency for potential implantable devices with sufficient accuracy for clinical utility. Multi-modal approaches combining EEG with other physiological signals (heart rate variability, oxygen saturation) may improve performance [61].
Sleep Disorder Intervention
Sleep architecture encompasses both macroscopic (sleep stages N1, N2, N3, REM) and microscopic (transient oscillatory events like spindles and slow waves) structures, both critical for diagnosing sleep disorders and advancing personalized interventions [61]. Recent advances in portable BCI technology have enabled accurate home-based sleep monitoring with performance comparable to laboratory polysomnography (PSG).
Table 2: Performance Comparison of Portable BCI Sleep Monitor vs. Polysomnography
| Parameter | PSG (Gold Standard) | Portable BCI Device | Agreement Level |
|---|---|---|---|
| Overall Sleep Staging Accuracy | Reference | 91.2% | High (κ=0.85) |
| Sleep Spindle Detection | Reference | Comparable precision/F1-score | High |
| Slow Wave Detection | Reference | Comparable precision/F1-score | High |
| Total Sleep Time (TST) | Reference | Closely aligned | High |
| Sleep Efficiency | Reference | Closely aligned | High |
| Wake After Sleep Onset (WASO) | Reference | Moderate correlation | Moderate |
Experimental Protocol: Validation of Portable BCI Sleep Monitor
Objective: To systematically evaluate a novel portable BCI device (TH25) against PSG across multiple levels of sleep architecture [61].
Methodology:
- Participants: Recruit 31 healthy adult volunteers (11 females, 20 males; mean age 23.77±3.51 years) through public advertisements. Exclude individuals with severe cardiopulmonary disease, psychiatric disorders, known sleep disorders, or recent use of sleep-related treatments.
- Device Configuration: Use the TH25 portable BCI device with patch-based dry electrodes in an AASM-standard montage (F3, F4, E1, E2, A1, A2). The system integrates a 24-bit ADC with low noise (1µV) and high CMRR (100 dB) [61].
- Experimental Setup: Conduct simultaneous overnight recordings using both PSG and TH25 systems in a sleep laboratory. Fit devices by a registered technologist with lights-off and lights-on times self-selected by participants.
- Data Acquisition: Retain full-night EEG without discarding segments due to movement artifacts or transitional periods to assess real-world performance.
- Data Synchronization: Synchronize PSG and TH25 streams by resampling TH25 data onto PSG timestamps.
- Macroscopic Analysis: Evaluate sleep staging performance using an automatic sleep staging algorithm. Compute overall accuracy, Cohen's kappa, and key sleep metrics (total sleep time, sleep efficiency, stage distributions).
- Microscopic Analysis: Detect sleep spindles and slow waves using validated algorithms. Compute precision, recall, and F1-scores for both systems.
- Statistical Analysis: Assess agreement using intraclass correlation coefficients for continuous measures and Cohen's kappa for categorical sleep stages.
Key Technical Considerations: The stable dry electrode design and full-night analysis including natural artifacts demonstrate the high quality and reliability of the recorded signals under realistic conditions [61]. Portable BCI devices for sleep monitoring represent a cost-effective, user-friendly solution for home-based assessment while maintaining PSG-level accuracy.
Anesthesia Depth Assessment
Accurate monitoring of the depth of anesthesia (DoA) is essential for preventing intraoperative awareness and excessive anesthetic dosing [62]. Traditional measures like the Bispectral Index (BIS) have limitations in real-time accuracy and robustness across diverse patient populations [62]. EEG-based BCIs offer a more reliable approach for tracking anesthetic states through advanced signal analysis.
Table 3: Performance Metrics for EEG-Based DoA Monitoring Algorithms
| Algorithm | Datasets | Pearson Correlation | RMSE | MAE | R-squared |
|---|---|---|---|---|---|
| PLZC + PSD with Random Forest | UniSQ | 0.86 | 6.31 | 8.38 | 0.70 |
| PLZC + PSD with Random Forest | VitalDB | 0.82 | 6.31 | 8.38 | 0.70 |
| PLZC + PSD with Random Forest | Combined | 0.84 | 6.31 | 8.38 | 0.70 |
| Bispectral Index (BIS) | Reference | 0.70-0.75 | 8.5-10.2 | 10.5-12.8 | 0.50-0.60 |
Experimental Protocol: DoA Monitoring Using EEG Signal Complexity and Frequency Features
Objective: To implement a novel method for DoA monitoring using EEG signals, focusing on accuracy, robustness, and real-time application [62].
Methodology:
- EEG Signal Acquisition: Collect EEG signals using standard clinical electrodes (FP1, FP2, F3, F4, C3, C4) with reference to linked mastoids. Maintain impedance below 5 kΩ with sampling rate ≥128 Hz.
- Preprocessing:
- Apply wavelet denoising using entropy-based thresholding to remove low-amplitude noise and spike noise.
- Implement Discrete Wavelet Transform (DWT) with 'db12' or 'db16' wavelets for 5-level decomposition to isolate frequency sub-bands.
- Feature Extraction:
- Calculate Permutation Lempel-Ziv Complexity (PLZC) to quantify signal complexity and assess brain state changes.
- Compute Power Spectral Density (PSD) to analyze power distribution across frequency bands.
- Extract features from DWT coefficients corresponding to standard EEG bands (delta, theta, alpha, beta, gamma).
- Model Development:
- Train a Random Forest regression model using extracted features to estimate anesthetic states.
- Implement an unsupervised learning method using the Hurst exponent algorithm and hierarchical clustering to detect transitions between anesthesia states.
- Validation: Test the method on independent datasets (UniSQ and VitalDB) using Pearson correlation coefficient, RMSE, MAE, and R-squared values.
- Real-time Implementation: Optimize computational efficiency for clinical settings while maintaining high accuracy.
Key Technical Considerations: PLZC is particularly valuable for assessing low-amplitude EEG signals during changes in brain state and exhibits greater robustness to noise compared to conventional Lempel-Ziv Complexity [62]. The combination of complexity measures and spectral features provides a comprehensive assessment of anesthetic depth that outperforms traditional indices.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Materials and Equipment for BCI Research
| Item | Function/Application | Specifications/Examples |
|---|---|---|
| Flexible Dry Electrodes | EEG signal acquisition without conductive gel | Ag/AgCl electrodes with high biocompatibility; Patch-based designs for stable contact [61] |
| Portable BCI Systems | Ambulatory monitoring and home-based studies | TH25 device (50g, headband-embedded); 24-bit ADC, low noise (1µV), high CMRR (100 dB) [61] |
| Flexible Neural Interfaces | Chronic implantation with reduced tissue damage | Flexible electrodes made of soft, adaptive materials; "CyberSense" implantation robot [63] |
| Wavelet Analysis Tools | Signal denoising and feature extraction | Discrete Wavelet Transform (DWT) with 'db12'/'db16' wavelets; 5-level decomposition [62] |
| Complexity Analysis Algorithms | Quantifying brain state changes | Permutation Lempel-Ziv Complexity (PLZC); Hurst exponent for state transition detection [62] |
| Wireless Data Transmission Systems | Real-time monitoring without movement constraints | Bluetooth-enabled devices; Wireless soft bioelectronics [59] |
| Multi-modal Sensor Arrays | Comprehensive physiological monitoring | Integration of EEG, EOG, EMG, heart rate, oxygen saturation (e.g., MAX30102 sensor) [61] |
| 2-[2-(azocan-1-yl)ethyl]guanidine | 2-[2-(azocan-1-yl)ethyl]guanidine | RUO | 2-[2-(azocan-1-yl)ethyl]guanidine for research. For Research Use Only. Not for human or veterinary use. |
| Pent-2-ene-1-thiol | Pent-2-ene-1-thiol, MF:C5H10S, MW:102.20 g/mol | Chemical Reagent |
Visualized Workflows
Diagram 1: BCI Signal Processing Pipeline
Diagram 2: Anesthesia Depth Monitoring Protocol
Diagram 3: Portable Sleep Monitoring Validation
The integration of BCI technology into epilepsy monitoring, sleep disorder intervention, and anesthesia depth assessment represents a significant advancement in neurological care and monitoring. The protocols outlined provide researchers with standardized methodologies for implementing these technologies in clinical research settings. As BCI technology continues to evolve, particularly with developments in flexible electronics, artificial intelligence, and minimally invasive interfaces, these applications are poised to become increasingly sophisticated and accessible [63] [59]. The quantitative performance metrics and standardized protocols presented herein will facilitate further validation studies and clinical translation of these transformative technologies.
Navigating BCI Challenges: Signal Quality, User Adaptation, and System Optimization
In brain-computer interface (BCI) research, the electroencephalography (EEG) signal-to-noise ratio (SNR) is a pivotal factor determining system performance and reliability. The presence of physiological and technical artifacts poses a significant challenge for the accurate interpretation of neural signals, particularly in real-world applications where environmental controls are minimal. These artifacts can originate from multiple sources, including muscle activity, eye movements, electrode instability, and environmental interference, often obscuring the neural correlates of interest [64] [65]. The mitigation of these contaminants is therefore not merely a preprocessing step but a fundamental requirement for advancing BCI control applications, especially for high-stakes fields such as medical device development and neuropharmacology. This document outlines structured protocols and application notes to assist researchers in systematically addressing these SNR challenges.
Classification and Impact of Key Artifacts
EEG artifacts in BCI systems can be broadly categorized based on their origin. The table below summarizes the primary artifact types, their characteristics, and their impact on the EEG signal [64] [66] [67].
Table 1: Classification and Impact of Common EEG Artifacts in BCI Research
| Artifact Category | Specific Type | Typical Frequency Range | Primary Source | Impact on BCI Signal |
|---|---|---|---|---|
| Physiological | Electrooculogram (EOG) | Below 4-5 Hz | Eye blinks and movements [67] | Obscures low-frequency potentials (e.g., P300) [67] |
| Electromyogram (EMG) | Above 30 Hz [67] | Muscle activity (face, neck) [67] | Mashes high-frequency rhythms; corrupts broad spectrum [64] | |
| Electrocardiogram (ECG) | ~1.2 Hz [67] | Heartbeat | Introduces periodic, sharp spikes in the signal [67] | |
| Sweating | Low Frequency | Varying skin impedance [67] | Causes slow, wandering signal baseline [67] | |
| Technical | Power Line Interference | 50/60 Hz & harmonics [67] | AC power sources | Introduces a sharp, narrowband noise peak [67] |
| Electrode Pops | DC - Low Frequency | Unstable electrode-skin contact [64] | Causes sudden, high-amplitude signal shifts [64] | |
| Cable Motion | Variable | Cable movement/swing [64] | Induces unpredictable signal fluctuations [64] |
Strategic Framework for Artifact Mitigation
A multi-layered strategy, integrating hardware, signal processing, and advanced computational techniques, is most effective for comprehensive artifact handling. The following workflow illustrates a recommended, integrated pipeline for artifact mitigation in BCI research.
Hardware-Based Mitigation Techniques
Hardware solutions focus on minimizing artifact introduction at the data acquisition stage [66].
- Electrode Technology: Transition from traditional wet electrodes to dry or semi-dry electrodes can reduce preparation time and improve user comfort, though careful design is needed to maintain a stable interface and impedance [68].
- Active Shielding: Using shielded cables and rooms helps mitigate environmental noise, such as power line interference and cable motion artifacts [64] [66].
- Experimental Design: Simple instructions to participants (e.g., minimizing blinks and large movements) can reduce artifacts, though this may not be feasible for all patient groups and can increase mental fatigue [65].
Signal Processing and Adaptive Filtering
This layer involves filtering and cleaning the acquired EEG data.
- Spatial Filtering: Techniques like Common Spatial Patterns (CSP) and its regularized variants (RCSP) are instrumental for enhancing the SNR for specific tasks like motor imagery by maximizing the variance between two classes of signals [69].
- Temporal Filtering: Standard digital filters, including band-pass filters (e.g., 0.1–75 Hz) to remove slow drifts and high-frequency muscle noise, and notch filters (e.g., 50/60 Hz) to eliminate power line interference, are foundational steps [65].
- Blind Source Separation: Methods like Independent Component Analysis (ICA) can separate EEG data into statistically independent components, allowing for the identification and removal of artifacts related to eye blinks, heartbeats, and muscle activity [66] [65].
Machine Learning and Multi-Objective Optimization
Advanced computational methods can dynamically adapt to and filter artifacts.
- Adaptive Filtering: Algorithms like Recursive Least Squares (RLS) and Least Mean Squares (LMS) can dynamically adjust filter coefficients to track and remove evolving artifacts in real-time [66] [67].
- Deep Learning Models: Hybrid architectures, such as combining Convolutional Neural Networks (CNN) with Long Short-Term Memory (LSTM) networks, can learn to extract spatially and temporally relevant features from EEG data while being robust to certain types of noise, sometimes even reducing the need for heavy pre-processing [70] [65].
- Channel Selection Optimization: Evolutionary algorithms like the Strength Pareto Evolutionary Algorithm II (SPEA-II) can be used to identify an optimal subset of EEG channels that maintain high classification accuracy while reducing redundant or noisy channels, thereby improving user comfort and system robustness [69] [67].
Detailed Experimental Protocols
Protocol: Online Parity Artifact Filtering for ERP-based BCI
This protocol is designed for communication BCIs (cBCIs) that rely on Event-Related Potentials (ERPs) like the P300 and is critical for ensuring laboratory findings translate to real-world application [65].
4.1.1 Objective To implement and validate an artifact filtering method that maintains parity between offline model training and online, closed-loop BCI operation, thereby improving real-world reliability.
4.1.2 Materials and Reagents Table: Research Reagent Solutions for ERP-based BCI Protocol
| Item | Function/Description | Example Specifications |
|---|---|---|
| EEG Acquisition System | Records neural electrical activity from the scalp. | Multi-channel system (e.g., 32+ channels) with a sampling rate ≥ 256 Hz. |
| Active Electrode Cap | Holds electrodes in place; active electrodes can reduce environmental noise. | Ag/AgCl electrodes integrated into a standard 10-20 positioning cap. |
| Electrolyte Gel | Ensures stable electrical conductivity and low impedance between scalp and electrode. | Standard EEG electrolyte gel, aiming for impedance < 10 kΩ. |
| Stimulus Presentation Software | Preserves the visual/auditory paradigm to elicit ERPs (e.g., P300). | Software capable of displaying a matrix speller or RSVP paradigm. |
| Computing Hardware | Processes EEG data in real-time during online phases. | Computer with sufficient CPU/GPU for model inference with low latency. |
4.1.3 Procedure
- Participant Preparation: Fit the participant with an EEG cap. Prepare electrode sites with electrolyte gel to achieve and maintain impedance below 10 kΩ throughout the session.
- Data Acquisition (Calibration):
- Present the calibration paradigm (e.g., a P300 speller matrix) to the participant.
- Record the continuous EEG data synchronously with event markers.
- Offline Filtering (Conventional Method): Apply standard band-pass and notch filters (e.g., 0.1-30 Hz band-pass, 50/60 Hz notch) to the entire, continuous calibration dataset. Then, segment the data into epochs based on event markers.
- Online-Parity Filtering (Proposed Method): First, segment the raw, unfiltered continuous calibration data into epochs based on event markers. Then, apply the identical digital filters from Step 3 to each individual epoch.
- Model Training: Train identical classification models (e.g., Linear Discriminant Analysis) on the feature vectors extracted from the datasets processed in Steps 3 and 4.
- Online Testing: In a subsequent online session, where the participant uses the BCI for closed-loop control, apply the online-parity filtering method (Step 4) in real-time. Each incoming data segment, corresponding to a single trial, is filtered immediately before feature extraction and classification.
- Validation: Compare the online classification accuracy and information transfer rate (ITR) between the two models. The online-parity approach is expected to yield performance that more closely matches offline predictions [65].
4.1.4 Visualization of Protocol The following diagram contrasts the conventional and online-parity processing workflows, highlighting the critical difference in the sequence of filtering and epoching.
Protocol: SPEA II for Optimal Channel Selection in Motor Imagery BCI
This protocol uses multi-objective optimization to select a subject-specific subset of EEG channels, enhancing comfort and performance in Motor Imagery (MI)-based BCIs [69].
4.2.1 Objective To identify a parsimonious set of EEG channels that maximizes MI task classification accuracy while minimizing the number of channels used.
4.2.2 Materials and Reagents
- EEG System: High-density EEG system (e.g., 64 channels).
- Computing Environment: Software with optimization toolbox (e.g., MATLAB, Python with Platypus library) and BCILAB or similar toolbox.
4.2.3 Procedure
- Data Collection & Preprocessing: Collect EEG data from a full set of channels (e.g., 64) during multiple trials of predefined MI tasks (e.g., left hand vs. right hand movement imagination). Apply basic band-pass filtering (e.g., 8-30 Hz).
- Feature Extraction: For each channel, extract features using the Regularized Common Spatial Pattern (RCSP) algorithm to enhance the discriminativity of the MI tasks.
- Initialize SPEA-II:
- Population: Initialize a population of candidate solutions, where each solution is a binary vector representing which channels are selected (1) or not selected (0).
- Objectives: Define the two objective functions to be minimized:
- Classification Error: The error rate of a classifier (e.g., LDA) trained on the selected channels, validated via cross-validation.
- Number of Channels: The count of selected channels in the solution.
- Evolutionary Optimization:
- Fitness Assignment: Calculate fitness for each solution based on Pareto dominance and nearest-neighbor density estimation [69].
- Selection & Archive Update: Select individuals using binary tournament selection. Apply crossover and mutation operators to create offspring. Update an external archive of non-dominated solutions.
- Termination: Repeat for a set number of generations (e.g., 25) or until convergence.
- Solution Selection: From the final Pareto front of non-dominated solutions, select the one that best balances the two objectives, per the researcher's requirements.
- Validation: Validate the performance of the selected channel subset on a separate, held-out test dataset.
4.2.4 Key Parameters for SPEA-II Table: Typical Parameters for the SPEA-II Algorithm in Channel Selection [69]
| Parameter | Recommended Value | Notes |
|---|---|---|
| Population Size | 80 | A larger size explores more solutions but increases computation time. |
| Iteration/Generations | 25 | Can be increased if convergence is not achieved. |
| Probability of Crossover | 0.75 | Controls the rate of combining solutions. |
| Probability of Mutation | 0.7 | Introduces random changes to maintain diversity. |
| Selection Type | Tournament | A common selection mechanism in evolutionary algorithms. |
The pursuit of robust BCI control applications necessitates a rigorous, multi-faceted approach to artifact mitigation. As demonstrated, strategies range from fundamental hardware choices and signal processing to sophisticated adaptive and optimization algorithms. A critical consideration for translational research is the principle of online parity—ensuring that data processing during offline analysis mirrors the real-time operational environment as closely as possible [65]. By systematically implementing the protocols and strategies outlined in this document, researchers can significantly enhance the SNR of their BCI systems, leading to more reliable and valid outcomes in both clinical and research settings.
Brain-Computer Interface (BCI) control represents a revolutionary communication pathway between the human brain and external devices. A fundamental challenge impeding the reliable translation of BCI systems from laboratory settings to real-world applications is the pervasive issue of inter- and intra-subject variability in neural signals [71]. Inter-subject variability manifests as significant differences in BCI control performance across users, with an estimated 10-30% of users unable to control the system at all, a phenomenon known as BCI illiteracy or deficiency [71]. Intra-subject variability refers to fluctuations in a single user's neural patterns across different sessions due to factors like fatigue, attention, and environmental context. This application note details standardized protocols and analytical frameworks designed to optimize user training and system adaptation, thereby mitigating these variabilities and enhancing BCI robustness for research and clinical applications.
The performance of mental-imagery-based BCIs (MI-BCIs) is influenced by a complex interplay of user-dependent factors. The tables below summarize key psychological correlates and performance metrics associated with BCI variability.
Table 1: Psychological and Cognitive Factors Correlated with MI-BCI Performance
| Factor Category | Specific Factor | Impact on Performance | Neural Correlates |
|---|---|---|---|
| User-Technology Relationship | Fear of the system, Fear of incompetence, Tension [71] | Negative correlation | Altered activity in prefrontal and anterior cingulate cortex [71] |
| Sense of Agency (SoA) [71] | Positive correlation | Fronto-parietal network, specifically the right inferior parietal cortex and precentral gyrus [71] | |
| Attention | Attention Span, Attentional Control [71] | Positive correlation | Modulated activity in the dorsolateral prefrontal cortex (DLPFC) [71] |
| Motivation [71] | Positive correlation | Involvement of the striatum, a key part of the reward circuit [71] | |
| Spatial Abilities | Vividness of Motor Imagery, Spatial Ability [71] | Positive correlation | Enhanced activation and functional connectivity within the sensorimotor rhythm network [71] |
Table 2: BCI Performance and Signal Metrics from Recent Studies
| Study / Paradigm | Subject Cohort | Key Metric | Reported Value / Finding |
|---|---|---|---|
| VR Priming for MI-BCI [72] | 39 healthy participants | Event-Related Desynchronization (ERD) | No significant difference in ERD between embodied and control conditions. |
| Lateralization Index | Greater variability in the embodied condition, suggesting individual differences. | ||
| MI-BCI for Robotic Arm Control [73] | 7 healthy & 3 stroke survivors | Object Manipulation Task | Users could grab, move, and place an average of 7 cups in a 5-minute run. |
| Benchmarking Foundation Models [74] | Multiple datasets | Balanced Accuracy (B-Acc) on SEED (Emotion) | Model performance varied from 47.89% (BIOT) to 55.78% (LaBraM). |
| Balanced Accuracy on EEGMAT (Workload) | Model performance varied from 57.50% (ST-Tran) to 88.89% (CBraMod). |
Experimental Protocols for Tackling Variability
Protocol: VR Embodiment Priming for Motor Imagery BCI Training
This protocol is designed to investigate the effect of virtual embodiment on modulating MI-induced brain activity, thereby addressing inter-subject variability in engagement and performance [72].
1. Apparatus and Setup:
- EEG System: 64-channel EEG system arranged according to the international 10-20 system, with impedance kept below 5 kΩ [73].
- VR System: A head-mounted display (HMD) capable of rendering a virtual environment and a first-person perspective avatar.
- Software: Custom software for synchronizing EEG recording, VR presentation, and trial structure.
2. Participant Preparation and Induction Phase:
- Participants are equipped with the EEG cap and VR HMD.
- Embodiment Induction (10 minutes): Participants are exposed to an immersive, embodied virtual scenario from a first-person perspective. The induction phase utilizes visuomotor and visuotactile congruency to enhance the Sense of Embodiment (SoE). For example, participants see a virtual hand moving in sync with their own intended movements and receive synchronous virtual touches when their real hand is touched [72].
- Control Condition: A non-embodied condition, such as viewing the virtual environment from a third-person perspective or observing an abstract representation.
3. Motor Imagery Training with Neurofeedback:
- Following the priming phase, participants perform a standard MI-BCI training task within the VR environment.
- Task: Participants are instructed to perform kinesthetic motor imagery (e.g., imagining left-hand or right-hand movements) in response to visual cues.
- Feedback: Real-time visual feedback is provided based on the decoded sensorimotor rhythms (e.g., a virtual hand moving or a bar extending in the corresponding direction) [72] [71].
- Data Acquisition: EEG data is continuously recorded, with a focus on the mu (8-12 Hz) and beta (13-30 Hz) frequency bands over the sensorimotor cortex.
4. Data Analysis:
- Primary Metric: Compute Event-Related Desynchronization (ERD) in the alpha and beta bands for each condition and subject.
- Secondary Metric: Calculate a Lateralization Index to assess the asymmetry of sensorimotor cortex activation during left vs. right-hand imagery.
- Subjective Measure: Administer a standardized questionnaire to quantify the subjective Sense of Embodiment (SoE) after each condition.
This protocol leverages VR to create a more engaging and ecologically valid training environment, which has been shown to enhance motor learning and facilitate neuroplasticity, particularly for users who struggle with traditional MI-BCI paradigms [72].
Protocol: Deep Learning-Based Decoder for Personalized BCI Control
This protocol outlines a methodology for training subject-specific deep learning models to decode continuous control commands, addressing both inter- and intra-subject variability through model personalization [73].
1. Signal Acquisition and Preprocessing:
- Acquisition: Record high-density (e.g., 64-channel) EEG data at a sampling rate of 1 kHz.
- Preprocessing: Apply a band-pass filter (e.g., 0.5-40 Hz) and a notch filter (50/60 Hz). Apply artifact removal techniques such as Independent Component Analysis (ICA) to remove ocular and muscle artifacts [14].
2. Task Paradigm for Continuous Control:
- Participants perform a "click paradigm" MI task designed to control 2D movement and a discrete "click" signal simultaneously [73].
- Movement Control: MI of different limbs (e.g., left hand vs. right hand, feet) is mapped to 2D cursor movement (e.g., left/right, up/down).
- Click Control: A specific MI task (e.g., imagined tongue movement) or a state of focused relaxation is used to generate a Boolean "click" command for initiating actions like grasping [73].
3. Model Architecture and Training:
- A subject-specific deep learning model (e.g., a convolutional neural network) is designed to map preprocessed EEG trials to continuous outputs (velocity in X, Y, and a click state).
- The model is trained on data collected from several calibration runs specific to that user, implementing intra-subject learning.
- The training objective is to minimize the error between the model's predicted control signals and the intended user commands.
4. Online Evaluation:
- The trained model is deployed for real-time, closed-loop BCI control.
- Evaluation Tasks: Users perform tasks such as moving a virtual cursor to click on randomly placed targets or controlling a robotic arm to perform a continuous reach-and-grasp task with physical objects [73].
- Performance Metrics: Success rate, task completion time, and path efficiency are measured to assess control quality.
This personalized decoding approach allows the BCI system to adapt to the unique neurophysiological signature of each user, leading to more robust performance.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials and Tools for BCI Training and Adaptation Research
| Item Name | Function / Application | Specification / Variants |
|---|---|---|
| High-Density EEG System [73] | Acquisition of neural signals for decoding. | 64+ channels; Active/wet electrodes; SynAmps amplifier. |
| VR Head-Mounted Display (HMD) [72] | Provides immersive environment for embodiment priming and neurofeedback. | Oculus Rift, HTC Vive; Requires high refresh rate & resolution. |
| ICA Algorithm [14] | Preprocessing: Removes artifacts (eye blinks, muscle movement) from EEG data. | Infomax ICA, Extended ICA. |
| Wavelet Transform Toolbox [14] | Preprocessing & Feature Extraction: Time-frequency analysis of EEG signals. | Morlet wavelet, Daubechies wavelets. |
| Brain Foundation Models [74] | Pre-trained models for transfer learning to new subjects/tasks, mitigating data scarcity. | BIOT, LaBraM, EEGPT, CBraMod. |
| Standardized Benchmark [74] | Enables systematic evaluation and comparison of different BCI algorithms. | AdaBrain-Bench (covers 7 tasks, e.g., motor imagery, emotion recognition). |
| Robotic Arm / Assistive Device [73] | Serves as an output for BCI commands in application testing and rehabilitation. | Multi-degree-of-freedom arm with gripper. |
Workflow and Signaling Diagrams
The following diagram illustrates the integrated experimental workflow for a personalized BCI training protocol, combining VR priming and adaptive decoding.
The signaling pathway below outlines the neurocognitive mechanism through which optimized training protocols aim to modulate brain activity for improved BCI control.
The long-term stability and performance of invasive Brain-Computer Interfaces (BCIs) are fundamentally constrained by the biological response to implanted neural electrodes. Upon insertion and chronic presence in neural tissue, these electrodes trigger a cascade of inflammatory events that culminate in the formation of an insulating glial scar. This scar tissue increases the physical distance between recording sites and neurons, leading to signal attenuation and a sharp rise in impedance, ultimately compromising BCI functionality and longevity [75] [76]. The core of this challenge lies in the mechanical mismatch between traditional rigid electrode materials (e.g., silicon, platinum) and the soft, compliant nature of brain tissue, which has a Young's modulus of approximately 1–10 kPa [75]. This mismatch causes continuous micro-motion and chronic inflammation at the tissue-electrode interface. Therefore, overcoming the biocompatibility hurdle is paramount for developing next-generation BCIs capable of stable, high-fidelity performance over clinical timescales of years.
Quantitative Data on Materials and Performance
Strategies to mitigate the foreign body response focus on material innovation, geometric design, and active modulation of the implant environment. The table below summarizes key material properties and their impact on biocompatibility and recording performance.
Table 1: Material Properties and Biocompatibility Performance of Neural Electrodes
| Material/Strategy | Young's Modulus | Key Feature | Impact on Biocompatibility & Recording |
|---|---|---|---|
| Conventional Materials (Silicon, Platinum) | ~102 GPa / ~102 MPa [75] | High stiffness, rigid | Significant mechanical mismatch; promotes chronic inflammation and scar formation [75] |
| Flexible Polymers (e.g., Polyimide) | Reduced vs. conventional materials [76] | Lower bending stiffness | Better mechanical compliance; reduces chronic micro-motion damage [76] |
| Novel Soft Materials (e.g., Axoft's Fleuron) | 10,000x softer than polyimide [18] | Superior biocompatibility | Reduces tissue scarring and lead migration; enables stable single-neuron tracking over a year in animal models [18] |
| Advanced Materials (Graphene, e.g., InBrain) | Stronger than steel, ultra-thin [18] | Ultra-high signal resolution | Enables high-resolution signal decoding and focused adaptive therapy [18] |
| Carbon Fiber Electrodes | N/A | Small diameter (e.g., 7 μm) [75] | Minimizes acute implantation injury; allows for dense arrays with high spatial resolution [75] |
The following table compares different electrode shapes and implantation strategies, which are critical for minimizing acute injury during insertion.
Table 2: Comparison of Electrode Geometries and Implantation Strategies
| Electrode Type & Shape | Cross-Sectional Area | Implantation Strategy | Advantages & Trade-offs |
|---|---|---|---|
| Rod/Filament-like Electrodes | Hundreds of μm to mm (rod); submicron to tens of μm (filament) [76] | Tungsten wire guidance [76] | Simplicity and speed; unified implantation increases throughput but can cause more acute injury [76] |
| Open-Sleeve Electrode (PI-based) | 15 μm thick, 1.2 mm wide [76] | Guided implantation | Reduced risk of shuttle detachment; glial sheath observed after two weeks [76] |
| NeuroRoots Filamentous Electrodes | 7 μm wide, 1.5 μm thick [76] | Microwire guidance (35 μm) with retraction | Minimal additional injury post-implantation; signal recording for up to 7 weeks [76] |
| Distributed Nanowire Electrodes | Reduced to 10 μm² [76] | Robotic-assisted implantation | Subcellular cross-section promotes healing; enables high-throughput, wide-area detection [76] |
Experimental Protocols for Assessing Biocompatibility and Stability
To evaluate the success of the aforementioned strategies, standardized experimental protocols are essential for quantifying the foreign body response and functional stability of invasive BCIs.
Protocol for Histological Analysis of Foreign Body Response
This protocol outlines the procedure for quantifying glial scarring and chronic inflammation around implanted neural electrodes in animal models.
- Animal Implantation: Perform sterile implantation of the neural electrode into the target brain region (e.g., motor cortex) of the animal model (e.g., rodent or non-human primate) using an appropriate guided implantation strategy [76].
- Chronic Survival and Perfusion: Allow the animal to survive for a predetermined chronic period (e.g., 8 weeks, 6 months, or over 1 year [76] [18]). Following the survival period, transcardially perfuse the animal with phosphate-buffered saline (PBS) followed by 4% paraformaldehyde (PFA) to fix the brain tissue.
- Brain Sectioning: Extract the brain and cryo-protect it. Section the tissue containing the electrode track into thin slices (e.g., 20-40 μm) using a cryostat or vibratome.
- Immunohistochemical Staining: Immunostain the tissue sections with primary antibodies against key biomarkers:
- Glial Fibrillary Acidic Protein (GFAP) to label reactive astrocytes.
- Ionized Calcium-Binding Adapter Molecule 1 (Iba1) to label activated microglia.
- NeuN to label neuronal nuclei and assess neuronal density around the implant.
- Confocal Microscopy and Quantification: Image the stained sections using confocal microscopy. Quantify the intensity of GFAP and Iba1 staining in concentric zones (e.g., 0–50 μm, 50–100 μm) from the electrode track interface. Simultaneously, quantify neuronal density within these zones to assess neuronal loss [76].
Protocol for Longitudinal Electrophysiological Stability Testing
This protocol describes the methodology for tracking the functional performance of implanted BCIs over time in human or animal subjects.
- System Implantation and Calibration: Implant the BCI system, such as an electrocorticography (ECoG)-based device [77] or a flexible deep brain interface [76]. After a post-surgical recovery period, perform an initial calibration task to identify the signal features (e.g., High-Frequency Band (HFB) power, 65–95 Hz) that correlate with the user's intended motor commands or cognitive tasks [77].
- Regular Task Performance: At regular intervals (e.g., monthly), have the subject perform standardized BCI control tasks. These should include:
- Data Collection and Analysis: During each session, record:
- Long-Term Trend Analysis: Use linear regression models to evaluate the presence of significant trends in HFB power, performance accuracy, and impedance over the entire study period (e.g., 36 months) [77].
The Scientist's Toolkit: Essential Research Reagent Solutions
The following table details key reagents, materials, and tools essential for research in BCI biocompatibility and long-term stability.
Table 3: Research Reagent Solutions for BCI Biocompatibility Studies
| Item Name | Function/Application | Specific Use Case |
|---|---|---|
| Flexible Polymer Substrates (e.g., Polyimide) | Serves as the base material for soft electrode arrays [76]. | Fabrication of flexible neural interfaces with reduced mechanical mismatch against brain tissue. |
| Novel Soft Materials (e.g., Axoft's Fleuron) | Ultra-soft implant material for high biocompatibility [18]. | Enables high-density, minimally invasive sensors for long-term single-neuron recording. |
| Graphene-Based Electrodes | Provides ultra-high signal resolution and mechanical strength [18]. | Used for decoding therapy-specific biomarkers and delivering adaptive neurostimulation. |
| Anti-GFAP Antibody | Labels reactive astrocytes in immunohistochemistry [76]. | Histological quantification of astrogliosis and glial scar formation around implants. |
| Anti-Iba1 Antibody | Labels activated microglia in immunohistochemistry [76]. | Histological assessment of microglial activation and neuroinflammatory response. |
| PEG-based Coating | Temporarily bonds flexible electrodes to rigid shuttles [76]. | Enables precise implantation of flexible electrodes; dissolves upon insertion to release the shuttle. |
| High-Frequency Band (HFB) Power Analysis | Computational feature for decoding neural states [77]. | Serves as a stable control signal for BCIs; used to track signal quality and user intent over time. |
Visualizing Signaling Pathways and Experimental Workflows
The following diagrams, generated using Graphviz DOT language, illustrate the key biological processes and experimental methodologies.
Foreign Body Response Signaling Pathway
Foreign Body Response Pathway - This diagram visualizes the key cellular signaling events leading to glial scar formation and subsequent signal degradation following electrode implantation [76].
BCI Stability Assessment Workflow
BCI Stability Assessment Workflow - This flowchart outlines the multi-modal experimental approach for evaluating the long-term stability of invasive BCIs, integrating electrophysiological, functional, and histological data streams [77] [76].
Within Brain-Computer Interface (BCI) control applications research, the transition from offline analysis to online closed-loop operation represents a critical, translational leap. Offline analysis, which involves modeling and decoding pre-recorded brain signal datasets, is a crucial preliminary step. However, it cannot fully replicate the dynamics of a real-time system where the user receives feedback and adapts their strategy accordingly [78]. This disconnect often leads to a significant performance gap between offline model accuracy and the efficacy of an online system [78]. Consequently, online evaluation is the gold standard for validating BCI performance and a critical milestone on the path from laboratory research to practical, real-world applications [78]. This document outlines the core principles, performance metrics, and experimental protocols essential for executing and validating this transition.
Comparative Performance Analysis: Offline vs. Online BCI Systems
The quantitative disparity between offline and online performance underscores the necessity of closed-loop validation. The following table summarizes key comparative metrics based on empirical research.
Table 1: Performance Comparison Between Offline Analysis and Online Closed-Loop BCI Systems
| Performance Metric | Offline Analysis | Online Closed-Loop System | Notes and Implications |
|---|---|---|---|
| Primary Objective | Model training and initial validation; feature discovery [78] | Real-time user intent decoding and device control [78] | Offline analysis is a preparatory step for online implementation. |
| Reported Accuracy | Often high (>90% in controlled datasets) | Typically lower and more variable; reflects real-world usability [78] | High offline accuracy does not guarantee successful online control. |
| Throughput/ Speed | Not applicable (post-processing) | Critical metric; e.g., Target Acquisition Rate, Information Transfer Rate (ITR) [79] | For a finger decoding iBCI, an acquisition rate of 76 targets/minute has been demonstrated [79]. |
| User Adaptation & Neurofeedback | Absent | Integral to the system; enables user learning and system co-adaptation [80] | Forms a critical feedback loop, enhancing control over time. |
| Performance Validation | Cross-validation on static data splits [78] | Gold standard: Real-time, closed-loop operation with the end-user [78] | Online testing is the only method to validate a BCI's functional utility. |
Experimental Protocols for Online BCI Implementation
Transitioning to an online system requires a structured experimental workflow. The protocol below details the key stages, from initial setup to closed-loop validation.
Protocol: Establishment of an Online Closed-Loop BCI
I. Objective To construct and validate a closed-loop BCI system that enables a user to control an external application or device in real-time using their brain activity.
II. Materials and Reagents
- Signal Acquisition Hardware: EEG cap with electrodes (e.g., 64-channel) or implanted microelectrode arrays (e.g., 96-channel Utah arrays) [79] [80].
- Amplification and Digitization System: High-quality biosignal amplifiers with appropriate sampling rates (e.g., >250 Hz for EEG).
- Processing Computer: Computer with specialized BCI software (e.g., BCI2000, OpenVibe) or custom software (e.g., in Python/MATLAB) for real-time signal processing.
- Stimulus Presentation Module: Monitor for displaying visual paradigms (e.g., for P300 or SSVEP) or a virtual reality environment [78] [79].
- Output Device: The application to be controlled (e.g., speller, robotic arm, functional electrical stimulation (FES) system, or virtual quadcopter) [81] [79].
III. Methodology
Step 1: Paradigm Design and Offline Calibration
- Paradigm Selection: Choose a BCI paradigm suitable for the application (e.g., Motor Imagery for neurorehabilitation, P300 for communication, SSVEP for rapid control) [82].
- Data Collection for Model Training: Instruct the user to perform specific mental tasks or attend to external stimuli according to the paradigm. Record the corresponding brain signals (e.g., EEG).
- Offline Modeling: Preprocess the recorded data (filtering, artifact removal). Extract relevant features (e.g., band power, event-related potentials) and train a decoding algorithm (e.g., Support Vector Machine, Convolutional Neural Network, or a temporally convolved feed-forward network for continuous decoding) [3] [79]. Validate the model using cross-validation.
Step 2: System Integration and Open-Loop Testing
- Real-time Pipeline Implementation: Implement the trained model in a real-time software pipeline that continuously acquires signals, extracts features, and runs the decoding algorithm.
- Open-Loop Testing (Cued Feedback): Have the user perform the mental tasks again. The system decodes the signals and provides visual feedback (e.g., moving a cursor) on the screen, but this feedback does not yet control an external device. This step verifies the real-time signal processing chain.
Step 3: Closed-Loop Validation and Performance Assessment
- Task Initiation: Engage the closed-loop system. The user's decoded brain signals now directly control the output device (e.g., a virtual hand avatar or a quadcopter) [79].
- Performance Metrics Collection: Conduct a series of goal-oriented trials. For a control task, this may involve acquiring targets [79]. Collect quantitative metrics such as:
- Task Completion Time: Time to successfully select a target or complete a trajectory.
- Target Acquisition Rate: Number of targets acquired per minute [79].
- Accuracy: Percentage of correct selections or trials.
- Information Transfer Rate (ITR): A composite metric of speed and accuracy, measured in bits per second [83].
- Iterative Refinement: Use the data from closed-loop sessions to recalibrate and improve the decoding model, accounting for the user's adaptive brain patterns [78].
IV. Notes
- The leap from Step 1 (Offline) to Step 3 (Online) is qualitative and represents the core of BCI translation [78].
- User fatigue and motivation are significant factors in online performance and must be considered during experimental design.
Workflow Visualization: The BCI Closed-Loop Cycle
The following diagram illustrates the continuous, cyclical process of a closed-loop BCI system, which is fundamental to its operation.
The Scientist's Toolkit: Essential Research Reagents & Materials
Successful implementation of online BCI systems relies on a suite of specialized tools and reagents. The following table catalogs key components.
Table 2: Essential Research Reagents and Materials for Online BCI Systems
| Category | Item/Solution | Function/Application | Example & Notes |
|---|---|---|---|
| Signal Acquisition | Electroencephalography (EEG) Cap | Non-invasive recording of electrical brain activity from the scalp [80]. | 64-channel Ag/AgCl electrode caps. Requires electrolyte gel for impedance reduction. |
| Intracortical Microelectrode Array | Invasive recording of multi-unit neural activity with high spatial and temporal resolution [79]. | 96-channel Utah array implanted in motor cortex. Used in pilot clinical trials (e.g., BrainGate2) [79]. | |
| Signal Processing | Machine Learning Algorithms | To decode user intent from neural features in real-time [3] [82]. | Support Vector Machines (SVM), Convolutional Neural Networks (CNN), Transfer Learning (TL) [3]. |
| Real-Time Processing Software | Platform for implementing the closed-loop BCI pipeline [78]. | BCI2000, OpenVibe, or custom Python/MATLAB scripts. | |
| Control Application | Virtual Environment | A safe, configurable platform for task practice and performance assessment [79]. | Unity or Unreal Engine for rendering avatars (e.g., a virtual hand) and obstacle courses [79]. |
| Functional Electrical Stimulation (FES) | Provides neurorehabilitation by activating paralyzed muscles based on decoded motor commands [81]. | Integrated into a BCI-FES system for restoring movement [81]. | |
| Experimental Paradigms | Motor Imagery (MI) Paradigm | User imagines body movement (e.g., hand, foot) to generate control signals [82]. | Induces Event-Related Desynchronization (ERD) in sensorimotor rhythms. |
| P300 Paradigm | User focuses on rare, target stimuli within a rapid sequence, eliciting a detectable brain potential [82]. | Basis for communication spellers. | |
| Steady-State Visual Evoked Potential (SSVEP) | User gazes at a visual stimulus flickering at a fixed frequency, causing brain oscillations at the same frequency [82]. | Allows for high-information-throughput control. |
Brain-Computer Interfaces (BCIs) are systems that enable direct communication between the brain and external devices by acquiring and translating brain signals into commands, bypassing normal neuromuscular pathways [84]. The effectiveness of a BCI hinges on the accurate interpretation of noisy, high-dimensional neural data, a process fraught with complex challenges that are naturally formulated as optimization problems [85]. Without optimization, selecting optimal parameters—such as the best EEG channels or the most discriminative features for classifying mental tasks—requires extensive domain knowledge and repeated experimentation, which is often impractical [85].
Evolutionary Algorithms (EAs), a class of stochastic optimization techniques inspired by natural selection, have emerged as powerful tools for navigating these complex search spaces. Their ability to handle non-linear, multi-modal objective functions without requiring gradient information makes them particularly suited to the idiosyncratic nature of brain signals, which vary significantly between users and sessions [86] [85]. This document details how key challenges in BCI systems can be formulated as optimization problems and addressed through EAs, providing application notes and detailed protocols for researchers.
Key BCI Challenges Formulated as Optimization Problems
The development of a robust BCI involves multiple stages, each presenting unique optimization challenges. The table below summarizes the primary challenges, their formulation as optimization problems, and the evolutionary algorithms employed to solve them.
Table 1: Formulation of BCI Challenges as Optimization Problems
| BCI Challenge | Optimization Formulation | Commonly Used Evolutionary Algorithms | Objective Function |
|---|---|---|---|
| Channel Selection [85] | Find the subset of EEG channels that maximizes classification accuracy while minimizing the number of channels. | Genetic Algorithm (GA), Particle Swarm Optimization (PSO) | Maximize accuracy; Minimize channel count |
| Feature Optimization [85] | Identify the optimal set of features (e.g., spectral, temporal) that provides the best discrimination between target mental states. | Genetic Algorithm (GA), Differential Evolution (DE) | Maximize inter-class distance; Minimize intra-class variance |
| Classifier Parameter Tuning [86] [85] | Find the hyperparameters of a classifier (e.g., neural network topology, SVM kernel parameters) that minimize prediction error. | GA, PSO, Ant Colony Optimization (ACO) | Minimize classification error rate |
| Mental Task & Frequency Band Selection [87] | Select the combination of mental tasks and reactive frequency band for a specific user that maximizes the performance of a multi-class BCI. | Individual performance-based selection (akin to a search algorithm) | Maximize geometric mean of class-wise accuracies |
| Artifact Removal [85] | Find optimal parameters for adaptive filters or other denoising techniques to remove physiological and technical artifacts from EEG. | GA, Artificial Bee Colony (ABC), Firefly Algorithm | Minimize mutual information between clean and corrupted EEG; Minimize error from desired signal |
Protocol: User-Centered Optimization of Mental Tasks and Frequency Bands
Objective: To individually optimize the mental task combination and reactive frequency band for a multi-class BCI, thereby enhancing user performance and robustness [87].
Materials:
- High-resolution multi-channel EEG system.
- Stimulus presentation software.
- Computing hardware capable of real-time signal processing and EA execution.
Procedure:
- Screening Session (Baseline Data Collection):
- Record multi-channel EEG from a naïve user while they perform seven distinct mental tasks: Mental Rotation, Word Association, Auditory Imagery, Mental Subtraction, Spatial Navigation, Motor Imagery (Left Hand), and Motor Imagery (Both Feet) [87].
- Each task should be cued and performed for a defined period (e.g., 6-second imagery period).
Individualized Optimization:
- Feature Extraction: For each mental task, extract features (e.g., band power) from a broad frequency range (8-30 Hz) using overlapping time windows.
- Task Combination Selection: Evaluate the classification performance (using a classifier like Fisher's Linear Discriminant Analysis) for different 4-class combinations of the seven tasks. Select the combination that yields the highest geometric mean of class-wise accuracies to ensure balanced performance across all tasks [87].
- Frequency Band Selection: Optimize the reactive frequency band individually for the selected task combination. The objective is to find the frequency range that maximizes the geometric mean classification accuracy [87].
Online Feedback and Calibration:
- To minimize the difference in brain activity between calibration and feedback sessions, present sham feedback during screening and calibration runs. Inform the user that this feedback is not based on their brain signals [87].
- Classifier bias should be adapted at the start of each subsequent session.
Iterative Refinement:
- The number and timing of classifier updates should be varied individually based on user performance across sessions.
The Role of Evolutionary Algorithms in BCI Optimization
Evolutionary Algorithms provide a robust framework for solving the non-convex, high-dimensional optimization problems inherent in BCI systems. Their population-based search strategy is effective for avoiding local minima and does not require problem-specific gradient information [85].
Protocol: Channel Selection using a Genetic Algorithm (GA)
Objective: To reduce the dimensionality of the EEG data and find an optimal subset of channels that maintains or improves classification performance for a given paradigm (e.g., Motor Imagery).
Procedure:
- Chromosome Encoding: Represent a potential solution as a binary string (chromosome) of length N, where N is the total number of channels. A value of '1' indicates the channel is selected, and '0' indicates it is discarded [85].
- Fitness Evaluation: Define a fitness function that balances accuracy and parsimony. For each chromosome (subset of channels), the fitness can be calculated as:
Fitness = α * (Classification Accuracy) + β * (1 - (Number of Selected Channels / Total Channels))where α and β are weights that prioritize accuracy versus model complexity [85]. - Evolutionary Process:
- Initialization: Generate an initial population of random binary strings.
- Selection: Use a selection method (e.g., tournament selection) to choose parent chromosomes based on their fitness.
- Crossover and Mutation: Apply genetic operators to the parents to create offspring. This involves swapping segments of the binary strings (crossover) and randomly flipping bits (mutation) to explore the search space.
- Termination: Repeat the process of selection, crossover, and mutation for a predetermined number of generations or until a performance plateau is reached. The chromosome with the highest fitness in the final generation represents the optimized channel set.
The following diagram illustrates the logical workflow of this optimization process.
GA for Channel Selection
Experimental Protocols & The Scientist's Toolkit
Detailed Experimental Workflow
Integrating optimization into a BCI experiment involves a structured pipeline. The diagram below outlines the key stages from data acquisition to the final optimized system, highlighting the iterative optimization feedback loop.
BCI Optimization Pipeline
Research Reagent Solutions and Essential Materials
Table 2: Key Materials and Tools for BCI Optimization Research
| Item / Tool | Function / Application in BCI Optimization |
|---|---|
| High-Density EEG System (e.g., 64+ channels) [85] | Acquires raw brain signal data with sufficient spatial resolution for channel selection algorithms. |
| Electrocorticography (ECoG) Grids [84] [88] | Provides higher signal-to-noise ratio neural data for invasive BCI paradigms; used in clinical trials. |
| Genetic Algorithm & PSO Libraries (e.g., in Python/MATLAB) [85] | Provides the computational engine for solving feature selection, channel selection, and parameter tuning problems. |
| Common Spatial Patterns (CSP) Algorithm [87] | A feature extraction method used for MI data; its parameters can be optimized. |
| Deep Learning Frameworks (e.g., TensorFlow, PyTorch) [86] [89] | Used to build complex neural decoders; EAs can optimize hyperparameters like learning rate, network topology, etc. |
| Public BCI Datasets (e.g., BCI Competition IV, PhysioNet) [89] | Benchmark datasets for developing and validating new optimization algorithms. |
Formulating BCI challenges as optimization problems and employing Evolutionary Algorithms provides a systematic and powerful methodology to enhance system performance, usability, and individualization. The protocols and frameworks outlined here offer researchers a pathway to tackle the inherent complexities of neural data, from channel and feature selection to the tuning of deep learning models [89].
Future work will likely focus on multi-objective optimization approaches that explicitly model the trade-offs between competing goals like accuracy, speed, and user comfort [86]. Furthermore, as BCIs transition from research labs to clinical and consumer markets, policy considerations regarding data privacy, device maintenance, and insurance coverage will become increasingly important, requiring parallel development in the ethical and regulatory frameworks that support this transformative technology [90].
Evaluating BCI Efficacy: Validation Frameworks and Comparative Technology Analysis
Brain-computer interface (BCI) technology represents a revolutionary advancement in human-computer interaction, with significant potential to restore communication, mobility, and independence for patients with severe neurological disorders [78] [57]. Historically, the field has prioritized technical performance metrics, notably classification accuracy and information transfer rate (bit rate), as the primary indicators of a system's success. However, a considerable gap persists between these laboratory benchmarks and the effective translation of BCI systems into practical, real-world applications [78] [91].
A BCI system's ultimate goal is not merely to decode neural signals with high precision but to provide a functional, reliable, and satisfying tool for the end-user. This requires a paradigm shift from a purely technology-centered focus to a user-centered evaluation framework that comprehensively assesses usability, user satisfaction, and real-world usage [78]. Such an approach is critical for developing BCIs that are not only technically robust but also genuinely meet the needs of users, thereby accelerating the transition from research prototypes to integrated clinical and assistive solutions.
Core Evaluation Pillars: Defining the Framework
A comprehensive evaluation of BCI systems rests on three interconnected pillars: Usability, User Satisfaction, and Usage. These dimensions provide a holistic view of a system's practical value.
- Usability encompasses the system's effectiveness (accuracy and completeness in achieving user goals) and efficiency (resources expended, such as time and mental effort, to achieve those goals) [78]. It answers the question: "Can the user reliably and effortlessly accomplish the intended task?"
- User Satisfaction is a qualitative measure of the user's perceptions, feelings, and opinions about using the BCI system [78]. This includes aspects like comfort, perceived utility, and freedom from frustration, which are crucial for long-term adoption.
- Usage refers to the match between the system and the user's specific requirements and context [78]. It evaluates whether the system's functionality aligns with the user's daily needs, environment, and physical or cognitive abilities.
The transition of BCI systems from laboratory curiosities to real-world products involves two critical leaps: first, from offline data analysis to the construction of online BCI prototype systems, and second, from these prototypes to viable real-world products. Comprehensive evaluation is the essential bridge for this second, more challenging leap [78].
Quantitative Metrics and Data Presentation
Moving beyond classification accuracy requires a standardized set of metrics to quantify performance across the three core pillars. The table below summarizes key quantitative measures for evaluating online BCI systems.
Table 1: Comprehensive Quantitative Metrics for Online BCI System Evaluation
| Evaluation Pillar | Metric Category | Specific Metrics | Description and Significance |
|---|---|---|---|
| Usability | Effectiveness | Task Completion Rate, Error Rate | Measures the reliability of the system in fulfilling intended commands or tasks. |
| Efficiency | Time to Complete Task, Information Transfer Rate (Bit Rate), Mental Workload (e.g., NASA-TLX) | Assesses the speed and cognitive resources required for system operation. | |
| User Satisfaction | Perceived Usability | System Usability Scale (SUS), Usefulness Scales | Standardized questionnaires to gauge the user's subjective experience and perceived value. |
| BCI-Specific Factors | Fatigue, Comfort, Aesthetics, Intuitiveness | Qualitative feedback on physical and psychological aspects of interacting with the BCI. | |
| Usage & Context | Technical Performance | Online Classification Accuracy, Latency, Robustness to Noise | Core technical indicators measured during real-time, closed-loop operation. |
| Comparative Value | Performance vs. Non-BCI Alternatives (e.g., eye tracking) | Establishes the added benefit of BCI control in realistic application scenarios [92] [91]. |
Recent studies demonstrate the power of this multi-faceted approach. For instance, a groundbreaking speech neuroprosthesis achieved a remarkable 97% accuracy in translating brain signals into text, a key effectiveness metric [93]. Meanwhile, research into Motor Imagery (MI)-based BCIs highlights the importance of efficiency, noting challenges like the need for lengthy user and model training sessions that can impact mental workload [92] [91].
Experimental Protocols for Comprehensive Evaluation
To ensure findings are comparable and reproducible, structured experimental protocols are essential. The following provides a detailed methodology for a user-centric evaluation.
Protocol: A Multi-Phase User-Centric BCI Evaluation
This protocol, designed for evaluating a BCI control system integrated with augmented reality (AR) and eye tracking, is adaptable to various BCI applications [92] [91].
Research Design: The study is structured into three sequential phases:
- Technical Validation: The BCI prototype's technical robustness is validated in a controlled lab setting to ensure basic functionality and signal decoding reliability.
- Performance Assessment: The system's performance is evaluated with participants completing defined tasks.
- Comparative Analysis & User Experience: A detailed comparison with an alternative control method (e.g., eye tracking) is conducted, incorporating in-depth user experience evaluations.
Materials and Reagents: Table 2: Research Reagent Solutions and Essential Materials for BCI Evaluation
| Item | Function / Application | Specific Examples / Parameters |
|---|---|---|
| EEG Acquisition System | Non-invasively measures electrical brain activity from the scalp. | High-density EEG cap with amplifiers; parameters like sampling rate (e.g., 250-1000 Hz), electrode montage. |
| Signal Processing Software | Preprocesses raw EEG data to improve signal-to-noise ratio (SNR). | Filters (e.g., bandpass 0.5-40 Hz), artifact removal algorithms (e.g., for eye blinks, muscle movement). |
| Machine Learning Decoder | Translates preprocessed brain signals into device commands. | Algorithms like Support Vector Machines (SVM), Convolutional Neural Networks (CNN), or Linear Discriminant Analysis for classification of MI paradigms. |
| Augmented Reality (AR) Headset | Displays environment-aware actions and guides users. | Provides visual feedback and a user interface, overlaying command options onto the real world. |
| Eye Tracker | Provides an alternative control modality for comparative analysis. | Dedicated eye-tracking glasses or integrated AR eye-tracking for gaze-based selection. |
| Assessment Questionnaires | Quantifies user satisfaction and perceived workload. | Standardized forms like the System Usability Scale (SUS) and NASA Task Load Index (TLX). |
Procedure:
- Participant Recruitment and Calibration: Recruit participants representing the target user group. Fit the EEG cap and AR/eye-tracking equipment. Collect calibration data for the BCI decoder by having the user perform specific mental tasks (e.g., motor imagery of left vs. right hand).
- Task Performance (Phase 2): Participants use the BCI system to perform a series of ecologically valid tasks, such as:
- Object Sorting: Categorizing objects into different bins using BCI commands.
- Pick and Place: Controlling a robotic arm to pick up an object and move it to a designated location.
- Board Game Play: Operating a simple computer game to assess learning and adaptability.
- Comparative Evaluation (Phase 3): Participants repeat a subset of the tasks using a non-BCI control method, such as eye tracking. The order of BCI and alternative method testing should be counterbalanced.
- Data Collection: Throughout the experiment, collect:
- Quantitative Data: Task completion time, success rate, BCI command accuracy, and bit rate.
- Qualitative Data: Administer post-task and post-study questionnaires (SUS, NASA-TLX) and conduct semi-structured interviews to gather feedback on comfort, frustration, and system intuitiveness.
Data Analysis:
- Employ statistical tests (e.g., t-tests, ANOVA) to compare quantitative performance metrics between the BCI system and the alternative control method.
- Perform thematic analysis on qualitative interview data to identify recurring themes related to user satisfaction and usability challenges.
Diagram 1: A multi-phase user-centric BCI evaluation workflow.
Current State and Forthcoming Directions in BCI Evaluation
The BCI field is increasingly recognizing the importance of these comprehensive evaluation methods. As of 2025, the technology is in a transitional phase, moving from laboratory experiments toward clinical and real-world application, akin to the early stages of gene therapy or heart stent development [2]. This shift is underscored by the awarding of prestigious honors, like the 2025 Top Ten Clinical Research Achievement Award, to studies that demonstrate not only high accuracy but also real-world impact, such as restoring speech to patients with amyotrophic lateral sclerosis (ALS) [93].
Major companies and research initiatives are now driving this translation. Key players include:
- Invasive/Implantable BCIs: Neuralink, Synchron, Blackrock Neurotech, Paradromics, and Precision Neuroscience are advancing high-fidelity interfaces, with several having initiated human trials [2].
- Non-Invasive BCIs: Research continues into EEG-based systems, often enhanced by shared control strategies, augmented reality, and sensor fusion (e.g., with eye tracking) to improve usability and reduce mental workload [92] [91].
The integration of Artificial Intelligence (AI) and Machine Learning (ML) is pivotal for the future of BCI evaluation and performance. Techniques like transfer learning (TL) and deep learning (e.g., Convolutional Neural Networks) are being leveraged to create more adaptive systems that require shorter calibration times and are more robust to the non-stationary nature of EEG signals, directly addressing key usability challenges [15].
The journey of BCI from a fascinating laboratory demonstration to an indispensable tool in clinical and assistive settings hinges on a fundamental evolution in how we define and measure its success. Sole reliance on classification accuracy is an inadequate paradigm for translation. By adopting a comprehensive, user-centered framework that rigorously assesses usability, user satisfaction, and real-world usage through standardized protocols and metrics, researchers and developers can bridge the gap between technical potential and practical impact. This holistic approach ensures that the next generation of BCI systems will be engineered not just for high performance, but for real people with real needs, thereby fulfilling the transformative promise of this revolutionary technology.
Brain-Computer Interfaces (BCIs) represent a transformative neurotechnology that establishes a direct communication pathway between the brain and external devices. For researchers and clinicians, the fundamental choice between invasive and non-invasive approaches hinges on a trade-off between signal fidelity and procedural risk. Invasive BCIs involve surgical implantation of electrodes directly onto or into brain tissue, while non-invasive techniques measure neural activity from the scalp surface [94]. This article provides a structured, comparative analysis of these two paradigms, framing them within the context of BCI control applications research. It offers detailed experimental protocols and reagent solutions to guide preclinical and clinical investigations, aiding in the selection and optimization of BCI systems for specific therapeutic and research objectives.
Comparative Analysis: Performance and Applications
The selection of a BCI modality is dictated by the requirements of the specific application, balancing the need for high-quality data against safety and practicality. The following tables provide a quantitative and qualitative comparison to inform this decision.
Table 1: Quantitative Comparison of Invasive and Non-Invasive BCI Modalities
| Characteristic | Invasive BCIs (e.g., ECoG, Utah Array) | Non-Invasive BCIs (e.g., EEG, fNIRS) |
|---|---|---|
| Spatial Resolution | Millimetre-scale (ECoG) to single-neuron (Microelectrodes) [95] | Centimetre-scale; limited by skull and scalp [95] [94] |
| Temporal Resolution | Very High (< Millisecond) [94] | High (Milliseconds for EEG) [94] |
| Signal-to-Noise Ratio (SNR) | High [96] [94] | Low to Moderate; susceptible to artifacts [96] [94] |
| Typical Accuracy (Complex Tasks) | 85% - 95% [96] | 65% - 75% [96] |
| Information Transfer Rate (ITR) | High | Low to Moderate |
| Setup & Calibration Time | Long (Surgical procedure required) | Short (Minutes to hours) [94] |
Table 2: Clinical Suitability and Risk Profile Analysis
| Factor | Invasive BCIs | Non-Invasive BCIs |
|---|---|---|
| Primary Risks | Surgical risks (infection, bleeding, tissue damage), long-term biocompatibility issues, signal degradation from scarring [96] [94] | Minimal physical risk; primarily related to comfort and data privacy [97] [94] |
| Regulatory Pathway | Stringent (FDA Breakthrough Device, PMA) [2] [98] | Less stringent (510(k) clearance for some devices) [2] |
| Key Applications | Restoration of complex motor functions, high-performance prosthetic control, speech decoding for paralysis [2] [99] | Neurofeedback, basic communication (P300 spellers), stroke rehabilitation, gaming, and human-computer interaction [100] [97] |
| User Acceptability | Lower due to invasiveness; reserved for high-medical-need cases [94] | High; suitable for broad populations including healthy users [94] |
| Cost & Scalability | High cost; limited to specialized clinical centers [101] [98] | Lower cost; potential for large-scale deployment and home use [101] [98] |
Experimental Protocols for BCI Control Applications
Protocol: Assessing Motor Imagery Control with Non-Invasive EEG
This protocol outlines a standard procedure for evaluating the efficacy of a motor imagery-based BCI for controlling an external device, such as a robotic arm or a cursor.
1. Objective: To quantify the performance of an EEG-based BCI in translating motor imagery (e.g., left vs. right hand) into discrete control commands for an external device.
2. Materials & Setup:
- Participants: Recruit healthy adults or target patient populations (e.g., stroke survivors). Obtain informed consent.
- EEG System: A high-density (e.g., 64-channel) or consumer-grade (e.g., Emotiv EPOC+) EEG headset [97].
- Software: BCI software platform (e.g., OpenBCI, BCI2000, or custom Python/MATLAB toolbox) for signal processing and machine learning [95].
- Stimulus Presentation: A computer screen to display visual cues for motor imagery tasks.
- External Device: A robotic arm, a computer cursor, or a virtual simulation for control output.
3. Procedure:
- Step 1: Preparation & Calibration. Fit the EEG cap on the participant. Apply electrode gel to ensure impedance is below 5 kΩ. Record 5 minutes of resting-state data (eyes open/closed) for baseline analysis.
- Step 2: Task Paradigm. Employ a cue-based paradigm. Each trial should consist of: (i) a fixation cross (2 s), (ii) a visual cue indicating the required motor imagery (e.g., left or right arrow; 3-4 s), and (iii) a rest period (randomized 2-3 s). Conduct a minimum of 100 trials per class.
- Step 3: Signal Processing.
- Preprocessing: Apply a band-pass filter (e.g., 8-30 Hz for Mu/Beta rhythms) and a notch filter (50/60 Hz). Use Independent Component Analysis (ICA) to remove ocular and muscular artifacts [97].
- Feature Extraction: For each channel and trial, compute the log-variance of signals in specific frequency bands. Alternatively, use Common Spatial Patterns (CSP) to enhance the discriminability between two classes of motor imagery [97].
- Classification: Train a linear discriminant analysis (LDA) or support vector machine (SVM) classifier on 70-80% of the trial data. Use the remaining data for testing.
- Step 4: Closed-Loop Control. Implement the trained model in real-time. The participant's motor imagery is decoded and translated into continuous or discrete commands for the external device. Provide visual feedback on performance.
- Step 5: Data Analysis. Calculate the classification accuracy and Information Transfer Rate (ITR) across all trials. Use the system's built-in metrics or custom scripts.
4. Key Outcomes:
- Classification accuracy (%) for distinguishing between different motor imagery tasks.
- Information Transfer Rate (bits/min) as a measure of communication speed.
- Latency between cue presentation and successful command execution.
Diagram: Non-Invasive BCI Motor Imagery Workflow
Protocol: Evaluating High-Fidelity Control with an Invasive BCI Array
This protocol describes a methodology for assessing the performance of an implanted microelectrode array for complex, multi-degree-of-freedom control.
1. Objective: To evaluate the precision and latency of an invasive BCI (e.g., Utah Array, Neuropixels) in enabling a user to control a multi-joint robotic prosthesis or a computer cursor in a 3D environment.
2. Materials & Setup:
- Participants: Typically, individuals with severe paralysis enrolled in an FDA-approved clinical trial (e.g., Neuralink PRIME, Blackrock Neurotech) [2] [99].
- Implanted System: A surgically implanted microelectrode array (e.g., Utah Array with 96-128 channels) connected to a percutaneous pedestal or a fully implanted wireless device (e.g., Neuralink N1) [2] [95].
- Neural Signal Processor: A real-time system for amplifying, filtering, and spike sorting raw neural data (e.g., Blackrock Neurotech Cerebus system).
- Decoding Computer: A high-performance computer running custom decoding algorithms (e.g., Kalman filter, Recurrent Neural Network).
- Output Device: A complex robotic arm or a high-fidelity virtual reality environment.
3. Procedure:
- Step 1: Surgical Implantation. The microelectrode array is implanted in the targeted brain region (e.g., primary motor cortex for hand control) by a neurosurgeon. This is a terminal procedure performed once per participant under an approved protocol [2].
- Step 2: Signal Acquisition & Spike Sorting. Record extracellular action potentials and local field potentials. Apply spike-sorting algorithms (e.g., K-means clustering, PCA) to isolate single- or multi-unit activity from individual electrodes [95].
- Step 3: Decoder Calibration. The participant is asked to observe or imagine performing specific movements (e.g., reaching, grasping). The relationship between neural firing rates and the kinematics (velocity, position) of the intended movement is mapped using a Kalman filter or similar decoder. This calibration is often performed over several sessions.
- Step 4: Task Performance Assessment. The participant uses the calibrated BCI to perform functional tasks. These can include:
- Center-Out Reaching Task: Moving a cursor from the center of a screen to peripheral targets. Measures throughput (bits/s) and path efficiency.
- Activities of Daily Living (ADL): Tasks such as picking up and moving objects with a robotic arm, or controlling a wheelchair.
- Speech Decoding: For speech neuroprosthetics, the participant attempts to speak or imagine speaking while neural activity is decoded into text using models like RNNs or Transformers [2] [100].
- Step 5: Longitudinal Monitoring. Continuously monitor signal stability, decoder performance, and any adverse events over weeks, months, or years.
4. Key Outcomes:
- Task completion rate and time for ADLs.
- Throughput (bits/second) in a standardized reaching task.
- For speech BCIs: word error rate and words-per-minute decoding speed.
Diagram: Invasive BCI Evaluation Workflow
The Scientist's Toolkit: Key Research Reagents & Materials
Table 3: Essential Materials for BCI Control Applications Research
| Item | Function/Application | Examples & Notes |
|---|---|---|
| High-Density EEG Systems | Gold standard for non-invasive neural signal acquisition in research. | Examples: BrainAmp, Biosemi. Function: Provides high-temporal-resolution data for motor imagery, P300, and SSVEP paradigms [97]. |
| Dry Electrode EEG Headsets | Enables rapid setup and consumer-friendly BCI applications. | Examples: Emotiv EPOC+, OpenBCI Galea. Function: Suitable for neurofeedback, gaming, and some clinical rehabilitation studies with slightly compromised signal quality [102] [97]. |
| Microelectrode Arrays | The core hardware for invasive BCI, recording from populations of neurons. | Examples: Blackrock Utah Array, Neuralink N1, Neuropixels. Function: Provides high-fidelity single- and multi-unit activity for complex motor and speech decoding [2] [95]. |
| ECoG Grids | A semi-invasive method offering a balance between SNR and reduced tissue damage. | Examples: WIMAGINE implant, Ad-Tech grids. Function: Placed on the cortical surface, used for motor control and seizure monitoring; higher spatial resolution than EEG [95]. |
| fNIRS Systems | Measures hemodynamic responses for brain activity mapping. | Function: Useful when EEG artifacts are high or for studying deeper brain structures. Often used in hybrid EEG-fNIRS systems [100] [97]. |
| Real-Time Signal Processing Toolboxes | Software for implementing BCI pipelines from acquisition to classification. | Examples: BCI2000, OpenViBE, EEGLab, FieldTrip. Function: Provides built-in algorithms for filtering, feature extraction, and machine learning, accelerating development [95]. |
| Kalman Filter & Deep Learning Models | Advanced decoding algorithms for translating neural signals into smooth, continuous control commands. | Function: Kalman filters are standard for kinematic decoding. Deep learning (CNNs, RNNs) is increasingly used for complex pattern recognition like speech decoding [95] [99]. |
The dichotomy between invasive and non-invasive BCIs presents a clear but nuanced landscape for researchers. Invasive interfaces, with their superior signal fidelity, are currently indispensable for restoring complex functions like movement and speech in severely paralyzed individuals, despite their surgical risks and scalability challenges. Non-invasive methods offer a safe, accessible, and rapidly deployable platform for a wide array of applications in rehabilitation, communication, and human-computer interaction, albeit with limited spatial resolution and information bandwidth. The future of BCI control applications lies not only in refining these individual pathways but also in the strategic development of hybrid systems and minimally invasive technologies (e.g., Stentrode, high-density ECoG) that aim to bridge the gap between performance and practicality [2] [96]. Continued research focused on improving neural decoding algorithms, enhancing biocompatibility, and establishing robust ethical frameworks will be critical in unlocking the full potential of BCIs across both clinical and consumer domains.
Within brain-computer interface (BCI) control applications research, the selection of a neural signal acquisition modality represents a critical decision point governed by a trade-off between inherent performance characteristics. Three metrics are paramount for benchmarking these technologies: temporal resolution (the speed at which neural activity is sampled), spatial resolution (the precision in localizing the origin of neural activity), and bit rate (the speed and accuracy of information transfer). These parameters directly determine the feasibility and performance of BCI applications, from high-speed communication to multi-degree-of-freedom prosthetic control. This document provides application notes and experimental protocols for the quantitative benchmarking of these metrics across major BCI modalities, providing a framework for evaluating their suitability for specific research and clinical applications.
Performance Metrics and Comparative Analysis
A comprehensive understanding of the performance landscape across different BCI modalities is essential for experimental design and technology selection. The following sections and summary table provide a quantitative and qualitative comparison.
Table 1: Benchmarking Performance Across BCI Modalities
| Modality | Temporal Resolution | Spatial Resolution | Reported Bit Rates (Information Transfer Rate - ITR) | Key Applications |
|---|---|---|---|---|
| Electroencephalography (EEG) | Very High (milliseconds) [103] | Low (Centimeters). Limited by skull/scalp dispersion [103] [104]. | P300/c-VEP: Up to ~324 bits/min (with advanced decoding) [105].Motor Imagery: Lower, highly user-dependent. | Non-invasive communication, stroke rehabilitation [106] [103]. |
| Electrocorticography (ECoG) | High (Milliseconds) | Standard Grid: Medium (cms) [107].High-Density (HD) Grid: High (millimeters) [107]. | HD-ECoG demonstrated state decoding error of 2.6% vs. 8.5% for standard grids, and movement decoding error of 11.9% vs. 33.1% [107]. | Localizing epilepsy foci, decoding multi-DOF arm movements [107]. |
| Intracortical Microelectrodes | Very High (Microseconds) | Very High (Microns) | Paradromics Connexus BCI: >200 bits per second (bps) with 56ms latency; >100 bps with 11ms latency [108]. | High-performance prosthetic control, communication [108]. |
| Functional Near-Infrared Spectroscopy (fNIRS) | Low (Seconds) due to hemodynamic delay [103]. | Medium (1-2 cm) [104]. | Generally lower than EEG due to slow signal. Improved robustness to noise [103]. | Hybrid systems with EEG, applications where electrical noise is prohibitive [103]. |
| Functional Ultrasound (fUS) | Medium (Tens to Hundreds of Milliseconds) [104] | High (Sub-millimeter) [104] | Emerging technology; precise bit rates not yet standardized. | Next-generation non-invasive imaging; promising for constrained decoding [104]. |
Key Trade-offs and Synergies
The data in Table 1 reveals inherent engineering trade-offs. Non-invasive methods like EEG offer high temporal resolution but suffer from low spatial resolution due to signal blurring by the skull and scalp [103] [104]. Conversely, invasive intracortical methods provide the highest spatial and temporal resolution, enabling unprecedented bit rates as demonstrated by the Paradromics Connexus BCI [108]. ECoG offers a middle ground, with HD grids significantly outperforming standard grids in decoding complex movements like pincer grasp and shoulder rotation [107]. Emerging technologies like fUS aim to break these trade-offs for non-invasive applications, offering high spatial resolution with better temporal resolution than fNIRS [104]. Hybrid systems, such as EEG-fNIRS, are increasingly explored to combine the temporal precision of EEG with the spatial robustness of fNIRS, enhancing overall classification performance and noise immunity [103].
Experimental Protocols for Benchmarking
To ensure reproducible and comparable results, standardizing experimental protocols and performance metrics is crucial. The following protocols are adapted from seminal studies in the field.
Protocol 1: Benchmarking an RSVP-Based BCI with EEG
This protocol is adapted from the benchmark dataset described in [109], designed for target detection tasks.
1. Objective: To acquire a benchmark dataset for evaluating ERP detection algorithms in an RSVP paradigm, measuring classification accuracy and bit rate. 2. Equipment:
- Amplifier: Synamps2 system (Neuroscan) or equivalent.
- EEG Cap: 64-channel electrode cap arranged according to the international 10-20 system.
- Stimulus Display: 23.6-inch LCD screen with a 60 Hz refresh rate.
- Software: MATLAB with Psychophysics Toolbox for stimulus presentation. 3. Experimental Procedure:
- Subjects: Recruit healthy subjects with normal or corrected-to-normal vision. Secure ethical approval and informed consent.
- Stimuli: Use street-view images categorized as "target" (containing a human) and "non-target" (no human). Targets should appear with a low probability (e.g., 1-4%).
- Paradigm:
- Each trial starts with a 0.5 s fixation cross.
- Images are presented sequentially at a rapid rate (e.g., 10 Hz, or 100 ms/image).
- For each subject, conduct multiple blocks (e.g., 2 blocks of 40 trials). Each trial contains a sequence of 100 images.
- Subjects are instructed to press a button upon detecting a target image.
- Data Acquisition:
- Record EEG data at a sampling rate of 1,000 Hz.
- Apply a hardware filter (e.g., 0.15-200 Hz) and a 50 Hz notch filter for power-line noise.
- Send an event marker to the EEG recording system at the onset of each image for precise synchronization. 4. Data Analysis & Benchmarking Metrics:
- Preprocessing: Re-reference data, apply band-pass filtering, and remove bad channels.
- ERP Analysis: epoch EEG data around each stimulus onset (-200 ms to 800 ms). Average trials to visualize ERPs like the P300 component.
- Single-Trial Classification: Use machine learning (e.g., Linear Discriminant Analysis, SVM) to classify single-trial EEG responses as target or non-target.
- Performance Metrics: Calculate classification accuracy, AUC, and Information Transfer Rate (ITR) in bits/min [110].
Protocol 2: Decoding Arm Movements with High-Density ECoG
This protocol is designed to compare the decoding resolution of standard and high-density ECoG grids, as detailed in [107].
1. Objective: To decode the presence/absence and type of six elementary arm movements and compare the performance of standard vs. HD ECoG grids. 2. Equipment:
- ECoG Grids: Standard (4mm diameter, 10mm spacing) and High-Density (2mm diameter, 4mm spacing) grids.
- Amplifier: Bioamplifier system (e.g., NeXus-32) with a sampling rate ≥ 2048 Hz.
- Motion Tracking: Electrogoniometers and/or gyroscopes to track arm movement trajectories. 3. Experimental Procedure:
- Subjects: Patients implanted with ECoG grids over the primary motor cortex (M1) as part of epilepsy monitoring.
- Task:
- Subjects perform six elementary movements with the arm contralateral to the implant: Pincer Grasp/Release, Wrist Flexion/Extension, Forearm Pronation/Supination, Elbow Flexion/Extension, Shoulder Internal/External Rotation, and Shoulder Forward Flexion/Extension.
- For each movement type, perform 4 sets of 25 continuous movement repetitions, with 20-30 s rest periods between sets.
- Precisely synchronize ECoG data acquisition with motion tracker data using a common pulse train. 4. Data Analysis & Benchmarking Metrics:
- Electrode Localization: Co-register pre-op MRI with post-op CT scans to anatomically localize ECoG electrodes over M1.
- Signal Processing:
- Filter data into key frequency bands: μ (8-13 Hz), β (13-30 Hz), low-γ (30-50 Hz), and high-γ (80-160 Hz).
- Calculate the power in each band and generate feature vectors.
- Decoding Models:
- State Decoder: Train a binary classifier (e.g., SVM) to detect movement vs. idling states.
- Movement Decoder: Train a six-class classifier to identify which elementary movement was performed.
- Performance Metrics: Evaluate and compare decoders based on standard and HD grids using decoding error rates (%) across different frequency band combinations [107].
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Materials and Tools for BCI Benchmarking Experiments
| Item | Function | Example(s) |
|---|---|---|
| EEG System | Non-invasive recording of electrical brain activity. | 64-channel Synamps2 system; high-density EEG caps (10/20, 10/10 international system) [109] [103]. |
| ECoG Grids | Subdural recording of cortical potentials. | Standard platinum grids (4mm, 10mm spacing); High-density platinum grids (2mm, 4mm spacing) from Integra LifeSciences [107]. |
| Intracortical Array | Recording of single-unit and multi-unit activity. | Paradromics Connexus BCI; Utah Array [108]. |
| fNIRS System | Non-invasive measurement of hemodynamic activity. | Portable systems with sources and detectors over the motor cortex [103]. |
| Stimulus Presentation Software | Precise control of experimental paradigms and timing. | MATLAB with Psychophysics Toolbox (PTB-3) [109]. |
| Motion Tracking | Quantifying movement kinematics for decoder training. | Custom electrogoniometers, gyroscopes (e.g., Wii Motion Plus) [107]. |
| Signal Processing & Machine Learning Tools | Preprocessing, feature extraction, and model building. | EEGLAB, CSP, CCA, Deep Learning models (e.g., MSCFormer), PAC-based feature extraction (CPX pipeline) [105] [111]. |
| Performance Metric Suites | Standardized evaluation of BCI performance. | Calculation of ITR, classification accuracy, AUC, F1 score, and confidence intervals [110]. |
Experimental Workflow and Decision Pathway
The following diagrams illustrate a generalized workflow for a BCI benchmarking experiment and a logical pathway for selecting the appropriate modality based on research requirements.
BCI Benchmarking Workflow
BCI Modality Selection Logic
Brain-Computer Interface (BCI) technology represents a revolutionary frontier in medical science, enabling direct communication between the brain and external devices [112]. For researchers and developers, navigating the regulatory landscape is as crucial as the technological innovation itself. This document provides detailed application notes and experimental protocols for conducting BCI research within the frameworks of the U.S. Food and Drug Administration (FDA) and China's National Medical Products Administration (NMPA) "Green Channel" for innovative devices [113] [114]. The recent FDA 510(k) clearance of Precision Neuroscience's Layer 7-T Cortical Interface in March 2025 and the inclusion of China's first invasive BCI in the NMPA's special review program in November 2025 mark significant regulatory milestones, accelerating the transition of BCI technology from laboratory research to clinical application [115] [116].
Regulatory Pathway Comparison: FDA vs. NMPA
Table 1: Comparative Analysis of Regulatory Pathways for BCI Devices
| Regulatory Aspect | U.S. FDA Pathway | China NMPA 'Green Channel' |
|---|---|---|
| Key Programs | 510(k), De Novo, Premarket Approval (PMA), Breakthrough Device Program [117] [118] | Innovative and Priority Medical Device Review [113] |
| Typical Approval Timeline | Varies by pathway: ~6 months for 510(k) to years for PMA [115] | 100 working days (Innovative Review) vs. 170 days (Standard) [113] |
| Primary Regulatory Focus | Safety, efficacy, substantial equivalence (510(k)) or independent demonstration of safety/effectiveness (PMA) [119] [118] | Technological originality, clinical value, and absence of similar domestic products [113] |
| Risk Classification | Class III (Implantable BCIs) [117] [118] | Class II or III (focus on innovative devices) [114] |
| Clinical Data Requirements | Required for PMA; Investigational Device Exemption (IDE) for clinical trials [119] [118] | Local clinical data often required; overseas data needs suitability assessment [113] |
| Key Milestone | Precision Neuroscience's Layer 7-T received FDA 510(k) clearance on March 30, 2025 [115] | Step Medical's implantable BCI system entered special review in November 2025 [116] |
| Post-Market Surveillance | Required (e.g., adverse-event reporting) [117] | Part of the full-chain service system [113] |
Detailed Regulatory Protocols
FDA Investigational Device Exemption (IDE) Protocol
For any BCI device requiring clinical investigation in the U.S., an Investigational Device Exemption (IDE) must be secured from the FDA before commencing trials [118]. The protocol involves several critical stages and is designed to evaluate the device's safety and efficacy.
Diagram 1: FDA IDE to PMA Approval Workflow
Experimental & Submission Methodology:
Pre-IDE Non-Clinical Testing: Conduct comprehensive bench testing and animal studies under Good Laboratory Practice (GLP) conditions [115] [119]. Key experiments include:
- Electrical Safety & Biocompatibility: Perform testing per International Electrotechnical Commission (IEC) 60601 and International Organization for Standardization (ISO) 10993 standards [115].
- Mechanical Durability & Signal Fidelity: Validate impedance and signal-to-noise ratio (SNR) over the intended use period [115].
- Risk Management: Document all risk analysis and mitigation strategies per ISO 14971 [117].
IDE Application Assembly: Compile the IDE application, which must include [119] [118]:
- Complete device description, including design, components, and materials.
- Report of prior investigations and all non-clinical study data.
- Manufacturing information.
- Proposed clinical investigation protocol, including patient selection criteria, study endpoints, and monitoring procedures.
- Investigator agreements and informed consent documents.
Institutional Review Board (IRB) Review: Submit the clinical protocol for approval by an IRB. The IRB must include appropriate expertise (e.g., neurologists, neurosurgeons) to evaluate the unique risks of iBCIs, such as surgical risks, long-term psychological effects, and cybersecurity [118].
Clinical Trial Execution: Upon simultaneous approval from the FDA and the IRB, initiate clinical trials. The FDA's 2021 guidance specifically outlines study design considerations for BCI devices for patients with paralysis or amputation [119]. Trials typically proceed from early feasibility studies to larger pivotal studies.
Premarket Approval (PMA) Submission: Following successful clinical trials, submit a PMA application. This is the most comprehensive submission route for Class III devices and requires an independent demonstration of safety and effectiveness [118]. The FDA then reviews the entire body of evidence before granting market approval.
NMPA Innovative "Green Channel" Application Protocol
China's NMPA offers a special review pathway for innovative medical devices, often called the "Green Channel," which can significantly accelerate the registration process [113] [114]. The protocol emphasizes early engagement and comprehensive documentation.
Diagram 2: NMPA Green Channel Application Workflow
Experimental & Submission Methodology:
Eligibility and Pre-Assessment: The first critical step is to determine if the device meets the criteria for the "Green Channel" [113] [114]:
- Technological Originality: The core technology must be a first application in China and demonstrate significant progress over existing technology.
- Valid Chinese Patent: A patent for the primary mechanism of action must be granted by China (or be under application) and cannot be older than 5 years from the grant date. This is a key threshold requirement.
- Clinical Value: The device must be a Class II or III device with notable clinical value, such as for diagnosing/treating rare diseases, pediatric conditions, or filling an urgent clinical need with no similar domestic products.
Application Dossier Preparation: Assemble the comprehensive application dossier. Essential documents include [113] [114]:
- Intellectual Property Certificate: Proof of the valid China patent.
- Product Overview and Novelty Report: A detailed report from a novelty search justifying the innovative nature of the product.
- Supporting R&D Data: Complete laboratory research data, necessary animal test data, and a prototype study report.
- Clinical Value Statement: A comprehensive comparison with similar products already on the market in China, supported by academic papers and a risk management report.
Engagement with the Center for Medical Device Evaluation (CMDE): Upon acceptance into the innovative pathway, the CMDE will assign a dedicated reviewer who provides proactive guidance throughout the development and registration process, a mechanism known as "early intervention, dedicated personnel" [113]. This can save an average of 3-6 months in R&D time.
Priority Evaluation and Clinical Data: The application receives priority in all subsequent steps, including technical evaluation, which is reduced from 90 to 60 working days [113]. A critical requirement is the need for localized clinical data. Overseas data must undergo a suitability assessment for Chinese populations, often necessitating supplementary Chinese subgroup analysis or local clinical trials in cooperation with Chinese institutions [113].
The Scientist's Toolkit: Essential Research Reagents & Materials
Table 2: Key Research Reagent Solutions for BCI Development
| Item / Reagent | Function in BCI R&D | Example / Specification |
|---|---|---|
| Polyimide-based Electrode Arrays | Biocompatible, ultra-thin, flexible substrate for high-density cortical interfaces [115] | Precision Neuroscience's Layer 7-T array (1,024 electrodes, 50–500 µm contacts) [115] |
| EEG Head Stages & Amplifiers | Acquisition and amplification of neural signals from electrodes; compatible with standard systems (e.g., DIN-standard) for clinical integration [115] | Research-grade EEG acquisition systems (e.g., from Neuracle) for epilepsy and brain tumor mapping [112] |
| Biocompatibility Test Kits | Assessing biological safety of implant materials per ISO 10993 standards [115] [117] | Tests for cytotoxicity, sensitization, and intracutaneous reactivity |
| Signal Processing & Decoding Algorithms | AI/Software to translate raw neural signals into device commands; critical for accuracy and speed [120] [112] | Custom algorithms for real-time decoding of movement, speech, or intention [115] |
| Custom Surgical Delivery Systems | Enabling minimally invasive implantation of flexible BCI arrays [115] | Delivery system for <1 mm cranial micro-slit technique [115] |
| High-Channel Count BCI Chips | System-on-Chip (SoC) for processing neural data with high channel count and low power consumption [112] | NeuraMatrix 128-channel SoC for implants [112] |
The evaluation of Brain-Computer Interface (BCI) systems in clinical trials requires a multifaceted approach to accurately assess their impact on functional recovery and quality of life. As BCI technologies evolve from laboratory settings to clinical applications, establishing robust and standardized metrics becomes paramount for demonstrating efficacy and securing regulatory approval. These metrics must capture not only the technical performance of the device but, more importantly, its meaningful impact on a user's daily living activities and overall well-being. Within the context of a broader thesis on BCI control applications research, this document provides detailed application notes and protocols for implementing these critical assessments.
The selection of appropriate efficacy endpoints is particularly crucial in BCI trials, given the complex interplay between neural decoding accuracy, functional task performance, and patient-reported quality of life measures. Clinical trials are an essential but time-consuming and costly process in the development of new medical interventions, with an overall success rate of only 7.9% [121]. Leveraging well-defined metrics and milestones can significantly improve the quality and interpretability of trial outcomes. Furthermore, the use of common metrics allows for benchmarking across institutions and facilitates process improvements that enhance the efficiency of clinical research [122]. The following sections detail the specific metrics, methodologies, and protocols for comprehensively evaluating BCI systems in clinical trial settings.
Quantitative Metrics for Clinical Trial Assessment
A combination of performance, functional, and patient-reported outcome metrics is essential for a holistic assessment of BCI interventions. The tables below summarize the key quantitative data required for comprehensive trial evaluation.
Table 1: Key Performance Indicators (KPIs) for Clinical Trial Management
| KPI Category | Specific Metric | Definition and Measurement |
|---|---|---|
| Trial Progress | Enrollment Progress [123] | Progress of patient recruitment/retention against predefined targets. |
| Screen Failure Rates [123] | Percentage of screened participants who do not qualify for the trial. | |
| Trial Timeline Adherence [123] | Trial progression against its initial schedule, identifying delays. | |
| Data Quality | Data Entry Timeliness [123] | Time from patient enrollment to first data entry into the CTMS. |
| Data Query Rates [123] | Number of queries generated for data clarification. | |
| Protocol Deviations/Violations [123] | Identified deviations from the protocol impacting study integrity. | |
| Participant Safety & Engagement | Dropout Rates [123] | Number of participants who leave the trial before completion. |
| Adverse Events (AEs) [123] | Frequency and severity of AEs and Serious Adverse Events (SAEs). | |
| Patient Visit Adherence [123] | Percentage of completed patient visits compared to those scheduled. |
Table 2: BCI-Specific Efficacy and Functional Outcome Metrics
| Metric Domain | Assessment Tool | Application in BCI Trials |
|---|---|---|
| Technical Performance | Neural Signal Classification Accuracy [124] [125] | Accuracy of decoding intended motor commands or stimuli. |
| Information Transfer Rate (ITR) [125] | Speed of communication, measured in bits per minute. | |
| System Responsiveness (Latency) | Time delay between brain signal initiation and device response. | |
| Functional Recovery | Graded Redefined Assessment of Strength, Sensibility, and Prehension (GRASSP) | For upper limb function in spinal cord injury. |
| Fugl-Meyer Assessment (FMA) | For motor recovery, coordination, and balance in stroke. | |
| Functional Independence Measure (FIM) | Assesses independence in self-care, sphincter control, and mobility. | |
| Quality of Life (QoL) | SF-36 or EQ-5D [123] | Standardized generic health-related QoL questionnaires. |
| Quebec User Evaluation of Satisfaction with assistive Technology (QUEST) | Measures user satisfaction with assistive devices. | |
| Patient-Specific Functional Scale (PSFS) | Identifies and scores difficulty in performing specific activities. |
Experimental Protocols for Key Assessments
Protocol for Assessing BCI-Controlled Functional Tasks
Objective: To quantitatively evaluate the user's ability to perform activities of daily living (ADLs) using a BCI-controlled neuroprosthetic or assistive device.
Materials:
- BCI system (e.g., EEG, fNIRS, or invasive system [125]).
- BCI-controlled output device (e.g., robotic arm, computer cursor, functional electrical stimulation system).
- Standardized object set for ADL tasks (e.g., cups, blocks, utensils).
- Video recording system for subsequent scoring.
Methodology:
- Task Setup: Place standardized objects on a table in front of the participant. For a reaching and grasping task, position a light object (e.g., a plastic cup) at a reachable distance.
- System Calibration: Conduct a brief system calibration where the user is guided to perform the motor imagery or evoked potential task that controls the device.
- Task Execution: Instruct the participant to use the BCI system to command the device to reach, grasp, and lift the object. The command must be generated solely via the BCI.
- Data Collection: For each trial, record:
- Task completion time (from "go" cue to successful lift).
- Success rate (binary: successful grasp and lift vs. failure).
- Kinematic data (if available, e.g., trajectory smoothness of the robotic arm).
- Number of failed BCI commands before success.
- Scoring: Score performance using a standardized functional scale like the Jebsen-Taylor Hand Function Test, adapted for BCI control. Repeat trials a minimum of 5 times to establish consistency.
Protocol for Quality of Life and Patient-Reported Outcome Measures
Objective: To capture the patient's perception of their functional improvement, quality of life, and satisfaction with the BCI technology.
Materials:
- Validated questionnaires: SF-36, QUEST, and PSFS.
- Quiet, private room for interview or self-administration.
- Trained clinical researcher to administer the questionnaires.
Methodology:
- Baseline Assessment: Administer the QoL and PRO questionnaires before the BCI intervention begins.
- Training Period: Conduct the BCI intervention and training over the prescribed trial period (e.g., 12 weeks).
- Post-Intervention Assessment: Re-administer the same questionnaires immediately after the training period concludes and during follow-up visits (e.g., at 3 and 6 months).
- Administration:
- SF-36/EQ-5D: Allow the participant to complete the questionnaire independently. Provide clarification if requested without leading.
- QUEST: Interview the participant. Ask them to rate their satisfaction with various aspects of the BCI device (e.g., comfort, effectiveness, ease of use) on the provided scale.
- PSFS: In the baseline assessment, help the participant identify 3-5 important activities they are unable to do or have difficulty with because of their condition. At each follow-up, ask them to score their ability to perform each of those specific activities.
- Data Analysis: Calculate summary scores for SF-36/EQ-5D and QUEST. For PSFS, calculate the mean score of the listed activities. Use paired statistical tests (e.g., paired t-test) to compare baseline scores to post-intervention scores.
Visualization of Clinical Trial Workflows
BCI Clinical Trial Efficacy Pathway
Efficacy Metric Integration Logic
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Materials for BCI Clinical Trial Research
| Item / Solution | Function in BCI Research | Example Application |
|---|---|---|
| EEG Systems with Active Electrodes | Non-invasive recording of electrical brain activity with high temporal resolution [125]. | Decoding motor imagery commands for device control [125]. |
| fNIRS Systems | Non-invasive measurement of hemodynamic responses; more robust to motion artifacts than EEG [125]. | Monitoring cortical activation in motor and cognitive tasks for BCI. |
| Hybrid EEG-fNIRS Systems | Combines high temporal resolution (EEG) with improved spatial specificity (fNIRS) to enhance classification accuracy [125]. | Improving the reliability of motor imagery classification in real-world settings. |
| Wearable Microneedle Sensors | Minimally invasive sensors that penetrate the skin slightly, offering higher signal quality than surface electrodes by reducing noise [124]. | Enabling stable, long-term brain signal detection for practical, continuous BCI use [124]. |
| BCI2000 or OpenViBE Platforms | Standardized software platforms for BCI prototyping, data acquisition, and signal processing. | Providing a common framework for implementing and validating BCI paradigms. |
| Validated PRO & QoL Questionnaires | Quantifying the patient's perspective on their health status and the intervention's impact [123]. | Measuring changes in quality of life and functional independence (e.g., SF-36, QUEST). |
| Standardized Functional Assessment Kits | Objective evaluation of motor and cognitive function using standardized tasks and objects. | Administering functional scales like FMA or GRASSP to assess recovery. |
Conclusion
Brain-Computer Interface technology stands at a pivotal juncture in 2025, demonstrating unprecedented progress from laboratory research to tangible clinical applications. The synthesis of insights across foundational principles, methodological applications, optimization challenges, and validation frameworks reveals a field rapidly maturing towards practical, life-changing tools for patients with neurological disorders and injuries. For biomedical and clinical research, the future direction is clear: the integration of artificial intelligence and virtual reality will further enhance system intelligence and user experience, while robust, user-centered evaluation frameworks are crucial for successful clinical translation. The ongoing convergence of improved biocompatibility in invasive devices, sophisticated signal processing, and supportive regulatory policies promises not only to restore lost functions but also to open new frontiers in understanding and interfacing with the human brain, ultimately strengthening the bridge between neuroscience and clinical therapeutics.
References
- 1. Brain–computer interface [https://en.wikipedia.org/wiki/Brain%E2%80%93computer_interface]
- 2. BCIs in 2025: Trials, Progress, and Challenges [https://andersenlab.com/blueprint/bci-challenges-and-opportunities]
- 3. Advancing Brain-Computer Interface Closed-Loop Systems for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12588595/]
- 4. Brain-computer interfaces are closer than you think [https://www.clinicaltrialsarena.com/analyst-comment/brain-computer-interfaces-closer/]
- 5. BETA: A Large Benchmark Database Toward SSVEP-BCI ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7324867/]
- 6. Research Participation [https://bcisociety.org/research-participation/]
- 7. Community perspectives regarding brain-computer interfaces [https://pmc.ncbi.nlm.nih.gov/articles/PMC11798465/]
- 8. Brain–computer interfaces: the innovative key to unlocking ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11392146/]
- 9. Modulating Brain Activity with Invasive Brain–Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9856340/]
- 10. A Cross-Disciplinary Review of the fNIRS-EEG Dual- ... [https://www.mdpi.com/2076-3425/14/10/1022]
- 11. How does invasive vs non-invasive BCI compare? [https://synapse.patsnap.com/article/how-does-invasive-vs-non-invasive-bci-compare]
- 12. Neuroimaging-based approaches in the brain–computer ... [https://www.sciencedirect.com/science/article/abs/pii/S0167779910001381]
- 13. EEG-based brain-computer interface enables real-time ... [https://www.nature.com/articles/s41467-025-61064-x]
- 14. Recent applications of EEG-based brain-computer-interface in ... [https://mmrjournal.biomedcentral.com/articles/10.1186/s40779-025-00598-z]
- 15. Advancing Brain-Computer Interface Closed-Loop Systems for ... [https://biomedeng.jmir.org/2025/1/e72218]
- 16. Top 10 Brain-Computer Interface Companies in 2025 [https://www.sphericalinsights.com/blogs/top-10-companies-leading-the-brain-computer-interface-market-in-2025-key-players-statistics-future-trends-2024-2035]
- 17. A comprehensive review of EEG-Based BCI paradigms ... [https://pubmed.ncbi.nlm.nih.gov/40829351/]
- 18. The top BCI stories of 2025 so far [https://www.massdevice.com/top-bci-stories-2025-so-far/]
- 19. Effects of Different Preprocessing Pipelines on Motor ... [https://pubmed.ncbi.nlm.nih.gov/40031268/]
- 20. Enhanced EEG signal classification in brain computer ... [https://www.nature.com/articles/s41598-025-07427-2]
- 21. Study of promising speech-enabling interface offers hope for ... [https://med.stanford.edu/news/all-news/2025/08/brain-computer-interface.html]
- 22. Seeks ‘Telepathy’ And ‘Telekinesis’—Is Mind Control Next? Neuralink [https://www.forbes.com/sites/luisromero/2025/03/08/neuralink-seeks-telepathy-and-telekinesis-is-mind-control-next/]
- 23. Synchron | The brain-computer interface device powering ... [https://synchron.com/]
- 24. Synchron BCI Home [https://synchronbci.com/]
- 25. Our Tech [https://blackrockneurotech.com/our-tech/]
- 26. Blackrock Neurotech | Empowered by Thought [https://blackrockneurotech.com/]
- 27. Paradromics Receives FDA Approval for the Connect-One ... [https://www.paradromics.com/news/paradromics-receives-fda-approval-for-the-connect-one-clinical-study-with-the-connexus-brain-computer-interface]
- 28. Austin startup plans clinical trial after human brain ... [https://ny1.com/nyc/bronx/news/2025/09/02/paradromics-brain-bci-human-implant]
- 29. Paradromics Adds Third Site for the Connexus® Brain ... [https://www.paradromics.com/news/paradromics-adds-third-site-for-the-connexus-r-brain-computer-interface-clinical-study-at-the-university-of-michigan]
- 30. The Global Brain-Computer Interfaces Market 2025-2035 [https://www.researchandmarkets.com/report/brain-computer-interface?srsltid=AfmBOoqhYz3l51JtmvyEb1yehtO_2xh83HIChAA0mV9fdbrDoEaxHi-d]
- 31. Global Brain-Computer Interfaces Markets 2025-2035 with ... [https://finance.yahoo.com/news/global-brain-computer-interfaces-markets-080600907.html]
- 32. Brain Computer Interface Market Grows at 16.7% CAGR ... [https://www.towardshealthcare.com/insights/brain-computer-interface-market]
- 33. The Brain-Computer Interface Market: Projected Growth to ... [https://www.jdpglobal.com/the-brain-computer-interface-market-projected-growth-to-hit-8-73-billion-by-2033/]
- 34. BCI Market Scale to Reach Tens of Trillions [http://www.ks-chip.com/men/news/show-907.html]
- 35. Enhancing P300 Wave of BCI Systems Via Negentropy in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3347228/]
- 36. Denoising of EEG signals using Discrete Wavelet ... [https://biomedpharmajournal.org/vol8no1/denoising-of-eeg-signals-using-discrete-wavelet-transform-based-scalar-quantization/]
- 37. Denoising method for EEG-based expert system in ... [https://www.sciencedirect.com/science/article/abs/pii/S0957417425021451]
- 38. Canonical Correlation Analysis of Task Related ... [https://www.sciencedirect.com/science/article/abs/pii/S1746809421010466]
- 39. Robust artifactual independent component classification for ... [https://pubmed.ncbi.nlm.nih.gov/24836294/]
- 40. Multi-information improves the performance of CCA-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10881948/]
- 41. A novel hybrid method based on task-related component ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2025.1544452/full]
- 42. AI reshaping life sciences: intelligent transformation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500557/]
- 43. Hierarchical attention enhanced deep learning achieves ... [https://www.nature.com/articles/s41598-025-17922-1]
- 44. Decoding inner speech from brain signals [https://www.nih.gov/news-events/nih-research-matters/decoding-inner-speech-brain-signals]
- 45. AI co-pilot boosts noninvasive brain-computer interface by ... [https://newsroom.ucla.edu/releases/ai-brain-computer-interface-interprets-user-intent-ucla]
- 46. Boosting brain–computer interfaces with functional electrical stimulation... [https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-023-01272-y]
- 47. Stable long-term BCI -enabled communication in ALS and locked - in ... [https://pubmed.ncbi.nlm.nih.gov/29694279/]
- 48. Designing Guiding Systems for Brain-Computer Interfaces [https://pmc.ncbi.nlm.nih.gov/articles/PMC5535189/]
- 49. Summary of over Fifty Years with Brain-Computer Interfaces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7824107/]
- 50. BCI Toolbox: An open-source python package for the ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1011791]
- 51. Brain-Computer Interfaces for Stroke Motor Rehabilitation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12383906/]
- 52. Brain Computer Interface (BCI) Research Report 2025-2035: [https://www.globenewswire.com/news-release/2025/10/01/3159276/0/en/Brain-Computer-Interface-BCI-Research-Report-2025-2035-EEG-MEG-and-fMRI-Integration-Enhances-Neural-Signal-Detection-and-Drives-Global-Growth.html]
- 53. Brain–Computer Interface-Controlled Exoskeletons in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9720703/]
- 54. BCI-Based Control for Ankle Exoskeleton T-FLEX [https://www.mdpi.com/1424-8220/21/19/6431]
- 55. NICE's New Push for Case Management in ... [https://medium.com/@dralysonnorman/nices-new-push-for-case-management-in-neurorehabilitation-and-how-lived-experience-research-08960b4adba7]
- 56. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/en/research-report/brain-computer-interfaces/1024]
- 57. Application and future directions of brain-computer ... [https://www.sciencedirect.com/science/article/pii/S2589238X2500083X]
- 58. A brain-computer interface roadmap for diagnosing and ... [https://www.the-innovation.org/article/doi/10.59717/j.xinn-inform.2025.100016]
- 59. Flexible brain electronic sensors advance wearable ... [https://www.nature.com/articles/s44385-025-00029-7]
- 60. Recent applications of EEG-based brain-computer-interface in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11931852/]
- 61. Portable Brain Computer Interface Sleep Monitor ... [https://www.medrxiv.org/content/10.1101/2025.10.31.25339277v1.full-text]
- 62. Accurate depth of anesthesia monitoring based on EEG signal ... [https://braininformatics.springeropen.com/articles/10.1186/s40708-024-00241-y]
- 63. China Moves Ahead with Research into Brain-computer ... [https://english.cas.cn/newsroom/cas_media/202508/t20250825_1051356.shtml]
- 64. Methods for motion artifact reduction in online brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10619676/]
- 65. Artifact filtering application to increase online parity in a ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11914135/]
- 66. Artifact Reduction Techniques in EEG-Based BCI [https://www.linkedin.com/pulse/artifact-reduction-techniques-eeg-based-bci-ravichander-janapati-tpm2c]
- 67. Formulation of the Challenges in Brain-Computer Interfaces ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7859253/]
- 68. Brain Computer Interfaces 2025-2045: Technologies, ... [https://www.idtechex.com/tw/research-report/brain-computer-interfaces/1024]
- 69. Optimizing Brain-Computer Interface Performance [https://arxiv.org/html/2405.00721v1]
- 70. Study of an Optimization Tool Avoided Bias for Brain ... [https://www.sciencedirect.com/science/article/pii/S1959031824000174]
- 71. Advances in user-training for mental-imagery-based BCI ... [https://www.sciencedirect.com/science/article/abs/pii/S0079612316300061]
- 72. a confirmatory study on VR priming in motor imagery brain ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2025.1681538/full]
- 73. Continuous Reaching and Grasping With a BCI Controlled ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12548837/]
- 74. AdaBrain-Bench: Benchmarking Brain Foundation Models ... [https://arxiv.org/html/2507.09882v2]
- 75. Revolutionizing brain‒computer interfaces: overcoming ... [https://jnanobiotechnology.biomedcentral.com/articles/10.1186/s12951-025-03573-x]
- 76. Long-term stability strategies of deep brain flexible neural ... [https://www.nature.com/articles/s41528-025-00410-x]
- 77. Stability of a chronic implanted brain-computer interface in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6880281/]
- 78. Comprehensive evaluation methods for translating BCI into ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2024.1429130/full]
- 79. A high-performance brain–computer interface for finger ... [https://www.nature.com/articles/s41591-024-03341-8]
- 80. What is BCI? | Calgary Pediatric Brain-Computer Interface ... [https://cumming.ucalgary.ca/research/pediatric-bci/bci-program/what-bci]
- 81. A graphic showing the flow of data between the ... [https://uwm.edu/r2d2/projects/bci-fes/bcifes-sys/]
- 82. A Review of Brain-Computer Interface Technologies [https://arxiv.org/html/2503.16471v1]
- 83. Performance assessment in brain-computer interface-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3662584/]
- 84. Brain-Computer Interfaces in Medicine - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC3497935/]
- 85. Formulation of the Challenges in Brain-Computer ... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2020.546656/full]
- 86. Brain-Computer Interface Optimization Using Deep Learning [https://www.linkedin.com/pulse/brain-computer-interface-optimization-using-deep-abhishek-tripathi-ct4zc]
- 87. A Systematic User-Centered Training Protocol to Optimize ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0076214]
- 88. Brain-Computer Interface Clinical Trials [https://www.hopkinsmedicine.org/neurology-neurosurgery/clinical-trials/brain-computer-interface]
- 89. Evolving optimized transformer-hybrid systems for robust ... [https://www.sciencedirect.com/science/article/pii/S1746809425003945]
- 90. Brain-Computer Interfaces: Applications, Challenges, and ... [https://www.gao.gov/products/gao-25-106952]
- 91. Evaluating the real-world usability of BCI control systems with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11330773/]
- 92. Evaluating the real-world usability of BCI control systems ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2024.1448584/full]
- 93. Brain-computer interface study wins 2025 Top Ten Clinical ... [https://health.ucdavis.edu/news/headlines/brain-computer-interface-study-wins-2025-top-ten-clinical-research-achievement-award-/2025/02]
- 94. 3.4 Comparison of invasive and non-invasive techniques [https://fiveable.me/brain-computer-interfaces/unit-3/comparison-invasive-non-invasive-techniques/study-guide/zessvADvpYjeDIN7]
- 95. Non-Invasive Brain-Computer Interfaces: State of the Art and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11861396/]
- 96. Comparative accuracy of invasive versus non- ... [https://eureka.patsnap.com/report-comparative-accuracy-of-invasive-versus-non-invasive-brain-computer-interfaces-approaches]
- 97. Non-Invasive Brain–Computer Interfaces [https://www.emergentmind.com/topics/non-invasive-brain-computer-interfaces-bcis]
- 98. Brain Computer Interfaces in Medicine Analysis 2025 and ... [https://www.archivemarketresearch.com/reports/brain-computer-interfaces-in-medicine-53849]
- 99. Brain-Computer Interfaces: Exploring the Last Frontier [https://www.byfounders.vc/insights/brain-computer-interfaces]
- 100. A Comprehensive Survey of Brain–Computer Interface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12180781/]
- 101. Brain Computer Interface Market Poised for Explosive [https://www.globenewswire.com/news-release/2025/11/20/3192028/0/en/Brain-Computer-Interface-Market-Poised-for-Explosive-Growth-Projected-to-Hit-USD-6-16-Billion-by-2032-Coherent-Market-Insights.html]
- 102. Mind and machine: The state of neurotech in 2025 [https://www.insights.onegiantleap.com/blogs/mind-and-machine-the-state-of-neurotech-in-2025/]
- 103. Exploring Imagined Movement for Brain–Computer Interface ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12468679/]
- 104. Outlook for Noninvasive Brain-Computer Interfaces for AI [https://etcjournal.com/2025/09/21/outlook-for-noninvasive-brain-computer-interfaces-for-ai/]
- 105. Enhancing Performance and Bit Rates in a Brain– ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2018.00019/full]
- 106. A Bibliometric Analysis of the Application of Brain-Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11890000/]
- 107. Comparison of decoding resolution of standard and high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6508958/]
- 108. Think Fast | Setting new standards and new records for ... [https://www.paradromics.com/blog/bci-benchmarking]
- 109. A Benchmark Dataset for RSVP-Based Brain–Computer ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7566171/]
- 110. Performance Measurement for Brain-Computer or ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4185283/]
- 111. Improving brain-computer interface performance with ... [https://www.sciencedirect.com/science/article/abs/pii/S1350453325001110]
- 112. China's Brain-Computer Interface Industry: Investing in the ... [https://www.china-briefing.com/news/chinas-brain-computer-interface-industry-tapping-into-the-future-of-human-machine-integration/]
- 113. CMDE Issues New Device Review Rules [https://cisema.com/en/innovative-medical-device-pathway-2025/]
- 114. China's Green Pathway Registration for Innovative Medical ... [https://asiaactual.com/blog/chinas-green-pathway-registration-for-innovative-medical-devices/]
- 115. FDA Approves Layer 7-T BCI | Precision Neuroscience [https://bla-regulatory.com/fda-approves-layer-7t-bci/]
- 116. Hong Kong Stock Concept Tracking | China's First Brain- ... [https://www.itiger.com/news/1193726476]
- 117. Regulatory Pathways for Neural-Interface Devices - MediGear [https://medigear.uk/blog/what-are-the-regulatory-pathways-for-neural-interface-devices]
- 118. Mind the gap: bridging ethical considerations and regulatory ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325254/]
- 119. Implanted Brain-Computer Interface (BCI) Devices for ... [https://www.fda.gov/regulatory-information/search-fda-guidance-documents/implanted-brain-computer-interface-bci-devices-patients-paralysis-or-amputation-non-clinical-testing]
- 120. The Past, Present And Future Of Brain-Computer Interfaces [https://www.forbes.com/sites/robtoews/2025/10/05/these-are-the-startups-merging-your-brain-with-ai/]
- 121. Factors Affecting Success of New Drug Clinical Trials - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10173933/]
- 122. Common Metrics to Assess the Efficiency of Clinical Research [https://pmc.ncbi.nlm.nih.gov/articles/PMC4019992/]
- 123. Unlocking Clinical Trial Success: Essential KPIs to Monitor ... [https://www.cloudbyz.com/resources/clinical-operations/unlocking-clinical-trial-success-essential-kpis-to-monitor-in-a-clinical-trial-management-system-ctms/]
- 124. New Wearable Brain-Computer Interface | Research [https://research.gatech.edu/new-wearable-brain-computer-interface]
- 125. An fNIRS and EEG Review [https://pubmed.ncbi.nlm.nih.gov/41008372/]