Assessing Segmentation Tool Reliability for Contrast-Enhanced MRI: A Guide for Robust Neuroimaging Research
This article provides a comprehensive analysis of the reliability and performance of various automated segmentation tools when applied to contrast-enhanced magnetic resonance imaging (CE-MR) scans.
Assessing Segmentation Tool Reliability for Contrast-Enhanced MRI: A Guide for Robust Neuroimaging Research
Abstract
This article provides a comprehensive analysis of the reliability and performance of various automated segmentation tools when applied to contrast-enhanced magnetic resonance imaging (CE-MR) scans. It explores the foundational challenges posed by technical heterogeneity in clinical CE-MR data and evaluates the impact of scanner and software variability on volumetric measurements. Methodological insights cover advanced deep learning approaches, such as SynthSeg+, which demonstrate high consistency between CE-MR and non-contrast scans. The content further addresses troubleshooting common pitfalls and offers optimization strategies for cross-sectional and longitudinal studies. Finally, it presents a rigorous validation and comparative framework, synthesizing performance metrics across tools to guide researchers and drug development professionals in selecting and implementing segmentation software for reliable, clinically translatable brain morphometric analysis.
The Foundational Challenge: Why CE-MR Scans Are Problematic for Automated Volumetry
Clinical brain magnetic resonance imaging (MRI) scans, including contrast-enhanced (CE-MR) images, represent a vast and underutilized resource for neuroscience research due to technical heterogeneity. These archives, accumulated through routine diagnostic procedures, contain invaluable data on brain structure and disease progression across diverse populations. However, the variability in acquisition parameters, scanner types, and imaging protocols has traditionally limited their research utility. This heterogeneity introduces confounding factors that complicate automated analysis and large-scale retrospective studies.
The reliability of morphometric measurements derived from these varied sources is paramount for producing valid scientific insights. Within this context, the development of robust segmentation tools capable of handling such heterogeneity is transforming the research landscape. Advanced deep learning approaches are now enabling researchers to extract consistent volumetric measurements from clinically acquired CE-MR images, potentially unlocking previously inaccessible datasets for neuroimaging research and drug development [1] [2]. This guide provides a comparative analysis of leading segmentation methodologies, evaluating their performance in overcoming technical heterogeneity to leverage CE-MR scans for scientific discovery.
Comparative Analysis of Segmentation Tools
Performance Benchmarking on CE-MR vs. Non-Contrast MR
The core challenge in utilizing clinical CE-MR scans lies in ensuring that volumetric measurements derived from them are as reliable as those from non-contrast MR (NC-MR) scans, which are typically acquired in controlled research settings. A direct comparative study evaluated this reliability using two segmentation tools: the deep learning-based SynthSeg+ and the more traditional CAT12 pipeline [1] [2].
Table 1: Comparative Reliability of Segmentation Tools on CE-MR vs. NC-MR Scans
| Segmentation Tool | Technical Approach | Overall Reliability (ICC) | Structures with Highest Reliability (ICC >0.94) | Structures with Notable Discrepancies |
|---|---|---|---|---|
| SynthSeg+ | Deep learning-based; contrast-agnostic | High (ICCs >0.90 for most structures) [1] | Larger brain structures [2] | Cerebrospinal fluid (CSF) and ventricular volumes [1] |
| CAT12 | Traditional pipeline; depends on intensity normalization | Inconsistent performance [1] | Information not specified | Relatively higher discrepancies between CE-MR and NC-MR [2] |
The findings indicate that SynthSeg+ demonstrates superior robustness to the variations introduced by gadolinium-based contrast agents. Its high intraclass correlation coefficients (ICCs) across most brain structures suggest it can reliably process CE-MR scans for morphometric analysis, making it a suitable tool for repurposing clinical archives. Inconsistent performance of CAT12 is likely due to its higher sensitivity to intensity changes, which affects its ability to generalize across different scan types [1] [2].
Tool Generalizability and Application in Disease Research
Beyond basic volumetric agreement, the value of a tool is measured by its generalizability across diverse real-world conditions and its ability to derive meaningful clinical biomarkers.
Table 2: Generalizability and Application of Segmentation Tools
| Tool / Model | Key Strength | Validation Context | Performance Metric |
|---|---|---|---|
| MindGlide | Processes any single MRI contrast (T1, T2, FLAIR, PD); efficient (<1 min/scan) [3] | Multiple Sclerosis (MS) clinical trials and routine-care data [3] | Detected treatment effects on lesion accrual and grey matter loss; Dice score: 0.606 vs. expert-labelled lesions [3] |
| MM-MSCA-AF | Multi-modal multi-scale contextual aggregation with attention fusion [4] | Brain tumor segmentation (BRATS 2020 dataset) [4] | Dice score: 0.8158 for necrotic core; 0.8589 for whole tumor [4] |
| SynthSeg Framework | Trained on synthetic data with randomized contrasts; does not require real annotated MRI data [5] | Abdominal MRI segmentation (extension of original brain model) [5] | Offers alternative when annotated MRI data is scarce; slightly less accurate than models trained on real data [5] |
The performance of MindGlide is particularly noteworthy. Its ability to work on any single contrast and its validation in detecting treatment effects in clinical trials directly addresses the thesis of repurposing heterogeneous clinical scans for research. Its higher Dice score compared to other state-of-the-art tools like SAMSEG and WMH-SynthSeg in segmenting white matter lesions further underscores the efficacy of advanced deep learning models in this domain [3].
Experimental Protocols for Benchmarking Segmentation Tools
To ensure the reliability and reproducibility of studies aiming to utilize clinical CE-MR scans, adhering to rigorous experimental methodologies is critical. The following section outlines the key protocols from cited studies.
Protocol 1: Comparative Reliability Study
This protocol is designed to directly assess the consistency of volumetric measurements between CE-MR and NC-MR scans.
- Dataset: The study utilized paired T1-weighted CE-MR and NC-MR scans from 59 clinically normal participants (age range: 21-73 years). Initially, 63 image pairs were collected, but 4 were excluded due to segmentation failures with one of the tools, highlighting a practical challenge in automated processing [2].
- Segmentation Tools: The images were processed in parallel using two segmentation tools: CAT12 (a standard SPM-based pipeline) and SynthSeg+ (a deep learning-based tool designed to be robust to contrast and scanner variations) [1] [2].
- Analysis: Volumetric measurements for various brain structures were extracted from the segmentations generated by both tools. The primary statistical analysis involved calculating Intraclass Correlation Coefficients (ICCs) to evaluate the agreement between measurements from CE-MR and NC-MR scans for the same individual. Furthermore, the utility of both scan types was evaluated by building age prediction models based on the volumetric outputs [1] [2].
Protocol 2: Validation in Clinical Trials and Real-World Data
This protocol validates a tool's performance in detecting biologically meaningful changes in heterogeneous data, which is the ultimate goal of repurposing clinical scans.
- Model Training: MindGlide was trained on a large dataset of 4,247 real MRI scans from 2,934 MS patients across 592 scanners, augmented with 4,303 synthetic scans. This extensive and varied training set is crucial for developing robustness to heterogeneity [3].
- External Validation: The model was frozen and tested on an independent external validation set comprising 14,952 scans from 1,001 patients. This set included data from two progressive MS clinical trials and a real-world routine-care paediatric MS cohort, featuring a mix of T1, T2, FLAIR, and Proton Density (PD) contrasts with diverse slice thicknesses [3].
- Outcome Measures: The model was evaluated on its ability to:
- Segment white matter lesions (compared to expert manual labels using the Dice score) [3].
- Correlate lesion load and deep grey matter volume with clinical disability scores (EDSS) [3].
- Detect statistically significant treatment effects on lesion accrual and brain volume loss in clinical trial settings [3].
Visualizing Workflows and Performance
The following diagrams illustrate the experimental workflow for benchmarking segmentation tools and the relationship between tool characteristics and their suitability for clinical scan repurposing.
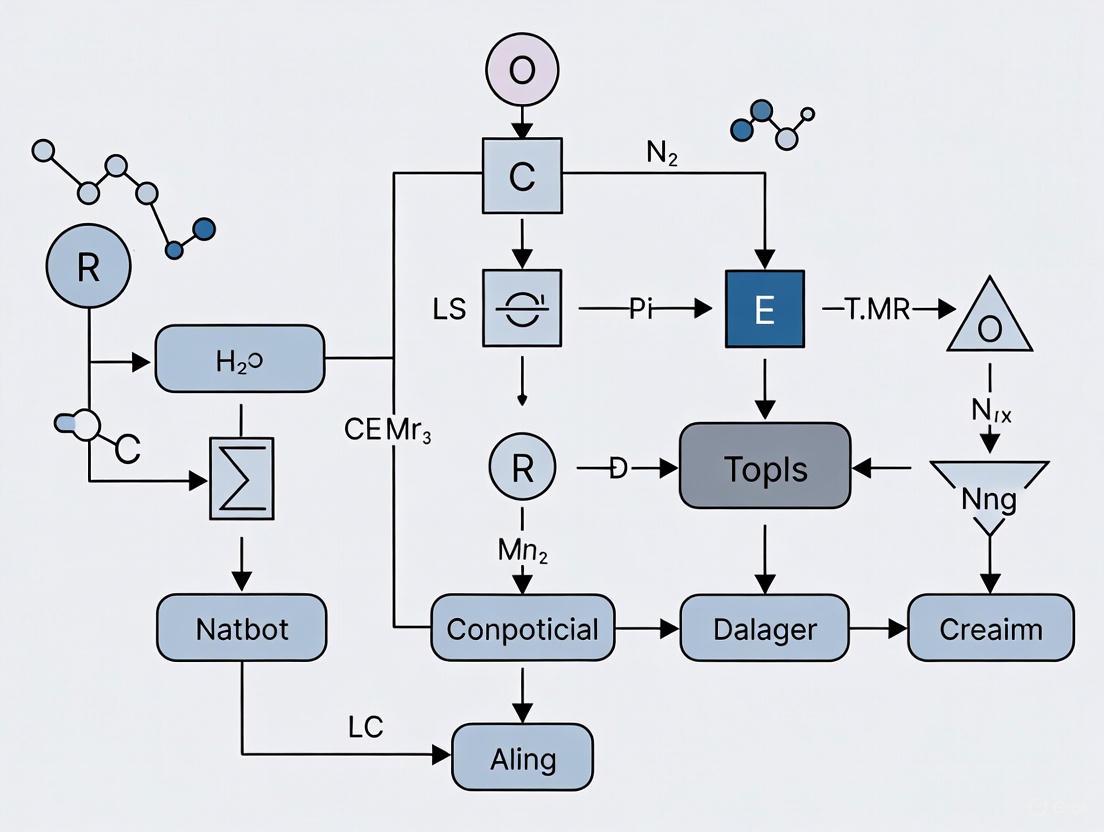
Diagram 1: Tool Benchmarking Workflow. This flowchart outlines the key steps for evaluating the reliability of segmentation tools on contrast-enhanced versus non-contrast MRI scans, from data input to final assessment.
Diagram 2: From Tool Robustness to Research Value. This diagram shows the logical relationship where a tool's robustness enables it to handle technical heterogeneity, which in turn unlocks the potential for repurposing clinical scans for research.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Software and Computational Tools for CE-MR Research
| Tool / Resource | Type | Primary Function in Research | Notable Features |
|---|---|---|---|
| SynthSeg+ [1] [2] | Deep Learning Segmentation Tool | Brain structure volumetry from clinical scans | Contrast-agnostic; high reliability on CE-MR; handles variable resolutions [1] [2] |
| MindGlide [3] | Deep Learning Segmentation Tool | Brain and lesion volumetry from any single contrast | Processes T1, T2, FLAIR, PD; fast inference; validated for treatment effect detection [3] |
| CAT12 [1] [2] | MRI Segmentation Pipeline | Comparative traditional tool for brain morphometry | SPM-based; serves as a benchmark; shows limitations with CE-MR heterogeneity [1] [2] |
| ITK-SNAP [6] [7] | Software Application | Manual delineation and visualization of regions of interest (ROI) | Used for ground truth segmentation in training datasets [6] |
| PyRadiomics [6] | Python Library | Extraction of radiomic features from medical images | Enables texture and heterogeneity analysis beyond simple volumetry [6] |
| BRATS Dataset [4] | Benchmarking Dataset | Training and validation for brain tumor segmentation | Provides multi-modal MRI data with expert annotations [4] |
The technical heterogeneity of clinical CE-MR scans, once a significant barrier, can now be effectively mitigated by advanced deep learning segmentation tools. The comparative data indicates that models like SynthSeg+ and MindGlide, which are designed to be robust to variations in contrast and acquisition parameters, show high reliability and are particularly suited for repurposing clinical archives [1] [3]. In contrast, more traditional pipelines like CAT12 demonstrate inconsistent performance when applied to CE-MR data [1] [2].
The successful application of these tools in detecting treatment effects in clinical trials for conditions like multiple sclerosis validates their potential to unlock new insights from old scans [3]. This capability significantly broadens the pool of data available for retrospective research and drug development, potentially reducing the cost and time of clinical trials. Future developments will likely focus on further improving generalizability across all brain structures—particularly addressing current discrepancies in CSF and ventricular volumes—and integrating these tools into seamless, end-to-end analysis pipelines for both clinical and research environments. By leveraging these sophisticated tools, researchers can transform underutilized clinical MRI archives into a powerful resource for understanding brain structure and disease progression.
Automated brain volumetry is a cornerstone of modern neuroimaging research and clinical practice, essential for screening and monitoring neurodegenerative diseases. However, the reliability of these measurements across different software, scanner models, and scanning sessions remains a significant challenge. This comparison guide objectively evaluates the performance of leading brain segmentation tools amidst these sources of variability, with particular emphasis on their application to contrast-enhanced MR (CE-MR) scans. Understanding these factors is crucial for researchers, scientists, and drug development professionals who rely on precise, reproducible volumetric measurements across multi-site studies and longitudinal clinical trials.
Quantitative Comparison of Segmentation Tools
Scan-Rescan Reliability of Volumetric Software
A comprehensive 2025 study systematically investigated the reliability of seven brain volumetry tools by analyzing scans from twelve subjects across six different scanners during two sessions conducted on the same day. The research evaluated measurements of gray matter (GM), white matter (WM), and total brain volume, providing critical insights into software performance variability [8].
Table 1: Scan-Rescan Reliability of Brain Volumetry Tools
| Segmentation Tool | Gray Matter CV (%) | White Matter CV (%) | Total Brain Volume CV (%) |
|---|---|---|---|
| AssemblyNet | <0.2% | <0.2% | 0.09% |
| AIRAscore | <0.2% | <0.2% | 0.09% |
| FreeSurfer | >0.2% | >0.2% | >0.2% |
| FastSurfer | >0.2% | >0.2% | >0.2% |
| syngo.via | >0.2% | >0.2% | >0.2% |
| SPM12 | >0.2% | >0.2% | >0.2% |
| Vol2Brain | >0.2% | >0.2% | >0.2% |
The coefficient of variation (CV) data reveals striking differences in measurement consistency. AssemblyNet and AIRAscore demonstrated superior scan-rescan reliability with median CV values below 0.2% for gray and white matter, and exceptionally low 0.09% for total brain volume [8]. This high reproducibility makes them particularly valuable for longitudinal studies where detecting subtle changes over time is essential. In contrast, all other tools exhibited greater variability with CVs exceeding 0.2%, potentially limiting their sensitivity for tracking progressive neurological conditions.
Statistical analysis using generalised estimating equations models revealed significant main effects for both software (Wald χ² = 22377.50, df = 6, p < 0.001) and scanner (Wald χ² = 91.76, df = 5, p < 0.001) on gray matter volume measurements, but not for scanning session (Wald χ² = 1.47, df = 1, p = 0.23) [8]. This indicates that while immediate repeat scanning doesn't significantly affect measurements, the choice of software and scanner introduces substantial variability.
Performance on Contrast-Enhanced vs. Non-Contrast MRI
The ability to extract reliable morphometric data from contrast-enhanced clinical scans significantly expands research possibilities. A 2025 comparative study evaluated this capability using 59 normal participants with both T1-weighted CE-MR and non-contrast MR (NC-MR) scans [1].
Table 2: Segmentation Tool Performance on CE-MR vs. NC-MR
| Segmentation Tool | Reliability (ICC) | Structures with Discrepancies | Age Prediction Comparable |
|---|---|---|---|
| SynthSeg+ | >0.90 for most structures | CSF and ventricular volumes | Yes |
| CAT12 | Inconsistent performance | Multiple structures | No |
The deep learning-based SynthSeg+ demonstrated exceptional reliability, with intraclass correlation coefficients (ICCs) exceeding 0.90 for most brain structures when comparing CE-MR and NC-MR scans [1]. This robust performance confirms that modern deep learning approaches can effectively handle the intensity variations introduced by gadolinium-based contrast agents. Notably, age prediction models built using SynthSeg+ segmentations yielded comparable results for both scan types, further validating their equivalence for research purposes [1].
Experimental Protocols and Methodologies
Multi-Scanner Reliability Assessment Protocol
The seminal scan-rescan reliability study employed a rigorous methodology to isolate variability sources [8]:
- Subject Cohort: Twelve healthy subjects (6 women, 6 men) with mean age 35.3 years (±8.5 years)
- Scanning Protocol: Examinations performed between March-November 2021 using six different scanners from the same vendor
- Temporal Design: Two separate scanning sessions conducted within 2 hours on the same day to minimize biological variation
- Software Evaluation: Seven volumetry tools tested, including both research tools and certified medical device software
- Statistical Analysis: Generalized estimating equations models to assess fixed effects of software, scanner, and session, with Wald χ² statistics and post-hoc analysis of interactions
This experimental design enabled researchers to quantify each variability source independently while controlling for biological changes that might occur between more widely spaced scanning sessions.
CE-MR Reliability Assessment Protocol
The contrast-enhanced MRI reliability study implemented this methodology [1]:
- Participants: 59 normal individuals aged 21-73 years, providing broad age representation
- Scan Types: Paired T1-weighted contrast-enhanced and non-contrast MR scans from each participant
- Segmentation Tools: CAT12 and SynthSeg+ for volumetric measurement extraction
- Analysis Approach: Intraclass correlation coefficients to quantify agreement between CE-MR and NC-MR measurements; age prediction models to validate clinical relevance
This protocol specifically addressed whether contrast administration fundamentally alters the ability to derive accurate morphometric measurements, a critical consideration for leveraging abundant clinical scans for research purposes.
Segmentation Reliability Workflow
The diagram below illustrates the key factors influencing segmentation reliability and their interactions, based on current research findings:
Segmentation Reliability Factors - This workflow illustrates how software, scanner, session, and contrast factors influence reliability metrics.
Research Reagent Solutions Toolkit
Table 3: Essential Research Tools for Segmentation Reliability Studies
| Tool/Category | Specific Examples | Primary Function | Performance Notes |
|---|---|---|---|
| High-Reliability Software | AssemblyNet, AIRAscore, SynthSeg+ | Automated brain volumetry | CV <0.2%, ICC >0.90 for most structures [8] [1] |
| Scanner Harmonization | Deep learning super-resolution (TCGAN) | Enhance 1.5T images to 3T quality | Reduces field strength variability [9] |
| Multi-Site Robust Algorithms | LOD-Brain (3D CNN) | Handle multi-site variability | Trained on 27,000 scans from 160 sites [10] |
| Quality Assessment Tools | Structural Similarity Index (SSIM), Coefficient of Variation | Quantify segmentation reliability | Detect protocol deviations [8] [11] |
| Contrast-Enhanced Processing | SynthSeg+ | Segment contrast-enhanced MRI | Maintains reliability vs non-contrast (ICC >0.90) [1] |
The evidence consistently demonstrates that software choice exerts the strongest influence on segmentation reliability, significantly outweighing effects from scanner differences or rescan sessions [8]. For research requiring high-precision longitudinal measurements, tools like AssemblyNet and AIRAscore provide superior reliability with CV values below 0.2% [8]. When working with contrast-enhanced clinical scans, deep learning-based approaches like SynthSeg+ maintain excellent reliability (ICC >0.90) compared to non-contrast scans [1].
To maximize segmentation reliability in research and drug development applications:
- Standardize Software Platforms: Use the same software tools throughout longitudinal studies and multi-site trials
- Leverage CE-MR Scans Confidently: Modern deep learning tools can reliably extract morphometric data from contrast-enhanced scans
- Implement Scanner Consistency: When possible, use the same scanner model and acquisition protocols across timepoints
- Adopt Harmonization Approaches: For multi-site studies, utilize algorithms specifically designed for cross-site reliability like LOD-Brain [10]
These strategies ensure that observed brain volume changes reflect genuine biological phenomena rather than technical variability, ultimately enhancing the validity and impact of neuroimaging research in both academic and clinical trial settings.
Magnetic resonance imaging (MRI) is indispensable in clinical and research settings for its exceptional soft-tissue contrast and detailed visualization of internal structures [12]. A fundamental parameter of any MRI system is its magnetic field strength, measured in Tesla (T), with 1.5T and 3T being the most prevalent field strengths in clinical use today [13] [14]. The choice between these field strengths carries significant implications for the quantitative volume measurements that are crucial for tracking disease progression in neurological disorders and for biomedical research [15] [16].
This guide objectively compares the performance of 1.5T and 3T MRI scanners, with a specific focus on their impact on the reliability of brain volume measurements derived from automated segmentation tools. As research and clinical diagnostics increasingly rely on precise, longitudinal volumetry, understanding the variability introduced by the imaging hardware itself is essential. This analysis is framed within broader investigations into the reliability of segmentation tools on contrast-enhanced MR (CE-MR) scans, providing researchers and drug development professionals with the data needed to inform their experimental designs and interpret their results accurately.
Technical Comparison: 1.5T vs. 3T MRI Scanners
The primary difference between 1.5T and 3T scanners is the strength of their main magnetic field. While a 3T scanner's magnet is twice as strong as a 1.5T's, the practical implications are complex and involve trade-offs between signal, artifacts, and safety [12].
Table 1: Core Technical Characteristics of 1.5T and 3T MRI Scanners
| Feature | 1.5T MRI | 3T MRI | Practical Implication |
|---|---|---|---|
| Magnetic Field Strength | 1.5 Tesla | 3.0 Tesla | The fundamental differentiating parameter. |
| Signal-to-Noise Ratio (SNR) | Standard | Approximately twice that of 1.5T [17] [12] | Higher SNR at 3T can be used to increase spatial resolution or decrease scan time. |
| Spatial Resolution | Good for most clinical applications | Superior for visualizing small anatomical structures and subtle pathology [17] | 3T is advantageous for imaging small brain structures (e.g., hippocampal subfields). |
| Scan Time | Standard | Potentially faster for images of comparable quality [14] [12] | 3T can improve patient throughput and reduce motion artifacts. |
| Safety & Compatibility | Broader compatibility with medical implants [13] | More implants are unsafe or conditional at 3T; increased specific absorption rate (SAR) [13] [17] | Patient screening is more critical for 3T; may exclude some subjects from studies. |
| Artifacts | Lower susceptibility to artifacts (e.g., from chemical shift or metal) [12] | Increased susceptibility artifacts, particularly at tissue-air interfaces [17] [12] | Can affect image quality near the sinuses or temporal lobes, potentially confounding segmentation. |
| Cost & Infrastructure | Lower purchase, installation, and maintenance costs [14] | 25-50% higher purchase cost; may require more specialized site planning [14] | 1.5T is often more cost-effective and accessible. |
The increased SNR is the most significant advantage of 3T systems. It provides a foundation for higher spatial resolution, which is critical for delineating subtle neuroanatomy. However, this benefit is accompanied by challenges, including increased energy deposition in tissue (measured as SAR) and a greater propensity for image distortions due to magnetic susceptibility [17]. These factors must be carefully managed through sequence optimization.
Impact on Automated Volume Measurements
The variability introduced by changing magnetic field strength is a critical concern in longitudinal studies and multi-center trials where patients may be scanned on different systems. Evidence suggests that this variability can be significant and is handled differently by various segmentation software tools.
Key Experimental Findings on Measurement Variability
A 2024 study directly investigated this issue by comparing the reliability of two automated segmentation tools—FreeSurfer and Neurophet AQUA—across 1.5T and 3T scanners [15]. The study involved patients scanned at both field strengths within a six-month period. The results provide a quantitative basis for understanding measurement variability.
Table 2: Reliability of Volume Measurements Across Magnetic Field Strengths (1.5T vs. 3T)
| Brain Region | Segmentation Tool | Effect Size (1.5T vs. 3T) | Intraclass Correlation Coefficient (ICC) | Average Volume Difference Percentage (AVDP) |
|---|---|---|---|---|
| Cortical Gray Matter | FreeSurfer | -0.307 to 0.433 | 0.869 - 0.965 | >10% |
| Neurophet AQUA | -0.409 to 0.243 | Not Specified | <10% | |
| Cerebral White Matter | FreeSurfer | Significant difference (p<0.001) | 0.965 | >10% |
| Neurophet AQUA | Significant difference (p<0.001) | Not Specified | <10% | |
| Hippocampus | FreeSurfer | Not Specified | Not Specified | >10% |
| Neurophet AQUA | Not Specified | Not Specified | <10% | |
| Amygdala | FreeSurfer | Significant difference (p<0.001) | 0.922 | >10% |
| Neurophet AQUA | Not Specified | Not Specified | <10% | |
| Thalamus | FreeSurfer | Significant difference (p<0.001) | 0.922 | >10% |
| Neurophet AQUA | Not Specified | Not Specified | <10% |
The study found that while both tools showed statistically significant volume differences for most brain regions between 1.5T and 3T, the effect sizes were generally small [15]. This indicates that the magnitude of the difference may not be biologically large. A key finding was that Neurophet AQUA yielded a smaller average volume difference percentage (AVDP) across all brain regions (all <10%) compared to FreeSurfer (all >10%) [15]. This suggests that some modern segmentation tools may be more robust to field strength-induced variability.
Furthermore, the study noted differences in the quality of segmentations; Neurophet AQUA produced stable connectivity without invading other regions, whereas FreeSurfer's segmentation of the hippocampus, for instance, sometimes encroached on the inferior lateral ventricle [15]. The processing time also differed dramatically, with Neurophet AQUA completing segmentations in approximately 5 minutes compared to 1 hour for FreeSurfer [15].
The Role of AI in Harmonizing Measurements
The challenge of field strength variability is being addressed through advanced AI and deep learning models. Research demonstrates that these tools can enhance the consistency of volumetric measurements across different scanner platforms.
One approach involves using generative models to improve data from lower-field systems. For example, the LoHiResGAN model uses a generative adversarial network (GAN) to enhance the quality and resolution of ultra-low-field (64mT) MRI images to a level comparable with 3T MRI [16]. Another model, SynthSR, is a convolutional neural network (CNN) that can generate synthetic high-resolution images from various input sequences, effectively mitigating variability caused by differences in scanning parameters [16]. Studies applying these models have shown that they can reduce systematic deviations in brain volume measurements acquired at different field strengths, bringing ultra-low-field estimates closer to the 3T reference standard [16].
The experimental workflow for such a harmonization analysis typically involves acquiring images from the same subjects on different scanner platforms, processing the data through these AI models, and then comparing the volumetric outputs to a reference standard.
Experimental Workflow for Cross-Field-Strength Analysis
Essential Research Reagents and Tools
For researchers designing studies involving volume measurements across different MRI field strengths, the following tools and software are essential.
Table 3: Key Research Reagents and Software Solutions
| Tool Name | Type | Primary Function in Research | Key Consideration |
|---|---|---|---|
| FreeSurfer | Automated Segmentation Software | Provides detailed segmentation of brain structures from MRI data. | Long processing time (~1 hr); shows higher volume variability with field strength (>10% AVDP) [15]. |
| Neurophet AQUA | Automated Segmentation Software | Provides automated brain volumetry with clinical approval. | Faster processing (~5 min); shows lower volume variability with field strength (<10% AVDP) [15]. |
| TotalSegmentator MRI | AI Segmentation Model (nnU-Net-based) | Robust, sequence-agnostic segmentation of multiple anatomic structures in MRI. | Open-source; trained on both CT and MRI data for improved generalization [18]. |
| DeepMedic | Convolutional Neural Network (CNN) | Used for specialized segmentation tasks, such as branch-level carotid artery segmentation in CE-MRA [19]. | Demonstrates the application of deep learning for complex vascular structures. |
| SynthSR & LoHiResGAN | Deep Learning Harmonization Models | Improve alignment and consistency of volumetric measurements from different field strengths, including ultra-low-field MRI [16]. | Key for mitigating scanner-induced variability in multi-center or longitudinal studies. |
The choice between 1.5T and 3T MRI systems presents a clear trade-off. 3T scanners offer higher SNR and spatial resolution, which can translate into superior visualization of fine anatomic detail and potentially faster scan times [17] [12]. However, this does not automatically guarantee more reliable volume measurements. The evidence indicates that changing the magnetic field strength introduces statistically significant variability in automated volume measurements, a factor that must be accounted for in study design [15].
The reliability of these measurements is not solely dependent on the scanner but is also a function of the segmentation tool used. Modern tools like Neurophet AQUA and AI harmonization models like SynthSR demonstrate that software can be engineered to be more robust to this underlying hardware variability [15] [16]. For researchers and drug development professionals, this underscores a critical point: rigorous study design must include a pre-planned strategy for managing cross-scanner variability, whether through consistent hardware use, sophisticated statistical correction, or the application of AI-powered harmonization tools to ensure that measured volume changes reflect biology rather than instrumentation.
In the evolving field of medical imaging, particularly with the rise of artificial intelligence (AI)-based analytical tools, scan-rescan reliability has emerged as a fundamental requirement for validating quantitative measurements. This reliability ensures that observed changes in longitudinal studies—such as monitoring neurodegenerative disease progression or treatment response—reflect true biological signals rather than methodological noise. For researchers utilizing contrast-enhanced MR (CE-MR) scans, understanding the performance characteristics of different segmentation software is crucial. This guide provides an objective comparison of various volumetry tools based on their scan-rescan reliability, quantified through the Coefficient of Variation (CV%) and Limits of Agreement (LoA), to inform selection for clinical and research applications.
Quantitative Comparison of Segmentation Tool Reliability
The reliability of automated brain volumetry software was directly assessed in a 2025 study that compared seven tools using scan-rescan data from twelve subjects across six scanners [8]. The following table summarizes the key reliability metrics for grey matter (GM), white matter (WM), and total brain volume (TBV) measurements.
Table 1: Scan-Rescan Reliability of Brain Volumetry Tools [8]
| Segmentation Tool | GM Median CV% | WM Median CV% | TBV Median CV% | Bland-Altman Analysis |
|---|---|---|---|---|
| AssemblyNet | < 0.2% | < 0.2% | 0.09% | No systematic difference; variable LoA |
| AIRAscore | < 0.2% | < 0.2% | 0.09% | No systematic difference; variable LoA |
| FreeSurfer | > 0.2% | > 0.2% | > 0.2% | No systematic difference; variable LoA |
| FastSurfer | > 0.2% | > 0.2% | > 0.2% | No systematic difference; variable LoA |
| syngo.via | > 0.2% | > 0.2% | > 0.2% | No systematic difference; variable LoA |
| SPM12 | > 0.2% | > 0.2% | > 0.2% | No systematic difference; variable LoA |
| Vol2Brain | > 0.2% | > 0.2% | > 0.2% | No systematic difference; variable LoA |
The data demonstrates a clear performance tier. AssemblyNet and AIRAscore showed superior repeatability, with median CVs under 0.2% for GM and WM and 0.09% for TBV. In contrast, the other five tools exhibited higher variability, with CVs exceeding 0.2% for all tissue classes [8]. The Bland-Altman analysis confirmed an absence of systematic bias across all methods, but the width of the LoA varied significantly, indicating differences in measurement precision [8].
For studies involving contrast-enhanced MRI, the choice of segmentation software is equally critical. A 2025 comparative study found that the deep learning-based tool SynthSeg+ could reliably extract morphometric data from CE-MR scans, showing high agreement with non-contrast MR (NC-MR) scans for most brain structures (Intraclass Correlation Coefficients, ICCs > 0.90) [1]. Conversely, CAT12 demonstrated inconsistent performance in this context [1].
Experimental Protocols for Reliability Assessment
The comparative data presented above are derived from rigorous experimental designs. Below, we detail the core methodologies used in the cited studies to guide researchers in designing their own reliability assessments.
Protocol 1: Multi-Scanner, Multi-Software Brain Volumetry
This protocol evaluated the effect of scanner, software, and scanning session on brain volume measurements [8].
- Subjects: Twelve healthy subjects (6 women, 6 men; mean age 35.3 ± 8.5 years).
- Scanning: Each subject was scanned on six different MRI scanners from the same vendor during a single session, and then rescanned within two hours.
- Volumetry Tools: The T1-weighted images from both sessions were processed by seven automated brain volumetry tools: AssemblyNet, AIRAscore, FreeSurfer, FastSurfer, syngo.via, SPM12, and Vol2Brain.
- Statistical Analysis: The statistical analysis involved fitting Generalised Estimating Equations (GEE) models to quantify the effects of software, scanner, and session on GM, WM, and TBV volumes. Scan-rescan reliability was primarily assessed using the percentage of coefficient of variation (CV%). Bland-Altman analysis was used to evaluate agreement and calculate the limits of agreement (LoA) between scan and rescan measurements [8].
Protocol 2: Contrast-Enhanced vs. Non-Contrast MRI Volumetry
This protocol specifically assessed the reliability of morphometric measurements from CE-MR scans [1].
- Participants & Imaging: Fifty-nine normal participants underwent both T1-weighted CE-MR and NC-MR scans.
- Segmentation & Analysis: The scans were processed using two segmentation tools: CAT12 and SynthSeg+. Volumetric measurements for various brain structures were extracted from both scan types.
- Reliability Assessment: Agreement between measurements from CE-MR and NC-MR scans was quantified using Intraclass Correlation Coefficients (ICCs). The efficacy of the derived volumes was further tested by building age prediction models for both scan types [1].
Visualizing Reliability Assessment Workflows
The process of establishing scan-rescan reliability follows a structured pathway, from data acquisition to the final statistical interpretation. The diagram below outlines this general workflow, which is common to the experimental protocols described.
Figure 1: Generalized Scan-Rescan Reliability Workflow. The "Rescan" step is critical for assessing measurement variability independent of true biological change.
A significant finding from recent studies is that the variability in final measurements is not solely due to the imaging process itself. The analysis software introduces substantial variability, as illustrated below.
Figure 2: Software-Induced Variability in Volumetry. Identical input images processed with different software algorithms can yield outputs with significantly different reliability metrics, such as the Coefficient of Variation (CV%) [8].
The Scientist's Toolkit: Essential Research Reagents and Materials
The following table details key software tools and methodological components frequently employed in scan-rescan reliability research.
Table 2: Key Reagents and Solutions for Reliability Research
| Tool / Material | Type | Primary Function in Research |
|---|---|---|
| AIRAscore | Automated Volumetry Software | Certified medical device software for brain volume measurement; demonstrates high scan-rescan reliability (CV < 0.2%) [8]. |
| SynthSeg+ | Deep Learning Segmentation Tool | Segments brain MRI scans without requiring retraining; shows high reliability (ICCs > 0.90) for contrast-enhanced MRI analysis [1]. |
| FreeSurfer | Neuroimaging Software Toolkit | A widely used, established academic tool for brain morphometry; used as a benchmark in comparative reliability studies [8]. |
| nnUNet | AI Segmentation Framework | An adaptive framework for automated medical image segmentation; used in developing models for complex structures like coronary arteries [20]. |
| ICC & CV% | Statistical Metrics | Quantifies reliability and agreement (ICC) and measures relative repeatability (CV%) for scan-rescan and inter-software comparisons [8] [21]. |
| Bland-Altman Analysis | Statistical Method | Assesses agreement between two measurement techniques by calculating the "limits of agreement" between scan and rescan results [8]. |
| Dice Similarity Coefficient (DSC) | Image Overlap Metric | Evaluates the spatial overlap between segmentations, often used to measure intra- and inter-observer consistency (e.g., manual vs. AI contours) [20]. |
The empirical data lead to a clear and critical recommendation for the research community: to ensure reliable and clinically valuable longitudinal observations, the same combination of scanner and segmentation software must be used throughout a study [8]. The choice between tools like AssemblyNet, which offers exceptional repeatability (CV < 0.2%), and more established platforms like FreeSurfer, can fundamentally impact the interpretability of results. Furthermore, for studies leveraging clinically acquired CE-MR scans, deep learning-based tools like SynthSeg+ provide a reliable pathway for volumetric analysis [1]. As quantitative imaging biomarkers become increasingly integral to diagnostics and clinical trials, a rigorous, metrics-driven understanding of scan-rescan reliability is not merely beneficial—it is indispensable.
Methodological Approaches: Leveraging Deep Learning for Reliable CE-MR Segmentation
The segmentation of structures from medical images, particularly Contrast-Enhanced Magnetic Resonance (CE-MR) scans, is a fundamental task in medical image analysis, supporting critical activities from diagnosis to treatment planning. For years, this domain was dominated by traditional image processing algorithms. However, the emergence of deep learning (DL) represents a potential paradigm shift, offering a fundamentally different approach to solving segmentation challenges. This guide provides an objective comparison of the performance between these two generations of technology, framing the analysis within broader research on the reliability of segmentation tools for CE-MR scans. We synthesize data from recent, peer-reviewed studies to offer researchers, scientists, and drug development professionals a clear, evidence-based perspective on the capabilities and limitations of each approach.
Understanding the Tools: A Technological Divide
The distinction between traditional and deep learning-based tools is not merely incremental; it represents a fundamental difference in philosophy and implementation.
Traditional Image Segmentation Tools rely on hand-crafted features and classical digital image processing techniques. These methods include:
- Thresholding: Converting images into binary maps based on pixel intensity values [22].
- Region-Based Segmentation: Grouping adjacent pixels with similar characteristics, often starting from "seed" points (e.g., region-growing, watershed algorithms) [22].
- Edge Detection: Identifying and classifying pixels that constitute edges within an image using filters like Canny edge detection [22].
- Clustering-Based Methods: Using unsupervised algorithms like K-means to group pixels with common attributes into segments [22].
These methods are generally interpretable and computationally efficient but often struggle with the complexity and noise inherent in biological images.
Deep Learning-Based Segmentation Tools use artificial neural networks with multiple layers to learn complex patterns and features directly from the data during a training process. The majority of modern medical image segmentation models are based on Convolutional Neural Networks (CNNs) [23]. A landmark architecture is the U-Net, which uses an encoder-decoder structure with "skip connections" to preserve detailed information lost during downsampling, making it particularly effective for medical images [22] [23]. These models learn to perform segmentation by analyzing large-scale annotated datasets, iteratively improving their parameters to minimize the difference between their predictions and expert-created "ground truth" labels [23].
The following diagram illustrates the core structural difference between a traditional pipeline and a deep learning model like U-Net.
Quantitative Performance Comparison
The theoretical advantages of deep learning are borne out by empirical evidence. The table below summarizes key performance metrics from recent studies across various clinical applications, using CE-MR scans or comparable MRI data.
Table 1: Performance Metrics of Deep Learning vs. Traditional Tools Across Anatomical Regions
| Anatomical Region & Task | Tool / Method | Performance Metrics | Key Findings / Clinical Relevance |
|---|---|---|---|
| Lumbar Spine MRI (Pathology Identification) [24] | Deep Learning (RadBot) | Sensitivity: 73.3%Specificity: 88.4%Positive Predictive Value: 80.3%Negative Predictive Value: 83.7% | Distinguished presence of neural compression at a statistically significant level (p < .0001) from a random event distribution. |
| Rectal Cancer CTV (Mesorectal Target Contouring) [25] | Deep Learning (nnU-Net Segmentation) | Median Hausdorff Distance (HD): 9.3 mmClinical Acceptability: 9/10 contours | Outperformed registration-based deep learning models, particularly in mid and cranial regions, and was more robust to anatomical variations. |
| Rectal Cancer CTV (Mesorectal Target Contouring) [25] | Deep Learning (Registration-based Model) | Median Hausdorff Distance (HD): 10.2 mmClinical Acceptability: 3/10 contours | Less accurate and clinically acceptable than the segmentation-based nnU-Net approach. |
| Hippocampus (Volumetric Segmentation) [26] | Traditional (e.g., FreeSurfer, FIRST) | N/A (Qualitative Assessment) | Tendency to over-segment, particularly at the anterior hippocampal border. Generally more time-consuming and resource-intensive. |
| Hippocampus (Volumetric Segmentation) [26] | Deep Learning (e.g., Hippodeep, FastSurfer) | Strong correlation with manual volumes; able to differentiate diagnostic groups (e.g., Healthy, MCI, Dementia). | Emerged as "particularly attractive options" based on reliability, accuracy, and computational efficiency. |
| Brain Tumor (Glioma Segmentation) [23] | Deep Learning (U-Net based models) | N/A (State-of-the-Art Benchmark) | Winning models of the annual BraTS challenge since 2012 are consistently based on U-Net architectures, establishing DL as the state-of-the-art. |
A critical metric for segmentation overlap is the Dice Similarity Coefficient (DSC), which measures the overlap between the predicted segmentation and the ground truth. While not all studies report DSC, its loss function counterpart was central to a rectal cancer study, which found that a deep learning segmentation model (nnU-Net) outperformed a registration-based model [25]. Furthermore, deep learning models have demonstrated high consistency in volumetric segmentation when scans are conducted on the same MRI scanner, a crucial factor for longitudinal studies in drug development [27].
Analysis of Experimental Protocols
To critically appraise the data, it is essential to understand the methodologies that generated it. The following table outlines the experimental protocols from key studies cited in this guide.
Table 2: Experimental Protocols from Key Cited Studies
| Study Reference | Imaging Data | Ground Truth Definition | Model Training & Evaluation |
|---|---|---|---|
| Lumbar Spine Analysis [24] | - 65 lumbar MRI scans (383 levels)- Average age: 42.2 years | MRI reports from board-certified radiologists. Pathologies were extracted and categorized (e.g., no stenosis, stenosis). | - DL model (RadBot) analysis compared to radiologist's report.- Metrics: Sensitivity, Specificity, PPV, NPV.- Reliability: Cronbach alpha and Cohen's kappa calculated. |
| Rectal Cancer Contouring [25] | - 104 rectal cancer patients.- T2-weighted planning and daily fraction MRI from 1.5T/3T scanners. | Manually delineated mesorectal Clinical Target Volume (CTV) by a radiation oncologist, adjusted as needed for daily fractions. | - Model: 3D nnU-Net for segmentation.- Data Split: 68/14/22 (Train/Val/Test).- Loss Function: Cross-entropy + Soft-Dice loss.- Metrics: Hausdorff Distance (HD), Dice, qualitative clinical score. |
| Hippocampal Segmentation [26] | - 3 datasets (ADNI HarP, MNI-HISUB25, OBHC) with manual labels.- Included Healthy, MCI, and Dementia patients. | Manual segmentation following harmonized protocols (e.g., HarP) considered the gold standard. | - Evaluation: 10 automatic methods (Traditional & DL) compared.- Metrics: Overlap with manual labels, volume correlation, group differentiation, false positive/negative analysis. |
| Brain Tumor Segmentation [23] | - Public datasets from BraTS challenges.- Multi-institutional, multi-scanner MRI of gliomas, metastases, etc. | Expert-annotated tumor sub-regions (e.g., enhancing tumor, edema, necrosis). | - Models (typically U-Net variants) trained on large public datasets.- Performance benchmarked annually via the BraTS challenge. |
A common strength across these deep learning protocols is the use of a validation set to tune hyperparameters and a held-out test set to provide an unbiased estimate of model performance [25] [26]. Furthermore, the use of data from multiple sites and scanners [24] [26] helps to stress-test the generalizability of the models, a vital consideration for clinical and multi-center research applications.
The Scientist's Toolkit: Essential Research Reagents & Materials
For researchers aiming to implement or evaluate these segmentation tools, the following table lists key "research reagents" and their functions.
Table 3: Essential Reagents for Segmentation Tool Research
| Item / Solution | Function & Application in Research |
|---|---|
| Annotated Datasets (e.g., BraTS, ADNI) | Provide the essential "ground truth" labels for training supervised deep learning models and for benchmarking the performance of both traditional and DL tools [23] [26]. |
| Deep Learning Frameworks (e.g., PyTorch, TensorFlow) | Open-source libraries that provide the foundational building blocks and computational graphs for designing, training, and deploying deep neural networks. |
| Specialized Segmentation Frameworks (e.g., nnU-Net) | An out-of-the-box framework that automatically configures the network architecture and training procedure based on the dataset properties, often achieving state-of-the-art results without manual tuning [25]. |
| Traditional Algorithm Suites (e.g., in OpenCV, ITK) | Software libraries containing implementations of classic image segmentation algorithms like thresholding, region-growing, and clustering, used for baseline comparisons or specific applications [22]. |
| Performance Metrics (Dice, Hausdorff Distance, Sensitivity/Specificity) | Quantitative measures that objectively evaluate and compare the accuracy, overlap, and clinical utility of different segmentation methods [24] [25] [23]. |
| Compute Infrastructure (GPU Acceleration) | High-performance computing hardware, particularly GPUs, which are critical for reducing the time required to train complex deep learning models on large medical image datasets [28] [25]. |
The evidence from recent and rigorous studies indicates that a performance paradigm shift is underway. While traditional segmentation tools maintain utility for specific, well-defined tasks, deep learning has established a new benchmark for accuracy, automation, and scalability in the analysis of CE-MR scans.
Deep learning models consistently demonstrate superior performance in complex segmentation tasks across neurology, oncology, and musculoskeletal imaging [24] [25] [23]. They show a enhanced ability to identify clinically relevant features and, crucially, integrate into workflows where efficiency is paramount. However, this power comes with demands for large, high-quality annotated datasets and significant computational resources. For the research and drug development community, the choice is no longer about whether deep learning is more powerful, but about how to best leverage its capabilities while managing its requirements for robust and reliable outcomes.
Clinical brain MRI scans, including contrast-enhanced (CE-MR) images, represent a vast and underutilized resource for neuroscience research [2]. The variability in acquisition protocols, particularly the use of gadolinium-based contrast agents, presents a significant challenge for automated segmentation tools, which are essential for quantitative morphometric analysis. Traditionally, convolutional neural networks (CNNs) have demonstrated high sensitivity to changes in image contrast and resolution, often requiring retraining or fine-tuning for each new domain [29]. This technical heterogeneity has limited the large-scale analysis of clinically acquired CE-MR scans.
Within this context, tools demonstrating contrast invariance are of paramount importance. SynthSeg emerged as a pioneering CNN for segmenting brain MRI scans of any contrast and resolution without retraining [29] [30]. Its enhanced successor, SynthSeg+, was specifically designed for increased robustness on heterogeneous clinical data, including scans with low signal-to-noise ratio or poor tissue contrast [31] [32]. This guide provides a detailed examination of SynthSeg+'s architecture, benchmarks its performance against alternative tools, and presents experimental data validating its reliability for analyzing CE-MR scans, thereby unlocking their potential for research.
Architectural Innovation of SynthSeg+
Core Framework and Domain Randomization
The foundation of SynthSeg's robustness is a domain randomisation strategy trained with synthetic data [29] [33]. Unlike supervised CNNs trained on real images of a specific contrast, SynthSeg is trained exclusively on synthetic data generated from a generative model conditioned on anatomical segmentations.
- Synthetic Data Generation: The model creates synthetic images by sampling intensities for each anatomical structure from a Gaussian Mixture Model (GMM). Crucially, generation parameters—including image contrast and resolution—are fully randomized for each minibatch from uninformative uniform priors [29] [34].
- Training Process: By exposing the network to an extremely wide and unrealistic range of image appearances, it is forced to learn domain-agnostic features tied to anatomical shape and context rather than specific intensity profiles [33]. This enables the single trained model to segment real scans from a wide range of target domains, including different MR contrasts and even CT, without retraining [29] [32].
The SynthSeg+ Hierarchy for Enhanced Robustness
While SynthSeg is generally robust, it can falter on clinical scans with very low signal-to-noise ratio or poor tissue contrast [31]. SynthSeg+ introduces a novel, hierarchical architecture to mitigate these shortcomings.
As illustrated in the diagram below, SynthSeg+ employs a sequence of networks, each conditioned on the output of the previous one, to progressively refine the segmentation.
This hierarchical workflow functions as follows:
- Initial Segmentation (
S1): The first segmentation network processes the raw, potentially noisy input scan to produce an initial segmentation estimate [31]. - Denoising (
D): A dedicated denoising network then takes the initial segmentation and the original input image. It generates a "cleaner," denoised version of the segmentation, which helps suppress errors and inconsistencies [31]. - Refined Segmentation (
S2): A second segmentation network, identical in architecture to the first, takes the original input image and the denoised segmentation from the previous step. Conditioned on this improved prior,S2produces the final, refined segmentation output [31].
This multi-stage, conditional pipeline proves considerably more robust than the original SynthSeg, outperforming both cascaded networks and state-of-the-art segmentation denoising methods on challenging clinical data [31].
Performance Benchmarking in CE-MR Analysis
Comparative Reliability on CE-MR vs. Non-Contrast MR
A pivotal 2025 study by Aman et al. directly evaluated the reliability of brain volumetric measurements from CE-MR scans compared to non-contrast MR (NC-MR) scans, using both SynthSeg+ and the CAT12 segmentation tool [2] [1].
Table 1: Comparative Reliability of Volumetric Measurements between CE-MR and NC-MR Scans
| Brain Structure Category | SynthSeg+ (ICC) | CAT12 (ICC) | Notes |
|---|---|---|---|
| Most Brain Structures | > 0.90 [2] | Inconsistent [2] | SynthSeg+ showed high reliability for most regions, with larger structures having ICC > 0.94 [2]. |
| Cerebrospinal Fluid (CSF) & Ventricles | Discrepancies noted [2] | Inconsistent [2] | |
| Thalamus | Slight overestimation in CE-MR [2] | Inconsistent [2] | |
| Brain Stem | Robust correlation (lowest among high ICCs) [2] | Inconsistent [2] |
The experimental protocol for this benchmark was as follows:
- Dataset: 59 paired T1-weighted CE-MR and NC-MR scans from clinically normal individuals (age range 21-73 years) [2].
- Methodology: Each scan was processed through both SynthSeg+ and CAT12 segmentation tools. The resulting volumetric measurements for multiple brain structures were then compared between CE-MR and NC-MR scans for each tool [2].
- Outcome Measurement: Reliability was quantified using Intraclass Correlation Coefficients (ICCs). The study also constructed age prediction models to assess the utility of the volumetric measurements from both scan types [2].
The conclusion was clear: "Deep learning-based approaches, particularly SynthSeg+, can reliably process contrast-enhanced MRI scans for morphometric analysis, showing high consistency with non-contrast scans across most brain structures" [2]. This finding significantly broadens the potential for using clinically acquired CE-MR images in neuroimaging research.
Generalizability Across Modalities and Populations
The robustness of the SynthSeg framework extends beyond CE-MR. The following table summarizes its validated performance across various imaging domains and subject populations.
Table 2: Generalizability of SynthSeg/SynthSeg+ Across Domains
| Domain | Performance | Key Evidence |
|---|---|---|
| CT Scans | Good segmentation performance, though with lower precision than MRI (Median Dice: 0.76) [35]. Suitable for applications where high precision is not essential [35]. | Validation on 260 paired CT-MRI scans from radiotherapy patients; able to replicate known morphological trends related to sex and age [35]. |
| Infant Brain MRI | Infant-SynthSeg model shows consistently high segmentation performance across the first year of life, enabling a single framework for longitudinal studies [34]. | Addresses large contrast changes and heterogeneous intensity appearance in infant brains; outperforms a traditional contrast-aware nnU-net in cross-age segmentation [34]. |
| Abdominal MRI | ABDSynth (a SynthSeg-based model) provides a viable alternative when annotated MRI data is scarce, though slightly less accurate than models trained on real MRI data [5]. | Trained solely on widely available CT segmentations; benchmarked on multi-organ abdominal segmentation across diverse datasets [5]. |
Practical Research Toolkit
Key Research Reagent Solutions
For researchers aiming to utilize SynthSeg+ for CE-MR analysis, the following tools and resources are essential.
Table 3: Essential Materials and Resources for SynthSeg+ Research
| Item/Resource | Function/Description | Availability |
|---|---|---|
| SynthSeg+ Model | The core deep learning model for robust, contrast-agnostic brain segmentation, including cortical parcellation and QC [33] [32]. | Integrated in FreeSurfer (v7.3.2+); available as a standalone Python package on GitHub [33] [32]. |
| Clinical CE-MR Datasets | Retrospective paired or unpaired CE-MR and NC-MR scans for validation and analysis studies [2]. | Hospital PACS systems, public repositories (e.g., ADNI [29]). |
| High-Performance Computing (CPU/GPU) | Runs SynthSeg+ on GPU (~15s/scan) or CPU (~1min/scan) [33]. | Local workstations or high-performance computing clusters. |
| FreeSurfer Suite | Provides the mri_synthseg command and environment for running the tool, along with visualization tools like Freeview [32]. |
FreeSurfer website. |
| Quality Control (QC) Scores | Automated scores assessing segmentation reliability for each scan, crucial for filtering data in large-scale studies [31] [32]. | Generated automatically by SynthSeg+ and saved to a CSV file. |
Implementation Workflow
The typical workflow for deploying SynthSeg+ in a research analysis, particularly for CE-MR scans, is outlined below.
This workflow involves:
- Data Acquisition: Gathering a heterogeneous set of clinical scans, which can include CE-MR images of varying resolutions and protocols [2] [31].
- Minimal Preprocessing: A key advantage of SynthSeg+ is that it requires no mandatory preprocessing (e.g., bias field correction, skull stripping), making it ideal for uncurated data [33] [32].
- Running SynthSeg+: The tool is executed, preferably using the
--robustflag for clinical data. It outputs segmentations at 1mm isotropic resolution and can simultaneously generate volumetric data and QC scores [32]. - Quality Control: The automated QC scores are used to identify and potentially exclude unreliable segmentations, ensuring the integrity of the downstream analysis [31] [35].
- Final Analysis: The robust volumetric measurements are used for morphometric analysis, enabling large-scale studies on clinical datasets [2] [31].
SynthSeg+ represents a significant leap forward in the analysis of clinically acquired brain MRI scans. Its hierarchical architecture, built upon a foundation of domain randomization, provides unparalleled robustness against the technical heterogeneity that has historically plagued clinical neuroimaging research. Experimental data confirms its superior reliability for volumetric analysis of contrast-enhanced MR scans compared to other tools like CAT12, closely replicating measurements from non-contrast scans [2]. Furthermore, its generalizability across modalities—from CT to infant MRI—demonstrates the power of its underlying framework [34] [35].
For researchers and drug development professionals, SynthSeg+ offers a practical and powerful solution for leveraging large, heterogeneous clinical datasets. By enabling consistent and accurate segmentation across diverse acquisition protocols and patient populations, it paves the way for large-scale, retrospective studies with sample sizes previously difficult to achieve, ultimately accelerating discoveries in neuroscience and clinical therapy development.
In the realm of neuroimaging research, particularly in studies involving contrast-enhanced magnetic resonance (CE-MR) scans, the reliability of automated segmentation tools is paramount. The foundation for any robust segmentation pipeline lies in its preprocessing steps, with skull stripping and intensity normalization being two critical components. These processes directly impact the quality and consistency of downstream analyses, including volumetric measurements, tissue classification, and pathological assessment. For researchers, scientists, and drug development professionals, selecting the appropriate preprocessing tools is not merely a technical choice but a determinant of the validity and reproducibility of experimental outcomes. This guide provides an objective comparison of contemporary methodologies, underpinned by experimental data, to inform the development of a reliable preprocessing pipeline for CE-MR research.
Skull Stripping Performance Comparison
Skull stripping, or brain extraction, is the process of removing non-brain tissues such as the skull, scalp, and meninges from MR images. Its accuracy is crucial, as residual non-brain tissues can lead to significant errors in subsequent segmentation and analysis.
Quantitative Performance of Skull Stripping Tools
A comprehensive evaluation of state-of-the-art skull stripping tools reveals notable differences in their performance across diverse datasets. The following table summarizes key quantitative metrics from recent large-scale validation studies.
Table 1: Performance Comparison of Modern Skull Stripping Tools
| Tool Name | Methodology | Primary Strength | Reported Dice Score | Key Limitation(s) |
|---|---|---|---|---|
| LifespanStrip [36] | Atlas-powered deep learning | Exceptional accuracy across lifespan (neonatal to elderly) | ~0.99 (on lifespan data) | Complex framework requiring atlas registration |
| SynthStrip [36] [37] | Deep learning trained on synthetic data | High generalizability across contrasts and resolutions | ~0.98 (on diverse data) | Slight under-segmentation in vertex region [36] |
| HD-BET [36] | Deep learning trained on multi-center data | Optimized for clinical neuro-oncology data | ~0.98 (on adult brains) | Subtle under-segmentation; struggles with infants [36] |
| ROBEX [36] | Hybrid generative-discriminative model | Robustness for adult brain imaging | <0.98 (lower on infants) | Noticeable under-segmentation in skull vertex [36] |
| FSL-BET [36] [37] | Deformable surface model | Speed and simplicity | <0.98 (varies with parameters) | Prone to over-segmentation at skull base [36] |
| 3DSS [36] | Hybrid surface-based method | Incorporates exterior tissue context | <0.98 | Over-segmentation in neck/face regions [36] |
| EnNet [38] | 3D CNN for multiparametric MRI | Superior performance on pathological (GBM) brains | ~0.95 (on GBM data) | Designed for mpMRI; performance may vary with single modality |
Experimental Protocols for Skull Stripping Evaluation
The quantitative data in Table 1 is derived from rigorous experimental protocols. A representative large-scale evaluation involved a dataset of 21,334 T1-weighted MRIs from 18 public datasets, encompassing a wide lifespan (neonates to elderly) and various scanners and imaging protocols [36]. The performance was primarily measured using the Dice Similarity Coefficient (Dice Score), which quantifies the spatial overlap between the tool-generated brain mask and a manually refined ground truth mask. A score of 1 indicates perfect overlap.
Another study focused on pathological brains, using a dataset of 815 cases with and without glioblastoma (GBM) from the University of Pittsburgh Medical Center and The Cancer Imaging Archive (TCIA) [38]. Ground truths were verified by qualified radiologists, and evaluation metrics included Dice Score and the 95th percentile Hausdorff Distance (measuring boundary accuracy).
Analysis and Recommendations
The data indicates that deep learning-based tools like LifespanStrip, SynthStrip, and HD-BET generally outperform conventional tools like BET and 3DSS, particularly in handling data heterogeneity [36]. The choice of tool, however, should be guided by the specific research context:
- For lifespan studies involving neonates, infants, or elderly populations, LifespanStrip is highly recommended due to its consistent performance driven by age-specific atlas priors [36].
- For studies with diverse MRI protocols or limited computational resources, SynthStrip presents a robust and generalizable option [36] [37].
- For neuro-oncology research involving brain tumors, tools like EnNet (if multiparametric MRI is available) or HD-BET are more appropriate, as they are validated on pathological brains where tissue appearance and boundaries are altered [38].
It is critical to note that all tools can exhibit failure modes. For example, several methods show consistent under- or over-segmentation in regions like the skull vertex, forehead, and skull base [36]. Furthermore, a recent study highlighted that skull-stripping itself can induce "shortcut learning" in deep learning models for Alzheimer's disease classification, where models may learn to rely on preprocessing artifacts (brain contours) rather than genuine pathological features [39]. This underscores the necessity of visual inspection and quality control after automatic skull stripping.
Intensity Normalization Techniques
Intensity normalization standardizes the voxel intensity ranges across different images, mitigating scanner-specific variations and improving the reliability of radiomic features and tissue segmentation.
Common Normalization Techniques
Unlike skull stripping, intensity normalization often involves simpler mathematical operations, but their selection and application are equally critical.
Table 2: Common Intensity Normalization Techniques in MRI
| Technique | Methodology | Use Case | Effect on Data |
|---|---|---|---|
| Z-score Normalization [40] | Scales intensities to have a mean of 0 and standard deviation of 1. | General-purpose; often used before deep learning model input. | Removes global offset and scales variance; assumes Gaussian distribution. |
| White Matter Peak-based Normalization [41] [39] | Normalizes intensities to the peak of the white matter tissue histogram. | Tissue-specific studies; common in structural T1w analysis. | Anchors intensities to a biologically relevant reference point. |
| Histogram Matching | Transforms the intensity histogram of an image to match a reference histogram. | Standardizing multi-site data to a common appearance. | Can be powerful but depends on the choice of a suitable reference. |
| Kernel Density Estimation (KDE) [41] | A data-driven approach for modeling the intensity distribution without assuming a specific shape. | Handling non-standard intensity distributions. | More flexible than parametric methods for complex distributions. |
Experimental Evidence and Protocols
The effect of intensity normalization was systematically investigated in a study on breast MRI radiomics. The research found that the application of normalization techniques significantly improved the predictive power of machine learning models for pathological complete response (pCR), especially when working with heterogeneous imaging data [41]. A key finding was that the benefit of normalization was more pronounced with smaller training datasets, suggesting it is a vital step when data is limited [41].
In a deep learning study for predicting brain metastases, a comprehensive preprocessing pipeline was implemented where MRI scans underwent skull stripping using SynthStrip followed by intensity normalization via Z-score normalization [40]. This combination contributed to the model's strong robustness and generalizability across internal and external validation sets.
A typical protocol for intensity normalization involves:
- Skull Stripping: This is often a prerequisite to ensure that intensity statistics are computed only from brain tissues [40].
- Background Exclusion: Voxels outside the brain mask are ignored.
- Statistical Calculation: Compute the chosen statistics (e.g., mean, standard deviation, white matter peak) from the voxels within the brain mask.
- Transformation: Apply the linear or non-linear transformation to all voxels in the image.
Integrated Preprocessing Workflow
For optimal results in segmenting CE-MR scans, skull stripping and intensity normalization should be implemented as part of a cohesive pipeline. The following diagram illustrates a recommended workflow and its logical rationale.
The Scientist's Toolkit: Essential Research Reagents & Software
Building a robust preprocessing pipeline requires both data and software tools. The following table details key "research reagents" – essential datasets and software solutions used in the field.
Table 3: Key Research Reagents for Preprocessing Pipeline Development
| Item Name | Type | Function/Benefit | Example Use in Cited Research |
|---|---|---|---|
| Public Datasets (ADNI, dHCP, ABIDE) [36] | Data | Provide large-scale, diverse, multi-scanner MRI data for training and validation. | Used for large-scale evaluation of LifespanStrip across 21,334 scans [36]. |
| Pathological Datasets (TCIA-GBM) [38] | Data | Provide expert-annotated MRIs with pathologies like glioblastoma for domain-specific testing. | Used to train and validate EnNet on pre-/post-operative brains with GBM [38]. |
| FSL (FMRIB Software Library) [39] [37] | Software Suite | Provides a wide array of neuroimaging tools, including BET for skull stripping and FLIRT/FNIRT for registration. | Used for reorientation (FSL-REORIENT2STD) and non-linear registration (FSL-FNIRT) [39]. |
| FreeSurfer [42] [36] | Software Suite | Provides a complete pipeline for cortical reconstruction and volumetric segmentation, including skull stripping. | Used as a benchmark in comparative studies of skull stripping and volumetric reliability [42] [36]. |
| Advanced Normalization Tools (ANTs) | Software | Provides state-of-the-art image registration and bias field correction (e.g., N4). | Used for bias field correction in multiple studies [39]. |
| Python-based Libraries (SimpleITK, SciPy) [37] | Software Libraries | Offer flexibility for implementing custom preprocessing steps, scripting pipelines, and data analysis. | Integrated into a pediatric processing framework for tasks like registration and normalization [37]. |
The reliability of segmentation tools in CE-MR research is fundamentally tied to the preprocessing pipeline. Evidence indicates that deep learning-based skull stripping tools like LifespanStrip and SynthStrip offer superior accuracy and generalizability compared to conventional methods, especially for heterogeneous data. For intensity normalization, techniques like Z-score and white matter peak-based normalization are essential for standardizing data and improving model robustness. The experimental data consistently shows that the choice of software introduces significant variance in results [42]. Therefore, to ensure reliable and reproducible outcomes, researchers must carefully select their preprocessing tools based on their specific data characteristics—such as patient age, pathology, and imaging protocol—and maintain consistency in the software used throughout a study.
The precise segmentation of brain metastases (BMs) on contrast-enhanced magnetic resonance (CE-MR) images is a critical step in diagnostics and treatment planning, directly influencing patient outcomes in stereotactic radiotherapy and surgical interventions [43] [44] [45]. Manual segmentation by clinicians is often time-consuming, labor-intensive, and subject to inter-observer variability, creating a significant bottleneck in clinical workflows [46] [43]. This case study explores the successful application of 3D U-Net-based deep learning models to automate the segmentation of brain metastases, objectively comparing their performance against manual methods and other alternatives. We situate this analysis within a broader thesis on the reliability of different segmentation tools for CE-MR research, providing researchers and drug development professionals with a detailed comparison of experimental protocols, performance data, and practical implementation resources.
Performance Comparison of Segmentation Models
The evaluation of automated segmentation models relies on standardized quantitative metrics that measure the overlap between automated and manual expert segmentations (the reference standard), as well as the physical distance between their boundaries.
Table 1: Key Performance Metrics for Segmentation Model Evaluation
| Metric | Full Name | Interpretation | Ideal Value |
|---|---|---|---|
| DSC | Dice Similarity Coefficient | Measures volumetric overlap between segmentation and ground truth. | 1.0 (Perfect Overlap) |
| IoU | Intersection over Union | Similar to DSC, measures spatial overlap. | 1.0 (Perfect Overlap) |
| HD95 | 95th Percentile Hausdorff Distance | Measures the 95th percentile of the maximum boundary distances, robust to outliers. | 0 mm (No Distance) |
| ASD | Average Surface Distance | Average of all distances between points on the predicted and ground truth surfaces. | 0 mm (No Distance) |
| AUC | Area Under the ROC Curve | Measures the model's ability to distinguish between lesion and non-lesion areas. | 1.0 (Perfect Detection) |
Table 2: Comparative Performance of 3D U-Net Models for Brain Metastasis Segmentation
| Study (Model) | Dataset | Primary Metric (DSC) | Other Key Metrics | Inference Time |
|---|---|---|---|---|
| Bousabarah et al. [44] (Standard 3D U-Net) | Multicenter; 348 patients | 0.89 ± 0.11 (per metastasis) | F1-Score (Detection): 0.93 ± 0.16 | Not Specified |
| BUC-Net [43] (Cascaded 3D U-Net) | Single-center; 158 patients | 0.912 (Binary Classification) | HD95: 0.901 mm; ASD: 0.332 mm; AUC: 0.934 | < 10 minutes per patient |
| 3D U-Net (ResNet-34) [46] | Multi-institutional; 642 patients | AUC: 0.82 (Lung Cancer), 0.89 (Other Cancers) | Specificity: 1.000 across subgroups | 66-69 seconds vs. 96-113s (Manual) |
| MEASegNet [47] (3D U-Net with Attention) | Public (BraTS2021) | 0.845 (Enhancing Tumor) | Not directly comparable (focus on primary tumors) | Not Specified |
The data reveals that 3D U-Net variants achieve high segmentation accuracy, with DSCs exceeding 0.89, indicating excellent volumetric agreement with expert manual contours [43] [44]. The high F1-score of 0.93 further confirms their effectiveness in the detection task, minimizing both false positives and false negatives [44]. A significant finding is the cancer-type dependency of model performance; one study reported a statistically significant lower AUC for metastases from lung cancer (0.82) compared to other primary cancers (0.89), highlighting the need for sensitivity optimization in specific clinical subpopulations [46]. Crucially, all developed models maintain perfect specificity (1.000), meaning they reliably exclude non-metastatic tissue, which is vital for clinical safety [46]. From an efficiency standpoint, these models offer a substantial reduction in processing time, with one model completing segmentation in approximately one minute—about 40-50% faster than manual annotation—freeing up expert time for other critical tasks [46] [43].
Detailed Experimental Protocols
Understanding the methodology is key to evaluating the reliability and reproducibility of these models. The following sections detail the standard experimental protocols used in the cited research.
Data Curation and Preprocessing
A rigorous and standardized preprocessing pipeline is fundamental to developing robust models.
- Patient Selection and Imaging: Studies typically use retrospective data from patients with confirmed brain metastases. The primary imaging modality is contrast-enhanced T1-weighted 3D MRI (e.g., 3D T1-weighted fast field echo or magnetization-prepared rapid gradient-echo sequences). Standard inclusion criteria involve adult patients (≥18 years) with complete clinical data and high-quality, artifact-free MRI scans [46] [43].
- Ground Truth Delineation: The reference standard for training and evaluation is established by manual segmentation performed by experienced radiologists or radiation oncologists (often with 8+ years of experience). Lesions are meticulously outlined on CE-MRI slices, with a third senior expert often consulted to resolve disagreements, ensuring high-quality ground truth [46] [43] [44].
- Image Preprocessing: A multi-step pipeline is employed:
- Resampling: Images are resampled to an isotropic voxel size (e.g., 0.833 mm³) to standardize spatial resolution [46].
- Skull Stripping: Non-brain tissues like the skull and scalp are removed using tools like SynthStrip to focus the model on relevant regions and reduce computational load [46].
- Intensity Normalization: Voxel intensities are normalized, often using Z-score normalization, to reduce scanner-specific variability and improve model convergence [46].
- Data Augmentation: Techniques such as random skewing, rotation, scaling, and flipping are applied during training to artificially expand the dataset and improve model generalizability [44] [48].
Model Architecture and Training
While based on the 3D U-Net, the models incorporate specific enhancements for the task of metastasis segmentation.
- Base 3D U-Net Architecture: The standard 3D U-Net consists of a symmetric encoder-decoder path with skip connections. The encoder (contracting path) uses 3D convolutions and pooling to capture contextual information, while the decoder (expanding path) uses transposed convolutions to precisely localize the metastases. Skip connections combine high-resolution features from the encoder with the upsampled decoder features, preserving spatial details [46] [48].
- Architectural Variants:
- Backbone Enhancement: One study replaced the standard encoder with a ResNet-34 backbone, initialized with weights pre-trained on ImageNet, to enhance feature extraction capabilities [46].
- Cascaded Design (BUC-Net): This approach uses two 3D U-Nets in sequence. The first stage generates a coarse segmentation, which is then refined by the second stage using both the original image and the coarse mask as input. This has proven particularly effective for segmenting small metastases [43].
- Attention Mechanisms (MEASegNet): Integrating channel and spatial attention modules into the U-Net helps the model focus on more relevant features, improving segmentation accuracy for small and complex structures [47].
- Training Strategy: Models are typically trained using a patch-based strategy (e.g., processing 128×128×128 voxel patches) to manage GPU memory constraints. The optimization is performed with algorithms like Adam, and the training objective is often a loss function combining Dice loss and cross-entropy to handle class imbalance between lesion and background voxels [46] [49].
The following diagram illustrates a generalized workflow for developing and validating a 3D U-Net model for metastasis segmentation, incorporating key elements from the described protocols.
The Scientist's Toolkit: Research Reagent Solutions
The following table details essential materials, software, and computational resources used in the featured experiments, providing a practical guide for researchers aiming to replicate or build upon this work.
Table 3: Essential Research Reagents and Resources for 3D U-Net Segmentation
| Category | Item / Tool | Specification / Function |
|---|---|---|
| Imaging Data | Contrast-enhanced T1-weighted 3D MRI | High-resolution (e.g., 1mm³ isotropic) volumetric scans for model input and validation. |
| Annotation Software | ITK-SNAP | Open-source software for semi-automatic and manual segmentation of medical images to create ground truth. |
| Computing Hardware | High-Performance GPU | NVIDIA Tesla P100 or equivalent with ≥16GB VRAM to handle memory-intensive 3D model training. |
| Deep Learning Framework | PyTorch / TensorFlow | Open-source libraries for building and training deep neural networks (e.g., 3D U-Net). |
| Preprocessing Tools | SynthStrip | Robust tool for skull-stripping MR images, critical for focusing the model on brain tissue. |
| Data Augmentation | BatchGenerators / TorchIO | Libraries for implementing on-the-fly spatial and intensity transformations to improve model robustness. |
This case study demonstrates that 3D U-Net models are highly effective and reliable tools for the automated segmentation of brain metastases on CE-MR images. The quantitative evidence shows that these models can achieve accuracy comparable to expert manual segmentation while offering a substantial reduction in processing time, which is crucial for streamlining clinical workflows. Key considerations emerging from the research include the cancer-type dependency of performance and the superior capability of advanced architectures like cascaded networks and attention mechanisms in handling small lesions. For researchers and drug development professionals, these models provide a robust foundation for quantitative imaging analysis, enabling more efficient and objective assessment of tumor burden in therapeutic studies. Future work should focus on improving sensitivity for specific cancer types and further validating these models in large, prospective, multi-center trials to cement their role in both clinical and research settings.
Troubleshooting and Optimization: Strategies for Enhanced Consistency and Accuracy
In neuroimaging research, longitudinal studies are essential for tracking the progression of neurological diseases, monitoring treatment efficacy, and understanding normal brain development and aging. However, the validity of findings from such studies is critically dependent on the consistency of measurement techniques over time. A fundamental yet often overlooked aspect of this consistency is the maintenance of fixed scanner-software combinations—the specific pairing of MRI scanner hardware with a particular software version of a segmentation tool. This guide examines the profound impact of these combinations on data reliability, providing a critical evidence-based recommendation for their preservation throughout longitudinal research projects.
The Critical Impact of Scanner and Software Variability
Evidence on Scanner-Induced Variability
Technical variability introduced by MRI scanners is a significant source of error in longitudinal studies. Even under controlled conditions, scanner effects can compromise data integrity.
- Inter-Scanner Variability: A key investigation demonstrated that even with two 3.0-T scanners of the exact same model, inter-scanner variability (bias) significantly affected longitudinal results for diffusion tensor imaging (DTI) metrics, including fractional anisotropy (FA), axial diffusivity (AD), and radial diffusivity (RD). This finding indicates that simply using the same scanner model is insufficient; the same physical unit is necessary for consistent measurements [50].
- Scanner Upgrades: The same study also revealed that scanner upgrades can introduce significant technical variability. An upgrade that involved only software, not hardware, still produced a significant effect on longitudinal DTI results. This underscores that any modification to the scanning environment, even if seemingly minor, can alter the resulting data [50].
Evidence on Segmentation Software Variability
Automated segmentation tools are indispensable for quantifying brain structures, but they are not interchangeable. Different algorithms can produce markedly different results from the same input data.
- Tool Comparison in Disease Cohorts: A systematic comparison of seven GM segmentation tools (including SPM, FSL, and FreeSurfer) in Huntington's disease patients and controls found large volumetric variability between tools, particularly in occipital and temporal regions. The results for longitudinal within-group change also varied considerably between software packages, highlighting that the choice of tool can directly influence the sensitivity to detect disease progression [51].
- Reliability vs. Accuracy: While tools like FreeSurfer demonstrate high test-retest reliability (consistency), they are not necessarily accurate in measuring true GM volume in healthy controls [52] [51]. This distinction is crucial for studies tracking absolute volumetric change over time.
- Performance in Pathological Brains: Most segmentation tools are developed and optimized for healthy brains. When applied to clinical cohorts with disease-specific anatomical changes (e.g., atrophy), their performance can degrade, leading to poor segmentation and biased results [52] [51].
Quantitative Comparison of Segmentation Tools
The table below summarizes key performance characteristics of commonly used, publicly available neuroimaging segmentation tools, based on empirical comparisons.
Table 1: Comparison of Publicly Available Automated Brain Segmentation Tools
| Software Tool | Key Methodology | Reliability & Performance Notes | Longitudinal Sensitivity |
|---|---|---|---|
| FreeSurfer [52] | Atlas-based, probabilistic segmentation, surface-based reconstruction. | High test-retest reliability [52] [53]. May be less accurate for absolute GM volume in healthy controls [51]. | Sensitive to disease-related change in Alzheimer's and HD cohorts [52] [51]. Reliable for hippocampal subregion volume tracking [53]. |
| FSL (FMRIB Software Library) [52] | Model-based segmentation (e.g., FAST), brain extraction (BET). | Reliable and accurate for GM segmentation in phantom and control data [51]. | Sensitive to GM change in Alzheimer's disease [52]. Shows variability in longitudinal change detection in HD [51]. |
| SPM (Statistical Parametric Mapping) [52] | Voxel-based morphometry (VBM), Gaussian Mixture Model. | Reliable and accurate in phantom data [51]. Can overestimate group differences in atypical anatomy [51]. | Sensitive to disease-related change in Alzheimer's and HD [52] [51]. Performance can be affected by image noise [51]. |
| ANTs (Advanced Normalization Tools) [51] | Multi-atlas segmentation with advanced normalization (symmetry). | A newer tool showing promise; performance varies by brain region and cohort [51]. | Shows variable sensitivity to longitudinal change in clinical cohorts like HD [51]. |
| MALP-EM [51] | Multi-atlas label propagation with Expectation-Maximization refinement. | A newer tool showing promise; performance varies by brain region and cohort [51]. | Shows variable sensitivity to longitudinal change in clinical cohorts like HD [51]. |
Experimental Protocols for Validating Segmentation Tools
To ensure reliable longitudinal measurements, researchers should empirically validate their chosen scanner-software combination before initiating a long-term study. The following protocols outline key experiments for establishing reliability and sensitivity.
Protocol 1: Test-Retest Reliability Analysis
This experiment assesses the short-term stability and precision of volumetric measurements from a specific scanner-software pipeline.
- Objective: To determine the intra-scanner, intra-software test-retest reliability of segmentation outcomes.
- Materials:
- Participants: A small cohort (e.g., n=5-10) of healthy control participants or phantoms.
- Scanner: The specific MRI scanner designated for the longitudinal study.
- Software: The specific version of the segmentation software (e.g., FreeSurfer 6.0).
- Method:
- Data Acquisition: Each participant is scanned twice on the same scanner within a short period (e.g., 1-2 weeks) to minimize biological change.
- Scan Parameters: Use the identical T1-weighted MRI sequence and parameters planned for the main longitudinal study.
- Segmentation: Process all scans using the same software version and processing pipeline.
- Data Analysis:
- Extract volumetric measures for regions of interest (ROIs) such as total GM, hippocampal subfields [53], or lobular volumes [51].
- Calculate the Intra-class Correlation Coefficient (ICC) for each ROI to quantify reliability. ICC values >0.9 are generally considered excellent [53].
- Compute percentage volume difference and Dice overlap coefficients to assess agreement [53].
- Expected Outcome: A highly reliable pipeline will yield high ICC values (>0.9) and low percentage differences for key ROIs, confirming its stability for repeated measurements [53].
Protocol 2: Longitudinal Sensitivity in a Clinical Cohort
This experiment evaluates the pipeline's ability to detect biologically plausible changes over time, which is the ultimate goal of a longitudinal study.
- Objective: To determine the sensitivity of the scanner-software combination to detect longitudinal change in a clinical population.
- Materials:
- Method:
- Data Processing: Process all longitudinal scans from both groups using the fixed software pipeline.
- Volume Extraction: Extract ROI volumes (e.g., hippocampal subfields, cortical GM) at all time points.
- Statistical Analysis: Employ Linear Mixed Effects (LME) modelling to estimate the rate of volume change over time within each group [53].
- Comparison: Statistically compare the slopes of change between the clinical and control groups. A sensitive pipeline will show a significantly steeper rate of atrophy in the clinical group for regions known to be affected by the disease (e.g., hippocampus in AD) [53].
- Expected Outcome: A sensitive and valid pipeline will detect statistically significant differences in the rate of volumetric change between groups, confirming its utility for tracking disease progression [53] [51].
The workflow for implementing and validating a fixed scanner-software combination is summarized in the diagram below.
The Scientist's Toolkit: Essential Research Reagents and Materials
For researchers designing a longitudinal neuroimaging study, the following "toolkit" comprises the essential components that must be carefully selected and documented.
Table 2: Essential Research Reagents and Materials for Longitudinal Neuroimaging
| Item | Function & Critical Consideration |
|---|---|
| MRI Scanner | The physical hardware for data acquisition. Critical: The specific scanner unit (not just model) must be identified and maintained for the study's duration to minimize inter-scanner variability [50]. |
| Segmentation Software | The algorithm for automated tissue/structure quantification. Critical: The specific software name and version must be documented and locked. Changes in version can alter outputs as significantly as changing tools [52] [51]. |
| Computing Infrastructure | Hardware and OS for running analysis software. Critical: Ensure processing environment consistency, as different operating systems or library versions can subtly influence results. |
| Phantom Datasets | Objects with known properties scanned to monitor scanner performance. Critical: Use for regular quality assurance to detect scanner drift over time [50]. |
| Reference Datasets | Public datasets (e.g., ADNI, OASIS) with known outcomes. Critical: Serve as a benchmark for validating the sensitivity of your pipeline to detect expected changes [52] [53]. |
| Harmonization Tools (e.g., ComBat) | Statistical tools for removing scanner and site effects. Critical: A contingency tool for mitigating variability if a break in the scanner-software combination is unavoidable [54]. |
The evidence from empirical comparisons is clear: both the MRI scanner hardware and the version of segmentation software are significant sources of non-biological variance in longitudinal neuroimaging measurements. This variability can obscure true biological change, reduce statistical power, and lead to inconsistent or erroneous findings.
Therefore, the critical recommendation is to establish and maintain a fixed scanner-software combination for the entire duration of any longitudinal neuroimaging study. This involves:
- Pre-Study Validation: Rigorously testing the chosen pipeline for reliability and sensitivity using test-retest and clinical validation protocols.
- Meticulous Documentation: Recording the exact scanner serial number and software version number in study protocols and publications.
- Strict Change Control: Treating any proposed change to the scanner hardware (including upgrades) or software version as a major protocol amendment, to be avoided if at all possible.
Adhering to this practice is not merely a technical detail but a fundamental requirement for ensuring the scientific validity, reproducibility, and success of longitudinal neuroimaging research.
Segmentation of medical images, particularly Contrast-Enhanced Magnetic Resonance (CE-MR) scans, is a foundational step in quantitative biomedical research and drug development pipelines. Its reliability directly influences downstream analyses, from tumor volume measurement to treatment efficacy assessment. Despite advancements in algorithm development, segmentation failures and tool-specific inconsistencies remain significant hurdles, potentially compromising the validity of research findings and clinical decisions. This guide objectively compares the performance profiles of prominent segmentation tools, analyzes the root causes of their failures using published experimental data, and provides a structured framework for researchers to enhance the robustness of their segmentation workflows. The focus is specifically on their application in CE-MR research, where contrast variability and complex lesion morphology present unique challenges.
Comparative Analysis of Segmentation Tool Performance
Evaluating segmentation tools requires a multi-faceted approach, examining not just raw accuracy but also usability, integration capabilities, and scalability. The following table summarizes the key characteristics of several prominent tools.
Table 1: Comparison of Key Image Segmentation Tools
| Tool Name | Primary Features | Integration & Scalability | Pros | Cons |
|---|---|---|---|---|
| DagsHub Annotation [55] | Web-based interface, pixel-level annotations, version control. | Integrates with TensorFlow, PyTorch; scalable for large projects. | User-friendly; strong collaboration tools; flexible pricing. | Limited customization for advanced users; initial learning curve. |
| Labelbox [55] | Cloud-based, ML-assisted workflows, automated quality assurance. | Integrates with TensorFlow, PyTorch, OpenCV; enterprise-scale. | Efficient annotation process; advanced quality control. | Higher cost; steep learning curve for non-technical users. |
| SuperAnnotate [55] | Comprehensive platform for images/videos, ML-based capabilities. | Integrates with popular ML frameworks; scalable architecture. | Handles large-scale datasets; robust automation. | Performance varies with complex datasets; requires technical know-how. |
| CVAT (Computer Vision Annotation Tool) [55] | Open-source, supports polyline and interpolation-based tasks. | Highly customizable via plugins/APIs; handles large datasets. | No licensing cost; strong community support. | High learning curve; advanced features need technical setup. |
Quantitative Performance in Medical Imaging
Beyond features, performance on specific medical imaging tasks is paramount. Independent studies using standardized metrics like the Dice Similarity Coefficient (DSC) reveal significant performance variations across algorithms and imaging modalities.
Table 2: Quantitative Performance of Segmentation Models in Medical Studies
| Study Context | Model / Tool | Modality | Key Performance Metric (DSC) | Notable Findings |
|---|---|---|---|---|
| Pediatric Brain Segmentation [56] | 3D U-Net | CT | 0.88 | Used as a baseline model in the study. |
| ResU-Net (1,3,3) | CT | 0.92 | Performance improvement over standard U-Net. | |
| ResU-Net (3,3,3) | CT | 0.96 | Demonstrated robust segmentation performance, highest in the study. | |
| Ischemic Stroke Lesion Segmentation [57] | Fully Connected Network (FCN) | DWI (MRI) | 0.8286 ± 0.0156 | Lower performance compared to U-Net architecture. |
| U-Net | DWI (MRI) | 0.9213 ± 0.0091 | Superior performance for lesion segmentation on DWI. | |
| Fully Connected Network (FCN) | ADC (MRI) | 0.7926 ± 0.0119 | Highlighted challenges with ADC-based segmentation. | |
| U-Net | ADC (MRI) | 0.8368 ± 0.1000 | Better than FCN on ADC, but higher variance and lower than DWI performance. |
The data shows that while modern tools like ResU-Net can achieve remarkably high DSC scores (e.g., 0.96 on brain CTs [56]), performance is highly dependent on the specific architecture, imaging modality, and clinical target. The consistent superiority of U-Net over FCN for stroke lesion segmentation [57] underscores the impact of model design, while the performance gap between DWI and ADC underscores the critical influence of input data characteristics.
Experimental Protocols and Methodologies
A critical step in understanding and addressing segmentation failures is a rigorous experimental setup. The following protocols, derived from recent studies, provide a blueprint for benchmarking tool performance.
Protocol 1: Deep Learning Model Training for Brain Segmentation
This protocol is adapted from the study on pediatric brain CT segmentation using ResU-Net [56].
- Objective: To automatically segment 10 brain regions (e.g., frontal lobes, temporal lobes, cerebellum) and establish normative volume databases.
- Dataset:
- Cohort: 1,487 head CT scans from 2-year-old children with normal radiological findings.
- Split: Divided into training (n=1,041) and testing (n=446) sets in a 7:3 ratio.
- Data Preprocessing:
- Resampling: Voxel spacing unified to 1×1×1 mm³ using linear interpolation.
- Intensity Normalization: Adaptive histogram equalization was applied to enhance contrast.
- Skull Stripping: The skull was removed using SimpleITK threshold segmentation to isolate brain tissue.
- Model Training:
- Architecture: ResU-Net, a hybrid model combining residual connections and U-Net's skip connections.
- Augmentation: Random flips and rotations on the training set to improve model robustness.
- Training Parameters: Multi-class cross-entropy loss function; Adam optimizer with a learning rate of 1×10⁻⁵; five-fold cross-validation.
Figure 1: Experimental workflow for deep learning-based brain segmentation.
Protocol 2: Comparing Segmentation Performance Across MRI Sequences
This protocol is derived from the research comparing DWI and ADC for stroke lesion segmentation [57].
- Objective: To compare the lesion segmentation performance of artificial neural networks on Diffusion-Weighted Imaging (DWI) versus Apparent Diffusion Coefficient (ADC) images.
- Dataset:
- Cohort: 360 patients diagnosed with ischemic stroke.
- Images: 999 paired slices of DWI (b-value=1000) and ADC from the same anatomical locations.
- Ground Truth: Manual masks of ischemic stroke lesions created by experts and cross-validated.
- Experimental Setup:
- Data Split: 80:20 ratio for training (n=799 images) and testing (n=200 images).
- Models: U-Net and a Fully Connected Network (FCN) were trained and compared.
- Validation: Five-fold cross-validation was employed.
- Evaluation Metrics: Dice Similarity Coefficient (DSC), Accuracy, Precision, and Recall.
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful segmentation requires more than just software; it relies on a suite of data and computational resources. The table below details key "research reagents" for this field.
Table 3: Essential Materials and Resources for Segmentation Research
| Item Name / Category | Function & Role in the Workflow | Specific Examples & Notes |
|---|---|---|
| Public Datasets [58] | Provide standardized, annotated data for training and benchmarking algorithms. | LiTS: 201 abdominal CTs for liver/tumor segmentation. 3DIRCADb: 20 CT scans for complex liver structures. ATLAS: First public dataset for CE-MRI of inoperable HCC. |
| Evaluation Metrics [58] | Quantify segmentation accuracy and reliability for objective comparison. | Dice Similarity Coefficient (DSC): Measures voxel overlap. Jaccard Index (JI): Ratio of intersection to union. Average Symmetric Surface Distance (ASSD): Assesses boundary accuracy. |
| Deep Learning Frameworks [55] [56] | Provide the programming environment to build, train, and deploy segmentation models. | PyTorch, TensorFlow. Essential for implementing models like U-Net and ResU-Net, and for transfer learning. |
| Quality Control Tools [59] | Identify segmentation inaccuracies and outliers to ensure data integrity. | Manual Inspection: Gold standard but time-consuming. Automated Tools (MRIQC, Euler numbers): Time-efficient and reproducible for large samples. |
Analysis of Failure Modes and Mitigation Strategies
The experimental data reveals common failure modes. In the stroke study, the lower and more variable DSC for ADC-based segmentation (0.8368 ± 0.1000) [57] points to failures linked to input data characteristics, where the lower contrast-to-noise ratio in ADC maps challenges the model. Furthermore, the heavy reliance on public datasets like LiTS and 3DIRCADb, which have limitations in sample size and lesion diversity [58], can lead to algorithmic bias and poor generalization.
To mitigate these failures, researchers should:
- Employ Multi-Modal Data: Where possible, use complementary image sequences (e.g., combining DWI and ADC [57]) or modalities to provide the model with more information.
- Implement Rigorous Quality Control: Adopt a semi-automated QC strategy, using automated tools like MRIQC to flag potential failures for manual inspection, balancing efficiency and reliability [59].
- Utilize Advanced Pre-processing: For MR images, frameworks like MedGA that use genetic algorithms to enhance bimodal histogram separation can significantly improve subsequent segmentation accuracy [60].
- Understand Metric Limitations: Recognize that a high DSC might mask poor performance in small or complex structures, and always supplement it with boundary-focused metrics like ASSD [58].
Segmentation failures driven by tool-specific inconsistencies are a critical concern in CE-MR research. This analysis demonstrates that there is no single "best" tool; rather, the choice depends on the specific imaging modality, anatomical target, and required precision. The U-Net architecture and its variants consistently show high performance, but their success is contingent on high-quality, representative data and rigorous evaluation beyond a single metric. By adopting the detailed experimental protocols, leveraging the essential research toolkit, and understanding common failure modes, researchers and drug developers can build more resilient segmentation workflows. This, in turn, enhances the reliability of quantitative imaging biomarkers, ultimately accelerating robust scientific discovery and therapeutic development.
In the field of medical image analysis, particularly in the segmentation of Contrast-Enhanced Magnetic Resonance (CE-MR) scans, deep learning models have demonstrated remarkable potential. However, their performance is heavily contingent on the availability of large, high-quality annotated datasets, which are often scarce in clinical research settings due to factors such as patient privacy concerns, rare pathologies, and the high cost of expert annotation [61]. This data scarcity can lead to models that suffer from overfitting and poor generalization to new data.
To combat these challenges, two primary regularization techniques have emerged as effective solutions: data augmentation and transfer learning. Data augmentation artificially expands the training dataset by applying label-preserving transformations to existing data, thereby increasing its diversity and quantity [62]. Transfer learning, conversely, leverages knowledge from a model previously trained on a related task or dataset, adapting it to the new target task where data may be limited [63]. This guide provides an objective comparison of these two approaches, focusing on their application in validating the reliability of segmentation tools for CE-MR scans, a critical task in areas like oncology and neurodegenerative disease research [64] [65].
Methodology and Technical Approaches
Data Augmentation: Techniques and Workflows
Data augmentation encompasses a range of techniques designed to artificially increase the size and diversity of a training dataset. These methods can be broadly categorized into classical and automated approaches.
Classical data augmentation typically involves predefined, often geometric or photometric, transformations. These include affine transformations such as rotation, scaling, and translation, which modify the spatial arrangement of pixels without altering their intensity values, making them particularly suitable for tasks where bone morphology is important [63]. Photometric transformations, like adjusting brightness, contrast, or adding noise, help models become more robust to variations in image acquisition [66].
Automated data augmentation employs Automated Machine Learning (AutoML) principles to algorithmically find the most effective combination of augmentation policies for a specific dataset. This approach treats augmentation as a combinatorial optimization problem, using search methods to select and tune transformations, thereby overcoming the limitations of manual trial and error [66].
The following diagram illustrates a typical workflow for applying data augmentation, integrating both classical and automated concepts:
Transfer Learning: Concepts and Implementation
Transfer learning involves adapting a pre-trained model to a new, but related, task. The underlying assumption is that features learned from a large source dataset (e.g., natural images or MRIs from a different anatomical site) can be transferable and provide a beneficial starting point for learning the target task [63] [67].
A common implementation involves using a network pre-trained on a large dataset and then fine-tuning its weights on the smaller target dataset. Often, only the weights of the final layers are updated, while the earlier convolutional layers, which capture general features like edges and textures, are kept frozen [63]. The success of transfer learning is highly dependent on the similarity between the source and target domains. For instance, one study showed that transfer learning from a model trained to segment shoulder bones was more effective for segmenting the femur (which resembles the humerus) than for the acetabulum (which has a different topology than the glenoid) [63].
The workflow for transfer learning is depicted below:
Experimental Comparison and Performance Data
Direct comparisons between data augmentation and transfer learning provide valuable insights for researchers. One study on the automatic segmentation of the femur and acetabulum from 3D MR images in patients with femoroacetabular impingement offers a clear, quantitative comparison.
Table 1: Performance Comparison of Data Augmentation vs. Transfer Learning for Hip Joint Segmentation [63]
| Anatomical Structure | Technique | Dice Similarity Coefficient (DSC) | Accuracy |
|---|---|---|---|
| Acetabulum | Data Augmentation | 0.84 | 0.95 |
| Acetabulum | Transfer Learning | 0.78 | 0.87 |
| Femur | Data Augmentation | 0.89 | 0.97 |
| Femur | Transfer Learning | 0.88 | 0.96 |
The results indicate that while both methods are effective, data augmentation yielded superior performance for the more complex acetabulum structure, likely because its shape is less similar to the shoulder bones from the source model. The performance for the femur was high and comparable for both techniques [63].
Beyond these core metrics, a comprehensive evaluation framework like the COMprehensive MUltifaceted Technical Evaluation (COMMUTE) is recommended for a complete picture. COMMUTE integrates four key assessments [68]:
- Quantitative Geometric Measures: Using metrics like DSC and Hausdorff Distance.
- Qualitative Expert Evaluation: Clinical acceptability ratings by domain experts.
- Time Efficiency Analysis: Measuring the time saved in contouring.
- Dosimetric Evaluation: Assessing the impact of segmentation variations on clinical outcomes like radiation treatment plans.
Practical Implementation Guide
The Researcher's Toolkit for Segmentation Reliability
Successfully implementing data augmentation or transfer learning requires a suite of methodological tools and reagents. The following table details essential components for a robust research workflow.
Table 2: Essential Research Toolkit for Segmentation Studies
| Tool Category | Specific Examples | Function & Application |
|---|---|---|
| Segmentation Software | 3D Slicer [69], ITK-Snap [69] | Open-source platforms for manual, semi-automated, and AI-assisted segmentation and analysis. |
| Evaluation Metrics | Dice Similarity Coefficient (DSC) [63] [68], Hausdorff Distance (HD) [68] | Quantitative measures of geometric overlap and boundary accuracy between automated and ground truth segmentations. |
| Validation Frameworks | COMMUTE Framework [68], CLEAR Checklist [69] | Structured methodologies for comprehensive technical and clinical validation of segmentation models. |
| Imaging Protocols | DICOM SEG Object Standard [69], Slice Thickness Guidelines [69] | Standards and protocols to ensure image quality, consistency, and interoperability of segmentation data. |
| AI Model Architectures | U-Net [63], ResNet50 [67] | Established deep learning network architectures commonly used as a base for segmentation tasks and transfer learning. |
Decision Workflow for Researchers
Choosing between data augmentation and transfer learning is not always straightforward. The following diagram outlines a decision pathway to guide researchers:
Both data augmentation and transfer learning are powerful, validated techniques for mitigating data limitations in medical image segmentation. The experimental evidence suggests that data augmentation can be a more universally reliable starting point, particularly when the target task lacks a highly similar pre-trained model [63]. However, transfer learning can achieve state-of-the-art results, especially when a well-chosen source model is available and the computational cost of training from scratch is prohibitive [67].
For researchers and drug development professionals validating segmentation tools on CE-MR scans, the choice is not necessarily mutually exclusive. A hybrid approach, utilizing transfer learning to initialize a model which is then fine-tuned on an aggressively augmented target dataset, often yields the best performance. The ultimate measure of success should extend beyond geometric metrics like Dice to include clinical utility, workflow efficiency, and impact on downstream tasks such as treatment planning [68] [69].
In clinical neuroscience and drug development research, magnetic resonance imaging (MRI) is indispensable for quantifying brain structures and pathological markers. A significant portion of clinically acquired scans are contrast-enhanced (CE-MR), primarily used for detailed vasculature and lesion delineation. Historically, these scans have been underutilized for computational morphometry due to concerns that the contrast agent might alter intensity-based automated measurements, creating a bottleneck in research workflows [1] [2]. The critical challenge is therefore to identify segmentation tools that can reliably leverage these existing clinical scans without sacrificing accuracy for speed, thereby optimizing the end-to-end research pipeline. This guide objectively compares the performance of leading segmentation tools when processing CE-MR scans, providing researchers and drug development professionals with data-driven insights to balance processing time and segmentation accuracy.
Quantitative Comparison of Segmentation Tools
Performance on Contrast-Enhanced MRI Brain Volumetry
A direct comparative study of T1-weighted CE-MR and non-contrast MR (NC-MR) scans from 59 normal participants provides key insights into tool reliability. The following table summarizes the volumetric agreement and performance of two segmentation tools, CAT12 and SynthSeg+, when applied to CE-MR images [1] [2].
Table 1: Comparative Performance of Segmentation Tools on CE-MR Brain Scans
| Segmentation Tool | Underlying Technology | Key Performance Metrics (CE-MR vs NC-MR) | Notable Strengths | Key Limitations |
|---|---|---|---|---|
| SynthSeg+ | Deep Learning (DL) | High reliability for most structures (ICCs > 0.90); stronger agreement for larger structures (ICC > 0.94) [1]. | Robust to contrast agents; high consistency in age prediction models using CE-MR [1]. | Discrepancies in CSF and ventricular volumes [1]. |
| CAT12 | Based on Statistical Parametric Mapping (SPM) | Inconsistent performance; demonstrated relatively higher discrepancies between CE-MR and NC-MR scans [1] [2]. | N/A | Segmentation failure on 4 out of 63 initial CE-MR scans [2]. |
Performance Across Diverse Anatomical Regions
The reliability of deep learning segmentation extends beyond cerebral volumetry. The following table synthesizes performance metrics from various clinical segmentation tasks, demonstrating the broad applicability of DL models.
Table 2: Deep Learning Segmentation Performance in Various Clinical Applications
| Clinical Application / Structure | Segmentation Model | Reported Performance (Dice Score) | Additional Metrics |
|---|---|---|---|
| Prostate (T2-weighted MRI) | Adapted EfficientDet | 0.914 [70] | Absolute volume difference: 5.9%; MSD: 1.93 px [70] |
| Cerebral Small Vessel Disease Markers | Custom DL Model | WMH: 0.85; CMBs: 0.74; Lacunes: 0.76; EPVS: 0.75 [71] | Excellent positive correlation with manual approach (Pearson's r > 0.947) [71] |
| Brain Tumor (MRI) | Multiscale Deformable Attention Module (MS-DAM) | Classification Accuracy: > 96.5% [72] | Enabled classification of 14 tumor types [72] |
Detailed Experimental Protocols
Protocol 1: Reliability of Volumetry on CE-MR Scans
A. Data Acquisition:
- Cohort: 59 paired MRI scans from clinically normal individuals (age range: 21-73 years; 24 females) [2].
- Scan Type: Paired T1-weighted CE-MR and NC-MR scans.
- Ethics: Approved by the relevant institutional review board; consent waived for retrospective analysis [2].
B. Image Preprocessing:
- Initial pool of 63 image pairs was carefully processed.
- Four scans were excluded due to CAT12 segmentation failure on CE-MR images, highlighting a specific vulnerability [2].
C. Segmentation and Analysis:
- Tools: SynthSeg+ and CAT12 segmentation tools were applied to all scans [1].
- Comparison: Volumetric measurements for various brain structures were compared between CE-MR and NC-MR scans.
- Statistical Analysis: Intraclass Correlation Coefficients (ICCs) were calculated to assess reliability. Age prediction models were also built and compared to evaluate downstream analysis impact [1] [2].
Protocol 2: Benchmarking Prostate Segmentation Models
A. Data and Ground Truth:
- Cohort: 100 patients with prostate adenocarcinoma [70].
- Imaging: T2-weighted MR images.
- Ground Truth: Established by consensus from two expert radiologists with over five years of experience [70].
B. Compared Methods: Six automatic segmentation methods were benchmarked:
- Multi-atlas algorithm (Raystation 9B)
- Proprietary algorithm (Siemens Syngo.Via)
- V-net (3D U-net evolution) trained from scratch
- Pre-trained 2D U-net (transfer learning)
- Generative Adversarial Network (GAN) extension of the 2D U-net
- Segmentation-adapted EfficientDet architecture [70]
C. Evaluation Metrics: Models were evaluated using a 70/30 and a 50/50 train/test split on:
- Dice Similarity Coefficient (Dice)
- Absolute Relative Volume Difference (ARVD)
- Mean Surface Distance (MSD)
- 95th-percentile Hausdorff Distance (HD95) [70]
Workflow and Logical Diagrams
Diagram 1: Clinical segmentation workflow for CE-MR scans.
Diagram 2: Advanced DL model with multiscale attention.
The Scientist's Toolkit: Key Research Reagents and Solutions
Table 3: Essential Tools and Datasets for Medical Image Segmentation Research
| Tool / Resource | Type | Primary Function in Research | Key Characteristics |
|---|---|---|---|
| SynthSeg+ | Software Tool | Brain MRI volumetry on both standard and contrast-enhanced scans [1]. | Robust to contrast agents; handles MRIs with different contrasts and resolutions [1]. |
| CAT12 | Software Tool | Brain morphometry within the SPM framework [2]. | Can be inconsistent with CE-MR; may fail or produce higher discrepancies [1] [2]. |
| EfficientDet (Adapted) | Model Architecture | Segmentation of organs (e.g., prostate) and potentially other structures [70]. | Achieved highest Dice (0.914) in prostate segmentation benchmark [70]. |
| Multi-Atlas Algorithms | Method | Automatic segmentation via image registration and label fusion [70]. | Found in commercial clinical software; performed significantly worse than DL (Dice 0.855-0.887) [70]. |
| Internal CSVD Dataset | Research Dataset | Training/validation for cerebral small vessel disease marker segmentation [71]. | Includes multisequence MRI with manual annotations for WMH, CMBs, lacunes, and EPVS [71]. |
| Proprietary Clinical Software (e.g., Syngo.Via) | Commercial Software | Provides segmentation tools within clinical radiology workflow [70]. | DL-based; performance may lag behind state-of-the-art research algorithms [70]. |
Validation and Comparative Analysis: Benchmarking Segmentation Tool Performance
In the fields of medical imaging research and drug development, the reliability of automated segmentation tools is paramount for generating robust, quantitative biomarkers from contrast-enhanced magnetic resonance (CE-MR) scans. Variability in scanner parameters, particularly magnetic field strength, can introduce significant measurement inconsistencies that may obscure true biological signals and compromise clinical trial outcomes [73] [27]. This guide establishes the COMMUTE Model (Comprehensive Methodology for Metric Uniformity and Tool Evaluation), a multifaceted validation framework designed to objectively compare the performance and reliability of leading brain segmentation tools when applied to CE-MR data. We present a structured comparison of FreeSurfer and Neurophet AQUA, leveraging published experimental data to evaluate their accuracy, reliability, and practical performance under varying magnetic field strengths (1.5T and 3T) [73].
Tool Performance Comparison
Quantitative Performance Metrics
The following tables summarize the key performance indicators for FreeSurfer and Neurophet AQUA, based on a multi-site study involving 101 patients for the 1.5T–3T dataset and 112 patients for the 3T–3T dataset [73].
Table 1: Volumetric Segmentation Accuracy (Dice Similarity Coefficient)
| Brain Region | Neurophet AQUA (3T) | Neurophet AQUA (1.5T) | FreeSurfer (3T) | FreeSurfer (1.5T) |
|---|---|---|---|---|
| Overall DSC | 0.83 ± 0.01 | 0.84 ± 0.02 | 0.98 ± 0.01 | 0.97 ± 0.02 |
Table 2: Volume Measurement Differences Across Magnetic Field Strengths
| Brain Region | Neurophet AQUA Avg. Volume Difference % | FreeSurfer Avg. Volume Difference % |
|---|---|---|
| Putamen | <10% | >10% |
| Amygdala | <10% | >10% |
| Hippocampus | <10% | >10% |
| Inferior Lateral Ventricles | <10% | >10% |
| Cerebellum | <10% | >10% |
| Cerebral White Matter | <10% | >10% |
Table 3: Comparative Processing Efficiency
| Tool | Segmentation Time | Key Reliability Metric |
|---|---|---|
| Neurophet AQUA | ~5 minutes | Smaller average volume difference percentage across field strengths [73] |
| FreeSurfer | ~1 hour | Comparable ICCs across field strengths, but larger volume differences [73] |
Key Comparative Findings
- Segmentation Quality: While both tools achieved clinically acceptable Dice Similarity Coefficients (DSC > 0.8), visual assessment revealed qualitative differences. Neurophet AQUA demonstrated more stable connectivity in segmented regions, notably without encroaching on adjacent structures like the inferior lateral ventricle, an issue occasionally observed with FreeSurfer [73].
- Measurement Reliability: Neurophet AQUA exhibited superior consistency in volumetric measurements when scanner field strength was changed, demonstrating an average volume difference percentage of less than 10% across most brain regions. FreeSurfer showed greater variability, with differences exceeding 10% in the same regions [73].
- Systematic Volume Differences: Systematic variations in absolute volume measurements were observed. Hippocampus volume was consistently larger when segmented with FreeSurfer, whereas Neurophet AQUA yielded larger volumes for structures like the putamen, amygdala, and cerebral white matter [73].
Experimental Protocols for Tool Validation
COMMUTE Model Validation Workflow
The COMMUTE Model prescribes a standardized workflow for tool evaluation, as illustrated below.
Detailed Methodological Components
Subject & Scanner Cohort Definition:
- Population: The referenced study included 101 patients (30 Asian, 71 Caucasian) for the 1.5T–3T dataset and 112 patients for the 3T–3T dataset, sourced from both hospital cohorts and open-source databases like the Alzheimer’s Disease Neuroimaging Initiative (ADNI) and Open Access Series of Imaging Studies 3 (OASIS3) [73].
- Scanner Parameters: MRI scans were acquired from both 1.5T and 3T scanners across multiple imaging centers to ensure heterogeneity and real-world applicability [73].
Ground Truth Creation:
- Expert Delineation: Three radiologists with 15, 9, and 5 years of experience established the ground truth through consensus manual segmentation [73].
- Validation Metric: The Dice Similarity Coefficient (DSC) was used as the primary metric for spatial overlap accuracy, calculated as twice the area of overlap divided by the sum of the areas of the two segmentations [73].
Automated Segmentation & Quantitative Analysis:
- Tool Execution: Each tool (FreeSurfer and Neurophet AQUA) was run on the same dataset according to their standard processing pipelines [73].
- Core Metrics:
- Accuracy: Dice Similarity Coefficient (DSC) comparing automated results to expert ground truth [73].
- Reliability: Intraclass Correlation Coefficient (ICC) and average volume difference percentage to assess consistency across different magnetic field strengths [73].
- Geometric Accuracy: Hausdorff Distance (HD) can be used to evaluate the largest segmentation boundary error [74].
The Scientist's Toolkit
Table 4: Essential Research Reagents and Resources
| Item | Function/Description | Example/Note |
|---|---|---|
| Multi-Scanner MRI Datasets | Provides real-world data with inherent variability to test robustness. | 1.5T and 3T scans from public databases (e.g., ADNI, OASIS3) and institutional cohorts [73]. |
| Expert-Rated Ground Truth | Serves as the benchmark for evaluating automated segmentation accuracy. | Manual segmentation by multiple radiologists achieving consensus [73]. |
| Statistical Analysis Software | Used for calculating reliability metrics and performing statistical comparisons. | Capable of computing ICC, DSC, HD, and performing tests like Friedman and post-hoc Nemenyi [73] [74]. |
| High-Performance Computing | Executes computationally intensive segmentation algorithms in a feasible time. | Essential for tools like FreeSurfer, which can take ~1 hour per case [73]. |
Implications for Drug Development
The reliability of segmentation tools directly impacts the quality of imaging biomarkers used in clinical trials. A phase-appropriate validation strategy is critical [75]. In early-phase trials, establishing that a tool can reliably segment structures of interest with minimal variability due to scanner differences is sufficient. For late-phase trials, where imaging biomarkers may serve as secondary or primary endpoints, a full validation per the COMMUTE model is warranted to ensure that measured changes reflect true biological effects rather than technical noise [73] [27]. This rigorous approach aligns with regulatory requirements for process validation in drug development, which demands a high degree of assurance that methods consistently produce reliable results [76].
The COMMUTE Model provides a structured framework for evaluating the performance of neuroimaging segmentation tools. Applied to FreeSurfer and Neurophet AQUA, it reveals a critical trade-off: while both tools are accurate, they differ significantly in processing speed and reliability across scanner platforms. Neurophet AQUA offers faster processing and superior consistency across magnetic field strengths, whereas FreeSurfer, while slower, provides high spatial overlap with expert ground truth. The choice of tool should be guided by the specific needs of the research or clinical trial—prioritizing efficiency and multi-site consistency versus maximal spatial accuracy. This decision-making process, supported by rigorous pre-validation as outlined in the COMMUTE model, is essential for generating robust, reliable quantitative data in drug development and neuroscientific research.
The quantitative assessment of medical image segmentation is fundamental to ensuring the reliability of tools used in clinical research and drug development. When evaluating segmentation performance, particularly on contrast-enhanced magnetic resonance (CE-MR) scans, researchers primarily rely on a suite of metrics, each quantifying different aspects of agreement between an automated result and a ground truth. The Dice Similarity Coefficient (DSC), Intraclass Correlation Coefficient (ICC), and Hausdorff Distance (HD) are among the most prevalent. However, a nuanced understanding of their strengths, weaknesses, and inherent biases is critical for their appropriate application. Framed within a broader thesis on the reliability of segmentation tools for CE-MR scans, this guide provides an objective comparison of these metrics, supported by experimental data, to inform their use in biomedical research.
Metric Definitions and Comparative Analysis
The following table outlines the core principles, interpretations, and primary applications of the three key metrics.
Table 1: Fundamental Characteristics of Segmentation Metrics
| Metric | Core Principle | Interpretation | Primary Application Context | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Dice Similarity Coefficient (DSC) | Measures the spatial overlap between two segmentations. Calculated as ( \frac{2 | X \cap Y | }{ | X | + | Y | } ) where X and Y are the segmentation voxels. | Ranges from 0 (no overlap) to 1 (perfect overlap). A value above 0.7 is often considered good agreement. | Evaluating overall volumetric segmentation accuracy; widely used for brain tumor, organ, and lesion segmentation [77] [78]. |
| Intraclass Correlation Coefficient (ICC) | Assesses the reliability and consistency of measurements. Quantifies how much of the total variance is attributable to between-subject differences. | Ranges from 0 (no reliability) to 1 (perfect reliability). Poor <0.4, Fair 0.4-0.59, Good 0.6-0.74, Excellent ≥0.75 [79]. | Measuring test-retest reliability of quantitative biomarkers (e.g., volume, thickness) derived from segmentations [79]. | ||||||
| Hausdorff Distance (HD) | Measures the largest distance between the boundaries of two segmentations. Defined as ( \max\left(\sup{x\in X}\inf{y\in Y}d(x,y), \sup{y\in Y}\inf{x\in X}d(x,y)\right) ). | A value of 0 indicates perfect boundary agreement. Larger values indicate larger local segmentation errors, measured in mm or voxels. | Quantifying the worst-case segmentation error, crucial for applications like tumor or vessel segmentation where boundary accuracy is critical [80] [81]. |
A deeper analysis reveals specific biases and practical limitations associated with each metric, which are summarized in the table below.
Table 2: Inherent Biases and Practical Limitations of Segmentation Metrics
| Metric | Inherent Biases | Practical Limitations & Implementation Pitfalls |
|---|---|---|
| Dice Similarity Coefficient (DSC) | Size Bias: Heavily penalizes errors in smaller structures more than identical errors in larger ones [82]. Sex Bias: As organ size often differs by sex, the same magnitude of error can result in a lower DSC for smaller structures, introducing a sex-based bias in model evaluation [82]. | Insensitive to the spatial location of errors; a segmentation can be disconnected or have inaccurate boundaries yet achieve a high DSC. |
| Intraclass Correlation Coefficient (ICC) | Model Dependency: The value can change significantly based on the statistical model used (e.g., ICC(1,k), ICC(2,k), ICC(3,k)) and the choice of random vs. fixed facets [79]. | Requires multiple measurements per subject, which can be resource-intensive. Low ICC can stem from either poor measurement reliability or true biological variability over time [79]. |
| Hausdorff Distance (HD) | Outlier Sensitivity: Being a max-distance measure, it is extremely sensitive to single outliers. A single stray voxel can drastically inflate the HD [80]. | Implementation Variability: Different open-source tools can compute HD with critical differences, leading to deviations exceeding 100 mm for the same segmentations, which undermines benchmarking efforts [83]. |
Alternatives to the standard formulations of these metrics have been proposed to mitigate their known issues. The Average Hausdorff Distance (AVD) was introduced to be less sensitive to outliers by considering the average of all boundary distances. However, a "balanced" version (bAVD) has been shown to further alleviate a ranking bias present in the original AHD. The formula is modified from ( \frac{GtoS}{G} + \frac{StoG}{S} ) to ( \frac{GtoS}{G} + \frac{StoG}{G} ), where ( GtoS ) is the directed distance from ground truth (G) to segmentation (S), and ( StoG ) is the reverse. This prevents the metric from being unfairly influenced by the size of the segmentation itself [80] [84].
Experimental Protocols and Data
Investigating the Relationship Between Image Quality and Segmentation Accuracy
Objective: To evaluate the correlation between MR image quality metrics (IQMs) and the performance of a deep learning-based brain tumor segmentation model [77].
Methodology:
- Data: Multimodal MRI scans (T1, T1Gd, T2, T2-FLAIR) from the BraTS 2020 training cohort (n=369) were used for model training and 5-fold cross-validation. An independent test set was curated from the BraTS 2021 cohort.
- Segmentation Model: A 3D DenseNet was trained for multiclass segmentation of enhancing tumor, peritumoral edema, and necrotic core. Performance was quantified using the DSC for the Whole Tumor (WT) region.
- Image Quality Assessment: All scans were processed with the MRQy tool to extract 13 IQMs per scan, including measures for inhomogeneity (CV, CJV, CVP) and noise (PSNR).
- Correlation Analysis: The Pearson correlation coefficient was computed between WT DSC values and the IQMs. Scans were then grouped into "better quality" (BQ) or "worse quality" (WQ) based on specific IQM thresholds. The model was trained and validated on different combinations of BQ and WQ sets to isolate the impact of specific quality attributes.
Key Findings: A significant correlation was found between specific IQMs and segmentation DSC. Models trained on BQ images defined by low inhomogeneity (CV, CJV, CVP) and models trained on WQ images defined by high PSNR (low noise) yielded significantly improved tumor segmentation accuracy on their respective validation sets [77].
Validating the Balanced Average Hausdorff Distance
Objective: To demonstrate the ranking bias in the standard Average Hausdorff Distance (AVD) and validate the superior performance of the balanced AVD (bAVD) [80].
Methodology:
- Data & Ground Truth: Time-of-flight MR angiography images from 10 patients with manually corrected cerebral vessel segmentations serving as ground truth.
- Error Simulation: A framework was developed to create 55 non-overlapping segmentation errors (e.g., oversegmentation, false positives). For each patient, 20 sets of 10 simulated segmentations were created by consecutively adding random errors.
- Ranking Experiment: Each set of simulated segmentations (with an increasing number of errors) was ranked using both AVD and bAVD.
- Statistical Analysis: The Kendall rank correlation coefficient was calculated between the metric-based ranking and the ground-truth ranking (based on the number of errors). The number of misranked segmentations for each metric was also counted.
Key Findings: The rankings produced by bAVD had a significantly higher median correlation with the true ranking (1.00) than those by AVD (0.89). Out of 200 total rankings, bAVD misranked 52 segmentations, while AVD misranked 179, proving bAVD is more suitable for quality assessment and ranking [80].
Relationships and Workflows in Metric Application
The following diagram illustrates the typical workflow for evaluating a segmentation tool, highlighting the roles of the different metrics and the key decision points based on the findings from the cited research.
Research Reagent Solutions
The following table details key computational tools and metrics essential for conducting rigorous segmentation reliability studies.
Table 3: Essential Reagents for Segmentation Reliability Research
| Research Reagent | Type | Primary Function | Relevance to CE-MR Research |
|---|---|---|---|
| MRQy [77] | Software Tool | Automated quality control for large-scale MR cohorts; extracts 13 image quality metrics (IQMs) per scan. | Quantifies technical heterogeneity in clinical CE-MR scans, enabling correlation of IQMs with segmentation performance. |
| 3D DenseNet [77] | Deep Learning Model | A convolutional neural network architecture for volumetric image segmentation, using dense connections between layers. | Used as a standard model for benchmarking brain tumor segmentation performance on datasets like BraTS. |
| Balanced Average Hausdorff Distance (bAVD) [80] | Evaluation Metric | A modified distance metric that reduces ranking bias by normalizing both directed distances by the size of the ground truth. | Provides a fairer assessment of segmentation boundary accuracy, especially for structures of varying sizes. |
| SynthSeg+ [1] | Segmentation Tool | A deep learning-based tool for brain MRI segmentation that is robust to sequence and contrast variations. | Demonstrates high reliability (ICCs >0.90) for volumetric measurements on both contrast-enhanced and non-contrast MR scans. |
| Intraclass Correlation Coefficient (ICC) [79] | Statistical Metric | Measures the test-retest reliability of quantitative measurements, crucial for longitudinal studies. | Assesses the stability of volume or shape biomarkers derived from segmentations of CE-MR scans over time. |
This guide provides an objective comparison of four neuroimaging segmentation tools—SynthSeg+, CAT12, FreeSurfer, and AQUA—focusing on their reliability for analyzing Contrast-Enhanced Magnetic Resonance (CE-MR) scans. With the increasing importance of utilizing clinically acquired images in research, understanding tool performance on CE-MR data is crucial for researchers, scientists, and drug development professionals. Based on current experimental evidence, deep learning-based tools like SynthSeg+ demonstrate superior reliability for CE-MR scans compared to traditional methods, potentially unlocking vast clinical datasets for retrospective research.
Clinical brain MRI scans, including contrast-enhanced images, represent an underutilized resource for neuroscience research due to technical heterogeneity. The presence of gadolinium-based contrast agents alters tissue contrast properties, creating significant challenges for automated segmentation tools designed for non-contrast images. This performance dive evaluates how modern segmentation approaches overcome these challenges, with particular emphasis on their application in reliable morphometric analysis for drug development and clinical research.
SynthSeg+
- Core Technology: Deep learning convolutional neural network trained with aggressive domain randomization [32] [33].
- Unique Capability: Contrast-agnostic segmentation that works out-of-the-box without retraining or fine-tuning [33].
- Key Features: Robust to any contrast, resolution (up to 10mm slice spacing), and works on both processed and unprocessed data [32]. Performs cortical parcellation, automated quality control, and intracranial volume estimation [32].
- CE-MR Performance: Specifically validated for contrast-enhanced scans with high reliability (ICCs > 0.90 for most structures) [2].
CAT12 (Computational Anatomy Toolbox)
- Core Technology: Extension of SPM12 using a unified segmentation approach with Tissue Probability Maps (TPMs) [85] [86].
- Key Features: Comprehensive voxel-based, surface-based, and region-based morphometric analyses [85]. Integrates Template-O-Matic for generating age-specific TPMs, particularly useful for pediatric populations [86].
- CE-MR Limitations: Demonstrates inconsistent performance on CE-MR scans, with segmentation failures reported in approximately 6% of cases [2].
FreeSurfer
- Core Technology: Automated pipeline for cortical surface reconstruction and volumetric segmentation [87] [88].
- Historical Context: Evolved from surface reconstruction for EEG/MEG inverse problems to comprehensive structural analysis [87].
- Key Features: Generates models of macroscopically visible brain structures, cortical thickness mapping, and hippocampal subfield segmentation [87].
- Strengths: Topology correction and spherical registration based on cortical folding patterns [87].
AQUA
- Core Technology: Two-dimensional U-Net architecture with Bottleneck Attention Modules for small lesion detection [89].
- Specialization: Automatic segmentation of white matter hyperintensities (WMHs) from T2-FLAIR scans [89].
- Key Features: Patch-based training optimized for small lesion detection, multicenter validation [89].
- Performance: Superior spatial (Dice = 0.72) and volumetric (logAVD = 0.10) agreement with manual segmentation compared to conventional methods [89].
Comparative Performance Data
Table 1: Volumetric Measurement Reliability on CE-MR vs. Non-Contrast MR Scenes [2]
| Brain Structure | SynthSeg+ ICC | CAT12 ICC | Notes |
|---|---|---|---|
| Cortical Gray Matter | >0.94 | Inconsistent | CAT12 showed higher CE-MR/NC-MR discrepancies |
| Cerebral White Matter | >0.94 | Inconsistent | Larger structures showed stronger agreement |
| Ventricular CSF | >0.90 | Inconsistent | Systematic differences in CSF volumes |
| Brain Stem | ~0.90 | Inconsistent | Lowest, albeit robust correlation for SynthSeg+ |
| Thalamus | >0.90 | Inconsistent | - |
| Overall Conclusion | High reliability | Variable reliability | CAT12 exhibited segmentation failures on CE-MR |
Table 2: Specialized Functionality Comparison
| Tool | Primary Use Case | Cortical Parcellation | WMH Segmentation | Contrast Agnostic |
|---|---|---|---|---|
| SynthSeg+ | Whole-brain segmentation on any contrast | Yes [32] | Via WMH-SynthSeg [32] | Yes [33] |
| CAT12 | Voxel-based morphometry | Yes [85] | Limited | No [2] |
| FreeSurfer | Cortical surface reconstruction | Yes [87] | Limited | No |
| AQUA | White matter hyperintensity segmentation | No | Yes (specialized) [89] | Not specified |
Table 3: Technical Specifications and Processing Requirements
| Tool | Platform | GPU/CPU Support | Processing Time | Input Flexibility |
|---|---|---|---|---|
| SynthSeg+ | Python/FreeSurfer [33] | Both (GPU: ~15s, CPU: ~1min) [33] | Fastest | Nifti, FreeSurfer formats; any contrast/resolution [32] |
| CAT12 | MATLAB [86] | CPU-based | Moderate | T1-weighted images preferred [85] |
| FreeSurfer | Standalone suite [88] | CPU-based | Long (hours) | T1-weighted images required |
| AQUA | Python/Deep Learning [89] | GPU-optimized | Fast | T2-FLAIR for WMH segmentation |
Experimental Protocols and Validation
- Sample: 59 normal participants (aged 21-73 years) with paired CE-MR and non-contrast MR scans
- Exclusion Criteria: Four subjects excluded due to CAT12 segmentation failure on CE-MR
- Analysis: Volumetric measurements compared using intraclass correlation coefficients (ICCs)
- Additional Validation: Age prediction models constructed to assess clinical utility of CE-MR volumes
- Dataset: MICCAI 2017 WMH Segmentation Challenge dataset (170 elderly participants)
- Comparison: Benchmarked against five established methods (LGA, LPA, SLS, UBO, BIANCA)
- Metrics: Dice score, logAVD, recall, and F1-score
- Special Analysis: Performance evaluation with and without small lesions (≤ 6 voxels)
- Context: Emerging application demonstrating SynthSeg's versatility
- Sample: 60 healthy controls scanned with Hyperfine Swoop (64 mT)
- Protocol: T1w and T2w 3D FSE sequences in axial, coronal, and sagittal directions
- Finding: Accurate brain volumes possible when combining orthogonal imaging directions
Workflow and Process Diagrams
The Scientist's Toolkit: Essential Research Materials
Table 4: Key Experimental Materials and Resources
| Resource | Function/Purpose | Application Context |
|---|---|---|
| CE-MR & NC-MR Paired Scans | Gold-standard reference for reliability testing | Validating tool performance on contrast-enhanced images [2] |
| MICCAI 2017 WMH Dataset | Benchmark for white matter hyperintensity segmentation | Evaluating AQUA performance against established methods [89] |
| Hyperfine Swoop Scanner | Ultra low-field MRI (64 mT) acquisition | Testing tool performance on accessible neuroimaging technology [90] |
| Template-O-Matic (TOM) | Generation of age-specific tissue probability maps | CAT12 pediatric analysis with customized templates [86] |
| ANTs (Advanced Normalization Tools) | Bias field correction and image registration | Preprocessing pipeline for ULF-MRI data [90] |
Key Findings and Recommendations
For CE-MR Scan Analysis
- SynthSeg+ is strongly recommended for studies utilizing contrast-enhanced clinical scans due to its demonstrated high reliability (ICCs > 0.90) and robustness to contrast variability [2].
- CAT12 shows inconsistent performance on CE-MR images with segmentation failures observed, limiting its utility for clinical datasets [2].
- FreeSurfer's comprehensive cortical analysis capabilities make it valuable for non-contrast research studies, particularly for cortical thickness measurement [86].
For Specialized Applications
- AQUA is the optimal choice for white matter hyperintensity segmentation, particularly for studies focusing on vascular dementia, multiple sclerosis, or cerebral small vessel disease [89].
- SynthSeg+ excels in challenging acquisition scenarios including ultra low-field MRI and heterogeneous clinical datasets [90].
- CAT12 remains valuable for voxel-based morphometry studies with standard non-contrast T1-weighted images, especially with its integrated quality control tools [85].
For Multi-Center and Large-Scale Studies
- SynthSeg+'s contrast-agnostic approach facilitates pooling of data across sites with different acquisition protocols, addressing a significant challenge in multi-center research [32] [33].
- Tools with automated quality control (SynthSeg+, CAT12) reduce manual inspection time in large-scale analyses [32] [85].
The reliability of brain segmentation tools on CE-MR scans varies significantly across platforms. Deep learning-based approaches like SynthSeg+ demonstrate superior performance for contrast-enhanced images, potentially enabling researchers to leverage extensive clinical datasets previously considered unsuitable for quantitative analysis. For drug development professionals, this expanded data pool could accelerate biomarker discovery and treatment monitoring. Traditional tools like CAT12 and FreeSurfer remain valuable for specific applications with standard non-contrast images, while specialized tools like AQUA address particular segmentation challenges like white matter hyperintensities. Tool selection should be guided by specific research questions, image types, and methodological requirements, with SynthSeg+ emerging as the most versatile option for heterogeneous clinical datasets.
The integration of artificial intelligence (AI) for automatic segmentation in clinical radiology and oncology workflows represents a significant advancement, promising enhanced efficiency and objectivity. This guide objectively compares the performance of various deep learning architectures and a novel foundation model for segmenting organs and tumors on Contrast-Enhanced Magnetic Resonance (CE-MR) scans. The reliability of these tools is paramount, as accurate segmentation of regions of interest (ROIs) is a critical step in numerous clinical applications, including radiotherapy planning, surgical guidance, and longitudinal treatment monitoring [69] [91]. Inaccurate contours can directly lead to suboptimal dosimetric calculations in radiation oncology, potentially affecting tumor control and normal tissue complication probabilities. This evaluation is framed within a broader thesis on the reliability of segmentation tools for CE-MR research, providing researchers and drug development professionals with a comparative analysis of current methodologies. We focus on quantitative performance metrics, computational efficiency, and qualitative expert evaluation to assess their clinical readiness.
Comparative Analysis of Segmentation Architectures
Deep Learning Models for Medical Image Segmentation
Deep learning (DL) techniques, particularly convolutional neural networks (CNNs), have become the state-of-the-art for automatic medical image segmentation [91]. These models automatically and successively extract relevant features at different resolutions and locations in images, enabling precise delineation of anatomical structures. The U-Net architecture, introduced by Ronneberger et al., was the first DL model to achieve widespread success in this field and continues to serve as a foundational benchmark [91]. Its encoder-decoder structure with skip connections helps retain important spatial features that might otherwise be lost during the training process [28]. Subsequent architectures have incorporated various modifications, including attention mechanisms, bottleneck convolutions, and residual connections, to further improve performance.
Performance Metrics for Segmentation Evaluation
The performance of segmentation models is quantitatively assessed using several well-established metrics that measure overlap, volume difference, and surface distance. The most common metrics include:
- Dice Similarity Coefficient (Dice): Measures the spatial overlap between the predicted segmentation and the ground truth mask. It ranges from 0 (no overlap) to 1 (perfect overlap) [28] [91].
- Intersection over Union (IoU): Calculates the area of overlap between the prediction and ground truth divided by the area of union.
- Precision and Recall: Evaluate the ratio of true positive predictions to all positive predictions (Precision) and to all actual positives (Recall) [28].
- Mean Surface Distance (MSD): The average distance between the surfaces of the predicted and ground truth segmentations [91].
- Hausdorff Distance (HD95): The 95th percentile of the maximum distance between the surfaces, which is less sensitive to outliers [91].
Table 1: Comparative Performance of Deep Learning Models on Breast DCE-MRI Segmentation
| Model Architecture | Dice Score | IoU | Precision | Recall | Inference Time (s) | Carbon Footprint (kgCO₂) |
|---|---|---|---|---|---|---|
| UNet++ | 0.914 (Highest) | - | - | - | - | - |
| UNet | 0.907 (Best Generalizability) | - | - | - | - | - |
| FCNResNet50 | 0.901 (Robust) | - | - | - | Reasonable | Lower |
| FCNResNet101 | - | - | - | - | - | - |
| DeepLabV3ResNet50 | 0.895 (Competitive) | - | - | - | - | - |
| DeepLabV3ResNet101 | - | - | - | - | - | - |
| DenseNet | - | - | - | - | - | - |
Note: The Dice scores and characteristics are based on a study comparing models for breast region segmentation in DCE-MRI [28].
Benchmarking on Prostate MRI Data
A separate study on T2-weighted MRI scans of the prostate provides a direct comparison of different segmentation strategies, including commercial clinical software. The study included 100 patients with ground truth segmentation masks established by expert radiologist consensus [91].
Table 2: Performance of Various Segmentation Techniques on Prostate MRI
| Segmentation Method | Dice Coefficient | Absolute Volume Difference (%) | Mean Surface Distance (pixels) | Hausdorff Distance (HD95) |
|---|---|---|---|---|
| EfficientDet (Adapted) | 0.914 | 5.9 | 1.93 | 3.77 |
| V-Net (3D U-Net) | 0.887 | - | - | - |
| Pre-trained 2D U-Net | 0.878 | - | - | - |
| GAN Extension | 0.871 | - | - | - |
| Syngo.Via (Siemens) | 0.855-0.887 | - | - | - |
| Multi-Atlas (Raystation) | 0.855-0.887 | - | - | - |
Note: The best performing method was the adapted EfficientDet, achieving a mean Dice coefficient of 0.914. The deep learning models were less prone to serious errors compared to the atlas-based and commercial software methods [91].
Experimental Protocols and Workflows
Data Acquisition and Preprocessing
The reliability of any segmentation model is contingent upon high-quality input data. The following protocols are essential for robust model training and evaluation:
- Image Acquisition: For breast DCE-MRI, scans are typically acquired using a 1.5 Tesla or 3 Tesla MRI scanner with a dedicated breast coil. Imaging parameters often include T1-weighted fast spoiled gradient echo (FSPGR) sequences with high spatial resolution (e.g., 0.97 x 0.97 mm²) [28].
- Data Preprocessing: Standard preprocessing steps involve converting DICOM images to NIFTI format, applying bias field correction (e.g., N4 algorithm), and resampling slices to ensure consistent volume across all patients [28] [91]. Intensity normalization through clipping to the 0th and 98th percentile interval followed by standardization to a fixed range is crucial for quantitative MRI analysis [91].
- Ground Truth Definition: Expert-defined segmentations are established by consensus from experienced radiologists (typically with more than five years of experience) to serve as the reference standard [91]. For breast region segmentation, novel boundary definitions may be employed that capture the anatomical structure while excluding noisy background pixels [28].
Model Training and Validation
To ensure robust model validation, a 10-fold cross-validation approach is often employed. This involves partitioning the dataset into ten subsets, training the model on nine subsets, and validating on the remaining one, rotating this process so that all subsets are used for validation [28]. This method provides a more reliable estimate of model performance and generalizability compared to a single train-test split. Models are typically trained using Dice loss as the optimization objective and evaluated on multiple metrics including Dice, IoU, Precision, and Recall [28].
Evaluation of a Novel Foundation Model: SAM2 for Breast MRI
Recent research has investigated the use of general-purpose foundation models for medical image segmentation, offering a zero-shot alternative to trained DL models. One study explored the Segment Anything Model 2 (SAM2) for 3D breast tumor segmentation in MRI, using only a single bounding box annotation on one slice [92].
Propagation Strategies: The study evaluated three slice-wise tracking strategies for propagating the initial segmentation across the 3D volume:
- Bottom-to-Top: Starting from the bottom-most tumor slice and propagating upward.
- Top-to-Bottom: Starting from the top-most tumor slice and propagating downward.
- Center-Outward: Starting from the central tumor slice (typically the largest and clearest) and propagating both upward and downward.
Performance: The center-outward propagation strategy yielded the most consistent and accurate segmentations, outperforming the other two approaches. This suggests that initializing from the most reliable slice reduces tracking errors over long ranges [92]. Despite being a zero-shot model not trained on volumetric medical data, SAM2 achieved strong segmentation performance with minimal supervision, offering a promising accessible alternative for resource-constrained settings.
The following workflow diagram illustrates the comparative evaluation process for segmentation models:
Comparative Evaluation Workflow
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Essential Materials and Software for Segmentation Research
| Item Name | Type | Function/Benefit |
|---|---|---|
| 3D Slicer | Software Platform | Open-source platform for medical image visualization and segmentation; allows for simultaneous display of multiple sequences [69]. |
| ITK-Snap | Software Platform | Interactive software application for segmentating structures in 3D medical images [69]. |
| N4ITK Bias Field Correction | Algorithm | Corrects low-frequency intensity non-uniformity (bias field) in MRI data, improving segmentation accuracy [91]. |
| NIFTI File Format | Data Standard | Neuroimaging Informatics Technology Initiative format; preferred over DICOM for processing as it simplifies data handling [28]. |
| DICOM SEG Object | Data Standard | Standardized format for storing and exchanging segmentation data, ensuring interoperability between systems [69]. |
| Duke Breast Cancer Dataset | Dataset | Large-scale collection of pre-operative 3D breast MRI scans with tumor annotations; used for benchmarking [92]. |
| MAMA-MIA Dataset | Dataset | Expanded version of the Duke dataset with expert-verified voxel-level tumor segmentations [92]. |
| BraTS Dataset | Dataset | Multimodal Brain Tumor Segmentation challenge dataset; widely used benchmark for brain tumor segmentation algorithms [93]. |
Visualization of Segmentation Propagation Strategy
The following diagram illustrates the top-performing propagation strategy for the SAM2 model as identified in the research, which can be a cost-effective alternative to fully supervised deep learning models:
SAM2 Center-Outward Propagation
Discussion and Clinical Readiness Assessment
Qualitative Expert Evaluation
Beyond quantitative metrics, qualitative expert evaluation is crucial for assessing clinical readiness. Radiologists and clinicians provide invaluable feedback on segmentation results, identifying failure modes that may not be captured by metrics alone. For instance, segmentations must accurately reflect anatomical boundaries to be clinically useful for surgical planning or radiation targeting. Studies have shown that implementing clear segmentation protocols with visual atlases and structured training can significantly improve delineation accuracy and consistency across observers [69]. Furthermore, a quality control framework should be employed to track both segmentation performance (e.g., Dice coefficient) and clinical workflow performance (e.g., radiologist adjustment time) when using AI-assisted tools [69].
Dosimetric Impact Considerations
The ultimate test of a segmentation tool's clinical readiness in oncology is its dosimetric impact—how segmentation accuracy influences radiation treatment planning. While the search results do not provide direct dosimetric studies, the high Dice scores (≥0.90) achieved by top-performing models on both breast and prostate MRI [28] [91] suggest potential for clinically acceptable segmentations. The deep learning models' consistency and lower propensity for serious errors [91] are particularly important for dosimetric calculations, where large outliers could lead to significant under-dosing of tumors or over-exposure of organs at risk. Future work should directly evaluate the dosimetric consequences of using these automated segmentation tools compared to manual delineation.
Computational and Environmental Considerations
The carbon footprint of AI models is an emerging concern in medical AI research. One study calculated the carbon footprint for model training using the formula: CFP = (0.475 × Training Time in seconds) / 3600, resulting in kilograms of CO₂ [28]. Models like FCNResNet50, which offer robust performance with lower carbon footprint and reasonable inference time, present a more environmentally sustainable option for widespread clinical deployment [28].
This comparison guide has objectively evaluated the performance of various segmentation tools for CE-MR scans within the context of clinical readiness. Traditional deep learning architectures like U-Net++ and adapted EfficientDet demonstrate high performance (Dice ≥0.91) on specific tasks such as breast and prostate segmentation, outperforming commercial clinical software in research settings [28] [91]. Meanwhile, emerging zero-shot foundation models like SAM2 show promising results for 3D tumor segmentation with minimal supervision, offering an accessible alternative for resource-constrained environments [92]. The clinical readiness of these tools depends not only on their quantitative performance but also on their integration into standardized clinical protocols, their acceptance by expert radiologists, and ultimately, their dosimetric reliability in patient care. Future research should focus on multi-institutional validation, real-time clinical workflow integration, and direct assessment of dosimetric impact to further advance the field of AI-assisted segmentation in medical imaging.
Conclusion
The reliability of brain volumetric measurements from CE-MR scans is no longer a prohibitive barrier, thanks largely to advanced deep learning segmentation tools. Studies consistently show that tools like SynthSeg+ can achieve high reliability (ICCs > 0.90) compared to non-contrast scans, enabling the vast repository of clinical CE-MR data to be leveraged for robust research. However, the choice of software and scanning parameters remains critical, as evidenced by significant scanner-software interaction effects. For future studies, adherence to consistent scanner-software protocols is paramount for longitudinal reliability. The promising performance of modern AI-based tools paves the way for their expanded use in clinical trials and drug development, particularly for tracking disease progression and therapeutic efficacy in oncology and neurodegenerative diseases. Future efforts should focus on standardizing evaluation benchmarks, improving model generalizability across diverse patient populations and scanner types, and further validating these tools in large-scale, multi-center prospective studies to fully integrate them into the biomedical research pipeline.
References
- 1. Comparative analysis of brain volumetric measurements ... [https://pubmed.ncbi.nlm.nih.gov/39788481]
- 2. Comparative analysis of brain volumetric measurements ... [https://www.sciencedirect.com/science/article/abs/pii/S0304394025000060]
- 3. Enabling new insights from old scans by repurposing ... [https://www.nature.com/articles/s41467-025-58274-8]
- 4. Enhanced brain tumor segmentation in medical imaging ... [https://www.nature.com/articles/s41598-025-21255-4]
- 5. Benchmarking of Deep Learning Methods for Generic MRI ... [https://arxiv.org/html/2507.17971v1]
- 6. MRI-based quantification of intratumoral heterogeneity for ... [https://insightsimaging.springeropen.com/articles/10.1186/s13244-025-01985-9]
- 7. Application of DCE-MRI radiomics and heterogeneity ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1523507/full]
- 8. Scan-rescan reliability assessment of brain volumetric ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12354914/]
- 9. Advancing 1.5T MR imaging: toward achieving 3T quality ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12213716/]
- 10. Fighting the scanner effect in brain MRI segmentation with ... [https://www.sciencedirect.com/science/article/pii/S136184152400015X]
- 11. ISMRM24 - Pitch: Software Tools [https://www.ismrm.org/24/pf/PP-26.htm]
- 12. 3T vs 1.5T MRI: How Do They Compare? [https://ezra.com/blog/3t-mri]
- 13. 1.5 Tesla Magnetic Resonance Imaging Scanners Compared ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3442613/]
- 14. 1.5T vs 3T MRI Comparison Guide [https://www.blockimaging.com/blog/bid/87030/3t-mri-vs-1-5t-mri]
- 15. Evaluating brain volume segmentation accuracy and ... [https://www.nature.com/articles/s41598-024-74622-y]
- 16. AI improves consistency in regional brain volumes ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2025.1588487/full]
- 17. MRI with ultrahigh field strength and high-performance gradients [https://pmc.ncbi.nlm.nih.gov/articles/PMC8387544/]
- 18. 2025 Margulis Award | RSNA [https://www.rsna.org/news/2025/november/2025-margulis-award]
- 19. Automated segmentation of the individual branches of the carotid... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-021-00568-6]
- 20. Auto-segmentation, radiomic reproducibility, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12034606/]
- 21. Within-participants reliability and measurement error of ... [https://www.sciencedirect.com/science/article/pii/S1078817424001056]
- 22. Image Segmentation: Deep Learning vs Traditional [Guide] [https://www.v7labs.com/blog/image-segmentation-guide]
- 23. A review of deep learning for brain tumor analysis in MRI [https://www.nature.com/articles/s41698-024-00789-2]
- 24. Reliability Analysis of Deep Learning Algorithms for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7735462/]
- 25. Comparison of deep learning-based segmentation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12590434/]
- 26. Evaluating Traditional, Deep Learning and Subfield Methods ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11947432/]
- 27. Deep learning-based automatic segmentation of brain ... [https://www.sciencedirect.com/science/article/pii/S200103702500128X]
- 28. Comparative analysis of deep learning architectures for ... [https://www.nature.com/articles/s41598-025-92863-3]
- 29. SynthSeg: Segmentation of brain MRI scans of any contrast ... [https://www.sciencedirect.com/science/article/pii/S1361841523000506]
- 30. SynthSeg: Segmentation of brain MRI scans of any contrast ... [https://arxiv.org/abs/2107.09559]
- 31. Robust Segmentation of Brain MRI in the Wild with ... [https://conferences.miccai.org/2022/papers/429-Paper2294.html]
- 32. SynthSeg - Free Surfer Wiki [https://surfer.nmr.mgh.harvard.edu/fswiki/SynthSeg]
- 33. BBillot/SynthSeg: Contrast-agnostic segmentation of MRI ... [https://github.com/BBillot/SynthSeg]
- 34. Learning Strategies for Contrast-agnostic Segmentation via ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10037234/]
- 35. Deep learning-based brain segmentation model ... [https://arxiv.org/html/2406.17423v1]
- 36. A lifespan-generalizable skull-stripping model for magnetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12360181/]
- 37. A comprehensive processing framework crafted for ... [https://www.spiedigitallibrary.org/conference-proceedings-of-spie/13407/1340723/A-comprehensive-processing-framework-crafted-for-pediatric-brain-MRI/10.1117/12.3047146.full]
- 38. A general skull stripping of multiparametric brain MRIs ... [https://www.nature.com/articles/s41598-022-14983-4]
- 39. Skull-stripping induces shortcut learning in MRI-based ... [https://arxiv.org/html/2501.15831v3]
- 40. Development and validation of a deep learning model ... [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1657604/full]
- 41. Image normalization techniques and their effect on the ... [https://www.sciencedirect.com/science/article/pii/S0720048X2500172X]
- 42. Scan-rescan reliability assessment of brain volumetric ... [https://www.nature.com/articles/s41598-025-15283-3]
- 43. Automated segmentation of brain metastases in magnetic ... [https://www.nature.com/articles/s41598-025-15630-4]
- 44. Development and external validation of an MRI-based ... [https://www.sciencedirect.com/science/article/pii/S0167814022045625]
- 45. Artificial intelligence in the task of segmentation and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500441/]
- 46. Development and validation of a deep learning model using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12500715/]
- 47. MEASegNet: 3D U-Net with Multiple Efficient Attention for ... [https://www.mdpi.com/2076-3417/15/7/3791]
- 48. Development and validation of the 3D U-Net algorithm for ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-021-00703-3]
- 49. Brain Tumor Segmentation in MRI Images with 3D U-Net ... [https://arxiv.org/html/2407.08470v1]
- 50. Effect of Scanner in Longitudinal Diffusion Tensor Imaging ... [https://pubmed.ncbi.nlm.nih.gov/21391276/]
- 51. Frontiers | Recommendations for the Use of Automated Gray Matter... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2017.00519/full]
- 52. A Review of Publicly Available Automatic Brain Segmentation ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8558983/]
- 53. Test-retest reliability and longitudinal analysis of ... [https://pubmed.ncbi.nlm.nih.gov/29341323/]
- 54. A method for harmonizing longitudinal multi-scanner ... [https://www.sciencedirect.com/science/article/pii/S1053811920306157]
- 55. Top 7 Image Segmentation Tools for 2025 [https://dagshub.com/blog/top-image-segmentation-tools/]
- 56. Automatic segmentation and quantitative analysis of brain ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12058743/]
- 57. Comparison of lesion segmentation performance in diffusion ... [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0324021]
- 58. A Review of Advancements and Challenges in Liver ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11355703/]
- 59. Quality control strategies for brain MRI segmentation and ... [https://www.sciencedirect.com/science/article/pii/S1053811921004511]
- 60. A novel framework for MR image segmentation and ... [https://www.sciencedirect.com/science/article/abs/pii/S0169260718317565]
- 61. Medical image data augmentation: techniques, ... [https://link.springer.com/article/10.1007/s10462-023-10453-z]
- 62. A systematic review of deep learning data augmentation in ... [https://www.sciencedirect.com/science/article/pii/S277244252400042X]
- 63. The impact of data augmentation and transfer learning on the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11308385/]
- 64. Integration of automatic MRI segmentation techniques with ... [https://www.sciencedirect.com/science/article/pii/S1053811925002678]
- 65. Quantitative Imaging Network (QIN) [https://dctd.cancer.gov/research/networks/qin]
- 66. Data augmentation with automated machine learning [https://arxiv.org/html/2403.08352v2]
- 67. Using transfer learning for automated microbleed ... [https://www.frontiersin.org/journals/neuroimaging/articles/10.3389/fnimg.2022.940849/full]
- 68. A comprehensive multifaceted technical evaluation framework ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12313850/]
- 69. ESR Essentials: a step-by-step guide of segmentation for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12559127/]
- 70. Comparison of automated segmentation techniques for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9921124/]
- 71. Deep learning-based automated segmentation for the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12150800/]
- 72. Automated multi-class MRI brain tumor classification and ... [https://www.nature.com/articles/s41598-025-92776-1]
- 73. Evaluating brain volume segmentation accuracy and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11489576/]
- 74. Benchmarking Multi-Organ Segmentation Tools for ... [https://arxiv.org/html/2504.07729]
- 75. Phase-Appropriate Drug Development – Validation Process [https://www.pharm-int.com/resources/phase-appropriate-drug-development-validation-process/]
- 76. Types of Validation in the Pharmaceutical Industry [https://www.valgenesis.com/blog/types-of-validation-processes-in-the-pharmaceutical-industry]
- 77. Evaluating the relationship between magnetic resonance ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11233231/]
- 78. A comparison of lesion mapping analyses based on CT ... [https://www.sciencedirect.com/science/article/pii/S0028393223000982]
- 79. A guide to the measurement and interpretation of fMRI test- ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7875178/]
- 80. On the usage of average Hausdorff distance for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7817746/]
- 81. Reducing the Hausdorff Distance in Medical Image ... [https://pubmed.ncbi.nlm.nih.gov/31329113/]
- 82. Sex-based Bias Inherent in the Dice Similarity Coefficient [https://arxiv.org/abs/2509.19778]
- 83. Understanding implementation pitfalls of distance-based ... [https://arxiv.org/abs/2410.02630]
- 84. On The Usage Of Average Hausdorff Distance For ... [https://arxiv.org/abs/2009.00215]
- 85. Manual Computational Anatomy Toolbox CAT12 [https://neuro-jena.github.io/cat12-help/]
- 86. Cortical thickness in brain imaging studies using ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12172744/]
- 87. FreeSurfer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3685476/]
- 88. FreeSurfer [https://surfer.nmr.mgh.harvard.edu/]
- 89. Automatic segmentation of white matter hyperintensities in ... [https://pubmed.ncbi.nlm.nih.gov/38000477/]
- 90. Morphological Brain Analysis Using Ultra Low‐Field MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC12207323/]
- 91. Comparison of automated segmentation techniques for ... [https://bmcmedimaging.biomedcentral.com/articles/10.1186/s12880-023-00974-y]
- 92. Towards Affordable Tumor Segmentation and Visualization ... [https://arxiv.org/html/2507.23272v1]
- 93. AI in MRI brain tumor diagnosis: A systematic review of ... [https://www.sciencedirect.com/science/article/pii/S0169743925000991]