Brain Imaging Data Analysis Workflows: A Comprehensive Guide from Foundations to AI
This article provides a comprehensive guide to modern brain imaging data analysis workflows, tailored for researchers, scientists, and drug development professionals.
Brain Imaging Data Analysis Workflows: A Comprehensive Guide from Foundations to AI
Abstract
This article provides a comprehensive guide to modern brain imaging data analysis workflows, tailored for researchers, scientists, and drug development professionals. It covers the foundational principles of data organization and standardization, explores both established and emerging AI-driven methodological approaches, addresses critical troubleshooting and optimization challenges in large-scale analysis, and outlines best practices for validation and reproducibility. By synthesizing current tools, standards, and computational strategies, this resource aims to equip practitioners with the knowledge to build robust, efficient, and clinically translatable neuroimaging pipelines.
Laying the Groundwork: Core Concepts and Data Standards in Neuroimaging
Neuroimaging experiments generate complex data that can be arranged in numerous ways. Historically, the absence of a consensus on how to organize and share this data has led to significant inefficiencies in neuroscience research. Even researchers within the same laboratory often opted to arrange their data differently, leading to misunderstandings and substantial time wasted on rearranging data or rewriting scripts to accommodate varying structures [1] [2]. This lack of standardization constitutes a major vulnerability in the effort to create reproducible, automated workflows for neuroimaging data analysis [3]. The Brain Imaging Data Structure (BIDS) was developed to address this critical need, providing a simple, easy-to-adopt standard for organizing neuroimaging and associated behavioral data [1]. By formalizing file and directory structures and specifying metadata files using controlled vocabulary, BIDS enables researchers to overcome the challenges of data heterogeneity and ensure the reliability of their analytical workflows [4].
BIDS Fundamentals: Core Principles and Structure
Organizational Philosophy and Design
BIDS is a community-driven standard that describes a formalized system for organizing, annotating, and describing data collected during neuroimaging experiments [4]. Its design is intentionally based on simple file formats and folder structures to reflect current laboratory practices, making it accessible to scientists from diverse backgrounds [1]. The core organizational principles of BIDS can be summarized as follows: using NIFTI files as the primary imaging format, accompanying key data with JSON sidecar files that provide parameters and descriptions, and employing a consistent folder structure and file naming convention as prescribed by the specification [5]. This structure is platform-independent and designed to be both intuitive and comprehensive, covering most common experimental designs while remaining adaptable to new modalities through a well-defined extension process [1] [2].
Directory and File Structure
The BIDS directory structure follows a consistent hierarchical pattern that organizes data by subjects, optional sessions, and data modalities. The general hierarchy is as follows: sub-<participant_label>[/ses-<session_label>]/<data_type>/ [5]. Key directories include anat for anatomical data, func for functional data, dwi for diffusion-weighted imaging, fmap for field maps, and beh for behavioral data. Additional directories such as code/, derivatives/, stimuli/, and sourcedata/ may be included for specialized purposes [5].
Table 1: Core BIDS Directory Structure
| Directory | Content Description | Example Files |
|---|---|---|
sub-<label> |
Participant-specific data | All data for a single participant |
ses-<label> |
Session-specific data (optional) | Data for different time points |
anat/ |
Anatomical imaging data | sub-01_T1w.nii.gz, sub-01_T1w.json |
func/ |
Functional MRI data | sub-01_task-nback_bold.nii.gz, sub-01_task-nback_events.tsv |
dwi/ |
Diffusion-weighted imaging | sub-01_dwi.nii.gz, sub-01_dwi.bval, sub-01_dwi.bvec |
fmap/ |
Field mapping data | sub-01_phasediff.nii.gz, sub-01_phasediff.json |
beh/ |
Behavioral data | Task performance data, responses |
File naming in BIDS follows a strict convention based on key-value pairs (entities) that establish a common order within a filename [5]. For instance, a filename like sub-01_ses-pre_task-nback_bold.nii.gz immediately conveys that this is the functional MRI data for subject 01 during a pre-intervention session performing an n-back task. This systematic approach ensures that both humans and software tools can readily parse the content and context of each file without additional documentation.
The BIDS Ecosystem: Tools and Applications
The BIDS specification is supported by a rich ecosystem of software tools and resources that enhance its utility and adoption. This ecosystem includes the core specification with detailed implementation guidelines, the starter kit with simplified explanations for new users, the BIDS Validator for automatically checking dataset integrity, and BIDS Apps—a collection of portable pipelines that understand BIDS datasets [1]. A growing number of data analysis software packages can natively understand data organized according to BIDS, and databases such as OpenNeuro.org, LORIS, COINS, XNAT, and SciTran accept and export datasets organized according to the standard [1] [2].
BIDS Validator and Quality Assurance
The BIDS Validator is a critical tool that checks dataset integrity and helps users easily identify missing values or specification violations [1] [2]. This tool is available both as a command-line application and through a web interface, allowing researchers to validate their data organization before analysis or sharing. The validator checks all aspects of a BIDS dataset, including file structure, required files, metadata completeness, and consistency across participants and sessions. For large-scale datasets, tools like CuBIDS (Curation of BIDS) provide robust, scalable implementations of BIDS validation that can be applied to arbitrarily-sized datasets [3].
BIDS Apps and Processing Pipelines
BIDS Apps are containerized data processing pipelines that understand BIDS-formatted datasets [3]. These portable pipelines—such as fMRIPrep for functional MRI preprocessing and QSIPrep for diffusion-weighted imaging data—flexibly build workflows based on the metadata encountered in a dataset [3]. This approach enables reproducible analyses across different computing environments and facilitates the application of standardized preprocessing methods across studies. However, this workflow construction structure can also represent a vulnerability: if the BIDS metadata is inaccurate, a BIDS App may build an inappropriate (but technically "correct") preprocessing pipeline [3]. For example, a fieldmap with no IntendedFor field specified in its JSON sidecar will cause pipelines to skip distortion correction without generating errors or warnings [3].
Table 2: Essential BIDS Tools and Resources
| Tool/Resource | Type | Function/Purpose |
|---|---|---|
| BIDS Validator | Validation Tool | Checks dataset integrity and compliance with BIDS specification |
| BIDS Starter Kit | Educational Resource | Simple explanation of how to work with BIDS |
| BIDS Apps | Processing Pipelines | Portable pipelines (fMRIPrep, QSIPrep) that understand BIDS data |
| CuBIDS | Curation Tool | Helps users validate and manage curation of large neuroimaging datasets |
| OpenNeuro | Data Repository | Public database for BIDS-formatted datasets |
| PyBIDS | Python Library | Python library for querying and manipulating BIDS datasets |
BIDS Extension Proposals: Expanding the Standard
The BIDS specification is designed to evolve over time through a backwards-compatible extension process. This is accomplished through community-driven BIDS Extension Proposals (BEPs), which allow the standard to incorporate new imaging modalities and data types [2] [4]. Since its initial focus on MRI, BIDS has been extended to numerous other modalities through this process, including MEG, EEG, intracranial EEG (iEEG), positron emission tomography (PET), microscopy, quantitative MRI (qMRI), arterial spin labeling (ASL), near-infrared spectroscopy (NIRS), and motion data [2] [4] [6].
The Motion-BIDS extension exemplifies this adaptive process, addressing the need to organize motion data recorded alongside human brain imaging and electrophysiological data [6]. Motion data is increasingly important in human behavioral research, with biomechanical features providing insights into underlying cognitive processes and possessing diagnostic value [6]. For instance, step length is related to Parkinson's disease severity, and cognitive impairment in older adults is associated with gait slowing [6]. Motion-BIDS standardizes the organization of this diverse data type, promoting findable, accessible, interoperable, and reusable (FAIR) data sharing and Open Science in human motion research [6].
Experimental Protocols and Implementation
Dataset Curation Protocol Using CuBIDS
For researchers working with large-scale, heterogeneous neuroimaging datasets, the CuBIDS (Curation of BIDS) package provides an intuitive workflow that helps users validate and manage the curation of their datasets [3]. CuBIDS includes a robust implementation of BIDS validation that scales to large samples and incorporates DataLad—a version control software package for data—as an optional dependency to ensure reproducibility and provenance tracking throughout the entire curation process [3]. The CuBIDS workflow involves several key steps:
- Initial Validation: Run
cubids-validateon the BIDS dataset to identify compliance issues. - Metadata Enhancement: Use
cubids-add-nifti-infoto extract and add crucial information from NIfTI headers to the corresponding JSON sidecars. - Acquisition Grouping: Execute
cubids-groupto identify unique combinations of imaging parameters in the dataset. - Targeted Curation: Use the grouping information to identify and correct metadata inconsistencies across participants.
- Provenance Tracking: Optionally use the
--use-dataladflag to implement reproducible version control throughout curation.
This protocol is particularly valuable for large, multi-site studies where hidden variability in metadata is difficult to detect and classify manually [3]. CuBIDS provides tools to help users perform quality control on their images' metadata and execute BIDS Apps on a subset of participants that represent the full range of acquisition parameters present in the complete dataset, dramatically accelerating pipeline testing [3].
BIDS Conversion Protocol
Converting raw neuroimaging data to BIDS format follows a standardized protocol:
- DICOM to NIfTI Conversion: Use tools like dcm2niix to convert raw DICOM files to NIfTI format.
- File Organization: Arrange NIfTI files according to BIDS directory structure (sub-
- Sidecar Creation: Generate JSON sidecar files containing relevant metadata for each imaging file.
- Tabular Data Preparation: Create participants.tsv, sessions.tsv (if multi-session), and other required tabular files.
- Dataset Description: Create dataset_description.json with mandatory fields (Name, BIDSVersion, DatasetType).
- Validation: Run the BIDS Validator to identify and correct any compliance issues.
This protocol ensures that data is organized consistently, facilitating subsequent analysis and sharing.
Research Reagent Solutions: Essential Tools for BIDS Workflows
Table 3: Essential Research Reagents and Tools for BIDS Experiments
| Tool/Reagent | Function/Purpose | Implementation Example |
|---|---|---|
| dcm2niix | DICOM to NIfTI Converter | Converts raw scanner DICOM files to BIDS-compliant NIfTI format |
| BIDS Validator | Dataset Compliance Checker | Validates BIDS dataset integrity before analysis or sharing |
| CuBIDS | Large Dataset Curation | Manages metadata curation for large, heterogeneous datasets |
| BIDS Apps | Containerized Processing Pipelines | Executes reproducible analyses (fMRIPrep, QSIPrep) on BIDS data |
| PyBIDS | Python API for BIDS | Queries and manipulates BIDS datasets programmatically |
| JSON Sidecars | Metadata Storage | Contains key parameters and descriptions for associated imaging data |
| DataLad | Version Control System | Tracks changes and ensures reproducibility throughout curation |
Benefits and Impact of BIDS Adoption
The adoption of BIDS provides significant benefits both for the broader scientific community and for individual researchers. For the public good, BIDS lowers scientific waste, provides opportunities for less-funded researchers, improves efficiency, and spurs innovation [1]. For individual researchers, BIDS enables and simplifies collaboration, as reviewers and funding agencies increasingly value reproducible results [1]. Furthermore, researchers who use BIDS position themselves to take advantage of open-science based funding opportunities and awards [1].
From a practical perspective, BIDS benefits researchers in several concrete ways: it becomes easier for collaborators to work with your data, as they only need to be referred to the BIDS specification to understand the organization; a growing number of data analysis software packages natively understand BIDS-formatted data; and public databases will accept datasets organized according to BIDS, speeding up the curation process if you plan to share your data publicly [1] [2]. Perhaps most importantly, using BIDS ensures that you—as the likely future user of the data and analysis pipelines you develop—will be able to understand and efficiently reuse your own data long after the original collection [1].
The Brain Imaging Data Structure addresses a critical need in modern neuroscience by providing a standardized framework for organizing, describing, and sharing neuroimaging data. By adopting simple file formats and directory structures that reflect current laboratory practices, BIDS has created an accessible yet powerful standard that promotes reproducibility, facilitates collaboration, and enhances the efficiency of neuroimaging research. The growing ecosystem of BIDS-compliant tools and databases, coupled with the community-driven extension process, ensures that the standard will continue to evolve to meet emerging needs in neuroscience and related fields. For researchers, scientists, and drug development professionals working with brain imaging data, adopting BIDS represents a fundamental step toward ensuring the reliability, reproducibility, and shareability of their research outputs.
The complexity of the brain necessitates the use of diverse, non-invasive neuroimaging technologies to capture its structural architecture, functional dynamics, and intricate connectivity. No single modality can fully elucidate the brain's workings; instead, a multimodal approach that integrates complementary data is paramount for a holistic understanding [7]. Structural MRI (sMRI) provides a high-resolution anatomical blueprint, while functional MRI (fMRI) maps cognitive processes through hemodynamic changes. Diffusion-weighted imaging (DWI) traces the white matter pathways that connect distant brain regions. In contrast, Electroencephalography (EEG) and Magnetoencephalography (MEG) offer a direct, millisecond-resolution view of neural electrical activity. This Application Note details the essential technical specifications, experimental protocols, and integrated applications of these core modalities, framing them within advanced brain imaging data analysis workflows critical for both basic research and drug development.
Modality Specifications and Comparative Analysis
Table 1: Technical Specifications and Primary Applications of Core Neuroimaging Modalities
| Modality | Spatial Resolution | Temporal Resolution | What It Measures | Primary Applications | Key Advantages | Principal Limitations |
|---|---|---|---|---|---|---|
| sMRI | Sub-millimeter | Minutes | Brain anatomy (grey/white matter volume, cortical thickness) | Anatomical reference, morphometry, tracking neurodegeneration | High spatial detail, excellent soft-tissue contrast | No direct functional information, slow acquisition |
| fMRI | 1-3 mm | 1-2 seconds | Blood-oxygen-level-dependent (BOLD) signal (indirect correlate of neural activity) | Functional connectivity, localization of cognitive tasks, network dynamics | Widespread availability, good spatial resolution for whole-brain coverage | Indirect and slow measure of neural activity, sensitive to motion |
| DWI | 2-3 mm | Minutes | Directionality of water molecule diffusion (white matter tract integrity) | Structural connectivity, tractography, assessing white matter integrity | Unique insight into structural brain networks | Inferior spatial resolution vs. sMRI, complex modeling |
| EEG | >10 mm (poor) | <1 millisecond | Electrical potential on scalp from synchronized postsynaptic currents | Brain dynamics, neural oscillations, event-related potentials, clinical monitoring | Excellent temporal resolution, portable, low cost | Poor spatial resolution, sensitive to non-neural artifacts |
| MEG | 3-5 mm (good with modeling) | <1 millisecond | Magnetic field on scalp from synchronized postsynaptic currents | Source localization of neural activity, brain dynamics, connectivity | Excellent temporal and good spatial resolution for source modeling | Extremely expensive, non-portable, insensitive to radial sources |
Table 2: Quantitative Performance in Benchmarking Studies
| Study Context | Modality/Comparison | Key Quantitative Finding | Implication for Workflow Design |
|---|---|---|---|
| Source Localization Accuracy [8] [9] | MEG alone | Higher accuracy for superficial, tangential sources | Optimal for sulcal activity |
| EEG alone | Higher accuracy for radial sources | Optimal for gyral activity | |
| MEG + EEG Combined | Consistently smaller localization errors vs. either alone | Multimodal integration significantly improves spatial precision | |
| Brain-Computer Interface (BCI) Classification [10] | 306-channel MEG | 73.2% average accuracy (1-second trials) | Benchmark for high-fidelity target detection |
| 64-channel EEG | 69% average accuracy | Good performance with high-density setup | |
| 9-channel EEG | 66% average accuracy | Usable BCI with optimized, portable setup | |
| 3-channel EEG | 61% average accuracy | Performance degrades but remains above chance | |
| Pharmacodynamic Biomarker Development [11] | fMRI, EEG, PET | Identifies four key questions for clinical trials: brain penetration, target engagement, dose selection, indication selection | Provides a structured framework for de-risking drug development |
Detailed Experimental Protocols
Protocol: Combined MEG and EEG for High-Fidelity Source Localization
This protocol is designed to capitalize on the complementary strengths of MEG and EEG to achieve superior spatiotemporal resolution in localizing neural activity [8] [9].
1. Experimental Design and Stimulation:
- Stimuli: Use focal, well-controlled stimuli (e.g., Gabor patches for visual cortex) that can evoke robust, localizable neural responses.
- Paradigm: Employ an event-related design. Present stimuli for 500 ms with a randomized inter-stimulus interval (e.g., 1-6.5 seconds) to facilitate deconvolution of the neural response.
- Task: Incorporate a behavioral task (e.g., fixation cross change detection) to ensure participant alertness and monitor performance. Discard trials with incorrect behavioral responses.
2. Simultaneous Data Acquisition:
- MEG: Record using a whole-head system (e.g., 306-channel Elekta Neuromag or CTF system). Sample data at a minimum of 1000 Hz. Ensure the subject's head position is monitored and corrected if necessary.
- EEG: Record simultaneously using a 64+ channel cap. Sync EEG and MEG acquisition systems using a shared trigger pulse. Use appropriate reference and ground electrode placements.
- Ancillary Data: Record the subject's head shape (via digitization) and the location of EEG electrodes relative to MEG head position indicators (HPIs) for co-registration.
3. Structural MRI Co-registration:
- Acquire a high-resolution T1-weighted sMRI scan for each subject.
- Co-register the MEG/EEG sensor data to the subject's anatomical MRI using the digitized head points and fiducial markers (nasion, left/right pre-auricular points).
4. Data Preprocessing:
- Filter data (e.g., 0.1-40 Hz bandpass for evoked responses).
- Apply artifact correction (e.g., Signal-Space Separation (SSS) for MEG; ICA for ocular and cardiac artifacts in EEG).
- Epoch data into trials time-locked to stimulus onset.
5. Source Estimation and Analysis:
- Construct a forward model using a boundary element model (BEM) based on the sMRI.
- Calculate an inverse solution (e.g., depth-weighted minimum-norm estimate (MNE) or dynamic statistical parametric mapping (dSPM)) using the combined MEG+EEG data.
- Compare the localization results against a ground truth, such as BOLD fMRI activation from an identical task, to validate accuracy.
Protocol: Integrating Neuroimaging in CNS Drug Development
This protocol outlines a precision medicine approach, using neuroimaging biomarkers to stratify patients and measure drug effects, thereby de-risking clinical trials [11].
1. Pre-Clinical and Phase 1: Establishing Target Engagement
- Objective: Determine if the drug candidate engages the intended brain target and produces a measurable functional effect.
- Modality: fMRI or task-based EEG/MEG.
- Design: Double-blind, placebo-controlled, crossover or parallel-group study.
- Procedure:
- Administer the drug or placebo.
- During expected peak plasma concentration, scan participants while they perform a cognitive task known to engage the target neural circuit.
- Analysis: Compare the neural activity (e.g., BOLD signal in a specific region, or EEG/MEG oscillatory power) between drug and placebo conditions. A significant difference confirms functional target engagement.
2. Phase 2: Patient Stratification and Dose-Finding
- Objective: Identify a biomarker that predicts clinical response and determine the optimal dose.
- Modality: Accessible and scalable modalities like EEG are preferred for larger trials.
- Design: Large, biomarker-stratified design.
- Procedure:
- At baseline, collect neuroimaging data (e.g., resting-state EEG) from all patients.
- Use a pre-defined biomarker signature (e.g., a specific EEG pattern) to stratify patients into "biomarker-positive" and "biomarker-negative" subgroups.
- Randomize patients to different dose groups or placebo.
- Analysis: Test the primary clinical outcome. The hypothesis is that the "biomarker-positive" subgroup will show a significantly better response to the drug compared to the "biomarker-negative" subgroup and placebo, demonstrating predictive validity.
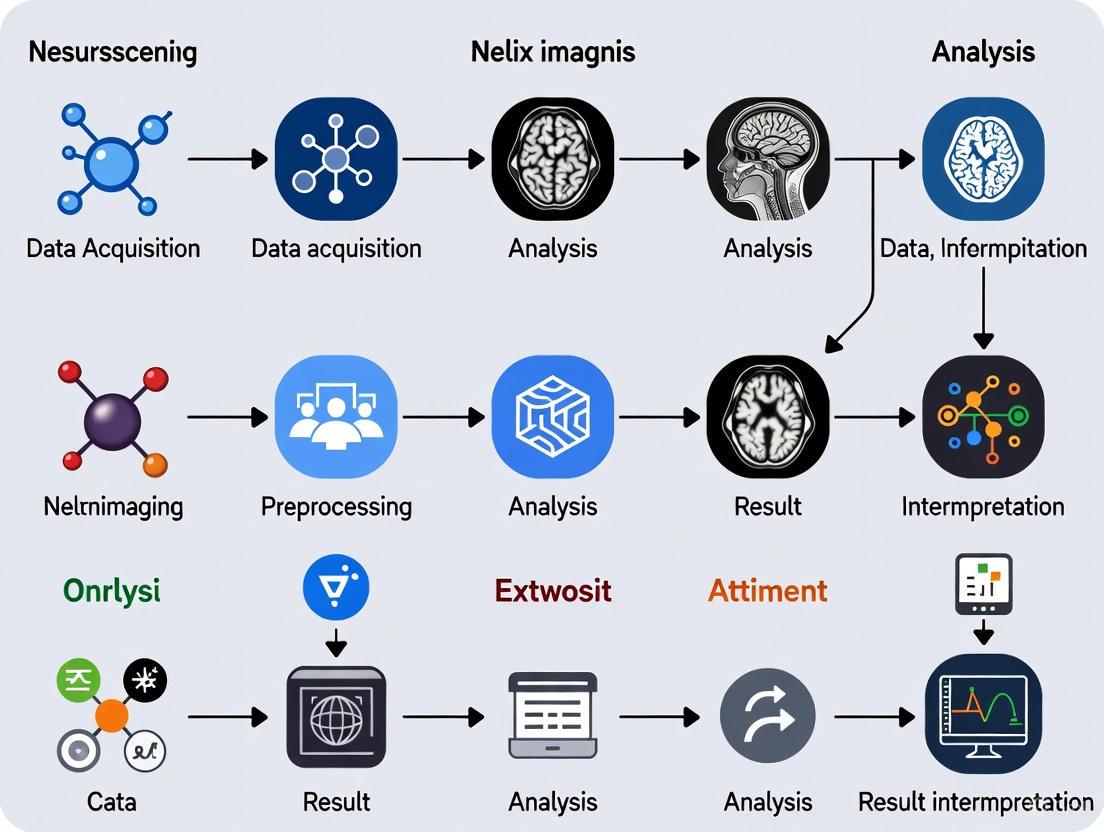
Visual Workflows and Signaling Pathways
Diagram 1: Multimodal Neuroimaging Data Analysis Workflow. This workflow integrates structural, functional, and electrophysiological data to produce validated biomarkers and insights.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Resources for Multimodal Neuroimaging Research
| Resource Category | Specific Examples & Functions | Relevance to Workflows |
|---|---|---|
| Public Data Repositories | Human Connectome Project (HCP) Data [7]: Provides pre-processed, high-quality multimodal data (fMRI, sMRI, DWI) for method development and testing. | Essential for benchmarking algorithms and accessing large-scale normative datasets. |
| Analysis Software & Platforms | FSFreeSurfer, FSL, SPM, MNE-Python, Connectome Workbench: Open-source suites for structural segmentation, functional and diffusion analysis, and MEG/EEG source estimation. | Form the core of the analytical pipeline; interoperability is key for multimodal integration. |
| Computational Frameworks | Graph Neural Networks (GNNs) [7]: Framework for analyzing brain connectivity data represented as graphs, enabling multimodal fusion and prediction. | Represents the cutting-edge for integrating structural and functional connectivity features. |
| Biomarker Platforms (Industry) | Alto Neuroscience Platform [11]: Uses EEG and other biomarkers to stratify patients in clinical trials for psychiatric disorders, validating the "precision psychiatry" approach. | Provides a commercial and clinical validation of the protocols described herein. |
| Experimental Stimuli | Natural Object Dataset (NOD) [12]: A large-scale dataset containing fMRI, MEG, and EEG responses to naturalistic images, enabling ecologically valid studies of object recognition. | Critical for experiments aiming to move beyond simple, controlled stimuli to understand brain function in natural contexts. |
The expansion of large-scale, centralized biomedical data resources has fundamentally altered the landscape of neuroimaging research, enabling unprecedented discoveries in brain structure, function, and disease. These repositories provide researchers with the extensive datasets necessary to develop and validate robust computational models, moving beyond underpowered studies towards reproducible neuroscience. For researchers and drug development professionals, navigating the specific characteristics, access procedures, and optimal use cases of these resources is a critical first step in designing effective analysis workflows. This guide provides a detailed comparison and protocols for four pivotal resources: UK Biobank, ABCD Study, OpenNeuro, and ADNI, framing their use within a comprehensive brain imaging data analysis pipeline.
Resource Comparison and Characterization
The major data resources cater to distinct research populations, data types, and primary objectives. The table below provides a systematic comparison of their core attributes for researcher evaluation.
Table 1: Comparative Overview of Centralized Neuroimaging Data Resources
| Resource | Primary Focus & Population | Key Data Modalities | Access Model & Cost | Sample Scale & Key Features |
|---|---|---|---|---|
| UK Biobank [13] | Longitudinal health of 500,000 UK participants; general population, adult (aged 40-69 at recruitment) [13] | Multi-modal imaging, genomics, metabolomics, proteomics, healthcare records, wearable activity [13] [14] [15] | Approved researchers; access fee for international researchers [13] | ~500,000 participants; Imaging for 100,000+ [13] [15]; Most comprehensive phenotypic data |
| ABCD Study [16] | Brain development and child health in the US; over 10,000 children aged 9-10 at baseline | Brain imaging (fMRI, sMRI), neurocognitive assessments, biospecimens, substance use surveys | Controlled access; no cost; requires Data Use Certification (DUC) [16] | ~10,000+ participants; Longitudinal design through adolescence |
| OpenNeuro [17] [18] | Open platform for sharing any neuroimaging dataset; diverse populations and focuses | Brain imaging data (BIDS-formatted), often with behavioral phenotypes | Open access for public datasets; free download and upload [18] | 1,000+ datasets; Platform for data sharing; No central cohort |
| ADNI [19] [20] | Alzheimer's Disease (AD) progression; older adults with Normal Cognition, MCI, and AD | Longitudinal MRI, PET, genetic data, cognitive tests, biomarkers (e.g., CSF, plasma) | Controlled access; application required; no cost for approved research [20] | ~2,000+ participants; Deeply phenotyped for neurodegenerative disease |
Data Access Protocols and Workflows
Gaining access to these resources involves navigating specific, and often mandatory, procedural pathways. The following protocols detail the steps for each.
UK Biobank Access Protocol
- Registration and Application: Researchers must register on the UK Biobank access management system and submit a detailed application outlining their research purpose, the specific data fields required, and the intended use [13].
- Approval and Costing: Applications are reviewed by the UK Biobank team. Upon approval, the researcher or their institution is invoiced for the data access fee, which contributes to the maintenance and expansion of the resource [13].
- Data Access: Once access is granted, researchers can download the data directly or, increasingly, analyze it in-place using the UK Biobank's Research Analysis Platform (UKB-RAP) to avoid transferring large datasets [13].
ABCD Study & ADNI Access Protocol
The ABCD Study and ADNI share a similar controlled-access model, governed by NIH policies.
- Data Use Agreement (DUA): The principal investigator must read and agree to the resource-specific Data Use Agreement, which outlines terms of use, data security requirements, and publication policies [16] [20].
- Online Application: The researcher must complete an online application form via the respective data hub:
- Review and Approval: The respective data sharing committee (e.g., ADNI's Data Sharing and Publications Committee) reviews applications, typically within two weeks [20].
- NIH Security Compliance: Approved users must comply with NIH Security Best Practices for controlled-access data, which often entails using institutional IT systems or cloud providers meeting specific security standards like NIST SP 800-171 [16].
- Account Maintenance: A provision of the access agreement is the submission of an annual update to maintain an active account [20].
OpenNeuro Data Access and Sharing Protocol
As an open-data platform, OpenNeuro simplifies data sharing and retrieval.
- Downloading Public Data: Users can search and download any publicly available dataset directly through the web interface or via the command-line interface (CLI) without any access application [18].
- Uploading Data: Researchers preparing to share data must format their dataset according to the Brain Imaging Data Structure (BIDS) standard. The platform runs the BIDS-validator automatically upon upload to ensure compliance [17].
The following workflow diagram summarizes the access pathways for these resources.
Experimental Design and Analytical Protocols
Leveraging these datasets requires careful experimental design. A recent study on brain-age prediction using multi-head self-attention models provides a concrete example of a cross-dataset analytical workflow [21].
Case Study: Brain Age Prediction Model
Objective: To develop a lightweight, accurate deep learning model for brain age estimation and evaluate its generalizability and potential bias across Western and Middle Eastern populations [21].
Datasets and Harmonization:
- Primary Training/Testing Data: 4,635 healthy individuals (aged 40-80) from Western datasets: ADNI, OASIS-3, Cam-CAN, and IXI [21].
- External Validation Data: 107 subjects from a Middle Eastern (ME) dataset (Tehran, Iran) [21].
- Data Split: 80% of the Western data (n=3,700) for training, 20% (n=935) for testing [21].
Model Architecture:
- Base Network: 3D Convolutional Neural Network (CNN) for feature extraction from structural MRI.
- Core Innovation: Integration of multi-head self-attention mechanisms to capture long-range spatial dependencies in brain images, enhancing feature learning.
- Efficiency: Model designed to be lightweight with approximately 3 million parameters [21].
Performance and Bias Analysis:
- Evaluation Metric: Mean Absolute Error (MAE) between predicted brain age and chronological age.
- Bias Correction: Application of a post-hoc linear regression correction (Y = aX + b) fitted on the Western training set to adjust predictions on the test sets [21].
Table 2: Brain Age Prediction Model Performance Across Datasets [21]
| Dataset | Number of Subjects (N) | Mean Age (Std) | MAE before Bias Correction (Years) | MAE after Bias Correction (Years) |
|---|---|---|---|---|
| Western Test Set (Total) | 935 | - | 2.09 | 1.99 |
| ADNI | 442 | 71.94 (5.09) | 1.24 | 1.23 |
| OASIS-3 | 348 | 64.60 (8.54) | 1.98 | 2.00 |
| Cam-CAN | 82 | 60.39 (12.17) | 4.30 | 4.43 |
| IXI | 63 | 58.37 (10.13) | 4.23 | 4.04 |
| Middle Eastern (ME) Dataset | 107 | 50.31 (4.76) | 5.83 | 5.96 |
Key Findings: The model achieved state-of-the-art accuracy on the Western test set (MAE = 1.99 years) but performed significantly worse on the Middle Eastern dataset (MAE = 5.83 years). Critically, bias correction based on the Western data further degraded performance on the ME dataset, highlighting profound population-specific differences in brain aging and the risk of bias in models trained on non-diverse data [21].
Protocol for fMRI Study Design: The Scan Time vs. Sample Size Trade-Off
A fundamental design consideration for functional MRI (fMRI) studies is the trade-off between scan time per participant and total sample size, especially under budget constraints. A recent Nature (2025) study provides an evidence-based framework for this optimization [22].
Key Empirical Relationship:
- Prediction accuracy of phenotypes from resting-state fMRI increases with the total scan duration (sample size × scan time per participant) [22].
- For scans ≤20 minutes, sample size and scan time are largely interchangeable; accuracy increases linearly with the logarithm of the total scan duration [22].
- However, diminishing returns are observed for longer scan times, with sample size ultimately being more critical for prediction power [22].
Cost-Efficiency Optimization:
- 10-minute scans are cost-inefficient for achieving high prediction performance [22].
- The most cost-effective scan time is at least 20 minutes, with 30 minutes being optimal on average, yielding ~22% cost savings compared to 10-minute scans [22].
- Overshooting the optimal scan time is cheaper than undershooting it, so a scan time of at least 30 minutes is recommended [22].
The following diagram illustrates the analytical workflow integrating data access, study design, and model validation.
The Scientist's Toolkit: Essential Research Reagents and Materials
Executing a robust neuroimaging data analysis requires a suite of computational tools and platforms that constitute the modern "research reagent."
Table 3: Essential Computational Tools for Neuroimaging Data Analysis
| Tool / Resource | Primary Function | Application in Workflow |
|---|---|---|
| BIDS Validator [17] | Validates compliance of datasets with the Brain Imaging Data Structure standard. | Essential pre-processing step before uploading data to OpenNeuro or other BIDS-compliant platforms. |
| OpenNeuro CLI [18] | A command-line interface for OpenNeuro. | Enables automated and efficient upload/download of large neuroimaging datasets, particularly useful for HPC environments. |
| DataLad & git-annex [17] | Version control and management of large files. | Foundation of OpenNeuro's data handling; allows for precise tracking of dataset revisions and efficient data distribution. |
| UKB-RAP (Research Analysis Platform) [13] | A cloud-based analysis platform provided by UK Biobank. | Allows approved researchers to analyze UK Biobank data in-place without the need for massive local download and storage. |
| NBDC Data Hub [16] | The NIH data ecosystem hosting ABCD and HBCD study data. | The central portal for querying, accessing, and managing controlled-access data from the ABCD study with streamlined Data Use Certification. |
| LONI IDA [20] | The Image and Data Archive for ADNI. | The secure repository where approved researchers access and download ADNI imaging, clinical, and biomarker data. |
Centralized data resources like UK Biobank, ABCD, OpenNeuro, and ADNI are powerful engines for neuroimaging research and drug development. The choice of resource must be guided by the specific research question, considering population focus, data modalities, and scale. As demonstrated, the analytical workflow—from navigating access protocols and optimizing study design to validating models across diverse populations—is critical for generating robust, reproducible, and meaningful scientific insights. The growing emphasis on population diversity and computational efficiency, as seen in the latest studies, will continue to shape the future of brain imaging data analysis.
The advent of large-scale neuroimaging datasets has fundamentally transformed brain imaging research, enabling unprecedented exploration of brain structure, function, and connectivity across diverse populations [23]. Initiatives like the Human Connectome Project, the UK Biobank (with over 50,000 scans), and the Alzheimer's Disease Neuroimaging Initiative have generated petabytes of imaging data, providing researchers with powerful resources for investigating neurological and psychiatric disorders [24] [23]. However, this data deluge presents substantial computational challenges that transcend the capabilities of traditional desktop computing environments. The size, complexity, and multimodal nature of modern neuroimaging data demand sophisticated computing infrastructure and specialized analytical approaches [25] [23].
Cloud and High-Performance Computing (HPC) platforms have emerged as critical infrastructures for managing, processing, and analyzing large-scale neuroimaging data [23]. These platforms provide the necessary computational power, storage solutions, and scalability required for contemporary brain imaging research. The integration of standardized data formats, containerized software solutions, and workflow management systems has further enhanced the reproducibility, efficiency, and accessibility of neuroimaging analyses across diverse computing environments [26] [24] [27]. This article presents application notes and protocols for leveraging cloud and HPC platforms in brain imaging data analysis workflows, with specific methodologies, performance benchmarks, and practical implementation guidelines for researchers, scientists, and drug development professionals.
Platform Comparison and Performance Metrics
Quantitative Performance of Scalable Processing Pipelines
Processing pipelines demonstrate significantly different performance characteristics across computing environments. The following table summarizes benchmark results for prominent neuroimaging pipelines evaluated on large datasets:
Table 1: Performance comparison of neuroimaging pipelines on large-scale datasets
| Pipeline | Computing Environment | Sample Size | Processing Time per Subject | Acceleration Factor | Key Innovation |
|---|---|---|---|---|---|
| DeepPrep [24] | Local workstation (GPU-equipped) | UK Biobank subset | 31.6 ± 2.4 minutes | 10.1× faster than fMRIPrep | Deep learning integration |
| DeepPrep [24] | HPC cluster (batch processing) | 1,146 participants | 8.8 minutes per subject | 10.4× more efficient than fMRIPrep | Workflow manager (Nextflow) |
| fMRIPrep [24] | Local workstation (CPU) | UK Biobank subset | 318.9 ± 43.2 minutes | Baseline | Conventional algorithms |
| BABS [27] | HPC (Slurm/SGE) | Healthy Brain Network (n=2,565) | Variable (dependent on BIDS App) | N/A (enables reproducibility) | DataLad-based provenance tracking |
DeepPrep demonstrates remarkable computational efficiency, processing the entire UK Biobank neuroimaging dataset (over 54,515 scans) within 6.5 days in an HPC cluster environment [24]. This represents a significant advancement in processing scalability compared to conventional approaches. The pipeline maintains this efficiency while ensuring robust performance across diverse datasets, including clinical samples with pathological brain conditions that often challenge conventional processing pipelines [24].
Computational Cost Analysis in HPC Environments
The economic considerations of large-scale neuroimaging data processing extend beyond simple processing time metrics. A critical analysis of computational expenses reveals substantial differences between pipelines:
Table 2: Computational expense comparison in HPC environments
| Pipeline | CPU Allocation | Processing Time | Relative Computational Expense | Cost Efficiency Advantage |
|---|---|---|---|---|
| DeepPrep [24] | Flexible (1-16 CPUs) | Stable across configurations | 5.8-22.1× lower than fMRIPrep | Dynamic resource allocation |
| fMRIPrep [24] | 1 CPU | ~6 hours | Baseline | N/A |
| fMRIPrep [24] | 16 CPUs | ~1 hour | Up to 22.1× higher than DeepPrep | Characteristic trade-off curve |
DeepPrep's stability in both processing time and expenses across different CPU allocations stems from its computational flexibility in dynamically allocating resources to match specific task requirements [24]. This represents a significant advantage for researchers working within constrained computational budgets, particularly when processing large-scale datasets.
Experimental Protocols for Scalable Neuroimaging
Protocol: Large-Scale Connectome Mapping Pipeline
This protocol outlines the methodology for mapping structural connectivity across large cohorts (n=1,800+ participants) using cloud-integrated HPC resources, based on validated approaches from published research [28].
Materials and Reagents
- High-quality diffusion MRI data
- T1-weighted structural images
- Population receptive field (pRF) mapping data
- Computational resources: Texas Advanced Computing Center (TACC) HPC clusters or equivalent cloud infrastructure
- Software platform: brainlife.io open-source platform
Procedure
- Data Acquisition and Transfer
- Acquire multi-shell diffusion MRI data with appropriate b-values (e.g., b=1000, 2000 s/mm²)
- Collect high-resolution T1-weighted anatomical images (1mm³ isotropic resolution recommended)
- Transfer data to HPC or cloud storage with integrity verification
Diffusion MRI Preprocessing
- Perform denoising using patch-based algorithms (e.g., MRTrix3 dwidenoise)
- Correct for eddy currents and subject motion using FSL eddy with outlier replacement
- Conduct B1 field inhomogeneity correction
Tractography Reconstruction
- Reconstruct fiber orientation distributions using constrained spherical deconvolution
- Generate whole-brain tractography with deterministic or probabilistic algorithms (e.g., 10 million streamlines)
- Apply spherical-deconvolution informed filtering of tractograms (SIFT) to reduce reconstruction bias
Visual Cortex Parcellation
- Map visual field representations onto cortical surface using population receptive field (pRF) modeling
- Subdivide visual areas according to visual field coordinates (upper/lower vertical meridian, horizontal meridian)
- Coregister pRF maps with diffusion data in common space
Connectivity Quantification
- Calculate connectivity density as number of axonal connections between visual areas divided by region volume
- Separate intra-occipital connections (within visual cortex) from long-range connections (afferent to visual areas)
- Normalize connectivity measures by region volume
Statistical Analysis
- Perform repeated-measures ANOVA to examine connectivity asymmetries
- Conduct post-hoc t-tests with multiple comparison correction (FDR, p<0.05)
- Implement lifespan analyses using linear mixed-effects models
Validation and Quality Control
- Verify pipeline performance by replicating known visual asymmetries (higher connectivity along horizontal vs. vertical meridians)
- Confirm expected hemispheric differences in connectivity patterns
- Implement automated quality control metrics for tractography reconstruction
Protocol: Reproducible Processing with BIDS App Bootstrap (BABS)
The BIDS App Bootstrap framework enables reproducible, large-scale image processing while maintaining complete provenance tracking [27].
Materials and Reagents
- BIDS-structured dataset
- BIDS App container (Docker or Singularity)
- HPC cluster with Slurm or SGE job scheduler
- DataLad installation (v0.15+)
Procedure
- Environment Setup
BABS Configuration
Workflow Initialization
Job Submission and Monitoring
Provenance Tracking and Reporting
Validation and Quality Control
- Verify complete audit trail for all processed participants
- Confirm checksum consistency for input and output files
- Validate BIDS derivatives compliance
- Ensure processing commands are fully recorded in DataLad history
Architecture and Workflow Visualization
Scalable Neuroimaging Architecture
The following diagram illustrates the integrated architecture of scalable neuroimaging pipelines across different computing environments:
Scalable Neuroimaging Architecture
Reproducible Processing Workflow
The workflow for reproducible large-scale processing using the BABS framework incorporates full provenance tracking:
Reproducible Processing Workflow
The Scientist's Toolkit
Essential Platforms and Software Solutions
Table 3: Essential research reagent solutions for scalable neuroimaging
| Tool/Platform | Primary Function | Key Features | Computing Environment |
|---|---|---|---|
| Neurodesk [26] [29] | Containerized analysis environment | Reproducible workflows, tool interoperability, BIDS compliance | Local, HPC, Cloud |
| DeepPrep [24] | Accelerated neuroimaging preprocessing | Deep learning integration, 10× acceleration, clinical robustness | GPU-equipped workstations, HPC |
| BABS [27] | Reproducible BIDS App processing | DataLad provenance, audit trail, HPC integration | Slurm, SGE HPC clusters |
| brainlife.io [28] | Open-source neuroscience platform | Automated pipelines, data management, visualization | Cloud-integrated HPC |
| DataLad [27] | Data version control | Git-annex integration, provenance tracking, distribution | Cross-platform |
| Flywheel [30] | Cloud data management | Data organization, metadata query, analysis pipelines | Cloud-agnostic |
Implementation Considerations
Computational Resource Allocation Effective utilization of cloud and HPC resources requires careful planning. Research teams should implement unique cost centers for labs and teams to promote responsible resource consumption [30]. The hidden costs of cloud computing, including long-running computational jobs, ingress/egress fees, and inefficient compute management, must be factored into project planning [30].
Data Organization and Management Structuring large multimodal data with comprehensive metadata enables programmatic access and intuitive exploration [30]. Data organization should be built into pipelines from the start rather than saved for later stages [30]. Distinguishing raw data from derived products with read-only permissions and avoiding data duplication supports effective access controls [30].
Environmental Sustainability The carbon footprint of neuroimaging data processing varies significantly across tools and approaches [31]. Measuring and comparing the environmental impact of different processing strategies, such as FSL, SPM, and fMRIPrep, enables researchers to make environmentally conscious decisions [31]. Climate-aware task schedulers and energy-efficient algorithms represent promising approaches for reducing the environmental impact of large-scale neuroimaging research [31].
Cloud and HPC platforms have become indispensable infrastructures for contemporary brain imaging research, enabling the processing and analysis of large-scale datasets that were previously computationally intractable. The integration of containerized software solutions, standardized data formats, and workflow management systems has enhanced both the reproducibility and accessibility of advanced neuroimaging analyses. Deep learning-accelerated pipelines like DeepPrep demonstrate order-of-magnitude improvements in processing efficiency while maintaining analytical accuracy [24]. Frameworks such as BABS provide critical provenance tracking capabilities that ensure the reproducibility of large-scale analyses [27].
Future developments in scalable neuroimaging will likely focus on several key areas. Federated learning approaches will enable collaborative model training across institutions without sharing raw data, addressing privacy and regulatory concerns [23]. The development of more energy-efficient algorithms and climate-aware scheduling systems will help mitigate the environmental impact of computation-intensive neuroimaging research [31]. Enhanced interoperability between platforms, standardized implementation of FAIR data principles, and continued innovation in deep learning applications will further advance the field. As these developments mature, researchers and drug development professionals will be increasingly equipped to translate large-scale brain imaging data into meaningful insights about brain structure, function, and disorders.
From Raw Data to Results: Workflow Tools and AI Methodologies
In modern brain imaging research, the choice of data processing workflow is a critical determinant of success. These workflows, or pipelines, are the structured sequences of computational steps that transform raw neuroimaging data into interpretable results. A fundamental dichotomy exists between fixed pipelines, which use a predetermined, standardized set of processing steps and parameters, and flexible pipelines, which allow for adaptive configuration, customization, and optimization of these steps. Fixed pipelines prioritize reproducibility, standardization, and ease of use, making them suitable for well-established analytical paths and large-scale data processing. In contrast, flexible pipelines emphasize optimization for specific research questions, adaptability to novel data types or experimental designs, and the ability to incorporate the latest algorithms, though they often require greater computational expertise and rigorous validation to ensure reliability.
The strategic selection between these approaches directly impacts the scalability, accuracy, and clinical applicability of research findings. For instance, the DeepPrep pipeline demonstrates the power of integrating deep learning modules to achieve a tenfold acceleration in processing time while maintaining robust performance across over 55,000 scans, including challenging clinical cases with brain distortions [24]. This document provides a structured framework, including application notes, experimental protocols, and decision aids, to guide researchers in selecting and implementing the optimal workflow strategy for their specific brain imaging projects.
Application Notes: Comparative Analysis of Pipeline Strategies
Performance Benchmarks and Clinical Applicability
Table 1: Quantitative Performance Comparison of Representative Pipelines
| Pipeline / Tool | Primary Strategy | Key Performance Metric | Reported Outcome | Clinical Robustness |
|---|---|---|---|---|
| DeepPrep [24] | Flexible (AI-powered) | Processing Time | 10.1x faster than fMRIPrep (31.6 vs. 318.9 min) | 100% completion on distorted brains |
| fMRIPrep [24] | Fixed (Standardized) | Processing Time | Baseline (318.9 ± 43.2 min) | 69.8% completion on distorted brains |
| USLR [32] | Flexible (Longitudinal) | Analysis Power | Improved detection of group differences vs. cross-sectional | Enables subject-specific prediction |
| NeuroMark [33] | Hybrid (Spatial Priors + Data-Driven) | Predictive Accuracy | Outperforms predefined atlases | Captures individual variability for biomarkers |
The data in Table 1 reveals a clear trade-off. Flexible and hybrid pipelines, such as DeepPrep and NeuroMark, demonstrate superior performance in computational efficiency and the ability to capture individual subject variability, which is crucial for clinical translation and personalized medicine [24] [33]. The USLR framework highlights another strength of flexible approaches: by enforcing smooth, unbiased longitudinal registration, it achieves higher sensitivity in detecting subtle, clinically relevant changes like those in Alzheimer's disease, potentially reducing the sample sizes required in clinical trials [32].
However, the fixed pipeline approach, exemplified by tools like fMRIPrep, provides a critical foundation of standardization and reproducibility. The challenge of variability is starkly illustrated in functional connectomics, where a systematic evaluation of 768 data-processing pipelines revealed "vast and systematic variability" in their suitability, with the majority of pipelines failing at least one key criterion for reliability and sensitivity [34]. This underscores that an uninformed choice of a flexible pipeline can produce "misleading conclusions about neurobiology," whereas a set of optimal pipelines can consistently satisfy multiple criteria across different datasets [34].
A Framework for Functional Decomposition
Choosing a pipeline often involves selecting a strategy for functional decomposition—the method of parcellating the brain into functionally meaningful units for analysis. A useful framework classifies these decompositions along three key attributes [33]:
- Source: The origin of the decomposition (e.g., Anatomical, Functional, Multimodal).
- Mode: The nature of the brain units (e.g., Categorical/discrete regions vs. Dimensional/overlapping representations).
- Fit: The degree of data-driven adaptation (e.g., Predefined, Data-driven, Hybrid).
Table 2: Functional Decomposition Atlas Classification
| Atlas / Approach | Source | Mode | Fit | Typical Use Case |
|---|---|---|---|---|
| AAL Atlas [33] | Anatomical | Categorical | Predefined | Standardized structural analysis |
| Yeo 17 Network [33] | Functional | Dimensional | Predefined | Resting-state network analysis |
| Fully Data-Driven ICA | Functional | Dimensional | Data-Driven | Exploratory analysis of a single study |
| NeuroMark Pipeline [33] | Functional | Dimensional | Hybrid (Spatially Constrained) | Individual differences, cross-study comparison |
Fixed pipelines typically employ predefined atlases (e.g., AAL, Yeo), which offer excellent interoperability and comparability across studies. In contrast, flexible workflows may leverage fully data-driven decompositions, which can better fit a specific dataset but struggle with cross-subject correspondence. Hybrid models, like the NeuroMark pipeline, represent a powerful compromise, using spatial priors derived from large datasets to ensure correspondence across subjects while allowing data-driven refinement to capture individual variability and dynamic spatial patterns [33]. This hybrid approach has been shown to boost sensitivity to individual differences while maintaining cross-subject generalizability [33].
Experimental Protocols
Protocol 1: Benchmarking Fixed vs. Flexible Preprocessing Pipelines
Objective: To quantitatively compare the processing time, computational resource utilization, and robustness of a fixed pipeline (e.g., fMRIPrep) against a flexible, AI-powered pipeline (e.g., DeepPrep) on a dataset that includes both healthy controls and pathological cases.
Materials:
- Imaging Data: A cohort of T1-weighted structural MRI and resting-state fMRI scans. The cohort should include at least 20 healthy control scans and 10 clinical scans from patients with conditions causing brain distortion (e.g., glioma, stroke) [24].
- Computing Environment: A high-performance computing (HPC) node or a local workstation equipped with CPUs and at least one GPU.
- Software: Docker or Singularity container platforms. The fixed pipeline (fMRIPrep) and the flexible pipeline (DeepPrep) should be installed as BIDS Apps [24].
Methodology:
- Data Standardization: Convert all raw DICOM files into the Brain Imaging Data Structure (BIDS) format. This can be automated using data management platforms like Flywheel, which provides built-in Gears for BIDS conversion [35].
- Pipeline Execution:
- Process the entire dataset (30 scans) through both fMRIPrep and DeepPrep.
- For resource analysis, run fMRIPrep by recruiting different CPU counts (e.g., 1, 2, 4, 8, 16) for a single participant and record the processing time and total CPU hours expended [24].
- Execute DeepPrep on the same participant in a GPU-enabled environment as recommended.
- Outcome Measures:
- Processing Time: Record the wall-clock time for each processed scan.
- Computational Cost: Calculate the total CPU hours and associated cloud computing costs (if applicable) for each pipeline.
- Pipeline Completion Ratio: For each pipeline, calculate the percentage of scans that completed preprocessing without fatal errors.
- Acceptable Ratio: Have a qualified analyst (or use an automated quality control tool) review the preprocessed outputs and visual reports for anatomical accuracy (e.g., correct tissue segmentation, surface reconstruction). Calculate the percentage of scans with acceptable quality [24].
Expected Outcomes: Anticipate results similar to the DeepPrep study, where the flexible pipeline showed a tenfold acceleration, lower computational expenses (5.8x to 22.1x lower), and superior completion (100% vs. 69.8%) and acceptable (58.5% vs. 30.2%) ratios on pathological brains [24].
Protocol 2: Evaluating the Impact of Pipeline Choice on Functional Connectomics
Objective: To assess how different data-processing pipelines for constructing functional brain networks affect the test-retest reliability and sensitivity to experimental effects of derived graph-theoretical metrics.
Materials:
- Imaging Data: A test-retest resting-state fMRI dataset, such as from the Human Connectome Project, where the same participant was scanned on multiple sessions [34].
- Pipelines: A subset of the 768 possible pipeline combinations generated by varying key steps [34]:
- Global Signal Regression (GSR): With vs. Without.
- Brain Parcellation (Node Definition): e.g., Anatomical (AAL), functional (Yeo), multimodal (Brainnetome).
- Number of Nodes: ~100, 200, or 300-400.
- Edge Definition: Pearson correlation vs. Mutual Information.
- Edge Filtering: Density-based (e.g., retain 5% of edges) vs. Weight-based (e.g., minimum weight 0.3) vs. Data-driven (Efficiency Cost Optimization).
- Network Type: Binary vs. Weighted.
Methodology:
- Network Construction: For a single subject's test-retest data, run a selected array of pipelines (e.g., 10-20 contrasting combinations) to reconstruct functional brain networks for each session.
- Topological Analysis: Calculate common network metrics (e.g., modularity, global efficiency) from each constructed network.
- Evaluation:
- Test-Retest Reliability: Calculate the intra-class correlation (ICC) of each network metric between the two sessions for each pipeline.
- Portrait Divergence (PDiv): Use this information-theoretic measure to compute the dissimilarity between the network topologies of the two sessions. A lower PDiv indicates higher reliability [34].
- Criterion Satisfaction: Classify each pipeline based on its ability to minimize motion confounds and spurious test-retest discrepancies while remaining sensitive to inter-subject differences.
Expected Outcomes: This protocol will likely reveal that a majority of pipeline combinations fail to meet all reliability and sensitivity criteria. The goal is to identify a subset of "optimal" pipelines that consistently produce reliable and sensitive network topologies, as demonstrated in the systematic evaluation by [34].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for Brain Imaging Workflow Development
| Tool / Solution | Function | Relevance to Pipeline Strategy |
|---|---|---|
| BIDS (Brain Imaging Data Structure) [35] | A framework for organizing and describing neuroimaging datasets. | Foundational standard for both fixed and flexible pipelines, enabling interoperability and automated data ingestion. |
| Deep Learning Modules (e.g., FastSurferCNN, SUGAR) [24] | Pre-trained neural networks for specific tasks (segmentation, surface registration). | Core components of flexible, accelerated pipelines like DeepPrep, replacing conventional algorithms. |
| Containerization (Docker/Singularity) [24] | Packages software and all dependencies into a portable, reproducible unit. | Critical for deploying both fixed and flexible pipelines consistently across different computing environments. |
| Workflow Manager (Nextflow) [24] | Manages complex computational workflows, enabling scalability and portability. | Key for scalable execution of flexible pipelines in HPC and cloud environments, dynamic resource allocation. |
| Spatial Priors (e.g., NeuroMark Templates) [33] | Data-derived templates used to guide and regularize subject-level decomposition. | Enables hybrid analysis strategies, balancing individual specificity with cross-subject correspondence. |
| Simulation-Based Inference (SBI) Toolkits (e.g., VBI) [36] | Enables Bayesian parameter estimation for complex whole-brain models where traditional inference fails. | A flexible approach for model inversion, quantifying uncertainty in parameters for biophysically interpretable inference. |
Workflow Decision Diagrams
Strategic Pipeline Selection
Implementing a Flexible Hybrid Analysis
The analysis of brain imaging data presents a significant challenge in terms of complexity, reproducibility, and scalability. Fixed neuroimaging pipelines address these challenges by providing standardized, automated workflows that ensure consistent processing across datasets and research groups. Within the broader context of brain imaging data analysis workflows research, these pipelines transform raw, complex magnetic resonance imaging (MRI) data into reliable, analyzable metrics, thereby accelerating scientific discovery and facilitating cross-study comparisons. This article examines three specialized pipelines—CIVET, PANDA, and DPARSF—that have been developed for distinct analysis types: cortical morphology, white matter integrity, and resting-state brain function, respectively. Each represents a tailored solution to specific analytical challenges while embodying the core principles of automation, standardization, and reproducibility that are crucial for advancing neuroimaging science. By integrating these pipelines into their research, scientists and drug development professionals can enhance methodological rigor, reduce processing errors, and focus intellectual resources on scientific interpretation rather than technical implementation.
Table 1: Overview of Specialized Neuroimaging Pipelines
| Pipeline | Primary Analysis Type | Core Function | Input Data | Key Outputs |
|---|---|---|---|---|
| CIVET | Cortical Morphology | Automated cortical surface extraction | T1-weighted MRI | Cortical thickness, surface models |
| PANDA | White Matter Integrity | Diffusion image processing | Diffusion MRI | Fractional Anisotropy (FA), Mean Diffusivity (MD), structural networks |
| DPARSF | Resting-State fMRI | Resting-state fMRI preprocessing & analysis | Resting-state fMRI | Functional connectivity, ALFF, ReHo |
Pipeline-Specific Methodologies and Protocols
CIVET: Cortical Morphometry Pipeline
The CIVET pipeline specializes in automated extraction of cortical surfaces and precise evaluation of cortical thickness from structural MRI data. Originally developed for human neuroimaging, it has been successfully extended for processing macaque brains, demonstrating its adaptability across species [37]. The processing is performed using the NIMH Macaque Template (NMT) as the reference template, with anatomical parcellation of the surface following the D99 and CHARM atlases [37]. This pipeline has been robustly applied to process anatomical scans of 31 macaques used to generate the NMT and an additional 95 macaques from the PRIME-DE initiative, confirming its scalability to substantial datasets [37]. The open usage of CIVET-macaque promotes collaborative efforts in data collection, processing, sharing, and automated analyses, advancing the non-human primate brain imaging field through methodological standardization.
CIVET Processing Workflow: From raw T1-weighted MRI to cortical thickness statistics.
PANDA: Automated Diffusion MRI Analysis
PANDA (Pipeline for Analyzing braiN Diffusion imAges) is a MATLAB toolbox designed for fully automated processing of brain diffusion images, addressing a critical gap in the streamlined analysis of white matter microstructure [38] [39]. The pipeline integrates processing modules from established packages including FMRIB Software Library (FSL), Pipeline System for Octave and Matlab (PSOM), Diffusion Toolkit, and MRIcron, creating a cohesive workflow that transforms raw diffusion MRI datasets into analyzable metrics [38] [39]. PANDA accepts any number of raw dMRI datasets from different subjects in either DICOM or NIfTI format and automatically performs a comprehensive series of processing steps to generate diffusion metrics—including fractional anisotropy (FA), mean diffusivity (MD), axial diffusivity (AD), and radial diffusivity (RD)—that are ready for statistical analysis at multiple levels [38]. A distinctive advantage of PANDA is its capacity for parallel processing of different subjects using multiple cores either in a single computer or in a distributed computing environment, substantially reducing computational time for large-scale studies [38] [39].
Table 2: PANDA Processing Modules and Functions
| Processing Stage | Specific Operations | Software Tools Utilized |
|---|---|---|
| Preprocessing | DICOM to NIfTI conversion, brain mask estimation, image cropping, eddy-current correction, tensor calculation | MRIcron (dcm2nii), FSL (bet, fslroi, flirt, dtifit) |
| Diffusion Metric Production | Normalization to standard template, voxel-level, atlas-level, and TBSS-level analysis ready outputs | FSL (fnirt) |
| Network Construction | Whole-brain structural connectivity mapping, deterministic and probabilistic tractography | Diffusion Toolkit, FSL |
The PANDA processing protocol follows three methodical stages. First, in preprocessing, DICOM files undergo conversion to NIfTI format using the dcm2nii tool, followed by brain mask estimation via FSL's bet command [38] [39]. The images are then cropped to remove non-brain spaces, reducing memory requirements for subsequent steps. Eddy-current-induced distortion and simple head motion are corrected by registering diffusion-weighted images to the b0 image using an affine transformation through FSL's flirt command, with appropriate rotation of gradient directions [38]. For studies involving multiple acquisitions, the corrected images are averaged before voxel-wise calculation of the tensor matrix and diffusion metrics using FSL's dtifit command. Second, for producing analysis-ready diffusion metrics, PANDA performs spatial normalization by non-linearly registering individual FA images to a standard FA template in MNI space using FSL's fnirt command, establishing the location correspondence necessary for cross-subject comparisons [38] [39]. Finally, the pipeline enables construction of anatomical brain networks through either deterministic or probabilistic tractography techniques, automatically generating structural connectomes for network-based analyses [38].
PANDA Workflow: Comprehensive processing of diffusion MRI from raw data to multiple analysis endpoints.
DPARSF: Resting-State fMRI Data Processing
DPARSF (Data Processing Assistant for Resting-State fMRI) addresses the critical need for user-friendly pipeline analysis of resting-state fMRI data, providing an accessible solution based on Statistical Parametric Mapping (SPM) and the Resting-State fMRI Data Analysis Toolkit (REST) [40] [41]. This MATLAB toolbox enables researchers to efficiently preprocess resting-state fMRI data and compute key metrics of brain function, including functional connectivity (FC), regional homogeneity (ReHo), amplitude of low-frequency fluctuation (ALFF), and fractional ALFF (fALFF) [40] [41]. The pipeline accepts DICOM files and, through minimal button-clicking parameter settings, automatically generates fully preprocessed data and analytical results, substantially simplifying the often complex workflow associated with resting-state fMRI analysis. DPARSF also creates quality control reports for excluding subjects with excessive head motion and generates visualization pictures for checking normalization effects, features that are essential for maintaining data quality in both single-site studies and large-scale multi-center investigations [40].
The DPARSF protocol encompasses comprehensive preprocessing and analytical stages. After converting DICOM files to NIfTI format using the dcm2nii tool, the pipeline typically removes the first 10 time points to allow for signal equilibrium [41]. Slice timing correction addresses acquisition time differences between slices, followed by head motion correction to adjust the time series of images so the brain maintains consistent positioning across all acquisitions [41]. DPARSF creates a report of head motion parameters to facilitate the exclusion of subjects with excessive movement. Spatial normalization then transforms individual brains into standardized Montreal Neurological Institute (MNI) space using either an EPI template or unified segmentation of T1 images, with the latter approach improving normalization accuracy [41]. The pipeline generates visualization pictures to enable researchers to check normalization quality for each subject. Subsequent smoothing with a Gaussian kernel suppresses noise and residual anatomical differences, followed by linear trend removal to eliminate systematic signal drifts [41]. For frequency-based analyses, bandpass filtering (typically 0.01-0.08 Hz) isolates low-frequency fluctuations of physiological significance while reducing high-frequency physiological noise [41]. The pipeline then computes key resting-state metrics: functional connectivity assesses temporal correlations between brain regions; regional homogeneity (ReHo) measures local synchronization using Kendall's coefficient of concordance; and ALFF/fALFF quantify the amplitude of spontaneous low-frequency oscillations [40] [41].
DPARSF Workflow: Automated processing of resting-state fMRI with integrated quality control.
The Scientist's Toolkit: Essential Research Reagent Solutions
Table 3: Key Research Reagents and Computational Resources
| Resource Name | Type | Primary Function | Compatibility/Requirements |
|---|---|---|---|
| FSL (FMRIB Software Library) | Software Library | Comprehensive MRI data analysis | Used by PANDA for diffusion processing |
| SPM (Statistical Parametric Mapping) | Software Package | Statistical analysis of brain imaging data | Core dependency for DPARSF |
| REST (Resting-State fMRI Data Analysis Toolkit) | Software Toolkit | Resting-state fMRI analysis | Integrated with DPARSF |
| NMT (NIMH Macaque Template) | Reference Template | Standard space for non-human primate data | Used by CIVET for macaque processing |
| D99 & CHARM Atlases | Parcellation Atlas | Anatomical labeling of brain regions | Surface parcellation in CIVET |
| MRIcron (dcm2nii) | Conversion Tool | DICOM to NIfTI format conversion | Used by both PANDA and DPARSF |
Comparative Analysis and Implementation Considerations
When selecting and implementing these fixed workflows, researchers must consider several practical aspects. Computational requirements represent a significant factor, with PANDA's support for parallel processing across multiple cores or computing clusters offering substantial efficiency gains for large diffusion MRI datasets [38] [39]. DPARSF similarly offers parallel computing capabilities when used with MATLAB's Parallel Computing Toolbox, dramatically reducing processing time for sizeable resting-state fMRI studies [40]. Quality control integration varies across pipelines, with DPARSF providing automated head motion reports and normalization quality visualizations [40] [41], while more recent frameworks like RABIES for rodent fMRI generate comprehensive quality control reports for registration operations and data diagnostics [42]. These quality assurance features are crucial for maintaining analytical rigor, particularly in large-scale studies or when combining datasets from multiple sites.
Flexibility within standardized workflows is another key consideration. While these pipelines offer fixed processing pathways, several provide configurable parameters—PANDA includes a friendly graphical user interface for adjusting input/output settings and processing parameters [38] [39], and DPARSF allows users to select different processing templates and analytical options [40]. This balance between standardization and configurability enables researchers to maintain methodological consistency while accommodating study-specific requirements. Implementation success also depends on proper data organization, with emerging standards like the Brain Imaging Data Structure (BIDS) being supported by modern pipelines such as RABIES to ensure compatibility and reproducibility [42]. For researchers working across multiple species, the adaptability of these pipelines is demonstrated by CIVET's extension to macaque data [37] and specialized implementations like RABIES for rodent imaging [42], highlighting the translatability of fixed workflow principles across model systems.
Fixed neuroimaging pipelines like CIVET, PANDA, and DPARSF represent transformative tools that standardize complex analytical processes across diverse MRI modalities. By providing automated, standardized workflows for cortical morphometry, white matter integrity, and resting-state brain function, these pipelines enhance methodological reproducibility, reduce processing errors, and accelerate the pace of discovery in brain imaging research. Their ongoing development and adaptation to new species, imaging modalities, and computational environments underscore the dynamic nature of neuroinformatics and its critical role in advancing neuroscience. For researchers and drug development professionals, mastering these fixed workflows offers the opportunity to generate more reliable, comparable, and scalable results, ultimately strengthening the foundation upon which our understanding of brain structure and function is built.
The complexity of modern brain imaging data necessitates robust, scalable, and reproducible analysis workflows. Flexible workflow environments address this need by enabling researchers to construct, validate, and execute customized processing protocols by linking together disparate neuroimaging software tools. These environments are crucial within a broader brain imaging data analysis research context as they facilitate methodologically sound, efficient, and transparent analyses, directly accelerating progress in neuroscience and drug development. This document provides detailed application notes and experimental protocols for three leading flexible workflow environments: LONI Pipeline, Nipype, and JIST. By summarizing their capabilities, providing direct comparative data, and outlining step-by-step methodologies, this guide aims to empower researchers and scientists to select and implement the optimal workflow solution for their specific research objectives.
Workflow Environment Comparison
Table 1: Comparative Overview of Flexible Workflow Environments
| Feature | LONI Pipeline | Nipype | JIST (Java Image Science Toolkit) |
|---|---|---|---|
| Primary Interface | Graphical User Interface (GUI) [43] | Python-based scripting [44] | Graphical User Interface (GUI) [43] |
| Tool Integration | Modules from AFNI, SPM, FSL, FreeSurfer, Diffusion Toolkit [43] | Interfaces for ANTs, SPM, FSL, FreeSurfer, AFNI, MNE, Camino, and many others [44] [45] | Modules from predefined libraries; allows linking of in-house modules [43] |
| Workflow Type | Flexible [43] | Flexible [43] | Flexible [43] |
| Parallel Computing | Supports multi-core systems, distributed clusters (SGE, PBS, LSF), grid/cloud computing [43] [46] | Parallel processing on multiple cores/machines [45] | Supports parallel computing on a single computer or across a distributed cluster [43] |
| Key Strength | User-friendly GUI; strong provenance tracking; decentralized grid computing [43] [46] | Unprecedented software interoperability in a single workflow; high flexibility and reproducibility [45] | Intuitive GUI for workflow construction; surface reconstruction workflows [43] |
Detailed Environment Specifications
LONI Pipeline
LONI Pipeline is a distributed, grid-enabled environment designed for constructing complex scientific analyses. Its architecture separates the client interface from backend computational servers, allowing users to leverage remote computing resources and extensive tool libraries [46] [47]. A core strength is its data provenance model, which automatically records the entire history of data, workflows, and executions, ensuring reproducibility and facilitating the validation of scientific findings [46]. The environment includes a validation and quality control system that checks for data type consistency, parameter matches, and protocol correctness before workflow execution, with options for visual inspection of interim results [43].
Nipype
Nipype (Neuroimaging in Python) is a community-developed initiative that provides a unified, Python-based interface to a heterogeneous collection of neuroimaging software packages [45]. Its core design principle is to facilitate interaction between these packages within a single, seamless workflow. A key feature is its interface system, which encapsulates processing modules from existing software (e.g., SPM's realignment, FSL's BET) as consistent Python objects [44] [48]. These interfaces are then connected within workflows and nodes, enabling the construction of highly customized, reproducible analysis pipelines that can leverage parallel processing to speed up computation [48] [45].
JIST
JIST is a plugin for the MIPAV application that focuses on providing a user-friendly graphical interface for creating automated image processing workflows. It allows users to drag and drop modules from a predefined library to construct a complete analysis protocol [43]. A notable feature is its support for module creation, enabling researchers to extend the built-in library with their own custom processing tools [43]. JIST is particularly recognized for its implementations of advanced image processing techniques, such as the CRUISE pipeline for cortical reconstruction using implicit surface evolution [43].
Experimental Protocol: A Basic fMRI Processing Workflow with Nipype
The following protocol details the creation of a basic fMRI processing workflow using Nipype, encompassing preprocessing and first-level model estimation. This serves as a practical, reproducible example for researchers.
Research Reagent Solutions
Table 2: Essential Software and Tools for the Protocol
| Item | Function/Description |
|---|---|
| Python (v3.7+) | The underlying programming language for Nipype. |
| Nipype Library | Provides the workflow engine, interfaces, and node architecture. |
| SPM12 | Statistical Parametric Mapping software; used for realignment, smoothing, and statistical modeling. |
| DataGrabber Node | A Nipype interface to flexibly select input neuroimaging data based on parameters like subject ID. |
| DataSink Node | A Nipype interface for storing and organizing processed results in a specified directory structure. |
| fMRI Data | Input functional MRI data in NIfTI format, ideally from multiple runs/subjects. |
Step-by-Step Methodology
Environment Setup and Import Libraries Ensure Python, Nipype, and SPM12 are installed. Begin a Python script by importing the necessary Nipype components and standard libraries.
Define Preprocessing Workflow Nodes Create nodes for realignment and smoothing, configuring their parameters.
Define First-Level Modelling Workflow Nodes Create nodes for model specification, design, estimation, and contrast estimation.
Create and Configure the Master Workflow Integrate the preprocessing and modelling workflows with data input and output nodes.
Execute the Workflow and Generate Graph Run the workflow and generate a graph representation for provenance and documentation.
Workflow Visualization
The following diagram illustrates the structure and data flow of the Nipype workflow created in this protocol.
Figure 1: Data flow and structure of the Nipype fMRI processing workflow.
The integration of artificial intelligence (AI) and machine learning (ML) into brain imaging data analysis has revolutionized neuroscience research and clinical practice. This transformation is particularly evident in the domains of classification and segmentation, where deep learning models, including Convolutional Neural Networks (CNNs) and Recurrent Neural Networks (RNNs), are enabling unprecedented precision in analyzing complex neuroimaging data. Within broader brain imaging data analysis workflows, these technologies facilitate the automated identification of pathological features, precise delineation of anatomical structures, and mapping of neural connectivity patterns. The application of these methods is accelerating progress in understanding brain function, tracking disease progression, and developing novel therapeutic interventions, making them indispensable tools for researchers, scientists, and drug development professionals working with increasingly large and multimodal neuroimaging datasets.
Quantitative Performance of Deep Learning Models in Neuroimaging
Recent studies have demonstrated the exceptional capabilities of various deep learning architectures when applied to brain image analysis tasks, particularly in the detection and classification of brain tumors from Magnetic Resonance Imaging (MRI) data. The quantitative performance of these models provides critical insights for researchers selecting appropriate tools for their specific applications.
Table 1: Performance Metrics of Deep Learning Models in Brain Tumor Classification
| Model Architecture | Training Accuracy (%) | Testing Accuracy (%) | Precision | Recall | F1-Score | Specificity |
|---|---|---|---|---|---|---|
| Ensemble CNN | 95.61 | 96.72 | ~0.96 | ~0.96 | ~0.96 | >0.98 |
| Vision Transformer (ViT) | 98.42 | 96.72 | ~0.96 | ~0.96 | ~0.96 | >0.98 |
| MobileNetV2 | 99.80 | 97.48 | ~0.97 | ~0.97 | ~0.97 | >0.98 |
| VGG16 | 99.36 | 98.78 | ~0.98 | ~0.98 | ~0.98 | >0.98 |
| YOLOv7 | - | - | - | 0.813 | - | - |
Beyond classification performance, the YOLOv7 model demonstrated substantial capability in localization tasks with a box detection accuracy of 0.837 and a mean Average Precision (mAP) value of 0.879 at a 0.5 Intersection over Union (IoU) threshold [49]. These metrics highlight the evolving sophistication of deep learning approaches in handling complex neuroimaging tasks that require both identification and spatial delineation of pathological features.
Experimental Protocols and Methodologies
Protocol 1: Whole-Brain Connectome Analysis for Behavior Prediction
The following protocol outlines a systematic workflow for employing multi-modal MRI data and dynamical brain models to predict human behavior, enhancing traditional neuroimaging analysis through model-based approaches [50].
Table 2: Workflow Steps for Model-Based Brain-Behavior Prediction
| Step | Process | Key Details | Output |
|---|---|---|---|
| 1 | Multi-modal MRI Data Acquisition | Acquire T1-weighted, rsfMRI, and dwMRI scans using standardized protocols (e.g., HCP S1200 dataset) | Raw MRI data in DICOM/NIfTI format |
| 2 | MRI Data Processing | Perform inhomogeneous field/motion corrections, tissue segmentation, cortical rendering, and image registration using tools like FSL, FreeSurfer, ANTs, AFNI | Preprocessed structural and functional images |
| 3 | Brain Parcellation & Connectome Construction | Apply atlas-based parcellation (e.g., Schaefer 100, Harvard-Oxford 96); compute Structural Connectivity (SC) via tractography, Functional Connectivity (FC) via Pearson's correlation | SC and FC matrices for each subject |
| 4 | Dynamical Model Selection & Optimization | Select whole-brain dynamical models; optimize parameters by fitting simulated FC (sFC) to empirical FC (eFC); maximize Goodness-of-Fit (GoF) | Optimized model parameters, simulated BOLD signals |
| 5 | Feature Extraction for Machine Learning | Calculate connectome relationships: eSC vs. eFC (empirical feature), eFC vs. sFC (simulated feature) | Feature matrices for classification/regression |
| 6 | Machine Learning Application | Apply ML algorithms using empirical features, simulated features, and their combination for sex classification or prediction of cognitive/personality traits | Prediction models with performance metrics |
This model-based workflow represents a significant advancement over purely data-driven approaches, as it incorporates simulated data as an additional neuroimaging modality that captures brain features difficult to measure directly [50]. The integration of simulated connectome features has demonstrated improved prediction performance for sex classification and behavioral score prediction compared to using empirical features alone.
Protocol 2: Automated Brain Tumor Detection and Classification
This protocol details a comprehensive methodology for implementing deep learning models, specifically YOLOv7, for the detection and classification of brain tumors from MRI data [49].
Table 3: Workflow for MRI-Based Brain Tumor Classification Using YOLOv7
| Step | Process | Key Details | Output |
|---|---|---|---|
| 1 | Data Collection & Curation | Obtain brain MRI dataset with labeled images (e.g., Roboflow with 2870 images); ensure class balance: pituitary, glioma, meningioma, no tumor | Curated dataset with annotations |
| 2 | Image Preprocessing | Apply aspect ratio normalization; resize images; enhance tumor localization for bounding box-based detection | Preprocessed MRI images ready for model input |
| 3 | Model Selection & Configuration | Implement YOLOv7 architecture; configure parameters for medical imaging context; optional: compare with other models (VGG16, EfficientNet) | Configured model ready for training |
| 4 | Model Training | Train on annotated dataset; employ data augmentation techniques; monitor for overfitting with validation split | Trained model with learned weights |
| 5 | Performance Evaluation | Assess using recall, precision, box detection accuracy, mAP at IoU thresholds (0.5, 0.5-0.95) | Comprehensive performance metrics |
| 6 | Clinical Validation | Compare model predictions with radiologist assessments; analyze discordant cases | Validated model ready for deployment |
The YOLOv7 framework has demonstrated particular effectiveness in this domain, achieving a recall score of 0.813 and a box detection accuracy of 0.837, with a mAP value of 0.879 at the 0.5 IoU threshold [49]. This balance of accuracy and efficiency makes it suitable for potential clinical implementation to support radiologists in analyzing brain tumors.
Workflow Visualization
The following diagrams illustrate key workflows described in the experimental protocols, providing visual representations of the complex processes involved in neuroimaging data analysis using AI and machine learning approaches.
Diagram 1: Model-Based Workflow for Brain-Behavior Prediction
Diagram 2: Deep Learning Pipeline for Brain Tumor Detection & Classification
The Scientist's Toolkit: Research Reagent Solutions
Successful implementation of AI and ML approaches for brain image classification and segmentation requires a comprehensive suite of computational tools, software frameworks, and data resources. The following table details essential components of the neuroimaging data analysis pipeline.
Table 4: Essential Research Reagents and Computational Tools for Neuroimaging AI
| Tool Category | Specific Tools/Platforms | Function in Workflow |
|---|---|---|
| Data Processing Platforms | Texera [51], Pypes [52], C-PAC, DPARSF | Collaborative data analytics; pre-processing pipelines for multimodal neuroimaging data; workflow management and reproducibility |
| Neuroimaging Software Libraries | SPM12, FSL, FreeSurfer, AFNI, ANTs, MRtrix3, PETPVC | Image registration, segmentation, normalization, bias field correction, tractography, partial volume correction |
| Programming Environments & ML Frameworks | Python, Nipype, TensorFlow, PyTorch, Scikit-Learn, Nilearn, Dipy | Workflow integration, deep learning model implementation, statistical analysis, specialized neuroimaging analysis |
| Computational Models & Architectures | VGG16 [53], YOLOv7 [49], Ensemble CNN [53], Vision Transformer [53], Whole-brain dynamical models [50] | Tumor classification, detection and localization, brain dynamics simulation, connectome-based prediction |
| Data Resources & Atlases | Human Connectome Project (HCP) [50], Schaefer Atlas, Harvard-Oxford Atlas [50], Roboflow MRI dataset [49] | Standardized datasets for model training and validation; brain parcellation templates for connectivity analysis |
This toolkit provides the foundational infrastructure for implementing the advanced AI and ML approaches described in this article. The integration of these components into cohesive workflows enables researchers to address complex challenges in brain image analysis, from precise tumor delineation to the prediction of cognitive and behavioral traits from neuroimaging data.
Advancements in brain imaging data analysis are revolutionizing the diagnosis, prognosis, and therapeutic assessment of neurological and psychiatric disorders. Moving beyond purely research-oriented applications, these technologies are increasingly being integrated into real-world clinical workflows. This integration is facilitated by the development of automated platforms, sophisticated machine learning models, and multimodal data fusion techniques. Framed within a broader thesis on brain imaging data analysis workflows, this article presents structured application notes and protocols detailing these clinical applications across Alzheimer's disease (AD), schizophrenia, and stroke assessment. The content is designed to provide researchers, scientists, and drug development professionals with actionable methodologies and comparative data.
Case Study 1: Alzheimer's Disease (AD) Assessment
Application Note: Deep Learning for Multi-Stage Classification
Clinical Challenge: Early and accurate diagnosis of Alzheimer's disease, including precise staging of its progression, is critical for timely intervention and patient management. Traditional methods often struggle with the subtle and continuous nature of neuroanatomical changes.
Solution: A novel Neuroimaging-based Early Detection of Alzheimer’s Disease using Deep Learning (NEDA-DL) framework demonstrates the power of hybrid deep learning models for superior classification performance [54]. This approach integrates structural and functional neuroimaging data to distinguish between multiple stages of AD with high precision.
Key Quantitative Results: The following table summarizes the performance of the NEDA-DL model in classifying AD stages [54].
Table 1: Performance of the NEDA-DL Model in Alzheimer's Disease Staging
| Model / Metric | Accuracy (%) | Sensitivity (%) | Specificity (%) | F1-Score (%) |
|---|---|---|---|---|
| NEDA-DL (Softmax) | 99.87 | 99.85 | 99.89 | 99.86 |
| Existing State-of-the-Art | < 99.00* | < 99.00* | < 99.00* | < 99.00* |
Note: Representative values indicating superior performance of NEDA-DL over existing methods cited in the study [54].
Experimental Protocol: Multi-Modal Neuroimaging Classification with NEDA-DL
Objective: To accurately classify a subject's brain scan into one of four AD categories: Non-Demented, Very Mild, Mild, or Moderate Alzheimer's disease using a hybrid deep learning model.
Materials & Reagents:
- Neuroimaging Data: T1-weighted Magnetic Resonance Imaging (MRI) and Positron Emission Tomography (PET) scans from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database [54].
- Software: Python environment with deep learning libraries (e.g., TensorFlow, PyTorch), and the NEDA-DL framework incorporating pre-trained ResNet-50 and AlexNet models [54].
Procedure:
- Data Preprocessing:
- Convert raw DICOM files to NIfTI format for compatibility.
- Perform skull-stripping to remove non-brain tissue.
- Apply spatial normalization to align all images to a standard template (e.g., MNI space).
- Execute intensity normalization to standardize voxel values across scans.
- For fMRI data used in other contexts, a processing toolkit like ABIDA can automate steps including slice timing correction, realignment, and nuisance covariate regression [55].
Model Implementation:
- Implement a hybrid architecture that fuses ResNet-50 and AlexNet.
- Utilize depthwise separable convolutions to reduce computational complexity.
- Employ CUDA-based parallel processing to accelerate model training and inference.
Training & Validation:
- Partition the dataset into training, validation, and test sets (e.g., 70:15:15 ratio).
- Train the model on preprocessed MRI and PET data using labeled data across the four stages.
- Use a cross-entropy loss function and an Adam optimizer.
- Validate model performance on the held-out test set using metrics in Table 1.
Logical Workflow: The diagram below illustrates the sequential and parallel steps in the NEDA-DL protocol.
Case Study 2: Schizophrenia Subtyping
Application Note: Data-Driven Neuroanatomical Subtyping
Clinical Challenge: Schizophrenia is a highly heterogeneous disorder with diverse clinical presentations and treatment responses. Symptom-based classification systems have limited biological validity and poor predictive power for outcomes.
Solution: Unbiased machine learning algorithms applied to structural MRI (sMRI) data can identify robust neuroanatomical subtypes independent of traditional symptom-based frameworks [56]. These data-driven biotypes align with variations in disease progression, cognitive function, and treatment outcomes, offering a path toward precision psychiatry.
Key Quantitative Results: The table below compares the diagnostic accuracy of different machine learning models using structural neuroimaging data for schizophrenia [56].
Table 2: Machine Learning Classification Accuracy for Schizophrenia Using sMRI
| Model Type | Reported Accuracy Range (%) | Key Features |
|---|---|---|
| Traditional Multivariate Models | 73.6 - 83.1 | Cortical thickness, subcortical volume |
| 3D Convolutional Neural Networks (3D-CNN) | 86.7 - 87.2 | Automated 3D spatial feature learning |
| Ensemble Deep Learning (Multimodal) | > 85.0 (representative) | Fusion of sMRI and fMRI features [57] |
Experimental Protocol: sMRI-Based Subtyping with Machine Learning
Objective: To identify distinct neuroanatomical subtypes of schizophrenia from structural MRI data using unsupervised clustering or supervised deep learning models.
Materials & Reagents:
- Imaging Data: High-resolution T1-weighted sMRI scans from cohorts like the ENIGMA-Schizophrenia consortium [56].
- Software: Machine learning libraries (e.g., Scikit-learn, PyTorch), neuroimaging processing tools (e.g., Freesurfer for cortical parcellation, DPABI/ABIDA for VBM preprocessing [56] [55]).
Procedure:
- Feature Extraction:
- Process sMRI data to extract quantitative features. This can involve:
- Cortical Parcellation: Calculating cortical thickness and surface area for predefined brain regions.
- Voxel-Based Morphometry (VBM): Measuring gray matter volume, concentration, or density on a voxel-wise basis.
- Process sMRI data to extract quantitative features. This can involve:
Model Training & Subtyping:
- For Unsupervised Clustering (Biotyping):
- Apply algorithms such as k-means or Gaussian Mixture Models to the extracted neuroanatomical features.
- Determine the optimal number of clusters using metrics like the silhouette score.
- For Supervised Classification (Diagnostic Aid):
- Train a 3D-CNN model directly on the sMRI volumes to distinguish schizophrenia patients from healthy controls, or to classify predefined subtypes.
- Use data augmentation techniques to increase model generalizability.
- For Unsupervised Clustering (Biotyping):
Validation & Correlation:
- Validate the identified subtypes by correlating them with external clinical variables (e.g., symptom severity, cognitive test scores, treatment response).
- Test the generalizability of the model on an independent, held-out dataset.
Logical Workflow: The diagram below outlines the key decision points in a schizophrenia subtyping pipeline.
Case Study 3: Post-Stroke Outcome Prediction
Application Note: Automated Prognostication from Clinical Scans
Clinical Challenge: Predicting long-term functional and cognitive outcomes after stroke is difficult but essential for personalizing rehabilitation and managing patient expectations. Current clinical methods often lack precision.
Solution: A fully automated, three-stage neuroimaging processing and machine learning pipeline can rapidly generate personalized prognostic reports from routine clinical imaging [58]. This platform integrates lesion location, network disruption features, and demographic data to predict chronic impairment.
Key Quantitative Results: The platform's performance in a proof-of-concept study is summarized below [58].
Table 3: Performance of an Automated Stroke Outcome Prediction Pipeline
| Pipeline Feature | Performance Metric | Result |
|---|---|---|
| Processing Speed | Time from DICOM to Report | < 3 minutes |
| Lesion Segmentation | Concordance with Manual Processing | 96% |
| Outcome Prediction | Accuracy (Enhanced vs. Basic Model) | Significantly Enhanced* |
Note: Models incorporating lesion location, network features, and demographics showed improved prediction accuracy compared to basic models [58].
Experimental Protocol: Automated Post-Stroke Cognitive Impairment (PSCI) Prediction
Objective: To automatically process a clinical MRI from an ischemic stroke patient and predict the risk of developing post-stroke cognitive impairment (PSCI).
Materials & Reagents:
- Imaging Data: Raw DICOM files from clinical MRI sequences (e.g., DWI, T2-FLAIR) acquired during acute stroke workup [58].
- Biomarker Data (Optional): Blood samples for analyzing potential blood-based biomarkers like Neurofilament Light Chain (NfL) or Brain-Derived Tau [59].
- Software: Automated pipeline software (e.g., as described in [58]), which includes deep learning models for lesion segmentation and pre-trained statistical models for outcome prediction.
Procedure:
- Automated Lesion Detection and Segmentation:
- Input raw DICOM files into the pipeline.
- The system automatically registers the brain to a standard template.
- A deep learning model segments the ischemic stroke lesion.
Feature Extraction for Prediction:
- Extract features from the segmented lesion, including:
- Lesion Location: Map the lesion to a standardized brain atlas.
- Network Disruption: Calculate measures of disconnection in functional or structural brain networks caused by the lesion.
- Extract features from the segmented lesion, including:
Outcome Prediction and Report Generation:
- Input the extracted lesion and network features, along with basic demographics (e.g., age, sex), into pre-trained statistical models. These models are trained on large, independent cohorts to predict long-term outcomes on specific cognitive domains.
- The pipeline automatically generates a structured PDF report using a large language model, summarizing the lesion location, arterial territory, and personalized prognostic estimates.
Logical Workflow: The integrated workflow for stroke outcome prediction, including potential biomarker integration, is shown below.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Tools and Resources for Neuroimaging Data Analysis Workflows
| Tool/Resource | Type | Primary Function | Example Use Case |
|---|---|---|---|
| ABIDA Toolbox [55] | Software | Automated preprocessing and analysis of resting-state fMRI data. | Simplifies calculation of ALFF, ReHo, and functional connectivity metrics for clinical researchers. |
| ADNI Dataset [54] | Data | Curated, multi-modal neuroimaging dataset. | Provides standardized MRI and PET data for training and validating AD detection models. |
| ResNet-50 / AlexNet [54] | Algorithm | Pre-trained deep learning architectures. | Used as a backbone for transfer learning in neuroimaging classification tasks (e.g., NEDA-DL). |
| 3D Convolutional Neural Network [56] | Algorithm | Deep learning model for 3D volumetric data. | Direct classification of sMRI volumes for schizophrenia diagnosis or subtyping. |
| ENIGMA Consortium Tools [56] | Software & Protocols | Standardized protocols for ROI-based analysis. | Enables large-scale, multi-site analysis of cortical thickness and subcortical volumes. |
| Blood-Based Biomarkers (NfL, BD-tau) [59] | Biochemical Assay | Serum/plasma biomarkers of neuronal injury. | Provides a minimally invasive method to predict and monitor Post-Stroke Cognitive Impairment (PSCI). |
Overcoming Hurdles: Ensuring Efficiency and Scalability
The advent of large-scale, open-source neuroimaging datasets has revolutionized brain science, enabling investigations with unprecedented rigor and statistical power [60]. However, this data deluge presents significant computational bottlenecks and storage challenges that can impede research progress. The maturation of in vivo neuroimaging has positioned it at the leading edge of "big data" science, with datasets growing in size and complexity [61]. This application note examines these challenges within brain imaging data analysis workflows and provides practical solutions for researchers, scientists, and drug development professionals navigating this complex landscape. Effective management of these large datasets is crucial for advancing our understanding of brain function in both health and disease.
The Scale of Neuroimaging Data
Neuroimaging data has experienced exponential growth in recent decades, with dataset sizes doubling approximately every 26 months [61]. This expansion is driven by technological advances across multiple imaging modalities that have increased both spatial and temporal resolution.
Table 1: Neuroimaging Data Specifications Across Modalities
| Data Type | Representative Size per Participant | Primary Factors Driving Size | 10,000-Participant Study |
|---|---|---|---|
| Structural MRI | ~100-500 MB | Voxel resolution, contrast weightings | ~1-5 TB |
| Functional MRI (BOLD) | ~500 MB - 5 GB | Temporal resolution, sequence duration, multiband acceleration | ~5-50 TB |
| Diffusion Tensor Imaging (DTI) | ~1-10 GB | Number of diffusion directions, b-values, spatial resolution | ~10-100 TB |
| Multimodal Imaging | ~1-15 GB | Combination of multiple sequences | ~10-150 TB |
The challenges extend beyond mere storage requirements. For example, the Adolescent Brain Cognitive Development (ABCD) dataset contains raw neuroimaging data requiring approximately 1.35 GB per individual, totaling ~13.5 TB for the initial release of ~10,000 individuals [60]. This estimate excludes the additional space needed for intermediate files during processing, quality control, and final results, which can substantially increase total storage requirements.
Computational Bottlenecks in Processing Pipelines
Processing Time and Resource Requirements
The computational demands of processing large neuroimaging datasets present significant bottlenecks. In practical experience, it can take 6-9 months for two to three researchers to download, process, and prepare data from large-scale studies for analysis [60]. This timeline includes:
- Downloading DICOM data (which can take weeks)
- Converting to NIfTI format (additional weeks)
- Skull-stripping anatomical images
- Registering images to common space
- Motion-correcting functional images
- Performing comprehensive quality control
Memory and Processing Constraints
As dataset sizes increase, traditional processing approaches encounter memory limitations that necessitate specialized computational strategies. Large-scale volumetric data, such as that from mouse brain mapping studies, requires specialized processing pipelines for tasks like image stitching and 3D reconstruction [62]. These processes demand substantial RAM and efficient memory management to handle high-resolution images that exceed system memory capacity.
Storage Infrastructure Solutions
Storage Architecture Considerations
Effective storage solutions for large neuroimaging datasets require careful planning and consideration of multiple factors:
Table 2: Storage Solution Comparisons for Neuroimaging Data
| Storage Type | Capacity Requirements | Advantages | Limitations | Use Cases |
|---|---|---|---|---|
| Local Storage | ~10-100 TB | Fast access, full control | High upfront costs, maintenance overhead | Individual labs, sensitive data |
| Cloud Storage | Scalable | Flexibility, accessibility, integrated processing | Ongoing costs, data transfer time | Multi-site collaborations, burst processing |
| Hybrid Solutions | Variable | Balance of control and scalability | Increased management complexity | Most research scenarios |
| Tiered Storage | Optimized by usage | Cost-effective for archival data | Retrieval latency for cold storage | Long-term data preservation |
When planning storage infrastructure, researchers must account for backup needs, which typically double the total storage requirement [60]. Strategic decisions about which intermediate files to backup can optimize costs while maintaining data integrity.
Raw vs. Processed Data Tradeoffs
A critical decision point involves choosing between storing raw versus processed data:
- Raw Data: Requires substantial storage (~TB scale for large studies) but preserves flexibility in preprocessing choices and enables custom analytical approaches [60]
- Processed Data: Dramatically reduces storage requirements (often by orders of magnitude) but locks researchers into predefined preprocessing decisions
For example, preprocessed connectivity matrices from the ABCD study require only ~25.6 MB of disk space—approximately 0.0001% of the space needed for raw NIfTI images and intermediate files [60]. This substantial reduction comes at the cost of analytical flexibility.
Experimental Protocol: Optimized Large-Scale Image Processing
Texera Pipeline for 3D Brain Reconstruction
The following protocol details an optimized pipeline for processing large-scale brain imaging data, adapted from a recent study demonstrating significant performance improvements [62]:
Materials and Reagents
- TissueCyte or serial two-photon tomography system
- Agarose (4% oxidized) for sample embedding
- Surecast solution (Acrylamide:Bis-acrylamide ratio of 29:1)
- VA-044 activator
- Phosphate buffer (1× PB) with 0.01% sodium azide
- Paraformaldehyde (4% PFA) for fixation
Procedure
- Sample Preparation
- Perform transcardial perfusion with 1× PBS followed by 4% PFA
- Post-dissection, fix mouse brains overnight at 4°C in 4% PFA
- Transfer to 1× PB solution with 0.01% sodium azide until imaging
Embedding and Sectioning
- Embed samples in 4% oxidized agarose solution
- Immerse in Surecast solution (4.5% Surecast + 0.5% VA-044 activator in 1× PB) at 4°C overnight
- Bake agarose-embedded brain at 40°C for 2 hours
- Return to 1× PB for overnight soaking before imaging
Image Acquisition
- Secure agarose-embedded brain on glass slide with adhesive
- Image using TissueCyte with 16× objective (FOV: 1,125 μm × 1,125 μm)
- Acquire ~11 × 14 tiles per color channel for each optical section
- Image one optical section 40 μm below surface before sectioning
Computational Processing on Texera Platform
- Apply deformation correction to individual tiles
- Perform brightness normalization to ensure uniform intensity values
- Execute optimized tile stitching algorithm
- Stack 2D sections to construct 3D whole-brain volume
- Render final brain data in 3D using Neuroglancer
Performance Optimization
- Implementation of specialized optimization methods reduces total processing time to 2.5 hours for a whole brain spanning 280 sections
- This represents >80% time reduction compared to non-optimized approaches and ~30% reduction compared to traditional parallel approaches [62]
Workflow Visualization
Figure 1: Optimized computational workflow for large-scale brain image processing
Collaborative Data Management Platforms
Platform Comparisons
Several specialized platforms have emerged to address the challenges of neuroscience data management, sharing, and analysis:
Table 3: Neuroscience Data Management Platforms
| Platform | Primary Focus | Data Standards | Unique Features | Scale |
|---|---|---|---|---|
| Pennsieve | FAIR data management and collaboration | BIDS, custom | Open-source, cloud-based, integrated visualization tools | 125+ TB, 350+ datasets |
| Brain-CODE | Multi-dimensional data across brain conditions | Common Data Elements (CDEs) | Federated data integration, virtual workspaces | Multi-site consortia |
| DANDI | Neurophysiology data sharing and analysis | NWB | JupyterHub interface, data streaming functionality | BRAIN Initiative archive |
| OpenNeuro | Free and open data sharing | BIDS | Minimal access restrictions, partnership with analysis platforms | Multiple modalities |
| brainlife.io | Reproducible neuroimaging analysis | Standardized 'Datatype' format | Application workflows, shared computational resources | Publicly funded |
These platforms share a commitment to the FAIR principles (Findable, Accessible, Interoperable, and Reusable), though they implement these principles to varying degrees [63]. Platforms like Pennsieve serve as the core for several large-scale, interinstitutional projects and major government neuroscience research programs, highlighting their importance in contemporary neuroinformatics [63].
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents for Large-Scale Brain Mapping
| Reagent/Resource | Function | Application Context | Specifications |
|---|---|---|---|
| TissueCyte/STPT System | Automated block-face imaging and sectioning | 3D whole-brain reconstruction | 16× objective, 1,125 μm × 1,125 μm FOV |
| Oxidized Agarose (4%) | Sample embedding medium | Tissue stabilization for imaging | Provides structural support during sectioning |
| Surecast Solution | Polymer matrix for embedding | Tissue integrity preservation | 29:1 Acrylamide:Bis-acrylamide ratio |
| VA-044 Activator | Polymerization initiator | Embedding process | Used at 0.5% concentration in Surecast solution |
| AAV Viral Tracers | Specific cell type labeling | Neural circuit mapping | e.g., AAV8-DIO-TC66T-2A-eGFP-2A-oG |
| Engineered Rabies Virus | Monosynaptic input mapping | Connectomics studies | EnvA-RV-SADΔG-DsRed for retrograde tracing |
| Texera Platform | Collaborative data analytics | Large-scale image processing | Enables interdisciplinary team collaboration |
| Neuroglancer | Volumetric data visualization | 3D brain data exploration | Web-based tool for high-resolution rendering |
Visualization and Analysis Tools for Large Datasets
Programmatic Visualization Approaches
Traditional GUI-based visualization tools become impractical with large datasets, making programmatic approaches essential [64]. Code-based visualization tools provide:
- Replicability: Establishing a direct link between data and figures [64]
- Flexibility: Streamlining workflow through reprogrammable inputs and settings [64]
- Scalability: Enabling iteration across thousands of images for quality control [64]
- Integration: Embedding visualizations directly within computational notebooks and reports [64]
Notable tools include NWB Widgets for exploring Neurodata Without Borders files, Suite2p for calcium imaging analysis, and DeepLabCut for markerless pose estimation [65]. These tools enable researchers to handle the visualization demands of large-scale datasets that would be infeasible with manual approaches.
Effective Visualization Principles
When creating visualizations for large neuroimaging datasets, several principles enhance effectiveness:
- Diagram First: Prioritize information to share before engaging with software [66]
- Select Appropriate Geometry: Match visualization types to data characteristics (amounts, distributions, relationships) [66]
- Maximize Data-Ink Ratio: Prioritize ink used for data over non-data elements [66]
- Ensure Color Accessibility: Maintain sufficient contrast ratios (≥4.5:1 for normal text, ≥3:1 for large text and graphical elements) [67] [68]
These principles help create visualizations that accurately and effectively communicate complex data patterns in large neuroimaging datasets.
Addressing the computational bottlenecks and storage challenges in neuroimaging "big data" requires integrated solutions spanning infrastructure, software, and methodology. The approaches outlined in this application note—from optimized processing pipelines and strategic storage architectures to collaborative data platforms and programmatic visualization—provide researchers with practical frameworks for managing large-scale brain imaging data. As neuroscience continues to generate increasingly large and complex datasets, embracing these solutions will be crucial for advancing our understanding of brain function and facilitating drug development efforts. The future of neuroimaging research depends on robust, scalable, and collaborative approaches to data management and analysis.
The expansion of large-scale neuroimaging datasets represents a paradigm shift in neuroscience, enabling the investigation of brain structure and function at an unprecedented scale and level of detail [23] [69]. Initiatives such as the Human Connectome Project, the UK Biobank, and the Brain Imaging and Neurophysiology Database (BIND) provide researchers with petabytes of imaging data, offering powerful resources to identify biomarkers and understand neurological disorders [23] [69]. However, this data abundance introduces significant statistical challenges that can undermine the validity and reliability of research findings if not properly addressed.
The analysis of large neuroimaging datasets inherently involves navigating three interconnected statistical pitfalls: low statistical power, multiple comparisons, and irreproducible findings. These challenges are particularly acute in neuroimaging due to the large number of dependent variables (voxels or connections), typically small sample sizes relative to these variables, and the complex, multi-stage processing pipelines required for data analysis [23] [70]. As the field moves toward larger datasets and more complex analytical approaches, understanding and mitigating these pitfalls becomes essential for generating scientifically valid and clinically meaningful results.
This application note examines these critical statistical challenges within the context of brain imaging data analysis workflows. We provide a structured analysis of each pitfall, present quantitative comparisons of their impact, detail experimental protocols for mitigation, and visualize key analytical workflows. By addressing these fundamental methodological issues, we aim to support researchers, scientists, and drug development professionals in conducting more robust and reproducible neuroimaging research.
Statistical Power in Neuroimaging Studies
The Power Problem: Definition and Status
Statistical power refers to the probability of correctly rejecting the null hypothesis when it should be rejected – that is, the likelihood of detecting a true effect when it exists [70]. In neuroimaging, the combination of a large number of dependent variables, relatively small numbers of observations, and stringent multiple comparison corrections dramatically reduces statistical power, particularly for between-subjects effects such as group comparisons and brain-behavior correlations [70].
Empirical assessments reveal a severe power crisis in neuroscience. Studies estimate the median statistical power in neurosciences falls between approximately 8% and 31% [71]. This fundamentally undermines research reliability, as underpowered studies not only reduce the chance of detecting true effects but also decrease the likelihood that a statistically significant result reflects a true effect [71]. The consequences include inflated effect size estimates and low reproducibility of results, creating ethical dimensions to the problem as unreliable research is inefficient and wasteful [71].
Table 1: Statistical Power in Common Neuroimaging Study Designs
| Study Design | Typical Sample Size | Median Power | Primary Limitations | Recommended Sample Size |
|---|---|---|---|---|
| Single Graph Metric | 30-50 | ~31% | Inadequate for subtle effects | 100+ |
| Multiple Graph Metrics | 30-50 | 8-20% | Multiple testing burden | 150+ |
| Edge-Level Connectivity (NBS) | 30-50 | <10% | Extreme multiple comparisons | 200+ |
| Brain-Behavior Correlation | 20-30 | <20% | High dimensionality | 150+ |
In brain connectivity investigations, power varies substantially depending on the analytical approach. An informal survey of 1,300 case-control brain connectivity studies published between 2019-2022 revealed particularly low power for edge-level analyses using network-based statistics (NBS), where power falls below 10% with typical sample sizes of 30-50 participants [72]. This differential power across network features can introduce structural biases in connectome research, making some connections or network properties systematically easier to detect than others [72].
Factors Influencing Statistical Power
Statistical power in neuroimaging is shaped by several interconnected factors, with sample size, effect size, and measurement reliability playing predominant roles. The relationship between these factors is complex, particularly in network neuroscience where power varies across different parts of the network [72].
Sample size exerts the most direct influence on power, with larger samples increasing the likelihood of detecting true effects. However, the required sample sizes for adequate power in neuroimaging are often substantially larger than those conventionally used. For brain-wide association studies, samples numbering in the thousands may be necessary for robust detection of subtle effects [72] [70].
Effect size presents particular challenges in neuroimaging research. Effects that achieve statistical significance in underpowered studies tend to overestimate true effect sizes due to publication bias and the winner's curse phenomenon [71] [70]. This inflation is more severe when statistical power is lower, creating a vicious cycle where underpowered studies produce exaggerated effect sizes that in turn lead to continued underpowered study designs based on inaccurate a priori power calculations [71].
Measurement error introduced by scanner variability, preprocessing pipelines, and physiological noise further diminishes power by adding noise to the measurements [72]. As neuroimaging data moves toward multi-site collaborations to increase sample sizes, site effects and protocol differences introduce additional variance that must be carefully managed through harmonization techniques [23].
Table 2: Factors Affecting Statistical Power in Neuroimaging
| Factor | Impact on Power | Management Strategies |
|---|---|---|
| Sample Size | Direct positive correlation | Multi-site collaborations; Public datasets; Prioritize sample size over number of variables |
| Effect Size | Direct positive correlation | Report realistic effect sizes from pilot studies/published literature; Focus on clinically relevant effects |
| Measurement Error | Inverse relationship | Protocol standardization; Improved preprocessing; Harmonization methods (e.g., ComBat) |
| Multiple Comparison Correction | Inverse relationship | A priori hypotheses; ROI analyses; Multivariate methods; Appropriate correction thresholds |
Multiple Comparisons and False Discovery Control
The Multiple Comparisons Problem in Neuroimaging
The multiple comparisons problem represents a fundamental challenge in neuroimaging analysis, where hundreds of thousands of statistical tests are conducted simultaneously across voxels, connections, or network features. Failure to adequately address this problem results in unacceptably high rates of false positive findings, while overly stringent correction can render studies incapable of detecting genuine effects [70].
In whole-brain voxel-wise fMRI analyses, the number of independent tests often runs into the hundreds of thousands while the number of observations remains relatively low (typically 15-30 subjects) [70]. Without appropriate correction, this combination guarantees a high false positive rate. However, the stringent thresholds necessary to control family-wise error rates dramatically reduce statistical power, creating a fundamental tension between false positive control and detection sensitivity [70].
The problem manifests differently across neuroimaging approaches. In mass univariate analyses (e.g., voxel-based morphometry, task-based fMRI), the challenge involves correcting across spatial elements [73]. In network neuroscience, the multiple comparisons problem extends to connections (edges), network properties, and nodal characteristics, creating complex dependency structures that complicate correction procedures [72]. Functional connectivity studies face particular challenges as they often examine thousands of connections simultaneously, requiring extremely conservative thresholds to control the false discovery rate across the entire connectome [72].
Multiple Comparison Correction Strategies
Various statistical approaches have been developed to address the multiple comparisons problem in neuroimaging, each with distinct strengths, limitations, and appropriate application contexts.
Traditional family-wise error rate (FWER) controls, such as Bonferroni correction, provide strong control over false positives but are often excessively conservative for neuroimaging data, where tests exhibit spatial dependencies. Random field theory offers a less conservative alternative that accounts for smoothness in imaging data but requires specific assumptions about the spatial properties of the data [72].
False discovery rate (FDR) methods control the expected proportion of false positives among significant findings, offering a more balanced approach between false positive control and statistical power. FDR approaches are particularly valuable in exploratory analyses or when prior evidence supports the presence of widespread effects [72].
Network-based statistics (NBS) provides a cluster-based approach for connectome-wide analyses, examining connected components rather than individual connections. This method enhances power for detecting network-level effects but may miss specific isolated connections and requires careful threshold selection [72].
Multivariate methods, including canonical correlation analysis and machine learning approaches, offer an alternative framework by combining information across multiple variables, thereby reducing the multiple comparisons burden. These methods can capture complex, distributed patterns but may sacrifice spatial specificity and require independent validation to ensure generalizability [72].
Reproducibility Challenges and Solutions
The Reproducibility Crisis in Neuroimaging
Reproducibility represents a critical challenge in neuroimaging research, with many published findings failing to replicate in independent samples [71]. This reproducibility crisis stems from multiple factors, including low statistical power, analytical flexibility, publication bias, and inadequate methodological reporting [71] [23].
The combination of low power and analytical flexibility creates particular vulnerabilities. When power is low, statistically significant results are more likely to represent inflated estimates of true effects [71]. When researchers employ analytical flexibility—making seemingly arbitrary choices in preprocessing, statistical modeling, or significance testing—they increase the likelihood of obtaining publishable but non-reproducible results [71]. This problem is exacerbated by publication bias, where studies with positive findings are more likely to be published than those with null results [71].
Methodological reporting represents another critical dimension of the reproducibility challenge. A review of methods reporting in fMRI literature found nearly as many unique analytical pipelines as there were studies, with many studies underpowered to detect plausible effects [71]. Inadequate reporting of effect estimates represents a specific reporting failure that damages the reliability and interpretability of neuroimaging findings [73]. The field has traditionally emphasized reporting statistical values (t- or z-values) while neglecting the effect estimates (β values) that provide information about the actual magnitude of brain responses [73].
Infrastructure for Reproducible Neuroimaging
Addressing reproducibility challenges requires both methodological rigor and infrastructural support. Several initiatives and platforms have emerged to facilitate reproducible neuroimaging research through data standardization, open tools, and collaborative frameworks.
The Brain Imaging Data Structure (BIDS) provides a standardized framework for organizing and describing neuroimaging datasets, defining imaging formats, parameters, and file naming conventions to support automated analysis and reproducibility [74] [75]. BIDS has been extended to encompass various imaging modalities, including recently introduced specifications for magnetic resonance spectroscopy (MRS-BIDS) [75]. This standardization facilitates data sharing and interoperability across research groups and analytical platforms.
The Brain Imaging and Neurophysiology Database (BIND) represents one of the largest multi-institutional, multimodal neuroimaging repositories, comprising 1.8 million brain scans from 38,945 subjects linked to neurophysiological recordings [69]. Such large-scale resources enable robust validation of findings across diverse populations and scanning platforms, directly addressing power limitations and enhancing reproducibility.
Neurodesk offers a containerized data analysis environment that facilitates reproducible analysis by ensuring tool compatibility and version control across computing environments [26]. By providing on-demand access to a comprehensive suite of neuroimaging tools within standardized containers, Neurodesk addresses the "dependency hell" problem that often undermines computational reproducibility [26].
Reproducible Neuroimaging Workflow. This diagram visualizes a standardized workflow for reproducible neuroimaging research, incorporating BIDS conversion, standardized preprocessing, analysis with effect size reporting, and data sharing.
Experimental Protocols and Methodologies
Power Analysis Protocol for Neuroimaging Studies
Conducting an appropriate power analysis represents an essential first step in designing robust neuroimaging studies. The following protocol outlines a comprehensive approach to power calculation for common neuroimaging study designs.
Protocol 1: A Priori Power Analysis for fMRI Studies
Effect Size Estimation: Derive realistic effect size estimates from pilot data, meta-analyses, or published literature in comparable populations. For novel investigations, consider using conservative estimates (e.g., Cohen's d = 0.3-0.5 for between-group differences) to account for potential inflation in published effect sizes [71] [70].
Power and Alpha Threshold Specification: Set desired power to at least 80-90% and alpha to 0.05, corrected for multiple comparisons. For whole-brain analyses, incorporate the expected number of independent tests based on simulation studies or previous work [70].
Sample Size Calculation: Use specialized power analysis software (e.g., G*Power, fMRIpower, neuropower) to determine required sample sizes. For complex designs (e.g., longitudinal, multi-site), consider simulation-based approaches that account for expected attrition and site variance [71].
Multiple Comparison Adjustment: Incorporate the multiple comparison correction strategy into power calculations. For FWE-corrected whole-brain analyses, use random field theory-based power estimators. For ROI-based analyses, adjust for the number of regions examined [72] [70].
Sensitivity Analysis: Conduct sensitivity analyses to determine the smallest detectable effect given practical sample size constraints. Report this minimal detectable effect alongside study results to contextualize null findings [70].
Validation and Reporting: Document all power analysis parameters, assumptions, and software implementations. For grant applications, include justification for sample size based on formal power calculations rather than convention or resource constraints alone.
Effect Size Estimation and Reporting Protocol
Accurate reporting of effect sizes is essential for interpretation, meta-analysis, and future power calculations. This protocol establishes guidelines for comprehensive effect size reporting in neuroimaging studies.
Protocol 2: Effect Size Estimation and Reporting
Effect Estimate Extraction: For each significant finding, extract and report the unstandardized effect estimate (e.g., β values from GLM analyses, correlation coefficients for functional connectivity) alongside corresponding statistical values (t-, z-, or F-values) [73].
Unit-Bearing Metrics: Express effect estimates in meaningful physical units where possible. For BOLD fMRI, convert β values to percent signal change to facilitate interpretation and cross-study comparison [73].
Standardized Effect Sizes: Calculate standardized effect sizes (e.g., Cohen's d, partial η²) for key comparisons to support meta-analytic efforts. Provide formulas or computational methods used for these conversions [73].
Confidence Intervals: Report confidence intervals (typically 95%) for all effect size estimates to communicate precision and uncertainty. Use bias-corrected methods when appropriate, particularly for small sample sizes [73].
Spatial Extent Documentation: For cluster-based inferences, report both peak and mean effect sizes within significant clusters or regions. Document the spatial distribution of effects to support interpretations of specificity and generality [73].
Implementation Considerations: Most neuroimaging software packages (SPM, FSL, AFNI) can be configured to output effect estimates alongside statistical maps. Custom scripts may be necessary for extracting and aggregating these values across significant regions.
Multiple Comparison Correction Protocol
Appropriate correction for multiple comparisons is essential for controlling false positive rates while maintaining reasonable sensitivity. This protocol outlines a systematic approach to multiple comparison correction in neuroimaging analyses.
Protocol 3: Multiple Comparison Correction Strategy Selection
Analysis Plan Specification: Pre-specify the multiple comparison correction method in the analytical plan, distinguishing between confirmatory and exploratory analyses. For confirmatory hypothesis-driven tests, use more stringent corrections (e.g., FWE); for exploratory analyses, consider FDR control [72] [70].
Correction Method Selection:
- For whole-brain voxel-wise analyses: Implement random field theory-based FWE correction or permutation testing [70].
- For ROI-based analyses: Use FWE correction across the number of predefined regions [72].
- For network edge analyses: Apply network-based statistics or FDR correction depending on the hypothesis [72].
Threshold Determination: Establish appropriate cluster-forming thresholds and extent thresholds based on simulation studies or methodological recommendations for the specific analytical approach [72].
Sensitivity Analysis: Conduct supplementary analyses with varying correction thresholds to demonstrate the robustness of findings. Report both corrected and uncorrected results with clear labeling [72].
Visualization and Reporting: Visualize results using standardized methods (e.g., glass brains, surface projections) that accurately represent corrected statistical maps. Clearly document all correction parameters in methods sections [72].
Validation Steps: For novel analytical pipelines, validate multiple comparison correction methods using null data to verify that false positive rates are appropriately controlled at the nominal level (e.g., 5%).
Multiple Comparisons Decision Framework. This diagram outlines a systematic protocol for selecting and implementing appropriate multiple comparison correction strategies in neuroimaging analyses.
Table 3: Research Reagent Solutions for Robust Neuroimaging
| Tool/Resource | Function | Application Context |
|---|---|---|
| BIDS Validator | Validates compliance with Brain Imaging Data Structure standards | Data organization and sharing; Ensures dataset completeness and metadata requirements |
| fMRIPrep | Automated preprocessing of fMRI data | Standardized pipeline for functional MRI preprocessing; Reduces analytical variability |
| Neurodesk | Containerized analysis environment | Reproducible computing environment; Tool version control; Cross-platform compatibility |
| ComBat | Harmonization of multi-site imaging data | Batch effect removal; Multi-site studies; Longitudinal analyses |
| BIND Database | Large-scale multimodal neuroimaging repository | Validation studies; Method development; Power enhancement through sample size |
| CAT12 | Computational anatomy toolbox for structural MRI | Voxel-based morphometry; Surface-based analysis; Tissue classification |
| dcm2niix | DICOM to NIfTI converter with BIDS sidecar generation | Data conversion; Metadata extraction; BIDS compatibility |
| FSL | FMRIB Software Library for MRI analysis | General MRI processing; Diffusion imaging; Functional connectivity |
| SPM | Statistical Parametric Mapping | Statistical analysis; Image processing; Computational anatomy |
The statistical challenges of power, multiple comparisons, and reproducibility represent interconnected pillars determining the validity of neuroimaging research. As the field continues to evolve toward larger datasets and more complex analytical approaches, addressing these fundamental methodological issues becomes increasingly critical. The protocols, resources, and frameworks presented in this application note provide actionable strategies for enhancing the rigor and reliability of brain imaging research.
Moving forward, the neuroimaging community must continue to develop and adopt practices that prioritize methodological robustness over expediency. This includes embracing large-scale collaborations, pre-registering analytical plans, implementing standardized processing pipelines, and comprehensively reporting both statistical values and effect estimates. By confronting these statistical pitfalls directly, researchers can fully leverage the potential of large neuroimaging datasets to generate meaningful insights into brain function and dysfunction, ultimately advancing both basic neuroscience and clinical applications.
Optimizing Pipeline Parallelization for Multi-Core and Distributed Computing
In brain imaging data analysis, the exponential growth of data volume and computational complexity presents significant challenges. Modern studies, particularly those involving large-scale datasets from initiatives like the Human Connectome Project, require processing of multi-modal magnetic resonance imaging (MRI) data including T1-weighted, resting-state functional MRI (rsfMRI), and diffusion-weighted MRI (dwMRI) [50]. Pipeline parallelization has emerged as a critical strategy for accelerating these workflows, enabling researchers to achieve throughput necessary for timely discovery. This approach decomposes complex analysis sequences into discrete stages that execute concurrently, much like an assembly line, maximizing resource utilization across multi-core processors and distributed computing clusters [76] [77].
The importance of optimized parallelization is particularly evident in clinical and translational research contexts, where accelerated processing can directly impact drug development timelines and patient stratification efforts. This document presents application notes and experimental protocols for implementing effective pipeline parallelization within brain imaging research workflows, with specific consideration for the unique characteristics of neuroimaging data and analytical methods.
Background and Fundamentals
Forms of Parallelism in Computing
Pipeline parallelization exists within a broader ecosystem of parallel computing approaches, each with distinct characteristics and optimal application scenarios:
- Data Parallelism: Applies the same operation to multiple elements of a dataset simultaneously. This approach is ideal for voxel-based morphometry or batch processing of subject images [76] [77].
- Task Parallelism: Executes different functions or tasks concurrently across computing resources. This suits heterogeneous workflows where different processing stages have varying computational requirements [76].
- Pipeline Parallelism: Segregates a sequential process into stages that operate concurrently on different data items, with output from one stage feeding as input to the next [76]. This is particularly effective for neuroimaging workflows that naturally decompose into sequential steps (e.g., preprocessing, registration, statistical analysis).
- Hybrid Approaches: Combine multiple parallelism forms to address complex workflow requirements, such as applying data parallelism within specific pipeline stages [77].
Hardware Foundations for Parallel Computing
Modern computing architectures provide multiple tiers of parallel processing capability:
- Multi-Core Processors: Contain multiple independent processing units on a single chip, typically with shared memory resources. Current generation processors feature numerous cores that efficiently handle pipeline stages with shared data dependencies [76] [77].
- Graphics Processing Units (GPUs): Contain thousands of smaller cores optimized for parallel processing of highly regular computational patterns, excelling at operations like image registration and convolution [76].
- Distributed Computing Clusters: Combine multiple nodes connected via high-speed interconnects, enabling parallelization across systems with distributed memory architectures [77].
- Specialized Accelerators: Include Tensor Processing Units and Field-Programmable Gate Arrays designed for specific computational patterns common in deep learning and signal processing applications [76].
Table 1: Hardware Platforms for Pipeline Parallelization
| Hardware Platform | Parallelism Type | Typical Use Cases | Key Considerations |
|---|---|---|---|
| Multi-core CPU | Task, Pipeline, Data | Preprocessing, statistical analysis | Memory bandwidth, cache hierarchy |
| GPU | Data, Pipeline | Volumetric registration, image filtering | Data transfer overhead, kernel optimization |
| Computing Cluster | All forms | Large-scale population analysis | Network latency, load balancing |
| Hybrid CPU-GPU | Hybrid | Complex multi-stage pipelines | Work partitioning, accelerator management |
Pipeline Parallelization Strategies for Brain Imaging
Principles of Pipeline Construction
Effective pipeline design begins with comprehensive workflow decomposition. Each processing stage should exhibit well-defined inputs and outputs, minimal shared state, and comparable computational intensity where possible. The pipeline depth (number of stages) and granularity (work per stage) must balance parallelization potential against overhead costs [76] [77].
Key design considerations include:
- Stage Dependencies: Identify sequential constraints that determine pipeline topology
- Data Volume: Assess memory requirements and transfer patterns between stages
- Computational Load: Balance processing requirements across stages to prevent bottlenecks
- Fault Tolerance: Incorporate checkpointing mechanisms for long-running pipelines
For brain imaging workflows, pipelines typically incorporate both sequential essential stages (with inherent data dependencies) and embarrassingly parallel stages (with independent operations across subjects or regions) [50].
Workflow Analysis and Profiling
Before parallelization, conduct comprehensive profiling of existing sequential workflows:
- Instrumentation: Insert timing measurements across workflow components
- Resource Monitoring: Track memory, storage, and network utilization patterns
- Dependency Mapping: Identify data flow and precedence relationships between operations
- Bottleneck Identification: Locate computational hotspots and resource contentions
This analysis informs strategic parallelization by quantifying potential acceleration opportunities and identifying stages that would benefit most from parallel execution [77].
Implementation Protocols
Multi-Core Pipeline Implementation
For shared-memory systems with multi-core processors, implement pipeline parallelization using threading models:
OpenMP Implementation
The Open Multi-Processing (OpenMP) API provides compiler directives for pipeline parallelization:
Thread-Based Implementation with Synchronization
For more complex pipeline control, implement explicit threading with synchronization primitives:
Table 2: Performance Comparison of Parallelization Techniques for Neuroimaging
| Parallelization Approach | Hardware Platform | Typical Speedup | Optimal Data Scale | Implementation Complexity |
|---|---|---|---|---|
| OpenMP Pipeline | Multi-core CPU (16-64 cores) | 3-8x | Medium (10-100 subjects) | Low |
| POSIX Threads | Multi-core CPU | 4-10x | Medium to Large | Medium |
| MPI Pipeline | Distributed Cluster | 10-50x | Large (>100 subjects) | High |
| GPU Acceleration | GPU + CPU | 5-20x (per node) | Compute-intensive stages | Medium-High |
| Hybrid MPI+OpenMP | Heterogeneous Cluster | 20-100x | Very Large (>1000 subjects) | Very High |
Distributed Pipeline Implementation
For large-scale studies requiring distributed computing resources, implement pipeline parallelization using message passing:
MPI-Based Pipeline Protocol
The Message Passing Interface (MPI) enables pipeline distribution across compute nodes:
Data Partitioning Strategy
Effective distributed pipelines require strategic data partitioning:
Case Study: ABIDA Platform Pipeline Optimization
The Automated Brain Imaging Data Processing and Analysis (ABIDA) platform demonstrates effective pipeline parallelization in neuroimaging. ABIDA integrates processing steps including data format conversion, slice timing correction, head realignment, spatial normalization, smoothing, detrending, and filtering [55].
ABIDA Pipeline Architecture
ABIDA employs a structured pipeline with explicit stage identification through filename encoding:
- Stage A: Slice timing correction
- Stage R: Head motion realignment
- Stage W: Spatial normalization
- Stage S: Spatial smoothing
- Stage D: Detrending
- Stage C: Nuisance covariate regression
- Stage F: Temporal filtering
This encoding enables pipeline state transparency and facilitates checkpointing for fault tolerance [55].
Performance Optimization Results
In comparative testing, ABIDA demonstrated significantly improved processing efficiency compared to traditional toolkits like REST and DPABI. The optimized parallelization reduced processing time for large cohorts while maintaining reproducibility [55].
Benchmarking and Performance Validation
Performance Metrics Protocol
Establish comprehensive benchmarking to validate pipeline optimization:
- Throughput: Measure subjects processed per hour across varying pipeline depths
- Speedup Ratio: Compare parallel versus sequential execution times: ( Sp = T1 / T_p )
- Parallel Efficiency: Calculate ( Ep = Sp / p ) where ( p ) is number of workers
- Scalability: Assess performance with increasing data volume and computational resources
- Resource Utilization: Monitor CPU, memory, and I/O usage throughout execution
Benchmarking Implementation
Table 3: Research Reagent Solutions for Parallel Neuroimaging
| Tool/Category | Specific Implementation | Primary Function | Application Context |
|---|---|---|---|
| Parallel Programming Models | OpenMP, MPI, CUDA | Abstraction for parallel hardware | Multi-core, distributed, and GPU acceleration |
| Neuroimaging Pipelines | ABIDA, DPABI, HCP Pipelines | Domain-specific workflow automation | Resting-state fMRI, structural processing |
| Data Format Tools | DICOM to NIFTI converters | Standardized data representation | Interoperability between pipeline stages |
| Performance Analysis | Intel VTune, NVIDIA Nsight | Performance profiling and optimization | Bottleneck identification in parallel code |
| Workflow Management | Nextflow, Snakemake | Pipeline definition and execution | Reproducible, scalable workflow orchestration |
| Container Platforms | Docker, Singularity | Environment reproducibility | Consistent execution across systems |
Advanced Optimization Techniques
Dynamic Load Balancing
Implement work stealing queues for imbalanced pipeline stages:
Memory Hierarchy Optimization
Maximize performance through strategic data placement:
- Cache-Aware Algorithms: Structure data accesses to maximize locality
- GPU Memory Management: Minimize host-device transfers through batching
- Distributed Shared Memory: Implement software caching for frequently accessed data
Fault Tolerance Protocols
Ensure reliability for long-running distributed pipelines:
- Checkpointing: Periodic saving of pipeline state to persistent storage
- Stage Replication: Critical stage duplication for failure recovery
- Speculative Execution: Parallel processing of ambiguous computational paths
Optimizing pipeline parallelization for brain imaging data analysis requires systematic approach encompassing workflow decomposition, appropriate technology selection, and rigorous performance validation. The protocols outlined provide foundation for implementing efficient parallel pipelines across multi-core and distributed computing environments. As neuroimaging datasets continue growing in scale and complexity, these optimization techniques will become increasingly essential for timely analysis in both basic research and drug development contexts.
Future directions include deeper integration of machine learning components within analytical pipelines, automated pipeline optimization through reinforcement learning, and specialized hardware acceleration for specific neuroimaging computational patterns. The continued evolution of programming models like SYCL and Kokkos promises enhanced performance portability across increasingly heterogeneous computing environments [78].
The integration of artificial intelligence (AI) into brain imaging data analysis has introduced powerful tools for automating tasks like tumor classification, segmentation, and disease detection [79] [80]. Convolutional Neural Networks (CNNs) and other deep learning models have demonstrated remarkable performance, with reported classification accuracies ranging from 95% to 99% and Dice coefficients for segmentation tasks between 0.83 and 0.94 [79]. However, the path to clinical adoption is fraught with significant technical challenges. Three critical hurdles stand out: overfitting due to limited medical data, the need for robust data augmentation to improve model generalization, and the 'black box' problem that obscures model decision-making and erodes clinical trust [79] [81] [80]. This document provides detailed application notes and experimental protocols, framed within brain imaging research, to help researchers and drug development professionals effectively mitigate these challenges.
Application Notes & Experimental Protocols
Protocol 1: Combating Overfitting with Transfer Learning
1. Principle: Overfitting occurs when a complex model learns patterns specific to the limited training data, failing to generalize to new, unseen data [79] [80]. Transfer learning mitigates this by leveraging features learned from a large, general-purpose dataset (e.g., ImageNet) and adapting them to a specific, smaller medical imaging domain [82].
2. Experimental Workflow for Sequential Transfer Learning:
The following workflow details the steps for applying transfer learning across multiple brain imaging datasets to enhance model performance and robustness.
3. Key Procedures:
- Model Selection and Preparation: Choose a pre-trained architecture like VGG16 or ResNet. The early layers, which detect general features (edges, textures), are typically frozen to prevent overwriting foundational knowledge [82].
- Sequential Fine-tuning: First, fine-tune the model on a primary target dataset (e.g., brain tumor MRIs). Then, use this adapted model as a new starting point for a second, related domain (e.g., Alzheimer's disease detection). This sequential approach leverages domain-relatedness in neuroimaging to enhance feature generalization [82].
- Performance Validation: Evaluate the model after each fine-tuning stage on a held-out test set from the respective domain. Metrics like accuracy, precision, recall, and F1-score should be reported [82].
4. Research Reagent Solutions:
| Reagent / Material | Function in Protocol |
|---|---|
| Pre-trained Model (e.g., VGG16) | Provides a foundation of general image features, reducing the need for vast amounts of medical data and training time [82]. |
| Brain Tumor MRI Dataset (e.g., BraTS) | Serves as the first target domain for fine-tuning, adapting the model to a specific neurological pathology [79]. |
| Alzheimer's Disease MRI Dataset (e.g., ADNI) | Serves as the second target domain, validating the model's ability to transfer knowledge to a related diagnostic task [82]. |
Protocol 2: Enhancing Generalization via Advanced Data Augmentation
1. Principle: Data augmentation artificially expands the training dataset by creating modified versions of existing images. This technique teaches the model to be invariant to irrelevant variations (e.g., scanner differences, orientation) and focuses on biologically relevant features, thereby improving generalization [79] [83].
2. Experimental Workflow for WB-MRI Data Augmentation:
This protocol outlines a specialized augmentation pipeline designed to address scanner variability in Whole-Body MRI (WB-MRI), improving model robustness across different imaging platforms.
3. Key Procedures:
- Base Augmentation: Apply standard geometric transformations such as affine transformations, rotations, and scaling to build initial invariance [82].
- MRI-Specific Augmentation: Implement advanced techniques that simulate artifacts and variations inherent to MRI acquisition. This includes adding noise, simulating motion artifacts, and varying image intensity to mimic differences in scanner protocols and vendors [83].
- Validation: It is critical to test the trained model on a separate validation set comprising data from multiple scanners and institutions to verify that the augmentation pipeline has improved generalization [83]. The Dice Similarity Coefficient (DSC) and Area Under the Curve (AUC) are key metrics for segmentation and classification tasks, respectively [83].
4. Research Reagent Solutions:
| Reagent / Material | Function in Protocol |
|---|---|
Augmentation Software (e.g., TensorFlow ImageDataGenerator, PyTorch Torchvision) |
Provides libraries for implementing both basic and advanced image transformations programmatically. |
| Multi-Scanner/WMulti-Vendor WB-MRI Dataset | Serves as the source of raw data and the benchmark for testing model generalization across different imaging platforms [83]. |
| GAN-based Synthesis Models | (Optional) Can be used to generate highly realistic, synthetic MRI data to further augment the dataset, especially for rare neurological disorders [82]. |
Protocol 3: Demystifying the 'Black Box' with Explainable AI (XAI)
1. Principle: The 'black box' problem refers to the opacity of complex AI models, making it difficult to understand the reasoning behind their predictions [81] [84]. Explainable AI (XAI) techniques provide visual or quantitative insights into model decisions, which is crucial for building clinical trust, debugging models, and validating that predictions are based on biologically plausible regions [82] [81].
2. Workflow for Integrating XAI into Model Validation:
This workflow integrates XAI methods post-training to audit and explain model decisions, ensuring they align with clinical understanding and building trust with end-users.
3. Key Procedures:
- Model Inference: Run a trained model on a new MRI scan to obtain a prediction (e.g., tumor classification) [82].
- XAI Application: Apply one or more XAI techniques to the model's prediction.
- SHAP (SHapley Additive exPlanations): A unified method that calculates the contribution of each pixel (feature) to the final prediction, providing a fine-grained attribution map [82].
- Grad-CAM (Gradient-weighted Class Activation Mapping): Generates a coarse localization heatmap highlighting the important regions in the image for the prediction [84] [82].
- Clinical Validation: The generated explanation maps must be reviewed and validated by clinical experts (e.g., radiologists, neuroscientists) to ensure that the model's focus aligns with known anatomical or pathological features [81] [82]. Studies show that such explanations can increase clinician trust in AI-driven diagnoses by up to 30% [81].
4. Research Reagent Solutions:
| Reagent / Material | Function in Protocol |
|---|---|
| XAI Software Libraries (e.g., SHAP, Captum) | Provide pre-implemented algorithms for calculating and visualizing feature attributions for deep learning models. |
| Grad-CAM Integrated Tools | Often built into deep learning frameworks or available as standalone modules to generate visual explanation heatmaps [84]. |
| Expert-Annotated Ground Truth Datasets | Used as a benchmark to validate whether the XAI heatmaps highlight clinically relevant regions, ensuring biological plausibility. |
The table below synthesizes key performance metrics from recent studies that implemented the aforementioned mitigation strategies in brain imaging analysis.
Table 1: Performance Metrics of AI Models Implementing Mitigation Strategies in Brain Imaging
| AI Model / Strategy | Primary Task | Reported Performance | Key Mitigation Addressed |
|---|---|---|---|
| CNN-Based Models [79] | Tumor Classification & Segmentation | Accuracy: 95% - 99%Dice: 0.83 - 0.94 | Baseline performance |
| Hybrid Architectures (e.g., CNN-SVM, CNN-LSTM) [79] | Classification & Segmentation | Accuracy: >95%Dice: ~0.90 | Overfitting, Performance |
| Transformer-Based Models (e.g., Swin Transformer) [79] | Classification | Accuracy: Up to 99.9% | Performance |
| Transfer Learning + XAI (VGG16-CNN Hybrid) [82] | Brain Tumor & Alzheimer's Detection | Accuracy: 93% - 94% (Tumor)81% (Alzheimer's) | Overfitting, Black Box |
| Advanced Data Augmentation for WB-MRI [83] | Segmentation across scanners | Improved DSC and AUC vs. standard augmentation | Generalization (Scanner Variance) |
| XAI Integration [81] | Clinical Trust in Diagnostics | Increased clinician trust by ~30% | Black Box |
In brain imaging data analysis, the integrity of scientific conclusions is fundamentally dependent on two core processes: the rigorous quality control (QC) of input data and the meticulous tracking of data provenance throughout the entire analytical workflow. The maturation of neuroimaging into a "big data" science, characterized by large, multi-site datasets and complex processing pipelines, has made these processes not merely best practices but essential components of rigorous, reproducible research [85]. This document outlines application notes and detailed protocols for implementing robust QC and provenance-tracking frameworks, specifically contextualized within brain imaging research for an audience of researchers, scientists, and drug development professionals.
Quality Control in Brain Imaging Workflows
The Critical Need for Automated Quality Control
Brain imaging data, particularly from clinical settings or large-scale data warehouses, is inherently heterogeneous. This heterogeneity arises from differences in scanners, manufacturers, acquisition parameters, and magnetic field strengths (e.g., 1.5T, 3T) [86] [87]. Furthermore, routine clinical data are susceptible to various artefacts, including motion, noise, poor contrast, and ghosting, which can severely compromise the reliability of downstream analysis and lead to erroneous findings due to "short-cut" learning in automated systems [87]. Visual inspection of images, while considered a gold standard, is subjective and prohibitively time-consuming for large datasets numbering in the thousands [86]. Therefore, developing and implementing automated, scalable QC tools is paramount.
Experimental Protocols for Quality Control
Protocol 1: Automated Quality Control of T1-Weighted (T1w) Brain MRI Scans
- Objective: To automatically classify T1w brain MRI scans from clinical research datasets as "accept" or "reject" based on image quality.
- Datasets: Utilize large, heterogeneous datasets. A proven approach uses data from multiple scanners and sites (e.g., N=2438, 11 sites, 39 scanner models) including both patient and control groups with an average age of 71 ± 8 years [86].
- QC Pipeline Processing:
- Classifier Training:
- Use visual QC ratings as the ground truth for training.
- Design a classifier (e.g., a Robust Undersampling Boost (RUS) classifier) that integrates the QC measures from the existing tools [86].
- Train the classifier on the multi-site dataset and evaluate its performance using cross-validation. Assess generalizability via leave-one-site-out validation and testing on data from different scanner manufacturers or field strengths [86].
- Performance Metrics: Evaluate based on balanced accuracy against visual QC. Reported results show a balanced accuracy of 87.7% on combined test data, with 86.6% for patients and 88.3% for controls [86].
Protocol 2: Quality Control for FLAIR MRI Sequences
- Objective: To ensure the quality of 3D FLAIR MRIs, which are crucial for visualizing white matter lesions, within a clinical data warehouse.
- Challenge: QC pipelines that rely heavily on pre-processing steps like tissue segmentation often fail on low-quality clinical images, with failure rates as high as 44% for images with severe noise [87].
- Methodology:
- Manual Annotation for Ground Truth: Images are manually scored by raters, typically on a scale (e.g., 1-5 for overall quality) or for the presence and severity of specific artefacts (e.g., motion, noise, contrast) on a three-point scale [87].
- Domain Adaptation: To minimize manual annotation, leverage transfer learning from related modalities. For example, use a deep learning model already trained on a large set of annotated T1w images and adapt it to the FLAIR modality using techniques like Domain Adversarial Neural Networks (DANN) or semi-supervised domain adaptation (SSDA) [87].
Performance Comparison of QC Tools
The table below summarizes the performance of different QC approaches as reported in the literature.
Table 1: Performance Comparison of Quality Control Approaches in Neuroimaging
| QC Method | Modality | Dataset Characteristics | Performance | Key Findings/Limitations |
|---|---|---|---|---|
| RUS Classifier [86] | T1w MRI | Multi-site (11 sites), ageing & clinical populations (N=2438) | 87.7% balanced accuracy | More robust than using MRIQC or CAT12 alone for clinical cohorts; generalizes well across sites. |
| MRIQC/CAT12 Alone [86] | T1w MRI | Multi-site (11 sites), ageing & clinical populations (N=2438) | Kappa ~0.30 with visual QC | Agreement with visual QC is significant but highly variable across datasets; not robust for clinical cohorts. |
| Deep Learning Model [87] | T1w MRI | Clinical Data Warehouse (N >5500) | >80% balanced accuracy | Effective for initial quality filtering of highly heterogeneous clinical data. |
| Tissue Segmentation-Based QC [87] | FLAIR MRI | Research Datasets | N/A | Fails on 24-44% of poor-quality clinical images, limiting applicability to clinical data warehouses. |
Provenance Tracking in Neuroscience Platforms
The Role of Provenance in Reproducible Research
Provenance tracking refers to the automated and detailed recording of the entire history of a data object: its origin, the computational processes applied to it, the parameters and software versions used, and the resulting derived data objects [85]. This creates a complete and reproducible chain of custody for every finding, which is critical for debugging complex pipelines, validating results, and ensuring research can be replicated.
Implementation on the brainlife.io Platform
The brainlife.io platform is a decentralized, open-source cloud platform that exemplifies the implementation of robust provenance tracking in neuroscience [85]. Its architecture provides a practical model for how provenance can be integrated into an end-to-end data analysis workflow.
- Microservice Architecture: The platform uses a microservice-based orchestration system (Amaretti) to manage data and computational jobs across high-performance clusters and clouds [85].
- Object-Oriented Data Model: Data is stored as standardized "datatypes," which allow automated app pipelining. Each data object is assigned a unique ID [85].
- Automated Provenance Tracking: The platform automatically tracks and records [85]:
- All data objects used as inputs and generated as outputs.
- The specific application (app) used for processing, including its version.
- The parameter sets used for each processing step.
- Provenance Visualization: The complete history of data generation is visualized as a provenance graph, allowing users to see the entire workflow that led to a specific result at a glance [85].
The Scientist's Toolkit: Essential Research Reagents and Solutions
This table details key software tools and platforms essential for implementing QC and provenance tracking in brain imaging research.
Table 2: Key Resources for Brain Imaging QC and Provenance Tracking
| Tool/Platform Name | Type | Primary Function | Relevance to Workflow |
|---|---|---|---|
| MRIQC [86] | Software Pipeline | Extracts no-reference quality metrics from T1w and other structural and functional MRI data. | Provides quantitative features that can be used to train automated QC classifiers or for initial quality assessment. |
| CAT12 [86] | Software Toolbox | Provides computational anatomy tools for processing structural MRI data, including QC metrics. | Serves as another source of automated quality measures for T1w images, complementing MRIQC. |
| brainlife.io [85] | Cloud Platform | A decentralized platform for end-to-end management, processing, analysis, and visualization of neuroscience data. | Automatically tracks provenance for all data objects and processing steps, ensuring reproducibility and FAIR data access. |
| SPM (Statistical Parametric Mapping) [87] | Software Package | Used for segmentation, normalization, and statistical analysis of brain imaging data. | Its segmentation tools (e.g., FAST) are sometimes used in quantitative QC pipelines, though they can fail on low-quality data. |
| Domain Adversarial Neural Network (DANN) [87] | Machine Learning Technique | A domain adaptation method to minimize the gap between source (e.g., T1w) and target (e.g., FLAIR) domains. | Enables the transfer of QC models from one imaging modality to another, reducing the need for extensive manual labeling. |
Benchmarking and Best Practices for Reliable Research
Establishing Robust Validation Frameworks for Analytical Pipelines
Application Note: Core Principles and Implementation
Robust validation frameworks are critical for ensuring the reliability, reproducibility, and clinical applicability of brain imaging data analysis workflows. These frameworks function as interconnected quality cycles, spanning from data acquisition and processing to algorithmic design and research dissemination [88]. In the context of brain imaging, where multi-site studies and complex artificial intelligence (AI) models are increasingly common, a systematic approach to validation mitigates risks associated with technical variability, model bias, and irreproducible findings [89] [88]. This document outlines the core principles, protocols, and practical tools for establishing such a framework, tailored for researchers, scientists, and drug development professionals.
Core Components of a Robust Validation Framework
A robust validation framework for analytical pipelines is built upon several interconnected pillars that ensure quality throughout the entire research lifecycle.
Table 1: Core Components of a Validation Framework for Brain Imaging
| Component | Description | Primary Function |
|---|---|---|
| Data Integrity & Harmonization | Addresses scanner variability and protocol differences across sites [88]. | Ensures that findings reflect biology, not technical noise. |
| Algorithmic & AI Robustness | Emphasizes reproducibility, interpretability, and generalizability of models [88]. | Provides reliable predictions that are valid across diverse, real-world datasets. |
| Rigorous Statistical Validation | Employs internal and external validation cohorts and performance metrics like AUC [90] [91]. | Quantifies model performance and ensures clinical utility. |
| Transparent Research Dissemination | Involves sharing code, data, and protocols to support reproducibility [88]. | Completes the "cycle of quality" and enables scientific scrutiny. |
Protocol: A Step-by-Step Guide to Pipeline Implementation
Phase 1: Data Cleaning and Validation Schema
The foundation of any reliable pipeline is clean, validated input data. This involves creating a structured schema to define data quality.
2.1.1 Define Data Schema: Using a tool like Pydantic in Python, create a contract for your data. For brain imaging metadata, this could include fields for participant age, sex, clinical scores, and scanner parameters, each with defined data types and allowable ranges [92].
2.1.2 Implement Custom Validators: Incorporate business logic and biological plausibility checks directly into the schema. Examples include validating that participant age is within a realistic range (e.g., 18-120) or that image resolution values are positive [92].
2.1.3 Automated Data Cleaning: Build a pipeline class to systematically handle common data issues.
- Duplicate Removal: Identify and remove duplicate records to prevent skewing analysis [92].
- Missing Value Imputation: Apply intelligent strategies based on data type. For numerical clinical data like blood biomarkers, median or mean imputation may be appropriate. For categorical data, a designated 'Unknown' category can be used [92].
Phase 2: Pipeline Architecture and Harmonization
A modular pipeline architecture ensures maintainability and scalability.
2.2.1 Pipeline Structure: Design the workflow as a sequential assembly line: Raw Data Input → Cleaning Stage → Validation Stage → Reporting Stage → Clean Data Output [92]. Each stage should perform a specific function and be individually testable.
2.2.2 Data Harmonization: For multi-site brain imaging studies, implement a harmonization framework to correct for scanner and protocol variability. This can involve vendor-independent quality assurance protocols or statistical corrections in image or feature space to separate biological variability from technical noise [88].
2.2.3 Quality Control Integration: Integrate checkpoints for quantitative MRI (qMRI) to assess and mitigate confounding factors like physiological noise and scanner instabilities. This ensures reliable and reproducible measurement of biomarkers [88].
Phase 3: Model Development and Validation
This phase focuses on building and rigorously testing predictive models.
2.3.1 Feature Selection: Use methods like Least Absolute Shrinkage and Selection Operator (LASSO) and multivariate logistic regression to identify the most relevant predictor variables from a larger set of clinical and imaging features [90].
2.3.2 Model Training & Comparison: Employ multiple machine learning (ML) methods (e.g., logistic regression, random forests, gradient boosting) to analyze data and identify the best-performing model [90] [91]. Utilize open-source software and frameworks like the Medical Open Network for AI (MONAI) for deep learning applications, incorporating data augmentation to improve model generalization [93].
2.3.3 Performance Validation:
- Internal Validation: Assess model performance on a held-out portion of your primary dataset using metrics like the area under the receiver operating characteristic curve (AUC) [90].
- External Validation: Test the model on one or more completely independent datasets to evaluate its generalizability and robustness [90] [91]. This is a critical step for verifying clinical utility.
- Model Interpretation: Use techniques like SHapley Additive exPlanations (SHAP) to interpret ML models and understand the contribution of different features to the prediction [90].
The following workflow diagram illustrates the complete validation pipeline, integrating the phases described above.
The Scientist's Toolkit: Essential Research Reagents and Materials
This table details key software tools and resources essential for implementing a robust validation framework.
Table 2: Research Reagent Solutions for Analytical Pipeline Validation
| Tool / Resource | Type | Function in Validation Pipeline |
|---|---|---|
| Pydantic [92] | Python Library | Creates data validation schemas using Python type annotations, enforcing data types and custom business rules. |
| Pandas & NumPy [92] | Python Libraries | Provides core data structures (DataFrames) and numerical operations for data manipulation, cleaning, and transformation. |
| MONAI [93] | PyTorch-based Framework | Enables deep learning for healthcare imaging, providing specialized layers, loss functions, and data augmentation tools. |
| OHDSI Software [91] | Open-Source Suite | Standardizes analytics for observational health data, supporting large-scale, reliable prediction model development and validation. |
| IBMMA [89] | R/Python Package | Provides a unified framework for meta- and mega-analysis of neuroimaging data, efficiently handling large-scale, multi-site datasets. |
| Pulseq & Gadgetron [88] | Open-Source Tools | Aids in vendor-neutral MRI sequence programming and image reconstruction, facilitating protocol harmonization across scanners. |
Protocol: Experimental Validation and Quality Assessment
Designing the Validation Experiment
A comprehensive validation experiment is crucial for benchmarking pipeline performance.
3.1.1 Cohort Definition:
- Derivation Cohort: Use this dataset for feature selection and model training. For example, a cohort of 400 critically ill patients was used to derive an ARDS prediction model [90].
- Internal Validation Cohort: A randomly selected hold-out set from the derivation cohort (e.g., 20-30%) used for initial performance assessment [90].
- External Validation Cohorts: One or more independent datasets from different locations or populations. An external cohort of 160 patients was used to validate the ARDS model, proving its generalizability [90].
3.1.2 Performance Metrics: Utilize multiple metrics for a thorough evaluation.
- Discrimination: Area Under the ROC Curve (AUC) to measure how well the model separates classes [90].
- Calibration: Decision Curve Analysis (DCA) to evaluate the clinical usefulness of the model [90].
- Segmentation Accuracy: For image-based models, use the Dice Coefficient (DC) to quantify the overlap between automated and manual segmentations [93].
Quality Control in the Clinical Setting
Maintaining quality in real-world environments requires dynamic processes.
3.2.1 Establish Quality Checkpoints: Map critical checkpoints across the entire imaging chain, from protocol setup and staff training to post-processing and reporting [88].
3.2.2 Employ Advanced Metrics: Move beyond basic metrics like signal-to-noise ratio (SNR). Implement task-based evaluations, artifact quantification, and visual integrity scores that better capture diagnostic utility [88].
3.2.3 Address Remote Scanning: For decentralized studies, mitigate quality risks with centralized protocol management, automated QA dashboards, and real-time performance monitoring [88].
The cyclical nature of a robust quality framework is visualized below, emphasizing its continuous and interconnected structure.
Within brain imaging data analysis, the selection of processing software is a critical decision that directly influences research outcomes and reproducibility. The four prominent software packages—FSL, SPM, FreeSurfer, and AFNI—collectively account for a substantial majority of published functional neuroimaging results [94]. Each package embodies different philosophical and algorithmic approaches to common processing problems, leading to measurable differences in output despite conceptual similarities in the overall analysis framework. This comparative analysis synthesizes evidence from reliability studies, processing workflow examinations, and technical implementations to guide researchers, scientists, and drug development professionals in selecting and utilizing these tools effectively within their brain imaging workflows.
Quantitative Performance Comparison
Intracranial Volume Estimation Reliability
A comparative study investigating automated intracranial volume (ICV) estimation across four software packages revealed significant variability in performance depending on the population studied, highlighting the importance of population-specific tool selection.
Table 1: Software Performance for ICV Estimation Across Populations [95]
| Population Group | Sample Size | Best Performing Software | R² Value | p-value |
|---|---|---|---|---|
| Adult Controls (AC) | 11 | SPM | 0.67 | < 0.01 |
| Adult with Dementia (AD) | 11 | Freesurfer | 0.46 | 0.02 |
| Pediatric Controls (PC) | 18 | AFNI | 0.97 | < 0.01 |
| Pediatric Epilepsy (1.5T) | 30 | FSL | 0.60 | 0.1 |
| Pediatric Epilepsy (3T) | 30 | FSL | 0.60 | < 0.01 |
The study demonstrated that the choice between atlas-based and non-atlas-based software significantly impacts measurement accuracy, with optimal performance dependent on the specific population under investigation [95].
Task fMRI Analysis Variability
Research exploring the impact of analysis software on task fMRI results has quantified substantial variability in outcomes. A comprehensive reanalysis of three published task fMRI studies using AFNI, FSL, and SPM revealed both qualitative similarities and marked quantitative differences in activation maps [94].
Table 2: Software Comparison in Task fMRI Analysis [94]
| Comparison Metric | Findings | Implications |
|---|---|---|
| Dice Similarity Coefficients | Range: 0.000 to 0.684 between thresholded statistic maps | High variability in spatial overlap of "significant" activations |
| Qualitative Similarities | Backed by Neurosynth association analyses correlating similar words/phrases to all three software's unthresholded results | Conceptual consistency in identified cognitive associations |
| Qualitative Differences | Marked differences in specific activation patterns and extent | Potential for different interpretive conclusions depending on software chosen |
This variability stems from fundamental differences in each package's implementation of processing stages, including preprocessing algorithms, statistical modeling approaches, and inference methods [94].
Experimental Protocols and Methodologies
Protocol for Finite Impulse Response (FIR) Analysis in FSL
Finite Impulse Response analysis allows for the flexible estimation of the hemodynamic response function without assuming a specific shape. The following protocol outlines the steps for implementing FIR analysis in FSL for task-based fMRI data [96]:
- Timing File Preparation: Convert event timing information into FSL-compatible three-column format (onset, duration, value) using text processing tools like awk.
- GUI Setup: Launch FEAT GUI and select "First-level analysis" and "Full analysis."
- Data Specification:
- Load the 4D BOLD data file
- Set output directory name
- Maintain defaults in Data and Pre-stats tabs unless experimental design requires modification
- Registration Configuration:
- Set both "Main structural image" and "Standard space" fields to "Full Search" and "12 DOF"
- Select the skull-stripped structural T1-weighted image as the main structural image
- FIR Model Specification:
- In the Stats tab, set "Number of original EVs" to match experimental conditions
- For each EV: Provide a descriptive name, select "Custom (3 column format)" for Basic shape, and select the corresponding timing file
- Set "Convolution" to "FIR basis functions"
- Define the Number of time-points (e.g., 10) and Window length (e.g., 20 seconds)
- Contrast Specification:
- Specify F-tests to evaluate significance across all time-points for each condition
- Create custom t-contrasts to test specific hypotheses about response patterns across time-points
- Batch Processing:
- Save the design file from the GUI
- Modify the design file for each subject using sed to update subject-specific paths and parameters
- Execute analysis using the feat command in a batch script
- Results Visualization:
- Concatenate individual time-point statistical maps using fslmerge
- Visualize results in fsleyes, overlaying F-statistic maps and FIR time-series on structural images
Protocol for Multi-Software Processing Validation
To ensure robust and reproducible findings, researchers can implement a cross-software validation protocol:
- Data Selection: Acquire publicly available datasets from repositories like OpenNeuro (formerly OpenfMRI) that include raw data and published results [94].
- Pipeline Implementation:
- Implement equivalent processing pipelines in AFNI, FSL, and SPM
- Maintain maximum possible similarity in processing parameters across packages
- Document all deviations necessitated by software-specific constraints
- Quality Control:
- Implement rigorous quality control measures for each software package [97]
- Verify processing completion and accuracy at each stage
- Inspect interim results for artifacts or irregularities
- Comparison Methodology:
- Compare both thresholded and unthresholded statistical maps
- Calculate spatial similarity metrics (e.g., Dice coefficients)
- Evaluate qualitative concordance with published findings
- Results Interpretation:
- Focus on consistent findings across multiple software packages
- Investigate discrepant results with consideration of software-specific algorithmic differences
Figure 1: Generalized fMRI Processing Workflow. This diagram illustrates the common stages in task-based fMRI analysis, implemented with varying algorithms across software packages.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Essential Software Tools for Neuroimaging Research [98] [43] [99]
| Tool Name | Primary Function | Key Features | Implementation |
|---|---|---|---|
| SPM | Statistical Parametric Mapping | General Linear Model implementation, MATLAB integration | MATLAB-based, requires commercial license |
| FSL | FMRIB Software Library | Comprehensive tools for fMRI, MRI, and DTI analysis | Linux-based, command-line focused |
| AFNI | Analysis of Functional NeuroImages | Extensive customization, scripting capabilities | C-based programs, multiple OS support |
| FreeSurfer | Cortical Surface Analysis | Cortical reconstruction, thickness measurement | Surface-based analysis, automated pipelines |
| Freesurfer | Cortical Surface Analysis | Cortical reconstruction, thickness measurement | Surface-based analysis, automated pipelines |
| Nipype | Workflow Integration | Integrates multiple packages, flexible pipeline creation | Python-based, enables best-in-breed approaches |
Workflow Integration and Parallel Processing Solutions
The development of workflow integration tools represents a significant advancement in addressing the challenges of multi-software neuroimaging analysis. These tools can be categorized into two primary approaches:
Flexible workflow tools including LONI Pipeline, JIST, and Nipype provide environments where users can construct customized analysis pipelines by combining modules from different software packages [43]. These systems support:
- Access to predefined module libraries from AFNI, SPM, FSL, FreeSurfer, and other packages
- Graphical or script-based workflow construction with dependency management
- Computational parallelization across multiple cores or computing clusters
- Validation and quality control mechanisms
Fixed workflow tools such as CIVET, PANDA, and DPARSF offer completely established processing pipelines for specific analysis types [43]. These provide:
- Fully automated processing from raw data to final results
- Optimized parameters for specific analysis modalities
- Reduced flexibility but increased standardization
Figure 2: Neuroimaging Workflow Integration Approaches. This diagram illustrates how flexible and fixed workflow tools integrate modules from different software packages.
The comparative analysis of FSL, SPM, FreeSurfer, and AFNI reveals a complex landscape where software selection significantly influences research outcomes. The evidence demonstrates that optimal software choice depends on multiple factors including the specific research question, population characteristics, imaging modality, and analysis requirements. Rather than seeking a universal "best" package, researchers should understand the comparative strengths and limitations of each tool, implement cross-software validation when feasible, and consider utilizing workflow integration platforms to combine the strongest elements of each package. This approach enhances methodological rigor and contributes to improved reproducibility in brain imaging research, ultimately supporting more reliable outcomes in both basic neuroscience and drug development applications.
Adhering to Community Best Practices for Data Analysis and Sharing
The expansion of brain imaging modalities, from structural and functional MRI to diffusion tensor imaging, has generated unprecedented volumes of neuroscientific data [100]. This data deluge presents both an opportunity and a challenge for the research community. Adhering to community-established best practices for data analysis and sharing has become fundamental for advancing a reproducible, collaborative, and efficient neuroscience ecosystem. This protocol outlines standardized methodologies for analyzing and sharing brain imaging data, framed within the context of a broader thesis on brain imaging data analysis workflows. The guidance is designed for researchers, scientists, and drug development professionals engaged in generating, processing, or utilizing neuroimaging data. By implementing these practices, the community can enhance the statistical power of studies, enable the validation of findings, and accelerate the translation of research into clinical applications [101].
The FAIR (Findable, Accessible, Interoperable, and Reusable) and CARE (Collective benefit, Authority to control, Responsibility, and Ethics) principles provide a foundational framework for responsible data stewardship [101]. Meanwhile, infrastructure like the Human Connectome Project (HCP) [102] and the Brain Imaging and Neurophysiology Database (BIND) [69] demonstrate the power of large-scale, shared data resources. This document integrates these overarching principles with practical, actionable protocols for the researcher's bench.
Community Standards and Data Sharing Infrastructure
The neuroimaging community has developed robust standards and infrastructures to support data sharing. Key resources and their characteristics are summarized in the table below.
Table 1: Key Data Sharing Infrastructures for Neuroimaging Data
| Infrastructure Name | Primary Focus / Data Types | Key Features | Notable Scale / Statistics |
|---|---|---|---|
| Human Connectome Project (HCP) [102] | Multimodal brain connectivity; MRI (3T, 7T), MEG | Extensive data processing pipelines; Lifespan studies (Development, Young Adult, Aging) | 1206 healthy young adults in S1200 release [102] |
| Brain Imaging and Neurophysiology Database (BIND) [69] | Multi-institutional, multimodal clinical imaging linked to neurophysiology | Integrates MRI, CT, PET, SPECT with EEG/PSG; Standardized clinical metadata extraction via Bio-Medical LLMs | 1.8 million scans from 38,945 subjects [69] |
| OpenNeuro [101] | General-purpose neuroimaging data repository | Supports Brain Imaging Data Structure (BIDS) format; facilitates sharing of individual datasets | Listed among platforms for sharing "long tail" science data [101] |
The drive for data sharing is supported by funding bodies and governments worldwide, including the NIH and the European Union's Horizon Europe program, which often mandate open data policies [101]. For researchers within the European Union, special consideration must be given to the General Data Protection Regulation (GDPR), which defines anonymization strictly and applies to any data that can be individualized to a single participant [101]. It is crucial to use platforms that comply with these regulations, which may involve "controlled access" protocols where users must sign Data Use Agreements [69].
Experimental Protocols for Data Analysis
Protocol 1: General fMRI Data Analysis Workflow
This protocol details a standard functional Magnetic Resonance Imaging (fMRI) analysis pipeline using the Statistical Parametric Mapping (SPM12) software package, a widely used tool in the community [103].
Workflow Diagram: fMRI Data Analysis with SPM12
Materials and Reagents:
- fMRI Data: Acquired using a standardized EPI sequence.
- Software Package: SPM12 (Statistical Parametric Mapping).
- Computing Environment: MATLAB or Octave.
- Anatomical Template: Standard space template (e.g., MNI space).
Procedure:
- Data Preprocessing: Execute the following steps in sequence [103]:
- Slice Timing Correction: Correct for acquisition time differences between slices.
- Realignment: Co-register all EPI images to the first image of the session to correct for head motion. The six estimated movement parameters should be saved for inclusion as regressors in the first-level model.
- Coregistration: Align the high-resolution anatomical image (T1-weighted) to the mean functional image generated during realignment.
- Normalization: Spatially normalize all coregistered images to a standard stereotaxic space (e.g., MNI space) to enable inter-subject comparisons.
- Spatial Smoothing: Apply a Gaussian smoothing kernel (e.g., 6-mm full width at half maximum) to increase the signal-to-noise ratio and account for residual anatomical variations.
First-Level (Within-Subject) Analysis: For each participant, specify a General Linear Model (GLM) where the hemodynamic response for all experimental conditions (e.g., Auditory Rhythm, Visual Rhythm, Controls) is modeled along with the six motion parameters as nuisance regressors [103]. This step generates statistical maps (contrast images) for each condition and contrast of interest per subject.
Second-Level (Group) Analysis: Implement a random-effects analysis to make inferences at the population level. For example, conduct an ANOVA to compare contrast images across experimental conditions and between groups (e.g., healthy controls vs. patient groups) [103].
Statistical Inference and Localization: Apply a voxel-wise threshold (e.g., p < 0.001 uncorrected) and a cluster-level family-wise error (FWE) correction (e.g., p < 0.05 FWE). Use a probabilistic brain atlas (e.g., SPM Anatomy Toolbox) to anatomically localize significant activations [103].
Protocol 2: Integrated Multimodal Connectivity Analysis
Integrating multiple imaging modalities provides a more comprehensive view of brain structure and function. This protocol, inspired by graph neural network approaches, combines fMRI, Diffusion Tensor Imaging (DTI), and structural MRI (sMRI) [7].
Workflow Diagram: Multimodal Brain Connectivity Integration
Materials and Reagents:
- Multimodal Data: Preprocessed fMRI, DTI, and high-resolution T1-weighted sMRI data from a cohort (e.g., from HCP-D [7]).
- Computational Tools: Python-based deep learning libraries (e.g., PyTorch, TensorFlow) and specialized neuroimaging toolkits (e.g., FSL, FreeSurfer).
- Code Repository: Publicly available code for the integrated graph neural network model [7].
Procedure:
- Feature Extraction:
- From fMRI: Compute functional connectivity matrices, typically representing Pearson correlation coefficients between the time series of predefined brain regions (e.g., from an atlas).
- From DTI: Reconstruct white matter tracts to compute structural connectivity matrices, representing the strength (e.g., fractional anisotropy, fiber count) of connections between brain regions.
- From sMRI: Extract regional morphometric features such as cortical thickness, surface area, or gray matter volume for each brain region.
Graph Construction: Model the brain as a graph where nodes represent brain regions (parcels from an atlas). Each node is attributed with features from the sMRI data. The edges between nodes are defined and weighted using the functional and structural connectivity matrices [7].
Model Training and Interpretation: Train an interpretable graph neural network (GNN) on the constructed brain graphs. The GNN learns to integrate nodal (sMRI) and edge-level (fMRI, DTI) information to make predictions (e.g., about cognitive scores or clinical status). Use the model's interpretability features to identify which brain circuits and connections are most informative for the prediction task [7].
Protocol 3: Assessing Glymphatic Function with DTI-ALPS
The glymphatic system, the brain's waste-clearance pathway, can be evaluated non-invasively using Diffusion Tensor Imaging Analysis along the Perivascular Space (DTI-ALPS). This protocol is relevant for research on neurodegenerative diseases like Alzheimer's disease [104].
Workflow Diagram: DTI-ALPS Index Calculation for Glymphatic Function
Materials and Reagents:
- DTI Data: Acquired on a 3T MRI scanner with a single-shot EPI sequence (parameters: TR/TE ~ 8600/64 ms, b-values = 0, 1000 s/mm², voxel size ~ 0.75×0.75×1.5 mm³) [104].
- Analysis Software: DTI processing software (e.g., FSL, DSI Studio) and a tool for ROI placement (e.g., MRIcron).
- Subject Cohort: Participants (e.g., patients with Alzheimer's Disease, Mild Cognitive Impairment, and normal controls) with informed consent and ethical approval.
Procedure:
- DTI Acquisition and Preprocessing: Acquire DTI data and perform standard preprocessing, including eddy-current correction and head motion correction.
- Region of Interest (ROI) Placement: In the hemisphere of the lateral ventricle body level, manually place four ROIs [105]:
- One ROI each in the projection fiber area (e.g., corticospinal tract) and the association fiber area (e.g., superior longitudinal fasciculus). These measure the primary direction of water diffusion within the fibers.
- Two smaller ROIs in the perivascular spaces (PVS) adjacent to the central veins running through these fiber tracts. These measure water diffusion along the x, y, and z axes.
- Diffusion Coefficient Calculation: For the PVS ROIs, extract the following diffusivity measures [105]:
- Dxx: The x-axis diffusivity (representing diffusion along the perivascular space).
- Dyy and Dzz: The y- and z-axis diffusivities (representing diffusion perpendicular to the perivascular space).
- ALPS Index Computation: Calculate the ALPS index using the formula [105]:
- ALPS index = mean (Dxx in projection fiber area, Dxx in association fiber area) / mean (Dyy in projection fiber area, Dzz in association fiber area) A lower ALPS index suggests impaired glymphatic activity, as seen in Alzheimer's disease and amnestic mild cognitive impairment [104].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Research Reagent Solutions for Brain Imaging Analysis
| Item Name | Function / Purpose | Example Use Case / Note |
|---|---|---|
| SPM12 (Statistical Parametric Mapping) [103] | A software package for the analysis of brain imaging data sequences (fMRI, PET, SPECT, EEG). | Used for standard GLM-based analysis and preprocessing of fMRI data. |
| BIDS (Brain Imaging Data Structure) [101] | A simple and intuitive framework for organizing and describing neuroimaging and behavioral data. | Ensures data interoperability and reusability; required by many repositories like OpenNeuro. |
| Graph Neural Networks (GNNs) [7] | A class of deep learning models for processing data represented as graphs. | Ideal for analyzing brain connectivity networks derived from fMRI and DTI data. |
| VB-Net Model [104] | A deep learning architecture based on V-Net with bottleneck layers for medical image segmentation. | Used for automated segmentation of enlarged perivascular spaces (EPVS) from MRI. |
| Bio-Medical Large Language Models (LLMs) [69] | Specialized AI models for processing and extracting structured information from biomedical text. | Automates the extraction of standardized clinical metadata from unstructured radiology reports. |
| dcm2niix [69] | A widely used DICOM to NIfTI converter. | The first step in standardizing raw scanner data into an analysis-ready format (NIfTI). |
Data Sharing and Publishing Protocol
A responsible data sharing protocol ensures that research data contributes to the broader scientific community while adhering to ethical and legal standards.
Workflow Diagram: Protocol for Public Data Sharing
Procedure:
- Ethical and Legal Preparation: Ensure that the study's informed consent forms explicitly allow for data sharing. For data involving EU citizens, compliance with the General Data Protection Regulation (GDPR) is mandatory. This often requires strict de-identification (e.g., defacing of structural scans) and may necessitate "controlled access" rather than fully open sharing to protect participant privacy [101] [69].
- Data Curation and Standardization:
- De-identification: Remove all direct identifiers from the data. Use specialized software to remove facial features from structural MRIs to further protect identity [69].
- BIDS Conversion: Organize the entire dataset according to the Brain Imaging Data Structure (BIDS) standard. This dramatically increases the data's interoperability and reusability [101] [69].
- Documentation: Create a comprehensive "README" file and a data dictionary describing the acquisition parameters, study design, variables, and any preprocessing steps already applied.
- Repository Selection and Deposit: Select an appropriate data repository based on the data type and regulatory requirements. Options include [101] [69]:
- OpenNeuro: For general BIDS-formatted neuroimaging data.
- Brain Data Science Platform (BDSP) / BIND: For large-scale multimodal clinical imaging linked to neurophysiology.
- ConnectomeDB: For data associated with the Human Connectome Project.
- Ensure the chosen repository provides a persistent digital object identifier (DOI) for the dataset.
- Publication and Citation: Publish the dataset and cite it in any related manuscripts using its DOI. The shared data should be licensed (e.g., CCO, CC-BY) to explicitly state the terms of reuse.
Visual Communication for Accessibility
Effective communication of scientific results requires ensuring that visual materials are accessible to all audience members, including those with color vision deficiency (CVD), which affects approximately 8% of men and 0.5% of women [106].
Guidelines for Accessible Design:
- Color Palette Selection: Avoid problematic color combinations such as red-green, green-brown, blue-purple, and green-blue [106] [107]. Use online tools (e.g., Adobe Color) to check potential color schemes against CVD filters.
- Leverage Multiple Visual Cues: Do not rely on color alone to convey information. Use a combination of shapes, patterns, and textures to differentiate elements in graphs and diagrams [106] [107]. For example, use circles, squares, and triangles for data points, or apply striped, dotted, and hatched patterns to bar graphs.
- Ensure High Contrast: Maintain a high contrast ratio (WCAG 2.1 recommends at least 4.5:1) between text and its background, and between adjacent data elements [106].
- Use Direct Labels: Where possible, label graph elements and diagram parts directly instead of relying on a color-coded legend [107].
- Quality Control: Print figures in grayscale or use a CVD simulator (e.g., Coblis) to check if all critical information is preserved without color [107].
Implementing FAIR Principles for Findable, Accessible, Interoperable, and Reusable Data
The application of the FAIR principles (Findable, Accessible, Interoperable, and Reusable) has become a critical framework for managing the complex, multimodal data generated in modern brain imaging research. The transformation of neuroscience toward open science has accelerated in recent years, driven by large-scale initiatives like the BRAIN Initiative, which has established open data policies to accelerate discovery [108] [109]. Brain imaging data presents unique challenges for FAIR implementation due to the diversity of data types (fMRI, DTI, M/EEG), multiple scales of investigation, variety of experimental paradigms, and the complexity of analysis workflows [109]. The International Neuroinformatics Coordinating Facility (INCF) has played a crucial role in promoting FAIR practices in neuroscience through training, standards development, and infrastructure coordination [109].
Computational workflows are particularly important in this context as they provide tools for productivity and reproducibility that democratize access to platforms and processing know-how [110]. These workflows handle multi-step, multi-code data pipelines and analyses, transforming data inputs into desired outputs through efficient use of computational resources. When designed according to FAIR principles, these workflows maximize their value as research assets and facilitate adoption by the wider community [110]. The implementation of FAIR principles ensures that brain imaging data and analyses can be discovered, understood, and reused by researchers across the global neuroscience community, thereby accelerating progress in understanding brain function and treating neurological disorders.
FAIR Principles Framework for Brain Imaging
The FAIR principles were formulated to establish minimum requirements for scientific data to be truly useful to the broader research community. Below is an explanation of each principle as applied specifically to brain imaging data:
Findable: Brain imaging data and workflows must be easily discoverable by both humans and machines. This is achieved through assignment of globally unique persistent identifiers (e.g., DOIs), rich metadata description, and registration in searchable resources [109]. Metadata should clearly include the identifier of the data they describe to facilitate discovery.
Accessible: Once found, data should be retrievable using standardized protocols. The retrieval protocol should be open, free, and universally implementable, with provisions for authentication and authorization where necessary for privacy or data protection. Importantly, metadata should remain accessible even when the data itself is no longer available [109].
Interoperable: Brain imaging data must integrate with other data and work with applications for analysis. This requires using formal, accessible, shared languages for knowledge representation, FAIR-compliant vocabularies, and including qualified references to other data [109]. This is particularly important for multimodal brain imaging studies that combine different data types.
Reusable: Data should be well-described to enable replication and reuse in new studies. This involves having a plurality of accurate and relevant attributes, clear data usage licenses, detailed provenance, and adherence to domain-relevant community standards [109]. Comprehensive documentation enables researchers to understand and build upon previous work.
Application Notes for Brain Imaging Data
Laboratory Implementation Practices
Effective FAIR implementation begins at the laboratory level with specific practices tailored to brain imaging research:
Table 1: FAIR Implementation Practices for Research Laboratories
| FAIR Goal | Principle | Laboratory Practices for Brain Imaging |
|---|---|---|
| Findable | Unique Identifiers | Create globally unique identifiers within the lab for all key entities (subjects, imaging sessions, experiments). Implement a central registry or use existing systems (e.g., RRIDs for reagents and tools) [109]. |
| Findable | Rich Metadata | Accompany each identifier with detailed metadata (e.g., dates, experimenter, description for experiments; acquisition parameters for imaging sessions). Use identifiers consistently in file names, folder names, and database entries [109]. |
| Accessible | Authentication & Authorization | Create a centralized, accessible store for data and code under a lab-wide account to prevent data from being scattered or accessible only via personal accounts [109]. |
| Interoperable | FAIR Vocabularies | Replace idiosyncratic naming with community standards like Brain Imaging Data Structure (BIDS) and community-based ontologies. Create a lab-wide data dictionary where all variables are clearly defined [109]. |
| Reusable | Documentation | Create a "Read me" file for each dataset with notes and information for reuse. Include detailed experimental protocols and computational workflows using dedicated tools like protocols.io [109]. |
| Reusable | Community Standards | Store brain imaging files in well-supported open formats (e.g., NIfTI). Adopt community standards within the lab, especially those required by target repositories [109]. |
| Reusable | Provenance | Version datasets clearly and document differences. Keep a stable "version of record." Use dedicated provenance tracking tools like NeuroShapes and ReproNIM [109]. |
| Reusable | Licenses | Ensure data sharing agreements are in place with all collaborators. For clinical neuroimaging datasets, verify that consents permit sharing of de-identified data [109]. |
Workflow-Specific FAIR Considerations
Computational workflows for brain imaging data analysis have particular FAIR requirements that build upon general data FAIRness. The Workflows Community Initiative's FAIR Computational Workflows Working Group (WCI-FW) has identified key considerations for workflow implementation [110]:
Workflow Composition: Workflows are composed of multiple components including software, tools, containers, and sub-workflows. Each component must be FAIR itself to ensure overall workflow FAIRness [110].
Separation of Specification and Execution: A key characteristic of workflows is the separation of workflow specification from its execution. The description of the process is a form of data-describing method that must be preserved and documented [110].
Provenance Capture: Workflows should automatically capture detailed provenance including execution logs, data lineage, parameter settings, and computational environment details. This is essential for understanding and reproducing analysis results [110].
Portability and Reproducibility: Using workflow management systems (e.g., Nextflow, Snakemake) and containerized software components (e.g., Docker, Singularity) aids portability and reproducibility, though they also face challenges such as security issues in cluster deployments and learning curves [110].
Experimental Protocols for FAIR Implementation
Protocol: Implementing FAIR Data Management in a Brain Imaging Laboratory
Objective: Establish a comprehensive data management system that implements FAIR principles for all brain imaging data generated by the laboratory.
Materials and Equipment:
- Laboratory information management system (LIMS) or electronic lab notebook
- Centralized storage system with automated backup
- Data curation and validation software tools
- Persistent identifier minting system (or access to repository that provides them)
Procedure:
Data Organization Planning
- Develop a data organization scheme that structures data hierarchically: Project → Subject → Session → Data Modality
- Create standardized naming conventions for files and folders that include critical metadata elements
- Document the organization scheme in a lab data management policy
Metadata Capture
- Create standardized metadata templates for each data type (structural MRI, functional MRI, DTI, M/EEG)
- Capture both experimental metadata (subject information, experimental conditions) and technical metadata (scan parameters, software versions)
- Use controlled vocabularies and ontologies where possible (e.g., Cognitive Paradigm Ontology, Neuroimaging Data Model)
Data Quality Control
- Implement automated quality control checks for incoming imaging data
- Document quality metrics and any issues identified
- Establish protocols for addressing data quality problems
Data Processing and Analysis
- Use version-controlled, containerized analysis workflows to ensure reproducibility
- Record all processing parameters and software versions used
- Capture intermediate processing stages for potential reuse
Data Publication Preparation
- De-identify data according to relevant regulations (HIPAA, GDPR)
- Select appropriate data usage license (e.g., CC-BY, CC0)
- Prepare comprehensive documentation including README files and data dictionaries
Data Repository Submission
- Select appropriate repository based on data type and domain
- Upload data and metadata according to repository specifications
- Mint persistent identifiers for the dataset
Validation:
- Conduct internal reuse tests where lab members attempt to use each other's data based only on the provided documentation
- Perform automated compliance checks against relevant standards (e.g., BIDS validator)
- Verify that all necessary components for replication are included and properly documented
Protocol: Implementing FAIR Computational Workflows for Brain Imaging Analysis
Objective: Create reproducible, reusable computational workflows for brain imaging data analysis that adhere to FAIR principles.
Materials and Equipment:
- Workflow management system (e.g., Nextflow, Snakemake, Galaxy)
- Containerization platform (e.g., Docker, Singularity)
- Version control system (e.g., Git)
- Computational infrastructure (HPC, cloud, or local cluster)
Procedure:
Workflow Design
- Define workflow components and their relationships
- Specify data flow between components
- Identify input parameters and output products
- Document computational requirements and dependencies
Implementation
- Write workflow specification using appropriate workflow language
- Containerize each analysis component to ensure environmental reproducibility
- Implement comprehensive error handling and logging
- Include data validation steps at critical points in the workflow
Testing and Validation
- Test workflow with sample data to verify functionality
- Validate outputs against ground truth or manual analysis
- Perform scalability testing with different data sizes and computational resources
- Verify portability across different computational environments
Documentation
- Create comprehensive documentation including purpose, inputs, outputs, parameters, and dependencies
- Provide usage examples with test data
- Document known limitations and edge cases
Publication and Sharing
- Register workflow in workflow registry (e.g., WorkflowHub)
- Mint persistent identifier for the workflow
- Publish in workflow-sharing platform with appropriate metadata
- Include example datasets and validation reports
Validation:
- Independent replication of analysis results by different researchers
- Performance benchmarking across different computing environments
- Usability assessment by researchers not involved in workflow development
Data Presentation and Visualization
Repository Comparison and Selection
Selecting an appropriate repository is critical for ensuring long-term FAIR compliance of brain imaging data. The neuroscience repository landscape is organized primarily by data type, with additional specialization by domain or region.
Table 2: Comparison of Neuroscience Repositories for Brain Imaging Data
| Repository | Primary Data Types | Persistent Identifier | Metadata Standards | Data Usage License | Community Standards |
|---|---|---|---|---|---|
| OpenNeuro | Neuroimaging | DOI | DataCite | CC0 | BIDS |
| Brain Imaging Library | Neuroimaging | DOI | DATS | CC-BY | BIDS |
| DANDI | Neurophysiology | DOI | NWB | CC-BY, CC0 | NWB |
| EBRAINS | Multimodal brain data | DOI | OpenMinds | Custom | Multiple |
| CONP Portal | Multimodal neuroscience | ARK, DOI | DATS | Varies | BIDS, others |
| SPARC | Peripheral nervous system | DOI | SDS, MIS | CC-BY | SDS |
| KiltHub (FigShare) | General repository | DOI | DataCite | Multiple options | Various |
When selecting a repository for brain imaging data, consider the following criteria [109]:
- Alignment with data type and domain
- Tool support and integration
- Curation services provided
- Support for data citation
- License options available
- Data size limitations and cost structure
- Long-term sustainability plan
Repository finder tools include the INCF Infrastructure Catalog, NITRC for neuroimaging repositories, re3data catalog, and the NLM listing of repositories [109].
Quantitative Data Presentation
For quantitative data in FAIR implementation, proper presentation is essential for interpretation and reuse. The following guidelines ensure clear communication of quantitative information [111] [112]:
Frequency Tables: Group quantitative data into class intervals for concise presentation. intervals should be equal in size, with typically 5-20 classes depending on the data spread [112].
Histograms: Use for displaying distribution of quantitative data, with class intervals on the horizontal axis and frequencies on the vertical axis. Bars should be contiguous since the data are continuous [112].
Frequency Polygons: Created by joining midpoints of histogram bars, useful for comparing multiple distributions on the same diagram [112].
Line Diagrams: Ideal for showing trends over time, such as data throughput or repository growth metrics [112].
Workflow Visualization
The following diagrams illustrate key workflows and relationships in FAIR implementation for brain imaging research.
FAIR Data Management Workflow
FAIR Stakeholder Ecosystem
Computational Workflow Architecture
Research Reagent Solutions and Materials
Implementation of FAIR principles for brain imaging data requires specific tools, platforms, and resources. The following table details essential solutions for establishing a FAIR-compliant research environment.
Table 3: Essential Research Reagents and Solutions for FAIR Brain Imaging Research
| Resource Type | Specific Solutions | Function in FAIR Implementation |
|---|---|---|
| Data Standards | Brain Imaging Data Structure (BIDS) | Standard for organizing and describing neuroimaging data to ensure interoperability [109] |
| Data Standards | NeuroData Without Borders (NWB) | Standard for neurophysiology data enabling data sharing and reuse [109] |
| Workflow Systems | Nextflow, Snakemake, Galaxy | Workflow management systems that automate analysis pipelines and enhance reproducibility [110] |
| Containerization | Docker, Singularity | Create reproducible computational environments for analysis components [110] |
| Repositories | OpenNeuro, Brain Imaging Library | Domain-specific repositories for sharing brain imaging data with community standards [109] |
| Repositories | DANDI, EBRAINS | Specialized repositories for neurophysiology and multimodal brain data [109] |
| Identifier Systems | Digital Object Identifiers (DOI) | Provide persistent identifiers for datasets and workflows [109] |
| Metadata Standards | DataCite, DATS | Standardized metadata schemas for describing research data [109] |
| Provenance Tools | ReproNim, NeuroShapes | Tools for capturing and representing data provenance and processing history [109] |
| Community Infrastructure | INCF Knowledge Space | Search and discovery platform for neuroscience resources across distributed repositories [109] |
Case Study: TotalSegmentator MRI - FAIR in Practice
A recent exemplary implementation of FAIR principles in brain imaging is the TotalSegmentator MRI tool, which received the 2025 Alexander R. Margulis Award for the best original scientific article published in Radiology [113]. This case demonstrates practical application of FAIR in several key areas:
Open Science Implementation: The researchers released the full model, training data, and annotations publicly, embodying the accessibility principle of FAIR. This open approach has driven widespread community engagement, with new MRI segmentation tools emerging almost weekly that benchmark against TotalSegmentator MRI [113].
Interoperability Achievement: The tool demonstrates interoperability through its sequence-agnostic design, functioning across diverse MRI protocols and overcoming a key limitation of traditional methods that require sequence-specific training. This enhances robustness and clinical versatility [113].
Reusability Evidence: The model was applied to a large internal dataset of 8,672 abdominal MRI scans to analyze age-related changes in organ volumes, demonstrating direct reusability for different research questions. This would have been impractical with manual segmentation approaches [113].
Findability Enhancement: As an award-winning publication in a prominent journal with open availability, the tool achieves high findability. The associated code and data are accessible through standard repositories, further enhancing discoverability [113].
This case study illustrates how FAIR implementation in brain imaging tools leads to accelerated innovation, validation, and adoption across the research community, ultimately advancing the field more rapidly than closed, non-standardized approaches.
The implementation of FAIR principles for brain imaging data analysis workflows represents a fundamental shift in how neuroscience research is conducted, shared, and built upon. As the field continues to generate increasingly complex and multimodal data, systematic application of Findable, Accessible, Interoperable, and Reusable practices becomes essential for scientific progress. The framework presented in these application notes and protocols provides a practical roadmap for researchers, laboratories, and institutions to enhance the value and impact of their brain imaging research.
Successful FAIR implementation requires collaboration across multiple stakeholders—research laboratories must adopt standardized practices, repositories must provide robust infrastructure, community organizations must develop and maintain standards, and funders must support sustainable ecosystems. Computational workflows play a particularly important role as they encapsulate methodological expertise and ensure reproducibility of complex analyses. As demonstrated by emerging tools like TotalSegmentator MRI, open FAIR-compliant approaches accelerate innovation and validation across the research community.
Moving forward, the neuroscience community must continue to develop and adopt standards, tools, and practices that lower barriers to FAIR implementation. The ultimate goal is a research ecosystem where brain imaging data and analyses can be seamlessly discovered, understood, and built upon by researchers across the globe, dramatically accelerating our understanding of brain function and our ability to treat neurological disorders.
Evaluating Model Generalizability and Clinical Translation of AI Algorithms
Translating artificial intelligence (AI) algorithms from research environments into clinical practice requires demonstrated generalizability of models to real-world data. One of the most significant obstacles to this generalizability is data shift, a data distribution mismatch between the model's training environment and the real-world clinical environments where it is deployed [114]. Most medical AI is trained with datasets gathered from limited environments, such as restricted disease populations and center-dependent acquisition conditions. When these models encounter data from different hospitals, patient demographics, or imaging equipment, their performance often decreases significantly—a phenomenon observed when models trained at one hospital fail at others [114]. This application note provides structured protocols and analytical frameworks for rigorously evaluating and improving model generalizability within brain imaging data analysis workflows.
Quantitative Frameworks for Generalizability Assessment
Systematic evaluation requires quantifying performance across diverse data populations. The following metrics and validation frameworks are essential for assessing model robustness.
Table 1: Key Quantitative Metrics for Generalizability Assessment
| Metric Category | Specific Metric | Interpretation in Clinical Translation |
|---|---|---|
| Performance Stability | Drop in AUC/Accuracy on external test sets | Indicates susceptibility to data shift; a drop >10% often signals significant generalizability problems [114]. |
| Data Shift Susceptibility | Performance variation across patient subgroups (age, sex, disease severity) | Reveals hidden biases; models should maintain performance across all relevant clinical subgroups [115]. |
| Out-of-Distribution Detection | Ability to flag samples deviating from training distribution | Critical for clinical safety; alerts when model operates outside its validated domain [115]. |
| Explainability Consistency | Stability of saliency maps/feature importance across sites | Ensures model uses clinically relevant features rather than spurious correlations [114]. |
Table 2: Multi-Center Validation Framework for Brain Imaging AI
| Validation Tier | Data Characteristics | Primary Objective | Acceptance Criteria |
|---|---|---|---|
| Internal Hold-Out | Random split from original dataset | Estimate baseline performance under IID assumption | AUC > 0.90, F1 > 0.85 for diagnostic tasks [114] |
| Temporal Validation | Data collected after training period | Assess temporal drift and model decay | Performance drop < 5% from internal validation [115] |
| External Geographic | Data from different hospitals/regions | Evaluate geographic generalizability | Performance drop < 10%, maintained AUC > 0.80 [114] [115] |
| Prospective Clinical | Data from routine clinical practice | Final validation before implementation | Clinical utility proven, no patient harm, usability feedback incorporated [113] |
Experimental Protocols for Generalizability Testing
Protocol 1: Cross-Site Performance Validation
Objective: To evaluate model performance across multiple clinical sites and identify performance degradation due to data shift.
Materials:
- Pre-trained AI model for brain imaging analysis (e.g., segmentation, classification)
- Internal test set from development site (N ≥ 100)
- External test sets from ≥3 independent clinical sites (N ≥ 50 per site)
- Computing infrastructure for model inference and evaluation
Procedure:
- Baseline Assessment: Run model inference on internal test set to establish baseline performance (AUC, sensitivity, specificity, Dice coefficient for segmentation tasks).
- External Testing: Execute identical inference pipeline on each external test set without model retraining.
- Performance Comparison: Calculate performance metrics for each external set and compare against baseline.
- Statistical Analysis: Perform McNemar's test for classification models or paired t-tests for segmentation metrics to identify statistically significant performance differences (p < 0.05).
- Shift Characterization: For sites showing significant performance drop, analyze potential shift sources (demographics, scanner differences, protocol variations).
Deliverables:
- Performance comparison table across all sites
- Visualization of performance variation (box plots)
- Report on identified data shift factors and their impact
Protocol 2: Explainability-Driven Failure Analysis
Objective: To use explainable AI (XAI) techniques to identify model susceptibility to data shift and spurious feature correlations.
Materials:
- Model with demonstrated performance variance across sites
- Representative samples from each site (N ≥ 20 per site)
- XAI toolbox (e.g., SHAP, LIME, Grad-CAM)
- Domain expert (radiologist/neurologist) for annotation
Procedure:
- Saliency Map Generation: Apply XAI methods to generate feature importance maps for correct and incorrect predictions across sites.
- Expert Evaluation: Domain expert evaluates saliency maps for clinical plausibility without knowing prediction correctness (blinded review).
- Feature Correlation Analysis: Identify non-anatomical or institution-specific features that disproportionately influence predictions (e.g., scanner-specific artifacts, positioning aids).
- Consistency Scoring: Develop quantitative scores for explainability consistency across sites.
- Failure Pattern Documentation: Categorize failure modes and link to specific data shift types.
Deliverables:
- Catalog of spurious features influencing predictions
- Expert-validated assessment of feature plausibility
- Recommendations for dataset augmentation to mitigate identified failures
Diagram 1: Explainability-Driven Data Shift Analysis Workflow
Protocol 3: Prospective Simulation for Clinical Deployment
Objective: To simulate real-world clinical deployment and identify workflow integration challenges before actual implementation.
Materials:
- Validated AI model with demonstrated cross-site performance
- Clinical workflow simulation environment
- Sample clinical cases (N ≥ 30) with varying complexity
- Clinical staff (radiologists, technicians) for usability testing
Procedure:
- Workflow Integration: Deploy model in clinical simulation environment matching target institution's PACS/RIS systems.
- Silent Mode Operation: Run model in "silent mode" where predictions are generated but not shown to clinicians, collecting performance data in background.
- Usability Testing: Introduce model predictions to clinical staff in controlled setting, collecting feedback on interface, trust, and integration points.
- Time-Motion Study: Measure time savings or delays introduced by AI integration.
- Failure Mode Analysis: Document all incorrect predictions and near-miss scenarios, assessing potential clinical impact.
Deliverables:
- Clinical workflow integration assessment
- Usability and interface improvement recommendations
- Go/No-Go decision for full clinical deployment
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools for AI Generalizability Research
| Tool Category | Specific Solution | Function in Generalizability Research |
|---|---|---|
| Data Harmonization | ComBat, RemoveBatchEffects | Statistical harmonization of multi-site imaging data to reduce scanner and protocol effects while preserving biological signals. |
| Automated Processing | ABIDA Toolbox [55] | Streamlines preprocessing of resting-state fMRI data with standardized pipelines, reducing operational complexity and variability. |
| Segmentation Engines | TotalSegmentator MRI [113] | Provides robust, sequence-agnostic segmentation of anatomic structures; cross-modal training (CT+MRI) improves generalization. |
| Explainability Frameworks | SHAP, LIME, Grad-CAM | Identifies features driving predictions, detects spurious correlations, and validates clinical plausibility across sites. |
| Domain Adaptation | DANN, ADDA | Algorithmic approaches to adapt models to new domains with limited labeled data, improving performance on shifted distributions. |
| Performance Monitoring | Custom drift detection scripts | Monitors model performance in production, alerting to data drift and performance degradation in real-time. |
Implementation Framework for Clinical Translation
Successful translation of AI algorithms from research to clinical practice requires systematic addressing of data shift challenges. The TotalSegmentator MRI project demonstrates a successful approach, where training on diverse datasets from multiple institutions and combining different imaging modalities (CT and MRI) actually improved segmentation performance and generalizability [113]. This suggests multi-modal training can serve as a form of data augmentation, helping models generalize better across different clinical environments.
Diagram 2: Clinical Translation Pathway for AI Algorithms
Implementation should also address the "last-mile" challenges of clinical integration, including workflow compatibility, interpretability demands, and ethical considerations. Lack of interpretability in AI models poses significant trust and transparency issues in clinical settings, advocating for transparent algorithms and requiring rigorous testing on specific hospital populations before implementation [115]. Furthermore, emphasizing human judgment alongside AI integration is essential to mitigate the risks of deskilling healthcare practitioners while leveraging the benefits of AI assistance.
Ongoing evaluation processes and adjustments to regulatory frameworks are crucial for ensuring the ethical, safe, and effective use of AI in clinical decision support. This includes addressing population shifts that occur when prediction models are applied to populations that don't match the underlying distribution of the training population, which can happen due to changes in hospital, hardware, laboratory protocol, or drift in population over time [115]. By implementing the protocols and frameworks outlined in this document, researchers can systematically address these challenges and accelerate the translation of robust AI tools into clinical brain imaging workflows.
Conclusion
The evolution of brain imaging data analysis is marked by a decisive shift towards standardization, automation, and intelligence. The adoption of frameworks like BIDS and reproducible workflow tools lays a necessary foundation for reliable science. Meanwhile, the integration of AI and deep learning offers unprecedented power for feature extraction and disease classification, pushing the boundaries of personalized medicine. The future of the field hinges on overcoming key challenges in computational scalability, model interpretability, and the seamless translation of analytical findings into clinically actionable insights. Success will require continued collaboration to refine best practices, develop open-source tools, and build even larger, more diverse datasets to power the next generation of discoveries in neuroscience and drug development.
References
- 1. The Brain Imaging Data Structure: BIDS [https://bids.neuroimaging.io/index.html]
- 2. Introduction - Brain Imaging Data Structure 1.10.1 [https://bids-specification.readthedocs.io/en/stable/introduction.html]
- 3. Curation of BIDS (CuBIDS): A workflow and software package ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9981813/]
- 4. Brain Imaging Data Structure [https://en.wikipedia.org/wiki/Brain_Imaging_Data_Structure]
- 5. Introduction to BIDS | Behavior and Neuroimaging Core ... [https://docs.ccv.brown.edu/bnc-user-manual/bids/introduction-to-bids]
- 6. Motion-BIDS: an extension to the brain imaging data ... [https://www.nature.com/articles/s41597-024-03559-8]
- 7. Integrated brain connectivity analysis with fMRI, DTI, and ... [https://www.sciencedirect.com/science/article/pii/S1361841525001173]
- 8. The advantage of combining MEG and EEG - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC2706118/]
- 9. Comparison to fMRI in focally stimulated visual cortex [https://www.sciencedirect.com/science/article/abs/pii/S1053811907002133]
- 10. Comparing MEG and EEG measurement set-ups for a brain ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0319328]
- 11. Neuroimaging Is The Future of CNS Drug Development [https://neurotechnology.substack.com/p/neuroimaging-is-the-future-of-cns]
- 12. A large-scale MEG and EEG dataset for object recognition ... [https://www.nature.com/articles/s41597-025-05174-7]
- 13. UK Biobank: Health research data for the world [https://www.ukbiobank.ac.uk/]
- 14. Data releases [https://www.ukbiobank.ac.uk/about-our-data/data-releases/]
- 15. Data release v20 [https://community.ukbiobank.ac.uk/hc/en-gb/articles/26655455734301-Data-release-v20]
- 16. Data Sharing [https://abcdstudy.org/scientists/data-sharing/]
- 17. Architecture - OpenNeuro documentation [https://docs.openneuro.org/architecture.html]
- 18. OpenNeuro documentation [https://docs.openneuro.org/]
- 19. ADNI | Subject Characteristics [https://adni.loni.usc.edu/data-samples/adni-data/subject-characteristics/]
- 20. ADNI Data [https://adni.loni.usc.edu/data-samples/adni-data/]
- 21. Advanced Brain Age Prediction Using Multi-Head Self ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12036470/]
- 22. Longer scans boost prediction and cut costs in brain-wide ... [https://www.nature.com/articles/s41586-025-09250-1]
- 23. Big Data in Neuroimaging: Infrastructure, Challenges, and ... [https://www.alliedacademies.org/articles/big-data-in-neuroimaging-infrastructure-challenges-and-future-perspectives-32724.html]
- 24. DeepPrep: an accelerated, scalable and robust pipeline for ... [https://www.nature.com/articles/s41592-025-02599-1]
- 25. Data analytics for high-throughput image-based cohort ... [https://www.fz-juelich.de/en/jsc/about-us/structure/simulation-and-data-labs/sdl-neuroscience/research/data-analytics-for-high-throughput-image-based-cohort-phenotyping]
- 26. Democratizing open neuroimaging: Neurodesk's approach ... [https://apertureneuro.org/article/144107-democratizing-open-neuroimaging-neurodesk-s-approach-to-open-data-accessibility-and-utilization]
- 27. A reproducible and generalizable software workflow for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12224434/]
- 28. A Data-Intensive Pipeline to Map the Human Brain ... [https://repositories.lib.utexas.edu/items/48e67fc7-aa4c-4591-9654-2c3e5b5141ba]
- 29. Neurodesk [https://neurodesk.org/]
- 30. Best Practices for Cloud-Based Neuroimaging Research [https://flywheel.io/insights/blog/best-practices-guide-resources-cloud-based-neuroimaging-research]
- 31. Neuroimaging research pipelines group [https://ohbm-environment.org/neuroimaging-research-pipelines-group/]
- 32. USLR: An open-source tool for unbiased and smooth ... [https://www.sciencedirect.com/science/article/pii/S1361841525002099]
- 33. Data-guided neuroimaging and visualization [https://apertureneuro.org/article/140427-data-guided-neuroimaging-and-visualization-from-functional-decomposition-to-dynamic-fusion]
- 34. Systematic evaluation of fMRI data-processing pipelines for ... [https://www.nature.com/articles/s41467-024-48781-5]
- 35. Top Neurology Imaging Data Management Challenges [https://flywheel.io/insights/blog/solving-challenges-around-neurology-imaging-data-management]
- 36. Virtual Brain Inference (VBI): A flexible and integrative ... [https://elifesciences.org/reviewed-preprints/106194v1]
- 37. CIVET-Macaque: An automated pipeline for MRI-based ... [https://www.sciencedirect.com/science/article/pii/S1053811920311071]
- 38. PANDA: a pipeline toolbox for analyzing brain diffusion ... [https://www.frontiersin.org/journals/human-neuroscience/articles/10.3389/fnhum.2013.00042/full]
- 39. PANDA: a pipeline toolbox for analyzing brain diffusion images [https://pmc.ncbi.nlm.nih.gov/articles/PMC3578208/]
- 40. Data Processing Assistant for Resting-State fMRI (DPARSF ... [http://www.rfmri.org/dparsf_v2_2]
- 41. DPARSF: a MATLAB toolbox for "pipeline" data analysis of ... [https://www.frontiersin.org/journals/systems-neuroscience/articles/10.3389/fnsys.2010.00013/full]
- 42. A standardized image processing and data quality platform ... [https://www.nature.com/articles/s41467-024-50826-8]
- 43. Frontiers | Parallel workflow tools to facilitate human brain MRI... [https://www.frontiersin.org/journals/neuroscience/articles/10.3389/fnins.2015.00171/full]
- 44. Interfaces and Workflows - Nipype - Read the Docs [https://nipype.readthedocs.io/en/latest/interfaces.html]
- 45. Neuroimaging in Python - Pipelines and Interfaces — nipy ... [https://nipype.readthedocs.io/]
- 46. Efficient, Distributed and Interactive Neuroimaging Data ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2718780/]
- 47. LONI Pipeline Processing Environment [https://loni.usc.edu/research/software?name=Pipeline]
- 48. Workflow from scratch - Nipype [https://nipype.readthedocs.io/en/latest/users/examples/workflow_from_scratch.html]
- 49. A deep learning approach for brain tumour classification ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1508326/full]
- 50. Effective workflow from multimodal MRI data to model- ... [https://www.nature.com/articles/s41598-025-04511-5]
- 51. Brain image data processing using collaborative ... [https://pubmed.ncbi.nlm.nih.gov/39050044/]
- 52. Pypes: Workflows for Processing Multimodal Neuroimaging ... [https://www.frontiersin.org/journals/neuroinformatics/articles/10.3389/fninf.2017.00025/full]
- 53. A Deep Learning Framework for Brain Tumor Detection ... [https://www.sciencedirect.com/science/article/pii/S277294192500208X]
- 54. A novel neuroimaging based early detection framework for ... [https://www.nature.com/articles/s41598-025-05529-5]
- 55. ABIDA: An Automated Brain Imaging Data Processing and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12316811/]
- 56. Subtyping schizophrenia via machine learning by using ... [https://www.nature.com/articles/s41398-025-03704-w]
- 57. Neuroimaging Data Informed Mood and Psychosis ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12421244/]
- 58. A Clinical Neuroimaging Platform for Rapid, Automated ... [https://www.medrxiv.org/content/10.1101/2025.05.09.25327310v1]
- 59. Blood-based biomarkers and neuroimaging for early detection ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12368349/]
- 60. A hitchhiker′s guide to working with large, open-source ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7992920/]
- 61. Human Neuroimaging as a “Big Data” Science - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3983169/]
- 62. Brain image data processing using collaborative ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11266044/]
- 63. Pennsieve: A Collaborative Platform for Translational ... [https://www.nature.com/articles/s41597-025-06075-5]
- 64. A Practical Guide for Generating Reproducible and ... [https://apertureneuro.org/article/85104-a-practical-guide-for-generating-reproducible-and-programmatic-neuroimaging-visualizations]
- 65. Analysis and Visualization Tools [https://nwb.org/tools/analysis/]
- 66. Principles of Effective Data Visualization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7733875/]
- 67. Understanding WCAG 2 Contrast and Color Requirements [https://webaim.org/articles/contrast/]
- 68. Understanding Success Criterion 1.4.11: Non-text Contrast [https://www.w3.org/WAI/WCAG21/Understanding/non-text-contrast.html]
- 69. The Brain Imaging and Neurophysiology Database (BIND) [https://bdsp.io/content/n1vba1x5qt62frfjem65/1.0/]
- 70. The relation between statistical power and inference in fMRI [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0184923]
- 71. Power failure: why small sample size undermines ... [https://www.nature.com/articles/nrn3475]
- 72. Statistical power in network neuroscience [https://www.sciencedirect.com/science/article/abs/pii/S136466132200328X]
- 73. Is the Statistic Value All We Should Care about in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6591724/]
- 74. DICOM datasets for reproducible neuroimaging research ... [https://www.nature.com/articles/s41597-025-05503-w]
- 75. MRS-BIDS, an extension to the Brain Imaging Data ... [https://www.nature.com/articles/s41597-025-05543-2]
- 76. Parallelism in Computing: A Deep Dive for 2025 [https://gganbumarketplace.com/ai_artificial_intelligence/parallelism-in-computing-2025/]
- 77. MCP Data Parallelism: Techniques & Trends 2025 [https://www.byteplus.com/en/topic/541942]
- 78. State of the Art in Parallel Programming for High ... [https://medium.com/@msaaduddin/state-of-the-art-in-parallel-programming-for-high-performance-computing-2025-82af1005c759]
- 79. Machine Learning in MRI Brain Imaging: A Review ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12609805/]
- 80. Using Deep Learning for Brain Imaging Data Analysis [https://www.news-medical.net/health/Using-Deep-Learning-for-Brain-Imaging-Data-Analysis.aspx]
- 81. Mastering Explainable AI in 2025: A Beginner's Guide to ... [https://superagi.com/mastering-explainable-ai-in-2025-a-beginners-guide-to-transparent-and-interpretable-models/]
- 82. Transfer deep learning and explainable AI framework for ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1618550/full]
- 83. Enhancing generalization in whole-body MRI-based deep ... [https://www.sciencedirect.com/science/article/pii/S266652122500081X]
- 84. Decoding Black Box AI: The Global Push for Explainability ... [https://trendsresearch.org/insight/decoding-black-box-ai-the-global-push-for-explainability-and-transparency/?srsltid=AfmBOoo8FIuIhmG1UmSF9y8put_LVSRbJZlcXn2V3_VPX9Ebec6-7icA]
- 85. brainlife.io: a decentralized and open-source cloud ... [https://www.nature.com/articles/s41592-024-02237-2]
- 86. Automated quality control of T1-weighted brain MRI scans ... [https://pubmed.ncbi.nlm.nih.gov/40800787/]
- 87. Automatic quality control of brain 3D FLAIR MRIs for a ... [https://www.sciencedirect.com/science/article/abs/pii/S1361841525001641]
- 88. ESMRMB 2025 focus topic: cycle of quality—from concept to ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12255560/]
- 89. Image-Based Meta- and Mega-Analysis (IBMMA): A Unified ... [https://www.sciencedirect.com/science/article/pii/S1053811925005579]
- 90. Establishment and validation of predictive model of ARDS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11730794/]
- 91. A standardized analytics pipeline for reliable and rapid ... [https://www.sciencedirect.com/science/article/pii/S0169260721004685]
- 92. Building a Robust Data Cleaning and Validation Pipeline [https://skillwisor.com/2025/06/25/building-a-robust-data-cleaning-and-validation-pipeline-a-step-by-step-guide/]
- 93. Development and validation of a deep learning-based ... [https://www.sciencedirect.com/science/article/pii/S2589537024003511]
- 94. Exploring the impact of analysis software on task fMRI results [https://pmc.ncbi.nlm.nih.gov/articles/PMC6618324/]
- 95. Comparative reliability analysis of publicly available ... [https://pubmed.ncbi.nlm.nih.gov/25570458/]
- 96. Chapter #3: FIR Analysis in FSL - Andy's Brain Book! [https://andysbrainbook.readthedocs.io/en/latest/FIR/FIR_ShortCourse/FIR_03_FSL.html]
- 97. why the results of same preprocessing steps are so different in ... [https://discuss.afni.nimh.nih.gov/t/why-the-results-of-same-preprocessing-steps-are-so-different-in-afni-and-spm-these-two-toolbox/7347]
- 98. What is the best software for processing fMRI data? [https://mriquestions.com/best-fmri-software.html]
- 99. Freesurfer – Knowledge and References [https://taylorandfrancis.com/knowledge/Engineering_and_technology/Biomedical_engineering/Freesurfer/]
- 100. Brain Imaging And Neuroimaging Market 2025 [https://www.linkedin.com/pulse/brain-imaging-neuroimaging-market-2025-artificial-fb3wf/]
- 101. Which infrastructure can I use to share human ... [https://apertureneuro.org/article/144839-which-infrastructure-can-i-use-to-share-human-neuroimaging-data-a-survey-and-literature-review-on-current-solutions-for-eu-researchers]
- 102. HCP Young Adult - Connectome [https://www.humanconnectome.org/study/hcp-young-adult/data-releases]
- 103. fMRI data analysis [https://bio-protocol.org/exchange/minidetail?id=17927810&type=30]
- 104. Quantitative assessment of brain glymphatic imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307369/]
- 105. DTI-ALPS mapping: A Novel Method for Analyzing ... [https://archive.ismrm.org/2025/4796.html]
- 106. Color Blind Design Guidelines: A Comprehensive Guide [https://venngage.com/blog/color-blind-design/]
- 107. How to design a colour blind-friendly scientific poster [https://www.animateyour.science/post/how-to-design-a-colour-blind-friendly-scientific-poster]
- 108. BRAIN 2025: A Scientific Vision - BRAIN Initiative - NIH [http://braininitiative.nih.gov/vision/nih-brain-initiative-reports/brain-2025-scientific-vision]
- 109. Psychology and Neuroscience - Data Management for Research [https://guides.library.cmu.edu/researchdatamanagement/FAIR_psychneuro]
- 110. Applying the FAIR Principles to computational workflows [https://www.nature.com/articles/s41597-025-04451-9]
- 111. Presentation of Quantitative Data [https://ihatepsm.com/blog/presentation-quantitative-data]
- 112. Presenting Quantitative Data Graphically [https://courses.lumenlearning.com/waymakermath4libarts/chapter/presenting-quantitative-data-graphically/]
- 113. 2025 Margulis Award | RSNA [https://www.rsna.org/news/2025/november/2025-margulis-award]
- 114. Translating AI to Clinical Practice: Overcoming Data Shift with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10190133/]
- 115. Artificial intelligence in clinical decision support and the ... [https://www.frontiersin.org/journals/digital-health/articles/10.3389/fdgth.2025.1403047/full]