11.7T Ultra-High Field MRI: A New Frontier in Neuroscience Research and Drug Development
The advent of 11.7 Tesla (T) Magnetic Resonance Imaging (MRI) marks a transformative leap for neuroscience, offering unprecedented spatial resolution and signal-to-noise ratio to probe the human brain at a...
11.7T Ultra-High Field MRI: A New Frontier in Neuroscience Research and Drug Development
Abstract
The advent of 11.7 Tesla (T) Magnetic Resonance Imaging (MRI) marks a transformative leap for neuroscience, offering unprecedented spatial resolution and signal-to-noise ratio to probe the human brain at a mesoscopic scale. This article explores the foundational technology behind scanners like the Iseult system, detailing its capability to acquire high-resolution images in vivo within minutes—a task requiring hours on conventional clinical systems. We examine its methodological applications in disease modeling, from detecting microstructural changes in glioblastoma to characterizing biomarkers in Alzheimer's disease models. The discussion also addresses the significant technical challenges of operating at such high fields, including radiofrequency field inhomogeneity and safety protocols, and reviews validation studies that correlate 11.7T findings with gold-standard histological methods. Finally, we consider the future implications of this technology for identifying novel disease biomarkers and advancing therapeutic development, providing a comprehensive resource for researchers and drug development professionals navigating this cutting-edge landscape.
The 11.7T Revolution: Unveiling the Brain's Mesoscopic Architecture
Ultra-high-field (UHF) Magnetic Resonance Imaging (MRI), defined as systems operating at 7 Tesla (7T) and above, represents a paradigm shift in non-invasive neuroimaging. By boosting the static magnetic field (B0), UHF MRI provides a supra-linear gain in signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR), enabling researchers to investigate the human brain at a mesoscopic scale—the level of cortical layers and columnar organizations [1]. This scale is critical for bridging the gap between microscopic knowledge from animal models and the macroscopic human brain connectome [2]. The development of the Iseult 11.7 T MRI scanner by the French Alternative Energies and Atomic Energy Commission (CEA) marks the forefront of this endeavor, being the most powerful MRI scanner for human imaging in the world [3]. This whitepaper provides an in-depth technical guide to the Iseult system, detailing its specifications, the experimental methodologies it enables, and its profound implications for neuroscience research and drug development.
The Iseult 11.7T Scanner: System Architecture and Technical Specifications
The Iseult project is the culmination of nearly 20 years of research and development, officially launched in the early 2000s as part of a French-German initiative to create a "human brain explorer" [4] [3].
Magnet and Cryogenic Design
The core of the Iseult MRI is an actively shielded NbTi magnet cooled by a superfluid helium bath at 1.8 K, a temperature lower than the 4.2 K used in standard MRI magnets [4] [2]. This design choice ensures cryostable operation and provides a large safety buffer. The magnet generates a homogeneous magnetic field of 11.7 T within a 90 cm warm bore, which is essential for whole-body human imaging [4].
- Active Shielding: Unlike passive shielding, which would require hundreds of tons of iron, the active shield uses additional superconducting coils to contain the magnetic field, thereby reducing the system's footprint and infrastructure demands [4].
- Superconducting Coil: The main coil consists of a stack of 170 double pancakes, utilizing 182 km of superconducting wire. The magnet itself is a massive 132-ton cylinder, 5 meters in length and 5 meters in diameter [2] [5].
- Field Homogeneity and Stability: The magnet achieves a remarkable homogeneity of 0.9 ppm peak-to-peak over a 22-cm-diameter sphere, with a temporal drift of only 3 ppb per hour at thermal equilibrium, which is critical for high-resolution imaging [2].
- Operation in Driven Mode: Due to the complexity of creating superconducting joints for its multi-strand wire, the Iseult magnet operates in driven mode, meaning it is permanently connected to its power supply. This is managed by a sophisticated Magnet Safety System (MSS) with voting redundancy to ensure high reliability [4].
Technical Specifications in Context
The table below summarizes the key technical specifications of the Iseult 11.7 T scanner and compares it with more common clinical and research MRI systems.
Table 1: Technical Specifications of the Iseult 11.7 T Scanner vs. Other MRI Systems
| Parameter | Iseult 11.7 T | Standard 3T (Clinical/Research) | Standard 7T (Research) | Source |
|---|---|---|---|---|
| Magnetic Field Strength (B0) | 11.7 T | 3 T | 7 T | [2] [5] |
| Magnet Weight | 132 tons | ~5-10 tons | ~20-40 tons | [2] [5] |
| Operating Temperature | 1.8 K | 4.2 K | 4.2 K | [4] [2] |
| Bore Diameter | 90 cm | ~60-70 cm | ~60-90 cm | [4] |
| Liquid Helium Capacity | 7,000 - 7,500 L | ~1,000-2,000 L | ~2,000-4,000 L | [2] [5] |
| Field Homogeneity (over 22 cm DSV) | 0.9 ppm peak-to-peak | Typically ~1-2 ppm | Typically <1 ppm | [2] |
| Typical In-Plane Resolution (Anatomical) | 0.19 x 0.19 mm² | ~1 x 1 mm² | ~0.5 x 0.5 mm² | [2] [6] |
The UHF Advantage: Gains in SNR, Resolution, and Contrast
The primary motivation for moving to ultra-high magnetic fields is the profound improvement in fundamental image quality metrics.
Signal-to-Noise and Contrast-to-Noise Ratios
The signal-to-noise ratio (SNR) increases supralinearly with the magnetic field strength ((SNR \sim B_0^{1.65})) [1]. This translates directly into the ability to acquire images with higher spatial resolution in a practical scan time. For example, the Iseult scanner can achieve a 0.19 x 0.19 x 1 mm³ resolution in just 4-5 minutes, a feat that would require hours on a clinical 3T scanner, making it infeasible for human subjects [3] [6]. This resolution represents a volume equivalent to a few thousand neurons, bringing the mesoscopic scale within reach [3].
Furthermore, for functional MRI (fMRI), the functional contrast-to-noise ratio (fCNR) sees multiplicative gains. The blood-oxygen-level-dependent (BOLD) effect, the primary contrast mechanism for fMRI, is itself dependent on field strength. The combination of increased image SNR and enhanced BOLD sensitivity leads to a dramatic ~10-fold gain in fCNR at 10.5T compared to 3T, with even greater gains expected at 11.7T [1].
Enhanced Magnetic Resonance Spectroscopy (MRS) and Chemical Detection
UHF MRI significantly improves the spectral dispersion in MRS, resolving metabolite peaks that are overlapped at lower fields. The Iseult scanner's high SNR will facilitate the detection of chemical species with weak signals [3] [5], including:
- Lithium: Used to treat bipolar disorders; allowing for precise assessment of its distribution in the brain to better understand its efficacy.
- Glucose and Glutamate: Molecules active in brain metabolism; contributing to the characterization of gliomas and neurodegenerative diseases [3] [5].
Methodological Challenges and Solutions at 11.7 T
Operating at 11.7 T presents unique physical challenges that require innovative hardware and software solutions.
Radiofrequency Field Inhomogeneity and Parallel Transmission
A major challenge at UHF is the shortening wavelength of the radiofrequency (RF) field (B1+). At 500 MHz (the resonant frequency for hydrogen at 11.7 T), this wavelength is comparable to the size of the human head, leading to severe constructive and destructive interference patterns. This results in inhomogeneous signal across the image, manifesting as bright and dark spots [2].
Solution: Parallel Transmission (pTx) The Iseult team deployed a custom-built 16-channel parallel transmission RF coil and sophisticated pTx pulse design algorithms [2].
- Methodology: Instead of using a single, uniform RF pulse, pTx uses multiple independent RF transmitters to apply tailored pulses simultaneously. These pulses are designed using algorithms like kT-points and GRAPE (Gradient Ascent Pulse Engineering) to achieve a uniform excitation or refocusing across the entire brain [2].
- Outcome: This approach mitigated the RF inhomogeneity problem, achieving a normalized root mean square error (n.r.m.s.e.) of ~8% for small flip-angle excitations and ~13% for refocusing pulses over the whole brain, effectively eliminating severe artifacts in vivo [2].
Specific Absorption Rate (SAR) Management
The energy deposited in tissue (SAR) increases with the square of the field strength, raising safety concerns related to localized heating [2] [7].
Solution: Virtual Observation Points (VOPs)
- Methodology: VOPs are a compression scheme used to accurately and efficiently monitor global and local SAR in real-time during pTx experiments, even with complex RF pulses [2] [8]. This ensures that the scanner operates within strict regulatory safety limits.
Gradient-Magnet Interactions
The powerful switching gradients inside the strong 11.7 T magnetic field can induce vibrations, acoustic noise, and unwanted perturbations to the main magnetic field (B0) [4].
Solution: Comprehensive Testing and Monitoring
- Methodology: Extensive commissioning tests were conducted to measure vibrations, acoustics, and field fluctuations during gradient activity. The Magnet Safety System was calibrated to define safe operating limits for the gradient coil to protect the magnet and ensure image quality [4].
Experimental Protocols for In-Vivo Human Brain Imaging
The first in-vivo human brain images at 11.7 T were acquired in 2023-2024 after regulatory and ethical approval [2]. The following workflow and protocol details the methodology used.
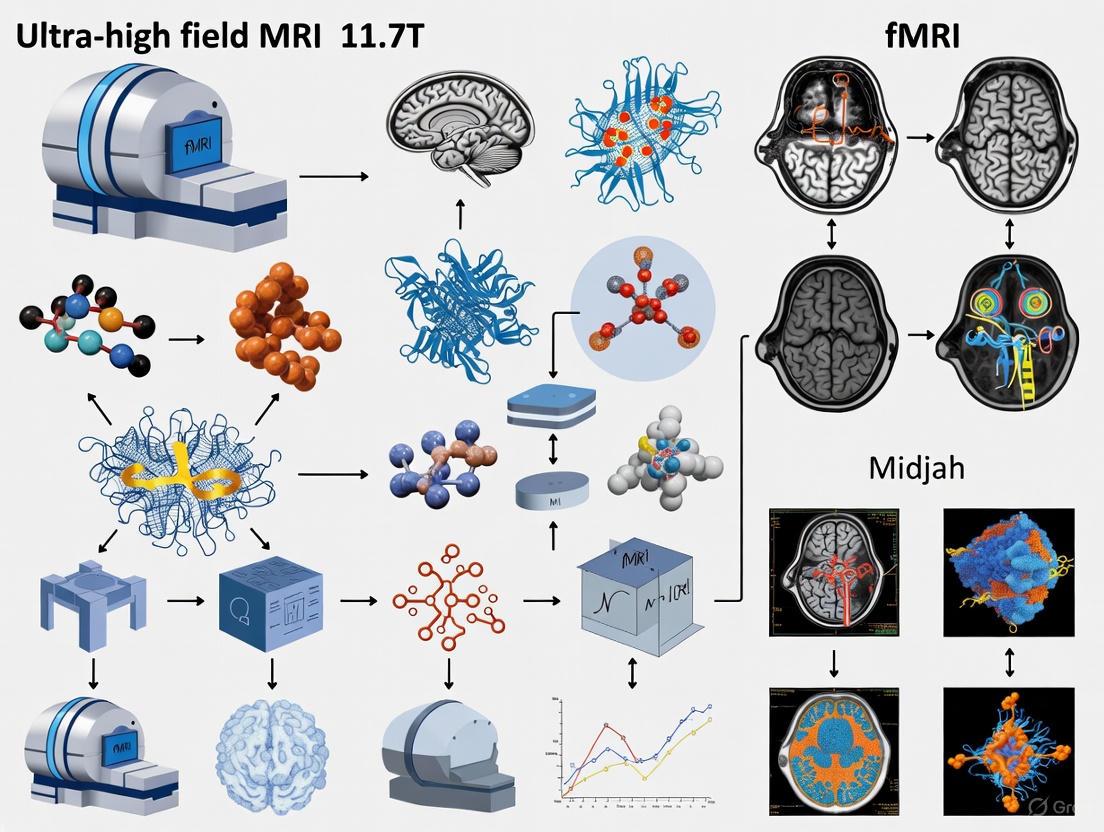
Diagram 1: Experimental Workflow for 11.7T Imaging
Key Steps in the Imaging Protocol
- B0 Static Shimming: For each participant, the static magnetic field was shimmed up to second order using a brain mask and a quadratic programming approach. This achieved an average field uniformity of 82.7 Hz standard deviation (0.17 ppm) over the brain [2].
- RF Pulse Design and pTx Calibration: Following B1+ field mapping for each participant, tailored RF pulses were designed using the kT-points (for excitations) and GRAPE (for refocusing pulses) algorithms. These were optimized under hardware constraints (peak and average power) and SAR limits [2].
- Image Acquisition: With the pTx pulses, T2-weighted and T2-weighted acquisitions were performed. Example parameters for a high-resolution scan included [2] [6]:
- Sequence: 2D T2-weighted Gradient Echo (GRE) or 3D T2-weighted Turbo Spin Echo.
- Resolution: (0.19 \times 0.19 \times 1 \, \text{mm}^3).
- Acquisition Time: ~4-5 minutes.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Key Materials and Technologies for 11.7T Experiments
| Item / Solution | Function / Role | Specification in Iseult Experiments |
|---|---|---|
| Parallel Transmission (pTx) Coil | Enables mitigation of B1+ inhomogeneity via multi-channel, tailored RF pulses. | Custom 16-transmit-channel head coil [2]. |
| High-Density Receive Array Coil | Maximizes signal reception and enables parallel imaging acceleration. | Although not specified for Iseult, 64- to 128-channel arrays are used at UHF to capture uiSNR [1]. |
| pTx Pulse Design Algorithms | Computes the shape and timing of RF pulses for each channel to achieve uniform flip angles. | kT-points (for excitation) and GRAPE (for refocusing) [2]. |
| SAR Management System | Ensures patient safety by monitoring and limiting radiofrequency energy deposition. | Virtual Observation Points (VOPs) for real-time monitoring [2] [8]. |
| High-Performance Gradients | Provides strong, fast-switching magnetic field gradients for spatial encoding. | Required for high-resolution readouts; interaction with 11.7 T field was extensively tested [4] [9]. |
| Cryogenic Plant | Maintains the magnet's superconducting state by providing continuous cooling. | Dedicated plant cooling 7,000 L of helium to 1.8 K [4] [2]. |
Safety and Physiological Considerations for Human Subjects
Before the Iseult project, the effects of prolonged exposure to an 11.7 T magnetic field on humans were unknown. A comprehensive safety study was conducted on 20 healthy volunteers scanned for 90 minutes, compared to a control group of 20 in a 0 T environment [2] [6].
Physiological, Vestibular, and Cognitive Metrics Monitored:
- Vital Signs: Blood pressure and heart rate.
- Vestibular Function: Balance tests to check for dizziness or vertigo.
- Cognitive Performance: Standardized cognitive tests.
- Genotoxicity: Blood samples drawn before and after exposure to assess chromosomal damage.
Result: Statistical analysis revealed no significant differences between the 11.7 T and 0 T groups across all tested metrics, providing initial evidence for the safety and tolerability of human imaging at this field strength for limited durations [2] [6].
Future Perspectives and Applications in Neuroscience and Drug Development
The Iseult 11.7 T scanner opens new frontiers for neuroscience research and the development of biomarkers for neurological and psychiatric diseases.
Targeted Research and Clinical Applications
The high resolution and unique contrasts will be leveraged to study [2] [6] [5]:
- Neurodegenerative Diseases: Alzheimer's and Parkinson's diseases, with a focus on iron content in basal ganglia and hippocampal integrity.
- Drug-Resistant Epilepsy: Identification of subtle malformations like focal cortical dysplasia and mesial temporal sclerosis that are missed at lower fields.
- Psychiatric Disorders: Schizophrenia and bipolar disorders, potentially by tracking drug distribution (e.g., lithium) and metabolic changes.
- Brain Tumors and Cerebrovascular Diseases: Assessing microvessels, angiogenesis, and small metastases with unprecedented detail.
Ongoing and Future Technological Developments
To fully unleash the potential of the 11.7 T platform, several technological advancements are underway [2]:
- Motion Correction Tools: To mitigate artifacts in high-resolution scans.
- Highly Accelerated Sequences: Using advanced reconstruction algorithms to reduce scan times further.
- More Efficient RF Coils and Higher Channel-Count Arrays: To better capture the intrinsic SNR gains.
- Advanced Contrast Mechanisms: Such as Chemical Exchange Saturation Transfer (CEST) imaging, which benefits greatly from UHF and can probe metabolites and pH [8].
The Iseult 11.7 T MRI scanner is a landmark achievement in engineering and physics, which has now successfully transitioned to a tool for in-vivo human brain imaging. By overcoming significant technical challenges such as B1+ inhomogeneity and SAR management through parallel transmission, it provides unmatched spatial resolution and SNR in practical scan times. The initial safety data is reassuring, and the future applications in mesoscopic-scale neuroscience and the study of neurological and psychiatric disorders are vast. This technology promises to bridge critical gaps in our understanding of brain organization and function, ultimately accelerating the development of new diagnostics and therapeutics.
Technical Specifications and Engineering Breakthroughs of the 11.7T Magnet
The development of the Iseult 11.7 Tesla (T) whole-body MRI magnet represents a monumental achievement in biomedical engineering, marking a new frontier in ultra-high field (UHF) human neuroimaging. This endeavor, initiated in the early 2000s as part of the French-German Iseult/Inumac project, was driven by the vision to create a "human brain explorer" capable of investigating the brain at an unprecedented mesoscopic scale [10] [2]. After nearly two decades of research, development, and commissioning, this 132-ton instrument has successfully demonstrated its capability for in vivo human brain imaging, providing an unparalleled combination of spatial resolution and signal-to-noise ratio (SNR) that promises to transform neuroscience research and the study of neurological disorders [2] [6]. This whitepaper details the technical specifications, fundamental engineering breakthroughs, and experimental methodologies that underpin the Iseult system, providing a comprehensive resource for researchers and drug development professionals engaged in advanced neuroimaging.
Core Technical Specifications of the Iseult 11.7 T System
The Iseult magnet is an engineering marvel designed to meet the extreme demands of stable, homogeneous ultra-high field generation. Its specifications reflect solutions to unique challenges in superconductor mechanics, cryogenics, and field stability.
Table 1: Primary Magnet Specifications of the Iseult 11.7 T System
| Parameter | Specification | Significance |
|---|---|---|
| Central Magnetic Field | 11.72 T [10] | Highest magnetic field used for human MRI; enables supreme SNR and spectral resolution. |
| Warm Bore Diameter | 90 cm [10] | Accommodates a human head and shoulders for whole-body imaging. |
| Magnet Weight | 132 tons [2] [11] | Reflects the massive scale required for active shielding and structural integrity. |
| Operating Current | 1470 - 1483 A [10] [11] | Current required to achieve target field with NbTi superconductor. |
| Operating Temperature | 1.8 K [10] [11] | Superfluid helium temperature for cryostable operation. |
| Stored Energy | 338 MJ [10] [11] | Highlights the immense energy managed by the protection system. |
| Field Homogeneity | < 0.5 ppm (peak-to-peak over 22 cm DSV) [10] | Essential for high-quality, artifact-free imaging. |
| Field Stability | 0.05 ppm/h [10] | Critical for advanced sequences, especially diffusion and functional MRI. |
Table 2: Cryogenic and Infrastructure Specifications
| Parameter | Specification | Significance |
|---|---|---|
| Coolant | Superfluid Helium [10] [11] | Provides superior heat conduction for cryostability. |
| Helium Bath Volume | ~7,000 liters [2] [6] | Large reservoir to maintain thermal equilibrium. |
| Conductor Material | Niobium-Titanium (NbTi) [10] | Mature, reliable superconductor technology. |
| Conductor Length | 182 km [2] [6] | Total length of superconducting wire in the coil. |
| Operating Mode | Driven (Non-Persistent) [10] | Eliminates need for persistent-mode superconducting joints. |
Fundamental Engineering Breakthroughs
Magnet and Cryogenic System Design
The core magnet design involved critical decisions that balanced performance, risk, and feasibility. A key choice was the use of Niobium-Titanium (NbTi) over more brittle alternatives like Nb₃Sn, prioritizing the material's maturity, cost-effectiveness, and reliability for a project of this scale [10]. The magnet is actively shielded, using a complex arrangement of superconducting coils to contain the magnetic field. This eliminated the need for a 750- to 2000-ton iron shield, which would have been structurally prohibitive for the NeuroSpin building [10].
To operate the extensive NbTi conductor in a cryostable regime, the system is cooled by a pressurized bath of superfluid helium at 1.8 K, serviced by a dedicated cryogenic plant. This superfluid bath provides an order of magnitude better heat conduction than conventional liquid helium at 4.2 K, ensuring the magnet remains stable against minor thermal disturbances [10] [2]. The sheer scale of this cryogenic system—involving thousands of liters of helium—is a breakthrough in its own right for an MRI installation.
Quench Protection and Safety Systems
Given the immense 338 MJ of energy stored in the magnetic field, a robust quench protection system was paramount. The Iseult project adopted a Magnet Safety System (MSS) with a philosophy more common to particle physics detectors than medical imaging systems [10]. This system is designed for high availability and reliability, continuously monitoring over 300 sensors. Its quench detection is based on a two-out-of-three (2oo3) voting logic for redundancy, triggering a controlled energy dump into an external resistor if a quench is detected [10]. This sophisticated safety architecture allows the magnet to operate at field without the need for permanent on-site supervision.
Mitigation of Radiofrequency Field Inhomogeneity
A major technical hurdle in UHF MRI is the inhomogeneity of the radiofrequency (B1+) field, caused by the shortened wavelength at 500 MHz (the Larmor frequency for hydrogen at 11.7 T). The Iseult team addressed this through advanced Parallel Transmission (pTx) technology [2]. A custom-built pTx coil with 16 transmit elements was used, driven by high-power (2 kW per channel) amplifiers. Researchers deployed specific RF pulse design algorithms like kT-points and Gradient Ascent Pulse Engineering (GRAPE) to mitigate B1+ inhomogeneity, achieving a normalized root mean square error (n.r.m.s.e.) of ~8% for excitations and ~13% for refocusing pulses over the entire brain [2]. This level of homogeneity is comparable to that achieved with volume coils at 3 T, representing a critical enabling step for practical human imaging at 11.7 T.
Experimental Protocol for In-Vivo Human Imaging
The first in-vivo human brain images at 11.7 T required a meticulously planned and approved experimental protocol to ensure both data quality and subject safety.
The Scientist's Toolkit: Key Research Reagents and Materials
Table 3: Essential Materials and Hardware for 11.7 T Experiments
| Item | Function / Application |
|---|---|
| Custom 16-Channel pTx Coil [2] | Mitigates B1+ inhomogeneity; enables application of tailored RF pulses for whole-brain coverage. |
| High-Power RF Amplifiers (2 kW/channel) [2] | Provide necessary power for RF pulses, especially critical for inversion and refocusing pulses. |
| Virtual Observation Points (VOPs) [2] | Enables real-time monitoring and management of Specific Absorption Rate (SAR) for patient safety. |
| Second-Order Shim System [2] | Corrects static B0 inhomogeneity, achieving an average standard deviation of 82.7 Hz (0.17 ppm) over the brain. |
| High-Resolution Phantoms & ex-vivo Samples [10] | Used for system calibration, sequence validation, and initial imaging tests prior to in-vivo studies. |
Safety Validation Protocol
As human exposure to an 11.7 T static field was uncharted territory, a comprehensive safety study was integrated into the imaging protocol. A cohort of 20 healthy volunteers was scanned for 90 minutes, while a separate control group of 20 subjects underwent an identical protocol with the magnetic field switched off (0 T) to control for psychological (nocebo) effects [2]. The assessments included:
- Physiological Monitoring: Continuous tracking of heart rate and blood pressure.
- Vestibular and Balance Tests: To assess potential effects on the inner ear and equilibrium [2] [6].
- Cognitive and Behavioral Measurements: To evaluate any impact on cognitive function [2].
- Genotoxicity Analysis: Blood samples drawn before and after the scan were analyzed for chromosomal damage [2] [6].
Statistical analysis (ANOVA) revealed no significant differences between the 11.7 T and 0 T groups across all tests (P = 0.54), providing the first evidence that prolonged human exposure to this magnetic field strength is safe and well-tolerated [2].
Applications in Neuroscience and Drug Development
The Iseult 11.7 T scanner opens a new window of opportunity for neuroscience and the development of biomarkers for neurological diseases. Its exceptional resolution and SNR enable researchers to probe the brain's microstructure and function at the mesoscopic scale, bridging the gap between macroscopic human imaging and microscopic animal studies [2].
Key application areas include:
- Neurodegenerative Diseases: Mapping hippocampal subfields in Alzheimer's disease, assessing iron content in the basal ganglia for Parkinson's disease, and visualizing cortical layers [2] [6].
- Epilepsy: Identifying subtle cortical malformations (e.g., focal cortical dysplasia) that are often missed by conventional 1.5 T or 3 T scanners in patients with drug-resistant epilepsy, potentially making them eligible for curative surgery [6].
- Oncology and Cerebrovascular Diseases: Characterizing brain tumors, detecting microvessels and small metastases, and providing sensitive detection of cerebral microbleeds related to traumatic brain injury or stroke [2] [6].
- Multinuclear Spectroscopy: Imaging of non-proton nuclei such as lithium (for bipolar disorder), sodium (23Na), and phosphorus (31P) to study energy metabolism and neurotransmitter cycling in unprecedented detail [2] [12].
- Advanced Microstructural Imaging: The ultra-high field provides sufficient SNR for high angular resolution diffusion imaging, which will enhance the accuracy of diffusion tensor imaging and tractography for mapping the brain's structural connectome [2].
The Iseult 11.7 T whole-body MRI system is a testament to two decades of international collaboration and engineering innovation. Its technical breakthroughs—from the actively shielded NbTi magnet cooled by superfluid helium to the sophisticated parallel transmission and safety systems—have successfully brought human neuroimaging into a new regime of magnetic field strength. The system provides a powerful, safe platform for neuroscience research, offering the spatial and contrast resolution necessary to explore the human brain at a mesoscopic level. As this technology continues to evolve, it holds immense promise for uncovering the pathological mechanisms of a wide range of neurological and psychiatric disorders, accelerating the development of new diagnostic biomarkers and therapeutic strategies.
Understanding the human brain at the mesoscopic scale, which bridges the gap between microscopic cellular circuits and macroscopic brain regions, represents one of the most significant challenges in modern neuroscience [2]. This scale, corresponding to spatial resolutions of approximately 0.1 mm, allows for the exploration of functional units such as cortical columns and layers that form the fundamental architecture of neural computation [13]. The pursuit of this goal has driven the development of ultra-high-field Magnetic Resonance Imaging (MRI) systems, culminating in the recent achievement of in vivo human brain imaging at 11.7 Tesla (T) [2]. This magnetic field strength substantially surpasses the previous human imaging record of 10.5 T and offers a supralinear gain in signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) [2] [13]. For researchers and drug development professionals, this technological leap provides an unprecedented tool for non-invasive, in-situ investigation of brain anatomy, function, and structural connectivity, with profound implications for identifying novel biomarkers and understanding the pathological mechanisms underlying neurological and psychiatric disorders [2] [14].
The core physical principle enabling this advance is the boost in intrinsic signal provided by higher magnetic fields. This increased signal can be leveraged to achieve higher spatial resolution within practically feasible acquisition times [13]. The Iseult 11.7-T MRI scanner, a project launched in the early 2000s by the French Atomic Energy Commission (CEA), has now successfully demonstrated this capability, acquiring human brain images in vivo and revealing details within the cortical ribbon that are not visible at lower field strengths [2]. This whitepaper details the technical specifications, experimental methodologies, and safety protocols that have made mesoscale in vivo brain imaging a reality, framing these developments within the broader context of ultra-high-field MRI applications for neuroscience research.
Technical Specifications of the 11.7 Tesla Iseult Scanner
The Iseult 11.7-T MRI system is an engineering marvel, representing nearly two decades of research and development. Its design fundamentally differs from conventional clinical MRI scanners, requiring innovations in magnet construction, cryogenics, and radiofrequency (RF) management to achieve the necessary field strength, homogeneity, and stability for human imaging [2] [13].
Magnet and Cryogenic System
The heart of the system is a 132-ton magnet with a 90-cm internal diameter, large enough to accommodate a human head [2] [13]. Unlike standard MRI magnets that use a solenoid design, the Iseult magnet consists of a stack of 170 double pancakes of superconducting wire, a design borrowed from high-energy physics magnets developed at CERN [13]. This configuration, coupled with a passive iron shim, achieves a remarkable homogeneity of 0.9 parts per million (ppm) peak-to-peak over a 22-cm-diameter sphere, which is essential for high-quality imaging [2]. To maintain the niobium-titanium superconductor in a cryostable state, the magnet is immersed in a bath of 7,000 liters of superfluid helium cooled to 1.8 Kelvin—a temperature significantly lower than the 4.2 K used in standard MRI systems. A dedicated cryogenic plant located beneath the scanner maintains this ultra-low temperature [2] [13].
Radiofrequency and Parallel Transmission System
A major hurdle in ultra-high-field MRI is the growing inhomogeneity of the RF field (B1+) used to excite nuclear spins, a consequence of the shorter wavelength (~500 MHz for hydrogen at 11.7 T) interacting with the human head [2]. The Iseult project deployed a sophisticated parallel transmission (pTx) system to mitigate this problem. The system uses a home-made 16-transmit-element RF coil driven by eight high-power (2 kW per channel) RF amplifiers [2]. Advanced pulse design algorithms, including kT-points and gradient ascent pulse engineering (GRAPE), are employed to tailor RF pulses that compensate for B1+ inhomogeneity while simultaneously constraining the specific absorption rate (SAR)—a measure of RF power deposition in tissue—to safe levels using Virtual Observation Points [2]. This approach achieved normalized root mean square errors (n.r.m.s.e.) of ~8% for excitations and ~13% for refocusing pulses over the whole brain, a level of homogeneity comparable to that intrinsic to volume coils at 3 T [2].
Table 1: Key Technical Specifications of the Iseult 11.7-T MRI System
| Component | Specification | Performance Metric |
|---|---|---|
| Magnet | 170 double-pancake coil design, 90 cm bore | Field Strength: 11.7 T; Homogeneity: 0.9 ppm over 22-cm DS [2] |
| Cryogenics | Superfluid helium bath | Operating Temperature: 1.8 K; Helium Volume: 7,000 L [2] |
| Gradient System | Not fully specified for Iseult | For reference, a next-gen 7T system achieves 200 mT/m amplitude and 900 T/m/s slew rate [15] |
| RF Transmit | 16-element parallel transmit coil | Amplifier Power: 2 kW per channel; B1+ inhomogeneity mitigated via pTx [2] |
| Static B0 Shimming | Quadratic programming approach | Achieved ~0.17 ppm (82.7 Hz) standard deviation over the brain [2] |
Experimental Protocols for Mesoscale Imaging
The initial in vivo study on the Iseult scanner was exploratory, designed to validate the hardware setup and safety for human use. The protocol was granted regulatory and ethics approval and involved scanning 20 healthy adult participants [2].
Safety and Physiologic Monitoring Protocol
Given that the effects of prolonged exposure to an 11.7 T magnetic field on humans were previously unknown, a comprehensive safety protocol was implemented. A separate control group of 20 participants was scanned with the magnetic field switched off (0 T) but with simulated MRI sounds to account for psychological (nocebo) effects [2] [13]. The following measurements were taken for both groups:
- Physiological, vestibular, and cognitive tests were performed to assess any immediate adverse effects [2].
- Genotoxicity assessment was conducted only for the 11.7 T group, using blood samples drawn before and after the 90-minute exposure to perform intra-participant comparisons [2].
- Statistical analysis revealed no significant differences related to magnetic field exposure across all tests, providing initial evidence for the safety of human scanning at this field strength [2].
Image Acquisition and Pulse Design Workflow
For each participant, a specific workflow was followed to acquire T2 and T2*-weighted images, which provide anatomical contrast sensitive to tissue microstructure and iron content, respectively.
The process begins with participant positioning within the magnet. Upon initiation, the first critical step is static B0 shimming performed up to the second order for each participant using a brain mask and a quadratic programming approach. This step optimizes the homogeneity of the main magnetic field, achieving an average standard deviation of 82.7 Hz (0.17 ppm) over the brain [2]. Subsequently, B0 and B1+ field mapping is conducted to characterize the static magnetic field and the transmit RF field for the individual participant's anatomy [2]. These maps are then used as inputs for the parallel transmission RF pulse design step. Here, algorithms such as kT-points (for small flip angle excitations) and GRAPE (for large flip angle refocusing pulses) compute RF pulses that compensate for the inherent B1+ inhomogeneity at 500 MHz [2]. This design process occurs under strict SAR monitoring using Virtual Observation Points to ensure patient safety by constraining RF power deposition [2]. Finally, with the tailored pulses, the T2 and T2*-weighted image acquisition is executed, yielding high-resolution images with minimal artifacts [2].
Table 2: Exemplary Imaging Protocol and Performance
| Parameter | Example Protocol | Performance Outcome |
|---|---|---|
| Sequence Type | T₂ and T₂*-weighted [2] | High CNR and SNR for anatomical detail [2] |
| Spatial Resolution | Up to 0.19 × 0.19 × 1 mm³ [2] | Reaches mesoscopic scale [13] |
| Acquisition Time | ~5 minutes for high-resolution scans [2] | Clinically feasible scan times [2] |
| Comparative Advantage | vs. 3T and 7T MRI | Higher spatial resolution for same CNR and time; clearer cortical ribbon details [2] |
The Scientist's Toolkit: Essential Research Reagents & Materials
Successfully conducting imaging studies at 11.7 T requires a suite of specialized hardware and software solutions. The following table details key components of this research toolkit.
Table 3: Essential Research Reagents and Materials for 11.7T Imaging
| Item / Solution | Category | Function in Research |
|---|---|---|
| Parallel Transmission RF Coil | Hardware | A 16-transmit-element coil to generate and control RF fields, mitigating B1+ inhomogeneity at 500 MHz [2]. |
| pTx Pulse Design Algorithms (kT-points, GRAPE) | Software | Computational methods to design complex RF pulses that correct for field inhomogeneities and control SAR [2]. |
| Virtual Observation Points (VOPs) | Software / Safety | A framework for monitoring and enforcing global and local specific absorption rate (SAR) limits in real-time during pTx [2]. |
| High-Power RF Amplifiers | Hardware | Provide sufficient power (2 kW per channel) for RF pulse transmission, crucial for achieving uniform inversion and refocusing [2]. |
| High-Channel-Count Receive Array | Hardware | A receiver coil with many channels (e.g., 64- or 96-channel) to increase signal-to-noise ratio and enable accelerated parallel imaging [15]. |
| Automated Color-Coding Software | Software / Analysis | Tools for tri-variate color-coded visualization of multiparametric maps or for highlighting longitudinal changes (e.g., in metastases) to improve diagnostic accuracy [16] [17]. |
Applications in Neuroscience Research and Drug Development
The ability to perform in vivo human brain imaging at mesoscale resolutions opens new frontiers for both basic neuroscience and applied clinical research. The high resolution and unique contrasts provided by 11.7 T MRI are poised to make a significant impact in several key areas.
Probing Microstructure in Preclinical Models
The utility of 11.7 T diffusion MRI has already been demonstrated in preclinical models, such as human brain organoids derived from induced pluripotent stem cells (iPSCs). One study achieved ≤40 μm isotropic resolution, providing a 3D view of organoid microstructure, including rosette-like formations, without the need for tissue clearing [14]. Furthermore, diffusion tractography methods were applied to model neuronal organization within these organoids [14]. This label-free, non-destructive imaging approach is a powerful modality for deep tissue imaging of whole organoids, with the potential to significantly impact the modeling of psychiatric disorders, neurodegenerative diseases, viral infections, and the assessment of neurotoxicity in drug screening pipelines [14].
Clinical and Translational Research Targets
The Iseult project and related ultra-high-field research have identified several high-priority clinical targets where mesoscale resolution can provide transformative insights [2] [13]:
- Drug-resistant focal epilepsy: For identifying subtle malformations like focal cortical dysplasia or mesial temporal sclerosis.
- Multiple sclerosis: To improve the detection of cortical lesions and visualize the central venule within lesions.
- Neurodegenerative diseases: For assessing iron content in the basal ganglia in Parkinson's disease, studying hippocampus status in Alzheimer's disease, and aiding deep brain stimulation planning.
- Brain tumors and cerebrovascular disease: Enabling better assessment of microvessels, angiogenesis, small metastases, and chronic stroke.
- Psychiatric disorders: Facilitating MR spectroscopy of neurotransmitters (e.g., lithium in bipolar disorder) and markers of energy metabolism (e.g., ³¹P).
The successful acquisition of in vivo human brain images at 11.7 T marks a watershed moment for neuroimaging, confirming the feasibility and safety of MRI at this extreme field strength. The technology now provides neuroscientists and drug developers with a tool to explore the human brain at a mesoscopic scale, revealing architectural features within the cortical ribbon that were previously inaccessible non-invasively [2] [13].
The immediate next steps for the technology focus on overcoming current limitations and further boosting performance. The development and implementation of motion correction tools are critical, as a significant portion of high-resolution scans in the initial study were corrupted by participant motion [2]. Furthermore, the deployment of highly accelerated acquisition sequences, more efficient RF coils, higher channel-count receiver arrays, and more powerful gradient systems is underway [2] [15]. These improvements will be essential for enabling high-resolution functional MRI (fMRI) and diffusion tensor imaging (DTI)/tractography, which were not within the scope of the preliminary study [2]. The ultimate goal is to bridge the gap between the extensive knowledge of microscopic circuits in animal models and the human brain connectome at a macroscopic scale, thereby generating new hypotheses about brain function and the mechanisms underlying mental illnesses [2].
In conclusion, the 11.7 T Iseult MRI scanner has transitioned from a visionary engineering project to an operational scientific instrument. By delivering mesoscale resolution in vivo, it provides an unparalleled window into the microstructure and function of the living human brain, offering tremendous potential to advance our understanding of both normal brain function and the pathological processes that underlie a wide spectrum of neurological and psychiatric disorders.
Demonstrated Safety and Tolerability of 11.7T for Human Scanning
The deployment of ultra-high field (UHF) magnetic resonance imaging (MRI) scanners at 11.7 Tesla (T) represents a monumental leap in neuroimaging capability, enabling mesoscale resolution of the human brain. This technical guide synthesizes evidence from the first in vivo human studies with the Iseult 11.7 T MRI scanner, which confirm that exposure to this intense magnetic field is safe and well-tolerated by human subjects. The data herein provide researchers and drug development professionals with a foundational safety profile, essential for designing future neuroscience research protocols and exploring novel biomarkers for neurological disorders.
The pursuit of understanding the human brain at a mesoscopic scale—bridging the gap between macroscopic connectomics and microscopic cellular circuits—has been a primary driver behind the development of ultra-high field MRI [2]. The Iseult 11.7 T MRI scanner, a project initiated in the early 2000s by the French Atomic Energy Commission (CEA), is at the forefront of this endeavor. Its 132-ton magnet, operating at a cryogenic 1.8 K with 7,000 liters of superfluid helium, represents a significant engineering achievement [2] [6].
For neuroscience, the superior signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) afforded by 11.7 T translate directly to an unprecedented ability to resolve fine anatomical details. Imaging at this field strength can achieve resolutions of 0.19 x 0.19 x 1 mm³ in acquisition times as short as four to five minutes—a feat that would require impractically long scans on conventional 3 T systems [2] [6]. This capability opens new windows of opportunity for investigating the cytoarchitecture of neuron clusters, cortical layers, and their structural connections, which are pivotal for confirming or refuting existing hypotheses about brain function and the mechanisms underlying mental illnesses such as depression, autism, and schizophrenia [2]. Furthermore, it holds promise for developing new biomarkers for conditions like drug-resistant focal epilepsy, multiple sclerosis, Alzheimer's disease, and Parkinson's disease [2] [6].
Comprehensive Safety Assessment of 11.7T MRI
Prior to the initial in vivo human scans, the highest magnetic field strength used for human MRI was 10.5 T [2]. The safety of human exposure to the more intense 11.7 T static field was, therefore, uncharted territory, with potential concerns rooted in the known physical interactions between strong magnetic fields and biological tissues.
Physiological and Vestibular Effects
The primary safety study for the Iseult scanner involved a carefully controlled protocol on 20 healthy adult participants who were scanned for 1.5 hours at 11.7 T [2]. A separate control cohort of 20 participants underwent the same protocol inside the scanner with the magnetic field switched off (0 T). To maintain blinding and control for psychological bias (the nocebo effect), the sound of MRI sequences was mimicked for the control group using a loudspeaker [2].
The study assessed multiple safety parameters, with results summarized in the table below.
Table 1: Key Safety and Tolerability Findings from the Iseult 11.7T Inaugural Human Study
| Safety Domain | Assessment Method/Target | Outcome at 11.7 T |
|---|---|---|
| Vital Signs | Blood pressure, heart rate [2] | No significant changes related to field exposure [2] |
| Vestibular Function | Nystagmus, vertigo, balance tests (e.g., Unterberger's stepping test) [2] [18] | No significant differences from 0 T control group; some transient vestibular effects are known UHF phenomena [2] |
| Cognitive Performance | Standardized cognitive tests [2] | No significant impairment detected [2] |
| Genotoxicity | Blood samples for chromosomal damage analysis pre- and post-exposure [2] | No significant genotoxic effects observed [2] |
| Overall Tolerability | Subjective experience and completion of 90-minute scan [2] | Scans were successfully completed, demonstrating practical tolerability [2] |
Statistical analysis of variance across all tests revealed no significant differences related to magnetic field exposure (P = 0.54 for group and run effects) [2]. This provides strong evidence that the 11.7 T static magnetic field does not induce acute harmful physiological, vestibular, cognitive, or genotoxic effects in healthy adults.
The findings are consistent with the known biophysics of UHF MRI. Theoretical concerns regarding Lorentz forces on blood flow in the aortic arch have not translated into clinically significant changes in cardiovascular parameters in human studies at fields up to 8 T [18]. The most commonly reported subjective sensations at UHF are vertigo and nystagmus, attributed to Lorentz forces on the ionic fluid within the semicircular canals of the vestibular system [18]. While these effects can be unpleasant, the data from the Iseult project confirm they are manageable and do not pose a serious health risk during a controlled scanning session.
Radiofrequency (RF) Energy and Specific Absorption Rate (SAR)
With increasing magnetic field strength, the operational RF frequency also increases (500 MHz for hydrogen nuclei at 11.7 T), which intensifies the challenge of RF field inhomogeneity and raises safety concerns related to localized power deposition or SAR [2] [18]. The Iseult project mitigated these risks through advanced parallel transmission (pTx) hardware and software. This system employed a dedicated 16-transmit-element head coil and utilized virtual observation points for SAR monitoring alongside RF pulse design algorithms (e.g., kT points and GRAPE) to tame the SAR and ensure it remained within safe limits [2]. This approach successfully mitigated the severe artifactual signal variations that would otherwise occur, yielding images with good signal homogeneity without severe RF inhomogeneity artifacts [2].
Detailed Experimental Protocols for Safety and Imaging
This section outlines the core methodologies used to establish the safety and initial imaging capabilities of the 11.7 T scanner.
Safety Validation Protocol
The following workflow illustrates the comprehensive safety assessment conducted for the Iseult 11.7 T scanner:
Diagram 1: Safety assessment workflow for the Iseult 11.7 T MRI scanner. The 0 T control group was used to isolate the effects of the magnetic field from other factors.
Imaging Protocol for In Vivo Human Brain
The acquisition of the first in vivo images required sophisticated engineering to overcome the inherent physical challenges of 11.7 T.
- Static B0 Shim: For each participant, static B0 shimming was performed up to the second order using a brain mask and a quadratic programming approach. This achieved an average field homogeneity of 82.7 Hz standard deviation (0.17 ppm) over the brain [2].
- RF Field Mapping and Pulse Design: Following B0 shimming, RF field (B1+) mapping was conducted. Subject-specific parallel transmission RF pulses were then designed using kT-points (for small flip-angle excitations) and the Gradient Ascent Pulse Engineering (GRAPE) algorithm (for large flip-angle refocusing pulses) [2]. This process was critical for mitigating the intrinsic B1+ inhomogeneity, which had a coefficient of variation of 45% over the whole brain in static shimming mode [2].
- Image Acquisition: With the tailored pTx pulses, T2-weighted and T2*-weighted acquisitions were performed. The system demonstrated the ability to produce high-fidelity images with resolutions reaching 0.19 x 0.19 x 1 mm³ in just a few minutes, revealing details of the cortical ribbon and cerebellar structures that are not visible at lower field strengths under comparable acquisition times [2].
The Scientist's Toolkit: Essential Research Reagents & Materials
Conducting research on an 11.7 T MRI system requires a suite of specialized hardware and software solutions. The following table details the key components used in the featured Iseult project.
Table 2: Key Research Reagent Solutions for 11.7T Human MRI
| Item/Technology | Function & Purpose | Specification/Implementation in Iseult Project |
|---|---|---|
| Parallel Transmission (pTx) Coil | Enables manipulation of the RF field to overcome B1+ inhomogeneity and control SAR. | Home-made 16-transmit channel coil with dedicated SAR monitoring via Virtual Observation Points [2]. |
| pTx Pulse Design Software | Designs subject-specific RF pulses to achieve uniform excitation/refocusing across the brain. | Utilized kT-points (for excitation) and GRAPE algorithm (for refocusing) pulses [2]. |
| High-Order B0 Shimming | Corrects static magnetic field inhomogeneities to improve image quality and spectral fidelity. | Implemented using a brain mask and quadratic programming up to 2nd order [2]. |
| High-Power RF Amplifiers | Provides sufficient power to drive the transmit coils effectively at high frequencies. | 2 kW per channel amplifiers were used; their high power was noted as essential [2]. |
| Multi-Channel Receiver Array | Increases signal-to-noise ratio (SNR) and enables accelerated parallel imaging. | A 128-channel receiver system was integrated; studies used 64- and 96-channel receiver head coils [2]. |
The inaugural in vivo human imaging on the Iseult 11.7 T MRI scanner marks a pivotal moment for ultra-high field neuroimaging. The data conclusively demonstrate that exposure to this intense magnetic field is safe and well-tolerated in healthy human volunteers over scanning durations typical for research protocols. The successful mitigation of technical challenges like RF inhomogeneity and SAR paves the way for its application in fundamental and clinical neuroscience.
The immediate next steps for the technology include the development and implementation of motion correction tools and highly accelerated sequences to leverage the available SNR for even higher resolutions and to combat motion artifacts, which corrupted a significant number of high-resolution scans in the initial study [2]. Furthermore, the deployment of more efficient RF coils, higher channel-count receiver arrays, and more powerful gradients is underway [2]. These advancements will be crucial for unlocking the full potential of 11.7 T for high-resolution functional MRI, diffusion tensor imaging, and tractography, ultimately transforming our understanding of the human brain in health and disease.
The strength of the main magnetic field (B0) in a Magnetic Resonance Imaging (MRI) scanner is a fundamental determinant of image quality, primarily by influencing the signal-to-noise ratio (SNR). SNR represents the strength of the desired MR signal relative to the background noise inherent in the measurement. A higher SNR enables the creation of images with greater clarity, finer detail, and the ability to visualize smaller structures. The pursuit of higher magnetic fields is driven by the need to see the human brain, the most complex organ in the human body, at a mesoscopic scale—a level of detail that bridges the gap between macroscopic brain areas and microscopic cellular circuits [2]. This whitepaper explores the SNR advantages and associated technical challenges of three field strengths—3 Tesla (T), 7T, and the cutting-edge 11.7T—framed within the context of their revolutionary potential for neuroscience research and drug development.
The relationship between field strength and SNR is foundational. In an ideal scenario, SNR increases linearly with B0; however, in practice, the gain is often supralinear, with studies observing SNR proportional to B0 raised to a power between 1.65 and 2.1 at ultra-high fields (UHF) [19]. This powerful boost is the catalyst for a cascade of benefits: it can be traded for higher spatial resolution within a practical scan time, improved contrast-to-noise ratio (CNR) for better tissue differentiation, or faster acquisition for enhanced temporal resolution or higher patient throughput [19] [12]. For neuroscientists and drug development professionals, this translates to an unprecedented ability to non-invasively probe the brain's structure, function, and metabolism, potentially revealing new biomarkers and therapeutic targets for neurological and psychiatric disorders [2] [6].
Fundamental Physics of the Signal-to-Noise Ratio (SNR) Gain
The fundamental source of the MR signal is the net magnetization created when hydrogen nuclei (protons), primarily in water molecules, align with a strong external magnetic field. The strength of this magnetization, and hence the intrinsic signal, is directly proportional to the strength of the B0 field. This is a consequence of the population difference between energy states of the protons, which increases with B0 according to the Boltzmann distribution. Doubling the magnetic field strength theoretically doubles the available signal.
However, the observed gain in practice is often more pronounced. At ultra-high fields (≥7T), the increase in SNR can be supralinear for several reasons. First, with higher field strength comes a higher resonance (Larmor) frequency. For biological tissues, the measurement noise is often sample-dominated, meaning it arises from the patient's body rather than the scanner's electronics. This sample-dominated noise increases linearly with frequency, but the signal increases even more favorably in certain scenarios, leading to the observed SNR gains beyond a simple linear relationship [19]. This enhanced signal is the key that unlocks higher-resolution imaging, as the signal must be sufficient to fill the smaller voxels used in high-resolution acquisitions.
Beyond the raw signal increase, the contrast mechanisms that underpin different MRI modalities are also profoundly affected by field strength. The longitudinal relaxation time (T1) of tissues lengthens with increasing B0, which can improve background suppression in techniques like time-of-flight (TOF) angiography and arterial spin labeling (ASL) [19]. Conversely, the transverse relaxation times (T2 and T2*) shorten, which can be a challenge but also enhances sensitivity to magnetic susceptibility differences. This heightened susceptibility effect is powerfully leveraged in techniques like Susceptibility-Weighted Imaging (SWI) and Quantitative Susceptitant Mapping (QSM) to visualize micro-bleeds, iron deposits, and venous structures, and in Blood Oxygen Level-Dependent (BOLD) functional MRI (fMRI) to achieve a higher spatial localization of neuronal activity [19] [12]. Furthermore, for magnetic resonance spectroscopy (MRS), the spectral separation of metabolite peaks widens linearly with B0, improving the detection and quantification of neurochemicals [12].
Technical Specifications and Performance Comparison
The leap in performance from conventional 3T clinical systems to 7T research scanners, and further to the frontier 11.7T systems, involves monumental engineering achievements. The following table summarizes the key specifications and capabilities of these three field strengths.
Table 1: Scanner Specifications and Performance Comparison
| Feature | 3T (Clinical/High-Performance) | 7T (Ultra-High Field) | 11.7T (State-of-the-Art UHF) |
|---|---|---|---|
| Typical Magnet Weight | ~6-7 tons | Varies | 132 tons [2] [6] |
| Typical Whole-Body Gradient Strength | 40-80 mT/m | Similar to 3T for whole-body; up to 200 mT/m for head-only [20] | Information Missing |
| Exemplary Head Gradient Strength | 300-500 mT/m (Connectome 2.0) [21] | 200 mT/m (NexGen) [20] | Information Missing |
| Exemplary Slew Rate | 200-600 T/m/s (Connectome 2.0) [21] | 900 T/m/s (NexGen) [20] | Information Missing |
| Representative RF Receive Channels | 32-64 | 64-128 [20] | 16-channel transmit array [2] |
| Cooling System | Liquid Helium (~4.2 K) | Liquid Helium | Superfluid Helium bath at 1.8 K [2] [10] |
| Key Imaging Applications | Clinical diagnostics, DTI, fMRI | High-res morphometry, SWI, high-CNR fMRI, MRS | Mesoscale T2/T2* anatomy, target for fMRI and dMRI [2] |
A critical component driving the latest advances is the gradient subsystem. The NexGen 7T scanner features a head-only asymmetric gradient coil with a third intermediate winding layer. This design allows for a massive performance of 200 mT/m amplitude and a 900 T/m/s slew rate, an order of magnitude greater than standard 7T whole-body gradients. This high performance is crucial for achieving ultra-high spatial resolution by enabling shorter echo times (reducing signal loss) and shorter readout periods (minimizing image blurring and distortion) [20]. Similarly, the Connectome 2.0 scanner, a dedicated 3T system for brain connectomics, uses a similar three-layer gradient design to achieve a remarkable 500 mT/m strength, pushing the boundaries of diffusion MRI to infer cellular and axonal features [21].
The 11.7T Iseult scanner represents a feat of engineering. Its 132-ton magnet operates at 1.8 Kelvin with a superfluid helium bath to maintain superconductivity at an unprecedented field strength for human imaging. A major focus at 11.7T is managing the radiofrequency (RF) field inhomogeneity caused by the short wavelength of the 500 MHz RF waves. This is addressed using a parallel transmission (pTx) system with 16 independent transmit elements and sophisticated pulse design algorithms to mitigate severe signal variations and control the specific absorption rate (SAR), a measure of RF power deposition in the body [2].
Quantitative SNR and Image Quality Metrics
The theoretical and observed gains in SNR and resolution across field strengths can be quantified, providing a clear rationale for the push towards UHF systems. The following table synthesizes key comparative metrics.
Table 2: Quantitative SNR and Resolution Metrics Across Field Strengths
| Metric | 3T | 7T | 11.7T |
|---|---|---|---|
| Theoretical SNR Gain (Relative to 1.5T) | ~2x | ~4.7-5.8x [19] | >7x (Theoretical) |
| Observed SNR Gain | Baseline | Up to ~2x over 3T for some applications [19] | Significant gain enabling mesoscale resolution [2] |
| Routine Isotropic fMRI Resolution | 2-3 mm | 0.8-1.0 mm | Target for <0.8 mm [2] |
| Demonstrated High-Res Anatomic Scan | Information Missing | <0.5 mm isotropic (NexGen 7T) [20] | 0.19 x 0.19 x 1 mm³ in 4-5 minutes [2] [6] |
| T1 Relaxation Time (Gray Matter) | Longest of the three (exact value depends on tissue) | Intermediate | Shortens relative to lower fields, improving background suppression in angiography [19] |
| T2/T2* Relaxation Time (Gray Matter) | Intermediate | Shorter than 3T | Shortest, enhancing susceptibility-based contrast [19] [12] |
A compelling visual demonstration of the resolution advantage comes from a direct comparison of T2*-weighted images acquired at 3T, 7T, and 11.7T with identical acquisition times. While the 3T and 7T images show progressive improvement, the 11.7T image reveals fine details within the cortical ribbon and around the calcarine fissure that are not visible at the lower field strengths [2]. This leap in resolution is made possible by the high SNR, which allows the scanner to resolve structures at a sub-millimeter, or "mesoscopic," scale within a clinically feasible scan time of just a few minutes. The NexGen 7T system also demonstrates this principle, achieving functional imaging at 0.35-0.45 mm isotropic resolution, which is sufficient to resolve cortical layer activity [20].
Experimental Protocols for Ultra-High Field Imaging
The Iseult 11.7T Human Imaging Protocol
The first in vivo human brain images at 11.7T were acquired following a rigorous and safety-focused protocol [2].
- Magnet and Homogeneity: The 132-ton superconducting magnet was shimmed to a homogeneity of 0.9 ppm peak-to-peak over a 22-cm-diameter sphere. Static B0 shimming for each volunteer achieved an average standard deviation of 82.7 Hz (0.17 ppm) over the brain.
- RF Pulse Design and Parallel Transmission: To counter severe B1+ inhomogeneity, the protocol used a home-made 16-channel parallel transmission (pTx) RF coil. Small flip-angle excitation and large flip-angle refocusing pulses were designed using kT-point and GRAPE (gradient ascent pulse engineering) algorithms, respectively, achieving normalized root mean square errors (n.r.m.s.e.) of ~8% and ~13% over the whole brain.
- Image Acquisition: Following B0 and RF field mapping, T2-weighted and T2-weighted acquisitions were performed. A key demonstration was a 2D T2-weighted acquisition repeated at 3T, 7T, and 11.7T on different participants with identical acquisition times (4 minutes 17 seconds), directly showcasing the resolution advantage at 11.7T.
- Safety and Tolerability Assessment: Given the uncharted territory of long exposures to 11.7T fields, the study included extensive safety monitoring on 20 volunteers. Physiological (blood pressure, heart rate), vestibular (balance), behavioral, and genotoxicity (chromosomal damage from blood samples) measurements were taken. A control group of 20 participants was tested with the magnetic field off (but with simulated scanner sounds) to account for nocebo effects. No significant differences were found between the groups, establishing initial evidence for the safety of 90-minute scans at this field strength [2] [6].
Next-Generation 7T High-Resolution fMRI Protocol
The NexGen 7T scanner protocol highlights how hardware advances beyond the magnet itself enable ultra-high resolution [20] [9].
- Gradient Performance: The "Impulse" head-gradient coil (200 mT/m, 900 T/m/s slew rate) was used. Its design minimized peripheral nerve stimulation (PNS), allowing the use of high slew rates. The shorter achievable echo spacing (0.58 ms for 0.6 mm resolution) reduced T2* blurring and geometric distortion in Echo Planar Imaging (EPI) used for fMRI.
- High-Channel Receive Arrays: The system was equipped with either a 64-channel or 96-channel receive array coil. Compared to a standard 32-channel coil, these arrays provided a ~30% improvement in SNR in the cerebral cortex, crucial for resolving thin cortical layers.
- High-Resolution fMRI: The combination of high intrinsic SNR from the 7T field, reduced g-factor noise from the high-channel arrays, and the high-performance gradients allowed the acquisition of functional images at 0.35-0.45 mm isotropic resolution. This resolution enables the mapping of neuronal activity across different cortical layers (laminae), providing insights into the direction of information flow within a cortical area.
The Scientist's Toolkit: Essential Research Reagents & Hardware
Achieving mesoscopic resolution in vivo requires a suite of specialized hardware and software solutions that extend far beyond a powerful magnet. The following table details key components of the UHF "toolkit."
Table 3: Essential Research Reagents and Hardware for Ultra-High Field Neuroimaging
| Tool Name | Category | Function in Research | Field Strength Relevance |
|---|---|---|---|
| Parallel Transmission (pTx) System | RF Hardware/Software | Mitigates severe RF (B1+) field inhomogeneity by using multiple independent transmit channels with tailored RF pulses. | Critical at 7T and essential at 11.7T [2] [19] |
| High-Density Receive Array Coils | RF Hardware | Increases signal-to-noise ratio (SNR) and enables higher acceleration factors (parallel imaging) by using many small receiver elements. | 7T (64-128 channels), 11.7T [20] |
| High-Performance Head Gradient Coils | Gradient Hardware | Enables higher spatial resolution and faster imaging by providing strong (Gmax) and fast (slew rate) magnetic field gradients for encoding. | 3T (Connectome 2.0), 7T (NexGen), 11.7T [20] [21] |
| Universal Pulses | RF Pulse Software | Pre-computed pTx pulses that work adequately across many subjects without time-consuming subject-specific calibration, streamlining workflow. | Promising solution for 7T+ clinical applications [19] |
| Advanced B0 Shimming | Shimming Hardware/Software | Corrects for static magnetic field inhomogeneities caused by tissue-air interfaces, which become more problematic at higher fields. | Essential at 7T and 11.7T [2] [19] |
| SAR Monitoring & Mitigation | Safety Software/Hardware | Monitors and controls the Specific Absorption Rate (SAR) of RF power, which increases with B0, to ensure patient safety. | Critical at UHF (7T, 11.7T) [2] [19] |
Applications in Neuroscience and Drug Development
The superior image quality afforded by UHF MRI, particularly 11.7T, opens new frontiers in neuroscience and therapeutic development. The primary application is bridging the scale between macroscopic human neuroimaging and microscopic findings in animal models by visualizing the brain's mesoscopic architecture [2]. This includes the cytoarchitectonic of neuron clusters and their connections, potentially allowing researchers to confirm or refute current hypotheses about brain function and the biological mechanisms underlying mental life and consciousness [2].
From a clinical and translational perspective, UHF MRI holds immense promise for identifying subtle pathological changes that are invisible at lower fields. Key targets include [2] [6] [12]:
- Drug-resistant focal epilepsy: Identifying subtle malformations like focal cortical dysplasia or mesial temporal sclerosis.
- Multiple sclerosis: Better visualization of cortical lesions and central veins within plaques.
- Neurodegenerative diseases: Assessing iron content in the basal ganglia for Parkinson's disease, hippocampal status in Alzheimer's disease, and precisely tracking the distribution of lithium in bipolar disorder.
- Brain tumors and cerebrovascular disease: Imaging microvessels for assessing angiogenesis, small metastases, and chronic stroke.
For drug development professionals, the ability to non-invasively measure brain metabolites (e.g., lactate, pyruvate, glutamate) and neurotransmitters with the enhanced spectral resolution of 11.7T MRS could provide valuable pharmacodynamic biomarkers [6]. This could reduce reliance on invasive procedures like intracerebral microdialysis and allow for more precise monitoring of treatment response in conditions from brain tumors to neurotrauma, ultimately accelerating the development of new central nervous system therapeutics.
The journey from 3T to 7T to 11.7T MRI represents a relentless pursuit of higher signal-to-noise ratio, a pursuit that fundamentally transforms our ability to visualize and understand the human brain. The SNR advantage at 11.7T is not merely incremental; it is the key that unlocks mesoscopic resolution, allowing in vivo imaging of brain structures and circuits at a level of detail previously attainable only through ex vivo histology. While significant technical challenges related to RF inhomogeneity and SAR management remain, solutions like parallel transmission are proving effective. The initial safety and imaging data from the Iseult 11.7T scanner are promising, confirming the applicability of MRI at this formidable field strength [2]. For neuroscientists and drug developers, these technological advances herald a new era of discovery, offering the potential to uncover the structural and functional underpinnings of neurological and psychiatric disorders and to develop targeted biomarkers and therapies with unprecedented precision.
From Bench to Bedside: Research Applications in Disease Modeling and Drug Discovery
Neurodegenerative diseases, including Alzheimer's disease (AD) and Parkinson's disease (PD), represent one of the most daunting challenges in modern medicine, affecting millions worldwide and imposing significant clinical and socioeconomic burdens [22]. The multifaceted nature of these conditions arises from intersecting genetic, metabolic, and environmental factors that culminate in progressive declines in cognition, motor control, and overall functionality. Despite relentless scientific efforts, effective interventions remain limited due to disease heterogeneity, prolonged preclinical phases, poor understanding of disease mechanisms, and diagnostic challenges [23].
The field is now at a transformative juncture, powered by two complementary technological revolutions: ultra-high-field neuroimaging and large-scale molecular biomarker discovery. The advent of 11.7-tesla (T) magnetic resonance imaging (MRI) represents a quantum leap in our ability to visualize the living human brain at mesoscopic scales, revealing previously inaccessible neuroanatomical details [2] [3]. Concurrently, international consortia like the Global Neurodegeneration Proteomics Consortium (GNPC) are establishing harmonized molecular datasets that enable the identification of disease-specific protein signatures [23]. This whitepaper examines how these advanced technologies are reshaping our understanding of neurodegeneration, with particular emphasis on their applications in AD and PD research, and provides technical guidance for researchers implementing these approaches.
Ultra-High-Field MRI: Technical Principles and Advantages
Ultra-high-field MRI systems, particularly the groundbreaking 11.7T Iseult scanner, offer substantial physical advantages over conventional clinical systems (typically 1.5T or 3T). The fundamental benefits stem from the supralinear gain in signal-to-noise ratio (SNR) with increasing magnetic field strength (B0), which scales approximately linearly with B0 [2] [12]. This enhanced SNR can be strategically leveraged to either boost spatial resolution, reduce acquisition time, or improve contrast-to-noise ratio—or achieve an optimal balance of all three parameters.
The Iseult project, launched in 2001 by the French Atomic Energy Commission (CEA), culminated in a 132-ton magnet operating at 11.7T, cooled by 7,000 liters of superfluid helium maintained at 1.8K [2] [3]. This engineering marvel achieves a field homogeneity of 0.9 ppm peak-to-peak over a 22-cm-diameter sphere with exceptional temporal stability (3 ppb per hour drift at thermal equilibrium)—specifications essential for high-resolution neuroimaging [2].
Table 1: Technical Advantages of 11.7T MRI Compared to Lower Field Systems
| Imaging Property | Relationship with Field Strength | Advantage at 11.7T |
|---|---|---|
| Signal-to-Noise Ratio (SNR) | SNR ∝ B₀ | Near-linear increase enables mesoscopic resolution |
| Spatial Resolution | Resolution ∝ B₀¹⁻³ | Achieves 0.2×0.2×1 mm³ in ~4 minutes [3] |
| Spectral Resolution | ΔF ∝ B₀ | Enhanced detection of neurochemicals (GABA, glutamate, glycogen) [3] |
| Magnetic Susceptibility | Δϕ ∝ B₀ × TE | Superior visualization of microvasculature, iron deposits, and microbleeds |
| T1 Relaxation Time | T1 = 1/(0.35 + 0.64 × B₀⁻⁰·⁷) | Lengthened T1 values enhance background suppression in angiography |
However, operating at 11.7T presents unique technical challenges, primarily radiofrequency (RF) field inhomogeneity resulting from the shortened wavelength of RF waves (500 MHz for water protons at 11.7T) [2]. This can cause severe artifactual signal variations in images. The Iseult team deployed parallel transmission (pTx) hardware and software with virtual observation points for specific absorption rate (SAR) monitoring to mitigate these effects [2]. Through dedicated RF pulse design algorithms (kT-points and GRAPE), they achieved normalized root mean square errors of approximately 8% for excitations and 13% for refocusing pulses over the whole brain—comparable to the intrinsic inhomogeneity achieved at 3T with volume coils [2].
Safety considerations for human exposure to such high magnetic fields were thoroughly investigated through physiological, vestibular, behavioral, and genotoxicity measurements on 20 volunteers. Statistical analysis revealed no significant differences between participants scanned at 11.7T and a control group at 0T, establishing the feasibility of human imaging at this unprecedented field strength [2] [24].
Applications in Alzheimer's Disease Research
The enhanced capabilities of 11.7T MRI are revolutionizing Alzheimer's disease research through improved visualization of pathological features and more sensitive detection of metabolic alterations. The mesoscopic resolution achievable with 11.7T reveals details within the cortical ribbon that remain invisible at lower field strengths, enabling more precise mapping of the characteristic neurodegeneration patterns in AD [2].
Hippocampal Imaging and Atrophy Assessment
The hippocampus, a brain region crucial for memory formation and consolidation, undergoes progressive atrophy in Alzheimer's disease. At 11.7T, the internal architecture of the hippocampus can be visualized with unprecedented clarity, potentially allowing researchers to identify subregional vulnerability patterns and track disease progression with enhanced sensitivity [25]. The high-resolution T2 and T2*-weighted images acquired at 11.7T provide exceptional contrast between hippocampal subfields, offering opportunities to detect the earliest signs of pathological changes, often before significant cognitive decline manifests [2] [25].
Amyloid and Tau Pathology Imaging
While direct detection of amyloid plaques and neurofibrillary tangles remains challenging for MRI, the enhanced susceptibility contrast at 11.7T improves visualization of potential surrogate markers. Cerebral microbleeds, which frequently co-occur with amyloid pathology and are associated with blood-brain barrier dysfunction, appear with greater conspicuity at ultra-high fields [22] [12]. Furthermore, the detection of subtle neuroinflammatory changes—a recognized component of AD pathogenesis—is enhanced through improved visualization of perivascular spaces and leptomeningeal contrast.
Complementing these structural advances, 11.7T magnetic resonance spectroscopic imaging (MRSI) enables more precise quantification of metabolic alterations in AD brains. The greater spectral separation at 500 MHz improves resolution of neurochemical profiles, potentially detecting early shifts in metabolites like myo-inositol (a glial marker), N-acetylaspartate (a neuronal integrity marker), and glutamate (the major excitatory neurotransmitter) [12] [3].
Applications in Parkinson's Disease Research
Parkinson's disease research is similarly being transformed by ultra-high-field MRI capabilities, particularly through enhanced visualization of the basal ganglia structures central to PD pathology and improved characterization of iron deposition patterns.
Basal Ganglia and Nigrostriatal Pathway Imaging
The substantia nigra pars compacta, which undergoes progressive degeneration in PD, contains neuromelanin and iron that create natural contrast at high magnetic fields. The 11.7T scanner dramatically improves visualization of this region, potentially allowing researchers to detect degenerative changes before significant cell loss occurs [2] [3]. Similarly, the basal ganglia nuclei—including the putamen, globus pallidus, and subthalamic nucleus—can be imaged with exceptional detail, supporting research into network-level dysfunction in PD [2].
The enhanced resolution enables more precise targeting for deep brain stimulation (DBS) planning, with potential to improve therapeutic outcomes and reduce side effects. The ability to visualize these small deep brain structures with unprecedented clarity may also facilitate the development of new surgical and neuromodulation approaches [2] [3].
Iron-Sensitive Imaging and Metabolic Profiling
Pathological iron accumulation in specific brain regions is a recognized feature of Parkinson's disease. The strong susceptibility effects at 11.7T make it exceptionally sensitive to these iron deposits, providing a potential biomarker for disease progression and treatment response [2] [12]. Quantitative susceptibility mapping (QSM) at ultra-high fields can precisely quantify iron content in the substantia nigra and other basal ganglia structures, offering a non-invasive method to monitor pathological processes.
Beyond structural and susceptibility-based imaging, 11.7T MRSI enables detailed investigation of metabolic disturbances in PD. The dopaminergic system, central to PD pathophysiology, can be indirectly studied through related metabolic pathways. Furthermore, the detection of neuromelanin and its degradation products may provide unique insights into the timing and progression of dopaminergic cell loss [3].
Table 2: 11.7T MRI Biomarkers in Neurodegenerative Disease Research
| Biomarker Category | Specific Markers | Alzheimer's Application | Parkinson's Application |
|---|---|---|---|
| Structural | Cortical thickness, hippocampal subfield volume | Early detection, tracking progression | Differential diagnosis |
| Susceptibility-Based | Iron content, microbleeds, venous morphology | Amyloid angiopathy assessment | Substantia nigra degeneration |
| Metabolic | GABA, glutamate, glutathione, energy metabolites | Neuronal integrity, excitotoxicity | Oxidative stress, dopaminergic metabolism |
| Vascular | Microvascular integrity, masseteric artery dilation | Vascular contribution to dementia | Autonomic dysfunction assessment |
| Connectivity | Structural and functional connectivity | Network disintegration patterns | Basal ganglia-cortical circuits |
Integrating Proteomics and Ultra-High-Field Imaging
The imaging advances provided by 11.7T MRI are powerfully complemented by large-scale molecular profiling initiatives. The Global Neurodegeneration Proteomics Consortium (GNPC) has established one of the world's largest harmonized proteomic datasets, comprising approximately 250 million unique protein measurements from over 35,000 biofluid samples (plasma, serum, and cerebrospinal fluid) [23]. This resource, accessible via the Alzheimer's Disease Data Initiative's AD Workbench, enables the identification of disease-specific differential protein abundance and transdiagnostic proteomic signatures of clinical severity.
Notably, the GNPC has identified a robust plasma proteomic signature of APOE ε4 carriership that is reproducible across AD, PD, frontotemporal dementia (FTD), and amyotrophic lateral sclerosis (ALS), suggesting shared molecular pathways underlying genetic risk [23]. Similarly, distinct patterns of organ aging across these conditions provide insights into the systemic nature of neurodegenerative processes.
The integration of ultra-high-field imaging data with deep molecular profiling creates unprecedented opportunities for multi-scale modeling of neurodegenerative diseases. Co-registration of mesoscopic structural information with proteomic signatures enables researchers to establish precise structure-function-molecular relationships, potentially identifying novel therapeutic targets and biomarkers for early intervention.
Experimental Protocols and Methodologies
Human Brain Imaging at 11.7T
The pioneering human imaging work with the Iseult 11.7T scanner employed carefully optimized protocols to balance image quality, acquisition time, and safety. The system utilizes a home-made parallel transmission RF coil with 16 transmit elements paired to eight 2-kW RF power amplifiers, with dedicated virtual observation points for SAR monitoring [2].
For anatomical imaging, T2 and T2*-weighted acquisitions have been successfully implemented using parallel transmission techniques to mitigate B1+ inhomogeneity. Representative protocol parameters include:
- Spatial Resolution: 0.19 × 0.19 × 1 mm³ to 0.2 × 0.2 × 1 mm³
- Acquisition Time: 4-5 minutes for high-quality anatomical images
- B0 Shimming: Second-order shimming using quadratic programming approach
- Typical B0 Homogeneity: 82.7 Hz standard deviation over the brain (0.17 ppm)
- RF Pulse Design: kT-points method for excitations; GRAPE algorithm for refocusing pulses
The safety protocol for human subjects includes comprehensive physiological monitoring, vestibular assessments (to detect potential vertigo or nystagmus), behavioral tests, and genotoxicity evaluation through pre- and post-scan blood samples [2]. These measures have confirmed the feasibility of 90-minute scanning sessions at 11.7T without significant adverse effects.
Preclinical Applications at 11.7T
In parallel with human studies, 11.7T systems are advancing preclinical research through exceptionally high-resolution imaging of animal models and cellular systems. For murine studies, methods for quantitative assessment of brain metabolism have been developed using non-contrast techniques including T2-relaxation-under-spin-tagging (TRUST) and phase-contrast (PC) MRI [26]. These approaches enable measurement of cerebral metabolic rate of oxygen (CMRO2) and cerebral blood flow (CBF) in approximately 20 minutes, providing valuable biomarkers in models of neurodegeneration.
Perhaps even more remarkably, 11.7T MRI has been successfully applied to image 2-mm diameter human brain organoids at isotropic resolutions ≤40 μm, enabling non-invasive, three-dimensional characterization of organoid microstructure without the need for tissue clearing or sectioning [25]. This approach reveals internal organizational features such as rosette-like structures and can even identify specific tissue types through diffusion tractography methods.
Table 3: Key Research Reagents and Resources for Neurodegeneration Research
| Resource Category | Specific Tools | Application and Function |
|---|---|---|
| Imaging Hardware | 11.7T MRI with parallel transmission | Mesoscale human brain imaging; B1+ inhomogeneity mitigation [2] |
| Pulse Sequences | kT-points, GRAPE algorithms | RF pulse design for ultra-high fields [2] |
| Molecular Profiling | SomaScan, Olink platforms | High-dimensional proteomic analysis [23] |
| Data Resources | GNPC dataset, AD Workbench | Access to harmonized proteomic data [23] |
| Cell Models | Human induced pluripotent stem cells (hiPSCs) | Generation of brain organoids for disease modeling [25] |
| Analysis Tools | Diffusion tractography, QSM | Microstructural characterization; iron quantification [25] [12] |
The convergence of ultra-high-field neuroimaging and large-scale molecular profiling represents a paradigm shift in neurodegeneration research. The 11.7T Iseult scanner provides unprecedented access to mesoscopic details of brain anatomy and pathology, revealing features in the cortical ribbon, hippocampal formation, and basal ganglia that were previously inaccessible in living humans [2] [3]. Concurrently, proteomic consortia like the GNPC are identifying robust molecular signatures that cut across traditional diagnostic boundaries, suggesting shared pathways in seemingly distinct neurodegenerative conditions [23].
Looking forward, several strategic priorities emerge for maximizing the impact of these technologies. First, the development of motion correction tools and highly accelerated acquisition sequences will be essential for pushing spatial resolution further while maintaining practical scan times [2]. Second, the implementation of more efficient RF coils with higher channel counts will improve both transmit efficiency and receive sensitivity [2] [25]. Third, the creation of standardized protocols for multi-modal data integration will enable researchers to fully leverage the complementary strengths of imaging and molecular biomarkers.
For researchers focusing on Alzheimer's and Parkinson's diseases, these technological advances offer concrete pathways toward improved early detection, disease subtyping, and therapeutic monitoring. The ability to visualize neurodegenerative processes at mesoscopic scales, combined with deep molecular profiling, promises to bridge the critical gap between neuropathological findings and clinical manifestations. This multi-scale approach will undoubtedly accelerate the development of targeted interventions for these devastating conditions, ultimately fulfilling the promise of personalized medicine in neurodegeneration.
Glioblastoma (GBM) is the most prevalent and lethal primary malignant brain tumor, characterized by its highly infiltrative nature. A critical challenge in its management is that tumor cells extend into the surrounding brain parenchyma beyond the margins of the visible lesion, leading to inevitable recurrence despite aggressive treatment. The presence of the blood-brain barrier (BBB) further complicates therapeutic efficacy by hindering drug delivery, particularly to these infiltrative zones [27] [28]. In clinical neuro-oncology, accurately delineating tumor infiltration is therefore paramount for surgical planning, radiation targeting, and treatment monitoring.
The advent of ultra-high-field (UHF) Magnetic Resonance Imaging (MRI), particularly at 11.7 Tesla (T), represents a paradigm shift in neuroimaging. Operating at a magnetic field strength nearly four times that of common clinical 3T scanners, 11.7T MRI offers a supralinear gain in signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR). This enhanced sensitivity enables imaging at a mesoscopic spatial resolution (~0.2 mm in-plane), revealing anatomical details and microstructural changes that are invisible at lower field strengths [2] [13]. For glioblastoma, this provides a powerful, non-invasive tool to probe the tumor microenvironment and its impact on the healthy tissue. The Iseult 11.7T MRI scanner, a landmark achievement by the French Atomic Energy Commission (CEA), has successfully demonstrated the safety and feasibility of in vivo human brain imaging, confirming that humans can tolerate 1.5-hour scans at this intense magnetic field without significant physiological, vestibular, behavioral, or genotoxic effects [2] [6]. This technical leap opens a new window of opportunity to explore brain pathology in unprecedented detail, positioning 11.7T diffusion tensor imaging (DTI) as a front-runner in the quest to visualize and understand glioblastoma infiltration.
The 11.7T Advantage: Technical Principles of DTI at Ultra-High Field
Diffusion Tensor Imaging (DTI) is an MRI technique that measures the direction and magnitude of water molecule diffusion in biological tissues. In highly structured tissues like white matter, water diffusion is anisotropic, meaning it is restricted across fibers but facilitated along them. DTI models this directional dependence to reconstruct 3D fiber tracts and quantify microstructural integrity through various metrics [27].
The fundamental parameters derived from DTI include:
- Fractional Anisotropy (FA): A scalar value between 0 and 1 that reflects the degree of directional preference of diffusion. A decrease in FA often indicates a loss of microstructural organization.
- Mean Diffusivity (MD): The average rate of diffusion in all directions, sensitive to cellular density and edema.
- Axial Diffusivity (AD): The rate of diffusion along the primary axis of the fiber.
- Radial Diffusivity (RD): The rate of diffusion perpendicular to the primary axis, which increases with demyelination or axonal damage.
At ultra-high magnetic fields, the physics of MRI changes favorably. The signal-to-noise ratio (SNR) increases approximately linearly with field strength, which can be directly invested to achieve higher spatial resolution, revealing finer anatomical details within the cortical ribbon and white matter pathways [2]. Furthermore, the magnetic susceptibility effect, which is the basis for T2*-weighted contrast, is heightened at 11.7T. This enhances the sensitivity of DTI to subtle micro-architectural changes, such as those caused by tumor cells displacing or disrupting healthy white matter tracts [29]. While challenges like increased radiofrequency field inhomogeneity exist, they can be mitigated with advanced technologies like parallel transmission and dedicated pulse design algorithms [2] [8]. This combination of superior SNR and enhanced contrast makes 11.7T DTI uniquely capable of detecting the elusive borders of glioblastoma infiltration.
Experimental Validation: A Post-Mortem 11.7T DTI Study
A seminal study by van den Elshout et al. (2025) provides crucial histological validation for the use of 11.7T DTI in detecting glioblastoma infiltration. This research directly correlated ex vivo DTI metrics from post-mortem GBM specimens with gold-standard histological and polarized light imaging (PLI) data, establishing a direct link between imaging findings and tissue pathology [29] [30].
Detailed Experimental Methodology
The experimental protocol was designed to ensure a rigorous, multi-modal correlation.
- Sample Preparation: Three post-mortem human brain specimens with a confirmed pathological diagnosis of glioblastoma were obtained. The samples were fixed and prepared for ex vivo MRI to preserve tissue integrity and minimize post-mortem artifacts.
- 11.7T DTI Acquisition: Imaging was performed on an 11.7T MRI scanner. The DTI sequence was optimized for ex vivo tissue to derive high-resolution maps of FA, MD, AD, and RD. The high field strength was critical for achieving the SNR necessary for robust tensor calculation at a fine spatial scale.
- Histological Correlation: Following MRI, the brain specimens were sectioned and stained for detailed pathological analysis.
- Hematoxylin and Eosin (H&E): Provided a general assessment of cellularity and cytoarchitecture.
- Luxol Fast Blue (LFB): A specific stain for myelin, used to evaluate myeloarchitectural integrity.
- Polarized Light Imaging (PLI): This technique was used to generate high-resolution fiber orientation maps in the brain sections, offering a direct measure of fiber architecture and disruption independent of DTI [29].
- Data Analysis: Regions of interest (ROIs) were defined for "Normal White Matter (NWM)" and "Tumor Infiltration" based on the H&E-stained nucleus density maps. The DTI metrics (FA, MD, AD, RD), LFB optical density, and PLI retardance values were extracted from these corresponding ROIs for statistical comparison using correlation analyses [29] [30].
Table 1: Key Statistical Results from the Post-Mortem Validation Study
| Metric | Finding in Tumor Infiltration vs. Normal White Matter | P-value | Biological Interpretation |
|---|---|---|---|
| Mean Diffusivity (MD) | Significant Increase | 0.036 | Increased water mobility due to disrupted tissue structure and edema. |
| Radial Diffusivity (RD) | Significant Increase | 0.010 | Loss of restricting barriers (e.g., myelin) perpendicular to axons. |
| Fractional Anisotropy (FA) | Not Significantly Different | - | Suggests overall directionality may be preserved despite infiltration. |
| Axial Diffusivity (AD) | Not Significantly Different | - | Primary diffusion direction along fibers may be less affected. |
| LFB Staining | Significant Decrease | 0.007 | Direct evidence of myelin loss or severe disruption in infiltrated zones. |
| PLI Retardance | Significant Decrease | <0.001 | Confirmation of microstructural fiber displacement and disorganization. |
Interpretation of Findings and Workflow
The core finding of this study is that 11.7T DTI can detect significant microstructural alterations in regions of glioblastoma infiltration, and these changes are primarily driven by myeloarchitectural alterations, such as fiber displacement and demyelination, rather than a simple increase in cellularity. The strong correlation between the DTI metrics (MD, RD) and the validated myelin-sensitive techniques (LFB, PLI) confirms that DTI at this field strength is exquisitely sensitive to the tumor's destructive impact on white matter organization [29]. The following workflow diagram illustrates the integrated experimental pipeline used in this validation study.
Beyond DTI: Multiparametric MRI and Metabolomic Correlations at 11.7T
While DTI provides powerful microstructural information, the full potential of 11.7T is realized through a multiparametric approach that integrates complementary imaging and spectroscopic techniques. This holistic view can offer a more comprehensive characterization of the tumor and its microenvironment.
- Relaxometry and Magnetization Transfer: Parameters derived from T1, T2, and T2* mapping, as well as the magnetization transfer ratio (MTR), provide insights into inflammation, vasogenic edema, hemorrhage, neoangiogenesis, and cellularity. Studies on GBM rat models have shown significant differences in T2, T1, and MTR between tumor regions and healthy tissue, serving as potential biomarkers for treatment response and disease progression [27].
- MR Spectroscopy (MRS) and Metabolomics: A key advantage of 11.7T is the enhanced resolution for spectroscopy. Ex vivo High-Resolution Magic Angle Spinning (HR-MAS) MRS, performed at 11.7T, can identify a wide range of metabolites from small tissue samples. In glioblastoma research, the ratio of Myo-inositol to total Choline (MCI) has been identified as a highly sensitive marker able to differentiate tumor from treatment-induced reactive astrocytosis with a sensitivity of 93% in recurrent GBM [31]. Furthermore, studies have noted elevated levels of myo-inositol and phosphocholine not only in the tumor core but also in contralateral, seemingly healthy regions of GBM models, suggesting a metabolomic impact of the tumor on distant tissue [27].
Table 2: Research Reagent Solutions for 11.7T GBM Research
| Reagent / Material | Function in Experimental Protocol |
|---|---|
| Luxol Fast Blue (LFB) | Histological stain used to validate myelin content and assess myeloarchitectural integrity against DTI findings [29]. |
| Hematoxylin and Eosin (H&E) | Standard histological stain for general tissue morphology and nucleus density mapping to define regions of interest [29]. |
| Glial Fibrillary Acidic Protein (GFAP) Antibody | Immunohistochemical marker for astrocytes; used to differentiate reactive astrocytosis (treatment effect) from tumor cells [31]. |
| Parallel Transmission (pTx) RF Coil | Advanced hardware to mitigate radiofrequency field inhomogeneity at 500 MHz (11.7T), enabling uniform signal across the human brain [2]. |
| Virtual Observation Points (VOPs) | Software-based safety system for Specific Absorption Rate (SAR) monitoring, ensuring compliance with safety limits during high-power 11.7T scans [2]. |
| Evans Blue / Gadolinium-DOTA | Contrast agents for validating blood-brain barrier permeability in preclinical models (Evans Blue for histology, Gd-DOTA for DCE-MRI) [28]. |
Future Directions and Clinical Translation Pathways
The application of 11.7T DTI and multiparametric MRI in glioblastoma research is still in its early stages, but the future directions are clear and promising. The immediate next steps involve the development and implementation of motion correction tools and highly accelerated acquisition sequences to improve image quality and efficiency for in vivo studies [2] [13]. Furthermore, the deployment of more efficient RF coils with higher channel counts and more powerful gradients is underway, which will further boost performance for high-resolution functional MRI and advanced diffusion imaging [2].
A critical frontier is the move towards integrative analytics, where DTI metrics are combined with metabolomic profiles from MRS, perfusion data, and genetic information to create powerful predictive models. This could lead to the development of non-invasive imaging biomarkers for specific genetic subtypes of GBM, early treatment response assessment, and the differentiation of true tumor progression from pseudoprogression or radiation necrosis [31] [27]. Techniques like Chemical Exchange Saturation Transfer (CEST) are also being actively explored at 11.7T, offering potential for pH mapping and imaging of metabolites like glutamate and glycogen [8].
The path to widespread clinical adoption faces challenges, primarily related to the high cost and specialized infrastructure required for 11.7T systems, including massive magnets and complex cryogenic plants [6]. For the foreseeable future, these systems will likely remain in specialized research centers. However, the knowledge gained from 11.7T research will be invaluable. It can be translated downward to improve protocols and data analysis methods for more widely available 3T and 7T clinical scanners, ultimately refining surgical planning, radiation targeting, and clinical decision-making for glioblastoma patients across the healthcare system.
A significant challenge in modern epilepsy research and treatment is the cohort of patients with drug-resistant focal epilepsy for whom no clear structural cause can be identified using conventional magnetic resonance imaging (MRI). Studies indicate that approximately 15-40% of patients with refractory epilepsy remain undiagnosed after undergoing conventional 1.5 Tesla (T) and 3T MRI scans [6]. This diagnostic gap frequently occurs because subtle cortical malformations, such as focal cortical dysplasia (FCD) type I, small cavernomas, or microscopic dysplastic features within low-grade glioneuronal tumors, often escape detection due to their minimal size and subtle appearance at standard clinical field strengths [32] [6]. These "MRI-negative" cases present a substantial obstacle for surgical planning, as defining the epileptogenic zone without a clear structural correlate reduces the likelihood of a seizure-free postoperative outcome.
Ultra-high field (UHF) MRI, defined as systems with magnetic field strengths ≥7T, represents a transformative technological advancement with the potential to bridge this diagnostic gap. The recent development and deployment of 11.7T human MRI systems, such as the Iseult CEA machine, mark a significant leap forward, offering unprecedented spatial resolution and signal-to-noise ratios (SNR) that enable researchers and clinicians to visualize the brain's microstructure in hitherto impossible detail [6]. This technical guide explores how these advancements are refining our understanding of epileptogenic networks and paving the way for more precise interventions in epilepsy research and therapy development.
Technical Advantages of Ultra-High Field MRI in Cortical Imaging
The fundamental benefits of increasing magnetic field strength for neuroimaging are rooted in physics. The signal-to-noise ratio (SNR) increases approximately linearly with field strength, which can be leveraged to achieve higher spatial resolution, improved contrast-to-noise ratio (CNR), or a combination of both [32] [6]. At 11.7T, this translates to an ability to resolve anatomical details at a submillimeter level, which is critical for visualizing the intricate laminar structure of the cerebral cortex and identifying subtle malformations that disrupt it.
Table 1: Quantitative Comparison of MRI Field Strengths for Brain Imaging
| Parameter | 3 Tesla (T) | 7 Tesla (T) | 11.7 Tesla (T) |
|---|---|---|---|
| Typical In-Plane Resolution | ~1.0 mm | ~0.15 - 0.5 mm [32] | ~0.19 mm [6] |
| Signal-to-Noise Ratio (SNR) | Baseline | ~2x higher than 3T | Vastly higher than 3T/7T [6] |
| Clinical Diagnostic Gain in Epilepsy | Standard of care | 18-67% added diagnostic gain in focal epilepsy [32] | Potential for further identification of elusive lesions [6] |
| Key Advantages | Wide clinical availability | Superior lesion conspicuity, gray-white matter differentiation [32] | Submillimeter resolution, potential for tracking metabolites like lithium [6] |
The enhanced gray-white matter tissue-contrast differentiation at UHF provides unparalleled clarity of the cortical ribbon, allowing researchers to detect blurring of the gray-white junction—a key hallmark of FCD [32]. Furthermore, the higher spatial resolution reduces partial volume effects, enabling more precise delineation of a malformation's boundaries and its relationship to functional brain areas, which is paramount for planning targeted interventions [32] [33].
Key UHF MRI Applications in Epilepsy Research
Visualizing Specific Epileptogenic Pathologies
UHF MRI demonstrates particular efficacy in characterizing a spectrum of lesions commonly associated with drug-resistant epilepsy. Dysembryoplastic neuroepithelial tumors (DNETs), for instance, exhibit a characteristic "soap-bubble" multicystic appearance on MRI. At 7T, the increased in-plane resolution up to 0.15 x 0.15 mm² provides exquisite detail of this internal architecture and allows for superior visualization of any dysplastic cortex at the tumor's edges, which is a critical factor in its epileptogenicity [32]. The 11.7T scanner is anticipated to push this characterization even further, potentially revealing histopathological correlations non-invasively [6].
For focal cortical dysplasia (FCD), the most common malformation diagnosed in patients with drug-resistant epilepsy, UHF MRI offers a significant diagnostic advantage. The improved SNR and CNR at 7T have been shown to improve the detection of FCDs, particularly those that are subtle or occult at lower fields [32]. The 11.7T platform, with its superior resolution, holds the promise of identifying even more elusive FCD variants and other subtle malformations like tuberous sclerosis complex abnormalities and gangliogliomas [6].
Advancing Metabolic and Functional Imaging
Beyond structural anatomy, UHF MRI profoundly benefits magnetic resonance spectroscopic imaging (MRSI) and functional MRI (fMRI). MRSI at 7T and above offers enhanced spectral resolution, allowing researchers to separate overlapping metabolite resonances and detect changes in neurometabolites like gamma-aminobutyric acid (GABA), glutamate, and lactate with greater accuracy [34]. This capability is crucial for investigating the neurochemical basis of epileptogenicity and assessing treatment responses. The Iseult 11.7T scanner may enable non-invasive measurement of lactate-to-pyruvate ratios, which could serve as a biomarker for hypermetabolic or injured brain tissue in the epileptic focus [6].
Similarly, fMRI at UHF provides enhanced sensitivity for mapping brain function. Researchers can localize critical functional areas, such as the primary motor or language cortex, with higher precision relative to a seizure onset zone. This is vital for designing surgical strategies that maximize resection of the epileptogenic lesion while minimizing the risk of postoperative neurological deficits [32] [35].
Experimental Protocols for UHF MRI in Epilepsy Research
Structural Imaging Protocol for Malformation Detection
A comprehensive UHF MRI protocol for epilepsy research integrates multiple sequences to maximize sensitivity to different tissue properties. A standard protocol on a second-generation 7T scanner (e.g., Siemens MAGNETOM Terra.X) or higher should include the following key sequences, optimized for high resolution and contrast [32] [33]:
- T1-Weighted 3D MP2RAGE (Magnetization Prepared 2 Rapid Acquisition Gradient Echoes): This sequence provides excellent T1 contrast with minimal sensitivity to B1+ inhomogeneities. It is ideal for cortical surface reconstruction and volumetric analysis. Example parameters at 9.4T include: isotropic voxel size of 0.6 - 0.8 mm³, TR/TI1/TI2 optimized for GM/WM contrast, and parallel imaging acceleration (GRAPPA) to manage acquisition time [33].
- T2-Weighted 3D FLAIR (Fluid Attenuated Inversion Recovery) SPACE (Sampling Perfection with Application optimized Contrasts using different flip angle Evolution): This sequence is highly sensitive to cortical hyperintensities and gliotic changes surrounding FCDs. It should be performed with tailored pTx pulses to mitigate B1+ inhomogeneity at UHF [32].
- T2*-Weighted 2D/3D GRE (Gradient Echo): This sequence is highly sensitive to heme products, making it indispensable for detecting cerebral microbleeds or cavernomas associated with epilepsy. It readily benefits from the increased susceptibility contrast at UHF [6].
Table 2: Essential Research Reagents and Materials for UHF Epilepsy Imaging
| Item Name | Function/Explanation |
|---|---|
| Dedicated Multi-Channel RF Coils | A 8Tx/32Rx coil array provides the necessary hardware for parallel transmission (pTx) and high-density signal reception, which is crucial for mitigating artifacts and achieving high SNR [32]. |
| Parallel Transmission (pTx) Pulses | Software-based pulse designs that dynamically shape the RF field to overcome the inherent B1+ inhomogeneity at UHF, ensuring uniform image quality across the entire brain [32]. |
| Diffusion Tensor Imaging (DTI) Post-Processing Software | Enables visualization of white matter tract displacement or infiltration by a lesion (e.g., DNET), which is critical for surgical planning and understanding network disruption [32]. |
| Validated Manual Segmentation Protocols | Gold-standard manual segmentations of cortical structures (e.g., from the UltraCortex repository) are essential for validating and training new automated algorithms to handle UHF data [33]. |
| B0 Shimming Algorithms | Advanced shimming techniques are required to correct for magnetic field inhomogeneities, which are more pronounced at higher field strengths and can cause image distortion [33]. |
Data Processing and Analysis Workflow
The analysis of UHF MRI data requires specialized pipelines to handle the high-resolution data and extract meaningful information. The workflow below outlines the key steps from data acquisition to the final identification of a cortical malformation.
Key steps in this workflow include:
- Data Preprocessing: Critical steps include B0 and B1+ inhomogeneity correction to address UHF-specific artifacts, gradient distortion correction, and anonymization of data for sharing or ethical review [32] [33].
- Multi-Modal Segmentation: High-resolution T1-weighted images (e.g., from MP2RAGE) are used to manually or semi-automatically segment the brain into gray matter, white matter, and cerebrospinal fluid. This process is greatly enhanced by using manually validated segmentations as a gold standard for algorithm training [33].
- Tractography Analysis: Diffusion tensor imaging (DTI) data are processed to reconstruct white matter fibers. This allows researchers to determine whether a lesion is displacing or infiltrating critical pathways, such as the arcuate fasciculus near a frontoinsular DNET [32].
- Multi-Parametric Integration and Identification: Data from all sequences and analyses are fused to create a comprehensive profile of the suspected malformation, correlating its structural appearance, metabolic profile (from MRSI), and relationship to functional and connective anatomy [32] [34].
The advent of ultra-high field MRI, particularly the groundbreaking 11.7T technology, is poised to revolutionize epilepsy research. By providing an unprecedented view of the brain's microstructure and metabolism, UHF MRI empowers scientists to uncover the subtle cortical malformations that have long eluded conventional imaging. This capability is fundamental to transitioning patients from the "MRI-negative" to the "MRI-positive" category, thereby opening doors to more targeted surgical and pharmacological interventions. As UHF MRI technology continues to evolve and become more accessible, its integration into large-scale research studies will undoubtedly accelerate the development of new biomarkers and therapeutic strategies, ultimately improving outcomes for individuals with drug-resistant epilepsy.
Ultra-high-field magnetic resonance imaging (MRI) represents a transformative tool in neuroscience, enabling the non-invasive exploration of neural architecture at a mesoscopic scale. The recent development and deployment of 11.7 tesla (T) MRI systems, such as the Iseult scanner, have facilitated the acquisition of human brain images with unprecedented resolution in vivo, revealing details within the cortical ribbon that are not visible at lower field strengths [2] [6]. This technological leap forward has profound implications for preclinical research, particularly in the realm of human brain organoids. These three-dimensional cellular models, which mimic the architectural features of a developing brain, are generated from human induced pluripotent stem cells and offer a physiologically relevant in vitro system for disease modeling and drug screening [14]. The integration of ultra-high-field MRI with brain organoid research creates a powerful, label-free platform for deep tissue imaging, allowing researchers to probe microstructure and neuronal organization without the need for physical sectioning or tissue clearing. This guide details the application of 11.7T diffusion MRI for the analysis of brain organoids, providing a comprehensive technical framework for researchers and drug development professionals seeking to leverage this cutting-edge methodology.
The 11.7T MRI Landscape: Technical Specifications and Capabilities
The Iseult 11.7T MRI scanner is the product of nearly two decades of research and development. Its key technical achievement is an immense, stable magnetic field that provides a substantial gain in signal-to-noise ratio (SNR) compared to clinical and other research-grade systems [2] [3].
System Specifications
The physical and technical requirements for an 11.7T system are extraordinary, as summarized in Table 1.
Table 1: Key Specifications of the Iseult 11.7T MRI System
| Parameter | Specification | Significance |
|---|---|---|
| Magnetic Field Strength | 11.7 T | Highest magnetic field used for human MRI; enables mesoscale resolution [2]. |
| Magnet Weight | 132 tons | Requires specialized infrastructure and installation [2] [6]. |
| Cooling System | 7,000-7,500 L of superfluid helium at 1.8 K | Essential for maintaining superconducting state; complex cryogenic management [2] [6]. |
| Superconducting Wire | 182 km | Enables generation of the intense magnetic field [6]. |
| Field Homogeneity | 0.9 ppm peak-to-peak over a 22-cm-diameter sphere | Critical for achieving high-quality, artifact-free images [2]. |
| Exemplary Resolution | 0.19 x 0.19 x 1 mm³ in 4 min 17 sec (in vivo) | Demonstrates the high-speed, high-resolution imaging capability impractical at lower fields [2] [6]. |
Overcoming High-Field Imaging Challenges
Operating at 11.7 T presents unique engineering and safety challenges that must be mitigated for successful application:
- Radiofrequency (RF) Field Inhomogeneity: The shorter wavelength of the 500 MHz RF field at 11.7 T causes severe signal variations. This is tackled using parallel transmission (pTx) hardware and software with dedicated pulse design algorithms [2].
- Specific Absorption Rate (SAR): The energy deposited in tissue increases with field strength. SAR is controlled using virtual observation points and advanced RF pulse design [2].
- Safety and Tolerability: Initial studies on 20 healthy volunteers exposed to the 11.7 T field for 1.5 hours showed no significant adverse physiological, vestibular, behavioral, or genotoxic effects, establishing its safety for human research [2] [24].
High-Resolution Imaging of Brain Organoids: An Experimental Framework
The translation of 11.7T MRI from in vivo human imaging to in vitro brain organoid analysis is a recent and promising development. A proof-of-concept study has demonstrated the feasibility of using 11.7T diffusion MRI microscopy to image 2-mm diameter spherical human brain organoids, providing a 3D view of organoid microstructure at ≤40 μm isotropic resolution [14].
Experimental Objectives and Workflow
The primary objective is to perform non-invasive, label-free characterization of whole brain organoids to assess their internal microstructure and model features of neuronal organization. The general workflow for this process is outlined in Figure 1 below.
Figure 1: Experimental workflow for 11.7T MRI of human brain organoids.
Detailed Methodologies for Key Experiments
Organoid Preparation and Imaging
- Organoid Generation: Brain organoids are derived from human induced pluripotent stem cells (iPSCs) using established differentiation protocols for specific brain regions, such as the hippocampus [14].
- MRI Preparation: Fixed or live organoids are prepared for imaging. For fixed samples, they are typically embedded in a suitable medium and placed in a compatible MRI-compatible tube or container designed for high-resolution microimaging systems.
- Image Acquisition: Data is collected using a preclinical 11.7T Bruker/89 mm microimaging system (or equivalent). The key acquisition parameters from the foundational study are detailed in Table 2.
Table 2: Quantitative Data from 11.7T Brain Organoid Imaging
| Imaging Metric | Performance Value / Detail | Experimental Significance |
|---|---|---|
| Isotropic Resolution | ≤40 μm | Provides a 3D view of organoid microstructure without physical sectioning [14]. |
| Imaging Technique | Multishell 3D Diffusion Imaging | Enables derivation of microstructural information and tractography [14]. |
| Correlative Technique | Immunofluorescence Microscopy | Validates MRI-identified features (e.g., rosette-like structures, choroid plexus) [14]. |
| Key Identified Structure | Protruding spherical structure correlated with choroid plexus | Demonstrates the ability to identify distinct anatomical regions within organoids [14]. |
| Primary Advantage | Label-free, deep-tissue imaging without tissue clearing | Complements and extends traditional histology, preserving sample integrity [14]. |
Data Processing and Tractography
Following acquisition, 3D diffusion data is processed to model tissue microstructural features. Tractography methods are then applied to map potential neuronal organization and streamlines within the organoid, inferring structural connectivity patterns from the diffusion of water molecules [14].
The Scientist's Toolkit: Essential Research Reagents and Materials
Success in this specialized field relies on a suite of sophisticated reagents and hardware. Table 3 lists the essential components of the experimental toolkit.
Table 3: Research Reagent Solutions for 11.7T Organoid Imaging
| Item | Function / Role | Specific Examples / Notes |
|---|---|---|
| Human Induced Pluripotent Stem Cells (iPSCs) | Cellular starting material for generating physiologically relevant brain organoids. | Critical for patient-specific disease modeling [14]. |
| Brain Organoid Culture Kits | Provide standardized reagents and protocols for directed differentiation of iPSCs into brain organoids. | Ensures reproducibility in generating hippocampal or cortical organoids [14]. |
| 11.7T Preclinical MRI System | High-field magnet system that provides the necessary signal-to-noise for micron-scale resolution. | E.g., 11.7T Bruker/89 mm microimaging system [14]. |
| Diffusion MRI Sequence Software | Customized pulse sequences for acquiring multishell 3D diffusion-weighted images. | Essential for probing tissue microstructure and enabling tractography [14]. |
| Parallel Transmission (pTx) Coil | RF coil hardware to mitigate B1+ field inhomogeneity at ultra-high fields. | A home-made pTx coil with 16 transmit elements was used for the Iseult scanner [2]. |
| Tractography & Processing Software | Computational tools for reconstructing neuronal streamlines from diffusion MRI data. | Used to model tissue microstructural features and map neuronal organization [14]. |
| Immunofluorescence Staining Reagents | Antibodies and labels for post-MRI histological validation of identified structures. | Validates MRI findings, e.g., staining for choroid plexus markers [14]. |
Applications in Drug Discovery and Development
The integration of high-resolution organoid imaging into the drug development pipeline holds the potential to de-risk and accelerate the discovery of new therapeutics for intractable neurological and psychiatric disorders.
Disease Modeling and Phenotypic Screening
Brain organoids can model a wide range of conditions, including psychiatric disorders, neurodegenerative diseases, and viral infections [14]. The 11.7T MRI platform allows for the longitudinal monitoring of these models to identify specific microstructural phenotypes associated with disease. For instance, it can detect differentiating rosette-like structures and other organizational anomalies that may serve as quantitative biomarkers for high-throughput compound screening [14]. This is particularly valuable in psychiatry, where the lack of clear biological mechanisms and the high failure rate of new drugs necessitate new tools for phenotypic screening [36].
Assessing Neurotoxicity and Treatment Efficacy
A key application is the objective assessment of neurotoxicity during drug safety screening. Changes in organoid microstructure, as revealed by diffusion MRI and tractography, can provide an early, sensitive readout of a compound's detrimental effects on developing neural networks [14]. Conversely, this platform can be used to evaluate the efficacy of novel therapeutic compounds by monitoring the restoration of normal microstructural features in diseased organoid models.
The application of 11.7T MRI to human brain organoids represents a powerful convergence of bioengineering, neuroscience, and imaging physics. This label-free approach provides a deep-tissue, three-dimensional window into the microstructure of these complex models, complementing and extending the capabilities of traditional destructive imaging methods.
The future of this field is bright. Ongoing technical developments, including the implementation of more efficient RF coils, higher channel count receivers, and motion correction tools, will further boost performance [2]. This will pave the way for functional MRI (fMRI) and advanced diffusion tensor imaging of organoids, allowing researchers to probe not just structure, but also function and connectivity [2]. As the technology matures, its role in validating organoid models and providing robust, quantitative endpoints for drug discovery will become increasingly central.
In conclusion, the union of ultra-high-field MRI and brain organoid technology creates a unique preclinical platform poised to make a significant impact on our understanding of brain development and disease, ultimately accelerating the development of new therapeutics for neurological and psychiatric disorders. By providing unprecedented views into the miniature worlds of brain organoids, 11.7T MRI helps ensure that these models fulfill their promise as faithful replicas of the human brain.
The non-invasive tracking of metabolites such as lithium, glutamate, and other neurochemicals represents a frontier in understanding brain function and developing treatments for neurological disorders. The advent of ultra-high-field magnetic resonance imaging, particularly at 11.7 Tesla, is poised to revolutionize this domain by providing unprecedented spatial resolution and spectral specificity. This technical guide explores the transformative potential of 11.7T MRI for neuroscience research and drug development, focusing on the methodologies enabling the detection and quantification of key metabolites that have previously eluded precise non-invasive measurement.
The fundamental advantage of ultra-high-field MRI stems from a supralinear gain in signal-to-noise ratio with increasing magnetic field strength. Research indicates that SNR increases as B0^1.65 to B0^1.94±0.16, far exceeding linear improvement [2] [37]. This enhanced sensitivity can be invested into higher spatial resolution, pushing imaging toward the mesoscopic scale—the critical level bridging microscopic neuronal circuits and macroscopic brain regions [2] [37]. Furthermore, increased field strength provides greater spectral separation for distinguishing metabolites with similar chemical structures, thereby enabling precise tracking of neurotransmitters, energy substrates, and pharmaceutical agents like lithium within the living human brain [38] [37].
Technical Advantages of 11.7T MRI for Metabolic Research
Signal and Resolution Capabilities
The Iseult 11.7T MRI system demonstrates remarkable imaging capabilities, achieving resolutions of 0.19 × 0.19 × 1 mm³ within acquisition times of approximately five minutes [2] [6]. This represents a significant advancement over conventional 3T and 7T systems, which would require substantially longer scan times to achieve comparable resolution, making such protocols impractical for clinical or research settings [6]. The system's enhanced resolution reveals anatomical details within the cortical ribbon and cerebellar structures that remain obscured at lower field strengths due to poorer spatial resolution [2].
Table 1: Comparison of MRI System Performance Characteristics
| Parameter | 3T MRI | 7T MRI | 11.7T MRI |
|---|---|---|---|
| Typical In-Plane Resolution | ~1.0 mm | ~0.7 mm | ~0.19 mm |
| Approximate Scan Time for Equivalent SNR | Baseline | ~4x faster than 3T | ~15x faster than 3T |
| Spectral Resolution | Standard | Improved | Superior |
| BOLD Contrast Sensitivity | Baseline | ~2x 3T | Further enhanced |
Multinuclear Spectroscopy and Spectral Resolution
Ultra-high-field MRI dramatically improves magnetic resonance spectroscopy capabilities. While clinical field strengths (≤3T) can reliably quantify only highly abundant metabolites such as total N-acetylaspartate and creatine, 11.7T enables detection of physiologically low-abundant metabolites including glutamate, glutamine, GABA, glutathione, and beta-hydroxybutyrate [38]. The enhanced spectral separation at 500 MHz (the resonant frequency for hydrogen nuclei at 11.7T) facilitates differentiation of closely overlapping metabolite peaks that are convolved at lower fields [38] [37].
Moreover, 11.7T systems provide sufficient sensitivity for X-nuclei MRS, enabling research on metabolically relevant nuclei such as ^13^C, ^2^H, ^17^O, and ^31^P [38] [37]. These nuclei offer unique insights into cerebral metabolic fluxes but are challenging to study at lower fields due to inherent low NMR sensitivity and natural abundance. For instance, ^31^P MRS can assess energy compounds like ATP and phosphocreatine, while ^13^C MRS with labeled substrates can track neurotransmitter cycling and energy metabolism in neuronal and glial compartments [38].
Key Metabolite Targets and Biomarker Potential
Lithium and Glutamate: Pathophysiological Significance
Lithium remains a cornerstone treatment for bipolar disorder, yet its therapeutic mechanisms are not fully understood, and monitoring brain concentrations currently requires invasive approaches. The enhanced spectral resolution at 11.7T may enable non-invasive lithium tracking, potentially revealing its distribution and pharmacokinetics in the human brain [6]. Similarly, glutamate, the primary excitatory neurotransmitter, plays critical roles in numerous neurological and psychiatric disorders, but its precise dynamics have been difficult to quantify in vivo.
Table 2: Key Metabolites Detectable with Ultra-High-Field MRS
| Metabolite | Biological Significance | Associated Disorders |
|---|---|---|
| Lithium | Mood stabilizer | Bipolar disorder |
| Glutamate (Glu) | Major excitatory neurotransmitter | Epilepsy, schizophrenia, depression |
| Gamma-Aminobutyric Acid (GABA) | Major inhibitory neurotransmitter | Anxiety, epilepsy, schizophrenia |
| Lactate | Energy substrate, hypoxia marker | Stroke, tumors, metabolic disorders |
| N-Acetylaspartate (NAA) | Neuronal integrity marker | Neurodegenerative diseases, injury |
| Glutathione (GSH) | Antioxidant | Neurodegenerative diseases, aging |
Metabolic Biomarkers for Specific Disorders
The 11.7T MRI technology enables investigation of metabolic alterations across a spectrum of neurological conditions. In Alzheimer's disease, researchers can track cerebral hypometabolism through altered oxygen extraction fraction and cerebral metabolic rate of oxygen, potentially identifying early biomarkers before structural changes occur [39]. For multiple sclerosis, the enhanced resolution enables visualization of cortical lesions and venous structures that correlate with disease progression [2] [6]. In epilepsy, previously undetectable focal cortical dysplasias become visible at 11.7T, potentially revealing seizure-onset zones in medically refractory cases [6] [40].
Experimental Methodologies and Technical Protocols
Parallel Transmission for Field Homogeneity
A significant technical challenge at 11.7T is the inherent inhomogeneity of the radiofrequency field caused by the shortened wavelength of RF waves at 500 MHz. The Iseult project addressed this through parallel transmission tools with dedicated virtual observation points for specific absorption rate monitoring [2]. This approach achieved normalized root mean square errors of approximately 8% for small flip angle excitations and 13% for large flip angle refocusing pulses over the whole brain—comparable to the intrinsic inhomogeneity achieved at 3T with volume coils [2].
Safety and Physiological Monitoring Protocols
Before human imaging, extensive safety validation was conducted. The initial protocol exposed 20 healthy adult volunteers to 90-minute scans at 11.7T, with comprehensive physiological, vestibular, behavioral, and genotoxicity measurements [2] [24]. A control group of 20 participants underwent identical testing with the magnetic field switched off (but with simulated MRI sounds to maintain blinding). Statistical analysis revealed no significant differences between groups across all measured parameters, establishing the safety and tolerability of 11.7T imaging for human subjects [2] [24].
Advanced Metabolic Imaging Techniques
Chemical Exchange Saturation Transfer (CEST) MRI presents a promising approach for monitoring metabolic activity. Studies at 7T have demonstrated that glucosamine, a safe dietary supplement, can be detected using CEST after intravenous administration, showing significant signal elevation in cortical regions, hippocampus, and thalamus [41]. The signal remains stable for over 40 minutes, attributed to glucosamine uptake and metabolic product accumulation, as confirmed by ^13^C NMR spectroscopy of brain extracts [41]. Multi-pool Lorentzian fitting of Z-spectra reveals increases in hydroxyl, amide, and relayed nuclear Overhauser effect signal components following glucosamine administration [41].
High-Resolution Diffusion and Functional Imaging
Beyond spectroscopy, 11.7T enables advanced microstructural imaging. Proof-of-concept studies using 11.7T diffusion MRI microscopy have achieved 40 μm isotropic resolution in human brain organoids, revealing rosette-like internal structures and enabling tractography modeling of neuronal organization [25]. This approach complements traditional immunohistochemistry without requiring tissue clearing, preserving native tissue architecture [25]. For functional imaging, the enhanced sensitivity to magnetic susceptibility differences improves blood-oxygenation-level-dependent contrast, potentially revealing previously unrecognized nodes in functional networks with greater specificity to microvascular contributions [40] [37].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagent Solutions for 11.7T Metabolic Imaging
| Reagent/Material | Function | Application Example |
|---|---|---|
| Parallel Transmission RF Coil | Mitigates B1+ field inhomogeneity | Human brain imaging at 11.7T [2] |
| Virtual Observation Points | Monitors and controls specific absorption rate | Safety assurance in human subjects [2] |
| Glucosamine-based Probes | CEST-detectable metabolic tracer | Brain metabolism mapping [41] |
| ^13^C-labeled Substrates | Enables tracking of metabolic fluxes | Cerebral metabolism studies [38] |
| Customized Sample Holders | Stabilizes delicate specimens without deformation | Brain organoid imaging [25] |
| Superfluid Helium Cooling System | Maintains magnet at 1.8 K for superconductivity | 11.7T magnet operation [2] |
Future Directions and Research Applications
The implementation of 11.7T MRI in neuroscience research opens numerous investigative pathways. The technology enables mesoscale resolution to bridge the gap between microscopic knowledge from animal models and the human brain connectome at macroscopic scale [2]. This may confirm or refute current hypotheses regarding brain functioning and generate new ones, particularly for mental illnesses such as depression, autism, and schizophrenia [2].
Specific research applications include:
- Drug-resistant focal epilepsy: Identification of focal cortical dysplasia and mesial temporal sclerosis
- Multiple sclerosis: Characterization of cortical lesions and venous contributions to pathology
- Brain tumors and angiogenesis: Assessment of microvessels, small metastases, and therapeutic responses
- Neurodegenerative disorders: Evaluation of hippocampal status in Alzheimer's disease and iron content in basal ganglia for Parkinson's disease
- Psychiatric therapeutics: Monitoring of lithium distribution in bipolar disorder and neurotransmitter imbalances [2] [6]
The 11.7T MRI technology represents a paradigm shift in metabolic imaging, offering the sensitivity and resolution necessary to track key metabolites like lithium and glutamate in the living human brain. While currently limited to research settings due to infrastructure requirements and costs, this technology provides an unprecedented window into brain metabolism at the mesoscopic scale. As methodological refinements continue and validation studies expand, the biomarkers and insights generated by 11.7T systems are poised to transform our understanding of brain disorders and accelerate the development of targeted therapeutics.
Navigating Technical Challenges: RF Inhomogeneity, SAR, and Operational Hurdles
Mitigating Radiofrequency (B1+) Field Inhomogeneity with Parallel Transmission
The pursuit of ultra-high magnetic field strength for magnetic resonance imaging (MRI), exemplified by the 11.7T (500 MHz) human scanner, is principally driven by the supralinear gain in signal-to-noise ratio (SNR) that enables mesoscale resolution neuroscientific research [42] [2]. However, this promise is challenged by a fundamental physical constraint: the shortening RF wavelength in tissue. At 11.7T, the wavelength becomes comparable to or smaller than the human brain, leading to destructive interference patterns of the electromagnetic field. This phenomenon manifests as severe B1+ field inhomogeneity, causing artifactual signal variations in images and significantly increased local specific absorption rate (SAR), which poses safety concerns [42] [2]. An efficient transmit array is vital in this regime to optimally use the available RF power, achieve efficient excitation, and operate within strict SAR constraints [42]. Parallel Transmission (pTx) has emerged as the pivotal technological solution to these challenges, enabling the mitigation of RF field inhomogeneity and the safe application of 11.7T MRI for groundbreaking neuroscience research.
Fundamental Principles of Parallel Transmission
Parallel Transmission (pTx) fundamentally reimagines RF excitation from a single, uniform source to a multi-channel, spatially diverse system. A pTx system employs an array of independently controllable RF transmit channels, each connected to a separate coil element surrounding the region of interest (e.g., the head). The core principle is that by precisely controlling the amplitude and phase of the RF pulse delivered through each of these channels, one can sculpt the overall excitation profile in space.
This spatial control allows the system to counteract the destructive interference patterns that cause B1+ inhomogeneity. The technical implementation relies on solving an inverse problem: given a desired target flip angle distribution across the brain, the system calculates the complex RF waveforms (magnitude and phase) for each channel that will best approximate this target, while simultaneously adhering to critical hardware (peak and average power) and safety (local SAR) constraints [2]. Advanced RF pulse design algorithms, such as kT-points and the gradient ascent pulse engineering (GRAPE) algorithm, are deployed to solve this problem, enabling homogeneous excitations for small tip angles and accurate refocusing pulses, respectively [2].
Hardware and Coil Design for 11.7T pTx
The hardware platform is the foundation of an effective pTx system. At 11.7T, conventional coil designs face significant loss mechanisms that must be optimized.
Transmit Array Architecture
The design of an 8-channel transmit array for 11.7T, as described by Chu et al., involves rectangular loops arranged on a cylinder. Key design optimizations include:
- Geometric Overlapping: Adjacent elements are overlapped to decouple them passively, minimizing electromagnetic coupling and ensuring independent control of each channel [42].
- Loop Dimensions: The length of the loops along the z-direction is a critical parameter. While a shorter loop (12cm, array-α) achieves a higher peak B1+ in the center, a longer loop (16cm, array-γ) provides a superior coefficient of variation (27.1% vs. 41% in circularly polarized mode) and better overall performance in RF pulse design simulations [42].
- Integrated RF Shield Design: The conventional cylindrical RF shield behaves like a waveguide at 499 MHz, leading to significant power loss (up to 22.5% of accepted power) through radiation. The introduction of a Folded-End Section (FES) shield reduces this radiated power to less than 5.7%, thereby improving the maximum B1+ in the middle of the brain from 1.05 μT to 1.45 μT for 8W total input power [42].
System Specifications
The Iseult 11.7T project utilizes a pTx coil with 16 transmit elements, though these are often paired to be fed by eight high-power RF amplifiers [2]. The necessity for high-power RF amplifiers (2 kW per channel) is underlined by the increased power losses at 500 MHz, which make RF-intensive pulses, like inversion pulses, particularly challenging to design [2].
Table 1: Key Hardware Specifications for 11.7T pTx Systems
| Component | Specification | Purpose/Rationale |
|---|---|---|
| Magnet | 11.7 T (500 MHz for 1H) [2] | Provides the fundamental SNR and contrast gains for neuroscientific research. |
| Transmit Channels | 16 elements (often used in 8 paired channels) [2] | Provides the spatial degrees of freedom needed for B1+ shimming and pTx pulses. |
| RF Amplifiers | 2 kW per channel [2] | Overcomes high power losses at 500 MHz and enables robust inversion/refocusing pulses. |
| Shield Design | Folded-End Section (FES) [42] | Reduces radiated power loss from >22% to <6%, boosting central B1+ by ~38%. |
| Coil Type | Multi-channel transceiver array [42] [2] | Serves for both parallel transmission and reception. |
Core pTx Methodologies and Pulse Design
RF Pulse Design Algorithms
The efficacy of pTx is realized through advanced RF pulse design. The primary algorithms are:
- kT-points: This method is used for designing small tip angle excitation pulses (e.g., 10°). It works by placing a small number of points (e.g., 5-7) in excitation k-space (kT) and optimizing the RF waveforms and accompanying gradients to create a homogeneous flip angle profile across the brain [42] [2]. This approach is highly effective under explicit power and SAR constraints.
- Gradient Ascent Pulse Engineering (GRAPE): The GRAPE algorithm is often used for designing large flip angle refocusing pulses (e.g., 180°). It is a powerful optimal control algorithm that efficiently computes RF and gradient waveforms to achieve a target magnetization profile, making it suitable for the refocusing pulses in T2-weighted turbo-spin-echo sequences at ultra-high field [2].
SAR Management with Virtual Observation Points
A non-negotiable aspect of pTx at 11.7T is the rigorous management of the Specific Absorption Rate (SAR). The use of Virtual Observation Points (VOPs) is the state-of-the-art method for SAR monitoring [2]. This technique creates a compact model of the complex SAR distribution within the body, allowing for real-time monitoring and enforcement of regulatory safety limits during RF pulse transmission. All pTx pulse designs must be performed under the explicit constraint of these VOP-derived SAR limits [2].
Diagram 1: The comprehensive workflow for mitigating B1+ inhomogeneity using Parallel Transmission at 11.7T, integrating specialized hardware, essential input data, and computational pulse design.
Experimental Validation and Performance at 11.7T
The implementation of pTx on the Iseult 11.7T scanner has been experimentally validated through in vivo human brain imaging. The performance metrics demonstrate the success of this technology.
Quantitative Performance Metrics
In vivo imaging on the Iseult system demonstrated that pTx enables high-quality imaging with effective mitigation of B1+ artifacts. Using pTx, the system achieved a normalized root mean square error (NRMSE) of approximately 8% for small flip angle excitations and roughly 13% for high flip angle refocusing pulses over the entire brain [2]. It is noteworthy that this performance in homogenizing the flip angle at 11.7T is comparable to the intrinsic B1+ inhomogeneity typically achieved with volume coils at 3T [2]. This represents a significant engineering achievement, taming the extreme inhomogeneity of 11.7T to a level familiar to clinical researchers.
Table 2: Performance Metrics of pTx at 11.7T from Experimental Studies
| Performance Parameter | Result | Context & Significance |
|---|---|---|
| Excitation Pulse Homogeneity (NRMSE) | ~8% [2] | For small tip angle excitations over the whole brain. |
| Refocusing Pulse Homogeneity (NRMSE) | ~13% [2] | For large flip angle refocusing pulses over the whole brain. |
| B0 Shimming Homogeneity | 82.7 Hz (0.17 ppm) std. dev. [2] | Static shimming up to 2nd order, essential for high-resolution. |
| Inversion Pulse Homogeneity (NRMSE) | 8% (5-12% range) [2] | Most challenging pulse; highlights need for high power and optimal channel pairing. |
| Radiated Power Loss with FES | < 5.7% [42] | Down from 22.5% with conventional shield; improves efficiency and B1+. |
Pulse Design Protocol for T2-Weighted Imaging
A typical experimental protocol for acquiring an in vivo T2-weighted image at 11.7T involves the following steps, as derived from the Iseult experiments [2]:
- B0 and B1+ Field Mapping: For each participant, acquire B0 and B1+ field maps. These are essential input data for the pTx pulse design algorithms.
- Static B0 Shimming: Perform 2nd-order B0 shimming using a brain mask and a quadratic programming approach to achieve a homogeneous static field (~83 Hz standard deviation over the brain).
- pTx Pulse Design: Using the acquired B1+ maps, design subject-specific RF pulses.
- For the excitation pulse (e.g., 10° target flip angle), use the kT-points algorithm with 5-7 kT-points and a duration of 0.5-1 ms.
- For the refocusing pulse (e.g., 180° target), use the GRAPE algorithm with a duration of 4 ms.
- All pulses are designed under explicit power and SAR constraints using the VOP model.
- Image Acquisition: Execute the T2-weighted sequence (e.g., a turbo-spin-echo variant) using the designed subject-specific pTx pulses.
The Scientist's Toolkit: Essential Research Reagents & Materials
For neuroscientists and developers working with 11.7T pTx, the following tools and components are essential.
Table 3: Essential Research Reagents and Solutions for 11.7T pTx Experimentation
| Tool/Reagent | Function in 11.7T pTx Research |
|---|---|
| Multi-Channel pTx Head Coil | The core hardware providing multiple, independent RF transmission channels for spatial control of the B1+ field [42] [2]. |
| Electromagnetic (EM) Simulation Software (e.g., CST Studio) | Used for designing, optimizing, and analyzing coil performance, loss mechanisms, and SAR distributions before physical construction [42] [43]. |
| Numerical Human Model (e.g., Duke Body Model) | Provides a realistic EM tissue model for simulations, enabling the prediction of in vivo B1+ fields and SAR during the design phase [42]. |
| High-Power RF Amplifiers (2 kW/chan.) | Provide the necessary power to drive RF pulses at 500 MHz, overcoming high tissue conductivity losses and enabling robust inversion pulses [2]. |
| Virtual Observation Point (VOP) Model | A compact safety model derived from EM simulations, used for real-time SAR monitoring and ensuring patient safety during pTx scans [2]. |
| Phantom Model (Cylindrical, distilled water) | Allows for experimental validation and calibration of coil performance (B1+ sensitivity, uniformity) and safety (SAR) before human scans [43]. |
Parallel transmission is not merely an enhancement but an enabling technology for human neuroscientific research at 11.7T. It directly addresses the fundamental challenge of B1+ field inhomogeneity, making safe and effective imaging possible at this ultra-high field strength. The experimental results from the Iseult scanner confirm that pTx, combined with optimized hardware, successfully mitigates RF inhomogeneity artifacts, yielding T2 and T2*-weighted images with high SNR and contrast-to-noise ratio at mesoscopic resolutions [2].
The future development of 11.7T MRI for neuroscience will involve the construction of more advanced pTx arrays with higher channel counts, the implementation of more efficient RF pulse design algorithms to reduce computation time, and the integration of motion correction tools. These advancements will further unlock the potential of 11.7T, paving the way for high-resolution functional MRI, diffusion tensor imaging, and the exploration of novel contrast mechanisms to study the human brain at an unprecedented level of detail [2] [12] [44].
Taming Specific Absorption Rate (SAR) for Safe Human Imaging
Specific Absorption Rate (SAR) is a critical safety parameter in magnetic resonance imaging (MRI), defined as the rate at which radiofrequency (RF) energy is absorbed by the human body, measured in watts per kilogram (W/kg). SAR management becomes progressively more challenging with increasing magnetic field strength. In the context of ultra-high-field (UHF) MRI, particularly the emerging 11.7 Tesla systems for human neuroscience research, SAR increases approximately with the square of the static field strength (B₀). This relationship means that moving from 3T to 11.7T could potentially increase SAR by a factor of approximately 15 for identical pulse sequences, creating significant technical hurdles for safe human imaging.
SAR is fundamentally concerned with preventing excessive tissue heating during MRI examinations. While SAR quantifies power deposition, the actual biological risk is determined by the resulting tissue temperature increase, which depends on additional factors including regional perfusion, baseline patient temperature, thermoregulatory capacity, and ambient conditions. Certain populations—including infants, the elderly, obese individuals, and those with compromised thermoregulation—are particularly vulnerable to RF heating effects. The scientific and clinical pursuit of higher magnetic fields is driven by substantial gains in signal-to-noise ratio (SNR) and contrast mechanisms essential for advanced neuroscientific research, including functional MRI at the cortical layer level, high-resolution diffusion imaging, and multinuclear spectroscopy. These applications necessitate sophisticated approaches to SAR management to ensure patient safety while maximizing the scientific potential of UHF MRI systems.
SAR Fundamentals and Regulatory Framework
Physical Principles and Determinants
The physical definition of SAR is derived from electromagnetic energy interactions with biological tissues:
SAR = σ|E|²/ρ
where σ represents tissue electrical conductivity (S/m), |E| is the root-mean-square electric field strength (V/m), and ρ is tissue density (kg/m³). Several key factors directly influence SAR magnitude in UHF MRI:
- Magnetic Field Strength: SAR increases with the square of the RF frequency, which is directly proportional to B₀. Thus, identical pulse sequences at 11.7T would generate substantially higher SAR than at lower fields.
- Pulse Sequence Parameters: Flip angle, repetition time (TR), and duty cycle significantly impact SAR. The relationship is quadratic with flip angle—a 180° pulse produces 4× the SAR of a 90° pulse.
- Tissue Properties: Electrical conductivity varies substantially across tissues (by approximately a factor of 10), with higher water-content tissues like blood and muscle absorbing more RF energy than fat or bone.
- Subject Characteristics: SAR increases significantly with body size and is concentrated peripherally, with approximately 87% of RF power dissipation occurring in the outer third of a homogeneous body model.
- Coil Design: Transmit coil geometry and design directly influence SAR distribution and magnitude, with multi-channel transmit arrays offering potential for SAR reduction through optimized field patterning.
Table 1: Primary Factors Affecting SAR in UHF MRI
| Factor | Relationship with SAR | Practical Implications |
|---|---|---|
| Static Field Strength (B₀) | Proportional to B₀² | 11.7T presents ~15× higher SAR than 3T for same sequence |
| Flip Angle (α) | Proportional to α² | 180° refocusing pulses significantly increase SAR |
| Tissue Conductivity (σ) | Directly proportional | Muscle, blood show higher absorption than fat, bone |
| Patient Size | Proportional to r⁵ (approximately) | Larger patients experience disproportionately higher SAR |
| Duty Cycle | Directly proportional | Sequences with many RF pulses per time unit increase SAR |
| Electrical Permittivity | Affects field distribution | Causes standing wave patterns at UHF, increasing field heterogeneity |
International Safety Standards and Limits
The International Electrotechnical Commission (IEC) standard 60601-2-33 establishes SAR limits for MRI equipment, defining three operational modes based on perceived risk. For the Normal Operating Mode, whole-body SAR is limited to 2 W/kg, while head SAR is limited to 3.2 W/kg, averaged over 6 minutes. The First-Level Controlled Operating Mode permits higher limits—4 W/kg whole-body—but requires medical supervision. The Second-Level Controlled Operating Mode has no specified upper SAR limits but requires approval from a local ethics committee or Institutional Review Board for research purposes.
These standards acknowledge that partial-body exposures permit higher localized SAR, with limits scaled according to the mass ratio (R) of exposed to total body mass. For extremities, even higher SAR values (up to 12-20 W/kg) are permitted under certain conditions. It is noteworthy that these limits are based on environmental temperatures ≤25°C, with derating required for higher ambient temperatures.
Table 2: IEC 60601-2-33 SAR Limits (W/kg) for Normal Operating Mode
| Tissue Region | Averaging Time | Limit (W/kg) | Notes |
|---|---|---|---|
| Whole Body | 6 minutes | 2.0 | Based on environmental temperature ≤25°C |
| Head | 6 minutes | 3.2 | Higher limit due to better thermoregulation |
| Partial Body | 6 minutes | 2.0-10.0 | Varies with exposed mass ratio (R) |
| Extremities | 6 minutes | 12.0-20.0 | Higher limits due to efficient heat dissipation |
Technical Strategies for SAR Management at 11.7T
Pulse Sequence Modifications
Pulse sequence design offers the most direct approach for SAR reduction in neuroscience research at 11.7T:
- RF Pulse Type Selection: Using adiabatic pulses and specially designed low-SAR pulse types that increase duration while reducing peak amplitude can significantly decrease SAR, though with potential trade-offs in minimum TE/TR and slice profile.
- Flip Angle Reduction: Strategically reducing flip angles decreases SAR quadratically, though this must be balanced against potential SNR reduction and contrast alteration.
- Repetition Time (TR) Increase: Lengthening TR reduces the duty cycle and time-averaged SAR, but increases total scan time and affects T₁-weighted contrast.
- Parallel Transmission (pTx): Multi-channel transmit systems (e.g., 16-channel transmit arrays) enable RF shimming and spatially tailored excitation, which can reduce both global and local SAR while improving B₁⁺ field homogeneity.
- Interleaved Acquisition: Strategic interleaving of sequence modules can effectively reduce time-averaged SAR by decreasing the RF duty cycle, though careful implementation is required to avoid unintended increases.
Hardware Innovations for SAR Reduction
Advanced hardware designs are essential for managing SAR at 11.7T:
- Optimized RF Coil Design: Traditional low-pass birdcage coils show performance limitations above 3T. Hybrid-type birdcage coils demonstrate superior B₁-field sensitivity and homogeneity at UHF, making them preferable reference coils for 11.7T systems. The diameter-to-length ratio (D/L-ratio) of these coils significantly affects SAR distribution, with a ratio of 0.7 optimizing sensitivity while a ratio of 1.0 improves field uniformity.
- Multi-Channel Transmit Arrays: Systems with 16-channel transmit capability allow for parallel transmission techniques that can optimize RF power distribution, reducing both overall and localized SAR while improving image uniformity.
- Asymmetric Gradient Coils: Next-generation head-only gradient coils with three-layer winding patterns (e.g., achieving 200 mT/m amplitude and 900 T/m/s slew rate) enable faster encoding, shorter echo times, and reduced echo train lengths—indirectly mitigating SAR by permitting more efficient sequence designs.
- High-Density Receive Arrays: 96- and 128-channel receiver arrays with reduced coil loop diameters (~4 cm) improve SNR in the cerebral cortex without increasing SAR, enabling higher acceleration factors that can reduce scan times and cumulative RF exposure.
Diagram 1: Multi-faceted technical approach to SAR management at 11.7T, combining pulse sequence modifications with hardware innovations.
Experimental Protocols for SAR Validation
SAR-Induced Temperature Measurement Protocol
Validating SAR simulations requires direct temperature measurement using MR thermometry:
Materials and Setup:
- Agar-gel phantom (10g/L NaCl, 1g/L CuSO₄, 7g/L agar in distilled water) in plastic container
- Custom circular surface coil (80mm diameter) for localized heating
- RF power amplifier, directional coupler, and power meter
- MRI system with proton resonance frequency (PRF) shift thermometry capability
- Reference oil phantoms for phase drift correction
Experimental Procedure:
- Phantom Characterization: Measure dielectric properties (conductivity, permittivity) of phantom materials using impedance analyzer.
- Coil Calibration: Measure quality factor (Q) of heating coil both unloaded and when loaded with phantom to determine power dissipation efficiency.
- Baseline Imaging: Acquire initial phase map using gradient-echo sequence (TR/TE: 30/10 ms, matrix: 256×256, multiple averages).
- RF Heating: Deliver calibrated RF power (e.g., 42.5W for 2 minutes) to heating coil at frequency offset from Larmor frequency to avoid interference with imaging.
- Post-Heating Imaging: Immediately acquire second phase map with identical parameters but reduced averaging to minimize cooling during acquisition.
- Temperature Calculation: Compute temperature change using PRF shift equation:
ΔT = (Δϕ - Δϕdrift)/(α × γ × B₀ × TE)
where α = -0.01 ppm/°C (PRF shift coefficient for water), γ = 42.58 MHz/T (gyromagnetic ratio), and Δϕdrift is phase drift correction derived from oil reference phantoms.
Numerical Simulation Protocol for SAR and Temperature
Computational modeling provides comprehensive SAR and temperature distribution data:
Computational Framework:
- Model Creation: Segment anatomical images to create 3D computational model of phantom or human anatomy.
- Material Property Assignment: Assign measured dielectric properties (σ, εr) and thermal parameters (ρ, perfusion, specific heat) to each tissue type.
- Simulation Setup: Use finite-difference time-domain (FDTD) method with 1mm resolution, perfect matched layer boundary conditions.
- Coil Modeling: Incorporate exact coil geometry, tuning, and drive point configuration.
- SAR Calculation: Solve electromagnetic field distributions and compute SAR = σ|E|²/ρ.
- Temperature Simulation: Apply bioheat transfer equation to model temperature evolution, incorporating perfusion effects.
Validation Metrics:
- Spatial correlation between simulated and measured temperature distributions
- Comparison of maximum temperature increase
- Analysis of thermal rise time constants in different tissue regions
Diagram 2: Integrated experimental and computational workflow for SAR validation, combining direct temperature measurement with numerical simulation.
Research Reagent and Material Solutions
Table 3: Essential Research Materials for SAR Investigation and Safety Validation
| Material/Equipment | Function/Application | Technical Specifications |
|---|---|---|
| Agar-Gel Phantom | Tissue-mimicking material for SAR validation | 10g/L NaCl, 1g/L CuSO₄, 7g/L agar; σ = 2.97 S/m, εr = 74.15 @165MHz |
| Dielectric Probe Kit | Measurement of tissue dielectric properties | Compatible with impedance analyzer; frequency range covering Larmor frequency at 11.7T (~498 MHz for ¹H) |
| FDTD Simulation Software | Electromagnetic field and SAR computation | Commercial package (e.g., XFdtd) with GPU acceleration for complex anatomical models |
| Custom Surface Coils | Localized RF delivery for experimental SAR studies | Circular design (80mm diameter); tunable to specific frequencies; Q-ratio ~0.05 (loaded/unloaded) |
| RF Power Monitoring System | Measurement of delivered RF power | Directional coupler, power sensor, and power meter; calibrated for accurate power measurement |
| Multi-Channel Transmit Array | Parallel transmission for SAR reduction | 16-channel system capable of independent phase/amplitude control for RF shimming |
| Hybrid Birdcage Coil | Optimized RF transmission at UHF | Combined capacitor placement on legs and end-rings; D/L ratio optimized for 11.7T applications |
| PRF Thermometry Sequence | Temperature mapping during RF exposure | Gradient-echo sequence with phase difference processing; high temporal resolution for thermal kinetics |
Application in 11.7T Neuroscience Research
The development of 11.7T human MRI systems represents the cutting edge of neuromedicine, promising unprecedented spatial resolution for visualizing cortical layers, columns, and fine-scale neuroanatomy. SAR management is particularly critical for these applications, as extended scan times and high-resolution protocols compound RF exposure concerns. Neuroscience applications at 11.7T benefiting from advanced SAR control include:
- Laminar fMRI: Studying neural processing across cortical layers requires sub-millimeter resolution (0.3-0.5 mm isotropic), demanding high SNR and contrast-to-noise ratio that only UHF systems can provide. SAR-intensive sequences must be optimized to maintain safety during prolonged acquisitions needed for detecting subtle hemodynamic changes.
- High-Angular Resolution Diffusion Imaging: Mapping complex white matter architecture at ultra-high resolution necessitates strong diffusion weighting and numerous gradient directions, creating significant SAR challenges that can be mitigated through parallel transmission and optimized sequence design.
- Multinuclear Spectroscopy: Non-proton nuclei (e.g., ²³Na, ³¹P) provide unique metabolic information but have intrinsically low SNR, requiring extended acquisitions where SAR management is essential for patient safety and compliance.
- Susceptibility-Weighted Imaging: Visualizing microvasculature and iron deposition benefits tremendously from the enhanced susceptibility contrast at 11.7T, but often uses SAR-intensive sequences that require careful optimization.
Advanced SAR management techniques enable these applications by ensuring regulatory compliance while maximizing the scientific return from limited scanner time. The integration of sophisticated RF monitoring, real-time SAR estimation, and subject-specific modeling will further enhance the safety and capability of 11.7T neuroscience research in the coming years.
Managing Acoustic Noise, Vibrations, and Gradient-Magnet Interactions
Ultra-high field (UHF) magnetic resonance imaging (MRI) systems, particularly those operating at 11.7 Tesla, represent a transformative advancement for neuroscience research, offering unprecedented gains in signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) for exploring the human brain at the mesoscopic scale [10] [2]. However, the very factors that enable this enhanced performance—increased static magnetic field (B₀) strength and more powerful gradient systems—also exacerbate significant technical challenges. Among these, elevated acoustic noise, mechanical vibrations, and their complex interactions with the main magnetic field pose substantial obstacles to both data quality and participant safety [10] [45] [46]. These interactions are not merely a nuisance; they can impair image quality through artifacts, limit the performance of gradient coils, and potentially compromise the validity of functional MRI studies by causing patient discomfort or inducing peripheral nerve stimulation (PNS) [45] [46]. For neuroscientists and drug development professionals utilizing 11.7 T scanners like the Iseult system, a thorough understanding and proactive management of these phenomena are essential for unlocking the full potential of UHF MRI in brain research [2]. This guide provides a technical overview of the sources, impacts, and mitigation strategies for these challenges, framed within the context of advanced neuroscience applications.
Fundamental Challenges at Ultra-High Field
Physics of Noise and Vibration Generation
In MRI, acoustic noise is primarily generated by the Lorentz forces acting on gradient coil conductors. When rapidly switching electrical currents pass through these coils in the presence of the strong static B₀ field, substantial forces are produced, causing the coil structure to vibrate and radiate sound energy [46]. The amplitude of these forces is proportional to the current in the gradient coils and the strength of the B₀ field. Consequently, as the static field increases to 11.7 T and gradient systems become more powerful to enable higher resolution and faster acquisitions, the resulting acoustic noise and vibrational energy increase significantly [45] [47].
Gradient-Magnet Interactions
At ultra-high fields, the interaction between the gradient system and the main magnet becomes a critical consideration. The Iseult 11.7 T magnet, for instance, operates in non-persistent mode and is cooled by a superfluid helium bath at 1.8 K to maintain cryostability [10]. The powerful, rapidly switching gradient fields can induce significant vibrations that pose several risks, including quenching from local heat overloads that might surpass the Gorter-Mellink limitation of helium heat dissipation [10]. Furthermore, these interactions can affect the temporal stability and homogeneity of the main magnetic field, which are paramount for high-quality imaging. Field monitoring of the Iseult system has revealed resonances at certain frequencies that require careful investigation to ensure they do not degrade image quality [10].
Quantifying the Problem: Data and Metrics
Acoustic Noise Levels Across Field Strengths
The following table summarizes typical sound pressure levels (SPLs) encountered in MRI environments, illustrating the escalating challenge at higher field strengths.
Table 1: Characteristic Acoustic Noise Levels in MRI
| Field Strength / Context | Pulse Sequence / Condition | Typical Sound Pressure Level |
|---|---|---|
| 1.5 T & 1.0 T [46] | Routine clinical sequences | Often exceeds 85 dB safety threshold |
| 7 T [45] | Conventional 3D T1-weighted TFE | 123.7 dBA (peak) |
| 7 T [45] | Conventional T2-weighted FSE | 116.3 dBA (peak) |
| 7 T [45] | T2-weighted FSE with SofTone | 97.0 dBA (peak) |
| Echo-Planar Imaging (EPI) [46] | One of the loudest sequences | 110 - 130 dBA |
Safety and Operational Limits
Prolonged exposure to noise levels above 85 dB risks hearing impairment, mandating the use of hearing protection for patients [45] [46]. Beyond auditory safety, high acoustic noise can induce patient anxiety and discomfort, negatively impact communication, and reduce exam success rates [45]. Furthermore, the swiftly alternating gradient fields can induce electric currents in conductive tissues, leading to peripheral nerve stimulation (PNS), which manifests as tingling or muscle twitching and can limit the achievable gradient performance [45].
Mitigation Strategies and Experimental Protocols
A multi-faceted approach is required to effectively manage noise and vibration at 11.7 T. The strategies can be broadly categorized into hardware, software, and facility-level solutions.
Software-Based Acoustic Noise Reduction
Software solutions modify the pulse sequence to mechanically reduce the output of the gradient coil, offering a highly flexible and immediately deployable strategy.
Protocol: Evaluating Software-Based ANR (e.g., SofTone) This protocol is adapted from a 2025 study investigating the SofTone ANR technique at 7 T [45].
- 1. Objective: To evaluate the efficacy of an ANR technique in reducing SPLs and perceived noise while maintaining diagnostic image quality for T2-weighted Fast Spin Echo (FSE) and 3D T1-weighted Turbo Field Echo (TFE) sequences in brain MRI.
- 2. Equipment & Setup:
- Scanner: A 7 T MRI system (e.g., Philips Achieva).
- RF Coil: A 2 transmit/32 receive head coil.
- Subject: Volunteers positioned head-first in a supine position.
- Hearing Protection: Standard protection must be used.
- 3. Data Acquisition:
- Each subject is scanned using both the conventional and the SofTone-optimized versions of the T2W FSE and 3D T1W TFE sequences.
- Acoustic Measurement: Peak A-weighted sound pressure levels (dBA) are measured during scanning.
- Subjective Feedback: Participant-perceived noise levels are recorded using a standardized scale (e.g., Borg CR10-scale).
- Image Acquisition: Parameters (e.g., slice thickness, matrix size) are kept nearly identical between conventional and SofTone scans, with only minor adjustments allowed (e.g., slight increase in minimum TE, increased receiver bandwidth) to accommodate the gradient restrictions.
- 4. Data Analysis:
- Statistical Tests: Use paired t-tests to compare SPLs and Wilcoxon's Signed-Rank Test to compare qualitative image scores.
- Image Quality Assessment: Qualitative image assessments are performed by multiple blinded neuroradiologists using ordinal scales rating factors like artifact interference and white/gray matter differentiation.
- 5. Key Findings from Literature: Application of SofTone at 7 T resulted in a dramatic reduction of peak SPLs: from 123.7 dBA to 101.5 dBA for 3D T1W TFE and from 116.3 dBA to 97.0 dBA for T2W FSE, while maintaining diagnostically acceptable image quality [45].
"Quiet" Gradient Coil Design
Addressing the problem at its source involves designing gradient coils that inherently produce less noise. This hardware-based approach is fundamental to next-generation scanner design.
- Lorentz Force Balancing: This technique, first proposed by Mansfield, involves designing coil windings such that the opposing Lorentz forces in the structure are balanced, thereby reducing the net vibrational force. Reductions on the order of 10 dB have been demonstrated [46].
- Active Acoustic Control (AAC): This method integrates a secondary "control winding" into the gradient coil structure. By driving this control winding with a specific current and phase, it can counteract the vibrational modes of the primary gradient winding. A model system demonstrated a remarkable noise reduction of 40 dBA inside the bore during an EPI sequence [47].
- Asymmetric and Split Coil Designs: Novel geometries, such as asymmetric half-connected coils or split designs, can avoid exciting certain resonant vibrational modes and guide acoustic energy away from the patient, thereby reducing perceived noise [46].
Passive Damping and Facility Design
Controlling the propagation of noise and vibration once it has been generated is crucial for protecting adjacent spaces and requires careful architectural planning.
- Facility Construction: MRI room walls should typically feature a double-stud "parent wall" construction with multiple layers of gypsum board on the shielding wall and ceiling to maximize airborne sound isolation [48].
- Vibration Isolation: For MRIs located on framed slabs above other spaces, a two-stage vibration isolation system is highly effective. This system uses an intermediate mass (e.g., a steel plate) sandwiched between two layers of elastomeric pads placed under the MRI feet to break the structure-borne noise path [48].
- Acoustic Absorbers: Micro-perforated panels (MPPs) can be used as acoustic absorbers within the bore, providing passive noise dampening across multiple frequency bands [46].
Ensuring Safety and Performance at 11.7 T
Before the first human images could be acquired on the Iseult 11.7 T scanner, a comprehensive safety study was conducted on 20 volunteers to ensure the innocuousness of such a high magnetic field [2].
Protocol: Initial In-Vivo Safety and Imaging at 11.7 T
- 1. Objective: To validate the safety and feasibility of human brain imaging at 11.7 T and mitigate the RF field inhomogeneity problem.
- 2. Setup:
- Scanner: Iseult 11.7 T whole-body MRI system.
- RF Coil: A home-made parallel transmission (pTx) RF coil with 16 transmit elements and Virtual Observation Points for SAR monitoring.
- 3. Safety & Imaging Procedure:
- Physiological Monitoring: A battery of physiological, vestibular, and cognitive tests was administered to participants both inside and outside the magnet.
- Control Group: A separate 0 T control group (uninformed of the field status) underwent identical testing with simulated MRI sounds to account for nocebo effects.
- Genotoxicity Assessment: Blood samples were drawn from the 11.7 T group before and after exposure for intra-participant comparison.
- B₀ Shimming: Second-order static B₀ shimming was performed using a brain mask and a quadratic programming approach.
- pTx RF Pulses: Parallel transmission pulses (e.g., kT points, GRAPE algorithms) were designed to achieve homogeneous excitation and refocusing across the brain while respecting SAR limits.
- 4. Outcome: The study found no significant adverse effects related to the 11.7 T field exposure, confirming the safety of human imaging. The use of pTx successfully mitigated RF inhomogeneity, producing the first in-vivo human brain images at 11.7 T with resolutions up to 0.19 × 0.19 × 1 mm³ [2].
Table 2: Key Research Reagents and Materials for UHF MRI Neuroscience
| Item | Function & Application in Neuroscience Research |
|---|---|
| Parallel Transmission (pTx) RF Coil | A multi-channel transmit coil is essential to counteract the severe B₁⁺ field inhomogeneity at 500 MHz (11.7 T), enabling whole-brain imaging with uniform signal [2]. |
| Dielectric Pads | Placed between the head coil and the participant, these pads help homogenize the RF field and increase signal intensity in challenging regions like the cerebellum and temporal lobes [45]. |
| Acoustic Noise Reduction (ANR) Software | Vendor-provided solutions (e.g., SofTone, Whisper) that restrict gradient slew rates and amplitudes to create a quieter scan environment, crucial for participant comfort in long fMRI studies [45]. |
| Field Camera or Monitoring System | Monitors the temporal stability of the B₀ field in real-time, critical for identifying and compensating for drift or vibration-induced field fluctuations during long acquisitions like diffusion tractography [10]. |
| Advanced B₀ Shimming Algorithms | Second-order or higher shimming using a brain mask is necessary to achieve sufficient B₀ homogeneity over the brain (~80 Hz standard deviation at 11.7 T) for high-resolution structural and functional imaging [2]. |
| pTx Pulse Design Software | Software implementing algorithms like kT-points or GRAPE is required to design RF pulses that simultaneously achieve target flip angles, mitigate SAR, and compensate for B₁⁺ inhomogeneity [2]. |
The management of acoustic noise, vibrations, and gradient-magnet interactions is not a peripheral concern but a central engineering challenge in the operation of 11.7 T MRI systems for cutting-edge neuroscience. A synergistic approach—combining innovative hardware designs like quiet gradient coils, sophisticated software controls for gradients and RF, and purpose-built facility infrastructure—is essential for mitigating these effects. The successful acquisition of the first in-vivo human brain images at 11.7 T, coupled with comprehensive safety data, marks a pivotal milestone, proving that these challenges can be overcome [2]. As the technology matures, the continued development of these mitigation strategies will be paramount for leveraging the full mesoscopic resolution of 11.7 T MRI to revolutionize our understanding of brain structure, function, and the pathological mechanisms underlying neurological and psychiatric diseases.
The deployment of ultra-high field (UHF) MRI systems, particularly the cutting-edge 11.7 Tesla (T) human scanners, represents a significant leap forward for neuroscience research. These instruments offer unprecedented spatial resolution and signal-to-noise ratios, enabling the exploration of the brain's microstructures and biochemical environment in exquisite detail [6] [37]. However, the infrastructure required to support these technological marvels is substantial. The very properties that make them powerful research tools—extreme magnetic fields and the superconducting materials that generate them—introduce profound challenges in cryogenics, magnetic shielding, and facility design. This whitepaper details these critical infrastructure and cost barriers, providing a foundational reference for researchers, institutions, and drug development professionals planning to work at the frontier of in vivo brain imaging.
Core Technical Barriers
Cryogenic Systems
The heart of an 11.7 T MRI system is its superconducting magnet, which requires extreme cooling to operate. The shift from lower-field systems to 11.7 T entails a quantum leap in cryogenic demands.
- Coolant Requirements and Operating Temperature: The 11.7 T Iseult magnet utilizes niobium-titanium (NbTi) superconducting wire and must be cooled to a temperature of 1.8 Kelvin (-271.35°C) using superfluid liquid helium [6] [37]. This ultra-low temperature is essential for maintaining the NbTi in a superconducting state, thereby allowing the magnet to carry the immense electrical currents necessary to generate a stable 11.7 T field without any electrical resistance.
- Cryogen Volume and Magnet Mass: The Iseult system requires a staggering 7,500 liters of superfluid liquid helium for its initial cooldown and stable operation. The magnet itself is a massive engineered structure, weighing 132 tons and incorporating 182 kilometers of superconducting wire [6]. This scale far exceeds that of clinical 3 T systems and presents significant challenges in terms of logistics, cost, and safety.
- The Helium Dependency and Future Directions: The reliance on large volumes of liquid helium represents a significant operational vulnerability and cost driver, given that helium is a non-renewable resource with fluctuating prices [49] [50]. Research into high-temperature superconductors (HTS) offers a long-term pathway to reducing this dependency, as HTS materials could potentially enable magnets cooled by liquid nitrogen, a more affordable and abundant cryogen [49] [51]. However, this technology for whole-body MRI is still in development.
Table 1: Cryogenic System Specifications for the Iseult 11.7 T MRI
| Parameter | Specification | Comparison to 7T/3T Systems |
|---|---|---|
| Operating Temperature | 1.8 K (-271.35°C) | Colder than standard LHe-cooled magnets (typically 4.2 K) |
| Coolant Type | Superfluid Liquid Helium | Same coolant type, but vastly larger volume and complexity |
| Coolant Volume | 7,500 liters | Substantially larger than commercial 7T systems |
| Superconducting Wire | 182 km of NbTi | Longer than lower-field systems; NbTi is standard LTS material |
| Magnet Weight | 132 tons | Heavier and more massive than previous generation magnets |
Cryogenic Cooling System Workflow
Magnetic Shielding and Physical Infrastructure
The immense magnetic field of an 11.7 T scanner necessitates extensive measures to contain it, protect the environment, and ensure safety, which directly translates into unique and demanding facility requirements.
- Passive and Active Shielding: The Iseult magnet employs an actively shielded double-pancake design to contain its magnetic fringe field [37]. Active shielding uses additional superconducting coils designed to counteract the magnetic field outside the main magnet. Despite this, the sheer strength of the 11.7 T field often requires supplementary passive shielding. For instance, a head-only 11.7 T system at the NIH uses 380 tons of iron for passive shielding, highlighting the massive physical infrastructure needed to manage the stray field [37].
- Spatial and Structural Demands: The Iseult system is a cylinder 5 meters long and 5 meters in diameter [6]. Housing such a large instrument, plus the iron shielding, requires a specially designed and reinforced facility. The floor must support immense weight, and the room's layout must account for the large "5 Gauss line" (the boundary beyond which the magnetic field is considered safe for the general public), which can extend far beyond the scanner room itself, influencing the entire building's design.
- Safety Protocols: Safety requirements are more stringent than for clinical systems. Staff require specialized training on the unique interactions between the ultra-high field and metallic objects, implants, and even physiological effects [6]. While initial safety assessments of the 11.7 T system for scans up to 1.5 hours have shown no significant effects on vital signs, cognition, or genotoxicity, continuous monitoring and rigorous protocols are mandatory [6].
Table 2: Shielding and Infrastructure Requirements
| Aspect | 11.7 T Requirement | Technical Implication |
|---|---|---|
| Shielding Method | Active Shielding + Massive Passive Shielding | 380 tons of iron shielding used for a head-only system [37] |
| Magnet Dimensions | 5 m (L) x 5 m (D) cylinder | Requires a very large, custom-built scanner room |
| Total System Weight | 132 tons (Iseult) to 110 tons (10.5 T Minnesota) | Necessitates significant structural reinforcement of the building |
| Fringe Field Management | Extended 5 Gauss Line | Impacts a larger area of the building site, requiring careful zoning |
Radiofrequency (RF) System Challenges
As the static magnetic field (B₀) increases, so does the operational frequency (Larmor frequency) for proton imaging. This relationship introduces unique challenges for the RF subsystems that transmit and receive the MRI signal.
- Increased Frequency and Insertion Loss: The 11.7 T system operates at a proton frequency of 500 MHz. RF interconnect components, such as coaxial cables and connectors, suffer from higher insertion loss at these frequencies. This loss, which scales as a square root function of frequency, results in less efficient power transmission and generates excess heat that must be managed, adding complexity to the system's thermal management [52].
- RF Power Deposition and Safety: The higher frequency also leads to increased Specific Absorption Rate (SAR), a measure of the RF power deposited in the patient's tissue. Managing SAR is a critical safety concern at UHF. Advanced methods like parallel transmission with multiple RF channels are required to create homogenous excitation fields while staying within safe SAR limits [37] [51].
- Advanced RF Coil Technology: Standard, single-channel RF coils are insufficient for 11.7 T imaging. Research systems rely on sophisticated multi-channel transmit/receive RF arrays. These arrays are essential for mitigating RF field inhomogeneity and achieving the ultimate signal-to-noise ratio promised by the high field [51]. One simulation study indicated that a 16-channel transmit array could enable brain imaging at 14 T, pointing toward the technology needed for 11.7 T [51].
Economic and Operational Considerations
Cost Analysis and Funding Models
The financial outlay for an 11.7 T MRI system is prohibitive for most individual institutions. The Iseult project was realized only through a French-German consortium involving government research agencies (CEA), industrial partners (Siemens Healthineers), and magnet specialists (Alstom) [6]. This collaborative, nationally-funded model is likely the standard for such extreme-performance instruments. Given the high costs and specialized nature, these systems are currently envisioned as national research resources rather than clinical tools, with access granted to the scientific community based on project merit [37].
The Research-Cinical Translation Gap
While 7 T MRI systems have received regulatory approval for certain clinical applications (e.g., brain and joint imaging), 11.7 T systems are firmly in the research domain [6] [37]. The infrastructure barriers detailed herein are the primary reason. The size, cost, and operational complexity of current 11.7 T prototypes make widespread clinical installation impractical in the immediate future. The focus for these machines is on foundational neuroscience, such as mapping cortical columns, tracking metabolic compounds like lithium, and uncovering subtle pathologies in epilepsy that are invisible at lower fields [6] [51].
Experimental Protocols for Neuroscience at 11.7 T
High-Resolution Anatomical Imaging Protocol
Objective: To acquire in vivo images of the human brain with sub-millimeter resolution for mapping fine-grained anatomy and identifying subtle malformations.
Methodology:
- Magnet Preparation: Ensure the 11.7 T magnet is shimmed and stable, with the cryogenic system maintaining a temperature of 1.8 K.
- RF Coil Setup: Employ a high-density, multi-channel transmit/receive head coil. Utilize parallel transmission technology to optimize the B₁ transmission field homogeneity.
- Pulse Sequence: Use a 3D T2-weighted turbo spin-echo sequence or a T2*-weighted 2D Gradient Echo (GRE) sequence.
- Imaging Parameters (Representative):
- Data Analysis: Compare the 11.7 T images directly with 3 T and 7 T acquisitions to quantify gains in signal-to-noise ratio and delineation of anatomical features.
Functional MRI (fMRI) and Metabolic Spectroscopy Protocol
Objective: To leverage the enhanced sensitivity and spectral dispersion at 11.7 T for high-specificity functional imaging and metabolic profiling.
Methodology:
- Magnet and Subject Preparation: Standard fMRI setup, with rigorous screening for contraindications specific to 11.7 T.
- BOLD fMRI:
- Use T2*-weighted GRE-EPI or spin-echo sequences to achieve microvascular specificity.
- The higher magnetic field enhances the Blood-Oxygenation-Level-Dependent (BOLD) contrast, improving the detection of neural activity, particularly in deeper brain structures [37].
- Magnetic Resonance Spectroscopic Imaging (MRSI):
- Utilize the enhanced spectral resolution to separate and quantify neurochemicals such as glutamate, lactate, and pyruvate.
- The goal is to non-invasively measure metabolite ratios that are currently accessed via invasive methods like intracerebral microdialysis [6].
- Safety Monitoring: Throughout extended scans (e.g., 1.5 hours), continuously monitor subject vital signs and conduct pre- and post-scan cognitive and balance assessments to ensure safety [6].
Experimental Workflow for 11.7T Neuroscience
The Scientist's Toolkit: Key Research Reagent Solutions
Table 3: Essential Materials and Technologies for 11.7T Research
| Item / Technology | Function & Relevance to 11.7T |
|---|---|
| Niobium-Titanium (NbTi) Superconducting Wire | The core material of the magnet windings; enables superconductivity at 1.8 K when carrying high current densities to generate the 11.7 T field [49] [37]. |
| Superfluid Liquid Helium | The essential cryogen that cools the NbTi magnet to its required operating temperature of 1.8 K, ensuring zero electrical resistance [6] [37]. |
| Multi-Channel Transmit/Receive RF Coils | Advanced phased-array coils (e.g., 16-32 channels) that are mandatory for managing B1+ inhomogeneity and achieving high signal-to-noise at 500 MHz [51]. |
| Parallel Transmission System | Hardware and software that drives multi-channel RF coils, allowing for precise control of the excitation profile and management of SAR, which is critical for safety and image quality at UHF [51]. |
| Metamagnetic Contrast Agents (e.g., FeRh) | Switchable contrast agents whose magnetic moment can be toggled with a magnetic field pulse. Their large moment change is particularly suited for creating detectable contrast at UHF, useful for cell tracking studies [53]. |
| Actively Shielded B₀ Insert Coil | A resistive magnet insert capable of applying a temporary, localized shift in the main magnetic field (e.g., ±0.77 T). Used in research to actively switch metamagnetic contrast agents or for other field manipulation experiments [53]. |
Protocol Optimization for High-Resolution Functional and Diffusion Imaging
The development of ultra-high-field (UHF) magnetic resonance imaging (MRI) scanners operating at 11.7 Tesla represents a transformative advancement in neuroscience research, offering unprecedented spatial resolution for studying the human brain at a mesoscopic scale. This field strength provides a supralinear gain in signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) compared to conventional 1.5T or 3T clinical scanners, enabling researchers to visualize architectural features of the brain that were previously inaccessible [2] [54]. The Iseult 11.7T MRI scanner, developed by the French Atomic Energy Commission (CEA), has demonstrated the capability to acquire high-resolution images of the human brain in just four minutes—a task that would require hours on standard hospital MRI systems [3]. This technological leap forward provides neuroscientists with a powerful tool for investigating both normal brain function and the pathological mechanisms underlying neurological and psychiatric disorders, with potential applications ranging from neurodegenerative disease research to drug development.
The fundamental advantage of 11.7T MRI stems from the stronger external magnetic field (B0), which enhances the polarization of water proton spins in biological tissues. This increased polarization translates to a stronger signal during imaging, which can be leveraged to achieve higher spatial resolution, reduced scan times, or an optimal balance of both [54]. However, operating at this field strength introduces significant technical challenges, including increased radiofrequency (RF) field inhomogeneity, heightened specific absorption rate (SAR) concerns, and more pronounced B0 field inhomogeneity artifacts [2] [10]. This technical guide provides comprehensive protocols for optimizing functional and diffusion imaging at 11.7T, addressing these challenges through advanced hardware solutions and pulse sequence modifications to fully exploit the potential of UHF MRI for neuroscience applications.
Technical Challenges and Solutions at 11.7T
Radiofrequency Field Inhomogeneity
At 11.7T, the Larmor frequency for hydrogen nuclei increases to approximately 500 MHz, resulting in a shortened wavelength of the RF field that approaches the dimensions of the human head. This leads to constructive and destructive interference patterns, manifesting as severe signal variations in images—a phenomenon known as the "dielectric effect" [2]. The conventional volume coils used in lower-field systems produce highly inhomogeneous B1+ fields at 11.7T, with a coefficient of variation of 45% over the whole brain [2].
Parallel Transmission (pTx) technology has emerged as the most effective solution to this challenge. By utilizing multi-channel transmit arrays with independent control over amplitude and phase for each element, pTx enables the generation of homogeneous B1+ fields throughout the brain [2]. The Iseult project employs a custom-built 16-channel transmit array paired with dedicated RF pulse design algorithms, including kT-points and Gradient Ascent Pulse Engineering (GRAPE) [2]. These advanced pulses are designed using active-set algorithms with simultaneous k-space optimization and explicit hardware constraints (peak power, average power) [2]. With proper pTx optimization, normalized root mean square errors (n.r.m.s.e.) of 13% or lower can be achieved over the whole brain—comparable to the intrinsic inhomogeneity achieved at 3T with volume coils [2].
Specific Absorption Rate (SAR) Management
The energy deposited in tissue increases approximately quadratically with field strength, making SAR management a critical safety concern at 11.7T [2]. Without proper mitigation, SAR limits can constrain sequence parameters and impede protocol optimization.
The Iseult scanner addresses this challenge through Virtual Observation Points (VOPs) for SAR monitoring and dedicated RF pulse design algorithms that explicitly incorporate SAR constraints [2]. These methods enable precise control over local and global SAR while maintaining imaging performance. Additionally, RF coil design plays a crucial role in SAR management; Hybrid birdcage (Hybrid-BC) coils demonstrate favorable SAR characteristics compared to traditional low-pass birdcage configurations at UHF [55].
B0 Field Inhomogeneity
Static magnetic field (B0) inhomogeneity increases linearly with field strength, leading to signal loss and geometric distortions, particularly in regions near tissue-air interfaces such as the orbitofrontal cortex and temporal lobes.
Effective B0 shimming is essential for high-quality imaging at 11.7T. The Iseult system employs second-order shimming using a brain mask and quadratic programming approach, achieving an average field homogeneity of 82.7 Hz standard deviation over the brain (0.17 ppm) [2]. For higher-order shimming, the system utilizes a 16-channel shim insert [25], which provides additional degrees of freedom to correct complex field inhomogeneities.
Table 1: Key Technical Challenges and Mitigation Strategies at 11.7T
| Challenge | Impact at 11.7T | Mitigation Strategy | Performance Metrics |
|---|---|---|---|
| B1+ Inhomogeneity | 45% coefficient of variation over whole brain | 16-channel parallel transmission with kT-points/GRAPE pulses | n.r.m.s.e. ≤13% over whole brain |
| SAR | Quadratic increase with field strength | Virtual Observation Points, SAR-constrained pulse design | Safe human imaging demonstrated |
| B0 Inhomogeneity | 0.17 ppm over brain without shimming | 2nd-order shimming with brain mask, 16-channel shim insert | 82.7 Hz standard deviation over brain |
| Acoustic Noise | Increased gradient interaction | Gradient coil optimization, passive damping | Slightly above enforced limits at certain frequencies |
Gradient Performance and Acoustic Noise
The Iseult 11.7T scanner incorporates a gradient system capable of 1500 mT/m maximum gradient strength [25], enabling high-resolution diffusion imaging. However, gradient-magnet interactions at 11.7T present uncharted challenges, as the powerful magnetic field can amplify vibrations and acoustic noise [10]. Acoustic measurements on the Iseult system show sound pressure levels slightly above enforced limits only at certain frequency intervals [10]. Vibration damping techniques and gradient waveform optimization help mitigate these effects, ensuring patient comfort and image quality.
Functional MRI Protocol Optimization
BOLD fMRI at 11.7T
Blood Oxygen Level Dependent (BOLD) functional MRI benefits significantly from the increased SNR and CNR at 11.7T. The higher field strength enhances magnetic susceptibility effects, leading to stronger BOLD contrast. Additionally, the spatial specificity of the BOLD signal improves as the venous contribution relative to the capillary contribution decreases [54].
For high-resolution BOLD fMRI, the following protocol parameters are recommended:
- Spatial Resolution: 0.5-0.8 mm isotropic, leveraging the increased CNR to resolve cortical layers and columns
- Parallel Imaging: Use high acceleration factors (R=3-4) with 64-128 channel receive arrays to maintain reasonable TR values
- RF Pulses: Employ pTx-tailored excitation pulses to ensure uniform flip angle distribution across the brain
- Echo Time (TE): Optimize for the specific tissue type and field strength (approximately 20-30 ms at 11.7T)
The NexGen 7T project demonstrates the potential of UHF fMRI, achieving resolutions sufficient to track neuronal activity across different cortical depths [9]. These advances are directly translatable to 11.7T systems, promising even greater spatial specificity for mapping brain function.
Arterial Spin Labeling (ASL) Perfusion Imaging
Arterial Spin Labeling provides a non-invasive method for quantifying cerebral blood flow (CBF). At 11.7T, the increased SNR and prolonged T1 relaxation times improve the sensitivity of ASL measurements [54].
Protocol optimization for ASL at 11.7T includes:
- Labeling Scheme: Pseudo-continuous ASL (pCASL) provides the best balance of SNR and labeling efficiency
- Post-Labeling Delay: Optimize based on the expected arterial transit time (approximately 1800-2000 ms)
- Background Suppression: Employ additional inversion pulses to minimize static tissue signal
- Readout: 3D GRASE or stack-of-spirits acquisitions with parallel imaging to minimize distortions
- Resolution: 1.0-1.5 mm isotropic, leveraging the increased SNR for higher spatial resolution CBF maps
Magnetic Resonance Spectroscopy (MRS)
11.7T provides significant advantages for MRS, including increased spectral dispersion and improved SNR [3]. This enables more reliable detection of low-concentration metabolites and the separation of overlapping resonances.
Optimal MRS protocols at 11.7T should incorporate:
- Voxel Size: 4-8 mL for single-voxel spectroscopy, 0.5-1.0 mL for spectroscopic imaging
- Water Suppression: Frequency-selective excitation schemes optimized for 11.7T
- Spectral Editing: Utilize the enhanced J-coupling and chemical shift dispersion for detecting GABA, glutathione, and other low-concentration metabolites
- B0 Shimming: Higher-order shimming is essential for achieving linewidths of <15 Hz
Diffusion MRI Protocol Optimization
High-Resolution Structural Connectivity
Diffusion MRI at 11.7T enables mapping of white matter architecture with unprecedented detail. The increased SNR can be leveraged to achieve higher spatial resolution or to increase the number of diffusion encoding directions for more accurate fiber orientation estimation [25].
Recommended protocol parameters for diffusion imaging:
- Spatial Resolution: 0.8-1.2 mm isotropic, compared to 1.5-2.5 mm at 3T
- b-values: Use multi-shell acquisitions (e.g., b=1000, 2000, 3000 s/mm²) to better characterize tissue microstructure
- Diffusion Directions: 64-128 directions per shell for robust orientation distribution function estimation
- Parallel Imaging: ACC factor of 2-3 to minimize TE and readout duration
- Simultaneous Multi-Slice: Acceleration factor of 2-3 to maintain feasible acquisition times
The Iseult system's high-performance gradients (1500 mT/m) enable shorter diffusion encoding times and reduced echo times, minimizing T2-related signal loss [25].
Advanced Diffusion Modeling
The enhanced SNR and angular resolution at 11.7T support more sophisticated diffusion modeling approaches:
- Neurite Orientation Dispersion and Density Imaging (NODDI): Multi-shell acquisitions with at least 2 b-value shells (typically b=1000 and 2500 s/mm²)
- Diffusion Kurtosis Imaging (DKI): Extends conventional diffusion tensor imaging to characterize non-Gaussian water diffusion
- Mean Apparent Propagator MRI (MAP-MRI): Provides a comprehensive characterization of water diffusion probabilities
Tractography and Connectomics
For brain connectome mapping, 11.7T offers significant advantages in resolving crossing fibers and mapping small white matter bundles:
- Fiber Tracking: Utilize constrained spherical deconvolution or multi-compartment models to resolve complex fiber geometries
- Probabilistic Tractography: Leverage the improved angular resolution to enhance tracking accuracy through regions of fiber crossing
- Resolution: The mesoscopic resolution achievable at 11.7T (0.2 mm in-plane) enables detailed mapping of intracortical connections [2]
Diagram 1: 11.7T Diffusion MRI and Tractography Workflow
Experimental Protocols for Preclinical Validation
Cerebral Blood Flow Measurement Using Phase-Contrast MRI
Phase-contrast MRI provides a non-invasive method for quantifying global cerebral blood flow (CBF). Optimization at 11.7T requires careful parameter selection based on vessel-specific flow characteristics [56].
Table 2: Optimized Phase-Contrast MRI Parameters for CBF Measurement at 11.7T
| Parameter | Internal Carotid Arteries | Vertebral Arteries | Rationale |
|---|---|---|---|
| VENC | 20 cm/s | 10 cm/s | Matches peak flow velocities (ICA: 13.8-14.4 cm/s, VA: 6.5-6.7 cm/s) |
| Spatial Resolution | 50 × 50 μm² | 50 × 50 μm² | Reasonable trade-off between partial volume effects and SNR |
| TR | 15 ms | 15 ms | Rapid spin replacement allows shorter TR without signal reduction |
| Acquisition Time | 96 seconds | 96 seconds | Enables CBF evaluation with test-retest variability of ~5% |
This optimized protocol enables quantification of global unit-volume CBF with high reproducibility (inter-rater correlation >0.95) and measured values of approximately 279.5 ± 11.1 mL/100g/min in mice [56]. Similar principles can be applied to human studies at 11.7T with appropriate scaling of parameters.
Brain Organoid Imaging for Disease Modeling
Human brain organoids provide a powerful 3D cellular model for studying brain development and disease. Diffusion MRI microscopy at 11.7T enables non-invasive, deep-tissue imaging of whole organoids without the need for tissue clearing [25] [57].
Sample Preparation Protocol:
- Fixation: Immerse organoids in 4% paraformaldehyde overnight at 4°C
- Cryoprotection: Transfer to 30% sucrose solution overnight
- Mounting: Secure organoids in specialized sample holders to prevent deformation during scanning
- Positioning: Center in RF coil using polyethylene tubing with PBS solution
Imaging Protocol:
- Field Strength: 11.7T vertical-bore superconducting magnet
- RF Coil: 5-mm transverse solenoid
- Resolution: ≤40 μm isotropic
- Contrast: T2-weighted and multishell 3D diffusion imaging
- Gradient Strength: 1500 mT/m maximum
- Application: Characterization of microstructural features in organoids modeling psychiatric disorders, neurodegenerative diseases, or viral infections [25]
This approach enables 3D visualization of organoid microstructure, including rosette-like internal structures and identification of specialized regions such as the choroid plexus, correlating with immunofluorescence findings [57].
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for 11.7T MRI Studies
| Item | Specifications | Function/Application | Example Use Cases |
|---|---|---|---|
| Hybrid Birdcage RF Coil | Multi-channel transmit/receive, optimized D/L ratio | B1+ field homogenization, improved signal sensitivity | Reference RF coil for 11.7T system performance validation [55] |
| Parallel Transmission System | 16-channel array, 2 kW per channel, virtual observation points | Mitigation of RF field inhomogeneity, SAR monitoring | Human brain imaging at 11.7T [2] |
| High-Performance Gradients | 1500 mT/m maximum strength, rapid switching | High-resolution diffusion encoding, reduced echo times | Diffusion tensor imaging, microstructural characterization [25] |
| Multi-Channel Receive Arrays | 64-128 channels, close-fitting design | Increased SNR, accelerated parallel imaging | High-resolution functional and diffusion MRI [9] |
| B0 Shim System | 16-channel second-order shim insert | B0 field homogenization, reduced susceptibility artifacts | All 11.7T applications, particularly MRS and fMRI |
| Head Stabilization System | Custom-fitted, motion-restricting | Minimization of motion artifacts | Long acquisitions for high-resolution mapping |
| Human Brain Organoids | iPSC-derived, 2-mm diameter spherical | Disease modeling, drug screening | Probing microstructural changes in psychiatric disorders [57] |
Future Directions and Applications in Neuroscience
The implementation of optimized protocols for 11.7T MRI opens new avenues for neuroscience research and drug development. The mesoscopic resolution achievable with this technology enables researchers to bridge the gap between macroscopic human brain imaging and microscopic findings from animal models [2]. Specific applications include:
- Neurodegenerative Disease Biomarkers: Detection of cortical lesions in multiple sclerosis, hippocampal substructure alterations in Alzheimer's disease, and iron content in basal ganglia for Parkinson's disease [2]
- Drug Development: Non-invasive assessment of drug efficacy in human brain organoid models [57]
- Cognitive Neuroscience: Mapping columnar and laminar organization in the cerebral cortex during cognitive tasks [9]
- Psychiatric Disorders: Identification of microstructural alterations in schizophrenia and bipolar disorders through enhanced MRS and diffusion imaging [3]
Future technical developments will focus on further improving image quality and acquisition efficiency. Key areas include advanced motion correction tools, highly accelerated sequences through compressed sensing and machine learning, more efficient RF coil designs, and the integration of artificial intelligence for image reconstruction and analysis [2] [54]. These advances will solidify the position of 11.7T MRI as an indispensable tool for unraveling the complexities of the human brain in health and disease.
Diagram 2: 11.7T MRI Technical Framework from Challenges to Applications
Validating Ultra-High Field Findings: Histological Correlations and Performance Benchmarks
This technical guide details the methodology and significance of post-mortem 11.7T diffusion tensor imaging (DTI) for validating microstructural changes in glioblastoma (GBM). Ultra-high field (UHF) MRI at 11.7T provides unprecedented resolution for detecting tumor infiltration beyond conventional imaging boundaries. This whitepaper outlines comprehensive experimental protocols for correlating DTI metrics with histopathological findings, presents quantitative results in structured tables, and visualizes complex workflows and relationships. The findings demonstrate that 11.7T DTI identifies significant myeloarchitectural alterations in GBM-infiltrated regions, validated through polarized light imaging (PLI) and luxol fast blue (LFB) staining. This approach establishes a rigorous framework for advancing neuro-oncological research and drug development by providing non-invasive biomarkers for tracking tumor progression and treatment response.
Ultra-high field (UHF) magnetic resonance imaging, operating at field strengths of 7 Tesla (7T) and above, represents a transformative technology in neuroscience research and neuro-oncology [58]. The pursuit of higher magnetic fields, such as 11.7T, is driven by the fundamental physical principle that signal-to-noise ratio (SNR) scales super-linearly with static magnetic field strength (B₀), enabling higher spatial resolution and enhanced tissue contrast [58] [33]. This technical advancement is particularly crucial for studying glioblastoma (GBM), the most aggressive primary brain tumor in adults, characterized by its highly infiltrative nature and microstructural complexity.
The clinical imperative for UHF MRI in GBM research stems from significant limitations in current standard imaging. Conventional 1.5T or 3T MRI fails to detect the full extent of tumor infiltration, leading to incomplete surgical resection and inaccurate radiation targeting [58]. Histopathological studies consistently demonstrate tumor cell presence well beyond abnormalities visible on standard MRI, explaining the high recurrence rates typical of GBM. UHF MRI addresses this critical gap by enabling visualization of microstructural changes at sub-millimeter resolution, providing a potential non-invasive method for detecting tumor infiltration before it becomes clinically apparent.
This whitepaper examines the specific application of 11.7T DTI for post-mortem GBM validation, correlating advanced imaging metrics with histological ground truth. By establishing precise structure-function relationships between DTI parameters and tissue pathology, this approach creates essential validation frameworks for translating UHF MRI biomarkers into clinical practice. The integration of 11.7T DTI with complementary techniques like PLI and LFB staining provides a multi-modal assessment of tumor-induced white matter alterations, offering researchers and drug development professionals powerful tools for evaluating therapeutic efficacy and disease progression.
Experimental Protocols and Methodologies
Tissue Preparation and Specimen Handling
The validation of 11.7T DTI findings requires meticulous tissue preparation to preserve microstructural integrity and ensure accurate imaging-histology correlation. The established protocol involves:
Specimen Collection: Post-mortem human brain specimens with confirmed GBM diagnosis are obtained through donor programs with appropriate ethical approvals. Three specimens typically provide sufficient data for initial validation studies [29].
Tissue Stabilization: Specimens are fixed in 10% neutral buffered formalin for a minimum of four weeks to ensure complete penetration and preservation of tissue architecture. This extended fixation prevents artifacts during subsequent imaging and histological processing.
Specimen Mounting: For MRI scanning, specimens are securely mounted in customized holders compatible with the 11.7T scanner bore. The use of perfluoropolyether (Fomblin) or similar susceptibility-matched fluids minimizes air-tissue interfaces and associated imaging artifacts.
Temperature Control: Throughout both imaging and storage periods, specimens are maintained at a constant temperature of 4°C to prevent tissue degradation and ensure measurement stability.
11.7T MRI Acquisition Parameters
The 11.7T DTI acquisition protocol is optimized for maximum contrast-to-noise ratio while maintaining practical scan durations:
Table 1: 11.7T DTI Acquisition Parameters
| Parameter | Specification | Rationale |
|---|---|---|
| Magnetic Field Strength | 11.7 Tesla | Maximizes signal-to-noise ratio and spatial resolution |
| Pulse Sequence | Diffusion-weighted spin-echo EPI | Optimal for DTI with minimal distortion |
| Spatial Resolution | 0.2-0.4 mm isotropic | Balances detail with acquisition time |
| Diffusion Directions | 30+ | Ensures robust tensor calculation |
| b-values | 0, 1000, 2000 s/mm² | Standard b-value + higher for restriction characterization |
| TR/TE | 6000/50 ms | Optimized for T2 and diffusion weighting |
| Averages | 4-8 | Improves signal-to-noise ratio |
The DTI protocol generates comprehensive datasets for calculating key diffusion metrics: fractional anisotropy (FA), mean diffusivity (MD), axial diffusivity (AD), and radial diffusivity (RD) [29]. These parameters are extracted from tensor calculations and mapped across the specimen for subsequent region-of-interest analysis.
Histological Processing and Staining Techniques
Histological validation employs complementary staining techniques to visualize different aspects of tumor pathology:
Hematoxylin and Eosin (HE) Staining: Standard HE staining provides overall cellularity assessment and basic tissue architecture. Nuclei are stained blue with hematoxylin, while cytoplasmic components appear pink with eosin. This staining enables identification of regions with high tumor cell density.
Luxol Fast Blue (LFB) Staining: LFB specifically targets myelin, staining intact myelin sheaths blue-green. This allows direct assessment of myeloarchitecture and visualization of demyelination patterns in tumor-infiltrated regions [29].
Polarized Light Imaging (PLI): PLI microscopy exploits the birefringent properties of myelin to visualize fiber orientation in unstained histological sections. PLI provides quantitative measurements of fiber alignment and density through retardance values [29].
All histological sections are precisely aligned with MRI data using fiduciary markers and custom registration algorithms to ensure accurate correlation between imaging and histology.
Data Analysis and Correlation Methods
The correlation methodology employs a rigorous multi-step process:
Region of Interest (ROI) Definition: ROIs are manually delineated on HE-stained sections based on nucleus density maps. Two primary ROI categories are defined: normal-appearing white matter (NWM) and regions with confirmed tumor infiltration [29].
Metric Extraction: DTI metrics (FA, MD, AD, RD), LFB optical density, and PLI retardance values are extracted from corresponding locations across all imaging modalities.
Statistical Comparison: Group-wise comparisons between NWM and tumor infiltration ROIs employ paired t-tests or Mann-Whitney U tests depending on data distribution. Significance is set at p < 0.05 with appropriate corrections for multiple comparisons.
Correlation Analysis: Linear regression models assess relationships between nucleus density, diffusion metrics, and myeloarchitectural parameters (LFB, PLI).
Diagram 1: Experimental workflow for 11.7T DTI-histology correlation
Key Findings and Quantitative Results
DTI Metric Alterations in Tumor Infiltration
Comparative analysis of DTI parameters reveals significant microstructural changes in GBM-infiltrated regions compared to normal white matter:
Table 2: DTI Metric Differences Between Normal White Matter and Tumor Infiltration
| DTI Metric | Normal White Matter | Tumor Infiltration | p-value | Biological Interpretation |
|---|---|---|---|---|
| Mean Diffusivity (MD) | Baseline | Significantly Increased | 0.036 | Elevated extracellular water content |
| Radial Diffusivity (RD) | Baseline | Significantly Increased | 0.010 | Myelin integrity disruption |
| Axial Diffusivity (AD) | Baseline | No Significant Change | >0.05 | Preserved axial fiber organization |
| Fractional Anisotropy (FA) | Baseline | Decreased (Trend) | >0.05 | Loss of structural directionality |
The significant increase in radial diffusivity specifically suggests myelin degradation, while elevated mean diffusivity indicates overall tissue disruption and increased water mobility in the extracellular space [29]. The preservation of axial diffusivity with increased radial diffusivity creates a distinctive diffusion profile for infiltrating tumor cells.
Histological Validation of Myeloarchitectural Changes
Quantitative histology confirms the DTI findings, demonstrating substantial alterations in myeloarchitecture:
Table 3: Histological Metric Comparisons
| Histological Metric | Normal White Matter | Tumor Infiltration | p-value |
|---|---|---|---|
| LFB Optical Density | Baseline | Significantly Decreased | 0.007 |
| PLI Retardance | Baseline | Significantly Decreased | <0.001 |
| Nucleus Density | Baseline | Significantly Increased | <0.001 |
The strong correlation between LFB values and PLI-retardance values (p < 0.001) validates both techniques as complementary measures of myelin content and organization [29]. This multi-modal histological approach provides a robust ground truth for interpreting DTI metric changes.
Correlation Patterns Between Imaging and Histology
Correlation analysis reveals distinctive relationships between imaging parameters and histological features:
Nucleus density shows significant correlation with diffusivity metrics (MD, RD) but not with myeloarchitectural measures (LFB, PLI) [29].
PLI-retardance values demonstrate strong correlation with LFB values (p < 0.001), confirming both techniques measure related aspects of myeloarchitecture [29].
The lack of correlation between nucleus density and myeloarchitectural changes suggests that cellular infiltration and myelin disruption, while spatially coincident, may represent partially independent pathological processes.
Diagram 2: Relationship between tumor infiltration and measurable changes
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of 11.7T DTI validation requires specialized materials and analytical tools:
Table 4: Essential Research Reagents and Materials
| Item | Specification | Application/Function |
|---|---|---|
| 11.7T MRI Scanner | Preclinical or specialized human system | Ultra-high resolution DTI data acquisition |
| Formalin Solution | 10% neutral buffered | Tissue fixation and preservation |
| Hematoxylin & Eosin | Histological grade | Cellular structure visualization |
| Luxol Fast Blue | Histochemical grade | Myelin-specific staining |
| PLI Microscope | Polarized light system with retardance measurement | Myelin fiber orientation quantification |
| Stereotactic Brain Matrix | Precision-machined alignment tool | Standardized sectioning for correlation |
| Image Registration Software | Multi-modal capability (e.g., ANTs, Elastix) | Alignment of MRI and histology data |
| Statistical Analysis Package | R, Python with neuroimaging libraries | Quantitative comparison of metrics |
Implications for Neuroscience Research and Drug Development
The validation of 11.7T DTI findings through histological correlation establishes crucial benchmarks for future research and therapeutic development. Several implications emerge from this integrated approach:
First, the identification of myeloarchitectural alterations as the primary driver of DTI changes in tumor-infiltrated regions provides a specific biological interpretation for non-invasive imaging biomarkers [29]. This enables more precise tracking of disease progression and treatment response in pre-clinical models and clinical studies.
Second, the multi-modal framework creates opportunities for evaluating novel therapeutic approaches targeting tumor invasion mechanisms. The ability to detect subtle microstructural changes before macroscopic tumor progression offers a sensitive metric for assessing drug efficacy in early development phases.
Third, the demonstrated correlation between PLI and DTI metrics suggests potential for translating ex vivo validation to in vivo applications. As UHF MRI becomes more accessible in clinical settings, these validated biomarkers could guide surgical planning and radiation targeting by revealing tumor infiltration beyond conventional imaging boundaries [58].
Future directions should focus on expanding these validation approaches to different GBM molecular subtypes, treatment-resistant populations, and earlier stages of tumor development. Integration with complementary techniques like magnetic resonance spectroscopy (MRS) and chemical exchange saturation transfer (CEST) imaging could provide additional dimensions of metabolic and molecular correlation.
Post-mortem 11.7T DTI validation with histological correlation represents a powerful paradigm for advancing glioblastoma research. The rigorous methodological framework outlined in this whitepaper enables precise characterization of tumor-induced microstructural changes, establishing validated imaging biomarkers for myeloarchitectural disruption. The significant differences in DTI metrics (MD, RD) and histological parameters (LFB, PLI) between normal white matter and tumor-infiltrated regions provide a robust foundation for interpreting in vivo imaging findings.
This multi-modal approach bridges the critical gap between cellular pathology and non-invasive imaging, offering researchers and drug development professionals a validated toolkit for investigating tumor biology and therapeutic efficacy. As ultra-high field MRI technology continues to evolve, these validation methodologies will play an increasingly essential role in translating imaging biomarkers from preclinical research to clinical application, ultimately contributing to improved outcomes for patients with this devastating disease.
{Abstract} The transition to ultra-high field (UHF) magnetic resonance imaging (MRI), defined as 7 Tesla (T) and above, represents a paradigm shift in neuroimaging. This technical guide benchmarks the quantitative gains in signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) afforded by UHF systems, with a specific focus on the nascent potential of 11.7T human scanners. We detail the fundamental physics underlying these gains, provide structured quantitative comparisons, outline essential experimental protocols for leveraging these advantages, and visualize the core concepts. Framed within the context of advanced neuroscience research and drug development, this whitepaper serves as a foundational resource for scientists seeking to utilize UHF MRI for unparalleled spatial resolution and biochemical sensitivity in studying the individual human brain.
{1. Introduction: The UHF MRI Paradigm} The drive towards higher magnetic field strengths is fundamentally motivated by the need to visualize the brain's complex structure and function at an increasingly granular level. The human brain operates at a microscopic scale, with functional units like cortical columns and layers measuring hundreds of microns [59]. While conventional 3T MRI scanners have been instrumental in neuroscience, their resolution limits often obscure this fine-grained organization. UHF MRI, particularly systems operating at 7T, 10.5T, and the recently unveiled 11.7T Iseult scanner, directly addresses this limitation by providing substantial gains in SNR and CNR [40] [60] [59]. These gains are not merely incremental; they are transformative, enabling a shift from group-level studies to precision neuroimaging of single individuals over multiple sessions [61]. For researchers and drug development professionals, this means an enhanced capacity to detect subtle pathological changes, map metabolic pathways with superior spectral resolution, and identify previously occult biomarkers of neurological disease, thereby accelerating therapeutic discovery.
{2. Theoretical Foundations of SNR and CNR at UHF} The core advantage of UHF MRI stems from the fundamental relationship between the static magnetic field (B₀) and the induced signal. SNR is the key determinant of image quality, governing the ability to distinguish true signal from stochastic noise.
2.1 Signal-to-Noise Ratio (SNR): The NMR signal is proportional to the net magnetization, which, at equilibrium, scales linearly with B₀. Noise in MRI originates primarily from stochastic molecular movement in the subject (body noise) and electronic resistance in the receiver coil. The standard theoretical model indicates that SNR increases approximately linearly with field strength (SNR ∝ B₀) [40] [62] [63]. In practice, this linear gain allows for a cubic improvement in spatial resolution, as SNR can be traded for smaller voxel volumes [59].
2.2 Contrast-to-Noise Ratio (CNR): While SNR measures signal against background noise, CNR measures the difference in signal between two tissues against the same background noise (CNR = (Signal₁ - Signal₂) / Noise). UHF MRI enhances CNR by altering tissue relaxation times (T1, T2, T2), which directly impacts image contrast. T1 relaxation times lengthen at higher fields, improving contrast in techniques like time-of-flight (TOF) angiography and arterial spin labeling. Conversely, T2 relaxation times shorten significantly, dramatically enhancing the sensitivity to magnetic susceptibility differences [40] [12]. This underlies the superior performance of UHF in susceptibility-weighted imaging (SWI), blood oxygenation level-dependent (BOLD) functional MRI, and the detection of iron and calcium deposits.
2.3 Technical Challenges: The benefits of UHF are accompanied by technical challenges that must be managed. These include increased B₁⁺ radiofrequency (RF) transmit field inhomogeneity, a higher specific absorption rate (SAR), and heightened susceptibility artifacts at tissue-air interfaces. Modern solutions, such as parallel transmission (pTx) RF systems and universal pulses (UP), are critical for mitigating these issues and realizing the full potential of UHF gains [40] [60].
{3. Quantitative Benchmarking Tables} The following tables synthesize the quantitative gains and performance metrics of UHF MRI compared to standard field strengths.
Table 1: Quantitative Gains in SNR and Physiologic Parameters at Different Field Strengths
| Parameter | 1.5T | 3T | 7T | 11.7T (Theoretical/Initial) |
|---|---|---|---|---|
| Theoretical SNR Gain (vs. 1.5T) | 1x | ~2x | ~4-5x | ~7-8x |
| Typical Anatomical Resolution | 1x1x1 mm³ | 1x1x1 mm³ | 0.5x0.5x0.5 mm³ [59] | Sub-0.5 mm³ [60] |
| Typical fMRI Resolution | 3-4 mm isotropic | 2-3 mm isotropic | ~1 mm isotropic [59] | <1 mm isotropic |
| T1 Relaxation Time | Reference | Increases | Increases further [40] | Longest |
| T2* Relaxation Time | Reference | Decreases | Shortens significantly [40] [12] | Shortest |
Table 2: Comparative CNR and Application Performance
| Imaging Application | Performance at 3T | Performance at 7T/UHF | Key Quantitative Benefit |
|---|---|---|---|
| BOLD fMRI | Good sensitivity and resolution | High sensitivity and specificity [59] | Increased CNR for functional activation [40] |
| Susceptibility-Weighted (SWI) | Detects larger microhemorrhages | Exquisite detail of venules and microbleeds [12] | Greater phase contrast, improved CNR [40] |
| Time-of-Flight (TOF) MRA | Good visualization of major arteries | Delineation of small arterial branches [12] | Enhanced background suppression, superior CNR |
| MR Spectroscopic Imaging (MRSI) | Resolution of major metabolites (e.g., Cho, NAA) | Detection of more metabolites with improved quantification [12] | Increased spectral separation (∝ B₀) and SNR |
| Sodium (²³Na) MRI | Limited by very low SNR | Feasible for quantifying tissue sodium concentration [12] [60] | Massive SNR boost for non-proton nuclei |
UHF MRI Gains Logic
{4. Experimental Protocols for UHF Neuroscience} To quantitatively benchmark UHF systems, specific experimental protocols are employed. The following details a multimodal approach, as used in recent precision imaging studies [61].
4.1 High-Resolution Structural Protocol
- Objective: To acquire anatomical data with high SNR for cortical segmentation and morphometry at the individual level.
- Sequence: 3D-MP2RAGE (Magnetization-Prepared 2 Rapid Acquisition Gradient Echoes).
- Key Parameters (7T Example): Isotropic voxel = 0.5 mm; TR = 5170 ms; TE = 2.44 ms; TI1/TI2 = 1000/3200 ms; Parallel Imaging (iPAT) = 3 [61].
- Benchmarking Method: Compare the visibility of hippocampal subfields, amygdalar nuclei, and gray-white matter boundary sharpness against identical sequences at 3T. The gain in SNR allows for robust segmentation of these structures without the need for group-level averaging.
4.2 High-Fidelity Functional Protocol
- Objective: To achieve high spatial resolution mapping of brain function and networks.
- Sequence: Multi-echo BOLD fMRI (echoplanar imaging).
- Key Parameters (7T Example): Isotropic voxel = 1.9 mm; TR = 1690 ms; Multiple TEs (e.g., 10.80, 27.3, 43.8 ms); Multiband acceleration (MB) = 3 [61].
- Benchmarking Method: Quantify the temporal SNR (tSNR) and BOLD CNR during a task or resting state. UHF systems demonstrate a significant increase in tSNR and greater sensitivity to activation in small, deep brain structures compared to 3T [40] [59]. Multi-echo acquisition helps isolate the BOLD signal from artifacts.
4.3 Quantitative Microstructural and Metabolic Protocol
- Objective: To characterize tissue properties such as myelin, iron, and metabolic concentration.
- Sequences:
- Magnetization Transfer (MT): Sensitive to myelin content.
- Multi-echo Gradient Echo (ME-GRE): Sensitive to iron deposition via T2* mapping.
- MR Spectroscopic Imaging (MRSI): For quantifying neuro-metabolites.
- Benchmarking Method: At 11.7T, the greatly increased spectral dispersion allows for clear separation of overlapping metabolite peaks (e.g., glutamate and glutamine) that are difficult to resolve at lower fields [12] [60]. Similarly, quantitative T2* and MT maps exhibit higher precision and dynamic range.
{5. The Scientist's Toolkit: Essential Research Reagents & Hardware} Successful UHF MRI research relies on a suite of specialized hardware and software "reagents."
Table 3: Essential Research Toolkit for UHF MRI Neuroscience
| Tool Category | Specific Item / Technology | Function & Importance |
|---|---|---|
| RF Coil Systems | 32-channel receive / 8-transmit channel head coil [61] | High-density arrays maximize signal reception; multi-transmit (pTx) mitigates B₁⁺ inhomogeneity, a critical requirement at UHF. |
| Pulse Sequences | Universal Pulses (UP) for pTx [60] | Pre-computed RF pulses that provide robust flip angle homogeneity across a population, ensuring reproducibility. |
| Advanced Reconstruction | Parallel Imaging (e.g., GRAPPA), Compressed Sensing, Deep Learning | Algorithms that mitigate artifacts, reduce scan times, and denoise images, compensating for some UHF challenges. |
| Multi-Nuclear Capability | Dedicated RF coils for ²³Na, ³¹P [12] [60] | Essential for probing cell energetics and sodium homeostasis, benefiting enormously from the SNR boost at UHF. |
| Precision Imaging Software | Dedicated pipelines for multi-session data alignment and connectome generation [61] | Enables the integration of structural, functional, and metabolic data across multiple scans for individual-level brain mapping. |
{6. Conclusion} Benchmarking studies conclusively demonstrate that ultra-high field MRI provides substantial and non-linear gains in SNR and CNR relative to conventional field strengths. The initial in vivo human imaging at 11.7T confirms the feasibility of pushing these gains even further, opening new horizons for neuroscience [60]. These quantitative advantages translate directly into the ability to resolve the human brain's architecture and functional organization at a sub-millimeter scale in individual participants. For the research and pharmaceutical development community, the adoption of UHF MRI is no longer a mere incremental improvement but a strategic imperative for uncovering novel disease mechanisms, validating therapeutic targets, and developing sensitive biomarkers for clinical trials. The future of personalized neuroscience and neurology will be fundamentally shaped by the resolution and sensitivity afforded by ultra-high fields.
The pursuit of higher magnetic field strengths in magnetic resonance imaging (MRI) represents a fundamental pathway to advancing human neuroscience research. Ultra-high-field (UHF) MRI systems provide a supralinear gain in signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR), enabling researchers to visualize the human brain at an unprecedented mesoscopic scale—bridging the gap between macroscopic brain mapping and microscopic cellular analysis [10] [2]. This technical guide provides a detailed comparative analysis of two pioneering platforms at the forefront of this endeavor: the Iseult 11.7 Tesla (T) whole-body scanner and the Next-Generation (NexGen) 7T head-only scanner. Both systems push the boundaries of magnetic field strength and hardware engineering, yet they embody distinct philosophical approaches to advancing neuroimaging capabilities. Their architectural differences reflect specialized optimizations for specific research applications within neuroscience, from mapping cortical layer activity to identifying novel biomarkers in neurodegenerative disease [9] [20].
The transition to UHF MRI brings distinct physical challenges that both systems must address. As the static magnetic field (B0) increases, the radiofrequency (RF) wavelength decreases, leading to B1+ inhomogeneity that can cause imaging artifacts [64]. Additionally, specific absorption rate (SAR) management becomes more critical due to increased tissue heating, while maintaining magnetic field homogeneity requires more sophisticated engineering solutions [2] [64]. Understanding how each platform addresses these fundamental physical constraints is essential for researchers selecting the appropriate tool for specific neuroscience applications.
System Architectures & Technical Specifications
Iseult 11.7T MRI Scanner
The Iseult 11.7T MRI scanner, developed by the French Alternative Energies and Atomic Energy Commission (CEA) in collaboration with Siemens Healthineers, represents a monumental achievement in magnet technology [10] [2]. As the world's most powerful MRI scanner approved for human imaging, its core architecture centers on a 132-ton actively shielded NbTi magnet cooled by a superfluid helium bath at 1.8 K [10] [6]. This cryogenic operating temperature is notably lower than conventional MRI magnets (which typically operate at 4.2 K) and is essential for maintaining cryostability in such a high-field system [10]. The magnet incorporates 182 km of superconducting wires and requires approximately 7,500 liters of superfluid helium, creating a stable magnetic field of 11.72 T with remarkable homogeneity (<0.5 ppm peak-to-peak over a 22-cm-diameter spherical volume) and temporal stability (0.05 ppm/hour drift) [10] [2].
Unlike conventional MRI systems that operate in persistent mode, the Iseult magnet operates in driven mode, meaning it remains connected to its power supply during operation [10]. This design decision stems from the technical challenges of creating superconducting joints with the multi-strand wire configuration used in the magnet. The system employs a sophisticated Magnet Safety System (MSS) based on voting redundancy (2oo3 logic) to ensure operational reliability, a concept more commonly used in particle detector magnets than medical imaging systems [10]. For RF transmission, the Iseult system utilizes a parallel transmission (pTx) system with 16 transmit elements and dedicated virtual observation points for SAR monitoring, which is essential for mitigating the pronounced RF field inhomogeneity challenges at 500 MHz (the Larmor frequency for protons at 11.7 T) [2].
Next-Generation 7T MRI Scanner
The NexGen 7T scanner, developed through an international collaboration directed by David Feinberg and funded by the NIH BRAIN Initiative, takes a different architectural approach by focusing on performance enhancements beyond the main magnetic field [9] [20]. While utilizing a standard 7T magnet, the system incorporates groundbreaking advancements in gradient performance and RF receiver technology specifically optimized for human brain imaging [20] [65]. The cornerstone of this system is the "Impulse" head-only asymmetric gradient coil that incorporates a novel three-layer winding design—adding an intermediate layer between the primary and secondary windings found in conventional gradient coils [20].
This innovative gradient design achieves unprecedented performance metrics of 200 mT/m maximum amplitude and 900 T/m/s slew rate, representing an order of magnitude improvement in performance (Gmax × SR) over standard 7T whole-body gradient coils and approximately five times the performance of previous generation head-only gradients [20]. The three-layer design provides additional degrees of freedom for simultaneously optimizing gradient field linearity, reducing peripheral nerve stimulation (PNS), and managing mechanical resonances and torque [20]. The cooling system also diverges from conventional approaches, using stainless-steel tubing surrounded by conductive filaments rather than hollow copper conductors [20].
For signal reception, the NexGen 7T integrates a 128-channel receiver system with both 64- and 96-channel receiver coil arrays, significantly increasing channel count compared to the standard 32-channel arrays typically used on conventional 7T scanners [9] [20]. These arrays feature reduced coil loop diameters (approximately 4 cm) to boost signal detection in the cerebral cortex [20]. The system also incorporates a 16-channel transmit system to reduce power deposition and improve image uniformity [20] [65].
Table 1: Core System Specifications Comparison
| Parameter | Iseult 11.7T Scanner | Next-Generation 7T Scanner |
|---|---|---|
| Magnetic Field Strength | 11.7 T | 7 T |
| Magnet Type | Actively shielded NbTi, whole-body | Not specified, head-only |
| Operating Temperature | 1.8 K with superfluid helium | Standard cryogenic (likely 4.2 K) |
| Magnet Weight | 132 tons | Not specified |
| Gradient Performance | Not specified (whole-body constraints) | 200 mT/m amplitude, 900 T/m/s slew rate |
| Gradient Coil Design | Standard whole-body | 3-layer asymmetric head-only "Impulse" coil |
| Receiver Channels | Not specified (pTx system with 16 transmit elements) | 128 channels with 64/96-channel arrays |
| Primary Imaging Target | Whole-body with brain focus | Head-only |
| Estimated Cost | Not specified (very high) | $22 million (USD) in development funding |
Comparative Technical Analysis
When comparing these two platforms, the fundamental distinction lies in their primary approach to enhancing spatial resolution. The Iseult system leverages the inherent SNR advantage of its higher field strength, which scales approximately linearly with B0, providing roughly 1.67 times the theoretical SNR of a 7T system [64]. In practice, this enables the Iseult scanner to achieve resolutions of 0.19 × 0.19 × 1 mm³ in just 4-5 minute acquisitions, a feat that would require hours-long sessions on conventional 1.5-3T hospital scanners [2] [66].
The NexGen 7T scanner, while operating at lower field strength, compensates through revolutionary gradient performance and high-density receiver arrays. The improved gradient system enables shorter echo spacing (0.58 ms at 0.6 mm isotropic resolution compared to 1.21 ms with standard body gradients), reducing T2* signal decay and geometric distortion while allowing shorter echo times for increased signal [20]. The high-channel-count arrays provide approximately 30% improvement in SNR in cortical regions compared to standard 32-channel arrays, while simultaneously reducing g-factor noise for higher parallel imaging acceleration [20].
Table 2: Performance Metrics and Research Applications
| Performance Metric | Iseult 11.7T Scanner | Next-Generation 7T Scanner |
|---|---|---|
| Spatial Resolution (Demonstrated) | 0.19 × 0.19 × 1 mm³ in 4-5 minutes [2] [6] | 0.35-0.45 mm isotropic for fMRI [20] [65] |
| Temporal Resolution | Not specified (enables shorter scan times) | Improved via higher parallel imaging acceleration |
| fMRI Applications | Potential for mesoscale functional imaging | Cortical layer-specific fMRI (0.5 mm) [20] |
| SNR Advantage | Supralinear gain from 11.7T field [2] | 30% cortical SNR improvement from arrays [20] |
| CNR Advantage | Enhanced for susceptibility-weighted contrasts | Improved for cortical layer differentiation [20] |
| Specialty Contrasts | Lithium distribution tracking [66] | Laminar diffusion imaging [20] |
| Clinical Translation | Neurodegenerative disease biomarker identification [6] | Neuroscience research with clinical potential [9] |
Experimental Methodologies & Research Protocols
Imaging Protocol Design for Mesoscale Neuroscience
Iseult 11.7T Imaging Protocol
The Iseult system requires specialized protocols to address UHF-specific challenges. For T2*-weighted imaging, researchers employ 2D gradient echo sequences with the following parameters: in-plane resolution of 0.19 × 0.19 mm² with 1 mm slice thickness, acquisition time of 4 minutes 17 seconds [2] [6]. To mitigate B1+ inhomogeneity, the protocol must incorporate parallel transmission techniques with kT-points or GRAPE (gradient ascent pulse engineering) pulse designs [2]. Static B0 shimming is performed up to second order for each participant using a brain mask and quadratic programming approach, typically achieving approximately 83 Hz standard deviation over the brain (0.17 ppm) [2].
For anatomical imaging, 3D T2 variable flip angle turbo spin-echo acquisitions provide high-resolution structural data. The system's exceptional homogeneity and field stability (0.05 ppm/hour drift) enable extended acquisitions without significant image degradation [10] [2]. RF pulse design must incorporate explicit SAR management through virtual observation points, with excitation pulses typically achieving normalized root mean square errors (n.r.m.s.e.) of 8% over the whole brain, and refocusing pulses achieving approximately 13% n.r.m.s.e. [2].
NexGen 7T Imaging Protocol
The NexGen 7T system leverages its enhanced gradients for high-resolution functional and diffusion imaging. For cortical layer fMRI, researchers utilize echo-planar imaging (EPI) with 0.35-0.45 mm isotropic resolution, enabled by the Impulse gradient's short echo spacing (0.58-0.68 ms for 0.5-0.6 mm resolution) [20]. This reduces T2* blurring (point spread function) compared to conventional gradients, with the Impulse coil maintaining minimal PSF up to 0.5 mm resolution, whereas standard whole-body gradients show increased PSF beyond 0.7 mm resolution [20].
For diffusion imaging, the high gradient performance (200 mT/m) enables high angular resolution diffusion imaging (HARDI) with enhanced sensitivity to complex white matter architecture [20]. The protocol typically uses multi-band acceleration combined with the high-density receiver arrays (96-channel) to reduce scan times while maintaining spatial resolution. The system's PNS-optimized design allows higher slew rates without exceeding stimulation thresholds, which is particularly beneficial for diffusion spectrum imaging (DSI) and other advanced diffusion techniques [20].
Safety and Operational Protocols
Iseult 11.7T Safety Protocol
Human imaging at 11.7T requires rigorous safety validation. The approved protocol includes comprehensive physiological monitoring (blood pressure, heart rate), vestibular assessment, cognitive testing, and genotoxicity evaluation (chromosomal damage analysis from blood samples) [2] [6]. Studies with 20 participants scanned for 90 minutes at 11.7T showed no significant differences compared to a 0T control group across all safety metrics [2]. All scans must operate in "First Level Controlled Operating Mode" with medical supervision due to elevated RF and gradient fields [67]. Specific absorption rate (SAR) monitoring is critical, requiring real-time calculation and management through virtual observation points [2].
NexGen 7T Safety Protocol
While operating at lower field strength, the NexGen 7T still requires careful safety protocols due to its high-performance gradients. The PNS supervision model was adapted based on healthy participant stimulation thresholds, with operating curves specifically calibrated for the Impulse coil [20]. Acoustic noise management is essential, with sound levels reaching 120.6 dB(A) for all axes combined, requiring hearing protection with at least 28-33 dB attenuation [20]. The system maintains SAR within safety limits through the 16-channel transmit system, which distributes power deposition more evenly than single-channel transmission [20].
Research Applications in Neuroscience
Cortical Layer and Columnar Imaging
The NexGen 7T scanner demonstrates exceptional capability for cortical layer-specific fMRI, routinely achieving 0.35-0.45 mm isotropic resolution to resolve neural activity across different cortical depths [20]. This enables researchers to track the direction of information transmission between brain areas by observing differential activation across cortical layers—a capability previously unavailable in human neuroscience [9] [20]. The high spatial resolution minimizes partial volume averaging between gray matter, white matter, and cerebrospinal fluid, essential for accurate interpretation of laminar activation patterns [20].
The Iseult 11.7T scanner provides complementary advantages for mesoscopic-scale cortical imaging, with its higher inherent SNR enabling even finer spatial sampling [2]. While comprehensive layer-fMRI results have not yet been published, the system's resolution capabilities (0.19 mm in-plane) suggest potential for visualizing cortical columnar organization and microvascular architecture that remains challenging at lower field strengths [2] [6].
Neurodegenerative Disease Biomarkers
Both systems offer significant potential for identifying novel biomarkers in neurodegenerative diseases. The Iseult 11.7T's enhanced susceptibility contrast enables superior visualization of iron accumulation in disorders like Parkinson's disease and amyotrophic lateral sclerosis (ALS) [6] [67]. The system can detect the "motor band sign"—a rim-like cortical hypointensity reflecting iron-laden microglia in the primary motor cortex of ALS patients—with greater clarity than lower-field systems [67]. Additionally, the system's sensitivity enables tracking of lithium distribution in bipolar disorder patients, potentially revealing mechanisms of treatment response [66].
The NexGen 7T contributes to neurodegenerative research through high-resolution diffusion imaging of white matter integrity and functional connectivity alterations in early disease stages [20]. The combination of high SNR and enhanced diffusion weighting provides superior characterization of microstructural changes in conditions like Alzheimer's disease and frontotemporal dementia [20].
Epilepsy and Surgical Planning
In epilepsy research, both systems offer advantages for identifying subtle malformations that often escape detection at conventional field strengths. The Iseult 11.7T can potentially identify focal cortical dysplasia and other epileptogenic lesions that are missed in 15-40% of refractory epilepsy patients using 1.5T or 3T MRI [6]. The NexGen 7T similarly enhances lesion detection, with its high-resolution structural and functional capabilities providing improved localization of epileptic networks for surgical planning [67].
Cerebrovascular Imaging
The exceptional susceptibility weighting at 11.7T makes the Iseult system ideally suited for cerebral microbleed detection and microvascular imaging [6]. This has implications for understanding cerebral amyloid angiopathy, traumatic brain injury (diffuse axonal injury), and hemorrhagic transformations [6]. The system's resolution enables visualization of venous structures and microvascular patterns that may serve as biomarkers for conditions like brain tumors, stroke recovery, and neurodegenerative diseases [2] [6].
Implementation Considerations for Research Institutions
Infrastructure and Cost Analysis
The Iseult 11.7T scanner presents monumental infrastructure requirements, including a 132-ton magnet requiring a dedicated cylindrical hall (10 m diameter, 15 m length) and sophisticated cryogenic support systems [10] [2]. The system consumes 7,500 liters of superfluid helium, requiring an on-site cryogenic plant and specialized commissioning expertise [10] [2]. These requirements result in extremely high capital and operational costs, currently limiting deployment to specialized national research facilities like the CEA Paris-Saclay center [10] [6].
The NexGen 7T scanner, while still requiring substantial investment ($22 million in development funding), represents a more feasible implementation target for academic medical centers [9]. The system utilizes a standard 7T magnet footprint, potentially enabling installation in existing MRI suites with appropriate shielding [9] [20]. The head-only design reduces some infrastructure demands while focusing capabilities on the neuroscientific applications of greatest interest to most researchers [20].
Dissemination and Accessibility
The NexGen 7T platform demonstrates a clearer pathway to broader dissemination, with Siemens Healthineers and MR CoilTech Ltd. planning to distribute systems to neuroscience imaging centers worldwide [9]. This accessibility model aligns with the project's goal of enabling "as many expert neuroscientists as possible to do as many experiments as possible" [9]. In contrast, the Iseult 11.7T remains a unique resource with limited accessibility, though its technological developments will likely influence future commercial UHF systems [2] [68].
Experimental Workflow
The following diagram illustrates the key decision points for researchers selecting between these platforms for neuroscience applications:
Core Imaging Technologies
Table 3: Essential Research Reagents & Solutions
| Resource | Function/Application | Implementation Examples |
|---|---|---|
| Parallel Transmission (pTx) Systems | Mitigates B1+ inhomogeneity at UHF through multi-channel RF transmission | Iseult: 16-channel pTx with virtual observation points for SAR management [2] |
| High-Density Receiver Arrays | Increases SNR and parallel imaging acceleration through dense coil positioning | NexGen 7T: 96-channel array with 4cm loop diameter for cortical signal [20] |
| Advanced Gradient Coils | Enables higher spatial resolution and faster encoding through increased amplitude/slew rate | NexGen 7T: 3-layer "Impulse" coil (200 mT/m, 900 T/m/s) [20] |
| Field Monitoring Systems | Tracks temporal field fluctuations for image quality assurance | Iseult: Field monitoring to identify mechanical resonances [10] |
| SAR Management Solutions | Controls tissue heating through real-time power deposition monitoring | Both systems: Virtual observation points and predictive algorithms [2] |
| B0 Shimming Solutions | Maintains field homogeneity across brain regions through active compensation | Iseult: Second-order shimming with quadratic programming [2] |
Pulse Sequences and Reconstruction Methods
kT-points Pulses: Spatially tailored RF pulses that mitigate B1+ inhomogeneity by applying a small number of RF pulses with different k-space locations [2]. Essential for Iseult 11.7T imaging to achieve homogeneous excitation across the brain.
GRAPE Algorithm: Gradient Ascent Pulse Engineering algorithm for designing optimized RF pulses that account for hardware constraints while achieving target excitation profiles [2]. Used for refocusing pulses at 11.7T.
Echo Planar Imaging (EPI) Optimization: Modified EPI sequences leveraging high-performance gradients for reduced echo spacing and echo train lengths [20]. Critical for high-resolution fMRI on the NexGen 7T system.
Parallel Imaging Reconstruction: Advanced reconstruction algorithms (e.g., GRAPPA, SENSE) that leverage multi-channel coil information for accelerated acquisition [20]. Enhanced on NexGen 7T through reduced g-factor noise from high-density arrays.
The Iseult 11.7T and Next-Generation 7T scanners represent complementary technological paradigms for advancing human neuroscience research. The Iseult system demonstrates that extreme field strength (11.7T) is technically feasible for human imaging and provides unmatched intrinsic SNR for anatomical and susceptibility-weighted imaging at mesoscopic resolutions [2] [6]. The NexGen 7T system showcases how sophisticated gradient and receiver array technology can push functional and diffusion imaging capabilities beyond what is achievable through field strength alone, enabling cortical layer-specific fMRI and high-angular resolution diffusion imaging [20] [65].
For the neuroscience research community, selection between these platforms involves careful consideration of research priorities, infrastructure resources, and accessibility. The Iseult 11.7T offers a unique national resource for anatomical mapping and novel contrast mechanism exploration, while the NexGen 7T provides a more distributable platform for functional and microstructural imaging [9] [68]. Both systems will drive the field toward finer spatial and temporal resolution, potentially transforming our understanding of brain organization in health and disease. As these technologies mature and disseminate, they will empower neuroscientists to address fundamental questions about human brain function at increasingly precise scales, from cortical layers and columns to individual axonal pathways and microvascular networks.
Validating Microstructural Changes in Disease Models with Polarized Light Imaging
Understanding microstructural changes in disease models is a cornerstone of modern neuroscience and drug development. Polarized Light Imaging (PLI) has emerged as a powerful, high-resolution technique for visualizing the ordered architecture of neural tissues, such as myelinated axons, which exhibit birefringent properties. This technical guide outlines how PLI can be utilized to validate microstructural findings, serving as a complementary validation tool for ultra-high-field magnetic resonance imaging (MRI), specifically 11.7 Tesla (T) systems. The recent advent of human 11.7T MRI, such as the Iseult system, enables the acquisition of brain images at a mesoscopic scale, revealing details within the cortical ribbon and cerebellar structures that were previously unresolvable with lower-field systems [2] [5]. However, interpreting the microstructural underpinnings of the MRI signal requires validation by a direct, label-free optical method. PLI, with its sensitivity to fiber directionality and capability to resolve features at a micrometer resolution, provides this critical link, offering a pathway to ground-truth the revolutionary, non-invasive insights provided by ultra-high-field MRI in both healthy and diseased brain models [69].
Technical Foundations of Polarized Light Imaging
Core Physical Principles
Polarized Light Imaging leverages the interaction between polarized light and optically anisotropic materials. In the context of neural tissue, the key anisotropy arises from the birefringence of the myelin sheath surrounding axons. Birefringence is an optical property of a material that has a refractive index that depends on the polarization and propagation direction of light [70] [71]. When unpolarized light passes through a polarizing filter (the polarizer), it becomes plane-polarized. As this polarized light interacts with a birefringent specimen, it is split into two perpendicular wave components: the ordinary and extraordinary rays. These rays travel at different velocities through the material, accumulating a phase shift (retardance). A second polarizing filter, called the analyzer, is placed after the specimen, typically in a crossed orientation (90 degrees) to the polarizer. The analyzer recombines these out-of-phase components, resulting in constructive and destructive interference that translates the specimen's birefringence into measurable contrast and intensity in the final image [71]. This allows for the visualization of sub-resolution microstructural details and the determination of the directionality (axis) of fibers [69].
PLI System Configuration
A standard PLI microscope requires several key components beyond a conventional brightfield microscope [71]:
- Polarizer: Positioned in the light path before the specimen.
- Analyzer: A second polarizer placed between the objective and the camera or eyepieces.
- Strain-Free Optics: Objectives and condensers specifically designed to avoid introducing spurious birefringence, often marked with P, PO, or Pol.
- Rotating Stage: A precision 360-degree circular stage to orient the specimen for orientation studies.
- Compensator Slot: Allows for the insertion of waveplates to enhance or quantify optical path differences.
For advanced biomedical applications, including backscattering (reflected light) imaging of bulk tissues, systems evolve into full Mueller matrix polarimeters. These systems can fully characterize the polarization-changing properties of a sample by measuring all 16 elements of the Mueller matrix, from which derived quantities like retardance, diattenuation, and depolarization can be calculated [69] [72].
Table 1: Key Optical Properties Measured in Polarized Light Imaging
| Optical Property | Description | Microstructural Correlation |
|---|---|---|
| Retardance (δ) | The phase shift induced between ordinary and extraordinary waves. | Indicator of birefringence strength, related to fiber density and myelin integrity [69] [72]. |
| Fast-Axis Orientation | The principal direction of birefringence at each pixel. | Reveals the in-plane orientation and alignment of fibrous structures (e.g., axon tracts) [72]. |
| Depolarization (Δ) | The extent to which a material randomizes the polarization state of incident light. | Associated with structural heterogeneity, such as densely packed cell nuclei or tissue disorganization [69] [72]. |
| Diattenuation (d) | The differential attenuation of light along different polarization axes. | Related to anisotropic absorption or scattering [69]. |
PLI and Ultra-High Field MRI: A Complementary Framework
The 11.7T MRI Benchmark
The Iseult 11.7T MRI scanner represents a monumental leap in imaging capability. Its immense magnetic field strength provides a supralinear gain in signal-to-noise ratio (SNR), which can be invested into vastly improved spatial resolution. It has achieved in vivo human brain images with a resolution of 0.19 x 0.19 x 1 mm³ in acquisition times as short as four to five minutes [2] [6] [5]. This mesoscopic resolution brings MRI closer than ever to visualizing the brain's micro-architecture, including cortical layers and fine anatomical details. The enhanced SNR and spectral separation at 11.7T also profoundly benefit other applications like functional MRI (fMRI), diffusion MRI, and magnetic resonance spectroscopic imaging (MRSI), which can track metabolites like glutamate and glucose [5] [37]. Furthermore, the heightened magnetic susceptibility contrast at 11.7T improves the detection of iron content and deoxyhemoglobin, directly benefiting BOLD fMRI and the study of conditions like Parkinson's disease [6] [37].
The Synergy of PLI and MRI
While 11.7T MRI provides unprecedented non-invasive visualization of the living brain, its resolution is still orders of magnitude coarser than the microscopic scale of individual axons and cells. This is where PLI becomes an indispensable partner in the validation pipeline, bridging the resolution gap between MRI and histology.
Table 2: Comparative Analysis of 11.7T MRI and Polarized Light Imaging
| Feature | 11.7T MRI | Polarized Light Imaging (PLI) |
|---|---|---|
| Resolution | Mesoscopic (~0.2 mm isotropic) [2] | Microscopic (~10 µm) [69] |
| Imaging Depth | Whole human brain | Surface/near-surface (or thin sections) |
| Key Contrasts | T1, T2, T2*, BOLD, Diffusion, Metabolites | Retardance, Fast-axis orientation, Depolarization |
| Sample Preparation | In vivo, non-invasive | Ex vivo, requires tissue extraction (and often sectioning) |
| Primary Strength | Non-invasive functional & structural connectivity in 3D | Direct, high-resolution mapping of fiber orientation and density |
| Microstructural Validation | Infers microstructure from indirect proxies (e.g., diffusion) | Directly images fiber microstructure and directionality [69] |
The synergy is clear: 11.7T MRI can identify regions of interest in the intact brain—for example, a suspected area of altered connectivity in a neurodegenerative disease model or a tumor margin—with high precision. Subsequent ex vivo PLI analysis of the corresponding tissue region can then validate the MRI-derived metrics by directly revealing the underlying axon density, myelin integrity, and fiber orientation, including crossing fibers that are challenging for diffusion MRI to resolve [69]. This combined approach powerfully links non-invasive in vivo imaging with ex vivo microstructural truth.
Experimental Protocols for PLI Validation
Sample Preparation and Imaging
Tissue Preparation: For transmission PLI, tissue is typically fixed and cryo-sectioned or paraffin-embedded into thin sections (e.g., 5-50 µm). For backscattering PLI, which is more applicable for validating 3D structures in thicker samples, fixed bulk tissue or entire organoids can be used without sectioning [69]. The samples are mounted on standard glass slides.
Data Acquisition with a Mueller Matrix Polarimeter:
- System Setup: A backscattering polarimeter is configured with a light source (often at multiple wavelengths, e.g., from blue to red), a polarization state generator (PSG), and a polarization state analyzer (PSA) [69].
- Mueller Matrix Measurement: The PSG illuminates the sample with a sequence of known polarization states. For each state, the PSA measures the resulting polarization state of the backscattered light. This process allows for the calculation of the full 4x4 Mueller matrix (M) for each pixel in the image [69] [72].
- Multi-Wavelength Imaging: Acquiring data across different wavelengths can provide information on light penetration depth and sensitivity to specific tissue components, as hemoglobin absorption varies with wavelength [69].
- Spatial Alignment for Multimodal Studies: For direct correlation with H&E staining or other modalities, a precise registration pipeline is essential. This involves initial rigid registration followed by non-rigid registration using algorithms like B-spline modeling to account for local deformations from tissue processing [72].
Data Processing and Parameter Extraction
The raw Mueller matrix data is decomposed to extract quantitative optical parameters. The following workflow outlines the standard processing steps, with a detailed diagram presented in the next section.
Diagram 1: PLI Data Processing Workflow
Interpreting PLI Data in Disease Contexts
Quantitative Microstructural Mapping
The extracted parameter maps provide direct quantitative insights into tissue health and organization:
- Retardance and Fiber Density: In a healthy white matter tract with highly aligned, myelinated axons, retardance is strong and the fast-axis orientation map shows a uniform direction. In disease models like multiple sclerosis or traumatic brain injury, where demyelination and axonal loss occur, a significant reduction in retardance magnitude is expected [69].
- Depolarization and Tissue Heterogeneity: Healthy, ordered tissue tends to preserve polarization to a greater degree. Pathological states, such as high-grade brain tumors (glioblastoma), are characterized by cellular pleomorphism and chaotic microstructures, leading to a higher depolarization power [72]. This can help delineate tumor boundaries that are indistinct in standard H&E staining.
- Resolving Crossing Fibers: A key advantage of PLI over diffusion tensor imaging is its potential to resolve complex fiber architectures. In regions where fiber bundles cross, the retardance pattern and orientation maps exhibit distinct signatures that can be computationally decoded, providing a ground truth for validating advanced diffusion MRI tractography algorithms [69].
Correlation with 11.7T MRI Findings
Validation experiments are designed to correlate PLI metrics with 11.7T MRI contrasts.
- PLI vs. Diffusion MRI: The principal direction of the fast-axis from PLI should align with the primary eigenvector from diffusion tensor imaging (DTI) in regions of coherent fiber tracts. Discrepancies, particularly in crossing fiber regions, can be used to refine and validate biophysical models of diffusion [69].
- PLI vs. Susceptibility-Weighted Imaging (SWI): Focal areas of iron deposition, which appear as hypointensities on SWI, can be investigated with PLI to determine the impact of the iron on the local myelin integrity and cytoarchitecture.
- PLI for Organoid Validation: The application of 11.7T diffusion MRI to map the microstructure of human brain organoids is an emerging field [57]. PLI can validate these MR-derived tractography maps by directly revealing the presence and orientation of neuronal fibers and rosette-like structures within the organoid, confirming the model's physiological relevance.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 3: Key Research Reagents and Materials for PLI Validation Studies
| Item | Function & Application |
|---|---|
| Fixed Brain Tissue (e.g., Ferret, Mouse, Human) | A standard biological substrate for establishing and validating PLI protocols and correlating with MRI data. Ferret brain is noted for its gyrencephalic structure and has been used in backscattering PLI studies [69]. |
| Tissue Phantoms (e.g., Electrospun Polymer Fibers, Aligned Silk) | Well-defined anisotropic structures used to characterize the imaging system's response to fiber orientation, inclination, and crossing without the confounding variables of biological tissue [69]. |
| Mueller Matrix Polarimeter | The core instrument for full-vector polarization imaging. It measures the 16-element Mueller matrix, enabling the calculation of all derived polarization properties [69] [72]. |
| Liquid Crystals or Birefringent Plastic Film | Used for system calibration and verification of polarization state generation and analysis. |
| Spectral Filters (Multi-Wavelength Kit) | Allows for investigation of wavelength-dependent effects, which can probe structures at different depths due to varying scattering and absorption properties [69]. |
| Immunofluorescence Staining Kits (e.g., for Myelin Basic Protein, Neurofilaments) | Provides a complementary, molecularly-specific validation method. PLI fiber orientation maps can be directly compared with immunostained axonal tracts. |
| Image Registration Software (e.g., ITKMontage, with SuperPoint & B-spline algorithms) | Critical for spatially aligning PLI images with H&E-stained slides, immunohistochemistry data, and ex vivo MRI scans to enable pixel-wise correlation [72]. |
The integration of Polarized Light Imaging with ultra-high-field MRI platforms like the 11.7T scanner is poised to become a gold standard for validating microstructural changes in disease models. Future developments will focus on further optimizing backscattering PLI systems for imaging thicker, bulk tissue samples that more closely resemble in vivo conditions, thereby strengthening the bridge to MRI [69]. The creation of large, aligned multimodal datasets, such as the paired Polar-H&E dataset comprising over 13,000 images, will be crucial for developing machine learning models that can predict polarization features from conventional histology or even infer microstructural information from MRI data alone [72]. Furthermore, the use of sophisticated tissue phantoms will continue to be essential for quantifying PLI's sensitivity to fiber inclination and curvature in three dimensions [69].
In conclusion, PLI provides a powerful, direct, and quantitative method for mapping the micro-architecture of neural tissue. When framed within the context of 11.7T MRI neuroscience research, it transitions from a standalone technique to a vital validation tool that grounds the mesoscopic findings of ultra-high-field MRI in microscopic reality. This synergistic combination accelerates our understanding of neurodegenerative diseases, psychiatric disorders, and brain tumor pathology, ultimately paving the way for new biomarkers and therapeutic strategies.
The quest to visualize the intricate architecture of the brain has long relied on immunofluorescence (IF) as a gold standard for cellular and molecular characterization. While this technique provides exceptional specificity through antibody-antigen interactions, it remains inherently invasive, destructive, and limited by tissue penetration and clearing artifacts. The emergence of ultra-high field magnetic resonance imaging (MRI), particularly at 11.7 Tesla (T), now presents a revolutionary, label-free alternative for probing brain microstructure at the mesoscopic scale. This technical guide examines how 11.7T MRI data compares to traditional immunofluorescence, framing this comparison within the context of advanced neuroscience research and therapeutic development.
The fundamental advantage of 11.7T MRI lies in its ability to provide non-destructive, three-dimensional visualization of intact tissue specimens without sectioning or staining. Where immunofluorescence requires tissue fixation, sectioning, and epitope-specific labeling that may alter native structure, 11.7T MRI generates contrast through intrinsic tissue properties such as water diffusion, proton density, and magnetic susceptibility [25] [73]. This capacity for deep tissue imaging at near-histological resolution positions 11.7T MRI as a powerful correlative bridge between macroscopic in vivo observations and microscopic molecular analyses.
Technical Capabilities and Resolution Limits
11.7T MRI Resolution Achievements
The exceptional signal-to-noise ratio (SNR) at 11.7T enables resolution capabilities previously unattainable with conventional MRI systems. For human brain imaging, the Iseult 11.7T scanner has achieved in vivo resolutions of 0.19 × 0.19 × 1 mm within acquisition times of just 4-5 minutes, a feat that would require hours at clinical field strengths of 1.5T or 3T [2] [6]. For ex vivo specimens where scanning time constraints are relaxed, resolution increases dramatically. The Chenonceau dataset demonstrates exceptional 100 μm isotropic resolution for anatomical imaging and 200 μm isotropic resolution for diffusion-weighted imaging of entire ex vivo human brains [73].
In specialized applications such as brain organoid imaging, 11.7T diffusion MRI microscopy has reached isotropic resolutions of ≤40 μm, sufficient to identify rosette-like internal structures and protruding spherical formations that correlate with choroid plexus differentiation observed via immunofluorescence [25]. This level of detail enables three-dimensional characterization of organoid microstructure without the physical sectioning required for traditional histology.
Immunofluorescence Resolution and Limitations
Immunofluorescence typically provides resolution at the cellular and subcellular level, with conventional fluorescence microscopy achieving approximately 200-250 nm laterally and 500-700 nm axially. Super-resolution techniques can push this to ~20 nm, far beyond current MRI capabilities [25]. However, this exceptional resolution comes with significant trade-offs:
- Tissue processing artifacts: Fixation, embedding, and sectioning can introduce deformation and shrinkage
- Antibody penetration limits: In whole-mount preparations, antibodies typically penetrate only 50-100 μm without specialized clearing techniques
- Epitope accessibility: Masking of target antigens can prevent accurate labeling
- Signal attenuation: Depth-dependent quenching affects quantitative measurements
Tissue clearing methods such as CLARITY attempt to address these limitations but require days to weeks of processing and can still result in tissue deformation and reduced fluorescent signals [25] [74].
Table 1: Resolution and Capability Comparison of 11.7T MRI and Immunofluorescence
| Parameter | 11.7T MRI | Traditional Immunofluorescence |
|---|---|---|
| Best Resolution | 40 μm (organoids), 100 μm (ex vivo human brain) | 200 nm (conventional), 20 nm (super-resolution) |
| Tissue Penetration | Unlimited (full 3D specimens) | 50-100 μm without clearing |
| Sample Integrity | Non-destructive, preserves native structure | Destructive (requires sectioning) |
| Multiplexing Capacity | Simultaneous capture of multiple contrast mechanisms | Sequential labeling limited by spectral overlap |
| Quantitative Nature | Direct water diffusion/property measurement | Indirect via antibody affinity |
| Throughput | Moderate (minutes to hours per scan) | Slow (days for processing and staining) |
| 3D Capability | Native volumetric imaging | Sequential sectioning and reconstruction |
Experimental Protocols and Methodologies
11.7T MRI Protocol for Brain Organoids
The application of 11.7T MRI to brain organoids requires specialized sample preparation and imaging parameters to balance resolution requirements with the integrity of these delicate structures [25]:
Sample Preparation:
- Human induced pluripotent stem cell (hiPSC)-derived hippocampal brain organoids (approximately 2mm diameter)
- Fixed in 4% paraformaldehyde (PFA) for structural integrity during scanning
- Positioned in customized polyethylene tubing sample holders within a 5mm transverse solenoid radiofrequency coil
- Immersed in phosphate-buffered saline (PBS) with gadoterate meglumine to reduce tissue T1 relaxation time
MRI Acquisition Parameters:
- Magnet System: 11.7T/89 mm Bruker AV3 HD microimaging system
- Gradient Strength: 1500 mT/m maximum
- Sequence: 3D diffusion-weighted multispin-echo sequence
- Resolution: ≤40 μm isotropic
- Diffusion Encoding: Multishell acquisition with b-values = 785, 1382, and 2412 s/mm²
- Reconstruction: Diffusion tensor modeling with tractography methods
Data Analysis:
- Tensor-derived metrics including fractional anisotropy (FA) and mean diffusivity (MD)
- Tractography for modeling neuronal organization and tissue microstructure
- 3D visualization and quantitative analysis of rosette structures and regional differentiation
Immunofluorescence Protocol for Brain Organoids
To validate MRI findings, parallel immunofluorescence analysis provides molecular specificity [25]:
Tissue Preparation:
- Fixation in 4% PFA overnight at 4°C
- Cryoprotection in 30% sucrose solution
- Embedding in OCT medium and sectioning at 10μm thickness using cryostat
- Alternative whole-mount staining with extended incubation periods
Immunostaining:
- Permeabilization with 0.2% Triton X-100
- Blocking with 10% goat serum/0.2% Triton X-100
- Primary antibody incubation overnight at 4°C:
- β-tubulin III (neuronal marker, 1:200)
- FOXG1 (forebrain marker, 1:1000)
- TTR (choroid plexus marker, 1:200)
- CTIP2, TBR1, PROX1 (layer-specific markers)
- Fluorophore-conjugated secondary antibody incubation (1:300)
- Nuclear counterstaining with Hoechst 33342
Imaging and Analysis:
- Epifluorescence or confocal microscopy imaging
- Multi-channel acquisition and image registration
- Qualitative and quantitative assessment of marker expression
- Correlation with MRI-identified structures
Comparative Analysis: Structural and Connectomic Applications
Brain Organoid Characterization
In brain organoid research, 11.7T diffusion MRI microscopy has demonstrated remarkable correlation with immunofluorescence findings. The technique successfully identified rosette-like structures that mirrored the organizational patterns revealed by β-tubulin III immunofluorescence, which labels neuronal populations [25]. Furthermore, MRI-detected protruding spherical structures showed direct correspondence with choroid plexus differentiation identified through TTR (transthyretin) immunostaining.
Perhaps most significantly, diffusion tractography applied to organoid imaging was able to model tissue microstructural features and map potential neuronal organization patterns that aligned with immunofluorescence findings, all without the need for tissue clearing or physical sectioning [25]. This capacity for non-destructive 3D assessment positions 11.7T MRI as particularly valuable for longitudinal studies of organoid development and disease modeling.
Human Brain Mapping at Mesoscopic Scale
For ex vivo human brain mapping, the Chenonceau dataset demonstrates how 11.7T MRI at 100μm anatomical and 200μm diffusion resolution reveals unprecedented architectural details [73]:
- Hippocampal subregions: Clear delineation of hippocampal strata and laminae
- Cortical laminar organization: Visualization of layer-specific patterns in the cortical ribbon
- Superficial white matter: Contrast differentiation between loco-regional and deep white matter bundles
- Fiber trajectory precision: Mapping of 90° turns in thalamic radiations toward frontal lobe
These structural insights approach the level of detail traditionally requiring histological processing, while maintaining the intact 3D relationships between structures that are lost in section-based techniques.
Table 2: Multi-Modal Validation of 11.7T MRI Findings with Immunofluorescence
| 11.7T MRI Finding | Correlative Immunofluorescence Validation | Research Application |
|---|---|---|
| Rosette-like structures in organoids | β-tubulin III patterning | Organoid development modeling |
| Choroid plexus differentiation | Transthyretin (TTR) expression | Barrier tissue formation |
| Neurite organization patterns | MAP2 and GRIK4 distribution | Neuronal connectivity studies |
| Hippocampal subfield delineation | PROX1 and TBR1 layer-specific expression | Memory circuit analysis |
| Cortical laminar architecture | CTIP2 and TBR1 laminar markers | Cerebral cortex organization |
| White matter integrity | Myelin basic protein (MBP) staining | Demyelinating disease models |
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of correlative 11.7T MRI and immunofluorescence requires specialized materials and reagents:
Table 3: Essential Research Reagents and Materials
| Item | Function/Purpose | Application Context |
|---|---|---|
| hiPSC Lines | Source material for generating brain organoids | Both techniques |
| 4% Paraformaldehyde | Tissue fixation preserving structure and antigens | Both techniques |
| Gadoterate Meglumine | Contrast agent for reducing T1 relaxation time | 11.7T MRI |
| Customized Sample Holders | Secure positioning without structural deformation | 11.7T MRI |
| Primary Antibodies Panel | Cell-type and structure-specific labeling | Immunofluorescence |
| Fluorophore-Conjugated Secondaries | Signal amplification and multiplexing | Immunofluorescence |
| CLARITY Hydrogel Solutions | Tissue clearing while maintaining compatibility | Multimodal imaging |
| Cryostat | Thin sectioning for immunohistochemistry | Immunofluorescence |
| Parallel Transmission Coils | Mitigating RF field inhomogeneity at high field | 11.7T MRI |
| Multishell Diffusion Encoding | Multi-parametric microstructural characterization | 11.7T MRI |
Experimental Workflows and Signaling Pathways
The complementary nature of 11.7T MRI and immunofluorescence is best leveraged through integrated experimental workflows that capitalize on the strengths of each technique.
Advantages, Limitations, and Future Directions
Complementary Strengths and Applications
The integration of 11.7T MRI and immunofluorescence creates a powerful synergistic relationship rather than a simple replacement scenario. 11.7T MRI excels in providing comprehensive 3D structural context, identifying regions of interest for targeted molecular analysis, and enabling longitudinal assessment of dynamic processes. Immunofluorescence remains indispensable for definitive cell-type identification, subcellular localization, and validation of MRI-derived structural hypotheses.
For drug development applications, 11.7T MRI offers unique capabilities for non-destructive screening of therapeutic effects on brain organoid microstructure and connectivity, serving as a bridge between in vitro assays and in vivo models [25]. The technology shows particular promise for modeling psychiatric disorders, neurodegenerative diseases, viral infections, and assessing neurotoxicity in compound screening.
Current Limitations and Technical Challenges
Despite its impressive capabilities, 11.7T MRI faces several practical limitations:
- Infrastructure requirements: Extraordinary costs and specialized facilities needed for installation
- Sample compatibility: Challenges in positioning delicate specimens without deformation
- Acquisition times: Extended scanning requirements for highest resolutions
- Contrast interpretation: Complex relationship between image contrast and underlying biology
Immunofluorescence, while providing unparalleled specificity, remains limited by:
- Destructive nature: Precludes longitudinal study of same sample
- Throughput constraints: Labor-intensive processing and analysis
- Volume limitations: Challenges in achieving uniform labeling in thick specimens
Future Perspectives in Ultra-High Field Neuroimaging
The rapid advancement of 11.7T MRI technology promises even greater integration with molecular imaging approaches. Future developments include:
- Enhanced contrast mechanisms: Improved differentiation of subtle microstructural features
- Higher throughput acquisitions: Reduced scan times through sequence optimization
- Multinuclear capabilities: Imaging of metabolic processes via nuclei such as 23Na and 31P
- Standardized correlative protocols: Streamlined workflows for combined MRI-IF analysis
- Clinical translation: Potential for human in vivo applications as safety is established [2] [6]
The comparison between 11.7T MRI and traditional immunofluorescence reveals not a competition for "gold standard" status, but rather a powerful partnership for comprehensive brain exploration. While immunofluorescence maintains its essential role in molecular identification and validation, 11.7T MRI establishes a new paradigm for non-destructive, three-dimensional structural analysis at the mesoscopic scale. For neuroscience researchers and drug development professionals, the integration of these technologies provides an unprecedented window into brain organization, connectivity, and pathology—enabling discoveries that neither approach could achieve in isolation. As ultra-high field MRI continues to evolve, its correlation with established molecular techniques will remain fundamental to extracting biologically meaningful insights from its extraordinary imaging capabilities.
Conclusion
The deployment of 11.7T Ultra-High Field MRI represents a paradigm shift in neuroscience research, providing a powerful 'mesoscope' that bridges the critical gap between macroscopic human imaging and microscopic cellular analysis. The technology has proven its value by revealing previously inaccessible details of brain microstructure and offering new contrast mechanisms for studying neurological and psychiatric disorders. While significant challenges related to cost, infrastructure, and technical optimization remain, the ongoing validation of its findings against histological gold standards builds a compelling case for its scientific rigor. Future directions will focus on integrating motion correction, developing more efficient RF coils, and leveraging higher channel counts to further push the boundaries of resolution for functional and diffusion MRI. For the drug development community, 11.7T MRI promises to deliver sensitive, non-invasive biomarkers for earlier disease detection and more precise monitoring of therapeutic efficacy, ultimately accelerating the journey from foundational research to clinical impact.
References
- 1. ULTRAHIGH FIELD and ULTRAHIGH RESOLUTION fMRI - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8112570/]
- 2. In vivo imaging of the human brain with the Iseult 11.7-T ... [https://www.nature.com/articles/s41592-024-02472-7]
- 3. A world premiere: the living brain imaged with unrivaled ... - CEA [https://www.cea.fr/english/Pages/News/world-premiere-living-brain-imaged-with-unrivaled-clarity-thanks-to-world-most-powerful-MRI-machine.aspx]
- 4. Commissioning of the Iseult CEA 11.7 T whole-body MRI [https://link.springer.com/article/10.1007/s10334-023-01063-5]
- 5. 11.7 Tesla: First images from the world's most powerful MRI ... [https://healthcare-in-europe.com/en/news/11-7-tesla-first-images-world-most-powerful-mri-scanner.html]
- 6. The Magnetic Power of the Future: The Iseult CEA 11.7 T ... [https://currents.neurocriticalcare.org/Leading-Insights/Article/the-magnetic-power-of-the-future-the-iseult-cea-117-t-mri]
- 7. Pros and cons of ultra-high-field MRI/MRS for human ... [https://www.sciencedirect.com/science/article/pii/S007965651830013X]
- 8. CEST perspectives for human brain applications at 11.7 T [https://archive.ismrm.org/2025/2020.html]
- 9. Ultra-High to Ultra-Low: MRI Goes to Extremes [https://www.embs.org/pulse/articles/ultra-high-to-ultra-low-mri-goes-to-extremes/]
- 10. Commissioning of the Iseult CEA 11.7 T whole-body MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC10140097/]
- 11. The Iseult 11.7 T Whole Body Magnet & MRI Research [https://ieeecsc.org/presentation/plenary/quest-ultra-high-fields-brain-mri-iseult-117-t-whole-body-magnet-mri-research]
- 12. Ultra-High-Field MR Neuroimaging - PMC - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC4472608/]
- 13. Ultra-high field for fast imaging of the human brain at ... [https://communities.springernature.com/posts/ultra-high-field-for-fast-imaging-of-the-human-brain-at-mesoscale-resolution]
- 14. 11.7T Diffusion Magnetic Resonance Imaging and ... - PubMed [https://pubmed.ncbi.nlm.nih.gov/39099731/]
- 15. Next-generation MRI scanner designed for ultra-high ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10703687/]
- 16. Color-coded visualization of magnetic resonance imaging ... [https://www.nature.com/articles/srep41107]
- 17. Automated Color-Coding of Lesion Changes in Contrast ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8985679/]
- 18. Safety of Ultra-High Field MRI: What are the Specific Risks? [https://link.springer.com/article/10.1007/s40134-014-0061-0]
- 19. 7 Tesla and Beyond: Advanced Methods and Clinical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8505159/]
- 20. Next-generation MRI scanner designed for ultra-high ... [https://www.nature.com/articles/s41592-023-02068-7]
- 21. Ultra-high gradient connectomics and microstructure MRI ... [https://www.nature.com/articles/s41551-025-01457-x]
- 22. Integrating Biomarkers, Neuroinflammation, and Imaging in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12109388/]
- 23. The Global Neurodegeneration Proteomics Consortium [https://www.nature.com/articles/s41591-025-03834-0]
- 24. Imaging the Human Brain With Ultra-Powerful MRI [https://www.pcrm.org/news/innovative-science/imaging-human-brain-ultra-powerful-mri]
- 25. 11.7T Diffusion Magnetic Resonance Imaging and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11295450/]
- 26. Quantitative assessment of brain metabolism in mice using ... [https://www.sciencedirect.com/science/article/pii/S2215016125000238]
- 27. Integrative Magnetic Resonance Imaging and Metabolomic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11118082/]
- 28. Exploring the Impact of Irradiation on Glioblastoma Blood ... [https://www.mdpi.com/2227-9059/12/5/1091]
- 29. Post-mortem 11.7T DTI Validation of Myeloarchitectural ... [https://www.sciencedirect.com/science/article/pii/S0361923025003387]
- 30. Post-mortem 11.7 T DTI validation of myeloarchitectural ... [https://pubmed.ncbi.nlm.nih.gov/40885452/]
- 31. Ex vivo MR spectroscopic measure differentiates tumor ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3098023/]
- 32. Ultrahigh-field imaging (7 Tesla) in DNET [https://pmc.ncbi.nlm.nih.gov/articles/PMC11867227/]
- 33. Submillimeter Ultra-High Field 9.4 T Brain MR Image ... [https://www.nature.com/articles/s41597-025-04779-2]
- 34. Emerging methods and applications of ultra-high field MR ... [https://www.sciencedirect.com/science/article/pii/S0003269721003808]
- 35. Pushing boundaries with ultra-high field MRI [https://www.frontiersin.org/research-topics/69609/pushing-boundaries-with-ultra-high-field-mri-innovations-and-applications-in-neuroscience]
- 36. Role of functional magnetic resonance imaging in drug ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2841045/]
- 37. Germany's journey toward 14 Tesla human magnetic resonance [https://pmc.ncbi.nlm.nih.gov/articles/PMC10140098/]
- 38. Multinuclear Magnetic Resonance Spectroscopy at Ultra-High ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10143499/]
- 39. Metabolic and vascular imaging markers for investigating ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11449888/]
- 40. MRI with ultrahigh field strength and high-performance gradients [https://pmc.ncbi.nlm.nih.gov/articles/PMC8387544/]
- 41. Metabolic brain imaging with glucosamine CEST MRI [https://www.nature.com/articles/s41598-023-48515-5]
- 42. Design and Optimization of Transmit Arrays for MRI at 11.7T [https://cds.ismrm.org/protected/22MProceedings/PDFfiles/0706.html]
- 43. A Preliminary Study for Reference RF Coil at 11.7 T MRI [https://pmc.ncbi.nlm.nih.gov/articles/PMC8875900/]
- 44. Ultrahigh field MR Neuroimaging - PMC - PubMed Central - NIH [https://pmc.ncbi.nlm.nih.gov/articles/PMC6784841/]
- 45. Evaluation of Software‐Optimized Protocols for Acoustic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12276638/]
- 46. Overview of Methods for Noise and Heat Reduction in MRI ... [https://www.frontiersin.org/journals/physics/articles/10.3389/fphy.2022.907619/full]
- 47. Model gradient coil employing active acoustic control for MRI [https://link.springer.com/article/10.1007/s10334-007-0086-y]
- 48. Tips To Reduce MRI Noise And Vibration In Healthcare ... [https://www.acentech.com/resources/tips-to-reduce-mri-noise-and-vibration-in-healthcare-environments/]
- 49. Superconductivity and Cryogenics in Medical Diagnostics ... [https://www.mdpi.com/2076-3417/15/23/12579]
- 50. Ultra-low-field MRI: a David versus Goliath challenge in ... [https://link.springer.com/article/10.1007/s11547-025-02091-y]
- 51. Scaling the mountains: what lies above 7 Tesla magnetic ... [https://link.springer.com/article/10.1007/s10334-023-01087-x]
- 52. Powering MRIs: 3 RF Interconnect Tips [https://timesmicrowave.com/powering-mris-3-rf-interconnect-considerations-to-save-time-and-money/]
- 53. Field switching of microfabricated metamagnetic FeRh MRI ... [https://www.nature.com/articles/s41598-025-85384-6]
- 54. Better neural images by combining ultrahigh field strength MRI ... [https://www.neuroscigroup.us/articles/JNNSD-8-147.php]
- 55. A Preliminary Study for Reference RF Coil at 11.7 T MRI [https://www.mdpi.com/1424-8220/22/4/1512]
- 56. Optimization of phase-contrast MRI for the estimation of global ... [https://pubmed.ncbi.nlm.nih.gov/30393888/]
- 57. 11.7T Diffusion Magnetic Resonance Imaging and ... [https://www.sciencedirect.com/science/article/pii/S2667174324000570]
- 58. Ultra-High-Field MRI in the Diagnosis and Management of ... [https://www.frontiersin.org/journals/neurology/articles/10.3389/fneur.2022.857825/full]
- 59. The future of ultra-high field MRI and fMRI for study of the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3389184/]
- 60. ISMRM24 - Ultra-Challenging Ultra-High Field Applications [https://www.ismrm.org/24/pf/O-54.htm]
- 61. Multimodal precision MRI of the individual human brain at ... [https://www.nature.com/articles/s41597-025-04863-7]
- 62. Signal-to-Noise Ratio (SNR) in MRI | Factors affecting SNR [https://mrimaster.com/snr/]
- 63. Low Versus Ultra-High Field MRI: How to Select Your ... [https://appliedradiology.com/articles/low-versus-ultra-high-field-mri-how-to-select-your-mri-fleet]
- 64. How to Implement Clinical 7T MRI—Practical Considerations ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11673481/]
- 65. Next-generation MRI scanner designed for ultra-high ... [https://pubmed.ncbi.nlm.nih.gov/38012321/]
- 66. The World’s Most Powerful MRI Machine Just Took Some Stunning Images | IFLScience [https://www.iflscience.com/the-worlds-most-powerful-mri-machine-just-took-some-stunning-images-73692]
- 67. Clinical 7 Tesla magnetic resonance imaging - PubMed Central [https://pmc.ncbi.nlm.nih.gov/articles/PMC11846079/]
- 68. The most powerful MRI scanner in the world delivers its first ... [https://www.cea.fr/english/Pages/News/premieres-images-irm-iseult-2021.aspx]
- 69. Evaluating backscattering polarized light imaging ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10704260/]
- 70. A Guide to Polarized Light Microscopy | Learn & Share [https://www.leica-microsystems.com/science-lab/industrial/a-guide-to-polarized-light-microscopy/]
- 71. Polarized Light Microscopy [https://www.microscopyu.com/techniques/polarized-light/polarized-light-microscopy]
- 72. Unlocking Pathological Insights with Polarization Imaging [https://arxiv.org/html/2503.05933v2]
- 73. an entire ex vivo human brain 11.7T anatomical and ... [https://cds.ismrm.org/protected/21MProceedings/PDFfiles/0214.html]
- 74. Diffusion tensor imaging measures of white matter ... [https://www.sciencedirect.com/science/article/pii/S235234091630779X]